By Norbert Gleicher, MD, Medical Director and Chief Scientist at The Center
for Human Reproduction in New York City. He can be contacted through the VOICE or directly at either
ngleicher@thechr.com
or ngleicher@rockefeller.edu
BRIEFING: In an initially rather unbelievable discovery, a consortium of Canadian, U.S., and international investigators have published a bombshell paper in Science magazine, demonstrating that the hypothalamic-pituitary-gonadal axis is not what everybody thought it was. Really unexpectedly, this paper revealed that a paracrine myokine called myostatin (also called growth differentiating factor 8, GDF8 and GDF11), which in several species (including humans) has been demonstrated to regulate muscle mass, also acts as a hormone that—in a mouse model—directly affected pituitary follicle stimulating hormone (FSH) synthesis and, therefore, indirectly ovarian function. This kind of FSHstimulating function has so-far exclusively only been attributed to other members of the transforming growth factor-ß family, so-called activins. These findings have to be considered revolutionary because they suggest a previously unknown endocrine axis between muscle and pituitary gland. Moreover, they may also mean that increases in muscle mass because of antagonism to myostatin may have adverse consequences on fertility.
*Articles were originally published in the Reproductive Times.
If there is one hormone we “fertility-experts” have believed we know and understand, it is, of course, follicle stimulating hormone (FSH). It, after all, is what we measure in every one of our patients and it is what we administer to almost every one of our patients. But—lo and behold—it now appears that even when it comes to FSH, we still have a lot to learn. A large consortium of investigators have published a fascinating paper in which they—based on investigations in several mouse models—demonstrated thatmyostatin, a member of the transforming growth factor-ß (TGFß) superfamily, also called growth differentiating factor 8 (GDF8), controls FSH secretion by the pituitary.1 Myostatin is produced by skeletal muscle and blocks the muscle’s cells’ growth and differentiation, and ends up affecting what has been known as the classical endocrine feed-back loop of the pituitary, releasing in response to hypothalamic gonadotropin releasing hormone, FSH and luteinizing
hormone (LH). Those two hormones then in female and male gonads produce steroid and nonsteroid hormones, which feedback on the pituitary, thereby inhibiting FSH production. The latter step of inhibition involves the hormone inhibin, in the female produced by granulosa and in the male by Sertoli cells.
The paper’s accompanying Commentary summarized the here- discussed study, identifying the “crosstalk” between peripheral muscle and this most basic hormonal loop feedback, a finding with potentially highly important consequences for fertility, as increasing muscle mass—consequently—may adversely affect fertility.2 Though unmentioned in paper and Commentary, this observation, of course, makes us immediately think about the female marathon runner who loses her menstrual pattern, to this point widely attributed to her loss of all bodyfat.3 Including the inhibitory function of myostatin
on pituitary FSH production athlete-amenorrhea may now have to be viewed as potentially having a multifactorial etiology. Concerns about fertility are, of course, limited to reproductive years.
As the Commentary also noted, myostatin levels— like FSH—increase with advancing female age, suggesting that rising myostatin may also contribute to rising FSH levels as women are getting older.2 As the authors of the Commentary further speculate, antagonists to myostatin, therefore, may benefit older people by increasing muscle mass, which—again left unmentioned—has become an increasingly relevant issue these days with the explosive growth in the utilization of PLG-1 receptor-agonists for weight loss in both sexes which with prolonged use leads to loss of muscle mass.4
That the hypothalamic-pituitary-gonadal axis in females deserves expansion is, of course, an argument made for many years by investigators at NYC’s CHR, pointing out the effect of adrenal androgen production on ovaries and the still-unaddressed mystery of why adrenal glands—which share an embryonic primordium with ovaries—demonstrate the highest density of ant-Müllerian hormone receptors after ovaries.5 That this expansion, however, would involve tissue like skeletal muscle outside of what traditionally have been viewed to be reproductive organs, is, however, of course more than unexpected and opens up new avenues which can be expected to redirect our current research emphasis on individual organs to a more comprehensive whole-body approach.
This paper, moreover, addressed an even more important unmentioned question which in recent years, because of so many unexpected developments in science, has become increasingly obvious: Why is science still always surprised when forced to recognize that what was considered established biological fact in reality is only the surface noise of a much more complex physiological system underneath? For one simple reason alone, we, indeed, should expect this to be the case: Every complex system—whether a rocket we are planning on sending to the moon or to Mars, or any biological entity—us humans included—would simply not exist were it dependent on single processes which are not backed up by multiple redundancies. Because science until recently never considered this fact (and one wonders how many scientists to
this day publish their discoveries daily as “isolated” phenomena, as if they were not part of universally multifactorial processes), we used to believe that every gene has only one function, or consider noncoding DNA, until just a few years ago believed to be a useless wasteland of DNA; or who cared about microvesicles which suddenly are seen everywhere fulfilling enormously important functions. Or how about what used to be called specks or micro-blobs, now called biomolecular condensates to reflect their increasing importance in cell physiology, also— suddenly—everywhere and just recently the subject of a beautifully illustrated article in Scientific America.6
The here discussed paper, therefore, maybe as its most important contribution, offers further evidence for the increasingly obvious notion that the more we know, the less we, indeed, know! And in many ways, this—at least for scientists—should be a very exciting conclusion.
1. Ongaro et al., Science 2025;387(6731):329-336
2. Steenwinkel T, Pangas SA. Science 2025;387(6731):249-250
3. Chen et al., Ann Transl Med 2023;11(2):132
4. Prado et al., Lancet Diabetes Endocrinol 2024; 12(11):P785-787
5. Gleicher et al., J Clin Endocrinol Metab 2017;10290;3569=3570
6. Ball P. Scientific American. February 2025.; pp 23-27

the balancing act between federal and state reproductive policies and their possible impact
David H. Barad, MD, MS, is Director of Clinical IVF and Research and a Senior Scientist at the
through the editorial of ice of the VOICE.

CHR.
He
can be reached
BRIEFING: In the first weeks of the new administration, President Trump has passed executive orders that will impact reproductive issues. 1,2,3 At times encouraged by often inflammatory comments in the media, some patients have become fearful that these or future rulings could affect their access to infertility services, especially in vitro fertilization (IVF). We here, therefore, briefly review what steps federal and state governments in reality have taken and how, if at all, those might affect fertility care.
*Articles were originally published in the Reproductive Times.
To start, it must be clearly stated that, currently, there exists no federal policy that restricts access to fertility care for members of the general public. Following the Supreme Court’s 2022 Dobbs decision overturning Roe v. Wade, the Biden administration issued Executive Orders 14076 and 14079 which actually expanded access to reproductive healthcare services, including contraception, maternal healthcare, emergency pregnancy and miscarriage care, and abortions. Interestingly, fertility services were, however, not included in these protections.
Upon reassuming office, on January 24, 2025, President Donald Trump signed Executive Order 14182, titled "Enforcing the Hyde Amendment," revoking the Biden administration’s previous Executive Orders 14076 and 14079, thereby announcing a clear shift in federal reproductive health care policy, potentially reducing certain protections and access to all above-named services.
But—again noteworthy—fertility services, once again, were not included.1
The restrictions announced by the Trump administration, thus, will undoubtedly impact general Ob/ Gyn practices, but do not in any way directly affect infertility care. There is, however, one exception affecting only members of the armed forces: As of January 31, 2025, the Department of Defense no longer reimburses service members for outof-state travel to obtain reproductive healthcare services that are not covered by TRICARE (health insurance of active service members and their families)—including in vitro fertilization (IVF). This policy reversal rescinds a directive from October 2022 that previously allowed such reimbursements.4
It is also important to note that— like other federally-funded health programs including Medicare and Medicaid—TRICARE never covered IVF, except in cases where an
individual’s infertility was military service-connected, as, for example, if it was caused by a combat injury. This change, however, clearly increases for all other service members seeking IVF the overall financial burden by adding related travel expenses. On a side note, because TRICARE never covered most fertility services, the CHR for many years has offered active-duty members of all branches of the U.S. military significant discounts for all fertility treatment-related costs.
The 2022 Dobbs decision overturning Roe v. Wade, of course, returned all regulations regarding abortion services back to the States. This led in February 2024 to a rather unconventional ruling of the Alabama Supreme Court, which suggested that frozen embryos under the state's wrongful death statute must be considered "minor children."5
Considering the potential legal consequences from such a bizarre
ruling, several clinics, including the University of Alabama at Birmingham Health System, unsurprisingly in their responses, immediately ceased all IVF-related operations.6 Prompted by concerns over access to fertility treatments, former President Donald Trump publicly urged Alabama lawmakers to protect IVF services, emphasizing his strong support for their availability. To address these legal concerns, the Alabama legislature swiftly passed a law granting full civil and criminal immunity to IVF providers for the loss or destruction of embryos during standard procedures.
Following the enactment of this law in March 2024, all Alabama clinics resumed their IVF services. Alabama is, however, not alone in having potentially IVF-restricting laws on the books. Louisiana, for example, has long-standing laws granting personhood rights to embryos, which have placed specific restrictions on in vitro fertilization (IVF) practices within the state. Since 1986, Louisiana law has recognized a viable in vitro fertilized human ovum as a "juridical person," affording it certain legal rights and protections (see below).7
LA-RS 9 §129: A viable in vitro fertilized human ovum is a juridical person which shall not be intentionally destroyed by any natural or other juridical person or through the actionsof any other such person.
Consequently, patients and fertility clinics in Louisiana are unable to dispose of surplus embryos locally. Patients who choose not to retain their excess embryos must transfer them to facilities in other states where disposal is legally permitted.
Due to opposition from the state’s powerful anti-abortion lobby, in May 2024, legislation aimed at ensuring the continued legality of IVF treatments in Louisiana was shelved.8 Anti-abortion lawmakers, who hold majority control in the Louisiana legislature, refused to remove language defining embryos as "human beings" from the bill. Louisiana Right to Life, the state’s largest anti-abortion organization, indicated it would likely oppose the bill without this language.
The concept of "fetal personhood" is a legal doctrine, from the moment of conception granting embryos the same rights as living individuals. The President’s recent executive order stating that federal agencies recognize only two sexes—male and female—as determined at conception and asserting that these sexes are immutable, has by some been interpreted as support for the concept of “fetal personhood.”9
Given President Trump's strong support for the widespread availability of in vitro fertilization (IVF)—even suggesting it should be available "for free"—it is likely that he does not endorse interpretations that would restrict IVF practices. This is also supported by the just released Executive Order on February 18, 2025, with the title, Expanding Access to In Vitro Fertilization,” which stated the following:
“Today, many hopeful couples dream of starting a family, but as many as one in seven are unable to conceive a child. Despite their hopes and efforts, infertility struggles can make conception difficult, turning what should be a joyful experience into an emotional and financial struggle.
My Administration recognizes the importance of family formation, and as a Nation, our public policy must make it easier for loving and longing mothers and fathers to have children.
In vitro fertilization (IVF) offers hope to men and women experiencing fertility challenges. Americans need reliable access to IVF and more affordable treatment options, as the cost per cycle can range from $12,000 to $25,000. Providing support, awareness, and access to affordable fertility treatments can help these families navigate their path to parenthood with hope and confidence.
Therefore, to support American families, it is the policy of my Administration to ensure reliable access to IVF treatment, including by easing unnecessary statutory or regulatory burdens to make IVF treatment drastically more affordable.
Within 90 days of the date of this order, the Assistant to the President for Domestic Policy shall submit to the President a list of policy recommendations on protecting IVF access and aggressively reducing out-ofpocket and health plan costs for IVF treatment. "
However, the debate over when an embryo attains human status lies at the intersection of abortion issues and IVF. Some anti-abortion advocates argue that life begins at conception, the moment of fertilization, and therefore, embryos should be granted legal protections and the rights of minor children from that point onward.
From a scientific standpoint this is, however, an untenable argument since natural conception also involves the “wastage” of a large majority of embryos. The best evidence is that even at peak fertility in their mid-20s, couples do not conceive every month they attempt to. It, indeed, takes on average about 3.4 months to conceive, even though a young couple at peak fertility can be expected to produce on average one embryo every month. In other words, even at peak fertility, over two-thirds of human embryos do not lead to implantation and pregnancy. How can they then be considered to deserve the rights of children?
If all embryos were to be legally regarded as persons, freezing, or failing to implant them could then, of course, be considered neglect, abuse, or even wrongful death. Fetal personhood laws, therefore, could criminalize standard IVF practices.
Project 2025 is a conservative policy agenda developed by the Heritage Foundation and allied organizations prior to the last election campaign. Despite denials by President Trump during the campaign of any association with this document, his administration has already implemented many policies that align with the Project 2025 agenda. Many executive actions, indeed, even closely mirror Project 2025's proposals, with some containing almost identical language.10
Unfortunately Project 2025’s agenda also includes strong advocacy for fetal personhood11 and, therefore, potentially contradicts President Trump’s own pronouncements in favor of expanded IVF utilization in the country as well as his recent Executive Order of February 18, 2025.3
During his 2024 presidential campaign, former President Donald Trump expressed strong support for in vitro fertilization (IVF), suggesting that the federal government or insurance companies could cover the associated costs. Interestingly this was also the solution Sean Tipton, MD, Chief Advocacy and Policy officer of the ASRM, expressed in an official response of the ASRM to the Executive Order when stating: “There is a fix to this problem: Require health insurance plans to cover IVF for patients who need it.12
At an August 29, 2024, town hall event in La Crosse, Wisconsin, he stated, "We want to produce babies in this country, right?" and emphasized his commitment to making IVF treatments accessible.13, 14 At the March for Life rally on January 24, 2025, President Trump basically reaffirmed his administration's prolife stance when reaffirming that, "we will again stand proudly for families and for life,"14 suggesting that he considers a pro-IVF position aligned with a pro-life position.
His advocacy for accessible IVF treatments, therefore, suggests he may—in contrast—not be fully aligned with the view that life starts at fertilization, as standard IVF procedures usually involve the creation and potential disposal of multiple embryos. This nuanced stance, however, well reflects his administration's emphasis on "common sense solutions" in reproductive health policy.
This conflicting stance between supporting IVF access and, at least to a degree, the anti-abortion movement, highlights a fundamental tension in reproductive policy. While promoting IVF funding could expand fertility options, enshrining fetal
personhood in law at state level could simultaneously restrict or criminalize standard IVF practices. This, of course, creates uncertainty for patients, providers, and policymakers alike.
Which brings us to the so-called Dickey–Wicker Amendment, also the subject of the following article in this issue of the VOICE. It is the name of an appropriation bill rider attached to a bill passed by United States Congress in 1995, and signed by former President Bill Clinton, which prohibits the United States Department of Health and Human Services (HHS) from using appropriated funds for the creation of human embryos for research purposes or for research in which human embryos are destroyed.15 The Amendment is a rider and attaches since its initial passage in 1996 automatically annually to the Labor, Health and Human Services, and Education appropriations bills and, therefore, automatically renews without debate.
As a result of complete lack of government funding for IVF research, advancements in IVF have largely relied on private funding and patient contributions. This reliance on non-federal sources has, of course, limited the scope and scale of potential advancements in IVF research.
As the following article specifically argues, if the Trump administration indeed wants to be supportive of IVF, it could finally terminate the Dickey–Wicker Amendment to make federal funds available for research that could advance IVF procedures. This would, of course, require an act of Congress.
1. Executive Order 14182—Enforcing the Hyde Amendment. (2025, January 24). Federal Register, 90(20), 87518752. https://www.federalregister.gov/ documents/2025/01/31/2025-02175/ enforcing-the-hyde-amendment
2. Trump reinstates 'Mexico City policy' ban on funding international abortions. (2025, January 24). Catholic News Agency. https:// www.catholicnewsagency.com/ news/261809/trump-reinstatesmexico-city-policyBan-on-fundinginternational-abortions
3. Executive Order Expanding Access for In Vitro Fertilization. https:// www.whitehouse.gov/presidentialactions/2025/02/expanding-access-toin-vitro-fertilization/
4. Associated Press. (2025, January 31). Pentagon strips travel reimbursement for troops seeking abortions, fertility treatment. AP News. https://apnews.com/article/ a18ce5dc08b654bfbcc147a4965ec470 https://doi.org/10.1093/jlb/lsad001
5. Associated Press. (2024, February 16). Alabama Supreme Court rules frozen embryos are children. AP News. https://apnews.com/article/alabamasupreme-court-frozen-embryoschildren-161390f0758b04a7638e2dde a20df7ca
6. Ginod, P., & Dahan, M. H. (2024). Embryos as unborn children: The Alabama Supreme Court's ruling and its possible impact for legal rulings in other states. Journal of Law and the Biosciences, 11(1), lsad001. https:// doi.org/10.1093/jlb/lsad001
7. Louisiana State Legislature. (1986). Destruction of in vitro fertilized human ovum. Louisiana Revised Statutes, Title 9, §129. https://legis. la.gov/legis/Law.aspx?d=108446
8. O'Donoghue, J. (2024, May 29). Louisiana lawmaker shelves IVF protection bill, leaving questions about legal challenges. WWNONew Orleans Public Radio. https:// www.wwno.org/politics/2024-05-29/ louisiana-lawmaker-shelves-ivfprotection-bill-leaving-questionsabout-legal -challenges
9. Hogue, I. (2025, January 23). Trump's Executive Order on Gender Attacks Abortion Rights. https://time. com/7210539/trumps-executiveorder-gender-abortion-rights/
10. Popli, N. (2025, January 24). Trump's early actions mirror Project 2025, the blueprint he once dismissed. Time https://time.com/7209901/ donald-trump-executive-actionsproject-2025/
11. The Heritage Foundation. (2023). Mandate for Leadership: The Conservative Promise. Washington, D.C.: The Heritage Foundation. Retrieved from https://www.heritage. org/mandate
12. Tipton S. The ASRM. February 18, 2025. https://www.asrm.org/ news-and-events/asrm-news/pressreleasesbulletins/asrm-responds-totrump-executive-order-on-ivf/
13. Reuters. (2024, August 29). Trump says IVF costs would be covered if he is elected. Reuters. https://www. reuters.com/world/us/trump-sayivfcosts-would-be-covered-if-he-iselected-2024-08-29/

14. National Public Radio. (2024, August 30). Trump says he'll support free IVF treatments in a second term. NPR. https://www.npr.org/2024/08/30/ nx-s1-5094454/trump-tells-townhall-crowd-that-he-supports- freeivf-treatments https://www.reuters. com/world/us/trump-says-ivfcosts-would-be-covered-if-he-iselected-2024-08-29/
15. 14. National Public Radio. (2024, August 30). Trump says he'll support free IVF treatments in a second term. NPR. https://www. npr.org/2024/08/30/nx-s1-5094454/ trump-tells-town-hall-crowd-that-hesupports- free-ivf-treatments
16. Trump, D. J. (2025, January 24). Remarks by President Trump at the 52nd Annual March for Life. The White House. https://www. whitehouse.gov/briefings-statements/ remarks-president-trump-52ndannual-march-life/
17. National Institutes of Health Revitalization Act of 1993, Pub. L. No. 103-43, § 121, 107 Stat. 122 (1993) Retrieved from https://www.congress. gov/bill/103rd-congress/senate-bill/1/ text

By Norbert Gleicher, MD , Medical Director and Chief Scientist at The Center for Human Reproduction
in New York City. He can be contacted through the
VOICE
or directly at either ngleicher@thechr.com or ngleicher@rockefeller.edu
BRIEFING: It is not widely known that in vitro fertilization (IVF) is the only routine treatment in all of medicine which—based on a Congressional amendment—is excluded from practical federal research funding. Considering that President Trump during his campaign spoke out emphatically in support of IVF, it may be time to discontinue the annual renewal of the amendment which since 1996 has occurred automatically by simply being attached without public discussion to the annual budget.
During the election campaign, in vitro fertilization (IVF) became a relevant policy issue for discussion.1 57% of tentative voters wanted to hear more about IVF from candidates. President Trump, to the chagrin of some of his followers, came out very strongly in support of IVF, even suggesting that it should be a free service.2
Though it is somewhat unclear what he meant by that, it is reasonable to assume he meant that, as in several other developed countries, IVF should be considered part of routine health care coverage.
As part of general medical insurance coverage, IVF is, indeed, free in many countries, though often with restrictions in either numbers of covered cycles or age. Likely the most generous IVF coverage in the world is offered by Israel, basically providing coverage for almost unlimited IVF cycles for up to three children. (Israel also reports the by far highest per-capita utilization of IVF cycles in the world.)
In the U.S., several states have passed mandated coverage generally attached to mandated coverage for obstetrical services. These mandates are, however, usually quite leaky, with the federal government representing the largest culprit by not offering IVF coverage under Medicaid and Medicare and offering coverage only in very rare exceptions for members of the military.

Though a strong argument can be made for insurance coverage, and especially in government programs for at least a limited number of cycles, such a federal mandate appears unrealistic at a time when significant federal budget cuts can be anticipated and the public’s appetite for government-mandated health services is clearly at a low point.
At the same time, the Trump administration has, however, an opportunity to improve the currently still very low utilization of IVF in the U.S. in comparison to many other developed countries at practically no additional cost. All it would take is stopping the automatic renewal of the so-called Dickey-Wicker Amendment of 1996, which, uniquely for IVF among all other existing medical procedures, prohibits federal funding for any research having anything to do with IVF.3 Since the federal government currently funds ca. 40% of all health care-related research, the negative effects of this almost 20 years old federal embargo, therefore, has been profound.
Here is the text of the amendment: SEC. 509. (a) None of the funds made available in this Act may be used for--(I) the creation of a human embryo or embryos for research purposes; or (II) research in which a human embryo or embryos are destroyed,

discarded, or knowingly subjected to risk of injury or death greater than that allowed for research on fetuses in utero under 45 CFR 46.204(b) and section 498(b) of the Public Health Service Act (42 U.S.C. 289g(b)).(b) For purposes of this section, the term `human embryo or embryos' includes any organism, not protected as a human subject under 45 CFR 46 as of the date of the enactment of this Act, that is derived by fertilization, parthenogenesis, cloning, or any other means from one or more human gametes or human diploid cells.
Named for its authors, representative Jay Dickey, a Republican from Arkansas, and Roger Wicker, a Republican from Mississippi, this amendment has remained unknown by most of the public; since 1996, it has every year automatically renewed without any public discussion, attached to the appropriations bills for the Departments of Health and Human Services, Labor, and Education.
Amazingly, It was actually never placed for a formal vote on the House floor. According to the Embryo Project Encyclopedia of Arizona State University, the amendment was instead only approved by the House Appropriations Committee of the 104th Congressional session in 1995 and, by the time the bill made it to vote in the House at 5:20 pm on January 25, 1996, the amendment was already in place in Section 128. After only one hour of debate, it passed the House by a vote of 37–42 at 7:41 pm. On the next day it was presented in the Senate and passed without amendment with a Yea-Nay vote of 82–8, and President Bill Clinton then signed the bill which became Public Law 104-99 on 26 January 1996.3
There are several good reasons why the availability of federal funding for IVF-related research fits well into the current Trump policy mantra of “America first:” Likely the most urgent one is the indisputable fact that, based on IVF cycle outcome reporting under Congressional mandate by the Centers for Disease Control and Prevention (CDC), U.S. IVF cycle outcomes, which historically steadily improved until 2010, since then have been steadily declining.4 In other words, the efficiency of IVF in the U.S. has, without anybody doing anything about it, been steadily declining for much too long.
The reasons are complex and multifactorial, and their discussion here would exceed the framework of this op-ed. One argument is, however, irrefutable: More
and better research with the help of federal funding over the last 20 years would very likely have resulted in better IVF cycle outcomes. And that could now be achieved with the stroke of the pen by simply no longer renewing the Dickey-Wicker amendment in the upcoming budget.
A second very obvious reason why the nation would benefit from federal research support for IVF is the recent recognition of a significant birth deficit awaiting the U.S. Improving national birth rates has been the principal motivation for above-noted most generous IVF benefits in Israel, but also has been a major reason for expanding IVF benefits in other countries suffering from increasing birth deficits, like Italy, Spain, China, Korea, and especially Japan. The recent commercial success of the 2024 film Joy, which tells the story of the three trailblazers who—seemingly against all odds—ultimately gave the world its first IVF baby in 1978, then called a “test-tube baby,” is another reflection of the popularity IVF has achieved in the general population. The birth of Louise Brown radically changed—and, indeed, in many ways reinvented—the medical practice of female as well as male infertility. As a consequence, the world has been able to welcome almost 10 million more citizens than would otherwise populate the globe, had the young nurse, Jean Purdy, physician-surgeon Patrick Steptoe, and reproductive biologist Robert Edwards not succeeded in producing the world’s first IVF baby.
The film not only succeeded in demonstrating the for too-long underreported contribution of the young Jean Purdy, but by also vividly demonstrated the meaning of this achievement for millions of infertile women and men, who—until IVF became available— simply had no chance of ever becoming biological parents with use of their own eggs and semen. And there are so many more infertile patients out there who deserve this opportunity!
1. Salganicoff A. Quick Takes . September 17, 2024. https://www. kff.org/quick-take/ivf-as-an-election-and-policy-issue/
2. Kapur S, Burns D. NBC News. September 10, 2024. https://www.nbcnews.com/politics/2024-election/donaldtrump-plan-mandate-free-ivf-republicans-congress-o pposition-rcna170327
3. Kearl M. Arizona State University. Embryo Project Encyclopedia. August 27, 2010.
4. CDC. ART Success Rates. https://www.cdc.gov/art/success-rates/index.html


By Sònia Gayete Lafuente, MD, PhD , a Foundation for Reproductive Medicine Research Fellow at the CHR. She can be reached through the editorial office of the VOICE.
BRIEFING: With this article, the author closes out a series of contributions to the VOICE pointing out the effects of our lifestyles on reproductive health. The current environmental pollution crisis has become a growing concern across the globe yet, despite significant consequences, pollution’s impact on human fertility has been barely discussed. While young people are increasingly aware of environmental issues, their global fertility rates have continued to decline, sparking interest in potential environmental causes. We here summarize how environmental factors—including increasing air pollutants, endocrine-disrupting chemicals (EDCs), toxic metals, and other everyday toxins such as plastics and other chemicals—are influencing female as well as male reproductive health and outline strategies to mitigate these risks.
*Articles were originally published in the Reproductive Times.
A good number of studies have by now revealed that environmental pollutants can significantly affect human fertility. Exposure to key factors such as temperature, radiation, and toxic substances— including endocrine disrupting chemicals (EDCs) — have been identified as major contributors to adverse outcomes, including altered menstrual cycles, diminished oocyte quality, impaired sperm parameters, and consequently reduced pregnancy rates. The recognition of these environmental hazards allows us to take proactive steps to limit exposure which, in turn, can help in preserving fertility and may also protect future offspring. Let’s explore them!
One of the primary culprits behind environmental pollutants’ impact on fertility are EDCs. These substances, found in a range of everyday products like plastics, pesticides, and cosmetics, are molecules which interfere with the body’s hormonal systems. Notable EDCs that have been linked to altered hormone regulation, female infertility, and reduced sperm quality include:
• Bisphenol A (BPA), present in some plastic containers and bottles, cans of food and beverages,

Tupperware, thermal paper for receipts, plastic optic lenses, one-time-use plastic utensils, some toys, and even plastic lining in water pipes or plastic bags of medical and dental devices.
• Phthalates, in soft plastic containers and packaging, personal care cosmetic products (perfumes, shampoos, nail polish, lotions, and creams), cleaning products with fragrances, flooring and vinyl products, synthetic materials in some furniture, and even toys made from soft polyvinyl chloride (PVC) or other soft plastics in all sorts of electronic devices and even clothing of synthetic elastic fabrics.
• Polybrominated diphenyl ethers (PBDEs), a group of chemicals used as flame retardants in a variety of consumer products, often in materials that need to meet fire safety standards, such as furniture (matresses sofas), electronics, textiles, and fireresistant insulation, etc. Organochlorine and pyrethroids, components found in some common pesticides used in gardening and farming.
Several studies have suggested that individuals experiencing sub-fertility tend to have higher concentrations of at least some of these toxic substances in their systems.
Amongst products for women, BPA exposure is particularly concerning. Several recent publications, indeed, pointed out that BPA is found at higher levels

in women who struggle with natural conception. In assisted reproductive treatments, exposure to BPA correlates with lower estradiol levels, fewer fertilized oocytes, and decreased implantation success. Animal studies have demonstrated BPA’s ability to disrupt ovarian development, folliculogenesis, and hormone secretion, especially raising concerns about its impact on conditions like polycystic ovary syndrome (PCOS) and endometriosis.
Hopefully, BPA will in the near future be restricted in its use or even banned, following the example of polychlorinated biphenyls (PCBs), a group of chemicals used from the 1920s till 1970s in several industrial applications, until banned in the U.S. due to their toxic persistence in the environment and accumulation in living organisms, causing several harmful ecosystemic and reproductive health effects.
Environmental pollution has also increased human exposure to harmful heavy metals, which pose significant risks to fertility. Toxic metals like mercury, lead, and cadmium can interfere with reproductive health at multiple levels—affecting development, hormone regulation, and overall reproductive function. Research has linked chronic exposure to these metals with conditions such as menstrual disorders, endometriosis, spontaneous abortions, and infertility.
Mercury is a well-known toxic metal found in fluorescent light bulbs, some batteries and even in some cosmetics. Because of worsening ocean pollution, this metal also builds up in fish and seafood across the globe and, therefore, enters the food cycle. Mercury can affect nervous, digestive, and immune systems in humans, with considerable potential negative consequences for fertility. Mercury exposure has, for example, been associated with reduced sperm count, motility, and abnormal morphology. While data on the effects of mercury on female fertility remain limited, evidence suggests that it alters hormone levels and its exposure during pregnancy may result in adverse outcomes such as birth defects and developmental delays in offspring.
Lead is another toxic metal mainly found in leadbased paint in older buildings, contaminated soil,
plumbing with lead pipes, and certain imported goods (toys or jewelry). It has been linked to spontaneous abortions.
Cadmium exposure is known to increase the risk of endometriosis and has also been associated with several other reproductive health issues. It is present in cigarette smoke, industrial emissions (such as from mining or battery manufacturing), and contaminated food (particularly shellfish, liver, and kidney meats). Importantly, it also acts as a metalloid-estrogen, interfering with estrogen receptors and potentially leading to different reproductive disorders. Given the growing body of evidence on the impact of heavy metals on female fertility, further research is urgently needed to understand the genetic, epigenetic, and biochemical mechanisms that contribute to reproductive impairment.
While it may be difficult to completely avoid environmental toxins, there are proactive steps individuals can take to reduce their exposure and protect their reproductive health. Here are some practical strategies:
• Minimize plastic use, as plastic containers and food packaging often contain BPA and other harmful chemicals.
• Opt for glass, stainless steel, or BPA-free plastics for food and drink containers.
• Look for "phthalate-free" labels on cosmetics, toys, and personal care products.
• Choose fragrance-free products, as phthalates are often used in fragrances.
• When possible, buy PVC-free products (e.g., in flooring, toys, and shower curtains).
• Avoid products with a strong synthetic smell, as they often contain phthalates in the fragrance.
• Be especially cautious with cosmetics, as many cosmetics and personal care products contain EDC like phthalates. Hence, choosing natural beauty products can help reduce your exposure.
• Choose organic products, especially organic foods which are less likely to be contaminated with harmful pesticides and other chemicals. Buying organic products, when possible, can reduce your exposure to these toxins. Many manufacturers are now shifting toward greener and more sustainable alternatives, especially in products meant for
babies or food storage. Especially for pregnant women, those trying to conceive, and new moms, it is particularly important to be mindful of items you use regularly.
Advocate for occupational exposure and public health safety policies to also benefit workers in certain industries who may be more likely to encounter chemicals and pollutants that can disrupt hormonal function and impair reproductive health. It is critical that health and safety policies specifically address the reproductive health risks of these individuals. Public health regulations must focus on reducing exposure in high-risk environments and ensure that industries comply with safety standards to protect the reproductive health of employees. Globally, we must advocate for stronger systemic environmental regulations that limit industrial emissions and the use of toxic chemicals in consumer products, since supporting policies aimed at reducing pollution will have a positive long-term impact on reproductive health and well-being. Preserving one’s fertility, a term widely used to describe the practice of egg or embryo freezing, of course, also may come into play, especially if you are aware that something unavoidable in your environment may adversely affect your fertility. Being a responsible consumer, you can under such a circumstance take a more proactive approach toward fertility preservation treatments that will enhance your overall future reproductive potential. This point applies equally to women and men because both eggs and sperm can be frozen (and, of course, so can embryos). Such a choice may be especially appropriate if you live in a highly polluted area or are exposed at work to known environmental toxins potentially affecting your reproductive health.
Encouragingly, this is all only your choice!
READING LIST
1. Sakali AK, Bargiota A, Bjekic-Macut J, Macut D, Mastorakos G, Papagianni M. Environmental factors affecting female fertility. Endocrine. 2024 Oct;86(1):58-69. doi: 10.1007/ s12020-024-03940-y. Epub 2024 Jul 2. PMID: 38954374. Green MP, Harvey AJ, Finger BJ, Tarulli GA. Endocrine disrupting chemicals: Impacts on human fertility and fecundity during the peri-conception period. Environ Res. 2021 Mar;194:110694. doi: 10.1016/j.envres.2020.110694. Epub 2020 Dec 30. PMID: 33385395.
2. Pivonello C, Muscogiuri G, Nardone A, Garifalos F, Provvisiero DP, Verde N, de Angelis C, Conforti A, Piscopo
M, Auriemma RS, Colao A, Pivonello R. Bisphenol A: an emerging threat to female fertility. Reprod Biol Endocrinol. 2020 Mar 14;18(1):22. doi: 10.1186/s12958-019-0558-8. PMID: 32171313; PMCID: PMC7071611.
3. Rzymski P, Tomczyk K, Rzymski P, Poniedziałek B, Opala T, Wilczak M. Impact of heavy metals on the female reproductive system. Ann Agric Environ Med. 2015;22(2):259-64. doi: 10.5604/12321966.1152077. PMID: 26094520.
4. Kumar S, Sharma A, Sedha S. Occupational and environmental mercury exposure and human reproductive health - a review. J Turk Ger Gynecol Assoc. 2022 Sep 5;23(3):199-210. doi: 10.4274/jtgga.galenos.2022.2022-2-6. PMID: 36065987; PMCID: PMC9450922.
5. Dutta S, Gorain B, Choudhury H, Roychoudhury S, Sengupta P. Environmental and occupational exposure of metals and female reproductive health. Environ Sci Pollut Res Int. 2022 Sep;29(41):62067-62092. doi: 10.1007/s11356-021-16581-9. Epub 2021 Sep 24. PMID: 34558053.


Older and older women are desiring pregnancy with their own eggs. We should do something about this.
By Norbert Gleicher, MD, Medical Director and Chief Scientist
at The Center for Human Reproduction in New York City. He can be contacted through the VOICE or directly at either ngleicher@thechr.com or ngleicher@rockefeller.edu.
BRIEFING: Even we here at the CHR had a hard time believing our just-completed 2024 patient age analysis: Once again, in only one year between 2023 and 2024, the CHR’s median patient age increased by a full point from 44 to age 45. This stands in stark contrast to a steady median age of around 36 years over the last decade of available data for all U.S. IVF clinics reporting to SART and CDC.
This article by Norbert Gleicher, MD, addresses this discrepancy, which on first impression may appear contradictory. He convincingly argues that while the CHR obviously attracts a very selected worldwide patient clientele of extremely advanced age, the seeming stability of age for national IVF cycles is misleading. What it in reality appears to reflect is the longstanding stability in age at which U.S infertile women are by their respective IVF clinics “advanced” into third-party egg donation.
He then takes this observation and expands on the subject of women seeking fertility treatments who must be expected to continue to get older and older, pointing out the need for IVF clinics to learn how to treat older patients with use of autologous oocytes, rather than driving them after age 42-43 automatically into donor-egg cycles, as currently is widely held practice.
*Articles were originally published in the Reproductive Times.
A little bit of background
Birth rates all over the world except for Africa and certain other underdeveloped regions are declining and in some highly developed countries, like Italy, Spain, South Korea, Japan, and even in mainland China, declining to economically threatening degrees. Recent headlines in the U.S. press point out that the U.S. is also close to missing replacement levels. But within this very obvious decline in overall births one unique finding may come as a surprise: Birth rates in older women are on the rise. More specifically, pregnancies and deliveries in women between 45 and 49, and even above 50, have been significantly rising, a finding in this oldest group of patients is almost exclusively the consequence of increasing donor-egg cycles.
The principal reason why the U.S and many other countries face such contradictory trends is the fact that women are delaying childbirth. And the later they start trying, the more likely they will develop fertility problems. Figure 1 demonstrates the increase in age at first birth and, cumulatively, for all births.
As is apparent from the figure, first and cumulative births followed since 2017 parallel curves. But these societal

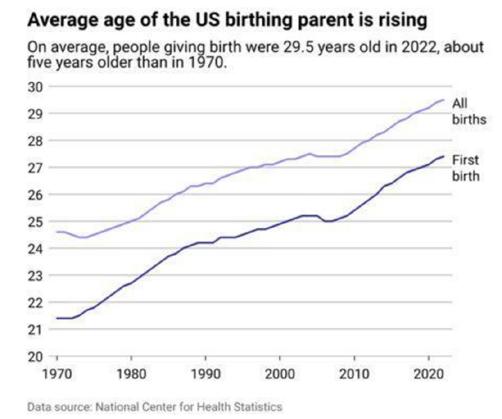
FIGURE 1. Delayed childbirth, the principal reason why women who are having children are getting older
developments do not only increase infertility problems; they, of course, also increase obstetrical and neonatal problems because pregnancy complications increase with female age. Taking care of older women during pregnancy is, therefore, increasingly becoming a subspecialty area of perinatal medicine, in major institutions involving teams
of obstetricians and physicians from a variety of medical specialties, depending on the needs of individual patients.1
Why, then, haven’t ages of U.S. patients undergoing IVF cycles significantly increased? With everybody agreeing that women are having babies at more advanced ages and that, therefore, infertility is on the rise (there, of course, are also other reasons), how come the median age of women undergoing IVF cycles (i.e., using their own eggs) has not significantly changed over the years, and remaining stable by hovering around 36 years? The CDC reported an average patient age of 36.3 years for 2022, the last year of data availability.2
This, of course, stands in stark contrast to The Center for Human Reproduction (CHR) where we have observed a dramatic increase in age in our IVF patients undergoing autologous IVF cycles , with the last two years having been especially pronounced: The year 2023 took us for the first time to a median age of over 44 and—even more remarkably as we just found out—2024 took us up to a median age of 45 years in one year alone (see Figure 2 below).
Interestingly and on a side note, this was also the second year in a row that the CHR improved ongoing pregnancy rates in this patient population: For several years until 2023, the average ongoing clinical pregnancy rate in this

patient population had been around 8%. In 2023, we for the first time saw an increase to 10%, and in 2024 data we just received, the rate further increased to 12%, a 33% increase in clinical pregnancy rate, which is really quite remarkable, considering the
age of this patient population (for further discussion of this matter, please see the “CHR News” section of the VOICE). The extremely obvious age difference between the national U.S. and the CHR patient age data, of course, raises the question: how can this discrepancy be explained? The answer is likely multifactorial, but one conclusion appears unavoidable: The CHR’s patient population going through autologous IVF cycles is radically different from the average U.S. patient population. This is, of course, anything but a new discovery for us here at the CHR, since as a “last resort center,” with over 90% of our patients consulting with the CHR after having failed elsewhere—and often repeatedly and at several IVF clinics—we have known for many years that we are serving a much more adversely selected patient population than the overwhelming majority of U.S. IVF clinics. What we, however, did not understand until very recently is that this difference in unfavorability in potential prognosis in recent years appears to have grown with increasing velocity.
And that can have only one reason: Most U.S. IVF clinics have for decades simply refused to change their practice
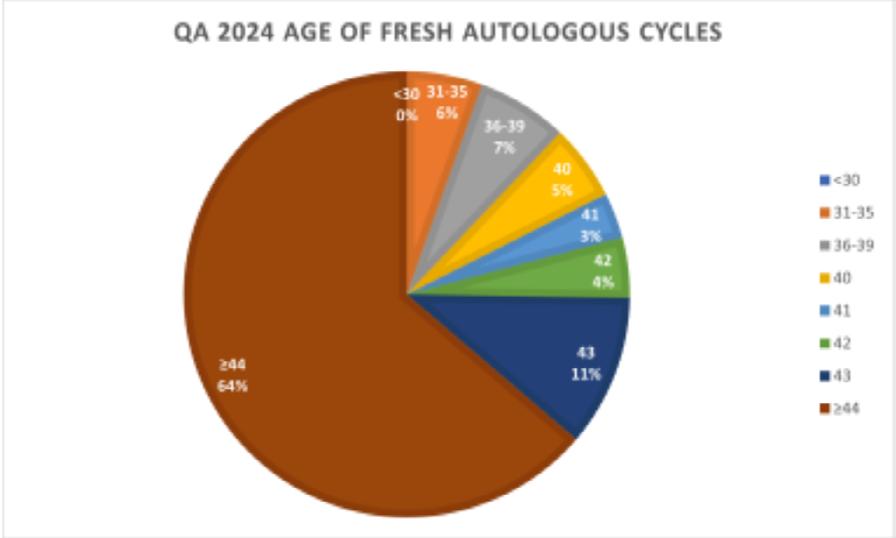
*This pie chart demonstrates the age distribution of all patients at the CHR who underwent an autologous IVF cycle in 2024 and had at least 1 transferrable embryo. The median age in this year for the first time exceeded 45. problems.

pattern of rather automatically advancing women above ages 42 to 43 into third-party egg donation. There simply is no other explanation for the national median age of women undergoing autologous IVF cycles in the U.S. having hardly budged in so many years in the face of very obvious increases in ages of infertile women seeking treatments. In parallel IVF autologous IVF cycles numbers after age 42-43 have remained minuscule. The annual CDC report for that reason, indeed, reports on the main page only about IVF cycles up to age 42.2
The CHR’s plight, on the other hand, was at the other extreme of the spectrum. As the relative percentage of patients above age 43, especially in most recent years, has been quickly growing, the CHR became known worldwide as one of the very few IVF centers where infertile women, even at more advanced ages, would still get serious treatment attempts with use of their own eggs, offering surprisingly reasonable pregnancy and live birth chances (we in 2023 for the first time reached a 10% ongoing clinical pregnancy rate for women who produced at least 1 embryo in their cycle; 2024 results will be available by April). The emphasis in the last sentence was meant to be on the word “serious” because our experience with patients who did still undergo some of those rare autologous IVF cycles above ages 42-43 one can still see in national outcome statistics, almost uniformly suggested that what they received were what we have come to call “alibi cycles.”
What is meant by this term is that many colleagues who, in principle, still believe that autologous IVF cycles above ae 42-43 are mostly futile, may agree to such cycles when pressured by their patients, but really only go through the motion, unconsciously or consciously wanting to prove to the patient that they were correct in recommending thirdparty egg donation. Patients then end up receiving the same kind of IVF cycles the clinic uses in younger women, and that, of course, makes little sense!
Which brings us to another important question: Why is most of the IVF field stuck on the notion that autologous IVF cycles above age 42-43 are not worth it? This notion is, indeed, difficult to understand, especially since it has dictated practice now for decades. As one of the last remaining first-generation IVF investigators in clinical practice, I still remember that in the very early days of IVF, clinics refused patients over age 38 because reported pregnancy rates, which even under that age were still very low, above age 38 were basically zero. Imagine if, at that point, the IVF field had decided to send every woman above age 38 into egg donation: where would the IVF field find itself today?
The argument must, therefore, be made that the apparent
lack of interest in pursuing autologous IVF cycles in women above ages 42-43 is self-defeating for the IVF field because, if one does not try, where does one learn?
Current third-party egg donation practice in this country (and in many other regions of the world where egg donation is allowed), therefore, makes little sense and one must ask: what other motivations may be behind this seemingly unchanging practice? And any answer to these questions—unfortunately and unavoidably—makes us dip into the weeds of IVF as a business practice, because donor egg IVF cycles are the by far most profitable IVF cycles for IVF clinics. They also, since the establishment of frozen egg banks, have become the logistically most simple cycles to manage; and, last but not least, they also produce the highest satisfaction levels for patients and treating physicians because they—of course—produce the highest pregnancy and live birth rates.
But this practice pattern also causes immense harm and pain to many patients who for religious or what they consider moral and/or ethical reasons cannot pursue donor eggs or who simply are not ready to give up on their genetic motherhood (not infrequently a sentiment even stronger expressed by the male than the female partner).
Recognizing a patient’s almost complete right to selfdetermination in making medical decisions, it is difficult for us at the CHR to understand how patients can be intimidated and/or strong-armed to pursue egg donation or are appeased in an “alibi cycle,” if they really are not yet ready to give up on their own eggs.
That this is becoming an increasing problem is no longer deniable. The time has come to encourage a special research effort into how to improve autologous IVF cycle outcomes in women above ages 42-43. As elsewhere in this issue of the VOICE discussed in an Editorial, Congress to this day still excludes IVF from practically all federal research funding. IVF research is, therefore, totally dependent on research support from private sources. Considering abovenoted demographic changes this country is undergoing and the increasing value other governments are now attributing to IVF births in their countries given declining birth rates, it seems high time for the U.S. to start supporting at least this kind of research support for IVF. Mr. President, we need your help!
1. Newman RA, Esakoff TF. Contemporary OBGYN.net. November/December 202418-21
2. CDC. 2022 Assisted Reproductive Technology (ART) Report. https://www.cdc.gov/art/php/national-summary/index.html

Our readers know that as a “last resort center,” the CHR serves not only a significantly older patient population than all other IVF clinics in the U.S. (and likely the whole world) but, overall, of course a much poorer prognosis patient population. Consequently, the CHR’s slogan “fighting for every egg and embryo” can be taken literally.
We, therefore, are extremely proud about our 2024 cycle outcomes which just became available: Despite the fact that our patient population continued to age, we succeeded in significantly improving our ongoing clinical pregnancy rate (which is predictive of live birth rate) for a second year in a row: In other words, while the age of our patients undergoing IVF cycles with use of their own eggs increased for a second year by a full percentage point now
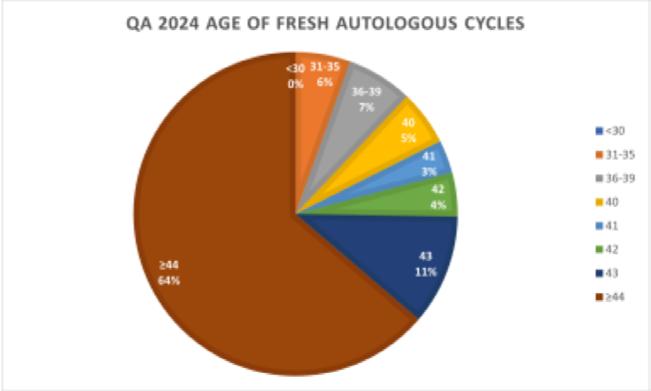
FIGURE 1. Age distribution of women undergoing autologous IVF cycle at the CHR in 2024 Here described IVF cycles represent the age distribution of all women undergoing IVF cycles during 2024 at the CHR, who had at least 1 day-3 embryo for transfer. As will be apparent, only 13% of women were under age 40, and virtually all of those had very low functional ovarian reserve. The median age for this patient population increased from 44 years in 2023 to 45 years in 2024.
reaching age 45, we further increased the ongoing clinical pregnancy rate from 10% in 2023 to 12% in 2024.
In more practical terms this means that in the last two years, between 2023 and 2024, the median age in our patients increased from age 43 to age 45 years (see Figure 1), while in the same time period our ongoing clinical pregnancy rate in women who had at least one day-3 transferable embryo (we in this patient population usually do not culture embryos to blastocyst-stage)
increased from 8% to 12%, a whopping 33.3% increase, 12% is, of course, not the ongoing clinical pregnancy rate of most IVF clinics, but in a patient population with median age of 45 years, most of whom were told at their prior IVF clinic that their only chance of pregnancy was with third-party donor eggs, this is a truly spectacular number and reflects truly amazing progress.
How can we account for these changes?
Dr. Gleicher’s “A Piece of My Mind” article in

this issue discussed that the general population of infertility patients, as women increasingly delay childbirth in this and in other countries, has continued to age, while, interestingly, U.S. national data, consistently for decades, have demonstrated an unchanged median age of 36 years for women undergoing autologous IVF cycles. The only possible explanation for this contradiction is, as noted in Dr. Gleicher’s article, the fact that most U.S. IVF clinics advance women above ages 42-43 years pretty automatically

Our readers know that as a “last resort center,” the CHR serves not only a significantly older patient population than all other IVF clinics in the U.S. (and likely the whole world) but, overall, of course a much poorer prognosis patient population. Consequently, the CHR’s slogan “fighting for every egg and embryo” can be taken literally.
We, therefore, are extremely proud about our 2024 cycle outcomes which just became available: Despite the fact that our patient population continued to age, we succeeded in significantly improving our ongoing clinical pregnancy rate (which is predictive of live birth rate) for a second year in a row: In other words, while the age of our patients undergoing IVF cycles with use of their own eggs increased for a second year by a full percentage point now reaching age 45, we further increased the ongoing clinical pregnancy rate from 10% in 2023 to 12% in 2024.
In more practical terms this means that in the last two years, between 2023 and 2024, the median age in our patients increased from age 43 to age 45
years (see Figure 1), while in the same time period our ongoing clinical pregnancy rate in women who had at least one day-3 transferable embryo (we in this patient population usually do not culture embryos to blastocyststage) increased from 8% to 12%, a whopping 33.3% increase, 12% is, of course, not the ongoing clinical pregnancy rate of most IVF clinics, but in a patient population with median age of 45 years, most of whom were told at their prior IVF clinic that their only chance of pregnancy was with thirdparty donor eggs, this is a truly spectacular number and reflects truly amazing progress.
How can we account for these changes?
Dr. Gleicher’s “A Piece of My Mind” article in this issue discussed that the general population of infertility patients, as women increasingly delay childbirth in this and in other countries, has continued to age, while, interestingly, U.S. national data, consistently for decades, have demonstrated an unchanged median age of 36 years for women undergoing autologous IVF cycles. The only possible explanation for this contradiction is, as noted in Dr. Gleicher’s article, the fact that most U.S. IVF clinics advance women above ages 42-43
years pretty automatically into third-party egg donation.
Since the CHR does not do this, older patients who do not wish to give up on genetic maternity of course flock to the CHR from all over the U.S. (and the world), creating the age difference pointed out above between national U.S. IVF data and the CHR.
WITH A MEDIAN AGE OF
Just like there seemingly is a very obvious reason for this age difference between the CHR’s patients and patients at all other IVF clinics, we believe also to know what the major reason is in the dramatic improvement in pregnancy and live birth chances in this difficult patient population at the CHR we have witnessed over the last two years (and
we very much hope to continue going forward): to a significant reason it has been the CHR’s HIER (Highly Individualized Egg Retrieval) Program.1,2
Though we started to develop this program several years ago, we only learned in the last few years how far we could— and needed to—take it in order to improve the chances of older women to conceive. To trigger ovulation at lead follicle sizes as small as 9-10mm— which sometimes means as early as on days 3 or 4 of a cycle—is nowadays routine at CHR and no longer surprising, considering the age of the CHR’s population. But if one considers that, at the beginning, we were hesitant to trigger even at 16mm, it will become understandable how far the CHR has come in individualizing IVF cycles in our so severely adversely selected patients. And we are not yet at the end of understanding the HIER process.
We already understand that follicle size is not the only parameter to determine early maturing of eggs in follicles. We, indeed, are in the process of defining certain ultrasound parameters that will tell us when a follicle starts to become overmature. What we have learned over the last year is that it is not always the biggest follicle of a patient
that is the most mature. In other words, more is to come, hopefully further improving our pregnancy and live birth chances in women with olderbehaving ovaries, which also includes younger women who suffer from premature ovarian aging (POA).
1. Wu et al., J Endocrinol 2015;226(3):167-180
2. Wu et al., J Ovarian Res 2018;16(11):23
Gleicher N, Barad DH, Patrizio P, GayeteLafuenete S, Weghofer A,
Ben Rafael Z, Takahashi S, Glujovsky D, Mol BW, Orvieto R. An additive opinion to the committee opinion of ASRM and SART on the use of preimplantation genetic testing for aneuploidy (PGT-A). J Assist Reprod Genet 2025;42:71-80
This is a very easy-toexplain paper: It basically was meant to express everything the recently revised combined ASRM/ SART opinion about PGT-A left out, not the least the fact that, if an expensive and invasive test with highly significant clinical consequences after over 20 years of utilization still (as the recent ASRM/ SART opinion finally, very
clearly stated) has not demonstrated any clinical outcome utility, why are we still using this test? And then there were, of course, some additional comments regarding this long overdue but still too timid committee opinion.
Patrizio P, Darmon S, Barad DH, Gleicher N. Greater PGT-A utilization in IVF clinics does not improve live birth rates but relates to IVF center ownership: a preliminary report. J Assist Reprod Genet 2025;42:81-84
And continuing with the theme of PGT-A, this very interesting original data study utilized national reported IVF cycle
outcome data to for the first time demonstrate that how much PGT-A an IVF clinic performs not only does not impact that clinic’s IVF cycle outcomes (as one would expect if PGT-A had any effect on IVF, good or bad), but is clinic ownership-associated. Specifically, non-medical ownership of IVF clinics (i.e., private equity, etc.) was significantly associated with increased PGT-A utilization in comparison to university/hospital owned or physician-owned clinics.
What a surprise!


In our last issue, we explored the business of building a good egg, starting with the cues and signals being exchanged between eggs, or more properly oocytes, and the surrounding cells of the ovary. Now we move into the territory of what happens to the egg once matured and fertilized.
FIGURE I
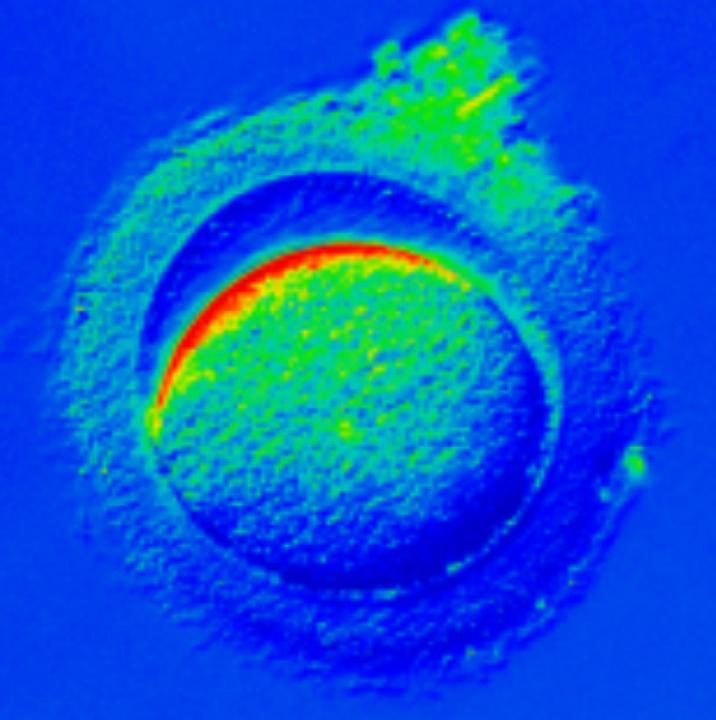
Figure 2 shows a 4-cell human embryo where the blastomeres have separated into equal sized cells that will eventually follow a path to becoming the inner cell mass and embryo proper OR will become positioned towards the outside of the embryo and will pursue a line of development leading to the placentathe so-called trophectoderm. Note this image is taken from Carnegie Collection and represents likely the first ever human embryo seen and studied at this stage of development.

Figure 1 demonstrates an egg shortly after being fertilized by ICSI. Quite often, the egg contracts away from the zona pellucida, a sign that forces are being generated in the cytoplasm that will rearrange the various organelles so that they are equally distributed each time the embryo divides by mitosis.
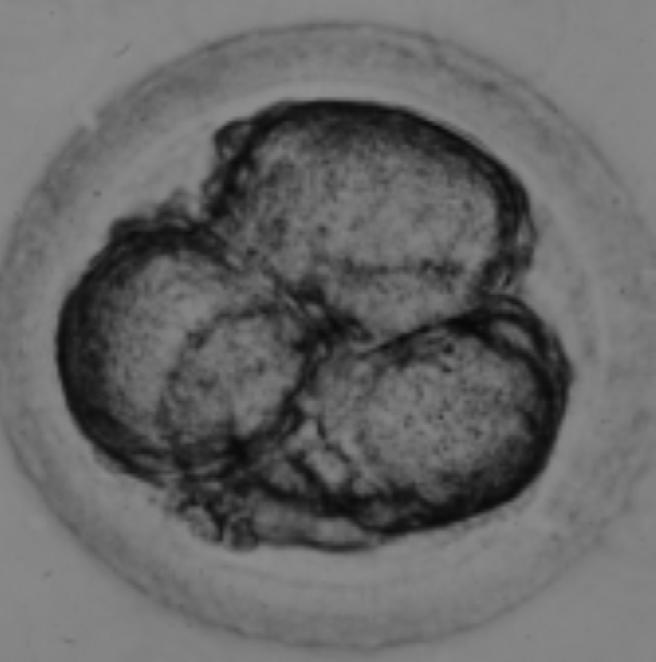
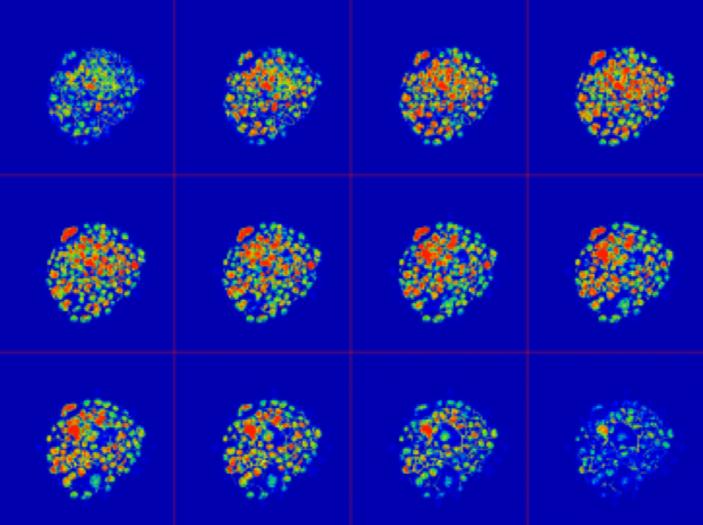
Figure 3. With the latest technologies available to scientists at the CHR and elsewhere, human embryos can be explored at very high magnification and in an intact state. Here is a gallery of sequential optical sections through an embryo made at the CHR that had three pronuclei in it after fertilization. The CHR laboratory cultured this embryo for 4 days and it resulted in a blastocyst that seems to be eliminating a chromosomally abnormal cell shown at 11 o’clock (red nucleus).

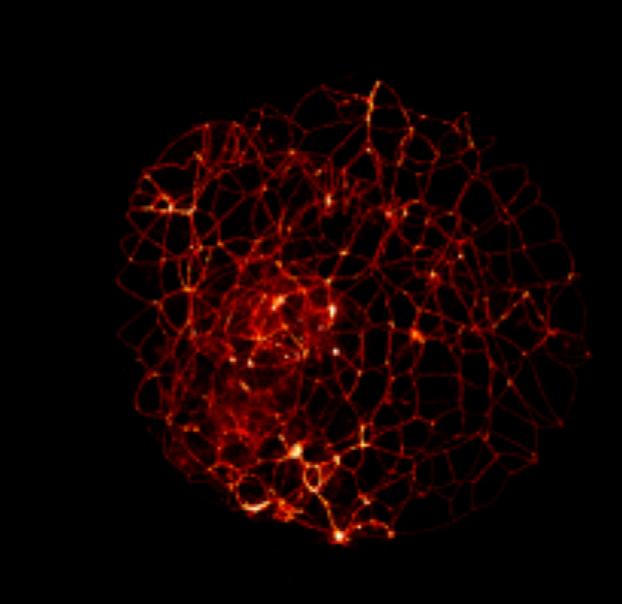
Figure 4. A similar blastocyst-stage embryo is shown after staining for a muscle protein known as actin. The linear pattern shown defines each of the cell boundaries that make up the outer cells of the trophectoderm that will go on to form the placenta.

BRIEFING: In this section, the VOICE offers opinions about medical news not necessarily connected to reproductive medicine, but with potential relevance to the field. News more directly related to reproduction are reported in a later section of this VOICE . Since outside opinions as well as the CHR’s positions can obviously be biased, it is important to reemphasize that we are fully cognizant that “expert” opinions in medicine are considered the lowest level of evidence and should be viewed as such by our readers. Unable to offer, therefore, consistent “truth” (assuming that something like that really exists in science), the VOICE strives to come in its selection of topics and in its content as close as possible to the most likely “truth of the moment.” We, therefore, welcome opinions from our readers, especially opposing ones.
*Articles were originally published in the Reproductive Times.
*Trump DOJ issues dismissal of all charges against Eithan Haim, MD
In the January-February 2025 issue of the VOICE , we reported that surgical resident Eithan Haim, MD , 34, was wrongly targeted by President Biden ’s Department of Justice, and was facing a potential decade-long federal prison sentence for revealing that Texas Children’s Hospital had lied when claiming it had stopped performing gender transitions for children.

As we pointed out in our earlier article, the absurd allegation was that Haim violated patient privacy laws. There, of course, was no breach of privacy in Haim going public with the revelation that the hospital’s announcement of a moratorium on transgender care on children was fake. He was a whistleblower for what is right in medicine but contradicted the Biden administration’s political position on gender-affirming medical care for children. How the Biden administration’s DOJ in response dealt with him is just one more example for how politicized this DOJ under Attorney General Merrick Garland had become and by how much it was willing to deviate in pursuit of perceived political opponents, not only from what was legal but also from what, in this medical case, had to be considered ethical. And imagine, Secretary Garland almost became a supreme court justice under President Obama .
As The Free Press reported on January 24, 2025, Haim had
received notice that day that Trump’s DOJ had dismissed all charges against him with prejudice, which mean that charges could not be refiled. 1 Though we in our last month’s article expressed the hope that something like this may happen once the Trump administration would take over, and though Haim expressed the opinion that “we took on the federal Leviathan and won,” it at least in one aspect must be viewed as a Pyrrhic victory: Though he raised over $1.2 million in crowdfunding, he and his wife incurred over $2 million in legal expenses, and, as The Free Press reported, he, therefore, predicted that “they would be paying legal bills for 20 years.” 1
And more than putting their political opponents in jail, economic bankruptcy is the real primary goal of weaponization of the judicial system, as we have witnessed starting in the Obama administration under Attorneys General Eric H. Holder Jr . (also called “Obama’s enforcer”) and Loretta Lync h and continuing

to previously unprecedented degrees during the Biden administration under Merrick Garland.
1. Yoffe E. The Free Press. January 24, 2025. https://www.thefp.com/p/ eithan-haim-we-took-on-the-federal
Antisemitism on university and college campuses continues, and even Jews disagree over definitions
The VOICE has in the past covered the outburst of antisemitism on university and college campuses after October 7 extensively, has also reported how this affects teaching, learning, and practicing medicine. Interestingly, however, the term “antisemitism,” coined in the 19th century by an avowed German Jew hater called Wilhelm Marr , is even among Jews becoming increasingly controversial and unpopular. Harvard University just settled two lawsuits accusing the university of having tolerated antisemitism on campus by, among other things, agreeing to a new definition of antisemitism that specifically includes the rejection of political Zionism as an antisemitic act, since anti-Zionism denies the Jewish people the right to its own state on its ancestral biblical lands. 1 This definition of antisemitism is called the International Holocaust Remembrance Alliance (IHRA) definition of antisemitism.
But even some Zionist Jews no longer like the term ‘antisemitism’ when expressing
hatred toward Jews, and not only because a Jew hater coined the term who believed that Jews were an “inferior” race (but were so-far awarded roughly 22% of all Nobel Prizes, when representing only 0.2% of the global world population). One, indeed, hears an increasing argument among Jews that a more forceful and clearly descriptive term was preferable since ‘Jew hate’ is so distinct (from other hates) that it must not be described using a term so opaque to 21st-century ears as “antisemitism,” that it makes Jews “sound even more exotic than we are. 2 On the other hand increasing numbers of Jews argue that it should be called exactly what it is, Jew hatred! 2,3
So Harvard settled, while Columbia University, where everything started, despite a special task force supposedly hard at work to combat antisemitism on campus (while allowing a Hamas acolyte professor of Arab descent to teach a course on Zionism), remains the nation’s likely oldest, deepest, and largest cesspool of college antisemitism, even if its Interim President Katrina Armstrong publishes great-sounding condemnations of class disruptions but at an organizational level has done almost nothing. 4
In addition to Harvard, many colleges and universities— suspecting that the price in the Trump administration for such settlements would go up—have settled investigations by the DOJ in the last few days of the Biden administration. Columbia and
Cornel (Ithaca) are not among those, and it increasingly looks like the Trump administration will be much harder on these schools of higher education, targeting not only the increase in campus antisemitism, but also DEI policies, faculty compositions, and a policy away from the indoctrination of students and back to the education of students.
That the Trump administration is serious in combating antisemitism became more than clear with publication of a formal “Presidential Action” on January 29, 2025. Here is the text: 5
By the authority vested in me as President by the Constitution and the laws of the United States of America, it is hereby ordered:
Sec 1. Purpose. My Administration has fought and will continue to fight anti-Semitism in the United States and around the world. On December 11, 2019, I issued Executive Order 13899, my first Executive Order on Combating Anti-Semitism, finding that students, in particular, faced anti-Semitic harassment in schools and on university and college campuses. Executive Order 13899 provided interpretive assistance on the enforcement of the Nation’s civil rights laws to ensure that they would protect American Jews to the same extent to which all other American citizens are protected. The prior administration effectively nullified Executive Order 13899 by failing to give the terms of the order full force and effect throughout the Government. This order reaffirms Executive Order 13899 and directs additional measures to advance the policy thereof in the wake of the Hamas terrorist attacks of October 7, 2023, against the people of Israel. These attacks unleashed an unprecedented wave of vile antiSemitic discrimination, vandalism, and violence against our citizens, especially

in our schools and on our campuses. Jewish students have faced an unrelenting barrage of discrimination; denial of access to campus common areas and facilities, including libraries and classrooms; and intimidation, harassment, and physical threats and assault. A joint report by the House Committees on Education and the Workforce, Energy and Commerce, Judiciary, Oversight and Accountability, Veterans’ Affairs, and Ways and Means calls the Federal Government’s failure to fight anti-Semitism and protect Jewish students “astounding.” This failure is unacceptable and ends today.
Sec. 2. Policy. It shall be the policy of the United States to combat antiSemitism vigorously, using all available and appropriate legal tools, to prosecute, remove, or otherwise hold to account the perpetrators of unlawful anti-Semitic harassment and violence.
Sec. 3. Additional Measures to Combat Campus Anti-Semitism.
(a) Within 60 days of the date of this order, the head of each executive department or agency (agency) shall submit a report to the President, through the Assistant to the President for Domestic Policy, identifying all civil and criminal authorities or actions within the jurisdiction of that agency, beyond those already implemented under Executive Order 13899, that might be used to curb or combat anti-Semitism, and containing an inventory and analysis of all pending administrative complaints, as of the date of the report, against or involving institutions of higher education alleging civil-rights violations related to or arising from post-October 7, 2023, campus anti-Semitism.
(b) The report submitted by the Attorney General under this section shall additionally include an inventory and an analysis of all court cases, as of the date of the report, against or involving institutions of higher education alleging civil-rights violations related to or arising from post-October 7, 2023, campus antiSemitism and indicate whether the Attorney General intends to or has taken any action with respect to such
matters, including filing statements of interest or intervention.
c) The Attorney General is encouraged to employ appropriate civil-rights enforcement authorities, such as 18 U.S.C. 241, to combat anti-Semitism.
(d) The report submitted by the Secretary of Education under this section shall additionally include an inventory and an analysis of all Title VI complaints and administrative actions, including in K-12 education, related to anti-Semitism — pending or resolved after October 7, 2023 — within the Department’s Office for Civil Rights.
(e) In addition to identifying relevant authorities to curb or combat anti-Semitism generally required by this section, the Secretary of State, the Secretary of Education, and the Secretary of Homeland Security, in consultation with each other, shall include in their reports recommendations for familiarizing institutions of higher education with the grounds for inadmissibility under 8 U.S.C. 1182(a)(3) so that such institutions may monitor for and report activities by alien students and staff relevant to those grounds and for ensuring that such reports about aliens lead, as appropriate and consistent with applicable law, to investigations and, if warranted, actions to remove such aliens.
Sec. 4. General Provisions. (a) Nothing in this order shall be construed to impair or otherwise affect (i) the authority granted by law to an executive department or agency, or the head thereof; or (ii) the functions of the Director of the Office of Management and Budget relating to budgetary, administrative, or legislative proposals.
(b) This order shall be implemented consistent with applicable law and subject to the availability of appropriations.
(c) This order is not intended to, and does not, create any right or benefit, substantive or procedural, enforceable at law or in equity by any party against the United States, its departments,
agencies, or entities, its officers, employees, or agents, or any other person.
That universities will not take the Trump administration’s actions lying down, was outlined recently in an article in The New York Times . 6 What’s the solution? The hiring of lobbyists with strong connections to the Republican party, of course! Two recent papers in the Rambam Maimonides Medical Journal offer further commentary on the subject. A first by exclusively U.S. academicians examined unprofessional antisemitic behavior at commencement ceremonies for the 25 U.S. medical schools ranked highest for research excellence (can we assume that their graduates more than others will represent the future of medicine in the U.S.?). 7 And here we quote the findings: Symbols of antisemitism (keffiyehs and three-part graduation stoles conveying antisemitic messages) were worn by students in 13/25 schools, representing ca. 2.5% of the graduating cohort. Wearing of buttons, carrying of banners/ signs, verbal interruptions of the ceremony, or students deviating from scripts occurs in a range of 0% to 22.5%, with a mean of 2.7 per school and 1.7% for medical schools.
The second paper by a group of worldwide academicians offered an international perspective on antisemitism in medicine following October 7. 8 Placing the occurrences after October 7 into a historical framework, the authors in this paper made

the claim that the explosion of antisemitism was “especially noticeable” in the world of healthcare and offered examples from four different countries by authors from these countries.
1. Krupnik MJ. Harvard Magazine. January 22, 2025
2. Rabbi Cythia Minster. The Jewish News of Northern California. July 6, 2023. https://jweekly. com/2023/07/06/heres-why-i-preferto-call-antisemitism-what-is-jew-hate/
3. Pittisky TL. Jewish Telegraphic Agency. June 19, 2023. https://www.jta.org/2023/06/19/ ideas/why-i-dont-love-jew-hate-as-asubstitute-for-antisemitism
4. Armstrong L. Columbia University. Office of Public Affairs. January 21, 2025. https://communications.news. columbia.edu/news/statement-interimpresident-katrina-armstrong-classdisruption
5. Presidential Action. Executive Order. Additional Measure to Combat Anti-Semitism. https:// www.whitehouse.gov/presidentialactions/2025/01/additional-measuresto-combat-anti-semitism/?utm_sour ce=substack&utm_medium=email
6. Sauk S. Blinder A. The New York Times. January 32, 2025. pA21
7. Roth et al., Rambam Maimonides Med J 2025;16(1):e0001
8. Gordon et al., Rambam Maimonides Medical Journal 2025;16(1):e0004
*Under pressure from the Trump administration, universities retreat from DEI and antisemitism—or do they?
As The Wall Street Journal recently reported, universities are following industry and Silicon Valley in allegedly (see explanation below) retreating from DEI. They according to The Journal have started suspending
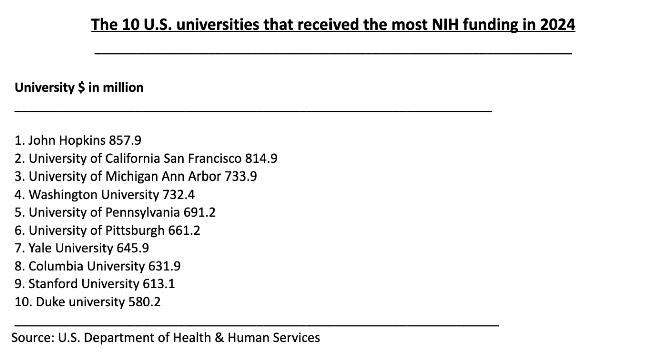
certain research projects, are cancelling selected conferences, and closing DEI offices on campuses in efforts not to “run afoul” of executive orders of the new Trump administration which require “the termination of all discriminatory programs.” 1
At risk are enormous government subsidies. The table just lists the universities that lead in NIH funding. As the article pointed out, this kind of federal funding is absolutely critical for research universities.
We on purpose above inserted the word “allegedly” because, as John Mac Ghlionn recently noted in an opinion article in the New York Post , from the private sector to academia, DEI isn’t dying but—with the same antiachievement consequences— only rebranding,” 2 This is usually achieved by merging DEI units and their staff into other program entities and or, simply, renaming the unit, with purposes and goals remaining exactly the same.
If we had to guess which leading university will feel the hammer of the Trump administration
first, our strong suspicion would be Columbia University in NYC. What even these days is still going on at that campus is almost unbelievable: As The Free Press reported, the university, for example, promoted an event at a Columbia literary society called Alpha Delta Phi (ADP) which had turned the society’s two-story building into an exhibition space for a demonstration project of support for Hamas and describing the whole exhibit as a “museum of terror.” 3 The exhibit specifically offered a spread of tools and the plans for the violent break in by students (and others) into Hamilton Hall, a seminal event during the initial “occupation” of the university campus by pro-Palestinian supporters. And in a speech at the event, a speaker called for a “Zionist-free New York City.”
But that is, of course not all: The university announced that one of its faculty members, Professor Joseph Andoni Massad , would in 2025 teach a course on Zionism at the university. He is a Columbia professor of Jordanian descent specializing in Middle Eastern studies in a long lineage
of Columbia academicians over almost half a century who have been outspoken supporters of Palestinian terrorism against Israel. His formal position is Professor of Modern Arab Politics and Intellectual History in the Department of Middle Eastern, South Asian, and African Studies at Columbia University.

While that in itself raises questions about his qualification for conducting a class on the subject of Zionism, he has publicly described Israel as a racist state that has no right to exist and, as a historian, has denied that Jews in the diaspora have historical roots in the Levant. Great choice, Columbia!
This appointment also seems to have been the last straw for Professor Avi Friedman , an award-winning faculty member in Columbia’s business school who in protest submitted his resignation from the faculty in a scathing letter to Katrina Armstrong , the current President of Columbia University.
And he minced no words, noting among other things: “The


university’s decision to appoint Massad to teach a class on Zionism represents a complete abandonment of academic integrity and unbiased scholarship. This appointment was not oversight–it means a deliberate choice that aligns with the university’s ideology. While freedom of speech is fundamental, it must be accompanied by accountability, particular when professors openly celebrate violence.” And he went on, “Your statement regarding Massad’s conduct was both inadequate and disingenuous. His comments were not mere slip-ups that, as you said, ‘created pain for many in our community and contributed to the deep controversy on our campus.’ Rather, they represent his consistent worldview, one he continues to promote through interviews, podcasts, and articles. He stands as a celebrated figure in the intifada movement—a status that Columbia now continues to endorse.”
And then there is, of course, Harvard University, which prior to the current Trump administration quickly reached a settlement regarding two Title VI civil rights lawsuits leveled against the school, promising to implement “strongest” protections of Jewish students against antisemitism on campus.5 Rumors, however, suggest that this settlement has not let Harvard off the hook when it comes to investigations by the Trump Justice Department. Other universities, including, of course, Columbia, but also Northwestern, the University of Minnesota, UC. Berkeley, UCLA, and Portland State among others also are supposedly being investigated.
Steven Davidoff Solomon , a prominent law professor at Berkeley, recently published another Op-ed article in The Wall Street Journal decrying the unchecked antisemitism at his university. This time, he, indeed, asked President Trump directly and publicly “to investigate his campus because of its hostile environment for Jews and women, thereby violating Title VI.” 6 Examples for discrimination he noted were, for example, inclusion in a list of lectures that students must attend at the university to be eligible for a course grade better than a B, which included a lecture denying any sexual assault by Hamas operatives on October 7, 2023. Moreover, the article also alleged that professors in even non-political subject areas like computer science have launched
into antisemitic outbursts against Israel in some of their lectures.
1. Subbaramian N, Belkin D. The Wall Street Journal . Updated January 31,2025. https://www.wsj.com/ us-news/education/trump-dei-banfederal-funding-higher-education8ae81c40 ; In print, February 2, 2025. pA3
2. Mac Ghlionn J. New York Post, February 2, 2025, p36 3. Sulkin M. The Free Press. January 6, 2025. https://www.thefp. com/p/Columbia-university-antiIsrael-museum-of-terror?utm_ source=substack&utm_medium=e mail 4. Schwalb J. The Washington Free Beacon. February 3, 2025, https://freebeacon.com/campus/ columbia-business-school-professorresigns-citing-pro-hamas-colleaguejoseph-mas sads-course-on-zionism/ 5. Zhukovsky N. The New York Sun. Updated January 21, 2025. https://www.nysun.com/ article/a-watershed-momentharvard-settling-antisemitismlawsuit-promises-to-implement-s trongest-protections-of-jewishstudents
6. Davidoff Salomon S. The Wall Street Journal, February 2, 2025. https://www.wsj.com/opinion/mrtrump-investigate-my-campus-hamasrape-denial-hostile-environment-forjews-an d-women-politics-77dec881
*Zuckerberg no longer believes in “factcheckers” and—maybe— “experts”
So after claiming first that his companies were not censoring, the Meta chief now throws the hammer at the Obama and especially the Biden administrations, practically claiming that government officials forced his companies into censoring what the government did not want the public to see or hear. And to
prove how “new-born” he was, he also announced that his companies would do away with “fact checkers.”
But the term “fact checker” has changed since the advent of social media. In the good old days when legacy media still ruled, we all were used to getting calls from fact checkers after we had given an interview: Was our name spelled correctly? Were our titles correct and complete? Did we really say so and so? And that was it; the fact checker checked whether the facts as writers noted in an article were correct.
But this is not what Zuckerberg’s “fact checkers” (we, therefore, on purpose put them under quotation marks) and even “fact checkers” in many legacy media these days are doing: The don’t call you; they don’t have to because they are “experts” who, therefore, already know what “real” or ‘fake” facts are. They don’t even have to ask; they know better anyhow! Does that sound familiar? Of course, it does because we have repeatedly in these pages attacked the excessive importance given to experts in medicine. An article in the recently reborn New York Sun, 1 therefore, is not too surprising but still seems a little far-fetched when the author tries to make the point that “Zuckerberg’s rebuke of so-called ‘fact checkers’ reflects a power shift away from experts.”
That does not mean that we— and it seems high time—do not
indeed perceive a power shift away from experts; but that appears to have more to do with Anthony S. Fauci, MD , requiring a prospective pardon from President Biden for all the lies he presented to the American people during COVID-19, than with “fact checkers” at Facebook.
1. Barone M. The New York Sun. https://www.nysun.com/article/ zuckerberg-rebuke-of-so-calledfact0checkers-reflects-power-shiftaway-from-experts


SOURCE: CNN
*And guess where the SARS CoV-2 virus really originated?
Interestingly, just hours after the new Trump administration took over, the CIA shifted the organization’s assessment on the COVID origin to a lab leak theory. And on a side note, this analysis allegedly started already in the Biden administration but apparently—gentlemanly—was left for the new CIA director in the Trump administration, 1 John Radcliff , to announce (we miss you already Dr. Fauci!).

Simple common sense— expressed in these pages of the VOICE in the early months of the pandemic— made this already then the most likely explanation, and it did not take the sophistication of a spy agency when it became known that China’s principal SARS virus research facility was in the city where the outbreak started, when the Chinese government announced a military takeover of this facility, when the Chinese government shut down all information about the outbreak, and when innumerable attempts at finding an animal source in the wet market of the city failed.
And then, of course, came the Fauci-NIH cover-up, until it became increasingly clear that not only was the Chinese national research center the most likely source, but the research that may have produced the virus was—likely secretly and illegally—financed by NIH funds provided by Fauci and Francis S. Collins, MD , then the head of NIH (and, therefore, the prospective and unlimited pardon of Fauci by Biden). What a story!
And what makes the story even more fascinating is the fact that the new NIH boss is Jay Bhattacharya, MD, PhD , who the Fauci/Collins team desperately tried to put on ice after he was one of the principal signatories of an open letter to the NIH, known as the Great Barrington Declaration, which severely criticized basically all of Fauci’s recommendations.
And he published two months
ago a summary of a devastating House report on the Department of Health and Human Services’ mostly false COVID propaganda on which the Biden administration spent almost $1 billion, making the point that any pharma company running such a campaign “would have been fined out of existence.” 2
1. Pandy E. Axios. August 26, 2025. https://www.axios.com/2025/01/26/ cia-covid-lab-leak-theory
2. Bhattacharya J. Brownstone Institute. November 2024. https:// www.todayville.com/1233511-2/
It is getting harder to open a medical or science journal without finding an article in one or the other way complaining about the current situation in medical and scientific publishing. Here are a few examples: Nature magazine suddenly discovered (we have been writing about this for years) that flawed trials pollute “gold-standard” medical reviews. 1 Of course they do, just as they pollute meta-analyses, and the “more garbage gets into the literature, the more garbage will come out of it,” to reinterpret an old IBM dictum.
And then there are, of course, all the problems with the peer review process which—at least in many journals—can only be described as, to different degrees, definitely lacking. An article in Medscape Medical News therefore unsurprisingly raised the question, “can science trust peer review?” 2 And guess who is asked to answer the
question? The US District Court for the Southern District of New York will be determining whether scientific publishers have been compromising the peer review process on purpose and for-profit because a California-based neuroscientist filed a class-action lawsuit against six of the most prominent publishing houses.
As the article, however, also points out, not everybody agrees that things are getting worse. Some so-called “experts” interviewed on the subject felt that these difficulties have turned a corner because of increasing research on the subject and more public discussion. We don’t think so, as our introduction already indicated; but we will see!
That our impression may be the correct one is also supported by an even more recent article in Medscape Medical News pointing out an increasing credibility crisis of scientific publications in general. 3 And artificial intelligence (A.I.) is not making things any better. To the contrary, indeed, quoting a paper in Science magazine, the article claims that journals have become inundated with lowquality contributions generated by A.I. Citing recent studies, the article also had nothing good to say about peer review, with valueless peer reviews, of course, severely damaging the integrity of scientific literature.
But likely the most surprising article we noted in our ongoing literature review was in The New York Times of January 24, 2025
(electronically), and on January 26, 2025, in print, written as a Guest Essay by Charles Piller, an investigative journalist for Science magazine, titled “Fraud Has Delayed A Cure for Alzheimer’s.” 4 In an unusually long piece occupying almost two full pages of the newspaper’s Opinion Page, Piller concluded that research into Alzheimer’s disease “has been rife with deception,” and what the article accused some prominent scientists of was outright scientific fraud.
Data fabrication in research on Alzheimer’s disease and Parkinson’s disease even resulted in the ouster of Eliezer Masliah, MD , as scientific director of the National Institute of Aging’s (NIA) neuroscience division after—among other accusations—having been found guilty of “falsifications and/or fabrications involving re-use and relabeled figure panels representing different experimental results.” 5
Masliah has been an author or co-author of over 800 peerreviewed papers and was considered one of the world’s leading experts on alphasynuclein, a protein involved in Alzheimer’s as well as Parkinson’s. Based on his now tainted research, this protein has been the target of several clinical drug trials.
Scientific fraud is, of course, at the very bottom of all problems medical and scientific publishing is suffering from. It not only involves the researcher(s) who


commit the fraud, but also the peer review process that does not discover the fraud, the journal that publishes the paper, the publisher who owns the journal, the academic institution that does not control what is happening in its laboratories, the professional society that does not speak up when it becomes clear that something in the field is not “kosher,” the granting organization with its own failed peer review process and follow up to awarded grants, and many other players. In short, the undeniable increase in scientific fraud is irrefutably symptomatic of a multi-organ disease for which a cure is urgently needed.
And now also a word about “predatory journals,”—so-called because they misrepresent themselves as scholarly journals for in principle mostly only financial gain and without usually even meeting scholarly publication standards. An Editorial in The New England Journal of Medicine recently addressed this subject in an attempt “to protect their prey” which, of course, are
the scientists who publish in these journals. 6 Suffice it to say, publishing papers in such journals will impress only the uninformed. Signed by 12 senior editors of leading medical journals, the Editorial basically summarized what can be done to minimize the impact of such predatory journals. Unsurprisingly, there, of course, exist mutual service benefits between paper mills and predatory journals which in practical terms means that one will rarely find a decent paper in a predatory journal. But that must be communicated. The editorial, therefore, divided its recommendations between authors, institutions, funding organizations, and journal editors. Definitely worth a quick read!
And while we are talking about paper mills and predatory medical journals, let’s also not forget about what one could call “predatory authors.” A News item in Nature magazine recently noted the proliferation of “precocious” early career scientists who have racked up huge numbers of citations since 2019. 7 According to a preprint (please note the preliminary nature of preprints!) these authors on average publish more than one paper per week (wow!).
And while they may just represent an especially busy and hardworking group of investigators, more than one paper per week, of course, raises serious questions, even if one works in a large group that shares authorship (Ioannidis

JPA, et al. Preprint at bioRxiv https:doi.org/n2cz.2024).
1. Van Norton R. Nature 20125;637:256-257
2. Turone F. Medscape Medical News. October 9, 2024. https:// www.medscape.com/viewarticle/ can-science-trust-peer-reviewlawsuit-targets-publishers2024a1000ifu?form =fpf
3. Kron T. https://www.medscape. com/viewarticle/scientificpublications-fac...O_mscpmrk_ bom_top-content_etid7195303&ua c=223637CN&impID=7195303
4. Piller C. The New York Times. January 24, 2025. https://www. nytimes.com/2025/01/24/opinion/ alzheimers-fraud-cure.html
5. Alzforum. October 17, 2024. https://www.alzforum.org/news/ community-news/data-fabricationousted-nia-neuroscience-directoreliezer-masliah
6. Laine et al., N Engl J Med 2025;3923):283-285
7. Soliman A. Nature 2025; 637:5255226
*Trouble at eLife
The science journal eLife has been in the news for some time. To be specific, it has been in the news since it announced a radically new publishing model involving not only open access (of course, no longer considered a new model), which posts all submissions sent out for review along with their reviews before deciding on accepting or rejecting a paper. Indeed, only a small minority of submitted papers are ultimately accepted.
Using this process now for some time, everybody receiving their weekly listing of papers (sometimes even bi-weekly) cannot but be impressed by the number of submissions. From a business standpoint—
considering a $2,500 review fee—the model, therefore, has obviously been very successful, leading to an explosive increase in recruited editors at the journal, though with some internal upheaval.
Now, however, Clarivate, the UKbased company that calculates a journal’s Impact Factor (IF), has announced that it will stop assigning eLife an IF (the IF reflects how often papers published in a given journal is cited in other publications and is, therefore, widely understood as a quality parameter for a journal). Unsurprisingly, as a recent article in Nature magazine noted, submissions have already dipped. 1 The article further notes that, while other journal/publishers have been enticed to consider this model, this new development may stop any considerations of adopting this model or even only parts of it.
1. Kwon D. Nature 2025;637:258-259
An article in Medscape Medical News under the section Business of Medicine recently reviewed the status of competition in the private health insurance market in the country, reaching somewhat contradicting conclusions. 1 On the one hand government data clearly demonstrate declining competition in markets between insurers since 2011. But the data also demonstrate that this trend
appears to have slowed and in some states may even have reversed.
At the same time the American Medical Association (AMA) considers a large majority of insurance markets to have remained stubbornly concentrated, with mergers further lessening competition. Especially in major metro areas concentrations are very significant: In 47% of major metro areas one single insurer dominates at least half of the market. Medicare Advantage markets were highly concentrated in 97% of metro areas.
Not to be forgotten—though not addressed in the article— concentration of economic power is observed not only in the insurance market. Provider functions are also increasingly concentrated through mergers of health care systems and purchases of physician practices by these health care systems. Neither is, of course, good for physicians and, therefore, nobody can be surprised that private practice medicine, which used to be the backbone of U.S health care is quickly disappearing.
With physicians having mostly lost even the little influence they used to have within hospitals and in determining fees in the insurance market, the new antagonists are the large regional health care systems and the major insurance providers in their geographic region. Mutual dependency has so-far mostly kept the peace
but—sooner or later—the core conflict between these two behemoths (the pricing of services) will reach crisis point. With expected decreases in Medicare, Medicaid, and other federal government reimbursements for medical services as recently suggested in The New York Times , 2 one can expect these clashes to be around the corner because health care systems have been subsidizing governmentpaid health care for decades through higher payments from private insurances. And they— understandably—have started to object!
1. Dotinga R. Medscape Medical News. https://www.medscape.com/ viewarticle/competition-remainselusive-private-insurance-market2025a10001tn?form =fpf 2. The New York Times. Anti-Poverty Programs. January 31, 2025; pA13
In the VOICE , of course, a steady subject for several years, we never get tired reading “bad stuff” about private equity in all of health care. A recent article in The Wall Street Journal, 1 therefore, unsurprisingly attracted our attention when it described a recent bipartisan Senate report as “blasting” the role of Private Equity in health care. The report, indeed, went so far as to state that these kinds of investments are putting the whole medical system in the U.S. at risk.
Our antipathy to Private Equity, of course, to a large
degree stems from its heavy involvement in the infertility field, but that is a separate subject, to be addressed elsewhere.
1. Cumming C. The Wall Street Journal. January 8, 2025. https://www.wsj.com/articles/senatereport-blasts-private-equitys-role-inhealthcare-b77d711f


If you don’t know yet who William Albert Ackman, MBA (Harvard) is, you are clearly in a small minority because, especially since the October 7 events, he has become very visible beyond the business community, where he was already very well known before. He is an American billionaire hedge fund manager who is the founder and chief executive officer of Pershing Square Capital Management, a hedge fund management company. He is married to Neri Oxman, PhD, who was a Professor at MIT and now owns her own company. The couple also heads a private research foundation through which they donate millions for medical and basic science research.
Though we have mentioned
Ackman in the VOICE regarding his activism against university and college administrations for not doing enough to fight the antisemitism on campuses after October 7 (Ackman was especially outspoken about what happened in those early days at his alma mater, Harvard), none of these issues are why we are bringing him up here. The reason for this short commentary is his announcement that he would like to merge his company –Pershing Square – with Howard Hughes Holdings in a move that would transform this company, in principle a real estate firm, into another modern-day Berkshire Hathaway, as an article in CoStar News 1 recently reported.
And why does this have relevance to medicine? Because this company controls the Howard Hughes Medical Institute (HHMI), one of the leading science philanthropies in the world with the mission of advancing basic biomedical research and science education for the benefit of humanity. 2 In other words, should this merger go through, Ackman, who already heads a major medical and science philanthropy, may, in combination with the HHMI, become a philanthropic powerhouse in size comparable to the NIH and, with it, one of the nation’s most important science voices. And, just apropos, Ackman in a very interesting recent interview publicly announced his availability for public office, should the country call.
1. Carlisle C. CoStar News. January 13, 2025. https://www.costar.com/ article/1369487906/bill-ackman-seeksto-transform-howard-hughes-holdingsinto-modern-d ay-berkshire-hathaway 2. https://hhmi-curt.cornell.edu/about/ howard-hughes-medical-institute/
Now that President Trump signed an executive order restricting gender-affirming treatments for minors, U.S. hospitals have been suspending what The Guardian calls “healthcare for transgender youth.” 1 But that is, of course, not what the executive order said: The order very clearly does not suspend health care to transgender youth; it only suspended gender transition treatments for minors and up to age 19 under a threat of withholding federal funding for hospitals providing such genderaffirming care.
But this imprecision in choosing the words in the headline to an article is, of course, not accidental, because a rather astonishing portion of legacy media outlets in the U.S. still appear to support gender transition treatments for minors: Other headlines document this fact: “Things to know about how Trump’s policies target transgender people” was for example a headline of NBC News based on an The Associated Press send-out on the 3rd of February. 2 And PBS, of course, two days earlier, also shared in this opinion following another Associated Press article by Geoff Mulvihill with the headline, “6 ways Trump’s executive orders
are targeting transgender people.” 3
And this is, of course, astonishing, as we here in these pages of the VOICE have extensively documented, especially in follow up to the Cass Review in the UK. Among very few news outlets, with The Free Pres s of course for many months leading the charge in the U.S., only the similarly minded recently reborn New York Sun , pointed out the hypocrisy prevailing in the U.S. press and in the U.S. medical community (in contrast to most European colleagues) in maintaining the orthodoxy that such treatments are safe and effective for gender-distressed minors. They, of course, aren’t, and to say otherwise is truly shameful, especially when the argument comes from the medical community. And an article in The New York Sun recently pointed out that prominent U.S. professional societies, such as the American Academy of Pediatrics and the American Medical Association, have indeed aggressively supported such treatments in the past and falsely described them as effective and even lifesaving in preventing suicides. 4
And, remarkably, the medical and legal establishment in the U.S. continues to a significant degree to line up in defense of continued medical practice that allows gender transition treatments of juveniles. 5
But most remarkably, New York Attorney General Letitia James (of over $500 million verdict in
Trump trial!) issued on February 3, 2025, a formal warning to New York hospitals that they would be in violation of state discrimination laws if they complied with President Trump’s executive order that outlawed certain sex-change treatments for minors. 6
By advising New York hospitals that they must defy the President’s executive order, James is very clearly reemphasizing her original election message as Attorney


General that she considers herself the leading political voice in New York state in opposing Trumpism which now, of course, includes the second Trump administration. Could this statement, therefore, be the start of her campaign for governor?
It certainly clearly demonstrates her continued intent of waging war against Trump, even though—and maybe exactly because—he once again resides in the White House.
REFERENCES
1. Betts A. The Guardian, February 3,

2025. https://www.theguardian.com/ us-news/2025/feb/03/trans-youthhealthcare-hospitals-trump
2. The Associated Press. February 3, 2025, https://www.nbcnews.com/ nbc-out/out-politics-and-policy/ trump-policies-transgender-peoplercna190424
3. Mulvihill G. The Associated Press. February 1, 2025, https://www. pbs.org/newshour/politics/6-waystrumps-executive-orders-are-targetingtransgender-people
4. Ryan B. The New York Sun. Updated January 24, 2025. https://www.nysun. com/article/new-research-raises-moredoubts-about-safety-and-benefitsof-gender-transition-tre atments-forminors
5. Aaron DG, Konnoth C. N Engl J Med 2025;392(6):526-527
6. Walker C. Tuthout. February 4, 2025. https://truthout.org/articles/ny-agletitia-james-tells-hospitals-they-mustdefy-trumps-anti-trans-order/
*And more on artificial intelligence (A.I.),
though it may be more bad than good news
One almost wonders which among the two papers we are mentioning here is worse: One, an Opinion article in Science 1 magazine by Frederik Joelving from R etraction Watch , reported that AI-generated commentaries flood medical journals, distorting journal metrics. A joint investigation by Science and Retraction Watch confirmed this fact at several journals in different specialty areas. Letter, comments, and editorials in several among them made up over half of all submissions. Interestingly over 80% of these commentaries are coming from South Asian countries, compared to less than 20% of research and review articles.
Their investigation furthermore
revealed that everybody appears to benefit from the scheme, even though it floods the literature with poor quality publications and threatened metrics for scholarly output and impact: authors get quick and easy publications and citations and don’t even need original data. For journals, moreover, it can be good business, especially if the journal has publication charges. And institutions, as the article pointed out, especially in India, use such papers for advertisement purposes. And we thought we by now know all the dirty laundry in medical publishing!
But now to the second paper, which may be bad news for very different reasons: Up to this point the widely held assumption in the medical community has been that A.I will, except in rare circumstances, not replace physicians as diagnosticians but “augment” their decision making. But as a recent paper in JAMA Network Open suggested, this may have been a much too optimistic view of the need for human intelligence. 2 The paper involved use of a large language A.I. model which somewhat surprisingly did not significantly affect physicians’ diagnostic reasoning. But even more surprisingly the large language model—alone—performed better than physicians, whether alone or with help of the large language model.
If confirmed in other studies, this observation would significantly affect how physicians have to view the
threat of being replaced, especially in certain functions and – maybe – in some medical specialties more than others. So far we, however, would consider the suggestions made in this paper as extremely preliminary. Moreover, the methodology behind this study seems somewhat questionable. So don’t start looking for another career yet; you still may make it to retirement!
1. Joelving F. Science 2024;386(6728):1331-1332
2. Goh et al., JAMA Network Open 2024;7(1):e2440969
*Medicine
is continuing in becoming an increasingly female profession
For the sixth year in a row more women than men have been entering medical school studies. 1 This stands in contrast to, for example, the 1980s, when only approximately 30% of medical students were female. And if we go back to the 1970s, even Ob/ Gyn residencies – in those days almost considered a surgical specialty – hardly ever had a female resident. And how that has changed: nowadays, Ob/Gyn residencies hardly ever have a male resident in their midst.
In 2024/2025, women were 57% of applicants, 55% of matriculants, pretty steady with the preceding year, where the respective percentages were 55% and 54% based on reports from the Association of American Medical Colleges (AAMC).

One big reason for this trend is that more women are getting undergraduate degrees and that the par to males is, indeed, increasing. As the article noted, in 1995 women and men had bachelor’s degrees at very similar percentages. Today women have a significant lead: 47% of women at ages 25-34 have one, but only 37% of men.
1. Gallegos A. Medscape Medical News. January 28, 2025. https://www.medscape.com/ viewarticle/more-women-enteringmedical-school-than-men-sixthstraight-2025a10002 1y?form=fpf
*And the anti-aging train rolls on It appears that a microRNA molecule, at least in mice, can rejuvenate aged animals by simply restoring old cells, thereby expanding their lifetime and demonstrating diminished aging markers. 1 The Chinese investigators of this paper propose an antiaging strategy which aims to reverse the proliferative arrest of senescent cells. Exosomal miR-302b is identified as a candidate that targets the cell cycle inhibitors Cdkn1a and Ccng2, rejuvenating aging mice by improving physical and cognitive functions, extending lifespan, and apparently demonstrating no safety concerns throughout a 24-months observation period.
The experiments were simple and straightforward: Using 20to 25-month-old mice (60-70 years in human years), they were injected with human exosomes either loaded with extra mir302b (affecting 2 genes in cell
division) or not. Saline was used in controls. Treated mice lived for approximately 4.5 months longer (roughly 9 years in humans) and re-grew hair and had better balance as well as grip strength. They also had lower inflammation markers. In short miR-302b treatment not only expanded life span, but also improved the animals physically as well as mentally, while reducing aging markers.
The paper was also subject to a News article in Nature magazine. And then there is a Commentary article by CHR friend and colleague Eli Adashi, MD, in The American Journal of Medicine , 2 in which he muses about human immortality by pointing out the progress made in antiaging research, offering a very optimistic outlook by concluding that, “all indications are that the ability to arrest aging with immortality in mind may just be a matter of time.” Of course, hoping that he is correct, it still appears important to differentiate between a concept of long(er)jevity and immortality. Mankind for the moment would be more than satisfied with only the former.
1. Bi et al., Cell Metab 2025;37:527-541
2. Simms C. Nature 2025;637:10301031
We saw this question raised in a book review in Nature magazine 1 and found it interesting enough to bring it here to our readers’ attention. The modern synthesis of evolution is still the current
textbook evolutionary theory, widely considered an absolute dogma. Now the author of the book review is telling us that new thinking on the subject is overdue, as offered by four eminent evolutionary biologists in a recently published book, “Evolution Evolving,” 2 (see figure belowt).
Lala et al., Evolution Evolving: The Developmental Origins of Adaptation and Biodiversity. Viking Books 2024 .
The dogma of “modern synthesis” claims that evolutionary adaptations exclusively occur through gradual and natural selection of DNA mutations which arise at random. The five authors of this book have for considerable since approximately 2015 been proposing as an alternative—the so-called “extended modern synthesis”—that how and/or where an organism develops also plays an important role. In other words, evolution is not only a process of natural DNA selection but also in what environment this selection occurs. 3

And the debate is hotly contested.
Examples for the importance of the environment abound: Take for example the Mexican tetra fish, of which some populations (A. mexicanus) are blind cave fish living in darkness. Other populations of the same fish exist as surface dwellers and have full vision. When those surface dwellers, however, are kept in full darkness for two years, they develop traits that mimic the blind cave fish.
So, which of the two theories is correct? To us it seems that both are correct, not different to the principles of epigenetics: The basis is the DNA; but then comes the environment into play, determining how this DNA functions.
1. Jablonka E. Nature 2025;637:539541
2. Kevin Lala et al., Evolution Evolving: The Developmental Origins of Adaptation and Biodiversity. Viking Books, 2024.
3. Lala et al., Proc R Soc B2015;B282.20151019
Here is what happens when we have our blood tested: Once the blood sample has been run through whatever testing mechanism is used, the result is compared with a previously determined average result in an average population of practically all ages. In other words, our result will be assessed as normal if it falls within a usually quite wide
range of what the test defines as “normal” or as “abnormal” in a general population, if the result falls outside of this range. But for several reasons this usually quite expansive range of normal creates problems: We, for example, have in these pages on many occasions raised the point that reproductive hormone levels must be viewed in an agedependent way (which, apropos, to this day only rarely happens). And an important new paper demonstrated an additional, and very logical, finding: Using the complete blood count (CBC)—likely the single most frequently ordered blood test in medicine—as an example, the study demonstrated that an individual’s results are overall in general very stable, and changes may, indeed, indicate disease. 1
Setpoint in healthy adult individuals were found associated with significant clinical risk, with absolute risks for some diseases and morbidities varying by more than 2% (this included myocardial infarctions, stroke, diabetes, renal disease, and osteoporosis) and absolute risk for 10 year-mortality varied by more than 5%. Here is very obviously yet another job waiting for A.I.!
1. Fot et al., Nature 2025;637:430-438
A word about stem cell donations
Far beyond just the medical literature, so-called stem cell donations have, indisputably, become one of the “hottest” subjects in medicine. They,
indeed, also have become one of the most “abused” subjects, likely best demonstrated by all the “stem cell clinics” that, often to the chagrin of the FDA, have opened in the U.S. and across the border in Mexico, which offer alleged treatments and cures for practically almost any malady. And reproductive medicine is, of course, no exception.
Information of “real” stem cell treatments, therefore, always are welcome and this is exactly what a brief recent article in JAMA is offering regarding allogeneic (from another individual obtained) stem cell donation entails. 1 This article not only appears timely but in a way also informs on the difference between “real” and “fake” stem cell therapies. Just one example: If you get your own fat-cells injected, those are “autologous” (your own) and not “allogeneic.” Moreover, just because you get your fat cells injected, does not mean that among the few cells injected are real stem cells.
1. Amonoo et al., JAMA 2025;333(1):8182
BRIEFING: That “food is medicine” is an increasingly prevalent phrase in medicine, and it also applies to fertility. This section of the VOICE caters to this concept in a wide variety of ways, from discussing serious nutritional science, to offering critical reviews of so-called nutritional supplements that are alleged to improve fertility and, often, not only don’t help, but may even hurt pregnancy chances. With obesity becoming an increasingly frequent co-diagnosis in infertility practice, weight loss with GLP-1 receptor agonist drugs are promising significant outcome benefits. The CHR has, indeed, been among the first fertility centers utilizing this new family of drugs. And, finally, on a lighter note, with a large majority of the CHR’s patients having to travel to New York City to receive care, many indeed even from outside the U.S., we here also offer the CHR’s (obviously biased) and very selective view of the city’s amazing restaurant scene.
The medical journal Lancet Diabetes & Endocrinology published a report by a global commission of experts, calling for a radical shift in how obesity is diagnosed, with a key change being less reliance on the body mass index (BMI).1 In another important change, the Commission identified when obesity is a risk factor (preclinical obesity) and when it represents a stand-alone illness (clinical obesity).
The changes arose from the recognition that, despite obesity affecting almost an eighth of the world population, 2 a global consensus on the classification and definition of obesity had not been reached before. Individuals living with obesity have different health profiles and needs, but are often discussed as a single entity, defined by one single parameter (BMI), or not discussed at all. The Commission included 56 leading experts from high-income, middle-income, and low-income countries and has been endorsed by more than 75 international medical organizations with a stake in obesity and the care of those affected.

The new, evidence-based definition distinguishes “clinical obesity,” a chronic, systemic disease state directly caused by excess adiposity, from “preclinical obesity,” a condition of excess adiposity without current organ dysfunction or limitations in daily activities but with increased future health risk. Given the limitations of BMI, the Commission uses other measurements of body size (waist circumference, waist-to-hip ratio, or waist-to-height ratio), in addition to BMI, to define obesity.
To start, current epidemiological data on obesity prevalence, which rely solely on BMI, must be updated to reflect obesity as a spectrum of medical presentations. Preliminary audits of available databases are already underway and suggest that a substantial number of people with obesity do not fulfill the criteria for clinical obesity. However, these analyses are limited by the use of historical, incomplete data. Therefore, databases must include a fuller picture of the individual's health-care status. Furthermore, there is substantial scope for stratification of clinical obesity into different subtypes, potentially based on their clinical presentation or pathophysiology, which should enable better management and understanding.
REFERENCES
1. Rubino et al., Lancet Diabetes & Endocrinol 2025; 2. NCD Risk factor Collaboration. The lancet 2024;403(10431):P1027-1050
A recent study in Nature Food attracted considerable attention because it suggested that prior survey-based studies linking allegedly consumed diets to health outcomes may be fatally flawed because of inaccuracies in the reporting of food intake by study subjects. Applying a validated equation to two large datasets (National Diet and Nutrition Survey and National Health and Nutrition Examination Survey), the investigators found that the level of misreporting was >50%. The macronutrient composition from dietary reports in these studies was systematically biased as the level of misreporting increased, leading to potentially spurious associations between diet components and body mass index.1
A Commentary article in Science also discussed the conclusions the nutrition field has to reach from this study. 2 One cited expert concluded that “we got to try and use new technologies to do better.” In other words, a significant portion of what we currently believe to link certain foods to certain diseases is probably inaccurate. This paper, of course, also explains why “diet data” have been so contradictory. A good example may be a recent article in the European Heart Journal which concluded that drinking coffee in the morning may be more strongly associated with lower risk of mortality than drinking coffee later in the day. 3 While even the general information by these Chinese investigators that coffee drinking reduces mortality is interesting, we would, considering the previously discussed publication, not put too much emphasis on this paper.
REFERENCES
1. Bajunaid et al., Nature Food 2025;6:58-71
2. Offord C. Science 2025;387:6732:352
3. Wang et al., Europ Heart J. 2025
This is, according to a recent paper in PloS One, what research at Ohio State University suggests.1 A recent summary of the paper by Healio summarized the study very well: (i) Ketosis with and without exogenous ketone supplementation resulted in realigned or restarted menses. (ii) Ketogenic as well as low-fat diets after six weeks resulted in weight loss, declines in BMI, positive changes in body composition, and insulin sensitivity.
Moreover, compared with a low-fat diet, nutritional ketosis—with or without exogenous ketones—can have a positive impact on self-reported menses (that menses is self-reported is, of course, here, too, of importance), restarting or realigning menstrual cycles. The first author of the paper in the Healio article2 was, indeed, quoted as noting that a 33-yearold participant in the study who never before had experienced a menses, after five days of being in a nutritional ketosis, experienced a first menses.
REFERENCES
1. Kackley et al., PloS One 2024;19(8):e0293670
2. Healio. December 11, 2024. https://www.healio.com/news/womens-health-obgyn/20241211/keto-diet-may-restart-realign-menstrual-cyclesfor women-with-obesity


Eric Topol, MD
THE RED-MEAT STORY: We simply cannot go without including at least some of Eric Topol’s commentaries in the VOICE. He recently offered two of those commentaries, fitting this section of the VOICE. In a first he offers an “Update on the Red Meat Story.”1 Here, too, he noted that many red meat studies relied on self-reporting and, therefore, have to be judged as unreliable.
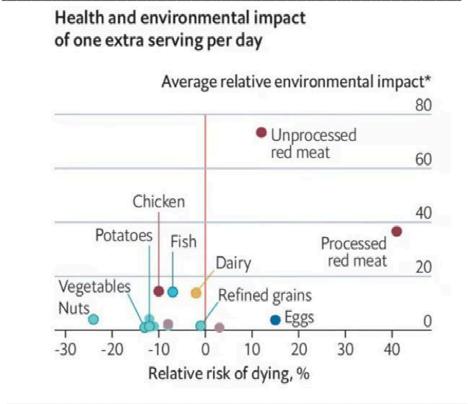
Summarizing current literature, the figure above demonstrates how poorly red meat (processed and unprocessed) relates to other food in relative risk of dying (and interestingly, also in adverse environmental impact).
He then, however, turned to a new paper in Nature Microbiology, 2 where the gut microbiome was assessed in over 21,500 participants. 656 vegans,
1,088 vegetarians, and 19,187 omnivores, with each having distinct microbial profiles: The omnivores’ profile was mostly determined by red meat microbes associated with inflammation and adverse cardiovascular fates and previously associated with inflammatory bowel disease (IBD) and colon cancer. Microbes associated with a vegan diet, however, showed the opposite effects and reduced inflammation and promoted cardiovascular health. Individuals with primarily a vegetarian diet fell inbetween the other two groups.
Topol then addressed another recent study in the medical journal Neurology which investigated longterm intake of red meat in relation to dementia risk and cognitive function in US adults. 3 The study involved 133,771 participants—interestingly 65.4% female—with mean baseline age 48.9 years. Participants with processed red meat intake of >).25 serving/day had a 13% higher risk of dementia than subjects with intake of <0.10 serving/day and a 14% higher risk of subjective cognitive decline, and was associated with accelerated aging in global cognition and in verbal memory. Unprocessed meat of >1.0 serving/day compared with <0.5 serving/day was associated with a 16% higher risk of subjective cognitive decline. Exchanging 1 serving of nuts and legumes per day for processed red meat was associated with a 19% lower risk of dementia, fewer years of cognitive aging, and a 21% lower risk of subjective cognitive decline.
Though this study, of course, also was dependent on participants’ memory – as above noted, not a satisfactory study design to assess associations between selected food intakes and medical consequences, the congruence of results in both studies of a rather large patient population further increase concerns about red meat intake, especially processed red meat.
ON MICROBIOTICA AND SUGAR CRAVINGS: And now to Topol’s second subject: how our gut microbiome can drive sugar craving.4 He noted that the gut microbiome communicates with the brain along four pathways: (i) Metabolites from the microbiome get into blood, cross the blood-brain barrier, affecting the brain directly; (ii) the hut microbiome signals the gut’s immune cells to secrete cytokines
and/or travel to the brain; (iii) gut bacteria or other microorganisms) make gut endocrine cells release hormones such as GLP-1 which enter the bloodstream and this way get to the brain, and (iv) gut microbiota signal the afferent gut nerve fibers which communicate with the brain. And, as he also noted, all of this is not a one-way street but bi-directional relationship between brain and gut, with the brain regulating the microbiome of the gut through the hypothalamic-pituitary axis and efferent nerve fibers through the vagus nerve plexus. In short hormones, the immune system, and neurons are engaged in steady crosstalk.
Topol in his article then refers to a recent review in The New England Journal of Medicine5 which described basic and translational research on the complex physiological processes of hunger, which regulate feeding habits and are influenced by socioeconomic, cultural, and behavioral factors.
Hunger is controlled by classic “homeostasis hunger,” driven by metabolic needs, while “hedonic hunger” describes food intake based on impulse, habits, stress and other stimuli. And the third cause of hunger is then the so-called “microbiota-driven hunger.” As it turns out gut lining cells contain free fatty acid 4 (Ffar4) receptors. Now a mouse study involving several mouse models shed some new light on what produces sugar preference. It appears mutations of the Ffar4 gene are important in sweet intake preference based on a study of 65,000 UK biobank participants and relationships.
And here are a few key findings Topol summarized as follows: (i) Depressed Ffar4 expression was linked to higher fasting blood glucose levels and sugar preference, a finding supported by data from the UK Biobank. Knockout of Ffar4 especially in gut intestinal cells increased sugar preference, while overexpression suppressed sugar intake. (ii) The bacterium Bacteroides vulgatus was causally linked to sugar intake and above described Ffar4 behavior. (iii) Panthothenic acid (Vitamin B5) was the first metabolite of B vulgatus significantly changed in culture, with its repletion in Ffar4 knockout mice (usually increase their sugar preference) now being significantly suppressed. Pantothenic acid in mice and humans also increased GLP-1 levels, which in turn stimulated release of fibroblast growth factor
(FGF21) which – when directly administered to the brain – inhibited sugar preference. Confirming, FGF21 knockout or recombinant protein showed an up and down effect on sugar preference.
This new paper thus identified the specific bacterium and its metabolite and proteins (GLP1, FGF21) which drive and inhibit sugar craving. A pretty interesting accomplishment with potentially significant therapeutic consequences for diabetes and obesity!
REFERENCES
1. Topol E.Ground Truth. January 19, 2025. https://erictopol. substack.com/p/the-updated-red-meat-story
2. Fackelman et al., Nat Microbiol 2025;10:41-52
3. Li et al., Neurology 2025;104(3). https://doi.org/10.1212/ WNL.0000000000210286
4. Topol E. Ground truth. January 26, 2025. https://erictopol. substack.com/p/how-our-gut-microbiome-can-drive 5. Fasano
A. N Engl J Med 2025;392:372-381
The last paper in the above section was a good transition to news about GLP-1s. And here is a quick update on this fascinating family of (in principle) old drugs with new uses as anti-obesity drugs. How important they have become for the general population is probably best documented by the fact that JAMA recently for the first time dedicated a “Patient Page” to these medications under the heading “Medications for Obesity.”1 The summary statement said: “(These) medications for obesity can help promote weight loss and improve outcomes for people with type 2 diabetes, hypertension, and abdominal lipid levels,” a statement that could, in its lack of specificity, almost have been written by lawyers for a nutritional supplement in order not to upset the FDA.
Medscape Medical News recently reported on a study by investigators from McGill University in Montreal, Canada, which in a systematic review

included 26 randomized controlled trials trying to determine which GLP-1 receptor agonist and coagonist already on the market or being currently investigated produced the greatest weight loss. And the answer was, Retatrutide, a still under investigation once-weekly triple glucose-dependent insulinotropic polypeptide (GIP/GLP-1, and glucagon receptor agonist) from Eli Lilly and Co., ahead of tirzepatide (Munjaro and other names also from Eli Lilly & Co.), a dual agonist, and by single agonist semaglutide (by Novo Nordisk). 2 The article itself appeared in The Annals of Internal Medicine and demonstrated no significant difference in side effects. 3
The article also reemphasized that treatment must be continued if significant regaining of weight is to be avoided. This was also subject of an article in JAMA which in detail addressed also social, ethical, financial, and – ultimately – medical considerations regarding the need for long-term treatments with these drugs.4
1. JAMA Patient page. JAMA 2025;333(1):96
2. Ault A. Medscape Medical News. January 7, 2025. https:// www.medscape.com/viewarticle/retatrutide-producesgreatest-weight-loss-2025a100009a?form=fpf
3. Moiz et al., Annals Int, Med 2025; https://doi.org/10.7326/ ANNALS-24-01590. Ahead of print.
4. Khan et al., JAMA 2025;333(2)113-114
This family of drugs is not yet approved for use in pregnancy. Indeed, some mouse studies have reported an increase in congenital abnormalities. The CHR, and likely most IVF fertility clinics that use these drugs in infertile patients, therefore, require a wash-out period of one month before starting treatment cycles after termination of GLP1 treatments. Preliminary studies of “accidental” use in pregnancy have, however, been reassuring, including a recently published review article of such “accidental” reports.1
A brief article in the BMJ reported on so-called “Ozempic babies,” alleged accidental pregnancies in women on oral contraceptives.1 The allegation is that slowed gastric emptying due to treatment with GLP1s increases the failure rate of oral contraceptives and leads to unwanted pregnancies. This hypothesis
has so-far, however, not been validated. Moreover, since some of these women, as one could expect, experienced miscarriages, the article also raises the question of whether GLP-1 agonists may increase miscarriage risk. 2 Real world evidence with these drugs is, however, so far not very suggestive of either one of these two suspicions which (on a side note) also have so far no possible physiological explanation that could explain how GLP-1s would cause these complications.
Related, a Mini Review In the JCEM recently addressed the literature regarding the potential clinical consequences of delayed gastric emptying with single GLO-1 agonists and the dual agonist Tirzepatid, 3 and found that retained gastric contents at time of upper GI endoscopy are, indeed, found quite frequently but only rarely cause pulmonary aspiration during anesthesia. The ultimate conclusion of the review was that there do not exist yet enough research data to reach any final conclusions.
REFERENCES
1. Drummond et al. Am J Obstet Gynecol 2024.08.024. https:// doi.org/10.1016/jajog2024.08.024
2. Nadaradjah S. BMJ 2025;388:q2440
3. Jalleh et al., JCEM 2025;110:1-15.
And finally, maybe somewhat removed from infertility practice, but certainly relevant to the management of obesity, GLP-1s could help with impulse control and addiction disorders.1
Although this ability of GLP1- receptor agonists has been suspected for some time, it is now coming increasingly into focus, as recently also pointed out in a News article in the BMJ. 2
REFERENCE
1. Xie et al., Nat Med 2025; https://doi.org/10.1038/s41591-02403412-w; ahead of print
2. Mahase E. BMJ 2025;388:r123
All listed restaurants are in Manhattan unless otherwise noted. Like all opinions about restaurants, ours are subjective and are to be understood as such. If you visit one of them, let us know whether you agree with our ratings. We value your feedback.
$ Inexpensive - Not worth the trip + Overall favorite of the CHR
$$ Moderately expensive
$$$ Expensive
$$$$. Special event expensive
• Good v Special vibe
•• Very good
M Michelin starred
••• Excellent V Vegetarian/vegan dishes on
•••• Uniquely delicious the menu
AUSTRIAN
Koloman +/•••/$$/v 16 W 29th Street (212) 790-8970 V; Excellent desserts
Wallsé +/•••/$$/v/* 344 W 11th (212) 352-2300 V; Excellent desserts
Hwa Yuan Szechuan +/•••/$$/v 42 East Broadway (212) 966-6002 V; Authentic Szechuan
Mr. Chow Downtown +/••/$$$/v 121 Hudson St., Tribeca (212) 965 9500 V Uptown 324E, 57th Street (212) 751 9030 V
CONTINENTAL
425 •••/$$$/v 425 Park Avenue (212) 751-6921 V; Gorgeous restaurant
FRENCH
Le Gratin ••/$$ 5 Beekman St. (212) 597-9020 V; Try the gratin potatoes
Le Charlot +/•• /SS 19 E 69th St. (212) 794-6419 V; Best steak au poivre & Thai mussels; great desserts
Le Bernadine +/••••/$$$$/ MMM 155 W 51st (212) 554-1119 V; Mostly seafood. Likely the best NYC restaurant
ITALIAN
Cipriani Downtown +/••/$$/v 376 West Broadway (212) 343 0999 Great food, beautiful people & Uptown 781 5th Avenue (212) 753-5566 Great food and high society
Elio’s +/•••/$$/v 1621 2nd Ave. (212) 772-2242 Best Italian home cooking and where everybody meets
Principe ••/$$/v 50 West Broadway (212) 335-0509 V; mostly seafood but one of the best chicken dishes
Sistina •••/$$$ 24 E 81st St. (212) 861-7660 V; Amazing wine list
FRENCH-ITALIAN
Café Carmellini •••/$$$$/v
JAPANESE
SUSHI
250 Fifth Avenue (212) 231 9200 V; Gorgeous place, top service; sophisticated and adventurous food
Sushi Ann +/••• /$$$$ 8 E 51st St. (212) 755-1780 V; Best quality fish; make reservation at the bar
GENERAL
Sakagura +/•••/$$
211 E 43rd St. (212) 953-7253 V; Amazing food; Best sake selection
Yakitori Torishin +/+++/$$$/M 362 West 53rd Street (212) 757-0108 Unique and amazing skewer restaurant
KOREAN
Jungsik •••/$$$$/ MM 2 Harrison St. (212) 219-0900 Where NYC’s Korean restaurant revolution was born …
Oiji Mi +/•••/$$/v / M 17 W. 19th St. (212) 256-1259 … and has continued
GREEK
Elias Corner (Queens) ••/$ 24-02 31st St. (718) 932-1510 Mostly seafood
HAMBURGERS
Jackson Hole Burgers (the “original”) +/••/$ 232 E 64th St. (212) 371-7187 Not a place for vegetarians
MIDDLE EASTERN-ISRAELI
Dagon ••/$$ 2454 Broadway (212) 873 2466 Best hummus in NYC
NEW YORK JEWISH DELI
P. J. Bernstein’s Deli •/$ 1215 3rd Avenue (212) 879-0914 All the great classics; pastrami, chicken soup PERUVIAN
Mission Ceviche •••/$$ 1400 2nd Avenue (212) 650-0014 If you like Peruvian –the best PIZZA
San Matteo Pizzeria e Cuccina ••/$ 1559 2nd Avenue (212) 861-2434 True Napoli POLISH
Karczma (Brooklyn) +/•/$ 136 Greenpoint Avenue (718) 349-1744 Great authentic Polish food – and dirt-cheap
ROMANIAN-JEWISH
Sammy’s Roumanian Steak House** $$ 112 Stanton St. (212) 673 0330 Authentic JewishRomanian Steak House, with entertainment
UKRAINIAN/RUSSIAN
Caviar Russe +/••••/$$$$/ M 538 Madison Avenue (212) 980-5908 V; Most underrated restaurant in NYC
Russian Samovar •/$/v 256 West 56th St. (212) 757 0168 Great Russian/ Ukrainian food and music
Any suggestions and/or comments, please write to social@thechr.com.



BRIEFING: The VOICE in this section offers commentaries on a broad survey of recent articles in the English literature which the CHR found of interest regarding the practice of clinical infertility, even if, at times, not immediately applicable to daily clinical practice. Articles are mostly chosen for two reasons: their potential translational value for immediate clinical practice or to help in determining where clinical practice might evolve to. Translational research has been at the center of the CHR’s success since its founding in 1981.
*Articles were originally published in the Reproductive Times.
A large group of colleagues from Boston, most employed by and/or past owners of the Boston IVF enterprise, one of the largest IVF clinic chains in the country, which since it was initially sold by its founders has changed hands two or three more times (it is hard not to lose track) and is now part of IVI-RMA, likely the largest private equity-owned worldwide IVF franchise, published a study which claimed to have examined “the effect of one of their a large-scale mergers on in vitro fertilization outcomes and patient satisfaction.
They concluded that clinical outcomes even after big mergers can be maintained. Patient response to the merger was, however, different and quite clearly demonstrated concerns (even though details were not given).
In general, we perceived this paper (which appeared in the format of a Research Letter) as overall rather unsophisticated, insufficiently transparent about how this retrospective study was performed and, to a degree, as rather obviously (and for several reasons) self-serving.
Our principal criticism of this paper is, however, the basic premise that the desirable goal of a merger should be no change. We would argue that this premise alone demonstrates the real conscious or subconscious concerns of the authors that their merger may have had adverse outcome consequences (indeed at least partially met in the perception of the newly formed enterprise by its patients). And – even more importantly – it in our opinion is an absolutely wrong target for a merger because – of course aside from financial gains –the goal of any merger is, at least theoretically, to do better on all fronts: better product, better service, better client perception, etc.
What this paper, therefore, instead projects, is deep pessimism, which (considering its results) indeed appears warranted: IVF outcomes appeared to have remained the same, though even that was not universal, as Clinic A lost some clinical pregnancy rate but appeared to have caught up by live births. Does that mean Clinic A got worse in managing IVF cycles and better in preventing miscarriages?
Considering the small differences, this is likely a silly question to ask; but telling, in how whimsical this study really is, especially considering that Boston IVF apparently treats an unusually young

patient population with mean ages of 34 to 35, when the mean age for all U.S. clinics for years has been over 36 years (The CHR’s in 2024, of course, was 45 years!).
But what is then the correct question to ask? Of course not only in reproductive medicine but, by now, in many (usually cash-flow rich) medical specialty areas, the real basic questions to ask is why are we allowing non-medical interests – and especially Private Equity – to take over medicine. 1 As PitchBook recently noted, private equity between 2018 and 2022 invested over $350 billion in U.S. health care assets, whether by purchasing physician practices, hospitals, or longterm care facilities, and there exist now already an abundance of studies demonstrating two typical changes once an enterprise is purchased by Private Equity: quality of care goes down and prices go up. 2
In a way, the here described study confirmed this as well, at least when it comes to quality because if patient dissatisfaction increases, this is, of course, per-se, a quality issue. Another example from the infertility field is one of the two recently newly published papers by CHR authors (see CHR News in this issue of the VOICE ) which reported that Equity-owned IVF clinics in the U.S. utilize PGT-A in IVF cycles significantly more heavily than clinics owned by physicians and/or hospitals/ universities. 3 Suffice it to say, here presented paper from our Boston colleagues made no mention of any of this.
And then – just before this VOICE went to print – a paper was published in JAMA that reported on a quite large investigation of patient care experiences after Private Equity acquisitions of U.S. hospitals, 4 and the results were anything but reassuring and, by no means surprising considering similar previously reported results. In comparison to control hospitals: Patient care experience in hospitals principle significantly worsened after acquisition by Private Equity in comparison to control hospitals, though we must acknowledge, the difference was much smaller than we would have anticipated.
Since Private Equity usually works on a tight time
schedule of five to seven years before resale, one would expect increasing patient complaints over time and that was, indeed, the case, with peaks of patient unhappiness (considering above-noted time schedule) unsurprisingly reached at three years.
1. Heyward et al., Fertil Steril 2025;123(1)179-181
2. Singh et al., N Engl J Med 2025;392(7):627-629
3. Patrizio et al., J Assist Reprod Genet 2025;42:81-84
4. Bhatla et al., JAMA 2025;333(6):490-497
To a large degree the consequence of Private Equity entering so robustly the fertility field, IVF practice has been growing in leaps and bounds, as in almost every U.S. city the number of IVF clinics over the last decade has significantly increased. But so have the unfilled job openings and, yes, the salaries of almost all positions in the IVF industry.
There simply is not enough staff for hire, not enough REs, not enough embryologists, and/or not enough IVF nurses (we call them at the CHR Clinical Coordinators). As a consequence, most clinics are understaffed and that, of course, has consequences at many different levels. The big, Private Equity-owned chains, moreover, even further aggravated this problem after paying off some major hospitals and/or medical schools –for taking over their formal fellowship programs, thereby securing the opportunity to pick first among the ridiculously small number of REI fellows who graduate every year.
That number under the current fellowship system stands at only approximately 55 REI fellows, who are required to undergo three years of additional training after four years of general OB/GYN residency, all, of course, at absurdly low salaries and with many among them already deeply in debt from student loans during college and medical school.
For our academic establishment, two years of fellowship, with one year primarily dedicated to

clinical training and the second year (supposedly) more geared toward academia and research activities (the emphasis here is on “supposedly” and will be discussed further below) was apparently not enough because the members of this establishment in their infinitive wisdom concluded several years ago that the reproductive endocrinology and infertility (REI) fellowship – in the best interest of this medical specialty field –must be extended to a third, pure-research year. And why was this additional year required? Because—according to the academic establishment—fellows in two years could not be given enough valuable research time to be seriously initiated into academic research careers and, thereby, raise the current very inadequate research level of the REI field as a whole. In other words, the academic leadership of the field in its infinitive wisdom seriously believed that extending the fellowship by a year would convince more fellows to join the academic club, rather than flee into private practice, as a large majority every year had chosen since establishment of a formal fellowship in the field.
And, most amazingly, the same leadership at least pretended to be surprised that after four years of college, four years for medical school, four years of OB/GYN residency, and three years of REI fellowship (i.e., after 15 years of overall incomenegative education) the result was exactly the opposite: Mostly Private Equity owned IVF clinic networks already signed fellows up in their first year of fellowship, with the consequence being that even prominent academic programs often can’t recruit enough REIs and often lose even their own graduates to Private Equity owned clinic chains.
Nobody should blame the fellows for their decisions; the real culprits behind the mess the field finds itself in is nobody else but the academic establishment which now has to face the logical consequences of its own, over decades, very obvious misdirection of the REI field: as in several other medical specialty areas – the establishment created this mess by initially on purpose restricting the number of fellowship programs in REI to not train too much “competition.” The three-year fellowship idea then really only further
aggravated the problem, bringing it to its current extremes.
Decrying the lack of quality research in the field and using this fact as motivation for a third year of fellowship, moreover, has little credibility because one, of course, must ask who – ultimately – has been over decades responsible for how sparse good and important research has been in the field? And the answer appears obvious: The culprit has, of course, over decades been no other than the academic establishment itself because it established, formulated, and executed the training of REI fellows. And – to be as transparent and factual as possible – it also abused fellowship programs for all of this time in pursuits of selfinterests rather than educational and scientific interests by often abusing fellows as a cheap workforce in pursuit of their own clinical practice goals rather than immersing them in academic pursuits, including serious research activities.
Instead, in the days of the two-year fellowships, a large majority of fellows pursued what can only be described as a six months period of “alibi research” and, now in the three-year program, they are instead “encouraged” to do 12 or even 18 months of such “alibi research,” while – in reality – of course, still often covering clinically for senior faculty in their clinical practice or – because of financial needs – moonlighting elsewhere.
The definition of “alibi-research,” also often called “pseudo-research” is, of course self-explanatory: It is simply poor-quality research, lacking all clinical and/or scientific significance. And we should not be surprised that this is what is going on in many – if not most – REI fellowships because fellows can be taught serious research only by teachers who, themselves, know – and pursue –serious research. And how many serious research laboratories and/or clinical research centers for REI exist these days in academic institutions in the U.S.? Obviously, not too many!
But to return to the main theme of this communication, the general staff shortages in the IVF field do not only involve reproductive endocrinologists (REs). The shortage also involves embryologists and specialized nurses. And one, therefore, has to ask what in vitro fertilization

(IVF) clinics can do in the face of such very obvious shortages? And looking at the problem practically – there is only one choice: you train your own staff. And while training embryologists and nurses has been common practice basically since the inception of IVF, training your own REs, is, of course, a very different story and has become a controversial issue, increasingly discussed in the medical literature.
A recent article in the Journal of Assisted Reproduction and Genetics (JARG) is a good example. In this Commentary article Gerard Letterie, DO, a REI from Pinnacle Fertility in Seattle, WA, addresses the issue of training residency-trained general OB/GYNs as physician extenders to REIs in the IVF field by – interestingly – likening it to the introduction of artificial intelligence (A.I.). 1 He is not the only one linking these two subjects, though from somewhat different viewpoints. Marcelle I. Cedars, MD, one of the REI field’s most accomplished academicians and strong proponent of a three-year fellowships, has done so recently as well in an Inkling article in Fertility and Sterility. 2 No fewer than 24 prominent authors from different academic institutions already in 2023 pointed out how difficult it has become to meet the demand for fertility services partially because of unfilled positions and suggested possible options, including the use of physician extenders to REIs. 3
Based on a recommendation by the Society for REI, their manuscript suggested the following and we are quoting:
The field should aggressively explore and implement courses of action to increase the number of qualified, highly trained REI physicians trained annually. We recommend efforts to increase the number of REI fellowships and the size complement of existing fellowships be prioritized where possible. These courses of action include: (a) Increase the number of REI fellowship training programs. (b) Increase the number of fellows trained at current REI fellowship programs. © The pros and cons of a 2-year focused clinical fellowship track for fellows interested primarily in ART practice were extensively explored. We do not recommend shortening the REI fellowship to
2 years at this time, because efforts should be focused on increasing the number of fellowship training slots (1a and b).
It is further recommended that the field aggressively implements courses of action to increase the number of and appropriate usage of non-REI providers to increase clinical efficiency under appropriate board-certified REI physician supervision.
Moreover, automating processes through technologic improvements can free providers at all levels to practice at the top of their license.
Except for the insistence on a threeyear fellowship, this summary based on recommendation by the Society for REI makes a lot of sense. It also allows (under supervision) for the training of general OB/GYNs as extenders of REIs in fertility clinics. We are also aware of clinics which have started using nurse practitioners and physician assistants in such positions. We, indeed, have been advised of clinics allowing them to perform egg retrievals and embryo transfers.
The CHR has experience in training general OB/ GYNs in infertility practice and we know from this experience that an average in the U.S. trained OB/ GYN can within one year easily become a clinically competent provider of fertility services, including of IVF (though, of course, excluding advanced surgical training). But advanced surgical infertility practice has evolved as its own subspecialty.
We, therefore, have become convinced that the current shortage in REIs can be rather quickly resolved by training general OB/GYNs within properly qualified one-year programs, fully recognizing that this will not include incentives or experience fostering research activities in these candidates. To reach that goal, a second year is required, not as a separate research year, but to allow for reduced clinical load during both years which allow routine integration of significant research into clinical practice throughout those two years.
Finally, there is one more group of candidates that deserves consideration in relieving the current

acute REI, embryology, and even nursing shortage in the country and that included formally trained staff in all three professions in selected foreign countries. REI is a medical specialty which in many countries is practiced very similarly to U.S. practice. Competent REIs from these countries should, therefore, literally within a few short months, be able to fully integrate into existing IVF programs, with many of such candidates, indeed, also offering much bigger hope for interest and future involvement in research and other academic activities. Individual states with such staff shortages should – obviously under strict criteria – be encouraged to offer quick licensing opportunities for qualified professionals.
Cedars feels that the currently unmet demand for staffing is, likely, a temporary phenomenon and can be expected to recede. 2 Considering the still much lower utilization of IVF in the U.S. than, for example, in Europe, we do not subscribe to this opinion. We, therefore, strongly believe that standard REI fellowships should be as soon as possible restricted to two years, with individuals—of course—given the opportunity for a third year if they (for example) wish to earn an additional degree in that year. In addition, oneyear fellowships should be approved in qualified IVF clinics, with qualification, of course, carefully tested upon completion of such a shortened fellowship.
A recent paper suggested that already in 2023, at least 25% of all approved formal U.S. REI fellowship programs were affiliated with private practice (basically Private Equity- owned) fertility clinics. 4 Why not go all the way and offer equal opportunity for staffing to all fertility enterprises, independent of ownership?
REFERENCES
1. Letterie G. J Assist Reprod 2024;41(120:3317-3321
2. Cedars MI. Fertil Steril. 2024; 122(2):228-229
3. Hariton et al., Fertil Steril 2023;120(4):755-766
4. Saleh et al., Fertil Steril Rep 2023; 4(4):332-336
*How
Because gynecologists and fertility specialists are currently usually only marginally involved, the gynecology literature (infertility literature included) has so-far largely ignored the controversies that have involved medical transgender care. This, of course, does not apply to the VOICE , which — especially over the last year since the Cass Review was published in the UK — has been covering the subject extensively. Several recent events and published articles now mandate further comments.
First and foremost, we must note that President Trump on January 28, 2025, issued an Executive Order under the somewhat unusual title, “ Protecting Children from Chemical and Surgical Mutilation. ” 1 Because this order has been widely referred to in the media, often with inappropriate or outright incorrect interpretations, we, here, offer some verbatim citations. But before we do this, we also want to point out that this Executive Order specifically referred only to children (under age 19 years of age). The Order does not apply to adults (over age 19).
REGARDING ITS PURPOSE: Across the country today, medical professionals are maiming and sterilizing a growing number of impressionable children under the radical and false claim that adults can change a child’s sex through a series of irreversible medical interventions. This dangerous trend will be a stain on our Nation’s history, and it must end.
Countless children soon regret that they have been mutilated and begin to grasp the horrifying tragedy that they will never be able to conceive children of their own or nurture their children through breastfeeding. Moreover, these vulnerable youths’ medical bills may rise throughout their lifetimes, as they are often trapped with lifelong medical complications, a losing war with their own bodies, and, tragically, sterilization.
Accordingly, it is the policy of the United States
that it will not fund, sponsor, promote, assist, or support the so-called “transition” of a child from one sex to another, and it will rigorously enforce all laws that prohibit or limit these destructive and life-altering procedures.
SELECTED DEFINITIONS: The phrase “chemical and surgical mutilation” means the use of puberty blockers, including GnRH agonists and other interventions, to delay the onset or progression of normally timed puberty in an individual who does not identify as his or her sex; the use of sex hormones, such as androgen blockers, estrogen, progesterone, or testosterone, to align an individual’s physical appearance with an identity that differs from his or her sex; and surgical procedures that attempt to transform an individual’s physical appearance to align with an identity that differs from his or her sex or that attempt to alter or remove an individual’s sexual organs to minimize or destroy their natural biological functions. This phrase sometimes is referred to as “gender affirming care.”
SELECTED INSTRUCTIONS: The blatant harm done to children by chemical and surgical mutilation cloaks itself in medical necessity, spurred by guidance from the World Professional Association for Transgender Health (WPATH), which lacks scientific integrity. [EDITORIAL COMMENT: In very similar circumstances as repeatedly before noted in the VOICE, the PGDIS (Preimplantation Genetic Diagnosis Society) is a highly biased professional group of individuals mostly making a living from preimplantation genetic testing for aneuploidy, or PGT-A. The membership of the WPATH is mostly made up of individuals making their living to a significant degree from gender-affirming care. Both of these societies – though claiming special expertise and entitlement to, therefore, establish guidelines for practice in their respective areas of practice – obviously have significant economic conflicts and potential biases in favor of performing treatments and, therefore, should be disqualified from establishing any guidelines for clinical practice.]
Agencies shall rescind or amend all policies that rely on WPATH guidance, including WPATH’s “Standards of Care Version 8”; and within 90
days of the date of this order, the Secretary of Health and Human Services (HHS) shall publish a review of the existing literature on best practices for promoting the health of children who assert gender dysphoria, rapid-onset gender dysphoria, or other identity-based confusion. The Secretary of HHS, as appropriate and consistent with applicable law, shall use all available methods to increase the quality of data to guide practices for improving the health of minors with gender dysphoria, rapidonset gender dysphoria, or other identity-based confusion, or who otherwise seek chemical or surgical mutilation.
The head of each executive department or agency (agency) that provides research or education grants to medical institutions, including medical schools and hospitals, shall, consistent with applicable law and in coordination with the Director of the Office of Management and Budget, immediately take appropriate steps to ensure that institutions receiving Federal research or education grants end the chemical and surgical mutilation of children.
Is there anybody who can argue with this executive order? We don’t believe so!
And now to the first related article, written by Abigail Shrier for The Free Press , which has probably in the U.S. been the most important media outfit to break the story about abusive transgender medical care in this country.

whose book, Irreversible Damage: The Transgender Craze Seducing Our Daughters is probably the most interesting exploration of the “mystery” of why during the last decade the diagnosis of “gender dysphoria” — before that almost exclusively only observed in boys and men – suddenly exploded into an epidemic among teenage girls. [Regnery Publishing; Publishing Date 6/29/2021]
U nder the title, “ How the Gender Fever Finally Broke ,” the article basically summarized itself in one sentence: “Loving, naive parents believed medical science was above politics and beyond question. Now, with the stroke of a pen, a destructive ideology has been eliminated.” 2
In its introduction, this excellent article noted two key occurrences in the truly bizarre history of medical care for gender transitions in children and juveniles: A first one involving almost incredulous numbers was the fact that the GoFundMe website in 2020 listed over 30,000 urgent appeals from young women seeking financial help to remove their perfectly healthy breasts. Over 30,000! The second occurrence is (from a medical standpoint) even more significant because it involved in the same year (December 2020) a Perspective article in the highly prestigious New England Journal of Medicine which – as Shrier noted – suggested that sex is actually “assigned” to newborns by doctors at birth (i.e., is not biologically predetermined).
Though, based on the routine inspection of sex organs after birth, that in principle is correct and, indeed, in extremely rare cases of mostly biological and chromosomal intersex conditions can be misleading, the three authors’ paper (the lead author a pulmonology fellow, a lawyer, and only the senior third author a prominent reproductive endocrinologist and close friend of the CHR), – we would hope without intent –basically proposed a new and quite revolutionary concept by arguing that, “sex designations on birth certificates offer no clinical utility, and can be harmful for intersex and transgender people. Moving such designations below the line of demarcation (in their opinion) wouldn’t compromise the birth certificate’s public health function but could avoid harm.” 3
And, as Shrier correctly noted, this statement broke news to gynecologists and other interested parties, including members of school communities, with schools outright starting to ask children in elementary school whether they might not like to identify as “genderqueer” or nonbinary.” 2
•Biological sex is based physical characteristics of genitalia at birth and other biological determinants.
•Gender is a sociological and legal construct, varies by culture, and is a Highly complex topic.
•Sexual differentiation occurs during fetal development and is driven by Genetic and hormonal factors.
•This process determines the development of (in principle only) female and male physical traits but can - due to hormonal and/or chromosomal result in a spectrum of outcomes (intersex).
•While XX and XY chromosomes are usually associated with, respectively, Female and male sex, sex-chromosome variations, such as XXY or XYY can occur in 1/1500-1/2000 live births, in those rare cases challenging the binary model of sex assignment as female or male.
•This means that the U.S. currently has ca. 200,00 – 330,000 so-affected individuals.
•Primary (genitalia and reproductive organs) and secondary sex characteristics (body hair and breast development) are shaped by genetics and hormones and can even within the same chromosomal sex vary widely. -----------------------------------------------------------------
And then there was Section 1557 of President Obama’ s Affordable Care Act, which very clearly included discrimination on the basis of “gender identity” as discrimination on the basis of “sex,” and immediately opened the purse as a huge source of funding for all treatments relating to gender transitions. And once a financing source has been identified for a new treatment, we in infertility, of course, know better than most other medical specialties how quickly a whole industry is created in collaborative efforts between pharma, hospitals, manufacturing, and, of course, practicing physicians to feed on this new financial

source. Once President Obama had written into law that individuals with issues regarding their gender identity had to be considered a “protected class,” this new industry was – for all practical purposes – already at work.
But things continued to get worse: As Shrier also noted in her article, WPATH, of course, very quickly issued practice guidelines, instantly used by all insurance companies as well as Medicaid and Medicare as “standard of care” [EDITORIAL COMMENT: Following exactly what the PGDIS ended up doing with equally catastrophic results for PGT-A] .
WPATH presented the guidelines as “evidencebased,” once again demonstrating that what for one highly conflicted professional society represents “best evidence” cannot be expected to correspond what an unbiased three-year study – like the Cass Review – would consider “best evidence” because one key conclusion of that document was, indeed, that there was insufficient “best evidence” for treating children and young adults with any of the treatments – whether chemical or surgical – the WPATH has found to represent evidence-based standard of care. And, as a lawsuit trying to overrule Alabama’s ban on gender transforming care for minors revealed, WPATH lacked any solid evidentiary basis for its guidelines and the society’s leadership knew this and suppressed publications of systematic reviews [EDITORIAL COMMENT: Following again exactly in the footsteps of the PGT-A scandal in reproductive medicine] .
What, however, made the situation much worse was the support of the Biden administration for these treatments. As Shrier noted, not only did Biden’s Justice Department sue states that enacted bans of such treatments for minors, but Assistant Secretary for Health Admiral Rachel L. Levine, MD, herself a well-known female transgender woman and, imagine that – a pediatrician!! – successfully pressured WPATH to drop the minimum age for medical as well as surgical treatments for minors in its 2020 published standard of care.

In the same year, the Department of Health and Human Services under her leadership published, indeed, a fact sheet that claimed that genderaffirming care for children and teens were crucial for their overall health and well-being.
The analogies to the mismanagement of the COVID-19 pandemic by the federal government are, of course, only too obvious and, of course, also only contribute to the mistrust in all government-provided health care information the public has had since the pandemic. Shrier points out that all the recent disclosures and especially President Trump’s new Executive Order regarding the subject hopefully finally have broken “the spell” that made parents (wrongly and often naively) believe that medical science was beyond politics.
She also pointed out that many bad actors, among those a pediatrician Assistant Secretary of Health, surgeons, medical endocrinologists (who to the luck of reproductive endocrinologists took the lead in this matter), psychiatric therapists, social workers and, of course, too many teachers, and even clergy took advantage of circumstances and joined the earnings bandwagon.
Finally, Shrier described in the article what has been happening with transgender care of minors as a “spell” over parents who allowed their children to transition at such young ages which, now, with publication of Trump’s Executive Order appears to have been finally broken, as the similarities in the incompetence of the federal government in managing this health problem in comparison to the management of the COVID-19

pandemic have come into increasing focus. She, indeed, sees those parents as naïve in having assumed that medical science was above politics and beyond questioning. The disgusting and factually incorrect threat from counselors they apparently almost always fell for (suicide, indeed, have been actually surprisingly rare) was, “Would you rather have a live son or a dead daughter?” The President’s new Executive Order does not necessarily prevent continued treatments of children that are privately paid for; but one can assume that those – at worst – will be rare because hospitals and universities will be hesitant to face the legal and potential financial consequences from the government for ignoring the Executive Order.
This makes the intervention by New York’s Attorney General Letitia James that more significant; on February 3, 2025, she advised New York hospitals to ignore the government's Executive Order since it contradicted state law. 5 At the point of this writing, what New York’s hospitals have decided to do – or not to do –going forward regarding the issue is unclear. Never a dull moment here in New York politics!
1. The White House. Executive Order. January 28, 2025. https://www.whitehouse.gov/presidential-actions/2025/01/ protecting-children-from-chemical-and-surgical-mutilatio n/
2. Shier A. The Free Press. January 30, 2025, https://www.thefp.com/p/abigail-shrier-how-the-genderfever-broke-trump-executive-order
3. Shteylyer et al., N Enl J Med 2020;183:2399-2401
4. ASRM. Press Release. February 5, 2025. https://www.asrm.org/news-and-events/asrm-news/pressreleasesbulletins/asrm-releases-fact-sheet-on-biological-se x-differentiation/
5. Lewis RC. City&State. February 3, 2025. https://www.cityandstateny.com/politics/2025/02/state-agsays-ny-hospitals-must-continue-offering-gender-affirming -care-minors/402711/
*What the Fauci pardon must mean
So, as one of his last acts in office, President Biden (or whoever made presidential decisions in the White House) decided that Anthony Fauci, MD, former director of the U.S. National Institute of Allergy and Infectious Diseases (NIAID) deserved – and needed – a presidential pardon.
Why would that be?
He, of course, lied to the American people over and over again; but for that you don’t need a pardon. Politicians lie to their constituents all the time, and nobody has ever gone to jail for that. To need a pardon must mean something much more serious, and in most cases (sic. the president’s son, Hunter, and his other family members) it involves bribes or other financial criminal acts like not paying taxes. And even though Fauci was at the end of his career the highest paid federal employee in the country (yes, his salary was higher than the President’s), one, therefore, must consider the possibility that he, among all of his other transgressions, possibly also dipped on occasions into the cash flow of some transactions. After all, so many politicians do that because, how otherwise do they all become millionaires within years in office, even considering their rather meager salaries

But our biggest suspicion is really a different kind of financial exposure, namely damages! It seems extremely unlikely that Fauci would have ever been indicted for lying to Congress (which he likely did). It also appears unlikely that he would have been indicted for clandestinely and against the law having financed the SARS-CoV-2 research in a China laboratory that, likely, resulted in the worldwide COVID-19 pandemic. But if he, indeed, did that, everybody who got sick from COVID or had a loved one dying – at least theoretically –could sue him for damages. This, in our opinion, is the most likely reason for the Presidential pardon. But such a pardon also has its disadvantages. The biggest is the fact that a pardon disqualifies a defendant from taking the Fifth in court. In other words, there is a good chance that we will see Fauci in a Congressional hearing – naked without the protection of not answering questions for fear
of self-incrimination. That could be interesting theater!
One thing is sure, funding from the NIH will change, whether such changes are temporarily stopped by federal judges or not. Ultimately, at least two major changes can be expected with very high probability: (i) The NIH will significantly cut so-called overhead costs to institutions, which are payments hospitals, universities and other entities receive to cover their indirect overhead costs if the research a grant supports is conducted at an institutional location. 1
Why can we be so sure? Because on February 7, 2025, the NIH announced its intention to do so for most universities and research centers. And all overhead will be included in those cuts, facility costs, equipment use, utilities, and maintenance. Most smaller institutions receive a ca. 30% indirect cost rates, which means 30% of the total grant payment for a project is assessed in the payout of the NIH grant, but does not go to the investigator but his university or other “landlord.” 30% overhead is, however, nothing in comparison to what leading academic institutions charge and currently receive in overhead costs. In places like Harvard or Rockefeller University indirect costs can exceed 80% of the grant amount. On some occasions institutions have even charged in excess of 100%.
According to the Healio article, the NIH spent over $35 billion (with “b”) in fiscal years on almost 50,000 grants, of which 26 billion involved direct costs, but $9 billion went to institutions for indirect costs. Rumor has it that indirect costs will in principle be capped at 15%, which could yield over $4 billion in savings for the NIH.
But whether institutions will agree with those cuts is questionable; who knows? Everybody knows that many of the most prominent schools (with the biggest – tax-exempt –endowments) would, likely, have a hard time maintaining their research facilities and research faculties with only 15% overhead costs. But what are their billion dollars
endowments for?
The University of Pennsylvania offered a statement to Healio , suggesting that its NIH funding would annually decline by $250 million, profoundly adversely affecting its research enterprise. And, interestingly, Sean Tipton, MD , chief advocacy and Policy officer of the ASRM, called on the American public to contact President Trump and Congress to demand that this announced “misguided” policy be reversed. As if NIH (as noted above) really supports much infertility research!
And, quite unprecedented for a medical journal, “an anonymous voice within the U.S. federal research system” – whatever that may mean –offered in the BMJ her/his feelings of “anger, despair, and defiance,” about the changes taking place in the U.S. federal research system. 2 And the person did not hold back, claiming for example that, “digital genocide will undo decades of progress toward informed and appropriate care and (of course disproportionally affect) those that are female, non-white, poor, and living in Republican states.”
That many individuals may hold such extreme opinions is, of course, these days no surprise and, indeed, expected. And they, of course, are entitled to them and should be protected in being allowed to express them. But like the use of “anonymous sources” in journalism, the use of information and/or opinion from such anonymous sources should be minimal and carefully considered. After all, how do we know what the qualifications are of this anonymous individual in expressing her/his opinion? Moreover, it is easy to make accusations when one does not have to consider possible consequences.
That an esteemed medical journal, like the BMJ , was willing to publish this article – in its anonymity likely unprecedented – is, however, astonishing and yet another demonstration of the wokeness that has taken over editorial offices in the medical publishing world, but with special fierceness in the U.K. As repeatedly noted before in the VOICE, The Lancet is, of course, the prime example, though – as the next subsection will demonstrate – the U.S. and some of the country’s leading medical journals don’t lag very far behind.

1. HEALIO. February 11, 2025. https://www.healio.com/news/hematologyoncology/20250211/discussion-about-nih-research-fundingcuts-requires data-time-and-careful-evaluation 2. Anonymous. BMJ 2025;388:r294
That medical journals have not yet caught up to the general anti-wokeness sentiment that has been gaining popularity in the country, was recently again quite apparent in several articles –mostly of course personal opinions – published in some of the leading medical and science journals. Here are some examples: Unsurprisingly, The New England Journal of Medicine excelled in this regard as well: It started with a group of U.S. authors in a Perspective article arguing that “the deluge of legislative and policy attacks on diversity, equity, and inclusion efforts threatens the integrity of the health care workforce and will ultimately worsen the health of the populace.” 1
Making a very similar point, two Stanford University faculty members in another Perspective article in the same medical journal lamented that “a study of a health equity curriculum was stopped in its tracks by the ban on diversity, equity, and inclusion efforts in federal agencies, with the study’s leaders seeing the sudden halt as a call to action.” 2 And since in medicine we believe that everything happens in threes, a third Perspective article in the same journal issue claimed that the voice of the CDC was “silenced” because one issue of the MMWR went unpublished in time. 3 To quote, “for more than 60 years, the MMWR has published lifesaving information on U.S. public health crises. The Trump administration’s pause on health communications has disrupted that essential mission.”
Seriously?! The rhetorical exaggeration in all of these declarations is, of course, only too obvious and not only counteracts all potential credibility for expressed concerns but also discourages any engagement with the arguments made. But
that also did not appear to be the intent of the editors of The Journal because – as has been customary for too long – they, despite three basically unanimous opinion papers on the subject declaring the end of the world as we knew it, did not find it necessary to also invite in balance a less emotional and more fact-based opinion on the subject.
The editors of The Journal quite obviously felt that even a 3-to-1-ratio would have been unacceptably unfair for the woke crowd which, of course, is always intolerant to any alternative opinion. A maybe better way to say the same thing is that woke arguments, in principle, can never stand up to really good and unbiased arguments!
How woke medical journal editors have become these days was also well demonstrated by an Opinion article the still relatively new editor-inchief of the BMJ co-authored, in which the two authors expressed the opinion that, “medical journal editors must resist a recent CDC order and anti-gender etiology.” 4 What the article referred to was an, indeed, rather ridiculous order by a temporary CDC leadership apparatchik that instructed CDC employees to retract and/or withdraw papers that – based on Executive Orders from the Trump White House that declared that there exist only two sexes, female and male – and that gender-transition treatments for children and young adults till age 19, were inappropriate.
Since when is it a medical journal’s editor’s job to be political?
And to demonstrate how political the BMJ , indeed, has become under its new editor-inchief, it published a paper by four U.S. writers from Baltimore (who probably couldn’t place their Opinion piece in a U.S. journal) in which they make the claim that “the elimination of protections against immigration action in health care facilities risks patient care, public health, and moral injury to providers.” 5 This is likely the same crowd that argued that the Israeli army going after murderous Hamas terrorists in permissive hospitals endangered their function as hospitals.

1. Guerra P, et al., N Engl J Med 2025. DOI: 10.1056/ NEJMp2500489; Online ahead of print.
2. Wang SXY, Chi K, N Engl J med 2025; DOI: 10.1056/ NEJMp501471. Online ahead of print.
3. Rasmussen et al., N Engl J Med 2025; DOI: 10. 1056/ NEJM2501622. Online ahead of print.
4. Clark J, Abbasi K. BMJ 2025;388:r253
5. Page KR, et al., BMJ 2025;388:r304
According to an Elon Musk tweet on X 1 last year $9 billion of a total of 35 billion the NIH paid out for research support was used for administrative overhead that went to institutions, with the ones receiving the most usually having tens of billions in endowments. Here are three examples:
•Harvard University received an indirect cost percentage of 69% and has an endowment of $53.2 billion.
•Yale University had an overhead rate of 67.5% and has an endowment of $41.4 billion.
•Johns Hopkins University had an overhead rate of 63.7%, and has an endowment of $13.1 billion.
Under the new rules, those rates – as noted above – will be reduced to 15%. Considering that all of these universities are not-for-profit enterprises and, therefore, pay no taxes, even that rate seems exaggerated.
Further pressure will come upon universities from the NIH, based on the announcement by Jay Bhattaacharyam MD, PhD, the new Director of the NIH, that the awarding of grants from the NIH will take into consideration the commitment to “free speech” at a university. Considering that Harvard in recent years always has come dead-last in surveys, this could mean significant losses for this university that will go beyond just the lower overhead percentage of 15%.
NIH
– Last year the NIH announced a new initiative under which investigators would be financially incentivized to repeat important
published studies to double check important reported biological results. And lo and behold, there so-far is little interest out there to do this work. Few investigators, indeed, appear interested in having their work repeated. New NIH director, Bhattacharya, as noted in a News article in Science magazine recently re-emphasized that such replication studies “should be at the center of what the NIH does.” And considering how much fake science these days appears in print, we could not agree more with this statement.
1. Musk A. on X. https://x.com/elonmusk/ status/18880221899848584767s=43&t=P_ bVvfV3w57FT4uz9jK43Q
2. Kaiser J. Science 2025;387(6730):126
In one of the organization’s usual emails, Inside Reproductive Health published an interesting update on the tumult that has been occupying what once was considered one of the most successful IVF clinic chains, Kindbody. After at its peak reaching a market valuation of over $1 billion (yes, you are reading correctly!), the company’s value today is only a fraction of that.
It has been some time since we reported on this company after the executive suit underwent a significant shake up. But shakeups have continued ever since. After initially having no problems raising funds and indeed receiving over $300 in funding since its founding, the company during 2024 failed in an attempt to raise an additional $50 million. After this happened, the Internet was overrun by reports that the company was looking for a buyer; but nobody was willing to come to the rescue, because, as Inside Reproductive Health now reports, the company is “quietly” trying to raise another $75 million, after prior raises for smaller sums apparently failed.
All of this is, of course, not a good sign but does not come as a surprise. Kindbody recently shut down six of its clinic sites in Los Angeles, Columbus, Ohio, Miami, Philadelphia, Portland, Oregon, and Southfield, Michigan. In addition, the company has failed in recruiting a new CEO,

after the last one resigned after a short stint (Gina Bartasi was the founder and initial CEO of the company), and the enterprise is currently comanaged by three senior executives.
The question behind the upheaval at Kindbody is, however, even bigger than it may appear: Is the poor financial performance which has been so obvious at this clinic chain, also happening at other clinic chains? In other words, are all IVF clinic chains greatly overvalued? We would not be surprised if the answer was yes!
1. Shinkman R. Inside Reproductive Health. February 20. 2025. https://www.fertilitybridge.com/news-ar ticles kindbody-clinic-closures-ceo-shuffle-75m-funding
THE PRAGMATIC CLINICAL TRIAL – As a recent Viewpoint article in JAMA recently pointed out, 1 so-called pragmatic clinical trials (PCTs) have become common. They can be defined as having the primary purpose of identifying clinical decision-makers about the comparative balance of benefits, burdens, and risks of a biomedical or behavioral health intervention at an individual or population level. They usually are integrated into routine health care delivery, thereby testing an intervention in the “real” world.
In proposing more use of PCTs in clinical medicine, the authors astutely pointed out that they could become even more useful to delivery systems in assessing policies and procedures through relatively minor accommodations of priorities, introduction of more flexibility in the level of evidence a given trial requires, shortening their duration of planning and implementation, etc. their concluding paragraph is deserving of a direct citation: “Populations in need of health care and the illness and issues that affect them are complex and evolving, as are health care systems. PCTs to guide care must account for this complexity and enable pivoting and learning.”
USING DATA AND STATISTICAL ANALYSIS IN THE FACE OF UNCERTAINTY – A recent book review in Nature magazine attracted our attention because of its subtitle, “A statistician offers a masterful
guide to embracing the unknown.” 2 And we were not disappointed.
As the author of the review well explained, the book (Spigelhalter, David. The Art of Uncertainty: How to Navigate Chance, Ignorance, Risk, and Luck. 2024, Pelican) had nothing to do with medicine or science in general, but used forecasting of the 2024 U.S. presidential election as a principle example to demonstrate how data can be used and how statistical analyses can be performed on these data to make informed decision in the face of uncertainty. And isn’t this exactly what we in medicine are asked to do on a daily basis?
A few points deserve special mention: Uncertainty is a personal phenomenon; it is determined by our own specific interplay between chance, ignorance, risk, and luck. Uncertainty is, therefore, not a characteristic of an event, but reflects our own knowledge, perspective, and assumptions we may make to better understand and event and/or predict it.
1. Platt et al. JAMA 2024;332(22:1875-1876
2. Min Y. Nature 2025;637:785
An Editorial in Fertility and Sterility , informed on an interesting and potentially important step several OB/GYN journals and their editors have taken by forming the OBGYN Editors’ Integrity Group (OGEIG) with the purpose in a collaborative effort to improve trustworthiness in published papers (obviously a desirable goal!). 1 The editors already published collaboratively unified criteria for publication of randomized controlled trials.
Such criteria, however, of course already exist and the criteria they published don’t differ to any significant degrees from what most medical journals nowadays are requesting. What we, especially in the infertility field, have been missing in the peer review process is more emphasis on defining patient populations in such trials and –even more importantly – how these data are to be interpreted, i.e., a proper interpretation by the author to which patients their study results are

REFERENCE
1. Editorial. Fertil Steril 2025;122(6):965-968
Hypothyroidism
Hypothyroidism is diagnosed when thyroid hormone is abnormally low or completely absent. The diagnosis can have several causes, including the absence of thyroid hormone after a thyroidectomy. In most cases the condition is, however, caused by an autoimmune response against thyroid epitopes. If thyroid autoantibodies are present to thyroglobulin (TG Abs) and thyroid peroxidase (TPO Abs), the condition is called Hashimoto’s thyroiditis, the most common autoimmune disease in women during reproductive years and, therefore, highly important for the infertility field.
For everybody interested in this condition, we strongly recommend a recent review article in the Lancet , 1 which already in its abstract clearly points out that pregnancy – aside of sex and age – requires individualized consideration of testing results and – if there is an important point to be made, then this is it! This is the best review article we have seen on this subject in quite some time.
REFERENCE
1. Taylor et al., Lancet 2025;404:1347-1364
That stress can affect ovarian function has been known for quite some time. Who, for example, is not aware that travel can affect a woman’s menstrual cycle (though that may or may not have a relationship with stress and may be more related to a woman’s circadian rhythm). Chinese investigators in a Review article now tried to make more sense of this association, 1 which, by most fertility specialists, will probably be accepted as fact, even though degrees of stress
are, of course, difficult to quantitate in humans. Moreover, if stress does adversely affect fertility, because history has told us that children have been born in the most severe famines and even in concentration camps during WWII, the penetrance of stress on fertility success must be quite limited.
Against this background, the Chinese investigators offer an interesting paper, out of all places, in the International Journal of Molecular Medicine on what is known on the subject and even suggests potential psychological interventions and nutritional strategies to improve ovarian function. Though at times maybe a bit speculative, overall, an interesting read, though one must avoid the promotion of premature associations and causations. For example, does chronic stress really lead to POI or is the stress the consequence of POI, which may have other causes. How does one study these different explanations?
1. Hu et al., Int J Molec Med 2025;55:34
________________________________________
CONFLICT STATEMENT: The CHR and several staff members are co-owners of several U.S. patents claiming fertility benefits for hypo-androgenic infertile women from supplementation with testosterone (and other androgens) and receive payment from licensing these patents. ________________________________________
A recent paper in Science magazine – somewhat surprisingly – linked in a bird species testosteronemediated adaptation in reproductive traits to a single gene with a somewhat unexpected expression in brain, gonads and — yes — blood! This is a second paper within weeks (see also the lead article in this issue of the VOICE which in detail reports the recent discovery that myostatin from skeletal muscles controls FSH secretion from the pituitary) which offers truly revolutionary new insights into hormonal actions. This paper by Loveland et al, 1 completely revises what has been known about how hormone levels are controlled

and how hormone-mediated traits evolve.
The bird model used in the study demonstrates a very significant degree of variation among males when it comes to sexually selected behavioral and physical traits. Testosterone has been suggested to drive these differences. Testosterone is, however, not a gene product. Therefore, there exists no gene that drives this differentiation, raising the question how, then, does testosterone do this?
In general sex steroids derived from gonads are believed to be the source for many different traits, especially behavioral traits believed to be derived from neural sensitivity to these steroids especially by the brain. The original suspicion was that the different phenotypes may be the consequence of expressions of genes that encode sex steroid receptors for androgens and estrogens or enzymes controlling testosterone production. But that did not turn out to be the case.
What really was responsible was the sequence and expression of the 17-beta hydroxysteroid dehydrogenase 2 ( HSD17B2 ). This is a gene that encodes an enzyme with the ability to inactivate testosterone. Derived forms of the enzyme turned out to convert testosterone to inactivity at least twice as fast as the original enzyme. Moreover, the study demonstrated high levels of derived HSD17B1 gene expression in six behaviorally important areas of the brain, suggesting, as an accompanying Perspective article in Science suggested, that inactivation of testosterone explained the distinctively less “aggressive” behavior of some male variants. 2
We loved this perspective article because it pointed out a realization about biology that appears increasingly generalizable: Our understanding of biology has over the last few decades gone only from extremely superficial to, at best, less-superficial: Just as the author of this Commentary noted that the here discussed study may be pointing to an emerging “rule of life” for hormone-mediated trends in general – or be even more generalizable to all complex traits – in evolution “every problem has many possible solutions, as endocrine systems can be modified in almost endless ways to generate behavioral
diversity.”
We have called this principle at the CHR the “redundancy of biological processes” and equated it to the need for multiple layers of redundancies of any rocket we have sent to the moon or are planning to send to Mars. Or, maybe, even more telling, all of humanity would not exist had evolution – as it progressed – not built in redundancies for almost all of our biological processes, as demonstrated here for reproductive and behavioral controls by androgens. In other words, we have just started to peel the onion!
1. Loveland et al., Science 20025387(67320:406-412
2. Rosvall Ka. Science 2025;387(6732)”358-359
We all, of course, are very familiar with prolactin secreting tumors of the pituitary; but have you heard about co-secreting adenomas, producing human growth hormone (GH) as well as prolactin (PL)?
In a recent study published in the JCEM , Spanish investigators reported on 604 cases. Since it has been for some time hypothesized that these adenomas may demonstrate subtypes with different presentations and/or prognosis, they now attempted – having access to so many patients – to establish a fitting classification. 1
The study included 474 individuals with pure GH excess and 130 with GH/PL adenomas. As it turned out the latter group was diagnosed at earlier ages and demonstrated lower IGF-1 levels. They also demonstrated a higher incidence of presurgical hypopituitarism, and the tumors were more frequently macroadenomas and more invasive at diagnosis. Therefore unsurprisingly, permanent arginine-vasopressin deficiency was also more frequent, though surgical cure rates turned out to be the same.
What the paper, however, failed to do (though we had hoped it would) is to establish a hard definition of these co-producing adenomas. But we now at least know that they exist!
REFERENCE
1. Wildemberg LR, Gadelha MR. J C. JCEM. 2025;110(1):e192-e193
And here we, of course, have another endocrine condition with significant relevance for reproductive medicine and, once more, it is the JCEM that brings us relevant information in a special supplement guest edited by Richard J Auchus, MD, PhD , one of the journal’s Associate Editors from the University of Michigan.
Eight articles offer an excellent overview over this condition which is caused by an inherited inability to synthesize cortisol due to a 21-hydroxylase deficiency in somewhere between 905 and 95% of all cases, caused by mutation in the CYP21A2 gene. The classical (in contrast to the nonclassical) form occurs only in approximately 1/16 000 births, while the non-classical form occurs in approximately 1/200 newborns. We usually are not big fans of supplements, especially if funded by the pharma industry (as this supplement is by Neurocrine Biosciences, Inc.), but here we are ready to make an exception because the eight articles do offer a comprehensive state-of-the-arts update on a widely misunderstood condition. 1
REFERENCE
1. JCEM Supplement Auchus R. Guest Editor. February 2025. Supplement 1.S1-S87
Whether anti-Müllerian hormone (AMH) levels in polycystic ovary syndrome (PCOS) patients matter during IVF has, to the best of our knowledge, never before been seriously investigated. This is, however, exactly what a Chinese paper recently did in Reproductive Biology and Endocrinology. 1
Though a retrospective study with the usual limitations of this study format, the study involved 4,719 alleged PCOS patients between the ages of 20 and 40. Unfortunately, the paper does not tell us criteria for the diagnosis of PCOS which is, of course, a significant shortcoming. Moreover, the paper also does not tell us which phenotypes of PCOS (and in which distribution) were included, both, of course, being very important details one would like to know.
Nevertheless, the data are interesting because the investigators, based on 25th and 75th percentile, divided the study population into three groups: Low, - <4.98ng/mL, n=1,198; medium, - 4.9810.65ng/mL, n=2,346; and high, - >10.65ng/ mL, n=1,175. Outcomes were live births, clinical pregnancies, cumulative pregnancy rates, and miscarriage rates.
Live birth rates for fresh embryos were 39.8%, 35.9%, and 30.4% for low, medium, and high AMH groups (P=0.017). Miscarriage rates were 11.3%, 17.1%, and 21.8% (P=0.018) but clinical and cumulative pregnancy rates did not differ statistically. The difference remained after adjustments significant for live birth rate difference between high and low AMH groups, and differences in miscarriage rates between low and medium as well as high AMH groups. In other words, high AMH is in PCOS patients associated



with lower live birth rates and higher miscarriage rates.
Here is why we found this article of special interest: Almost a decade ago in 2016, the CHR’s team of investigators published a paper in the Journal of Translational Medicine reporting a similar effect of AMH in infertile patients, defined by FSH and AMH as either good, intermediate, or poor prognosis patients. The effect was U-shaped—and we are talking here about infertile women but not necessarily PCOS patients— in that higher AMH at youngest ages was beneficial (i.e., higher AMH was associated with better live birth rates); but with advancing age, up to a point still being associated with better pregnancy rates, increasing miscarriage rates, however, led to declining live birth rates.
As in this new paper, the conclusion of the CHR’s investigators at the time was that too high AMH levels, in some still unknown ways, depressed live birth rates mostly by increasing miscarriage rates. 2 And this is exactly what this Chinese study also suggests. The question still to be answered, therefore, is how does very high AMH cause miscarriages?
REFERENCES
1. Zhao et al., Reprod Biol Endocrinol 2025;23:15
2. Gleicher et al., J Transl Med 2016;14:172
An interesting study by California investigators of a
national data set involving 14,312,619 deliveries offered within the last year a second very credible data set on GC cycle outcomes, demonstrating that this patient population— somewhat surprisingly considering how carefully GCs supposedly are selected—face quite significant pregnancy outcome complications. 1 That former study was a systematic review and meta-analysis. 2 This paper demonstrated that GC pregnancies between 2017 and 2020 increased by 55%, and there is good reason to believe that this increase, especially after COVID, has further accelerated.
GC pregnancies in this paper were more frequently multiple gestation pregnancies (14.7% vs 1.8%, P<0.001), demonstrated more placental abruptions (3.5% vs. 1.1%), and low lying placenta (1.6% vs. 0.2%). Among singleton pregnancies, late preterm pregnancies were more frequent (10.8% vs. 6.4%), as were peri viable deliveries (1.1% vs. 0.4%), and postpartum hemorrhages (12.2% vs. 4.1%). Interestingly, the chance of a Cesarean section was, however, higher in non-GC pregnancies (23.6% vs 31.6%) and all of the above noted other associations were less robust in multiple (mostly twin) pregnancies.
Both of these latter findings are, of course, very interesting findings in themselves, in that they reemphasize the highly exaggerated national Cesarean section rate and the still widely held incorrect belief that twin pregnancies carry with
them clinically significantly increased maternal and neonatal complications. Both of these subjects have been on several occasions discussed in the pages of the VOICE before and we, therefore, do not want to rehash them here.
What then are the conclusions from this and the previously noted prior data set? (i) GC pregnancies must be viewed as higher risk pregnancies and, therefore, must receive the appropriate attention; and (ii) maybe it is time to clamp down on the GC selection process. The impression at the CHR— especially since the COVID pandemic—has been that GC candidates passed by many GC agencies have declined in quality.
1. Masjedi et al., J Assist Reprod Genet 2025;42:201-211
2. Matsuzaki et al., JAMA Network open 2024;7(7):e2422634
The IVF field does not lack controversial treatments, but only very few have generated as much contradictory outcome data as Endometrial Scratching (ES) and whenever that is the case the principal explanation one comes to in analyzing these discrepancies almost always ends up being either differences in patient populations studied and/or differences in how a treatment was applied. Unfortunately, the peer review process still allows publications of papers that do not point out these two obviously essential
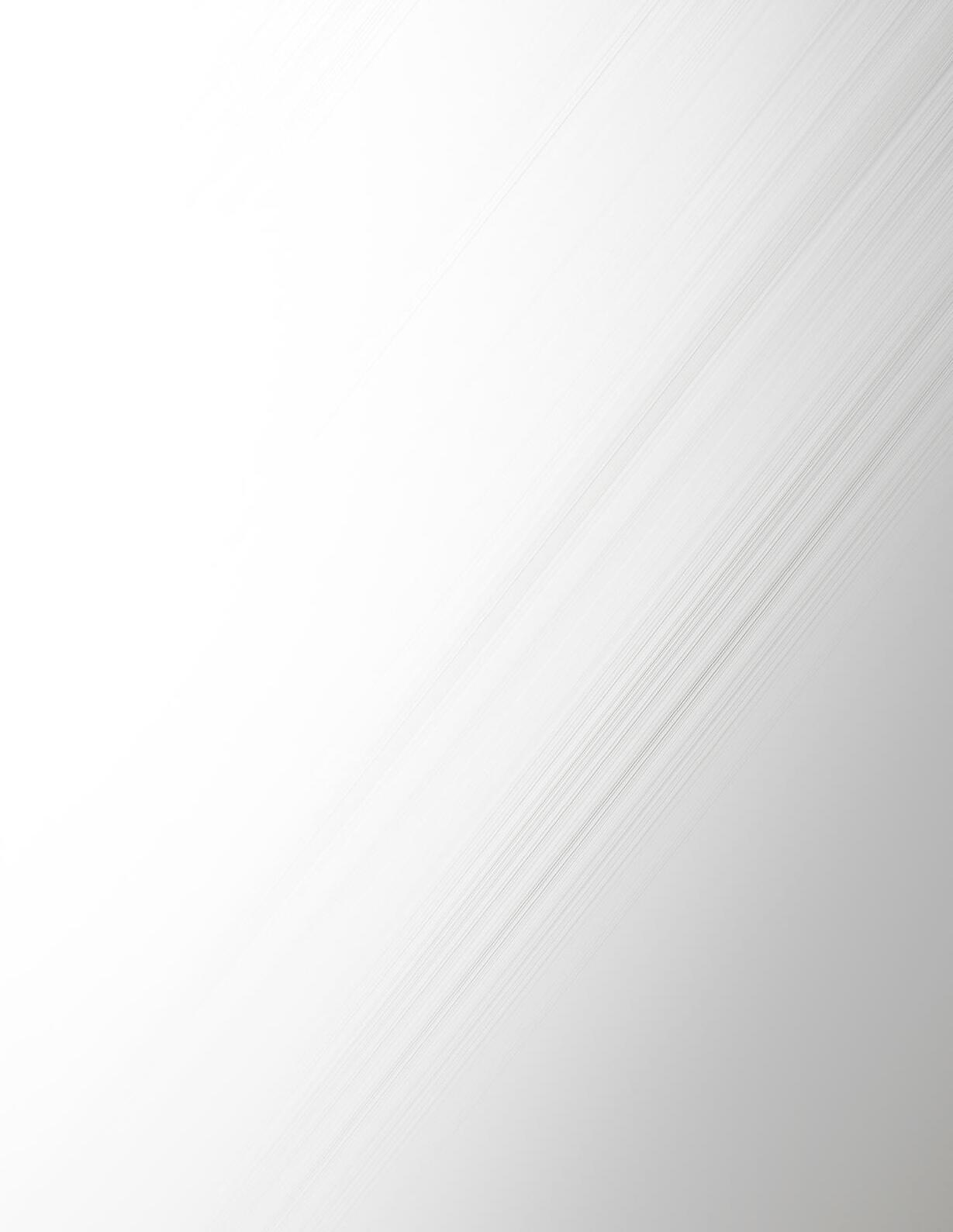
A good (or should we say “terrible”) example was a recent paper by U.S. and Brazilian investigators in the JARG 1 which really demonstrated almost everything that is wrong with the peer review process in infertility and, therefore, is directly responsible for much of the confusion about so many clinical treatments in the field.
The study is a retrospective case control study—in itself, of course, a source of bias because there must have been reasons why some patients received ES and others did not. The best evidence for that is, indeed, the reported finding in the study that women undergoing scratching had (as an unexpected finding) more endometritis. One, therefore, for example could argue that, had they not been chosen preferentially for ES, the procedure might have shown an outcome advantage over nonscratching.
Yet in this paper the authors concluded that endometrial scratching before frozen euploid embryo transfer did not influence pregnancy outcomes but increased the chance of second trimester pregnancy loss. One, of course, also could argue that these results may suggest that chronic endometritis may increase miscarriages. But such presumed associations and conclusions are all, of course, invalid because the investigators did not even attempt to adjust their very marginal statistical findings accordingly.
We are discussing this paper—a very deserving recipient of a WORST PAPER AWARD —in this issue of the VOICE to make once more the often-beforemade point that publishing these kinds of papers, even if they are by prominent authors, does not help in resolving controversial issues. Very much to the contrary: such papers only further feed the controversy and prevent patients from getting the right treatments.
1. Lindekugel et al., J Assist Reprod Genet 2025. doi: 10.1007/s10815024-03360-x. Online ahead of print. [Recipient of WORST PAPER AWARD ]
Since the earliest papers appeared in the infertility literature suggesting that frozen embryo transfers in delayed cycles improve IVF outcomes over fresh embryo cycles, 1 the CHR has considered this especially in recent years rapidly gaining trend to represent just another major misdirection of IVF practice. And, as so many times before on other subjects, the CHR was proven correct. 2
Now, Chinese investigators – as based on cycle numbers in China only they can – offered one of their multicenter prospectively randomized studies, this time as a “pragmatic” trial (we elsewhere in this issue of the VOICE discuss what that means) – randomizing on day of egg retrieval patients 1:1 to undergo either delayed frozen embryo transfer or fresh transfer in
the retrieval cycle. 3 For some reason the study also claims that the study was performed in poor prognosis patients, but the patient selection criteria say otherwise because entry into the study was allowed for up to 9 retrieved oocytes (we at the CHR would love to have such poor prognosis patients!!).
Primary outcome for the study was live birth (over 28 weeks), with secondary outcomes being clinical pregnancies, singleton and twin pregnancies, pregnancy loss, ectopic pregnancies, maternal and/or neonatal complications, and –importantly – cumulative live birth rates within one year from randomization.
In an intention to treat analysis of 838 women (419 frozen and fresh, respectively) with median ages of 34 and 33 years and tubal factor in 55.9% and 56.6% (again obviously not poor prognosis patients), live births were lower in the frozen transfer group (32% vs. 40%; P<0.009), as were clinical pregnancies (39% vs. 47%) and cumulative live birth rates (44% vs. 51%). None of the other secondary outcomes demonstrated any difference.
The authors concluded that fresh transfer “may be a better choice” in poor prognosis patients than a freeze-all strategy with delayed frozenthawed transfer but we have to disagree: This study actually confirmed once again that in a general average risk population (as one would expect in a pragmatic trial), an all-freeze

embryo strategy harms the patients’ live birth chances. In real poor prognosis patients, this harm will, of course, be even bigger. It is time to stop this nonsense! Readers interested in this subject may also enjoy the Editorial that accompanies the article in the BMJ , 4 even though its very prominent authors also overlooked the fact that this study really did not report on poor prognosis patients.
REFERENCES
1. Shapiro et al., Fertil Steril 2021;96:516-518
2. Zaat et al., Cochrane Database Syst Rev 2021;2:CD011184
3. Wei et al., BMJ 2025;388:e081474
4. Cornelisse S, Mastenboek S. BMJ 2025;388:r49
All
you want to know about triggering follicles—except for timing
CHR friend and colleague from Israel, Raoul Orvieto, MD , one of the most prolific authors in the fertility field with many areas of research interest, is probably best known for his work on different ovarian stimulation protocols and as the “father” of the double-trigger with chorionic gonadotropin (hCG) and GnRH agonist (GnRHa). That he recently published a review on follicle triggering in IVF cycles 1 is, therefore, noteworthy.
He offers a detailed review of various trigger options and explains which of them should be used in which patient populations. His work on women with low functional reserve, indeed, induced the CHR to
switch several years ago in this patient population from single hCG to double trigger (of course, after first verifying and confirming his results).
The article does not address the timing of ovulation triggers which at the CHR over the last decade has become a central theme of research as well as clinical practice in what the Center has come to call Highly Individualized Egg Retrieval (HIER). 2 In principle this means earlier and earlier triggering as women age, which – because of the very advanced ages of most CHR patients – now means that many, if not most, patients at the Center are now triggered at lead follicle sizes of 12mm or even smaller. As repeatedly noted in these pages, this experience has led us to believe that in many ways the timing of HIER is likely even more important than the selection of trigger method.
REFERENCES
1. Orvieto R. Reprod Biol Endocrinol 2025;23:12
2. Gleicher N. J IVF Worldwide 2023;1(1): https://jivfwwscholasticahq. com/article/85177
By Lyka Mochizuki, MSc, who until 2024 was a research associate at the Center for Human Reproduction (CHR) in New York City and now is a Visiting Scientist. She introduced conflict resolution to controversial issues in the reproductive medicine literature, starting with preimplantation genetic testing for aneuploidy (JARG 2020;37;677-687), and
can be contacted through the editorial office of The VOICE
BRIEFING: A recent, quite excellent review article on “add-ons” to IVF in the medical journal Human Reproduction was the impetus for Lyka Mochizuki, MSc., a former research associate and current Visiting Scientist at the Center for Human Reproduction in New York City, to go somewhat beyond the scope of our usual literature review of a single paper and offer a Scoping Review of the subject with what we believe are some important new insights. We believe you will agree and, therefore, are featuring her comments here as an independent article.
__________________________
In vitro fertilization (IVF) has been a groundbreaking advancement in reproductive medicine, offering hope to individuals and couples facing infertility. However, the emergence of IVF “addons” — optional treatments and procedures marketed as enhancements to success rates 1 — has sparked significant debate within the medical community. Many of these add-ons lack sufficient scientific evidence to prove their efficacy, leading to ethical concerns, increased financial burden on patients, and professional disagreements among fertility specialists.
IVF “add-ons” include treatments such as embryo glue, assisted hatching, preimplantation genetic testing for aneuploidy (PGT-A) in younger patients, immunological therapies, endometrial
scratching and many other tests, instrumentations, and procedures. While all of these interventions are often marketed as ways to improve implantation and pregnancy rates, scientific studies have often failed to support their effectiveness.
They, therefore, often lack high-quality evidence as Maheshwari et al., for example, suggested as early as 2016 for routine blastocyst-stage embryo transfer 2 and in 2022 for routine delayed frozen in comparison to fresh blastocyst stage embryo transfers, 3 both “add-ons” to IVF at the CHR identified as likely leading contributors to declining live birth rates in IVF in the U.S since 2010 (an observation further discussed and referenced below), lacking robust randomized controlled trials (RCTs) demonstrating their efficacy.
The UK’s Human Fertilisation and Embryology Authority (HFEA), therefore, has categorized most add-ons as “red” or “amber” on their traffic-light rating system, meaning there is no or conflicting evidence supporting their benefits. 4 Studies on endometrial scratching, for example, have not shown consistent improvements in implantation rates. 5
“Add-ons” may also contribute to placebo effects and other psychological influences, as many patients undergoing IVF feel pressured to try anything that might improve their chances of success, leading to emotional and psychological bias in evaluating these treatments.
Figure 1. Graphic abstract of here discussed paper defining ESHRE’s approach to “add-ons” in reproductive medicine having led to no fewer than 42 recommendations covering diagnosis, diagnostic tests, laboratory tests in general, interventions, and clinical management.
Perceived benefit may, therefore, be due to placebo effects rather than actual physiological improvements. 6
“Add-ons” also may cause financial and ethical concerns: They unquestionably increase costs of treatment, placing additional financial strain on patients without clear benefits. Professional bodies like the American Society for Reproductive Medicine (ASRM) and the European Society of Human Reproduction and Embryology (ESHRE), therefore, discourage the routine use of unproven “add-ons,” citing concerns about misleading claims and lack of transparency.
Most importantly, however, many “add-ons” have potential for harm among those some immunological treatments with potential for significant side effects, which can introduce unnecessary medical risks without improving pregnancy and live birth rates. 7 Misuse
and/or overuse of PGT-A in younger patients may unnecessarily discard viable embryos, reducing a patient’s cumulative chances of success. 8
Having originally invented the term “add-on” to IVF to describe mostly unvalidated additions to routine IVF practice with the alleged intent of improving IVF outcomes, European colleagues have, of course, earned the right to do with this term whatever they wish. But that also means that we can criticize what they have done with this term and, based on a recent publication in Human Reproduction by no fewer than 14 authors from all over Europe, apparently continue to do, as the graphical abstract of this paper above well documents (Figure 1). 9
ESHRE’s effort, as described in above cited paper is, of course, laudable and exceeds in detail and quality everything offered by its counterpart in the U.S., the ASRM/SART conglomerate.

But exactly because it is so comprehensive and expansive, it also dilutes the message, and that is a pity.
As the paper noted, the lack of regulation for the use of “addons” and the often very limited requirements for inclusion of “add-ons” into routine clinical IVF practice resulted in many cases in their introduction to market and routine clinical utilization without proper prior validation studies.
This fact is, in itself, indeed good reason to develop evidence-based guidelines and information to help patients as well as physicians in making informed decisions about their use. But 42 such recommendations, consisting of four diagnoses and diagnostic tests, 17 laboratory tests and interventions, and 21 clinical management “add-ons” in our opinion are too much, and overwhelm patient as well as physician audiences. But even more importantly, they suggest that all 42 recommendations are equally important and that is, of course, very misleading.
ESHRE categorized the 42 “addons” it currently addresses in its good practice recommendations into four groups: (I) “recommended;” (II) “can be considered;” (III) “currently not recommended for routine use;” and (IV) “currently not recommended.” It is worthwhile noting that only 5/42 reviewed “add-ons,” ultimately, were “recommended” or described as “can be considered.” The remaining 37 “add-ons” were
“not recommended for routine clinical use” or outright “not recommended.”
The CHR’s investigators in 2019 identified preimplantation PGT-A as a very likely principal contributor to declining live birth rates in autologous IVF cycles around the world between 2010 and 2016. 10 A recent stillunpublished study of the CHR then, in addition, identified the explosive growth of all-freeze cycles in the U.S., mandating delayed frozen-thawed embryo transfer cycles in place of fresh embryo transfers, as the major culprit for the continuing linear decline of IVF cycle efficiency in producing live births until the year 2021 (Gleicher et al., unpublished data).
PGT-A and all-freeze IVF cycles replacing fresh embryo transfers, therefore, with great likelihood are currently the two practice changes in IVF most responsible not only for IVF after 2010 having failed to further improve outcomes, but for the fact that live birth rates in the U.S., Indeed, have declined by approximately one-third since 2010. Shouldn’t this fact alone earn these two practice changes special attention from ESHRE (and for that matter also ASRM and SART, its U.S. counterpart)?
We certainly think so!
Another excellent example for how illogical this list of 42 “addons” is, presents itself in the fact that only 1/42 of these “add-ons” was outright “recommended,” and that was – almost bizarrely – that high
concentrations of hyaluronic acid (HA) in transfer media “may improve live birth rates in fresh embryo transfers.” Even assuming that to be the case, that ESHRE giving this single “add-on” the only top grade, of course, says a lot about the other 41 reviewed “addons,” but also documents the absurdity of, intentionally or unintentionally, for all practical purposes equating all 42 listed “add-ons” in the mind of the IVF field by addressing them all together as if they had identical impacts on IVF practice.
What instead is needed is not the kind of bureaucratic ranking of these 42 “add-ons” offered by ESHRE, but a clear and statistically accurate assessment of how these 42 “add-ons” have been affecting IVF practice. Should such an analysis then, indeed, confirm the prominent adverse outcome effects of especially PGT-A and all-freeze cycle reported by the CHR’s investigators, then it appears high time for our professional organization to stop playing bureaucratic games by giving “add-ons” fancy designations without logical follow up, as, for example at the end of 2024, again happened, when the ASRM’s and SART’s ethics committees, years overdue, finally opined that PGT-A after over 20 years of increasing clinical utilization in general infertile patient populations still has no definable clinical utility and in certain sub-populations may actually reduce live birth chances. 11
Yet, after over 20 years of

unbroken constant increases in PGT-A utilization, neither ASRM/ SART nor ESHRE (or for that matter any other professional genetic society for example) has been able to reach the only logical next conclusion that, if something has not improved outcomes in over 20 years of promised outcome improvements, isn’t it high time to stop using this treatment, especially when it also adds significant costs to an already exorbitantly expensive IVF cycle?
1. Perrotta M. Biomedical Innovation in Fertility Care. Bristol University Press. July 16. 2024; pp21-47
2. Maheshwari et al., Reprod Biomed Online 2016; 32(2):142-146
3. Idem. Hum Reprod 2022;37(3):476487
4. Human Fertilisation & Embryology Authority (HFEA) 2023; Treatment addons. www.hfea.gov.uk
5. Lensen, S. et al. 2021. Cochrane Database of Systematic Reviews, Issue 6. Art. No.: CD009517. DOI: 10.1002/14651858.CD009517.pub4.
6. Harper et al. BioMedicine Online,2017; 34(6), 583-587.
7. Wheatley et al. J Reprod Immunol 2020; 137, 103078
ESHRE. Hum Reprod Update 2021; 27(1), 1–1
8. Serdarogullari et al., Hum Reprod. 2025, 40(2):398-404
9. Gleicher et al., Hum Reprod Open 2019(3):hoz017
10. ASRM Practice Committee Documents. The use of preimplantation genetic testing for aneuploidy ; A Committee Opinion (2024). https:// www.asrm.org/practice-guidance/ practice-committee-documents/ the-use-of-preimplantation-genetictesting-for-aneuploidy-a-committeeopinion-2024/
Be careful what you believe, especially when the source is only a
In mid-December several news outlets including Inside Precision Medicine 1 published articles reporting that a start up called Gameto 2 in a press release reported the birth of the “first baby born using technology that matures eggs outside the body.”
Maturing eggs outside the body is, of course, called in vitro maturation (IVM) and has been part of IVF – in various forms –for decades. The CHR has with very good results been using so-called rescue IVM (rIVM) routinely to mature immature eggs routinely for over a decade.
Immature eggs are obtained in almost all IVF cycles. Several colleagues have been reporting standard IVM, often without any or only very limited gonadotropin stimulation, especially in women with polycystic ovary syndrome (PCOS), primarily in attempts to avoid hyperstimulation of patients’ ovaries, but also trying to avoid the considerable costs of gonadotropin drugs. How the press release by Gameto was interpreted by the media was, therefore – to say it mildly – highly exaggerated because considerable numbers of women have given birth for decades with oocytes obtained after IVM.
Gameto is a relatively new start up which advertises itself as a “female-led biotech company developing treatment solution to improve women’s reproductive health throughout
their lives: from egg freezing, infertility, and diseases of the reproductive years to menopause and conditions that occur afterward” and features an impressive scientific advisory board, including David Albertini, PhD , (of course very familiar to readers of the VOICE from his contributions), a former Laboratory Director at the CHR, and now a Visiting Scientist, and Harvard University’s George Church, PhD , 2 likely the world’s most entrepreneurial leading scientist based on the number of companies he has founded or co-founded, probably most widely known for trying to resurrect the mammoth in one of these companies.
There is no scientifically verified information available on the “first baby birth” reported by Gameto, because nothing on this case has been reported in the medical literature so-far. What is known is the following: The company in this case probably used induced pluripotent stem cells (iPSCs) to produce granulosa- and/or cumulus-like cells and co-cultured immature oocytes of a patient with these cells, according to the press release. There is very little news in this idea; indeed, the CHR years ago tried such cocultures with granulosa and cumulus cells in rIVM and did not see improvements in oocyte maturation in comparison to no co-culture.
The reported case, moreover, did not eliminate gonadotropin stimulation of the ovaries completely but only reduced it by what was claimed to be 80%
of medication dosage. In other words, except for the addition of iPCs-sourced granulosa/cumulus cells in co-culture (which in the CHR experience has not shown much effectiveness), this is exactly the same process on the same immature oocytes (the CHR has matured routinely through rIVM oocytes from follicles as small as 6mm for many years.
Unless a detailed publication describing this case (and since a single bird does not yet make spring, hopefully other cases), demonstrates additional really new interventions which, moreover, in a controlled trial produce better maturation results than already reported, one can consider the company’s description of the importance of this case only as exaggerated: As it looks right now, this case is not a “milestone, nor a “turning point in reproductive health and technology in IVF.” And whether it has “immense potential” is as of this point also questionable.
We are nevertheless spending so much time on this announcement because it, of course, reminds us of many other announcements by several new companies founded in the infertility space over the last two decades which were as grandiose as this one, led to the inclusion of several products into routine IVF care (and rather remarkable valuations of the companies), only years later in real scientific studies to be found to be useless and – at times – even harmful to patient success. We, of course, hope that this will not be the case



We are nevertheless spending so much time on this announcement because it, of course, reminds us of many other announcements by several new companies founded in the infertility space over the last two decades which were as grandiose as this one, led to the inclusion of several products into routine IVF care (and rather remarkable valuations of the companies), only years later in real scientific studies to be found to be useless and – at times – even harmful to patient success. We, of course, hope that this will not be the case here!
And if we are already talking about the premature introduction of new technologies to the IVF field, when in 2023 Dutch colleagues published a paper in the prestigious medical journal The Lancet , describing a system alleged to allow homebased ovulation monitoring, the CHR in the VOICE briefly commented on it with some skepticism but submitted a much more detailed critique for publication to the medical journal. Now, over a year
later, we received notice that our Letter-to-the-Editor was accepted and is in print. 3
It simply seems that the IVF field does not learn from experience. The examples don’t seem to stop: After spending hundreds of millions of dollars for closed incubation systems with real time video monitoring of embryos based on the promise of improving IVF outcomes, everybody by now agrees that these systems are interesting research utilities but do not improve IVF outcomes. 4 Because the CHR does not introduce major changes to its routine IVF practice, unless having inhouse confirmed their potential benefits, we never brought these systems on line because our own studies already 10 years ago in 2015 revealed that they did not improve IVF cycle outcomes for our patients. 5
There are too many other examples of unvalidated inclusions of tests and procedures into routine IVF, also discussed elsewhere in this issue of the VOICE in addressing “add-ons” to IVF in general. Whether in involves tests, instrumentations, or procedures, just because some researchers

or a company (both of these obviously self-interested parties often in collaboration) make a claim of effectiveness in improving IVF, does not mean that this claim applies to all infertility patients or, in many cases, that the claim really is supportable to even an infertility patient.
The infertility field must finally recognize this reality and must take the logical next steps in preventing the premature and unvalidated introduction of more and more poorly validated new tests and treatments into routine IVF care because, once accepted, it is almost impossible to get rid of them!
ON IVF : Also on the subject of the impact of industry on clinical IVF practice, a recent paper in Fertility and Sterility by New York City investigators from the Albert Einstein/ Montefiore and Columbia University programs offers some more information: 6 The study in principle attempted to determine whether industry payments to physicians were associated with differences in clinical IVF practice and resulting clinical outcomes.
And, without going into the technical details of the study which warrant some criticism, the conclusions, nevertheless, appear credible: Industry payments were not associated with overall IVF outcomes at clinics. However, large clinic set-ups with larger numbers of physicians (which one can assume to include most –
primarily private Equity – owned IVF clinic chains) appear more likely to utilize more “addons” such as PGT-A and frozen embryo transfers dues to allfreeze cycle practices.
If this sounds familiar, you are correct: The CHR’s investigators, indeed, reported just recently as well that Private Equity-owned IVF clinics utilized more PGT-A than academic/hospital- and physician- owned clinics. 7 And then you have to go just one subsection back from this one in our literature review, and you will find this issue as well addressed. Nobody, of course, should be surprised that private equity is trying to make as much money as possible in as short a time as possible. After all, their investment cycle is on average only 5-7 years long.
1. Inside Precision Medicine. December 17,2024. https://www. insideprecisionmedicine.co/topics/ patient-care/first-baby-born-usingtechnology-taht-matures-eggs-outsidethe-body/
2. https://www.gametogen.com/
3. Gleicher et al., Lancet 2025, Online ahead of print.
4. Bhide et al., The Lancet 2024.404(10449):256-265
5. Wu et al., Reprod Biol Endocrinol 2016;14:49
6. Jain et al., Fertil Steril 2025;123(1):115-119
7. Patrizio et al., J Assist reprod genet 2025;42:81-84
And for a change, some really interesting research news affecting
DURING CULTURE: That embryos produce a secretome into the media they are cultured in has been by now known for some time. For some reasons, the small country of Austria has, indeed, become a major center of investigations surrounding this secretome with one group in Vienna and a second group in Innsbruck and Bregenz hard at work in trying to potentially elucidate translational findings with potential clinical applicability.
At the Foundation for Reproductive Medicine Conference (FRMC) in December of 2024, Alok Javali, PhD –originally from the amazing laboratory of Nicolas Rivron, PhD in the Vienna-based group, and now a co-founder of a startup company called “dawn-bio,” indeed offered a very interesting talk on substances identified in the secretome of embryos with clinical potential to improve embryo culture.
This group in 2022 published a groundbreaking paper in Nature magazine of a human blastoid model formed from stem cells with capacity to attach to hormonally stimulated endometrial cells, thus mimicking implantation, which perfectly lent itself to the study of the human embryo secretome. 1 The same group a year later offered further practical detail regarding this model. 2
Now, however, a mostly Innsbruck-based group offered a very interesting paper in
Reproductive Biology and Endocrinology , basically following the same hypothesis that the embryonic secretome should reveal important substances with potential to affect IVF cycle outcomes. 3 Prospectively collecting spent media from successful and unsuccessful human embryos in leading to implantation, they analyzed those media by protein array or used them to stimulate monocyte derived dendritic cells as targets. The idea was to determine the immunomodulatory properties of spent media on the dendritic cells which could inform on the immunology of implantation.
What they found was that human blastocyst-stage embryos secrete and abundance of molecules with abilities to significantly affect and even regulate immune cells in their environment. Specifically, dependent on implantation outcome from a given embryo, its spent media affected dendritic cells differently.
All of these data suggest that treasure-hunting in spent media for biologically active substances appears to be a promising strategy not only for a better understanding of early embryo physiology and implantation, but also of how translational knowledge may be obtained to improve embryo quality during in vitro culture and, potentially, implantation.
REFERENCES
1. Kagawa et al., Nature 2022;601-605
2. Heidari Khoei, et al., Nat Protocols. 2023;18:1584-1620
Endocrinol 2024;22:150

3. Kyvelidou, et al., Reprod Biol
There are always new articles about PGT-A in the literature; unfortunately, they rarely offer valid new data. The JARG , for example, this time published an Opinion article by French and Egyptian co-authors which – though overall more objectively critical of PGT-A than many other recently in these pages discussed opinions on PGT-A – nevertheless summarizes the subject with quite typical noncommittal language, like this: “PGT-A has not consistently proven its effectiveness. The clinical values of PGT-A, therefore, remains controversial.” 1
This despite the fact that even the ASRM last year finally concluded that PGT-A to this date has been unable in general populations to affect any single outcome parameter of IVF. 2 The paper then, however, at least also notes that more recent intention-to-treat studies (with earlier studies having been mostly improperly designed studies using embryo transfers as reference point for outcome calculations), at best, showing only slight improvements and, at worst, a negative impact on cycle outcomes.
In other words, the medical literature – very slowly – finally appears to be shifting the direction of its stance toward PGT-A toward the recognition that a clinical practice which, at least in the U.S. in some IVF clinic has even become mandatory, really offers no real outcome advantages to patients and for many patients may, indeed, be harmful. And at an additional expense of at least ca. $5,000 for every IVF cycle!
And then there is Fertility and Sterility – the principal lead journal of the ASRM which, as noted above, just, years overdue, published a Practice Committee Opinion pointing out that PGT-A in over 20 years of clinical utilization under different names has been unable to demonstrate any clinical utility. 2 The journal, however, now nevertheless published a systematic review and metaanalysis by Turkish colleagues (one currently faculty at Yale University in Connecticut) 3 that concluded that “current lowquality evidence suggests that PGT-A enhances life birth rates per embryo transfer and per patient in unexplained repeated pregnancy loss,” without noting the fact that PGT-A outcome assessments with reference embryo transfer are obviously biased toward good prognosis patients and, therefore, inappropriate.
And then there was, of course, a Reflection article attached to this paper which is mean to be a commentary – usually written by one of the paper’s reviewers,
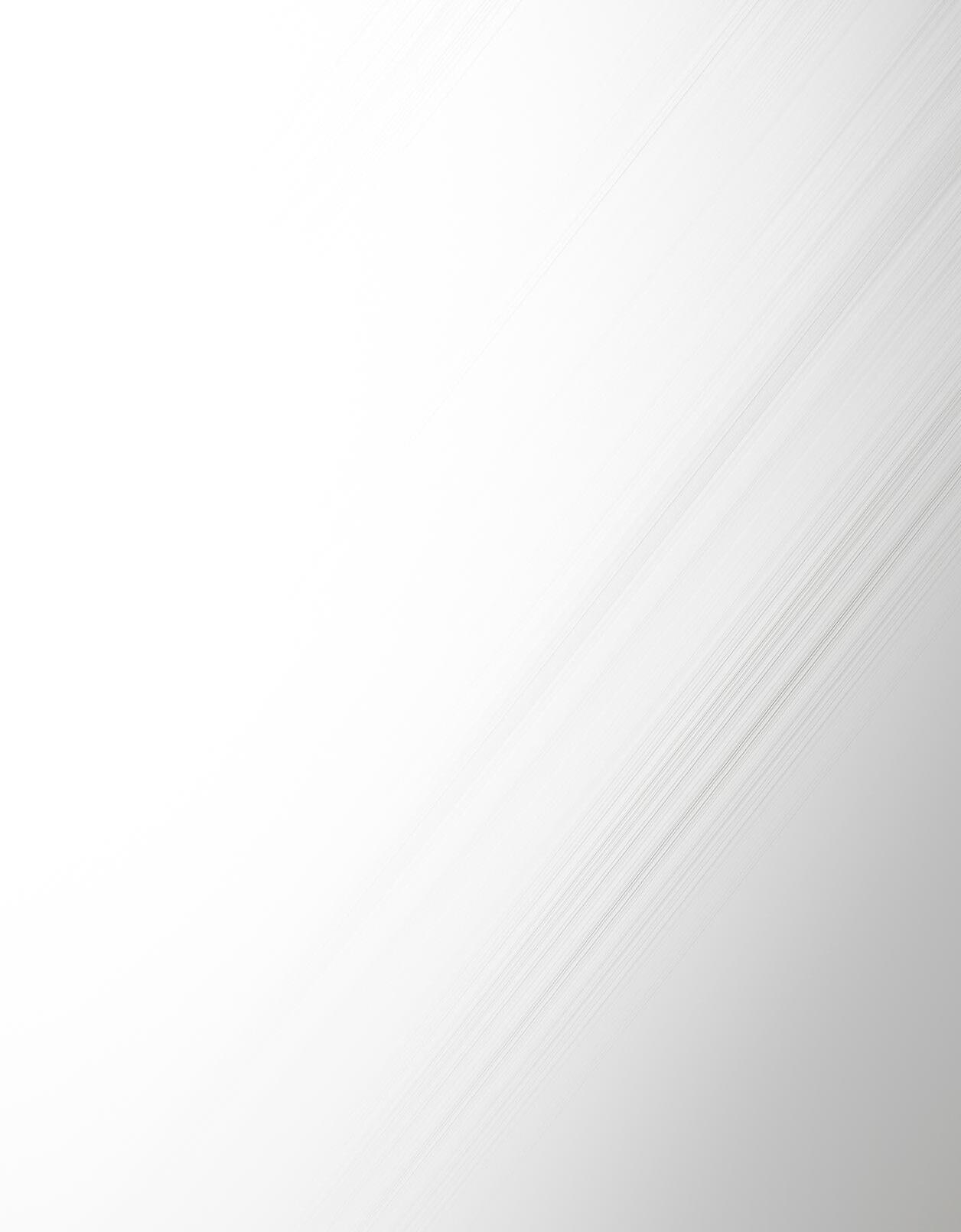
in this case a leading miscarriage expert. 4 And guess what: The commentary argues that “it is time for new guidelines for recurrent pregnancy loss, integrating genetic testing of products of conception” (which we, of course fully support) “with PGT-A” (which we, of course, do not support). 4
One is, of course, left asking, where is the peer review process and where are the journal editors in the decision-making process about PGT-A articles? As long as such obviously incorrect conclusions are allowed to be published in our most important medical journals in the field, who can be surprised that patients and IVF practitioners remain confused about the utilization of PGT-A!
And since we are already talking about Fertility and Sterility , here is another paper worth mentioning in the here discussed context: Including some very prominent names in the field, a group of U.S. investigators – based on a national data set – recently published a paper in this journal under the heading, “Success rates with PGT-A testing for aneuploidy in good prognosis patients are dependent on age.” 5
But the dependence on age was not – as one might have expected – a decline in effectiveness with advancing female age but, exactly, the opposite: PGT-A was reported to improve in effectiveness with increasing patient age, an observation recently also suggested by some other papers
in the literature but, based on simple logic (and mathematics) totally counterintuitive, considering the declining number of eggs and embryos women have at their disposition with advancing age.
At least these authors noted that they were reporting on goodprognosis patients; but what they – like others before them –overlooked is that PGT-A in every patient population investigators may choose for study will always select out best-prognosis patients because the decision to use PGT-A will always be made with significant consideration of how many embryos may be available for testing. If that number is even smaller than the number one is willing to transfer, why do PGT-A for an additional $5,000?
In other words, the recent message from some (unfortunately still existing) supporters of PGT-A utilization in IVF that, while not working in younger patients, PGT-a in older women does show outcome improvement (as this paper is also trying to demonstrate) is statistically total malpractice. The CHR’s investigators are currently working on a paper to demonstrate this fact with solid national statistical data.
1. Viville A, Aboulghar M. J Assiste Reprod genet 2025;412:63-69
2. ASRM Practice Committee Documents. https://www.asrm. org/practice-guidance/practicecommittee-documents/the-use-ofpreimplantation-genetic-testing-foraneuploidy-a-committee-opinion-2024/ 3. Mumusoglu et al., Fertil Steril 2024;123(1):121-136
4. Kutteh et al., Fertil Steril 2025;123:67-68
5. Harris et al., Fertil Steril 2025;123(3):428-438
We, of course, have repeatedly in these pages expressed our unhappiness about the concept of polygenic risk testing of human embryos, which is now already offered by some laboratories and IVF clinics in the U.S. as a commercial product. Two recently published articles in the same issue of Nature magazine, however, went beyond this practice, now raising the possibility of heritable embryonic polygenic editing.
In an article the authors describe an “analysis” (of the literature), they conclude that polygenic genome editing “could theoretically yield extreme reductions in disease susceptibility.” As examples they cite coronary heart disease, diabetes, schizophrenia, major depressive disorders, and Alzheimer’s disease. In addition, risk factors could be addressed, like lipidemias and hypertension. At the same time, the authors recognize significant ethical issues in their models: For example, they concluded that this process – if successful – may deepen health inequities by being available only to the rich. In addition, by changing gene variants to reduce certain risks, other risks may be increased. 1
An accompanying Commentary by three scientists from the U.S and Israel is more blunt in clearly stating that embryo

editing is unsafe and unproven. 2 Referring to the authors of the original paper who concluded from their models that the technology to do this kind of embryo testing will be of such low risk and of such high effectiveness in every individual that deploying it on a large scale may be justified even for relatively low risks, the authors of the Commentary question both of these conclusions. They furthermore ask “whether it is wise to distract stakeholders, including the public, with a technology that is still a long way off at best, and might never actually be safe?”
We couldn’t agree more!
REFERENCES
1. Visscher et al., Nature 2025;637:637645
2. Carmi et al., Nature 2025;637:554556
With cfDNA test increasing in utilization beyond just routine noninvasive prenatal screening (NIPS) as recently here in the VOICE discussed regarding the accidental diagnosis of cancers during early prenatal testing, a recent review article in the Journal of the Endocrine Society was timely. The main purpose of the paper was to determine through NIPS established discrepancies between sex prediction and fetal sex after prenatal noninvasive cfDNA screening. 1 This very clearly presented review article concluded that beyond screening for common autosomal trisomies
(in chromosomes 13, 18, 21).
NIPS offers an opportunity to discover fetal and parental sex chromosome variations by addressing also fetal and parental sex chromosome variations, suspect other healthrelated conditions like for example cancers, and predict fetal sex. Physicians, however, must be aware of potential discordances between fetal sex predictions by prenatal cfDNA screening and/or prenatal ultrasound and actual phenotype and sex chromosomes at birth, as neither noninvasive cfDNA screening nor prenatal ultrasound are 100% accurate in fetal sex prediction. Most discrepancies are not due to fetal causes. Atypical sex development of infants, described as “difference in sex development (DSD),” however, represent ca. 30%.
REFERENCE
1. Witchel et al., J Endocrine Soc. 2025;9:bvaf007
Y-chromosome genes may regulate spermatogenesis even if they show no phenotypes when individually deleted.
A consortium of European investigators published an interesting article in Science magazine adding important information regarding which genes on the Y chromosome regulate spermatogenesis. 1 The findings using a mouse as well as a human model were, indeed, quite surprising because
they suggested that that certain Y genes may regulate spermatogenesis even if they show no specific phenotypes when individually deleted.
The issue here is that the mammalian Y chromosome contains several gene families which have been known in some way to be involved in spermatogenesis and, therefore, have also been associated in male infertility. To study which genes specifically control spermatogenesis, the authors, using CRISPRCas9, therefore generated 13 mouse models with specific deletions in Y chromosome genes and gene combinations previously implicated in cases of male infertility. What they also found is that in murine spermatogenesis more Y genes are involved than previously estimated which are functionally active in more processes in spermatogenesis than was previously thought.
AZFa, AZFb, and ACFc gene deletions are believed to cause most Y-chromosome associated male infertility and automatically remove multiple Y genes when deleted. To determine which of these genes, therefore, is causing the fertility problem can be very complex. Here discussed paper now informs about the possibility that male infertility may at time be the consequence of cumulative loss of several Y genes, with each of them on their own having only minimal effects on spermatogenesis. The paper, moreover, also noted that some Y genes are also expressed outside of the testis, with such

Y chromosome loss now having been linked to aging and related diseases, like cancer and heart disease.
REFERENCE
1. Subrini et al., Science 2025;387(6732):393-400
And the X chromosome impairs the development of male fetal germ cell
And since we don’t want to be discriminatory toward the X chromosome, there is also interesting news to report on X (and we are not talking about Elon Musk ). Chinese investigators figured out how an extra X chromosome impairs the development of fetal male germ cells. 1
The development of fetal germ cells (FGCs) regulates the dosage of X-linked genes. However, in which way aberrant dosages of X-linked genes (like, for example in Klinefelter syndrome, XXY) impair FGCs was so-far not well understood, even though Klinefelter syndrome offers a natural model.
This paper demonstrated that in Klinefelter cases most FGCs are arrested in early stages, characterized by upregulation of genes related to pluripotency, along with downregulation of genes involved in FGC differentiation. Overall, the study demonstrates how the extra X chromosome in Klinefelter impairs the development of male FGCs.
REFERENCE
1. Lu et al., Nature 2024;635:960-968
In an “A Piece of My Mind” article in a recent JAMA issue, a female physician reported her own experience to disseminate the message that an excessive family history of cancers should sound the alarm bells and result in the genetic evaluation of individuals for cancer risk. 1 And that does not only mean screening for BRACA 1 and BACA 2 mutations which we all know are associated with significantly increased breast and ovarian cancer risk (they also are associated with increased pancreatic cancer, an increasingly frequently diagnosed cancer in women).
Concerned because of repeated cancers in her family, the physician was seeking a way “to be watched.” By coincidence, her hospital had an excellent ovarian cancer surveillance program that was willing to accept her, even though she did not fulfill all of their usual criteria (it sometimes is, after all, good to be a physician). She consequently had annual ultrasounds and CA125 assessments. After 17 years of negative surveillance, another family member was diagnosed with cancer, and raising this fact in her medical community, a genetic counselor recommended she undergo a genetic evaluation for cancer risks.
Even though her mot her’s cancer had been checked for Lynch syndrome (and was found to be negative), and, while she had other gynecological cancers in the family but did not have a family history of ovarian cancer, she decided to ask for 84-cancer gene panel. Everybody was shocked when this test revealed that she carried a mutation in the RAD51D gene, which denotes a 10-20% lifetime risk for ovarian, fallopian tube, or primary peritoneal cancer risk, and also increases breast cancer risk. As a consequence, she had prophylactic surgery, and a very early-stage ovarian cancer was discovered in the specimen.
Even as a physician, she acknowledged never to have heard about the RAD51D gene! It in principle protects against cancers and, when mutated, becomes permissive. And while the cancer risk from such a mutation is not as high as a BRACA mutation, it is, still, significant and there are now quite a large number of cancer genes known, certainly making it worthwhile to test patients who have unusually high cancer rates in their families.
REFERENCE
1. Di Maggio D. JAMA 2024;322(20):1703-1704

The SARS-CoV-2 virus is still around and changing
LONG COVID – In a recent paper in JAMA Network Open involving 12,276 participants, females were demonstrated to have a significantly higher risk of long COVID in comparison to males, even though males had more severe disease and demonstrated a higher mortality. Overall, female sex was associated with a 1.31-times higher risk of long COVID in a full model with matching on demographic and enrollment factors, social determinants of health, and hospitalization and vaccination status during first infection. In a reduced model including only age, race, and ethnicity, female sex showed an even higher risk ratio for long COVID (1.44). Though this difference was small, it nevertheless suggests that factors downstream of an individual’s sex attenuate the estimated risk ratio of long COVID.
This difference was apparent at all ages, except between 18 and 39 years, and if the analysis in females was restricted to only non-pregnant women, applied to women of all ages. The association of long COVID risk, thus, was associated with female sex, which in turn was also associated with age, pregnancy, and was menopausal status
dependent, with no elevated risk observed in women between ages 40 and 55 years. Trying to explain this finding, the authors concluded after a review of the literature and in consideration of their data that differences in hormonal levels may partially explain the higher prevalence of long COVID in females younger than 55 years.
The authors also conclude that the sex-specific predilection of women to long COVID may have similar causes as other post viral sequelae, such as Epstein-Barr, Lyme disease, and others. But there, of course, is also similarity with autoimmune conditions which are known to be much more frequent in women than men, though – like here with COVID – men have more severe disease. Moreover, autoimmune diseases also tend to flare with termination of fetal-placental tolerance peripartum and, often, during months postpartum.
This so-called prospective NIH RECOVER Adult cohort study, thus, pointed out that females infected by the SARS-CoV-2 virus demonstrate the same predilection toward long COVID as females demonstrate to other post-viral and especially autoimmune conditions. As the authors noted, these findings further highlight the need to identify biological mechanisms contributing to sex specificity.
In a Medical News article, the JAMA noted that the so-called XEC is this winter’s likely dominant SARSCoV-2 variant. It apparently
arose from the recombination of two other variants, both descendants of the original Omicron virus, and closely related to variants targeted by this year’s COVID-19 vaccines (called JN.1 and KP.2).
This is likely the reason why COVID in this year’s “flu season” apparently is playing only a second or even third fiddle, with other flu and flu-like viruses dominating the scene. Indeed, flu viruses which during the COVID pandemic had almost completely disappeared, this year have been making a quite remarkable comeback, probably enhanced by the population's hesitance about getting flu shots.
It needs to be restated here, despite the controversy surrounding vaccinations since the pitiful performance of FDA and CDC during the COVID pandemic, that the CHR still strongly recommends that women trying to conceive or already pregnant receive anti-COVID as well as antiflu vaccinations. As we have repeatedly noted in these pages, there are two major reasons for this recommendation: (i) Both infections – if caught while pregnant – are usually clinically more severe than in the non-pregnancy state; and, (ii) if the mother is vaccinated, she passes her immunity to her offspring which, therefore, also has passive immunity for at least three months post-birth.
1. Shah et al., JAMA Network Open 2025; 8(1):e245

And since we are talking about immunizations, a few minutes on immunizations in general appear timely. As noted above, vaccinations have become very controversial after the federal government sent during the COVID pandemic so many misdirections out into the ether of public opinion. The nomination of Robert F. Kennedy, Jr . as Secretary of Health and Human Services (HHS) – neither a physician nor a trained scientist and well known as an anti-vaxxer – also did not help much in instilling new trust into federal health care agencies.
SO FAR IN THE U.S. — And, finally, after four years having eradicated Measles from the country, the Centers for Disease Control (CDC) just reported three outbreaks of Measles since the beginning of 2025. According to the CDC, as of February 28, 2025, the U.S. knows of at least 164 cases (there usually are many more unknown) in Alaska, California, Georgia, Kentucky, New Jersey, New Mexico, New York City, Rhode Island, and Texas. More likely, the disease is already in most states. 1 Media on March 6, 2025, reported that a second person – this time an unvaccinated adult – has died from the disease (the first was a child). 2
Measles was declared eliminated from the U.S. in the year 2000
and the reason was obviously a very satisfactory level of herd immunity in the population through the highly successful measles, mumps, rubella (MMR) vaccine.
The CHR tests immunity to all three of these viral diseases in all patients because all three conditions, if acquired in pregnancy, can have devastating consequences on mothers, pregnancies, and newborns. And we have been nothing but astonished by the increase in the number of patients we have found in more recent months and years deficient in immunity to one or more of these three diseases. This is obviously a sign of declining herd immunity in the population.
When a patient is diagnosed as no longer immune for any of these three diseases, the CHR uniformly strongly recommends a refresher of the MMR vaccine. Since it is a live virus vaccine, such a re-vaccination is recommended at least one month before conception.
The Advisory Committee for Immunization Practices (ACIP) of the CDC is charged with overseeing the country’s vaccination practices. 3 It holds three regularly scheduled meetings each year. Because of the change in administration, its recently scheduled meeting between February 26-28, 2025, was postponed. Its tentative agenda can be viewed at the reference listed below. 4 Members of the Committee can be expected to change significantly.
1. CDC. Measles (Rubeola). Febrauary 28, 2025. https://www.cdc.gov/ measles/data-research/index.html
2. The Washington Post, updated March 7, 2025. https:// www.washingtonpost.com/ health/2025/03/06/measles-deathoutbreak-new-mexico/
3. Advisory Committee on Immunization Practices (ACIP) of the CDC; February 26-28, 2025. https:// www.cdc.gov/acip/index.html
4. CDC. https://www.cdc.gov/ acip/downloads/agendas/ agenda-2025-02-26-28-508.pdf
This was the headline of a recent News article in Science magazine, referring to an antibody-dodging norovirus variant that appears to be driving a major outbreak in the U.S. and elsewhere. 1
The association with the Ferrari name comes from the fact that the virus is “racing” through cruise ships, homes, and long-term care facilities in a “remarkable” winter surge affecting especially the Northern Hemisphere, with everybody ending up in the bathroom, some in hospitals, and a small number even ending up dead.
The virus usually causes explosive diarrhea and vomiting which, fortunately, only lasts for ca. 24 hours. Affected individuals, however, remain infectious because they continue shedding the virus which can remain infectious on surfaces for weeks since it is resistant to many disinfectants. Moreover, there currently exists no vaccine against this virus.

It is believed to cause in the U.S. alone approximately 20 million cases of acute gastroenteritis a year, results in ca. 70,000 hospitalizations and kills approximately 800 people annually. The costs caused by the virus have been estimated to be approximately $10.6 billion (!) annually.
A recent paper in Science Translational Medicine now, however, offers some hope for an oral norovirus vaccine which in a 1b clinical trial was found to be safe and elicited mucosal immunity in older adults between 55 and 80 years. 2
REFERENCES
1. Cohen j. Science 2025;387(6731)”235236
2. Flitter et al., Science Transl Med 2025; 17:788
Here is a short summary of the (as of March 7, 2025) most recent National Situation Summary from the CDC regarding Bird Flu, also called the H5N1 virus: 1
• H5 bird flu is widespread in wild birds worldwide and is causing outbreaks in poultry and U.S. dairy cows with several recent human cases in U.S. dairy and poultry workers.
• While the current public health risk is low, CDC is watching the situation carefully and working with states to monitor people with animal exposures.
• CDC is using its flu
surveillance systems to monitor for H5 bird flu activity in people.
• There is no known person-toperson spread at this time.
• The current public health risk is low.
• Total U.S. cases as of March 7, 2025: 70
• Deaths: Only 1 case
A recent paper in Nature magazine explored the molecular and ecological factors driving the sudden expansion in H5N1 host range and assessed the likelihood of different zoonotic pathways leading to an H5N1 pandemic. 2 The virus has become capable of transmission from mammal to mammal in multiple species, including in European fur farms, South American marine mammals, and U.S dairy cattle. Fear is now spreading that humans may be next. It has become apparent that in dairy cattle, farmed mink, and South American marine mammals, mammal to mammal transitions has occurred in several combinations of mammals, raising the question of whether humans might be hit next. 2
The swine has historically been considered the optimal intermediary host to help avian influenza viruses to adapt to mammals before the jump to humans takes place. It now, however, appears that changes in the ecology of the H5N1 virus have opened new evolutionary pathways, with especially dairy cattle, farmed mink, and South American sea lions representing such new pathways.
The concern about spread to humans has now been growing for some time. A recent News report in the BMJ made this clear after a second admission to a hospital with the diagnosis was reported in the U.S. 3
1. CDC. Avian influenza (Bird Flu), March 7, 2025; https://www.cdc.gov/ bird-flu/situation-summary/index.html
2. Peacock et al., Nature 2025; 637:304-313
3. Taylor L. BMJ 2025; 388:r396
Yes, there has been an outbreak reported in the western part of the Democratic Republic of Congo (Africa) which the WHO initially described as having resulted in 53 deaths among 431 cases (12.5% mortality) and as of February 27, 2025, reported as 60 deaths in 1096 cases of this still unidentified disease (5.6% mortality). 1
And then there is a new dermatophyte, Trichophyton mentagrophytes genotype VII (TMVVII), as the cause of a newly emerging sexually transmitted fungal infection reported in four patients by the CDC’s weekly MMWR In a Notes from the Field report. 2
We have on prior occasions in these pages raised the question of whether the number of unusual infectious events have been increasing and – if that was, indeed, the case – whether such an observation would indicate increased evolution of pathogens and/or a weakening of the human immune system? A recent Viewpoint article in

JAMA was supportive of such concerns by noting that the U.S. healthcare system faces growing challenges from emerging and reemerging pathogens and calling for improved alert systems for emerging infectious diseases. 3 We would have to agree!
REFERENCES
1. Dyer O. BMJ 2025;388:r417
2. Zucker et al., MMWR 2024;73(43):985-987
3. Bhadella N. JAMA 2025;333(2):115116
That the EBV may also have a role to play in autoimmunity has been for some time suspected. Now several investigators published an excellent review article in Nature Reviews Rheumatology on the subject, which we strongly recommend to interested readers.
EBV has in the past been associated with several autoimmune diseases, including SLE, Sjögren’s syndrome, rheumatoid arthritis, and multiple sclerosis. The article especially concentrates on the potential mechanisms by which the EBV likely promotes autoimmunity, which includes EBV nuclear antigen1 – mediated molecular mimicry of human autoantigens; EBV-mediated B cell reprogramming, including EBV nuclear antigen2-mediated dysregulation of autoimmune susceptibility genes, etc.
REFERENCE
1. Robinson etS al., Nat rev Rheumatol 2024;20:729-740
SOME GENERAL INFORMATION ON THE SYNERGY BETWEEN AUTOIMMUNITY AND REPRODUCTION – To recognize and acknowledge how conceptually connected autoimmunity and pregnancy are in biological terms is essential for both of these major areas on scientific exploration. And what establishes this essential conceptual link is only one thing: the development of “tolerance.”
Let us explain: Our daily survival is fully dependent on the normal functioning of our immune systems which, in principle, have two basic functions: As we know, it is our immune system that protects us from invaders, such as bacteria, viruses, parasites, etc. Our immune system, however, also protects us from developing cancers and – here is its second major function –it does all of this while, at the same time also fully recognizing that it, in all of its protective functions, it is not supposed to attack our own body’s components, a process called self-tolerance.
In other words – if functioning correctly – our immune system can differentiate between “self” and “foreign” and, even within “self,” it can differentiate between healthy and unhealthy “self,” fully recognizing that “self” in principle is never to be attacked (unless, as in cancer unhealthy), while “foreign” always must be attacked as soon as it gains access to our organism. That maintaining normal functions within the immune system, therefore, must be a highly complex and multilayered process appears obvious. And, while enormous progress has been made in understanding how our immune systems work (and at times malfunction), much is still to be discovered.
And like all complex systems, from our bodies to rockets we are sending to the stars, our immune system at times malfunctions in one or more of its components. If such a malfunction involves self-tolerance, we develop autoimmunity; if it involves failure to recognize and/ or failure to properly attack an invader, we develop an infectious disease, and if it means that the immune system fails to eliminate early cancer, we develop cancer.
So, what does all of this then have to do with reproduction?
The answer is: everything! And the reason is that an embryo which has to implant in a woman’s uterus is genetically a foreign invader, attempting to achieve what our immune

system sees as one of its principal responsibilities: to exactly avoid such invasions from happening.
Under normal circumstances, 50% of this invader is “foreign” because it genetically represents the woman’s male partner (if an egg donor is involved, the invading embryo is even 100% “foreign”). Under normal circumstances the female immune system, therefore, should instantly aggressively attack this invading organism and reject it, similarly to how it would with great likelihood reject an organ transplant from the same male. But, fascinatedly, no such rejection occurs if the woman’s immune system works properly because, once made aware of the embryo’s desire to implant (i.e., to invade), the female’s immune system reprograms itself in a highly embryo-specific way that allows it – and only it without any accidentally accompanying bacteria, viruses, etc.- to enter the holy grounds of the woman’s body without being rejected.
In other words, the woman’s immune system induces immunologic “tolerance” for the paternal part of the embryo that under all basic biological rules should aggressively be rejected. And—though still only partially understood—the tolerance pathways induced in this process by the maternal immune system have quite significant similarities with pathways our immune systems use for above-described “self-tolerance” which prevents our immune system from attacking our own bodies. These
pathways also share similarities with pathways parasites induce in hosts that allow them to evade the host’s immune system and, as increasing evidence suggests, similar pathways of tolerance inductions in certain ways may also have over evolutionary processes been acquired by cancers, thereby allowing them to evade the usual immune responses and metastasize.
Returning to the invading embryo during implantation, the maternal immune system does not only have to deal with the 50% allogeneic half of the embryo but also with the other 50% which represents the mother’s own genetics. In other words, the maternal immune system has to face an invader with its own genetic makeup; yet, if it were to mount an immune response against this autologous half of the embryo, that at the same time would be an “auto-immune” response which, of course would be destructive to the mother’s wellbeing.
In short, the fact that the maternal immune system – if functioning normally – does not attack the invading (i.e., implanting) embryo in many ways has to be viewed as a “miracle of nature” and, of course, must represent an enormously complicated cascade of reprogramming events within the maternal immune system. And in women with a hyperactive immune system (i.e., evidence of autoimmunity, inflammation, and/or just severe allergies) this reprogramming
process often malfunctions to smaller or larger degrees, resulting in the embryo not being fully protected from being attacked and pregnancies, therefore, prone to miscarriages.
-
We feel that this somewhat lengthy introduction to this section is necessary to explain why autoimmunity is in such a symbiotic relationship with reproduction. On a clinical level this relationship is well demonstrated by the fact that several autoimmune diseases characteristically improve clinically (patients “feel better than they have felt in ages”) after the first trimester, once normal tolerance of the pregnancy has been established and the tolerance pathways established for pregnancy also cross-react with self-tolerance.
At the same time, every pregnancy in patients with any autoimmune disease faces increased risks early in pregnancy when tolerance must be established (as noted, leading to miscarriages) and again in the third trimester and leading into the postpartum period because pregnancy tolerance in women with hyperactive immune systems often – one indeed can say almost always – wears off early, leading to premature labor and deliveries in association with practically all autoimmune diseases, increased risk for preeclampsia, and significant risk for peripartum and postpartum autoimmune disease flares and, often, first clinical

presentation of autoimmune diseases.
And autoimmunity is common, affecting in the U.S. approximately 5% of the population or by 2022, over 15 million people. 1 Roughly two-third of cases occurred in women (63%, a 1.7 to 1 ratio), increasing with advancing age, and peaking above age 65. Autoimmunity, moreover, is highly polygenic in that having one autoimmune disease predisposes significantly to other autoimmune diseases. Indeed, roughly 24% were reported to have two, 8% had three, and 2% had four or more.
The most frequently diagnosed autoimmune disease is rheumatoid arthritis, followed by psoriasis, type 1 diabetes, Grave’s disease, and autoimmune thyroiditis (Hashimoto’s). Moreover 19/20 autoimmune diseases were more frequent in women than men. 2
MENOPAUSAL HORMONE THERAPY INCREASES
AUTOIMMUNE DISEASE RISK – A recent paper in Rheumatology offered rather convincing evidence that menopausal hormone therapy increased risk for developing systemic lupus erythematosus (SLE) and systemic sclerosis (SSc). 3
Studying 943 women with SLE and 733 with SSc, the authors found close associations between menopausal hormone use and both conditions. Moreover, women who received systemic as well as local hormone treatments had
the highest risk of developing both conditions. Another consideration in using hormone replacement therapy in postmenopausal women!
AND SO, APPARENTLY, DOES AN EXTRA X CHROMOSOME – Two investigators from Jefferson University in Philadelphia investigated the dose effect of an extra X chromosome on the development of SLE and Sjögren’s syndrome, both autoimmune diseases with significant female preponderance. In Klinefelter syndrome (KS) the prevalence of SLE has been known to be increased for some time.
What they found was that the extra X chromosome in KS and triple X syndrome conferred a nonproportional, synergistic dose effect on the development of SLE and SjD when compared with the general population. 4 Considering the many immune system-related genes on the X chromosome, this finding should be no surprise. That this fact was now, however, confirmed, informs to a degree why females have such a preponderance in autoimmune diseases in comparison to males.
NAME CHANGES FOR DISEASES: DO THEY REALLY MAKE A DIFFERENCE? – A recent article by Healio informed about several name changes for major autoimmune rheumatologic diseases, including ankylosing spondylitis, Sjögren’s syndrome. We, of course have all used the term ankylosing spondylitis for decades; we also agreed to a subdivision for this term
into radiographic and nonradiographic subtypes; but we will now have to get used to calling under its new name, “axSpA” and, whether it is visible on X-ray is only of academic but not clinical interest. 5
Sjögren’s syndrome also has been assigned a new name to better reflect the current understanding of the disease and its clinical seriousness, but here the change is easy to implement by just changing “syndrome” to “disease” but the reasoning for the renaming appears a little strained.
1. Choudhury J. Medscape Medical News. January 13, 2025. https://www. medscape.com/viewarticle/around-5us-population-diagnosed-autoimmunedisease-2025a10000of
2. Abend et al., J Clin Invest 2025;135(4):e178722
3. Patasova et al., Rheumatology 2025; keaf004.doi: 10.1093/rheumatology/ keaf004. Online ahead of print.
4. Palmer A-K, Tan IJ. ACR Open Rheumatology 2025;7(1):e11778
5. Healio. November 22, 2024. https://www.healio.com/nes/ rheumatology/20241121/ name-change-for-sjrens-axialspondyloarthritis-a-big-deal-forresearchspatients
– Coming off gluten and dairy as part of an antiinflammatory diet has become a common dietary support intervention in autoimmune conditions. To a degree it also has become “fashionable” in infertility practice because gluten especially—a protein in wheat, rye, and barley—can induce significant symptoms in individuals. This becomes apparent in patients with celiac

disease (which, of course is an autoimmune disease of primarily the gut) but can also elicit all kinds of symptoms in patients with just “sensitivity” to gluten. The prevalence of celiac disease in the population is ca. 1%.
Now a large consortium of investigators from all over the world has reported interesting new information on how gluten initiates the celiac disease pathology in the gut. And it is not, as was believed, that gluten induces the inflammatory response inside the gut wall, exclusively involving immune cells. Using gut organoids, they discovered that the epithelium of the gut 1 , made up of usually unrelated cells to the immune system, also plays an important part in producing the inflammatory response to gluten. Specifically, they discovered that Gluten antigens are efficiently presented by MHCII-expressing IECs, resulting in the activation of glutenspecific CD4+ T cells, which is then enhanced by gluten pre-digestion with microbial elastase.
Therapeutics directed at intestinal epithelial cells may, therefore, offer a novel approach for modulating both adaptive and innate immunity in patients with celiac disease.
REFERENCE
1. Rahmani et al., Gastroenterology 20024;167(6):1113-1128
A Research Letter by Danish investigators in JAMA discovered a close association between severe ulcerative colitis and carrier status for HLADRB*01:03, a relatively low frequency allele. The authors suggest that, given the low cost of typing a single HLA allele, it could be useful for risk assessment of patients at diagnosis. 1
REFERENCE
1. Vestergaard et al., JAMA 2024;332(22):1941-1943
Several decades ago, the FDA prohibited in the U.S. the concept of paternal lymphocyte immunization of women with repeated pregnancy loss. There were several reasons behind this decision, among those concerns about some published data which suggested that the procedure may even further enhance the frequently already hyperactive immune system of the miscarrying female. But we hear from patients from outside the U.S., including Canada and Mexico, that there still are IVF clinics that offer this treatment.
One such clinic in Iran now published a study that suggested that paternal lymphocyte immunization may confer benefits in improving pregnancy outcomes, though, paradoxically,
“its efficacy may be influenced by the presence of Anti-TPO antibodies.”
Though the authors concluded that their findings highlight the complex interplay between immune dysregulation and pregnancy outcomes in repeated pregnancy loss, this is not how we would interpret their date and here is why: AntiTPO negative patients with lymphocyte therapy had a lower miscarriage rate (10.53 %) compared to anti-TPO positive RPL patients with lymphocyte immunization (40 %). That observation in our opinion pretty categorically notes that what really matters is not the lymphocyte treatment, but the TPO Ab status of the patient and, if as above noted, a woman already has a hyperactive immune system (i.e., positive TPO Abs), lymphocyte immunization can make things worse!
Of course, as a likely consequence, pregnancy and live birth rates were also higher (89.47 %) in anti-TPO negative patients with lymphocyte treatments compared to antiTPO positive RPL patients with LIT (60 % and 56 % respectively), though it is unclear whether this difference is really significant. Simply a poor paper! For this issue of the VOICE , it clearly deserves a WORST PAPER AWARD . 1
REFERENCE
1. Ebrahimi et al., Hum Immunol 2025;86(2):111229. Recipient of the WORST PAPER AWARD

A recent paper 1 and accompanying Editorial 2 in JAMA addressed what the impact on the future attitude toward pregnancy may be in women who experienced significant morbidity in a pregnancy. Though it is to a degree what we call a “self-fulfilling prophecy study” because it is largely predictable in its outcome, some of such studies do have value (many, or most, don’t and are a waste of time, money and effort), and this is one of those.
As expected, the study revealed that women who in a pregnancy experience significant morbidity were then less likely to have subsequent birth especially after severe uterine rupture, cardiac complications, cerebrovascular accidents, and severe mental health conditions in a first birth. Sibling analysis – though we are not certain to what degree – was not suggestive of any familial cofounding but what was not isolated in the study was the effect of medical advice. And medical advice is, of course, very influential and traditionally always very conservative and sometimes too conservative.
A good example is maternal cardiac disease, which with very few exceptions can be safely managed within a qualified medical setting. 3 But whether a patient has access to such a setting may, and should be, decisive in reaching a decision about a future pregnancy. We, therefore, fully agree with the authors’ conclusion that adequate reproductive counseling and availability of enhanced antenatal care are crucial for the decisionmaking process of women who experienced prior severe morbidity in a pregnancy, as they, of course, also are for every woman with a significant medical problem planning a first pregnancy.
1. Tsamantioti et al., JAMA 2025;333(2):133-142
2. Husby A, Boyd HA. JAMA 2025;333(2):122-123
3. Elkayam et al., J Am College Card 2016;68(4):396-410
As the British National Health Service Blood and Transplant website notes, women can try having a child after a kidney transplant. A woman’s fertility, indeed, will likely improve. Transplant recipients are, however, advised to wait at least a year before trying, to give time for tolerance pathways for the kidney to fully establish themselves. Moreover, treating physicians need to be informed because immunosuppressive medication patients take may have to be changed. 1
But unintended pregnancies happen quite frequently in this population, leading recently to publication of an interesting paper describing the effects of such unintended pregnancies on pregnancy outcomes and graft survival. 2
Among 1,723 pregnancies of kidney transplant recipients, 1,081 (62.7%) were intended and 642 (37.3%) were unintended pregnancies. Risk factors for unintended pregnancy included younger age, Black race, nulliparity, chronic hypertension, and transplant from a deceased donor. Unintended pregnancy was independently associated with allograft loss at 2 years from the end of pregnancy (8.1% vs 3.5%, AOR 2.27, 95% CI, 1.32–3.94, P=.003) but not allograft survival (adjusted hazard ratio 1.22, 95% CI, 1.00–1.49, P=.05). There were no differences in severe maternal morbidity (3.3% vs 3.6%) or neonatal composite morbidity (12.9% vs 14.3%) by pregnancy intention.
1. NHS Blood and Transplant Website. https://www.nhsbt.nhs.uk/organtransplantation/kidney/living-with-akidney-transplant/ 2. O&G Open 2024;1(4)::p.040
It is now well accepted that pregnancy is a diabetogenic state. This means that women who already are prediabetic or diabetic may, respectively, become diabetic or may need more treatment once pregnant than in the non-pregnant state. Gestational diabetes is, however, distinct from these two circumstances in that it is

defined by the development of diabetes during pregnancy which after delivery, however, resolves.
An excellent recent review in the JCEM of gestational diabetes, which was first reported in 1824 in Berlin, Germany, deserves attention. 1 Focusing mostly on the clinical management of this condition, the paper reviews lifestyle-based therapy as well as pharmacotherapy and obstetric management, and discusses the lifelong potential health consequences a diagnosis of gestational diabetes then represents. Clearly a recommended read!
REFERENCE
1. McIntyre et al., J Clin Endocrinol Metab 2025;110:e19-e31
Non-chromosomal congenital anomalies increase at very young as well as advanced maternal ages.
It has been known for quite some time that too young as well as too old age reduces fertility treatment success, for example in IVF. It also has been reported that chromosomal abnormalities demonstrate a similar pattern in pregnancies, with very young and older women demonstrating more aneuploidy than women at inbetween ages. Now, however comes a paper from Hungarian investigators which also demonstrates the same pattern for non-chromosomal congenital abnormalities. 1
Selecting for a systematic review 72 studies in the literature,
maternal age >35 years was associated with increased risk for congenital abnormalities and rising further notably after age 40. Specifically cleft lip/palate and cardio-vascular defects were associated with age over 40. Conversely, gastroschisis was associated with very young maternal age under 20 years.
REFERENCE
1. Pethö et al., Am J Obstet Gynecol 2024;231(5):P490-P500
A first placentacentric treatment of preeclampsia or, maybe, even much more?
A very interesting hypothesis has in recent years been gaining ground among investigators which tries to explain not only how the normal maternal immune system tolerates an embryos immediately from implantation at a microscopic size, but until delivery, by which time the average fetus is at roughly 3.5kg average weight (and often even larger). In other words, the maternal immune system must adjust to exponential growth of the invading, and usually well tolerated parasite, called a fetus.
And this is exactly where the placenta enters the discussion because the placenta is, of course growing in parallel with growth of the fetus. And it does so outside of the fetus and, ultimately, is not only disposable but was apparently destined by nature to be disposed of once it has done its job.
The placenta, widely believed in its principal function meant to provide oxygen and nutrition to the fetus, has now, however, been hypothesized to have a perhaps even more basic function in preventing the euploid fetus from being rejected. And since this organ grows in parallel with the fetus, it maintains in normal pregnancies the effectiveness of this function until the onset of labor and the subsequent delivery. As of that point the placenta is no longer needed and, therefore, is disposed of by nature.
How the placenta protects the fetus from rejection is still largely unresolved, but above noted hypothesis suggests that protection of the fetus from rejection may be the principal reason why the placenta until term remains contaminated by aneuploid cells, while the fetus for very obvious reasons, of course, cannot be seeded by aneuploid cells. Proponents of this hypothesis – which has been ruling at the CHR for decades – indeed, have proposed that similar to cancer, where especially aneuploidy of metastatic disease has been demonstrated to “confuse” immune checkpoints enough to allow cancers to spread, in principle does the same for the placental-fetal unit in helping the placental aneuploidy to confuse the mother’s immune checkpoints which, outside of pregnancy, would violently attack any allogeneic invasion into the body.
Considering that preeclampsia

is increasingly recognized as an immunologically mediated condition of the placenta (likely the cause of waning immune tolerance to the fetus), a recent paper in Nature magazine was for us of great interest. 1
As the authors noted, now widely considered a placental disorder, pre-eclampsia affects 3-5% of pregnancies and is a leading cause of maternal and fetal morbidity. Currently no treatment exists to either prevent or treat the condition, except for delivery of fetus plus placenta, which in a large majority of cases almost instantly “cures” preeclampsia (there exist rare exceptions where preeclampsia can occur postpartum or last into the postpartum period).
It has been reported that lipid nanoparticles ferry therapeutic mRNA to the placenta. 2 The investigators in here discussed study, therefore, concluded that, with no drug available to slow disease progression in preeclampsia, engineering ionizable lipid nanoparticles (LNPs) for extrahepatic messenger RNA (mRNA) delivery to the placenta could be a therapeutic option for preeclampsia. In their paper, they, therefore, used highthroughput screening to evaluate a library of 98 LNP formulations in vivo before identifying a placenta-tropic LNP (LNP 55) that mediated more than 100-fold greater mRNA delivery to the placenta in pregnant mice than a formulation based on the FDA approved Onpattro LNP (DLin-
From this observation, they suggested the existence of an endogenous targeting mechanism based on β2glycoprotein I adsorption that enables LNP delivery to the placenta. They then confirmed their hypothesis by demonstrating in mouse models of inflammation as well as hypoxia-induced preeclampsia that a single administration of LNP 55 encapsulating vascular endothelial growth factor (VEGF) mRNA resolved maternal hypertension (a typical symptom of preeclampsia) until the end of gestation.
Using their VEGF mRNA LNP 55 therapeutic, they in addition demonstrate improvements in fetal health and partially restored the placental vasculature, the local and systemic immune landscape and serum levels of soluble Fmslike tyrosine kinase-1, a clinical biomarker of pre-eclampsia.
For the authors the most important conclusion of their study was, of course, the potential of this mRNA LNP platform for treating placental disorders such as preeclampsia. In our opinion, their accomplishment was, however, even bigger because they for the first time conclusively confirmed that preeclampsia, indeed, must be considered an immunologic placental disorder.
From that, as already noted above, one can then further conclude that the placenta, indeed, must be actively
involved in production and maintenance of immunological tolerance during pregnancy. And, if this is really the case, the placenta may teach us how to induce perfect tolerance against allogeneic organ transplants and – maybe also – how to enhance tolerance pathways in general, which may also offer new treatment avenues for autoimmune diseases.
But that may not even yet be the end of the story. Because – as also increasingly appears likely – cancers have over evolution “stolen” pregnancy’s ability to induce tolerance and applied this ability to the cancer’s survival in an immunologically hostile host immune system, understanding in detail how the placenta succeeds in maintaining tolerance for a logarithmically growing fetus, we should also be able to learn how to interrupt the development of such tolerance which, in turn, could teach us how to better treat metastatic disease.
1. Swingle, et al., Nature. 2025;637(8945):4120421
2. Eccleston A, Nat Rev Drug Discov 2025;24(2):90
It is practically impossible to open just a few medical journals each week without finding an article on the negative effects of low Vitamin D levels in one or the other medical condition. Yale University’s F. Perry Wilson, MD, MSCE , whose weekly Medscape Impact Factor we frequently

cite in these pages for its smart analyses of published data, in his most recent posting actually made fun of all of the various claims having allegedly shown positive Vitamin D effects, challenging readers to show him even one example where such an effect was really confirmed.
But of course, to his own surprise, he finally had found a paper that did exactly that and, therefore, became the subject of his weekly Commentary,1 in which he in his very detailed and analytical ways reexamined the data in the paper, confirming that Vitamin D, indeed, was beneficial in a large study of patients with Multiple Sclerosis (MS), as the figure in the top right demonstrates. 2
Which brings us back to reproductive medicine because a paper in The American Journal of Clinical Nutrition recently also reported Vitamin D effects dependent on maternal status during pregnancy on fetal growth patterns and adverse pregnancy outcomes. 3 In a study that claimed to determine whether first and second trimester maternal Vitamin D levels affected fetal growth patterns and obstetrical outcomes, the authors concluded that first trimester levels, indeed, were linear associated with fetal growth and low levels of Vitamin D (< 40nmol/L) were associated with higher risk of preterm birth. In contrast secondtrimester Vitamin D levels did not demonstrate any of these associations.
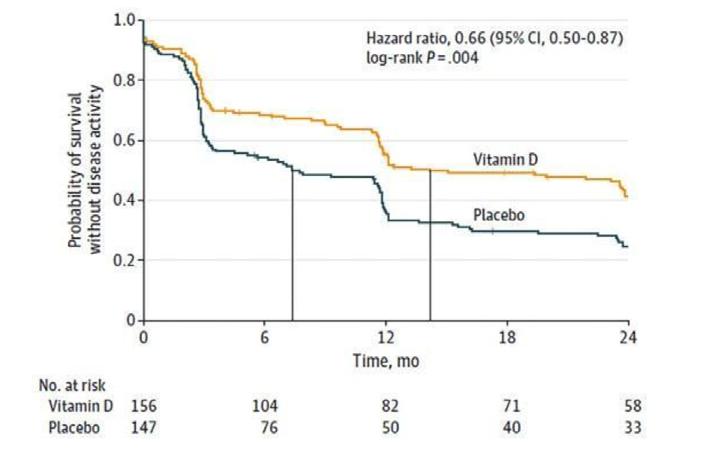
We are not certain that this study would withstand Wilson’s analysis as well as the MS study did. But, considering how inexpensive Vitamin D supplementation is, and considering that most women nowadays take a prenatal vitamin that contains Vitamin D, it may make sense to consider some additional supplementation during the first trimester, though caution regarding the data is indicated and here is why: Some time ago, the so-called VITAL trial, a 5.3 years long randomized 2x2 factorial, double-blind, placebocontrolled trial suggested that Vitamin D supplementation significantly reduced the general autoimmune disease incidence. A follow-up study two years after trial termination then demonstrated, however, that the protective effects of 2,000 IU of daily Vitamin D had fully dissipated. 4,5
What made, moreover, this finding even worse for Vitamin D, was the fact that 1,000 mg per day of n-3 fatty acids, which
in a parallel investigation in the VITAL trial had also proven to be effective, in this twoyear follow up maintained its effectiveness. Clearly an additional example that even published prospectively randomized clinical trials are not always reliable and, certainly, not always the final word.
1. Wilson FP. Medscape Impact factor. March 10, 2025. https://www. medscape.com/viewarticle/rare-winvitamin-d-this-time-ms-2025a10005ul
2. Thouvenot et al., JAMA 2025; doi:10.1001/jama.2025.1604 Online ahead of print.
3. Beck et al., Am J Clin Nutr 2025;121(2):376-384
4. Costenbader et al., Arthrit Rheumat 2024. https://doi.org/10.1002/ art.42811
5. Osterwell N. Medscape Medical News. February 7, 2025. https://www. medscape.cm/viewarticle/preventingautoimmune-diseaseses-new-findingsvitamin-d-omega-2024a10002nc
really increasing stillbirths and neonatal death?
This is what Australian

investigators suggested in a recent paper in the JCEM that obviously passed peer review. 1 And that is troublesome at multiple levels because the authors very clearly intended to suggest – and said so outright in the paper – that the risk of perinatal death may be increased in pregnancies conceived with Clomiphene Citrate. And they did so, even though one would expect the authors to know that decades ago studies demonstrated that these increased risks are mostly associated with medical characteristics of infertile patients rather than the treatment method used to achieve pregnancy.
To simply minimize this point by adding to the abovenoted conclusion that “while established cofounding factors related to infertility were taken into account, there may be some residual contribution of underlying infertility,” is simply not good enough. Everybody in the field knows that and one, for example, must wonder why the control group was not simply another group of infertile women receiving gonadotropins in place of Clomid?
This kind of paper makes infertility practice around the world more difficult because it unnecessarily frightens patients. Reviewers and editors, therefore, should at least have insisted on much clearer emphasis on the principal weakness of the study: the absence of an adequate control group. We, therefore, can only reemphasize a point
routinely made in these pages: Every study starts with careful selection of study and control populations. Nothing is more important!
1.
Moore et al., J Clin Endocrinol Matab 2024;dgae741
In a retrospective multicenter study at tertiary centers in Austria, Germany, Italy, Sweden, and the U.S., 72 adult women with congenital adrenal hyperplasia (CAH) were included, among them 34 with nonclassical CAH, 21 with simple virilizing and, 17 with salt wasting forms. They experienced 133 pregnancies, 112 live births, and 25 abortions.
Though these numbers appeared to lie within somewhat low but still normal range, patients, interestingly, demonstrated a clearly prolonged time to conception: In the salt wasting form this meant a median of 11 months; in the simple virilizing form it took a median of 24 months, and it took only 8 months in the non-classical type. Moreover, even this timing was achieved with use of fertilityenhancing medication (25.6%) and assisted reproductive techniques (30.8%). Indeed, over half of all participants qualified for a diagnosis of infertility since it took them over 12 months to conceive. Average number of live births was, however, at 1.4-1.6, comparable to general populations and similar among
CAH subtypes.
The spontaneous abortion rate at 18% was also in the normal population range, but Cesarean sections were more frequent (60.9%).
1. Auer et al., J Endocr. Soc. 2024;9(1):bvae211
It does not happen often that we discuss papers in the cardiology literature here; but here are two exceptions: In an article in the JACC Advances colleagues in cardiology reported on cardiovascular complications in pregnancy in women with psoriasis. 1
Psoriasis is, of course, an autoimmune disease and, even though it in many, if not most cases, is not considered a major medical problem, it is associated with all the typical complications of autoimmune diseases in association with pregnancy, including increased risks for miscarriages, premature labor and delivery and, as this study again confirmed, preeclampsia/eclampsia. What came as somewhat of a surprise was the finding of more cardiac arrhythmias in these patients, a finding to the best of our knowledge not reported before.
More important is, however, to reemphasize that obstetrical risks in patients with autoimmune diseases, as we like

to repeat often in these pages, is not linked to one or the other laboratory tests as often argued in the reproductive immunology literature. And many risks are also not particularly linked to one or the other autoimmune disease (though there, of course, are disease-specific risks as well) but to the hyperactive immune system characteristic of all autoimmunity.
In a second paper, interestingly, Ob/Gyn colleagues from the U.S. reported in a cardiology journal on cardiovascular complications in the year after delivery of a twin pregnancy. 2 This is a question which, to the best of our knowledge, had never before been investigated.
And results were, indeed, very interesting: Using the Nationwide Readmission Database of U.S. hospitals between 2010 and 2020, cardiovascular readmissions in the first years after readmission in twin and singleton pregnancies were 1105.4/100,000 and 734.1/100,00 deliveries. Compared to singleton pregnancies without hypertensive diseases of pregnancy (including preeclampsia), the adjusted hazard ratio for a cardiovascular readmission was the highest for twins with hypertensive disease, followed by singletons with hypertensive disease, and twins without hypertensive disease.
These are fascinating findings, though we would interpret them somewhat differently from the authors who emphasized
that – compared to singletons without hypertension, even in absence of hypertension, twin pregnancies demonstrated increased admission rates in the first postpartum year, suggesting that twin pregnancies put an increased strain on the maternal cardiovascular system. But the authors in our opinion did not stress enough the additional risk a hypertensive pregnancy denotes, of course, more so in twin pregnancies.
The study, therefore, really suggests that all twin pregnancies should be carefully followed during the first postpartum year, but especially hypertensive twin pregnancies and maybe also hypertensive singleton pregnancies.
Finally, readers of the VOICE will likely be familiar with the CHR’s disagreement with the widely held belief in infertility as well as obstetric/perinatal practice that twin pregnancies in young and healthy women carry with them significant increased maternal and/or fetal risks. As the CHR’s investigators have published in several papers over the years, this incorrect conclusion held by so many colleagues has been mostly based on the comparison of outcomes in one twin pregnancy to one singleton pregnancy, an inappropriate statistical comparison because it compares apples with oranges (i.e., one vs. two newborns). A correct comparison must compare outcomes of one twin pregnancy to two consecutive singleton pregnancies, and even such a comparison falls short because an infertile woman can
never be guaranteed the chance of a second pregnancy.
At the same time we, however, now must acknowledge that the reported findings in this paper may, indeed, represent a valid argument against twin pregnancies in infertility practice.
1. Agrawal et al., JACC Advance 2025; 4(2):101562
2. Lin et al., Europ Heart J. 2025;:ehaf003
The National Center for Health Statistics at the CDC in February published maternal mortality rates in the U.S. for 2022. Maternal mortality rates decreased significantly from prior years (see below Figure1).
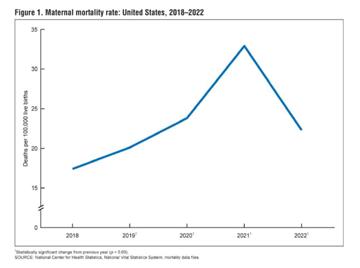
This applied to practically all races (see Figure 2 at the top of next page) but the observed decrease for Asian non-Hispanic women was not statistically significant. In 2022, the maternal mortality rate for Black women (45.9 deaths/100,000 live births) remained, however, significantly higher than the rate for White (19.0), Hispanic (16.9), and Asian (13.2) women.

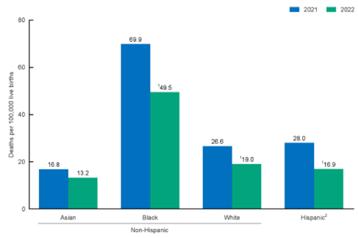
1 Statistically significant decrease from previous year (p < 0.05).
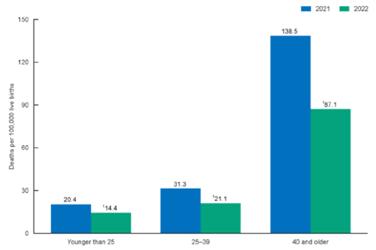
2 Hispanic people may be of any race.
NOTE: Race groups are single race.
SOURCE: National Center for Health Statistics, National Vital Statistics System, mortality data files.
Rates also decreased significantly for all age groups from 2021 to 2022 (Figure 3 below). Rates in 2022 were 14.4 deaths per 100,000 live births for women younger than 25, 21.1 for those ages 25–39, and 87.1 for those age 40 and older. The rate for women of age 40 and older was six times higher than the rate for women younger than age 25. Differences in the rates between age groups were statistically significant. Though these rates in this one year greatly improved, one bird still does not make spring. U.S. maternal mortality rates are still among the highest among developed countries and clearly require further improvements.
THE EVOLVING GENOMICS OF PCOS PHENOTYPES – Though there is disagreement on how many phenotypes exist within the condition generally called PCOS, it is only relatively recently that investigators have attempted to define phenotypes not only phenotypically but also genomically. Within such a context, we previously noted in these pages especially the work of the New York Mount Sinai group, 1 which from such genomic studies concluded that PCOS basically represented two distinct entities with great similarity to what the CHR’s investigators concluded based on clinical observations. 2
Now, based on the hypothesis that genetic risk loci could influence measurable PCOS phenotype traits, U.S. investigators investigated 404 PCOS patients (diagnosed not by Rotterdam but by NIH criteria) and 408 normoandrogenic controls with regular menses and identified several associations: In a combined analysis of cases and controls, 2 variants in loci containing the genes PRSS23 and FSHB were associated with gonadotropin levels. Two variants in loci
containing NEIL2/GATA4 and CYP3 were associated with androgen levels. Three variants in loci containing SHBG, ZBTB16, and CYP3 were associated with ovarian morphology. One variant in the locus containing FTO was associated with hip circumference and was influenced by body mass index. 3
Unsurprisingly and correctly, they concluded that these results demonstrated that genetic risk variants associated with PCOS may influence hormones, ovarian morphology, and risk for obesity, all classical findings in a majority of women currently considered to be PCOS patients.
But, sadly, the study made the usual patients selection error which unfortunately characterizes basically almost all published PCOS studies and that is the assumption that every PCOS patient is hyperandrogenic.
While most, indeed, are a distinct and in our opinion greatly undercounted group of PCOS patients, under Rotterdam criteria defined as phenotype D (also called the “lean” or, erroneously, nonhyperandrogenic phenotype), was basically excluded from this study by defining the PCOS group as uniformly hyperandrogenic.
The D-phenotype is hyperandrogenic between menarche and ca. age 25, then enters the normal androgen range for a decade (ages 25 to 35 is when most PCOS cases are diagnosed,
which is the reason why this phenotype erroneously under Rotterdam criteria is considered non-hyperandrogenic) and after age 35 enters hypo-androgenic terrain. 2
By either purposefully excluding these PCOS patients or, alternatively, by unknowingly including them with hyperandrogenic women, all PCOS – the here presented one included – are unfortunately “contaminated.” That this study, nevertheless, was still able to demonstrate above noted associations, therefore, suggests that the observed associations must be quite pronounced and deserve further exploration.
AND PCOS – Related to the preceding, a recent study by Chinese investigators in the JCEM demonstrated in a bidirectional 2-sample Mendelian randomization study a causal association between elevated BMI and the risk of PCOS. 4 The study also demonstrated that the severity of PCOS may contribute to elevated BMI levels.
Though all of these findings linking phenotypical features of PCOS to specific genotypes so far do not contribute much to our clinical appreciation of PCOS, they help in establishing a new direction for research in PCOS (hopefully with proper patient selection for study and control groups).
REFERENCES
1. Dapas M, Dunaif A. Endocr. Rev 2022;43(6):927-965
2. Gleicher et al., Biomedicines 2022;10(7):1505
3. TIDWELL ET AL., J Endocr Soc 2024;9(1):bvae219
4. Fang et al., J Clin Endocrinol Metab 2025;
PREGNANCY OUTCOMES IN ENDOMETRIOSIS PATIENTS
– The literature on how endometriosis patients do in their pregnancy once they conceive, is surprisingly sparse. A paper by French investigators on the subject in Fertility and Sterility , therefore, attracted our attention. 1
The endometriosis group reported infertility more often before the studied pregnancy (34.7 vs. 5.0%), experienced more hospitalizations during the pregnancy (27.4 vs. 19.8%), and more planned cesarean sections (14.0 vs. 8.7); moreover, they more often were nulliparous (51.7 vs. 43.4%) and more often experienced preterm births before 37 weeks (11.1% vs. 7.7%) and before 33 weeks (3.1% vs 2.2%). Adjusted relative risks for confounding factors was also higher in the endometriosis group for preterm delivery <37 weeks and <33 weeks. Adjusted risk ratios for secondary outcomes, such as preeclampsia, placenta previa, postpartum hemorrhage, and small-forgestational-age status of <10th and <5th percentiles were also higher in the endometriosis group. The adjusted risk ratios for stillbirth and small-for-


gestational-age status of <3rd percentile and after stratification for preterm birth at <37 and <33 weeks, however, did not differ significantly for the secondary outcomes. Only the risk of placenta previa was higher in the medically assisted reproduction than non-medically assisted reproduction subgroups.
In short, endometriosis is a truly nasty disease when it comes to reproduction. It not only often makes conception difficult, but even once you are pregnant, you still have a harder time delivering a healthy baby.
These are important findings because they are further evidence for endometriosis being a truly systemic disease. Also very interesting is the association with preterm labor and delivery, which is, of course, a typical characteristic of autoimmune diseases. 2 And the CHR’s Norbert Gleicher, MD, decades ago noted the close association of endometriosis with autoimmunity, indeed raising the question of whether endometriosis should be viewed as an autoimmune disease.3
ENDOMETRIOSIS AND ADENOMYOSIS
PERIIMPLANTATION TO IVF WITH TNF-α? – TNF-α (Tumor Necrosis Factor-alpha), produced by monocytes and macrophages during inflammations, is a socalled inflammatory cytokine, responsible for a range of signaling events in cells, leading to their destruction (necrosis) and absorption (apoptosis). It also plays important roles in resistance to infections and
cancer.
Several studies suggested that increased secretion of tumor necrosis factor alpha (TNF-α) played a key role in pro-inflammatory response in women with endometriosis/ adenomyosis. Moreover, the cytokine is also considered to be embryotoxic and may impair endometrial receptivity. Consequently, inhibitor of TNF-α, such as etanercept (Enbrel®) and adalimumab (Humira®), have in very preliminary studies been used in attempts to improve in endometriosis/adenomyosis patients (both obviously inflammatory diseases) IVF outcomes. Chinese investigators now published as study on the use of adalimumab in frozen embryo transfer which, at times, can offer more controlled results than fresh IVF cycles regarding implantation chances. 4
Unfortunately, the study for several reasons was of very limited quality: First, it was designed as a retrospective study of 141 women diagnosed with endometriosis and/or adenomyosis. Though similar in composition, these two conditions, nevertheless, reflect distinctively different clinical phenotypes, and bunching them together into one study group, therefore, does not make much sense. As a retrospective study, it, moreover, is, of course, exposed to all the possible biases retrospective studies always provide, including, of course, very significant differences in ovarian stimulation and, most importantly, 84 women were,
and 57 patients were not treated with adalimumab; and there must have been good reasons why some did and others did not receive this treatment, even though demographics and patient characteristics between the two groups were “comparable.”
The authors reported that adalimumab significantly improved implantation rates and clinical pregnancy rates but had no difference in ongoing pregnancy rates and live birth rates. After adjustments for age, BMI, number of failed prior transfer, and other factors in multiple regression analysis, untreated patients had a significantly lower clinical pregnancy rate and very similar chance of ongoing pregnancy and live birth rates. In short, even though the authors in their conclusions tried to “invent” what they called “clinical relevance” of TNF-α, treatment, there was really absolutely nothing there.
Because of the poor quality of the paper, it, however, would also be inappropriate to consider this study as evidence that TNF-α does not improve IVF outcomes in endometriosis and/or adenomyosis patients because, conceptually, such treatment would make sense. But without properly obtained evidence of effectiveness, using TNF-α inhibitors apparently without informed consent from patients that such treatment in fertility practice must still be considered experimental appears ethically very questionable.

It is, of course also of concern that a paper of such poor quality and with such very obvious ethical concerns made it through peer review and the editorial process at one of the two existing international reproductive immunology journals.
1. Vendittelli et al., Fertil Steril 2025;123(1):137-146.
2. Gleicher N. Clin Rev Allergy Immunol 2010;39(3):194-206
3. Gleicher et al., Obstet Gynecol 1987;70(1):115-122
4. Liu et al., J Reprod Immunol 2025;167:104415
Ovarian cancer detection by ultrasound: are we finally there?
As an important recent paper in Nature Medicine demonstrated, A.I.-trained detection models significantly outperformed expert as well as non-expert ultrasound examiners on all evaluated metrics. 1 Based on these findings, the authors (from 20 precipitating centers) concluded that transformerbased models exhibit strong generalization and above human expert-level diagnostic accuracy, with the potential of alleviating the shortage of expert ultrasound examiners.
Though, as already noted in the introductory sentence, this is an important paper, it at the same time raises several important questions before radiology departments should run out there and purchase marketed A.I. programs for the
detection of ovarian cancers. We, for example, know that even trained sonographers vary in accuracy of their findings. In other words, we don’t know how good the expert and non-expert sonographers in 20 participating centers in different countries were; but we know that they must have included many very good and at least some pretty bad sonographers. The question, therefore, remains open: how does A.I. compare to very good and not so good technicians?
A similar circumstance existed in the fertility field with the increasing use of closed incubation systems in embryology, which have been claimed to be cost-effective by saving valuable embryologist time (with IVF clinics these days experiencing similar shortages of embryologists as radiologists and infertility clinics experience with sonographers). For the CHR, these closed incubation systems, however, did not work out because in this center’s very adversely selected patient population, the “do everything the same way for everybody approach” did not work. At the same time – assuming they are checking – it seems to work well in other IVF clinics with a more typical infertility patient population.
Therefore, the real question to be asked from A.I.-based ovarian cancer detection systems is not whether they can “replace” sonographers. Of course they can, sooner or later; the question is just at what detection level?
And that, indeed, is the real question this paper failed to address: At what time point is the system able to detect ovarian cancer? The diagnostic problem is not that ovarian cancers are not detected; they are not detected early enough to improve the prognosis of the patient, and whether A.I.-driven ultrasounds can lead to earlier diagnosis is, therefore, the real question that must be answered as quickly as possible.
1. Christiansen et al., Na Med 2025;31:189-196
Is sensitivity to chemotherapy dependent on fluctuations in ovarian hormones? – According to a recent paper in Nature magazine, that, indeed, appears to be the case based on mouse as well as human data. 1 These observation as a Commentary in the same issue noted, suggest the possibility that – at least breast cancer survival rates (the cancer investigated) could be improved simply by timing treatment, or at least treatment onset, to a specific stage of the menstrual cycle. 2 As the Commentary, however, also noted, this article offers only proof of concept in support of a hypothesis. Now clinical trials need to determine whether the hypothesis really improves cancer survival.
And if we are already talking about the female breast, it is well known that aneuploid epithelial cells are a common presence in breast cancer. Indeed, aneuploidy is a very
common feature in most cancers. A recent study in Nature magazine, now, however, reported that even normal breast tissue harbors rare populations of aneuploid epithelial cells which increase with age. 3
The authors in the discussion of their paper also ask and answer the logical follow-up question, which is, if aneuploid cells are “normal” in normal breast tissue, does this also apply to other tissues/organs. And they answer this question with a likely yes. And if that were to be confirmed, the next followup questions are even more obvious: What is their purpose, and could they represent cells at increased risk of becoming the original stem cells of freshly arising cancers? And how do
these cells interphase with the host’s immune cells? Could they, maybe, even have the opposite function of just sensitizing the host’s immune system enough to kill off freshly arising initial cancers?
What an excellent example for how science works! An unexpected, seemingly coincidental finding, raising so many new and fascinating questions to be pursued.
1. Bornes et al., Nature 2025;637:195204
2. Ingman WV. Nature 2025;637:39-41

AGING – This was recently the title in over one-inch-large letters in a Feature article in Nature magazine, which tried to make the point that menopause has been for too long ignored. 1 In reviewing what is going on in this arena of medical practice, the article concentrated on two major developments: First, for several good reasons, on the return to popularity of hormone replacement therapy and, second, on attempts to delay menopause through such drugs as rapamycin, a drug widely used in solid organ transplantation, but also in anti-aging medicine. The article in this context also again referred to the clinical trial Zev Williams, MD, the REI division head at Columbia University in NYC, is conducting on rapamycin use, which we have having repeatedly referred


to in these pages.
On a theoretical basis, rapamycin may, indeed, be able to stop (or at least slow) ovarian aging; but it will take time to, first, even work out dosages and length of treatments to reach also still to be defined endpoints for such treatments. There, however, can be no doubt that ovarian aging and menopause have been for too long overlooked, not only in their medical relevance but also in their societal importance. The article, therefore, was timely.
– In a register-based emulation targeted trial using the Swedish national register, Swedish investigators looked at a very old and still very controversial issue: cardiovascular risk from postmenopausal hormone replacement therapy (HRT). 2 They once again noted a increased risk of ischemic heart disease and venous thromboembolism with use of oral continuously combined contemporary menopausal hormone therapy.
Tibolone (Livial®), a selective tissue estrogen action regulator, in the U.S. because of sideeffects not FDA- approved, was associated with an increased risk of arterial thrombotic events including ischemic heart disease, cerebral infarction, myocardial infarction, but not venous events.
The authors interpreted their results as reminders of how
different hormone combinations in different ways affect cardiovascular (and other) risks.
1. Peeples L. Nature 2025;637:782784
2. Johansson et al., BMJ 2024;387:e078784
Sherman J. Silber, MD , is undoubtedly one of the most successful REI practitioners since the establishment of this medical subspecialty, but he – undoubtedly – is also its most unique one. Not only is he almost alone in reaching such recognition as a urologist in a field so clearly dominated by obstetrician/gynecologists and by not only contributing on the male-fertility side of the field by – in its time – becoming, likely, one of the most successful microsurgeons worldwide in reversing vasectomies, but also in contributing very significantly to progress on the female side of infertility. And he did this in many different ways, but especially in becoming a world leader in fertility preservation through ovarian tissue freezing and reimplantation, a procedure initially developed for young women on the verge of losing their ovarian function to toxic medications, but now even used more widely for other indications as well. And he in this process was also the first to report the first successful ovarian transplant between identical twins.
The occasion for giving him his long-deserved credit here is a
paper he recently published as lead author in Fertility and Sterility, in which he (and coauthors) reported the first successful ovarian cortex transplant to a Turner syndrome patient. 1 And, as always, he is to be congratulated on this new achievement at an age when most of his colleagues are already enjoying retirement. We, however, in this case have also to politely disagree with him on his conclusion that ovarian cortex allotransplantation now will become a much more frequently performed fertility preservation method and not only in cases of Turner syndrome or in replacement of whole ovary transplants.
While in replacement of whole ovary transplants, this may, indeed, be a technically simpler and, therefore, valuable approach, otherwise we do not see the utility. Indeed, we do not even see the utility of doing such a transplant in the reported Turner syndrome case. If the purpose was pregnancy, why not do a simple egg donation cycle, which does not require surgery and does not require chemotherapy and, at some point, a second surgery to remove the allogeneic graft.
This circumstance to a smaller degree mimics the now in several centers offered concept of uterine transplantation (though, of course, regarding surgery a much smaller feat). When the first uterine transplant was reported by Swedish colleagues, we were in total awe of their technical accomplishment, especially
since over years they did it ethically, by developing the project initially in animal models before going on to the human experience.
But even then – and, frankly speaking, to this day – we have had difficulties with the risk-benefit considerations of a uterine transplant surgery, considering that the first consideration in medicine is “to do no harm.” Like we still have great difficulty with the concept of a uterine transplant requiring multiple surgeries for donor and recipient of the uterus and requiring at least temporary immune suppression for the recipient as well as the pregnancy she ultimately may or may not carry, it here seems that
the surgery and immunosuppression of the patients was even less needed: If pregnancy was the only ultimate goal, why not simply use an egg donor?
But this, of course, is not meant to take anything away from the intellectual and technical accomplishment this case report represents! We just don’t want to see it repeated too often!
1. Silber et al., Fertil Steril 2025;123(1):156-163

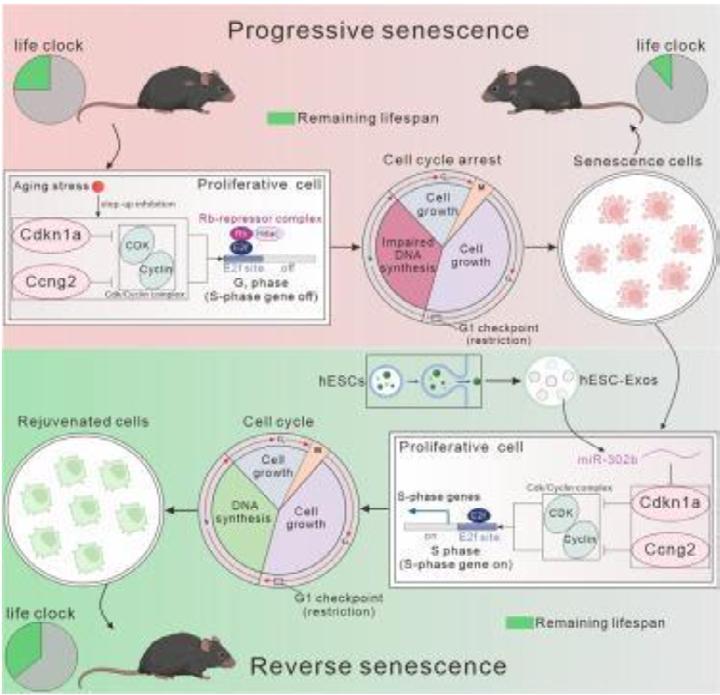
It does not happen that so many superstars in reproductive biology from all over Europe publish a paper together as was the case with the paper we are presenting here that appeared not too long ago in Cell 1 But this was not even the most interesting aspect of the paper. That, clearly, was the reported findings!
So, let’s get started: It is well known that many mammals can interrupt embryo development in a reversible way, and this usually happens at the blastocyst stage. In mice, this is achieved by decreasing the activity of the mTOR signaling pathway. It is unknown whether this ability is conserved in mammals in general and in humans in particular.
In this amazing paper the authors demonstrated that decreasing the activity of the mTOR signaling pathway induced human pluripotent stem cells (hPSCs) as well as blastoids (made from stem cell lines) to enter a dormant state with limited proliferation, developmental progression, and capacity to attach to endometrial cells. In other words, human blastoids under mTOR inhibition demonstrate a diapause-like response that has Graphic abstract of here discussed paper1 Bi et al., Cell Metabolism 2025;37(2):P527 -541
not been described in human preimplantation-stage embryos.
In this paper presented in vitro assays showed that around the blastocyst stage, similar to other species, the ability to enter dormancy is active in human cells and is reversible at both functional and molecular levels.
The theoretical possibility to pace human blastocyst development has, of course, quite amazing potential implications for IVF practice. Blastoids in such dormancy, for example, demonstrated altered developmental progression and attachment. Mouse and human cells, moreover, demonstrated species-specific metabolic profiles in dormancy.
REFERENCE
1. Iyer et al.,., Cell 2024;187:6566-6583
In another quite remarkable paper in Cell Metabolism , Chinese investigators demonstrated that human embryonic stem cell-derived exosomes (hESC-Exos) reversed senescence by restoring the proliferative capacity of SnCs in vitro.
IhESC-Exos treatment in aging mice remodeled the proliferative landscape of senescent cells, leading to rejuvenation, as evidenced by extended lifespan, improved physical performance, and reduced aging markers. miR302b enriched was identified in hESC-Exos that specifically targeted the cell cycle inhibitors Cdkn1a and Ccng2. miR-302b
treatment also reversed the proliferative arrest of senescent cells in vivo, resulting in rejuvenation without safety concerns over a 24-month observation period.
These results summarized in the graphic abstract from the paper below, demonstrate that exosomal miR-302b has the potential to reverse cellular senescence. This finding, of course, has major potential clinical significance if it can be reconfirmed in the human experience. It then could offer a promising approach to mitigate senescence-related pathologies as well as the aging process in general. And all of that is obviously applicable to the ovaries, at least theoretically!
REFERENCE
1. BI et al. Cell Metab 2025;37:1-5
As also discussed in the Pregnancy and Obstetrical Management section of this literature review, successful pregnancies rely heavily on the placenta’s complex and gene-regulatory networks. Their disruption leads to pregnancy complications and developmental defects.
The authors of here discussed paper 1 produced a spatial multiomic landscape of the human placenta at molecular resolution in an attempt to elucidate the molecular architecture of the first
trimester human placenta. Paired analyses unraveled intricate tumor-like gene expression and transcription factor motif programs potentially sustaining the placenta, as earlier discussed, in an in-principle hostile uterine environment, supporting the earlier mentioned notion that the placenta – in addition to its respiratory and nutritional functions, also serves as the immunological shield, allowing for tolerance of the fetus.
REFERENCE
1. Ounadjela JR, et al., Nat Med 2024;30:3495-3508



*Articles were originally published in the Reproductive Times .
Likely induced by the recent class action lawsuits filed in the U.S. and previously extensively discussed in these pages, TIME magazine on March 6, 2025, published a quite lengthy article on preimplantation genetic testing for aneuploidy (PGT-A), already in its title indicating that patients who utilized PGT-A in their IVF cycles now are claiming that the test made them discard embryos with potential for normal pregnancies and births. 1
Since the CHR has, of course, been on the forefront of criticizing the increasing utilization of PGT-A for over 20 years, and in the process has significantly contributed to repeatedly changing PGT-A-related practices in IVF, it is not surprising that TIME’s health correspondent who wrote the article interviewed Norbert Gleicher, MD , the CHR’s Medical Director and Chief Scientist, on the subject in gathering information. She then extensively quoted him after noting that “the chorus of PGT-A skeptics is getting louder,” though, “arguably no one so vocal as Dr. Norbert Gleicher.”
What she unfortunately did not point out is that the CHR’s educated opposition to chromosomal testing of embryos started already around 2006, when the whole world was still convinced that chromosomal testing of embryos would greatly improve IVF cycle outcomes. The CHR’s investigators then, based on a reanalysis of several French studies, concluded that (at least in older women) PGT-A likely was actually reducing pregnancy and live birth chances, a year later confirmed by Dutch colleagues in a by now quite legendary prospectively randomized study.
What the reporter also failed to note in her article was how pretty much all the proponents of PGT-A utilization she also extensively cited, have since come a long way in recognizing many of the shortcomings of PGT-A which they for years stringently had denied. They since, indeed,
for example started routinely transferring socalled “mosaic” embryos, after for many years automatically having discarded them in the thousands and accusing the CHR of acting “irresponsibly” after the CHR already in 2014 started transferring selectively by PGT-A as chromosomal abnormal signed out embryos and reporting in October of 2015 the first four healthy and chromosomal-normal pregnancies from such transfers in the world.
Though the reporter deserves kudos for in very understandable fashion presenting both sides of the still raging conflict surrounding PGT-A – as also demonstrated by the filed class action suits – it is a little difficult to understand how she, for example, would let a prominent proponent of PGT-A get away with the statement that “about 90% of patients opt in after receiving information about the test.”
They, of course, opt in if the information they receive is incomplete and biased in favor of PGT-A. And that the informed consents given to patients are often incomplete and biased we know here at the CHR as a fact because we hear from patients every day what they were told before signing up for PGT-A. And we are getting these insights when these same patients after failed IVF cycles with use of PGT-A then move their allegedly “abnormal” embryos to the CHR for potential transfers or, simply, choose to do another fresh IVF cycle at the CHR without use of PGT-A.
And here is another ridiculous claim from another prominent proponent of PGT-A, which went uncontested in the article, when he stated that PGT-A “is very powerful when done well,” but in his view “isn’t always done well.” Everybody in medicine, of course, knows that whenever in medicine somebody claims outcomes that only the claimant (and equally interested parties) can achieve, alarm bells should immediately go off because every last ounce of credibility in science, including medicine is, of course, based on reproducibility of results! But otherwise, a well-
presented and written article, worth the read!
That the controversy surrounding PGT-A finally is getting more attention is well demonstrated by the fact that almost at the same time as the abovediscussed article in TIME magazine, another less known but upcoming journal, TRUTHDIG , published an almost identical article on exactly the same subject and in some regards even more detailed. The writer was Amy Klein , who has shown a longstanding interest in reproductive medicine and also attended the 2024 Foundation for Reproductive Medicine Conference (FRMC), which the CHR cosponsored.
She, indeed, primarily quoted the same three experts as the TIME article, including the CHR’s Norbert Gleicher, MD , who very clearly restated his (and the CHR’s) longstanding opinion that PGT-A, except in rare occasions, really does not offer any outcome advantages in IVF. To the contrary, several subgroups
of patients may actually reduce their pregnancy and live birth chances by utilizing PGT-A in their IVF cycles, while spending significant additional money on an already a-priori very expensive IVF cycle.
When confronted by this fact and the recent ASRM/ SART Committee opinion about PGT-A, which clearly stated that PGT-A has been unable to demonstrate any outcome benefits for IVF whatsoever, the other two “experts” resorted automatically back to the same excuse proponents of PGT-A have been using over and over again for over 20 years of being false prophets, by claiming that those who reported no benefits from PGT-A simply don’t know how to do PGT-A right. And, as already noted before, whenever somebody in science (and medicine) claims to be the only one who can do something – and especially when the person has been making this claim for over 20 years – the only worthwhile response is a good laugh, though, coming from prominent “experts,” such a comment is, of course not really a joke but really bad taste!
1. Ducharme J. TIME. March 6, 2025. https://time. com/7264271/ivf-pgta-test-lawsuit/
2. Klein A. Truthdig. March 7, 2025. https://www.truthdig.


*“Since October 7th I have been two
BRIEFING: We are here reprinting with great pleasure and admiration a posting by Kara Goldman, MD, a mother, a RE, and an associate professor at the Feinberg School of Medicine of Northwestern University in Chicago. It first appeared on REIs for Israel and, in our opinion, is deserving of much wider distribution
*Article was originally published in the Reproductive Times .

Kara Goldman, MD
S ince October 7th I have been two different mothers: There’s the mother that I allow my children to see – the one who reassures my kids that good will prevail over evil. Who stifles her grief, so her kids maintain the weightless innocence of childhood. That’s the mom that was required of me today.
I stole glances at the Times of Israel website while waiting in line at a California theme park. I snapped pics of my sweet girls with Hello Kitty when I learned that 4 caskets were returned to Israel. I wept silently to myself while four blissfully unaware kids ate ice cream and skipped between rides.
When I learned later in the day that Shiri’s body was not with her sons’ murdered bodies, I was on a tram ride through Universal Studios with my own sweet baby boy napping on me with his little fist curled up by my neck. I couldn’t help but see the parallel between the haunting images of Shiri, Kfir, and Ariel in those final terrifying
moments before they were taken hostage. I read the news with terror, not understanding how this nightmare could get any worse. And yet— my kids needed lunch, and there was no time for grief because my kids deserve these rare moments of unencumbered joy.
Every moment since October 7th has been like this. My son is only a few months younger than Kfir, and I have seen the Bibas family every day in every moment of my own parenthood. The early mornings when my sweet boy wakes eagerly searching for snuggles and milk, the diaper changes when he thrashes around and giggles while I chase him down with wipes, the moments of uncontrollable tears that require patience and love. The milestones-- new teeth, first steps, first words. I couldn’t imagine how any of that would look in captivity, but I took the smallest amount of comfort thinking that Shiri was with her children and would rise to the insurmountable maternal tasks required of her. Now that we know their bodies weren’t together, this is a new depth of grief. For how long were those sweet innocent boys alone? Was she there to comfort them when they were being murdered? It’s unbearable.
Yes, since October 7th I have been two different mothers. The mother at Universal Studios today who wouldn’t dare let my daughters know that the ‘baby hostages’ they’ve worried about for 500 days are no longer with us. And there’s the mother who they don’t see--- the one who, in the quiet moments after all four are asleep, fears that the world is all too comfortable with the murder
of Jewish children.
There’s the version of me from October 6th, and the forever changed person since October 7th. But this— today marks a darker turning point in the evolution of Jews everywhere. A flicker of hope has been extinguished.
Tomorrow morning I’ll wake up early with the kids on our last day of vacation and actively work to build happy memories, and I’ll save the brokenmother version of myself for after they’ve gone to sleep.
And then on Monday, we’ll return them to school greeted by the usual site of multiple armed guards protecting the Jewish children and staff within. We will decide when and how to share with them the tragic news uncovered today, but until then we’ll protect whatever shred of innocence we can.
And we’ll pray that the world finally starts to care about the lives of Jewish children.
We are including a copy of this heartbreaking posting into the CHR VOICE barely two days after the world became aware of the unspeakable atrocities conducted by military forces loyal to the new Syrian fundamentalist Muslim government against Christians and Alawites. The excesses of Muslim fundamental extremism must be brought to an end!


BRIEFING: In response to his monthly A PIECE OF MY MIND article which first appeared in the January 2, 2025 Reproductive Times and a few weeks later in the January/February double-issue of the CHR VOICE with the title, “A probably too long and personal take on modern-day antisemitism in education, academia, science, and medicine,” the author and CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, received the below reprinted letter from a German colleague. It has been translated from German to English with an A.I. program by the CHR’s Director of Research and Clinical IVF, David Barad, MD, MS. We are very pleased to present the letter here, which Dr. Gleicher received on February 21, 2025.
*Articles were originally published in the Reproductive Times .
Dear Colleague Norbert Gleicher,
Please allow me to write to you in German and to respond so late to your article A Piece of My Mind from early January.
I was unsure whether a response from a German to your article would be welcome. However, the events of the past few days have compelled me to write to you.
What we are witnessing are horrifying, incomprehensible, and unspeakably cruel atrocities committed by Hamas, who have taken people hostage, treated them in inhumane ways, and brutally murdered them. When we see the images of how emaciated and mistreated the survivors of captivity look upon their release, when we read their reports of months of abuse, while at the same time noticing the good condition in which Arab criminals are released from Israeli prisons, there can be no doubt about who adheres to human standards in a lawful manner and who does not. It is a scandal that the inhumanity of Hamas is not more clearly called out by name.
Through their unimaginable cruelty in dealing with innocent people, including infants and young children, Hamas members have stripped themselves of their human dignity. Such individuals have forfeited their claim to be considered human.
We, who in our profession fight daily for the creation of new human life, can grasp the immense loss suffered by the father of Ariel and Kfir Bibas, as well as the loss to all of humanity through the ruthless and despicable murder of
these two innocent children and the subsequent desecration of their bodies.
I stand in shock before these acts of horror and before the fact that the government of my country wants to send these murderers and their accomplices in Hamas hundreds of millions of euros, -supposedly for humanitarian purposes, but in reality to further finance their gruesome and contemptuous acts. I am deeply ashamed and outraged by this and can only assure you that I will raise my voice against it.
Together with my Jewish friends here in Berlin, I sincerely hope that the Israeli hostages will return home as soon as possible, and that this entire Hamas nightmare will be brought to an end once and for all.
Dear colleague Gleicher, hoping that my message is not unwelcome to you, I sincerely wish you Shabbat Shalom and all the best.
Best regards,
Dr. Matthias Bloechle Berlin

EDITORIAL COMMENT: We, of course, cannot publish every comment we receive but could not resist publishing this letter. A big Thank You in the name of Dr. Gleicher and the whole Editorial Team to Dr. Bloechle in Germany. We, of course, especially appreciate receiving this letter from Germany, and not only for the obvious historical reasons but also because we, of course, are delighted that both of the CHR’s communication outlets, the VOICE and The Reproductive Times, are now reaching a growing public outside of the U.S.