

DEVELOPMENTAL ANOMALIES OF NEURAL SPINAL AXIS

TERMINOLOGY

• Spinal Dysraphism
• Improper closure of midline mesenchymal, osseous, and/or nervous issues
• Spina bifida-incomplete closure of the bony spine


Craniorachischisis: Total failure of neurulation




Myeloschisis = Myelocele
“midline cleft anomaly of the spinal cord, partial or complete”

• Spina Bifida Aperta
• Older term
• Bony Defect with protrusion of material
• Simple meningocele
• Myelocele
• Myelomeningocele
• Closed versus open skin defect? cystic” protrusions through

• Meningocele “manque”
• Elongation of the conus nerve roots or neuroglial tissue, with attachment to the posterior dura with tethering, with or w/o lipoma, but without disruption of the posterior neural arch or overlying tissues
• Rare in isolation but seen in combo!






• Anencephaly
• Absent cranial vault
• Brain is “absent” = minimal amorphous neurovascular mass
• Exencephaly
• Absent cranial vault
• Normal “amount” of brain but abnormally developmed


Anencephaly





Iniencephaly



Closed or Open (encephalocele)





TARTORI CLASSIFICATION

TARTORI CLINICAL-RADIOLOGICAL CLASSIFICATION
• Open Spinal Dysraphism OSD
• Myeloceles
• Myelomeningoceles
• Hemimyelomeningoceles



• Closed Spinal Dysraphism CSD
• CSD with SubQ Mass
• Lipoma with dorsal Defect

• Fatty Mass or cyst
• Lipomyelomeningocele (LMMC)
• Simple Meningoceles
• CSD without SubQ Mass
Simple=Dimple
Failure of Disjunction & Caudal Regression

Intraspinal Lipoma
Dorsal Dermal Sinus
Tethered Cord
Filum Fibrolipoma
Complex
Failure of Gastrulation & Notochord Integration
Neurenteric cyst

Diastematomyelia
Caudal Agenesis
Segmental Spinal
Dysgenesis
OPEN SPINAL DEFECT MYELOMENINGOCELE MMC




Lemon sign
Banana sign
MMC CHIARI II
Tectal beaking, CC dysgenesis, hydrocephalus/colpocephaly, aqueductal stenosis, small posterior fossa with towering cerebellum, cerebellar tonsillar crowding and medullary kinking, syrinx

Fetal MR
Squared off frontal horns


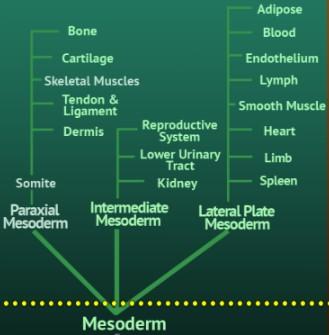
• 3 phases
• Gastrulation/Notocord Integration 2 nd-3rd weeks
• Two layer embryonic plate divides into three laters (ectoderm, mesoderm, endoderm)
• Notocordal cells enter and extend cranially
• Neuroenteric canal forms temporarily
• Primary Neurulation 3rd-4th weeks
• Notochord interacts with overlying ectoderm, fusion to form the neural tube
• Secondary Neurulation 5th-6th weeks
• Cells of Hensen’s node migrate caudally to presacral region
• Retrogressive differentiation & Canalisation
EMBRYOLOGY


PRIMARY NEURULATION DEFECT
OPEN SPINAL DEFECT OSD MYELOCELE, MYELOSCHISIS

The placode remains “flat” and meninges are deep to the bony defect




OPEN DEFECT, CHIARI II MYELOMENINGOCELE
MMC



Placodr extends beyond the spinal defect, into a dilated cyst



Post repair, difficult to differentiate underlying original anomaly



MMC pre repair
MMC post repair
MYELOMENINGOCELE (MMC)
• 30-46% asstd SCM Split Cord
Malformation
• Above, at, or below OSD
• 5% duplicated central canal
• 10% asstd Hemimyelocele
• Single or separate dural tubes
• One hemicord to MMC
• One hemicord could be:
• Normal
• Tethered by filum
• MMC at lower level
• Dorsal dermal sinus



TARTORI CLASSIFICATION


• Theories:

• Anomaly of Primary Neurulation with Premature Disjunction


LIPOMA WITH DORSAL DEFECT
CSD WITH (OR W/O) SUB Q MASS

Lipomyelocele Lipomyelomeningocele

Key: The intrathecal fat associated with the low cord must be contiguous with the subcutaneous fat!





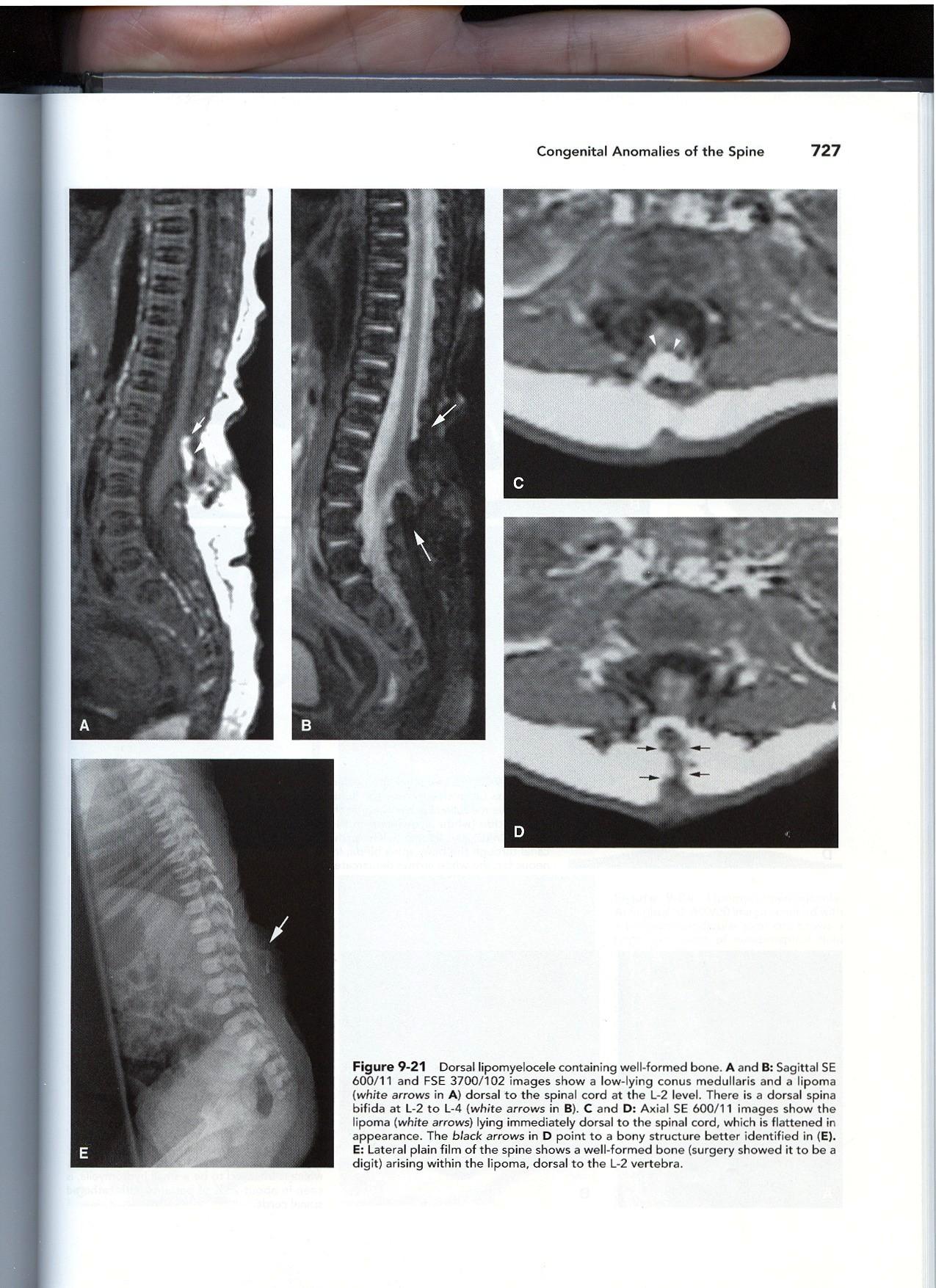

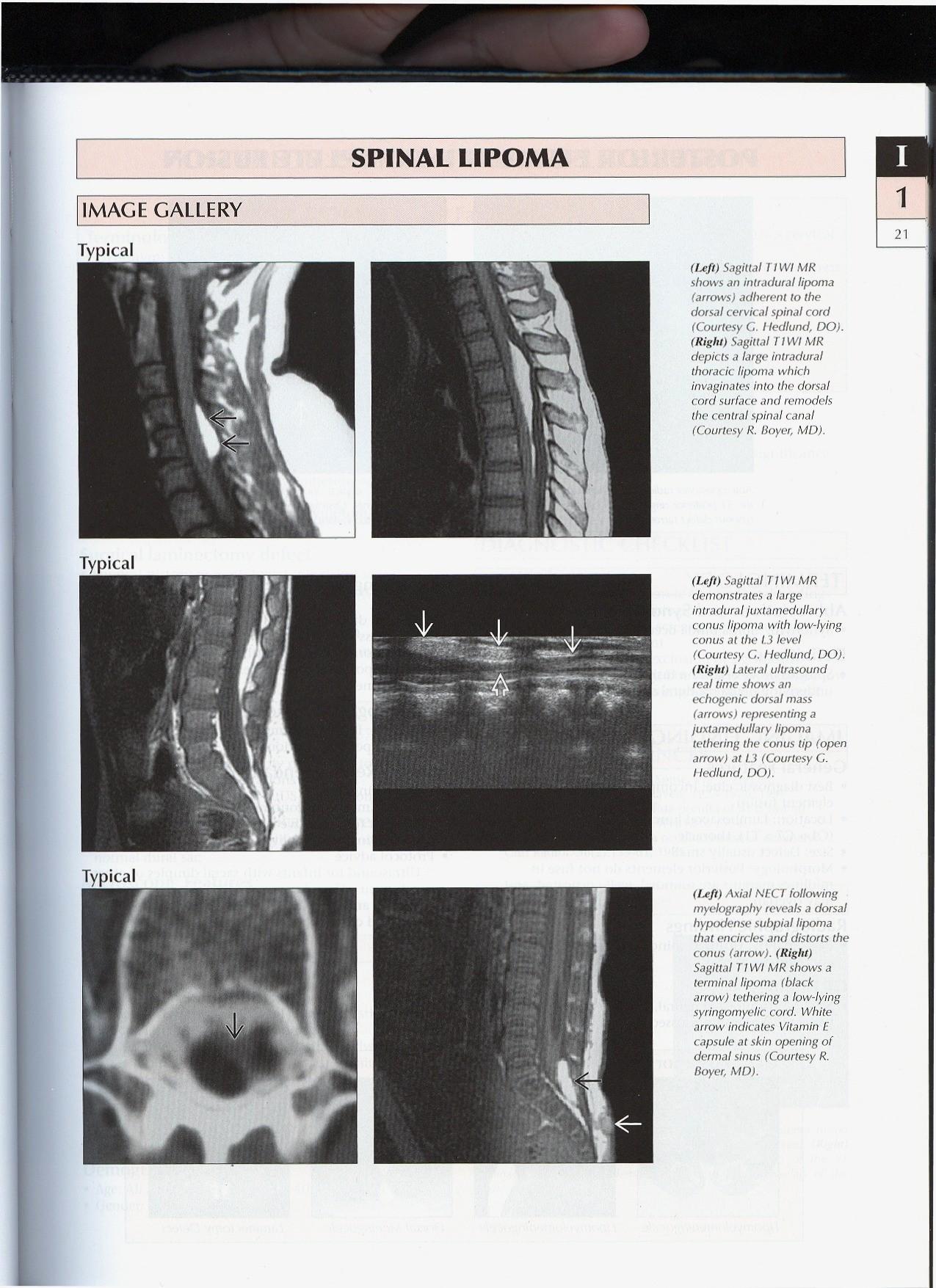
CSD WITHOUT MASS INTRADURAL/INTRASPINAL LIPOMA
• INTACT DURA
• Fat is NOT contiguous with the subQ fat
• Dorsal surface cord 75%
• Subpial, filling placode
• normal skin
• 2% syrinx
• “Lipoma with Dorsal Defect”
• Bony spine may or may not be intact





“LIPOMA
WITH DORSAL DEFECT”
INTRASPINAL LIPOMA
TERMINAL LIPOMA
TRANSITIONAL LMMC


Defined by geographic location of the fat… the further “south” the lipoma is located…


TRANSITION TO CAUDAL REGRESSION FEATURES

• Syrinx 20%
• Dermal Sinus Tracts
• Caudal cell mass anomaly
• Fibrolipoma of filum
• Sacral hypogenesis 25%
• Anorectal, GI, GU 5-10%
• Tumors:
• Dermoids/epidermoids, hamartomas, angiomas, arachnoid cysts

Terminal Lipoma/ Transitional LMMC

Terminal Lipoma with Dermal Sinus Tract in the setting of Caudal Regression
CLINICAL-RADIOLOGICAL CLASSIFICATION
CLOSED SPINAL DEFECT WITH MASS

• Closed Spinal Dysraphism
• CSD With SubQ Mass
• Lipomas with Dorsal Defect of bony canal
• LMC & LMMC
• Meningocele: No neural tissue in the cyst.
• Myelocysoceles
• Cervical or Terminal
• CSD Without SubQ Mass

Meningocele with Low Lying Conus
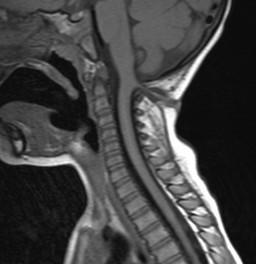
CERVICAL MYELOCYSTOCELE
• Dilated central canal/syrinx, herniates through bony defect
• Fibrous stalk with neural tissue
• +/- dilated subarachnoid space
• No hydrocephalus
• Better prognosis




TERMINAL MYELOCYSTOCELE
CSD WITH SUBQ MASS
• Rare, = Syringocele
• Central cord canal expands thru spinal defect
• Asstd terminal lipoma
• more rarely, in association with a LMC/LMMC or Teratoma
• Associated anomalies:

• Imperforate, anus, ambiguous genitalia, vertebral segmentation anomalies
• Hydrocephalus uncommon
• poorer prognosis





TARTORI CLASSIFICATION

SECONDARY NEURULATION
CAUDAL DEDIFFERENTIATION
• Normal Conus Position:
• Conus ascends in canal due to faster spinal bone growth
• 24 weeks L3
• 40 weeks inferior L2
• 3 months mid L2 >90%

Sacrococcygeal hypogenesis= caudal regression




CSD: WITHOUT MASS SIMPLE
• “Tethered Cord”
• Intraspinal Lipoma/Transitional LMC
• Filum Fibrolipoma
• Tethered Low Lying Cord
• Dermal Sinus Tract
• Is it draining?


“The Dimple…”
THICKENED FILUM FIBROLIPOMA OF THE FILUM TERMINALE
• Normal Filum > 1mm at L5-S1, axial plane, similar to adjacent nerve roots
• Conus may be normal or low in position



Watch for loss of the normal “pointy: conus or abnormal posterior “tethered” look to the filum at the conus
Chemical shift of fat on PD/T2










DERMAL SINUS
INFECTED DERMOID
Meningitis or Ventriculitis infectious or chemical due to release of cholesterol crystals
Abscess, mass effect on cord
Difficult to distinguish from epidermoid Tethering Arachnoiditis





TARTORI CLASSIFICATION

GASTRULATION & NOTOCHORDAL FORMATION AND INTEGRATION

Intercalation: notochord fuses with endoderm > primitive neurenteric canal (communication between the central canal of notochord and the yolk sac)



FAILURE NOTOCHORD INTEGRATION
= SPLIT CORD MALFORMATIONS
• Diastematomyelia
• Two hemicords,
• reunite below low lying conus
• Unilateral set of nerve roots
• Scoliosis 50-60%
• Diplomyelia
• Two hemicords, seperate dural sheaths
• Complete bilateral set of nerve roots
• rare


Hypertrichosis
Horse’s Mane
Fawn’s Tail

DIASTEMATOMYELIA I II





FAILURE NOTOCHORD INTEGRATION AND GASTRULATION
• Combined Integration/Intercalation
• AND Neurenteric Canal
• Persistent connection between the endoderm and ectoderm
• With or without split cord anomalies
Split Cord anomaly with Complex Dorsal Enteric Fistula



GASTRULATION ANOMALIES
• Dorsal Enteric Fistula
• Complete connection tw/ bowel and skin
• Dorsal Enteric Diverticulum
• Remnant of prox tract, near mediastinum or bowel
• Dorsal Enteric Cyst
• Remnant of mid tract, near vertebral canal
• Dorsal Enteric Sinus
• Remnant of post tract, near skin


• Intradural extramedullary 80%
• Intramedullary 10-15%
• +/- vertebral anomaly
• +/- DSM
• DDX Tumor





• Failure of Gastrulation & Notochord Integration
• Gastrulation anomalies
• Split cord anomalies
• Failure of Notochord Formation
• Aggressive Apoptosis of Notochord, ?vascular?
• Complex Caudal Regression syndromes – Caudal Dysgenesis/Agenesis
• SFA = Segmental Spinal Dysgenesis
SEGMENTAL SPINAL DYSGENESIS SEGMENTAL AGENESIS

• Segmental agenesis or dysgenesis of the L or T-L spine
• Often combined with caudal regression or agenesis of the sacrum
• Segmental abnormality of the underlying spinal cord seen above and below the agenesis
• Horseshoe kidney, sits in kyphosis

FAILURE OF NOTOCHORD FORMATION SEGMENTAL SPINAL DYSGENESIS
ASSTD COMPLEX CAUDAL REGRESSION/AGENESIS
Extreme cases of caudal agenesis: insult to caudal mesoderm or notochord prior to 4th week - toxic, infectious, ischemic insult
• Lumbosacral Agenesis
• Bony Spinal and Dural Stenosis
• 15 % diabetic mothers



CAUDAL REGRESSION SYNDROME SIRENOMELIA
• Sirenomelia – Mermaid syndrome
• complete vascular hypoperfusion ?
• Complex vertebral anomalies, scoliosis
• GI, imperforate anus malformed genitalia
• GU, neurogenic bladder



SECONDARY NEURULATION CAUDAL DEDIFFERENTIATION CAUDAL REGRESSION ANOMALIES


CAUDAL REGRESSION TYPE I

Saber shaped conus or blunted conus, above T12


CAUDAL REGRESSION TYPE II


Low lying conus Look for sacral or coccygeal hypodevelopment or anomaly
May have associated fibrolipoma of the filum, terminal lipoma or transitional LMC/LMMC, terminal myelocystocele



Tip: Watch out for multiple findings! (Second finding is the hardest to find…)


VACTERL


• Vertebral anomalies
• Anorectal atresia
• Cardiac
• TE fistula
• Renal
• Limb anomalies



ANTERIOR SACRAL MENINGOCELE
• Embryology unclear
• 5% retrorectal “tumors”
• 2-3 decade, F=M
• Symptoms
• Mass effect
• Pain, nerve root
• Fluid shifts, HA’s
• Simple
• NF I
• Marfans
Scimitar or sickle shaped sacrum
• Dorsal & Lat Meningoceles, ?unclear etiology
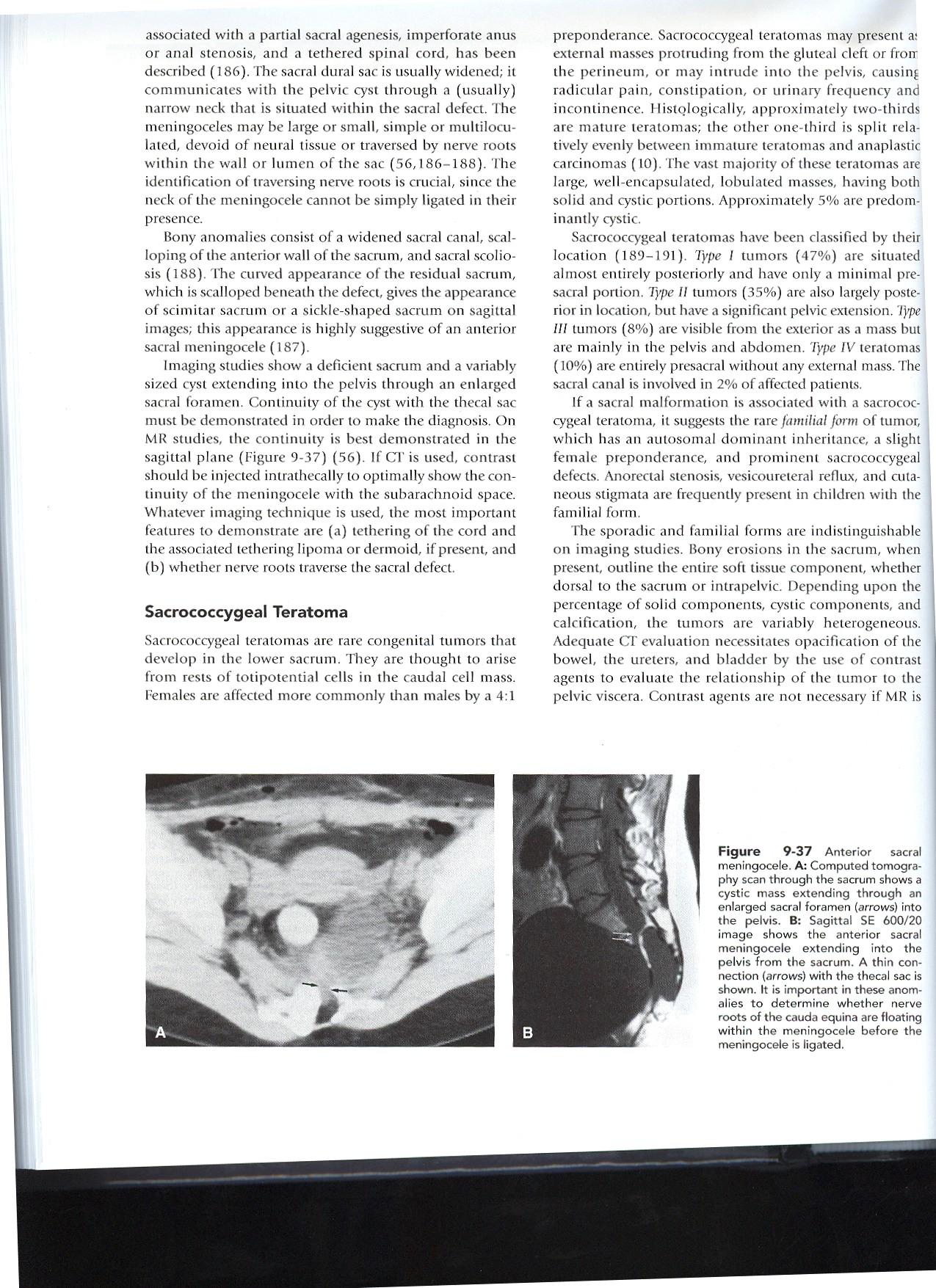



• Why Image?
• NOT simple meningocele
• Course of nerve roots, if they traverse the sacral defect, Surgery!
• HINT: look at the pelvis!




Bicornuate uterus
COMPLEX CAUDAL REGRESSION SACROCOCCYGEAL TERATOMA
• Origen?
• Totipotential cells of the caudal cell mass?
• Totipotential cells of Henson’s node at the primitive pit?
• females > males
• 2/3 mature



• 1/3 immature and anaplastic carcinomas
SC TERATOMA
• Classification
– Type I
• External 47%
– Type II
• External>Internal 35%
– Type III
• Internal>External 8%
– Type IV
• Presacral 10%
• Better prognosis (decreased incidence of malignancy) if:
• Extrapelvic
• Cystic








5 YEAR OLD GIRL WHO PRESENTS WITH ACUTE ONSET
ASCENDING LOWER EXTREMITY WEAKNESS…




