









BRIEFING: With the elections of President and Congress behind us, and a second Trump administration beginning on January 20, 2025, the question asked by many in reproductive biology and reproductive medicine is: what, good or bad, can be expected from this new administration? And while we sense a certain degree of pessimism among some colleagues, we believe, as we will here note, that there really is good reason for optimism.
It was a decisive win for Trump and the Republican party in the November 5 election, and it sent a message. As former President Barack H. Obama once noted, “elections have consequences.” Those consequences may be even more profound if the same party controls the presidency, the Senate and – as of the time of this writing – possibly also may continue to control the House, while in many cases also being able to count on a majority in the decision-making processes of the Supreme Court.
One cannot blame colleagues–for example those dependent on federal NIH grants–who are concerned, especially as many already experienced budget cuts to some grants under the Biden administration. Their concerns are further strengthened by Elon Musk’s suggestion that the government could safely cut $21 or $22 trillion in U.S. budgetary spending, as any such efforts, of course, would have to involve NIH budgets.
But at the same time, excess government spending cannot continue unchallenged because even our existing debt as a nation of ca. $35 trillion is already for all practical purposes unaffordable, considering the nation’s annual interest payments on this debt by now exceeds the country’s annual Pentagon budget. Cuts, therefore, will undoubtedly come; but the good news in all of this may be that these cuts will be supervised by Musk, who in taking over Twitter (now renamed X) has demonstrated that he is not only the world’s leading living inventor and business strategist, but also the world’s most effective cost-cutter.
Colleagues worried about their federal funding, moreover, can be assured that any administrative entity overseen by him in cutting national expenses will undoubtedly know how to distinguish between scientific merits of a grant and DEI (diversity, equity, and inclusion)-based funding, which during the Biden presidency – unfortunately – has dramatically increased.

For several good reasons, it also appears unlikely that a second Trump administration will give in to pressure from the Republican Party’s extreme right and/or religious wing (as Biden unfortunately did to the Democratic Party’s extreme left wing) because after his landslide election victory he is in a much more dominant position within the Republican Party than Biden ever was within the Democratic Party. During his first term he for all practical purposes abstained from any interventions in reproductive biology and the infertility field but, during the recent election campaign, demonstrated significantly more interest, and, clearly, in a positive way, by, for example, supporting in vitro fertilization (IVF) in the strongest terms.3We therefore see absolutely no reason to expect any adverse activities for the IVF field. Very much to the contrary, Trump very blatantly went on the record in favor of in vitro fertilization (IVF) practice and even proposed a national insurance mandate for IVF.3
It is also important to note that Trump’s defense of reproductive rights did not only involve IVF practice (i.e., both sexes) but, indeed, also the abortion issue, where Trump very openly (and at the risk of antagonizing abortion opponents in his own party) argued against a complete abortion ban. The abortion issue is, of course, likely the single most important issue for the extreme right in his party. As the election demonstrated, his support of a gestational age-limit for voluntary termination (though not for rape and threat to maternal life) as determined by each state, a stance by now supported by a large majority of the country’s population, proved successful because it apparently defanged the most potent argument of Democrats against the Republican party in the 2022 Congressional election that had ended up so disappointingly for Republicans.
Concerns about research restrictions and, maybe, a new opportunity
We would here, indeed, argue that considering Trump’s public position in favor of IVF, his second term may finally offer an opportunity to get rid of the so-called “Dickey-Wicker Amendments,” so named after Rep. Jay Woodson Dickey Jr of Arizona and Rep. Roger Wicker of Missouri who in early 1996 – in other words in the still very early days of IVF – spearheaded the enactment of two far-reaching Congressional amendments which assured the prohibition of public funding of gun violence research and human embryo research by the CDC and the NIH.4
Regarding research on human embryos, the language prohibits any federal funds from being used for “the creation of a human embryo or embryos for research purposes” or “research in which a human embryo or embryos are destroyed, discarded, or knowingly subjected to risk of injury or death.” The consequences have been tragic for IVF practice because it made IVF the only routine medical treatment excluded from all federal research funding in the U.S. It is easy to imagine how much further IVF practice would have evolved over the last almost 30 years, had federal funding been available for IVF research.
And here is why and how the Dickey-Wicker Amendments have survived unchanged for almost three decades: they under the law annually renew by being automatically attached to the appropriation bills of the Departments of Health and Human Services, Labor, and Education.
Considering Trump’s very strong statements in support of increasing utilization and availability of IVF, we see here an opportunity for the new administration to demonstrate its commitment to IVF by finally doing away with the Dickey-Wicker Amendments, at least as they relate to IVF. We would describe the likelihood that the Trump administration would end the prohibitions of federal research funding for IVF – if appropriately advised – as highly probable, and the time to start the lobbying process is now, so that the new administration can include this subject into the list of initial legislative changes planned for the first 30 days.
Who will become the new Health and Human Services (HHS) Secretary will, of course, greatly matter. We have heard considerable concern about Robert Kennedy Jr. (RFK Jr.) being chosen for this position and the concern is primarily based on his very controversial anti-vaccination beliefs. Those views (and his views on climate change) in our opinion make it unlikely that he will get a cabinet post. Instead, we suspect that Trump will use him in a similar function to Elon Musk as head for a specific task involving multiple cabinet departments, in this case charged with improvement of the general health of the U.S. population.
Politico recently suggested several other candidates as well for this position.5 They are listed below:




for all portraits, Politico)
None of these five candidates elicits the same negatives of RFK Jr. We, however, feel that Politico overlooked one serious candidate for the job, and that is Ben Carson, MD, who has remained close with Trump during his exile and as HUD Secretary during Trump’s first administration did an excellent job and would make a superior HHS Secretary.
In summary, contrary to the panic we hear expressed by many colleagues especially in academia and, indeed, also behind the scenes by some professional societies in the field, we feel optimistic about the future of reproductive biology and reproductive medicine during the upcoming Trump 2.0 administration. Making government less controlling can only help! REFERENCES

1. The Washington Post. October 29, 2024. https://www.washingtonpost.com/business/2024/10/29/elon-musk-2-trillion-budget-cuts-trump-election/
2. Dennis S. Financial Review. October 29, 2024. https://www.afr.com/world/north-america/musk-wants-3trn-cut-from-the-us-budget-it-d-be-difficult-20241029-p5km44
3. ASRM. Press release. August 29, 2024. https://www.asrm.org/news-and-events/asrm-news/press-releasesbulletins/trump-calls-for-ivf-ca-legsend-ivf-bill-to-gov/
4. Adashi EY, Cohen LG. JAMA Forum Archive. Published online November 5, 2015. Doi:10.1001/jamahealthforum.20150045. https://jamanetwork.com/channels/health-forum/fullarticle/2760581
5. Politico Staff. Politico. November 4, 2024. https://www.politico.com/interactives/2024/potential-cabinets/trump-second-term-cabinet/
David F. Albertini, PhD, Editor-in-Chief of the Journal of Assisted Reproduction and Genetics (JARG); Professor, Bedford Research Foundation, MA; Visiting Senior Scientist at The Center for Human Reproduction, NY; and Visiting Researcher at Rockefeller University, NY.
BRIEFING: One of the world’s most accomplished reproductive biologists offers his year-end assessment, with the conclusion that 2024 must be described as the ‘year of the embryo.’
In a twisted and somewhat unexpected turn of events, this year has brought out possibly the worst and the best when it comes to the biology and politics of human embryos. Following the recent trend of exploring the potential of pluripotent stem cells to generate equivalents of the peri-implantation stages of human development, a notable and remarkable series of papers appeared this year. Somewhat surprisingly, the latest research extended efforts of previous years by describing “synthetic” embryo models with properties not unlike those expected during or immediately following the time of implantation. Time will tell just how useful these models will be when it comes to deepening our understanding of why so many pregnancies fail at this critical juncture in human development.

And along with the technological breakthroughs at the heart of producing and characterizing such models, mounting ethical concerns this work delivers to a society already sensitized to the promise and perils this line of research constitutes, the politicization of all things embryos and human ARTs has muddied the conversation that should be occurring between science and society. At stake here could be opportunities to solve the perplexing riddle to explain the successes and failures that contribute naturally to species survival.
What rises to the surface of our collective quest to understand human development within the confines of technological bravado and ethical agency is both the biological and clinical relevance to the earliest stages of human development, and a sense of humility and respect
for the emergent complexities inherent to the fateful meeting of egg and sperm.
As articulated by Hopwood recently, the year 2024 in a sense represented a new dawning of human developmental biology, the overarching discipline of the past work on human embryos that now can be viewed in a context of where these advances will bring us into the future.1 This has been a difficult and challenging transition to effect in part because of the unintended mismatch between basic research, clinical ARTs, and ethical implications over the past decade, as elaborated upon by Brivanlou and Gleicher.2 While sorting out a system that achieves balance between these three domains is an ongoing effort of great import, original scientific contributions in 2024 have enlightened all parties as to a number of remarkable behaviors and properties exhibited by human embryos.
Most striking among these features of the human conceptus was the demonstration in 2016 that human embryos could manifest a level of self-organization in culture such that many of the post-implantation lineages emerged with little to no prompting and in the total absence of the female reproductive tract and female contribution.3, 4 What has followed these foundational observations is nothing short of a multinational effort that recognized, and exploited experimentally, the possibility that under appropriate conditions, these self-organizing principles were capable of recapitulating specific aspects of human development using pluripotent stem cells.
So it was that the propagation of blastocyst-like structures, or “blastoids” as they came to be known, was demonstrated yielding what appeared to be morphological equivalents of the preimplantation embryo at day 5/6 of development 5, 6 (and see Figure 1). The next developmental stage requiring demonstrating took aim at the epiblast itself and the germ layer precursors of endoderm, mesoderm, and ectoderm that would echo emergence of gastrulation-like events.7, 8 And finally, that pluripotent stem cells could be coaxed into pursuing fates associated with extraembryonic

components was achieved.9, 10
While we cite here only a subset of the papers contributing to this year’s advances with stem cell-based models, we note with a measure of caution that most all investigations in this area reveal “likenesses” in the form of morphology and gene expression patterns to human embryos, though conditions resulting in reproducible and efficient production of models have yet to be achieved. Nonetheless, the future is bright for further refinement of model systems that in time will avail their utility for many applications such as media testing, drug screening and the like.
Of the more highly suggested uses for such models are those underscoring the prevalence of miscarriage, in line with ongoing studies that have already been adopted using both placental and embryonic stem cells. 11 With mounting interest in deriving stem cells capable of following lineages that specify either embryonic (epiblast) derivatives, or those of extraembryonic nature (yolk sac, placenta), it can be anticipated that more complete and interactive models will result as has been exploited in some of the work reviewed above. 10
Arriving at this point in pursuit of understanding human development comes after a long and storied history using animal models as both guideposts and sentinels for technological implementation and conceptual design and rigor. 12 While the mouse has by far been the most experimentally and genetically tractable, the history of developmental biology evidences the casting of a broad net to have included invertebrate and vertebrate models from which fundamental principles of embryogenesis obtain. It is interesting in this light to keep in mind that like all eutherian mammals, the evolution of placentation coincides with the female gamete becoming a “yolkless” entity. 13
While to some the importance of this dimension to development may conjure up an appreciation for how the placenta evolved to sustain and nourish the developing fetus (against the backdrop of the well-known luteoplacental shift for establishment and maintenance of pregnancy), others have come to recognize that while not “yolky” the eggs of humans do depend on the maternal endowment of organelles and informational molecules that drive and support development up to, and possibly beyond, implantation. This unique feature of the human egg, and the remarkable self-organizing capabilities noted previously,3, 4 finds its basis in an ever-increasing body of evidence consistent with the idea that building a developmentally competent egg embodies much more than genetic determinants realized during the intraovarian process of oogenesis.
Two recent publications begin to delineate the nongenetic dimension of early development at two critical junctures-zygotic gene activation (ZGA) and compaction, the time when the first lineage allocation takes place whereby fetus and placenta begin to take on their proscribed future identities. 14, 15
In conclusion, the year 2024 has more than filled its
bill as the year of the embryo, bringing to the forefront the arena of synthetic embryos and all the while raising more questions than ever regarding the mysteries of early development that continue to capture the attention and imagination of all engaged in grasping the meaning of life for our species.
1. Hopwood N. Past and future of human developmental biology. Development. 2024;151(17).
2. Brivanlou AH, Gleicher N. The evolution of our understanding of human development over the last 10 years. Nat Commun. 2021;12(1):4615.
3. Deglincerti A, Croft GF, Pietila LN, Zernicka-Goetz M, Siggia ED, Brivanlou AH. Self-organization of the in vitro attached human embryo. Nature. 2016;533(7602):251-4.
4. Shahbazi MN, Jedrusik A, Vuoristo S, Recher G, Hupalowska A, Bolton V, et al. Self-organization of the human embryo in the absence of maternal tissues. Nat Cell Biol. 2016.
5. Sozen B, Jorgensen V, Weatherbee BAT, Chen S, Zhu M, ZernickaGoetz M. Reconstructing aspects of human embryogenesis with pluripotent stem cells. Nat Commun. 2021;12(1):5550.
6. De Santis R, Brivanlou AH. The treasure inside human naive pluripotency, generation of trophectoderm and blastoids. Cell Stem Cell. 2021;28(6):985-7.
7. Karvas RM, Zemke JE, Ali SS, Upton E, Sane E, Fischer LA, et al. 3D-cultured blastoids model human embryogenesis from pre-implantation to early gastrulation stages. Cell Stem Cell. 2023;30(9):1148-65 e7.
8. De Santis R, Rice E, Croft G, Yang M, Rosado-Olivieri EA, Brivanlou AH. The emergence of human gastrulation upon in vitro attachment. Stem Cell Reports. 2024;19(1):41-53.
9. Weatherbee BAT, Gantner CW, Iwamoto-Stohl LK, Daza RM, Hamazaki N, Shendure J, et al. Pluripotent stem cell-derived model of the post-implantation human embryo. Nature. 2023.
10. Oldak B, Wildschutz E, Bondarenko V, Comar MY, Zhao C, Aguilera-Castrejon A, et al. Complete human day 14 postimplantation embryo models from naive ES cells. Nature. 2023;622(7983):562-73.
11. Puscheck EE, Ruden X, Singh A, Abdulhasan M, Ruden DM, Awonuga AO, et al. Using high throughput screens to predict miscarriages with placental stem cells and long-term stress effects with embryonic stem cells. Birth Defects Res. 2022;114(16):1014-36.
12. Hopwood N. Species Choice and Model Use: Reviving Research on Human Development. J Hist Biol. 2024;57(2):231-79.
13. Rothchild I. The yolkless egg and the evolution of eutherian viviparity. Biol Reprod. 2003;68(2):337-57.
14. Fabreges D, Corominas-Murtra B, Moghe P, Kickuth A, Ichikawa T, Iwatani C, et al. Temporal variability and cell mechanics control robustness in mammalian embryogenesis. Science. 2024;386(6718):eadh1145.
15. Festuccia N, Vandormael-Pournin S, Chervova A, Geiselmann A, Langa-Vives F, Coux RX, et al. Nr5a2 is dispensable for zygotic genome activation but essential for morula development. Science. 2024;386(6717):eadg7325.
See also in this issue of the VOICE Dr. Albertini’s Photo Gallery on page __, as well as his article on our quickly evolving knowledge regarding oocyte aging, while in primitive primordial follicles a so-called resting stage in ovaries, on page __.
By Norbert Gleicher, MD, Medical Director and Chief Scientist at The
Center for Human Reproduction in New York City. He can be contacted through the VOICE or directly at either ngleicher@thechr.com or ngleicher@rockefeller.edu.

BRIEFING: On October 16, a consortium of law firms announced the filing of several nationwide class action lawsuits accusing genetic testing companies of misleading consumers about preimplantation genetic testing for aneuploidy (PGT-A) testing during in vitro fertilization (IVF) treatments. The lawsuits as of this point are only directed at a small group of leading commercial laboratories offering PGT-A testing. Other defendants can be expected to be added. Whatever the outcomes of these lawsuits will ultimately be years down the road, the IVF field has changed overnight with this filing. How far-reaching these changes will be is difficult to predict. Only so much is clear: they will be substantial, and will not only involve the clinical practice of IVF. They will affect the complete economic structure of the IVF field as it has evolved over the last two decades.
A brief introduction PGT-A is the most recent name attached to the idea that chromosomal evaluations of embryos prior to potential transfer into the uterus will allow for reliable selection of euploid embryos for transfer and, therefore, improve pregnancy and live birth chances, while reducing failures of embryo to implant and reducing miscarriages due to aneuploid embryos. The concept was initially proposed in the late 1990 as a promising way of improving IVF cycle outcomes and has since only grown in popularity, first under the name preimplantation genetic screening (PGS) and later renamed PGT-A. This rise in popularity remarkably occurred despite the test’s repeated failures to live up to its many promises of improving IVF cycle outcomes.

For those truly interested in finding out the clinical value of PGT-A (to this day a majority of IVF clinics, for reasons discussed below, appear really disinterested, unfortunately), it became increasingly apparent that, for several rather obvious biological and statistical reasons, PGT-A was—with very few exceptions—unable to improve IVF cycle outcomes and, in at least some subgroups of patients, actually significantly harmed chances for a successful IVF pregnancy.
In many developed countries—the U.S. included—clinical utilization of PGT-A has, however, despite significant negative clinical implications, paradoxically continued to increase. Why this has been the case appears to be multifactorial and will be one of the main subjects to be addressed by the courts in response to the recently announced class action lawsuits regarding PGT-A utilization in IVF brought by a consortium of law firms in several states 1. At this point, the defendants are only several leading commercial genetic laboratories (with likely more to come), accused of fraud in misleading consumers about the value of PGS/PGT-A testing. Whether only patients are considered “consumers” or whether this definition also includes IVF clinics appears as of this moment unclear but, very obviously, has considerable legal significance, considering that genetic laboratories and IVF clinics from the beginning have been splitting the income from every PGS/PGT-A cycle, with the clinic charging for performing the embryo biopsies and the laboratory charging roughly for performing the genetic analysis of the embryo biopsy. Genetic laboratories and IVF clinics, therefore, have practically identical financial incentives to perform PGS/PGT-A.
Though IVF clinics have so-far not be named as defendants in the recently filed class action suits (unless corporate entities owned genetic testing laboratories as well as IVF clinics), many appear—for several reasons—potentially vulnerable. As already noted, they receive basically identical fees from patients undergoing IVF cycles involving PGT-A and this fact has actually increased in importance for clinics in recent years, for two reasons. First, clinics receive payments for PGT-A from patients out of pocket in cash, undiscounted and in advance of cycle start and, therefore, without billing costs. This is the case because third-party insurers in the U.S. to this day generally do not cover PGT-A, even if they cover IVF. The reason is that they (rightly) consider PGT-A still an experimental procedure (to the best of our knowledge only one exclusive insurer for the infertility field currently also offers coverage including PGS/PGT-A). A second reason has been declining average cycle revenue at many IVF clinics because rapidly expanding coverage for at least limited IVF cycle numbers under general medical insurance plans and insurance-covered cycles usually being greatly discounted, average cycle reimbursement rates, especially in markets with considerable insurance coverage have plummeted. In such geographic areas, payments for PGS/ PGT-A biopsies, therefore, significantly increased proportional importance.
A Wall Street analyst, indeed, suggested to me in 2022 that for a rapidly growing number of IVF clinics PGT-A revenue, already then, represented the clinic’s profit margin. In other words, how often PGT-A clinics applied PGT-A to their patients IVF cycles often was the difference between being in the green or red with their budgets. Somewhat unsurprisingly, therefore, (one, of course, would hope that such financial incentives did not drive clinical utilization decisions), more U.S. IVF clinics, therefore, have been practically mandating PGT-A for most of their patients.
That the recently announced class action suits will reduce the country’s PGT-A utilization must be expected. While here addressed suits are the first in the U.S., they are not the first in the world (see further details below) and, likely, also not the last ones in the U.S. since other law firms outside of the consortium that filed here-discussed suits also already announced interest in the subject.

Declining revenue for PGT-A cycles, therefore, will undoubtedly affect the profitability of fertility clinics and, therefore, will diminish the commercial interest and the value of IVF clinics, a highly relevant subject for discussion, considering that private equity in recent years has been guzzling up private physician-owned fertility clinics.
And if clinic valuations drop, this in turn will put earlier private equity investments under water, as they no longer will be able to expect profitable exits in the usual five-to-seven-year time spans. In short, the fertility field over the coming years may see unprecedented changes arising out of these legal filings. They, indeed, may represent the most consequential occurrence in the fertility field since birth of Louise Brown on July 25, 1978, the first successful IVF pregnancy in the world.
A short history of PGS/PGT-A
The hypothesis that testing embryos for chromosomal abnormalities before transfer and that exclusion from transfer of aneuploid (chromosomal-abnormal) embryos would improve pregnancy chances for remaining euploid (chromosomal-norma) embryos was first proposed in the late 1990s by Yuri Verlinski, PhD, a brilliant geneticist colleague and friend with strong clinical interest in IVF. In full disclosure, he several years later ended up purchasing my Chicago fertility center, which allowed me to move full-time back to New York City.
His assumption that this kind of embryo deselection prior to transfer would improve IVF outcomes was built on three premises, all on their own correct but in unison, as was later learned, mistaken: (i) It was known that a large percentage (in those days believed to be over 50%) of miscarriages occurred because they demonstrated aneuploidies. (ii) Since only a small number of specific chromosomes were found to be abnormal in miscarriages, one could conclude that abnormalities of other chromosomes simply never implanted. (iii) It, therefore, at the time appeared correct to deduce that deselecting chromosomal abnormal embryos from transfers, should increase pregnancy and live birth
chances per transfer for remaining euploid embryos.
In addition, this (at the time PGS) hypothesis was, however, based on an even older hypothesis which to this day has remained a dogma in IVF practice: the socalled concept of embryo selection. The basis for this hypothesis—probably first formulated in the literature in the early 1980s by Jacques Cohen, PhD, at the time working in NYC—was the belief that in a complete cycle cohort of embryos, there must be embryos with significantly better and poorer pregnancy chances. The function of embryo selection, therefore, was to find the “best” embryo(s), once again with the purpose of improving pregnancy rates and time to pregnancy. After embryo morphology (the anatomy of embryos, how they look under the microscope), testing embryos for chromosomal abnormalities, there fore, basically became the sec ond-most-utilized embryo se lection method. Though both these hypotheses from the earliest days of IVF on, and to these days, by many colleagues still are con sidered dogmas, they both—as so often happens in medicine—proved to be mostly mistaken.
At the time, representative of a still very small first generation of IVF experts—like many other colleagues—I found myself severely disappointed when Belgian nvestigators in three small early clinical trials of what then was called PGS were unable to demon strate outcome benefits from PGS. When my col league at The Center for Human Reproduction (CHR) in NYC, David Barad MD, MS, and I were trying to find faults with the Belgian studies, recalculating their data statistically, we not only confirmed their conclusion that PGS did not improve IVF outcome; we, indeed, discovered in those data preliminary evidence that PGS may reduce pregnancy chances in older women in IVF cycles.
Though this experience already in 2007-2008 led us from being enthusiastic about PGS to becoming skeptics, it took many more years of research at our fertility


center, in collaboration with colleagues at other institutions, and in following the work of colleagues in The Netherlands, to not only fully convince ourselves of the shortcomings of PGS, but also to try convince others through a long list of publications in peer-reviewed medical journals. Because everybody besides us and a handful of colleagues from all over the world, at that time was still absolutely convinced of the PGS-hypothesis, our first paper on the subject in 2007, recalculating data derived from above-noted Belgian studies, was outright rejected by every decent fertility journal and practically all good general medical journals. It indeed for over a year remained unpublished in a drawer until The New England Journal of Medicine published a prospectively randomized trial of PGS by Dutch colleagues which, indeed, demonstrated declining pregnancy rates in older women as a consequence of PGS 92. Only then did Alan DeCherney, MD (see figure), at the time editor-in-chief of Fertility and Sterility, recall and publish our paper. 3
Why skeptics of the rapidly expanding utilization of PGS/ PGT-A initially failed to convince their colleagues

Ever since our first paper on the subject, our center and a very small group of colleagues from other countries fought what can only be described as a valiant battle against an overwhelming majority of colleagues in the IVF field, who increasingly presented themselves as “the experts” in the field and—as experts are supposed to do—quickly formed their own society: the Preimplantation Genetic Diagnosis International Society (PGDIS), which suddenly also considered itself qualified to issue professional guidelines regarding the utilization of PGS and later PGT-A. This society of alleged “experts” indeed became the official spokesperson for the field and—with it—the principal organization responsible for the misdirections of PGS/PGT-A practice.
But it was not alone because a core constituency of the society’s membership were representatives of the rapidly expanding PGS/PGT-A testing industry, which, of course, aggressively supported growing utilization of PGS/ PGT-A by fertility clinics and—flush from rapidly increasing revenue—was able to exert influence on other important opinion leaders, including the medical publishing industry and even professional societies.
As is customary, medical publishing, of course, used those perceived as leading “experts” on PGS/PGT-A as peer reviewers of submitted manuscripts. With few exceptions, they, of course, were (or at least pretended to be) geneticists, professionally biased and economically often obviously conflicted in favor of the PGS-hypothesis, as several among them were owners or co-owners of some of the leading PGS/PGT-A laboratories. Unsurprisingly, the medical literature became favorably biased toward PGS/PGT-A and unfavorably biased against opponents of the procedure who found it increasingly difficult to get their papers published (and, yes, we were among the latter group).
Though still unable to prove outcome improvements from PGS, “experts” however, because of all this help, had, nevertheless, absolutely no difficulties in explaining away critical studies. They, indeed, often even prevented them from being published. But fortunately, in science, the truth is difficult to suppress in the long run. But this is when the “expert” community (under the guidance of the PGDIS) for the second time misused its standing in the field by fabricating yet another false excuse for the failures of PGS/PGT-A. Once again, it was not the fault of the PGS/PGT-A hypothesis; the PGDIS, indeed, reaffirmed it in a formally published opinion in a medical journal (where the opinion did not even undergo peer review). Once again, the fault was mechanistic; the available technology to test embryos chromosomally was simply still not good enough to correctly diagnose aneuploidy in

embryos.
In other words, instead of finally starting at least to consider the possibility that the basic hypothesis behind chromosomal testing of embryos may be flawed (hypotheses in medicine, of course, very frequently turn out to be flawed), the new “expert” claim (or should we call it “excuse”) why PGS/PGT-A to that point had remained unsuccessful—publicly declared in a guidance document by the PGDIS without even the slightest evidence—was that the available technology used was still insufficient.
And this is when the PGDIS declared the need for another round of major changes how PGS/PGT-A should be technically pursued, what we and others have come to call PGS/PGT-A 2.0: Not only the most frequently affected, but all 46 chromosomes should be tested and the only acceptable methodology to be used (at that time) was to be next generation sequencing (NGS). Instead of biopsying embryos on day-3 after fertilization (cleavage-stage) by removing 1-2 out of 6-8 blastomeres, embryo biopsy would be simply moved to blastocyst-stage (days 5-6 after fertilization) and trophectoderm biopsy should replace blastomere biopsy with the removing of on average 5-6 cells. The rational for the latter was, in principle, that this change would improve accuracy of testing because it would produce a larger amount of testable DNA.
As has happened repeatedly in recent years with the introduction of many add-ons to IVF, changes in in procedure may not show immediately, but may become visible downstream only later. For example, that many infertile women demonstrate diminished ability to grow embryos in vitro to blastocyst-stage (a very important point we will return to) was obviously not considered when embryo biopsy was moved from cleavage to blastocyst-stage but, of course, automatically will, in at least some patients, affect cycle outcomes. Failure to recognize this fact, unsurprisingly, has, therefore, become the reason of considerable false outcome reporting with PGS/PGT-A.
We at the time coined the term PGS 2.0 for this new approach to PGS, which the IVF field—short of a very small number of skeptics—welcomed with open arms, once again convinced by “experts” that this, indeed much more accurate form of embryo testing for aneuploidy, would finally result in promised outcome improvements in pregnancy and live birth rates in association with IVF. But all improvements in techniques and technologies will, of course, remain ineffective if the underlying biological hypothesis is false.
Why – paradoxically – opponents of PGS/PGT-A rather than proponents were called upon to prove their point A widely accepted clinical, ethical, and practical rule in medicine has been since modern medicine evolved that the burden of proof lies with proponents of new treatments. Yet, when it came to PGS/PGT-A, this longstanding principle was put on its head: after also being unable to verify IVF outcome benefits for PGS/PGT-A with PGS 2.0, “experts” suddenly started arguing that it was upon skeptics to disprove the experts’ representations. In other words, the burden of proof was no longer on proponents of PGS/PGT-A, but on the skeptics, even though in the meantime significant such evidence had been published.
Our group in collaboration with colleagues from Rockefeller University’s physics department, for example, demonstrated beyond reasonable mathematical doubt that a 5-6-cell trophectoderm biopsy could never be representative of a blastocyst-stage human embryo. Even under biologically unrealistic best assumption of even distribution of aneuploid cells in mitotic aneuploidies, a valuable test would require a biopsy of over 25 cells, obviously a totally unrealistic expectation 4. But indisputable biological facts were apparently not enough and, indeed, were widely ignored.
In 2014, our fertility center, therefore, reached the conclusion that, with traditional scientific arguments failing to make an impact, only one “ultimate” study might have a chance of impressing the field: Building on the widely accepted fact that monosomic embryos practically never implanted (miscarriages never demonstrated monosomic aneuploidies), our center, in collaboration with two other NYC-based fertility centers, under an experi-

mental protocol offered infertile women who had undergone PGS but had no embryos reported to be euploid, the opportunity to transfer “aneuploid” embryos with reported monosomies (PGS laboratories at that point still reported embryos only binary as either “euploid” or “aneuploid”). The hypothesis of the study was that, should these embryos produce chromosomal-normal euploid pregnancies, this would represent the ultimate proof that embryo biopsies in PGS produced significant false-positive results.
In October of 2015, I presented at the annual ASRM Conference, in that year in Baltimore, on the last day in front of a packed house the first four chromosomal-normal embryos following transfers of embryos which—as of that point—every IVF clinic in the world would have discarded as untransferable 5. Several weeks later, Italian colleagues reported six normal pregnancies following such transfers in a research letter in The New England Journal of Medicine 6. But—almost shockingly—not much changed; the utilization of PGS by IVF clinics continued at even accelerate pace!
A new name for the procedure and further confusion by introduction of a third potential embryo biopsy diagnosis: “Mosaicism.” But, considering this news—and especially since our report within a few weeks was confirmed by Italian colleagues—absolutely no response was not an option for our “expert” colleagues and the solution was, once again, not a reevaluation of the underlying PGS-hypothesis but the claim that, once again, the testing procedure had been incorrect. Again publicized in an alleged guidance document, the PGDIS “experts” conclusion was that the “abnormal” embryos transferred that resulted in euploid pregnancies could not really have been “aneuploid,” but must have been “mosaic.” The seemingly logical conclusion, therefore, was that the mechanics of the procedure must again be “improved” by starting to report embryo biopsy results no longer binary as euploid and aneuploid but trinary as “euploid,” “mosaic,” and “aneuploid.” And to reemphasize the importance of this change and the expectancy that this change will, indeed, finally fully validate the procedure, the process also was renamed from PGS to PGT-A. We gave it the acronym PGS 3.0.
How problematic all these decisions were from the beginning is best reflected in the biological ignorance about preimplantation-stage embryology these two changes demonstrated: The “experts” in this case represented by another guideline document of the (PGDIS – defined “mosaicism” as evidence of a second (or more aneuploid) cell lineage in the 5-6-cell trophectoderm biopsy, a categorically incorrect biological definition of mosaicism. The correct diagnosis of mosaicism is, of course, presence of a second (or more) aneuploid cell lineage in a complete organism (arising from a single cell), in this case the complete blastocyst-stage embryo. And the difference between these two definitions is, of course, substantial and the mix-up is inexcusable.
This error is not only inexcusable on biological grounds because it is so obvious, as previously noted mathematical model established beyond reasonable doubt that 5-6, but also because more than one cell lineage in such a biopsy can do only one thing, defining the embryo with certainty as mosaic and with equal certainty as neither euploid nor aneuploid.
The same, however, cannot be said about the resulting diagnoses of “euploidy” and “aneuploidy” because here the “experts” picked definitions out of hot air: “Euploidy” was originally defined as <20% aneuploid DNA in the biopsy (by correct definition any aneuploid, strictly speaking, even a single aneuploid cell, renders an embryo mosaic) and is by now defined by various PGT-A laboratories as <40% and, by some, even as less than 50% aneuploid DNA. In other words, a significant portion of currently as “euploid” reported embryos in reality are mosaic embryos. And similarly, “aneuploidy” without any data in support, was arbitrarily defined as >80% aneuploid DNA, again suggesting that at least a minority of such cases may also be mosaic embryos.
While it initially was unclear how the PGDIS concluded that mosaicism should be defined by 20-80% of a second (or more) cell lineage, Santiago Munné, PhD, probably the historically most important “expert” on PGS/ PGT-A in the world, currently according to the PGDIS website the Scientific Director of the Center of Repro-

ductive Medicine of the Maastricht University Medical Center in The Netherlands, in a paper in Reproductive Biomedicine Online offered a rather astonishing explanation. It went something like this: Since a trophectoderm biopsy on average involves 5 cells, “mosaicism” (under the unique definition of PGS/PGT-A “experts”) would have to mean that between 2-4 of these 5 cells had to be aneuploid. In other words, between 20% to 80% of aneuploid DNA, therefore, would reflect a “mosaic” biopsy. Why a biopsy between, for example, 0.1% and 19% would still be considered a “euploid” result, was basically left unexplained; but the 80% to 100% range was explained as, simply, meaning all 5 cells of the biopsy were aneuploid.
That this was the explanation for the “guidance” released by the PGDIS in 2016 on how – going forward –PGT-A results should be reported to IVF clinics is, of course, almost unbelievable in its biological naiveté. What, however, can only be described as definitely inexcusable is that the IVF field accepted these definitions, obviously once again trusting in the expertise of the “experts” in the field.
That this enormous mislabeling of large embryo numbers after PGT-A has had – and to this day still has -highly significant clinical consequences is undeniable (more on that below). The degree of misdirection induced by the 2016 PGDIS “guidance” document is, however, best demonstrated by the fact, by now, most “experts” acknowledge that (at least some) mosaic embryos can be safely transferred, indeed producing similar pregnancy and live birth rates as PGT-A untested embryos. Indeed, even the ASRM acknowledged this fact. 7
The introduction of mosaicism as a diagnosis for embryos for all of these reasons, therefore, to significant degrees only further confused patients and the IVF provider community. Many IVF clinics, therefore, requested that genetic testing laboratories go back to binary “euploid” and “aneuploid” reporting. That many – if not most – truly mosaic embryos still have excellent pregnancy and live birth rates and can be safely transferred, however, raises serious clinical as well as ethical questions about such binary reporting because it, very obviously, leads to non-use and/or disposal of many embryos with potential pregnancy and live birth chances.
Summarizing the current status of PGT-A in the U.S. is, unfortunately, not a very satisfying experience. The very obvious main reason for this judgment is the fact that the utilization of PGT-A in IVF cycles is still continuing to grow, with increasing numbers of IVF clinics practically mandating the procedure to their IVF patients. It remains to be seen whether the very recent ASRM and SART Practice Committees’ opinion which finally (better late than never), formally concluded that PGT-A in general populations offers no outcome benefits whatsoever 7 , will have an impact. In the absence of changes in how “the business of infertility” has evolved over the last two decades, we frankly doubt it. IVF clinics owned by private equity, for example, have become the highest utilizers of PGT-A in the U.S. (Patrizio P. et al.; personal communication and unpublished data). They now also are responsible for more than half of all U.S. IVF cycles.

Considering the huge number of human embryos with pregnancy potential which over the last 20 years of PGS and PGT-A utilization have not been used and/or mistakenly discarded one cannot but conclude that PGS/ PGT-A must be viewed as one of the most damaging (and maybe the most damaging) fertility treatments ever introduced into practice. Its continuing utilization under current practice criteria, therefore, must be viewed with considerable concern.

And adverse consequences go significantly beyond only missed chances of conception. They also involve large numbers of often still young women who, after several PGT-A cycles which produced only “aneuploid,” non-transferrable embryos were told that their only chances of motherhood were through third-party egg donation or adoption. This was, indeed, a central theme in a prior class action suit regarding PGT-A in Australia. As ABC News recently reported, it settled for – in comparison to the U.S. lawsuits - a paltry $56 million 8. The case involved Monash IVF, one of the largest IVF provider chains in Australia and other countries (mostly in Asia) and was based on only 700 claimants (the number of potential claimants in the U.S. class action suits would, of course be dramatically bigger).
The ABC report quoted one of the lead plaintiffs, Michelle Pedersen and her husband Damien Pedersen, who donated their embryos to research after Monash informed them after PGT-A testing that they were “unviable.” As a consequence, they decided to adopt and only later learned that how their embryos had been assessed by PGT-A “could have been an error.”
In one sense, Monash (which as part of the settlement acknowledged culpability) acted even more irresponsible than most other IVF clinics using PGT-A because the clinic utilized so-called non-invasive PGT-A (niPGT-A) which does not rely on an embryo biopsy but extracts an embryo’s DNA from the culture medium in which the embryo was cultured. This very new technology, in most so-far published studies, however, turned out to be even more inaccurate than traditional PGT-A. Monash, indeed, admitted that this new test gave identical results to the standard biopsy test in only 75-85% of cases.
The use of niPGT-A outside of an openly declared clinical trial with appropriate informed consent is, therefore, not only legally inappropriate but ethically shameful. Yet several U.S. clinics also already offer it in replacement of the standard PGT-A test, a point apparently not even yet addressed in the recently filed class action suits in the U.S..1
What happened in the past is, unfortunately irreversible and – rightly – will enter into the otherwise highly successful history of IVF as a major black eye. The IVF field, however, now has the responsibility to at least minimize future damages. In practical terms this means that our professional organizations must, finally, speak out. It is not enough to recognize that unrestricted PGT-A in IVF was a failure. It must also be stated that the routine practice of PGT-A must be limited, and this must happen now!
It is not acceptable that the field of IVF continues to promote a procedure that offers no outcome benefits, while causing significant harm to so many infertility patients. The field also must learn from this experience and stop the promotion of several other recent add-ons to IVF, which, like PGT-A, have entered routine IVF practice with no evidence of utility. And, finally, we also must acknowledge the power of financial incentives in promulgating useless, and often harmful, procedures in infertility practice.
It is difficult to predict how the recently filed class action lawsuits will fare in the U.S. legal system. As we know, such lawsuits can take many years to resolution by either settlement or judgment. This author and several colleagues from other fertility clinics have in their publications repeatedly warned that, unless the infertility profession self-regulates and intervenes in the unrestricted practice of PGS/PGT-A, either government or the courts will step in.
For very obvious reasons, we in this case wished we had not been so correct in our assessment of PGS/PGT-A since approximately the year 2007. We, however, would like to take this occasion to issue one more warning: Be warned of many of these so-called PGD/PGT-A “experts!”
You will be seeing them resurfacing because of these recently filed class action lawsuits in return for fat expert-witness honoraria. And in many cases, you will be surprised to see on which side of the case they will appear, it will not be in defense of PGS/PGT-A!
How do we know? Because this has been the tactic of PGS/PGT-A “experts” all along: As here described before, all prior shake-ups of PGS/PGT-A (from PGS 1.0, over PGS 2.0, to PGS 3.0) were not voluntary, but occurred –uniformly based on work of skeptics – after prior representations of “experts” were no longer sustainable. Instead of acknowledging their prior mistakes, the “experts” always represented and concomitantly misrepresented themselves to the public as innovators of the next PGS/PGT-A they developed because they had recognized that the old PGS/PGT-A was not working as had been misrepresented to the public.
In full analogy, one, therefore, now can expect to see the resurfacing of some of these prominent PGS/PGT-A “experts” who for over 20 years have represented the foundation of PGS/PGT-A utilization in the U.S. and around the world, though not for the defense but the plaintiffs in those class-action suits. Those “experts,” after all, really have always pointed out the shortcomings of PGS/PGT-A. Didn’t you hear them?
References
1. News release. Accesswire, October 16, 2024. https://www.accesswire.co/929424/constable-law-justice-law-collabor...es-for-misleading-consumers-about-pgt-a-testing-during-ivf-treatment
2. Mastenbroek et al., N Engl J Med 2007; 357(1):9-17
3. Gleicher et al., Fertil Steril 2008; 89(4):780-788
4. Gleicher et al., Reprod Biol Endocrinol 2017;15(10:33
5. Gleicher et al., Fertil Steril 2015;104(suppl 3):e9
6. Greco et al., N Engl J Med 2015;373:2089-2090
7. Practice Committees of ASRM and SART. Fertil Steril 2024;122(3):421434
8. ABC News. August 22, 2024. https://www.abc.net.au/news/2024-08-23/monash-ivf-reproductive-industry-class-action-lawsuit/104259240

David F. Albertini, PhD, Editor-in-Chief of the Journal of Assisted Reproduction and Genetics (JARG); Professor, Bedford Research Foundation, MA; Visiting Senior Scientist at The Center for Human Reproduction, NY; and Visiting Researcher at Rockefeller University, NY.
BRIEFING: As women are, likely, born with all their oocytes (eggs), it is reasonable to assume that oocytes—like somatic cells—are subject to aging, as they sit there in ovaries subcapsular in the midst of highly primitive so-called primordial follicles, waiting to be recruited into folliculogenesis. In this article the author offers a state-of-the-art update on our now greatly improved understanding of oocyte aging.
Female gametes, called oocytes, are precious commodities with an unusual history and an even more remarkable stage presence. For humans, as is the case for mammals in general, oocytes present special challenges due to unique properties they exhibit in sharp contrast to sperm or any other somatic cells of the body. For one thing, no other cell persists in a dormant or primordial state for as long as oocytes do. While most oocytes stored in ovarian primordial follicles will never reach the stage of development and maturation capable of yielding a viable embryo following fertilization, those that do undergo long periods of dormancy before initiating growth and differentiation within a follicle that will ultimately undergo ovulation.
As a result of their long-term storage, oocytes become subject to the wear and tear of progressive and unstoppable somatic aging, a condition that takes its toll on those oocytes that have been stored over the long haul. Among the properties most likely impacted with respect to the impact of aging on oocyte quality, meiosis and the genetic consequences of aberrant spindle function and errors in chromosome segregation have dominated in the literature. But sustaining the oocyte in a suspended state of animation in its primordial form or realizing the events that guarantee successful growth and final maturation, emerges as a complicated matter as to how the process of oogenesis manages to keep this remarkable cells’ house in order over the course of our reproductive lifespan. 1
A new study from the laboratory of Melina Schuh, PhD, at the Max Planck Institute for Multidisciplinary Sciences in Germany, prompts us to think differently when it comes to sustaining the female germ cell pool over the course of time. Using a well-balanced and innovative set of investigational tools, asking the question of oocyte housekeeping in a new way Harasimov et al., turn attention away from the genome and towards the proteome as a sentinel for why and how to achieve the unique demands of longevity for the mammalian oocyte. 2 As with many frontline research efforts, this work challenges paradigms of the past and may in fact give substance to some of the more puzzling and perplexing aspects of oocyte aging implicit to current approaches for the treatment of human infertility. More on the topic of the oocyte proteome later!
That human oocytes demonstrate risky behaviors when it comes to reinitiating and completing meiosis has been recognized for years with the attendant focus on changes in recombination and spindle complexities offering insights into the maternal aging conundrum. 3 Much has been made of the oocyte aneuploidy problem across the age spectrum of humans with contemporary research efforts identifying many of the unusual properties of the specific proteins (and their timely post-translational modifications) drawn upon during chromosome alignment and segregation. 4-7 Drilling down on the proteomic players that orchestrate the meiotic dance of the chromosomes has until recently posed barriers to obtaining mechanistic insights that could guide and inform both research direction and clinical applications for the future. Herein lies the breakthroughs on proteomics in maternal aging.

Taking a variety of approaches that combine some human materials and an abundance of subject matter using the experimentally tractable mouse models, several laboratories are expanding our knowledge base on just what the oocyte stores, and in what form, beyond the traditional model of organelles and stored mRNAs and proteins that would be inherited by the zygote upon fertilization.2,8,9 While much of the “housekeeping stuffs” like mitochondria, Golgi complexes, and an endo-lysosome system have been known for years, 1 the demonstration of protein complexes of various kinds as both membrane-less condensates and lattices are now being viewed not only as reserves for future biosynthetic necessities during oocyte growth, maturation and post-fertilization events but as uniquely ling-lived assemblies subject directly, or indirectly, to the cumulative vagaries of advanced maternal aging. Notably, the extreme lifespan extending tendencies for proteins of oocytes are not unique to the oocyte itself but seem to be associated with the “house” withing which the oocyte lives, thrives, and potentially dies, -the all-important follicle in the ovary. 2
In a way, this line of thinking recapitulates a notion deeply embedded in the comparative biology of oogenesis having to do with the role of yolk as the nutritional substrate upon which most animals rely to support their post-fertilization development. 10 And not to short change how important the regulation of protein stores is to the many aspects of oocyte maturation and early development that have been linked genetically to arrested maturation or zygotic development, the substance of the maternal dowry is becoming appreciated for much more than contributions to the meiotic and mitotic spindle and the establishment of cytoplasmic-nuclear exchange at the all moments of zygotic gene activation.11, 12
Karyopherins are but one of many proteins now understood to perform essential functions in the embryo and having their origins during the growth and maturation of mammalian oocytes.13 And not only their biosynthesis and micromanagement over the lengthy lifespan of the oocyte are matters to be contended with, but the protein-based devices that constitute the Maternal Subcortical Complex (SCMC) are likely to be subject to some of the same rigorous controls exerted through proteostasis determining, in the end, which zygotes sustain term development and which do not.14
The final road to building and sustaining a good egg is long and punctuated by events and processes over a chronology that plays out over months in humans and weeks in a mouse. But the lifespan of an ovarian primordial oocyte is a lifetime, at least in terms of the years intervening menarche and menopause. Keeping the “egg house” in order thus becomes one of the great challenges in a society increasingly reliant upon Assisted Reproductive Technologies to manage and effect their family planning desires. The time has come to position the proteome and protein longevity on the basic science and clinical map for the future, something being enabled by the introduction of new experimental models of human ovary function. 15


1. Oogenesis. Coticchio G, Albertini DF, De Santis L, editors. New York: Springer; 2013.
2. Harasimov K, Gorry RL, Welp LM, Penir SM, Horokhovskyi Y, Cheng S, et al. The maintenance of oocytes in the mammalian ovary involves extreme protein longevity. Nat Cell Biol. 2024;26(7):1124-38.
3. Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2:280-91.
4. Hassold T, Maylor-Hagen H, Wood A, Gruhn J, Hoffmann E, Broman KW, et al. Failure to recombine is a common feature of human oogenesis. Am J Hum Genet. 2021;108(1):16-24.
5. Gruhn JR, Zielinska AP, Shukla V, Blanshard R, Capalbo A, Cimadomo D, et al. Chromosome errors in human eggs shape natural fertility over reproductive life span. Science. 2019;365(6460):1466-9.
6. Holubcova Z, Blayney M, Elder K, Schuh M. Human oocytes. Error-prone chromosome-mediated spindle assembly favors chromosome segregation defects in human oocytes. Science. 2015;348(6239):1143-7.
7. So C, Menelaou K, Uraji J, Harasimov K, Steyer AM, Seres KB, et al. Mechanism of spindle pole organization and instability in human oocytes. Science. 2022;375(6581):eabj3944.
8. Jentoft IMA, Bauerlein FJB, Welp LM, Cooper BH, Petrovic A, So C, et al. Mammalian oocytes store proteins for the early embryo on cytoplasmic lattices. Cell. 2023.
9. Zaffagnini G, Cheng S, Salzer MC, Pernaute B, Duran JM, Irimia M, et al. Mouse oocytes sequester aggregated proteins in degradative super-organelles. Cell. 2024;187(5):1109-26 e21.
10. Rothchild I. The yolkless egg and the evolution of eutherian viviparity. Biol Reprod. 2003;68(2):337-57.
11. Sang Q, Zhou Z, Mu J, Wang L. Genetic factors as potential molecular markers of human oocyte and embryo quality. J Assist Reprod Genet. 2021;38(5):993-1002.
12. Wang W, Miyamoto Y, Chen B, Shi J, Diao F, Zheng W, et al. Karyopherin alpha deficiency contributes to human preimplantation embryo arrest. J Clin Invest. 2023;133(2).
13. Sharif M, Detti L, Van den Veyver IB. Take your mother’s ferry: preimplantation embryo development requires maternal karyopherins for nuclear transport. J Clin Invest. 2023;133(2).
14. Bebbere D, Albertini DF, Coticchio G, Borini A, Ledda S. The subcortical maternal complex: emerging roles and novel perspectives. Mol Hum Reprod. 2021 doi: 10.1093/molehr/gaab043.
15.


By Sònia Gayete Lafuente, MD, PhD,
who is a Foundation for Reproductive Medicine Research Fellow at the CHR. She can be reached through the editorial office of the VOICE.
BRIEFING: Fertility can be influenced by a myriad of lifestyle factors, yet misconceptions and pseudoscience often overshadow the evidence. This article explores critical components of lifestyle contributions, providing a better understanding of how these elements impact fertility. Additionally, the article addresses the role of alternative therapies, evaluating their scientific grounding in fertility enhancement.

Dietary habits, physical activity, emotional well-being, and exposure to toxins play pivotal roles in general and reproductive health. Despite a wealth of information, many myths persist regarding optimal practices for those trying to conceive.
Recent studies confirmed that a balanced diet rich in fruits, vegetables, whole grains, and healthy fats can enhance fertility. Despite all reported attempts to design specific “fertility diets,” currently there exists no one specific diet menu that has proven to increase IVF treatment outcomes, for example. Certain patterns of the Mediterranean diet have, however, been associated with improved reproductive health in both males and females, being rich in antioxidants, vegetable protein, fiber, monounsaturated fatty acids (MUFAs), omega-3, vitamins, and minerals. Importantly, this diet has been shown to protect against chronic diseases associated
with oxidative stress, which also translates into pregnancy success. Conversely, increased consumption of hypercaloric and high-glycemic-index foods with high content of refined sugars and trans fats, and reduced consumption of dietary fiber, may detrimentally affect ovulation and sperm quality, therefore impairing fertility.
While such supplements as folic acid are recommended to all women for preconception health, others lack robust evidence. Efficacy of supplements such as coenzyme Q10 (CoQ10), vitamin D, and omega-3 fatty acids are widely accepted but really require further investigation. An enormous variety of over the counter “fertility supplements” on the market are usually blends of many substances at negligible doses and/ or without any evidence of efficacy. Moreover, they can at times interfere with activities of prescription medications. Consequently, we recommend against the self-prescribing of
“fertility supplements” and strongly suggest prior consultation with a knowledgeable physician before spending a lot of money on supplements that may not improv, and may at times even harm, pregnancy chances. One frequently encountered example is inositols, often prescribed to women with polycystic ovary syndrome (PCOS). They, indeed, are appropriate prescriptions for certain cases of PCOS; in others the inositols may, however, be harmful because they may counteract androgen supplementation with dehydroepiandrosterone (DHEA) or testosterone. Therefore, women and men should consult healthcare providers to tailor supplement regimens to their individual clinical needs.
Likely at least in part due to fat reduction and cardiovascular benefits, regular physical activity is also closely linked to improved fertility in females and males. Excessive exercise can, however, have adverse effects, particularly for women, by disrupting menstrual cycles. For instance, prolonged highintensity physical stress can lead to significant caloric deficits and/or increased cortisol and prolactin levels with subsequent negative feedback to the hypothalamic-pituitary-ovarian axis, consequently interrupting women’s normal menstrual cycles.
Lacking robust data supporting specific training programs during the pre-conceptional period, a balanced approach that promotes moderate exercise (considered to be 30-60 minutes of cardiovascular activity 5 times weekly) is generally recommended to optimize overall reproductive health. Additionally, resting and metabolic recovery time could also play a role, with limited data pointing to the possibility that decreased sleep time (less than 7 hours daily) could negatively affect female fertility. These data, however, still require confirmation.
Alcohol consumption is often considered socially acceptable, but its negative effects on gonadal function in both females and males have been consistently reported in over 30 years. In women, excessive alcohol consumption can disrupt hormonal balances, leading to irregular menstrual cycles and impaired ovarian function, which may result in, or contribute to, infertility.
Alcohol use during pregnancy in addition is associated with the so-called fetal alcohol syndrome, characterized by abnormalities in facial features and mental status.
In men, alcohol can affect sperm numbers and quality, reduce motility, and increase the likelihood of abnormal sperm morphology. Moreover, alcohol is associated with cellular oxidative stress and inflammation, further compromising
reproductive health. Although complete alcohol abstinence is ideal during the periconceptional period, occasional and mild social intake prior to pregnancy is generally considered acceptable by most health professionals.
Tobacco consumption is remarkably common. Despite progressive declines in the U.S., recent reports still suggest a prevalence of over 20% in individuals of reproductive age, a rather disturbing percentage, given the well-known negative effects on reproductive and sexual function as well as general health. Smoking—both traditional and electronic cigarettes and vapes—is linked to reduced fertility due to its detrimental effects at many levels of reproductive function, including reproductive hormones, ovarian function, and sperm quality. In women, smoking is associated with decreased fertility, increased risk of spontaneous abortions, and ectopic pregnancies. Smoking may also accelerate the decline in reproductive function and lead to 1 to 4 years earlier menopause. Using assisted reproductive technologies (ART) including in vitro fertilization (IVF), heavy smokers can require almost twice as many IVF attempts to conceive compared to nonsmokers. This negative effect is much less pronounced in occasional or light smokers. Smoking during pregnancy, of course, also remains a major cause of maternal, fetal, and infant morbidity and mortality, and should strongly be discouraged.
In men, smoking can lead to lower testosterone levels and impaired sperm function due to defective spermatogenesis, sperm maturation, and sperm function. Underlying these effects is elevated oxidative stress, DNA damage, and cell death, with all these factors playing important synergistic roles. While evidence suggests that semen quality and sperm competence are in smokers lower dose-dependently, it has not been definitively proven that smoking reduces male fertility.
Harmful effects, moreover, carry over to passive smoking, with nonsmokers exposed to significant tobacco smoke experiencing similar reproductive issues to smokers.
On a positive note, smoking is likely the main reversible cause of diminished ovarian reserve and reduced sperm quality. Parameters can be expected to significantly improve after a few months of smoking cessation. Therefore, all smokers should be advised of this and strongly encouraged to quit smoking as soon as possible in their fertility journey. For smoking cessation, medications such as varenicline, bupropion, and combination nicotine therapy should be prioritized under medical supervision; in randomized trials, they have been shown to be approximately twice as effective as placebo.
Stress, quality of life, and reproductive function, especially in women, strongly interphase and, hence, affect fertility. Consequences, therefore, are more often found in infertile than fertile females. Moreover, infertility itself often can lead to feelings of grief, anxiety, and depression, affecting relationships and overall well-being.

Despite the often profound psychological ramifications of infertility, they are frequently overlooked. Understanding these emotional challenges is critical for healthcare providers to be able to offer appropriate support. Patient groups, professional therapy, and mindfulness practices have all shown efficacy in helping individuals cope with the infertility-related emotional burden. Creating a supportive network and fostering open conversations about emotional experiences can alleviate feelings of isolation, frustration, and hopelessness. For these reasons, recognizing and addressing the psycho-emotional impact of infertility on patients but also healthcare providers is essential from the initial consultation on at an IVF center. Appropriate tailored support strategies can then empower individuals on this complex journey.
Treating the psychological needs of infertility patients has increasingly been recognized as an area of subspecialty, with increasing numbers of licensed fertility psychologists and therapists and even coaches available to serve infertile individuals and couples. Emerging evidence also appears to support the positive effects of mindfulness and of other stressreduction techniques on fertility outcomes and by improving emotional well-being, indirectly influencing reproductive health.
While the treatments described above represent the mainstay of currently available treatments, so-called alternative
therapies are making quick inroads. They include a broad variety of technical procedures, pharmaceutical interventions, and what we like to call pseudo-treatments, the latter often marketed as fertility enhancers without really having offered sufficient scientific data in support of their claimed utility.
The most common examples are herbal medications where even content is often undefined; or consider homeopathy and mind-body practices such as yoga, also to this group of intervention especially in association with IVF. They also include the very popular use of acupuncture because the literature in support of specific outcome benefits is really lacking.
The CHR, nevertheless, does not object to peri-implantation stage use of acupuncture because it may have beneficial psychological effects on the patient, even though outcome benefits in terms of pregnancy and live birth rates do not appear likely. Most common form of acupuncture in this setting usually involves two sessions on the day of embryo transfer, before and after the procedure, respectively, but can also take different formats and timing.
Much more concerningly are increasing numbers of other “add-ons” to fertility treatments –mostly to IVF– that have appeared in recent years on the market, often with too little or no established evidence at all in support of some claimed efficacy. Among those we would include so-called “fertility massage,” which has been alleged to enhance circulation and relieve tension in the reproductive organs. In our opinion there is no evidence that these effects can really be expected, and we are somewhat concerned about potential adverse effects on a pregnancy, especially in the third trimester. But, as massages obviously have beneficial stress-relieving effects if well-performed, we, of course, do not oppose them.
Another in our opinion unsupported benefit is the so-called cupping therapy, also alleged to improve circulation and relieve muscle tension, and potentially supporting reproductive health, as are alignments of spine and pelvis by chiropractic practitioners, and the so-called energy therapies, like Reiki or healing touch, alleged to promote relaxation and “balanced energy.”
Use of herbs, like chaste tree (Vitex), red clover, and maca root are common and widely claimed to support reproductive health, yet usually lack even minimal scientific validation. Academic research is limited, and many studies have small sample sizes or lack standardization, resulting in mixed findings. Most importantly, potential risks associated with unregulated herbal use must be considered. The CHR in general opposes the use of herbal products for two specific reasons which especially apply to Chinese herbs: First, their exact content is only rarely
known, and many contain estrogenic compounds which can interfere with testing of patients during IVF cycles. Moreover, at least one well-performed study in the literature in Europe reported lower pregnancy rates in IVF cycles with use of Chinese herbs.
The interplay between lifestyle factors and fertility is complex, necessitating a nuanced understanding of diet, exercise, emotional health, and toxicities, among other factors. By favoring evidence-supported practices, patients can enhance their fertility journeys while navigating around common myths and misconceptions. Through ongoing research, the CHR is committed to exploring all these here-discussed dimensions of good health because the better the overall health of our patents is at time of their treatment for infertility, the quicker and the more successful CHR will be in helping them to achieve pregnancy.
l considered experimental and is not a standard treatment in fertility clinics.
PRP therapy offers a promising avenue for treating thin endometrium by potentially enhancing the uterine lining’s thickness and receptivity. While early studies show encouraging results, more extensive research is needed to establish its efficacy and safety conclusively.
In summary: RIF is challenging to define, and even when a definition is established, diagnosing a specific cause or prescribing an effective treatment remains difficult. Initial steps should involve diagnosing and treating underlying conditions such as polyps, fibroids, or uterine scarring. Additionally, lifestyle modifications like reducing stress, quitting smoking, maintaining a healthy weight, and limiting alcohol consumption can be beneficial. While a well-timed embryo transfer during a natural menstrual cycle can be successful, providing hormonal support to the endometrium with sequential estrogen and progesterone is often a primary approach to treating a thin endometrium. Further medical treatments such as the use of sildenafil (Viagra), endometrial scratching, intrauterine administration of Granulocyte Colony-Stimulating Factor (G-CSF), and intrauterine PlateletRich Plasma (PRP) remain promising, but the mechanisms of action and effectiveness of each of these measures need to be validated in future well-structured randomized trials.
READING LIST
1. Łakoma K, Kukharuk O, Śliż D. The Influence of Metabolic Factors and Diet on Fertility. Nutrients. 2023 Feb 27;15(5):1180. doi: 10.3390/nu15051180. PMID: 36904180; PMCID: PMC10005661.
2. Alesi S, Habibi N, Silva TR, Cheung N, Torkel S, Tay CT, Quinteros A, Winter H, Teede H, Mousa A, Grieger JA, Moran LJ. Assessing the influence of preconception diet on female fertility: a systematic scoping review of observational studies. Hum Reprod Update. 2023 Nov 2;29(6):811-828. doi: 10.1093/humupd/dmad018. PMID: 37467045; PMCID: PMC10663051.
3. Zhao F, Hong X, Wang W, Wu J, Wang B. Effects of physical activity and sleep duration on fertility: A systematic review and meta-analysis based on
4. prospective cohort studies. Front Public Health. 2022 Nov 3;10:1029469. doi: 10.3389/fpubh.2022.1029469. PMID: 36408057; PMCID: PMC9669984.
5. Sansone A, Di Dato C, de Angelis C, Menafra D, Pozza C, Pivonello R, Isidori A, Gianfrilli D. Smoke, alcohol and drug addiction and male fertility. Reprod Biol Endocrinol. 2018 Jan 15;16(1):3. doi: 10.1186/s12958-018-0320-7. PMID: 29334961; PMCID: PMC5769315.
6. Practice Committee of the American Society for Reproductive Medicine. Electronic address: asrm@asrm.org; Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility: a committee opinion. Fertil Steril. 2018 Sep;110(4):611618. doi: 10.1016/j.fertnstert.2018.06.016. PMID: 30196946.
7. Dai JB, Wang ZX, Qiao ZD. The hazardous effects of tobacco smoking on male fertility. Asian J Androl. 2015 NovDec;17(6):954-60. doi: 10.4103/1008-682X.150847. PMID: 25851659; PMCID: PMC4814952.
8. Lyngsø J, Kesmodel US, Bay B, Ingerslev HJ, Pisinger CH, RamlauHansen CH. Female cigarette smoking and successful fertility treatment: A Danish cohort study. Acta Obstet Gynecol Scand. 2021 Jan;100(1):58-66. doi: 10.1111/aogs.13979. Epub 2020 Sep 18. PMID: 32865819.
9. Palomba S, Daolio J, Romeo S, Battaglia FA, Marci R, La Sala GB. Lifestyle and fertility: the influence of stress and quality of life on female fertility. Reprod Biol Endocrinol. 2018 Dec 2;16(1):113. doi:


the case for a fair informed consent for patients and a fair evaluation of clinics
David H. Barad, MD, MS, is Director of Clinical IVF and Research and a Senior Scientist at the CHR. He can be reached through the editorial office of the VOICE.
BRIEFING: The author explains the intricacies of fair patient consent and clinic evaluations, both closely linked. The article is not meant as criticism of the current reporting system of SART (and for that matter also the CDC), but as an encouragement for further improvements in the systems. Only if outcome analyses will allow for outcome stratification by detailed patient characteristics and, therefore, appropriate adjustments, will these registries be able to further enhance IVF.

The landscape of assisted reproductive technology (ART) is inherently complex, with success metrics that depend not only on clinical expertise but also significantly on patient demographics and treatment philosophies. This complexity becomes particularly evident when outcomes are scrutinized, such as in quality assurance audits by the Society for Assisted Reproductive Technology (SART), to which a majority of IVF clinics (though by no means all) annually voluntarily report their cycle outcome data. SART, a daughter society of the American Society for
Reproductive Medicine (ASRM), in turn, accumulates all data and publishes detailed annual reports. The society then in an additional function statistically evaluates aggregate data and informs individual clinics if they are outliers.
And because the CHR’s patient population is absolutely unique in comparison to almost 500 clinics reporting to SART, the CHR very frequently received notifications for an outlier status. The CHR’s most recent one was triggered by a relatively low reported live birth rate per embryo transfer among

women under 38 years for the year 2022 and served not only as the motivation for this article but also demonstrates how such data analyses without proper context can be misleading.
The profile of patients the CHR serves has, of course, a profound impact on reported outcomes. In 2022, 41% of cycles performed for women under 38 demonstrated significantly diminished ovarian reserve (DOR), at that young age defined by an AMH level of less than ~1.5 ng/mL. 1 At such a young age, this subset of patients—due to obviously prematurely aging ovaries (POA)—inherently faces lower implantation and live birth rates than women with normal functional ovarian reserve (FOR). Reasons for these lower rates are reduced oocyte quality as well as quantity in association with POA.
Unsurprisingly, many of these patients arrived at the CHR from all around the world with lengthy histories of unsuccessful treatments at other IVF clinics. Their reproductive backgrounds, moreover, usually go beyond just multiple failed prior IVF cycles; in over half of all cases, they arrive having been advised to pursue donor eggs and having been refused by their prior clinics to even consider further treatments with autologous oocytes.
Practices that report exceptionally high live birth rates can typically be assumed to selectively treat patients with only more favorable prognoses. These clinics often turn away individuals seeking IVF with their own oocytes if they do not meet certain minimal criteria, whereas at CHR, due to its inclusive patient approach which—after fully transparent informed consent—prioritizes patients’ desires, such individuals usually will still be given access to treatments with autologous oocytes, as long as a pregnancy chance appears still possible, even if remote.
This philosophy has positioned CHR as one of the world’s leading “last resort” IVF centers for patients from all over the world. At the CHR, over 90% of new patients fall into this challenging category. Expectations for pregnancy and live birth expectations, therefore, must be accordingly
adjusted. At the same time, rather than discouraging so-affected patients with overly pessimistic estimates, it is important to offer them conservative-realistic expectations about success with their own eggs in comparison to obviously much better chances with young donor oocytes.
During the queried period, many patients we treated at CHR arrived after experiencing multiple failed IVF cycles elsewhere—often three to five attempts— indicating possible underlying factors in their infertility that may still be unrecognized, whether maternal or embryonic in origin. These patients’ medical histories stand in sharp contrast to those undergoing their first IVF attempts, when success rates are naturally expected to be much higher.
Uniquely since 2014, the CHR’s cycle outcomes also include transfers involving allegedly non-euploid embryos. Questioning the accuracy and validity of routine preimplantation genetic testing for aneuploidy (PGT-A) —then still called preimplantation genetic screening (PGS)—the CHR in collaboration with other colleagues started in 2014 to selectively transfer some embryos in testing described “aneuploid.” In 2015, as the first center in the world, the CHR reported chromosomal-normal births after such transfers 2 and has since steadily transferred allegedly chromosomalabnormal embryos. Moreover, after establishing a registry for such cases, we have been regularly reporting cycle outcomes in the literature.
Since the CHR (except in rare circumstances) usually does not recommend the use of PGT-A to its patients, here, too, almost all cases involve patients at other centers refused such transfers who moved their allegedly “abnormal” embryos to the CHR. In the year 2022, two women under 38 years old had such transfers, which resulted in one healthy live birth. Like the CHR’s high acceptance rate of patients elsewhere refused treatments with their own eggs, this practice also underscores the CHR’s patient-centric model that respects informed patient decisions, yet places the center’s reported metrics at odds with clinics transferring only genetically screened, euploid embryos.
The SART benchmark of an 18% pregnancy rate, taken as a lower 95% confidence interval for women under 38, fails to reflect the heterogeneity of treatment approaches and patient inclusion criteria. Practices that focus solely on transferring high-quality, euploid blastocysts will naturally report more favorable statistics compared to those that accept challenging cases or—for example —allow transfers of noneuploid embryos.
This difference in clinical practice represents not just varying success rates, but often reflects fundamentally different philosophies of patient care and should be better addressed in the comment section of SART reports because very few patients (and likely even only a minority of physicians) understand this point. Unsurprisingly, despite great improvements in SART reporting, patients are still only insufficiently informed about expected outcomes in IVF, and colleagues, for whatever reasons, still direct many infertile women to third-party egg donation too early, in the CHR’s opinion.
To present a more accurate assessment of outcomes, stratifying patient populations into subgroups based on patient characteristics such as AMH levels and prior infertility/IVF history is essential. Highlighting these distinctions clarifies whether a clinic prioritizes clinic outcomes or goes beyond that by attempting to optimize cycle success rates of individual patients, based on highly individualized treatment pathways. Additionally, it is crucial to contextualize results with evidence-based literature, showing the challenges faced by patients with diminished ovarian reserve and histories of previous treatment failures.
All of this points to a need for fair benchmarking by discussing the selection biases inherent in higher success rates featured by many clinics as marketing tools. Patients are not only entitled to choose what kind of clinic they wish to attend; they also should be able to make the judgment with relative ease and that requires significant additional improvements to the current SART and CDC reporting systems.
The disparities in IVF outcome comparisons underscore the importance of a nuanced understanding of reported statistics. The pursuit of equitable, patient-centered reproductive care means embracing all infertility cases, - not only the easy ones. More complex cases, of course, will not always enhance reported success rates but will fulfill a vital role in patients’ treatment expectations. The analogy for doing otherwise, would be for a cardiac surgeon to operate only on patients with single vessel disease and then claim better outcome in comparison to a surgeon who even treats patients with multiple small vessel disease.
Success of an IVF clinic is not only defined by the overall success in achieving pregnancies and live births, but in the success rate in giving patients what they (not we doctors) define as success. In other words, directing a woman prematurely into egg donation because egg donation - of course – will improve pregnancy and live birth chances for almost everybody - is not really “success” even if this woman conceives on a first try. If she then for the rest of her life ends up wondering whether she could not have achieved the same goal with her own eggs, we, indeed, would consider such an approach an almost inexcusable failure of patient care.
1. Natalist. https://natalist.com/blogs/learn/whats-a-good-amh-atevery-age?srsltid=AfmBOoonD0MULWyZYMo8OfBEUXrA4HRxMGt u4Akte-yH1q6KD0-PW784
2. Gleicher et al., Fertil Steril 2015;104:e59



By Norbert Gleicher, MD, Medical Director and Chief Scientist
at The Center for Human Reproduction in New York City. He can be contacted through THE VOICE or directly at either ngleicher@ thechr.com or ngleicher@rockefeller.edu.
Briefing: Inflammation is an extremely common occurrence in humans, so it is unsurprising that inflammation frequently coexists with infertility and pregnancy. As a component of what can be considered to represent a “hyperactive” immune system, inflammation is something the CHR does not like to see in women undergoing infertility treatments because hyperactive immune systems are closely associated with increased miscarriage risk and—with less evidence to this point—implantation failure. As one of the most prominent reproductive immunologists in the country and building on over 40 years of research and clinical practice in this arena, the author of this article objectively points out how little is still known about the interdependence of pregnancy and the maternal immune system and, on purpose subjectively, summarizes how the CHR has come to view subspecialty area in infertility care that is unfortunately still widely unexplored.
Everybody has, of course, heard the word “inflammation,” and everybody has an opinion about what it means to have inflammation; but whatever we may believe inflammation is, in reality it is much more. It is pervasive, since every human being at any given moment may, indeed, have inflammation somewhere in the body, often without even knowing. On the other hand, inflammation may manifest itself as fever, pain, swelling, and local heat production of an inflamed area of the body. And at the same time normal physiological processes can be dependent on occurrence of inflammatory processes, among those several in reproduction, such as ovulation, implantation, labor, and others.
At the same time inflammation is also a normal defense mechanism in abnormal circumstances. When one gets injured, the body is invaded by bacteria, viruses, chemicals, etc., and yes, under certain circumstances by the fetus.
It may be symptomatic or not at all, just as an inflamed tooth may hurt or not. And even just an inflamed tooth—as the diagnosis already gives away—is, of course, also an inflammation.
In other words, inflammation can be good in defending us and it can be bad in attacking our bodies. It can be acute or chronic. It can be caused by as trivial a thing as an inflamed tooth, or it may be the consequence of a life-threatening autoimmune disease. In short, inflammation is everywhere and nowhere, it is essential for many important physiological processes, but inflammation can also kill us. It is an almost allencompassing term and, therefore, has only limited value as a primary diagnosis.
As already noted, inflammatory processes are omnipresent. When acute, they are simple to suspect and usually easy to diagnose.
They can cause discoloring of an inflamed area or flushed skin in a local area of inflammation, with or without tenderness in the area or mild pain (and not elsewhere) or can cause swelling, for example after a knee injury. But inflammation can also be local without localized symptoms, as it can be systemic with and without symptoms. And then, inflammation can be chronic, as in cases of autoimmunity, inflammatory bowel disease, cardiovascular disease, and even in certain cancers. Even mental/psychiatric diseases have now been associated with inflammation and, certainly neurodegenerative diseases, like Alzheimer’s disease. It has been estimated that inflammatory diseases account for more than half of all death in the world. 1
How a laboratory diagnosis is established, of course, depends on the underlying diagnosis. At the CHR the search for inflammation is part of every patient’s initial basic work-up and includes several standard inflammatory markers, all routine medical tests: A white blood cell count (WBC) in a CBC with differential, an erythrocyte sedimentation rate (ESR), a C-reactive protein (CRP), and an interleukin-6 (IL-6). We also look for thyroid autoimmunity, obtain an antinuclear antibody (ANA) panel, and antiphospholipid antibody (APA) panel. In addition, we look at total immunoglobulin levels in IgM, IgG, IgE, and IgA and – if the patient has a past history or family history of autoimmunity – we may go into more detail in our initial evaluation, with the principal goal not being the discovery of a previously unknown inflammatory and/or autoimmune disease (that happens only very rarely), but to determine whether the female
infertility patient demonstrates evidence of a hyperactive immune system.
And this is the point where the CHR approach to the immune system in infertile women significantly diverts from how many of our colleagues treat immune patients: Though it matters, of course, what kind of inflammatory and/or autoimmune condition a patient suffers from, over many decades of research the CHR has come to the conclusion that this is not the central question in treating infertile women with immune problems. The really important question is whether a patient shows signs of a hyperactive immune system.
If she does, she is definitely at increased risk of miscarriages and likely at increased risk of failure to implant (the latter is less wellestablished than the miscarriage risk).
In other words, we do not chase after individual markers (because there are too many nowadays) and, therefore, also do not run up diagnostic testing costs thousands of dollars because patient only very rarely have an undiagnosed, specific disease. Patients who do have a specific disease are usually already diagnosed. A large majority of infertile women with hyperactive immune systems do not know that they have a hyperactive immune system, and secondly, have only selected laboratory abnormalities and not really enough for a specific disease diagnosis.
The CHR, therefore, performs only a limited “checklist” of above
noted immune parameters (unless a couple’s history asks for more) to determine the likelihood of a hyperactive immune system. This, for example, does not include the investigation of NK cells (as many colleagues do) – and not only because peripheral NK cells in blood have nothing to do with endometrial NK cells which can only be obtained by endometrial biopsy – but because what determines the treatment offered to affected patients is not NK cells or APAs but the question of whether a patient has a hyperactive immune system or not. Once she is determined to have evidence of a hyperactive immune system, the severity of noted laboratory findings then determine the degree of treatment the patient will receive.
Pregnancy has a unique relationship with the maternal immune system, with the principal reason being that every embryo trying to implant in the mother’s uterus is either a so-called semiallograft (50% genetically from mother and father, respectively) or even a full 100% allograft when egg and sperm are genetically distinct from the woman carrying the pregnancy [i.e., either a pregnancy established with an egg donor or where a couple uses a gestational carrier (GC) for their embryos].
It is, however, one of the ground rules of our biological existence that our immune systems’ primary function is to defend us from being invaded by genetically foreign organisms. Based on this ground rule, every embryo trying to implant into a uterus should
be immediately rejected by the maternal immune system, even more so in donor eggs and GC carrier pregnancies. And, yet, in an overwhelming number of cases, this does not happen.
Why that is, has not been fully established yet, even though certain local mechanisms –including local endometrial Treg cells – have been identifies as important local contributors to the implantation process. 2 While these local mechanisms may at least partially explain the initial development of maternal tolerance toward an implanting embryo, they do not explain the tolerance of a solid organ transplant growing with logarithmic speed (called the fetal-placental unit) by the maternal immune system.
How the maternal immune system tolerates such a massive “tumor” is still unexplained, though certain features appear obvious: (i) Local immune processes may help in implantation; but the embryo – in successful implantation – buries into the endometrium for at least 10 days completely independent of any maternal input and unaffected by a maternal immune response 3 even though the endometrium, in principle, must be hostile to any penetration, since women would otherwise be steadily infected by transvaginal invaders. (ii) Such an uncontested invasion is only explainable by the maternal immune system having made the invading embryo immunologically “invisible” by reprogramming itself from being hostile to being tolerant of this embryo. Data suggest that this reprogramming through induction of tolerance pathways occurs in response to certain messages received by the endometrium from the embryo.
It is this reprogramming process leading to the induction of tolerance pathways that malfunctions in women with hyperactive immune systems, whatever the cause. Consequently, women with hyperactive immune systems are at increased risk for miscarriages and also, likely, implantation failure, because if tolerance pathways are not properly induced, the implanting embryo remains at least partially immunologically visible and, therefore, is attacked by the maternal immune system. A first intervention in suppressing such unwanted maternal immune responses, therefore, must be in place, ideally before the embryo enters the endometrial cavity.
As is so often the case in medicine, there is no one treatment for all women with hyperactive immune systems. Here we return to the different etiologies of hyperactive immune systems: A woman whose immune system is hyperactive because of autoimmunity will have to be treated differently from a woman whose immune system hyperactivity is primarily inflammatory in nature, or is both autoimmune and inflammatory. And treatment will also vary based on the severity of laboratory abnormalities.
At a very basic level, corticosteroids will be first line of drugs in cases of autoimmunity, while anti-inflammatory medications, like Plaquenil, will be first choice in women with primarily inflammatory conditions. Because autoimmune diseases almost uniformly also have inflammatory components, both drugs may be used in unison (systemic lupus
erythematosus, SLE, is a good example). Also considered a rather automatic treatment in both conditions is low-dose aspirin (mostly at a dose of 81mg daily) which has also become vogue in the prevention of preeclampsia during pregnancy, where it usually is prescribed in slightly higher dosing. These are, indeed, the three Level I medications at the CHR for women with hyperactive immune systems. Based on a recent systematic review, 4 the CHR no longer automatically uses anticoagulation, unless a patient has a diagnosed thrombophilia.
Where patients require longer-term anti-inflammatory pretreatment before IVF cycle starts, patients at the CHR are often placed on an anti-inflammatory multicomponent non-prescription supplement. An example is Conflam-Forte, soon to be relaunched Ovaterra by Fertility Nutraceuticals, LLC, in NYC, to the CHR’s specifications; this supplement contains a multitude of anti-inflammatory compounds and does not have the potential side-effects on eyes that Plaquenil has, requiring an eye exam every six months.
In more severe cases, additional medications are added. The CHR’s Level II medications are Intralipid and intravenous gamma globulin (IV-Ig), with IV-Ig greatly preferred over Intralipid. Fortunately, Level I and II medications will be sufficient for an overwhelming number of patients with hyperactive immune systems but, on occasion, patients may need even more (Level III). This is when so-called “biologicals” come into play, with this term indicating that these drugs were made from living organisms or their products. They are currently our most powerful
weapons for stopping inflammation. Among the most well-known examples are Humira (adalimumab) (by AbbVie) and Enbrel (etanercept, by Amgen and Pfizer). Another level III medication at CHR, indeed, the longest one in use is granulocyte colony stimulating factor (GCSF).
None of these drugs has, however, been specifically studied in pregnancy and the CHR, therefore (except for GCSF), consider these drugs as still experimental if used during pregnancy. From post-marketing studies of women who conceived on these drugs often unintentionally, there is, however, increasing evidence that their use in pregnancy is safe.
References
1. https://my.clevelandclinic.org/health/symptoms/21660-inflammation
2. Lindau et al., J Reprod Immunol 2021;146:103330
3. Deglincert et al., Nature 2016;533(7602):251-254
4. Tamiris Barbosa Dias et al., JBRA Assist Reprod 2021;25(1):10-27


This issue of the VOICE spans the annual Foundation for Reproductive Medicine Conference (FRMC) on December 6-8, 2024, which the CHR has the honor of co-sponsoring every year. Here we present the final program for this year’s—as always remarkable—conference. Please join us for what has by now become a very special and worldwide event, bringing together leading basic scientists and clinicians to review, advance, and apply new knowledge translationally to reproductive biology and clinical practice in reproductive medicine under the motto, “think differently.”


This month we take a deep dive into the inner workings of the human embryo. While the CHR adheres strictly to its motto of “Fighting for every egg,” in the end what everybody in IVF is seeking is that highest quality embryo with the best chances of yielding a healthy offspring. Since joining the CHR 10 years ago, Dr. Albertini has brought his long-standing interests in how cell cycle and cytoskeleton direct the development of the fertilized egg into a healthy blastocyst. The following images provide a glimpse into the tools of the trade he has been applying during his tenure here at the CHR..
FIGURE I
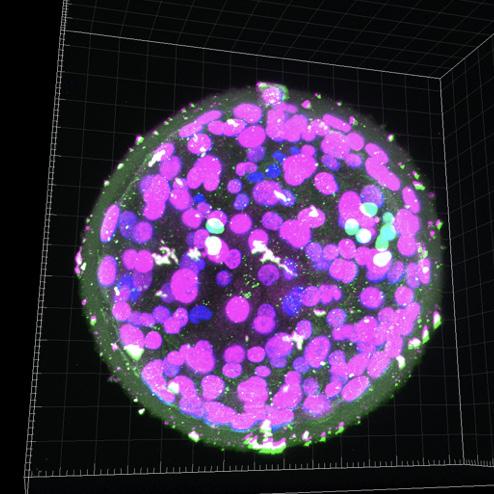
FIGURE 1: This to research donated embryo demonstrates the 3-dimensional perspective of a blastocyst-stage embryo, with individual cellular components highlighted in different colors with special antibody biomarkers (in collaboration with the Brivanlou Laboratory at Rockefeller University in NYC).
FIGURE III

FIGURE 3: Unfortunately, and all too often, eggs fertilized by IVF or ICSI start their development on schedule but stop precisely at the stage when the decision is made to encourage some cells to become the embryo whereas others would become the placenta. This embryo is arrested at the 5-cell stage and is showing signs of abnormal cell division (see microtubules in green).
FIGURE II
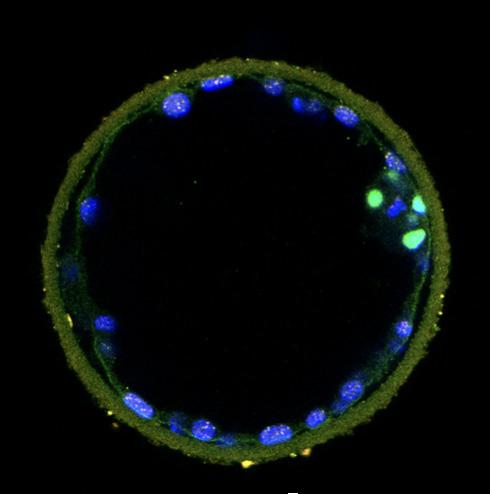
FIGURE 2: By taking a thin slice of this blastocyst, we begin to identify two of the cell types comprising the blastocyst-in green, a subset of cells that will go on to form the embryo proper and eventually fetus, while the cells lining the outer limits (blue nuclei with speckles) are designated to become the placenta (in collaboration with the Brivanlou Laboratory at Rockefeller University in NYC).
FIGURE IV
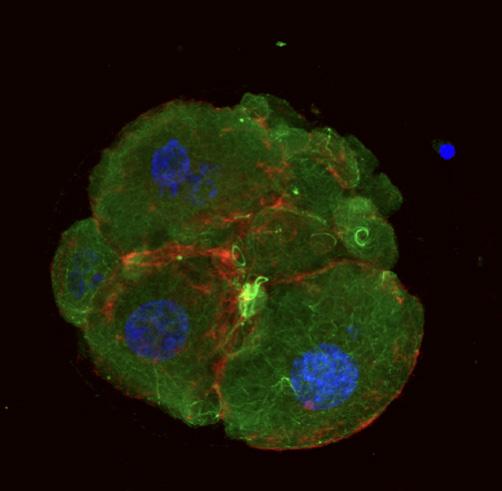
FIGURE 4: This embryo has developed into a compacted morula, the stage at which decisions to become embryo or placenta take place. But even though signs of normal cell division are seen, the reasons why this embryo was unable to continue its journey to the blastocyst stage remain unknown and are the subject of ongoing research at the CHR.
BRIEFING: The VOICE in this section offers opinions about news which in preceding months attracted our attention and which we believe in some ways are relevant to the practice of medicine. We separate them into two subsections: (i) Local, National, and International News; and (ii) General Medical News not directly related to reproduction (direct medical news are reported in a later section of this VOICE). Since outside opinions and CHR’s positions on various issues can obviously be biased, it is important to reemphasize that we are fully cognizant that “expert” opinions in medicine are considered the lowest level of evidence and should be viewed as such by our readers. Unable to offer, therefore, consistent “truth” (if something like that really exists in science), the VOICE strives, in its selection of topics and in its content, to come as close as possible to the most likely “truth of the moment.” We, therefore, especially welcome from our readers contrarian submissions to our own opinions. They should be submitted with the subject line “Opinion” to social@thechr.com. Local, National, and International News.
Partially reprinted and edited with permission of authors and The Reproductive Times.
One, indeed, can get the impression that this is the case. Chris Cummings recently reported in The Wall Street Journal that some physician groups are trying very hard to limit the further expansion of private equity into U.S. healthcare. 1 As the article notes, many of these groups are also trying to influence legislatures to restrict further takeovers in medicine by private equity.
Reproductive medicine – and especially the infertility field – has, of course, been a primary target, with over half of all U.S. IVF cycles apparently already “owned” by private equity.
This fact was already noted earlier in this issue of the VOICE in a discussion of several class-action lawsuits that recently were filed in the U.S., accusing the genetic testing industry of fraudulently misrepresenting to the public the advantages of preimplantation genetic testing for aneuploid (PGT-A) (page __). We are pointing this article out here because Norbert Gleicher, MD, its author, suggests that should these lawsuits reduce the utilization of PGT-A in association with IVF, as he expects, current financial models of IVF clinics which have been so enticing for private equity to enter the fertility field may change. And a change in involvement and (even more so) a substantial withdrawal of private equity from the infertility field, would, of course, greatly affect practice values.
According to a Professor at Oregon Health & Science University quoted in The Journal article, 61% of physicians have a negative view of private equity, and only less than 11% look at private equity positively. We suspect that these 11% probably are older physicians close to retirement who are planning on selling their practices to private equity.
1. Cummings C. The Wall Street Journal. September 22, 2023. https:// www.wsj.com/articles/doctors-organize-to-push-back-against-private-equity-takeovers-16aa2c94 or in print September 23, 2024. pB8
In a formal statement on behalf of the ASRM, its president at the time, Paula Amato, MD (now the society’s immediate past president) expressed that the Society was “thrilled” that Governor Gavin Newsom signed into law SB 729, which greatly expanded the availability to IVF by defining same sex couples and single individuals who need IVF to have a child as “infertile.” The news release also noted that this new state law “brought California to the forefront of IVF cover-
REFERENCE
1. Amato P., ASRM Press Release. September 29, 2024. https://www. asrm.org/news-and-events/asrm-news/press-releasesbulletins/fertility-care-gets-win-california/

The VOICE, especially over the past year, has repeatedly pointed out the rapidly growing number of reports about research misconduct in medicine. Now this scourge has reached the highest levels of the National Institutes of Health (NIH), with the director of the neuroscience division at the National Institute of Aging (NIA), Eliezer Masliah, MD, having been “relieved of his position” because of research misconduct, as formally announced by the NIH.1
And it does not seem to have been just “little mistakes,” like when a prominent dean at an even more prominent university was forced to resign because—being busy as a dean— he had failed to properly supervise his laboratory which published a few papers (his name on them) demonstrating similar “errors” to the papers from Masliah’s laboratory. In an investigation at the NIH, Masliah was found guilty of falsifications and/or fabrications and the reuse and relabeling of figures representing two different studies.3 In other words, not only little guys cheat in their research to advance their careers; biggies do the same, and it would be interesting to study what their motivations are.
After labs run by famous university deans and other senior academicians were found to have cheated, and after presidents of famous universities were found to have plagiarized the work of others, they all were given the opportunity to resign from their prestigious positions, while maintaining salaries and other perks by staying on the faculty, but Masliah was outright fired. He either did really terrible things or we still have a two- (or even more)-tiered system that protects the more prominent boys and girls over those a little less prominent. Considering that Masliah’s misconduct allegedly involved no fewer than 123 published papers,1
maybe both was the case in this instance.
And related, Andrew D. Weeks, Professor of International Maternal Health at the University of Liverpool, in the U.K., recently penned an appropriate article that is worth reading under the title, “A new system is needed to tackle research misconduct.”2 He points out that modern evidence based medicine was built on trust and peer review: Trust that researchers not deliberately fabricate scientific research, and the belief that peer review in journals would be the gatekeepers of high quality research. Unfortunately, the trust in both has been lost.
1. National Institutes of Health, News Release. September 26, 2024. https://www.nih.gov/news-events/news-releases/statement-nih-research-misconduct-findings
2. Week A. BMJ 2024; 386. Doi: https://doi.org/10.1136/nmj.q2011
On October 28, 2024, Vanessa Burns, a PhD student at the Wellcome Sanger Institute in the U.K. reported in BioNews 1262 that Netflix was sued for disclosing the identities of three women who were conceived through the utilization of donor semen in a documentary. 1 The documentary, called Our Father, reported on the story of obstetrician-gynecologist Donald Cline, MD, routinely described in the media as a “fertility doctor.”
The accusations against him of having fathered (secretly and without informing his patients) no fewer than 94 children during the years 1979-1986 (patients were told that the donor semen came from medical students) has been made on repeated earlier occasions against several other prominent physicians in the fertility field in those very early days of modern infertility practice. Donor semen was in those days widely used fresh in many general OB/GYN offices immediately after donation and medical students and residents were, indeed, the usual donors.
But the fraudulent use of Dr. Cline’s own semen is not the subject of this report. What makes his story different and resurrected the interest in his case which finally resulted in the doctor’s conviction on two felony charges in Indiana in 2018, 2 is the fact that three women sued Netflix in 2022 for allowing the (very well received) documentary to reveal their identities and—by doing so—causing them “reputational injury, distress, embarrassment, and emotional trauma.”
Though Netflix tried to squash the case, a judge allowed two out of the three cases to proceed (the third woman had had contact with media organizations before Netflix approached her). A date for the trial is not set yet.
1. Burns V. BioNews 1262. October 28, 2024. https://www.progress. org.uk/netflix-sued-for-disclosing-idetities-of-donor-conceived-people/
2. Ashley B. The Ribbon Box. July 18, 2022. https://theribbonbox.com/ fertility/the-man-behind-our-father-dr-donald-cline
According to a recent report in The Wall Street Journal, the average annual cost of family coverage health insurance has reached approximately $25,000. 1 This compares to roughly $6,000 in the year 2000 and reflects a 2024 increase alone of 7%. And while most of this increase affects employers, workers’ contributions have, of course, increased in parallel and so have deductibles (see the figure below). The latter, moreover, increased significantly especially in small companies.
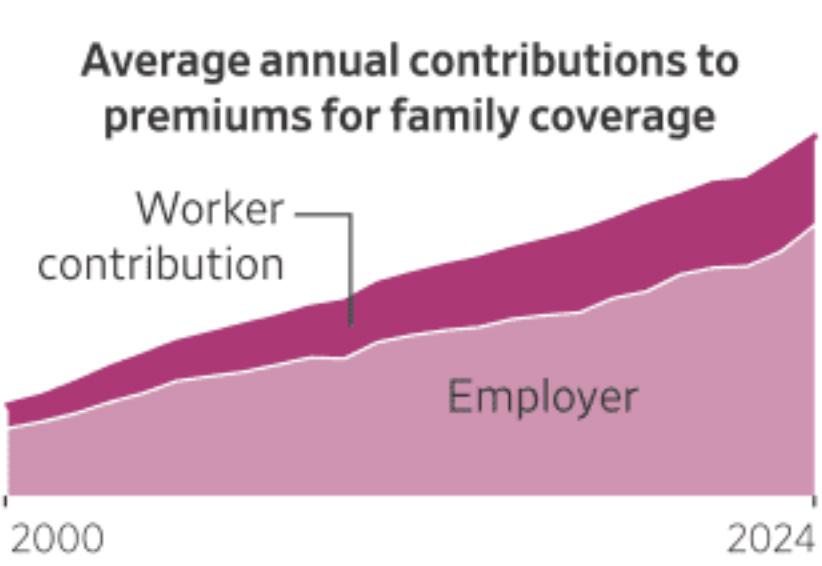
Source: WSJ1
The article specifically also broke out data regarding socalled family building benefits, which included coverage for fertility medications, IVF, intrauterine inseminations (IUIs), adoption, cryopreservation, and “others,” and they
were still more than disappointing: specifically, even among companies with over 200 employees, barely ca.12% covered IVF, only approximately 15% covered fertility medications, roughly 10% covered IUIs, and 5% or fewer covered adoptions, cryopreservation (i.e., egg-freezing), and other fertility treatments. The article also noted that most employers still are holding off on weight loss drugs which, of course, also has potential relevance for fertility treatments.
With the numbers regarding fertility coverage still being so disappointing among large companies, one can assume that they are even worse in smaller companies with fewer employees. These numbers very obviously reemphasize what the fertility field in the U.S. has been aware of for some time: infertile couples in a large majority are underserved. This fact, indeed, has been one reason why the CHR in 2023 started to offer smaller employers in the New York tristate area with up to 100 employees significantly discounted infertility coverage, including IVF. Human resources and/ or benefit managers of smaller-size companies in our area seeking competent fertility coverage for their employees, therefore, should contact Ms. Jolanta Tapper, COO of the CHR, at jtapper@thechr.com or 212-994-4400.
REFERENCE
1. Evans M, Ulick J. The Wall Street Journal. October 9, 2024. https://www.wsj.com/health/healthcare/health-insurance-inflation-charts-612812ed
The so-called bird flu (H5N1) is causing increasing concerns. Not only has the virus infected hordes of cows, and with it the milk industry and a good number of its employees, but Reuters 1 (and other news organizations) recently also reported the first case of H5N1 bird flu in a pig in Oregon. This has significance because pigs were implicated in transmissions to humans in the H1N1 flu pandemic in 2009-2010. The farm has been quarantined.
Related, Reuters also reported a few days earlier that Sanofi, GSK, and CSL were tapped by the U.S. government to expand the supply of bird flu vaccine 2, a sign that concerns about a possible bird flu pandemic are growing.
REFERENCES
1. Douglas L, Polansek T. Reuters. October 30, 2024. https://www. reuters.com/business/healthcare-pharmaceuticals/us-detects-h5n1bird-flu-swine-first-time-2024-10-30/
2. Reuters. October 4, 2024. https://www.reuters.com/business/ healthcare-pharmaceuticals/sanofi-gsk-csl-tapped-expand-us-birdflu-vaccine-supply-bloomberg-news-reports-2024-10-04/
And since we already are repeatedly quoting Reuters, here is one more: The agency recently reported that the FDA put a trial of the pharma company Novavax on hold, which was testing a combination vaccine against COVID and the flu after one person reported nerve damage. 1 He demonstrated symptoms of a motor neuropathy and/or damage to nerve cells that control muscles and movement.
Since other similar vaccine combinations had not found similar risks, the company issued a statement that it did not believe that this case of neuropathy was caused by the vaccine and that it was looking forward to resuming the approval process by starting a Phase 3 trial as soon as possible. The company’s shares, nevertheless, dropped as a consequence by 24%, per the report, wiping out $400 million from the company’s value.
REFERENCE
1. Satija B. Reuters. October 16, 2024. https://www.reuters.com/business/healthcare-pharmaceuticals/us-fda-places-trials-two-novavaxvaccines-hold-2024-10-16/
This is, indeed, what appears to be happening, as suggested by a recent article by Rupa Subramanya in The Free Press. It has become a must-read for everybody in academia since it lays bare the transformative changes introduced by the National Science Foundation (NSF) in its funding of research.1 And one is left astonished, disturbed, and extremely worried because the funding of grants by scientific merit seems to, by significant degrees, to have been replaced by funding grants – first and foremost – based on their perceived social and political values.
This is how grants claiming to explore “white supremacy” and “non-normative forms of gender and sexuality” were apparently advanced over much more scientifically-substantial studies with the potential to change the world, which –
at least in its past – had been the goal of the NSF in awarding grants to researchers. Concluding that DEI has been transforming the NSF, Subramanya’s article becomes terrible news for anybody interested in maintaining the country’s increasingly shaky lead in scientific research.
Her Free Press article noted a recent Congressional report (in full disclosure, from Republican members of the U.S. Senate Committee on Commerce, Science & Transportation) based on an analysis of all NSF grants between 2021 and April of 2024 which revealed almost unbelievable numbers: From over $20 billion awarded in grants by the NSF in these approximately three years, over $2 billion (over 10% of funded grants) no longer prioritized scientific quality in awarding grants but prioritized other aspects of grant submissions. And this did not happen accidentally, but, according to Subramanya, has become a central feature of grant-awarding by the NSF.
And the U.S. is, of course not alone in this. We were recently made aware that the U.K.-based Wellcome Trust, with a £36.8 billion investment portfolio (USD $47,683 billion), instituted similar changes to its grant selection processes, allegedly awarding between 25% and 33% of total grant evaluation points to considerations of whether applicants paid appropriate attention to DEI.
How far this redirection of grant support by the NSF has gone off into the political becomes obvious if one looks at some of the grant recipients: Marwa Elshakry in the Congressional report was found to be a co-recipient of a grant (and to be fully transparent again, considering many other cited grants, it was a relatively small-sum grant) meant to identify how (and, yes, this almost impossible-to-understand word scramble was really the chosen subject of the application) “hegemonic narratives have sought to obfuscate not only the contemporary existence of non-normative sexual experiences in certain national contexts, but also aimed to bury any historical traces of non-normative forms of gender and sexuality” 1 .
Marwa Elshakry, PhD, an Associate Professor at Columbia University

in NYC in the Department of History, who specializes in the history of science, technology, and medicine in the modern Middle East. She earned her PhD from Princeton University 2 .
She being a grant recipient of the NSF is of interest for sev-
eral reasons: (i) The subject of her grant apparently does not correspond to what Columbia University describes as her area of specialty (see footnote to figure above); (ii) As Subramanya notes in her article, Elshakry and her co-recipient on the grant, history student Jamil Sbitan, were among several grant recipients from the NSF who held leadership positions of prominence during the campus protests against Israel at Columbia University where the unrests and encampments at university campuses around the country had their beginning after the events of October 7, 2023. (iii) Considering that Elshakry allegedly justified the October 7 massacre by Hamas, was allegedly since November of 2023 a “coordinating member” of the Columbia anti-Israel group called Faculty and Staff for Justice in Palestine-CBT (FSJP-CBT), 3 and therefore – very obviously – must be viewed as a supporter of Hamas and the organization’s policies in Gaza, the subject of her NSF grant can only be viewed as hypocritical in view of how the subjects addressed in this project would be viewed by Hamas in Gaza.
Interestingly, Elshakry is according to Subramanya on (we assume paid) leave this semester, which is how Columbia University has been avoiding firing many faculty members who, after October 7, breeched Columbia University rules (and often federal laws). In “laying low” in its responses to obvious transgressions by students and faculty members after the October 7 in support of the atrocities committed by Hamas, the administration of Columbia University, as just recently was revealed, followed the rather shocking advice of Senate Majority Leader Chuck Schumer (Dem., NY; and, interestingly, the highest-ranking Jewish elected official in the country), recently released in a report from the House Education and the Workforce Committee. The report claims that Schumer allegedly advised the then-President of the university, Minouche Shafik, after pro-Hamas violence had broken out on campus, “to keep heads down” and not to be concerned about the horrors because “political problems are really only among Republicans.” 4
The obscenity of Schumer’s words, of course, go far beyond just the fact that he is Jewish. We, indeed, would argue that one’s religion – as much as possible – should not affect one’s politics. But what makes this alleged Schumer episode so obscene is that it reflects how the politics (of the left) in the country have assumed full control over higher education with full cooperation from the educational establishment at even the nation’s most prominent universities.
But since we are already talking about Chuck Schumer, whose political base from the very beginning has been in Brooklyn, and especially in the Jewish Orthodox community, he, indeed, increasingly resembles Senator Bernie Sanders (Dem., VT, and another prominent senator of Jewish de-
scent) in his anti-Israeli activism, first by attacking the qualifications of the current Israeli prime minister and, absurdly, accusing him of being “a barrier to peace with Hamas.” But probably even more surprisingly, Schumer has for months been singlehandedly blocking the passage of the so-called Antisemitism Awareness Act by the Senate after it passed the House with overwhelming bipartisan support (320 to 91), by refusing to bring it to a vote. And what has been the reason? According to reports in the media, because “it divides Democrats.” 4
This bill would define antisemitism by including anti-Zionism in the definition, of course a point opposed by the Democrats’ extreme left with obvious strong sympathies for Hamas. The bill would also force colleges and universities toward stronger enforcement of anti-discrimination laws, once again—considering the Democrat party’s extreme left—not what their ideology prescribes.
What all of this demonstrates is that the antisemitism that surfaced its ugly head after October 7, 2023, is only a symptom of a much bigger crisis in society. Medically speaking, the symptom is antisemitism, but the disease is an education system that, from kindergarten throughout college and university, is now controlled by ideological zealots with the so-far successful intent – as the last year well demonstrated – to indoctrinate our children and grandchildren in their revolutionary theories. And as the article by Subramanya in The Free Press laid bare, the disease has also infected our major research funding organizations, turning them into funders of the disease and, thereby, providing further nutritional support to the cancer.
1. Subramanya R. The Free Press. October 10, 2024. https://x.com/ TheFP/status/1844061951556714998
2. Columbia University. https://history.columbia.edu/person/ elshakry-marwa/
3. Canary Mission. https://canarymission.org/professor/Marwa_ Elshakry
4. The Editorial Board. New York Post. November 1, 2024. https:// nypost.com/2024/11/01/opinion/traitor-chuck-schumer-sold-out-topro-hamas-thugs-at-columbia/
Here is interesting news from a prominent medical school.
The University of Connecticut (UConn) School of Medicine – after using for two millennia, like most other Western medical schools, the Hippocratic Oath to ‘do no harm’ as the foundation of medicine, has now reached the conclusion that the oath was outdated. According to the leadership of the university, the oath had to be expanded to also pledge to advance DEI in medical practice.
The school announce the new oath as follows: “We have revised our medical school’s Hippocratic oath to include active pledges to identify and mitigate personal biases, to uphold human rights, to respond to medical myths with evidenced based information and without judgment, to actively support policies that promote social justice and specifically work to dismantle policies that perpetuate inequities, exclusion, discrimination, and racism.”
The change was (of course) prompted by the university’s Diversity, Equity, and Inclusion Committee and what is there left to say after two millennia in which the old oath served as one of the pillars of Western civilization, as an article in Do No Harm Medicine pointed out 1 .
What is then left to say? One wonders when this committee is planning to adjust the Ten Commandments?
REFERENCE
1. Do No Harm Medicine. 11, 2024. https://donoharmmedicine.org/2024/09/11/uconn-dei-hippocratic-oath/#:~:text=%E2%80%9CWe%20have%20revised%20our%20medical,justice%20and%20specifically%20work%20to
Almost unnoticed here in the U.S. except by an article in The New York Times 1 , Italy passed a law that criminalizes the pursuit of surrogacy abroad. In Italy surrogacy has already been illegal but the new law even prohibits its pursuit outside the country. For some reason the article appears to emphasize the effect of the law especially on gay fathers, while the problem – of course – affects the whole L.G.B.T.Q+ community, infertile couples, single men, and even some single women.
To pass such a law appears not only inhumane but plainly stupid for Italy, considering that the country is experiencing one of the 10 lowest birth rates in the world (see figure) 2 . In the so-called developed world the birth rate required for replacement of the existing population is 2.1 children per woman. Italy’s birthrate of 1.26, therefore, points toward
the disappearance of the Italy we all know and love in the not-too-distant future, unless the country finds ways to improve its birth rate.
As the article notes, it is unclear whether the law will withstand legal challenges. Despite having been at the forefront in some areas of IVF research, the country has had its own complex legal history regarding IVF, usually attributed to the influence of the Roman Catholic Church in the country. Several restrictions on what around the world were considered routine IVF practices, therefore, could be introduced in Italy only after legal challenges to existing restrictive laws. In our opinion, it, therefore, would not be surprising if this new law would be rather short-lived.

Source: Statista, CIA.Gov
REFERENCES
1. Bubola E. The New York Times. October 16, 2024. https://www. nytimes.com/2024/10/16/world/europe/italy-surrogacy-law.html
2. Gupta C. Indian Express. October 23, 2024. https://indianexpress. com/article/trending/top-10-listing/top-10-countries-with-the-lowest-fertility-rates-in-2024-9634294/
A recent article by Heather Landi in Fierce Healthcare 1 noted that in the 10-year period between 2012 and 2022, national health expenditures increased from $2.8 trillion to $ 4.5 trillion (+61%) and is expected by 2032 to have grown to $7.7 trillion (another +71%). If one compares these costs to the national domestic product (GDP), this quite a significant proportion. While insurance coverage during this time period has improved – uninsured declined from 48.6 million
to 28 million (-42.4%), life expectancy in the U.S. is only negligibly higher and almost 4 years below OECD countries. Obesity, diabetes, and behavioral health problems have been steadily increasing in prevalence. 30-day mortality rates in hospitals are, moreover, rising sharply, even if COVID deaths are excluded.
So, what is then the conclusion? The article suggests that all stakeholders, whether an employer or payer, life science company or provider, will have to stop extracting value from the health care system in ways that maximize profits. Instead, efforts have to be directed at delivering value for the money spent, in the process optimizing the value for whoever ultimately pays for the medical treatment.
The concept of value-based medical care is, of course, nothing new. To the contrary, it, indeed, has become one of those “fashions of the moment” in recent years; but according to the article value-based care policies so-far implemented, have in principle failed.
Looking at the infertility field from such a viewpoint, this, of course, should not surprise. One just has to look at all the “add-ons” introduced to IVF practice over the last 20 years with no evidence for any outcome benefits. Or how about all the changes in IVF practice that have led to the need for more treatment cycles, like for example routine all-freeze protocols? We, indeed, would argue that a study of value-based care in IVF over the last 20 years would demonstrate a straight line downward for every dollar spent. One strong hint that this, indeed, is likely the case is the declining live birth rate in U.S. IVF cycles since ca. 2010, when the introduction of unvalidated “add-ons” to IVF started to accelerate 2 .
REFERENCES
1. Landi H. Fierce Healthcare. October 1, 2024. https://www.fiercehealthcae.com/providers/new-analysis-points-troubling-trends-ushealthcare-costs-rise-health-outcomes-worsen.
2. Gleicher et al., Hum Reprod Update 2019;(3):hoz017
REGULATED BY THE FDAand how that pertains to the infertility field
According to Forbes, 1 the FDA in 2016 warned the public for the first time about so-called for-profit “stem cell clinics” that offered a variety of alleged stem cell therapies with claims of curing everything from COVID-19 and Alzheimer’s
disease to hair loss and aging. In an article from November 2022, the NIH tried to “put stem cell-based therapies into context,” 2 noting that the FDA over the past three decades has approved several stem cell-based products, including bone marrow transplants, which have been transformational for many cancer patients, and therapies for blood and immune system disorders. Other approved treatments included products for dental uses and tissue growth and for skin burns. Since the early 2000s, stem cell-based therapies have been explored in many eye diseases, including age-related macular degeneration and glaucoma. 2 Stem cell-based therapies are also being explored for neuroegenerative diseases such as stroke and Alzheimer’s disease, and for countless other conditions.
The article then, however, also noted that increasing numbers of rogue clinics had started taking advantage of patients desperate for cures by claiming dramatic results, often exaggerated in sensational media testimonials. Those clinics – according to the authors – often mimic legitimate medical practices that extract a patient’s own stem cells, concentrate or modify the cells, and then re-inject them. Some manufacturers offer stem cell-based derived products, such as “biologic eye drops” made with placenta extract or amniotic fluid to treat dry eye. Those clinics also often provide misleading information and advertise their practice as running clinical trials without, of course, following standard required clinical trial rules, including registration and/or FDA regulatory approval.
The article further noted that these unproven and unregulated stem cell treatments carry significant risk, from administration site reactions to more dangerous systemic adverse events. For example, injected cells can multiply into inappropriate cell types or even dangerous tumors. A 2017 report, indeed, described one Florida clinic that blinded patients with stem cell eye injections. 3 The authors also noted that the Pew Charitable Trusts gathered 360 reports of adverse events related to unapproved stem cell therapies, including 20 cases that caused death. 4 Further, adverse events are likely underreported because these products are not FDA approved or regulated. Many unproven stem cell-based therapies cost thousands of dollars to patients and are not covered by insurance. Further, even if patients avoid adverse events from these therapies, they may suffer consequences from delaying evidence-based treatments.
A legal blog recently addressed this subject 4 based on the fact that the legal authority of the FDA to regulate what was happening in such clinics was unclear and a recent court case established some clarity. The blog described the case as follows: This case required a decision whether the FDA can regulate certain stem cell mixtures advertised as
treatments for a host of medical conditions. Defendants were doctors who created such a mixture by removing fat tissue from a patient and breaking it down to concentrate the portion containing (mesenchymal) stem cells. The result was a mixture of stem cells, other types of cells, and cell debris called stromal vascular fraction (SVF), which then was administered for example directly into a patient’s knee to treat osteoarthritis. In recent years, clinics offering similar stem cell mixtures have proliferated despite concerns over whether such treatments are safe and effective.
Without going into further legal detail (for that the reader is referred to reference #4 which in great detail very well explains how the appellate court reached its conclusions in a logical and stepwise approach), the FDA wone the case with the court deciding that what the clinic did was inject a drug/ treatment which gave the FDA the authority to oversee the process.
Practically, this means that the FDA has the authority to regulate “stem cell clinics” and the question that now arises is how interested the FDA will be in shouldering this burden and how aggressively the agency, therefore, will end up pursuing these “rouge” clinics, as classified by the NIH. 2
What all of this means for infertility: For infertility practice, we see two potential consequences: The first relates to the use of stem cells in infertility practice and we currently are aware of two potential applications: the use of bone marrow-derived stem cells in the treatment of Asherman’s syndrome which has entered human applications in formal clinical trials,5,6 and the use of stem cells for intraovarian “rejuvenation” treatments which have been successfully investigated in a mouse model 7 but, to the best of our knowledge, have not yet been investigated in human trials, though we are aware of companies 8 and IVF clinics 9 already advertising such treatments.
The CHR is concerned about the injection of stem cells into ovaries without at least prior proper safety studies in animal models because stem cell therapies for some time have been known to carry a risk of cancer induction, 8 and ovarian tissue is known to be cancer prone. 9
The second relevant issue that arises from above noted court case is a question asked in response to the detailed report on the trial by the blog 4 involving the use of platelet rich plasma (PRP). PRP has, of course become widely utilized worldwide in fertility clinics, both intrauterine as well as intraovarian.
Above-described court decision, however, does, indeed,
raise the question whether injection of PRP can be equated to injection of stem cell products? The answer is more likely no than yes, but good arguments can be made on both sides: On the one hand, it seems likely that certain exceptions published by the FDA may apply. For example, the FDA allows for such an exception if tissues are immediately returned into the body of the patient, which is usually the case with PRP treatments. On the other hand, an argument for FDA supervision can be made, considering how different production of PRP is in different clinics, and how much clinical protocols differ. Likely the most important argument for better control over PRP treatments in infertility is, however, their still questionable utility, considering the scarcity of published trials.
In contrast to most other fertility clinics, the CHR, therefore, considers the use of PRP in infertility still as an experimental procedure and – moreover – is conducting several clinical trials of the use of PRP in different patient groupings.
1. Haseltine WA. Forbes. November 13, 2021. https://www.forbes. com/sites/williamhaseltine/2021/11/13/unregulated-stem-cell-clinics-endanger-patients-and-limit-research/
2. Wai et al., NIH. November 16, 2022. https://www.nih.gov/about-nih/ what-we-do/science-health-public-trust/perspectives/putting-stemcell-based-therapies-context
3. Kuriyan et al., N Engl J Med 2017;376(11):1047-1053
4. Segal J. Medical Justice Blog. November 1, 2024. https://medicaljustice.com/blog/regulation-of-stem-cell-clinics-sands-are-shifting/
5. Benor et al., J Assist Reprod Genet 2020;37(7):1511-1529
6. Flores et al., Fertil Steril 2024;122(4Suppl):E36-37)
7. Elias et al., eBioMedicine 2023;94:104715
8. https://ovoskill.com/
9. Meyer-Hermann M. Sci Reports 2018;11776
10. American Cancer Society. https://www.cancer.org/cancer/types/ ovarian-cancer/causes-risks-prevention/risk-factors.html
According to a recent article in The New York Times, Amherst College and the Massachusetts Institute of Technology experienced a significant drop in Black student enrollment for the new academic year. 1 The University of Virginia also reported a drop, but it was smaller. Other schools reported mixed results. School officials attributed those drops to last year’s Supreme Court decision that prohibited race-conscious admissions policies, though final consequences are not yet clear. At least one school administrator suggested that elite schools may, indeed, see a drop, while solid second-tier schools may very well see increases in enrollment of minorities.
1. Hartocollis A, Saul A. The New York Times. August 31, 2024. https:// www.nytimes.com/2024/08/30/us/black-enrollment-affirmative-action-amherst-tufts-uva.html
Likely accentuated by the recent elections, gender affirming care has remained a core subject in the political conflict between left and right, and we are not even referring here only (or even in principle) to gender-affirming care for incarcerated people or undocumented immigrants. We are just flabbergasted by how a relatively rare medical circumstance and its treatment could have become such a central concern for society.
We must bring up two recent occurrences: The first is a truly remarkable article in The Free Press by Tiger Reed, 1 a 44-year-old librarian who since 2016 has been married to Jamie Reed, known as the whistleblower who exposed in 2023 the alarming effects of gender-affirming medical care given to minors at the Washington University Transgender Center in the St. Louis Children’s Hospital in an article in The Free Press. 2 They also are mother and father of five children, two from Jamie’s prior marriage and three they adopted together.
And if you have not already started to expect some kind of a shocker, here it is: After living for 13 years as a married trans-man, he now was publicly announcing that he was detransitioning back to being a woman again.
And here is why, using, more or less, his own words: He had grave doubts about Jamie—at the time working as a case manager at the hospital in St. Louis—blowing the whistle. He wondered why she just didn’t quietly quit in protest of what she had witnessed. He was scared for himself, her, and their five children’s safety (and still is) and all of this “created a huge rift in their marriage which they are still working on to heal.”

He then, however, noticed something he initially did not want to face but which ultimately became unavoidable to recognize: His spouse and a growing number of knowledgeable critics had been correct!
“There was something fundamentally amiss with the message – especially to younger people – that a swift gender transition was a safe, all-purpose solution to profound problems.” And with this acknowledgment, he had to start addressing his own doubts about his own original transition.
Like Jamie has been speaking out against medical practices affecting young children and teenagers, Tiger now believes that he must speak out about adult gender medicine, “and how people have been misled – sometimes unintentionally – by gender clinicians about its safety and effectiveness.”
He also noted the Cass Review in England 3 (repeatedly discussed in recent months in the VOICE), which noted “the lack of scientific underpinnings for the widely accepted treatments of gender dysphoria especially in children – hormones and surgery – while failing to explore the often complex personal and psychological histories that lead people to believe that transition is what they need.”
And then there were – just recently – stories all over the newspapers that one of those academic gender physicians funded by the NIH to investigate long-term effects of gen-
der-based medical interventions in young children withheld publication of study results, once she recognized that the study did not demonstrate the beneficial long-term effects they had expected: puberty blockers—as the Cass Review already had properly deduced from the study of published literature—in young children did not improve the children’s mental health.
The principal investigator of this NIH-funded study (the broader project apparently had received $9.7 million in funding) was Johanna Olson-Kennedy, MD, a graduate of Chicago Medical School, who now is the Medical Director of the Center for Transyouth Health and Development at the Children’s Hospital in Los Angeles and Professor of Clinical Pediatrics at the Keck School of Medicine of the University of Southern California in Los Angeles. The New York Times, which must be given credit where credit is due for covering the subject of medical gender transition better and in more detail than any other U.S. publication, described Olson-Kennedy’s study as “unpublished because of politics.” 4
Interviewed by The New York Times reporter Anzeen Ghorayshi, Olson-Kennedy explained the delay in publication of the results of the study as “not wanting to weaponize the work” – of course, an inexcusable excuse for withholding any study results (to place results into an appropriate framework is an author’s responsibility in the discussion section of every publication). It is, however, potentially a breach of law when it involves federally funded research, and it seems unlikely that this investigator will ever be given again access to federal funding. Her standing at the NIH was likely also not helped by furthermore claiming in her interview that NIH cuts in her funding also contributed to the delay in publication. Not only is this excuse (to be polite) equally far-fetched as the first one, but based on the New York Times article, it was also denied by the NIH.

Johanna Olson-Kennedy, MD
What this scandal, however, once more demonstrates is the intrusion of politics into medical research as well as practice. Olson-Kennedy – unconsciously or consciously if she is
as smart as her position would suggest – was working in a politically highly controversial field, and likely, had secured considerable federal funding in anticipation of producing confirmatory data, not for a very logical hypothesis, but for a politically very opportune hypothesis. When the data did not support the political hypothesis, she decided to withhold it from publication because – once known – other parts of her grant support might have evaporated. At least she had the integrity of not manipulating the data!
This is, however, one more brilliant example that demonstrates the need to award research grants based on scientific merit and not based on political and/or ideological popularity of ideas.
1. Reed T. The Free Press. November 3, 2024. https://www.thefp. com/p/tiger-jamie-reed-detransition-wash-u-transgender-affirming-care
2. Reed J. The Free Press. November 3, 2024. https://www.thefp. com/p/i-thought-i-was-saving-trans-kids
3. Cass H. The Cass Review. 2024; https://cass.independent-review.uk/ home/publications/final-report/
4. Ghorayshi A. The New York Times. October 23, 2024. https://www. nytimes.com/2024/10/23/science/puberty-blockers-olson-kennedy.
– and infertility is a good example
A recent article by Heather Landi in Fierce Healthcare 1 noted that between 2012 and 2022, national health expenditures increased from $2.8 trillion to $4.5 trillion (+61%) and are expected to have grown to $7.7 trillion (another +71%) by 2032. If one compares these costs to the national domestic product (GDP), this is a quite significant proportion. While insurance coverage during this time has improved—uninsured declined from 48.6 million to 28 million (-42.4%)—life expectancy in the U.S. is only negligibly higher and almost 4 years below OECD countries. Obesity, diabetes, and behavioral health problems have been steadily increasing in prevalence. 30-day mortality rates in hospitals are, moreover, rising sharply, even if COVID deaths are excluded.
So, what is the conclusion? The article suggests that all stakeholders, whether an employer or payer, life science company or provider, will have to stop extracting value from the health care system in ways that maximize profits. Instead, efforts have to be directed at delivering value for the money spent, in the process optimizing the value for whoever ultimately pays for the medical treatment.
The concept of value-based medical care is, of course, nothing new. To the contrary, it, indeed, has become one of those “fashions of the moment” in recent years; but according to the article value-based care policies implemented so far, have in principle failed.
Looking at the infertility field from such a viewpoint, this, of course, should not surprise. One just has to look at all the “add-ons” introduced to IVF practice over the last 20 years with no evidence for any outcome benefits. Or how about all the changes in IVF practice that have led to the need for more treatment cycles, like for example routine all-freeze protocols? We, indeed, would argue that a study of value-based care in IVF over the last 20 years would demonstrate a straight line downward for every dollar spent. One strong hint that this is likely the case is the declining live birth rate in U.S. IVF cycles since ca. 2010, when the introduction of unvalidated “add-ons” to IVF started to accelerate. 2
REFERENCES
1. Landi H. Fierce Healthcare. October 1, 2024. https://www.fiercehealthcare.com/providers/new-analysis-points-troubling-trends-ushealthcare-costs-rise-health-outcomes-worsen.
2. Gleicher et al., Hum Reprod Update 2019;(3):hoz017
It is no secret that physicians hate prior authorization requirements and—as those have multiplied—that feeling has, if anything, only strengthened over time. The issue was recently raised by Lisa Marshall in respect to cancer treatments in an article in Medscape Medical News. 1 Working off a 2023 paper in JAMA Network Open that had offered further support for the notion that the need for prior authorization often causes harm to patients (the urgency in cancer care makes it a very good example), in a survey study of cancer patients, a full 22% of patients were found not to have received the care recommended by their treatment team because of pre-authorization requirements. 1
This is, of course, scandalous, and only adds to the argument that insurance companies increasingly are not only insuring but are—for all practical purposes—managing clinical care, and for that they are not licensed! Interestingly, when Marshall contacted the national trade group, America’s Health Insurance Plans (AHIP), nobody returned repeated requests
for an interview to comment on her story. Indeed, what is left for the health insurance industry to say?
1. Marshall L. Medscape Medical News. https://www.medscape. com/viewarticle/cancer-doesnt-wait-how-prior-authorization-harms-care-2024a1000hxt?form=fpf
2. Chino et al., JAMA Network Open 202
The fragmentation of medicine into traditional medical specialties and sub-specialties is now almost a century old and largely unchanged. Now comes Vivek Subbiah, MD, an expert in early-phase drug development, who in a brief article in Nature Medicine argues that it is time for reform. More specifically, he suggests that “transforming the fragmented silos of medicine into a wheel of collaboration, holds the key to tackling complex health challenges for generations to come.”1
We wholeheartedly agree! Increasingly, we find ourselves sharing more common research interests with colleagues in other medical specialties than in our own medical specialty of obstetrics and gynecology. This kind of realignment, of course, would have to start with medical school education and medical specialty training in residencies and fellowships. But a revolutionary reorganization of medicine along such lines appears increasingly unavoidable.
REFERENCE
1. Sbbiah V. Nat Med 2024;30:2394
Recently we heard a colleague at a prominent university complain that the postdocs at the university now had their own union and that this completely changed the relationships in their research laboratories. A recent article in Medscape Medical News, therefore, caught our immediate attention because it noted that residents are also joining unions in droves.1
The subjects they are fighting for are adequate parental leave, fair pay, and—believe it or not—adequate healthcare. Five weeks of paternal leave in California are not considered adequate and the goal of the local union now is eight weeks. Mass General Brigham Hospital in Boston certified its union in June of 2023, but there is still no contract in place between residents and the hospital. A major complaint is
that nurse practitioners and physician assistants are earning almost twice as much as residents.
1. Hochwald et al., Medscape Medical News. October 7, 2024. https:// www.medscape.com/viewarticle/why-residents-are-joining-unionsdroves-2024a1000iap?form=fpf
It was war in the South (Hamas, Gaza) since October 7, 2023, when Hamas terrorists in a surprise attack killed over 1200 Israelis of all ages in most gruesome ways and abducted over 200 as hostages; and it was direct war in the North (Hezbollah, Lebanon) since October 8, 2023, when Hezbollah, in solidarity with Hamas, started daily rocket attacks on Northern Israel, requiring the evacuation of over 70,000 Israeli citizens from that part of the country.
But the situation has gotten worse since then, and with Gaza destroyed and the Hamas leadership killed, the fighting is, nevertheless, ongoing. And over 100 Israeli citizens (including some Americans with dual citizenship) are still hostages in the labyrinth of underground tunnels crisscrossing the Gaza Strip. Barely half of them—among those an infant—are believed to still be alive.
The situation in the North has also deteriorated, with the Israeli army, after decapitating almost the complete civilian and military leadership of Hezbollah—once again—entering the southern part of Lebanon in an effort to displace all Hezbollah from all the area north of the Litany River, where under a prior U.N. resolution not a single Hezbollah fighter was supposed to set foot. And then things got even worse because, losing one surrogate after the other, Iran started attacking Israel and Israel started responding by attacking Iran directly rather than its surrogates.
Though presenting all of this in the News section of a medical publication may seem surprising, it really should not be, considering how much has been written about this Middle East conflict in medical journals. Nature magazine, for example, dedicated three full pages by Josie Glausiusz, a freelance science journalist who specializes on the Middle East,
describing how Palestinian and Israeli researchers continue working amid destruction of homes and labs and deaths of colleagues.1
In contrast to the balanced article in Nature, The Lancet turns to Clotilde Bigot (what an interesting name!), a freelance journalist and photographer based in Beirut, Lebanon, for an anti-Israeli hack piece on “Jenin’s struggle for health care access amid Israeli (military) incursions.”2 Anti-Israeli hack pieces in The Lancet are, of course, nothing new and will under the current editor-in-chief probably never end.
Unsurprisingly therefore, The Lancet in the same month also reprinted a Letter-to-the Editor without comment which – unopposed – was given the opportunity to use the Hamas slogan of an ongoing genocide in Gaza. 3 As a medical journal, The Lancet would obviously do better to stay out of politics if it cannot be balanced. Moreover, just as one should be able to expect such a prominent medical journal to use medical definitions correctly, so should this journal be aware of the correct definition of “genocide.” But neither editorial office nor the publisher apparently care, unfortunately continuing a long history of antisemitism and anti-Zionism in this journal.
And if we are already talking about antisemitism and anti-Zionism, things do not appear to get better on colleges; very much to the contrary as several recent articles suggest: A recent article by Dion J Pierre in The Algemeiner noted that, based on a study by the AMCHA Initiative (an antisemitism watchdog), the anti-Zionist campus organization Faculty for Justice in Palestine (FJP) is fueling antisemitic hate crimes and the collapse of discipline and order on college campuses all over the country. FJP is a spinoff of Students for Justice in Palestine (SJP), a group which has been repeatedly demonstrated to maintain links to several Islamic terror organizations. The MCHA report documented that campuses with established FJP chapters are experiencing multiple times higher assaults and death threats against Jewish students than campuses without presence of this organization. 4
In noting that campus problems did not start on October 7, Rachel O’Donoghue noted in Honest Reporting how the media became campus co-conspirators and concluded that for a meaningful reform to take root in American colleges, it must begin with a renewed commitment from the media. 5
That things, indeed, are getting worse, at least on some campuses, was recently reported by Sharon Otterman in The New York Times, 6 and who can be surprised that it again involves the Columbia University campus in NYC. The same student group that sparked the national encampment movement on the Columbia campus (Columbia University
Apartheid Divest), now announced that “it supports liberation (of Palestine) by any means necessary, including armed resistance” and described the October 7 attack on Israel as a “moral, military, and political victory.” And we, of course, have not read about any actions taken by the Columbia University administration against this group and its student as well as faculty members.
And then, of course, there is Harvard University, this time the target of an Op-ed in The Wall Street Journal by the novelist Dara Horn. 7 She noted in her piece that she had “the dubious distinction of serving on Harvard’s (by now infamous) Antisemitism Advisory Group, which went so badly that she ended up as a witness in Congress’s investigation of Harvard and – when she recently spoke at a summit for the Harvard Jewish Alumni Alliance, she had to be escorted across campus by an armed guard.” Her principal argument in the Op-ed was that at Harvard (and likely at other schools as well) “antisemitism begins in the classroom.” Yet, “the university ignored a suggestion to review its courses and lectures for academic rigor” regarding the subject of antisemitism.
She then ended her piece with ahistorical anecdote which elicited special resonance at the CHR since Norbert Gleicher, MD, the CHR’s Founder, Medical Director and Chief Scientist, grew up in Vienna, Austria, started medical school at Vienna University, and has held a Visiting Professorship at the university for many years:
“In the early 20th century, the University of Vienna, founded in 1365 (and the second-oldest university after Bologna University in Italy) was one of the world’s academic giants, until it caved in to student groups and faculty who celebrated terrorists and tyrants (what history now describes as Nazism). Today U.S. News & World Report ranks it 215th in global universities, slightly below the University of Cincinnati. Harvard has been around for only about 400 years, which in Jewish historical time is about 15 minutes. Maybe in another 400 years, Jews will look back and see that Harvard followed the University of Vienna’s path, its buildings mere memorials to what was once the world’s best education.”
The University of Vienna then


And, finally, we want to conclude the discussion of this subject with a Commentary by two academics from two different U.S. medical schools in The American Journal of Medicine, in which they propose “a way forward for the moral imperative of countering antisemitism in US medicine.
8 Basically following the argument made by Horn in her Oped, they conclude that everything starts with education, and requires engagement, empathy, and—yes—enforcement.
1. Glausiusz J. Naure 2024;634:501-503
2. Bigot C. Lancet 2024;404:1292-1293
3. Elnakib et al., Lancet 2024;404:1105-1106.
4. Pierre DJ. World Israel News. September 27, 2024. https://worldisraelnews.com/pro-hamas-faculty-group-fueling-antisemitism-on college-campuses-new-study-finds/
5. O’Donoghue R. United with Israel. https://unitedwithisrael.org/thecampus-problem-didnt-start-on-october-7-and-it-wont-end-thi-year/
6. Otterman S. The New York Times October 11, 2024. https:// www.nytimes.com/2024/10/09/nyregion/columbia-pro-palestinian-group-hamas.html
7. Horn D. The Wall Street Journal. September 22, 2024. https:// www.wsj.com/opinion/harvards-antisemitism-begins-in-the-classroom-jews-israel-education-e281604a
8. Wald HS, Roth S. Am J Med 2024;137(10):915-917
It increasingly appears we are drowning in misinformation. Traditional media accuse social media of being the main culprits, but as the most recent election campaign once again deftly demonstrated, our traditional media are also distributing misinformation. Like everybody and everything, medicine and science are also affected, and Science magazine, therefore, recently dedicated several interesting articles to the subject of misinformation.
All three articles are by Kai Kupferschmidt, a contributing
correspondent for Science. 1 In the first he noted that research on misinformation “has exploded,” though those trying to make some sense of the subject still face some basic challenges. And those start with the fact that the definition of what represents “misinformation” has really not been established yet. Even so-called “experts” strongly disagree (one of course under such circumstances must also wonder about the definition of what an “expert” is) whether, for example, lies, deepfakes, conspiracy theories, pseudoscience, propaganda, rumors, etc., indeed, represent misinformation.
A second major problem arises from the fact that, these days, everything seems – and to a degree is – politicized. As the articles notes, “we all are equally guilty” – especially in believing fake news about the other side. And a third problem is that the harm caused by misinformation is difficult to define because misinformation can change beliefs, and beliefs can lead to actions, and this sequence of events is, of course, for several reasons difficult to study, not the least because it would seem unethical to purposefully expose somebody to misinformation just to wait for that person to do something crazy.
And a final problem lies with the increasing difficulty of getting access to real life data often owned by companies which have no interest in sharing such data. Moreover, all of these problems are global.
A second article has the title (in very large letters) “YOU WON’T BELIEVE THIS,” and what is meant is that researchers are trying to “inoculate” people against misinformation by – as with some vaccines – giving small doses of (in this case) information about a certain subject ahead of time. Yes, this potential “therapy” indeed goes back to 1954, when some U.S. prisoners in the Korean war chose to stay in North Korea instead of coming back home. They were assumed to be “brainwashed,” and “experts” declared that our younger people must be taught more about American ideals to make them more resistant to enemy propaganda. It is basically the same theory that these days drives the concept of inoculation which is also called “prebunking.” However, it is only one among several experimental techniques currently under investigation which are trying to make people stop falling for and spreading misinformation.
The third article in many ways is the least revealing and least interesting because it basically features one researcher, Kate Starbird, PhD, whose research tracks falsehoods and then attempts to counter them in real time.
REFERENCES
1. Kupferschmidt K. Science 2024;386(6721)478- 482
2. Idem: 483-485
3. Idem 386-489
We recognize that how much medical journals should be involved in politics – and especially in election politics – has become a contentious subject. As medicine must survive and prosper in a politically increasingly splintered world, to simply ignore politics is no longer possible. Fair and balanced commentaries, therefore, can offer valuable contributions at times to often overheated debates. But this does not mean that leading medical journals should in a political debate lend their pages to pure propaganda for one side or the other.
Yet this is exactly what happened when JAMA – paradoxically exactly in its November 5 (number 17 issue) on Election Day published a Viewpoint article by three Boston University authors under the heading, “Health and the 2024 US Election” and titled, “The US Presidential Election’s High Stakes for the Future of Medicine.” 1 The article basically offered a (very negative) opinion (which we at least partially share) about the so-called Project 2025, while noting that the Republican Party Platform included (only) a few sentences on health care-related issues, while “specifics may be found within a policy ‘playbook’ published by Project 2025 outlining a comprehensive, concrete transition plan for each federal agency.”
And this sentence in their article was an indisputable lie because candidate Trump on innumerable occasions during the campaign had very definitely distanced himself from Project 2025 and, indeed, clearly stated that he not only had nothing to do with the document but opposed it on several grounds. 2
Project 2025 is also known as the “2025 Presidential Transition Network” and has been as a product of the Heritage Foundation, a conservative think tank. 3 The paper was, however, presented by the three authors as not only reflecting Trump’s opinions but as representing his plan of action regarding US healthcare during his second administration. That JAMA would publish such a misleading article is, therefore, really inexcusable because the claim that Project 2025 was foreseeing Trum’s action as president remained a major talking point of the Harris campaign until the end, even though the claim had been so many times rebutted by Trump.
If editors choose to allow politics into the pages of their journals (and nobody, of course forces them to do so), they, of course, concomitantly acquire the responsibility for such
publications. Here JAMA, the flagship journal of the American Medical Association (AMA) very obviously failed in this responsibility.
REFERENCES
1. Huberfeld et al., JAMA 2024;332(1&):1421-1422
2. The New York Times. September 12, 2024. https://www.nytimes. com/article/project-2025.html
3. 3.The Heritage Foundation. 2025. Mandate for Leadership. The Conservative promise; eds: Dans P, Groves S. https://static.project2025. org/2025_MandateForLeadership
Now it involves Spain: Juan Manuel Corchado, PhD, a professor of computer sciences and head of the University of Salamanca, Spain’s oldest university, has been accused of inflating his citation count. 1 Springer Nature retracted no fewer than 75 studies by the Spanish rector. 2

And then there is China: Science magazine also reports that China demonstrated that even whole countries can cheat. You have to give it to this country, it is well organized. Wanting to boost its global science ranking, it had to boost the ranking of its papers. And now it turns out that a “home-bias” in locally within China citing preferentially Chinese papers, did the job. Indeed, a majority of citations to (by citations) top-ranked papers came from within China.
REFERENCE
1. O’Grady C. Science 2024;336(6717):10-11
2. El Pais.. October 17, 2024. https://english.elpais.com/science-tech/2024-10-17/springer-nature-retracts-75-studies-by-the-university-of-salamanca-rector-and-his-collaborators-for-fraudulent-practices.html
3. Normile D. Science 2024;385(6717):11-12
3 YEARS OF MEDICAL SCHOOL ARE ENOUGH –
That is at least the impression based on a recent article and press release from NYU Langone.1, 2 Academic and residency performance between an accelerated 3-year MD program and the standard 4-year medical school program did not differ significantly in a trial program at NYU Grossman School of Medicine in NYC: 3-year students scored an average of 84% on their pre-clerkship exams; 4-year students 83%. They also had similar scores in clinical skills, communication, critical thinking and medical knowledge.
Considering the threatening shortage of physicians despite record numbers of new medical schools being established in the U.S., it should not surprise that 3-year programs are becoming increasingly common. 3 They not only will speed up the new physician supply, but – according to studies – could produce lifetime savings between $250,000 and $400,000

And the next step should be the shortening of residencies and sub-specialty fellowship. Does it really take 4 years to train a general Ob/Gyn? It definitely does not, for example, take three years to train a competent reproductive endocrinologist and infertility specialist (REI)! At the CHR, we can do that probably in one year for clinical competence and in two years for clinical as well as academic excellence. In other words, we could produce a new generation of highly competent REIs within 5 years from graduating medical school and within 8 years after college, with college being yet another subject that deserves scrutiny.
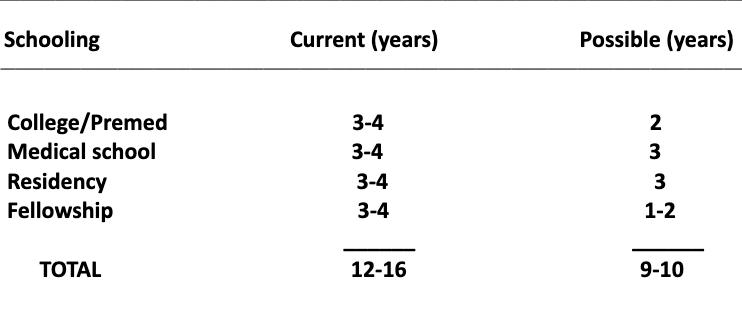
The table above demonstrates what would seem possible with just a little good will and imagination. As the table demonstrates, it should be possible to shorten the time after high school from 12-16 years to 9-10 years. The potential advantages and cost-saving for the country and individuals who wish to become physicians appear obvious. An easier and shorter route would also make the medical field more attractive again as a career choice.
REFERENCE
1. Satyamoorthi et al., Academic Medicine 2024. ():10.1097/ ACM.0000000000005896, October 15, 2024
2. NYU Langone Health Press Release, October 15, 2024. https:// nyulangone.org/news/accelerated-three-year-medical-school-students-perform-well-peers-traditional-four-year-programs
3. Palmer K. Inside Higher Education. November 4, 2024.
Scientists at Tel Aviv University in Israel discovered unexpectedly a previously unknown cancer mechanism that prevents the immune system from attacking tumors. Once they reverse the mechanism, the immune system is stimulated, and attacks cancer cells and eliminates them.1 The investigators discovered that skin-specific, UV-induced suppression of T-cell killing activity is mediated by an upregulation of Ly6ahigh T-cell subpopulation. These cells—independent of the UV effects—are in the tumor microenvironment induced by chronic type-1 interferon and treatment with anti-Ly6a
antibody enhanced the antitumor cytotoxic activity of T cells and reprogrammed their mitochondrial metabolism via the Erk/cMyk axis. In mice resistant to anti-PF1 therapy treatment with the Ly6a antibody inhibited tumor growth.
REFERENCE
1. Maliah et al., Nt Commun 2024;15:8354
Investigators from Stanford University (and collaborators) published a rather astonishing series of three papers in Nature magazine, demonstrating that extrachromosomal DNAs (ecDNAs) – also described as “small DNA circles”—are major drivers of cancer development. In their first paper the authors attempted to determine the prevalence and the clinical relevance (i.e., prognostic potential) of ecDNAs in thousands of cancers. In the process they discovered a new non-Mendelian method of inheritance that contradicts pretty much everything we used to believe about inheritance and, in the future, should lead to new therapies for cancer which target those small DNA circles. As the authors also noted, some clinical trials are underway.
ecDNA was in 2017 demonstrated to play a major role in cancer cell survival and proliferation. In the first of the three recent papers, the investigators found 17.1% of cancers contain ecDNAs. And their presence indicated metastatic spread and poorer clinical outcomes. The surprise was that some ecDNAs did not encode cancer causing genes directly but contained enhancer sequences which activate genes on other ecDNAs and in the process link ecDNA circles. In other words ecDNAs have to work together to enhance cancer growth.
Their second paper investigated what happens to ecDNAs when cancer cells divide and another surprising finding was that daughter cancer cells may have ecDNAs and others may not. In practical terms this provides a survival mechanism for the cancer because at least some populations of cells will have the right combination of ecDNAs to allow those cells to escape standard cancer treatments and – by doing so – establish drug resistance, and this finding, of course, is completely contradictory to the widely accepted Mendelian rule of independent assortment.
The third paper in the series addressed a possible new treatment approach toward cancer, considering what was learned about ecDNAs before and attempted to exploit a vulnerability of ecDNAs-containing cancer cells which is the
cancer cells’ dependency on excessive transcription of copying DNA into RNA. Excessive transcription occurs—as noted in the first paper—because of the interconnections between ecDNAs. If that process can be interrupted, cancer cells die. The interruption was achieved by blocking a checkpoint protein (CHK1) which is essential for cell division and, indeed, led to cancer cell death. Consequently, CHK1 blockers are already in clinical trials.
REFERENCES
1. Bailey et al., Nature 2024;635:193-200
2. King et al., Nature 2024;635:201-209
3. Tang et al., Nature 2024;635: 210-218
4. Conger K. Stanford Medicine. November 6, 2024. https://med.stanford.edu/news/all-news/2024/11/ecdna-cancer.html
A recent study in PNAS finally offer some explanations for the longevity of naked mole rats in comparison to all other rodents.1 These hairless rodents can achieve lifespans of 30 years or older (and, no, being hairless is not the story!). Here is the story in short: Everything starts with so-called retrotransposons.
They are epigenetically silenced, highly repetitive virus-like elements which, as science finally figured out, constitute nearly half of all mammalian genomes. The authors describe it in the paper as the “retrobiome” which through multiple explosive retrotransposon amplifications emerged during mammalian evolution. Its derepression has been linked to cancer risk and aging.
To assess current and past retrobiome activity, the authors devised a computational genomic methodology using processed pseudogenes, intronless cDNA copies of mRNAs formed as a “side product” of retrobiome activity. Their analyses then revealed that the retrobiome in naked mole rats had remained dormant for millions of years, while other rodents (mice and rats as well as other species) demonstrated active retrobiomes.
From these observations the authors concluded that retrobiomes may affect longevity or—to say it in a different way—low activity in certain sequences of the retrobiome favors longevity, while high activity may shorten lifespans. Interesting stuff!
REFERENCE
1. Kogan et al., PNAS 2024;121(45):e2313581121
It took an article in The New York Times to learn about this amazing story:1 the writer, Kate Morgan, reports on a woman who, after a propane explosion in a kitchen, was so badly burned with second and third degree burns all over her body, including her face, that she was placed for more than six weeks into an induced coma in the burn-trauma unit of a hospital. The treating physicians decided to use a rarely used tool in burn care for her face: They cut placenta into thin layers and applied those to her badly burned face and this— as the patient is quoted in the article to have commented afterwards—was “the best thing they could have done ever.” And she followed up by saying that her 47-year-old face “looked exactly like it did before” (and an accompanying photo, indeed, demonstrates no scarring whatsoever in a smiling face; see photo).

The article further noted that it has been known for some time that placental grafts like this can do miracles. They can reduce pain and inflammation and heal burns without scarring and even can restore vision and help with chronic wound healing. Yet from among roughly 3/5 million annually delivered placentas, only a minimal number are currently use. The vast majority – as the article noted – end up in hospital incinerators.
All of this is happening because placental tissue does not get attacked as “foreign” by the burn victim’s immune system. For-profit companies have, therefore, started manufacturing placental grafts and are selling them at quite amazing prices; according to the article, they go for $200 and $3,000 per each square centimeter (cm2). But it seems worth it!
REFERENCE
1. Morgan K. The New York Times. October 8. 2024; https://www. nytimes.com/2024/10/08/well/placenta-donations-burns-wounds. html
Since its establishment in 1964, the so-called Helsinki Declaration has undergone several revision while remaining the guiding light for the ethical conduct of research in medicine. And – following the Zeitgeist – it in the process, of course, had to go a little bit woke by (among other depiction of wokeness) for example stressing that inequities in research must be avoided or no longer referring to research “subjects,” but research “participants.” But not every change is driven by the current pandemic of wokeness: The revised document also attempts to protect better healthy trial volunteers and that is, of course, a very good thing. A lot of consents will have to be rewritten.
REFERENCE
1. Bibbin Domingo et al., JAMA. October 18, 2024.Published online. doi:10.1001/jama.2024.22530
THE ENERGY IT TAKES TO MAKE A BABY HAS BEEN VASTLY
Carissa Wong resurrected this subject recently in a Feature article in Nature magazine, pointing out that an Australian ecologist and evolutionary biologist in May of this year suggested that the extra energy it takes a human to produce a baby could be as much as 24 times more than had been previously estimated in what were considered the best models. What appears to make up the difference from earlier estimates are so-called indirect costs, the energy mothers expend in making (!) and carrying their pregnancies (in contrast to the direct costs which is the energy invested and stored in their offspring). These new data now suggest that, contrary to older models, indirect costs by-far outweigh direct costs.
REFERENCES
1. Wong C. nature 2024;634:768-769
2. Ginthere etal., science 2024;384:763-767
Inflammation – especially when localized – is, of course, always characterize by heat; but what this heat does to immune cells has so-far not been well understood. Now a paper in Science Immunology offers some insights.1 As it turns out, fever can enhance the function of T cells. A temperature of 39° C enhanced metabolism, proliferation, and effector function in mice of CD4 T cells and also slowed Treg Cells’ suppressive effects. But that is not all: fever also drives mitochondrial damage, which in turn drives apoptosis, which removes in the mouse and in humans a substantial amount of T-helper cells.
REFERENCE
1. Heintzman et al., Sci Immunol 2024;10.1126/sciimmunol.adp.3475
In a Research Briefing in Nature Medicine Argentieri MA and van Dujin CM from Mass General in Boston and the University of Oxford in the UK, developed a machine learning model (we are learning the enormous possibilities of A.I. in medical research!) that used blood proteomic to estimate a proteomic age clock for a large number of samples from the UK Biobank (n=45,441) over an age range between 40 and 70 and then validated the data in two other biobanks with smaller sample sizes.
The study identified 204 proteins which accurately predicted chronological age and 20 proteins that captured 91% of the accuracy of the larger model. The accuracy was the same in the other two biobanks from China and Finland. Proteomic aging was associated with the incidence of 18 major chronic diseases affecting different organs and was also associated with telomere length, frailty index, and several cognitive tests. For example, the bottom decile of proteomic aging developed Alzheimer’s disease over the following 10-15 years in less than 1% of cases.1
This is, of course, amazing stuff, and only the beginning of so much more to come in term of not only predicting disease risk and mortality, but also in assessing treatments to prevent diseases and extend life spans. This remarkable study was also discussed in a Research briefing in Nature Medicine. 2
REFERENCES
1. Argentieri MA, van Dujin CM. Nat Med 2024;:2415-2416
2. Carrasco-Zanini J, Langenberg J. Nat Med 2024;30:2419-2420
Hard to believe, but Rockefeller University, the institution with the largest number of Nobel Prize awardees, is selling some of its art collection: specifically, two pieces by Joan Mitchell are scheduled for auction and expected to bring as much as $32 million to the university, which has owned the two painting for almost 70 years.1 Both canvases were completed by the abstract expressionist in 1955 and David Rockefeller, then the chairman of the board, acquired them for the university. Cash must be tight at Rockefeller University these days, considering how little impact $32 million will have on the university’s overall budget.

According to the New York Times report on the pending sale, Rockefeller University has endowment assets of $2.5 billion but took in only $777 million during a fund-raising campaign over the last five years, a quite small yield considering the university’s scientific prominence and the financial wealth its board used to represent.
REFERENCE
1. Barron J. The New York Times. October 30, 2024. https://www.nytimes.com/2024/10/30/nyregion/rockefeller-university-joan-mitchell-paintings.html
That gut health may be involved in the development of Parkinson’s disease has been suspected for some time and has been summarized under the so-called “gut-first hypothesis.” What, however, may be the inciting event has remained unknown. In a new study published in JAMA Network Open, 1 investigators now developed evidence that that upper gastrointestinal mucosal damage was associated with increased risk to develop Parkinson’s disease. Specifically, patients with Parkinson’s were found to have more likely a history of H pylori infection, a history of having been treated with proton-pump inhibitors, with chronic non-steroidal anti-inflammatory medication use, gastroesophageal reflux disease, smoking, constipation, and dysphagia. The authors concluded that patients with these diagnoses may require special vigilance for Parkinson’s disease.
REFERENCE
1. Chang et al., JAMA Network Open 2024;7(9):e2431949
This is what, according to an article by Derek Bagley in Endocrine News, the audience at Endo 2024 believed after presentation of an abstract about a male contraceptive gel that suppressed sperm production faster than anything else proposed before. Supposedly the Boston Convention Center “was abuzz.”1
The treatment was presented as a Phase 2b clinical trial of a gel applied to both shoulders, which contained segesterone acetate (called Nestorone, also an ingredient of the Annovera vaginal birth control ring) and testosterone. A total of 222 men completed at least three weeks of daily treatment with the gel, which contained eight milligrams of segesterone acetate and 74 milligrams of testosterone. Study subjects applied the gel once daily to each shoulder blade (to reduce the risk of exposing the gel to others).
The gel induces an endocrine feedback loop between the pituitary and the gonads, which involves secretion of luteinizing hormone (LH) from the pituitary that causes the testes to make testosterone and follicle-stimulating hormone (FSH). Segesterone acetate stops the pituitary from secreting LH and FSH, shutting down the production of testosterone. Local testosterone concentration in testes is higher than in blood; when testosterone falls below a threshold, the testes stop producing sperm. But men would like to maintain a normal libido and muscle mass, so the gel replaces testosterone in blood, though without it accumulating in the testes.
As the article also noted, researchers see male contraception as a women’s health issue since women are the ones who get pregnant if they don’t have a contraceptive, and women don’t always have the best experiences with contraceptives.
REFERENCE
1. Bagley D. Endocrine News. October 2024. https://endocrinenews. endocrine.org/shouldering-responsibility-could-a-male-contraceptive-gel-be-a-birth-control-game-changer/
Antibodies against the cell-membrane component phosphorylcholine (anti-PC) have been reported to be protective against atherosclerosis, cardiovascular disease (CVD), and other chronic inflammatory conditions. Two underlying potential mechanisms appear to be anti-inflammatory, clearance of dead cells, and inhibition of oxidized low-density lipoprotein effects.
Most of related research has, however, so-far been done only in men. In a very interesting article in the JACC Swedish investigators now determined the role of IgM anti-PC on the incident of CVD among women. In a total of 932 women, age 66 ± 6 years, IgM anti-PC levels were measured. Prospective associations with any first CVD, ischemic heart disease (IHD), myocardial infarction (MI), and ischemic stroke were assessed, with the model adjusted for potential confounding factors.
Over 16 years (13,033 person-years), 113 cases of composite CVD were noted. IgM anti-PC was statistically significantly inversely associated with risk of ischemic heart disease, and with myocardial infarction (MI), but not with ischemic stroke. The authors concluded that IgM anti-PC may play an active role in inhibition of CVD development in women, especially MI. Furthermore, low IgM anti-PC levels may play a role in identifying those at risk. 1 Postmenopausal women in the highest of three possible antibody levels demonstrated a 73% lower risk of CVD than women with lowest levels of antibody.
A few additional comments appear in place: (i) The antibody to phosphorylcholine is a so-called “natural” autoantibody. This means that we all have this antibody even in absence of any disease. (ii) This autoantibody should not be mixed up with another natural autoantibody, the anti-phosphatidylcholine antibody, which is one of several anti-phospholipid
antibodies (APAs) and—like other APAs—has been associated with miscarriage and thrombosis risk. (iv) Here the association is inverted in contrast to APAs (high levels are good, while with APAs high levels are bad). (v) This has not only diagnostic significance but may also lead to therapeutic utilization of this antibody. (vi) Isotype IgM antibodies are the acute-phase reactants in the first 30 days of exposure to a stimulant, demonstrating another principle in recent years better and better understood: some inflammatory process— especially if low grade—can be beneficial.
The authors concluded—and we fully agree—that chronic inflammation contributes to atherosclerosis and CVD, and that low levels of anti-PC among men and women contributes to this process. They, furthermore, suggested that involved mechanisms include anti-inflammatory activity of the antibody and increased clearance of dead cells and oxidized lipids, furthermore suggesting that the raising of anti-PC antibodies through immunization deserves consideration as a preventive treatment for certain CVDs.
1. Frostegård ey al., G Am Col Card. 2024; Epublished DOI: 10.1016/j. jacadv.2024.101298
CENTRAL ILLUSTRATION: Antibodies Against Phosphorylcholine and Risk of Cardiovascular Disease in Women

Frostegärd J, et al. JACC Adv. 2024;10.1016/j.jacadv.2024.101298

BRIEFING: A recent article in Medscape Medical News asked a question we asked in the VOICE months ago: “Are GLP1s the newest fertility treatments”?1 We, indeed, not only asked the question, but also answered it—with a great degree of certainty—in the affirmative, not only because GLPs are so incredibly successful in achieving weight loss, but because their effectiveness has transformed weight loss into a practical treatment goal that until now had not been realistic because so many infertile couples, of course, do not have the time to delay their treatment for too long.
GLP-1s, therefore, once again lead this section of the VOICE, followed by News from the Restaurant Scene. And, of course, our list of favorite restaurants in NYC, primarily for the benefit of the many out-of-town visitors to the CHR who this month, because of the annual Foundation for Reproductive Medicine Conference, will be present in NYC in larger numbers than usual.
REFERENCE
1. O’Mary L. Medscape Medical News. November 8, 2024. https://www.medscape.com/viewarticle/are-glp-1s-newest-fertility-treatment2024a1000kfa?form=fpf
And this new family of wonder drugs is marching on: A new study in the New England Journal of Medicine reports that once-weekly semaglutide in individuals with obesity and knee osteoarthritis with moderate-to-severe pain, unsurprisingly, resulted in significantly greater reduction in body weight and osteoarthritis-related pain than placebo. 1 An accompanying editorial, however, made additional important points: 2 First, the author notes that obesity increased the risk of knee osteoarthritis in two ways: Through obvious mechanical stress from the excessive weight on the joints, but also through the excessive visceral adipose tissue which secretes adipocytokines and other soluble mediators of pain. In addition, inflammation in the joints also contributes to pain and so do structural deteriorations through cartilage loss.
As the editorial notes, unfortunately, anti-cytokine therapies, which have been successful in rheumatoid arthritis, have been shown to be much less successful in osteoarthritis. GLP1s obviously facilitate weight loss, but also have anti-inflammatory and immunomodulatory effects. The authors in other words suggest that the observed improvement in knee pain may not only be due to the wight loss.
And knee osteoarthritis is not the only new indication for GLPs: An abstract at the annual ASRM conference in Denver presented by researchers from Harvard University claimed that GLP-1s offer in women with type 2 diabetes better protective benefits from developing uterine fibroids than metformin and insulin. This has relevance because, as the investigators noted, type 2 diabetes and obesity are associated with insulin resistance which, in turn, is associated with increased risk of developing fibroid tumors. 3 Does this mean that GLP-1s may be able to decrease the prevalence of fibroids in genetically predisposed women even if they are not obese and diabetic?


And not to be forgotten, in patients with type 2 diabetes semaglutide was also shown to be associated with a 40% to 70% reduction in risk for first-time Alzheimer’s disease, in comparison to other diabetes medications. 4
But not everything that shines is gold: One increasing concern – though so-far available data are still contradictory – is the possible association of significant weight loss from GLP-1s (especially in older individuals) with sarcopenia 5 which – as the article notes – creates a twofold increased risk of mortality.
Also based on an abstract at ASRM 2024 in Denver an anonymous article in Healio quotes Richard S. Legro, MD, chair of OB/GYN at Penn State Health in Hershey, PA, as reemphasizing that, due to GLP-1s, the subject of wight loss for obese patients with infertility is coming up in counseling more often than before, “but comes with its own list of risks and benefits that must be carefully considered.” 6
The two key takeaways of the article were that (i) women with obesity can (still) successfully become pregnant, often without fertility treatments; and (ii) clinicians should avoid perpetuating stigma when discussing weight loss with patients struggling to conceive.
We are not sure we would word the conclusions in this way because Lego himself very well describes how quintessential an issue obesity has become in regard to infertility in women as well as men: Ca. 40% of all infertility patients are obese. Moreover, obesity is associated with basically every adverse fertility outcome, from time to pregnancy, to pregnancy loss, pregnancy complications, preterm delivery, gestational diabetes, preeclampsia, Cesarean section rates large for gestational age infants, and neonatal adverse outcomes.
While noting all of these associations, he in the next sentence is quoted as saying that the effects of obesity are “exaggerated in the public’s and clinicians’ minds.” Sounds to us a little contradictory!
Finally, a Feature article by life science reporter Mariana Lenharo in Nature magazine asked the quintessential

question, why do obesity drugs seem to treat so many other ailments? The final answer is, of course, not known yet, but it is already obviously clear that it is more than just weight loss that offers so many different clinical benefits. One of those, as the article notes, is the taming of inflammation. Another is – because of the ability to cross into the brain – substantial central-nervous system effects from anti-addictive behavior, to Parkinson’s and Alzheimer’s (see above), and according to most recent reports maybe also in depression.
1. Bliddal et al., N Engl J Med 2024’391:171573-1583
2. Felson DT.N Engl J Med 2024;391:17:1643-1644
3. Jin Hsieh et al., Fertil Steril 2024. DOI: 10.1016/j.fertnstert.2024.07.360
4. Wang et al., Alzheimer’s Dement 2024:;1-12. DOI: 101002/alz.14313
5. Lucas EJ. Medscape Diabetes & Endocrinology. October 16, 2024. https://www.medscape.com/viewarticle/unseen-cost-weight-loss-and-aging-tackling-sarcopenia-2024a1000inn?form=fpf
6. Healio.October 21, 2024. https://www.healio.com/news/womens-health-ob-gyn/20241021/patients-need-honest-data-why-weight-loss-is-notan-easy-answer-for-infertility
That dietary restrictions in calorie intake can have a positive impact on longevity has been reported for several decades, first demonstrated in animal models and more recently also in human experience. Now, however, comes a group of investigators from several U.S. institutions who offer interesting new mouse data that suggest that the impact of dietary restrictions on health and lifespan does not necessarily correlate.
The study demonstrated that both caloric restriction and intermittent fasting resulted in lifespan extension in proportion to the degree of restriction. Lifespan was heritable and genetics affected lifespan more than dietary restriction. The strongest trait associations with lifespan included retention of body weight through periods of handling. Health effects differed between interventions and exhibited inconsistent relationships with lifespan extension. 40% caloric restriction had the strongest lifespan extension effect but led to a loss of lean mass and changes in the immune repertoire that could confer susceptibility to infections. Intermittent fasting did not extend the lifespan of mice with high pre-intervention body weight, and two-day intermittent fasting was associated with disruption of erythroid cell populations. Reduced adiposity and lower fasting glucose were not associated with increases, strongly suggesting that dietary restrictions do more than counteracting the negative effects of obesity.
Health effects differed between interventions and exhibited inconsistent relationships with lifespan extension. The strongest lifespan extension effect was seen with 40% caloric restriction but led to a loss of lean mass and caused changes in immune function which could increase susceptibility to infections. Intermittent fasting did not extend the lifespan of mice with high pre-intervention body weight, and with prolonged two-day intermittent fasting erythroid cell populations were disrupted.
Interestingly, reduced adiposity and lower fasting glucose were not associated with increased lifespan. This observation alone suggests that dietary restrictions go beyond just counteracting effects of obesity.
Improving health and extending lifespan are, thus not synonymous. From a clinical standpoint this raises the important question which of these two endpoints is more relevant in considering aging interventions in preclinical models and clinical trials.
REFERENCE
1. DiFrancesco et al., Nature 2024;634:684-694

Related to the above, yet distinct, a recent article in Nature magazine by journalist Nic Fleming in turn explored how scientists—in attempts to improve immune function and health and/or treat diseases— investigate the link between what people eat and how their immune system responds. 1 Data for example suggest that intermittent fasting can reboot the immune system, or beneficial bacteria in the gut can be helped through a plant-based diet. Mushroom tea in place of coffee may improve anti-cancer immunity, etc.
The article makes it clear that this is a new field which has made great strides in the last five years but still has some way to go. And then there is the widely known association between obesity and a whole variety of diseases, from cardio-vascular to some immunological diseases and even cancer. All of these disease groups, of course, interact very closely with our immune systems. Just switching from high- to low-fiber diets within days reprograms the immune system, for example in mouse models and in humans. Switching mice to a high-fat diet suppresses their immune system and makes them more susceptible to infections.
Anybody who has ever witnessed the effects of an anti-inflammatory diet on some women with very advanced endometriosis knows that this is not only imagination and/or a placebo effect. What we feed our bodies without question can affect our immune systems. The principal question that still remains to be answered, however, is which diets for which conditions?
REFERENCE
1. Fleming N. Nature 2024;634:529-531.
A new framework for the management of obesity in adults
The below figure reflects in graphic format the new framework for diagnosis, staging, and management of obesity proposed by the European Association for the Study of Obesity, recently proposed after a consensus process in Nature Medicine. 1
REFERENCE
1. Busetto et al., Nat Med 2024;30:239-2399


More future Michelin-starred restaurants for NYC – and a preliminary new restaurant review
The Michelin Guide on November 12 announced 19 more restaurants in addition to the over 400 the larger NYC area already holds. We must acknowledge that we have become increasingly skeptical when it comes to the judgment of many of the Michelin inspectors who allegedly constantly survey in secret the landscape of cities with Michelin listings. But one cannot argue with the persistent influence of these ratings and we, therefore, introduce to you here the newcomers as announce by the Michelin Guide.1 We are sure that one or the other will appear in these pages in the coming year described in more detail if found worthwhile for being exceptional (good or bad). The idea is that some of our readers may want to try some of these newcomers before us. And here they are in alphabetic order:
ACRU – Contemporary bistro, Greenwich Village
Supposedly the Atomix team is behind the scenes responsible for this new prix fixe place in Greenwich Village (Chef is Daniel Garwood) which – as we learned during a visit – is trying to bring Australian cuisine to NYC. We have in recent years been rather disappointed by the food at practically all new restaurants of the Atomix group, and Acru, unfortunately, was no exception. On a side note, the place does not offer any coffee drinks, though they do offer deserts.
BAYON – Traditional Cambodian, Upper East Side
BUNGALOW – Traditional Indian, Lower East Side
CAFÉ BOULUD – Traditional French, Upper East Side
Previously reviewed by the VOICE and after several visits deemed very disappointing.
CÉSAR – French and mostly seafood, Tribeca
A PRELIMINARY REVIEW: We recently had the opportunity to visit the new restaurant of César Ramirez for the first time. As the name already indicates, this new place, after his rather nasty falling-out with the ownership of Chef’s Table, is now all his. At least after this first visit, we are not sure that this is such a good thing—but more on that later.

We have known Ramirez for many years, starting with his days with David Bouley and, later on, during his long stewardship at Chef’s Table at Brooklyn Fare, first in its original Brooklyn location and later in the Hudson Yard area in Manhattan. This restaurant, of course, first earned three Michelin stars when still in Brooklyn in the back of a local supermarket, a concept it retained after moving to the Hudson Yards area in its current Manhattan location. Ramirez was from the beginning one of Bouley’s most talented apprentices (we to this day admire Bouley as likely the city’s single most talented chef and culinary teacher since the mid-1970s) and, therefore, were not surprised when Ramirez transformed this small backroom counter-space restaurant in Brooklyn into a three-star Michelin restaurant that became a pilgrimage site for Manhattan foodies.
However, we also have to acknowledge that after its move to Manhattan, the Chef’s Table lost not only some of its original charm as a real “backroom” (by becoming a much sleeker “back-room”) but – more importantly – Ramirez’s cooking progressively appeared to lose more and more of its initial creativity. And then came the painful breakup between Ramirez and the owners of Chef’s Table which not only ended up in court but also resulted in the temporary closing of Chef’s Table (it has now reopened under two new co-chefs, and we are planning a visit soon) and led to the opening of César, with Ramirez fully in charge as the principal owner.
We, thus, were very much looking forward to our first visit to César, hoping for the resurrection of Ramirez’s original talent and creativity. Unfortunately, this was not what we discovered: Finding a locked restaurant door without an explanation (or a bell), one for a moment is left asking whether the place is at all open. After we knocked at the door, a young lady unlocked it and asked for the name on the reservation before leading us to our table.

In analogy to the Chef’s Table restaurant, César has roughly one-third of its seats along a counter surrounding the wide-open kitchen of the restaurant, but in contrast to Chef’s table also has roughly a dozen small and widely-spaced tables filling the rest of a large and very roomy space, of sleek modern design. One can assume that, once reservations increase (the restaurant does not accept walk-ins, which likely is the reason for the locked front door), the currently unusually large spaces between tables are meant to offer an opportunity for having more tables in the space.
The restaurant offers two tasting menus, the Chef’s Tasting Menu at $365 per person and a Seafood Tasting Menu at $265 per person, with parties having to choose the same menu. But we also learned that extras to those menus, which the staff gallantly offers without noting their rather exorbitant additional costs (Caviar addition to a soup dish, $75 per person; White Truffle and Uni addition to a Dover Sol course, $225 per person; and an almost uneatably bad Wagyu dish, $185 per person), increasing the per-person cost of a tasting menu by a total of $485 per person to $850 and $750 per person, of course still excluding additional extras, like water, drinks, wine,

coffee and, of course, tips. To escape a tasting menu at César for less than $1,000 per person, therefore, appears impossible.
Is it worth it? One, of course, must ask whether any restaurant meal can be worth a price tag of over $1,000 per person? And, if there, indeed, exists such a meal anywhere in the world, we have so-far not encountered it. And it very definitely was not the meal we got served on this evening. Among the 11 courses of the Chef’s Tasting Menu (plus above noted extras), our small group found only two courses to be “excellent.” Two courses, including above-noted extra Wagyu steak dish and one of two desserts that were offered, were so bad that we returned them almost untouched; and the remaining 9 courses were simply forgettable.
Add to this a painfully slow (though very polite) service that stretched the dinner out to over three hours (despite quite large kitchen and wait staffs) and a rather small clientele for a weekend evening, this restaurant has a long way to go to earn any Michelin accolades. As of now, it does not come even close to joining the CHR’s Favorite Restaurant List. There is, after all, still Le Bernadine (3 Michelin stars) and Caviar Russe (1 Michelin star) which offer similar (and better) fare at a fraction of the cost.
DAPHNE’s - Italian American, Brooklyn
ISHQ – Traditional Indian, Lower East Side
JOO OK – Fine-dining Korean, Koreatown
LE VEAU D’OR – Traditional French, Upper East Side
A traditional name since 1937, recently taken over by the Balthazar and Minetta Tavern team, just received a somewhat disappointing New York Times review of only 2 stars.
LINGO – American and European comfort food with Japanese influences, Brooklyn
LUNGI – Traditional Indian and Sri Lankan, Upper East Side
OCTO – Contemporary Asian Korean Chinese fusion, Koreatown
ODRE – Korean, East Village
OKONOMI – Contemporary mostly Japanese seafood, Brooklyn
SAWA – Middle Eastern, Brooklyn
SEE NO EVIL PIZZA – Pizza, Midtown West

THEODORA – Mediterranean, Brooklyn
UZUKI – Japanese, Brooklyn
VEERAYS – Contemporary Indian, West Village
REFERENCE
1. Michelin Guide, November 12, 2024. https://guide.michelin.com/us/en/article/dining-out/michelin-guide-new-york-new-additions-restaurant
According to Eater, Le Café Louis Vuitton has opened on the fourth floor of the new temporary Louis Vuitton location1 which will last for several years while the principal Vuitton store, taking up the whole building on the north-east corner of Fifth Avenue and 57th Street, will be demolished from the inside out and rebuilt with significantly more square footage. The new temporary space is in the old Nike store almost kitty-corner from the new construction site, with rumors circulating that completion of this project may take up to five years.

The concept of the restaurant is similar to L’Avenue at Saks just a few blocks south on Fifth Avenue which is a partnership between the department store and the L’Avenue restaurant of the famous Hotel Costes group in Paris.
Le Cafe Louis Vuitton on the 4th floor of the new temporary Louis Vuitton store on 57th Street

REFERENCE
1. McCart M. Eater, New York. November 14, 2024. https://ny.eater.com/2024/11/14/24296341/le-cafe-louis-vuitton-opening-stephen-starr?ueid=f1e79ceb7d146f06663408e592a07377&utm_source=Sailthru&utm_medium=email&utm_campaign=Eater%20NY%2011/14/2024%20 am&utm_term=Eater%20NY
All listed restaurants are in Manhattan unless otherwise noted. Like all opinions about restaurants, ours are subjective and are to be understood as such. If you visit one of them, let us know whether you agree with our ratings. We value your feedback.
SYMBOLS WE USE IN OUR RATINGS
$ Inexpensive - Not worth the trip + Overall favorite of the CHR
$$ Moderately expensive
$$$ Expensive
$$$$. Special event expensive
• Good v Special vibe
•• Very good M Michelin starred
••• Excellent V Vegetarian/vegan dishes on
•••• Uniquely delicious the menu
AUSTRIAN
Koloman +/•••/$$/v 16 W 29th Street (212) 790-8970 V; Excellent desserts
Wallsé +/•••/$$/v/* 344 W 11th (212) 352-2300 V; Excellent desserts
CHINESE
Hwa Yuan Szechuan +/•••/$$/v 42 East Broadway (212) 966-6002 V; Authentic Szechuan Mr. Chow Downtown +/••/$$$/v 121 Hudson St., Tribeca (212) 965 9500 V Uptown 324E, 57th Street (212) 751 9030 V
CONTINENTAL
425 •••/$$$/v
425 Park Avenue (212) 751-6921 V; Gorgeous restaurant FRENCH
Le Gratin ••/$$
5 Beekman St. (212) 597-9020 V; Try the gratin potatoes
Le Charlot +/•• /SS 19 E 69th St. (212) 794-6419 V; Best steak au poivre & Thai mussels; great desserts
Le Bernadine +/••••/$$$$/ MMM 155 W 51st (212) 554-1119 V; Mostly seafood. Likely the best NYC restaurant
Cipriani Downtown +/••/$$/v
376 West Broadway (212) 343 0999 Great food, beautiful people & Uptown 781 5th Avenue (212) 753-5566 Great food and high society
Elio’s +/•••/$$/v 1621 2nd Ave. (212) 772-2242 Best Italian home cooking and where everybody meets Principe ••/$$/v
50 West Broadway (212) 335-0509 V; mostly seafood but one of the best chicken dishes
Sistina •••/$$$ 24 E 81st St. (212) 861-7660 V; Amazing wine list FRENCH-ITALIAN
Café Carmellini •••/$$$$/v
JAPANESE
SUSHI
Sushi Ann +/••• /$$$$
250 Fifth Avenue (212) 231 9200 V; Gorgeous place, top service; sophisticated and adventurous food
8 E 51st St. (212) 755-1780 V; Best quality fish; make reservation at the bar
GENERAL
Sakagura +/•••/$$ 211 E 43rd St. (212) 953-7253 V; Amazing food; Best sake selection
Yakitori Torishin +/+++/$$$/M 362 West 53rd Street (212) 757-0108 Unique and amazing skewer restaurant
KOREAN
Jungsik •••/$$$$/ MM 2 Harrison St. (212) 219-0900 Where NYC’s Korean restaurant revolution was born …
Oiji Mi +/•••/$$/v / M 17 W. 19th St. (212) 256-1259 … and has continued
GREEK
Elias Corner (Queens) ••/$ 24-02 31st St. (718) 932-1510 Mostly seafood HAMBURGERS
Jackson Hole Burgers (the “original”) +/••/$ 232 E 64th St. (212) 371-7187 Not a place for vegetarians
Dagon ••/$$ 2454 Broadway (212) 873 2466 Best hummus in NYC NEW YORK JEWISH DELI
P. J. Bernstein’s Deli •/$ 1215 3rd Avenue (212) 879-0914 All the great classics; pastrami, chicken soup PERUVIAN
Mission Ceviche •••/$$ 1400 2nd Avenue (212) 650-0014 If you like Peruvian –the best
PIZZA
San Matteo Pizzeria e Cuccina ••/$ 1559 2nd Avenue (212) 861-2434 True Napoli POLISH
Karczma (Brooklyn) +/•/$ 136 Greenpoint Avenue (718) 349-1744 Great authentic Polish food – and dirt-cheap
ROMANIAN-JEWISH
Sammy’s Roumanian Steak House** $$ 112 Stanton St. (212) 673 0330 Authentic JewishRomanian Steak House, with entertainment
UKRAINIAN/RUSSIAN
Caviar Russe +/••••/$$$$/ M 538 Madison Avenue (212) 980-5908 V; Most underrated restaurant in NYC
Russian Samovar •/$/v 256 West 56th St. (212) 757 0168 Great Russian/ Ukrainian food and music
Any suggestions and/or comments, please write to social@thechr.com.




BRIEFING: The VOICE in this section offers commentaries on a broad survey of recent articles in the English literature which the CHR found of interest, even if, at times, not immediately applicable to daily clinical practice. Articles are mostly chosen for their potential translational value to clinical medicine, often helping in determining where clinical practice will likely go. Translational research has been one of the CHR’s principal goals since its founding in 1981.
We survived the “big” election – some may say barely – and, as somewhat of a pleasant surprise, we did so without uproar and/or destruction in the streets. Compare this to the Netherlands, Belgium, France, or the U.K. where demonstrations recently have turned violent. The scenes in French cities after the country’s recent election were a good example. But that does not mean that politics do not invade medical practice, including in reproductive medicine.
We see it in medical journals like The Lancet, which will always find a reason to criticize Israel; 1,2 but never found it worthwhile to note that nobody from the Red Cross has in over a year visited Israel’s over 100 remaining hostages in Gaza even once, and that included one infant.
And then there is, of course, the issue of political correctness that is permeating academia probably more so than any other sphere of life. In that regard, we were impressed by an Op-ed in The Wall Street Journal by Roland Fryer, a professor of economics at Harvard (yes “liberal” Harvard), a founder of Equal Opportunity Ventures, and a senior fellow at the Manhattan Institute, with the heading, “The Economics of Political Correctness.” 3
In it he makes the point, which we paraphrase thus, that scholars must be incentivized to tell the truth, and not (as has become practice) to hide it and, instead only promote socially acceptable ideas. Only a decade ago, this statement would have attracted little or no attention because its content would have seemed so obvious. Nowadays, however, in most contemporary academic circles this statement would be probably viewed as discriminatory or even racist.
The author asked what can be done and concluded the following: A careful reassessment of how members of

academic faculties are hired and promoted. To say it even more bluntly, he noted that “instead of having faculty candidates sign statements swearing fealty to DEI, perhaps we should have them promise to tell the truth (what an idea!).” And in addition, academic institutions must create “high-powered incentives” for people who are – regardless of politics – correct in what they say or do.
He concludes – and we are here quoting verbatim – “I am gravely concerned about the rise of political correctness on college campuses, its effect on the type of analysis that is being published and being taught, and how this will undermine, among many other things, efforts to help the marginalized in America. Such efforts will succeed only if they are rooted in the truth.” We couldn’t agree more!
And – believe it or not – big company bosses have stopped chasing after Ivy League Degree job candidates, as another recent article in the Wall Street Journal pointed out, 4 “pedigrees from elite universities, like Harvard and Yale, now often work against job seekers from such schools. 4 They just often appear to be too miseducated!
1. Irfan et al., Lancet 2024;404:1725-1726
2. Gilmour S. Rahman S. Lancet 2024;404:1726
3. Fryer R. The Wall Street Journal. November 11, 2004, pA15. https://www.wsj.com/opinion/the-economics-of-political-correctness-scholars-needincentives-to-find-truth-not-hide-it-263c7aa1
4. Borchers C. The Wall Street Journal. November 11, 2024. https://www.wsj.com/opinion/the-economics-of-political-correctness-scholars-needincentives-to-find-truth-not-hide-it-263c7aa1
It is difficult these days to get a straight answer from colleagues in response to the question of how business is these days. We hear it’s very busy which – we would assume – means that business must be good. After all, patients report months-long waiting periods for an appointment at some clinics. But why is then everybody you speak to these days among service providers seemingly so unhappy?
That is, except maybe for longstanding CHR friend Andrea Vidali, MD, a practicing reproductive endocrinologist in NYC who has achieved significant prominence in endometriosis surgery and has seen his surgical practice booming like never before. Almost everybody else, however, seems to be complaining, and that appears weird, considering that staffing shortages in virtually all positions in the infertility field have pushed salaries into the stratosphere.
So why is that?
There, of course, is likely no one answer that applies to everybody; but what may represent a unifying link for all of this restlessness we are perceiving in the field appears to be the various consequences from a major generational change that has been taking hold over the last decade. The first generation of providers of IVF services started to retire ca. 15 years ago and since they usually owned their clinics, they ended up selling them. Their willingness to cash out spurned the unprecedented industrialization of infertility, with the field going from almost exclusive ownership by physicians and academic institutions going to ever-increasing ownership by private equity and other non-medical financial entities. Consequently, physicians are – mostly – no longer in charge of the field and, if what we are really hearing from all over the U.S. and Canada, this appears to be at the core of much of the unhappiness.
Now in the U.S. additional uncertainty is provided by the outcome of the elections and by a series of class action suits filed (see article on page 8) . We also elsewhere in this issue of the VOICE (page 3) address the concerns

heard from many colleagues who are expecting restrictions in IVF practice from Republican control of the government. As noted elsewhere, we do not share this opinion and, indeed, believe that the IVF field may receive additional support from the government, as President-elect Trump was very clear about wanting to expand access to IVF.
The Wall Street Journal, however, reported that venture capital and startups in reproductive health are nervous and are “scenario planning” how the elections might affect abortion services and other areas in reproduction. 1 Especially Kindbody, a nationwide network of infertility clinics, according to the article is concerned and “is prepared in case states enact IVF restrictions.”
REFERENCE
1. Gormley B. The Wall Street Journal., November 2, 2024.. https://www.wsj.com/articles/reproductive-health-startups-prep-for-election-outcome-d7f27bee
European colleagues recently published an interesting paper on variability in mammalian embryogenesis which, of course, also relates to us humans. 1 For the longest time molecular and cellular variability has been considered detrimental. More recently, however, it has become apparent that such variability plays a crucial role in cellular decision making and robustness. This makes the early variability in gene expression, cleavage timing, and in mechanical parameters in embryos an excellent model. In investigating embryos, they found that stochastic variability in cleavage timing played a very important role in achieving developmental consistency. Minimizing surface energy and compaction, moreover, select configurations with minimal energy needs and drive transitions in this direction, which leads to a decline in spatial variability. Finally, the zona pellucida apparently constrains the range of structures in early embryos. Combined robustness is ensured and these observations, moreover, demonstrate the potential adaptive benefit of stochastic processes in biological systems in general.
In a related paper in Nature magazine, 2 using quail embryos as a model, French investigators demonstrated that mechanical forces that drive embryogenesis self-organize with contractility locally self-activating, followed by the resulting tension then acting as a long-range inhibitor, in this way shaping the embryo. The process also modulates gene expression which in turn facilitates emergence of specific embryonic territories. Like above-noted paper, this study also confirms the importance of mechanical forces for self-organization of embryos.
REFERENCES
1. Fabreges et al., Science 2024;386(6718):164
2. Caldarelli et al., Nature 2024;633:887-894
OVULATION IN THE MOUSE: A German team of investigators at the Max Plank Institute for Multidisciplinary sciences in Göttingen under the leadership of Prof. Dr. Melinda Schuh for the first time was able to observe and videotape ovulation of a follicle – in this case a mouse follicle.1,2 The authors demonstrated that ovulation proceeds through three distinct phases, namely: (i) follicle expansion, (ii) contraction, and (iii) rupture, which then results in the release of the egg. Follicle expansion is driven by hyaluronic acid secretion and an osmotic gradient-directed fluid influx into the follicle. Then, smooth muscle cells in the outer follicle drive follicle contraction. Follicle rupture begins with stigma formation, followed by the exit of follicular fluid and cumulus cells and the explosive release of the egg.

Image from a video depicting a mouse egg being released from a follicle in real-time.
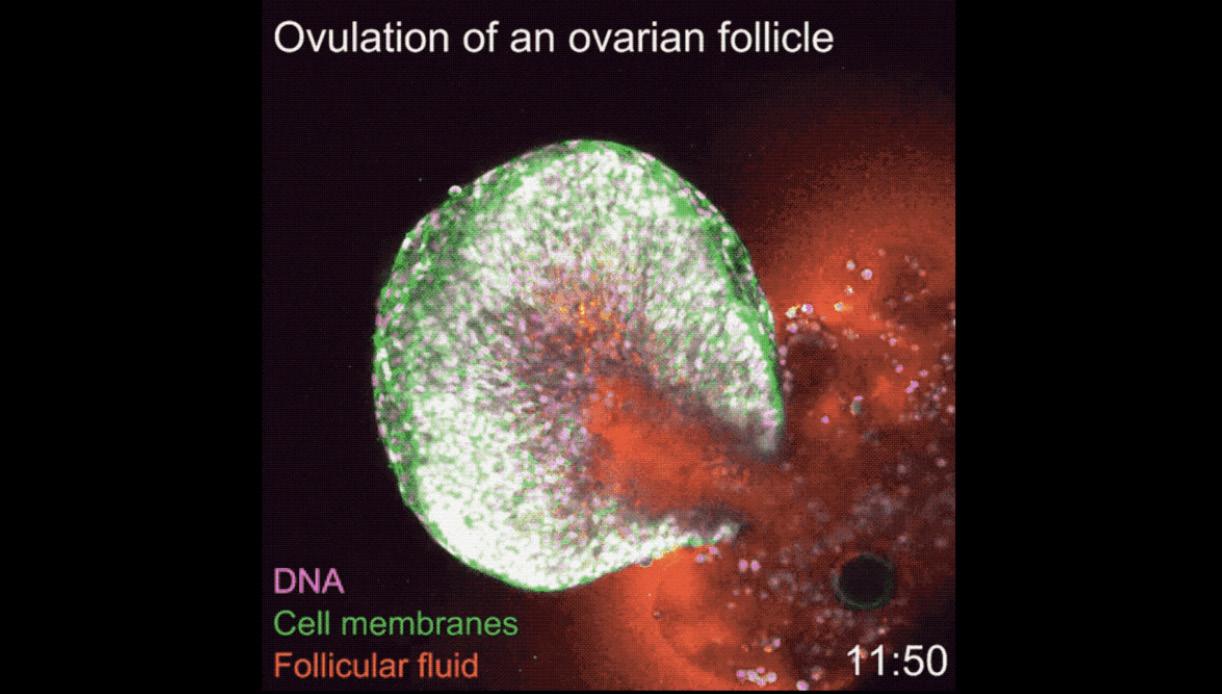
And going from egg to embryo, researchers from the U.K and again Germany recently also reported the high resolution of single cell expression on a gastrulating human embryo. 3 The study investigated a single donated human embryo staged at 16-19 days post-fertilization. The researchers then divided the single embryo into all of its single cells and sequenced the mRNA of 1195 individual cells making up the embryo, creating a very detailed map of gene expression at these crucial stages of embryo development.
This study thus exceeded the 14-day rule of human embryo maintenance for experiments.
REFERENCES
1. Thomas et al., Nat Cell Bio 2024;26:1997-2008
2. Cooke E. Live Science October 29, 2024. https://www.livescience.com/health/fertility-pregnancy-birth/watch-1st-ever-video-of-ovulation-occurring-in-real-time
3. Qiu et al., Nature 2024;626:1084-1093
In a 40 month study of male monkeys, Chinese scientists documented significant anti-aging effects from metformin. Specifically, brain aging regressed by 6 years, and metformin protected brain structures, while enhancing cognitive abilities. The dosage the monkeys received was 20mg/kg. 1 These data add to a significant amount of earlier data that suggests anti-aging benefits from metformin.
REFERENCE
1. Yang et al. Cell 2024;187:6358-6378

Israeli investigators offered in Human Reproduction Update another systematic review and meta-regression analysis. The findings are well summarized in the figure below: As the figure once again demonstrated return rates are extremely low (in this case 11%). Per woman live birth rates are somewhat low (28%) but have to be considered reasonable, especially if they are viewed age-adjusted.

What is the message?
It appears increasingly clear that planned (social) egg-freezing is not a very economic way to extend fertility; but it – of course – is better than nothing! And related, three prominent REs recently published an Insights in Women’s Health article in JAMA that adds to the subject, 2 in which they reemphasize several generally well-known demographic facts:
Women are often unaware that success with fertility treatment declines with age. Misleading reports of children born to high-profile older women (usually the product of oocyte donation cycles) also do not help. Like in most of the developed world, the fertility rate in the US has declined from 70.9 births per 1000 women in 1990 to 56. 1 per 1000 in 2022 At the same time, the age at first birth had risen from 27 years in 1990 to 30 years in 2019 as more women postpone first birth. Not very promising developments!
REFERENCES
1. Hirsch et al., Hum Reprod Update 202; 30(5):558-568
2. Seifer et al., JAMA 2024. Doi:10.1001/jama.2024.18207
Being such a complex and heterogenous condition affecting at least 10% of women during reproductive years, and yet so little is known about endometriosis. One principal reason for the still widespread ignorance about endometriosis is, likely, the fact that – to this day – we cannot be certain who has the disease because we cannot perform laparoscopies on everybody and even that would not solve the problem because so much of endometriosis is microscopic and can be missed even with laparoscopy.
This is why a recent report caught our attention that claimed that the possible solution may be a non-invasive stool test. 1

Yes, it may be again the gut microbiome, as a recent study by U.S. based investigators from several universities suggests: 2 It appears that women with endometriosis have a distinct stool metabolome for non-invasive diagnosis. Their bacteria-derived metabolites are associated with those in inflammatory bowel disease (IBD). Moreover, bacteria-derived 4-hydroxyindole levels are lower in stool from women with endometriosis, and 4-hydroxyindole appears to inhibit the onset and progression of endometriosis.
These are the first findings that suggest a distinct stool metabolite signature in women with endometriosis, which could serve as stool-based non-invasive diagnostics. Furthermore, the gut-microbiota-derived 4-hydroxyindole could be a therapeutic candidate for ameliorating endometriosis.
What is not mentioned in the paper is that the observation of similarities with the microbiome of IBD might also explain why endometriosis – like IBD – demonstrates so much concurrence with autoimmunity.
1. Thomas A. Medscape Medical News . October 15, 2024. https://www.medscape.com/viewarticle/does-road-treating-endometriosis-start-gut-2024a1000itr?form=fpf
2. Talwar et al., Science Direct. 2024. https://doi.org/10.1016/j.medj.2024.09.006
3. Tulandi T, Vercellini P. Reprod Biomed Online 2024;49(3):104292
Many cases of endometriosis are associated with significant pain. Current treatments, however, are limited in their ability to relieve this pain and leave many patients with persistent and often agonizing pain. A recent Commentary article in Cell Reports Medicine very well reviewed this problem highlighting how recent work in the context of chronic pain has altered our understanding and how current treatment options have the potential to improve clinical care. 1
The historic and current understanding of pain mechanisms in that endometriosis-associated pain (EAP) can involve nociceptive, neuropathic, and nociplastic mechanisms. Moreover, there is also increasing understanding of the importance in pelvic pain of viscero-visceral hyperalgesia between pelvic organs, the gut-brain axis, and the hypothalamic-pituitary-adrenal (HPA) axis. Furthermore, we now also understand that there is a bidirectional relationship between pain and psychological distress (such as anxiety and depression), fatigue, and sleep, which further complicates the picture and can contribute to the impact of EAP on quality of life.
It is also increasingly clear how important and common dyspareunia is for women with EAP, a symptom generally particularly poorly considered in preclinical models. Although there are preclinical endometriosis models where sensitivity to vaginal distension can be demonstrated, it remains to be seen whether this can be reversed with therapeutic strategies.
REFERENCE
1. Coxon et al., Cell Reports Med 2024; 5(10): 101769
A recent unsigned editorial in The Lancet attempted to point out the roots of the slow progress in endometriosis research.1 Referring to a recent paper in Nature Genetics, 2 the editorial noted the publication of a recent map of the endometrium across the menstrual cycle, suggesting a new understanding of processes that may be involved in the occurrence of endometriosis. The editorial, however, also notes that “basic science is a long way from reaching the clinic.”
The editorial puts the onus on governments and their funding processes, noting that at least some are “slowly waking up to the substantial health burden of endometriosis.”
In a short Commentary in Reproductive Medicine Online, Togas Tulandi and Paolo Verecellini reemphasized the increasingly accepted hypothesis that endometriosis is really a systemic disease, 3 while investigators from Belgium in a Review article in the same journal reemphasize how frequently unexplained infertility diagnoses really represent a failure to diagnose endometriosis, 4 a point made by the CHR’s Norbert Gleicher back in 1994. 5

REFERENCES
1. Editorial, Lancet 2024;404:1279
2. Marecková, et al. Nat Renet 20224; 56:1925-1937
3. Tulandi T, Vercellini P. Reprod Biomed Online 2024;49(3):104292
4. Van Gestel et al., Reprod Biomed Online 2024;49(3):103848
5. Gleicher N. Immunol Allerg Clin North Am. 1994;14(4):753-758
Yale University’s chair of OB/GYN, Hugh S. Taylor, MD, has been for some time one of the strongest proponents of endometriosis as a systemic disease. He has now published with a colleague an Opinion paper in JCEM suggesting such an association. 1 In it, the two authors noted that studies have demonstrated an association between endometriosis and earlier menopause onset. Recent studies also found a correlation between endometriosis and an increased risk of cardiovascular disease (CVD). The authors suggest that endometriosis, early menopause, and cardiovascular risks may be linked by primary or secondary mechanisms. In large cohort studies, relevant risk and confounding factors, such as oophorectomy, were considered to refine estimates of associations. The authors, however, criticized that none of the studies considered endometriotic cystectomy, a frequent treatment for endometriosis-associated pelvic pain and infertility, as a cofounding factor and endometriotic cystectomies, of course often can harm ovarian reserve and may even lead to early menopause.
REFERENCE
1. Younis JS, Taylor HS. J Clin Endocrinol Metab 2024; 109(100:e1946-e1949
This paper by Dutch investigators in the JCEM tackled at once two major diagnostic problem in women with PCOS: (i) The fact that different assays often produce quite divergent results and, (ii) that – once a patients has a PCOS diagnosis assigned – outcomes are usually no longer differentiated between the different PCOS phenotypes. 1
Importantly, the authors, therefore, developed assay-specific and age-specific AMH curves and – in doing so – correctly also rejected the currently still widely held false concept of universal cut-off values for the diagnosis of PCOS. They, moreover, also integrated by ultrasound obtained polycystic ovarian morphology (PCOM) into their models, another important acknowledgment of reality since, under still widely applied diagnostic criteria for PCOS, AMH levels and PCOM are still mostly excluded from diagnosing PCOS (as further discussed below, an in 2023 published new international PCOS guideline finally recommended the inclusion of PCOM in a PCOS diagnosis in adults only).
Like in all clinical research, nothing is more important than the correct definition of studied patient populations and we, indeed, have made the point repeatedly in these pages that failure to do so in most PCOS studies is, likely, the principal reason why progress in PCOS research over the last 30 to 40 years has been so dismal.

The authors of this paper also correctly pointed out the importance of correct phenotype diagnoses, as non-fertility related differences in long-term patient prognosis, of course, differ significantly between phenotypes, with some being destined to develop metabolic syndrome in a high percentage, while phenotype D under Rotterdam criteria does not demonstrate this risk but carries a significant risk of developing a hyperactive immune system (autoimmunity, inflammation, allergies).

The authors are congratulated on an important paper, as only our Dutch colleagues can produce based on the unique collaboration model they have developed for academic institutions in the country.
And related, in another study of again Dutch, but this time also Australian investigators, the authors investigated AMH as a diagnostic biomarker for PCOS and (as noted above) PCOM through a systematic review and meta-analysis. 2 The study concluded that excessive AMH levels alone are insufficient for a PCOS diagnosis and are nonspecific for PCOM in adolescents. While acknowledging limitations of their study, the authors, however, in our opinion – in contrast to above noted study – reach all the wrong conclusions by claiming that “no international (???) cut-off value can be recommended for a PCOS and/or PCOM diagnosis. Above-noted Dutch study, of course, very clearly demonstrated the opposite.
The authors of this study, however, nevertheless contributed a very valuable message through their paper, even though it may not have been the message they wished to provide – and that message was to demonstrate once more the obscenity of so many published systematic reviews which include garbage-data form poorly performed studies, expecting that aggregated garbage will, suddenly stop stinking. The old IBM dictum, “garbage in, garbage out,” however, still holds. This paper reaffirmed this point and, therefore, was awarded the “Worst Paper Award” for this issue of the VOICE.
1. Barbagallo et al., J Clin Endocrinol Metab 2024;109:2561-2570
2. Van der Ham et al., Fertil Steril 2024;122(4):727738” [“Worst Paper Award”}
And here is another still highly controversial subject regarding PCOS: the significance of androgen levels in PCOS patients. This time an international group of investigators conducted yet another systemic review and meta-analysis in an attempt to assess different androgen levels in reaching a diagnosis of biochemical hyperandrogenism. Unfortunately, this systematic review and meta-analysis – for obviously the same reasons as already pointed out above in the preceding section – also did not do very well and here is why:
More or less the same group of “experts,” in 2023 published briefly noted above “International PCOS Guidelines” which – among several recommendation – suggested the use of total testosterone (TT) and free testosterone (FT) as first-line laboratory tests for assessing biochemical hyper-androgenism. The only thing this paper could basically do, is to confirm this recommendation and spell out some technical advice regarding what testing methods should be used for androgens (which also are anything but new). The final “wider implications” the authors suggested for their paper was that “further studies should focus on establishing optimal normative cut-off values in large, unselected, and ethnically diverse cohorts of women.”
In other words, another completely useless study that offered no new insights and – on top of it – in its recommendations for future investigations got it completely wrong: While establishing optimal normative cut-off values for androgens is, of course, a laudable goal (maybe they should consult with our colleagues from the Netherlands on how to do this), such studies should not be performed in large, unselected, and ethnically diverse cohorts of women but in exactly the opposite, i.e.,- well-defined and highly homogenous patient groups, so that it becomes possible to design treatments targeted to these well-defined women. This article, therefore, just barely missed a “Worst Paper Award” designation.
REFERENCE
1. Demis Bizuneh et al., Hum Reprod Update 2024; dmae028, https://doi.org/10.1093/humupd/dmae028
And in continuation of demonstrating why the progress in PCOS research has been so dismal, here is another paper by another group of PCOS “experts” which in fancy language describes their scientific effort as an “epidemiological study of observational data” alleging to investigate the association between obesity and PCOS. Including – in their literature review – 85,956 patients from 58 published studies, this paper concluded that “the prevalence of PCOS and obesity appear modestly associated, although their data cannot establish causality.” And the comes, of course, the usual gibberish: “This study also emphasizes the need to undertake only high-quality studies in assessing PCOS epidemiology.” 1

Really? And, if that is so, why was this study conducted and published in the first place without looking at PCOS phenotypes, when everybody knows that the D-phenotype under Rotterdam criteria is a “lean” PCOS phenotype, while the other three phenotypes are not? Where is, therefore, the differentiation? It at times is truly astonishing how self-contradicting and absurd motivations, data analyses, and conclusions of some studies can be which, still, make it through peer review in even reputable medical journals.
This paper is an excellent example for that and, therefore, unquestionably deserves a “Worst Paper Award.” Once again, here presented recent PCOS publications demonstrate so well why “expert opinions” holed the lowest evidence level. They, indeed, should hold a negative evidence value because all they usually do – and there, likely, is no better example for this than PCOS because no other condition in reproductive medicine has gone through so many “expert consensus conferences” – is to inform incorrectly!
REFERENCE
1. Amiri et al., J Clin Endocrinol Metab 2024;109:2640-2657
Three colleagues from the University of Chicago and Harvard University recently published an interesting, though to a degree highly speculative, paper in which they argued that when a woman gestates a genetically “unrelated” embryo (i.e., a 100% allogeneic embryo, while most pregnancies, involving the mother’s own eggs, are only semi-allogeneic, - i.e., 50%), the gestating woman’s immune system develops tolerance to the pregnancy less well than in a semi-allogeneic pregnancy. A 100% allogeneic pregnancy will arise if the mother uses third-party donor eggs or if a gestational carrier gestates a pregnancy from an unrelated couple.
Consequently, the authors claim that such allogeneic pregnancies are “riskier” and that patients (i.e., donor egg recipients and gestational carriers) must, therefore, be informed accordingly. While up to this point, their article makes sense (even though they do not offer any quantitation of the alleged risk), their paper then crosses over into Lalaland, when they propose treating 100% allogeneic pregnancies like organ transplants in matching “donor” and “recipient.” That is, of course, total absurdity that can only be offered by clinically ignorant theoreticians who never took care of pregnancies conceived and delivered with donor oocytes and/or carried by gestational carriers.
This paper, however, does address a potentially very interesting model that – if properly investigated – could, likely, significantly contribute to our still very poor understanding of maternal tolerance toward the fetus.
REFERENCE
1. McCoy et al., Early Hum Development 2024;196:106072
In a very interesting but still somewhat preliminary study, investigators from several U.S. organizations determined gene expression profiles of so-called ovarian support cells (OSCs) and – after stripping – cumulus-free oocytes in their bidirectional influences. They reported that rIVM with use of OSCs significantly improved MII formation rates in comparison to just media use with no effects on morphology or spindle assembly. rIVM oocytes also demonstrated a closer transcriptomic maturity signature to routine MII control oocytes. The authors concluded that rIVM with OSCs produces oocytes with improved nuclear maturity and suggested potentially enhanced cytoplasmic maturation in oocytes as well and they suggested furthermore that their results supported the existence of bidirectional crosstalk of cumulus-free oocytes and ovarian support cells. 1
If correct, these kind of studies may, indeed, become useful in improving rIVM. We, however, are skeptical because the CHR’s investigators several years ago compared in a small unpublished study cycle outcomes between stripped and un-

stripped oocytes and found no difference. This study, however, did not have the insights this study offered through gene expression profiles and we, therefore, are looking forward to follow-up studies from this group of authors.
REFERENCE
1. Paulsen et al., J Assist Reprod Genet 2024;41:2021-2036
Swedish investigators now reported an increased risk for congenital heart defects in children conceived through IVF (1.84% vs. 1,15%; AOR 1.36; 95% CI 1.31-1.41). 1 Independent of conception method, the risk was – of course (because we are dealing with 2 or more instead of 1 potentially affected newborns) higher in multiple pregnancies. Risks were similar between ICSI and IVF and fresh and frozen embryo transfers.
So, here we have once again (as in the single embryo transfer circumstance) an obviously statistically biased conclusion which nevertheless led The New York Times to the headline, “Heart Defects Are Likelier From IVF.” 2 And the error lies, of course, in the fact that the birth of two children creates more risk for the pregnancy than the birth of 1 child. A correct analysis, therefore, should have adjusted outcomes for number of birth and should not have the number of pregnancies as reference point. And, despite increasing utilization of elective single embryo transfer, IVF still produces more multiple births than spontaneous conception The conclusion that IVF increases the risk of offspring for congenital abnormalities is, therefore, likely complete nonsense.
REFERENCE
1. Sargisian et al., Europ Heart J. 2024; ehae572, https://doi.org/10.1093/eurheartj/ehae572
2. Rosenbuth T. The New York Times. October 1, 2024. pA19
A national French study once again confirms what the CHR has claimed for almost 20 years: That blastocyst-stage embryo transfer improves cumulative life birth rates is a myth which, finally, must be acknowledged. 1 in addition, as also claimed by the CHR for many years, the study demonstrated that in IVF cycles which produce only small embryo numbers, cleavage-stage transfers, indeed, likely offer improved outcomes in comparison to blastocyst-stage transfers.
One more example where a longstanding IVF practice at the CHR has been proven correct when it contradicted “common wisdom.”
REFERENCE
1. Fauque et al., Reprod Biomed Online 2024;49(6):104384






