Radiology News Radiology News


p. 20
p. 4
p. 14
p. 34
p. 46
p. 48
p. 23




p. 20
p. 4
p. 14
p. 34
p. 46
p. 48
p. 23

Concerts on the Memorial Union Terrace. Leisurely bike rides around Lake Monona. Fresh, spicy cheese bread from the farmers’ market.
There’s a lot to love about summer. Welcoming new people to our department ranks high on my list!
In addition to the new residents and fellows eager to learn, 15 faculty members joined us since our January newsletter. There are also new faces on our leadership teams. Some like Vice Chair of Practice Transformation and Center for High Value Imaging Director Dania Daye, MD, PhD and Vice Chair of Research Christoph Lee, MD, MS, MBA have come from the two coasts. Others like Vice Chair of Clinical Operations Gregory Avey, MD and Director of Fellowships Kelly Capel, MD have been with us since their training.
While people are, by far, our most precious resource, we also need to invest in our equipment and buildings to ensure continued high-quality care. For this reason, I am pleased to share that UW Health has approved initial funding of a seven-year scanner replacement plan, which front loads critical replacements into the first three years.
Construction is also well underway to add a 27-bed prep and recovery space at the University Hospital and expand the Emergency Department’s radiology capacity at East Madison Hospital. With the increase in hard hat areas, many of us, including myself, have made a new home at “800 Ubay”, the of fices in suites 205 and 210 on 800 University Bay Drive that are just a short walk from the University Hospital. Come over and visit sometime!
Finally, I wanted to express my continuing gratitude for all the diligent and thoughtful work of everyone in our department. It because of your contributions that we continue to thrive even in the face of national and local challenges. I’m grateful to be part of this impactful time of our history!
On, Wisconsin!
Scott Reeder, MD, PhD

Our fellows are off to practice across the country - including right here in our department! We wish all of them well!
Abdominal Imaging and Intervention
Jacob Anderson, MD: Private Practice, Madison Radiologists
Alex McDonald, MD: Private Practice, Baptist Health Louisville in Louisville, KY
Troy Tenbrunsel, MD: Academic Practice, UW–Madison (Community Division)
Breast Imaging and Intervention
Kayla Berigan, MD: Private Practice, Grand Traverse in Traverse City, MI
Lewis Jordan, MD, MPH, MS: Academic Practice, UW–Madison (Breast Imaging & Intervention)
Carrie Anne Orlikowski, MD, JD: Academic Practice, University of North Carolina at Chapel Hill
Cardiothoracic Imaging
Saralyn Beckius, MD: Private Practice, Advanced Radiology Services in Grand Rapids, MI
Thekla H. Oechtering, MD, PD Dr med: Academic Practice, UW–Madison (Cardiovascular Imaging)
Taylor Sellers, MD: Academic Practice, UW–Madison (Thoracic Imaging)
MRI
Aishwariya Vegunta, MD: Private Practice, Sanford Health in Sioux Falls, SD
PET-CT/Molecular Imaging
Tomas Romero, MD: Academic Practice, UW–Madison (Nuclear Medicine & Molecular Imaging)

and graduating

Musculoskeletal Imaging and Intervention
Afshin Ameri, MD: Private Practice, Rhode Island Medical Imaging
Brody Brisk, MD: Private Practice, Dakota Radiology in Rapid City, SD
Alex Cook, DO: Private Practice, West County Radiological Group in Saint Louis, MO
Andrew Liu, MD: Private Practice, Minneapolis Radiology Associates
Adam Miller, MD: Academic Practice, University of Southern California, Los Angeles
Neuroradiology
Garrick Biddle, MD: Private Practice, Sutter Medical Group in Sacramento, CA
Turner Daines, DO: Private Practice, Eastern Radiology Associates in Billings, MT
James Newton, MD: Private Practice, Advanced Radiology Services in Grand Rapids, MI
Isaiah Tan, MD: Academic Practice, UW–Madison (Community)
Mohamed Shaif Yusufishaq, MD: Private Practice, Aurora Health Care in Southeast Wisconsin

Graduating Diagnostic Radiology residents Cory Pierson, Alexander Moeller, Matthew Elissa, Kevin McDonald, Benjamin Prout, Erik Winterholler, Alexander Graves, Cullen Fleming, Rasheed Nawaz, and Allison Couillard at the graduation ceremony.
Faculty, family and friends celebrated graduating residents and wished them success in future endeavors.
Diagnostic Radiology
Allison Couillard, MD: Interventional Radiology Independent Residency, UW Hospitals and Clinics
Matthew Elissa, MD: Abdominal Imaging & Intervention Fellowship, UW Hospitals & Clinics
Cullen Fleming, MD: Neuroradiology Fellowship, University of California, San Francisco
Alexander Graves, MD: Private Practice, Avera in Sioux Falls, SD
Kevin McDonald, MD: Cardiothoracic Imaging Fellowship, UW Hospitals & Clinics
Alexander Moeller, MD: Abdominal Imaging & Intervention Fellowship, UW Hospitals and Clinics
Rasheed Nawaz, MD: Neuroradiology Fellowship, UW Hospitals and Clinics
Cory Pierson, MD: Neuroradiology Fellowship, UW Hospitals and Clinics
Benjamin Prout, MD: Abdominal Imaging & Intervention Fellowship, UW Hospitals & Clinics
John (Erik) Winterholler, MD: Abdominal Imaging & Intervention Fellowship, UW Hospitals & Clinics
Interventional Radiology
Irfan Hassan, MBBS: Private Practice, Wichita Radiological Group in Wichita, KS
Elliott Russell, MD: Academic Practice, UW Hospitals and Clinics (Interventional Radiology)

Interventional Radiology Program Director Mark

graduating




Matthew Elissa, MD
UW Hospitals and Clinics


David Turner, MD University of Kentucky

Austin Webs, DO University of Minnesota
Sarah LaPierre, MD University of Connecticut
Alexander Moeller, MD
UW Hospitals and Clinics
John (Erik) Winterholler, MD
UW Hospitals and Clinics

Hannah Hodges, DO University of New Mexico

Jared Katchen, MD Fort Leonard Wood

Kevin McDonald, MD
UW Hospitals and Clinics
Benjamin Prout, MD
UW Hospitals and Clinics

Amy Shah, MD Case Western MetroHealth

Andrew Moore, MD
University of Kansas

Kaitlin Robling, MD
Rush University



Aaron Cronican, MD
HCA Sunrise Health GME Consortium


Lisa Park, MD
Mather Hospital - Northwell Health

Rasheed Nawaz, MD UW Hospitals and Clinics
Brendan Franz, MD
Henry Ford Hospital
Osvaldo Velez-Martinez, MD
University Hospitals Cleveland Medical Center


Luis Ortiz-Figueroa, MD Penn State Health Medical Center

Cory Pierson, MD UW Hospitals and Clinics

Andrew Healey, DO Madigan Army Medical Center

Nolan Shen, DO University of Minnesota
Brantley Grimball, MD
Memorial Health University Medical Center

Cameron Kendall, MD Naval Medical Center




Jacob Guest, MD
Rush Medical College of Rush University Medical Center


Lauren Penn, MD
UW School of Medicine and Public Health
Tanner Redlin, MD
University of South Dakota, Sanford School of Medicine

Olivia Meier, MD
Rush Medical College of Rush University Medical Center
Antonio Lopez, MD
Drexel University College of Medicine

Anita Rong, MD
Wake Forest University School of Medicine

Alyssa Wohlfahrt, MD
Tufts University School of Medicine
Joshua Martens, MD
UW School of Medicine and Public Health

Benjamin Weber, MD
UW School of Medicine and Public Health
Eduardo Miranda Mora, MD
UW School of Medicine and Public Health

Benjamin Yeske, MD
UW School of Medicine and Public Health

Chamil Jinadasa, MD
Faculty of Medicine of the University of Colombo

There’s no denying that residency can be an overwhelming time. One of the great benefits of training at the University of Wisconsin Department of Radiology is the Resident Wellness Committee, run by residents, for residents.
When he began his residency in 2021, Cullen Fleming, MD could tell that the COVID-19 pandemic had taken a toll on the resident culture, and he sought to lift everyone’s spirits. Because radiologists often work collaboratively, Dr. Fleming established weekly interdepartmental volleyball events, which transitioned to social events in colder months. Several months into organizing these events, he of ficially joined the Resident Wellness Committee, eventually becoming the team lead.
The committee has made great strides under Dr. Fleming’s leadership over the years, establishing fun annual events including a cutest pet or plant contest, fall food drive, Halloween costume competition, a half-day wellness outing and more. Throughout the year, smaller social events are regularly held.
Dr. Fleming encourages other trainees to help lead activities.
Madeline Jentink, DO organizes a resident book club that meets about once a month at different coffee shops in the Madison area. Books are recommended and voted on by members, and span across genres.
Moving forward, Emily Kruger, MD will lead the committee after Dr. Fleming departs to begin his fellowship training. She initially joined
to get to know upper-level residents when she started her residency. Dr. Kruger has been helping plan activities for the past two years and started the tradition of giving each resident a ‘birthday bag.’
Her favorite committee activities include the cutest pet or plant contest, and the welcome week events to get to know the incoming residents. She’s excited to work with residents to see what events everyone is interested in for the upcoming year and is planning to incorporate family-friendly activities as many of the residents have young children.




On Saturday, May 3, department members and alumni came together at the annual Zachary Clark Radiology Research Symposium to celebrate the outstanding research our trainees and medical students conduct over the year.
After a light breakfast and social hour, Department Chair Scott Reeder, MD, PhD welcomed attendees. During his opening remarks, Dr. Reeder shared that he considered the theme word for the event to be ‘curiosity’ – a fitting choice as at its core, research is fundamentally driven by curiosity.
This year, fellows, residents and medical students delivered 10 oral presentations and exhibited 17 electronic abstracts on diverse topics, including the application of artificial intelligence (AI), which has seen rapid expansion and adoption in the larger field of radiology. Moderators Allison Grayev, MD and Giuseppe Toia, MD introduced each oral presenter and passed the mic for audience questions.
Following an intermission to view electronic exhibits, Dania Daye, MD, PhD delivered the keynote address “From Innovation to Operation: Leading Through High Value Imaging.” Dr. Daye, who recently joined the faculty as an associate professor in the Section of Interventional Radiology, also serves as director of the Center for High Value Imaging and vice chair of practice transformation.
In her address, Dr. Daye shared her vision for the newly formed Center for High Value Imaging, highlighting MRI as a case study
for how the department is improving patient care at Eastpark Medical Center through quicker exam and turnaround times.
The symposium concluded with the presentation of awards for best oral presentations and electronic exhibits. Oral presentations were judged by Prashant Nagpal, MD; Matthew Smith, MD, PhD; and Timothy Ziemlewicz, MD while Teresa Chapman, MD; Leslie Nelson, DO; and Andrew Ross, MD, MPH served as the electronic exhibit judges.
Best Oral Presentation by Fellow: Adam Miller, MD
Best Oral Presentation by Resident: Anna Marie Sorensen, MD
Best Oral Presentation by Medical Student: Hassan Rizvi
Best Electronic Presentation by Fellow: Alexander McDonald, MD
Best Electronic Presentation by Resident: German Banez Rueda, MD
Best Electronic Presentation by Medical Student: Alankrit Shatadal








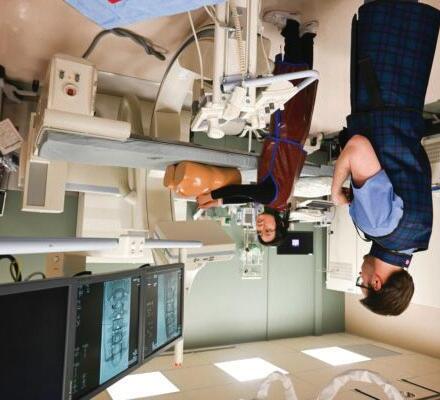
On April 3, 2025, the UW Department of Radiology hosted No Scalpel, No Problem, a hands-on workshop for medical students. Hosted in partnership with the UW School of Medicine and Public Health’s Radiology Interest Group (RIG) and Interventional Radiology Interest Group (IRIG), the event was led by Jade Anderson, MD and Sean Golden, MD. The evening gave students experience with the technique-based side of radiology.
“This event was inspired by a desire to bridge the gap from what medical students typically learn about radiology—mostly image interpretation—and the highly procedural, hands-on aspects of the field,” said Dr. Anderson. “We wanted to expose students to the active, patient-facing, decision-making side of diagnostic radiology.”
Over 30 students attended the event and were broken into three groups so they could rotate through three sessions, which were interventional radiology, breast and body ultrasound intervention, and spine imaging. Within each session, stations were set up to focus on an individual procedure. Department faculty and trainees guided students through each station, offering real-time instruction and insight into their day-to-day practices.
Led by Dr. Golden, the interventional radiology session showcased complex image-guided vascular and non-vascular procedures. Students performed a mock artery embolization using an endovascular simulator at one station.
Another station demonstrated cryoablation, a minimally invasive medical procedure in which extreme cold can be used to freeze diseased tissue, such as malignant tumors. Students saw how the process works with a tank of clear gel that had several cryoprobes in place. The demonstrators activated the cryoablation system, causing the cryoprobes to cool and form small ice balls at the ends.
Additionally, students participated in stations that demonstrated a mechanical thrombectomy, Y-90 radioembolization, embolization coils, and G-tube placements.
“We had tremendous support in making the interventional radiology session a success,” said Dr. Golden. “The event has already prompted several students to reach out regarding shadowing.”
This session featured demonstrations of ultrasound-guided biopsy techniques for breast, abdominal and musculoskeletal imaging.
Thomas LoDuca, MD and Lewis Jordan, MD, MPH, MS led the breast intervention station. Dr. Jordan reflected on how the event exposed students to the radiology field.
“I think seeing a program like this while in medical school actually shows how procedural the field of radiology is,” said Dr. Jordan. “It’s awesome that we are able to interpret imaging findings and use those same images to do biopsies or place localization devices. It is truly a special part of medicine.”

He hopes students walk away from this workshop with a deeper appreciation for the scope of radiology specialties. “We’re doing more than interpreting images,” Dr. Jordan explained. “I would also hope that they would remain encouraged to learn about all of the medical specialties beyond the surface level.”

At the abdominal station for ultrasound intervention, faculty members Leslie Nelson, DO; Giuseppe Toia, MD; Matthew Lee, MD; and Michio Taya, MD demonstrated how to locate and obtain a biopsy sample by creatively using raw chicken breasts to simulate healthy tissue, with olives placed inside to represent abnormal growths or tumors. This setup helped students identify and visualize how these anomalies may appear on a scan.
Anand Narayan, MD, PhD served as a model for the musculoskeletal ultrasound demonstration. The participants witnessed how ultrasound can be used in image-guided intervention of the extremities, including arms.
Spine Intervention Session
This station, led by Monica Cooley, MD and Nicholas Laucis, MD, combined diagnostic imaging with interventional pain procedures like epidural steroid injections.
Dr. Cooley and Dr. Laucis showed students how to perform the interventional procedure using the images scanned by the C-arm as a guide for administering epidural steroid injections on a mannequin.
An anatomical model of the spine was also used as a visual aid when describing and demonstrating the interventional procedure. Students administered the injection and received guidance and encouragement from their instructors and peers.
Medical students had positive feedback about the workshop. Many noted this was their first time handling ultrasound probes or simulating image-guided procedures, and several shared that the experience sparked or deepened their interest in radiology. Faculty also appreciated teaching and interacting with students in a dynamic, low-pressure setting.
Dr. Anderson emphasized the importance of events like No Scalpel, No Problem and hands-on learning early in medical training.
“It breaks down stereotypes about the field and shows the active, procedure-oriented side of radiology,” she said. “For many students, this kind of exposure helps radiology become a more tangible career path—rather than something abstract behind a screen.”


Through a variety of activities, the UW Department of Radiology continued our commitment to introducing the next generation to the field of radiology.
As part of the UW Department of Radiology’s efforts to attract people from historically underrepresented groups, Jade Anderson, MD, Jason Stephenson, MD, and resident Sean Duminie, MD attended the Student National Medical Association’s Annual Medical Education Conference. In addition to representing the department at the UW recruitment booth, the team led a radiology career panel and demonstrated ultrasound-guided aspirations using a homemade phantom mold.
CT scans provide a glimpse into the ancient past
On Thursday, May 1, 2025, a group of high school students from Wyoming gathered around a CT scanner at the Wisconsin Institute for Medical Research (WIMR). Tim Szczykutowicz, PhD operated the equipment to scan a rock from the students’ home on the Wind River Reservation. In a few moments, they would see a fossilized creature that once roamed their homeland millions of years ago.
The students’ visit was part of a partnership between the University of Wisconsin Geology Museum and the Wind River Reservation. The Geology Museum mentors students from the reservation in the science and methodologies of fossil preparation, care, and preservation. The mentorship program helps the Wind River Reservation build the capacity to prepare and curate an extensive fossil collection that is still in rock from their sovereign land.
The students mentored through the program work with their elders to learn about the links between the fossils and the Tribe’s history.
The Geology Museum regularly partners with WIMR to conduct CT scans as part of preparing fossils. Knowing a fossil’s location within a rock improves the chance of extraction with minimal damage. Using CT imaging and incorporating the knowledge of Indigenous peoples paves a new way to study and practice the science of paleontology.

In addition to Dr. Szczykutowicz, PET/CT Research Program Manager Marne VanderPas helped coordinate the visit. CT Instrumentation Technologist Melissa Hruska assisted Dr. Szczykutowicz with scanning the fossils and educating the students.
Interdisciplinary undergraduate program helps solve clinical radiology challenges
For two decades, our faculty and biomedical engineering students have taken great strides in solving clinical radiology challenges through the Biomedical Engineering (BME) Design program. This semester, Ken Lee, MD, MBA; Andrew Ross, MD, MPH; and Matthew Smith, MD, PhD served as clients for the program.
Over the course of the semester, the students work to develop solutions for the clinical challenge their clients present. This work regularly leads to real results, including over 30 patent disclosures, 24 industry-sponsored projects, and three companies formed in the past three years alone.
Timothy Szczykutowicz, PhD participated nearly every semester in the past decade and possesses a deep appreciation for the program. His work with BME students has resulted in eight papers, a patent, and meaningful, lasting mentor-mentee relationships.
Dr. Lee worked with two groups this year; one focused on developing a minimally invasive tool to remove Baker’s cysts, and another developing a wearable device to measure muscle mass.
He initially pitched the ‘Cyst Blaster’ in 2023 and has continued to work with students to refine the product since. The group designed a prototype that aims to provide a treatment that completely removes Baker’s cysts, which have a high rate of reoccurrence. The work has won the 2025 Spring Student Choice Award and an honorable mention for the Tong Biomedical Design Award.
“It’s really fun and rewarding to work with motivated undergraduate students who want to help solve a clinical problem,” Dr. Lee said. “The interdisciplinary collaboration leads to solutions you may not have considered.”
As a first-time participant, Dr. Ross focused on the logistics and process for developing a medical device. Over the semester, he

worked with his team to create a prototype to better control needles in complex injections, such as fluoro-guided cervical spine injections.
“The students were very enthusiastic and keen to understand the clinical issues surrounding the device we were working on,” Dr. Ross said. “They came to shadow procedures, gave me weekly progress updates, and had creative approaches to solving the problem.”
While this semester marked his first time as a client, Dr. Smith wasn’t new to the program. During his time as an undergraduate, he worked on several projects, including ones with radiology faculty members Aaron Field, MD, PhD and Victor Haughton, MD. Describing this full-circle moment, Dr. Smith shared “It’s a privilege to help train and guide the next generation. They have so much potential, and these engineering students can improve the world with the right direction and encouragement.”
Dr. Smith’s team built a phantom to replicate blood flow in the lungs. While phantoms typically have a continuous constant flow, blood flow through the lungs is pulsatile. To more accurately represent the pulsatile flow, the students created a phantom that replicates the dynamic blood flow through the lungs. The phantom is used with x-ray pulsatility index (XPI) to create time of arrival maps.




UW Department of Radiology faculty and residents championed the importance of research and patient care to state and federal of ficials. Through various efforts, faculty members Oliver Wieben, PhD; Robert Bour, MD; Jade Anderson, MD; Pallavi Tiwari, PhD; Anand Narayan, MD, PhD; and Mai Elezaby, MD shared their professional insights with government representatives and the public in pursuit of funding and legislation to help launch careers and save lives.
Residents Erik Winterholler, MD and Erin Sullivan, MD also engaged in efforts to establish dialogue with government leaders. Department alumni Karla Wetley, MD and Jennifer Bergin, MD supported their fellow Badgers in these pursuits.
Dr. Wieben goes to Washington
On March 31, 2025, Dr. Wieben and Sundaram Gunasekaran, PhD from the Department of Biological Systems Engineering met with staff members from the of fices of U.S. Sens. Tammy Baldwin and Ron Johnson, and Rep. Pocan to advocate for science and research funding. The American Institute for Medical and Biological Engineering (AIMBE) and the university coordinated the meetings.
“The recent significant delays in study section and council meetings and distribution of funds to already approved grants, including noncompetitive renewals, have put an unnecessary burden on the progress of science,” said Dr. Wieben. “Our medical physics program admitted only half as many PhD students as usual because of the uncertainties in funding. These disruptions will result in further amplifying the shortage of board certified medical physicists
and impact the career decisions of young scientists in possibly not pursuing graduate school or leaving academia given the unpredictable job market.”
On May 7, 2025, faculty, trainees and alumni met with U.S. Rep. Mark Pocan as part of the American College of Radiology’s Capitol Hill Day. The Wisconsin Radiological Society scheduled the meeting.
“Typically, we meet with of fice staffers on these types of visits,” explained Dr. Winterholler. “But Rep. Pocan made time to meet with us personally.”
Faculty members Dr. Bour and Dr. Anderson joined Dr. Winterholler, along with resident Dr. Sullivan, alum Dr. Wetley and Srijyotsna (Lucky) Volety, MS, a PhD student in the Department of Medical Physics. The group raised awareness of the Radiology Outpatient

Ordering Transmission (ROOT) Act, which would promote valuebased care, help patients avoid unwarranted imaging and radiation exposure, and reduce Medicare spending on low-value imaging.
While Rep. Pocan stated that action is challenging in the current legislative environment, he also expressed concern for Wisconsinites, including physicians.
“He took time to listen and understand the radiologists’ perspective and responded to our concerns with genuine interest,” said Dr. Winterholler.
Dr. Tiwari presents at UW–Madison Day at the Capitol UW–Madison Day at the Capitol on April 30, 2025, provided the public an opportunity to hear from faculty, students, alumni. The Faculty Flash Talks, a feature of the event, are brief showcases of leading research from UW faculty, educating the public on how state-funded projects can benefit society.
Dr. Tiwari presented her research on the use of AI in medical imaging, which she leads as part of the Integrated Diagnostics and Analytics (IDiA) Laboratory for Precision Medicine efforts. Dr. Tiwari encouraged others to be open to using AI in health care.
“There is the potential for AI applications in health care to make diagnoses more ef ficient and reliable,” said Dr. Tiwari. “This can result in people seeing positive benefits by saving money on their health care and having better patient outcomes.”
Dr. Tiwari believes RISE-AI, part of the Wisconsin Research, Innovation and Scholarly Excellence (RISE) Initiative, is a step forward, adding more faculty to focus on developing and refining
AI technology. However, it may not be enough to reach the goal of improving AI for health care applications.
“More work and support is needed,” said Dr. Tiwari.
Dr. Narayan advocates for breast cancer screening coverage
On May 28, 2025, Dr. Narayan testified on behalf of the Wisconsin Radiologic Society at a Wisconsin State Senate hearing in support of Senate Bill 264. Section of Breast Imaging and Intervention Chief Dr. Elezaby and alum Dr. Bergin also attended the hearing.

If this legislation passes, Wisconsin would join several other states requiring health insurance policies to cover diagnostic examinations and supplemental screenings for individuals with increased risk of breast cancer or extremely dense breast tissue.
Dr. Narayan testified that the cost of these life-saving examinations is often a barrier for most women.
“Unlike screening mammograms, which are covered by law without copays or deductibles, diagnostic exams can cost a lot of money, even if women have health insurance,” said Dr. Narayan. “This often leaves women with a terrible choice: either pay hundreds or thousands of dollars...or skip the test and hope for the best.”
On June 2, 2025, the Wisconsin Senate Health Committee voted unanimously (5-0) to move Senate Bill 264 to the Wisconsin Senate floor, taking a step closer to becoming a law.
“I’m excited that the bill has moved forward,” said Dr. Narayan. “Passing this bill is an important step to ensure that women all over Wisconsin get access to our best tools to find breast cancer early,”

Perry Pickhardt, MD is the principal investigator for the UW subaward of the 3-year $750K Pershing Square Sohn Cancer Prize for “Defining the Physiologic and Molecular Etiology of Cachexia with Population-Scale Computational Radiology” from the Pershing Square Sohn Cancer Research Alliance.
Matthew Lee, MD received a 2-year $180K grant for “AIdriven Abdominal CT-based Biomarkers for Predicting Cardiometabolic Risk in Early and Middle-Aged Adults” as a 2025 American Roentgen Ray Society Scholarship recipient.

Nicholas Burris, MD received a 1-year $87K grant for “Linking in vivo hemodynamics with outcomes in Type B aortic dissection using 4D flow MRI” from the National Institutes of Health.

Michael Veronesi, MD, PhD received a 6-month $392K grant for “LAT1 targeted radionuclide theranostics with 18F-FET PET and 131I-IPA for treatment of GBM” from Telix Pharmaceuticals.


Scott Reeder, MD, PhD and Diego Hernando, PhD are co-investigators for a 4-year $153K grant for “Developing a Cardiac MRI Guided Therapy for Hemorrhagic Myocardial Infarction” from the National Institutes of Health.
Andrew Wentland, MD, PhD received a 1-year $68K grant for “Technical Development and Validation of Synthetic Images in Multiphasic CT Examinations of the Kidneys” from the Fall Research Competition and the Wisconsin Alumni Research Foundation (WARF).

John-Paul Yu, MD, PhD received a 2-year $220K grant for “Molecular, Behavioral, and PET/MRI Correlates of Psilocybin Therapy” from The Foundation of the American Society of Neuroradiology.

Ali Pirasteh, MD received a $110K grant for “Best practice for assessing liver metastatic disease from rectal cancer” from Bayer in partnership with University of California, San Diego.


Ran Zhang, PhD and Tyler Bradshaw, PhD received a 1-year, $50K grant for “Large language models for enhanced mammography data retrieval” from Flywheel.
On June 10, 2025, Radiology published Perry Pickhardt MD’s study, “CT Colonography versus Multitarget Stool DNA Test for Colorectal Cancer Screening: A CostEffectiveness Analysis.” The study quickly made the news as several media outlets covered the research, including RSNA News, AuntMinnie.com, The Imaging Wire, Applied Radiology, Physician’s Weekly and Yahoo.com. RSNA also featured it in their monthly highlights from their publications.
The study revealed CT colonography to be a more clinically effective and cost-saving method for colorectal screening compared to multitarget stool DNA (mt-sDNA) testing. While conventional colonoscopy is the standard for detecting signs of colorectal cancer, CT colonography and mt-sDNA are less invasive alternatives.
Dr. Pickhardt, along with coauthors Loredana Correale, PhD and Cesare Hassan, MD, PhD, compared mt-sDNA and CT colonography because a Medicare expansion covers them. The expansion coincides with rising rates of colorectal cancer in younger patients, which in 2021 prompted the U.S. Preventive Services Task Force and several medical societies to lower the recommended age for screening from 50 to 45. With the rising demand for testing and the availability of alternative methods, the study evaluated the effectiveness of these tests both clinically and in terms of cost.
The researchers used a Markov model to simulate the progression and screening outcomes in a model of 10,000 individuals ages 45 to 75. The model projected 7.5% of participants would develop colorectal cancer without screening, which aligns with current data.
The team examined three approaches for detection. One method implemented mt-sDNA testing every three years. The second used CT colonography every five year with optical colonoscopy for immediate removal of polyps measuring at least 6 mm. The final used a CTC strategy that involved a three-year CT colonography follow-up for small polyps between 6 and 9 mm and the removal of large polyps measuring over 10 mm via conventional colonoscopy.
The research found that both CT colonography and mt-sDNA screenings greatly reduced colorectal cancer incidence. However, both CT colonography strategies resulted in a 70-75% reduction in cancer incidence, while mt-sDNA achieved a 59% reduction.
Routine preventive evaluation is the best route to prevent and identify colorectal cancer in its early stages, but the current standard has its drawbacks.
“In the U.S., conventional colonoscopy remains the dominant screening test for colorectal cancer, despite the fact that it is the most expensive and invasive option,” said Dr. Pickhardt.
Optical colonoscopies require patients to prepare several days in advance of the procedure, limiting their diet and fluid intake. Patients are also required to bring another person to drive them home after the procedure, as the anesthesia takes up to 24 hours to wear off, impairing the ability to operate a vehicle safely.
The findings from Dr. Pickhardt and his team are reassuring as these affordable, noninvasive procedures will be in higher demand to combat colorectal cancer in younger patients. Medical providers can utilize the study’s findings to develop early cancer detection strategies that can better fit patients’ time and budgets compared to relying solely on conventional colonoscopies.


In late February, the UW Department of Radiology became the first site in the Midwest and second in the nation to administer patient doses of GE HealthCare’s new cardiac PET radiopharmaceutical, Flyrcado (flurpiridaz F 18) injection. Through a long-standing collaboration with GE HealthCare, Nandakumar Menon, MD and Sarah Thordsen, MD introduced the use of the radiotracer that could increase patient access to cardiac stress PET imaging.
Positron emission tomography myocardial perfusion imaging (PETMPI) is a heart scan that uses small amounts of radioactive material and a camera to show how blood flows to the heart muscle, helping physicians diagnose coronary artery disease, assess heart muscle viability, and guide treatment decisions. In addition to being a noninvasive alternative to coronary angiogram, PET-MPI produces superior images, more accurate results, faster scans, and lower radiation exposure compared to single-photon emission computed tomography (SPECT), another type of MPI.
“PET imaging reveals an organ’s function at the molecular level, providing critical insights that complement clinical information and anatomic imaging for more comprehensive evaluation,” explained Dr. Menon, an assistant professor in the Section of Nuclear Medicine and Molecular Imaging. “PET MPI combines precision, ef ficiency and accuracy – helping us quantify coronary flow like never before, leading to better diagnosis and patient care.”
Although the department conducted 48% more cardiac PET scans in 2024 than in 2023, availability of PET MPI radiotracers poses a challenge to continued growth. Currently, the department primarily uses 13N-Ammonia produced in our Radiopharmaceutical Production Facility. Supporting a wide variety of clinical and research needs limits the facility’s capacity to produce 13N-Ammonia.
Available in ready-to-use unit doses that can be ordered as needed, Flyrcado could help. In addition, the agent’s half-life is significantly longer than existing PET MPI tracers, enabling exercise stress tests.
“Humans are constantly in motion,” noted Dr. Thordsen from the Division of Cardiovascular Medicine within the Department of Medicine. “If we only image a body after it’s been still for a long period, we aren’t getting the full picture of how blood flows.”
“Today is a celebration of tradition and partnership,” said Chair Scott Reeder, MD, PhD. “We have a tradition spanning nearly three decades of working with GE HealthCare to advance patient health through imaging innovation. It’s also about the partnerships that make this work possible. That includes the partnership with GE HealthCare and the cross-departmental partnership that Dr. Menon and Dr. Thordsen have formed that led to this important milestone.”
The importance of collaboration was evident throughout. Dr. Menon and PET/CT Research Program Manager Marne VanderPas met with GE HealthCare regularly to coordinate logistics. Once the Flyrcado arrived, VanderPas’s team of PET technologists went into action. Jered Meyer carefully handled the radioactive dose, Trish Tolan prepared the PET/CT scanner, and Riley Diekvoss consulted with the physicians and GE HealthCare scientists on the injection technique. The team successfully conducted two procedures using Flyrcardo injections and are prepared for future exams.

Nuclear Medicine and Molecular Imaging
Section Chief Steve Cho, MD discussed his work in the growing field of theranostics for an article in UW Health’s Advances newsletter.
In addition to treating patients at UW Health | Carbone Cancer Center, Dr. Cho is an active researcher and part of Carbone Cancer Center’s growing work in theranostics. This field of nuclear medicine combines “therapy” and “diagnostics” and uses a dual approach of imaging technology and targeted therapies to identify and treat advanced stage cancers.
“Dating back to the 1930s and also under the “Atoms for Peace” program in the 1950s, people started to figure out how to use radioactivity, not to harm patients, but to be able to treat patients. [Theranostics] has been around for quite a bit of time, starting with radioactive iodine for thyroid cancer,” Dr. Cho said. “There’s really nothing new under the sun, it’s just a new term, although the technology has improved significantly.”
By utilizing radioactive drugs that are attracted to specific receptors on the surface of tumor cells, theranostics researchers can map cancer sites and deliver treatment directly to the cancerous cells. This approach is especially significant for treating patients whose cancer has spread throughout the body, as it can treat multiple cancer sites simultaneously.
Dr. Cho employs theranostics in his clinical work, specializing in treating patients with targeted radiopharmaceutical drugs. In his research, he is investigating how treatment doses can be optimized to limit toxicity to patients while still effectively treating tumors.
Speaking to the impact that theranostics can make for patients, Dr. Cho shared, “If you can extend someone’s quality of life for several years so that they can see their kids graduate from school or see them get married, this makes an important and deep impact on their life and the people around them, which I think is tremendously gratifying.”


Steve Cho (right) treats patients with theranostic drugs and is researching how to calculate precision doses of those tailored to each patients’ needs.
The Radiological Society of North America (RSNA) featured the new MRI Smart Suite at UW Health’s Eastpark Medical Center in the article, “Optimized MRI Suites Enable High-Volume Turnaround, Better Access for Patients,” which was published on May 8, 2025 and included in the recent RSNA News issue. UW Department of Radiology Chair Scott Reeder, MD, PhD provided an overview of the process his team took to collect and analyze data before applying the insight to the architectural design.
The article also included information about a similar initiative at Mass General Brigham in Boston. Growing demand for medical imaging acted as the impetus for both efforts.
“If you’re growing at 10% per year, that means you’re doubling your volumes every seven years,” Dr. Reeder said in the article. “It’s unsustainable to double your volume by purchasing more scanners. So, you either must add more shifts, or you need to learn to scan more ef ficiently, shorten your protocols and address the operational challenges that this presents.”
To address this, Dr. Reeder launched the MR2025 strategic plan in 2019 while serving as the clinical chief of MRI and senior vice chair of research. Once he and his team analyzed data on scan times and scheduling, they adjusted protocols to shorten specific scans and started planning the Smart Suite.
Opened in October 2024, the Smart Suite was inspired in part by a design implemented at NYU Langone Health. “We have two doors and two scanner tables per room. When one patient is in
the magnet, the next patient is prepared on deck, ready to go,” Dr. Reeder said.
Early numbers show a stark improvement with room turnaround times dropping from 12 minutes to about two minutes. This decrease allowed for shorter time slots and more appointments.
“We’ve increased the number of staff to handle the rapid throughput,” Dr. Reeder said. “It’s a great environment; they’re like a SWAT team moving patients around between the systems.”
In addition to improving MRI operations at Eastpark Medical Center, the MR2025 initiative’s success contributed to the launch of the Center for High Value Imaging by UW Health and the UW School of Medicine and Public Health. A patient-centered strategy, high-value imaging aims to improve patient access and experience as well as maximize actionable imaging-derived information. This ef ficiency is core to being good stewards of human and technological resources.

During the American College of Radiology (ACR) 2025 annual meeting, University of Wisconsin Department of Radiology resident John (Erik) Winterholler, MD submitted and defended the resolution “Ionizing Radiation Protective Apparel for Healthcare Workers.”
After two amendments from the medical physics caucus, the ACR accepted the resolution as policy, marking it as the first ACR policy from the department authored solely by residents to pass in many years.
In addition, it was the only resolution authored by residents outside of elected resident leaders submitted to the ACR 2025 meeting.
The authors include Dr. Winterholler; Isha Pathak, MD; Elizabeth Stoeckl, MD; Erin Sullivan, MD; Zachary Hansen-Cole, MD; and Cullen Fleming, MD. Notably, the team featured residents in each year of training from first- to fourth-year residents.
Emphasizing the importance of well-fitting lead protective apparel for different body types, the full policy reads:
BE IT RESOLVED that the American College of Radiology encourages healthcare institutions to provide adequate fitting lead protective apparel and in adequate numbers for different body types. Where reasonably achievable, ancillary protective equipment need be available for those areas not covered by a standard lead apron.


In addition to this notable accomplishment, Jade Anderson, MD co-authored 13 resolutions, of which eight were adopted and three referred.

The season of annual meetings brings together faculty, trainees, students and alumni from across the country. It also brings opportunities for our department members to shine!
Society for Cardiovascular Magnetic Resonance (SCMR) Annual Meeting
January 29 – February 1, 2025 • Washington, DC
David Bluemke, MD, MSB, PhD gave the plenary address in honor of his receipt of the Gold Medal in 2024.
Society of Abdominal Radiology (SAR) Annual Meeting
February 16-21, 2025 • Tucson, AZ
Perry Pickhardt, MD gave the plenary address in honor of his receipt of the Gold Medal in 2024.
Matthew Lee, MD received the Emerging Investigator Award for his scientific presentation “A Novel CT-based Biological Age Model Using Explainable Automated Abdominal CT Biomarkers for Longevity Prediction.”
Society of Thoracic Radiology (STR) Annual Meeting
March 1-5, 2025 • Huntington Beach, CA
Resident German Banez Rueda, MD received a certificate of merit poster award for his poster “Aunt Minnies That Aren’t: Do Not Be Deceived by Appearances.”

Faculty, alumni and friends bring the Wisconsin spirit to the SAR meeting.
Wisconsin Radiological Society (WRS) Annual Meeting
April 4-5, 2025 • Kohler, WI
During the meeting, the following faculty members were announced as leaders:
• Robert Bour, MD was announced as president.
• Anand Narayan, MD, PhD was announced as president elect.
• Jade Anderson, MD was announced as a councilor. She was also appointed as the Young Physician Section Leader for the Wisconsin Medical Society (WMS) Board of Directors.
American College of Radiology (ACR) Annual Meeting
May 3-7, 2025 • Washington, DC
Meghan Lubner, MD was inducted as a Fellow of the American College of Radiology (FACR). Former Community Division member, Frank Thornton, MD also earned the FACR.
International Society for Magnetic Resonance in Medicine (ISMRM) Annual Meeting
May 10-15, 2025 • Honolulu, HI
Dania Daye, MD, PhD shared insight from her session on the challenges of implementing AI algorithms as well as the new Center for High Value Imaging in an AuntMinnie.com video.

American Association of Endocrine Surgeons (AAES) Annual Meeting
May 17-19, 2025 • Milwaukee, WI
Jason Pinchot, MD was named the Medical College of Wisconsin’s Stuart D. Wilson Historical Lecturer and delivered the plenary session.
Society for Imaging Informatics (SIIM) Annual Meeting
May 21-23, 2025 • Portland, OR
Tyler Bradshaw, PhD’s session was featured in the article “SIIM: Informatics key to future of theranostics” by AuntMinnie.com.
Postdoc research fellow Fatima Rashidi, MD received the Second Place Poster Award for “Impact of FDG PET/MRI on Management of Patients with Chronic Spinal Pain.”



After serving as associate vice chair of clinical operations, Gregory Avey, MD has been appointed vice chair of clinical operations. The role was previously held by Michael Tuite, MD since 2012.

Dania Daye, MD, PhD has joined the department as inaugural vice chair of practice transformation and the inaugural director of the Center for High Value Imaging (CHVI).

Christoph Lee, MD, MS, MBA has joined the department as the new vice chair of research.
Frank Korosec, PhD served in role as interim since Scott Reeder, MD, PhD became chair.

Kelly Capel, MD has been appointed director of fellowships. The role was previously held by Gregory Avey, MD.
Stéphane Desouches, DO has joined the department as the inaugural section chief of the Section of Emergency Radiology.

Thomas LoDuca, MD has been appointed associate program director of the Breast Imaging & Intervention Fellowship program.

Alan McMillan, PhD has been appointed associate section chief for the Section of Imaging Sciences.

Mohammed Bhuiyan, PhD has joined the department as the inaugural director of the Radiopharmaceutical Production Facility.



John Khalil, MD; Matthew Shore, MD; and Roberta Strigel, MD, MS have been elected to the department’s Finance Committee for a 2-year term.
The University of Wisconsin Department of Radiology has established the new Section of Emergency Radiology to support the growing demand for imaging, especially during evening hours. This new section will be led by Stéphane Desouches, DO who joined the department in April 2025.
Most recently, Dr. Desouches was an associate professor at the Medical College of Wisconsin where he served as vice chair of education since 2022. He was named Resident Advocate of the Year four times. He completed the Association of University Radiologists’s Radiology Management Program in 2023.
He also practiced and specialized in musculoskeletal and thoracic radiology at Froedtert Hospital.
“We are fortunate to have Dr. Desouches step into this important leadership role,” said Chair Scott Reeder, MD, PhD. “His dedication to education and passion for advancing emergency radiology will be a tremendous asset to our trainees and faculty.”
Our emergency departments are busy and are showing continued growth in the number of patients requiring care. Imaging volumes in the Emergency Department are highest between 4:30 and 9 p.m., but demand extends well past midnight.
The new Section of Emergency Radiology addresses this increasing volume of images requiring analysis off-hours. The section will include dedicated Emergency Radiology faculty members who will help cover evenings.
“The chance to help build a new section from the ground up including developing workflows, interdepartmental relationships, and extra-clinical opportunities was not one I could pass up,” explained Dr. Desouches.

In addition to helping manage the volume, Emergency Radiology faculty will also be available for trainees to consult. The new section presents valuable learning possibilities and opportunities that Dr. Desouches is eager to cultivate.
“I am looking forward to working with the residents to develop workflows and communication avenues to improve interaction and promote a culture of learning,” said Dr. Desouches. “Working through call cases is a formative part of training and I look forward to adding what I can to the process for our residents.”

In 2024, UW Health and the UW School of Medicine Public Health launched the Center for High Value Imaging (CHVI) to improve patient access, experience and outcomes through high-value imaging. With Director Dania Daye, MD, PhD now at the helm, the center will transform the way diagnostic imaging and image-guided therapies are delivered.
In the recent Wisconsin Medical Journal article, “High-Value Imaging in an Era of Uncertainty, Growth, and Disruptive Technologies,” UW Department of Radiology Chair Scott Reeder, MD, PhD and medical school Dean Robert Golden, MD mapped out the current state of imaging and how CHVI will become the model for highvalue imaging innovation and care delivery.
Since its inception with the discovery of X-rays 130 years ago, the field of medical imaging has revolutionized medicine and continues to evolve rapidly. The widely cited survey of physicians by Fuchs and Sox ranked ‘MRI and CT Scanning’ as the No. 1 medical innovation and those are just two modalities. Through imaging, patients are diagnosed, treatments are monitored, procedures are guided, and scientific hypotheses are tested.
“At UW Health, we expect to perform more than 1 million exams per year by the time we celebrate our Department of Radiology’s centennial anniversary in 2027,” Drs. Reeder and Golden noted in the article. “With such utilization comes great cost in capital equipment and in the rapidly growing workforce needed to operate equipment, interpret exams, and treat patients.”
At the same time, the field of radiology is on the forefront of technological advancements, including the application of artificial intelligence (AI). More than 77% of the over 1,000 US Food and Drug Administration-approved AI technologies are in radiology.
Much of this work is being conducted within the UW Department of Radiology. For example, Perry Pickhardt, MD uses AI tools for opportunistic screenings, whereby actionable information can be derived from previously obtained medical images to benefit patients. In addition, Pallavi Tiwari, PhD developed an AI model to identify why glioblastoma tumors are more aggressive in men than women.
“The confluence of economic and sustainability pressures, strains on the workforce, continued success and growth of medical imaging, and emergence of advanced analytics and disruptive AI-based technologies all converge toward a new paradigm of ‘high-value imaging.’” Drs. Reeder and Golden explained in the article.
A patient-centered strategy, high-value imaging aims to improve patient access and experience as well as maximize actionable imaging-derived information. This ef ficiency is core to being good stewards of our human and technological resources.
Recent CHVI accomplishments include the introduction of a “Smart Suite” to improve MRI operations at the new Eastpark Medical Center in October 2024, which was spearheaded by MRI Modality Chief Ali Pirasteh, MD, Senior Vice Chair of Clinical Operations Michael Tuite, MD and Associate Vice Chair of Clinical Operations Gregory Avey, MD. Advanced analytics and innovative architectural design resulted in reduced MRI wait times and a more than 50% increase in patient throughput.
In February 2025, CHVI launched an MRI command center staffed by a lead radiology technician who uses real-time dashboards to make data-informed decisions across our various locations. The technicians have already seen benefits like streamlined scheduling, decreased pressure on staff, and opportunities for education.
The work has just begun and inaugural Director Dania Daye will lead in expanding the center’s impact. Dr. Daye joined the department in April 2025 as vice chair of practice transformation and an associate professor in the Section of Interventional Radiology. In 2024, the Society of Interventional Radiology Foundation awarded Dr. Daye the Dr. Gary J. Becker Young Investigator Award, recognizing her work on AI-based technologies for quality and operations.
In collaboration with internal and external partners, Dr. Daye has outlined a multiyear plan focusing on three strategic initiatives: patient care and community service, research and innovation, as well as education. Initiatives feed into each other, while always keeping the patient as the primary focus.
“Our goal is to establish CHVI as a world-renowned leader in setting standards for high-value imaging and care delivery through improved patient access, experience and outcomes,” Dr. Daye explained. “There are many elements required to accomplish this, such as optimizing the translation of innovation into operations. But one of the first steps is to build a multidisciplinary network of collaborators dedicated to improving patient care through highvalue imaging.”
“The potential of the Center for High Value Imaging is immeasurable,” noted Dr. Reeder. “And with Dr. Daye’s leadership and expertise, that potential will lead to meaningful improvements in patient care.”





In July 2024, Allison Grayev, MD became the director of the Diagnostic Radiology Residency program in the department. Primed by years of educational experience, she demonstrated how an inclusive leadership style can result in positive changes.
Since taking the reins, Dr. Grayev has empowered residents to have agency in their training and helped ensure the already successful program continued to meet the needs of both the department and the residents.
“I have been fortunate to take over an excellent residency program, which has allowed me to focus on aspirational goals for the future,” noted Dr. Grayev. “To that end, we’ve spent this first year fact finding – what’s working for the residents and what isn’t.”
Through these efforts, Dr. Grayev discovered residents faced an increasing demand for overnight imaging requests from the emergency department. At the education retreat in January, she worked with trainees to develop a new call structure.
“Dr. Grayev anticipated the developing problem, created a task force including residents, and implemented a practical solution,” said Vice Chair of Education David Kim, MD. “Her ability to communicate and include relevant groups in the decision-making process and ultimately get buy in was impressive.”
Dr. Grayev also wanted to ensure the residents were acknowledged for handling the increased demand for imaging requests. With the support of Chair Scott Reeder, MD, PhD and Dr. Kim, Dr. Grayev
is advocating for residents to receive additional pay until the new Section of Emergency Radiology became fully staffed.
Assistant Director of Education Katie Ricks, MS observes the real changes brought about by the culture of transparent communication and feedback Dr. Grayev fosters. “The collaborations have led to the creation of a new swing shift, a new phone tree structure, and changes to rotations, all of which has improved education and training for our residents.”
Dr. Grayev gained an insider’s perspective to our programs when she completed her Neuroradiology fellowship here. In 2010, she returned to Madison to join the Section of Neuroradiology as faculty.
Early on in her time as faculty, Dr. Grayev focused on educational initiatives including the UW School of Medicine and Public Health’s ForWard Curriculum. Dr. Grayev created a new preclinical radiology curriculum. By exposing students to the field earlier, She has helped to foster an increased interest rate for medical students to pursue a career in radiology. Her contributions earned her the Dean’s Teaching Award in 2021.
While Dr. Grayev’s first year as program director included many accomplishments, she’s not slowing down. The program currently offers opportunities for dual board pathways in early specialization in interventional radiology (ESIR), nuclear medicine and pediatric radiology. Dr. Grayev hopes to create an educational pathway as well as one for management and leadership.
“Our program has always been at the forefront of creating great radiologists,” said Dr. Grayev. “I want to create opportunities to shape the radiology leaders of tomorrow – while allowing residents to find the paths that best align with their career aspirations.”

The UW–Madison Institute for Clinical and Translational Research (ICTR) funds research activities that inform subsequent external funding proposals through its Pilot Awards Program. Alan McMillan, PhD experienced this firsthand when he received a award for his research project in 2015; now, a decade later, Dr. McMillan serves as co-director for the program.
“That award was the catalyst for what has become an enduring and incredibly fruitful collaboration with a valued colleague in the Department of Electrical and Computer Engineering” Dr. McMillan explained. “It’s the perfect example of how these pilot awards do more than fund a project; they build bridges between departments and disciplines that can last for years.”
Overseeing the release of funding opportunity announcements and managing the scientific peer review process are two of Dr. McMillan’s primary responsibilities. As such, he ensures funding opportunities align to the institution’s strategic goals, and that they meet the everevolving needs of the research community. He also facilitates a fair, transparent and rigorous peer review process that guarantees each applicant a thorough evaluation.
Dr. McMillan began in his role with Co-Director Meghan Brennan, MD, MS from the Division of Infectious Disease in January 2025. They are part of a team that includes Pilot Awards Program Manager Bri Deyo, MPH; Director of Workforce Development Peggy Hat field, PhD; and Senior Associate Executive Director Christine Sorkness, RPh, PharmD.
What’s the experience been like, going from an applicant to working on the team that reviews and selects the projects?
It has been an incredibly rewarding transition. There’s a profound sense of fulfillment in being able to “give back” to the very program that provided a crucial stepping-stone in my own research. Having been on the applicant side for ICTR and many other proposals, I have a deep appreciation for the effort and hope that goes into every single proposal. Now, being part of the team that facilitates this process for others is a tremendous privilege. I am honored to contribute to the cycle of innovation and discovery.
Has being a past awardee given you any insight as you navigate your new role?
Absolutely. My experience as a past awardee has fundamentally shaped my perspective on this role. I firmly believe that pilot funding is the lifeblood of academic research. It’s the essential seed money that allows high-risk, high-reward projects to take root. These are the kinds of innovative, and sometimes unconventional, ideas that might not initially secure funding from larger federal agencies but have the potential to be truly transformative. Without the resources to support a graduate student or a scientist and to gather preliminary data, many of these groundbreaking research avenues would simply never be explored.
Is there anything that’s surprised you about being co-director?
While perhaps not surprising, I have been deeply impressed by the immense professionalism and capability of the ICTR group. It’s one thing to interact with the program as an applicant, but it’s another to see the inner workings and the dedication of the entire team. The commitment to fostering research and supporting investigators is truly remarkable.

In honor of International Women’s Day on March 8, we interviewed three of our leaders who uphold our department’s operations to the highest standards in educational, research and clinical endeavors.
Allison Grayev, MD, a professor in the Section of Neuroradiology, serves as the Diagnostic Radiology Resident program director. Prior to being appointed to that role in 2024, she was an associate program director for over a decade.
Sara John, BS RT (R), is the associate director of research for the department. She began her career as an MRI technologist assistant at UW Hospitals and Clinics and has held numerous roles at the Wisconsin Institute for Medical Research (WIMR) throughout her time with the department.
Meghan Lubner, MD, a professor in the Section of Abdominal Imaging and Intervention and is the clinical and research CT modality chief. She was appointed director of CT research in 2011, and director of abdominal CT in 2014 before becoming modality chief in 2017.
Visit the article online and read their full interviews to learn more about the important contributions they make every single day, and what advice they have for other women interested in pursuing leadership roles.

Allison Grayev, MD
Diagnostic Radiology Residency Program Director
One of the highlights from the department’s education retreat is a new call structure for residents. How did you develop this initiative? The key to any change that we make is to use data to support decisions and to consider how stakeholders are affected. Thanks to the informatics team, we were able to create an overlapping schedule to cover the busiest times after hours, thus optimizing our staf fing. We were able to introduce recovery days for our residents to balance out their increasing call burden, which will be more palatable with the upcoming expansion of our residency program.
Are there any other exciting ideas you’re exploring in your first year as program director?
We are currently working with Collective Minds and informatics to create a new teaching file platform that would include the ability to embed videos and articles, as well as options for formative assessment.
Informatics is also playing a role in ongoing work that we are doing to implement improved feedback to residents after overnight shifts through implementation of large language models to compare preliminary and final reports. Ultimately, I would love to create individualized learning plans at scale using data from cases that residents dictate to identify potential knowledge gaps, both in terms of diagnoses and modalities, utilizing metadata already collected with each study.

Sara John, BS RT (R)
Associate Director of Research
What first sparked your interest in the research field?
Growing up, I was always fascinated by science, and having my dad as my high school chemistry teacher only fueled that interest. When I went to college, I knew I wanted to enter the medical field, but I wasn’t sure in what capacity. I attended UW–Milwaukee, which had just launched a bachelor’s program in radiologic technology. A friend in the program encouraged me to explore it, and I did.
When I discovered that UW Hospitals and Clinics was one of the clinical placement options, I knew it was meant to be. Having grown up in Mount Horeb, I was aware of UW’s amazing reputation, and this was the perfect opportunity to return. During my studies, I worked as an MRI technologist assistant and had the chance to observe an MRI research scan. That experience was pivotal. When a position as an MRI technologist in radiology research opened up, I jumped at the chance to apply! It was the perfect opportunity to continue my radiology career while also being part of exploring cutting-edge imaging technologies to improve future patient care.
What is your favorite part about your job?
My favorite part of my job is, without a doubt, the people I work with. We have an incredible research team, and the faculty members and investigators are always so appreciative. The teamwork and collaboration within our department are outstanding, and everyone genuinely cares about improving patient care.

Meghan Lubner, MD Clinical and Research CT Modality Chief
How long have you been in the Clinical and Research CT Modality Chief role?
What initially drew your interest? I was appointed director of CT research in 2011, and director of abdominal CT in 2014. I became modality chief when Myron Pozniak, MD stepped down in 2017.

I have always considered CT a workhorse imaging modality that is really fundamental to our work as radiologists in general; and in abdominal imaging in particular. CT is fast, versatile, profoundly clinically impactful in a variety of situations, and continues to reinvent itself as a modality as the technology continues to develop.
What are some elements of the job that surprised you?
The challenges around COVID-19, the iodinated contrast shortage, and ongoing workforce challenges have surprised me; and have required team problem-solving and collaboration. While they were challenging obstacles to overcome, they made me appreciate our ability to put our heads together and work out how we could continue to provide great care for our patients.
The development and emergence of photon-counting CT has surprised me in delightful ways, bringing to fruition some of the most exciting CT advances of my career.

Mosa Alhamami, PhD, MCCPM joined the Sections of Imaging Sciences and Clinical Imaging Physics as an assistant professor (CHS) and director of interventional radiology physics. He practiced as a clinical diagnostic medical physicist most recently as an assistant professor at UMass Chan Medical School, Beth Israel Lahey Health in Burlington, MA. He is interested in innovative imaging methods that enable noninvasive monitoring.

Dania Daye, MD, PhD joined the Section of Interventional Radiology as an associate professor (CHS). She serves as director of the Center for High Value Imaging and vice chair of practice transformation. After training, Dr. Daye practiced at Massachusetts General Hospital. She was also an associate professor at Harvard Medical School and the director of the Precision Interventional and Medical Imaging (PIMI) lab at the MGH/HST Martinos Center for Biomedical Imaging.

Mohammed (Parvez) Bhuiyan, PhD joined the Section of Imaging Physics as an associate professor (CHS) and director of the Radiopharmaceutical Production Facility. Most recently, Dr. Bhuiyan worked at the University of Chicago’s cyclotron facility as associate director. He has worked in nanoparticle fabrication and labeling, MRI and fluorescence imaging contrast agents, and small molecule labeling with radionuclides for imaging and therapy.
Stéphane Desouches, DO joined the new Section of Emergency Radiology as an associate professor (CHS) and section chief. Previously, Dr. Desouches was an associate professor and vice chair of education at the Medical College of Wisconsin. During his tenure, he was named Resident Advocate of the Year four times and was chair of the Radiology Education Committee and Radiology Residency Education Workgroup.
Jennifer Febbo, MD joined the Section of Thoracic Imaging as an associate professor (CHS). Before joining our department, Dr. Febbo was an assistant professor and section chief of Cardiothoracic Radiology at the University of New Mexico Health Sciences Center Department of Radiology.

Sanna Herwald, MD, PhD joined the Section of Interventional Radiology as an assistant professor (tenure). After earning her medical degree and PhD from Tufts University, Dr. Herwald completed her residency at Stanford University Medical Center.

Lewis Jordan, MD, MPH, MS joined the Section of Breast Imaging as an assistant professor (CHS) after completing his fellowship with us. He did his internship at Weiss Memorial Hospital in Chicago, and his residency at Rush University Medical Center.
Christoph Lee, MD, MS, MBA joined us as the inaugural Tom Grist, MD/GE HealthCare Foundation Distinguished Chair in Radiology Research, vice chair of research, and professor (tenure) in the Section of Breast Imaging and Intervention section. Most recently, Dr. Lee was professor of radiology and founding director of the Northwest Screening and Cancer Outcomes Research Enterprise at the University of Washington and Fred Hutchinson Cancer Center. He is currently the principal investigator of multiple R01 grants awarded by the National Institutes of Health (National Cancer Institute).

Deepa Pai, MD, MHSA joined the Section of Pediatric Radiology as a clinical professor (CT). Dr. Pai served as chief of pediatric musculoskeletal imaging section at Children’s Minnesota before joining us.

Taylor Sellers, MD joined the Section of Thoracic Imaging as assistant professor (CHS) after completing his fellowship with the department. He completed his internship and residency in diagnostic radiology at University of Iowa Hospitals & Clinics, and served as chief resident.

Tomas Romero, MD joined the Section of Nuclear Medicine and Molecular Imaging as an assistant professor (CHS) after completing his fellowship with the department. After obtaining his medical degree, he worked as an emergency doctor in Venezuela before transitioning to research support work and then returned to medical training.
Isaiah Tan, MD joined the Community Radiology division as a clinical assistant professor. He completed his internal medicine internship, diagnostic radiology residency, and neuroradiology fellowship at UW Hospitals and Clinics.
Thekla Oechtering, MD, PD

Dr med joined the Section of Cardiovascular Imaging as an assistant professor (tenure). She is the director of 4D flow MRI and co-director of Radius. Before joining the faculty, she served as a visiting assistant professor, scientist and fellow with the department.


Elliott Russell, MD joined the Section of Interventional Radiology as a clinical assistant professor. Dr. Russell completed his integrated interventional radiology residency and served as chief resident at UW Hospitals and Clinics.

Wenhui Zhou, MD, PhD joined the Section of Breast Imaging and Intervention as an assistant professor (tenure). He earned his medical degree and PhD at Tufts University. He did his diagnostic radiology and nuclear medicine residencies, as well as fellowship at Stanford University Medical Center. During residency, he was chief resident.




Richard Bruce, MD promoted to Professor (CHS)

Prashant Nagpal, MD promoted to Professor (CHS)

Anand Narayan, MD, PhD promoted to Professor (CHS)

Timothy Szczykutowicz, PhD promoted to Professor (CHS)
Tyler Bradshaw, PhD promoted to Associate Professor (CHS)

Laura Eisenmenger, MD promoted to Associate Professor (Tenure)

Matthew Shore, MD promoted to Clinical Associate Professor
Matthew Niemeyer, MD appointed to
Associate Professor (CHS)
Alisa Walz-Flannigan, PhD appointed to
Associate Professor (CHS)


A career in academic medicine is more than a job — it’s a calling. UW Department of Radiology faculty balance the art of teaching, clinical practice, and the pursuit of groundbreaking research, all while shaping the future of medical imaging. But with so many responsibilities, navigating the career landscape can be challenging.
That is where the professional development team comes in. The department recognized the value of aiding and advising the faculty to ensure they reach career milestones. The first step was establishing the role of vice chair of faculty development and enrichment.
Jessica Robbins, MD holds the distinction of being the department’s inaugural vice chair of faculty development and enrichment, a position she has held since 2018. Dr. Robbins’s early career experiences influence her approach to the role.
“Many of the challenges I faced as a junior faculty informed the processes we developed to make the experience of going through promotion seamless and less onerous,” Dr. Robbins said. “I now meet with each prospective faculty candidate to discuss the different career tracks and expectations of each track.”
Once established as the vice chair, Dr. Robbins began to create a team, and did not have to look far. Colleen Pilsner, MS initially joined the department in 2019 as a medical program assistant in the Section of Abdominal Imaging and Intervention, the same section as Dr. Robbins. She assisted Dr. Robbins with her faculty development work for nearly a year before she was officially hired as a professional development specialist in February 2022.
The team welcomed Chelsea Hanewall as the second professional development specialist in February 2024. Previously Hanewall had served as the graduate program manager in the UW School of Medicine and Public Health’s (SMPH) Medical Scientist Training Program, which enables students to earn both their MD and PhD in an integrated program.
When it comes to career guidance at the department, potential and current faculty can expect a personal touch. While SMPH provides broad support within the school, the faculty development team focuses on specific requirements and accolades for radiology. As an integral partner in the department’s faculty recruitment efforts, Dr. Robbins meets with every potential faculty hire to discuss their goals and explain the available resources and support for their enrichment. Then she and her team continue that relationship upon hiring.
“We created an onboarding and orientation meeting with new faculty to explicitly review the school’s expectations for promotion on the individual faculty member’s selected career track,” said Dr. Robbins. “We have developed a ‘playbook’ for promotion oversight committees to ensure that early career faculty receive the same guidance as they move through the early stages of their career leading up to their first promotion.”


On July 1, 2025, Nicholas Burris, MD began a 5-year term as the inaugural David A. Bluemke, MD, PhD Professorship in Radiology. Dr. Burris formally received the honor at the 2025 University of Wisconsin School of Medicine and Public Health Faculty Investiture Celebration, held on June 18, 2025.
“Dr. Burris has spent over 10 years pushing the boundaries of our understanding of aortic diseases through imaging, inventing new methods along the way,” said Department Chair Scott Reeder, MD, PhD. “His efforts are multi-disciplinary, highly collaborative and have uncovered new disease paradigms that may dramatically advance care for patients with diseases of the aorta. He is an exceptional researcher, inventor and colleague.”
Faculty member David Bluemke, MD, MSB, PhD’s parents, Dorothy and the late Duane Bluemke, established the professorship in their son’s honor in 2023 with the intent of attracting or retaining existing talent to the Department of Radiology. As a recent addition to the faculty, the professorship recognizes Dr. Burris for his work developing cutting-edge techniques in cardiovascular imaging.
In January 2025, Dr. Burris joined the department as an associate professor in the Section of Cardiovascular Imaging and director of aortic imaging. Previously, he practiced at the University of Michigan with a dual appointment in the Radiology and Biomedical Imaging departments. During his time in Michigan, Dr. Burris served as director of structural heart imaging and associate director of the multi-disciplinary aortic program (MI-AORTA). His research focuses on various techniques for advanced aortic imaging,
including the examination of 4D Flow MRI to define hemodynamic factors that promote risk of complications in aortic dissection, the subject of a 5-year, National Institutes of Health (NIH) R01 funded project. Further, he closely collaborated with industry partners on the invention and development of vascular deformation mapping (VDM), and image analysis technique for 3D quantification of aortic growth, an effort funded by an NIH Small Business Innovation Research (SBIR) grant.
At the investiture ceremony, Dr. Burris received support not only from his peers but from the individuals who made this honor possible.
“Having Dr. Bluemke and his family at the investiture ceremony was truly special,” said Dr. Burris. “While I already knew David well as a respected colleague, it was an honor to get to know his mother, Dorothy, and sister, Susan, more personally. Their family’s generous gift will have a lasting impact on my research and academic goals, and being able to thank them in person—and share a bit about myself and my own family—made the occasion especially meaningful.”
Erica Knavel Koepsel, MD, who was appointed to the Andrew B. Crummy Professorship last year, also participated in the investiture ceremony.


When she was a fellow at the UW Hospitals and Clinics, current Abdominal Imaging and Intervention faculty member Leslie Nelson, DO began researching how CTbased AI tools could visualize biomarkers of body composition changes in patients using semaglutide.
For the retrospective study, she reviewed data from 241 patients who had underwent abdominopelvic CT scans both within ve years before and within five years after beginning semaglutide use. She and the team looked for changes in visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT), intermuscular adipose tissue (IMAT) area, liver volume, and other markers.
Patients who had lost weight while using semaglutide showed decreases in VAT, SAT, muscle area, and liver volume, and an increase in liver attenuation. The weight gain group showed an increase in VAT, SAT, and IMAT, and a decrease in muscle attenuation.
The research team concluded that semaglutide therapy leads to patterns of body composition changes, with potential implications for cardiometabolic risk. The team also acknowledged that the readings were beyond what can be measured in a clinical setting, such as recording the patients’ weight or waist circumference. These kinds of readings could prove essential in understanding how medications like semaglutide can impact the body before and after treatment but can also provide suggestions for lifestyle modification that can help improve the quality of life for patients.
While she was still a fellow, Dr. Nelson presented her research at the 2024 Zachary Clark Radiology Research Symposium and secured the Best Oral Presentation by a Fellow award.
“I was honored to present our research and receive the award. It was very meaningful to share our project with the Department of Radiology, which we worked hard on throughout my fellowship” said Dr. Nelson.

The research was later published by the American Journal of Roentgenology (AJR) on September 4, 2024 and quickly garnered additional attention. It was highlighted by AuntMinnie in an article from September 11, 2024. The paper also received the Best of AJR Award in the Multispecialty section in December 2024.
AJR also included it as part of the “Study Guide for “Intrapatient Changes in CT-Based Body Composition After Initiation of Semaglutide (Glucagon-Like Peptide-1 Receptor Agonist) Therapy.”
A monthly feature by the publication, the study guides are designed to help build skills in evidence-based radiology.
“The mentorship I have received from the Department of Radiology has been the driving force behind our success, especially from Perry Pickhardt, MD,” said Dr. Nelson. “The mentorship from our co-authors, Matthew Lee, MD; John Garrett, PhD; and Joshua Warner, MD, PhD also helped guide and inspire me as an early career researcher.”

Faculty from the University of Wisconsin Department of Radiology and the Cyclotron Research Group traveled to Rotterdam, the Netherlands in March 2025 for the inaugural Radiology & Nuclear Medicine Symposium that the department and the department of Radiology & Nuclear Medicine at Erasmus University Medical Center (MC) co-sponsored.
As part of the growing relationship between the Department of Radiology and Erasmus MC, the international symposium offers an opportunity to connect and exchange ideas in-person. Coordinated by Rianne van der Heijden, MD, PhD; Edwin Oei, MD, PhD; Sandip Biswal, MD; and Kenneth Lee, MD, MBA. UW attendees also included Diego Hernando, PhD; Alan McMillan, PhD; Jonathan Engle, PhD; and Jason Mixdorf, PhD from the Cyclotron Research Group. Representatives from GE HealthCare were also in attendance, as the Department of Radiology and Erasmus MC operate the same equipment from that manufacturer.
In addition to nearly identical infrastructure and equipment, both institutions share common values regarding research and education. One of Erasmus MC’s core tasks is Valorization, defined as “the social or economic use of knowledge gained through research.” The Wisconsin Idea of UW–Madison is similar in that research, education, and resources should influence people’s lives beyond the boundaries of the classroom and campus. The Departments of Radiology of UW–Madison and Erasmus MC are also interested in pain imaging and sports injuries using quantitative imaging techniques, such as MRI and PET.
Although there are many parallels, a few differences contribute to the beneficial partnership between the two organizations, encouraging the exchange of ideas and technology.
“UW–Madison is really strong in the development of new MRI pulse sequences,” explained Dr. van der Heijden. “Erasmus MC is really strong in clinical translation of new techniques and population-based imaging amongst others. This makes us the optimal partners.” Differences also help both group’s research efforts.
“Even though we are conducting the same research, the individuals involved on each team may have a unique approach or thought process,” said Dr. Biswal. “Someone from Erasmus may have a different perspective on a study that our department may not have considered but may be beneficial to the findings or data.”
The inaugural 3-day symposium included presentations from UW–Madison and Erasmus MC faculty on topics related to musculoskeletal imaging, including techniques from radiological and nuclear medicine and image analysis.


In addition to sharing ideas and information through the presentations, the visiting faculty toured the Radiology and Nuclear Medicine Department at Erasmus MC. They viewed their host’s equipment, including the PET-MRI and the newly acquired total body PET-CT scanner.
There were also demonstrations in the newly established Erasmus MC / TU Delft MOtion Biomechanics & Imaging (MOBI) Lab. The MOBI Lab focuses on measuring and tracking joint loading during
movement in real time with a treadmill, cameras and fluoroscopy, providing opportunities for the early detection and treatment of osteoarthritis.
A select group of participants donned protective clothing and booties for a tour of the Erasmus MC cyclotron. The equipment has several built-in safety measures, including multiple barriers and leadlined walls.
Currently, the Department of Radiology and Erasmus MC are partnering on a clinical trial using PET-MRI for identifying chronic pain generators, as well as imaging research focused on musculoskeletal MRI, PET physics and AI.
Other coordinated efforts include studies of MRI cartilage segmentation, quantitative imaging in tendons, and perfusion of soft tissue masses.
In addition to continuing this work, the two groups have plans for future partnerships. That includes holding next year’s symposium in Madison. While this year’s symposium mainly focused on musculoskeletal imaging, it could expand to other topics, including neuroradiology and abdominal imaging.


On June 4-5, 2025, the UW Carbone Cancer Center hosted the inaugural Initiative for Theranostics and Particle Therapy (ITPT) Symposium. The ITPT, led by Jamey Weichert, PhD and Zachary Morris, MD, PhD, was launched in 2024; providing personalized treatment for patients with cancer and establishing world-class programs for theranostics and particle therapy research and education.
In addition to Dr. Weichert’s involvement as cochair, radiology faculty members Steve Cho, MD; Jonathan Engle, PhD; and Amy Fowler, MD, PhD served on the initiative’s executive committee.


The symposium featured leading experts in radiochemistry, radiobiology, dosimetry and theranostics, showcasing clinical applications and the latest advancements for tailored cancer treatments.
Drs. Weichert and Morris delivered opening remarks, transitioning to the keynote presentations by Steven Larson, MD, emeritus member of the Molecular Imaging and Therapy Service Department of Radiology Memorial Sloan Kettering Cancer Center and Richard Wahl, MD, professor of Radiology and Radiation Oncology at the Mallinckrodt Institute of Radiology. Additional sessions were hosted over the two-day symposium.
The symposium was made possible in part by the involvement and sponsorship of key theranostic companies and the Wisconsin Alumni Research Foundation (WARF).

On July 10-11, 2025, over 120 individuals from 21 institutions gathered for the UW Department of Radiology’s Magnetic Resonance in Madison Conference. The conference featured presentations by experts in the field, covering topics ranging from flow techniques, large language model (LLM) applications, and image reconstruction.
James Pipe, PhD, director of high value MRI as well as the MR Technology and Use Design (MRTUD) group, led the efforts to establish this inaugural conference. The organizing committee included members from the radiology and medical physics departments: Walter (Wally) Block, PhD; Diego Hernando, PhD; Samuel Hurley, PhD; Kevin Johnson, PhD; Mark (Marty) Pagel, PhD; and Oliver Wieben, PhD. GE HealthCare MRI Scientist Ty Cashen, MD, PhD also served on the committee.
“As sharing content electronically becomes easier, one of the primary purposes of conferences is networking with colleagues.” Dr.
Pipe shared. “We wanted to create a venue that was conducive to fostering discussions and building relationships.”
In addition, the organizers focused on creating an environment where students could gain experience presenting their work, a goal that they met with nearly 50% student participation from all attendees.
Li Feng, PhD from New York University; Garry Gold, MD from Stanford University; Catherine Hines, PhD from GSK; and Michael (Miki) Lustig, PhD from the University of California, Berkeley were keynote speakers for the conference. Dr. Feng discussed the history of radial MRI, an approach which allows faster scanning with fewer artifacts, and highlighted the many important contributions towards radial MRI methodology that have come out of UW–Madison.
Emphasizing the many important facets of working together, Dr. Gold shared his personal experience as a patient; pointing out the value, from a patient’s experience, of the work being done by attendees at the conference.
Dr. Hines, head of imaging at GSK, returned to her alma mater to give an enlightening talk on the role of imaging in drug development at all stages of the pathway.
Known for his many innovations in MRI, Dr. Lustig gave a lecture on using novel technology to monitor patient motion, respiration and heart rate in ways that could greatly improve the way MRI data is collected and processed. In addition to the presentations, 29 posters were featured, and both days included casual networking opportunities and group discussions.
Future conferences will be held on a biyearly basis.



Scott Reeder,
MD,
PhD and Thomas Grist, MD

MKE Lifestyle interviewed Scott Reeder, MD, PhD and Thomas Grist, MD for the article “Partnerships and Breakthroughs” published January 27, 2025. Focused on Wisconsin’s recent Tech Hub designation and the University of Wisconsin’s longstanding collaboration with GE HealthCare, the article also featured GE HealthCare VP-Advanced Technology Jay Hill.
“The Regional Tech Hub program is intended to catalyze investment in technologies that are essential to economic growth, national security, and job creation,” said Dr. Reeder. “In Wisconsin, the tech hub designation will capitalize on our global leadership in health care technologies to position Wisconsin as a leader in ‘precision health,’ or personalized medicine.”
GE HealthCare and UW announced a 10-year research collaboration in 2023, expanding on a partnership that has spanned over 40 years.
“Our initial collaboration focused on the co-development of magnetic resonance imaging (MRI) but has expanded to computed tomography (CT) and molecular imaging, and more recently to artificial intelligence, machine learning and digital health,” Dr. Grist explained. Read the full recap here.
The Milwaukee Journal Sentinel interviewed Pallavi Tiwari, PhD for the article “From chasing spy balloons to saving family farms, AI in Wisconsin has arrived,” published April 1, 2025. The piece explored how Wisconsin’s status as a growing hub for AI education and innovation, especially for medical research and healthcare. Read the full recap here.
Thomas Grist, MD was featured in The Washington Post’s “China’s restrictions on rare earths could hurt U.S. healthcare,” published April 18, 2025. In the article, health care experts explain how patients suffering conditions like brain tumors, liver cancer and heart attacks may be impacted if Beijing’s restriction of rare earth minerals leads to shortages. Read the full recap here.
Reeder, MD,
and
HealthTech interviewed Department Chair Scott Reeder, MD, PhD and Director of Informatics John Garrett, PhD for the article “How Can AI Help Transform Radiology?”
They explained how radiologists at the UW School of Medicine and Public Health are adopting and developing tools powered by artificial intelligence (AI).
Within the department, AI image reconstruction algorithms enable improved image quality and faster captures for MRI, CT and PET scans; cutting the scan time down by 30-50%.
AI isn’t only helping improve the scan duration and throughput; it’s being used to help analyze images and diagnose patients. Dr. Reeder shared how an AI tool can triage images from the emergency department.
“We see cases where an X-ray is acquired, and a minute or two later, it’s flagged and pops up on the workstation. I read that case next, and sure enough, if there is an abnormality, I call the emergency physician and say, ‘This patient has this urgent finding,’ and they can treat the patient immediately.” Read the full recap here.

Perry Pickhardt, MD was quoted in the BBC article “How AI can spot diseases that doctors aren’t looking for,” published January 16, 2025. The article examines the use of AI in opportunistic imaging, which is when medical images taken for one health concern are reviewed to potentially detect an undiagnosed issue. Read the full recap here.

Jonathan Engle, PhD co-authored “Making theranostics a priority in the fight against cancer” for Modern Healthcare with Ben Newton, PhD from GE HealthCare and Anthony Chang, PhD from BAMF Health. Read the article on Modern Healthcare’s website.

Tabby Kennedy, MD received the UW Health Physician Excellence Award for Clinical Educator.
Dr. Kennedy developed two educational websites for learners across the world. Through her leadership in transforming the MD curriculum, she raised the prominence of radiology.
Known for her clinical expertise and mentorship, she holds learners to the highest standard while inspiring confidence and growth in those around her.
Reinier Hernandez, PhD received a Distinguished Honors Faculty Award. In addition, the FDA has cleared an Investigational New Drug application for ART-101, developed by Dr. Hernandez’s lab to treat prostate cancer.
Richard Bruce, MD; Dania Daye, MD, PhD; and Erica Knavel Koepsel, MD were selected for UW Health’s Physician Leadership Development Program.
Medical student Max Golden was selected as a Top 20 Presenter at ESGAR for his abstract, which David Kim, MD and Perry Pickhardt, MD co-authored.
Kenneth Lee, MD co-authored “Plateletrich plasma for patellar tendinopathy: a randomized controlled trial correlating outcomes and quantitative imaging,” which has been selected for “Best of Radiology Advances 2024.”
Radiology featured an article written by Anand Narayan, MD, PhD and Dania Daye, MD, PhD titled “Six Steps to Improving Health Equity Using Quality Improvement and Patient Safety Tools.”
Ran Zhang, PhD received a 2024 Editor’s Recognition Award for reviewing with Distinction from Radiology.
Paul Laeseke, MD, PhD and JP Yu, MD, PhD received a 2024 Journal of Vascular and Interventional Radiology (JVIR) Editor’s Award for Outstanding Laboratory Investigation.
Giuseppe Toia, MD; Meghan Lubner, MD; and Matt Lee, MD’s work on workflow interruptions was featured in Radiology Business.
The Imaging Wire featured two papers authored by faculty members:
B. Dustin Pooler, MD; John Garrett, PhD; Matthew Lee, MD; and Perry Pickhardt, MD’s publication “CT-Based Body Composition Measures and Systemic Disease: A Population-Level Analysis Using Artificial Intelligence Tools in Over 100,000 Patients.”
J. Louis Hinshaw, MD participated in a “BackTable” podcast, about multidisciplinary approaches to renal cancer care.
Tim Szczykutowicz, PhD’s paper studying the best practices for scan speeds and duration in the article “Are CT Scans Too Slow?”
Christoph Lee, MD, MS, MBA was featured in the AuntMinnie.com article “SaMD-based AI is poised to ‘transform clinical care.’”
Emeline Hanna, a graduate student advised by James Pipe, PhD, was awarded a Graduate Research Fellowship from the National Science Foundation (NSF).
Elizabeth Burnside, MD, MPH was a guest on the “Contrast & Clarity with the JACR” podcast, focusing on AI in radiology.
Weibo Cai, PhD was elected as a fellow of the American Association for the Advancement of Science (AAAS).
Dr. Caialso won a 2025 American Institute for Medical and Biological Engineering Professional Impact Award, receiving the Mentoring Award.
Joshua Warner, MD, PhD was featured in the Microsoft blog “Developing nextgeneration cancer care management with multi-agent orchestration.”
Dr. Warner also achieved board certification in Clinical Informatics (CI).
In addition to celebrating the graduates, the Resident Graduation Ceremony celebrated outstanding department members and educators.
Jamey Weichert, PhD; Tyler Bradshaw, PhD; and Steve Cho, MD were featured in the article “Theranostics and Particle Therapy” published in the Wisconsin Medical Alumni Association’s Quarterly magazine.
Pallavi Tiwari, PhD‘s article “AI Helps Identify Sex-Specific Risks Associated with Brain Tumors” was also featured.
Alisa Walz-Flannigan, PhD was featured in the American Board of Radiology’s (ABR) The Beam newsletter.
Mai Elezaby, MD; Tabby Kennedy, MD; Eric Monroe, MD; and Jessica Robbins, MD received Editor’s Recognition Awards with Distinction from RadioGraphics.
Tim Szczykutowicz, PhD received an Editor’s Recognition Award with Special Distinction from RadioGraphics.
Vinny Meduri, MD was selected by graduating medical students as a ‘hooder’ for the 2025 Graduation Ceremony.
The Journal of Computed Assisted Tomography (JCAT) recognized two publications for achieving highest score: Giuseppe Toia, MD’s manuscript “The Environmental Impact of Iodinated Contrast Media – Strategies for Optimized Use and Recycling”
Ran Zhang, PhD; Timothy Szczykutowicz, PhD; and Giuseppe Toia, MD’s manuscript “Artificial Intelligence in Computed Tomography Image Reconstruction: A Review of Recent Advances”
Allison Couillard, MD received the RSNA Roentgen Resident Research Award.
Kelly Capel, MD received the Resident Award for Outstanding Teaching by a Faculty Member.

Aaron LeBeau, PhD was featured in the “Radiolab” podcast episode “The Shark Inside You,” discussing his work developing shark antibodies for cancers.
Alexander Moeller, MD received the John H. Juhl Award for Clinical Excellence in Chest Imaging.
Jacob Anderson, MD received the Resident Award for Outstanding Teaching by a Fellow.
B. Keegan Markhardt, MD received the Medical Student Award for Outstanding Teaching by a Faculty Member.
CT Rad Tech Doug Verhulst and Ultrasonographer Chris Busse received the Resident Award for Outstanding Technologist.
Kevin McDonald, MD received the Medical Student Award for Outstanding Teaching by a Resident.
Ryan Woods, MD has been accepted into the Association of Academic Radiology (AAR) Radiology Management program.

George Carberry, MD completed his residency and Abdominal Imaging and Interventional fellowship at University of Wisconsin Hospital and Clinics in 2016. Currently, Dr. Carberry works as the head of the Interventional Radiology (IR) section at Radiology Associates of the Fox Valley, located in Neenah, WI. Learn more about Dr. Carberry, and his time at UW–Madison below!
What career milestones have you achieved since your time at UW–Madison?
Now eight years since graduating, I’m considered a “mid-career” radiologist which seems wild, because it feels like just yesterday I was still in training. In these past eight years I’ve become the head of the interventional radiology section in my group and have taken on additional administrative roles.
What’s your favorite aspect of being a radiologist?
Being able to image, diagnose and treat conditions of every organ system in the body – the variety keeps things interesting!
How would you say your training at UW–Madison has helped you in your career?
Residency and fellowship training at UW was very well-rounded. We had great training in all sections of radiology. This has been very helpful in my broad community-based practice.
What’s your favorite memory from your time at UW?
One memorable incident was when Mark Kleedehn, MD and I needed a cow liver for a poster we were doing on ultrasound
imaging. We picked up the frozen liver wrapped in plastic and stored it in the resident lounge refrigerator overnight. The next day we found the fridge leaking thawed cow liver juices all over the place. It took hours to clean up, weeks to get the smell out, and months until our co-residents forgave us.
What advice would you share with prospective and current trainees at UW–Madison?
Work hard and don’t beat yourself up for making mistakes – that’s why you’re in training, and these are the cases you will remember best.
Is there anything else from either your time at UW or your career after that you’d like to share?
UW is a fantastic place to get your residency and fellowship training. After graduating you will find that many radiologists don’t get the well-rounded and personalized training that we get at UW. We are lucky to have that experience!







Alumni and colleagues from across the country joined us for the first University of Wisconsin Radiology Summit hosted by the Department of Radiology. Don’t miss out on the perfect opportunity to earn an estimated 15 CME, catch up with new and old friends, and ski the beautiful mountains in Park City, Utah.
The early bird gets the freshest powder and best price! Early bird pricing and a group rate for the Grand Summit Hotel are available for a limited time.