Sophie Mitchell YE AR 13
UNDERFUNDING
NHS
COVID-19'S UNFLATTERING MIRROR
T
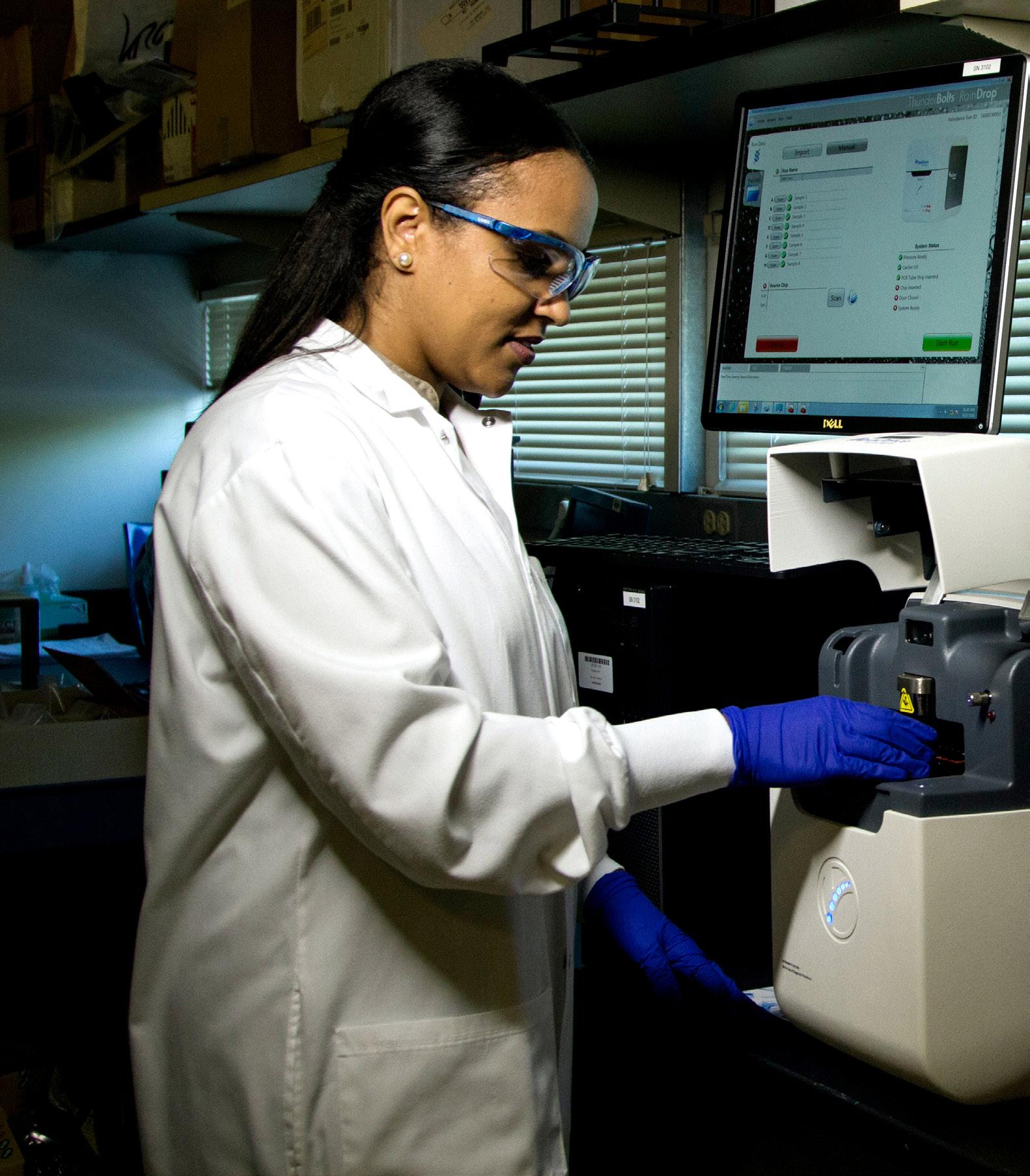
he NHS has been at the forefront of media coverage throughout the Covid-19 pandemic. For once, its funding is not being cut nor is the NHS at the forefront of a political campaign. It is rather the focus of universal national support, with every Thursday being dedicated to ‘Clap for our NHS and Carers.’ We of course admire those individuals on the front line, risking their lives to save others. But, despite all of this positivity and public support, there has been considerable concern at negative issues such as lack of PPE and ventilators at the outset (leaving NHS staff and patients vulnerable), consistent issues relating to testing and, of course, the very high death-rate in nursing/care homes. The structure of the NHS in England and Wales was established by the National Health Service Act 1946. The Act implemented a system where each person would be assigned to a specific general practitioner, allowing them to access further support from the system. It also relied on the introduction of National Insurance in 1912, ensuring that everyone would have access to all medical, dental and nursing care without needing to pay for it at the time. However, it was not as popular as first imagined. So much so that the BMA (British Medical Association) decided not to join in 1948. However, they were quickly convinced after they were offered a lucrative payment structure for consultants and the NHS was established on the 5th of July 1948. Now, however, the NHS faces a new threat. Since SARS-CoV-2 (COVID 19) became a global pandemic, the NHS is now more needed than ever. We have seen ICUs overrun with patients needing round the clock care, some even needing mechanical ventilation and sedation. Unfortunately, many of those who enter intensive care never recover. Our own Prime Minister, Boris Johnson, was treated on an ICU ward. A&Es have had to expand RESUS capacity to children’s units, and paediatric respiratory specialists have been retrained to work with adults. Furthermore, we are now seeing members of the public, an NHS volunteer task force, supporting the community to ensure our hospital resources can remain available to all. However, there are some elements of our healthcare system that are struggling through no fault of their own. We have seen hospitals and care settings with a lack of PPE, meaning doctors, nurses and other health care workers have been put at risk. Despite constant assertions from our government that we have enough
52
P O RT S M O U T H P O I N T. B LO G S P OT.CO M
PPE and they are doing all they can to access more, we are still seeing problems with supply several months since the pandemic began. As of late May it is reported that scores of NHS staff have died as a result of working on the front line (not including staff from care homes, delivery workers, transport workers and other essential staff). But others, including retired staff who returned to work within the NHS, have also died. These people have given their lives to save others. Their names are listed at the end of this article. Their sacrifice shall be remembered. But surely this is an unflattering reflection of our NHS? That we had to ask retired staff to return to ensure staffing levels were high enough to save lives. That we had to ask fashion designers to make PPE to ensure levels were high enough. That we had to ask F1 manufacturers and hoover makers to supply us with enough ventilators to support as many as we could. The funding has been cut year on year; the budget for public health services is now £850 million lower than in 2015/16 and by 2021, the budget will have been cut by 25% from its 2015/16 level in real terms. At the end of 2018, £1bn of cuts to public health services and the training of nurses and doctors over the following year were concealed within Government plans to boost the NHS budget by £20bn by 2023. It is the poorest communities that are being hit the hardest by these cuts. Hopefully, after this crisis is over, we will see the newfound respect for our NHS continued, with further support and funding to improve a service at the forefront of saving lives. Hopefully, our own Prime Minister will see that the NHS is not a commodity to use in political warfare. All being well, people will learn to respect our health service, using A&E when they need to rather than turning up with alcohol-inflicted injuries for example. The NHS has never been so important. Our health service is at the forefront of everyone’s minds as are those who go to work every day and risk their lives for others. Yes, the Covid-19 pandemic has held up an unflattering mirror to the NHS’ lack of funding; however, it has also proved a reflection on a country that can pull together to support each other in a time of crisis. We, as a nation, have progressed and it’s fair to say life will never be the same again. We have come out on the other side stronger; let us hope (and insist) that the NHS will benefit in future budgets.