Neonatal Encephalopathy
HIE Pre Term to Term
Pre Lecture Test: Abnl DWI in a neonate with Seizures.
Choices: HIE….Infection (specific?)….Metabolic… other
Neonatal Encephalopathy/Hypoxic Ischemic Injury
PreTerm versus Term Patterns of Injury: 2 Principles
Selective Vulnerability
Certain cell types or cells at different stages of maturation are more susceptible to ischemia than others
Metabolic/Energy Demands
Greatest energy demands become the first to be “energy depleted”
▪ Greatest metabolic activity driven by Myelination
3 “Need to Know” items:
Gestational Age
Maturity of the Brain
Pre Term <34-36 weeks
Term >34-36 weeks
Severity of Hypoxic-Ischemic Event drop in O2, glucose drop in perfusion pressure
Duration of Insult
Neonatal Encephalopathy – PreTerm & Term
Metabolic Need drives Cytotoxic Cascade includes inflammation, hyper excitotoxicity, apoptosis
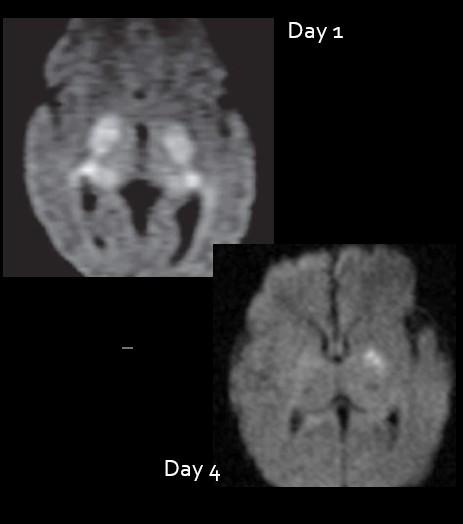
Image
Too Early or
Too Late!
Initial exam optimum at 72-84 hours (Follow up MR imaging at day 7-10 if discordant with clinical exam)
2 days
4 days Image too soon…underestimate injury. Image too late…miss injury.
Day 4 (72 hours)
Pseudonormalization
Day 7
Patterns of Injury in Neonatal Encephalopathy
Hypoxic Ischemic Injury
PreTerm Patterns
Diffusion Restriction is determined by duration & Severity of Insult
Thanks toT. Reher, MD
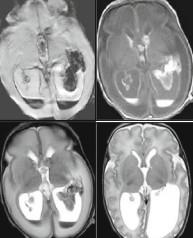
Pre Term Mild- Mod HIE: GM & IV Hemorrhage
I Sub ependymal, at CT Groove
II Into ventricles w/o hydro
III Vent enlargement >10 mm at atrium
[IV] PHVI Periventricular Hemorrhagic Venous Infarct
Grade I
Grade II
Grade III
Be careful of the Ganglionic Eminence! Can be seen up to 44 weeks gestation.
MRI: IVH Grades I-III
Selective Vulnerability of the PreTerm Ependymal Vasculature
Consequences; Arrested development of the interneuron oligodendrocytes and late radial glia Post hemorrhagic hydrocephalus
Periventricular Venous Hemorrhagic Infarction
Local damage to immature germinal matrix capillaries at the junction with primitive subependymal venous structures
Leads to obstruction of bleeding vein, with upstream thrombosis, finally hemorrhagic infarction
Back hemorrhages into the ventricular system or in association with Grade I-III GM hemorrhages.
PVHI (IV) Prognosis worse than grades I-III GM Heme
Predictors of Developmental Outcome on Term MRI
Volume loss in cerebral peduncle
Use mastoid view (Left mastoid view, right down)
Asymmetric myelination of PLIC on MRI
Classic PVL 22-32 weeks
Selective Vulnerability of Oligodentrocyte precursors
Pre Term Arteries:
First immature peripheral pial vessels on the surface grow to GM first, less to WM
Simple channels without muscular layers, no vasomotor capacity, simple endothelial endplates
Vascular “sparse” WM Zone up to 32 weeks
Pathophysiology:
Selective Vulnerability of pre oligodendrocytes (pre OLs) seen at 22-32 weeks, which are “vulnerable” to ischemia
▪ mature stages OLs begin to appear at 32-34 weeks
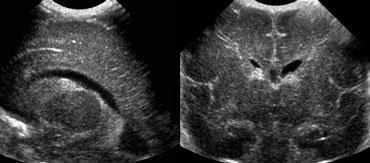
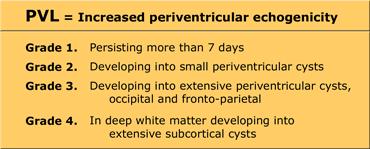
Classic PVL
“Flare”
Normal day 1-7
Grade I
Persists after day 7
Acute to Chronic PVL on MRI (often at Term)
White Matter Injury of Prematurity
Acute 2-4 days
WM T2 Hyperintensity
Foci of focal T1 shortening, not hemorrhage
Late acute/subacute phase
T1 shortening:
▪ Hemorrhage
▪ Inflammation (microglial inflammatory activation)
▪ Reperfusion in setting of weakened capillaries & increased venous pressure
White Matter Injury of Prematurity = PVL
Term Equivalent MRI – imaging often not specific
Flare/PVL at 28 weeks
Term Equivalent Late changes
PVHI at 32 weeks
Term Equivalent
Poor prognosis with:
Major destructive events
Cerebellar hemorrhages
IVH with PVHI
WM Injury of PM/PVL*
MRI WM injury most predictive of adverse NDI outcome 30 weeks
Term Equivalent
Patterns of Injury in Neonatal Encephalopathy
Term Injury Pattern driven by Metabolic Need
NE/HIE/HII
TERM Neonatal Encephalopathy to include HIE
FVM Fetal Vascular Malperfusion
Potential Maternal Risk Factors
Antepartum - inadequate placental perfusion
▪ Hypotension
▪ Pre eclampsia
▪ History of Infertility treatment
▪ Multiple gestation
▪ Prenatal infection
▪ Thyroid disease
Intrapartum
▪ Abruptio placenta
▪ Impaired oxygenation of mother
▪ asthma, PE, anemia, pneumonia
Potential Fetal Risk Factors
Antepartum
▪ Fetomaternal hemorrhage
▪ Fetal thrombosis
▪ Fetal bradycardia
Intrapartum
▪ Forceps delivery
▪ Breech extraction
▪ Umbilical cord prolapse
▪ Abruptio placenta
▪ Tight nuchal cord
Post partum <10%
▪ RDS
▪ Neonatal sepsis
▪ Shock
▪ Cardiac anomalies
Placental Pathology in Full Term Infants, Inflammation
Chorioamnionitis… FIR Fetal Inflammatory Response
“Brain is primed…”
Arrow: Post limb internal capsule PLIC
Open arrow: Ventrolateral nucleus of the thalamus
TERM Injury is driven by metabolic need=Myelination PLIC
Perirolandic subcortical WM
PeriRolandic Fissure
Post limb internal capsule PLIC
Ventrolateral nucleus of the thalamus
Term Severe Injury - MRI
Loss of Posterior Limb Internal Capsule “PLIC Sign”
T1 Normal Myelin Signal in
Term HII
Acute Injury
Subacute Injury
Lack (or delay) of return to normal PLIC myelin signal predicts poorer outcome.
Term HIE Patterns driven by metabolic need. Patterns determined
by duration and severity of injury.
Thanks toT. Reher, MD
Profound Insult and Short Duration: Metabolic Demand
Insult Pattern is Driven by Metabolic Need = Myelination
Grey Matter greater [GLU], results in greater excitotoxic injury
Basal ganglia, thalamus, perirolandic cortex, variable visual cortex, dorsal brainstem
Term HII Late Appearance HIE
Severe Asphyxia – Chronic
Acute/Subacute Injury
Early Day 4-10
Clinical: “toe walker” (spasticity with variable developmental delay and/or cognitive difficulties)
Mild to Moderate Insult, Short duration
“Partial Prolonged” Watershed Parasagittal Injury
▪ Save central gray at expense of cortex and WM
Moderate Insult & Prolonged: “Partial Prolonged” Mixed Patterns: Classic or Subcortical watershed injury often sparing central grey matter
Hemodynamic Instability Attempt at auto regulation
▪ But will ultimately decompensate
There has been metabolic conservation centrally (areas of myelination/function) at the expense of the periphery cortex or subcortical white matter.
▪ Often spares the perirolandic and basal ganglia
Subcortical depth of sulcus U-fiber watershed injury
▪ Opposite pattern to the central Profound/Short duration injury
Moderate or intermittent injury, Prolonged duration
Early: Often looks “normal”…due to symmetry
Late: Endstage MultiCystic Encephalomalacia
Thanks toT. Reher, MD
Confounders…Seizures, Hypoglycemia
Beware seizure activity Increases metabolic need
Lack of energy substrate
Deep White Matter Lesions, Watershed Hypoperfusion Injury, Inflammatory Response
(T1 hyperintense, non hemorrhagic)
First described 1991
Not seen in “normal” birth cohorts (Rooks et al,Tripler 2009)
2002 HIE manifestation
Signal Characteristics
T1 bright
Mildly T2 dark
+/- Diffusion restriction
▪ Ischemia/hypercellularity
No susceptibility blooming
▪ If seen, suggests blood products or venous sludging
Inflammatory cytokine response with activated Microglial release with Activated Oxygen and Nitrogen
Species, toxic to cells…
Preterm
What to do with diffusion restriction in a neonate? Not everything is HIE/NE!
HIE most common >80-90%
Trauma
Infection
Toxic/Metabolic Encephalopathy
Hypoglycemia
Kernicterus
Hypernatremia
Inborn Errors of Metabolism
Congenital lactic Acidosis…
What do I do with neonatal diffusion restriction? Pay
attention to pattern and time of presentation.
Birth Day 3 Day 7-10 1 month
Early Neonatal Sepsis
TORCH
HIE HPeV Rotovirus Group B Str
HSV E Coli Serratia Listeria Enterococci
Late neonatal Sepsis
H Flu Meningococcus Strept Pneumoniae
Day 5-7
Metabolic, normal at birth with decompensation, lactic acidosis…
Congenital Infections:
TORCH toxo, rubella, CMV, HSV
SCRATCHEZ syphilis, AIDS, chickenpox, HSV, enterovirus, ZEKA
CMV vs ZEKA
Both can have lenticulostriate vasculopathy on US
Both can have microcephaly, ventriculomegaly, migrational anomalies (lissencephaly/PMG), pontocerebellar hypoplasia
Both have white matter hyperintensities
CMV: DNA virus, herpesvirus family
ZEKA: RNA virus, mosquito borne Flaviviridae family
at the ependymal margin
ZEKA: occipital lobe cysts, band or clumped dystrophic subcortical calcifications, virus affects the footplates of the glial ray “ladder”
Neonatal Viral Infections:
Parechovirus (HPeV) in early neonatal period Rotovirus, in NICU
Transmitted in utero or perinatally (presents at 1-2 wks, Szs)
Dominated by leukoencephalitis due to cytokine induced inflammatory damage of theoligodendrocytes/ periventricular white matter
Periventiruclar White matter punctate ischemia
▪ In PreTerm, white matter edema with cysts
▪ Restriction in basal ganglia and thalami less common
Sagittal sinus thrombosis
Brainstem encephalitis
HPeV: Frontal WM, Extreme capsule
Rotovirus: more confluent, more severe effects on cognitive development
Streptococcus: most common cause of infection under 1 year of life
Key: ischemia without complex effusions
Streptococcus species
Group B: transmitted at delivery, early onset
Pneumococcus: >1 month, late onset
Complications:
Ischemic
▪ Inflammatory small vessel vasculopathy
Extra axial collections
▪ small, reactive SD, non restricting
Ventriculitis is uncommon
HSV: Congenital/Acquired in birthing process often presents at 3/5 days-2 weeks
▪ Herpes simplex encephalitis
▪ In neonate, Cortex
3 patterns:
FrontoTemp
PLIC
Cortex
progresses or “weeps into” the subcortical white matter
Watershed or “stardust appearance”
What do I do with neonatal diffusion restriction? Pay attention to pattern and time of presentation.
Birth Day 3 Day 7-10 1 month
Early Neonatal Sepsis
TORCH
HIE
HPeV Rotovirus Group B Str
HSV E Coli Serratia Listeria Enterococci
Late neonatal Sepsis
H Flu Meningococcus Strept Pneumoniae
Childhood
Neonatal
Sepsis: Early (0-7 days) vs Late (1 week to 1 month) Onset
Late: 1 week to 1 month
Acquired post natal
▪ Coag neg Staphylococcus
▪ Staph aureus
▪ Enterococci
▪ Multidrug resistant gram neg rods
▪ E. coli
▪ Other: Klebsiella, Pseudomonas, Enterobacter, Citrobacter, Serratia
▪ Candida, fungal
White matter injury with dilated ventricles
Cerebritis, Empyemas, abscesses
E. Coli
Key: subdural effusions/empyemas, ventriculitis
Second most common < 1 year
Complications: due to severemeningeal inflammation
Extraaxial collections 45%
▪ 50-60% “empyemas” with diffusion restriction
Ventriculitis with enlargement
Infarctions 25%
Typically small, underlying the areas of enhancing meningeal infection, cerebritis
3 week neonate
Serratia
Serratia marcescens
Gram neg
Often colonizes NICUs
▪ seen in preterm infants
Age: 2 weeks – 2 months
Complications
Multiple large parenchymal abscesses with striated internal appearance on t2
3 separate NICU patients, under 2 months
Bacterial Meningitis
immunologically normal infants older than 1 month, decreasing in immunized countries
Haemophilus influenzae type B (Hib)
Cerebritis
Subdural empyemas
Abscess
Ventriculitis/ependymitis
Obstructive hydrocephalus
N. meningitis
Streptococcus pneumoniae
Can mimic “embolic stroke”
Diffusion restriction but related to vasculitis
Meningococcus: gram neg N. Meningitidis
Older infants
Complications:
Extra axial subdural collections common
▪ prefrontal reactive > empyemas
Cortical gyriform enhancement
▪ Without restriction
▪ Cortical inflammatory changes with or without underlying laminar necrosis
Often without diffusion restriction 5 months 4 months
What the devil do I do with all that diffusion restriction? Pay attention to pattern and time of presentation.
Decreasing number of neonatal bacterial cases and increasing number of viral cases, because of increase in vaccine usage, better PCR tech.
Birth Day 3 Day 7-10 1 month
TORCH
Early Neonatal Sepsis
HIE HPeV Rotovirus Group B Str
Late neonatal Sepsis Childhood
HSV E Coli Serratia Listeria Enterococci H Flu Meningococcus Strept Pneumoniae
Enteroviruses
HSV1/2 EBV
Varicella /VZV
Neonatal Viral Infections:
Parechovirus (HPeV) young, Enterovirus in older
Varicella Zoster in older
Varicella Zoster
▪ Cerebellitis
▪ Cerebral Arteriopathy
▪ stroke, M1 propensity
Enterovirus
Most common in older childhood (5-10 yrs)
▪ Abrupt onset fever, headaches
▪ meningitis/encephalitis/myelitis
Neonates:
▪ 2-7 weeks
▪ Poor feeding
▪ Irritability
Varicella Cerebellitis
Inflammatory Arteriopathy
Post Test: Neonate with Seizures….Day 3. HIE vs Infection vs Metabolic?
Post Test: Neonate with Seizures….Day 3. HIE vs Infection vs Metabolic?
DDX: Metabolic, Infection
Look at age & presentation, patterns of diffusion restriction A B C
Human Parechovirus, Rotovirus Group B Strep
Maple Syrup Urine Dz
D. Maple Syrup Urine Disease
branched chain aminoacidopathy
BCAA: leucine, isoleucine, valine
BCKA: deficiency of Branched Chain keto-acid (BCKA) dehydrogenase enzyme
Maple syrup smell in cerumen first 24 hrs, later in urine day 5…
Sxs: poor feeding, dystonic movements (boxing/cycling), fluctuating opththalmoplegia, seizures
Must treat within first 5 days to maintain good neuro outcome
MRI:
Restricting Intramyelinic edema and myelin destruction
MRS: wide doublet at 0.9 ppm BCAA/BCKA accumulation