Short History of American Child Protection Agency (Myers,2009) 1642: earliest legal actions
1869: IL Supreme Court overturns defense
“Parents should raise their children as they see fit”
1875: rescue of Mary Ellen Wilson
Civil War orphan, placed in home in NYC’s Hell’s Kitchen
Discovered by Etta Wheeler, medical missionary
No law or court to turn to for her removal from the home…
Approached Henry Bergh, founder of ASPCA
American Society for the Prevention of Cruelty to Animals
Removed Mary Ellen under this habeas corpus
Founded the NYSPCC
NY Society for the Prevention of Cruelty to Children
1875-1930’s
Non-governmental child protection societies
Great Depression: Roosevelt’s New Deal
1935 Social Security Act: mandated formation of state child welfare service agencies
You are part of a TEAM!
“ShakingBaby”Triad…Caffey,1946-70s…Pushbacksasearlyas1987…LegalDenialism1990…
Medical History
Whenwasthechildlastnormal?
Doesthestoryfit?
Caregiver’sresponsetotrauma?
Physical Exam
Sentinel Injury
Petechial hemorrhages
Psychosocial HX
Single or young parents
Unstable home in transition
Race
Lower socioeconomic status
Other forms of abuse or violence in the house
Multiple births
Birth, Developmental status
Prematurity
Delayed or handicapped
“Raccoon Eyes” Subgaleal Hematoma, delayed 1-3 days post injury
Bleeding between periosteum & fibrous galea aponeurotica of the scalp in the setting of trauma
Fracture of base of anterior skull base
Often spares the subcutaneous fat
Often no skin bruising over vertex
Racoon eyes delayed 1-3 days post injury
NAT HINT: Abusive:fragmentedhairswith split ends of different lengths
“raccoon eyes”
DDX: skull base metastatic neuroblastoma
Classic AHT “TRIAD”… Subdural Hematoma, Encephalopathy, Retinal Hemorrhage (ThetermTRIADisnolongerused…changedtoAbusiveHeadtrauma,2009)
“Thebabyfelloffthe couch…outofmyarms…” No history or conflicting/changing story
Fall from low heights (4-6 ft)
Multiple poorly constructed biomechanical studies in prior to 2008, looking at “falls”, animal models, computer modeling…
“noproof!”
Plunkett,2001,ForensicMedicine.FatalPediatric headinjuriescausedbyshortdistancefalls:75,000 playgroundinjuries,18deaths,
BUTno infants
“Outcomes literature”…severe intracranial injury is rare from short fall.
EPIC: 6 deaths under 5 yrs per 2.5 million
Chadwick et al, 2008: day care injuries: 2 deaths/6 million
2017: 24Newbornsin hospital fall from 2m: single linear skull fracture, no other significant injury
Imaging findings in “Fall from Low Height”
Impact Injury
3% linear skull Fracture
Associated Venous Subdural
NO parenchymal hemorrhage
uncommon, seen in intermediate 6-15 ft falls
SDH thin and focal without neurological changes/HIE
Subpial or SAH focal
Brain contusions rare, asymptomatic
No Ischemia
AHT Finding? Classic Arterial Epidural Hematoma Most often with blunt impact force
Accidental > AHT
Laceration of the middle meningeal artery
In Infants
With or Without Fracture
flexible skull
non fused meningeal arteries
Can see arterial injury without fracture
Fractures: Most common fracture in both AHT and Acc Trauma is single Linear Fracture.
“Egg Shell” Fracture: Increasing complexity of fractures correlated with AHT “Ping Pong” Fracture, seen at birth/newborn
On CT, DDX fracture versus suture… Plain film can be helpful. Bilateral Parietal skull fractures… If fracture crosses TWO sutures, increases predictive value for AHT.
SuturalVariant?Inforensiclit…
Mechanism of Injury
AHT/NAT
Accidental
High Speed MVA
Multiple impact trauma
Falling down stairs
“Crush”
TV cabinet falls on toddler
Adult fall with infant in arms
Frontal or occipital single impact trauma
Neonatalskullismalleable,bendsandreturns tonormalwithimpacttransmittingforces
Fall forward or backwards off monkey bars
Normal 2 year old
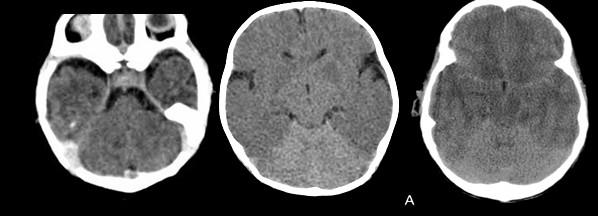
Timing of Injury: Can we use Cerebral Edema on CT? Loss of grey white juncture
White cerebellar sign
Pseudo Subarachnoid Hemorrhage
Reversal of Basal Ganglia Sign
Timing of Injury on CT: EDEMA? Bradburyetal,2013,SerialNeurimagingofAHT Postemaetal,2014,AgedeterminationSDH:surveyofradiologists…
Edema: first see in 1.2-2 hrs
Evident by 24 hours post injury
100% Evolution over time helpful 1.5 hours 6 hours
Do NOT age blood on CT by “density”…
Do not connect timing of event with age of blood on MRI… Bradford, Choudhary, et al 2013
On CT:
If SDH/homo variant: 1st hypodense component appear between .3 and 16 days
Last hyperdense component disappears between 2-40 days
If SDHHy, Hete: most common type at presentation
Last hyperdense component seen at 181 days
?rebleeding
MRI: Aging of Subdural Hematomas Vezina,2009 (referencetoexpectedevolutionofparenchymalhematomas,Bradley1993)
Hyperacute/Acute IC OxyHb <12-24 hr Iso - Dark Iso-Bright
Acute IC DeoxyHb 1-3 days Iso-Dark
Early Subacute IC MetHb 3 d to 1-2 wks
Late Subacute EC MetHB 1-2 wks to 1-2 mos
Chronic Hemosiderin Few wks – mos/yrs
SDH more unpredictable May not show hemosiderin deposition
Use the layering sedimentation debris for aging the blood
Age determination of SDH: A systematic review Sieswerda-Hoogendoorn, 2014 “MRI:Too much overlap between early stages and “pattern types” to predict age”
Overlap between
HyperAcute T1 Iso/T2Hyper Acute blood
and
T1 Hyper/T2Hypo Early Subacute Intracellular MetHb
1dayminimumto 13(-39) max indeterminant for timing of injury event
“Understanding subdural collections in Pediatric AHT.” Wittschieber et all, AJNR 2019, Institute of Legal Medicine
Wittschieber et al, AJNR 2024, …
Classification of “SDC” Subdural Collections Hahnemannetal,2023,CharacterizationofSDC… Wittschieberetal;.2024,SDH,ForensicImplications…
A. SDH: Subdural Hematoma, Homogeneous (Isodense, thin on CT)
B. SDHy: Subdural Hygroma, simple, no neomembranes, no fluid-fluid levels,
C. SDHHy Homo: Subdural hematohygroma, homogeneous variant; simple CSF, No neomembranes/flui-fluid levels, can have slight T2 hypointense signal
D. SDHHy, Hete: Subdural hematohygroma, heterogeneous variant, often with dependent blood products
E. cSDH: SDC with neomembranes, loculated fluid fluid levels
Do Not “AGE” Blood or correlate with timing of AHT Injury. Use Terms such as “Staging” or “Minimum Time to Appearance”
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation” Application of “minimum age concept”
A. SDH, Acute, Minimum 0 hour to 9 days
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation”
Application of “minimum age concept”
A. SDH, Acute
B. SDHy, Homogeneous subtype
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation” Application of “minimum age concept”
A. SDH, Acute
B. SDHy, Homogeneous
C. SDHy, Homogeneous
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation”
Application of “minimum age concept”
A. SDH, Acute
B. SDHy, Homogeneous
C. SDHy, Homogeneous
D. SDHHy, arrow?
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation”
Application of “minimum age concept”
A. SDH, Acute
B. SDHy, CT
C. SDHy, MRI
D. SDHHy, Homo, crossing normal veins
E. SDHHy, Hetero, CT “mixed density”
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation”
Application of “minimum age concept”
A. SDH, Acute
B. SDHy, CT
C. SDHy, MRI
D. SDHHy, Homo, MRI
E. SDHHy, Hetero, CT “mixed density”
F. SDHHy, Hetero, MR
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation”
Application of “minimum age concept” A. SDH, Acute
B. SDHy, CT
C. SDHy, MRI D. SDHHy, Homo, MRI E. SDHHy, Hetero, CT “mixed density” F. SDHHy, Hetero, MR
G. ?cSDH, CT, arrow?
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation”
Application of “minimum age concept”
A. SDH, Acute
B. SDHy, CT
C. SDHy, MRI
D. SDHHy, Homo, normal vein
E. SDHHy, Hetero, CT “mixed density”
F. SDHHy, Hetero, MR
G. ?cSDH, CT, ?neomembrane
H. cSDH, confirm with MR+, neomembrane with “enriched corners” I.
Do Not “AGE” Blood or correlate with timing of AHT Injury.
Use Terms such as “Staging” or “Age Estimation”
Application of “minimum age concept”
A. SDH, Acute B. SDHy, CT C. SDHy, MRI
D. SDHHy, Homo, MRI
E. SDHHy, Hetero, CT “mixed density”
F. SDHHy, Hetero, MR
G. cSDH, CT
H. cSDH, MR+, neomembrane with “enriched enhancement at corners”
I. cSDH, MR+, neomembranes, f-f levels
Application of “Minimum Age Concept” in Reporting, and For Example, cSDH: “cSDH is identified, accordingly to available study data, a minimum time Y=2 weeks has elapsed since the causative trauma has occurred”…mayseenewhemorrhagewith notrauma,minimaltrauma,orrepeatAHT.
Hahnemann et al, 2023, Characterization of SDC…
Encourage repeat Imaging, Consider high resolution imaging and/or contrast for neomembrane (Min day formation 9-10 days)
Hahnemann et al, 2023
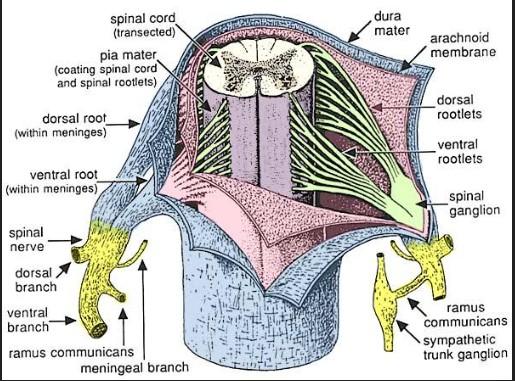
Normal anatomy of the Dura Squireetal,2009
Mack,2009
Intradural venous plexus prominence in infants up to 2 yrs then regresses, no muscular layer
Border cell zone = loose multilayer “flaky” cells adherent to the arachnoid membrane
“SDH”=intradural hemorrhageatthedura bordercelllayer
Added High Profile AHT Findings: Bridging vein rupture/thrombosis seen in up to 95% AHT at autopsy.
Yamashima,1984:
Vein 50-200 micrometers in subarachnoid space, narrows to 20 micrometers at dural cuff
9-11 large bridging veins
Smooth muscle cuff at dural entry zone, weak
Hanneman, 2015 “tadpole sign”
Choudharyetal, 2015
“lollipop” sign
Literature began to question whether the “AHT” shaking scenario had enough “force” to rupture these veins…
Nakagawa,2014PHDThesis:
“DetailedstructureoftheVenous Drainage….relevancetoNAT….”
Multiple accessory smaller veins draining directly into the dura…
Use of T1 COR Vasc to confirm rupture of bridging vein… Bridging vein injuries in shaken baby syndrome : Forensicradiological metaanalysis with special focus on the tadpole sign].
Wittschieber et al, 2021
No full rupture but often just “injured”…most literature now looks at high resolution gradient imaging
“Venous Injury” on MRI… using high resolution gradient imaging in AX and COR planes Neomembranes: form 9-21 days or longer,
corner“enriched enhancement”
Seenatcornerof membrane(whitearrows)
May, or more often may not, be associated with hemosiderin deposition
Be cautious!
Normal 9-12 major (50 total) bridging veins will traverse the hygromas, along with additional smaller veins…
If see “susceptibility” along the vein, may be acute or chronic injury.
SDH Rebleeding: nontraumatic (re)bleeding along the neomembrane…
Should be:
Small volume
asstd with old SDH and/or neomembranes
Asymptomatic
macrocephaly
Should not be associated with:
New neurological deterioration
New parenchymal brain injury
New subarachnoid hemorrhage
New subdural blood away from original SDH
“Rebleeding” 15% of priorAHT victimswithSDH, without acute neurological symptoms.
Bradfordetal2013
Feldman et al, 2015
Wright et al 2019
AHT “Triad”: Parenchymal Injury : “Hypoxic
Ischemic Injury” Pathophysiology:
Ischemic injury based on immunoreactivity to certain HIE mediated proteins rather than DAI or shear injury
Brainstem Injury, leads to Apnea
CPG: Central Pattern Generator
Not found in SIDS
Diffuse Global Watershed Partial Prolonged Unilateral Underlying the thin SDH
ASL in AHT HIE: useful? Mixed pattern of hyperperfusion/reperfusion injury and hypoperfusion
(Wong et al, J: ASL in AHT, J Neuroradiology 2017)
Normal ASL in 5 week old infant
1 mo old, AHT
5 mo old, post AHT, with resuscitation
Now must use other tools:
The Team!
Eye findings
Other “High Impact” Imaging Findings
HIE, aging of DWI
Bridging Vein Injury
Contusional Lacerations
Spinal Injury
Eye Findings 85% of AHT
Hallmark of AHT:
Macular Retinoschisis: Acc-Dec vitreoretinal traction
Added “High Profile” AHT Findings: Parenchymal Lacerations, Suggestive of AHT
Also, High speed mva
Infants under 6 months
Frontal and temporal
Layering blood products > sedimentation levels
Often at the subcortical white matter-cortex juncture
Likely rotational shear forces in the white matter
also called contusionalclefts
NAT: Spine MRI Cervical or Total, without contrast ½ to 2/3 of AHT have unsuspected spinal injury only .3-2.7% have bony abnormality on C spine
Brain swelling and herniation
Cord edema/ischemia Kadom et al, 2014, >75%
“Soft tissue or ligamentous injury” in the Cervical Spine Posterior soft tissue edema 50%
Interspinous ligamentous edema/injury
In cervical region, as high as 71% <1 year of age
Chaudhary, Kadom, Rabbitt 2019 Colombari, 2021
Craniocervical Dissociation Injury AHT
High Impact MVA
Posterior occipital impact injury with fall backwards
Spinal Injury patterns in AHT: SDH, compression fxs
[Choudharyetal,2014][Colombarietal,2021]
Nuchal ligament tear
Interspinous edema
Prevertebral fluid
Anterior vertebral body fracture T12 75% spine MRI: Extensive subdural/epidural hemorrhage, thecal sac tapering
Look for crowding and anterior displacement of the nerve roots
Age Differences: Cervical ST Injury <1 yrs
T-L Fx/Heme older 1-2 yrs
T-L juncture prevalence, ?rib cage stability?
Source of Blood? Extension from intracranial SDH
Ok if large volume SDH or PF SDH
If SDH small, will not have enough pressure/volume to extend below the foramen magnum
Primary Spine Injury:
Spine cord surrounded by meninges
Dura mata is single sheet in close contact with arachnoid layer
Artery/veins run between arachnoid and pia
Spinal nerve roots are site of CSF absorption
Surrounded by high density venous network, prone to bleeding
Post Mortem Studies:
Injury Patterns Cord injury: 20-70% with B-APP Pos axons…
Meningeal hemorrhage
Nerve root avulsion/dorsal root ganglion heme
Source?
Laceration of radicular veins at weak point passing from subdural to subarachnoid space
Supported by damage to dorsal nerve root avulsion, dorsal root ganglion hemorrhages
Spinal cord injury as Indicator of Abuse in Forensic Assessment of AHT, Colombari, International Journal of Legal Medicine, 2021
SDH is related to Birth Related Trauma… PotentialDelayed“Rebleeding”phenomenon? Subtemoporal hematoma: subpial variant with or without venous ischemia
Birth
Up to 68% associated with SDH
Asymptomatic
Thin <3mm
Posterior fossa, associated with tentorium/falx
Resolved within the first postnatal month without sequelae
Canyouspontaneously“bleed”intoBESSI?
< 2-6% of BESSI associated with SD Collections (1.7% hemorrhagic)
HINT: Check head growth charts to see if BESSI was even evident prior…
Expansion of the subarachnoid space can happen rapidly in the setting of acute trauma with arachnoid disruption
HINT: If see rebleed in prior BESSI, Recommend evaluation for abuse under 2 years of age.
Remember your Mimics:
Glutaric Aciduria type I
Metabolic/Genetic
Menkes syndrome
Glutaric Aciduria type I
Rare, Aut Recessive
Macrocephaly
Widened sylvian fissures and arachnoid spaces
SDH or SDHyromas
Rare RH
Rupture of arachnoid cyts
General High Predictive Value Rules for Imaging: AHT versus Non AHT AHT: Seen with Angular Deceleration forces without or with impact
RH
Particularly in combination with rib fractures
Spine Injury Pattern
Brain Injury
Lacerations SDH
Convexity (unilateral) or interhemispheric
No Impact Injry
HIE: Unilateral
Skull fractures
Complex, crosses two sutures
Non AHT: Seen in Translational forces from “short fall” history
Isolated Skull fracture
Epidural hematoma
Scalp swelling, impact injury
No predictive value:
Subarachnoid hemorrhage
Focal contusion
DAI
HINT: Pay attention to subcortical collections of blood in frontal regions…
“Certainty” index of AHT by mechanism of injury using Clinical Features Maguire et al, EstimatingtheProbability ofAHT:Apooledanalysis, Pediatrics 2011, 2017.
Meta review, confirmed AHT Under 3 years
Bruising
Seizures
Apnea
Long Bone Fractures
Retinal Hemorrhage
Rib Fractures
Kelly et al, 2015
Under 2 yrs
No history of trauma (90%)
No external evidence of impact (90%)
Complex skull fractures (79%)
SDH (89%)
HIE (97%)
2 mo old, normal vaginal delivery, no history, new onset irritability, scalp swelling
Start and End with the Imaging: Infantnotedtobeirritableatdaycare,presentedtoER…
The Triad … stayawayfromthisterm…it isalegalconvention
There is no single imaging finding that is pathognomonic for AHT.
HIE in the setting of SDH, RH, and/or Cervicomedullary injury predictive of AHT.
Use the Minimum Age Principle, try not to age blood
KEY: Child Protection TEAM
Arriving at a consensus, looking at all available data.
CT:
Edema by 1-2 hours
Hyperdensity 0-9 days (181???)
MRI:
(Hyper)Acute Blood T1 iso, T2 Dark: 0-2 days
Early Subacute Blood is T1 Bright: Day 2 (1?) Min
Enhancing membranes: Day 9 Min
Added Predictive Injury patterns:
HIE unilateral under SDH
Bridging Vein Injury “Tadpole”
Contusional Clefts
Craniocervical or Spinal Injury
Use your consensus statements in court.
U.S.vsDuran,2019:precedentusingthisconsensusstatementtodispute “expertmedicalwitness”testimony
Often time the Judges are the “gatekeeper” and heavily uses consensus statements and peer review literature.
See the evidence-based ACR Appropriateness Criteria for Suspected Child Physical Abuse (2016) at htps://acsearch.acr.org/docs/ 69443/NarraGve/
Legal Controversy… Check all your “lifelines” before you leap!
Check all your “lifelines” before you leap!
Check all your “lifelines” before you leap!
Understanding the Medical Literature Understand the LegaL Literature Refer to the ASPR Consensus Statement and Biblio Abbreviated
AHT Biblio 1. Nixon et al. ImagingofAbusiveHeadTrauma:AReviewandUpdate. Curr Radiol Rep. 2016.
2. Knox et al. SubduralHematomaRebleedinginRelationtoAbusiveHead Trauma.J Fam Viol. 2016.
3. Choudhary et al.Imagingofspinalinjuryinabusiveheadtrauma:a retrospectivestudy.Pediatr. Radiol. 2014.
4. Kadom et al. UsefulnessofMRIdetectionofcervicalspineandbrain injuriesintheevaluationofabusiveheadtrauma. Pediatr Radiol. 2014.
5. Vinchon et al. Subduralhematomaininfants:canitoccurspontaneously? Datafromaprospectiveseriesandcriticalreviewoftheliterature.Child Nerv Syst. 2010.
Abbreviated AHT Biblio 6. Piteau et al. Clinicalandradiographiccharacteristicsassociatedwith abusiveandnonabusiveheadtrauma:asystematicreview.Pediatrics, 2012.
7. Kemp et al. Neuroimaging:whatneuroradiologicalfeaturesdistinguish abusivefromnon-abusiveheadtrauma?Asystematicreview. Arch Dis Child, 2011.
8. Squier et al. Theneuropathologyofinfantsubduralhaemorrhage. Forensic Sci Int, 2009.
9. Sieswerda-Hoogendoorn et al. Agedeterminationofsubduralhematomas withcTandMRI:asystematicreview.Eur J Radio, 2014.
10. Wittschieber et al. Subduralhygromasinabusiveheadtrauma: pathogenesis,diagnosis,andforensicimplications. AJNR, 2015.
Abbreviated AHT Biblio 11. McLean et al. Doesintracranialvenousthrombosiscausesubdural hemorrhageinthepediatricpopulation?AJNR, 2012.
12. Palifka et al. Parenchymalbrainlacerationsinabusiveheadtrauma. ASNRmeeting.May 2014.
13. Adamsbaum et al. Datingtheabusiveheadtraumaepisodeand perpetratorstatements:keypointsforimaging. Pediatr Radiol, 2014.
14. Hahnemann et al. Imagingofbridingveinthrombosisininfantswith abusiveheadtrauma:the“TadpoleSign”.Eur Radiol. 2015.
15. Feldman et al. Initialclinicalpresentationofchildrenwithacuteand chronicversusacutesubduralhemorrahgeresultingfromabusivehead trauma. J Neursurg Pediatr. 2015.
Abbreviated AHT Biblio 16. Hsieh et al. RevisitingNeuroimagingofAbusiveHeadTraumain InfantsandYoungChildren. AJR. 2015.
17. Bradbury et al. Serialneuroimagingafterabusiveheadtrauma. J Neurosurg: Pediatrics. 2013.
18. Hedlund et al. NeuroimagingofAbusiveHeadTrauma. Forensic Sci Med Pathol. 2009.
19. Adamsbaum et al, commentary. Abusiveheadtrauma:don’toverlook bridgingveinthrombosis.Pediatr Radiol. 2012.
20. Yilmaz et al. MultifocalSignalLossatBridgingveinson Susceptibility-WeightedImaginginAbusiveHeadTrauma. Clin Neuroradiol. 2015.
Abbreviated AHT Biblio 21. Choudhary et al. Venousinjuryinabusiveheadtrauma. Pediatr Radiol. 2015.
22. Vezina. Assessmentofthenatureandageofsubduralcollectionsin nonaccidentalheadinjurywithCTandMRI.Pediatr Radiol. 2009.
23. McKeag et al. Subduralhemorrhageinpediatricpatientswith enlargementofthesubarachnoidspaces.J Neurosurg Pediatrics. 2013.
24. Matschke et al. Encephalopathyanddeathininfantswithabusivehead traumaisduetohypoxic-ischemicinjuryfollowinglocalbraintraumato vitalbrainstemcenters.Int J Legal Med. 2015.
25. Kadom et al. UsefulnessofMRIdetectionofcervicalspineandbrain injuriesintheevaluationofabusiveheadtrauma.Pediatr Radiol. 2014.
26. Choudhary et al. Imaging of spinal injury in abusive head trauma: a retrospective study. Pediatr Radiol. 2014.
27. Ronning et al, ParasagittalvertexclotsonheadCTinfantswith subduralhemorrhageasapredictorforabusiveheadtrauma.Pediatric Radiology, 2018.
28. Choudhary, Understandingtheimportanceofspinalinjuryinabusive headtrauma(AHT).Pediatric Radiology, 2020.
29. Rabbitt et al, Characteristicsassociatedwithspineinjuryonmagnetic resonanceimaginginchildrenevaluatedforabusiveheadtrauma. Pediatr Radiol.
30. Lenoe, 2017.
31. Choudhary et al, Consensusstatementonabusiveheadtraumain infantsandyoungchildren. Pediatric Radiology, 2018.
“Thebabyfelloffthecouch…bunkbed…outofmyarms…”
Suspicious HISTORY:
No history or conflicting/changing story
Fall from low heights (4-6 ft)
Multiple poorly constructed biomechanical studies in prior to 2008, looking at “falls”, animal models, computer modeling…
“noproof!”
Plunkett,2001,ForensicMedicine.FatalPediatrichead injuriescausedbyshortdistancefalls:75,000 playgroundinjuries,18deaths,
BUTno infants
“Outcomes literature”…severe intracranial injury is rare from short fall.
EPIC: 6 deaths under 5 yrs per 2.5 million
Chadwick et al, 2008: day care injuries: 2 deaths/6 million
2017: 24Newbornsin hospital fall from 2m: single linear skull fracture, no other significant injury
Imaging findings in “Fall from Low Height”
3% linear skull Fracture
Associated Venous Subdural
Intracranial Hemorrhage uncommon, seen in intermediate 6-15 ft falls
DH thin and focal without neurological changes/HIE
Subpial or SAH focal
Brain contusions rare, asymptomatic
No Ischemia
Impact Injury
SDHisrelatedtoBirthRelatedTrauma… PotentialDelayed“Rebleeding”phenomenon… Subtemporal hematoma: may be large, subpial Can resolve with no intervention
Birth
Up to 68% associated with SDH
Looney/2007, Rooks/2008, Whitby/2004
No vertex parasagittal clots, Ronning, 2018
Bridging vein rupture at birth? Found1.5%births, Bartoli, 2022
Asymptomatic
Increased incidence with forceps and vacuum, or C-section during labor, but also in normal vaginal deliveries
Thin <3mm
Posterior fossa, associated with tentorium/falx
Resolved within the first postnatal month
Rarely up to 3 months, but no rebleeding reported
NOevidencefordelayedonsetofacute collapse/coma/deathduetoexpandinghematomaor rebleedingintoabirthrelatedSDH
Canyouspontaneously“bleed”intoBESSI?
Rule: < 2-6% of BESSI associated with SD Collections (1.7% hemorrhagic)
HINT: Check head growth charts to see if BESSI was even evident prior…
Expansion of the subarachnoid space can happen rapidly in the setting of acute trauma with arachnoid disruption
Tucker,Choudharyetall,2016:
538 macrocephaly
21 SDC (2.9%)
18 w/ BESS
3 evaluated for AHT
1 confirmed
Greineretal,2013
108 Children with BESSI
6 (5.6%) Asymptomatic SDH
2 reported for abuse due to complexity
HansenetalOverall,2018:
Over50%hadothersuspicious injuries Clinicalpresentationcannotbe usedtoexcludeAHTinBESS
HINT: If see rebleed in prior BESSI, Recommend evaluation for abuse under 2 years of age.
Other controversies SDHiscausedby…DVT Deep Venous Thrombosis occurs first from other causes such as dehydration
Raises intracranial pressure
Leads to bridging vein rupture
Leads to ischemia (venous), RH, and SDH
Extravasation of blood into the subdural compartment
Pattern of brain injury (ischemia) is different with DVST, in all age groups
Rebuttals:
Anderstetal(2021): IPSS:
216CSVT(>69Heme,>20(9.3%)w/SDH)
Youngerpatients,under2years
2 evaluated for AHT from other findings
McLean(2012)
36infants/youngchildrenwithDVST,found noSDH
Hypoxic Ischemic Injury Why Unilateral pattern? No unilateral vascular injury
Why?
Seizure injury?
Excitotoxicity or altered metabolism triggered by superimposed subdural hemorrhage?
“Second impact syndrome”
TBI in adolescents
Similar SDH with unilateral HIE
WM restriction
Secondary Energy Fairlure & Apoptosis
Infantile traumatic brain injury with biphasic course & late reduced diffusion (TBIRD)
Acute (infectious) encephalopathy with biphasic seizures and late reduced diffusion (AESD)
Takase et al, Journal of Neurological Sciences, 2018.
“Bright tree appearance”
Starts in the subcortical white matter, pattern corresponding to the last unmyelinated white matter under 2 yrs age
Often “spares” the rolandic fissures
Immaturity of the brain
Inflammatory response to TBI
Altered cytokines
Neuroexcitotoxity due to excess Glutamine
Controversy: DoesSpontaneousSDHexistinInfants? “SSDHI”totheNeurosurgeons… Vinchon, 2010:
Prospective, admitted for “apparent head injury” found to have SD collection (n=164)
10% cases SSDHI (n=14)
Diagnosis of exclusion
Factors leading to SSDHI?
Dehydration?
Prior trauma?
Infection?