






Welcome to the May-June issue of the CHR’s VOICE. As always, we are offering a wide potpourri of original articles and commentaries, as well as opinions about what we consider to be publications of interest for the reproductive endocrinology and infertility (REI) community. But this time, the VOICE contains at the very beginning one additional extremely important component: two articles addressing legal issues of considerable importance for the fertility field. In the first, the CHR’s Norbert Gleicher, MD, informs about the new legal standards for the filing of medical malpractice suits claiming negligence, as created by the American Law Institute.
In the second article – a real first for the VOICE – an outside voice, Allison Freeman, JD, the lead lawyer of the group of plaintiff lawyers who at the end of 2024 had filed a series of lawsuits against U.S. national PGT-A laboratories, offers a short article explaining her own very personal motivations for filing these lawsuits. Especially since the VOICE, of course, does not take sides in any legal matter, that Ms. Freeman chose the VOICE to tell her story is remarkable and informs about the quickly growing impact the VOICE has been able to make in the reproductive medicine community in recent years.
We, therefore, hope that this will be an example for other outside voices who want to share their opinions with our rapidly growing community of readers and want to encourage these voices to submit their communications to our publication by writing us at social@thechr.com.
All other articles in this issue were, as always, selected for the obvious relevance of their content and, often, for their message. We believe that you will find in this issue of the VOICE a good number of really interesting articles because we steadily screen social networks, chatrooms, and other sources for the most interesting topics that appear to attract at any given moment special attention from our community of readers.
The same also applies to our literature reviews, which, as has become practice, are again presented in two separate sections, one addressing issues in general medicine, science, and academia, and a second section that is more directed to covering subjects that more specifically relate to reproduction. In both sections, we are not shameful in presenting the CHR’s opinions which – we are certain – our readers by now are fully aware of – not always follow current mainstream, but attempt to do so objectively and – at least in the more important and at times more controversial points – making certain that our opinions are openly and transparently referenced.
Finally, and on a somewhat lighter note, this issue also offers, among several other subjects, once again a special section on nutrition, obesity as an infertility diagnosis, and – yes – some information on the New York City (NYC) restaurant scene –mainly meant for the CHR’s many out-of-town patients. We are, of course, fully cognizant of how stressful the days in NYC can be when the primary purpose of the visit is an IVF cycle, and aside from some sightseeing and a wonderful Broadway show, there is nothing more stress-reducing than a good meal in a nice restaurant.
We still love eggs

By Norbert Gleicher, MD, Medical Director and Chief Scientist at The Center for Human Reproduction in New York City.
He can be contacted through the VOICE or directly at either ngleicher@thechr.com or ngleicher@rockefeller.edu
BRIEFING: What in medicine represents malpractice has been defined by the so-called “standard of care” in the community. The American Law Institute (ALI) recently, however, suggested an updated standard that relied more on “best available evidence” on which treatment should be based. Though for several weeks, basically ignored by the media, this issue suddenly, however, caught fire in the media after an article appeared on the subject in JAMA . Here, Norbert Gleicher, MD, the author of this article, while welcoming the proposed changes, questions whether they really will produce realistic changes in the nation’s medical malpractice situation, as some medical specialties are considered at crisis levels.
Any change in how the legal system addresses medical malpractice is, of course, great news in all of medicine. Yet even though the American Law Institute (ALI) already in 2024 offered a new legal standard for the definition of what represents medical malpractice, medical and non-medical main media started buzzing about this development only now because The New England Journal of Medicine published.
The ALI is an organization akin to a professional medical society, made up of judges, academicians in law, and practicing attorneys, which, again akin to medical practice guidelines – drafts, approves, and publishes restatements of the law, principles of the law, model acts, and other proposals for law reform.1
A Special Communication article in the JAMA just summarized this effort, which, one can hope, will overall have a positive impact on the medical field.2 This, with considerable marketing fanfare, announced article by several lawyers (some also hold MD degrees), offers an even for laypeople easily

understandable explanation of the ALI’s restatement of the law regarding this issue.
As Joyce Frieden, Washington Editor of MedPage Today noted in an article on February 26, 2025, addressing the JAMA article in citing one of the authors, “the new standard of (medical) care presents a shift away from strict reliance on medical custom and invites courts to incorporate evidence-based medicine in malpractice law.”3 As the authors of the original article put it, “the updated standard form the ALI shifts away from traditional reliance on customary practice toward a more patient-centered concept of reasonable medical care.”
As the article, however, also notes, this change does not make prevailing medical practice completely disappear from consideration when defining a level of reasonable medical care based on skill and knowledge regarded as competent among similar medical clinicians under comparable circumstances. The new standard, however, also acknowledges that juries, under

some circumstances, could override contemporary practices if the jury perceived those to fall short of contemporary practice.
Frieden’s article quoted the JAMA article’s lead author as saying that, under this new legal standard, “physicians should not fear liability, as long as they are practicing good medicine.”
While this, of course, would be an ideal premise for any malpractice reform, we here at The Reproductive Times are skeptical because this is not how we necessarily understand the JAMA article. It, of course, makes sense to replace the concept of standard of care because, simply for practical purposes, standard of care always significantly lags behind best available evidence. The transition from bench (research) to bedside (clinical application), however, routinely takes at least 10-15 years but can be highly variable.4 That fact alone already disqualifies the until-now ruling “standard of care” to be maintained.
But as the JAMA article correctly noted, while switching the main criterion from a standard of community care to a desired practice standard reflecting best available evidence, of course, creates significant new legal uncertainty.
We, for example, would argue that – strictly applied – physicians in academic institutions would have to practice at a different level of expectation than physicians in a community hospital because, as noted above, academic physicians will, of course, learn of new developments often years ahead of their community brethren.
And then there is the next important question: what is the best standard of care? Is advising every IVF patient to have her embryos tested for aneuploidy through preimplantation genetic testing (PGT-A)?
Some plaintiffs’ lawyers very obviously don’t believe that, as recently filed class action suits against several PGT-A laboratories suggest, and with more such suits against at least some IVF clinics expected. Or is advising every woman above age 42 that third-party egg donation is her only chance of pregnancy, based on the best available evidence. We certainly don’t believe so, but many colleagues do!
So, what does this new legal standard announced by the ALI then really mean? Probably less than suggested by the attention this announcement is suddenly receiving.
The authors of the JAMA article explain it this way: The new proposed standard represents a shift away from strict reliance on medical custom and a suggestion for courts to start incorporating evidence-based medicine into malpractice law. It is also important to note that malpractice law is a state-controlled issue and, as the paper correctly notes, states may adopt the ALI recommendations at different times and to varying degrees.
1. https://www.ali.org/
2. Aaron et al. JAMA 2025; 333(13);1161-1165
3. Frieden J. Medpage Screenshot 2025-05-29 at 3.52.13 PM Today. February 26, 2025. https://www.medpagetoday.com/ practicemanagement/medicolegal/114397
4. DocWire News Editors. July 14, 2023. https://www. docwirenews.com/post/bench-to-bedside-translating-sciencefrom-the-lab-to-the-clinic

By Allison Freeman, JD, Managing Partner of Constable Law and the IVF Advocate. She can be contacted through the editorial office of the VOICE.
BRIEFING: When, in the last quarter of 2024, several class action consumer lawsuits were filed shortly before the Annual Scientific Meeting of the ASRM (in that year in Denver, CO), “class action” became the buzzword of the conference. Now, almost a year later, things have calmed down, but the work on both sides of the case is, of course, continuing, and the interest in these cases in the IVF community has remained high. When Allison Freeman, the lead attorney in all of these cases, therefore, offered the VOICE an article explaining her motivations for filing these cases, we, of course, could not resist. And here is the piece unedited, as she submitted it.
Our litigation team made up of Constable Law, Berger Montague and Justice Law Collaborative has filed seven class action consumer protection lawsuits based upon the false and misleading claims made to sell PGT-A testing to consumers.
The seven lawsuits are as follows:
Weinberg, et.al. v. CooperGenomics, Inc. and CooperSurgical, Inc., which was filed September 27, 2024 in the District of New Jersey
Donamaria v. Reproductive Genetic Innovations, Inc., which was filed October 4, 2024 in the Northern District of Illinois
Cruz, et.al. v. Progenesis, Inc., which was filed October 7, 2024 in the Southern District of California
Petersen, et.al. v. Natera, Inc., which was filed October 8, 2024 in the Northern District of California

Klosowski, et.al. v. FPG Labs, LLC d/b/a Ovation Fertility, U.S.
Genetic Lab, LLC d/b/a Ovation Genetics, and US Fertility, LLC, which was filed October 31, 2024 in the District of Delaware
M.M., et.al. v. Igenomix USA, Inc., Vitrolife Group, Vitrolife AB, and Vitrolife, Inc., which was filed March 4, 2025 in the Southern District of Florida
Tyman, et.al. v. CCRM Parent Holdings, Inc., CCRM Practice, LLC, and CCRM Management Company Holdings, LP, which was filed May 7, 2025 in the District of Colorado
The lawsuits allege consumer fraud, breach of warranty, and related causes of action arising out of defendants’ advertising and sale of PGT-A testing. Specifically, the lawsuits allege that PGT-A is scientifically unproven, inaccurate, and lacks proper validation, yet has been aggressively marketed using a host of false and misleading claims. These claims include that PGT-A testing is 97 to 99% accurate, increases the success of IVF, decreases the chance of miscarriage, leads to a higher chance of pregnancy, increases live
birth rate, increases the chance of implantation and pregnancy, and reduces the time and cost of pregnancy. The lawsuit against CCRM also includes causes of action related to CCRM’s interference with patients’ embryos.
These lawsuits were not filed quickly. In fact, I began investigating and researching PGT-A more than two years before the first suit was ever filed. It all started with my own experience. When I first heard about a test that claimed to increase my chances of having a healthy baby through IVF, it sounded too good to be true, so I declined. A couple of years later, when I began IVF again, the push for PGT-A had only intensified. I was bombarded with cartoon videos, promotional webinars, and follow-up phone calls, all promising results that, once again, felt too good to believe so I passed a second time.
Still, I kept questioning my decision, especially after a representative from one testing company told me that not buying the test at my age was “insane.” At the same time, I started hearing

similar stories from friends and family. People were telling me they’d lost embryos because of PGT-A results and were not allowed to decide what to do with their embryos. That was the turning point. I couldn’t ignore the growing number of voices or the unsettling questions I had about how a single test had come to hold so much power over people’s fertility journeys.
I started reading and investigating everything I could relate to PGT-A, including science journals, clinical studies, articles, and even message board posts from others in the fertility community. I would fall asleep only to wake up in the middle of the night with another question I wanted to look into, which would lead to more reading and investigating at all hours of the night. Eventually, I had gathered enough information to believe there was a serious issue with the way PGT-A was being marketed and sold to IVF patients across the country. However, I wanted to be sure.
At that point, I decided to bring my concerns to my law partner. Since he had no personal experience with IVF or fertility treatment, I knew he could offer a fresh, unbiased perspective that wasn’t clouded by the emotional weight I carried. I shared my notes, my research, and my questions with him. After digging into the material, he agreed that something didn’t add up, but he also wanted to be certain. So together, we began reaching out to experts.
We spoke with reproductive endocrinologists, genetic counselors, molecular biologists,
embryologists, bioethicists and anyone willing to talk to us about PGT-A. Again and again, we heard the same message that PGT-A is being sold to consumers with misleading claims and without the solid scientific backing those claims demand. It became clear that the test was being marketed in ways that were false, misleading and unsupported by science, but the question then became:
Although I’m a lawyer, filing lawsuits wasn’t my first instinct. I started by reaching out to those in positions of oversight and influence. I wrote to my state attorney, the FDA, and the FTC. I also contacted a few state senators and representatives who I believed might take interest in the issue. Most never responded and the few who did made it clear that they wouldn’t be getting involved.
That’s when we realized litigation might be our only path forward. But tackling an issue of this scale with scientific complexity that affects countless individuals meant we couldn’t go it alone. We joined forces with dedicated co-counsel firms who share our passion and dedication. Together, we’re not just suing to hold the defendants liable but also to hopefully create real change.
Since filing, we have received four motions to dismiss and one motion for judgment on the pleadings which are legal attempts by the testing labs to have the cases thrown out before any evidence is reviewed. Their position is that the lawsuits lack a legal basis to move
forward. Ultimately, that decision rests with the court.
Responses are not yet due in the two most recent cases, which were filed against Igenomix/Vitrolife and CCRM. However, Vitrolife has acknowledged the filing publicly, stating that it is aware of the lawsuit and is reviewing the matter with its legal counsel.
Every day, we hear from IVF patients whose voices carry both pain and hope. They thank us for filing these lawsuits and tell us they’re searching for something simple but powerful: truth, transparency, and change. That is what drives us forward.
The fertility journey is one of the most personal, emotional, and vulnerable paths someone can walk. These are people already facing enormous hurdles—physically, emotionally, and financially—just to try and grow their families. They deserve better. We see them. We hear them. And we are fighting for them—not just when it comes to PGT-A testing, but in the face of anything that misleads, harms, or obscures the truth from those seeking to build a family.
Of course, impartial in all of these lawsuits, the VOICE welcomes opposing opinions to the article presented here.
By Sònia Gayete Lafuente, MD, PhD,
who is a Foundation for Reproductive Medicine Research Fellow at the Center for Human Reproduction (CHR) in NYC. She can be reached through the editorial office of the VOICE or directly at sgayete@thechr.com.

BRIEFING: Offering numerous physiologic and emotional benefits for babies as well as mothers, breastfeeding is widely acknowledged as the optimal feeding method for newly born infants. For over a decade the World Health Organization (WHO), the American Academy of Pediatrics (AAP), the American College of Obstetricians and Gynecologists (ACOG), and many other professional medical societies have globally endorsed exclusive breastfeeding for at least 4-6 months, with gradual introduction of complementary foods thereafter. Meanwhile, research continues to highlight health advantages of breastfeeding, including adaptative nutrition to the baby’s needs, improved cognitive development, enhanced immune function, stronger bonding, and emotional health regulation for both mother and child. Interestingly, this also extends to mothers who did not experience pregnancy, such as women who become moms by using a gestational carrier, or by shared motherhood with their pregnant same-sex partners. Surprisingly often not known to non-carrying mothers, medical lactation induction can enable them to, still, breastfeed their babies, a point this article attempts to raise awareness about.
*This article was originally published
Nutritional superiority - Breast milk is the gold standard in infant nutrition because it provides a balanced combination of proteins, fats, carbohydrates, and antibodies. It meets the baby's needs in a dynamic way that no formula can replicate. For example, mothers of babies that demand to be fed more often and, therefore, usually in smaller quantities, will produce less caloric milk with more simple sugars and less fats, while mothers of babies that demand to be fed less often and in larger quantities will produce more calorie-concentrated fatty milk.
Immunity boost - Antibodies in breast milk, especially of IgA isotype, help protect the baby from infections, particularly during the early months after delivery, when the baby’s immune system is still developing with initial environmental exposures. Moreover, breast milk helps establish a healthy gut microbiota in the offspring, which plays a crucial role in the development of the immune system and of normal digestion.
Bonding & attachment - Breastfeeding fosters a unique bond between the mother and child. The physical closeness during nursing promotes attachment, emotional security, and a sense of trust, which are foundational for the baby’s emotional development.
Long-term reduced risks of chronic conditionsLong-term research indicates that breastfed babies are at a lower risk of developing obesity, diabetes, asthma, and certain childhood cancers. Some studies also show better cognitive development and higher IQ scores in breastfed children.
Hormonal benefits - Breastfeeding releases the hormone oxytocin from the pituitary to aid in the
so-called milk ejection reflex (i.e., lactation), but also has the function of helping the uterus to contract postpartum and preventing postpartum bleeding. This effect, then over subsequent weeks, allows the uterus to return to its pre-pregnancy size. Interestingly, oxytocin, also called the “love hormone,” in addition to promoting the fetal-maternal bonding process, thereby enhancing the unique emotional connection between mother and offspring.
Enhanced emotional & mental health - Breastfeeding also fosters an added sense of closeness with the baby, which, in turn, has been reported to reduce the risk of maternal postpartum depression. Additionally, the act of breastfeeding promotes relaxation and emotional well-being through hormonal responses that reduce stress and foster emotional stability during the postpartum period, and can create a sense of accomplishment and emotional satisfaction. Nourishing a child simply provides feelings of empowerment and fulfillment.
Long-term weight loss, metabolic health, & even reduced risks of certain cancers - Nursing burns calories, helping mothers more quickly return to their pre-pregnancy weights. Breastfeeding has also been linked to a lower subsequent risk of obesity and type 2 diabetes in mothers and reduces a mother's risk of developing breast and ovarian cancers. The longer a woman breastfeeds, the greater the reduction in those risks.


For those mothers who did not experience pregnancy but still wish to breastfeed, lactation induction is a very viable option. This option applies to mothers using gestational carriers and female partners of pregnant women who wish to share in the breastfeeding of their offspring.
The process combines hormone therapy, intensive breast pumping, and at times even prolactin treatments to stimulate milk production in the nonpregnant woman. The goal is to mimic the hormonal environments of a pregnant woman in the third trimester of pregnancy and post-partum, which encourages the breasts to produce milk. And this treatment should be prescribed under the supervision of a healthcare provider. The table below offers the details.
After the baby’s delivery, start breastfeeding immediately and continue pumping. Also consider the possibility that the amount of lactation may not be sufficient, in which case supplementation with formula or pasteurized donor milk may be needed. Here is more detail:
Breastfeeding - Breastfeeding should be initiated immediately after birth, even if maximal milk supply has not been established yet. Breastfeeding will further stimulate the breasts to produce milk.
Continued pumping – Pumping should even continue after feedings to further stimulate milk supply. The more often breasts are stimulated to produce milk, whether through direct breastfeeding or pumping, the better the chances of establishing a good milk supply.
Supplementation – Especially during initial weeks, there may be a need to supplement with formula or pasteurized donor milk until a more solid milk supply has been established.
By following a lactation induction protocol as outlined here and ensuring ongoing support and monitoring from a qualified healthcare provider, almost all nonpregnant women can successfully induce lactation and begin breastfeeding their babies immediately after birth. For women who did not themselves carry the pregnancy, the experience of breastfeeding their child may be even more important than for women who had already established a “crosstalk” with their child during pregnancy. It is, however, a unique and rewarding experience for every woman and her child, which plays an essential role in the unique relationship between mother and child, truly a lifelong bond beyond the womb.
Meek JY, Noble L; Section on Breastfeeding. Policy Statement: Breastfeeding and the Use of Human Milk. Pediatrics. 2022;150(1):e2022057988.
Prentice AM. Breastfeeding in the Modern World. Ann Nutr Metab. 2022;78 Suppl 2:29-38.
Del Ciampo LA, Del Ciampo IRL. Breastfeeding and the Benefits of Lactation for Women's Health. Rev Bras Ginecol Obstet. 2018;40(6):354-359.
Masi AC, Stewart CJ. Role of breastfeeding in disease prevention. Microb Biotechnol. 2024;17(7):e14520.
McGowan C, Bland R. The Benefits of Breastfeeding on Child Intelligence, Behavior, and Executive Function: A Review of Recent Evidence. Breastfeed Med. 2023;18(3):172-187.


By Norbert Gleicher, MD, Medical Director and Chief Scientist at The Center for Human Reproduction in New York City. He can be contacted through The Reproductive Times or directly at either ngleicher@thechr.com or ngleicher@rockefeller.edu
BRIEFING: It is now exactly 20 years since my colleague David Barad, MD, MS, and I published our first paper reporting on the potential fertility benefits of supplementing selected patients with DHEA (dehydroepiandrosterone). This and several quickly following papers on the same subject ended up changing infertility practice in many – maybe most – fertility clinics in the world (Reference 1). It was a paper reporting on a CHR patient in her early 40s who, completely unknown to us at the CHR, had started self-supplementing with DHEA because a first IVF cycle had yielded only one egg and one embryo. She had been advised that, assuming a similar second cycle, further repeat IVF cycles with the use of her own eggs would not make much sense anymore. She then, however, made us scratch our heads, - wondering what was going on - in subsequent back-to-back cycles, as the patient from cycle to cycle produced more and more oocytes and embryos. Only after her 6th consecutive cycle, did she finally clarify what was going on, when disclosing that she - completely on her own – had started supplementing with DHEA. It was this disclosure that then initiated years of DHEA-related research at the CHR, resulting in a large number of published studies in several leading peer-reviewed medical journals and – to this day – the only U.S. patents approved for claims of treatment benefits for androgens (including DHEA) supplementation in selected infertile women. On the occasion of this 20th anniversary, this article presents an update on the subject of androgen supplementation in selected infertile women, with special emphasis on DHEA supplementation.
BEFORE CONTINUING TO READ, PLEASE NOTE THE FOLLOWING
The author of this article is a co-owner of several U.S. user patents which claim clinical benefits in hypo-androgenic female infertile women from supplementation with androgens. He and the CHR receive royalty payments for these patents fromcompanies producing androgen supplements, including a company called Fertility Nutraceuticals, LLC, of which he is also a shareholder.
Introduction
There are few issues in infertility practice as controversial as androgen supplementation. Though this article is meant to offer a general overview of androgen supplementation in selected female infertility patients, it is really primarily geared at trying to explain why androgen supplementation has remained so controversial and why, as of this time point, it really no longer should be considered at all.
I am always surprised to still regularly confirm in my discussions with patients and colleagues that a majority in both groups (yes, physician colleagues as well!) –whether proponents or opponents of androgen supplementation – usually lack even minimal knowledge of why androgen supplementation is indicated in
selected infertile women. Let us, therefore, discuss this issue first. For us at the Center for Human Reproduction (CHR) in NYC and for most of the infertility field, androgen supplementation arose as a serious research issue only around 2004. Though several small studies had been before published suggesting that various drugs may in some women increase oocyte yields in IVF cycles– among them only one study reporting on use of the mild androgen, dehydroepiandrosterone, DHEA),
the real study of androgens in female infertility only started in ca, 2004 at the CHR in NYC with because of a single patient who wanted to cryopreserve her eggs: This then 42-year old female patient with extremely low functional ovarian reserve (LFOR) – unknown to the center’s physicians – initiated self-supplementation with DHEA. She decided on supplementing with this hormone after researching the literature for compounds that might improve the dismal one oocyte yield she had produced in her first IVF cycle at the CHR.
Other drugs she identified in her literature search for their alleged ability to improve oocyte yields required prescriptions. DHEA, under an obscure U.S. law considered a food supplement (even though in many other countries, because of abuse by athletes and body builders, DHEA is considered a controlled substance), she could purchase over the counter without prescription and without having to tell anybody at the CHR.
Going back-to-back month after month in consecutive IVF cycles, she demonstrated steadily improving oocyte yields and increasing numbers of cryopreservable embryos, until her gonadotropin dosage had even to be reduced because she had developed a typical ovarian PCOS phenotype, which – paradoxically - even put her at risk for ovarian hyperstimulation. After her sixth cycle – with everybody at the CHR scratching their head in search of an explanation – she, smilingrevealed her secret: she had secretly started to self-supplement with 75mg of dehydroepiandrosterone (DHEA) daily, because I had
advised her that we would not start additional IVF cycles if her oocyte yield remained that small.1
The year was 2004, and, like other IVF clinics, the CHR had absolutely no idea why and how DHEA might improve oocyte yields in older women with low FOR (LFOR). The observations in these index patients were, indeed, so surprising and yet so obvious that our hands-on observations of a single female patient in her 40s gave us confidence enough regarding the potential beneficial effects of DHEA on older ovaries to intensely start investigating DHEA in women with LFOR.
We quickly discovered that available DHEA products were extremely uneven in potency and, often, did not even contain the alleged dose of DHEA. Serious studies, therefore, were impossible with these products. A DHEA product of consistent quality, including consistent absorption (dependent on particle size during micronization) and overall production quality, consequently became an essential prerequisite. We, therefore, contracted a pharmacy in NYC to compound such a special DHEA product under highly specific production criteria. This DHEA was then, without exception, used by the CHR’s patients over the initial years of the study of DHEA supplementation at the CHR. On last count, the CHR’s investigators have since published 36 peerreviewed publications on DHEA supplementation, a large majority in efforts to improve infertility treatment outcomes and in a small minority in efforts to improve hypo-androgenic loss of libido.
Though in initial studies, we very quickly confirmed the beneficial effects of DHEA supplementation on several outcome parameters in infertile women with low androgen levels, we made only slow progress in our understanding of how these outcome improvements came about. But that changed very quickly when Aritro Sen, PhD, and Stephen R. Hammes, MD in 2010 reported a mouse study in which they had knocked out androgen receptors on granulosa cells and oocytes and noticed that the knockouts on granulosa cells severely interrupted follicle maturation, while receptor knock out on oocytes showed hardly any effects.2
Not only did this paper instantly explain our observation with DHEA, but this paper also initiated years of a highly effective collaboration between Sen and Hammes and the CHR that allowed us to further our understanding of androgen effects on ovaries by going back and forth between mouse and human studies in explaining things. Concomitantly, as – not the least because of the CHR’s publications - the popularity of DHEA supplementation in infertility continued to increase (an internet survey after several years suggested that ca. half of the world’s IVF clinics had started to supplement patients with androgens), clinical research also expanded worldwide.
Not all studies, however, confirmed the effectiveness of DHEA that the CHR had reported, and study results in humans became quite contradictory. Animal studies, in contrast, however, uniformly confirmed the initial mouse data of Sen and Hames, which, of course,
fully corresponded with the clinical data the CHR’s investigators had reported. And these animal data were not only restricted to mouse models but also included larger animal models, including sheep and monkey models. All uniformly confirmed that good/normal testosterone levels were essential during small follicle-growing stages (i.e., between secondary and small antral follicles) in synergistically with FSH, supporting follicle growth and maturation. Too low androgens reduced egg numbers as well as egg quality. Proper supplementation of abnormally low androgens leads to normal testosterone levels, then, however, reconstitutes more and betterquality oocyte yields, leading to more pregnancies and fewer miscarriages.
And these small as well as large animal data, in contrast to clinical human data, have to this day remained undisputed.
Then why is androgen supplementation in female infertility still so controversial?
That is exactly the main question this communication is attempting to answer. Considering the overwhelming and consistent animal experience explaining in detail the benefits of androgen supplementation in hypoandrogenic females, we, indeed, have great difficulties in finding a single valid explanation because –in our opinion (which, of course, possibly may be biased considering above posted Conflict Statement) the resistance to selective androgen supplementation to this day found
in many peer-reviewed publications does not make logical sense. This is especially the case if one considers that the same skeptics regarding androgen supplementation often proclaim full support for a plethora of equally (or even more) controversial treatments, but do not have any/or comparable animal data in support. Moreover, many of these treatments (often called “addons” to IVF; think, for example, PGT-A, etc.) add significant costs to fertility treatments, while the costs of androgen supplementation with DHEA are, in comparison, only a pittance.
One principal argument one always hears from skeptics of androgen supplementation is that there are no properly conducted prospectively randomized clinical trials in the literature that would support such androgen supplementation, and this is, of course, correct. But most of routine medical practice - and not only in infertility – is lacking support from such trials. And many of these practices exist with much less or, at times, no animal data in support at all. Moreover, even a majority of randomized clinical trials to guide clinical practice in various medical areas have features that disqualify them from meeting their purpose.3
Infertility practice, in addition, has an excellent excuse for not producing enough prospectively randomized studies in comparison to other medical practice areas as - understandably - infertile women are often not willing to be randomized to placebo because, especially when the problem is LFOR, the potential loss in time may harm their overall pregnancy chances. We know this concern
from personal experience because the CHR in the early years of DHEA research secured generous funding for a prospectively randomized clinical trial, but had to abandon it because we were unable to recruit sufficient numbers of willing patients. We then, after representation that they would have no problems with patient recruitment, indeed, transferred the funding to a European group of IVF clinics, only to find out that they, too, had misread their recruitment chances.
All of this, of course, did not prevent investigators from conducting androgen supplementation studies using either small prospectively randomized studies with inadequate statistical power or study designs of lower evidence levels. Not even one of them, to the best of our knowledge, moreover ever noted specifics regarding the DHEA they used in their studies. That those studies often produced contradictory results, therefore, cannot surprise. But there were major additional problems with many of these studies: Likely the most important one was that, once again, to the best of our knowledge, not even a single one of those studies ever evaluated androgen levels in infertile women before starting them on DHEA supplementation. Consequently, when colleagues reported in the literature on androgen supplementation with DHEA or testosterone, they either did so in randomized or supplemented patients without knowing whether they were hypo-androgenic or not. And this, of course, introduces an absolutely fatal error into any clinical study because, as
investigating whether treating a headache with aspirin in individuals who don’t have a headache makes no sense, so, of course, supplementing an infertile woman who has normal androgen levels does not make sense. As any prospectively randomized headache study of aspirin, of course, would have to be restricted to patients with headache, every DHEA supplementation study in infertile women, of course, would have to be restricted to hypo-androgenic infertile women.
Of course, supplementing an infertile woman who has normal androgen levels does not make sense. As any prospectively randomized headache study of aspirin, of course, would have to be restricted to patients with headache, every DHEA supplementation study in infertile women, of course, would have to be restricted to hypo-androgenic infertile women.
In other words, the contradictory findings of DHEA and/or direct testosterone supplementation in female infertility, to a large degree, can be traced to incorrect study designs. Studies that showed positive DHEA/testosterone effects in concordance with the CHR’s results and animal experiments, likely, had simply more hypo-androgenic participants than studies that showed no effects from DHEA/testosterone supplementation.
Related, the same error in study design – also explains similarly contradictory findings reported in the literature for pretreatment of infertile women with growth hormone (GH). Since GH works
through insulin growth factor-1 (IGF-1), GH supplementation makes only sense if IGF-1 levels are abnormally low.
Most fertility clinics, however, do not test IGF-1 levels in their patients, and – once again – we are unfamiliar with even a single GH study in the medical literature in infertile females that preselected their study participants based on predetermination of IGF-1 levels. And low IGF-1 levels are even rarer than low androgen levels. Even in a very aged female infertile population like the CHR is serving, the percentage of low IGF-1 is less than 5%.
But this is not yet the end of the story; why has androgen supplementation data in the literature been so contradictory? Another point of crucial misunderstanding has been in almost all studies, the timing of DHEA (and GH) supplementation. We previously noted that androgen effects on follicles are especially important during the so-called small growing follicle stages between secondary follicle and small antral follicle stages, and that, after that stage, follicles still need at least 6-8 weeks to reach gonadotropin sensitivity, when they become reactive to gonadotropin treatments.
In practical terms, this means that DHEA/testosterone supplementation must start at least 6-8 weeks before the IVF cycle starts. If treatments start later, later generations of follicles will receive most of the supplementation benefits, but not the planned IVF cycle. And, once again, a
review of the DHEA/testosterone supplementation literature clearly demonstrates that in a majority of published studies, androgen supplementation before IVF cycle start was much shorter than required. Indeed, in many studies, androgen supplementation was started only with the IVF cycle start. One, therefore, once again, cannot be surprised that androgen supplementation in so many studies has not shown clinical effectiveness.
DHEA or testosterone supplementation?
Patients often ask why we prefer DHEA supplementation over direct testosterone administration. The principal reason is the difference in treatment risk: Testosterone is usually given transdermal by gel. This must be done very carefully because everybody who comes in touch with the gel will instantly absorb the hormone. This means that if mom has testosterone gel on her arm, she should not come close to any of her children. Moreover, testosterone floods the whole body, producing identical testosterone levels in every organ. It, therefore, is very easy to overdose androgen levels with direct testosterone supplementation, and too high androgens can be worse for fertility treatments than too low androgens.
Oral DHEA, in contrast, as the precursor of testosterone (i.e., our bodies make testosterone from DHEA), for several reasons, can hardly ever overdose a patient. A first reason is that DHEA has –what is called – very low “bindingaffinity” to the androgen receptor on granulosa cells (and elsewhere).
This means that, even if DHEA levels are too high, it does not have many androgenic effects. Moreover, since most organs produce their testosterone locally and often have different “best” testosterone levels, each organ, including the ovaries, will take out of circulation only as much circulating DHEA as this organ needs to reach its desired testosterone level. For both reasons, overdosing and complications from too much DHEA are, therefore, practically almost impossible.
Side effects and other potential dangers of DHEA and/or testosterone, including cancer risk
We already noted in the preceding paragraph that too high testosterone levels may be worse for fertility than too low levels. Once androgen supplementation is initiated, it is, therefore, important to continue monitoring androgen levels at regular intervals. At the CHR, this means ca. 30 days after initiation - and then usually roughly every three months – and an androgen panel including sex hormone binding globulin (SHBG) is obtained. The typical androgen screen involves DHEA, DHEA-S, free testosterone, total testosterone, and SHBG, which usually go the opposite way from testosterone: if testosterone is low, SHBG will be elevated. We, therefore, use SHBG to determine the effectiveness of androgen supplementation. A concern often expressed by patients and colleagues is increased cancer risk, especially breast cancer risk, and to a lesser degree, ovarian cancer risk. And while understandable, such concern is really not warranted, and here
is why: It stems primarily from the fact that a small fraction of a woman’s testosterone is converted to estrogen, and estrogen can make breast cancers with estrogen receptors grow quicker. Whether estrogen also induces fresh breast cancers is more controversial.
But even assuming it does (which by no means is certain), that – in itself – would not be a reason to withhold androgen supplementation either via DHEA or testosterone, and here is, again, why: The rise in estrogen caused by conversion from testosterone is much smaller than the rise of estrogen after a woman conceives. In other words, the estrogen exposure from being pregnant is substantially bigger and usually longer (over nine months of pregnancy) than it would be from DHEA and/or testosterone supplementation during infertility treatments.
In practical terms, this, therefore, means that if a woman is cleared for pregnancy, this automatically also means she is cleared for androgen supplementation.
This issue arises, of course, especially in women with a history of prior breast cancer or with a history of genetic predisposition toward breast cancers, as is, for example, the case in women who are carriers of BRCA1/2 gene mutations or other cancer genes which increase breast cancer risk. And the rule then is very simple: if a patient under cancer surveillance by her oncologist has been cleared for pregnancy, she can also be pretreated with androgens, whether DHEA or testosterone, directly. Other side effects are usually even
milder with DHEA than with testosterone. The reason is, once more, the fact that DHEA itself is a very “mild” androgen in contrast to testosterone. Consequently, other side effects of DHEA, like oily skin, acne, rarely mild hirsutism (usual primarily facial hair growth), and, rarely, mild hair loss, are usually immediately reversible when treatments are stopped or even if medication dosages are just reduced.
Before we address this question, we once again want to point out our above-noted Conflict Statement. We above also already noted that, because of uneven and often poorquality DHEA products on the market, we, over several years, conducted initial DHEA studies at the CHR exclusively using DHEA compounded for CHR patients by a pharmacy in NYC according to our specification with special attention paid to particle size which is responsible for absorption rates. They, of course, must be stable in order to provide stable dosing to patients.
This arrangement over several years worked well, but the medication costs for the patient were obviously quite high. The CHR by that time had earned several U.S. user patents for the use of androgens (DHEA as well as testosterone) in selected infertile women. We, therefore, contacted most major pharma companies active in the infertility field and tried to interest them in developing a DHEA pharma product (in contrast to an over-the-counter product)
with quality parameters identical to the compounded product we had used in our initial DHEA studies. Unfortunately, none of the companies was interested because they – likely correctly – considered the market as too small for such an effort, which would – at very high development costs - have required formal FDA approval for such a DHEA product.
The CHR, therefore, decided to start production of a DHEA product as a food supplement for its patients on its own (which, of course, required much less front-up investment), with initially the only purpose, of being able to offer the CHR’s patients a DHEA product with identical characteristics to the originally compounded DHEA, though at lower and more affordable costs.
This is how Fertinatal® was born, which over the years has won a worldwide following [produced by Ovaterra, a Fertility Nutraceuticals LLC, subsidiary, New York, N.Y.]. Concomitantly, we started licensing other companies under our patents to sell their DHEA for fertility purposes, though only if we were convinced of the quality of their product and of their quality assurance process.
While the CHR, out of principle, does not make specific product recommendations for any medication or supplement, including Fertinatal® and/or any other product of Ovaterra, a large majority of DHEA products on the market, as will be obvious, do not claim any effects from their products on female fertility. Only those licensed by Fertility Nutraceuticals LLC have the ability to make such representations. Licensure of products to point
toward female fertility effects, therefore, has its value.
Hypo-androgenism is not only associated with lowered female fertility and poorer fertility treatment outcomes, but also with lower general energy levels in women, decreased sex drive, libido, and often especially perimenopausal and menopausal, with dry vaginas. One company several years ago received a patent for local vaginal DHEA treatments and the CHR’s investigators more recently reported that oral DHEA treatment in infertile women with low androgen levels also improved their sexual function (patent pending).4
2005;84(3): 756
2. Sen A, Hammes SR. Mol Endocrinol 2010;24(7):1339-1403
3. Hutchinson et al., eLife 2022;11:e79491
4. Kushnir et al. Endocrine 2018;63:632-638

Cheers to another
20
years!

By Norbert Gleicher, MD, Medical Director and Chief Scientist at The Center for Human Reproduction in New York City. He can be contacted through The Reproductive Times or directly at either ngleicher@thechr.com or
in the U.S. correctly as “highly regulated healthcare.” It, however, gets on somewhat thinner ice when immediately after that noting that in post Dobbs America (Dobbs v. Jackson Women’s Health Organization was the Supreme Court case that on June 24, 2022, returned questions about abortion rights from federal to state law), “access to reproductive healthcare, including access to ART (including IVF), is increasingly caught in the political crosshairs.”
BRIEFING: In reaction to a recent mailing from the ASRM, Dr. Gleicher, in this article, argues that – especially considering recent political events - linking ART/IVF automatically with the much more controversial abortion issue, represents a tactical as well as ethical/moral mistake for the reproductive medicine community. Recent political events, indeed, offer a unique opportunity to separate ART/IVF once and forever from the abortion issue, a false link initially made in the early days of IVF when anti-abortion and anti-IVF opinions mostly overlapped. With the very obvious success of IVF (almost 10 million births worldwide), both medical interventions, however, are no longer overlapping, as even increasing percentages of still stringent anti-abortion voices have come to appreciate the importance of ART/IVF. Continuing the automatic linkage between abortions and ART/IVF appears, therefore, nonsensical and self-defeating, and the correct argument should be that abortions and ART/IVF have nothing to do with each other. To the contrary, with one striving to end pregnancies and the other to produce pregnancies, they each stand on exactly opposite moral as well as practical grounds from each Everybody in the fertility arena is, of course, used to a steady stream of written communications from our mother ship, the American Society for Reproductive Medicine (ASRM). But recently, we received something new, a formal mailing (or should we call it a document) that summarized “oversight lessons for assisted reproductive technology (ART) for the U.S. from abroad.”1 In plain language, the ASRM is basically suggesting that how oversight of the IVF field is conducted in other countries may have some relevance for the U.S. More specifically, the ASRM feels that “any attempt to compare the U.S. regulation of medicine in general, and ART in particularly, should reflect a comprehensive understanding of the specifics and nuances of each nation’s healthcare and regulatory landscape.”
In describing the current status of ART in the U.S., the ASRM document then characterizes ART
What somewhat worries us about this and similar statements from other professional organizations, rightly concerned about reproductive rights, is that they basically accept the automatic conceptual link between ART and abortions, purposefully created by the right-to-life movement in the early days of IVF, when the rightto-live and anti-IVF movements were basically one and the same.
That has, however, changed, and nothing demonstrated this fact better than the last presidential election campaign, when the Trump campaign, led by Mr. Trump himself, let it be known that it wholeheartedly not only supported the unrestricted availability of IVF, but fully supported an even broader access to IVF services.
But, maybe, even better evidence for the need to uncouple ART/IVF from the abortion issue was what happened in Alabama after the bizarre Alabama Supreme Court decision to give personhood to human embryos.2 Understandably, all Alabama-based IVF clinics immediately closed; but –remarkably – in what, likely, was the quickest passage of a law in the state legislature, the state instantly indemnified IVF clinics from any claims that might arise from this strange court decision.3 In other words, one of the most conservative states with strong opinions about
abortions, very obviously, has also strong opinions about ART/IVF, and they completely diverge from their abortion opinions.
To continue linking the abortion issue with ART/IVF, therefore, makes absolutely no sense for proponents of reproductive rights and proponents of medical selfdetermination in general. In reality, not only does such a link between abortions and ART/IVF really not exist, but abortions and ART (including, of course, IVF) pursue exactly opposing goals: Abortions terminate pregnancies, while ART strives to achieve pregnancies. To automatically link them is not only harmful and self-defeating for ART, including IVF, but, therefore, really almost silly!
Recent political events, indeed, offer the opportunity to present this divergence more aggressively to the public in attempts to further hasten this separation. In specifically eschewing the legal changes the Italian Supreme Court fostered on the country, the ASRM document then noted the court’s acknowledgment that in 2005 IVF births represented 1.22% of all Italian births; yet by 2022, the percentage had increased almost fourfold to 4.25%. And considering that Italy has one of the lowest birth rates in the world, vastly below replacement levels, this development alone deserves notice from the public.
Declining birth rates throughout the world in more developed countries – this phenomenon does not only apply to the western world as countries like Japan,
Korea, and even China are now also severely affected by declining birth rates and the very troubling economic consequences that come from such a development – indeed offer another important economic argument in favor of aggressively supporting the use of IVF.
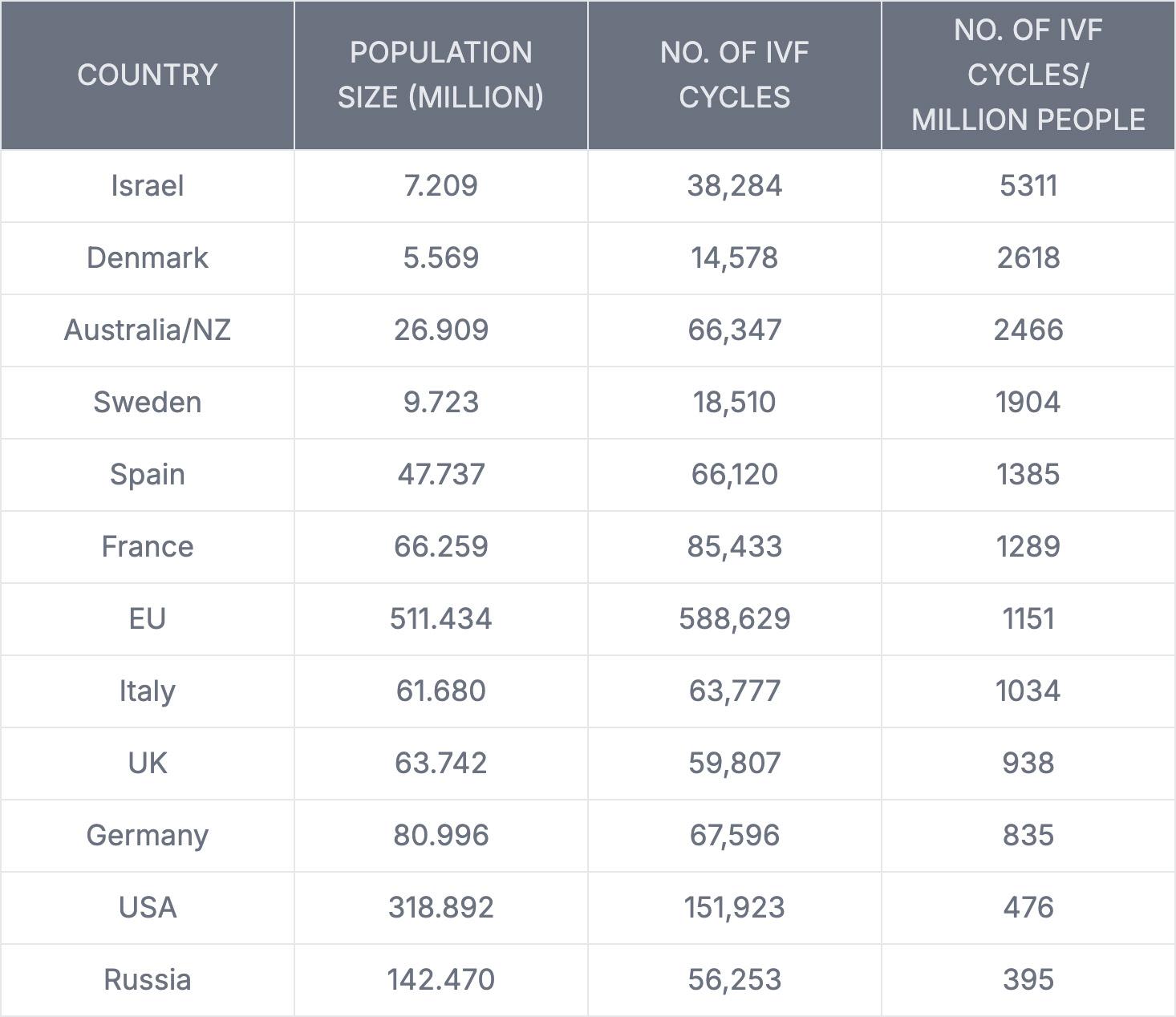
No country has recognized this fact as early as Israel which, therefore, demonstrates the, by far, highest per capita utilization of IVF in the world4 (below Table 1 lists the 12 countries with the largest IVF utilization per capita approximately 10 years ago) because the government pays for almost unlimited IVF cycles until a family has achieved at least three children. This, interestingly, stands in stark contrast to other developed countries where -very surprisingly for example in Scandinavian countries known for their liberal medical coverage – rather low female ages are used to limit IVF coverage In Sweden, for example, the upper age of IVF treatments can be between 37 and 41 for women but, of course, between 54 and 56
for males.5
In other words, especially IVF practice after over 40 years has achieved unprecedented ethical, moral, financial, and political support that should be used by professional organizations to completely de-link IVF from the abortion issue. If somebody still raises such a connection, the answer should only be: what are you talking about!
1. ASRM. Advocacy resources. https:// www.asrm.org/advocacy-and-policy/ fact-sheets-and-one-pagers/art-oversightlessons-for-the-us-from-abroad/
2. Johns Hopkins Bloomberg School of Public Health. February 27, 2024. https:// publichealth.jhu.edu/2024/the-alabamasupreme-courts-ruling-on-frozen-embryos
3. Mulvihill G. AP. March 6, 2024. https:// apnews.com/article/alabama-ivf-cliniclawsuit-immunity-things-know-0d16d3be 139f42c96bc3ab35c4467f55
4. Birenbaum-Carmeli D. Reprod Biomed Soc. Online;216-23. doi: 10.1016/j. rbms.2016.05.004
5. The Swedish National Council for Medical Ethics. February 2013. https:// smer.se/wp-content/uploads/2013/03/ Slutversion-sammanfattning-eng-Assistedreproduction.pdf
By Sònia Gayete Lafuente, MD, PhD, who is a Foundation for Reproductive Medicine Research Fellow at the Center
Reproduction (CHR) in NYC. She

for Human
can be reached through the editorial office of the VOICE or directly at sgayete@thechr.com.

BRIEFING: All over traditional as well as social media, emotional and mental health-related aspects of reproductive health and fertility, as well as their counterparts, infertility, pregnancy loss, and other reproduction-linked issues, have lately become important topics of discussion. Always shaped by personal and family, as well as cultural backgrounds, and often increasingly political, conversations about these subjects have never felt more urgent. If one is only willing to look, one often finds experiences of hope and heartbreak, resilience and vulnerability, as well as shame and silence, only too often hidden behind splashing headlines and hashtags with the purpose of excluding even close friends and family and leaving the individual to process things quietly and alone. Unsurprisingly, so-affected women are often not only physically but also severely emotionally damaged in identity, relationships, and overall emotional well-being. This brief article is only the first in a planned series of articles in the VOICE by this author, inviting readers, including, of course, infertility patients, but also healthcare providers and, hopefully, policymakers, to engage more deeply with the emotional aspects of reproductive health. Today’s article attempts to point out some of the suffering patients experience along their fertility journey, divided into three stages where support is most needed: the pressure to conceive, the struggle with infertility, and the grief of pregnancy loss.
Societal pressure to conceive and its impact on mental health
The expectation to conceive is
still deeply rooted in society. Even from people who know little or almost nothing about the person they are talking to, their question may not even be whether a woman wants children at all, but when or
even why she is not already having them now. The psychological toll from such social pressure can, of course, be significant and usually increases in intensity with age. Ethnic and religious backgrounds

often further complicate things, and queer individuals may face an especially difficult time. Now imagine that an infertile woman faces these questions who, quietly, may have tried for a long time to conceive. How must she feel?
And then there is, of course, also the "fertility clock," called the biological clock. What is meant by this term is the unfortunately indisputable fact that female fertility declines with advancing age, with this decline speeding up after age ca. 38 years. As women get older and remain childless, societal pressures, therefore, further increase and become especially painful for infertile patients who often do not wish to share knowledge of their infertility, even with their closest friends and family. For so-affected women, fertility then sometimes becomes a symbol of personal worth, making the woman feel inadequate even vis-à-vis close friends and family. And yet, only rarely are these struggles publicly or, even in the infertility literature, addressed.
To truly support reproductive well-being, we must normalize conversations around familybuilding wishes and timelines and recognize that choosing when, how, or whether to parent is deeply personal and worthy of respect. We also must recognize that having children, a concept for millennia baked into routine societal behavior, in several Western as well as Asian societies can no longer be counted on. There are several reasons for this development: Women in many societies are no longer as eager to get married, and maybe even more importantly, having children in many developed
countries has become extremely expensive. Consequently, many developed countries, the U.S. included, face declining birth rates, not even being able to meet replacement levels for their dying citizens.
The emotional rollercoaster of infertility and navigating vulnerability and uncertainty Infertility is not only a medical diagnosis but often an emotional crisis. Month after month, test after test, hope builds, and then, more often than not, collapses.
Infertility practice is, indeed, likely the only medical specialty outside of experimental medical practice in which treatment failure rates by far exceed success rates. In other words, every treatment cycle, not different from natural conception, even at peak fertility at young ages, will, with greater likelihood, not lead to pregnancy but result in embryo implantation, ongoing pregnancy, and, ultimately, a healthy birth. Suppose one considers the healthy live birth of a baby the ultimate success of any fertility treatment. In that case, the failure rate, indeed, further increases, considering that roughly half of all embryo implantations are lost during pregnancy before the viability of a fetus is reached.
Returning to patients with infertility, many find themselves feeling vulnerable in ways they never anticipated, and these feelings can have consequences. For example, not infrequently, intimacy with partners can become challenging, as anticipated time
planning of the couple gets delayed and delayed again. Moreover, once again, cultural and religious backgrounds may make things even more complicated than they already are. For example, different religions disallow several infertility treatments and/or require patients and their fertility services providers to jump through, at times, complicating hoops to even be able to apply for fertility treatments.
And then there are, of course, again cultural backgrounds with more or less societal emphasis on parenthood. Pregnancy-delaying and/or preventing issues will, in societies where pregnancy, especially for women, is these days framed as a central life achievement, often take on lifethreatening connotations. But simply feeling too embarrassed to share their struggle with friends and family — fearing judgment and/or pity — and, therefore, emotionally isolating, will already intensify their suffering.
Healthcare providers must be aware of the importance of the cultural backgrounds of their patients and must be sensitive to the emotional weight patients often carry with them when they finally take the step of reaching out to a fertility clinic for help. It is then the provider's responsibility - whether nurse, embryologist, or physician - to ensure patients feel not just monitored but truly seen, heard, and taken care of. Nothing is more disempowering than feeling rushed or even just treated like a commercial transaction by those meant to help. Emotional support must be an integral part of fertility services at all fertility clinics and should never become another layer

From hope to heartbreak: Grieving for a baby - never met! Few experiences compare to the grief of losing a pregnancy. A phrase often heard from patients is, "one moment, - the promise of life; and the next, it is gone." Whether it is a miscarriage, stillbirth, or even a medically or socially necessary abortion, the loss is real, and the undeserved self-blame can be profound. Yes- even for those who, for whatever personal reasons, had to decide to terminate a pregnancy, losing a pregnancy is never easy and always painful. And almost every loss comes with maternal guilt. What did I do wrong? What could I have done to prevent it from happening? Women start wondering about their diet, was what they had lifted too heavy, or whether it was their intercourse. In fear of a potential repeat, what they could have done differently becomes, at times, an allconsuming question. And, although rarely logical, it is a powerful emotion, as it is human nature to try to find answers, make sense of things, and, hopefully, find a way to avoid a repeat.
In the currently popular culture of glorifying one's autonomy over our body, it becomes almost impossible to accept that some outcomes are just beyond our control. This kind of thinking also characterizes the early pregnancies for those lucky enough to get to this point. The first question on the ultrasound table, then, is unsurprisingly often: "Is there still a heartbeat?" And once confirmed, - exhaling, “thank God… I couldn't sleep all week thinking about it."
Grief for lost pregnancies can even continue beyond later successful births when some parents continue to celebrate hypothetical birthdays, milestones never reached, and love never fully given. These silent anniversaries can echo for years.
Addressing the emotional needs of infertility patients comprehensively Emotional care for infertility patients is often somehow left behind, even in fertility clinics that provide excellent clinical care. One hears only too often from patients of having had the feeling of "being in the production line of a factory, never having seen the same physician, or, especially in more recent times, only having been able to see the nurse practitioner or physician assistant rather than their own doctor" (not that RNPs and PAs cannot provide excellent care).
Good patient support requires validation. People healing from failed fertility treatments or pregnancy loss need safe spaces to cry, share, express anger, and even rage, or simply be able to acknowledge to themselves that "this happened to me." This acknowledgment alone can be powerful because it can break the patient's isolation and build resilience. Understanding this, in some cases, may then lead to the realization that therapy can help, but so can patient groups, online communities, or any caring person who listens without assuming, without judging, and without trying to fix. At the Center for Human Reproduction, I have learned that, after initial consultations with patients, the most important consultations are those after failed treatment cycles.
Mental health professionals must be increasingly integrated into routine infertility care. As infertility providers, we must support systemic changes with more accessible mental health services and policies that respect the complexities of reproductive journeys, hopefully creating a culture where healing is not a private burden but a collective responsibility.
While grief may never fully disappear, healing is possible. The key lies in integrating the pain and honoring what was lost, while still choosing to move forward. Ultimately, almost everybody finds new ways to love, hope, and move forward - sometimes as parents, sometimes not.
If you are reading this right now and find yourself somewhere on the here-described spectrum, ranging from uncertainty about your fertility to the deep pain of loss, we hope that you now understand that your experience matters and, most importantly, that you are not alone!
Bindeman J, Abbasi R, Sacks PC. The Mental Health Traumas of Infertility: Impact and Consequences. Obstet Gynecol Clin North Am. 2025 Mar;52(1):133-143. Cuenca D. Pregnancy loss: Consequences for mental health. Front Glob Womens Health. 2023 Jan 23;3:1032212.
Ruderman RS, Yilmaz BD, McQueen DB. Treating the couple: how recurrent pregnancy loss impacts the mental health of both partners. Fertil Steril. 2020 Dec;114(6):1182.
Massmann K, Jagannatham S, Stone J, Platt LD. The Impact of Stillbirth on Maternal Wellbeing. Obstet Gynecol Clin North Am. 2025 Mar;52(1):145-156.
Bar V, Hermesh T, Reshef P, Hermetz S, Hertz-Palmor N, Gothelf D, Mosheva M. Healing hearts: mind-body therapy for mothers after stillbirth's silent grief. Front Psychiatry. 2025 Feb 28;16:1534616.

BRIEFING: The following article originally appeared in the Wellington Neighbors Magazine (Wellington is a suburb of Palm Beach, FL), where the author and her son reside. The photograph below was on the cover. In a text message to the VOICE , the author noted, “I put heart and soul into the article.” And she, indeed, did! But even more importantly, she, in this article, is a voice for thousands of single women who face the difficult choice of whether to remain childless or make the challenging decision to become, with all the associated difficulties, a single parent. She chose to go for it and was rewarded with a truly amazing young man in the house after all. We know because we had the opportunity to meet him, and he is already taking good care of his mom.


My name is Olga Dragunsky . I have a 5-year-old son, Arnold. The reason I felt compelled to tell my story of having a child on my own is to encourage other single women to follow their desire of becoming a parent.
Let’s start from the beginning. I was born in Moscow, Russia, and was brought to Chicago with my twin sister by our mother. We were 16 years old and didn’t speak a word of English. The only times we felt comfortable were in math classes since mathematical formulas didn’t require English proficiency. By the end of the year, we were fluent in English.
Later, both of us graduated from George Washington University with a degree in International Finance and Marketing and a minor in Business Law.
My first encounter with infertility happened while working at a leading genetics institute in Chicago. To my surprise, I saw countless patients going through In-Vitro Fertilization hoping one day to become parents. Never did I think I would be going through this journey as well. It was my destiny!
Like most young women, I dreamed of being swept off my feet by prince charming, getting married first, and then having children. Theoretically, that was the premise for my future, but I was too determined to be successful professionally and lost track of time, not realizing my biological clock was ticking.
One day, it was time to make a decision, and I made it! I decided to have a child on my own by using a sperm donor. It took me a very long and painful seven years to reach my goal. Endless shots and a shattered heart after every negative pregnancy test, but my persistence and my desire to become a mother did not allow me to give up. And finally, my dream came true. Fifty years old, I gave birth to my beautiful boy Arnold Giovanni .
I would be lying if I said being a single mom is super easy. Sleepless nights, worrying when Arnold gets sick, running between my demanding job and his activities, and everything else that comes with the territory of being a mother. But, at the end of the day, to hear Arnold’s laugh, his first spoken word “Mama,” seeing his first accomplishments in reading and writing, later cheering on sidelines of his soccer games, tennis or anything he enjoys, and getting a big squeeze followed by “I love you Mommy,” I realize how lucky and blessed I am.
Arnold and I moved to Wellington last December after I accepted a fantastic opportunity at PAM Health Rehabilitation Hospital in Jupiter. It took us a few months to settle, but we love living here, spending time with neighbors, enjoying pool and holiday parties, and going to the Lion Country Safari and shows at the Kravis Center. We are looking forward to the season of Polo matches and Saturday Night Lights.
I feel very honored to be on the cover of Wellington Neighbors Magazine . I take pride in sharing the experience of my journey to motherhood. My message is rather simple, if you really want to be a mother, go for it! I have met so many incredible smart and
s uccessful women who have told me, “I wish I had enough guts to do what you have done”.
It makes me so sad to hear that. Take motherhood into your own hands. If you are in your twenties/ early thirties and still single, freeze your eggs. That way you can take a breather.
Believe in yourself and trust advanced modern medicine! If I could do it, you can do it too! Remember you don’t have to justify yourself. Motherhood comes in different shapes and sizes! Everyone has a different journey in life. There is nothing wrong with having a baby first and then finding your soul mate. Down the road, the last thing you want is to look back and regret not having a child.
Having my son was, without a doubt the best decision I have ever made! My dear known and unknown women, my sisters, I wish all of you luck!
We could not agree more! And as a special note to our younger female readers, listen to the author’s comment about fertility preservation through egg freezing at a younger age.



BRIEFING: Something broke in the world on October 7, 2023, and we are not referring here only to the atrocities committed on that day by the savages of Hamas when they invaded Israel—murdering and raping attendees at a music festival in the desert dedicated to peace, and 'exterminating' whole families (the word 'exterminating' is intentionally used here to evoke historical reference to the Holocaust), murdering and burning innocent children in their homes in front of their parents, and parents in front of their children, and abducting over 200 hostages of all ages, including almost newborns.
What appears to have broken the world on that day — and essentially ever since — was the world’s response to these occurrences. Nowhere were these responses more disappointing than on university campuses across the globe, including in the United States. That the most educated youth — often at the most prestigious universities — could not only sympathize with a terror organization like Hamas (which had already been designated a terrorist organization by the U.S. and many other governments prior to October 7, 2023), but openly identify with it ('we are Hamas'), was simply shocking. Even more shocking, however, was the response of many university faculties and administrations — especially at elite institutions such as Harvard, Columbia, and, in Europe, Oxford University — making it abundantly clear that some of the world’s allegedly finest academic institutions have reached a major crisis point in fulfilling their educational obligations to students and society at large.
Instead of educating the youth of the country in an unbiased manner, faculty, especially at elite universities, have been taken over by followers of Critical Theory, often infused with strong Marxist undertones, and have indoctrinated their student bodies accordingly. The results have been largely catastrophic, not only for universities but for society as a whole. These outcomes include the 'defund the police' movement; justice systems increasingly tolerant of lawbreaking — often showing more concern for perpetrators than for their victims; gender reassignment procedures for children; males competing in women’s sports and sharing bathrooms and dressing rooms; open borders; sanctuary cities and states; and DEI (diversity, equity, and inclusion) initiatives that have, in some cases, fostered reverse racism and renewed segregation. Other consequences include the abandonment of meritocracy and discrimination, such as against Asian applicants in university admissions, and Jewish students in the wake of October 7.
But most disturbingly, significant numbers of the country’s youth have even become tolerant of the idea that murder — and in the case of the Hamas atrocities, even worse — is a morally acceptable tool for attempting to change society. Examples of this new moral low can be found not only in the identification of so many young people at universities with Hamas and its goals despite extensive documentation of the Hamas atrocities on October 7, but — closer to home — in the cold-blooded murder of Brian Thomson, UnitedHealthcare CEO, by Luigi Mangione (26 years old), who shot him several times in the back with a homemade gun in front of New York’s Hilton Hotel, and who has since become, for many, a real folk hero.
The Center for Human Reproduction (CHR) addresses in this Editorial opinion what we currently consider to be an educational as well as administrative crisis in academia that must be addressed through a radical reorganization of especially leading academic institutions. This does not mean that the government should control who teaches and what is taught in private academic institutions. But even private institutions are forbidden to discriminate against student groups by race, religion, and in any other way, and if universities do not follow the law in this regard, the government not only can, but under the law must, withhold federal funds from colleges and universities. And even private colleges and universities should offer as unbiased an education as possible: After all, schools at all levels should educate and not indoctrinate!
Moreover, if universities become “politically engaged” in support and/or in opposition to one political party and/or candidacy (and here a correct definition of what that means is, of course, of great importance), they, rightly, may – and should - lose their tax-exempt status.
In concluding remarks, this Editorial also comments on how the current crisis in academia affects the reproductive medicine field.
Introduction
It, of course, is exaggerated to say that all of academia is in crisis. That is clearly not the case. Indeed, the vast majority of academia is actually not only unaffected by the craziness involving some academic institutions, but may, indeed, benefit from what is currently happening to a majority of elite universities and colleges, which traditionally have been receiving enormous sums of money from the federal government.
As those elite universities and colleges – considering the political behavior of many of their students and faculty members – increasingly struggle with maintaining their elite image and status in society, lower ranked academic institutions

with more balanced student bodies and faculty, and – importantly – wiser and, therefore, better administrations may end up being the ultimate winners from all the uproar currently playing out in media on a daily basis. Those second and third-tier institutions will end up recruiting better students who, in past years, would have preferred to attend one of those so-called elite schools. Look, for example, at the significant losses in early registration Harvard University has reported and compare this, for example, with the brand-new and extremely popular University of Austin in Texas, which, already in its current second year of recruiting a class, may be more difficult to get accepted at than Ivy League schools. Per the university’s website, its very telling motto is, “Dare to Think!”



Dare to Think!
We, therefore, address only the very obvious troubles elite institutions like Harvard, Yale, and Columbia University find themselves in (there, of course, are many more of those institutions in trouble). The higher they were nationally ranked before October 7, 2023, the deeper they now are threatened to fall, and the more they now, of course, have to lose.
Take, for example, the currently most obvious case— Harvard University, like Columbia University and other prominent universities around the country. For several good reasons, Harvard, for example, attracted the attention of the federal government because of alleged violations of its charter after taking only insufficient actions against pro-Hamas student groups on campus that selectively harassed Jewish students. Harvard, therefore, has already (at least for the time being) lost billions of dollars that the University, like pretty automatically for decades, had expected from the federal government.
President Trump himself, moreover, announced that, considering the University’s handling of very obvious anti-Semitism on campus and other discriminations of minorities (Harvard at that point was already under a consent decree with the government that mandated an end to racially based admission processes that discriminated especially against Chinese applicants for admission), the Justice Department should determine whether the University’s not-for-profit status should be terminated.
Harvard has 53.2 billion dollars in its endowment — the largest endowment among all academic institutions — but this money is only partially freely available to cover daily administrative and/ or research support. Most of t he funds in the endowment are restricted to only certain uses. Here is a quick summary from the Harvard in the graphic below.
These are, of course, quite impressive numbers! What the University, however, does not disclose on its website, but what media reports have stated, is that — in addition to being tax-exempt — Harvard in 2025 could have expected in excess of $10 billion (yes, billions) in grant support from the federal government. If one then imagines that the federal government may, indeed, have the power not only to cancel those $10 billion-plus — but also the University’s tax-exempt status — it will immediately become very obvious that even an endowment of $53.2 billion — especially if mostly restricted — does not bode well for Harvard’s economic future.
$6.4 billion the University's annual operating expenses in the 2024 fiscal year 14,600 different funds make up Harvard's endowment 70% of the endowment's annual distribution is donor-directed to specific programs, departments, or purposes
$56.2 billion the University's endowment in the 2024 fiscal year
How diversity-equity-inclusion (DEI) became a dominant practice on campuses
The Republican Congress and the Trump

administration very obviously don’t like what has been transpiring at most leading academic institutions since October 7, 2023, with pro-Hamas encampments and, at times, violent demonstrations expressing support for an organization that committed barbaric acts of horrific rapes, murders, and abductions involving even babies and children. They then simply murdered a majority of the abducted who didn’t die from starvation, including a mother with her two little children. Hamas, moreover, has for years been defined as a “terrorist organization” by both Democratic and Republican administrations.
In our opinion, rightly, the current Republican administration, however, views what has been transpiring on so many campuses — especially elite universities—since October 7, 2023, as much more problematic than that because the administration sees a majority of protesting students as only the final product of a chain-linked education system that increasingly has gone off balance for decades. Almost exclusively leftist educators, from basic kindergarten to academic faculties at colleges and universities —recruited, in turn, by almost exclusively leftist administrations at all levels of the education system — have made these elite universities the end product of a decades-old, multi-generational process of classical Marxist-style indoctrination strategies, first expressed mostly in West German universities post-WWII by such intellectuals as Theodor W. Adorno (1903–1969) and Herbert Marcuse (1898–1979), before coming to the U.S. and influencing such later well-known individuals as Angela Davis , Abbie Hoffman , and Jürgen Habermas
This process, of course, also did not end with administrations; it even reached into boardrooms, as Harvard once again probably demonstrated

better than any other Ivy League school. The closest to a company board at Harvard is the current 13 members of the Harvard Corporation (a self-feeding board), with its chair being Penny Pritzker, heiress of the Pritzker fortune. She served as Commerce Secretary in the Obama administration, and guess who her brother is? Yes, you probably guessed right — Jay Robert "J.B." Pritzker , the current Democratic governor of Illinois and likely 2028 presidential candidate.
As a major proponent of DEI, according to reports in the media, Penny Pritzker was almost singlehandedly responsible for the appointment of Claudine Gay, PhD , as President of Harvard. She allegedly insisted on a non-white female candidate by refusing to even interview male candidates. That Gay turned out not to be the best (who can forget her performance at the Congressional hearing on antisemitism?) does, therefore, not surprise: a typical product of decades of academic DEI, her publication list was not even deserving of a professorship (and even that list was allegedly accomplished by plagiarizing). But none of that, of course, mattered as long as she fulfilled the really important criteria of being female and Black! One can, therefore, view the current status of the country’s leading universities not only as a steadily growing takeover of those institutions by ideas mostly stemming from the Frankfurt School of Critical Theory.




Marcuse was, in the U.S. and elsewhere, indeed widely celebrated as the “father of the New Left” and became the dominant theorist of the student movement in the 1960s and 1970s in Germany, Austria, France, and, ultimately, also in the U.S.
How effectively Critical Theory has conquered U.S. academia over the decades since is better understood once one comprehends Critical Theory’s most basic worldview: while Critical Theory has followed many different political strategies since the mid-20th century, it is united by one socio-political purpose, which is to better understand human experience with the purpose of bringing about social change— because a single truth does not exist. Understanding Critical Theory, therefore, explains the relativity of morality — how some of the allegedly best-educated children at elite institutions can support Hamas; how a person can become a sympathetic and admired figure who point-blank shoots to death the CEO of a major health insurance company, and how prosecutors trained in Critical Theory can express more sympathy for criminals than for their victims.
Critical Theory, therefore, also explains DEI and how diversity could replace meritocracy and equity could replace equality. Consequences are not only significant but diverse. It is how Harvard got a president like Claudine Gay and how, over the last decade, almost all leading universities and colleges got a female president. And whenever the sex of a person or her skin color becomes more important than the person’s professional qualifications, the quality of performance declines. And if this happens over decades, the consequences will be felt not only in academic institutions but also in the control towers of our airports, the cockpits of airplanes and helicopters (Washington, DC), in small and large corporations, and — yes — also in emergency and operating rooms in medicine.
What are the options for academic institutions that find themselves in the crosshairs of the federal government?
While initially obviously motivated by the nationwide, at times violent, pro-Hamas demonstrations on campuses by students (how
much non-university-based individuals and NGOs were involved in many of these events is apparently currently still the subject of investigations), the current Trump administration, however, understood the roots of what was happening at our elite universities. If there was to be success in changing the culture of these colleges and universities, it was obvious that decades of “inbreeding” of faculties, administrations, and institutional boards had to be reversed. And that, of course, would require major surgery!
Consequently, the government’s demands from universities like Columbia and Harvard significantly expanded from initial demands of only controlling the campus activism of radical, mostly pro-Hamas students, to the much broader goal of changing the culture of these institutions from the ground up. This meant starting with a radical improvement in the diversity of opinion among teaching faculties — faculty members with conservative opinions in many departments at many prominent universities currently hardly exist, and/or, if they exist, are often hesitant to express their opinions, if at all — and rebalancing leftist-Marxist and Critical Theorybased curricula. In other words, the demands of the Trump administration, under the threat of withholding federal funding, increased beyond the initial demands of controlling campus anti-semitism and other forms of discrimination.
At the time of this writing, demands and responses from only two Ivy League universities are known— Columbia and Harvard—and the responses of these two universities could not have been more different, really representing the binary options universities currently have if the Trump administration perceives them to be discriminatory to minorities among their student body. If they want to secure continuous funding from the federal government, they have to agree to address the above-noted inequities pointed out by the government at all levels — and have to do so at times under the control of outside experts.
Columbia University caved quickly. But then, the new temporary President of Columbia — Columbia — on a side note, she is a physician — who had replaced Columbia’s permanent female president after her resignation following a similarly obscene performance in the same hearing on campus anti-

Semites before Congress as the above-noted Harvard president, did not have the guts to acknowledge the agreement with the government. In front of members of Columbia’s—for decades—well-known proPalestinian and often openly anti-Semitic faculty, led by its Middle Eastern Studies Department, she then, as The Intercept reported, reassured its Middle Eastern studies scholars behind the scenes—“to appease Trump, threw them to the wolves.” 2 And that was then the end of her temporary presidency at Columbia. 2
The following, quoted from the Editorial Policies and Procedures of The Intercept , characterizes its political stance well:
"At The Intercept , we strive to hold the powerful accountable with truthful and aggressive reporting. We seek to be fair in our coverage, which means allowing people or institutions a reasonable window to respond to reporters’ inquiries before publishing a story that contains significant revelations about them. It does not mean mandating “balance” when one perspective on a subject — such as the science of climate change, or the justification for a war crime — is clearly without merit (sic., - a typical Critical Theory statement!)."
Provost Alan Garber, MD , became interim President at Harvard when Claudine Gay, PhD, was forced to resign and has since become the permanent president of the institution and chose the opposite strategy of fighting the government. As a recent precinct article in The New York Times noted, 3 Garber, indeed, agrees with many of the criticisms brought by the government against Harvard and, even

before a recent in house commission concluded that Jewish as well as Muslim students had been exposed to significant discrimination by the University (Harvard apparently still believes in equity because we are not aware of, for example, violent demonstrations on campus against Muslim students), that the university “had a problem with antisemitism on campus.” Conveniently himself Jewish, he, however, is also a highly recognized academic physician, health care economist, previously at Stanford University in California, and medical school administrator who clearly reached his many leadership positions based on merit and, apparently, never strived to become president of Harvard.
Recruiting a powerhouse of – interestingly – conservative lawyers close to the Trump administration, he decided to fight the government in court, according to The New York Times article, 3 allegedly “incensed that the government wanted to control faculty recruitment and curriculum of the university.” For many at universities and in the media, this decision – instantly – elevated him to being a “hero” of the resistance to the Trump agenda, and it will be interesting to see how many other colleges and universities under government scrutiny will follow the Columbia or Harvard example. Considering Barber’s personality as described in The New York Times article, his fight-fight-fight position seems somewhat of a surprise, and one must wonder whether this was, in principle, really his decision or was driven by the real top leader of the university, the chairwoman of the Harvard Corporation, Penny Pritzker whose personality profile and, of course, political history, fits such a decision much better. Interestingly, billionaire and philanthropist Bill Ackman, MBA , as recently at Bloomberg 4 and other news outlets, not for the first time quite outspoken about the level of antisemitism and political indoctrination at his alma mater, Harvard, called for Pritzker’s removal from her position and a change in Harvard’s response to the government’s demands from legal warfare to negotiations .4 Finally, a little-known fact by the public is that the Pritzker and Trump clans have a long and not very positive history of a partnership in real estate in the 1990s (the Hyatt Hotel on 42nd Street) that didn’t work out too well. 5

To a degree, colleges and universities are a microcosm of societies, at least of educated societies, and – even more importantly – they reflect to a degree the future political leadership of the country. Consequently, considering what campuses these days reflect, what is currently happening at so many institutions of higher learning, therefore, must be concerning.
But hold on for a moment: In favor of Hamas and a murderer of a healthcare executive protesting students represent only a very small fraction of the total student body and seemingly observable numbers even still appear exaggerated because, as has become abundantly clear, many participants in these demonstrations – on and off campus - not infrequently include more behind masks hiding often paid professional agitators who may have nothing to do with the campuses where they are protesting than students at the university. Most of these demonstrations are well organized, obviously supported by NGOs (which the government allegedly has started to investigate, with the goal of also potentially depriving them of their tax-exempt status because of political activities.
A second interesting observation is the large majority of female protestors in comparison to males who usually take part in those demonstrations. At the most recent library takeover at Columbia University, 61 out of 80 arrested protestors were female. 6
And then there are, of course, at all of these demonstrations also the usual political agitators, as already noted, often not only paid, but also supplied with face coverings (why are these still permitted/) and obviously prefabricated placards and signs as well as highly sophisticated loudspeaker systems. Bluntly speaking, there is lots of money behind these demonstrations, likely involving similar sources to those that financed Occupy Wall Street (OWS) and Black Lives Matter (BLM), with the single biggest donor likely being the little – but very rich – country of Qatar, which as media reported has also donated billions of dollars to U.S. universities (one wonders why?)
And now to what is, likely, the most interesting aspect of all of these demonstrations, which still appear to be everywhere. For the second year in a row, protesters again showed up in front of the annual Met (fashion) Gala at the Metropolitan Museum of Art in New York City. At a time when the youth of the country once again appears obsessed with an international political problem (interestingly, there are hardly any demonstrations in favor of one or the other side in the Ukraine war, the Sudan war, the conflict in Libya, the conflict in Syria, the fighting between India and Pakistan, and we could go on and on), the trend toward the political right especially among young men is strengthening. It appears that even students are getting increasingly tired of the indoctrination they find themselves exposed to at our elite universities!
And how does all of this relate to medicine in general and especially reproductive medicine?
Reproductive medicine is, of course, an integral part of medicine, and what is happening in academia in general, therefore, matters to medicine in general, including reproductive medicine in all of its many versions. Currently threatened cuts in budgets of, for example, the NIH, therefore will have consequences for research in reproductive physiology and biology in general but – maybe somewhat surprising for many readers – for two reasons will have only relatively little impact on the infertility field: First, with infertility in the U.S. over the decades increasingly having moved out of hospitals into ambulatory and, often, private settings, the amount of academic research in the field – never a very prominent endeavor – has in the U.S. only further declined. And when nobody asks for grants, the NIH cannot award them.
A second reason is maintenance of the so-called Dickey-Wicker amendment by Congress which basically prohibits almost all federal funding for almost all IVF-related research and clinical practice unless – as we in these pages previously suggested the amendment – hopefully - this year will finally be terminated by the Trump administration when the time comes to submit this year’s federal budget. The amendment, otherwise, automatically renews

every year with the passage of the annual budget bill. The current Congress, therefore, has a unique opportunity to greatly improve IVF-related research in the U.S if it repeals and finally terminates this amendment (Mr. Musk and Mr. President, are you listening?!).
Otherwise, the practice of fertility medicine faces the same academic problems that other medical specialties encounter. Medicine as a whole has changed at the physician level from a Conservative into a much more Progressive profession.
In parallel, professional organizations not only within the fertility field but in all of obstetrics and gynecology have radically changed, none more so than the American College of Obstetricians and Gynecologists (ACOG), which has truly become a bastion of DEI and progressive ideology that we often have difficulties following. To say it bluntly, the leadership of ACOG at times appears so lost in difficult-to-understand, bombastic ideology that one must wonder what the organization these days really stands for. One, therefore, has to give credit where credit is due to the leadership of the ASRM, which during recent years of “wokeness” just did the minimum to not be called out by the more radical membership of the society. Job well done!
At the same time, it must also be acknowledged that within less than two physician generations, the field of obstetrics and gynecology has undergone a successful sex change operation, from being a strongly male-dominated specialty to an overwhelmingly female-dominated medical field. Indeed, all of medicine is becoming increasingly a female profession, though not without significant complicating consequences: Though women make up now a majority of medical school students, they, still, make up only 37 percent of practicing doctors; 7 and the reasons are manifold but, of course, circle around motherhood, part-time work, and even just giving up on practicing medicine.
That women don’t practice the same number of hours as men can, therefore, of course, is not a surprise; but this fact, of course, will greatly contribute to the
already existing physician deficit in the country, which is only expected to get worse. And, in the practice of equality, one must also acknowledge that male physicians now also routinely take paternity leaves when their children are born – an idea only several decades ago unthinkable – and now widely accepted.
But likely the biggest threat to medical academia –and in no medical specialty, likely, more threatening than in reproductive medicine – is the lack of desire by physicians to join academic faculties. With private equity controlling rapidly increasing percentages of the infertility practice market in the U.S. and in many other countries and aggressively competing for physicians in a medical specialty that annually produces less than 100 graduating fellows in the subspecialty of reproductive endocrinology and infertility (REI), academic faculties are starved of quality candidates. And this represents an enormous problem for the specialty already now, and can only get worse, because who will then drive the field forward?
At a time when important sections of academia are in much of a mostly self-created and mostly political-ideological crisis, at least partially associated with academia, the field of medicine is, of course, fully exposed to all the storms currently clouding the future of many of our nation’s most cherished academic institutions. Medicine and, especially the practice of infertility medicine, in addition, however, also faces many field-specific problems for too long, and now threatens the quality


and progress in the field. Currently, already very obvious trends make changes in infertility practice unavoidable. Their seriousness, however, still appears widely underestimated in the field. We hope this article will be a reminder. It started with the statement that “something broke on October 7, 2023, which literally worldwide brought to the surface a level of anti-semitism not seen since Nazism in the 1930s and on.
In closing, it is important to note that the medical field is not spared in all of these developments. Who can forget the two Australian nurses who, in a video interview with an Israeli journalist (lower small photo on left), publicly claimed to have killed Israeli patients (and to kill more) – whether they really did it or not (see photo montage below). 8 They were fired from their jobs at a Sydney hospital, and a police strike force was established to focus on the antisemitic crimes since the Israel-Hamas war began in 2023 to investigate potential offenses stemming from the online video that contained the original claim, including breaches of hate speech law. Except that we are unaware of any conclusion reached so far by the strike force! An article in The New York Sun reported on this video with the headline, “Video of Australian Nurses pledging to kill Israeli Patients is just ‘the tip of the iceberg’ in Australian health care system.” 9 But one does not even have to go as far as Australia: The U.S. co-author of a recently published study by StandWithUs very recently noted that academia (medical academia included) today is increasingly cultivating an environment which is hostile to Jews, as well as members of other religious and ethnic groups.
According to this report, 62.8% of Jewish health care professionals employed by a campus-based medical center reported having experienced antiSemitism since October 7, 2023 — the study was titled “Anti-Semitism in American Healthcare: The Role of Workplace Environment.” Overall, the study suggested that almost 40% of all Jewish-American health care providers encountered anti-semitism in this period in their workplace either personally or by observation. 10 The study included 645 Jewish health care providers, among whom many claimed to have been subject to ‘social and professional isolation,’ while 26.4% felt “unsafe or threatened.”
1. Harvard University. https://www.harvard.edu/about/ endowment/
2. Bose M, Biazzo S. The Intercept. April 16, 2025. https:// theintercept.com/2025/04/16/columbia-middle-easternstudies-trump-attacks/
3. Kolata G, Peters JW. The New York Times, May 3, 2025. https://www.nytimes.com/2025/05/03/us/harvard-alan-garbertrump-administration.html
4. Lorin J. Bloomberg. May 5, 2025, https://www.bloomberg. com/news/articles/2025-05-05/ackman-slams-harvard-formismanagement-calls-for-pritzker-exit
5. McCormick et al., Wall Street Journal, May 6, 2025. https:// www.wsj.com/us-news/education/penny-pritzker-harvardboard-trustees-f3545e40
6. Sabes A, McAdams A. FOX NEWS. May 8, 2025. https:// www.foxnews.com/us/mostly-women-arrested-columbiauniversity-library-takeover-nypd
7. O’Connell-Domenech A. The Hill. February 22, 2024. https://thehill.com/changing-america/respect/ equality/4479304-more-women-than-ever-are-becomingdoctors-heres-why-there-are-still-so-few/#:~:text=Women%20 now%20make%20up%20more,37%20percent%20of%20 practicing%20doctors.
8. McGuirk R. AP News. February 12, 2025. https://apnews. com/article/australia-bankstown-hospital-nurses-kill-israelis4600438279d0a1e5b75f9a31a3108ff3
9. Zhukovsky N. New York Sun. February 17, 2025. https:// www.smh.com.au/politics/federal/footage-shows-pair-inhospital-uniforms-bragging-about-killing-israeli-patients20250212-p5lbf3.html
10. Pierre DJ. The Allgemeiner. May 7, 2025. https://www. standwithus.com/post/new-study-exposes-antisemitism-inuniversity-medical-centers

BRIEFING: Spheres within spheres within spheres! That is just what we are demonstrating this month as our image gallery takes aim at the nucleus of the oocyte (or egg as we call it once it has matured). As in all cells, the nucleus contains the DNA where "genes" are organized into linear sequences forming a template for the production of RNA molecules. The DNA is complexed with proteins and supercoiled into something called chromatin that, in oocytes, takes on an unusual disposition, referred to as chromosomes (just a high school refresher!). But the nucleus of oocytes itself is highly specialized and has historically been known as the germinal vesicle (or GV, for short).
Besides the chromosomes, seen as filamentous or fibrous structures (see FIGURES 2-3), the GVs of most all animal oocytes (yes, they look very similar whether from a mouse, a monkey, a cow, or a human) contain a single dense spherical structure. This nucleolus is a factory for the synthesis of ribosomal RNAs that constitute the protein-synthesizing machinery of the cytoplasm. Oocytes, being the largest cells in the body, also contain an abundance of ribosomes, which are used during the development of the embryo following fertilization.
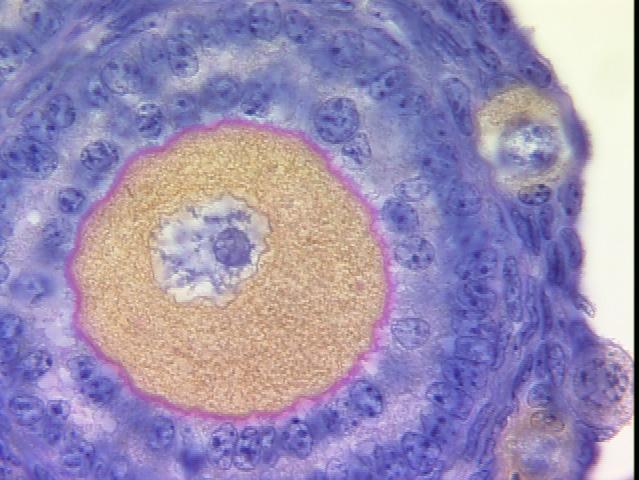
FIGURE 1 shows a section of a small follicle. The oocyte is outlined in pink (surrounded by the zona pellucida). The central nucleus (or GV) has a large blue sphere - the nucleolus. Two small, undeveloped follicles are seen at the image border.
FIGURE II shows a more high-powered view of a GV at the edge of the oocyte and chromosomes, and the nucleolus
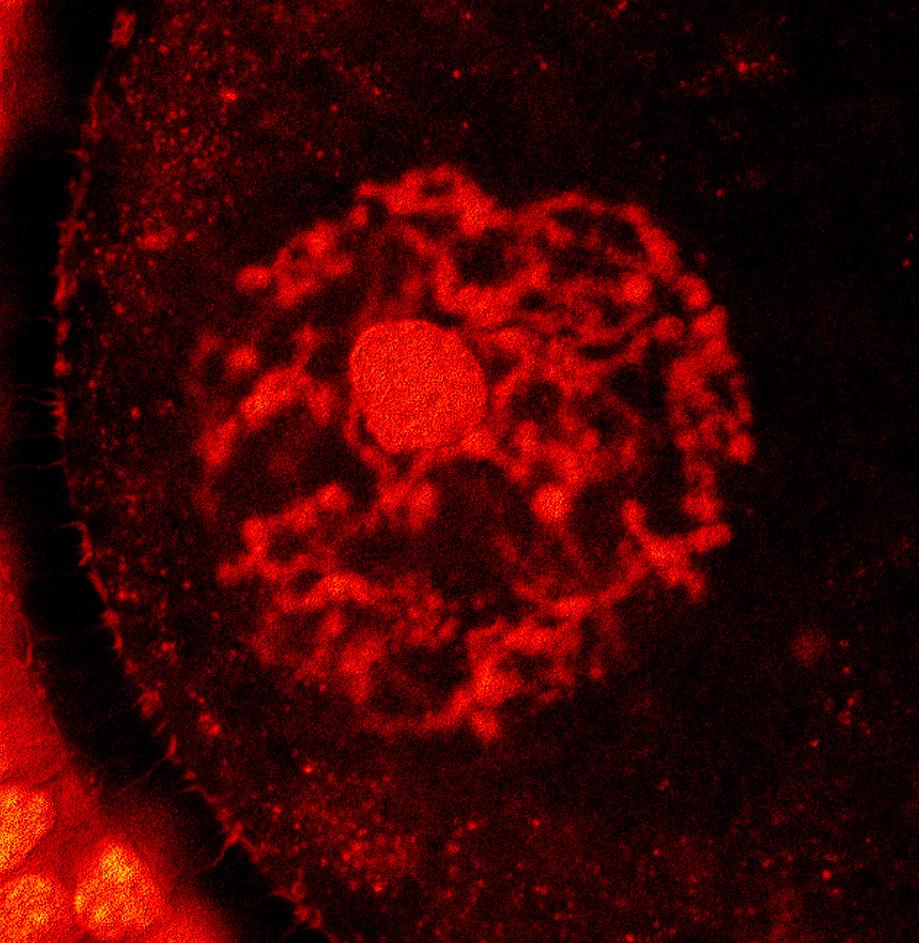
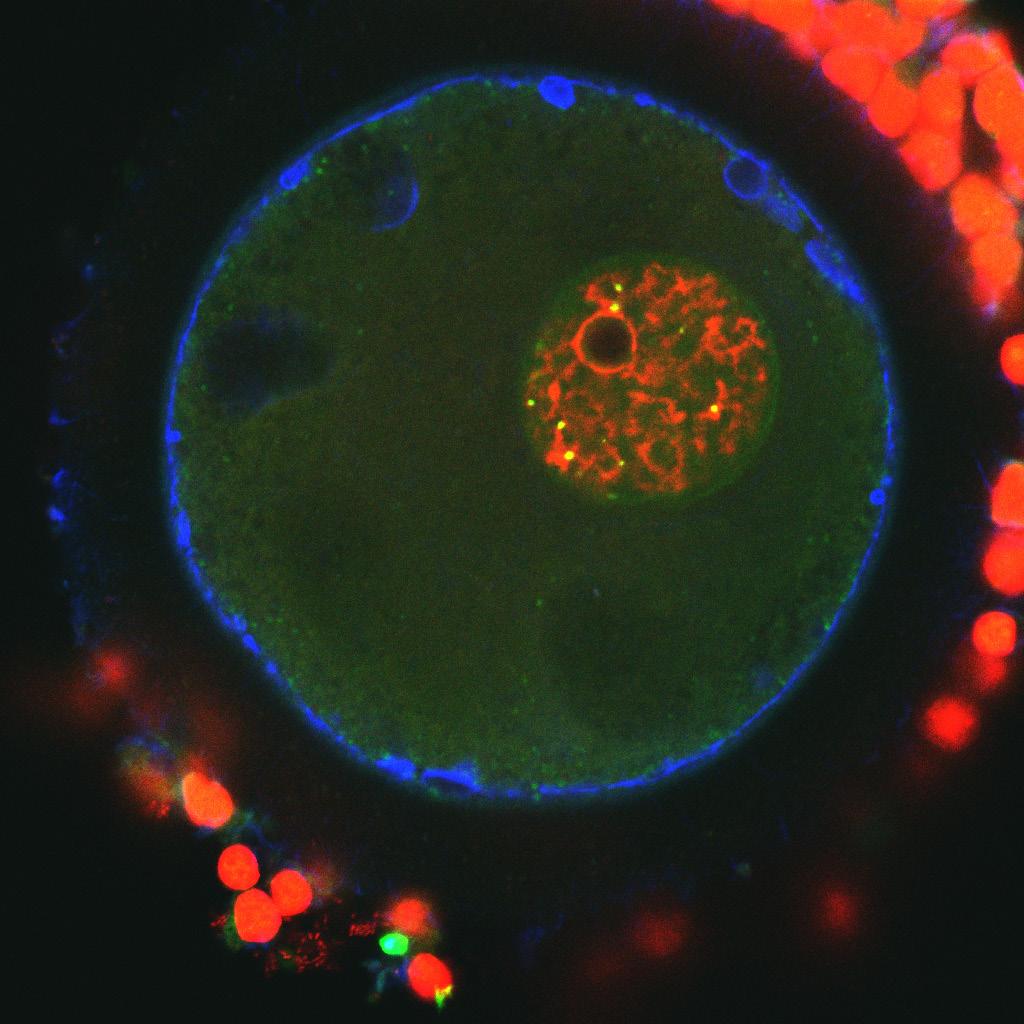
Figure III

FIGURE III illustrates in more detail the central nucleus andnucleolus (GV), including its red chromosomes, some of which encircle the nucleolus
FIGURE IV is a 3-dimensional reconstruction of the entire GV after chromatin (DNA) labeling. The beaded appearance along the length of each chromosome reflects inactivated areas of the genome unable to participate in the process of RNA production (transcription) .
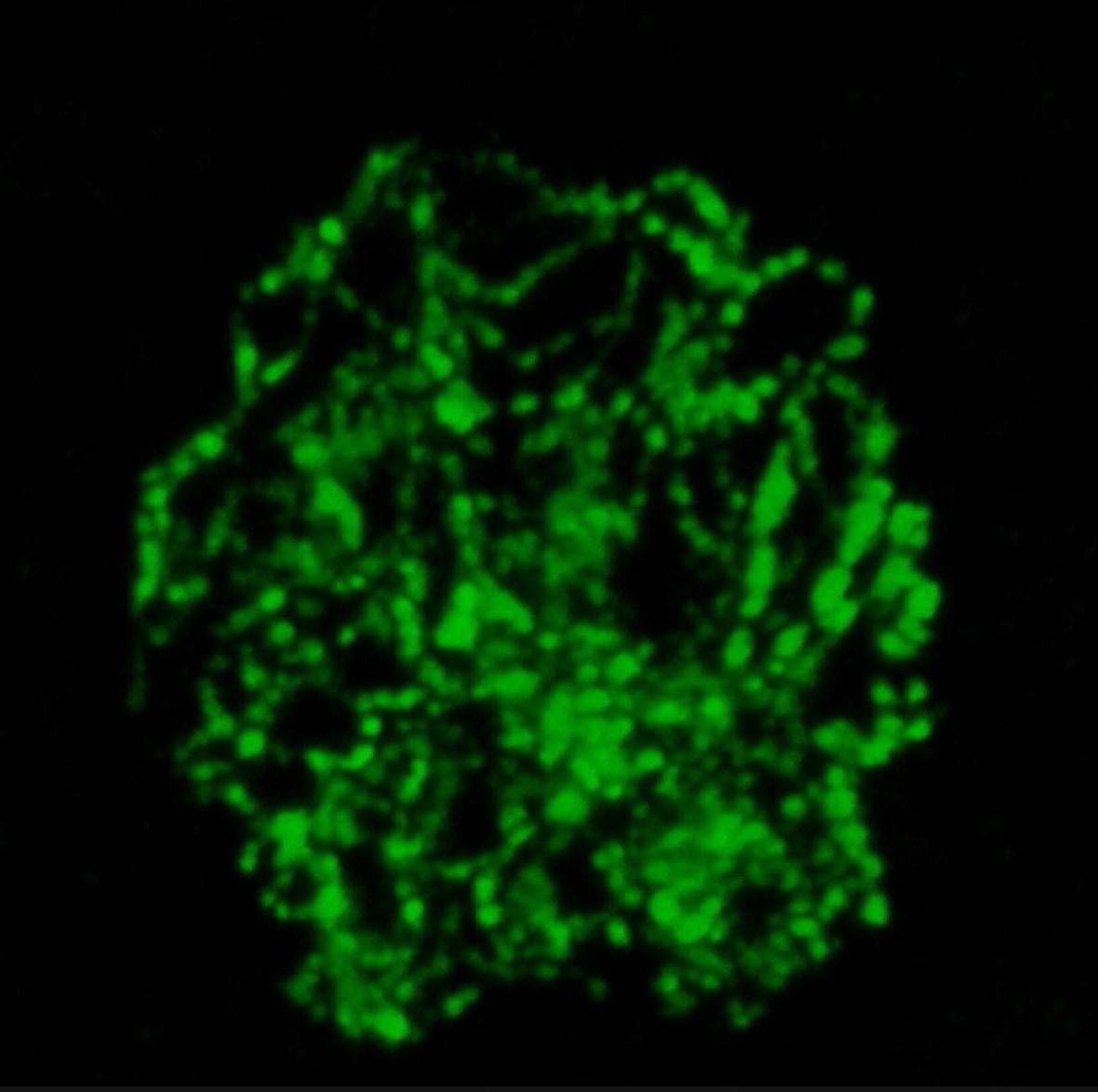
IV

BRIEFING: In this section, the VOICE offers opinions about medical news not necessarily connected to reproductive medicine, but with potential relevance to the field. News more directly about reproductive medicine is reported in a later section of this VOICE . Since, like outside opinions, the CHR’s positions on issues can be biased, it is important to reemphasize that we are fully cognizant that “expert” opinions in medicine are considered the lowest level of evidence and should be viewed as such by our readers. Unable to offer, therefore, consistent “truth” (assuming that something like that really exists in science), the VOICE strives to come in its selection of topics and its content as close as possible to the most likely “truth of the moment.” We, therefore, welcome from our readers, especially opposing opinions.
Direct-to-consumer genetic testing (DTCGT) - much to be concerned
With 23andMe now in bankruptcy, there is a belief among some that the golden days of direct-toconsumer genetic testing are passé, but we don’t think so. Very much to the contrary, we believe that this part of the medical testing market is just getting started. For several reasons, 23andMe, indeed, must be viewed as a bad example for the field: While initially enormously successful (it reached a market valuation as a public company of over $ 1 billion), the interest in this test declined because it, of course, is only a one-time test. The potential client pool, therefore, from day one on, shrank daily. Because the company was aware of this fact, it knew that it had to develop other income sources if it wanted to maintain growth and this is where the company’s leadership misfired: The company’s main shareholder and CEO decided that she wanted 23andMe
to become a pharmaceutical company, speculating that the company’s enormous genetic data base would allow for relatively quick development of new drugs.
Rather unsurprisingly, this, however, turned out to be a somewhat too simplistic business plan, overlooking not only the length of time it takes to develop new drugs, but also the enormous costs of bringing a new drug to market. In other words, had 23andMe followed a different and more realistic business plan, considering the huge cash that drove the company initially, it very likely would still be a thriving and successful enterprise because DTCGT, actually, has captured the imagination of the public.
Consider, for example, the fact that even preimplantation genetic testing of aneuploidy (PGT-A) in association with IVF is in a way a DTCGT. It is, after all, ultimately, the patient who decides whether she wants her embryos tested or not. And commercial PGT-A laboratories and IVF clinics know that very well, – unsurprisingly marketing PGT-A very
aggressively – and not always fully transparently – to consumers.
Within the context of DTCGT, a recent paper offered a systematic review on the subject that is worth noting. Their search identified 40 articles eligible for inclusion published between 2009 and 2022.1 1%-57% of consumers utilizing DTCGTs shared their test results with a health care professional; 19%-76% of health care professionals had experiences with consumers who shared their test results with them. Family members were informed in 18%-98%.
At the same time, considerable concern has been expressed regarding DTCGT and demanding better regulation of such tests,2 a subject especially in the BMJ pursued at least since 2011.3 Yet, even though a test like PGT-A is used daily to determine which human embryos are or are not transferred, has remained practically completely unregulated. Considering the consequences that arise from this test are of such profound lifelong importance to patients, the absence of any form

of regulation of PGT-A by the FDA can only be described as shameful.
And coming back to 23andMe, -that this company has offered predictions of disease risks based on their consumer testing, has worried experts since this reporting started because, unless a disease is determined by a single gene (i.e., in monogenic diseases which are either dominant, recessive, or sex-linked), it is determined in its frequency by the intricate interplay between several (often quite a large number) of genes and predictions (called polygenic risk scoring) becomes very complicated.
By the time of its shutdown, the company offered predictions for 240 health conditions according to a recent article in Nature magazine.4 More specifically, starting with Parkinson's disease and coeliac disease for which the company received initial FDA approval for testing, this number has since grown to 50 diseases. This is at a time when clinical medicine is still struggling with the concept of polygenic disease screening for some of the most common medical conditions.
Unsurprisingly, clinicians have questioned the reliability of the company’s reports.
And, yes, since we above already classified PGT-A as a – in a way – DTCGT, how about polygenic risk screening of human embryos in IVF? That is, of course, in the U.S. also already being offered to consumers by a small number of commercial labs and several U.S. IVF clinics, as recently in detail described in The New York Times in an excellent three-part series of
very personal articles on IVF by Anna Louie Sussman who herself has given birth through the IVF process.5
Somewhat surprisingly, while dedicating almost the complete second part of the article series to polygenic risk screening of embryos, she in the series not even once raised the still increasing utilization of PGT-A which currently has become part of routine IVF in more than half of all U.S. IVF cycles, and that despite that the ASRM (American Society for Reproductive Medicine) and SART (Society for Assisted Reproduction) in late 2024 in a formal statement concluded that PGT-A to this day has in general fertility populations failed to produce any outcome advantages for IVF whatsoever.
And while Sussman very well described the ethical, moral and technical issues of polygenic risk scoring of embryos, she failed to notice in her article series that several major professional organizations – whether fertility related or representing the genetics field – have come out with formal policy statements not only recommending against polygenic risk screening of human embryos but with current knowledge declaring this test performed on human embryos as unethical. And ASRM, according to rumors, is expected to finally (better late than never) come out with a similar condemnation of this test. And not that we believe that such a statement will affect those laboratories and IVF clinics who are offering polygenic risk scoring of embryos already. That can only be achieved by a word from the FDA!
1. Van Steijvoort et al., Open res Europe 2025;5:74
2. Flinter FA. BMJ 2025;388:r14
3. Hauskeller C. BMJ 2011;342:d2317
4. Kwon D. Nature 2025;638:14-15
5. Sussman Al. The New York Times. April 8, 2025. https://www.nytimes. com/2025/04/19/opinion/embryo-ivfbabies.html
Based on media reports, only three Pharmacy Benefits Managers, all controlled by pharma companies, control over 90% of all prescription pricing in the U.S. In other words, Big Pharma sets its own prices and the public, therefore, pays astronomical prices through Medicare (i.e., taxes). Deservedly, a recent posting on X called it “a racket.”1 Here is an example they offered: Initial purchase price for the cancer medication Imatinib is allegedly $7. Their cost to get the medicine out the door is $10, which adds up to $17. Guess how much Medicare pays for it?
The answer is $2,400! Supposedly, the drug was filled 250,000 times in a year, costing Medicare $ 600 million!
1. Wall Street Apes. February 21, 2025. https://x.com/wallstreetapes/

There is, of course, always something to report about the scientific publishing industry, and most, unfortunately, it is often not very positive. So, let’s get going:
Many, if not most, medical journals, in their basic settings, already not very positive against conservative concepts, for very obvious reasons, are not very happy with the Trump administration. Consequently, the editorial team of the JAMA Network found it necessary to “reaffirm the JAMA Network’s commitment to the health of patients and the public.”1 In short, lots of clichés and no really new information.
One is left wondering how one, as the official publishing arm of the American Medical Association (AMA), can be politically so uncritically biased. And we are not even referring to the consistent bias expressed against Trump administration policies, as in the referenced article. The discrimination goes much further because, wherever controversy exists, one uniformly finds only one side of controversial issues being given the opportunity of representation.
And the JAMA Network is, of course, not alone in those biases. We elsewhere in this issue pointed already out many of the biases by even the most prominent and respected journals (like, for example, the Nature journals). It, indeed, is practically almost impossible to find medical journals where one could get the
impression of biases towards the other side. In other words, politics has successfully infiltrated the medical and scientific publishing business, and we are, of course, not the only ones to have noticed. The government seems to have noticed, too.
Recent media reports, indeed, indicate that a federal prosecutor has been sending probing letters to a so-far small number of medical journals accusing them of political bias. Understandably, the response from the medical publishing industry was not very positive. For example, National Public Radio (NPR), just defunded by the Trump administration) interpreted these letters as causing concern that the administration was “trying to restrict free speech among scientists.”2 Among journals that allegedly received such a letter, not surprisingly, was the prestigious New England Journal of Medicine. 3
The projection behind this “fear’ is, however, becoming just as obvious as it has become obvious in daily U.S. politics: Whatever one side accuses the other of doing, one can expect the accusing side to have done for quite some time. That a medical journal like the New England Journal of Medicine would (according to NPR) be concerned about getting censored by the government is absurd, considering the biased article selection that has, of course, been going on at The Journal for decades.
And the JAMA Network appears to follow in the New England Journal’s footsteps and, indeed, to a rather amazing degree when in above cited paper condemning alleged U.S. federal censorship as an attack on science.1 And in another
JAMA article Rochelle Walensky, MD, who served under President Biden as the 19th director of the U. S. Centers for Disease Control and Prevention (CDC), offeredwith her husband as co-author (a pediatric oncologist at Harvard), a not too friendly Viewpoint article claiming that the Trump administration is putting U.S. science in peril.4


Among the layoffs at the CDC, based on decisions made by the Department of Government Efficiency, was, apparently, the entire IVF team responsible for managing the CDC registry and its annual reports.5 Whether this layoff is final is unclear at the time of this writing. Several Democrat senators, indeed, wrote a letter to the Trump administration demanding a reversal of the decision.
And while we agree that firing of the whole IVF crew, likely, was not necessarily a very smart move, things – as they often are – in reality end up being more complex than on first impression: After all, the U.S. currently has two IVF reporting systems in parallel,

- the Congress-mandated CDC reporting system and a system administered by SART. But do we really need two systems (the work for IVF clinics is considerable because both systems at time request different information. Moreover, even though the CDC system is mandated by law, participation is incomplete (going unenforced for decades). Though both systems in a large majority receive information from the same clinics, the data are similar but not completely congruent because, with different clinics in the pool, differences in data analyses are obviously expected.
But it is truly amazing how completely the medical publishing industry, whether privately owned by big publishing companies (i.e., Nature, by Nature-Springer, a German concern) or by notfor-profit, usually professional societies (JAMA by AMA, New England Journal of Medicine by the local Massachusetts Medical Society, Fertility & Sterility by ASRM) have uniformly embraced a leftish outlook on the world, while actively preventing publications that would oppose such an opposing view.
And somewhat related, Nature magazine recently published an interesting news item titled “Journal snatchers buy publications and turn them rogue.”6 What this means is that business interests purchase established journals with the obvious primary intent of improving profitability, and suddenly, previously credible journals begin doing unexpected things, such as accepting poorer-quality papers and, of course, hiking acceptance fees. According to the article, dozens
of formerly credible journals have unfortunately already gone down this route.
1. Bibbins-Domingo, et al. JAMA 2025;333(13):1121-1122
2. Chang A. NPR. May 2, 2025. https://www.npr.org/transcripts/nxs1-5374993#:~:text=A%20federal%20 prosecutor%20has%20been,restrict%20 free%20speech%20among%20scientists.
3. Rosenbluth T. New York Times; April 25, 2025. https://www.nytimes. com/2025/04/25/health/nejm-prosecutorletter.html
4. Walensky R, Walensky LD. JAMA 2025;333(11):933-934
5. McGrath M. Forbes. April 3, 2025. www.forbes.com/sites/ forbestv/2025/04/03/hhs-job-cuts-entirecdc-team-focused-on-infertility-and-ivfis-gone
6. Singh Chawla D. Nature 2025;461;1516
How quickly even social fashions can fade
Not only have big corporate entities been eliminating their diversity programs, but the Trump administration has taken over at a surprising speed. Science magazine recently reported that the Howard Hughes Medical Institute, one of the nation’s largest research philanthropies, has now also followed suit by allegedly “killing its $60 million diversity program.”1 The largest private funder of medical research in the U.S., which has an endowment of almost $26 billion, declined to answer questions from a journalist of Science magazine concerning this decision.
But, considering the January 21, 2025, executive order from the White House, “Encouraging the Private Sector to End Illegal Discrimination [i.e., Diversity, Equity, and Inclusion], even notfor-profit foundations have become concerned about becoming targets for investigations by Donald Trump’s Department of Justice.
1. News. Science 2025;387(6735):702
Are British science and medical journals more woke-prone than their U.S. counterparts? One could think so if one follows Nature journals, - and especially the mothership of all Nature journals,Nature magazine (the BMJ and The Lancet, of course, also have valid claims to being leaders of wokeness in medicine among journals. Nature magazine in one recent issue published back-to-back two articles under the heading “World view” which illustrated this point: Sounding almost like a Bolshevik call to arms and/or revolution, the author of the first suggested that, “if faculty members unite across institutions, they can become a force that the federal government cannot ignore.” And she went on to argue that “higher education establishments must not be bullied into abandoning their mission to promote DEI.”1
A little outdated, we would counter-argue, considering recent developments at colleges and universities in response to the Trump administration’s policy edicts, but certainly not surprising, considering postdocs at many leading universities are unionizing40

or have already unionized.
And then there was the immediately following article by – how appropriate – a political anthropologist, social psychiatrist, and psychoanalytic clinician with apparently no institutional home but – from where else but Chicago, Illinois – who noted that, “there can never be an apolitical approach to public health.”2 Seriously?
This is, of course, a perfectly fine opinion to have and to express. Still, it, once again, sounds more like a call to revolution rather than resolution of (obviously existing) problems when the author further argues that “we must insist upon transforming U.S. health systems, not simply seek to preserved them.” Would the magazine ever consider accepting a hypothesis paper that does not suggest how to proof the hypothesis? We don’t think so, but who says that political opinions really have to have a base in reality?
Political bias by Nature magazine can also be deducted from how it on several occasions in recent weeks and months has commented on prominent appointments by the Trump administration: Take, for example, Jay Bhattacharya, MD, MBA, the new Director of the U.S. National Institutes of Health (NIH) who before that – especially during the COVID-19 pandemic - was a rather lonely voice as a health economist (he is an MD with MBA degree) not only as a professor at the mostly ultra-liberal Stanford University, but practically was declared persona-non-grata by the medical establishment of the country with which he strongly disagreed in how the pandemic was managed. Nature
magazine, in an article before his confirmation, therefore, described him in bold letters “as known for his controversial opinions on COVID-19,” – but failing to point out that almost all of his controversial opinions, in contrast to those from the establishment, turned out to be correct.3
But it, of course, is not only the British journals: The New England Journal of Medicine, quite obviously, is also still longing for a return to the better days of DEI. It even published a Perspective article that “mapped in all 50 states political attacks on DEI in education in their severity,”4 like in preceding Nature magazine, immediately followed by another Perspective article advocating for “sustaining equity efforts in the face of regression.”5
Why is it that both of these very prominent journals see nothing wrong in publishing two consecutive articles with very obvious – we have to say it –political opinions, yet neither of them found it necessary to, maybe, offer at least one contrarian article in the series. In other words, the resistance in academia is alive and well!
1. Calisi Rodriguez. Nature;639:277
2. Reinhart E. Nature 2025;639:278
3. Nowogrodzki J. Nature 2025;639-282283
4. Guerra et al., N Engl J Med 2025;392(10):941-44
5. Wang et al., N Engl J Med 2025;392(10):944-945
While the National Institutes of Health (NIH) are widely known for funding a gigantic extramural research program of $39 billion annually that mostly goes to a small group of major research universities, it is less widely known that the NIH also supports a $5.2 billion intramural research program (representing ca. 12% of the total grant money available to the NIH), through which the agency basically funds its own research and maintains a small research hospital. And, as a recent news article in Science magazine reported,1 this program is – to say it mildly – under stress because contracts of many senior scientists working within this program are not being renewed under the new Trump administration.
Such renewals, as the article notes, used to be basically automatic. Affected scientists, therefore, find themselves suddenly, scientifically as well as financially, under completely unexpected circumstances. Many, because of considerable incentives the agency offered, indeed, left tenured academic positions to join the NIH staff. Those including special pay rules based on a statute called Title 42 which allows the agency to pay higher salaries than the federal pay scale usually allows, - the special intent, of course, being to attract top talent (on a sidenote, this is also how by now infamous Dr. Anthony Fauci became the highest-paid federal employee, even exceeding the salary of the U. S. President).

Many scientists who relocated to the NIH were also attracted by the opportunities this program offered for so-called “blue sky research,” which defines risky research with high stakes but also high rewards if things work out as hoped. To a degree – and unfortunately not addressed in the Science articlethis fact has, however, also been at the core of increasing criticism the intramural NIH program has been facing in recent years: It is now widely considered to have become stale, producing less and less breakthrough discoveries, and basically having become a selfserving funding program for a click of NIH insiders.
The program, therefore, does indeed require a major reorganization. The very supportive Science article for this intramural program of the NIH, therefore, not unsurprisingly, only quoted NIH insiders. Scientists on the outside who routinely compete for NIH funds through the extramural program would probably argue that there is no reason why grants should be awarded to insiders at the NIH under different criteria than outsiders face. A recent Viewpoint article in JAMA also noted that almost two decades have passed since the agency underwent a comprehensive review by Congress.2 It seems time!
REFERENCES
1. Kaiser J. Science 2025;387(6738):1028
2. Walensky R, Walensky LD. JAMA 2025;333(11):933-934
What a stupid question, you may think in reading the heading of this section! How can a brand-new university, in its first year of having accepted students and offering classes in only a very limited number of subjects, be the new Harvard?
But, hold off in declaring us even more insane than you already suspected us to be, we, of course, in no way want to suggest that the University of Austin can in any significant way be compared to Harvard University (just consider Harvard’s $53 billion treasure chest, aside of its history, real estate, etc.). Why we ask this question, and why we strongly believe that the University of Austin, indeed, may be the new Harvard, is neither based on institutional age, history, real estate, or financial acumen, but simply on how these two so hugely different universities see themselves serving students these days.
Historically, the whole world looked toward Harvard (and a handful of other leading universities in the world, of course) as the pioneers and mostly unreachable examples for how higher education should be offered. Today, it is not Harvard (or Columbia University, or Yale, or Oxford, or Cambridge, etc.). It is – yes, already in its first year – the University of Austin in, out of all places, Texas!
First announced in an article by its Founding President, Pano Kanelos, PhD, on November 8,
2021 in an article in The Free Press1 (on a sidenote, Bari Weiss, cofounder of The Free Press, is also a co-founder of the University), he started the article with the following two sentences (and please note that they were written almost exactly two years before the tragic events of October 7, 2023, which became the diagnostic revelation for how severely damaged especially the country’s elite institutions of higher learning are): “So much is broken in America. But higher education might be the most fractured institution of all.”
And he continued: ”There is a gaping chasm between the promise and the reality of higher education. Yale’s motto is Lux et Veritas, light and truth. Harvard proclaims: Veritas. Stanford is told Die Luft der Freiheit weht: The wind of freedom blows. These are soaring words. But in these top schools, and so many others, can we actually claim that the pursuit of truth, once the central purpose of the university – Remains the highest virtue? Do we honestly believe that the crucial means to that end – freedom of inquiry and civil discourse – prevail when illiberalism has become a pervasive feature of campus life?”


And if this is so far not enough to believe us, go to the university’s website,2 where you, for example, will find the following:
DARE TO BUILD. The University of Austin is dedicated to the fearless pursuit of truth.
You will also find the following regarding admission:
Your merit earns you undergraduate admission – and a full-tuition scholarship
And you will find below a quote from Jacob Howland, Provost and Dean of Intellectual Foundations at the University (note the connotations of his institutional title). The Intellectual Foundation program at the university encompasses the first two years of the undergraduate curriculum. Before assuming this position at the University of Austin, he was a Professor of Philosophy at the University of Tulsa, where he especially lectured on Plato, Aristotle, Xenophon, Hegel, and others. He is the son of Bette Lee Howland (1937-2017), a wellknown American write and literary critic who wrote for Commentary Magazine.
“Our students will learn the foundations, blessings, and challenges of a free and prosperous society. They will grasp the importance of law, virtue, order, beauty, and the sacred. They will appreciate the distinct vitality of the American form of government and way of life."

university in 2021, The Texas Tribune described the mission of the university to create a “fiercely independent” school that offers an alternative to what the founders see as a rise in “illiberalism” on college campuses elsewhere.3
And if you are not convinced yet, we suggest you read a recent article by Boris Fishman, BA, in The Free Press (On a side note, The Free Press’s Bari Weiss is one of the founders of the University).
Under the heading, “I’m a Liberal at a ‘Conservative’ University. How Did I End Up here?,” the subheading of his articles notes: “My students know they can disagree passionately with their classmates – a more meaningful definition of ‘safe space’ than what I encountered teaching in the Ivy League.”4
Boris Fishman, BA now teaches

creative writing and literature at the University of Austin, and is the author of several well-received novels.

Already at the time of the initial announcement of the new
With this academic year ending and Harvard’s applications having according to press reports significantly decreased, it will be interesting to see what happened
to acceptance/rejection rates for 2025/2026 at these two universities. As soon as we find out, we will let you know.
1. Kanelos P. The Free Press. November 8, 2021. https://www.thefp.com/p/we-cantwait-for-universities-to 2. https://www.uaustin.org
3. McGee K. Texas Tribune. November 8, 2021.https://www.texastribune. org/2021/11/08/university-austinfounders-college-culture/ 4. Fishman B. The Free Press. March 22, 2025. https://www.thefp.com/p/liberalconservative-university-uatx-borisfishman
Qatar is, to a large degree, behind the explosion of anti-semitism
It seems that everybody by now understands the double game Qatar has been playing in the Middle East since October 7, 2023, and, indeed, long before that date, - that is, except apparently for President Trump and his Middle East (and Russia, Ukraine, and God know for what else) envoy and New York real estate magnate, Steve Witkoff. The Saudis and Emiratis told the world years ago that the Qatari ruling house could not be trusted but nobody listened, not even the Israeli government that allowed Qatar to play a leading role as a “honest” brokers between Israel and Hamas in hostage negotiations, even though they have hosted and financially supported the civilian Hamas leadership in luxury housing for years and, as recently was revealed have encouraged Hamas to reject settlement compromises offered by Egypt and “hold out for better deals.”1
According to the Middle East Forum, Qatari money has also provided Qatar with a “grip on education, causing the explosion of campus antisemitism” seen all around the world.2 To quote from the article: “nothing prepared me for the jaw-dropping moment I experienced while watching a recent Al Jazeera podcast. Khaled Al-Hroub, a professor at Northwestern University in Qatar, spoke (at a recent Al Jazeera podcast) not as an academic but as a mouthpiece for Hamas, painting the terrorist group as a symbol of resilience. His rhetoric was not just disturbing – it was dangerous. This wasn’t an isolated case of radical bias. It was a symptom of a larger, well-funded infiltration by Qatar, which has spent billions to manipulate American academia, indoctrinate students, and turn campuses into breeding grounds for hate.
And more recently, The Free Press published, likely, the most informative article on the subject by Frannie Block and Jay Solomon under the telling title, “How Qatar Bought America,” noting that Qatar – this tiny Gulf nation – “has spent almost $100 billion to establish its influence in Congress, universities, newsrooms, think tanks, and corporations (and this does not even yet include above-noted Boeing plane to be gifted to President Trump).”3 As the article suggests, it seems rather easy to imagine what it wants in return.
1. AllIsrael News. April 28, 2025. https:// allisraelnews.com/qatar-pushed-hamasto-reject-latest-hostage-deal-offer-waitfor-better-proposal-report
2. Ayoub A. Middle East Forum. February 25, 2025. https://www.meforum.
org/mef-online/qatars-grip-on-educationis-causing-an-explosion-of-campusantisemitism
3. Block F, Solomon J. The Free Press. May 13, 2025. https://www.thefp.com/p/ how-qatar-bought-america?utm_ source=substack&utm_medium=email
There is likely no other organ in the human body that is a better model for the study of human aging than the ovary. The principal reason is obvious: It is the one organ in the human body that clearly ages ahead of all other organs and, indeed, at an average age of 52, ceases to function. Like other organs, it – moreover - in ca. 10% of cases ages prematurely and in ca. 1% of women ceases to function before age 40. And it does all of this in contrast to its male counterpart, the testis, which, while certainly aging, still fulfills its reproductive function into very advanced ages, as some male personalities known to everybody these days have well demonstrated (see table).
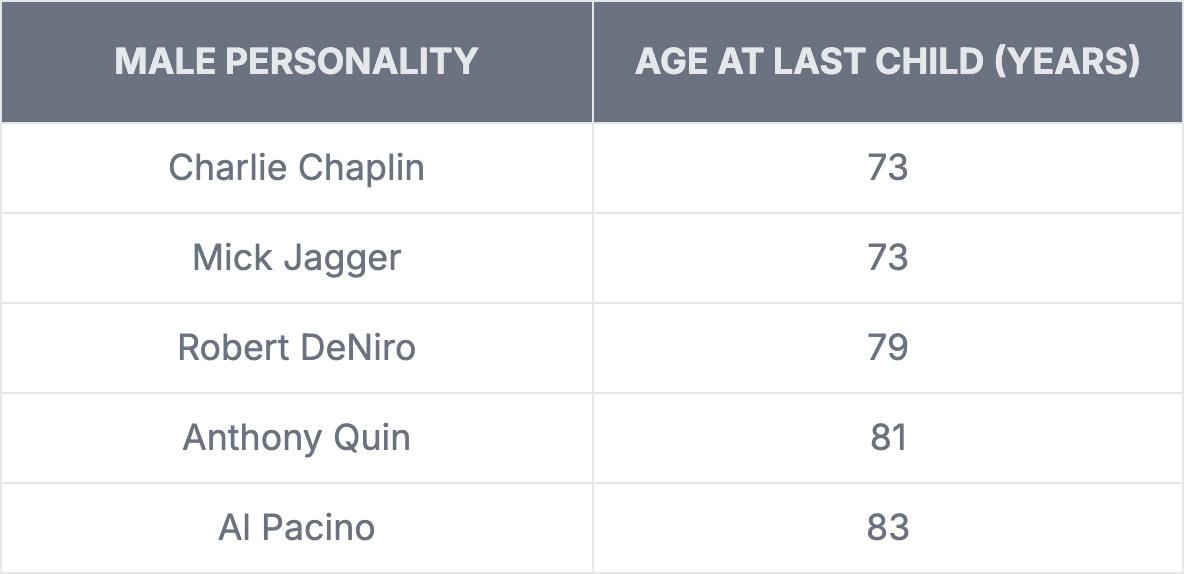
With the ovary, thus, being a very obvious target organ for aging research in general, the opposite is also true: Whatever is discovered in general human aging research may have relevance for ovarian aging. The VOICE, therefore, follows aging research closely.


As JoAnn Manson, MD, DrPH, professor of medicine at Harvard Medical School, recently reported in an article in Medscape OB/ Gyn, 1 this is exactly what a study (COSMOS) presented at the 2025 American Heart Association meeting in New Orleans, suggested. The study attempted in a prospectively randomized trial to answer the question whether daily multivitamin supplementation could slow biological aging, as assessed by DNA methylation in epigenetic clocks of the body.
She also noted in her article that prior studies had already demonstrated similar results. For example, the Physician Health Study II and the 2022 U.S. Preventive Services Task Force Review reported that such vitamin supplementation reduced the incidence of invasive cancers, with the occurrence of cataracts, and with lower memory loss and cognitive decline in three substudies of the COSMO trial. The conclusion that these effects may be the consequence of biological aging, therefore, made sense.
Assessing biological aging using five different epigenetic clocks in the COSMO trial, all five demonstrated signals for slower aging compared to the placebo controls of about 10-20% over two years, reflective of ca. four months of aging. It may be time to start taking a daily multivitamin!
1. Manson J-A, E. Medscape Ob/Gyn. https://www.medscape.com/viewarticle/ multivitamins-slow-biological-aginglarge-trial-2025a10006u7
Steady consumers of this publication by now, of course, know how much we appreciate Eric Topol, MD’s Ground Truths on Substack as a source. Today is no exception because he recently published one of his comprehensive analyses under exactly this title, pointing out the proliferation of several new companies in the consumer space promoting alleged improvement in lifespan, health span, and use of extensive testing to achieve early detection of diseases and/or even prevent diseases.1 The figure to the right from his publication lists some of these companies. And for those among our readers who are interested in even more detail, the table below offers some rather telling details.
His article, as always, of course, offers significantly more detail, and, for those interested in this subject, we, therefore, recommend the following easily available reference on the Internet. While based on a “quick poll,” the interest in the subjects of longevity and health span appears still to be limited (only 13% indicated to have been consumers of one or

more of 10 companies in the marketplace, with 6% claiming to have benefitted and 7% having
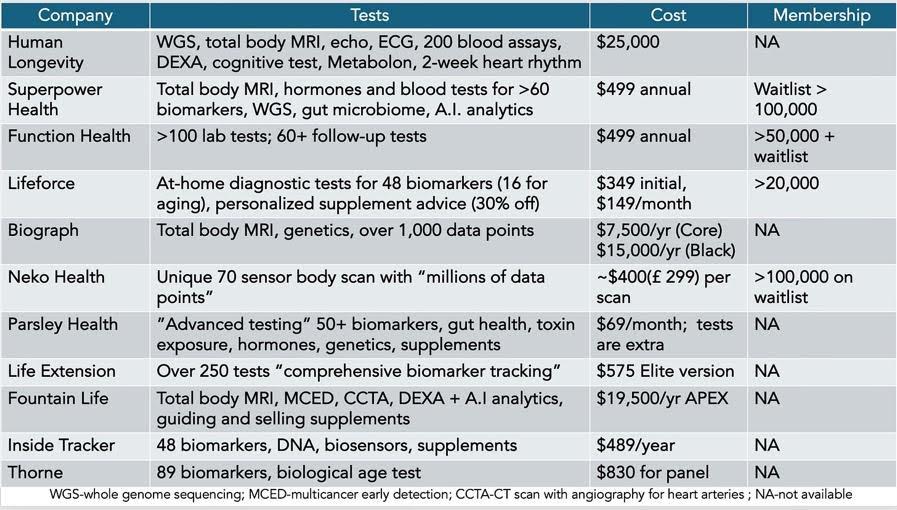

experienced no clear benefit), this, nevertheless, very clearly appears to be a rapidly expanding new “medical specialty area.”
As further expression of our admiration for Topol's new career of having become one of the best –if not the best – translator of new medical science developments for the broader public, here is a plug for his new book, Super Agers: An Evidence-based Approach to Longevity, published on May 6. It lays out an approach to the primary prevention of the three principal age-related diseases, cancer, cardiovascular conditions, and neurodegenerative disorders, as artificial intelligence (AI) can now determine who is vulnerable to one of these conditions and at what age they will likely manifest themselves. Early risk, then, is of course much more concerning than later risk and will undoubtedly become the target of new treatment efforts.
And related, Heidi Leford, a writer for Nature magazine, in a much shorter piece basically addressed the same subject by pointing out that, “armed with an influx of cash and public enthusiasm, researchers are now looking to improve how aging is measured.”2 The hype currently surrounding aging research, according to the article, however does not always reflect how controversial the concept of measuring aging has remained.
Above-noted so-called epigenetic clocks have been used in by now innumerable studies of different organs, but, as one scientist interviewed by her noted, they typically have so far not been sufficiently validated to be useful in clinical trials. What
her article, however, even more clearly lays bare is that to this day really no agreement on what these markers are supposed to measure: A survey of participants at a scientific conference on aging revealed that approximately 30% defined aging as “loss of function over time.” Others, however, defined aging as “accumulation of damage with time; yet others as a “developmental stage,” and yet others as “an increase in disability and death.
1. Topol E. Ground Truths. March 22, 2025. https://erictopol.substack.com/p/ the-business-of-promoting-longevity
2. Ledford H. Nature 2025;638:875-876
When really does human consciousness arise?
This was the question addressed at a gathering of scientists at the recent Infant Consciousness Conference at New York University (NYU). As Kelly Servick reported in a short article in Science magazine,¹ this is, of course, a rather complicated — and especially these days, a very controversial — issue, not least because how consciousness is defined is, in itself, still a subject of debate.1 Unsurprisingly, the meeting, therefore, did not offer a simple answer. A survey of participants suggested that many (47%) considered the idea of fetal consciousness “compelling” between weeks 24 and birth; the early postnatal period until ca. 6 months was second with 13%, and a somewhat surprising 10% selected the early prenatal period before 24 weeks gestational age.
This question, of course, has relevance to the abortion debate
but also bears upon premature deliveries and their care in NICUs. Within this discussion maybe the so-far most important conclusion from this debate was expressed by one of the participating scientists, who noted that “any firm pronouncement that the fetus feels intense pain starting at a certain gestational week is doing a disservice to science because it is putting an absolute where there just isn’t one.”
1. Servick K. Science 2025;387(6739):1132-1133
This is what a recent article in The Wall Street Journal adapted from a recently published book in the U.K. by a British neurologist suggested when pointing out that “the rise in diagnoses for everything, from autism to ADHD (and many other conditions), may be doing more harm than good.1 Considering the recently resurfaced debate regarding spiking autism rates with the appointment of Robert F. Kennedy Jr. as Secretary of the Department of Health and Human Services (HHS), this question, of course, achieved further relevance.

That symptoms may be psychosomatic, rather than indicators of a physical disease, or only extremes of the normal range, has been, of course, known since even before Freud. But that things have been further deteriorating because of Internet-driven selfdiagnoses, and often non-medical sources have by now also become indisputable, raising the question whether we all may not be slowly turning into hypochondriacs from all the unnecessary testing we are doing.
1. O’Sullivan S. The Wall Street Journal., March 17, 2025. https://www.wsj.com/ health/healthcare/we-are-turning-toomany-people-into-medical-patientsad46ea33 (in print March 22-23, 2025)
That life birth rates are declining in most parts of the world is by now well documented. But birth trends also reveal other interesting changes. One that recently attracted considerable attention in the media was the fact that, according to data from the CDC, more women above age 40 recently gave birth than teens.1 This development attracted so much media attention because it reflects major trends in U.S. delivery rates, declining teen pregnancy rates, and increasing pregnancy and delivery rates in older women. Birthrates in women over age 40 have jumped 193% since 1990 (from 1.2% of all births to 4.1%). Women under age 30 in 1990 reflected 69.8% of all births, but by 2023, only 48.6%. In contrast, women over age 30 in

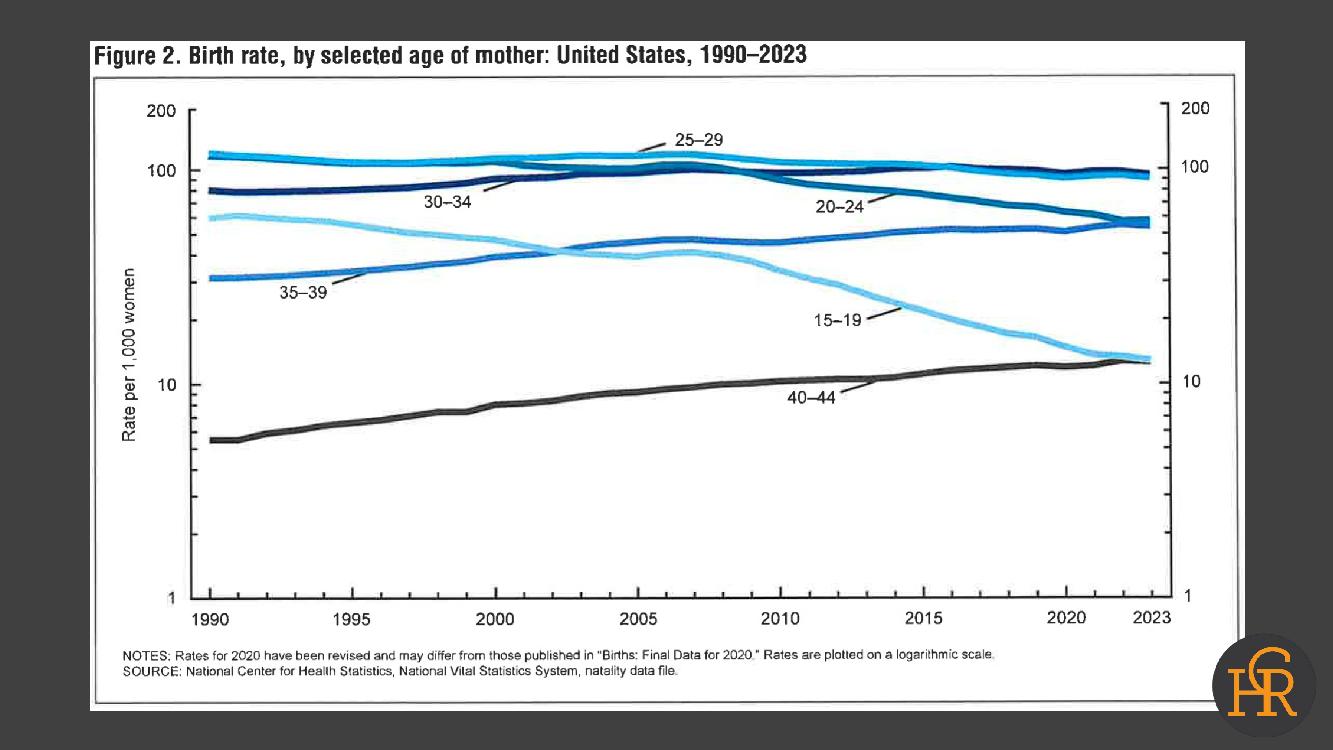
Both of the above figures represent the newest data from the National Center for Health Statistics. The figure on the top demonstrates that birth rates since approximately 2010 have been steadily declining. The bottom figure demonstrates that the declines are restricted to women above age 35. Women aged 35-39 and women aged 40 and above, in contrast, have been increasing in the number of deliveries.
1990 accounted for only 30% of all births, while by 2023 they represented 51.4%. Delaying childbirth, thus, does not only involve older women but really women of all ages. These observations are, of course, of major societal importance, but, maybe even more importantly, the report also demonstrated that the U.S., since ca. 2010, has produced overall birth rates below replacement levels. This means that, in the absence of immigration to the U.S. from other countries, the U.S. population could have shrunk, a development by now common to many major countries in the world which lack the immigration patterns of the U.S., which of course, carries with it

very negative economic connotations for affected countries. Related, it is also worthwhile noting that a recent TikTok video gathered a whopping 1.3 million views. Why does it relate? Because a couple with kids at ages 27, 21, 19, and 15 announced that “they were pregnant again,” and it generated lots of discussion (and controversy) about motherhood late in life.2
1. Driscoll AK, Hamilton BE. Nat Vital Stat Reports 2025;74(3):1-10
2. Tenety E. Mother. Updated December 10, 2024. https://www.mother.ly/news/ viral-tiktok-pregnancy-announcement/

How often are children genetically unrelated to their alleged father?
This is, of course, a question contemplated over centuries, if not millennia, but – interestingly – only exceedingly rarely subject to scientific curiosity. It was, therefore, refreshing to see that Science magazine had no problem in addressing this issue in a recent feature article by Andrew Cury, spending, indeed, four full pages on the subject.1 We, of course, don’t have the space for so much detail; but here is the essence: As it turns out, a Belgian gentleman by the name Werner van Beethoven was disappointed to find out that he was not – as his family had assumed over generations –genetically related to the famous 18th century composer Ludwig van Beethoven.
at KU Leuven, Belgium) who had developed a rather unusual research interest, - combining genetic and genealogical data, primarily in an effort to determine how often women have children with men they are not partnered with or as he named this circumstance, - “extra-pair paternity (EEP).”2

What the likely percentage might be has, as Cury called it in his article, been subject to “zombie statistics,” suggesting that as many as ca. 10% of all births were affected. What Larmuseau’s research, however, suggested is that this number appears highly exaggerated and, indeed, was also quite variable over historical times, while also differing depending on where people were living (i.e., city living, for example, increased the percentages).
How can geneticists retrospectively assess whether, generations apart, two men are genetically related? That is, indeed, easier done than one would expect because Y chromosomes are passed unchanged from father to son. This means that male descendants over generations share their Y chromosome. When Werner van Beethoven, therefore, did not demonstrate the same Y chromosome as Ludwig van Beethoven, Larmuseau had to offer the disappointing, but biologically very obvious truth to the contemporary Beethoven family in Belgium that they, genetically, were not related to Ludwig van Beethoven, as they for generations had believed.
1. Curry A. Science 2025;387(6738:103— 1034
2. Larmuseau et al., Current Biology 2019;29(23): P4102-4107.E7
Almost everybody, by now, of course, probably knows that one can become addicted to many things, starting, of course, with drugs, alcohol, smoking, gambling, and – yes - sex; but who knew that one can also become addicted to shopping?
The person responsible for smashing the family’s long held assumptions was a Belgian genetic genealog by the name Maarten H. D. Larmuseau (Professor in Human Genetic Genealogy
In a 2019 study, Larmuseau et al. reported that estimated EPP rates among married couples varied between 0.4% to 5.9% and peaked among families with a low socioeconomic background living in densely populated cities of the late 19th century.2 In Europe, EEP, overall, appeared closer to 1%.1
But this is exactly what a recent feature article by Emma Marris in Nature magazine scientifically exquisitely described1. From China to Brazil and Germany, a surge of people have become addicted to shopping, in part driven into their addictions by companies using gaming strategies to hook people. And, as the article somewhat surprisingly also noted, - that one

can get addicted to shopping has been known already since 1899, when the German psychiatrist Dr. Emil Wilhelm Georg Magnus Kraepelin (1856-1926), the father of psychopharmacology, described what he in German called “krankhafte Kauflust” (translated as “diseased addiction to buying”).

As the Nature article, however, in addition noted, experts now worry that this problem has been getting increasingly worrisome because of the rise of e-commerce through companies like Amazon, Shein, and Temu, which use game-like strategies to sell items. Concerns even reached the European Commission, which started an investigation of Temu, likely the most active e-commerce company in using gaming strategies.
Countries where, according to the article, compulsive shopping has been documented by researchers include the U.S., Turkey, Poland, Germany, India, Brazil, South Korea, and Pakistan. Pakistan identified almost one-third of university students as compulsive buyers, both online and in retail situations. The problem appears most pronounced in China, where allegedly 29.1% of the general
population is already compulsive shoppers.
Though not yet recognized as an addiction by the International Classification of Diseases (JAMA) and the Diagnostic and Statistical Manual of Mental Disorders (DSM), brain studies have demonstrated similar patterns to gambling addiction (i.e., an addiction within the broader category of behavioral addictions). A scientist is quoted to have commenting, “the dopaminergic reward system is on fire.” A group of experts in 2021 agreed on the term “compulsive buying disorder” for this condition. Like drug and alcohol addictions, shopping addiction appears to be a spectrum disorder, with some people being only mildly affected while others end up with a severe addiction.
How to treat the condition is still undefined, but – so far – cognitive behavioral therapy has been the main approach. As the article also notes, addicts, thus, are mostly left to their ways, with communities being established of people with shopping problems, which congregate on social network platforms like Reddit.
1. Marris E. Nature 2025;639:26-28
If you ever wondered whether physicians and/or other health care providers in any way benefit medically from being providers in medicine, a recent paper in JAMA Internal Medicine offered
some answers.1 In a populationbased cross-sectional study of 3,606,791 U.S. individuals at ages 25 to 74 years, age-adjusted and sex-adjusted mortality rates per 100,000 were, indeed, lower for most health care workers compared with non–health care workers.
Looking at the numbers in a little more detail, as expected, females had overall lower mortality rates than males in non–health care occupations (male-to-female rate ratio, 0.55). Several health care occupations, including physicians, however, did not demonstrate such a female advantage. Black workers had the highest mortality rates across all occupations. The largest disparity between Black and White individuals was, however, observed among physicians (Black to White rate ratio, 2.13), mostly due to cancers, heart disease, and COVID-19. Black female physicians had higher mortality rates than all other physician subgroups and White female individuals in non–health care occupations. Hispanic workers had, however, lower overall mortality than White workers in non–health care occupations, and in high-income non-health care occupations specifically, this pattern was reversed for several health care occupations, including physicians.
Too bad, however, that this very interesting paper in its conclusions then had only platitudes to when noting that, “the results of this cross-sectional study suggest that, although physicians and most health care workers experienced lower mortality rates compared with the general population, this benefit did not fully extend to

female individuals or racial and ethnic minority groups. Renewed efforts are needed to address health inequities within the health care workforce.”
Though this conclusion, in principle, is not incorrect, it, in its political correctness, is overlooking what, likely, represents the by-far most interesting finding of the study, and that is the fact that the White-Black difference in mortality was the most significant among physicians. We would argue that – at least in the degree of this difference – this is a very unexpected finding, which –frankly – is difficult to explain because why would the difference be so much bigger among the best educated and economically most favorable medical workers (i.e., physicians)?
If we want to better understand the inequality in health outcomes between Black and White populations (and other races), this is probably a much more important question to address than the cliché statement the authors chose when suggesting a need for “targeted interventions to address health inequities within the health care workforce.” For physicians, the finding that their Black colleagues have a much higher mortality should offer an overwhelming motivation to find out what the underlying reasons may be.
On a side note, the literature also convincingly demonstrates that IVF cycles in Black women, after all routine adjustments for known co-variables, produce significantly lower pregnancy and live birth rates than in Asian and especially Caucasian populations (the difference compared to
Caucasian women was ca. 30%).2 CHR investigators suggested several years ago that this may be the consequence of differences in CGG repeat patterns in the FMR1 gene between the races.3 But a uniformly accepted explanation for these discrepancies has not been achieved yet.
1. Patel et al., JAMA Intern Med 2025; 2025; doi:10.1001/ jamainternmed.2024.8432. Online ahead of print.
2. Ghidei et l., F&S reports 2021;3(2Suppl):14-21
3. Kushnir et al., PLoS ONE 2014.9(7):e102274
Now, detransitioning individuals are also starting to speak up
Increasing numbers of adults who transitioned in childhood have, in recent months, started to speak out after deciding to detransition. They report on chilling mental health (and other) health effects, especially among those who underwent “gender affirming” surgery.
Regrettably, they received only very limited coverage from mainstream media in the U.S., and reports about these individuals almost exclusively come from a small number of independent news outlets like The Free Press and The New York Sun, and from media outlets on the political right.1 The silence of the U.S.
medical establishment and most media regarding this subject is, indeed, deafening, especially when it comes to gender affirming treatments for children and teenagers.
This, of course, stands in stark contrast to many European countries and especially the U.K., where publication of the Cass Review in 2024 really got the ball rolling, as we have since then repeatedly addressed in the VOICE And, as The Atlantic previously suggested after the Cass Review, 2 the U.K. is continuing to “leave the U.S. gender medicine debate behind” by now announcing a first large-scale landmark study on the effects of puberty blockers on children with gender distress.3
As this recent article in The Sun noted, the stakes of this hotly anticipated clinical trial have now only heightened, as the incoming Trump administration – like most of European countries – based on the Cass Review consider the issue settled and do not allow gender transition treatments of children and young adults until mostly age 22 which, basically, also prohibits any further studies (as we noted in the prior VOICE, New York State Attorney, Letitia James, warned New York hospitals from following the Trump administration's presidential order to this effect!). Unsurprisingly, the NIH, therefore, also “killed” existing grants on transgender issues, as Science magazine recently reported.4
More surprising is the continued support for gender-affirming treatment of children by the medical establishment in the U.S., as once again well demonstrated by yet another

passive-aggressive Viewpoint article in JAMA, 5 the official principal journal of the American Medical Association (AMA), criticizing current restrictions of such treatments. The AMA once used to be a conservative professional organization, but now, in its “politics,” has become indistinguishable from other leading liberal medical journals, like The New England Journal of Medicine, The British Medical Journal (BMJ), or The Lancet. We do not recall even a single article in defense of the Cass Review - a three-year effort by the prior president of the British Academy of Pediatrics, in any of these journals, though all of them have repeatedly offered their pages to criticism of the Cass Review.
What makes the very obvious bias regarding this subject from the U.S. medical establishment even more obvious, is the very recent publication of a “Review of Evidence and Best Practice” from the Department of Health and Human Services (HHS) on May 1, 2025, under the title “Treatment for Pediatric Gender Dysphoria,” which the HHS published “against the backdrop of growing international concern about pediatric medical transition.”6 More on this extremely detailed report in a moment, but first, another example of the amazing support aggressive treatment for pediatric gender dysphoria is still receiving from at least important political groups within the medical establishment.
Unsurprisingly, the report –immediately after its release – received criticism from especially political liberal sources, well summarized in an article
by Lindsey Dawson in KFF (formerly known as the Kaiser Family Foundation – therefore obviously defining its political leanings toward the left side of the political spectrum, - but now no longer connected to the Kaiser Permanente and, therefore, only called KFF. It describes itself on its website as an endowed notfor-profit and as “the leading health policy organization in the U.S., with the scope and reach to be a counterweight to health care’s vested interests and a voice for people.”7 Tellingly, Dawson is KKF’s Associate Director of HIV Policy and Director of LGBTQ Health Policy. Of course, no political bias here!
And, apropos, though she claimed that the HHS review “immediately after its release received criticism from researchers, advocates, and medical associations for its methods, lack of alignment with current guidance, promotion of misinformation, support of certain practices, and decision not to disclose the authors, the document received significantly more laudatory comments than criticisms. Further documenting her very obvious bias, most of her article addressed only “conversion practices.” Unsurprisingly, The New York Times, of course, also expressed considerable skepticism regarding the HHS report, though one cannot argue with one point that The Times, as well as Dawson’s article, made: namely, that the authors of the report were not identified, “pending a postpublication review process that would begin in the coming days.”
Considering President Trump had in January issued an executive order (“Protecting Children
from Chemical and Surgical Mutilation”) that mandated a report on the subject from HHS within 90 days, it almost sounds like HHS relied on ChatGPT or another AI service to issue the report. After all, the initial review of this subject that radically changed opinions – the so-called Cass Review in the U.K. – took three years to produce.9
But we wanted our readers to decide on their own and, therefore, offer here an unedited reprint of the Executive Summary of the HHS report.6 It speaks for itself and, to a significant degree, also reflects the conclusions of the Cass Review.
• Gender dysphoria is a condition that involves distress regarding one’s sexed body and/or associated social expectations. Increasing numbers of children and adolescents in the U.S. and other countries are diagnosed with gender dysphoria. Internationally, there is intense disagreement about how best to help them.
• The term “rapid onset gender dysphoria” (ROGD) has been suggested to describe a new clinical presentation of gender dysphoria. Despite sharp disagreement about the concept’s validity, symptoms consistent with ROGD have been recorded in clinics in the U.S. and other countries.

• In the U.S., the current approach to treating pediatric gender dysphoria aligns with the “gender-affirming” model of care recommended by the World Professional Association for Transgender Health (WPATH). This model emphasizes the use of puberty blockers and cross-sex hormones, as well as surgeries, and casts suspicion on psychotherapeutic approaches for the management of gender dysphoria.
• The understandable desire to avoid language that may cause discomfort to patients has, in some cases, given rise to modes of communication that lack scientific grounding, that presuppose answers to unresolved ethical controversies, and that risk misleading patients and families. This Review uses scientifically accurate and neutral terminology throughout.
• In many areas of medicine, treatments are first established as safe and effective in adults before being extended to pediatric populations. In this case, however, the opposite occurred: clinician-researchers developed the pediatric medical transition protocol in response to disappointing psychosocial outcomes in adults who underwent medical transition.13
• The protocols were adopted internationally before the publication of the first outcome studies. In recent years, in response to dramatic shifts in the number and clinical
profiles of minor patients, as well as to multiple systematic reviews of evidence, health authorities in an increasing number of countries have restricted access to puberty blockers and cross-sex hormones, and, in the rare cases where they were offered, surgeries for minors. These authorities now recommend psychosocial approaches, rather than hormonal or surgical interventions, as the primary treatment.
• There is currently no international consensus about best practices for the care of children and adolescents with gender dysphoria.
• Evidence-based medicine is widely recognized by health authorities worldwide as the foundation of highquality care. Consistent with its principles, this Review undertook a methodologically rigorous assessment of the evidence underpinning pediatric gender medicine.
• Specifically, this Review conducted an overview of systematic reviews—also known as an “umbrella review”—to evaluate the direct evidence regarding the benefits and harms of treatment for children and adolescents with gender dysphoria. Existing systematic reviews of evidence, including several that have informed health authorities in Europe, were assessed for methodological quality. The umbrella review found that the overall quality of evidence concerning the effects of any
intervention on psychological outcomes, quality of life, regret, or long-term health is very low. This indicates that the beneficial effects reported in the literature are likely to differ substantially from the true effects of the interventions.
• Evidence for harms associated with pediatric medical transition in systematic reviews is also sparse, but this finding should be interpreted with caution. Inadequate harm detection in pediatric gender medicine may reflect the relatively short period of time since the widespread adoption of the medical/ surgical 14 treatment model; the failure of existing studies to systematically track and report harms; and publication bias. Despite the lack of robust evidence from populationlevel studies, important insights can be drawn from established knowledge about human physiology and the effects and mechanisms of the pharmacological agents used.
• The risks of pediatric medical transition include infertility/ sterility, sexual dysfunction, impaired bone density accrual, adverse cognitive impacts, cardiovascular disease and metabolic disorders, psychiatric disorders, surgical complications, and regret.
• In the U.S., the most influential clinical guidelines for the treatment of pediatric gender dysphoria are published by WPATH and the Endocrine Society. A recent systematic

of international guideline quality did not recommend either guideline for clinical use after determining they “lack developmental rigor and transparency.”
• Problems with the development of WPATH’s Standards of Care, Version 8 (SOC8) extend beyond those identified in the systematic review of international guidelines. In the process of developing SOC-8, WPATH suppressed systematic reviews its leaders believed would undermine its favored treatment approach. SOC8 developers also violated conflict of interest management requirements and eliminated nearly all recommended age minimums for medical and surgical interventions in response to political pressures.
• Although SOC-8 relaxed the eligibility criteria for access to puberty blockers, crosssex hormones, and surgeries, there is compelling evidence that U.S. gender clinics are not adhering even to those more permissive criteria.
• The “gender-affirming” model of care, as practiced in U.S. clinics, is characterized by a child-led process in which comprehensive mental health assessments are often minimized or omitted, and the patient’s “embodiment goals” serve as the primary guide for treatment decisions. In some of the nation’s 15 leading pediatric gender clinics, assessments are conducted in a single session lasting two hours.
• The voices of whistleblowers and detransitioners have played a critical role in drawing public attention to the risks and harms associated with pediatric medical transition. Their concerns have been discounted, dismissed, or ignored by prominent advocates and practitioners of pediatric medical transition.
• U.S. medical associations played a key role in creating a perception that there is professional consensus in support of pediatric medical transition. This apparent consensus, however, is driven primarily by a small number of specialized committees, influenced by WPATH. It is not clear that the official views of these associations are shared by the wider medical community, or even by most of their members. There is evidence that some medical and mental health associations have suppressed dissent and stifled debate about this issue among their members.
• The principle of autonomy in medicine establishes a moral and legal right of competent patients to refuse any medical intervention. However, there is no corollary right to receive interventions that are not beneficial. Respect for patient autonomy does not negate clinicians’ professional and ethical obligation to protect and promote their patients’ health.
• The evidence for the benefit of pediatric medical
transition is very uncertain, while the evidence for harm is less uncertain. When medical interventions pose unnecessary, disproportionate risks of harm, healthcare providers should refuse to offer them even when they are preferred, requested, or demanded by patients. Failure to do so increases the risk of iatrogenic harm and reduces medicine to consumerism, threatening the integrity of the profession and undermining trust in medical authority.
• Proponents of pediatric medical transition claim that regret is vanishingly rare, while critics assert that regret is increasingly common. The true rate of regret is 16, not known, and better data collection is needed. That some patients report profound regret after undergoing invasive, lifechanging medical interventions is clearly of importance. However, regret alone (just like satisfaction alone) is not a valid indicator of whether an intervention is medically justified. Patients may regret medically justified treatments or feel satisfied with unjustified ones.
• A natural response to the absence of credible evidence is to call for more and better research. Even if high-quality research, such as randomized controlled trials on pubertal suppression or hormone therapy, were feasible, however, conducting it may conflict with well-established ethical standards for human subjects research.
• The rise in youth gender dysphoria and the corresponding demand for medical interventions have occurred against the backdrop of a broader mental health crisis affecting adolescents. The relationship between these two phenomena remains a subject of scientific controversy.
• Suicidal ideation and behavior are independently associated with comorbidities common among children and adolescents diagnosed with gender dysphoria. Suicidal ideation and behavior have known psychotherapeutic management strategies. No independent association between gender dysphoria and suicidality has been found, and there is no evidence that pediatric medical transition reduces the incidence of suicide, which remains, fortunately, very low.
• There is a dearth of research on psychotherapeutic approaches to managing gender dysphoria in children and adolescents. This is due in part to the mischaracterization of such approaches as “conversion therapy.” A more robust evidence base supports psychotherapeutic approaches to managing common comorbid mental health conditions. Psychotherapy is a noninvasive alternative to endocrine and surgical interventions for the treatment of pediatric gender dysphoria. Systematic reviews of evidence have found no evidence of adverse effects of psychotherapy in this context.
1. Curl J, New York Sun. March 7, 2025. https://www.nysun.com/article/ study-reveals-chilling-mental-healthside-effects-among-patients-undergoinggender-affirming-surgery
2. Lewis H. The Atlantic. April 12, 2024. https://www.theatlantic.com/ideas/ archive/2024/04/cass-report-youthgender-medicine/678031/
3. Ryan B. New York Sun, March 18, 2025. https://www.nysun.com/article/ uk-plans-landmark-study-on-pubertyblockers-effect-on-children-with-genderdistress-critics-express-doubt-it-willadvance-the-weak-evidence-base
4. Reardon S. Science 2025;387(6739(:1136
5. Gorin et al., JAMA 2025;333(10):841842
6. Department of Health and Human Services. May 1, 2025. https://opa.hhs. gov/sites/default/files/2025-05/genderdysphoria-report.pdf
7. Dawson L. KFF. May 6, 2025. https://www.kff.org/mental-health/ issue-brief/u-s-department-of-healthand-human-services-report-onpediatric-gender-dysphoria-and-genderconversion-efforts/#:~:text=On%20 May%201%2C%202025%2C%20 the,Secretary%20to%20publish%20an%20 evidence
8. Ghorayshi A, Harmon A. The New York Times. May 1, 2025, https://www. nytimes.com/2025/05/01/health/federalreport-denounces-gender-treatments-foradolescents.html
9. Cass H. https://webarchive. nationalarchives.gov.uk/ ukgwa/20250310143933/https:// cass.independent-review.uk/home/ publications/final-report/
We have previously discussed in these pages rising concerns about rapidly growing numbers of paper retractions in even very prominent medical and science journals. No wonder, then, that the publishing world has suddenly started to pay more attention to the subject. Here
are a few interesting papers that caught our eye: A news article in Nature magazine, for example, reported that many highly cited scientists also have retractions.1 And, interestingly, researchers with retractions (coincidentally ??) also had higher self-citation rates and published more papers.1
One, of course, can interpret these findings in different ways: A benign interpretation would be that more papers allow for more errors. In other words, before accusing somebody of being an unreliable and/or superficial (if not even fraudulent) researcher, shouldn’t we adjust the statistics for the number of publications of an author?
On the other hand, Jackson Ryan reports that more than 8,000 of the most cited researchers in the world (not only including medical researchers) were recently reported to have at least one retraction.1 The study headed up by one of the, currently, best known epidemiologists with a longstanding interest inin publication fraud, Stanford University’s John P.A. Ioannidis, MD, Professor of Medicine/Health Research & Policy/Biomedical


Data Science/Statistics, split most cited scientists into two groups, 217,097 cited in their field in the top 2% over their careers, and a second group of 223,152 scientists who represented the top 2% for citation impact in 2023. As it turned out, 4% of the most highly cited authors had at least one retraction. In comparison, those most cited over their careers had retractions in 3.3%, and – surprise, surprise – retractions were the highest in India, the Chinese mainland, and Taiwan, and the lowest in Finland, Belgium, and Israel.3
The article quotes a neuropsychologist with an interest in scientific integrity research as

correctly stating that this study provided only weak circumstantial evidence that the paper's described findings reflect “a real issue.” But, at the same time, one can also not argue with another quote cited by Ryan in the article: “We should look carefully at authors with high citation rates, and not just assume they are great researchers.” We couldn’t agree more!
And somewhat related, Nature magazine recently published an
interesting News item under the heading, “Journal snatchers” buy publication and turn them rogue.”4
1. Ryan J. Nature 2025;638:306-307
2. Ioannidis JPA., PLoS Biol 2025;23,e30029999
3. Van Noorden R. Nature 2025;638:596599
It, of course, is not enough just to publish a paper; academia also judges the paper by how frequently other papers cite it. And here, Nature magazine informs once more about something you probably will not find mentioned anywhere else: Catchy, clear, and concise three-part phrases in the title of papers boost their citation numbers.1 The Nature article cites as the source of this information a study published preprint by German economists. Catchy, clear, and concise, thus, joins shorter and funny titles as well as punctuation marks as characteristics of article titles that help published papers garner more citations. Isn’t it interesting what economists study these days!
1. Singh Chawla D. Nature 2025;639:847848
So, with the world around us seemingly going in so many different ways, bonkers, here is one more. Some of our politicians have seemingly nothing more important to concentrate their legislative efforts on than the banning of “woke words.”
And some of these initiatives, we would argue, unsurprisingly considering that reproduction always appears to be at the edge of controversy, affect standard terms used routinely in reproductive medicine. So, for example, Democratic West Virginia lawmakers introduced a bill with the intent of banning “woke words” and agendas from state government content.1 Out is “pregnant woman” and in is “pregnant people;” out is “woman” and in is “womxn” or “womyn” (how do you even pronounce that??); or out is again “woman” and in is “birth-giver.”
Or take Democratic Wisconsin Governor Tony Evers who used the annual budget proposal to change language in state law when it comes to issues involving same sex couples and in vitro fertilization (IVF) by even replacing words like “mother” and “father.”2 Out was - still somewhat reasonable - “husband” and “wife” for “spouse;” but then things got weird: Out was “woman,” “mother,” and “wife,” and in was “person who is inseminated,” or “inseminated person.” Quoting a posting by a Republican U.S. Rep, the article in the Milwaukee Journal Sentinel pointed out that these changes would require a change from “Happy Mother’s Day” to “Happy Inseminated Person’s Day.” How crazy can political correctness get?!
1. Koch A. FOX News. February 18, 2025. https://www.foxnews.com/politics/statetakes-woke-language-introduces-bill-banterms-pregnant-person-chestfeeding 2. Beck M. Milwaukee Journal Sentinel; Updated February 27, 2025. https:// www.jsonline.com/story/news/ politics/2025/02/27/what-to-know-aboutinseminated-person-language-in-tonyevers-budget/80493208007/
Biological age vs. Calendar age - which is more relevant?
So let’s start with a few by now wellestablished facts (i) our calendar age does not always reflect our biological age; (ii) our biological age is not always the same in every one of our body’s organs; and (iii) we are not very good yet in determining the biological clock in our bodies. In other words, some people are, at least in some respects, biologically younger, and others are biologically older than their chronological age would suggest. And improving our ability to determine biological age, therefore, would appear to be a worthwhile goal for research.
This is why a preprint-stage paper in eLife attracted our attention, which developed a mathematical model to predict biological age by leveraging physiological traits across multiple organ systems and allowed for, what the eLife assessment described as, convincing results, utilizing comprehensive data-driven approaches. However, additional external validations (as almost always) could further strengthen generalizability.1 The model, however, does provide a way to identify environmental and genetic factors impacting aging and lifespan, in the process revealing new factors potentially impacting aging and lifespan, including genes involved in synapse biology and – believe it – a tendency to play computer games. The authors concluded by stating that they identified a small number of readily measure physiological traits that, together, assess a person’s biological age and may be used clinically to evaluate therapeutics designed to slow aging and extend healthy life.
From this preprint paper, it is just a small jump to yet another of F. Perry Wilson, MD’s Impact Factor commentary on Medscape, in which Yale University’s Wilson always brilliantly comments on the statistical validity of new medical studies.2 And the article he addressed this time was an article in Neurology, claiming to examine the risk of dementia based on biological, not calendar age.3
But, as he started the discussion, he correctly asked which biologic age, because there are, of course, a whole lot of biological ages in the literature, making the claim of relevance. Some use DNA-methylation (so-called epigenetic clocks); others measure more obvious parameters, like, for example, blood pressure, lipid profiles (so-called phenotypic clocks), etc. In the study of neurology, two wellvalidated phenotypic clocks were used (see below chart in yellow and blue).

Though somewhat overlapping, they showed only a very weak correlation coefficient of 0.29. Obviously, we are still far away from an ideal universal biological clock! But remember, as noted above, different organs may have different biological clocks. The above depicted biological clocks may, therefore, reflect well different organs.
In the paper, the question then became whether either one predicted the risk of dementia better. And the answer was interesting: And it was not the calculated biological age of individuals, but the difference between the biological age and real age; is biological aging ahead or behind? And if biological age was ahead of calendar age, the risk of dementia went up by 1% for each year (a biological age of 55 in a 45-year-old gave a participant in this study a 10% increased dementia risk). These data were similar for both above-described
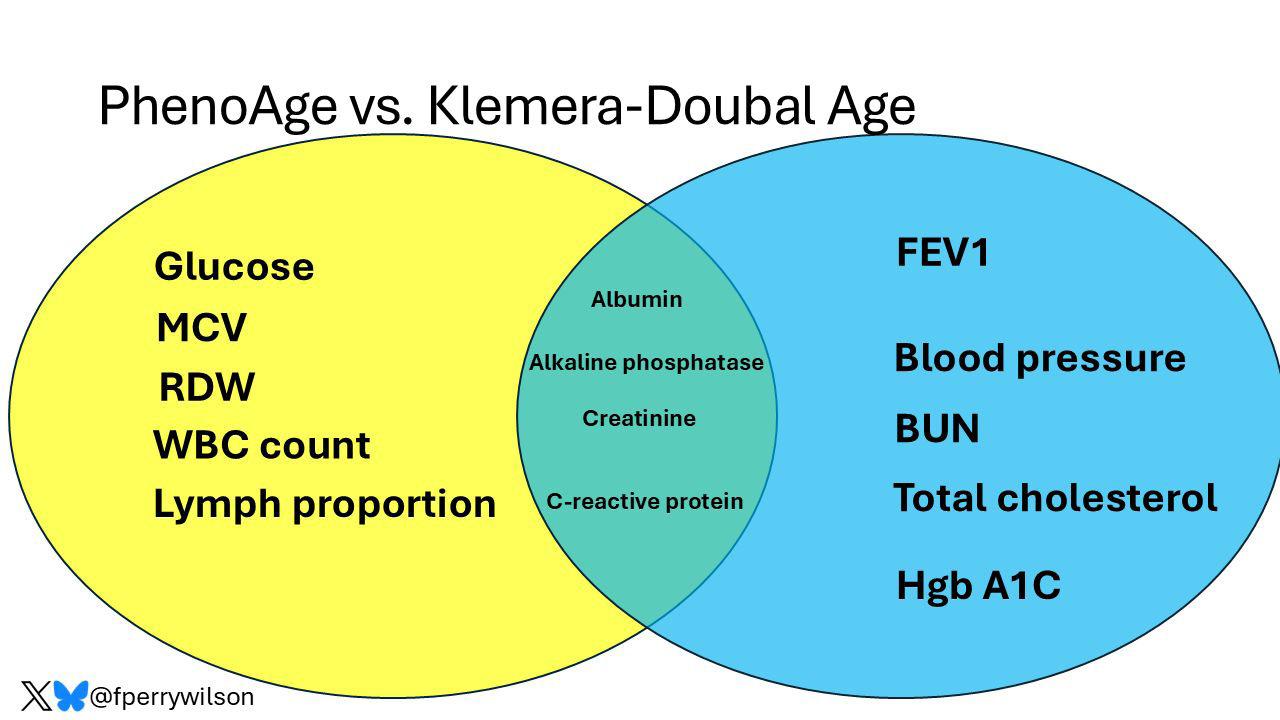
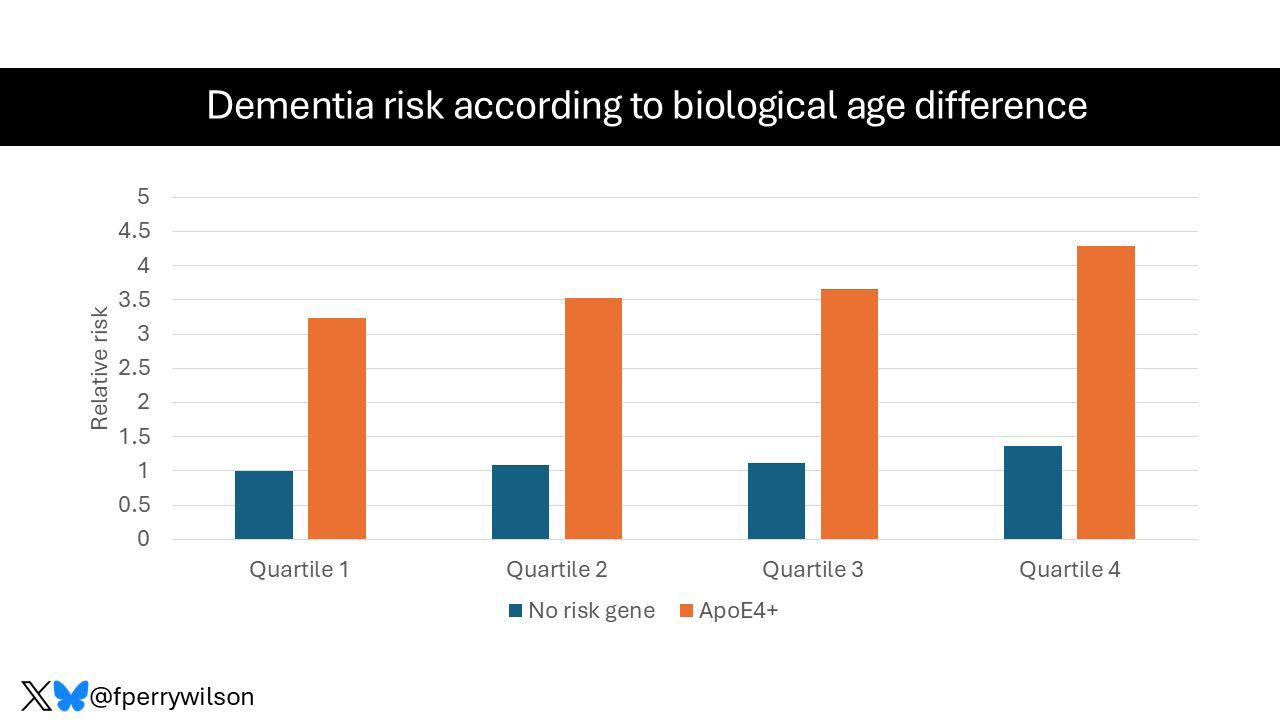

biological age clocks.
1. Libert et al., eLife. https:;doi. org/10.7554/eLife.92092.2
2. Wilson FP. Impact Factor on Medscape. April 30, 2025. https://www. medscape.com/viewarticle/biologicalage-vs-calendar-age-which-predictsdementia-2025a1000acl
3. Bo et al., Neurology 2025;104(10):https://doi.org/10.1212/ WNL.0000000000213616; ahead of print.
Was Fauci's pardon a good thing?
This is at least what one of his major academic victims, the new National Institutes of Health (NIH) boss, Jay Bhattacharya, MD, MBA, appears to have concluded, according to a recent article in The Free Press. 1 Tony Fauci, MD and his then boss at the NIH, Francis Collins, MD, PhD (his predecessor at the NIH), almost destroyed his academic career at Stanford University in 2020, accusing J. B. of quackery when he spoke out against COVID-19 restrictions for low-risk individuals the two NIH “professors” had convinced the government to mandate.
Once he, moreover, became one of the three main co-sponsors of the so-called “Great Barrington Declaration,” Fauci and Collins, indeed, made him into a pariah within the medical establishment when, as the article noted, Collins in a 2020 in a likely on purpose leaked e-mail to Fauci called J.B. a “fringe epidemiologist” and asked for a “quick and devastating published takedown” of the Declaration. And Collins did not hold back later either: For The Washington Post, he described J.B. as “dangerous” and judged his work “as not representing mainstream science.”
What a perfectly executed and telling irony by President Trump to appoint J.B. as Collins’ successor! J.B's two co-sponsors of the Declaration, Martin Kulldorf, PhD (a Swedish biostatistician and Professor of Medicine at Harvard University until his dismissal in 2024), and the highly awarded Oxford University Professor Sunetra Gupta, PhD, did not do much better. The Declaration has, however, since been signed by not less than 941,261 individuals.2 It started with this sentence:

"As infectious disease epidemiologists and public health scientists we have grave concerns about the damaging physical and mental health impacts of the prevailing COVID-19 policies and recommend an approach we call Focused Protection."



Here is, however, the really interesting commentary of J.B. according to Maya Sulkin’s article in The Free Press: “I think he was deeply wrong in his scientific ideas in 2020, but I believe he was sincere in them. I think that he was trying to do what he viewed as the best for the American people.” J.B., therefore, was “actually in favor of Fauci’s pardon,” calling President Biden’s preemptive pardon of Fauci “a really good thing,” even though his mask mandates and school closings led to highly significant learning loss, something The Great Barrington Declaration had warned about.
1. Sulkin M. The Free Press. April 1, 2025. https://www.thefp.com/p/jaybhattacharya-fauci-pardon.
2. The Great Barrington Declaration. October 4, 2020. https://gbdeclaration. org/
The amazing thing is that nobody really knows. This is not different from, for example, autoimmune diseases, which have a dramatically higher prevalence in women than men. It, of course, must be “the hormones" is what the literature is telling us. But is that also really true?
A quite lengthy News Feature article in Nature Medicine by Sofia Moutinho on the subject offered an interesting update (certainly worth a read). Still, it was left to conclude that the increased risk of disease may be linked to changes in the female brain during menopause, along with social and cultural influences.

Sounds exactly like what we now know for decades already about autoimmune diseases. But how and why is this happening?
REFERENCES
1. Moutinho S. Nat Med 2025.31:7047

Walking regularly can help preserve cognitive function as we age


Just two articles earlier in this issue of the VOICE we noted that the CHR this year celebrates the 20th anniversary of the first paper published by the CHR’ s investigators regarding androgen supplementation of hypoandrogenic infertile women in 20051 and that this publication not only changed the trajectory of the CHR, but – at the same time – also changed infertility practice at many fertility clinics around the world. If you haven’t yet read this article, we strongly suggest you go back a few pages in this issue of the VOICE and do so because this article explains why in the CHR’s opinion not every fertility clinic supplements hypo-androgenic infertile women with androgens yet – and especially with DHEA (dehydroepiandrosterone) even though they should!
This paper ended up being only the first of so far 33 peer-reviewed publications on this subject from CHR investigators and added another worldwide practicechanging innovation to the list of such innovations produced at the CHR.
Did you, for example, know that the concept of vaginal egg retrieval under ultrasound control was invented at the CHR.2 Suffice it to say that vaginal egg retrieval made current-day IVF practice possible because up to that point egg retrievals were in principle
performed surgically through laparoscopy in operating rooms under general anesthesia.
Or did you know that the CHR pioneered transvaginal tubal catheterization for obstructed tubes,3 which days now routinely performed by many radiologists.
And then there, of course, are many other important innovations in the infertility field in later years of IVF practice, from the emphasis on the immune system,4 the center’s almost 20 years of opposition to preimplantation genetic testing for aneuploidy (PGT) of human embryos during IVF,5 recently finally confirmed by the ASRM and SART in its clinical validity,6 and groundbreaking other practice changes mostly in IVF cycles of older women, including the truly revolutionary HIER (Highly Individualized Egg Retrieval),7 and rescue in vitro maturation of premature oocytes.8
DHEA supplementation of hypoandrogenic women was, however, clearly the accomplishment that turned the CHR from a regional into a worldwide infertility center of last resort and, ultimately, led to the absolutely unique patient population from all over the globe that the CHR has the honor of serving these days. Letting our patients and especially our younger colleagues know how special the CHR really is in today’s IVF world, therefore, at this time appeared opportune.
1. Barad DH, Gleicher N. Fertil Steril 2005;84(3): 756
2. Gleicher et al., Lancet 1983;2(8348):508-509
3. Gleicher N, Confino E. Radiology 1990. Published Online: https://doi. org/10.1148/radiology.177.2.589-a
4. Gleicher N, El-Roeiy A. Am J Obstet Gynecol 1988;159(1):223-227
5. Gleicher et al., Trends Mol med 2021;27(8):731-742
6. ASRM & SART Practice Committees. Fertil Steril 2024;122:421-434
7. Wu et al., J Ovarian Res 2018;1191):23
8. Nicholas et al., iScience 2023;26(8):107308
To quote the organization called Scholar GPS in a written notice to the CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, its existential purpose is to rank worldwide socalled Highly Ranked Scholars™ for their exceptional performance in various science and medicine fields, disciplines, and specialties. In the organization’s notice to Dr. Gleicher, it for the second year in a row “celebrated his exceptional performance,” especially pointing out his “prolific publication record, the high impact of his work, and the outstanding quality of his scholarly contributions which placed him into the top 0.05% of all scholars worldwide.”
To quote the organization called Scholar GPS in a written notice to the CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD,
its existential purpose is to rank worldwide so-called Highly Ranked Scholars™ for their exceptional performance in various science and medicine fields, disciplines, and specialties. In the organization’s notice to Dr. Gleicher, it for the second year in a row “celebrated his exceptional performance,” especially pointing out his “prolific publication record, the high impact of his work, and the outstanding quality of his scholarly contributions which placed him into the top 0.05% of all scholars worldwide.”

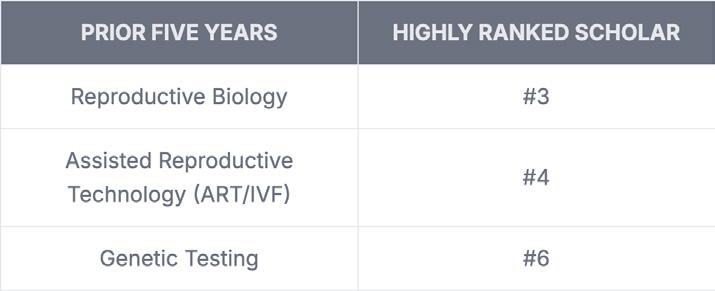

To the left are summaries for the years 2023 and 2024 of areas in which he was awarded Highly Ranked Scholar (with specific rank) for his lifetime achievements, as well as the last 5 years only.
We would say a pretty remarkable worldwide honor two years in a row! And, of course, CONGRATULATIONS to Dr. Gleicher!

Under this heading, report publications by members of the CHR research staff in peer-reviewed medical and scientific journals. Today, we, for example, report on three publications in Human Reproduction Open, The Lancet, and Human Reproduction that appeared in print since the preceding issue of the VOICE.
Gleicher N, Gayete-Lafuente S, Barad DH, Patrizio P, Albertini DF. Why the hypothesis of embryo selection in IVF/ICSI must finally be reconsidered. Hum Reprod Update 2025(2):hoaf011
This paper was already addressed earlier in this issue of the VOICE in the CHR’s press release. The CHR’s authors in this paper question the basic concept of trying to select “best” embryos from among a cohort of embryos in a given IVF cycle, which has been a bedrock of IVF practice almost since its existence. One, indeed, can say that no subject in IVF has since its founding attracted as much research attention and investments as the concept of embryo selection. The authors in this paper now, however, pointed out that not only has embryo selection uniformly failed to offer embryo selection beyond basic morphology which every embryology laboratory in
the world automatically performs,but several methods of embryo selection, such as routine extended embryo culture to blastocyst stage and preimplantation genetic testing for aneuploidy (PGT-A) in significant subpopulations of infertility patients actually reduce pregnancy and live birth chances. The CHR, therefore, considers this paper to be one of the most important opinion articles its investigators have contributed to the literature in recent years.
Gleicher N, Mochizuki L, Barad DH. Home-based IVF monitoring. Lancet 2025;405:892-893
This brief letter-to-the-editor article in The Lancet, one of the most prestigious medical journals in the world, had a long incubation period because it was accepted for publication almost a year ago and, likely, for editorial space reasons, just appeared in print recently. It was a commentary from several CHR staff members on a paper The Lancet had published by colleagues from the Netherlands, in which they claimed to have developed a home monitoring system for IVF patients that worked. The CHR’s investigators, in their commentary, however, pointed out shortcomings in study design, which was an open-label multicenter randomized non-inferiority trial of home-based ovulation monitoring but only for frozen-thawed IVF cycles (obviously a much easier target for home monitoring than fresh IVF cycles).
Every IVF services provider in the world would, of course, welcome a functioning home monitoring system that could replace the often-daily patient visits to IVF clinics that patients (and their providers) currently have to face up to. But, as the study actually quite blatantly demonstrated, we are not there yet, and the absence of a response from the authors suggests that they, indeed, agree.
Gleicher N. Empirical use of growth hormone in IVF makes no sense. Hum Reprod 2025; 40(5):971-972
This is another brief letter-to-the editor article, this time involving an article published in the medical journal Human Reproduction, in which the CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, basically attempted to correct the false message a paper conveyed that had appeared in the journal, incorrectly and with rather inappropriate bravado, claiming to have proven – beyond reasonable doubt – that human growth hormone (GH) treatment does not improve IVF outcomes.
Unfortunately, however, the authors really conducted a study that breached some of the most basic rules of study design by selecting a totally inappropriate study and control populations and then, on top, administering GH and placebo with completely inappropriate and, therefore, totally ineffective timing.
Papers in prestigious journals like Human Reproduction, the mothership of all ESHRE journals, are not only important but usually affect medical practice around the world. And they do so, of course, especially when the authors, as in this case, make categorical claims. In this case, they made the baseless claim that using GH in IVF is simply a waste of time, effort, and cost.
This, of course, does not mean that the use of GH in IVF really does make a difference. This, clearly, was not the purpose of Gleicher’s communication because that, of course, would require a welldesigned and well-executed study. But, as the letter clearly stated, any such study would require a proper
patient selection for study and control groups and proper timing of treatment.
In the meantime, his letterto-the-editor, hopefully, will prevent at least some colleagues from completely discarding the possibility that GH may, indeed, be helpful in selected infertile women with abnormally low insulin growth factor -1 (IGF-1) levels, which is the chemical messenger induced by GH that synergistically with follicle stimulating hormone (FSH) – similarly to androgens – drives follicle growth and maturation especially at small follicle-growing stages between secondary and small antral follicles.
But, since these early-stage follicles still require 6-8 weeks to reach gonadotropin sensitivity, GH treatment must be started at least 6-8 weeks before the IVF cycle starts. In the study, patients were treated only during the IVF cycle, with the potentially desired effects, therefore, only detectable in cycles one to two months downstream.
And the CHR also, quite prominently, made it again into the general public media. Interestingly, two lengthy articles on the same subject – preimplantation genetic testing for aneuploidy (PGT-A)appeared at almost the same time in two major publications: a first in TIME magazine where Jamie Ducharme, one of the magazine’s health correspondents,
on March 6, 2025, addressed the PGT-A issue, starting with the fact that patients recently filed several class action suits against PGT-A laboratories for being misinformed about the test.1

The second article by Amy Klein in Truthdig was published one day later on March 7, 2025,2 and covered in principle exactly the same subject from exactly the same viewpoint, - the filing of above-noted class action suits,which the VOICE already in detail had addressed in its NovemberDecember 2024 issue.3

The two reporters, indeed, also interviewed the same three physicians for comments, among them the CHR’s Norbert Gleicher, MD. Unsurprisingly, the other two “experts” were unabashedly procontinued utilization of PGT-A. At the same time, Gleicher, of course, representing the long-held CHR opinion, opposed the utilization of PGT-A in most infertile women.
1. Ducharme J. TIME., March 6, 2025. https://time.com/7264271/ivf-pgta-testlawsuit/
2. Klein A. Truthdig., March 7, 2025, https://www.truthdig.com/articles/priceyivf-test-may-be-selling-false-hope/ 3. The CHR VOICE. November/December 2024. https://centerforhumanreprod.com/ the-chr-voice-newsletter/the-novemberdecember-2024-voice
On February 21, 2025, The CHR’s Norbert Gleicher, MD, visited the REI division of the Department of Obstetrics, Gynecology and Reproductive Sciences, University of Miami, Miller School of Medicine, Miami, FL, where CHR collaborator and friend Pasquale Patrizio, MD, is the division head,
to give a talk of “Difficult cases in REI practice.” The division had just weeks earlier moved its IVF unit into a brand-new and very impressive facility close to the Miami airport, and, as Dr. Gleicher reported, even the Chinese lunch served was excellent!


BRIEFING: The VOICE here reprints a press release form the Center for Human Reproduction (CHR) in which the center announces the publication of a paper in Human Reproduction Open by some members of its research staff which argues that the hypothesis of embryo selection (beyond basic embryo morphology), which has been an undisputed dogma in IVF practice since shortly after the first birth from IVF, when IVF switched from natural, mostly single follicle cycles to stimulated multiple follicle cycles, has basically proven to be a complete failure. The hypothesis suggests that in every IVF cycle’s embryo cohort are significantly better and poorer prognosis embryos beyond what standard embryo morphology can detect, and that, therefore, new tests and procedures must be pursued to “select” the best embryos for transfers. That this hypothesis is still aggressively pursued to this day is best demonstrated by the onslaught of reported artificial intelligence (AI) studies reported as allegedly demonstrating promise. All practice changes – without exception - introduced to IVF alleging improvements in IVF cycle outcomes based on the hypothesis of embryo selection over more than 40 years, including – to name only the two most impactful ones - routine extended embryo culture to blastocyst stage and preimplantation genetic testing for aneuploidy (PGT-A) –have, however, by now been demonstrated not to improve IVF outcomes in general IVF population and, indeed, to be detrimental for significant subpopulations. Besides explaining why, on a biological basis, embryo selection makes little sense in a large majority of women, the publication, therefore, argues that the concept of embryo selection in IVF beyond standard morphology should be finally laid to rest. The overwhelming majority of resources dedicated to the task of improving embryo selection in IVF over many decades must be redirected toward more promising research goals.
New York City–based Fertility Center publishes an important article in Human Reproduction Open: “Why the hypothesis of embryo selection in IVF/ICSI must finally be reconsidered.”
March 24, 2025
Since almost its initial establishment, the success of in vitro fertilization (IVF) has been based on obtaining through use of so-called fertility drugs more than the usual single oocyte (egg) that a natural ovulatory cycle produces in a female. Multiple oocytes then allowed for the production of multiple embryos with improved cumulative pregnancy and live birth chances. Having multiple embryos available, however, immediately raised the question, which among them
are the best embryos to transfer first, leading to the concept of “embryo selection,” which has since become a dogma of IVF practice.
The assessment of “embryo morphology” (how embryos look under the microscope) was the first method of embryo selection applied and, at least to a degree, proved valuable in ranking available embryos in their chances of leading to pregnancy and delivery. But IVF practice demanded more categorical results. The search for better embryo selection methods, therefore, became the most actively pursued research goal in worldwide IVF practice, to this day consuming otherwise unmatched resources in the IVF field.
On first impression, some of these efforts appeared to bear fruit, as investigators, for example, claimed that
extended embryo culture from day-3 after fertilization (cleavage-stage) to days 5-7 (blastocyst-stage) improved IVF cycle outcomes. As a consequence, the embryos of almost all IVF cycles are now routinely, at significant added cost, cultured to blastocyst stage, even though many studies have since demonstrated that this practice in general populations does not improve pregnancy outcomes and in some patient sub-populations, indeed, reduces pregnancy and live birth chances.
Other investigators proposed testing of embryos for chromosomal abnormalities (aneuploidy) to deselect chromosomal abnormal embryos from transfers, as we now know, wrongly claiming that this would improve IVF outcomes for the remaining normal (euploid) embryos. This procedure, first introduced over 20 years ago and now called preimplantation genetic testing for aneuploidy (PGT-A), is currently - at an additional costs of at least $5,000 per cycle - still used in the U.S. in over half of all IVF cycles despite 2024 joined opinions of the American Society for Reproductive Medicine (ASRM) and Society for Assisted Reproductive Technology (SART) that none of the by proponent claimed outcome benefits from PGT-A have indeed, been confirmed. Somewhat unsurprisingly, PGT-A, therefore, has recently become the subject of several class-action suits in the U.S. In Australia, one such suit was already settled in 2024.
Worldwide disappointing experience with these two IVF practices and several others relying on the hypothesis that better embryo selection would improve IVF cycle outcomes, now led a group of investigators from NYC’s Center for Human Reproduction – an internationally recognized fertility center – to publish a paper in Human Reproduction Open, a medical journal of the European Society for Human Reproduction and Embryology (ESHRE), in which they call for embryo selection attempts beyond embryo morphology to be finally laid to rest.1
Because a majority of research dollars in the infertility field still are spent on embryo selection procedures – confirmed by the current boom in proposed A.I. offerings in the service of embryo selection - the
authors of the paper, moreover, not only call for an end to clinical embryo selection procedures but also an end to the excessive research funding of projects involving the hypothesis of embryo selection. IVF practice, indeed, could greatly benefit from switching this funding to more promising areas of potential exploration.
The authors in the paper also explain why, simply for basic biological reasons, embryo selection cannot work. The most obvious among those explanations is that every embryo cohort in a single IVF cycle acquires a predetermined maximal cumulative pregnancy chance once the number of available and transferrable embryos has been established, which can no longer be improved (though it can be negatively affected by poor practice).
This group of investigators also, as early as 2020, noted the association of declining live birth rates in fresh IVF cycles in the U.S., apparently linked to the increasing use of PGT-A.2 Their argument of redirecting research dollars to goals other than embryo selection goals, therefore, appears logical and cost-effective.
1. Gleicher N, Gayete-Lafuente S, Barad DH, Patrizio P, Albertini DF. Why the hypothesis of embryo selection in IVF/ICSI must finally be reconsidered. Human reproduction Open;2025(2):hoaf011
2. Gleicher N, Kushnir VA, Barad DH. Worldwide decline of IVF birth rates and its probable causes. Human Reproduction Open 2020.

BRIEFING: On Saturday, May 17, 2025, for the first time in U.S. history, a U.S. fertility clinic offering in vitro fertilization services (IVF) was targeted in a car bombing. Considering the political extremism expressed in this assault, the CHR released the following statement to the public.selection in IVF over many decades must be redirected toward more promising research goals.
We were horrified to learn about yesterday’s bomb explosion in Palm Springs, California, that apparently killed the perpetrator of the bombing but also wounded several other innocent bystanders. The bomb also severely damaged a local fertility clinic that offers in vitro fertilization (IVF). Fortunately, the damage did not involve critical areas in the clinic, including the laboratory area where gametes and embryos are stored. According to media reports, Akil Davis, the Assistant Director of the FBI’s Los Angeles field office, noted last night that this IVF clinic was the principal target of the bombing, described the event as “intentional terrorism,” and noted that the agency’s joint terrorism investigators were on the scene. The Los Angeles Times reported today that an internal briefing circulated Saturday afternoon by senior officials within the Los Angeles Police Department and viewed by the newspaper, noted that the FBI had confirmed the suspect bomber himself was the sole fatality. That briefing also notes that police had found two rifles — an AK-47 and an AR-platform rifle — along with ammunition next to the vehicle that had exploded close to the IVF clinic.
The CHR, of course, condemns the bombing of this IVF clinic in the strongest possible terms and, indeed, condemns any form of violence, including violence against any medical facility and any health care provider, not only IVF clinics. Our concerns and condemnation, however, as of this point go even further because this bombing offers yet another example for the morally and legally unacceptable radicalization of our society over recent years which in certain political circles has increasingly legitimized even extreme violence in pursuit of what their ideology considers to represent morally and economically noble goals. Moreover, surprisingly large segments of our society appear to sympathize with these ideas, as the public response demonstrated following assassination attempt on prominent politicians, including two on the nation’s current president, and the recent shameful murder of a senior medical insurance executive, husband, and father, walking to a business meeting in New York City.
This is not the place and time to delve into the causes and sources of this radicalization. Still, it is no secret that the ideologies leading to this radicalization to a significant degree can be sourced to the faculties of some of our leading universities, as recently widely reported in the media, often supported by financial contributions from countries not supportive of U.S. policies. A radical reform of the country’s higher education, especially at its so-called elite institutions, appears overdue.
On behalf of The Center for Human Reproduction (CHR),
Norbert Gleicher, MD President, Medical Director, and Chief Scientist
Sunday, May 18, 2025
BRIEFING: The “food is medicine” is an increasingly frequently heard phrase in medicine that also applies to fertility. This section of the VOICE caters to this concept in a variety of ways. A prominent current subject is, for example, weight loss with GLP-1 receptor agonist drugs, since obesity is becoming an increasingly frequent co-diagnosis in infertility practice.
What is causing the recently noted mild decline in national obesity rates?
Recently published data suggested that, for the first time in many years, national obesity rates have mildly declined in 2023 after plateauing in 20221 (as shown in Figure 4 stems from a recent report by the National Center for Health Statistics).
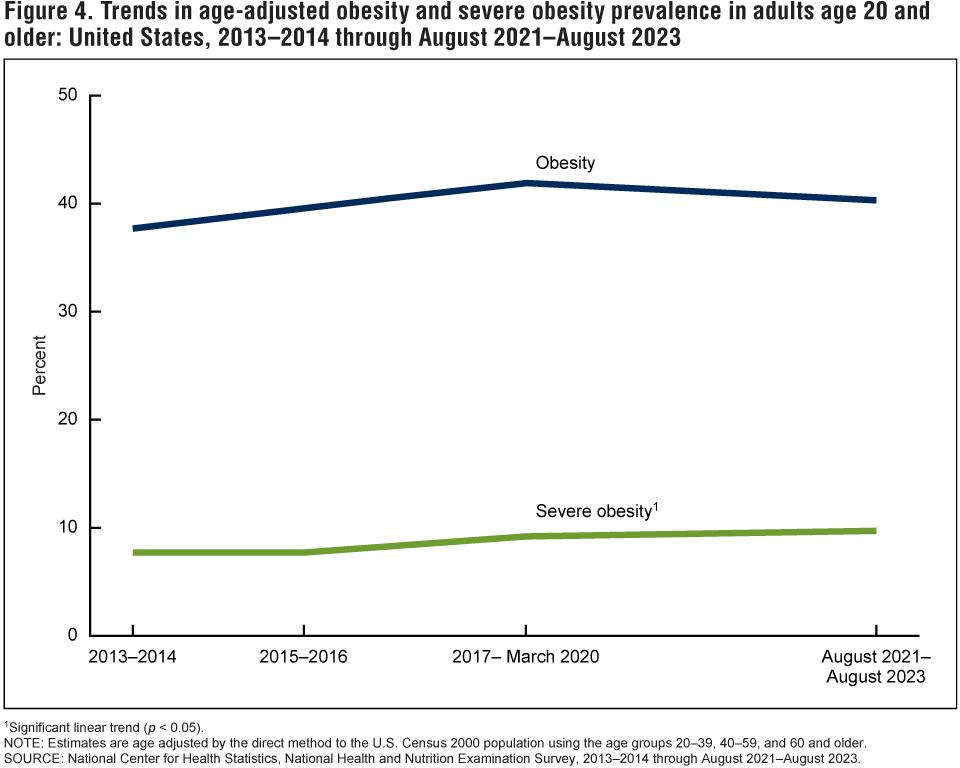
A recent Commentary in Medscape Diabetes & Endocrinology, indeed, argued that the increasingly popular GLP-1RAs do not yet explain this observed drop in obesity and that other factors must have played a role.2
The most notable decrease was in the South, which –interestingly – also had the

highest observed per capita GLP-1 receptor agonist (GLP1RA) dispensing rate. The paper reporting this decline, however, also noted that dispensing does not necessarily mean uptake. The South, indeed, also experienced disproportionately high COVID-19 mortality among individuals with obesity.
For us, somewhat far-fetched, however, appears the argument in the paper that the excessive mortality of obese patients during the COVID pandemic may have affected obesity rates. Moreover, more severe COVID cases among obese patients, according to this author, may have led to significant weight loss. He unquestionably was, however, correct that first and second generation GLP-1RAs were FDA-approved only after the national obesity rate had already plateaued.
The author of the article was also correct in acknowledging that with increasing utilization of especially second-generation medications like tirzepatide (in the U.S. sold as Mounjaro) the national obesity crisis must be expected to improve further, as a just recently published
study demonstrated a whopping 25.3% weight loss in obese patients at 88 weeks of treatment with these drugs. And it, of course, is not only about weight loss as an end goal; weight loss also improves fertility and, ultimately, general health and life expectancy.
1. Rader et al., JAMA Health Forum 2024; 5(12):e243685
2. Freedhoff Y. Medscape Diabetes and Endocrinology. January 17, 2025. https:// www.medscape.com/viewarticle/obesitymedications-dont-explain-decreaseobesity-rates-2025a10000in
tea consumption do for cancer risk, and what about consumption in pregnancy?
This is, indeed, what a recent article in Medscape Medical News cautiously suggested.1 An expert out of the Atlanta office of the American Cancer Society quoted in the article noted that, though evolving evidence appears encouraging, it is not enough yet to result in formal dietary recommendations, at least not yet.

A weak and inconsistent benefit for coffee has been reported for primarily breast and ovarian cancers, and more persuasive evidence for liver, endometrial, and colorectal cancers. And a recent meta-analysis suggested similar benefits for coffee and tea when it comes to head and neck cancers. The authors of this study, involving 9500 cancer cases and almost 16,000 controls from 14 different studies, reported that with four or more cups of caffeinated coffee, the risk of head and neck cancers was significantly reduced. Daily coffee consumption alone reduced oropharyngeal, hypopharyngeal, and oral cavity cancers.

Coffee and tea, historically the most consumed social drinks
Interestingly, caffeine in coffee and tea does, however, not appear to be the primary mediator for cancer risk. In a colorectal cancer study, for example, even decaffeinated coffee reduced colorectal cancers by 18%, which was even more than caffeinated coffee achieved. As a consequence, the thinking now is that polyphenols – bioactive compounds in caffeinated coffee, decaffeinated coffee, and tea may be the responsible parties. They have demonstrated antioxidative and anticancer properties in cancer cell lines. There was, however, one exception, and that was laryngeal cancer, which was found to be increased among tea drinkers, with some possible explanations offered
but no hard evidence on why that may be the case.
Maternal tea and coffee consumption during pregnancy in several (rather poor-quality studies) has in the past been associated with premature birth, low birth weight, both obviously associated with the offspring’s neurological development. As it, however, now turns out according to a recently published Chinese study in Scientific Reports,2 found the opposite, namely a positive association between maternal tea consumption during pregnancy and children’s cognitive development. Children of mothers with a continuous tea drinking pattern throughout pregnancy had higher cognition, fine motor, and gross motor scores than children of mothers who drank tea only in the 1st trimester. Tea-drinking in the second and third trimesters was more strongly associated with outcomes than tea-drinking in the 1st trimester. Second and third trimesters, therefore, appear to be key periods for recommended maternal tea consumption. No significant association in either good or bad was found with maternal coffee consumption.
It, thus, appears that there is little reason to recommend to pregnant women to completely abstain from coffee and tea during pregnancy, as is practice in the U.S. (and many other countries) to this day. And tea may, indeed, offer a positive outcome effect. But the CHR has felt this way for quite some time because we always argued that, if
coffee, indeed, cause significant adverse effects, we would have noticed them in countries with heavy coffee consumption (for example, Italy, France, and Austria) and heavy tea consumption (for example China, Japan, and Russia) a long time ago.
1. Smith J. Medscape Medical News. February 10, 2025. https://www. medscape.com/viewarticle/coffee-andtea-linked-reduced-cancer-risk-cupmurky-2025a10003ca
2. Ouyang et al., Scientific Reports 2025;15:8832
Should we replace butter with plant-based oil?
A recently published study in JAMA Internal Medicine involving 221,000 adults from 3 cohorts over a time span of 33 years demonstrated that higher butter intake was associated with increased cancer as well as total mortality, while higher plantbased oil intake was associated with lower cardiovascular disease mortality and lower total cancer mortality.

Every 10-gram increase per day in butter intake was associated overall mortality by 7%. A 10-gram increase per day in plant-based oils was associated with a 13% lower risk. Of death from all causes, an 11% lower overall cancer death
risk, and a 6% lower risk of death from cardiovascular diseases. The authors, therefore, concluded that substitution of butter with plantbased oils, like olive oil, soybean, and canola oils, may substantially reduce premature death risks in middle-aged and older adults.1 An accompanying Commentary then suggested that, based on these data, rather modest diet changes could provide highly significant overall health benefits.
REFERENCES
1. Zhang et al., JAMA Intern Med 2025; doi:10.1001/jamainternmed.2025.0205. Online ahead of print.
2. Mark Park Y-M, Park Y JAMA Intern Med 2025; doi:10.1001/ jamainternmed.2025.0203; Online ahead of print.
How important are so-called micronutrients?
This is a question a review article in The New England Journal of Medicine recently attempted to answer.1 It started with the important fact that there exist approximately 20 essential micronutrients for health, which, if deficient, individually have distinct consequences on metabolome, proteome, and genome. Moreover, one-third of people worldwide have at least one micronutrient deficiency. The paper furthermore notes that national surveys provide cross-sectional data, but inferring causality between deficiency and disease is difficult. Consequently, supplementation recommendations are still limited in their evidence.
given to pregnant women and young children. The WHO has, for example, for the longest time recommended iron and folic acid supplementation for pregnant women. But that may, especially for pregnancy, not be enough in general, and especially in poorer populations, because such deficiencies only seldom exist in isolation. Especially in pregnancy, prenatal vitamins are, therefore, now often recommended to contain around 15 micronutrients, including proteins, energy, and essential fatty acids. For example, lipid-based nutrient supplements (LNS) suggested that small quantities of LNS in children aged 6 to 24 months reduced death risks by 27%. Micronutrient supplementation to pregnant women has been reported to decrease low birth weight by 9-14%.
1. Allen LH. N Engl J Med 2025; 392(10):1006-1016
And how can one avoid further discussion of GLPs?
We, indeed, can’t because too much new is, indeed, swirling around GLP-1s (glucagon-like peptide 1 receptor agonists)!
greater weight loss – and potentially also somewhat better tolerance (i.e., side effects). But a third generation of medications is already underway, as recently well summarized in a Feature article in Nature magazine.
As the article noted, over 100 treatments are currently under already announced development to “deliver greater and healthier weight loss,” many, if not most, involve GLP-1s. One relatively big concern associated with the use of these drugs over the longer term has been muscle loss that accompanies weight loss (see also below). A new experimental drug, called bimagrumab (where are all of these weird new drug names coming from?), appears to counter this loss. Newly investigated GLP1s aim to increase weight loss, improve tolerability, ensure longlasting effects (current drugs lead to significant returning weight gain after treatment cessation), and offer options for a broader range of patients.

AND IN PREGNANCY?
As the article points out, supplementations are most often
And so, let’s get started with some general news: As already repeatedly discussed in earlier issues of the VOICE, we currently have two generations of GLP-1s on the market, with the second generation (tirzepatide, sold under the brand names Zepbound and Mounjaro) offering somewhat
The first generation of GLP-1s, representing semaglutide, differs from tirzepatide, which not only mimics GLP-1 but also mimics the so-called gastric inhibitory polypeptide (GIP). GIP further revs up the individual’s energy metabolism and affects how the body stores and burns nutrients, thereby increasing weight loss in comparison to first-generation semaglutide (20% vs. 14% of bodyweight). Several companies now attempt to add further weight loss pathways to next-generation drugs, several building on rare gene variants that have been linked to low body weight.

We are certain that this subject will offer, for the foreseeable future, future, interesting material for the VOICE, as the many benefits from these new weight loss drugs on other health issues (beyond obesity) are coming increasingly into focus.
A recent Perspective article in JAMA explored the effects of these new weight loss drugs on the performance of bariatric surgery in this country, which since 2023, when GLP-1s for weight loss made their first clinically significant appearance, leading to a 25% to 30% decline in the number of these surgeries.2 Predictions, moreover, suggest another 10% to 15% decline over the next 10 years (in our opinion a too conservative estimate), even though bariatric surgery must, still, be considered the most effective and longest lasting treatment for severe obesity and, while upfront more expensive, over time it may be the better bargain (at least at current medication costs) for as long as the weight loss drugs must be continued long-term, - like drugs for any chronic disease.
Another Perspective article in JAMA recently noted that “patients are (because of much lower costs) flocking to compounded weight loss drugs, while raising the question of how save those are.3 The article noted that the FDA had
already, in 2024, raised concerns about the safety of compounded products. As of November 2024, over 600 adverse events were reported to the FDA from these compounded medications, though most were consistent with side effects identical to those reported with FDA-approved GLP-1s. And the price difference has been substantial, from $1,000 to $1,300 down to $200 to $300 per month.
Between February 19 and 26, 2025, the shares of the telehealth company Hims & Hers Health Inc. plummeted by 28% because the FDA announced that the supply of GLP-1s to the market was no longer insufficient. And this was, Rebekah Ninan from Petri-Flom at Harvard Law School reported, devastating news by the national compounders like Hims & Hers because it was only the FDA’s prior declaration of a shortage that allowed them to breach by pharma companies like Novo Nordisk held prior patents (Section 503 of the Food and Drug & Cosmetics Act).4
With this loophole now closed, we are, therefore, witnessing the end of almost all GLP-1 compounding, certainly of all openly compounding from bigger companies like Hims & Hers.
As Ninan’s article also noted Novo Nordisk received recently praise for announcing a direct to consumers sales program of Wegovy (its first generation product) at a greatly discounted monthly price of $499 which, however, still represents a doubling of the compounded price or even more and hundreds of thousands of users who had relied
on compounded products will now have to transition to the Novo Nordisk or even more expensive other products if they want to maintain their treatments.
We have already noted the concern about significant muscle loss with prolonged use of GLP-1s and that a drug called bimagrumab may be able to reduce or even prevent this loss.1 Now investigators from the Salk Institute in La Jolla, California, reported in the Proceedings of the National Academy of Sciences that – at least in a mouse model - B cell lymphoma 6 (BCL6) is required to maintain muscle mass.5 this is achieved by BCL6 suppressing expression of suppressor of cytokine signaling 2, a negative regulator of growth hormone signaling since BCL6 sustains the anabolic actions of GH in muscle. Interestingly, this is how muscle mass is maintained during fasting. If confirmed to function similarly in humans, BCL6 may have therapeutic potential not only in preventing muscle loss from the use of GLP-1s but also in combating muscle wasting due to age and conditions like sarcopenia and cachexia.
Among the many new indications for GLP-1s, The New England Journal of Medicine just added another very important one,

prevention of progression from prediabetes to type 2 diabetes in women with obesity and prediabetes.6 After 17 weeks off treatment with tirzepatide (2nd generation GLP-1) or placebo, 2.4% of the participants who received tirzepatide and 13.7% of those who received placebo had developed type 2 diabetes (hazard ratio, 0.12; 95% CI, 0.1 to 0.2; P<0.001). This is a pretty amazing difference, considering how short the observation period was. Longer observation studies will, however, undoubtedly follow.
THE NEUROBIOLOGY OF EATING CONTROL
A really excellent Review article by colleagues from the U.K. recently described in Endocrinology the neurobiology of eating control.6 The article is not only recommended because it really offers an update on our (still very limited) understanding of how GLP-1 signaling modulates eating demand, but also because it seems increasingly likely that the same or similar signals also affect other addictions besides food addiction.
NO,
NOT FORGOTTEN ABOUT GLP-1s IN INFERTILITY AND IN PREGNANCY
Three articles, indeed, have addressed these issues since our last review of GLP-1 utilization in reproductive medicine in the January-February issue of the VOICE. A first in Obstetrics & Gynecology, significantly outdated and described as a Narrative
Review, can really be skipped because of its superficiality.7 It describes GLPs as contraindicated in pregnancy, which is incorrect and unnecessarily threatening to patients who conceived unplanned while on GLPs.
Though GLPs currently, for safety concerns, should still be terminated one month before conception attempts because adequate safety data are still being accumulated, preliminary postmarketing reports indicate that they, likely, are not associated with any fetal risks. The authors' concluding sentence of the paper’s abstract, that ”obstetriciangynecologists should work with patients to manage these medications before they become pregnant, between pregnancies, and after delivery,” summarizes well the banality of this paper.
A more interesting mini review is offered by New York’s Zaher Merhi, MD, in Fertility Sterility Reports because it offers insights into the still largely unknown and/or contradictory reported physiological effects of these drugs on reproductive organs and, therefore, makes an interesting read.8 And then there is the ubiquitous “Reflection” article from one of the reviewers of almost every paper that appears in any of the Fertility Sterility journals, and not only reveals who one of the reviewers was, but has converted these journals more into opinion rather than science journals. This does not mean that some articles will not benefit from commentaries. Of course, some will, but most will not, and certainly just repeating what the paper said is just a waste of time
for readers and a waste of valuable paper, even if such opinions, because often quoted, improve a journal’s impact factor.
Here, the commentary, moreover, ends with a typical formulary and nonsensical conclusion that stated: “Before high-quality data exist, it may be premature to be prescribing them for fertility or pre-pregnancy indications in obese non-PCOS women.”9 Where has this reviewer been for the last two to three years?”
1. Dolgin E. Nature 2025;638:308-310
2. Schweitzer K. JAMA 2025;333(9):743745
3. Ruder K. JAMA 2025;333(8):652-655
4. Ninan R. Petrie Flom. Harvard Law School. March 14, 2025. https://petriflom. law.harvard.edu.
5. Wang et al., Proc Natl Acad Sci 2025; 122(4):e2408896122
6. Jones LA, Brierley DI. Endocrinology 2025;166:bqae167
7. Finkle J, Brost BC. Obstet Gynecol 2025;145(3):286-296
8. Merhi Z. F S Reports 2025; 6(1):4-9
9. Mandelbaum RS. F.S. Reports. 2025(1):10.

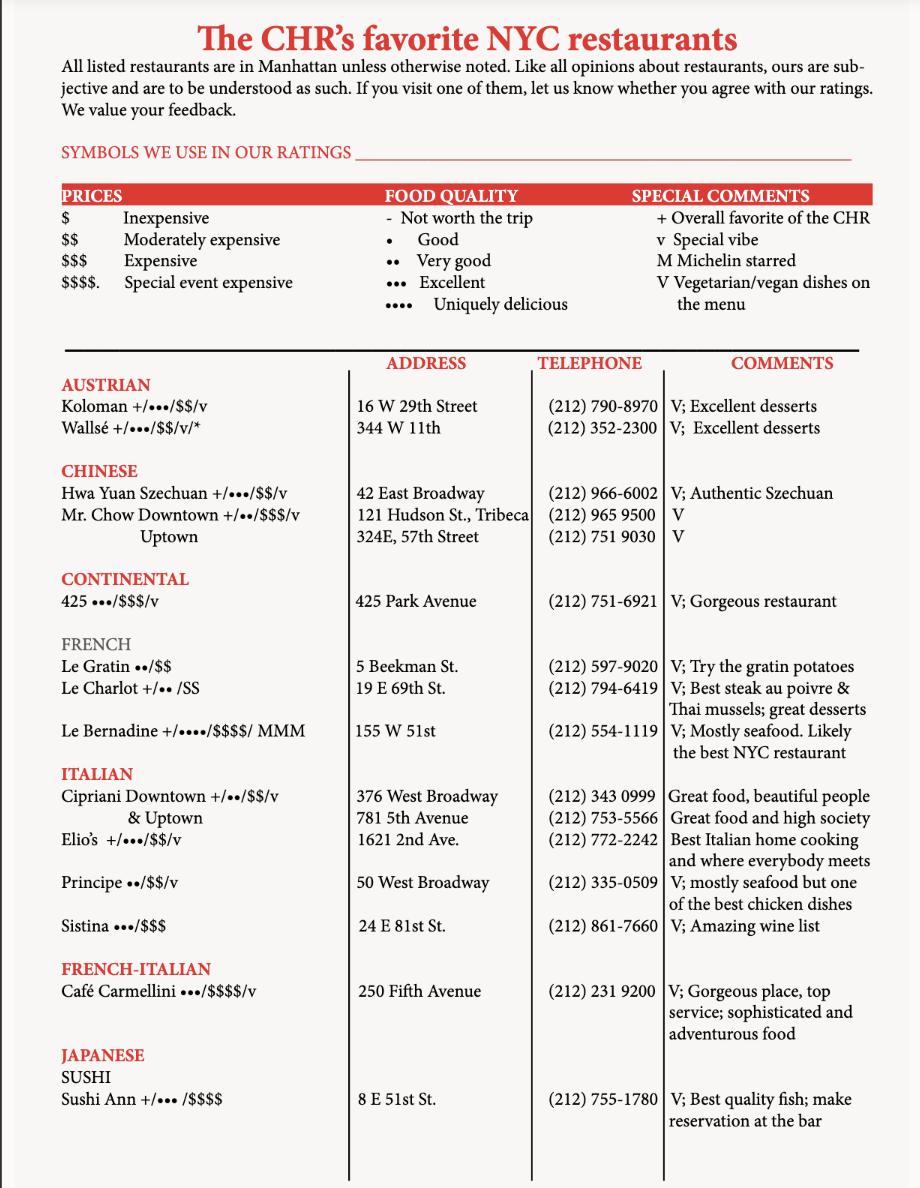


CRANE CLUB**/$$$Continental
85 10th Avenue (at 15th Street)
Tel.: (212) 970 - 2200

When the current Crane Club opened in November of 2024 in part of the space that once housed Mario Batali’s rather grandiose Del Posto restaurant (Mel’s Pizzeria now occupies the rest of that original space), Eater called the Crane Club an “ambitious” restaurant. And this what it on several levels really is: A beautifully designed space, basically encompassing a large bar area (which also features a few tables), and a very elegant main dining room (see picture below) with generously distanced tables and a smaller secondary dining room on each side of the bar through which the restaurant is entered. A dining area on the second floor is mostly meant for private events, but is opened up to the general public when needed and available.
As the name of the restaurant already indicates, the Crane Club also offers a “Members Only” lounge in the basement, which we here do not address. And that a young and quite glitzy crowd appreciates all of these offerings has since the restaurant’s opening become very obvious from the
fact that even in the bar room, reservations are difficult to come by unless made far in advance.
But for those lucky enough to have a reservation, the service - both at the bar and in the dining areas - is truly impeccable, among the best we have encountered in the city, exceeding even many highly starred Michelin restaurants that will remain unnamed. The staff is not only attentive and incredibly well informed but also appears to genuinely enjoy what they are doing.
Melissa Rodriguez remains in charge of the kitchen, which she already headed at Del Posto and later, when she and Jeff Katz (as front manager) took over the Del Posto space and opened in 2022, Al Coro as its (Italian) successor, which received two Michelin stars. Now managed by the Tao Restaurant group (recently taken over by the high-end investment firm Mohary Hospitality, the restaurant, according to Eater, from the beginning was set up to reflect “super luxe cooking and service,” with the intent of “becoming an iconic restaurant.”
Unsurprisingly therefore, there are also significant changes from those predecessor restaurants, reflective of the Zeitgeist of the current restaurant scene in New York City: First, the Crane Club is no longer an exclusively Italian restaurant with French influences but also offers significant Spanish and other contributions to its menu; and, second, it no longer insists on a tasting menu but – reflective
the overall trend toward smaller food portions, sharing of dishes, and fewer courses – in offering what has to be considered an even somewhat small à la-carte menu for an ‘iconic” restaurant, heavy on vegetable dishes, raw sea food and steaks, much of the offering cooked over a Spanish Mibrasa grill.
Which brings us to the food, which we, in summary, would describe as good but somewhat inconsistent. For example, the wood-fired Dover sole ($100) one night was perfectly cocked and absolutely delicious but at a second visit somewhat overcooked and too dry. As also already noted, except for the plethora of vegetable dishes, we found the menu to be somewhat short on choices and not very interesting. The raw seafood tower at $60 per person, though excellent, was, considering the price, sparse in offerings. We also found the offered desserts somewhat disappointing.
Whether solidly good food is enough to become an “iconic” restaurant for the long term remains to be seen. We, overall, very much liked our three visits so far to the restaurant, though more so because of the exquisite service and the general atmosphere the restaurant offers than because of its food choices and food quality. We, therefore, are, as of this moment, also holding off on adding the Crane Club to our list of recommended restaurants, but would not be surprised if a few more visits will convince us to do so after all.

FOUQUET’s***/$$$ - French
28 Desbrosses Street, Tribeca Tel.: (917) 965-2584

Named after its famous Paris sibling in the Hôtel Barrière Fouquet since 1899, this quintessential Parisian brasserie under Chef Pierre Cagnaire has several similarities with above above-reviewed Crane Club, but is ultimately a very different restaurant. Also located in downtown Manhattan, this brasserie can only be entered from inside the hotel, and though good hotel-based restaurants in New York City have become more common over recent years, to find excellent cuisine in a hotel restaurant is still the exception. But this brasserie does serve excellent food, and does so consistently, though this does not come inexpensively, and by that we mean that it is more expensive than the Crane Club. Like the Crane Club, it serves a relatively young and chic downtown clientele (during one of our recent visits, New York Senator Kirsten Gillibrand was one of the guests at a large group table of mostly younger guests).
The restaurant is more traditionally elegant in design and significantly smaller than the Crane Club, and its very popular bar has many
fewer stools. The bar is also part of the main dining room, which can become somewhat of a problem when, as was the case above, noted larger group of guests gathers for drinks by the bar before taking their seats at their table. With us occupying a table right by the bar, we were significantly impinged upon physically and, because of the noise levels produced, almost lost our ability to converse with each other until the group’s members took their seats.
New York’s Brasserie Fouquet is not a new restaurant; it has been around for over five years and, therefore, has had all the time in the world to mature. Its food is consistently excellent, covering all the French classics and offering choices for almost any taste and food group. But it does so, possibly reflective of the hotel’s very exclusive (i.e., expensive) pricing, at the upper limits of reasonable for what the restaurant overall offers.
Considering this fact, we were surprised to find that the quality of service significantly varies between visits. In three recent visits, the service was twice excellent (with the above-described interruption by the large group of guests at the bar), but once, on a Monday evening, if that may be considered an explanation, quite significantly missed the point.
We, for all of these reasons, are still hesitant to add Brasserie Fouquet to our recommended restaurant list, but – like with the Crane Club –would not be surprised if we, after a few more visits, make it official.
LY LY VIETNAM COOKHOUSE***/$/
Vietnamese
306 E. 81st St./2nd Avenue
Tel.: (347) 251–9060
Only a little over five months old, this relatively small sub-basement Vietnamese restaurant is one of these very rare raw diamonds of ethnic cuisine, which in the old days used to be much more common in New York City.
No wonder the Michelin guide already recommended it as “under consideration” for “star-dom.”
To quote the restaurant’s website, the name “Ly Ly” comes from the lily flower, which symbolizes honesty and integrity—basically a fancy way of saying we really, really care about what we do.”
And we can confirm that this is really the case. This is an authentic Vietnamese restaurant, like we have been unsuccessfully looking for over quite some time on the Upper Eastside that offers a wonderful spread of very inexpensive culinary experiences (and “slinging tiki cocktails”) from street food, to a “mean bowl of pho,” and more sophisticated seafood as well as meat dishes. And the restaurant is relatively close to the CHR and, therefore, quickly has become one of our primary delivery sources. And, yes, it also joined our Recommended Restaurants list.


BRIEFING: In this section, the VOICE offers opinions about recent articles in the medical literature directly referring to reproductive medicine and infertility practice. Like in the earlier general medicine section, the commentaries on papers in the recent literature are, again, to a degree, subjective opinions of the CHR. And, while hopefully mostly unbiased, they are usually referenced. We are starting today with a section on legal issues, but want to point out that in this issue of the VOICE discussed two very important legal issues for reproductive medicine already in the two opening full-length articles.
How to resolve fortunately rare embryo mix-ups?
Embryo mix-ups between couples are fortunately very rare events, but still occur at a certain minimal rate. We over the last several years reported in the VOICE about two such cases in the U.S. – one in NYC leading to closure of the clinic – and a second case in California, in which the mix up was discovered only moths after births of the offspring, at a time when the newborns had already spent months in the homes and families of their birth- rather than genetic mothers, further complicating circumstances, as the decision reached to return the children gradually to their genetic mothers.
We also discussed in the VOICE in recent times a case of mix-up in one of the largest IVF laboratories in Israel, which serves as an embryology hub for multiple infertility clinics and individual fertility specialists in private practice. And it is one case from this laboratory that recently made headlines again because of a truly surprising court decision.
In this case, a mother discovered in 2022 that she had been implanted with a “wrong” embryo. The case reached the court, where the judge decided that the child should be turned over to its biological (i.e., genetic) parents. This judgment was appealed by the couple, who in the meantime had raised the child by the name Sophia, and the Appellate Court granted their appeal, ruling that this couple would be legally recognized as 5-month-old Sophia’s parents and that
she would remain in their custody.1 That this court decision was also prominently featured in the U.S. press,2 supports the notion that this judgment at some point may also have relevance for cases of embryo switches in the U.S.
But for the time being, U.S. courts, still, appear in such cases to favor the biological parents because, low-and-behold, a very similar case was just reported when a woman from the state of Georgia in May of 2023 was implanted at an IVF clinic in Savannah, GA, with what – at birth – turned out to be a likely “wrong” embryo, as the White female who had used a White sperm donor gave birth to a Black child.3
Despite the very obvious error, the mother wanted to keep the child and kept taking care of the child, until a court gave the biological parents of the child custody. A statement released by the birthmother’s lawyer said: “To carry a baby, fall in love with him, deliver him, and build a uniquely special bond between mother and baby, all to have him taken away. I’ll never fully recover from this.”
After genetically confirming that she was not the genetic mother of the child, she informed Coastal Fertility Specialists, a reputable fertility center where she had undergone her IVF cycle. The clinic then informed the biological parents, who sued for custody when the baby was three months old. The birth mother then gave up custody voluntarily since her lawyers advised her she had no chance of winning in court. She now sues the Coastal Fertility Specialists and still does not know what happened to her embryo(s) and whether it, too, was transferred to a “wrong” recipient.
1. Maanit C. Haaretz. March 11, 2025, https://www.haaretz. com/israel-news/2025-03-11/ty-article/.premium/ivf-mixupcourt-overturns-ruling-toddler-sophia-to-stay-with-birthmother/00000195-81a1-db87-abf7-ebbb40040000
2. Chatterjee N. U.S. News. February 18, 2025. https://ca.news. yahoo.com/woman-sues-fertility-clinic-losing-150051081.html
3. Gregory J. BBC News. February 19, 2025. https://www.bbc. com/news/articles/cvgw3e8zj4vo
Did you know that Bloomberg News sued the Centers for Disease Control (CDC) under FOIA, likely for oocyte donor data?
We had no idea until we, as SART members, got a letter informing us about the fact that Bloomberg News had sued the CDC under the Freedom of Information Act (FOIA), seeking certain records from the CDC’s National Assisted Reproductive Technology Surveillance System data set. In the meantime, it appears that the complete FOIA section at the CDC was laid off. SART leadership believes that “Bloomberg is particularly seeking information about health complications experienced by patients, especially egg donors, associated with ART procedures.”
If Bloomberg is, indeed, investigating egg donor morbidity in the U.S., we would welcome this because – since ”selling” and “buying” human eggs has in the U.S. become a legal industry (after the ASRM settled in 2015 a lawsuit against the society by egg donors accusing the society of restriction of trade by recommending maximal payment to egg donors),2 we have gotten the impression – we want to point out that the CHR has not formally studied this subject and, therefore, as of this moment cannot express a formal opinion regarding these issues – that egg donors in the U.S. are being stimulate much more aggressively than before and that selection criteria have weakened. Should our suspicions be confirmed, then both of these developments could contribute to greater egg donor morbidity in the donation cycle.
SART in this e-mail also raised the possibility that the CDC may contact IVF clinics regarding information for this FOIA request and advised clinics to consult with their legal counsel before responding. Within this context, it is important to note that neither SART nor the ASRM, as SART’s mother organization, has issued a formal opinion to its membership on how to respond. Interesting!
1. SART Leadership. SART Response to Recent CDC Requests. Via email. March 20, 2025
2. Gershman J. Wall Street Journal. February 3, 2016. https:// www.wsj.com/articles/fertility-industry-group-settles-lawsuitover-egg-donor-price-caps-1454515313
The Petrie-Flom Center at Harvard Law, of course, does not need any introduction as the likely leading medical ethics and law-centered institution in the country. That it dedicated a two-part article by Christi Guerrini, JD, MPH, and Amy McGuire, JD, PhD, both faculty at the Center for Medical Ethics and Health Policy at Baylor College of Medicine, to the 23andMe bankruptcy is, therefore, notable. In the first part,1 the paper notes the uncertainties that come with this major bankruptcy and cautions individuals who submitted genetic samples to the company. The article noted that the focus of concern has been the 15 million DNA profiles the company has on record, when the concern should also extend to large numbers of still existing customer biospecimens, ancestry and health-related reports, responses to research surveys, and other self-reported personal information.
Future ownership of the company will depend on the bankruptcy court and who the new owners will be. Concerns have been expressed that they may not be well-versed in dealing with genetic confidentiality issues the company is obliged to under the law. Strongly recommended by many experts, many customers have already had their data deleted. Commentators described this as a “mass exodus” before the sale of the company, which could significantly reduce the value of the company. The Federal Trade Commission (FTC) has made known its position that the company must “keep its promises to its clients.” The same message was also received from many state attorneys.
According to this article, it is too early to know whether the FTC will formally intervene, but it has already conveyed “interests and concerns.”
Part 2 of the paper further discusses privacy concerns and also “calls to action.” It notes that clients who choose to delete their records do so forever. The

authors also note that there may still be time since Ann Wojcicki, who was the cofounder and CEO of the company, is bidding on the company (she had to resign as CEO to be able to bid). Her repeat ownership may be either reassuring or concerning to some people, dependent on whether they trust her leadership intentions or not.2
In short, if you sent your biological specimen to 23andMe, be forewarned!
1. Guerrini C, McGuire A. Petrie_Flom at Harvard Law. April 28, 2025. https://petrieflom.law.harvard.edu/2025/04/28/the23andme-bankruptcy-uncertainty-caution-and-a-call-to-actionpart-1/
2. Idem. https://petrieflom.law.harvard.edu/2025/05/07/the23andme-bankruptcy-privacy-considerations-and-a-call-toaction-part-2/
A Chief Legal Officer of one of the largest integrated private equity-owned fertility networks weighs in on embryo rights, IVF restrictions, PGT, and excessive clinic reporting of cycle outcomes
Inside Reproductive Health, the podcast of Fertility Bridge, has in the past repeatedly been a very valuable source of information for the VOICE, offering mostly insights into the business of infertility. Founded by Griffin Jones, he over a good number of years has built Fertility Bridge in Buffalo, NY, into a full-service marketing firm which now, unfortunately, almost exclusively only offers “paid featured content.” Giving him credit, he, for full transparency, marks (in very small print) every commercially sponsored article.

One of his biggest clients appears to be Inception Fertility, likely the most extensively integrated Private Equity-owned fertility company, made up of The Prelude Network of infertility clinics, My Egg Bank (a leading frozen egg bank), HavenCryo (longterm cryo-storage), inspireRx (pharmacy), BUNDL (IVF cycle financing), and NutraBloom (a fertility nutraceutical company). And Inception’s Chief Legal Officer, Mathew K. Maruca, JD, was recently handed the full program of the May 15, 2025, Inside Reproductive Health podcast,1 to comment on almost everything, from “personhood laws and their impact on IVF” (we suggest you read in that regard also Norbert Gleicher, MD’s, A Piece of My Mind article on page 17), an alleged “myth of excess embryos and IVF success rates,” basically claiming that efforts are underway to restrict embryo numbers that can be produced in an IVF cycle, “the burden of excessive (IVF) reporting requirements,” again alleged to be in the works by some legislators in trying to restrict embryo numbers, “the misunderstanding of PGT and its role in reproductive health” (from an IVF clinic network that from the beginning has been – and still is - among the strongest advocates of PGT-A) and, finally, “on advocating for evidence-based fertility policies (seriously?! – from the Prelude Network of IVF clinics!).
In short, we are kind of sorry for Inside Reproductive Health because even though their materials are now produced much more professionally, the content, unfortunately, will apparently become less and less of interest for our readers who expect a more objective presentation of evidence.
1. Maruca MK. Inside Reproductive Health. May 15, 2025. https://www.fertilitybridge.com/news-articles/legislation-trendsivf-embryo-personhood-pgt-restrictions-2025
In their Clinical Practice articles, The New England Journal of Medicine starts with a clinical case and then asks the authors of the article to offer evidence supporting various strategies for diagnosis and treatment, followed by - if they exist - formal guidelines. In one recent issue of The Journal, the
clinical problem was a couple (the woman at age 36) presenting, despite regular intercourse, after one year of failed attempts at pregnancy. The authors were Nanette Santoro, MD, past Chair of Ob/Gyn at the University of Colorado, and now a member of Shady Grove – Colorado, and Alex J. Polotsky, MD, from Shady Grove – Colorado.1 They did a very good job in discussing a basic infertility work-up for a couple with primary infertility, followed by treatment options.
What for us, however, was missing was the purpose for the article: For fertility specialists, the article was absolutely non-contributory, and for the general gynecologist, it may have offered a refresher function at a sufficiently primitive level. But considering current referral habits in the country, the length of this article could really have been shortened to only one sentence: Considering the female’s age of already 36 years and the couple’s desire for three children, they should be asap referred to a fertility specialist.
1. Santoro N, Polotsky AJ. N Engl J Med 2025;392(11):11111119
The difference between fertility and fecundity rates
Legacy and well as social media were buzzing recently after age-specific “fertility” trends were published by the CDC for the years 1990-20231 (see also our commentary in the section of General Medical News on pregnancies in women over age 40, on page 47). The emphasis of our comment here today is on the word “fertility” because the CDC should do a little better in explaining the terminology of “fertility,” which is the natural ability to reproduce. The “fertility rate,” moreover, is the average number of children an average woman gives birth to. This term, however, must be distinguished from the term “fecundity,” which refers to a woman’s inherent biological potential to reproduce by producing offspring.
When the CDC report then suggests a “steep decline” in fertility among U.S women under age 30,2 this should not be misunderstood as these young women suddenly becoming infertile. They just don’t want to get pregnant as young as women used to get pregnant, an observation increasingly prevalent not only in the U.S. but also in Europe and Asia.
1. Driscoll AK, Hamilton BE. Nat Vital Stat Rep 2025;74(3):1-9; March 6, 2025
2. Thomson D. Healthday, March 17, 2025. https://www. healthday.com/health-news/pregnancy/steep-decline-in-fertilityamong-us-women-younger-than-30
It is truly amazing what colleagues waste their time on without giving it thought or, at least, studying the literature first. And it is even more amazing that they can get their paper published, in this case in the American Journal of Obstetrics and Gynecology (AJOG), which apparently has only very limited REI expertise on board. Here, Iranian investigators claim to report on a meta-analysis of not less than 202 observational studies (can you imagine the time it took to go through 202 papers?) to reach the overwhelmingly old conclusion that AMH values are predictive of polycystic ovary syndrome (PCOS). No kidding!
But, once again – and we as well as others have been screaming into the wind that AMH levels are, of course, age dependent and that, therefore, AMH studies must be age-adjusted – all of this work was done without age adjustments and, therefore, is completely wasted. And we, of course, know why that is: because – even if they had wanted, they would not have been able to translate those 202 study populations into one cohesive study group because almost all AMH studies on PCOS in the literature (and also in other frameworks than PCOS) lack age-adjustments. What misery and definitely a paper worth a “WORST PAPER IN ISSUE AWARD”
We thought the AJOG had recovered, as none of the Journal’s REI papers in recent months had won the award. But, as this paper demonstrates, we may have celebrated too early. Considering how few REI papers this journal publishes, here award given here is already too many.
1. Barghi et al., Am J Obstet Gynecol 2025;232(2):164-187.e31 (WORST PAPER IN ISSUE AWARD)

And another ridiculous study, this time of various treatments of women with low functional ovarian reserve (LFOR)
This time it is not Iranian colleagues but, because of the large number of authors (this time, the n=15 and most are Italian, of course, including Laura Rienzi, PhD, and Filippo Maria Ubaldi, MD) - we like to call this group jokingly the European IVF Mafia (Laura Rienzi has published per PubMed 193 papers between 2000 and 2025). So, we here report that the European IVF Mafia published yet another meta-analysis, this time, though, at least of randomized trials. But that alone – unfortunately - did not make it a much better paper than above criticized Iranian paper. To the contrary, in many aspects the paper is even more absurd.
The authors want us to seriously believe that (note!!) – after duplication removal, titles and abstracts of 4,806 articles were scrutinized, from among which 124 were in their full text assessed for eligibility. And among those, only 38 were selected for final data analysis, but not for one treatment in women with low functional ovarian reserve (LFOR), but for 13 different treatments (must be their lucky number!) Those treatments were specifically (in paratheses number of patients studied): dehydroepiandrosterone (DHEA, n=1,336); testosterone (n=418); high vs. low dose gonadotropin stimulation (n=957); delayed start protocols with GnRH-antagonists (N=398); letrozole (n=612); clomiphene citrated (1,113); growth hormone (311); luteal phase stimulation (n=570; dual trigger (n=139); dual stimulation (168); luteinizing hormone (979), estradiol pretreatment (552); and corifollitropin alfa (n-561). And what did they study? The primary outcome was live birth rate or ongoing pregnancies. Secondary outcomes were oocyte numbers, M2 oocytes, clinical pregnancies, and miscarriages.
What did they report to have discovered? Among all 13 interventions, testosterone supplementation was found to be associated with higher live birth/ ongoing pregnancy rates. (4 studies for a total of only 368 patients with at least 13 – and likely more – variables). In patient groupings between 300 and 400, testosterone, DHEA, and delayed-start protocols significantly improved oocyte numbers, while women
with lower dose gonadotropins (surprise, surprise!!) retrieved smaller egg numbers than women with higher dose gonadotropins (905 patients studied). No other differences were found (what a surprise!!)
Reading this paper, unbelievably accepted and published by Fertility and Sterility, it is difficult to even decide where to start the criticism. Of course, no statistical adjustments were done for age, as all fertility treatments are, of course, age-dependent. The authors included, by design, at least 13 variables, where were the adjustments for those? How and for how long were the various treatments given, etc. It is simply unbelievable that this paper was even submitted in the first place; it is even more amazing that this paper went through peer review, and it is, finally, unconscionable that this paper was accepted and published by the main journal of the ASRM. We wonder whether it was first rejected by Human Reproduction.
As proponents of androgen supplementation in a to this practice sometimes-hostile world, we actually should be happy that women with LFOR with testosterone and DHEA supplementation demonstrated significant improvements in pregnancy outcomes and egg numbers. But considering the shamefully inadequate study design of this paper, it is not even worthwhile pointing out that the variability of patients likely washed out even more significant findings. If there were a special award for the worst paper among worst papers, this manuscript would have earned this award with honors. As we have only the WORST PAPER IN THIS ISSUE AWARDS, that is, however, all we have available for this paper as well.
1. Conforti et al., Fertil Steril 2025; 123(3):457-476. (WORST PAPER IN ISSUE AWARD)
How do cumulative IVF outcomes of two consecutive elective single embryo transfer (eSET) cycles compare to outcomes of one 2-(double-) embryo transfer (2-ET?
This is the question that a paper in Human Reproduction recently addressed1 which caught our
attention because the CHR has for many years been outspoken – ignoring for a moment that nobody can guarantee an infertility patient a second cycle chance after a failed first cycle – that this represents the most correct statistical way to test the widely held believe that 2-ETs should in most patients be avoided because they – due to larger twin pregnancy numbers - create excessive maternal and neonatal risks in comparison to eSETs. And when the question is addressed in this way, significant alleged increased outcome risks for twin offspring and/or their mothers really disappear.2
The reason why, as the literature has done for decades, outcome comparisons between one twin pregnancy and one singleton pregnancy are incorrect should be obvious to everybody: a statistical outcome comparison must compare apples with apples (i.e., same outcomes). In the traditional comparison of one singleton to one twin pregnancy, the outcomes, however, differ: the first produces one offspring, and the second leads to the birth of two. And for infertile patients, especially when already for some time trying to conceive and/or being older, ending up with one or two children makes a significant difference. With combined risks from two pregnancies and one twin pregnancy being similar, most infertility patients – by wide margins – will, if only asked, of course choose a 2-ET, – again also recognizing that no fertility patient can, after a first singleton pregnancy, ever be guarantee of a second pregnancy and, of course, also not considering the additional effort, time, and treatment costs a second pregnancy attempt would require.
Here discussed paper attracted our interest because it, based on data from the U.K. HFEA registry, came to different conclusions. It, indeed, concluded that two consecutive eSETs may provide greater or comparable live birth rates with lower multiple births, preterm births, pregnancy loss, or neonatal death rated compared to 2-ETs. We, therefore, asked where this outcome discrepancy between these British data and prior studies is coming from. And here are the answers: First, the question arises how solid (i.e., how statistically significant) the observed risk differences in favor of eSETs were? And the answer is not very much indeed: median life birth rates were 0.47 and 0.41, respectively (for a marginal P<0.05); 2-ETs, of course, produced more twin pregnancies, more preterm births, and more miscarriages as well as neonatal deaths but the differences were again rather
minor and may, indeed, have had other causes, as the 2-ET patient group was a full 3 years older (mean 35.6 vs. 32.5 years) and, therefore, unsurprisingly, had approximately 1 less oocyte retrieved (mean 12,18 vs. 13.08).
The authors deserve credit for acknowledging that certain confounders were not considered and that results vary between different age groups and other patient characteristics. They also very carefully noted that two consecutive eSETs may (the emphasis is on “may”) result in slightly higher live birth rates in women up to age 39, but in women above age 39, offered no advantage.
But then, they unfortunately went politically woke by summarizing their results in concluding that two consecutive eSETs are the better way, and here are once more the reasons why they were wrong: (i) Cumulative live birth rates were almost identical at 0.47 and 0.41 rates. (ii) 0.41 is, of course, a very reasonable live birth rate for a 2-ET cycle in an average-age patient population (mean age 35.6); but 0.47 is really an awful live birth rates for 2 eSET cycles, - and on top of it at much younger age (median 32.5 years). (iii) Add to this the time delays for a second child, the additional treatment costs, and –ultimately – that a second successful pregnancy can never be guaranteed, one is left again with the very clear message that current eSET recommendations followed in Europe, the U.S., and most of the rest of the world make little sense. Too bad the current intellectual bias – or should we call it political correctness – regarding this subject is so pronounced that the authors cannot even properly interpret their data.
1. Tighe et al Hum Reprod 2025;40(5):885-894
2. Gleicher N. Hum Reprod 2017;28(2):294-297
How do IVF outcomes differ in hyperandrogenic PCOS vs. nonhyperandrogenic PCOS?
We found this recently published paper in the International Journal of Women’s Health of interest for all the wrong reasons. The main reason was, however, that it addressed a subject the CHR has been researching and working on clinically for years.

A few introductory explanations may help: PCOS (polycystic ovary syndrome) is not one disease but is made up of several so-called phenotypes, which have historically been bunched together under the term PCOS because of certain common denominators. There is disagreement about how many phenotypes make up PCOS. However, a majority of REIs would likely say that the number is four, and would still describe them as phenotypes A, B, C, and D (the socalled Rotterdam Criteria), with A, B, and C generally described as hyper-androgenic and D as the only non-hypo-androgenic phenotype (often also called the “lean” phenotype because the other 3 usually are characterized by obesity).
Colleagues from Jordan now reported on 149 PCOS women of specifically only phenotypes A (also called the “classical” phenotype and above defined phenotype D, and compared both of these patient groups to a control population without PCOS. They allegedly (emphasis on “allegedly”) found that non-PCOS patients did better than both PCOS groups when it came to mature oocyte numbers, fertilization rates, and good quality embryos on day-3 after fertilization. Pregnancy outcomes were significantly lower in phenotype A PCOS women than in phenotype D, as well as in non-PCOS control patients. Interestingly, phenotype D PCOS patients had, however, similar pregnancy outcomes as nonPCOS control patients.1 Unfortunately, this is a terrible paper, not only full of grammatical mistakes and typos but clearly insufficient in study design and data analysis. So, why are we then presenting and discussing it here?
The reason is simple: the paper offers at least some information on an important subject that almost no other papers in the literature have covered, namely a direct comparison of IVF outcome between phenotypes A and D. As noted, it does so poorly (patient selection is insufficiently defined and patient numbers are probably statistically insufficient to offer minimal statistical power, etc.). These data, therefore, must be considered with considerable caution. The two principal reported findings, therefore, must be considered with this in mind. That several IVF outcome parameters were better in non-PCOS than both groups of PCOS patients in some respects makes sense, but in others is only further evidence for the poor quality of the study. For example, that
non-PCOS control patients would produce more oocytes than PCOS patients makes absolutely no sense. Moreover, that fertilization rates and embryo quality were lower in PCOS patients, at best, must be considered controversial because much of the published literature does not support these findings.
The two finding of the study which for us made at least some sense and made this paper a worthwhile read, were that pregnancy chances turned out to be significantly lower in PCOS phenotype A than D PCOS phenotypes and, of course, also were lower than in in non-PCOS patients, while they did not differ between phenotype D and non-PCOS control patients. And here are the reasons for these alleged findings: In contrast to other PCOS phenotypes, there basically exists no medical literature on the D-phenotype. The CHR’s investigators, several years ago, when first getting interested in this phenotype, found only a single paper in the English literature about primarily the PCOS-D phenotype, and even that paper referred only peripherally to this phenotype.
As summarized by CHR investigators a few years ago,2 research performed at the CHR and published even several years earlier, revealed important new findings about the D phenotype, which are highly relevant to the here discussed paper. A very important such finding was the fact that the D-phenotype, by Rotterdam Criteria, also defined as the only non-hyperandrogenic PCOS phenotype, in reality, is also a hyperandrogenic phenotype. The error by the Rotterdam Criteria in defining the D phenotype as non-androgenic stems from the fact that hyperandrogenism in D phenotype is only temporary at young ages after menarche (ca. 25% of teens undergoing menarche demonstrate a PCOSlike ovarian phenotype3) This stands in contrast to hyper-androgenism in phenotypes A, B, and C, which persist into advanced female ages. The D phenotype, after initial hyperandrogenism in teens, normalizes androgen levels usually by approximately age 25.
After this time, women remain in normal range for approximately 10 years, though they continue to drop their androgen levels due to progressive deficiency of the zona reticularis in adrenals, which are responsible for ca. 50% of female androgen production (the other 50% comes from the theca in
ovaries). By approximately age 35, these women then actually become hypo-androgenic (and frequently also become infertile for the first time). Because these patients, thus, usually remain in normal androgen range between roughly ages 25 to 35, when 95% of PCOS diagnoses are made, this PCOS patient population by Rotterdam Criteria was described as normo-androgenic.
We are spending so much effort on this very poor paper because phenotype D patients are in infertility practice, very frequently overlooked. Reasons are not the false description of being normo-androgenic but the fact that these women also do not present with what are widely considered typical phenotypical stigmata for PCOS, including truncal obesity, hirsutism, acne, anovulation, and, therefore, irregular menses. They usually are lean, attractive women with regular ovulatory menstrual patterns. Nobody, therefore, suspects them of being PCOS patients, and they, therefore, do not undergo the required diagnostic workups.
This is especially relevant for phenotype D women above age 35, when they usually enter progressively hypo-androgenic territory and, therefore, become progressively infertile (at younger ages they are – as this paper also suggests – practically normo-fertile, even though they, due to a hyperactive immune system – which after age 35 is seen in up to 85% of phenotype D women - may be at increased risk for miscarriages).
REFERENCES
1. Khamaiseh et al., Int J Women’s Health 2025;17:561-569
2. Gleicher et al., Biomedicines 2022;10(7):1505
3. Nicolaides et al., Acta Biomed 2020;91(3):e2020085
Can manipulation of the endometrial immune environment improve IVF outcomes?
This is, indeed, exactly what a French group of investigators recently suggested in a paper in Frontiers in Immunology, 1 and we wish we could believe it. Their study allegedly started with several logical first steps: They enrolled 493 between 2015 and 2023 (quite a long, drawn-out study!) in whom they obtained luteal-phase endometrial biopsies, which were used to perform what the investigators called “endometrial immune profiling.” Without going into too much
detail, such profiling involved certain cytokine biomarkers. If this testing revealed an immunological endometrial “dysregulation,” these patients were randomized to standard IVF (no immune treatment) or so-called “personalized” embryo transfer they also called “precision therapy” and, as they explained, adapted to the immune abnormalities found. The primary endpoint of the study was live birth rate in a first embryo transfer.
And the claim then was that the live birth rate with precision care (41.4%) was significantly better than with standard IVF (29.7%; P =0.035), - by no means an impressive difference and especially troubling because the authors noted that the difference was especially notable in patients with morphologically poor embryos and women with 2 or more failed embryo transfers. Our interpretation of these latter associations would, indeed, be that something else but the endometrium may be the problem in these IVF cycles. How can one keep treatment protocols in IVF steady over so many years? And then on top of it, there were all of these individual so-called “precision” treatments which, of course, greatly varied but really only impressed based on their total lack of sophistication: Endometrial scratching, supplementation with hCG in the luteal phase, and advise to have sexual intercourse post-embryo transfer. What kind of “immunological precision medicine is that?
Moreover, the protocol changed halfway, basically simply giving up on randomization. And then in 2017 inclusion criteria were amended. In short, not surprising at all, given the alleged 10-year study length, this was anything but a prospectively randomized study. In short, yet another completely worthless immunological study making completely unwarranted claims about reproductive immunology. This will not help the recovery of the reproductive immunology field, and, on a sidenote, it will also not help the poor image of the Frontier journals in the scientific community. And we almost forgot, the first two authors allegedly were awarded two patents for the treatment(s) in this paper. What a crazy world we are living in, and – clearly a “WORST PAPER IN ISSUE AWARD” from the VOICE
1. Lédée et al., Front Immunol 2025;1523871

Obviously a paper that must have circulated between medical journals for some time – there is no other reason why the reported study period went only until 2020 – we are nevertheless pleased that the here discussed manuscript, finally, did see the light of being published in JARG1 because it offers yet another opportunity to address the use and abuse of preimplantation genetic testing for aneuploidy (PGT-A) in U.S. IVF practice.
Using national SART registry data but weighing each clinic individually and equally, - so not to skew national data with large-volume clinics, the study, nevertheless, reported interesting trends in national IVF practice: ICSI utilization clearly increased at all patient ages between 2014 and 2020, with by 2020 over half of all U.S. clinics utilizing ICSI in more than 90% of cycles (p<0.001). Utilization of routine blastocyst-stage culture increased again in all age groups (p<0.001), with more of it happening in women under age 40 than in older women. PGT usage (the data do not distinguish between PGT-M and PGT-A, with an overwhelming majority of cycles, however, being PGT-A cycles) increased 3-4-fold across all age groups (p<0.001). Moreover, by 2020, PGT was utilized in 40—50% of cycles in women under age 42.
Correctly, the authors suspected in their comments that the observed increases in all three IVF practices were interrelated with the rise of, in principle, the utilization of PGT-A. And this PGT-A-dependent trend in utilization has apparently continued beyond 2020. A more recent analysis of three time periods around 2022 revealed PGT-A utilization in the U.S. was already at 57.2%, 56.8%, and 56.2%.2 Recently published 2023 SART data reported a total of 169,783 oocyte retrievals and only 15,928 fresh embryo transfers, which represents only 9.8% of all cycles. This does not mean that over 90% of all U.S. IVF cycles included PGT-A (and, therefore, froze all embryos), but it clearly means that the percentage of PGT-A utilization must have further increased beyond the high 50s seen already in 2022.3
Considering the rapidly increasing literature which clearly demonstrates that none of the promised outcome improvements proponents of PGT-A have
claimed over more than 20 years with always new excuses for earlier failures, has to this day been confirmed (even finally also acknowledged by the ASRM/SART Practice Committees),4 these are astonishing changes are really difficult to understand. Since clinical research data actually should discourage the wide use of PGT-A in association with IVF, one can only conclude from these findings that U.S. IVF practice is following all the wrong financial incentives.
1. Claffey et al., J Assist Reprod Genet 2025;42:799-807
2. Hunkler et al., Fertil Steril 2025; ahead of print. https://www. fertstert.org/article/S0015-0282(25)00100-1/abstract?
3. ASRM. April 23, 2025. https://www.asrm.org/news-andevents/asrm-news/press-releasesbulletins/us-ivf-usage-increasesin-2023-leads-to-over-95000-babies-born/
4. ASRM/SART Practice Committees. Fertil Steril 2024; 122(3):421-434
The CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, recently criticized a paper by Italian investigators in Human Reproduction who, based on an extremely poorly designed study, incorrectly concluded that “all treatments of IVF cycles with growth hormone (GH) were useless.”1
His commentary on this paper was then published by Human Reproduction2 (see also Recent CHR publications on page 59), basically making two central arguments: GH benefits on ovarian function in principle are exerted through insulin growth factor-1 (IGF-1). Consequently, if IGF-1 levels in a patient are normal, there is no sense in administering GH. And there is, of course, even less purpose to testing whether GH is effective in improving IVF outcomes in infertile women with normal IGF-1 levels.
Now, Chinese investigators reported a prospectively randomized study including 128 women who in the past demonstrated “poor embryonic development” in IVF cycles, and in these women, an at least welldefined patient population – tested prospectively whether GH vs. no-GH made any difference in a subsequent IVF cycle.3 GH-treated women required significantly lower total gonadotropin dosages (p<0.006) and shorter stimulation (p<0.049). High-quality embryo numbers, however, did not
improve.. The investigators, however, did measure their patients' IGF-1 levels, and those in the lowest quartile, indeed, demonstrated a marginal improvement in higher quality embryos (p<0.049). Clinical pregnancies also numerically increased with GH supplementation from 38.5% to 46.25%, but, considering the relatively small study size, unsurprisingly, this difference was not statistically significant.
This was, of course, for several reasons – and mostly because of marginal power - anything but a perfect study, but – as already noted – the study included IGF-1 analyses and also involved pretreatment with GH in two cycles before IVF cycle start. This is important because IGF-1 exerts its ovarian effects at small growing follicle stages, and these follicles require at least 6-8 weeks of further maturation to reach gonadotropin sensitivity, which makes them receptive to gonadotropin stimulation in an IVF cycle. And in contrast to above above-noted Italian study, which really offered nothing but hubris, this study at least offers some hope for the still unproven hypothesis that in infertile women with low IGF1 levels, GH supplementation through at least approximately two menstrual cycles before IVF cycle start may improve IVF outcomes.
Unfortunately, the investigators allowed only women under the age of 40 to enter the study. This basically means that the observations reported are potentially only applicable to relatively younger patients. But, nevertheless, this is a potentially important paper with a tempered message, and in strong contrast to the rather obnoxious tone of the above-noted Italian paper1 that really had absolutely no basis for any of the claims it made.
REFERENCES
1. Mourad et al., Hum Reprod 2025;40:77-84
2. Gleicher N. Hum Reprod 2025;40(5):971-972
3. Tang et al., Reprod Biol Endocrinol 2025;23:42
What causes low functional ovarian reserve in women with chronic hepatitis B (positive surface antigen)?
A recent paper by Chinese investigators in BMC Medicine reported some very impressive – but at the same time difficult to interpret – results.1 Specifically, based on 38,861 infertile women in first IVF cycles,
the authors identified 1,574 with positive HBsAg. The latter group was matched with a hepatitis B-negative group of infertile women by age and BMI, and the here discussed paper compared IVF cycle outcomes in both groups.
Women with positive HBsAG demonstrated lower antral follicle count, lower AMH, higher FSH, required more stimulation, and produced fewer oocytes, including fewer MII oocytes. In contrast, e-antigen-positive and negative women demonstrated no differences. They thus concluded that HBsAg positivity significantly impairs a woman’s functional ovarian reserve.
We, however, have a hard time integrating this paper into what has already been known for quite some time about the impact of chronic hepatitis on IVF: As the article, indeed, points out in the discussion, there is considerable literature available which pretty uniformly reported no adverse outcomes from chronic hepatitis on IVF outcomes.2 If functional ovarian reserve were to be affected as described in the discussed paper, one would, however, expect an adverse outcome on IVF. Moreover, as the paper also points out, while there are various possible hypotheses that could explain a negative effect of the virus on functional ovarian reserve, none have been established. In short, we are not certain that this is a credible paper.
1. Li et al., BMC Medicine 2025;23:58
2. Wang et al., Fertil Steril 2019;112(2): 250-257.e1
The ASRM is starting a training program for embryologists, raising some important questions beyond just training
Everybody in the field, of course, knows that there is a substantial shortage of embryologists. On first impulse the recent announcement of the American Society for Reproductive Medicine (ASRM) that it was launching “a groundbreaking initiative designed to help alleviate the burden of training new embryologists,”1 called the Clinical Embryology Learning Laboratory (CELL, - how cute!), therefore, sounded like a very good idea.
Per this announcement, which was distributed to ASRM members on February 22, 2025,

“CELL is a 10-months structured curriculum, combining virtual and in-person didactic lectures, including 10 weeks of immersive, hands-on training at the state-of -the-art CooperSurgical embryology training center,” and this is where – in our opinion –the problem with this announcement starts and ends.


CooperSurgical is a very successful company that, in a very short time, has achieved an amazing market valuation on Wall Street. One, indeed, would go no wrong in calling the company today the likely most dominant supplier of goods and services to the infertility field, offering – per their own representation – over 600 clinically relevant medical devices used by women’s health care providers,2 one of the most widely used lines of embryo culture media, including the brands ORIGIO, SAGE, and LifeGlobal Media,3 and, of course, other embryology laboratory supply, from small disposables to large equipment items. And the company is also one of the largest providers of genetic testing services in the world, of course, including preimplantation genetic testing for aneuploidy (PGT-A).
The latter business also made the company one of the targets of class action suits by a consortium of plaintiff lawyers5 (see also the article by the lead lawyer of this group, Allison Freeman, JD, on page 5 of this
issue). And this is not the only area in which the company faces a class action lawsuit: After recalling supposedly defective embryo culture medium, a recent class action suit accused the company’s product of destroying embryos in the process.6
But it is these days difficult to be a company with a billion-dollar market valuation and, therefore, deep pockets, without having to face lawsuits. We, therefore, do not wish to be in any way judgmental regarding CooperSurgical, and the CHR is, indeed, a client of the company. The CHR, moreover, of course, has no opinion and does not take sides in any of the aforementioned class action suits.
We, however, nevertheless wonder about the ASRM’s offer to train embryologists at a CooperSurgical facility, which, of course, will train embryologists using the company’s instruments, supplies, culture media, and services, including such controversial services as PGT-A, and will do so in accordance with the company’s believes and representations –and allow us to suggest – will, like any corporation, see this as an opportunity to advance its corporate interests. And who could blame them!
But this announcement raises an even larger point, namely the increasing entanglement of the ASRM and its daughter society, the Society for Assisted Reproductive Technology (SART), with industry as well as Private Equity, which already controls over half of the country’s IVF cycles.
We fully understand and appreciate the partial financial dependency of our professional societies on these interest groups, but that should not, and cannot, result in selling out to them. One can already wonder about some activities, like above abovenoted CELL. But at times, inaction may be even more telling. An example was the 2024 combined ASRM/ SART Practice Committee Statement regarding PGT-A, which finally, and with considerable delay, correctly concluded that, to this day, PGT-A (in over 20 years) has, in IVF in general patient populations, demonstrated absolutely no outcome benefits.7
And – if this is the case - why did ASRM/SART, for example, not automatically conclude that routine IVF practice should stop the utilization of PGT-A? Who else but the ASRM/SART, except for a government
agency like the Food and Drug Administration (FDA), can make such an authoritative statement? And don’t we already have more than enough government involvement?
And, yet, ASRM/SART apparently don’t care that patients are, in ever bigger numbers, continuing to spend at least another $5,000 per egg retrieval out of pocket (because not a single insurance company covers PGT-A, - even if the insurance covers IVF) and, in doing so, in many cases are actually reducing their pregnancy chances because of not using and/or discarding embryos with false-positive results and still significant pregnancy chances.8 ASRM/SART, wake up!
1. ASRM. February 22, 2025. Via e-mail and https://www.asrm. org/asrm-academy/professional-engagement/cell-program/ 2. CooperSurgical. Instagram. https://www.instagram.com/ coopersurgicalmedicaldevices/?hl=en
3. CooperSurgical – https://www.coopersurgical.com/ procedures/integrated-embryo-culture-solutions/
4. CooperSurgical. https://www.coopersurgical.com/healthcareproviders/support-compliance/service/
5. Justice Law Collaborative. October 16, 2024. https://www. justicelawcollaborative.com/newsandupdates/press-release-classaction-lawsuits-filed-against-genetic-testing-companies-formisleading-consumers-about-pgt-a-testing-during-ivf-treatment
6. PGT-A class action McCroskey K. Newswire. February 4, 2025. https://www.classaction.org/news/coopersurgicalsrecalled-ivf-solution-destroyed-embryos-class-action-lawsuitalleges
7. ASRM/SART Practice Committees. Fertil Steril 2024; 122(3):421-434
8. Barad et al., Hum Reprod 2022;37(6):1194-1206
Can time-lapse embryo imaging using AI predict the ploidy of embryos?
It does not happen too often that Nature
Communications publishes a clinical article regarding IVF. And it is even rarer that such an article in this journal is poor and misleading. But, somewhat surprisingly, both of these things happened with the publication of a relatively recent paper, mostly from our colleagues down the street at Weill Cornell Medicine here in Manhattan.1
We, of course, have seen quite a large number of recently published papers that have alleged that their Artificial Intelligence (AI) programs could improve on standard embryo selection in IVF cycles, as offered by most time-lapse imaging systems currently
on the market. Frankly, none impressed us so far, not only because we so far have seen none which, credibly, really improved cumulative pregnancy rates from an embryo cohort obtained in an IVF cycle, but because even the best AI program will fail if there is not enough difference between the different choices to make a difference. And, as we recently tried to make the point,2 this – simply for biological and mathematical reasons - is really the case with all embryo selection methods, including AI. None of them can change the cumulative pregnancy and live birth chance of an embryo cohort. The best they can do, and even that only with luck and rarely, is to shorten the time to pregnancy to minor degrees.2
With this introduction, let’s get back to the WeillCornell paper, which not only claimed quality assessment of embryos as all of its predecessors and/ or successors we have seen have done insufficiently, but also claimed to be able to predict embryo ploidy. And that, of course, would make a huge difference and be an extremely valuable finding. The authors in the paper present BELA, which they describe as a “state-of-the-art ploidy prediction model that surpasses previous image and video-based models without necessitating input from embryologists.” And, using multitask learning, BELA – as the authors reported – achieved a “whopping” (meant facetiously!) 0,76 area under the receiver operating characteristic curve for discriminating between euploidy and aneuploidy.
This is, of course, a totally unacceptable level of accuracy to determine whether an embryo can be transferred or not, and, therefore, raises two questions: (i) Why was this paper submitted in the first place? And (ii) why was this paper accepted for publication?
Though the authors attempted to answer at least the first question by noting that BELA matches the performance of models trained on embryologists’ manual scores for such predictions, but that, of course, should not be a good enough reason for publication of this paper because morphological assessments of embryos by embryologists have, of course, proven absolutely worthless in distinguishing between euploid and aneuploid embryos. The authors furthermore acknowledged that BELA cannot even replace current PGT-A technology in predicting aneuploidy, and even if that does not offer any

outcome benefits for IVF.3
And then the authors make the totally unsupported claim that BELA “exemplifies how such (AI) models can streamline the embryo evaluation process,” and this is, of course, complete nonsense. If anything, this study demonstrated the current potential limits of AI in doing so! And this, of course, also means that we still do not understand why a prestigious journal, like Nature Communications, chose to publish this paper.
Which brings us to a very recent paper by CHR-friend and colleague, Zeev Shoham, MD, from Israel, in the new Journal of IVF Worldwide 4 The article offers a comprehensive review of AI in reproductive medicine, primarily focusing on AI tools DeepEmbryo, icONE, iDAScore, and ERICA, and making the point that AI is destined to transform assisted reproductive technologies in embryo selection, gamete assessment, personalized protocols, and cycle outcome predictions.
As already noted above, we do not necessarily share this opinion because most of these efforts are currently still based on the concept of embryo selection, which we consider to be the likely most harmful failed hypothesis in IVF practice since the birth of the Brown baby.2 The article, however, offers a kind of state-of-the-art review of AI in regard to infertility practice and, therefore, is worth reading.
1. Rajendarn et al., Nat Commun 2024;15:7756
2. Gleicher et al., Hum Reprod Open 2025;(2):hoaf011
3. ASRM/SART Practice Committees. Fertil Steril 2024; 122(3):421-434
4. Shoham Z. J IVF Worldwide 2025;3(2):1-8
The fact that IVF practice – like fashion – goes through cycles of new “ideas,” which then often very quickly and without proper validation studies become routine practice, has been a subject in the VOICE since its inception. The CHR, indeed, coined the term “fashion of the moment” for these new practice patterns, which then, often very quickly, turn into what British colleagues coined the term “add-ons.” One of these new “fashions of the
moment” is priming with medroxyprogesterone 17-acetate to prevent spontaneous ovulation during exogenous ovarian stimulation, so-called progestinprimed ovarian stimulation or PPOS, first proposed in 2015 by Chinese investigators.1
Now, another paper from China reported that in good-prognosis patients, PPOS adversely affected cumulative live birth rates and embryo quality when compared to GnRH analogues to prevent premature LH surges and ovulation.2 Though this study was performed in only good-prognosis patients undergoing PGT-A and unrecognized cofounders may very well be responsible for these findings, they, nevertheless, should induce some soul searching among those who, once again, obviously prematurely have jumped on the bandwagon of progestin priming. If this approach adversely affects outcomes in even good-prognosis patients, these adverse effects must be expected to be even stronger in poorer-prognosis patients.
REFERENCES
1. Kuang et al., Fertil Steril 2015;104(1):62-70.e3.
2. Zhou et al. J Clin Endocrinol matab 2025;110:611-623
Bacterial vaginosis is a very frequent diagnosis in women during their reproductive years and frequently reoccurs even after successful treatment. That such reoccurrences may be due to reinfections transmitted from the male partner has been known for ever and it, therefore, was somewhat surprising that a recent paper in The New England Journal of Medicine got an unusual amount of media attention when reporting that male-partner co-treatment with combined oral and topical antimicrobials reduced the rate of recurrence if women.
REFERENCES
1. Vodstrcil et al., N Engl J Med 2025;392(10):947-957
We are presenting this study, which is currently only a highly valued, reviewed preprint in the journal eLife, because it is one of the first studies to report on a potential connection between the seminal microbiome and semen quality as well as male fertility.1 Other studies have been published before, but mostly because of small sample sizes, different patient populations, and differences in data analyses have yielded varying results. And it appears that here presented study improved on prior ones in all of those criteria. Moreover, the study size was substantial, with 223 men enrolled, 63 men with proven paternity, 46 being the male partner in a couple with repeated pregnancy loss, 58 with male factor infertility, and 56 being the male factor in a couple with so-called unexplained infertility.
As expected, of course, high sperm DNA fragmentation, elevated ROS, and oligospermia were lower in men with proven paternity, in all patient groups, semen microbiota clustered in three major genera: (i) Streptococcus; (ii) Prevotella; and (iii) Lactobacillus and Gardnerella. Interestingly, the Prevotella genus had the highest microbial richness (p<0.001), alpha-diversity (p<0.001), and bacterial load (p<0.0001), but bacterial composition and/or load were not associated with semen analysis, ROS, or DNA fragmentation.
The conclusions of this study, therefore, were rather disappointing in that the only association made was that men with unidentified seminal Flavobacterium are more likely to have abnormal semen analyses. It increasingly appears that – except for gut microbiota – microbiota elsewhere in the body are not of great significance.
REFERENCES
1. Mowla et al., eLife https://doi.org/10.7554/eLife96090.3
Azoospermia/oligozoospermia and prostate cancer increased in families of women with primary ovarian insufficiency
Because non-obstructive azoospermia (NOA) and primary ovarian insufficiency (POI) demonstrate common genomic markers, they may also predispose to cancers. Utah investigators, therefore, hypothesized
that NOA or severe oligo-azoospermia and the risk of male cancers would be higher in families of women with POI.
And there was, indeed, an increase in risk of NOA/ severe oligo-azoospermia in relatives of women of women with POI. The risk in first-degree relatives was 2.8 (p<0.03); among second-degree, it was 3.1 (p=0.02), and 1.8 in 3rd degree 1.8 (p=0.03).
Families with POI and NOA/oligo-azoospermia also demonstrated an even closer association with prostate cancer risk, in first-degree relatives 3.5 (N.S. p=0.16); second-degree relatives 3.1 (p<00008) – likely a finding based on too few first-degree relatives.
The authors concluded that the data demonstrate excess familial clustering of severe spermatogenic impairment along with prostate cancer risk in relatives of women with POI, supporting a common genetic contribution to POI, spermatogenic impairment, and prostate cancer.
1. Allen-Brady et al., J Endocrine Soc 2025;9:bvaf030
The discussion about sperm DNA fragmentation continues
There is really no new data on the importance of sperm DNA fragmentation in the literature; another test that would qualify for the term “fashion of the moment,” since the evidence for it being clinically significant does not really exist. So why then the confusion?
Because of papers like the narrative review recently published by Greek colleagues for whatever reason in the International Journal of Molecular Science (does not sound like a journal with too much expertise in male infertility) which just offered yet another example for authors simply not understanding their own data or being just so biased and set in their opinions that they see any outcome of data as confirmatory of their thinking.
In the here discussed review paper, the 17 (!!!!) authors selected 28 publications for their review, among which only 14 “provided data regarding the impact of DNA fragmentation on seminal parameters, suggesting correlations between increased DNA fragmentation and significantly lower sperm count,

lower concentration, lower motility, and abnormal morphology. Fifteen papers offered data on how DNA fragmentation relates to reproductive outcomes. Among those studies, only 2 correlated higher fragmentation with higher aneuploidy rates, and only 7 with lower pregnancy rates and live birth rates.
And from these ridiculously low numbers of studies (a huge majority, of course, demonstrated absolutely no associations with DNA fragmentation results), the 17 authors concluded that, “ultimately these studies highlighted collectively the importance of measuring sperm DNA fragmentation in the assessment of male infertility.” Truly unbelievable, and clearly worth a “WORST PAPER IN ISSUE REWARD.”
And since we are already on the subject, Frontiers in Endocrinology recently published a “collection” of articles on the subject (we mentioned above in these pages already made the point that we are not big fans of Frontiers journals). Summarized in a brief editorial,2 the first research article concluded that high sperm fragmentation was associated with an increase (x 5.76) in early miscarriages due to embryo aneuploidy. The second paper in the series was, however, completely unrelated to sperm fragmentation. A third study confirmed what has been known for many years, namely that a quick second ejaculation often produces better quality semen than the first, including in sperm fragmentation parameters.
A first review concluded that testicular sperm may have lower fragmentation than ejaculated sperm, but also found that currently available data are too limited to reach conclusions. The second review, also including a meta-analysis of data from the literature, suggested that shorter abstinence periods between ejaculations improved sperm fragmentation results, suggesting only a 2-day abstinence period.
REFERENCES
1. Stavros et al., Int J Molec Sci 2024;25:10167. “WORST PAPER IN ISSUE REWARD”
2. Ribas-Maynou J. Front Endocrin 2025;16:1570774
The FDA issues warning letter to Sperm Bank, Inc., dba. Fertility Center of California in San Diego
If you are looking for donor sperm, this is relevant: The letter was issued after the FDA determined that, after issuing citations following inspectional observations, the response the agency received from the sperm bank was inadequate to address the agency’s concerns. After offering a very detailed listing of 4 failures to comply, the sperm bank was further advised in the letter from the Director of the Office of Compliance and Biological Quality at the Center for Biological Evaluation and Research that its owner, Martin D. Bastuba, MD, must take prompt action to correct the violations addressed in the FDA’s letter and prevent their recurrence. He was also advised that failure to promptly correct these violations may result in regulatory action being initiated by the FDA without further notice.
1. FDA. February 14, 2025. https://www.fda.gov/inspectionscompliance-enforcement-and-criminal-investigations/ warning-letters/sperm-bank-inc-dba-fertility-centercalifornia-694273-02142025
Adding pro-cumulin to a biphasic in vitro maturation (IVM) system modulates human oocyte and cumulus cell transcriptomes
We in the ART/IVF section of this literature review have already discussed the clinical aspects of IVM in PCOS and older women. Here we wish to point out a very interesting paper from a consortium of international investigators in Molecular Human Reproduction in which the authors present compelling data to suggest that pro-cumulin – a GDF9-BMP15 heterodimer – may increase cumulus cell and oocyte transcriptome regulation, thereby increasing the number of developmentally competent oocytes after biphasic IVM treatment (i.e., after short gonadotropin exposure and ovulation trigger).1
These data may very well offer a hint on how IVM results could be improved, and the CHR’s clinical investigators are already at work finding out.
1. Cava-Cami et al., Mol Hum Reprod 2025;31(1):gaaf001
Image-based identification and isolation of micronuclei and extracellular vesicles in reproductive medicine
The paper we are discussing here has nothing directly to do with infertility. Still, micronuclei are, suddenly, everywhere and – very likely – have an important function everywhere, including in reproductive medicine in general and infertility in particular. They, for example, have been reported to produce higher blastocyst formation rates if present in embryos at the 2-cell stage.1
Another already reviewed preprint, in eLife, therefore, attracted our attention because it reported on the possibility of machine-learning-based image analysis of micronucleated cells, which then allows for a better understanding of what processes they are involved in. Increased micronucleus frequency is, for example, a hallmark of cancer development and aging, and micronuclei are potent drivers of genomic structural changes, are proinflammatory, and signal metastasis as well as senescence.2
Similarly, extracellular vesicles are suddenly everywhere and – also – have been associated with innumerable physiologic as well a pathologic interventions. They, for example, have been shown to be involved in implantation.3 We strongly suspect that micronuclei and extracellular vesicles in the near future will be demonstrated to play important roles in reproductive physiology and – probably – also pathology. Stay tuned, new technology allows for amazing things!
1. Yao et al. Eur J Obstet Gynecol Reprod Biol 2024;302:26-32
2. DiPeso et al., eLife 2025; https://doi.org/10.7554/ eLife.101579.2
3. Chen et al., Front Endocrinol (Lausanne) 2022;13:809596
A paper from Columbia University here in NYC (yes, they do not only demonstrate in support of Hamas!) in Nature Aging could really become a milestone paper for the infertility field as much as for aging in general. The paper presents a very comprehensive singlenuclei multi-omics atlas of ovaries of four individuals at a young age (23-29 years) and of four women mostly beyond reproductive age (49-54 years).
What they found is obviously only a start, but it can form the basis for fascinating research. Here is what they reported in their Nature Aging paper: Across all cell types, they found coordinated changes in transcriptomes and chromatin accessibilities with aging. Especially – and not as a surprise - the mTOR signaling pathway turned out to be very prominent in the ovary. In the aged ovary, the transcription factor CEBPD appears to play a significant role in practical all cell types of the ovary.1
Moreover, integration of their multi-omics data with genetic variants found at natural menopause suggested a global impact of functional variants on gene regulatory networks across all cell types in the ovary. We are anxiously waiting for and expecting follow-up studies. The biggest question of them all is, of course, how do we stop the aging process, and not only in the ovaries.
1. Jin et al., Nature Aging 2025;5:275-290
Especially because of their associations with breast (69% lifetime) and ovarian cancer (15% lifetime) risks, BRCA1&2 genes are very important in reproductive medicine. Especially BRCA2 is, however, well-established clinically actionable, as a recent article in Nature magazine described the gene1 for predisposing toward several other cancers as well, including prostate and pancreatic cancers. BRCA2, however, has so far over 5,000 different variants, with many of uncertain significance in their predictability for the various cancers.

This is why a recent paper by Chinese investigators is of so much importance because they strived to, finally, be able to classify these thousands of variants. Without going into the technical details how they accomplished this amazing feat, they succeeded in assigning 6,959 out of 6,960 (i.e., all but one variant) to seven categories of pathogenicity, with 91% of variants being classified as pathogenic or likely benign or as benign or likely benign and only ca. 9% remained unassigned. As the authors noted, these new assignments should greatly improve the advice and treatment of individuals with BRCA2 variants.1
1. Huang et al., Nature 2025;638:528545
A new understanding of why women may generally age better than men
It is no secret that women live longer than men. Some claim that women are more resistant to cognitive decline than men (consider President Biden!). U.S. investigators from several universities now may have found another reason why women are doing so much better, and it may have to do with their second X chromosome, the so-called “silent” or “inactivated” X chromosome (Xi). Or to be more specific, reactivation of the silent Xi gene may be the secret weapon.
As it turns out, aging remodels transcription on the Xi as well as the active X chromosome (Xa) in the brain across hippocampal cell types and does it more on the two X chromosomes than on autosomes. What this practically means is that select genes on Xi underwent activation, including in the cells of the so-called dentate gyrus, which is critical to learning and memory. The authors make the valid point that a better understanding of how Xi may confer the observed female advantage in age could be used to counter brain aging in both sexes.1
While this study is, of course, fascinating, and we would hope the authors are correct in their attribution to the Xi, we are at several levels somewhat skeptical: (i) We still fail to understand how all of this would affect longevity? (ii) We also wonder why evolution would prolong life expectancy in this way while shortening reproductive capacity in the same sex. Wouldn’t one expect from evolution the opposite? (iii) The evidence for more resistance toward cognitive
decline in women is not well established. Indeed, women have twice the incidence of Alzheimer’s,2 though that is often attributed to their longer lifespan.
In short, let’s wait and see!
1. Gadek et al., Sci Adv. 2025;11(10):eads8169
2. Beam et al., J Alzheimers Dis. 2018;64(4):1077-1083
Organoids have revolutionized research in biology in general and in medicine specifically. They are self-organizing cell structures of various cell lineages which, basically, can, to a large degree, mimic diverse tissues and even organs and, therefore, can serve in the study of basic biology, for example, embryology, and in the study of specific diseases. They also have demonstrated potential utility in regenerative medicine. Nature Medicine recently published a very comprehensive review article on the clinical applications of human organoids. It makes fascinating reading.1
REFERENCES
1. Verstegen et al., Nat Med 2025;31:409-421
We don’t have much to report in general gynecology in this issue of the VOICE, except for the fact that an important nationwide prospective cohort study of contemporary hormonal contraceptives (mostly birth control pills) demonstrated increased risk for arterial thrombotic events. Legacy media, as well as social media, have, however, been surprisingly quiet regarding these findings.
about
It was left to Danish investigators and the British Medical Journal (BMJ) – usually one of the politically most woke medical journals around – to publish a so-called “real world,” nationwide, prospective cohort study of currently in use hormonal contraceptives
that demonstrated a significant increase in strokes and myocardial infarction in users of these contraceptives.1
Apparently, nobody wants, however, to talk about this study. A quick Google search showed that the JAMA and New England Journal of Medicine reported on the study, but among major newspapers and magazines, only U.S. News & World Report published an article on the subject.2 And almost nothing but deadly silence otherwise from legacy media as well as social media.
We can only guess why: it must be a concern about yet another big “right-wing conspiracy” after the Dobbs vs Jackson Women’s Health Organization decision of the Supreme Court that terminated Roe v. Wade and relegated abortion decisions back to the states. There is simply no other explanation for avoiding discussions about this important study but concern that some on the political right may use this study to attack the current liberal use of contraceptives.
As the BMJ correctly noted in a summary of what was and was not known before publication of this study, observational studies and meta-analyses, even before this study, already suggested an increased risk of arterial thrombotic events with hormonal contraceptive use, but findings were inconsistent and often based on outdated studies. Evidence on the effects of mode of administration, estrogen type, progestin type, and duration of use was, moreover, lacking. And the BMJ also correctly summarized the findings of the Danish study by concluding that this nationwide study found that contemporary estrogenprogestin and progestin-only contraceptives – except for the levonorgestrel-releasing intrauterine device - were associated with an increased risk of arterial thrombotic events, by doubling them from ca. 1% to 2%. The highest risk estimates were observed with estrogen-containing products. Somewhat surprisingly, duration of use did not seem to influence the risk.
As the article noted, it is estimated that at least 245 million women worldwide use hormonal contraceptives. A doubling of risk from 1% to approximately 2% would, therefore, mean approximately an additional 2.5 million cases of stroke or myocardial infarction in women worldwide. Wouldn’t it make sense, not to prohibit hormonal contraceptives, of course, to talk about this more openly? Instead of silence, this important study
should be used to emphasize to physicians and to inform the public that women at special risk for thrombotic arterial events should use nonhormonal contraceptives, - except, of course, for the levonorgestrel-releasing IUD or, hopefully, other nonhormonal contraceptives the pharma industry may now develop following this report.
1. Yonis et al., BMJ 2025;388:e082801
2. Mundel E. U.S, News & World Report. February 13, 2025; https://www.usnews.com/news/health-news/articles/2025-02-13/ certain-birth-control-pills-devices-linked-to-higher-heart-risks
It finally looks like the interest in menopause research is increasing, and it is time! Two papers attracted our interest: In the first, Canadian investigators reported on the interplay between age at menopause and synaptic integrity on Alzheimer’s disease risk, and they reported a very significant interaction between age at menopause and synaptic integrity when it came to faster cognitive decline and elevated tau. These relationships were furthermore attenuated if women took menopausal hormone therapy. It, thus, appears that endocrine processes at midlife (or their sequelae) may affect synaptic vulnerability to Alzheimer’s, suggesting that timely interventions in hormonal factors and synaptic health could improve resilience against Alzheimer’s in women.1
A second paper by Swedish investigators investigated in a case-control study whether menopausal hormone therapy affected the risk of developing systemic lupus erythematosus (SLE) and systemic sclerosis (SSc), classical multi-organ autoimmune diseases.2 943 SLE and 733 SSc patients revealed a highly significant associated risk between menopausal hormone therapy and SLE as well as SSc. Moreover, the highest risk association was found in women who receive both systemic and local treatment. These associations remained after adjustments for socio-economic factors, further strengthening the widely held hypothesis that female hormones play a significant role in the much higher prevalence of autoimmune diseases in women than men.
1. Wood Alexander et al., Sci Adv 2025;11:eadt0757
2. Patasova et al., Rheumatology (Oxford) 2025; 64(6):35633570)

Especially considering that this paper comes (with some Australian participation) out of China, where we are used to very large study participant numbers, this has to be considered a small study. But the patient population chosen for this retrospective observational study (with, therefore, obvious limitations) is interesting, offering in many ways a surprisingly wellcontrolled outcome experience.1
The study, involving treatment cycles between 2016 and 2023, includes 140 women with various causes of infertility who previously experienced two or more pregnancy losses (including at least one following an IVF cycle). They now underwent blastocyst warming (i.e., thawing of previously cryopreserved blastocyststage embryos). Among those patients, 72 had undergone PGT-A in this thaw cycle on a total of 274 blastocysts, and 74 women went directly to embryo transfer without PGT-A.
The fact that the choice for or against utilization of PGT-A was not randomized and, indeed, goes in the manuscript mostly unexplained is, indeed, the most important weakness of this paper (there are also other weaknesses). Using generalized estimating equations with some cofounding adjustments, the primary study outcome (and principal reason why this study is of interest) was the cumulative live birth rate.
Ages, gravity, and number of prior pregnancy losses did not differ between the two study groups. As one would expect, the PGT-A group, however, showed more prior aneuploidies in pregnancies (68.1% vs. 39.2%; p< 0.001). No other statistically significant differences were, however, apparent, though the PGT-A group, again as expected, had marginally more blasts cryopreserved (median 4 vs. 3; P=0.06)
The study findings were as follows: 14/72 (19.4%) had no euploid embryos for transfer, in itself an important finding, considering the young age of the
PGT-A group of 34.9±5.0 years. All tested blastoids, indeed, demonstrated only a 48.6% euploidy rate. The cumulative live birth rate was significantly lower in the PGT-A group (25/72, 34.7% vs. 39/74, 52.7%; P=0.048). Secondary outcomes, including individual cycle live birth rates and miscarriage rates, however, did not differ.
Here reported difference in cumulative cycle outcomes, of course, reached significance only barely, but considering the relatively small study size, this is not surprising. As already noted, this study has substantial design shortcomings beyond those already mentioned and including the long study enrollment period of seven years during which undoubtedly substantial practice changes were introduced at the IVF clinic where the study was performed. But the study is, nevertheless, informing because it reports on cumulative outcomes, and that is what, ultimately, matters in every IVF cycle – fresh or frozen-thawed.
Once an embryo cohort has been established, this cohort has, in principle, an unchangeable cumulative outcome (unless, of course, the laboratory or physicians are incompetent). Though still widely advocated by many colleagues and much of the genetic testing industry, the believe that PGT-A may influence this cumulative outcome, as in these pages repeatedly discussed before, is simply ridiculous! It is now well established – and even confirmed by a recent ASRM/SART Practice Committee Opinion2 – that PGT-A does not improve IVF cycle outcomes and does not, as shown again here, even in repeat aborters, reduce miscarriage rates to significant degrees.
All PGT-A, in the best of all circumstances, therefore, can achieve is a marginally shorter time to pregnancy. But, as discussed, the study also demonstrates that the outcome benefit is only rarely and only in the bestprognosis patients achieved. Much more frequently, as again shown in this paper, PGT-A actually adversely affects the cumulative pregnancy chances of patients. We, therefore, can only again and again repeat the next logical question: Why then perform PGT-A at all at an additional out-of-pocket expense of at least $5,000?
1. Cai et al., Reprod Biol Endocrinol 2025;23:31
2. ASRM/SART Practice Committees. Fertil Steril 2024; 122(3):421-434
The place of prenatal diagnosis after preimplantation genetic testing for aneuploidy (PGT-A) of embryos?
This is an interesting question, somewhat surprisingly only very sporadically raised in the literature in the past and addressed as a societal recommendation in the JARG by – out of all candidate organizations – the Italian Society of Human Genetics.1 This society is obviously a genetics society and not an Ob/Gyn or even fertility-related society, even though Italy has more of the latter than most other countries. Italy has, likely, also the most aggressive IVF practice community in Europe when it comes to promoting PGT, and especially PGT-A in IVF cycles, even outbidding Spain.
One of the leading voices of this community, Antonio Capalbo, PhD, is, indeed, a co-author of here addressed opinion paper. He is with two co-authors listed as having conceptualized the paper and with one co-author to have initiated the drafting of the recommendations (!!). Interestingly, he, however, lists no potential conflict of interest in the publication, even though Google lists him as the Chief Scientific Officer (CSO) at Juno Genetics, one of the world’s

largest commercial PGT (preimplantation genetic testing) laboratories, - per its website offering laboratory services in the U.S., Spain, U.K., and Italy. This is especially important to understand as background since the document makes such blatantly incorrect statements as: “The main indications for PGT-A are advanced maternal age
(over age 35), repeated implantation failure and multiple spontaneous abortions. The document also incorrectly notes that, “the main advantage of this analysis (i.e., PGT-A) are reduction of time to reach pregnancy and reduction of chromosomal-abnormal miscarriages and (therefore) pregnancy terminations.” The document, indeed, also claims that “regardless of age, PGT-A is also recommended in cases of PGT-M in order to maximize the probability of obtaining a full-term pregnancy.” A recent ASRM/SART combined opinion, of course, concluded otherwise, when finding that PGT-A to this day has not found any clinical utility in association with IVF.2
Astonishingly, the opinion paper also describes PGT-A as a test “with high specificity” (i.e., low false positive rate, <5%) and still describes the prevalence of “mosaicism” at blastocyst stage as “rare.”
The term mosaicism is here in parentheses because, as repeatedly discussed before in the VOICE, the PGT-A industry’s definition of ”mosaicism” is biologically incorrect since it refers only to the presence of more than one cell lineage in an on average 5-6-cell embryo biopsy, while the biologically correct definition refers to the prevalence of more than one cell lineage in a complete organism, i.e., the complete blastocyst. This incorrect definition of mosaicism explains the obviously incorrectly low false positive rate noted in this document because multiple 5-6 cell embryo biopsies – with each producing <5% positive results - would, of course, produce a much higher real cumulative mosaicism rate.
But, considering how much PGT-A is utilized in association with IVF, not only in Italy and the U.S., all of this, of course, does not devalue the basic question of what should be the prenatal diagnostic followup after transfer of an allegedly “euploid” embryo. Moreover, with increasing numbers of IVF clinics now also offering selected embryo transfers with socalled “mosaic” embryos, the question appears even more timely.
The document addressed obstetrical follow-up to PGT-M (preimplantation testing for monogenic diseases), PGT-SR (testing for parental structural chromosomal abnormalities), PGT-A (testing for chromosomal abnormalities), but did not address PGT-P (polygenic risk screening of embryos). Because little controversy exists regarding PGT-M and PGT-SR, we restrict our comments here to what the document has to say regarding PGT-A.

Here are the document’s recommendations, accompanied in bold by the CHR’s comments reflecting the center’s practice pattern:
Since the risk of fetal aneuploidy after a euploid embryo transfer has been alleged to be lower than the risk in the general prenatal population, a standard pregnancy follow-up is usually recommended, including for women of advanced reproductive age.
We (and the ASRM)2 disagree that transfer of an euploid embryo affects IVF cycle outcomes but agree that the pregnancy should be treated with routine obstetrical care.
NIPT (non-invasive prenatal testing) is not indicated, as circulating cell-free fetal DNA has the same embryological origin as the tissue investigated in PGT-A.
We disagree. If an NIPT would be indicated in a spontaneous pregnancy, it is also indicated here.
The detection of presumed chromosomal mosaicism in the few cells of the biopsy may not reflect the constitution of the entire embryo, nor can it predict its viability.
We agree.
Laboratories that perform PGT can decide whether or not to report the finding of presumed mosaicism in the final PGT-A report. This decision must be communicated to the couple during the pre-test counselling, together with the parameters used to define an embryo suggestive of mosaic and what threshold the laboratory has established to define a high- or low-grade mosaic.
This, in our opinion, inappropriately places the burden of reporting genetic testing results on the patients at a time when they can have absolutely no idea how many embryos they will have for transfer.
The European Society for Human Reproduction and Embryology (ESHRE) recommendations suggest that a threshold lower or higher than 50% should be used to define the degree of low- or high-grade mosaicism, respectively.
This is an arbitrary cut-off with no hard data to support, when the biology is, of course, gradual. The CHR, therefore, - obviously with appropriate informed consent – transfers selective “highmosaic” and even as “aneuploid” reported embryos. As pregnancy and live birth chances will decline with increasing mosaicism, “aneuploid” transfers will, of course, have the lowest pregnancy and live birth chances. But chances are not zero and, therefore, warrant such transfers before going to egg donation. The CHR has seen (and reported) several normal pregnancies and deliveries following “aneuploid” embryo transfers.3
Due to the high diagnostic inaccuracy and uncertainty of mosaicism on samples of just a few cells, it is not possible to attribute a diagnostic value to the finding of embryonic mosaicism. It is suggested to use more appropriate terminology, such as pseudomosaicism, apparent mosaicism, or presumed mosaicism.
We would agree, but have not seen any PGT-A laboratory using any other term but “mosaicism.”
It is not possible to consider an embryo with apparent low-grade mosaicism following PGT-A as aneuploid. Of course not, they have been demonstrated to basically have almost identical pregnancy and live birth chances to embryos reported as “euploid.”
It is not recommended to perform a new IVF cycle if the couple still has embryos with presumed lowgrade mosaicism available for transfer. It is not recommended to discard embryos with a presumed low degree of mosaicism.
We agree.
It is not recommended to proceed with a second biopsy of embryos with a low degree of presumed mosaicism to confirm their chromosomal status. We agree.
Given the heterogeneity in the quality metrics adopted by various laboratories, discriminating between a presumed low-grade mosaic and a technical artefact may not always be possible. In these instances, the laboratory may be led to report as “low-grade mosaic” profiles that present suggestive deviations in correspondence of specific chromosomes because they showed low-quality profiles.
Convoluted and basically not understandable.
Contradicting its own above pointed out statements, the document also notes that all published studies have highlighted a high reproductive potential of embryos with presumed mosaicism, which, in blind prospective studies even equivalent to that of euploid embryos. Interestingly, the Italian society's opinion offers the position of ESHRE on the subject, a document in which Antonio Capalbo, PhD, again was the second author and which, quite obviously, was the source of the Italian document.4
The CHR which already in 2015 was the first IVF center in the world to report chromosomally normal pregnancies after transfer of by PGT-A as “abnormal” reported embryos (we started offering such transfers under an experimental protocol in collaboration with two other IVF clinics in New York City already in 2014) likely offers transfers of more “abnormal” embryos than any other IVF clinic in the U.S. or abroad and – in absence of guidelines – had to develop its follow-up policy after transfer of allegedly “abnormal” embryos in house. The policy basically followed two rules: (i) Patients who conceive are treated age-appropriately, which these days means that everybody has a NIPT at ca. 9-10 weeks gestational age. As long as the NIPT confirms a chromosomal normal pregnancy, no further prenatal testing is required if the transferred embryo is euploid, though CVS or amniocentesis is offered. (ii) Patients who had allegedly “abnormal” embryos transferred, whatever the abnormalities, also have an NIPT at 9-10 weeks, but are recommended to have a CVS or amniocentesis even if the NIPT suggested a chromosomal normal pregnancy.
Two special circumstances deserve special mention: If a NIPT is positive, the CHR always recommends an amniocentesis as the most accurate follow-up test, and
we have seen confirmation of chromosomal abnormal pregnancies, but have also seen normal amniocenteses after positive NIPT (i.e., a false-positive NIPT). The CHR, therefore, never recommends pregnancy termination after positive NIPT alone.
The second circumstance may be almost unique to the CHR because of the “abnormal” embryos the center is willing to transfer, and it involves the occurrence of a miscarriage after transfer of a chromosomal “abnormal” embryo, whatever the abnormality may have been. In such cases, the assumption usually is that the miscarriage was caused by the chromosomal “abnormal” embryo that was transferred. In many cases, that may, indeed, have been the case when we karyotyped the products of conception.
But so far, we have already seen three documented cases where the products of such miscarriages revealed absolutely normal karyotypes, suggesting that the pregnancy loss was not chromosomal, even though the pregnancy was the result of an allegedly chromosomal “abnormal” embryo. These cases demonstrate the importance of infertility practice of always karyotyping products of conception after miscarriages.
1. Grati et al., J Assist Reprod Genet 2025;42:1015-1024
2. ASRM/SART Practice Committees. Fertil Steril 2024; 122(3):421-434
3. Barad et al., Hum Reprod 2022;37(6):1194-1206
4. ESHRE Working Group on Chromosomal Mosaicism. Hum Reprod Open 2022;4(hoac044
5. Gleicher et al., Fertil Steril 2015;104(3):e59
And since we were already talking about noninvasive prenatal cell-free DNA (cfDNA) screening (NIPT), here are a few words about a review article in the Journal of the Endocrine Society, which discussed discrepancies between sex prediction and fetal sex results after NIPT.1 The article noted that based on better performance and higher sensitivity as well as specificity than the former practice of biochemical markers screening, the American College of Obstetricians and Gynecologists and American College of Medical Genetics and Genomics

recommend NIPT screening for trisomy 21, 18, 13, and sex chromosome aneuploidy for all pregnant women. cfDNA, however, also offers information about fetal sex chromosomes, as the paper noted, a highly desired piece of information for many parents. Moreover, information about sex can also help in managing X-linked diseases. cfDNA-based sex prediction and appearance of fetal genitalia by prenatal ultrasound scan or at birth have, however, not always coincided raising concerns about a fetuses/ infant’s potential atypical sex development, in this politically very correct paper (referring to pregnant people rather than pregnant women) described as a difference in sex development (DSD).
The review then outlined principles and limitations of cfDNA technology, summarizing recent findings related to cfDNA test performance in the prediction of sex chromosome abnormalities and DSD conditions. The review also attempted to define the technical and biological causes of discrepant results, provide recommendations to consolidate efforts by prenatal and clinical management teams in challenging situations, and discuss ethical considerations associated with fetal sex prediction and prenatal DSD diagnosis.
Without going into further detail, this review basically reemphasizes the point made in the preceding section: NIPT is not perfect and can give false-positive as well as false-negative results, which may also apply to the two sex chromosomes. Though rare, this is an interesting paper to read for those rare occasions.
REFERENCES
1. Witchel et al., J Endocrine Soc 2025; 9:bvaf007
The increasing problem of cannabis use in pregnancy
As repeatedly addressed in these pages, with legalization in most states, the use of cannabis among pregnant women has significantly increases. Today, we offer some new observations in recent publications. A group of behavioral and psychiatric investigators on the West Coast recently published a study involving
no less than 356,343 pregnancies between 2011 and 2022. It determined whether preconception and prenatal cannabis use affected nausea and vomiting during pregnancy (NVP).
What they found was not surprising, starting with the degree of cannabis use preconception (11.3%, of that 2.7% used it daily, 2.4% weekly, and 6.3% monthly or less) and prenatal 6.5%, and, comparable in frequency: 0.7%, 0.7%, and 1.4% respectively.1 3.7% of patients had unreported positive toxicology.
3.6% of patients were diagnosed with severe and 16.0% with mild NVP. Self-reported preconception daily cannabis use was associated with greater odds of mild and severe NVP when compared with no use, as was self-reported weekly use and selfreported prenatal daily cannabis use compared with no prenatal use compared with individuals without prenatal use.
And now a quick switch to what cannabis use in pregnancy does to offspring based on an Australian study.2 As one would suspect, the news is not good: The investigators in a linkage cohort study investigated 222,600 mother-child pairs for maternal cannabis use disorder (CUS) and the risk of disruptive behavioral disorders (DBDs) in offspring, and children exposed to CUD had – after adjustments for covariates – 3 times increased risk of DBDs. CUD, as the authors suggested, therefore must be viewed as an independent predictor of childhood DBD risks, reemphasizing the need for interventions to reduce cannabis use among reproductive age women.
U.S. state and federal legislators, we have a problem!
REFERENCES
1. Young-Wolff et al., Obstet Gynecol 2925;e145(5):p:519-522
2. Tadesse et al., Psych res 2025;346:116404
Decidualization resistance in women with a history of severe preeclampsia
The Carlos Simon Foundation now starts providing the infertility field with interesting research papers at a quite steady pace. We are impressed!
The newest paper by investigators from the Foundation in Spain and with contributions from scientists at the University of California in San Francisco is an interesting paper in Nature Medicine, 1 which introduces us to the concept of endometrial decidualization resistance, which we learn is implicated in several obstetrical and gynecological conditions, including preeclampsia. Looking at 11 endometrial samples from patients with severe preeclampsia and 12 control samples, they found preeclampsia-associated shifts in cell composition with a stromal mosaic state, characterized by proliferative stromal cells alongside decidualized cells with concurrent epithelial mosaicism and a dearth of epithelial-stromal transition associated with decidualization. Additional observations using other multi-omics indicated disrupted responses to steroid hormones, especially estrogen.
To be honest, the paper is somewhat overwhelmed in the amount of data produced, even though patient numbers were somewhat small, and one is almost forced to ask, so what? Yes, we have a better understanding of decidualization resistance, but – practically – in what way do these new insights advance our understanding of preeclampsia or change prevention and/or treatments?
REFERENCES
1. Muñoz-Blat et al., Nat Med 2025; 31:502-513
Pregnancy-induced hypertension (PIH) and future autoimmune diseases
It is by now well accepted that several immune mediators, including complement proteins, cytokines, and innate as well as adaptive immune cells, play a role in the regulation and elevation of blood pressure.1 That pregnancy-induced hypertension also may be, in some way, linked to immune system function and/or dysfunction at the time, has, especially when it comes to preeclampsia, also been suspected for decades. Taiwanese investigators now took this oftenbefuddling association a step further by basically wondering whether pregnancy-induced hypertension may have some commonality with autoimmune disease risk.
Working with health care records from 102 health care organizations with 131 million patient records between 2006 and 2020, they tried to assess risk for
developing autoimmune diseases between the ages of 16 and 45. To determine risk, the investigators established two study groups: women with pregnancyinduced hypertension (PIH; i.e., gestational hypertension, preeclampsia/eclampsia) and a normotensive control group in pregnancy (women with autoimmune disease and/or hypertension and with complications of pregnancy before 20 weeks of gestation were excluded). The primary outcome of the study was risk of autoimmune disease within an 18year follow-up.
Pregnancy-induced hypertension was found in 13.4% of women. Those with PIH demonstrated a significantly higher risk of developing later in life an autoimmune disease (HR 1.87, 95% CI 1.60-2.18), including diseases like multiple sclerosis, Addison’s disease, antiphospholipid syndrome, inflammatory bowel disease, and mixed connective tissue disease. Moreover, this risk increased with the severity of pregnancy-induced hypertension.
Though the in the paper presented data are interesting, the authors, in our opinion, missed half the message of their paper. They, of course, understood that part of the message that suggested an increased lifetime risk for autoimmune diseases in women with PIH history, but they overlooked the fact that – as repeatedly before discussed in these pages – pregnancy and autoimmunity share significant structural commonality through the physiological fact that both circumstances are dependent in the establishment of immune tolerance: pregnancy in tolerance toward the paternal allogeneic haplotype and autoimmunity on the tolerance of “self.”
And the involved tolerance pathways share common denominators since certain autoimmune diseases greatly improve in the mid-trimester of pregnancy when pregnancy tolerance of the fetal semi-allograft peaks, only to diminish toward the end of pregnancy and end with delivery of fetus and placenta, a period when autoimmune diseases, therefore, tend to flare. Famous British rheumatologists in the 1970s, therefore, described pregnancy as the perfect “model” for the study of autoimmune diseases!
1. Harrison DH, Patrick DM. Hypertension 2024;81:1659-1674

More information on what causes preterm labor
Spontaneous labor before 37 weeks of gestational age is considered “premature.” According to the most recent CDC data for the year 2022, the rate declined from 2021 by 1% to 10.4%. But premature birth rates also greatly varied between Black (14.6%), Hispanic (10.1%), and White women (9.4%).1 Premature labor, therefore, is a major – and maybe the major - problem in worldwide obstetrical practice. And infertile women, by definition, are at increased risk for premature deliveries.2
Though thus clearly associated with several risk factors, what induces labor – whether at term or prematurely – in not yet well understood, though it appears increasingly likely that initiation of labor –except under traumatic conditions, usually is always the consequence of an abatement in maternal-fetal tolerance by the maternal immune system, which in turn induces pro-inflammatory lymphokines and cytokines.3
Within such a context, a recent paper in the American Journal of Obstetrics & Gynecology by Czech investigators attracted our attention, which investigated regulatory T cell numbers in spontaneous preterm labor.4 Seven women experienced spontaneous preterm labor between weeks 23 and 33, while 36 control patients delivered at term. Women with preterm labor demonstrated significant reductions in all analyzed regulatory T cell subpopulations preceding the onset of premature labor. Regulatory T cell soaffected were: CD4+CD25+FoxP3(p=0.0217); CD4+CD25+FoxP3+CD45RA, p<0.0216; CD4+CD25+FoxP3+ Helios+, p<0.0260; CD4+CD25+FoxP3+CD39-,p<0.0427
REFERENCES
1. CDC Maternal Infant Health. November 8, 2024. https:// www.cdc.gov/maternal-infant-health/preterm-birth/index.html
2. Sanders et al., Reprod Health 2022;19:83
3. Yockey LJ, Iwasaki A. Immunity 2018;49(3):397-342
4. Koucky et al., Am J Obstet Gynecol 2025;232:222.e1-11
Ending at least some of the many rumors surrounding the causes of autism
The reported increase in autism over the last few decades has led to a rather frantic search for its causes. Robert F. Kennedy, Jr, the new HHS
secretary, even pledged to “find” the environmental causes of autism by September of this year.1 Relevant to this burgeoning issue, two investigators from NYU recently published an interesting paper in Nature Medicine, which is definitely worth reading because the study refutes a common wisdom about autism.
It is currently widely accepted that a number of maternal conditions in pregnancy are associated with autism risk in offspring. Their study, using data from more than a million children, indicated that such causalities are extremely unlikely. They instead – much more likely – arise from genetic and other familial factors.2 And if the complete article is too much to read, the authors also published a summary in the form of a Research Briefing in the same journal.3
1. Seitz A. AP. April 17, 2025. https://apnews.com/ article/robert-kennedy-autism-cases-health-secretaryca210c5c37e12d6377a1af16ae4f4fbc
2. Khachadourian et al., Nat Med 2025;31:996-1007
3. Janecka M, Khachadourian V. Nat Med 2025;31:749-750
What happens when chemotherapy becomes necessary in pregnancy?
There is a good reason why the CHR mandates mammograms in women above age 40 (or even at younger ages in some women with strong breast cancer family histories) before fertility treatments are instigated: A breast cancer diagnosis in the middle of pregnancy often mandates heartbreaking binary decision making between best interests of mother and offspring. In addition, we have found this policy also to be very effective, because these mammograms detect at the CHR every year several unexpected cancers. As we also insist on follow up of abnormal PAP smears and other historically relevant issues in a new patient’s take-in consultation, the CHR every year also makes other cancer diagnoses: We, for example, just diagnosed unexpectedly before cycle start a very early endometroid cancer in a still very young woman, pointing out that this problem, of course, is not only restricted to breast cancer; every cancer diagnosis during pregnancy creates often almost unsurmountable problems and demands difficult decisions.
A Canadian study published in the Journal of the National Cancer Institute (JNCI) now addressed the issue of cancer chemotherapy in pregnancy and how it affects pediatric outcomes, and the news was not all bad.1
Out of 1150 cases from Canadian cancer registries, 142 (12.3%) received chemotherapy during pregnancy. Exposure to such chemo was associated with a higher risk of severe neonatal morbidity and mortality, but – interestingly – not with neurodevelopmental disorders and disabilities or complex chronic conditions. Of all severe neonatal morbidities and mortalities, 75% and 100%, respectively, were associated with preterm births at less than 37- and 34-week gestational age, respectively. In short, outcomes of children born after pregnancies involving maternal chemo in general appear to have a relatively favorable outcome after all, even if women receive the chemotherapy during pregnancy. However, preterm births are, of course, very common and likely contribute to increased rates of adverse neonatal outcomes.
Unfortunately, the study was, however, severely underpowered to differentiate between different chemotherapies. By throwing all possible chemotherapy treatments into one basket, one should not and cannot expect much reliable revelation when the complete study involves only 142 cases.
1. Metcalfe et al., JNCI. 2025; 117(3):554-561
If there is a medical subject, legacy and social media have not overlooked, then it is the high maternal mortality rate in the U.S. Bur even though the rate improved in 1923 to 669 deaths in comparison to 817 in 2022; i.e., it went from 22.3 per 100,000 live births to 18.6 per 100,00 live births, still a quite abhorrent rate in comparison to most other so-called developed countries.1 Figure 1 (see right) reprinted from a Healio article on February 1, 2025, demonstrates the difference in maternal deaths per 100,000 births, and the differences are truly embarrassing.2 Even our neighbor, Canada, demonstrates less only slightly above one-third the U.S. rate.
Unfortunately, the country has not made any inroads into these numbers in many years. There are likely many explanations, some social, others economical, and yet others a simply poor medical system providing obstetrical care to a very diverse patient population. That U.S. mothers are getting older (also discussed elsewhere in this issue of the VOICE) also does not help. Neither does the politicization of the subject, when the Healio article, for example, states that a “key piece of the puzzle is inequity.”
While inequity may play a role, like many of above above-noted associations and many more not addressed here, the fact that Blacks have the highest morbidity and mortality is not only restricted to poor Blacks. A 2023 New York Times article pointed this fact out:3 Black women are three times more likely to die during pregnancy or in the postpartum period related to pregnancy than White women, and these differences persist through education as well as income levels. Black women with college degrees still have 1.6 times the mortality of White women.
We therefore have to acknowledge that with all the research by government, academia, foundations, etc, we still do not fully understand the high maternal mortality in the U.S., and that is a shame.
1. Hoyert DL. CDC, National Center for Health Statistics. https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2023/ maternal-mortality-rates-2023.htm#:~:text=In%202023%2C%20 669%20women%20died,rate%20of%2022.3%20in%202022.
2. Bascom E. Healio. February 14, 2025. https://www.healio. com/news/primary-care/20250214/it-is-no-wonder-the-us-hasa-maternal-mortality-crisis-heres-why-and-what-can-be-done
3. The New York Times. https://www.nytimes.com/ interactive/2023/02/12/upshot/child-maternal-mortality-richpoor.html
4. Commonwealth Fund, June 4, 2024. https://www. commonwealthfund.org/sites/default/files/2024-06/Gunja_ MaternalHealth-InternationalComparison_PR.pdf
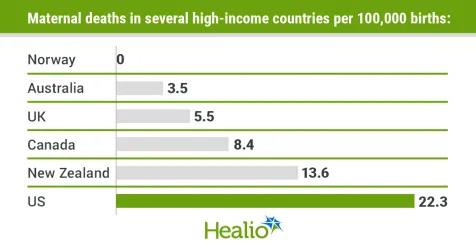

We have a frequently saying at the CHR: “We don’t like inflammation.” What we mean by making this point is that chronic inflammation is one of the three major causes for why a woman’s immune system may be in a hyperactive state (the other two are autoimmunity and allergies, but obviously often intermingled with inflammation). And what we really mean by making this statement is that we don’t like hyperactive immune systems in our patients because women with hyperactive immune systems often have difficulties in establishing and maintaining the required immune tolerance toward the paternal semiallograft, called an embryo and that means trouble for normal female fertility, often also including increased miscarriage risk.
It is, unfortunately, rare that other colleagues in the field think along similar lines, and it is even rarer when colleagues write a paper addressing these issues. But this is exactly what two Israeli colleagues from the Hebrew University in Jerusalem just did with an excellent review in Reproduction, which, in so far as an unprecedented fashion, summarized the effects of chronic inflammation on female fertility.1 We, therefore, very strongly recommend reading this article in full.
The article notes that chronic inflammation causes serious medical conditions in many organs and tissues and affects female fertility. It has a negative impact on oocyte quality, folliculogenesis, hormone production, immune signaling, and other processes that affect fertility. Inflammation, of course, also plays important roles in the battle against pathogens, even has roles in human reproduction and development, and tissue homeostasis. However, when it becomes chronic, it can become a serious medical problem. The article also discusses possible mechanisms by which adverse effects on fertility may be handled and how interventions may mitigate the effects of chronic inflammation. The effect of chronic inflammation is tightly correlated with and resembles the effect of aging, drawing interesting parallels between these processes.
1. Ameho S, Klutstein M. Reproduction 2025;169:e240197
If you have never heard about IgG4-related disease (IgG4-RD) or diseases, you are not alone. This is a (or are several) relapsing fibroinflammatory, immunemediated disorder(s) that can affect a variety of organs. Since the year 2000 has been recognized as a single disease and can be very difficult to diagnose. The etiology is not well understood, except for the fact that an overactive immune system leads to inflammation in a variety of organs. When the pancreas is involved, the condition is often also referred to as autoimmune pancreatitis (AIP-1).
The disease occurs in women of all ages and men mostly between the ages of 50 and 70. In women, it can often mimic cervical and uterine cancer.1 The disease can also affect the ovaries, in which case the findings are dense fibrosis, obliterative phlebitis, and lymphocytic and plasma cell-rich infiltrates that contain abundant IgG4-positive plasma cells.2 It often presents as a tumor-like growth and is most common in salivary glands, the pancreas, and the retroperitoneum.
So far, the condition has no improved therapy. A recent paper in The New England Journal of Medicine, however, promises that Inebilizumab may be an effective treatment.3 It reduced the risk of flares and increased the likelihood of flare-free complete remission at 1 year, thereby confirming the role of CD19-targeted B-cell depletion as treatment for IgG4-RDs. Inebilizumab is a humanized monoclonal antibody that binds and depletes CD19+ B cells, including plasmablasts and plasma cells.
REFERENCES
1. Pacyna et al., Gyn Oncol Rep 2023;45:101137
2. Akyol et al., Turk Patoloji Derg 2021;37(1):63-66
3. Stone et al., N Engl J Med 2025;392:1168-1177
Did you know that there exists a neuroimmune connectone?
We found a recent article in Nature magazine fascinating because it informed on the fact that the nervous and immune systems have complementary roles in the adaptation of organisms to environmental changes. It pointed out that he mechanisms that mediate crosstalk between the nervous and immune systems, called neuroimmune interactions, are poorly understood and then summarized advances in the understanding of neuroimmune communication, with a principal focus on the central nervous system (CNS), especially its response to immune signals and the immunological consequences of CNS activity. The article then, in addition to other relevant subjects, highlights these themes primarily as they relate to neurological diseases, the control of immunity, and the regulation of complex behaviors.1
More evidence for the Epstein-Barr Virus (EBV) connection with multiple sclerosis?
Multiple sclerosis (MS) is, of course, a classical autoimmune disease. Swedish and U.S. investigators from Stanford University in California recently reported in PNAS a rather strong impact of the EBV tatt, likely greatly affecting the immune microenvironment in MS lesions.2 Spatial relationships with glial cells and neurons may have significant potential consequences for disease progression and potential therapeutic interventions. Especially in more aggressive subtypes of MS, the investigators found EBV-related markers enriched in MS lesions, which may drive sustained inflammation (see opposite page) and may disrupt the blood-brain barrier. The findings of this paper further strengthen the connection between the EBV and MS and suggest antiviral and immune-modulatory therapeutic strategies for MS, which, combined, could mitigate inflammation and neuronal damage.
A recent article in Healio Rheumatology argued that recent advanced in our understanding of RA have been nothing but extraordinary and are laying the groundwork for new therapeutic strategies.3 And while the article, indeed, lists several relatively new insights into the disease, paradoxically, the talk is still about what “may” work, and what “may be done” in the future. Treatment, though with increasing use of biologicals very obviously progressed, is still anything from convincing in its specificity and effectiveness.
Here, with the same optimism expressed in the preceding article about RA, an article in Medscape Medical News claims that new ideas about the pathogenesis of PsA may drive new treatments.4 Here, the news is, however, to some degree, indeed, revolutionizing since over the past year, new evidence has emerged in support of the idea that psoriatic arthritis (PsA) is neither exclusively immune-mediated nor a classic autoimmune disease. Both mechanisms may, indeed, be essential in disease pathogenesis, and it is innate immune cells that possess adaptive properties that may lead to worsening of inflammation of the skin and joints.
PsA, thus, joins psoriasis, ankylosing spondylitis, and Crohn’s disease in a group of diseases that might be triggered and sustained by both autoimmune and other immune-mediated events. What then is the difference? Typical autoimmune diseases must be characterized by specific autoantigens and autoantibodies responding to them (i.e., anticitrulline antibodies in RA), while in an immunemediated disease, immune cells are profoundly dysregulated, but (at least so far) no specific autoantigens have been recognized. We have in infertility a very good example for this, namely the occurrence of immune-related ovarian failure, which has been for decades closely associated with autoimmunity in affected patients. Yet, a specific ovarian autoantigen has not been identified (except in women with Addison’s disease).

These findings, therefore, may have major relevance to female infertility.
1. Wheeler MA, Quintana FJ. Nature 2025;638:333342
2. Orr et al., PNAS 2025;122(11):e2425670122
3. Volansky R. Healio Rheumatology. February 21, 2025. https:// www.healio.com/news/rheumatology/20250220/advancesin-rheumatoid-arthritis-pathogenesis-nothing-short-ofextraordinary
4. Kirkner MR. Medscape Medical News. January 7, 2025; https://www.medscape.com/viewarticle/new-ideas-psapathogenesis-may-drive-new-treatments-2025a100009g
Have Israeli investigators really discovered a new part of the immune system with significant clinical implications?
This is at least what the BBC claimed,1 referring in a recent report to a paper in Nature2 that suggested that researchers in Israel discovered a part of the immune system that can be a goldmine for potential antibiotics, so-called proteasomes.1 In this paper, the investigators uncovered a previously unknown role for proteasomes (until now believed to mostly have only a role in antigen presentation on major histocompatibility complex class I for T cell-mediated immunity through proteasome-derived peptides).
Their role lies in the constitutive and bacterialinduced generation of defense peptides that impede bacterial growth both in vitro and in vivo by disrupting bacterial membranes. In silico prediction of proteome-wide proteasomal cleavage, moreover, identified hundreds of thousands of potential proteasome-derived defense peptides with cationic properties that may be generated on the way to degradation to act as a first line of defense.
The investigators also demonstrated that bacterial infection induces changes in proteasome composition and function, including PSME3 recruitment and increased tryptic-like cleavage, enhancing antimicrobial activity. Proteasome-cleaved peptides, thus, may have previously overlooked functions downstream of degradation. As the authors suggested, proteasome-derived defense peptides, therefore, could provide an untapped source of natural antibiotics for biotechnological applications and therapeutic interventions in infectious diseases and in immunocompromised conditions, an obviously very
welcome development, considering the sparsity of new antibiotics.
1. Gallagher J. BBC. March 5, 2025; https://www.bbc.com/news/ articles/cpv4jww3r4eo
2. Goldberg et al., Nature 2025;639:1932-1041
And COVID is still with us... General News
Though the sporadic return of outdoor seating areas with the arrival of warmer temperatures in NYC is this time fortunately not caused by COVID-19, COVID is still with us. And we apparently have a new variant (again coming out of China) slowly assuming dominance all over the world. It is called the NB.1.8.1 variant, and by the WHO is designated as a “variant under monitoring.”1
The CDC swabs travelers at random in order to monitor viruses entering the country and has already picked up the new variant in late March, with cased reported in California, Hawaii, New York, Ohio, Rhode Island, Virginia, and Washington as of approximately May 28, 2025. Since the new variant is still part of the Omicron family, immunity from recent vaccines and recent infections should still apply.
And then there was, of course, the expected controversy when it comes to vaccinations, which everybody expected with the appointment of Robert F. Kennedy, Jr, as the new secretary of HHS when he, likely prematurely, announced that the COVID vaccine would no longer be recommended for healthy children and pregnant women.2 But it did not take too long for even his own CDC agency to contradict him.3 And ACOG, of course, disagreed with Kennedy’s statement that vaccination was no longer recommended for pregnant women or women who intended to conceive.4 Similarly, the ASRM is continuing to recommend vaccination, as does the CHR, though we recognize the patient’s right to decide.
Rheumatologists have expressed concern about too broad Long COVID definitions.5 They specifically raised concerns about the 2024 definition of Long COVID from the National Academies of Science, Engineering, and Medicine (NASEM), citing both a lack of specificity and the inclusion of autoimmune rheumatic diseases despite inconsistent evidence.
An interesting short article in Nature magazine summarized our lessons COVID-19 taught the world about the human immune system:6 (i) antibodies aren’t everything; T cell responses are also important. (ii) Early alarms in the immune system spread far; interferon responses, for example, were found all over the body. (iii) The nose knows; COVID taught us to appreciate local immune responses, in this case, in the nose. And (iv) Causes of post-viral illness; Long COVID reemphasized the previously questioned concept of long-term post-viral syndromes.
1. Park A. Time. May 28, 2025. https://time.com/7289133/newcovid-variant-nb-181/
2. Goodman B. CNN Health. May 27, 2025. https://www. cnn.com/2025/05/27/health/covid-vaccine-pregnant-womenchildren-recommendation
3. REUTERS, May 30, 2025. https://www.reuters.com/business/ healthcare-pharmaceuticals/us-cdc-keeps-recommendationcovid-vaccines-healthy-kids-report-says-2025-05-30/
4. ACOG. May 27, 2025. https://www.acog.org/news/newsreleases/2025/05/acog-statement-on-hhs-recommendationsregarding-the-covid-vaccine-during-pregnancy
5. Tucker ME. Medscape Medical News. February 12, 2025. https://www.medscape.com/viewarticle/rheumatologistsconcerned-broad-long-covid-definition-2025a10003ll
6. Ledford H. Nature 2025;638:19-20
Concerned about another major national disease outbreak, the noise surrounding Avian Influenza appears to have become much more subdued. After concerns about transmission into cattle and domestic cats,1 and – of course – infections in humans,2 the CDC advised expedited influenza subtyping in hospitalized patients with flu-like symptoms to identify Bird Flu cases earlier.3 Another sign that we may have reached the end of the Bird Flu scare is, of course, declining egg prices, closely followed as a
1. Naraharisetti et al., Morbidity Mortality Weekly Report 2015;74(5)61-65
2. Garg et al., N Engl J Med 2025;392(9):843-854
3. Bock A. JAMA 2025;333(9):741-742
4. McMillan A. Procurement Magazine. February 12, 2025, https://procurementmag.com/supply-chain-management/efficioon-rising-cost-of-eggs
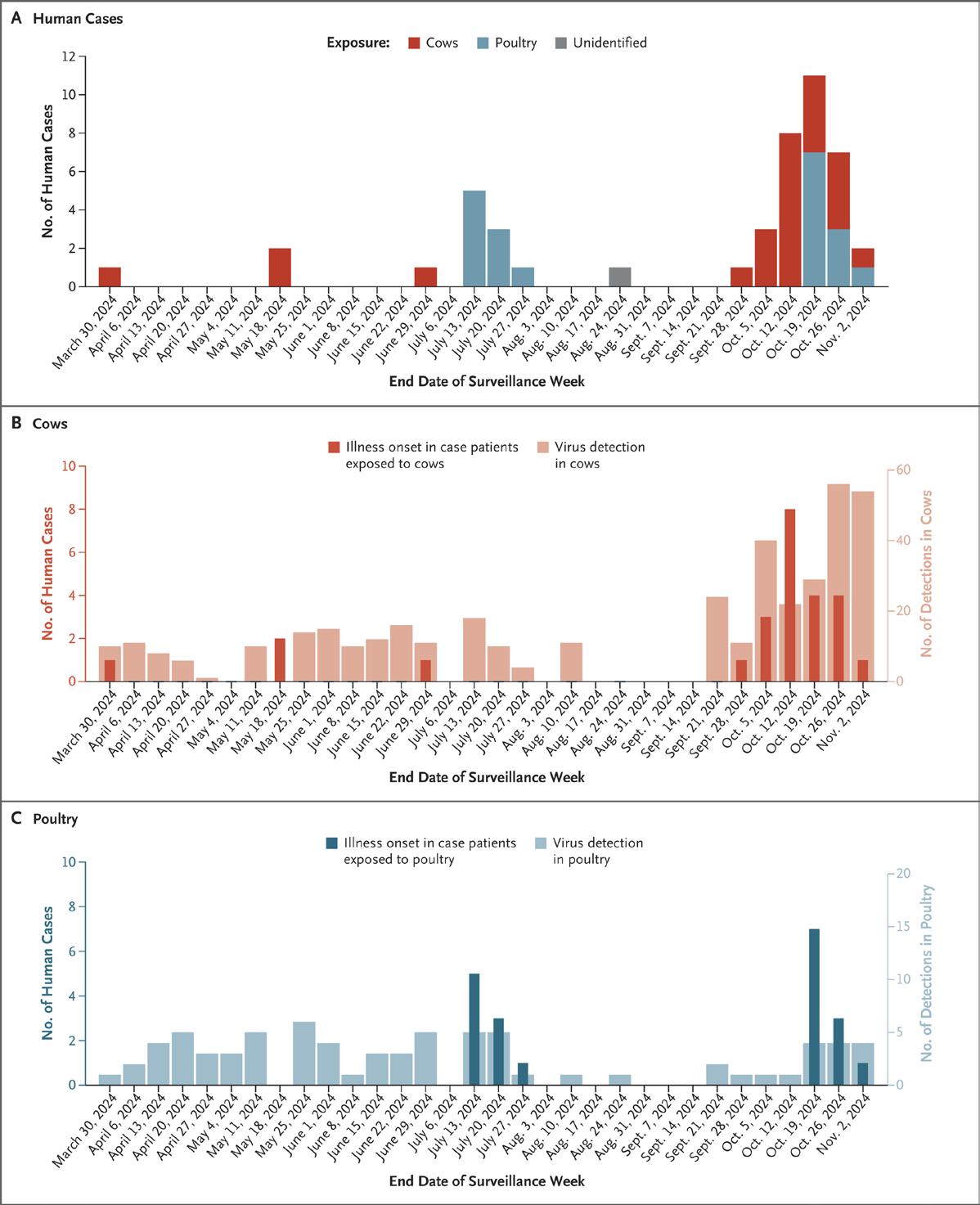
Human H5N1 cases by illness date, and number of infected dairy cows and poultry3




