8 minute read
What Healthcare Can Learn from Aviation Shapol Mohamed
Shapol Mohamed YEAR 13
WHAT healthcare CAN LEARN FROM
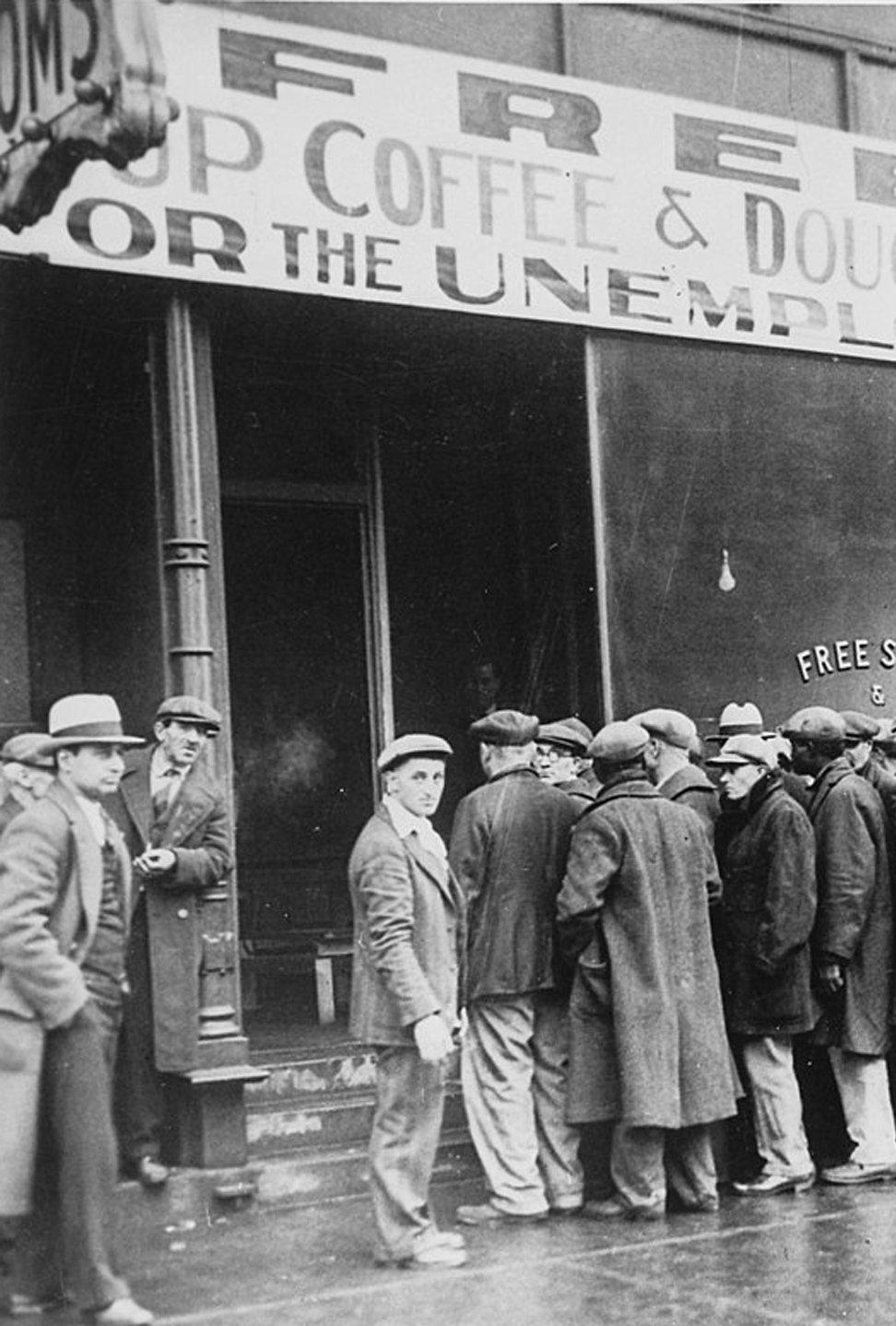
One of the most and wife to Martin, has had a BBC significant causes documentary produced about her. One of death in the morning she was due at the hospital to world is also have her sinus problem treated. The one of the most doctor had told her the chances of overlooked. It is complications were tiny and they had not malaria, HIV, done the same procedure countless times. or COVID-19, but medical errors. At 8:35 Elaine was in the operating
According to the World Health theatre and for the anaesthesia to be Organisation, four in ten patients are delivered had a cannula, a straw-shaped harmed in primary care, such as at GPs, tube, inserted into the back of her hand. and 80% of those cases are preventable. Anaesthetics are strong drugs that disable Meanwhile, in hospitals, one in ten patients many of the patient’s vital functions, and are harmed. Globally, this breathing is usually assisted causes 2.6 million deaths. by an inflatable pouch that For comparison, annually THE RELUCTANCE is inserted into the mouth malaria and HIV cause OF THE and sits just above the 405,000 and 770,000 deaths, HEALTHCARE airways. The oxygen is respectively. Coronavirus SECTOR TO MAKE then pumped in artificially. has caused 350,000 deaths ERRORS MORE In Elaine’s case, there at the time of writing this. TRANSPARENT was a problem; her jaws Medical errors do not HAS SLOWED had tightened whilst she discriminate between rich PROGRESS. was, essentially, in a deep and poor countries - both sleep and the mask was are affected equally. Clearly, unable to be inserted into this is a significant problem that needs her mouth. Of course, that had happened to be tackled and I think we can reduce plenty of times before and the surgeons that number by introducing a few simple were ready to try with smaller masks. At measures. 8:37, she was beginning to turn blue and
Now, you might be giving me the look her oxygen levels were 75%. that a parent gives a toddler searching Meanwhile, Martin and the kids were the dog’s mouth for the thing that makes buying the cookies that Mum always the barking noise. It’s a cute idea but liked, so they could give them to her in idiotic. You might be saying: how can the afternoon. you do that? Doctors don’t kill patients Back in the operating theatre, the on purpose. Of course, they don’t - medics tried another type of mask to sit healthcare professionals have the purest over the mouth and nose; it still didn’t intentions to help. work. This wasn’t anything too unusual.
Elaine, mother to Victoria and Adam Following standard protocol, at 8:41 a paralysing agent was injected to disable her jaw completely so that her mouth was now fully open. A light was shone in the back of her mouth so the tube could be inserted directly into her airway; this was normally visible, a hole with the vocal cords on either side, but in this case they were hidden by the mouth’s soft palate. The situation was becoming critical. The surgeon kept jabbing the tube, hoping that he would find the airways. At 8:43, at 40%, the oxygen levels were so low that they were troublesome to measure; Elaine’s heart rate fell to 69 then to 50, meaning there was little oxygen getting to the heart. The problem with low oxygen levels is that your brain starts to swell; that can prove fatal.
Thankfully, in this situation, there is one last option that surgeons can turn to: tracheostomy, whereby an incision is made directly into the throat and the tube is inserted directly into the windpipe, completely bypassing the mouth. As you can imagine, this is risky but it is the last resort.
Twelve minutes in, the nurse prepared the tracheostomy kit and notified the surgeons. The surgeons, under pressure, ignored the nurse. Time was passing and the nurse thought perhaps the surgeons had already thought about that option but ruled it out for a reason that she was unaware of. Elaine was now deep blue and her heart rate was a meagre 40 beats per minute. Every second wasted narrowed her chances of survival. The surgeons continued their increasingly frantic attempts to force in the tube while the nurse continued to agonise over whether to speak up.
It took 20 minutes for the surgeons to bring Elaine’s oxygen levels back up to 90% and by then it was already too late. Later, an MRI scan was taken of her brain and it showed irreparable brain damage at best.
At 11 am, Martin got a call telling him to get to the hospital as soon as possible. Knowing something was wrong, he left the kids at home, with the cookies they had baked for their Mum. The surgeons had said it was a routine operation with very low chances of complication. Elaine was young and healthy. Martin couldn’t figure
out what could possibly have gone wrong.
He arrived at the hospital and found Elaine in a coma. Thirteen days later, he brought his children to see their mother for the last time. Elaine was one of those 2.6 million preventable casualties that occur annually due to medical errors.
Now, of course, all the healthcare professionals were under pressure. However, one cannot understand why an investigation was not carried out. An investigation only occurred after years of campaigning by Martin. This is the problem. There is a lack of investigations within the healthcare sector when something goes wrong; as a result, learning from failure is rare.
During lockdown, I have read two books, The Checklist Manifesto by Atul Gawande, a world-renowned surgeon, and Black Box Thinking by Matthew Syed, an Oxford PPE graduate, Olympian, columnist, sports commentator and overall great guy. Gawande’s book talks about problems faced by surgeons; Syed’s explains how we could all benefit from a personal black box, just like aircraft. The two books combined could portray a solution.
The fact that the healthcare sector has been reluctant to make errors more transparent has slowed progress. Galen was a hugely influential surgeon not only during his lifetime in the 2nd century CE but for many centuries afterwards through
his writings; his teaching must have killed a plethora of patients. For example, he was a strong advocate of bloodletting; if a patient survived, the physicians would say “Oh my! Bloodletting is so effective! It saved the patient’s life!” And if the patient died, they would say “The patient was so weak that even bloodletting couldn’t save them.” Now, this may seem like an insane idea to us in the twenty-first century, but his teaching survived for 1,300 years, until the late fifteenth century. The reason why Galen remained influential for so long is that his theories were never subjected to proper investigation or tests.
As previously noted, surgeons do work under immense pressure and within severe time constraints - so do airline pilots. When an aircraft crashes, it dominates newspaper headlines. Investigations take place to find out the root cause of the catastrophe. Documentaries are made about it. Politicians hold press conferences. A profusion of articles are posted online. There is often a huge public outcry. Major incidents often take an aircraft manufacturer to the brink of collapsing, as seen with Boeing. As a result, the industry is careful to reflect on failures and learn from them; key to this process is the black box. Black box thinking has allowed the aerospace industry to perfect their engineering works of beauty. As a result, aircraft are poetry in motion. They have done such a good job that the chances of dying in an plane crash are 1 in 11 million, significantly better than the 1 in 10 chance of dying due to a medical error, according to John Hopkins University. If medical errors were investigated more transparently and actions were taken to reduce those same errors from occurring in the future, then they would become far less prevalent.
A straightforward method used by pilots to make sure they have done everything correctly is the checklist. For example, checklists enabled Chesley Sullenberger in 2008 to safely land US Airways Flight 1549 in the Hudson River to prevent the aircraft from crashing into Manhattan. As a result, no lives were lost. A similar approach could help reduce medical error; indeed, checklists have been adopted in many hospitals across the world and have saved many lives as a result. According to a study by Harvard, nearly 20% of medical errors are due to infection. This could be easily prevented by making sure that healthcare professionals have given antibiotics to patients before an incision is made in the patient during surgery. This step can be missed very easily when surgeons and nurses are working under pressure. A checklist can help with that, as Atul Gawande explains in his book. Checklists could have also helped Elaine if the surgeons had followed a checklist that reminded them of the option of tracheostomy.
Atul Gawande has been working with the World Health Organisation for some time now to have this very simple and easy procedure implemented globally, while Matthew Syed has been advocating more transparency so that we can learn from medical errors rather than brush them under the carpet. It is important that the medical profession, like the airline industry, remove the stigma around failure and look at medical errors as an opportunity for us to save lives in the future.