












By Sònia Gayete Lafuente, MD, PhD,
who is a Founda tion for Reproductive
Medicine Research Fellow
at the CHR. She can be reached through the editorial office of the VOICE.
BRIEFING: In recent years, wearable technology has transformed the landscape of personal health and fitness management. Devices such as smartwatches, fitness bands, and sensor-enabled clothing are now commonplace, offering unprecedented access to real-time data on metrics like heart rate, activity levels, and sleep quality. These advancements shaped as fashionable smart accessories and jewelry have empowered users to monitor physiologic responses in different scenarios and take a more proactive approach to their health. In social settings where healthy lifestyle, wellness, and preventative selfcare have become popular, wearable devices have attracted great interest and demand and are partnering with luxury fashion houses and highest-end fitness clubs, while advertised by celebrities and social media influencers. But what’s the science behind it?


Beyond applications in general fitness, wearable devices are rapidly expanding into specialized health domains, including chronic disease management, mental health monitoring, and even early inflammatory disease detection. In fact, with advancements in their miniaturized sensors, wearables have moved from simple step counters to very sophisticated tools deemed capable of tracking complex processes such as ovarian cycles. In the fertility field, ovulation and menstrual cycle monitoring stand out as significant promising practical solutions for individuals as well as healthcare providers in gynecology. Their accuracy and reliability compared to standard methods are, however, still debatable. Therefore, this article aims to explore the current state of wearable devices in gynecology and fertility health and further aims to address the broader implications of integrating these technologies into personalized care.
applications
Wearable devices are being increasingly used to track various physiological parameters relevant to fertility health. Some of the key tools include:
(i) Basal Body Temperature (BBT) Tracking: monitoring BBT can help identify ovulation and, therefore, the so-called fertile window and, with it, chances of conception.
(ii) Menstrual Cycle Tracking: Wearable devices can also track menstrual cycles based on mathematical algorithms, including data from the user’s menstrual calendar and bleeding patterns, along with BBT. This information can be used to identify irregularities and help predict upcoming ovulations and, thereby, optimize fertility.
(iii) Direct and Indirect Hormone Level
Monitoring: Some wearable devices can infer hormone levels, such as estrogen and progesterone, which reflect ovarian function and play a crucial role in fertility and reproductive health.

in the U.S. that help track the fertile window by utilizing parameters like BBT or urinary hormone levels. These devices, worn on the wrist, fingers, intravaginally, or inside the ear, demonstrate high accuracy in detecting various stages of the menstrual cycle, including the luteal phase, fertile window (generally with an accepted error of +/- 1 to 1.5 days), and menstruation.


Progesterone and estrogen levels are indirectly inferred by monitoring physiological changes associated with hormonal fluctuations. The key surrogate parameters include: BBT (which increases slightly after ovulation in response to progesterone rise), heart rate and its variability (since estrogen and progesterone influence the autonomic nervous system, affecting these cardiac parameters during different menstrual phases), respiratory rate (given that progesterone can increase respiratory rate, which some wearables detect as a marker of luteal phase), and skin conductance or electrodermal activity (since sweat gland activity, indirectly measurable through skin conductance, may be influenced by estrogen). Studies suggest that devices incorporating direct hormone level measurements from urine sensors are often more accurate while remaining user-friendly.

Amongst the most reliable devices is the Ava Fertility Tracker (top photo). It is a bracelet worn during sleep which monitors multiple physiological signals to predict ovulation and to identify the fertile window, and was in 2021 the first to receive FDA 510(k) clearance, thereby becoming the first machine learning device approved to aid women in ovulation prediction. This was also followed that same year by the Ava bracelet, the popular Oura ring integrated with the Natural Cycle app (middle photo), also FDAapproved. Although the Oura ring is not in itself cleared by the FDA for fertility tracking, its integration with the approved birth control app Natural Cycles allows for enhanced fertility tracking capabilities. In fact, multiple commercial integrations of wearable devices have been recently launched with the aim of increasing the accuracy of fertility tracking, among those the Kegg plus Mira device (bottom photo), another popular example that combines data from cervical mucus impedance and urine hormone levels.
While wearable devices have shown significant promise in gynecology and fertility tracking, their reliability is still a crucial factor to consider. Several studies have evaluated the accuracy of wearable devices in tracking fertility-related parameters. A recent extensive narrative review identified 23 commercially available, nonprescription wearables
All of these devices represent significant progress in the use of digital non-invasive methods for fertility tracking. However, significant challenges remain. Research evaluating the accuracy and reliability of these technologies is limited, and the few available studies often lack standardized validations. Moreover, factors such as device calibration, user compliance, and individual variability among others can impact the accuracy of their measurements.

The market for technology aimed at tracking ovulation to support conception is rapidly expanding in the U.S., attracting the increasingly tech-smart reproductive-age female population. The milliondollar question for wearable fertility trackers is whether these devices could one day replace traditional cycle monitoring in Assisted Reproductive Technologies (ART). Imagine a system where realtime hormone levels, captured non-invasively by a patient’s wearable device, are seamlessly shared with healthcare providers through electronic medical records or patient platforms in real-time. This would allow the monitoring if intrauterine insemination or in vitro fertilization (IVF) cycles remotely, or would permit embryo transfer timing and/or other treatment adjustments without so frequent clinic visits. Such innovations are already hinted at by systems like Oova, which use at-home LH and progesterone urine tests (now integrated with a BBT-tracker bracelet) to send results via digital platforms.
Expanding on this concept, wearable devices might take remote cycle monitoring to the next level, offering continuous, non-invasive data collection that could revolutionize how fertility treatments are managed. However, realizing this vision will require significant advancements in technology. Moreover, the infertility field has seen already too many insufficient validations of new “add-ons” to infertility practice and must make sure through rigorous studies that this will not happen again here. In addition to the somewhat-limited reliability compared to direct blood hormone measurements, other practical challenges must also be overcome. For example, careful ethical considerations come up regarding privacy and security of digital health data. Finally, the high cost of many of these devices poses an accessibility barrier, highlighting the need for more cost-effective solutions to reach broader consumer access.
As the technology continues to evolve, we can expect to see more sophisticated devices that empower women with valuable insights into their reproductive health. For now, however, their use should be limited to the simplest stages. Expectations expressed by industry have been that wearable devices could help reduce healthcare costs by enabling women to track their fertility treatment
cycles remotely, thereby reducing the need for clinic visits and laboratory tests. Considering the history of reproductive medicine, we, however, remain skeptical because we are still waiting for an “add-on” to IVF that has lowered IVF costs. The opposite has, indeed, always been the case. Let’s see where the science takes us. For now, still only one cycle at a time!
Alzueta E, de Zambotti M, Javitz H, Dulai T, Albinni B, Simon KC, Sattari N, Zhang J, Shuster A, Mednick SC, Baker FC. Tracking Sleep, Temperature, Heart Rate, and Daily Symptoms Across the Menstrual Cycle with the Oura Ring in Healthy Women. Int J Womens Health. 2022 Apr 8;14:491503. doi: 10.2147/IJWH.S341917. PMID: 35422659; PMCID: PMC9005074.
Cromack SC, Walter JR. Consumer wearables and personal devices for tracking the fertile window. Am J Obstet Gynecol. 2024 Nov;231(5):516-523. doi: 10.1016/j.ajog.2024.05.028. Epub 2024 May 18. PMID: 38768799.
Goodale BM, Shilaih M, Falco L, Dammeier F, Hamvas G, Leeners B. Wearable Sensors Reveal Menses-Driven Changes in Physiology and Enable Prediction of the Fertile Window: Observational Study. J Med Internet Res. 2019 Apr 18;21(4):e13404. doi: 10.2196/13404. PMID: 30998226; PMCID: PMC6495289.
Lyzwinski L, Elgendi M, Menon C. Innovative Approaches to Menstruation and Fertility Tracking Using Wearable Reproductive Health Technology: Systematic Review. J Med Internet Res. 2024 Feb 15;26:e45139. doi: 10.2196/45139. PMID: 38358798; PMCID: PMC10905339.




By H. Duncan, M.F.A., a writer and copy editor of The VOICE
A recent article by Melissa Dahl in Slate painted a grim picture of the emotional and financial burden of extensive fertility treatments. The headline— “Who Does 11 Rounds of IVF? Me, Apparently”— almost says it all. One of the profiled couples said they initially intended to undergo just one round of in vitro fertilization regardless of outcome, only to find themselves still trying cycle after unsuccessful cycle three years later—and depleting their savings in the process.
IVF has become a beacon of hope for many individuals and couples facing infertility challenges. However, the financial implications of such treatments can be daunting and can contribute to the psychological strain of infertility, especially when the course of treatment takes longer than anticipated or planned for.
Understanding the costs involved and exploring available financing options is crucial for those considering fertility treatments in the United States. (This topic was explored in the September 2024 CHR VOICE in a piece about the ethical implications of the costliness of fertility care, particularly stemming from insufficient insurance coverage.) Fortunately, new financial programs are becoming available to make the pathway to parenthood possible.
The expenses associated with IVF can vary significantly based on factors such as geographic location, clinic reputation, and individual medical needs. On average, a single IVF cycle in the U.S. costs between $12,000 and $14,000, according to
Forbes. However, this base price often excludes additional necessary procedures and medications. When these are factored in, the total cost for one cycle typically ranges from $15,000 to $20,000.
It’s important to note that many patients require multiple cycles to achieve a successful pregnancy.
The Society for Assisted Reproductive Technology (SART) reported that the live-birth rate for the first cycle of IVF was just under 40% for women under 35 years old, a rate which decreases with the mother’s advancing age.
Consequently, the cumulative costs can escalate, making financial planning essential.
Insurance coverage for fertility treatments in the U.S. is limited and varies by state; many patients find themselves bearing a significant portion of the costs out-of-pocket. Given the substantial expenses, many patients seek alternative financing options to manage the costs of fertility treatments. Some of the avenues available include:
‣ Personal Savings and Loans: Utilizing personal savings is a common approach, though it may deplete resources intended for other purposes. Alternatively, some individuals opt for personal loans, which can offer immediate funds but come with interest obligations.
‣ Credit Cards: While convenient, using credit cards to finance fertility treatments can lead to high-interest debt if not managed carefully.
‣ Clinic Payment Plans: Many fertility clinics offer in-house payment plans or packages that allow patients to spread out payments

over time. It’s advisable to inquire directly with clinics about such options.
‣ Specialized Fertility Financing Programs: Dedicated financing programs are designed to assist patients in managing the costs of fertility treatments. These programs often provide more favorable terms tailored to medical expenses.
Recognizing the financial challenges associated with fertility treatments, the Center for Human Reproduction (CHR) in New York City has partnered with PatientFi to offer a compassionate financing solution. PatientFi is committed to making fertility care more accessible by providing friendly monthly payment plans. Their approach considers the whole patient, not just credit scores, allowing for higher approval rates and more substantial financing amounts. With no hidden fees, PatientFi approves funding up to $50,000.
Key features of PatientFi include:
‣ Soft Credit Check: Patients can review their financing offers without impacting their credit scores, ensuring a stress-free application process.
‣ Instant Access to Funds: Upon approval, patients receive immediate access to funds, enabling them to commence treatment without delay—something especially important to older patients for whom time is of the essence.
‣ Flexible Usage: Financing can be utilized across various services, including clinic procedures and associated pharmacy costs, providing comprehensive support throughout the fertility journey.
By collaborating with PatientFi, the CHR aims to alleviate the financial burdens of fertility treatments, empowering patients to pursue their dreams of building a family with confidence and financial peace of mind.
In addition to financing through PatientFi, CHR is proud to offer income-based discount programs as well as discounts for active-duty military families. CHR also offers a unique, costeffective multiple IVF cycle program to women with diminished ovarian reserve (DOR) who will likely require more than one IVF cycle to achieve pregnancy.
Reading List
Dahl, M. Slate. https://slate.com/technology/2025/01/ivfinfertility-insurance-parenthood-debt.html
Kulkarni, Y. The CHR VOICE. https://centerforhumanreprod. com/the-chr-voice-newsletter/september-2024
Conrad, M. Forbes. https://www.forbes.com/health/ womens-health/how-much-does-ivf-cost/?utm_ source=chatgpt.com
https://www.sartcorsonline.com/rptCSR_PublicMultYear. aspx?reportingYear=2020&utm_source=chatgpt.com https://patientfi.com/fertility/patient/
https://centerforhumanreprod.com/discount-ivf-programs https://centerforhumanreprod.com/multiple-ivf-cycleprogram
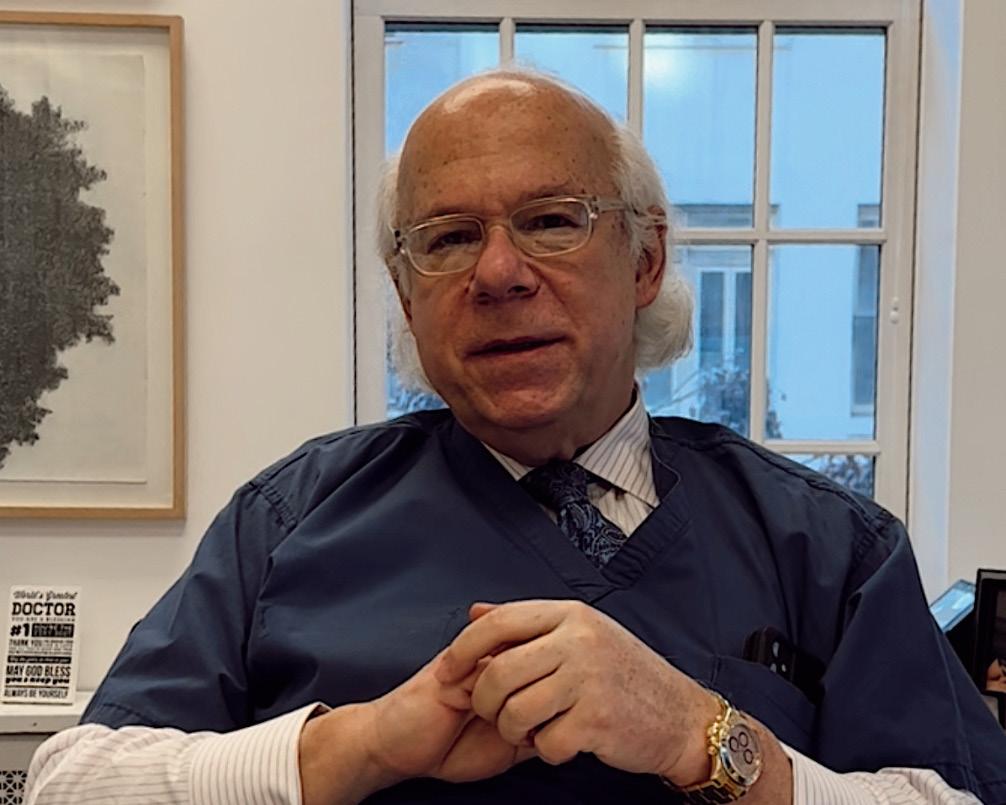
By Norbert Gleicher, MD, Medical Director and Chief Scientist at The Center for Human Reproduction in New York City. He can be contacted though the VOICE
or directly at either
ngleicher@thechr.com or ngleicher@rockefeller.edu.
As I write this during the few remaining days of a year which has been one of my life’s most challenging, I find myself more introspective than in prior years, when looking forward to the New Year. Most traumatic occurrences are at least to a degree foreseeable and, therefore, at least subconsciously somewhat expected, while others—fortunately rarer—will hit you like a lightning strike, leaving you simply overwhelmed. No worry; I will not bore you with the little stuff. This article is about the lightning strike that affected every fiber in my body and—if you don’t know it yet from the subtitle of this essay—it was the eruption of vile and very open antisemitism all around the globe, including in this country. Though personally basically agnostic for most of my life, antisemitism has, nevertheless, a very special relevance for me, because its extreme, the Holocaust, robbed me of my very large family (my father had 11 older siblings, my mother had only one sister, the only survivor of both sides of the family besides my then -still unmarried parents). I, therefore, never had the opportunity to have grandparents or aunts, uncles or cousins, as all perished in Nazi Germany’s gas chambers. And then, as fate wanted it, I ended up growing up as a young Jew in post-WWII Vienna, Austria, of course, a very central place for the development of European antisemitism and, ultimately German Nazism (more on that below). That this past year’s experiences were explosive is, therefore, an understatement. They changed what I have been reading, what I have been watching nightly into the early morning hours on TV, and, for the first time in my life, they turned me into an Internet junky. Of course, they also affected my political thinking and, probably worst of all, made me fearful of the future—not for myself, but for my children and children’s children. All of this introspection, of course, also engulfed my professional life and ultimately led to this article, which to a degree, therefore, is personal but—because I am a physician-scientist—also extends its tentacles into education, science, academia and, of course, the practice of medicine.
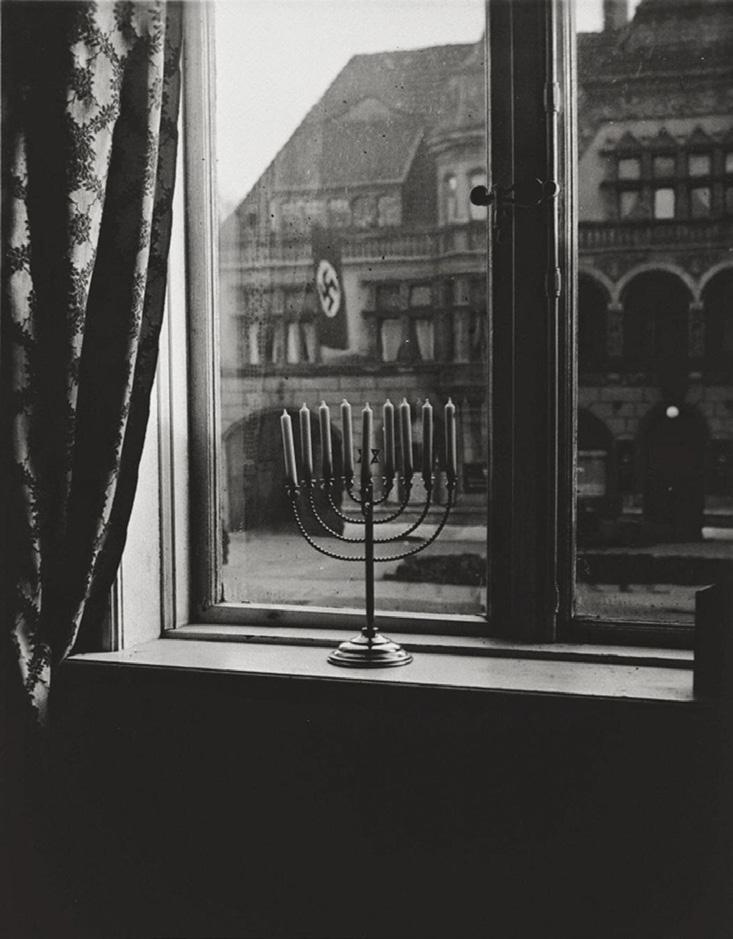
It is just a few days before Christmas and Chanukah, and I am in my office starting a first draft of this article. For so many different reasons, 2024 has been a really unusual year. Even the dates of Christmas and Chanukah this year are unusual. Because of the differences between the Georgian and Jewish calendars, there usually are days, sometimes even weeks, between these two holidays of light; but not so this year since Chanukah begins at sundown on Christmas Day, December 25.
One in this rare concurrence can see symbolically the obvious interdependence between Christianity and Judaism, considering that—in historical terms—Christianity started as a Jewish sect during the 1st century AD, with its founder and initial followers mostly being Jewish (for more detail, consider the following references: 1,2). Opinions still differ on how long it took for the two religions to separate: Some scholars argue that the process started by the end of the 1st century; others
believe that the separation occurred gradually, starting in the middle of the 2nd century; and yet others argue that the separation only occurred in the 4th century, when in the year 380 Christianity became the state religion of the Roman Empire.
Historically, however, undisputed is that this 4th century was also the beginning of antisemitism, witnessed by the first recorded persecutions of “Jewish Christians” by “Nicene Christians,” with the former having to seek refuge outside of the Roman Empire. Suffice it to say, Christianity and Judaism did not do well together over the following centuries, with Christianity often at the core of not only what nowadays would be called antisemitism, but of forced religious conversions of Jews to Christianity, expulsions of Jews from many countries (during different time periods from Spain, Portugal, and England, etc.), and outright ethnic cleansing (during inquisitions in Spain, Portugal, Mexico, etc.).
And it all, of course, peaked in the 20th century in the Holocaust against Jews, committed by an in principle Christian nation—Germany—with mostly silence from the rest of the Christian world, including the Vatican. German primacy in the Holocaust was historically so overwhelming that it diverted history’s attention away from smaller culprits, such as Austria, Hungary, Ukraine, the Soviet Union under Stalin, as well as other nations which to different degrees collaborated with Nazi Germany and/or pursued their own antisemitic annihilations, like Stalin’s Russia.
And this is the point where this article becomes personal because, as the first child of a young couple of Holocaust survivors in Poland (their miraculous survival during the Holocaust and equally miraculous reunification after the war was subject of a book published in 20183), I was only one year old when my parents concluded that Jews were not safe under the newly established Communist regime in Poland and decided to emigrate to what was then the brand-new state of Israel in 1949. As will be obvious considering the historical circumstances of the time (Israel, against all odds, had won its first war against all of its neighbors’ combined Arab armies), to make this journey must have been a difficult decision for my parents, considering that in those years Israel basically was mostly only desert and had no infrastructure to speak of. To illustrate why the recently—especially in academia— widely heard argument that anti-Zionism cannot be equated with antisemitism is wrong, I will later return to my parents’ decision “to make Aliah” (the term Jews use emphasize their return to Israel, what is for them the Holy Land).
The track to Israel for Europe’s Holocaust survivors in those days led through certain key cities, from where the Jewish Agency then organized travel to Israel. For our young family of three, it meant that we had to make it to Vienna, Austria, then still (like Germany) occupied by the “four powers” of the post WWII period, the U.S., Russia, the U.K., and France. But as we made it successfully to Vienna, all the planning went to waste because my mother fell seriously ill, preventing the family from continuing the journey to Israel as planned.
Basically penniless, with the only valuable private property being two huge glass containers of “schmaltz,” which my parents for months considered their primary sustenance (I allegedly was more privileged), my father—while my mother was recovering—had to find a way to generate some income. By the time she had fully recovered, he successfully had developed a small import-export business between the four occupied sectors of the city of Vienna (with each of the four powers being responsible for one of the sectors, there were real border checks between them if one wanted to pass from one sector into another). And as a consequence, we never got back on the track “to make Aliah” and, paradoxically, Vienna— the city where Adolf Hitler had spent important formative years of his younger life before moving to Germany— consequently, became the city where I ended up growing up, went to school, and started my medical studies at the city’s once world-renowned and, after Bologna in Italy, secondoldest medical school in the world. Though only 22 years later, I, however, at least symbolically completed my family’s return to Israel when I switched my medical school studies from Vienna to Tel-Aviv University in Israel, where I graduated in 1973.
Being Jewish in Vienna in those post-WWII years was an “interesting” experience: A first reason was, of course, the country’s and especially the city’s past history as the capital of one of the big European empires,- the Austrian Hungarian Habsburg monarchy. And while Vienna in the days up to WWI was one of the world’s principal cultural as well as medical capitals, the monarchy was also, after Napoleon’s emancipation of French Jewry in 1791, the second empire to fully emancipate its Jewry in 1867 under Emperor Franz Joseph I (of Sissi movies’ fame). And even though—and maybe exactly because—Vienna at that time housed a rapidly growing and increasingly prosperous Jewish population (the medical faculty at the university was, for example, to a very significant degree Jewish and Vienna’s cultural and economic life had lots of very prominent Jewish representatives), the city also became the breeding ground for a rabid and very typical form of Viennese antisemitism.
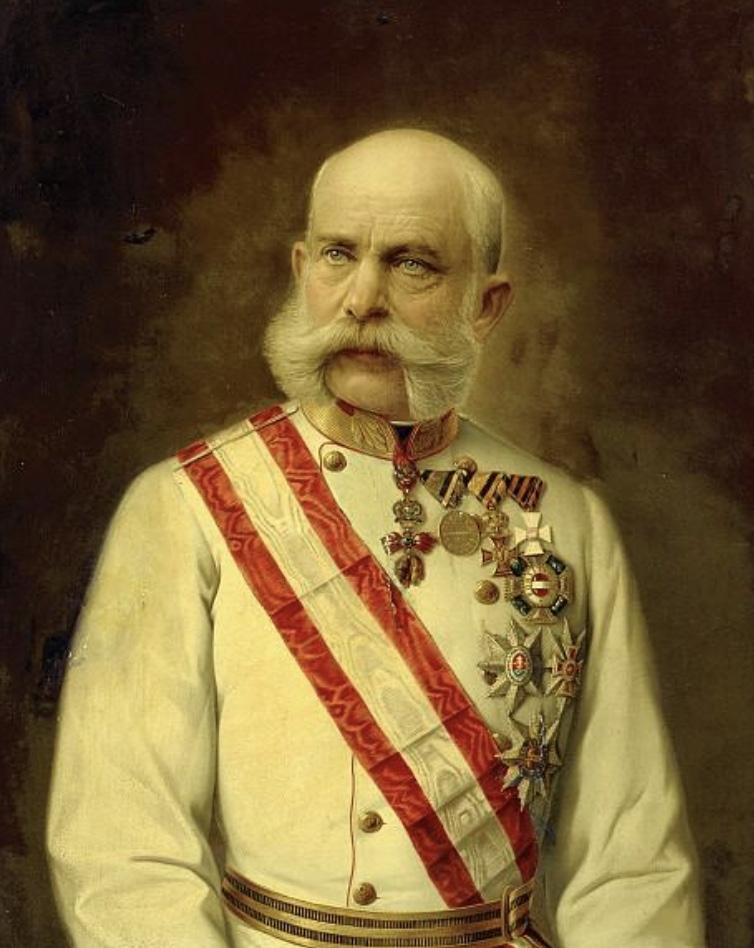
A painting of Franz Josef I, Emperor of Austria and King of Hungary (1848-1916)
Its likely most prominent practitioner was the city’s Mayor between 1897 and 1910, Karl Lueger, a lawyer-politician who was well known for his rabid antisemitism. The following is a good example from a Lueger speech, given at meeting of the Christian Socialist Workers’ Association held on 20 July 1899 in Vienna:
“Here in our Austrian fatherland the situation is such that the Jews have seized a degree of influence which exceeds their number and importance. (Interjection: ‘Very true!’) In Vienna the poor craftsman has to go begging on Saturday afternoon, to turn the labor of his hands to account, he has to beg at the Jewish furniture dealer’s. (‘Quite right!’) The influence on the masses, in our country, is in the hands of the Jews, the greater part of the press is in their hands, by far the largest part of all capital and, in particular, high finance, is in Jewish hands, and in this respect the Jews operate a terrorism of a kind that could hardly be worse. For us, in Austria, it is a matter of liberating Christian people from the hegemony of Jewry.”
It also speaks for itself that he is most remembered not for having been the mayor who transformed Vienna into a modern city, but for one sentence he uttered in response to a reporter’s question, how come he had chosen (a very attractive and very wealthy) Jewish woman for the opening dance at one of Vienna’s famous balls. His answer was, “who is a Jew is mine to say!”

Karl Lueger who
city
Gustav Mahler, and many other cultural authorities.4
Some historians concluded that Lueger’s antisemitism influenced Adolf Hitler who in 1908 had moved from a small Austrian village called Braunau to Vienna to pursue a career as a painter. He later mentioned in his infamous book manifesto, “Mein Kampf,” how impressed he was by the mayor’s charisma and popular appeal. On another occasion, he described him as “the greatest German city mayor ever” (Hitler, of course, considered his home country, Austria, to be an integral part of the German Reich). Some historians believe that Hitler attributed much of Lueger’s popularity to his antisemitism and from this concluded that one could build a political career on antisemitism.
It, therefore, probably does not surprise that a monument to Karl Lueger on the Dr. Karl Lueger Platz in the center of the city of Vienna (its 1st district) has remained controversial. After exploring varying options, the city decided—as CNN recently reported—to keep the bronze statue of the mayor in its prominent place, though with a rather small but symbolic change: Proposed by the Viennese contemporary artist Klemens Wihlidal, the statute would be mildly tilted by 3.5 degrees to the right, as he did not wish to change the monument, but “the view and perspective of it.”5

The proposed modified statue of Karl Lueger at a tilt ….
According to the artist, it was meant to cause “an irritation, or even more, a moment of insecurity, which only become
perceptible upon a second look, reminiscent of a sinking ship and evoking the feeling of transience and impermanence, as if one had to watch the monument about to topple over or at least expect that it won’t stand for much longer.”
I am retelling the story of the statue because it is symbolic of the Viennese antisemitism I grew up with in my younger years. You always felt that it was there; but it only rarely reached the surface. In my own experience, when it lifted its ugly head, it usually happened in the school system. I recall discussing the subject repeatedly with my (Catholic) girlfriend who—unsurprisingly—never was cognizant of its presence and, therefore, was convinced I was over-sensitive in my perceptions. That is, until one of our closest friends confided to her “that he really never understood how she could date a Jewish boy like me for so long.”
What has happened to this statute is so symbolic for the Viennese Zeitgeist because the city’s intent to reflect its “unhappiness” about Lueger’s antisemitism was met by Wihlidal’s proposal, though without necessarily offending those who opposed more stringent rejections, like moving the statue to a less prominent location or placing it into a museum. In that sense this Viennese debate was not different from what we have been experiencing in the U.S. in recent years regarding statues of prominent Americans accused of having been slave owners. Seeing such statutes more as historical artifacts and art pieces rather than personal expressions of admiration, I in general oppose their removal (unless, of course, they become target for symbolic pilgrimages); but this is not where the story ends.
It ends by offering a perfect example of what all over the world is called the Viennese “Lebsenskunst” (translated as “art-ofliving”), which now for many consecutive years has made Vienna, based on surveys, the most “livable” city in Europe. As Britannica noted:6
Viennese “Lebenskunst” survived over history, allowing for life in Vienna at almost the same pace and style as a century ago. The same concerts are given in the same rebuilt concert halls, and a theatrical or operatic success still stimulates lively conversation. One can drink the same sourish local wines in the taverns on the outskirts of town called Heurige, consume the same mountains of whipped cream at Sacher’s and Demel’s, and sample the same varieties of coffee drinks in countless cafés. And it is exactly this “Lebenskunst” which, still, has Lueger’s statute staying fully upright in its original location, with – according to CNN – nobody at the city being able to say when the tilt may be installed (see below).5

…. and in current reality
The same sense of subterranean antisemitism I had experienced growing up in Vienna did not seem to exist in the U.S.. There, of course, were intermittently antisemitic incidents reported in the media, but the perpetrators were usually very obvious cuckoo—in need of psychiatric treatments or—at times—selected members of the Black Muslim community. But my subconscious antisemitism sensors reactivated when, upon our return to NYC from Chicago, my younger daughter was accepted to one of New York’s most privileged (and expensive) private high schools.
I initially could not point out where my internal disquiet was coming from, but I quickly recognized that my own experience with the Viennese school system was the obvious trigger, as I increasingly perceived a change in how my daughter was educated, best described as a rapidly increasing switch from education to what seemed to me more like indoctrination. In retrospect, I should have noted these changes in the country’s education system already earlier when my two daughters – several years apart – attended a highly regarded private Jewish day and middle school in Chicago. Though political indoctrination was not as apparent there as later in abovenoted NYC high school, what was already very much apparent was a clearly ideologic rather than scientific commitment of the school to medically intervene in the well-being of my children, even if I disagreed.
It happened when my older daughter allegedly tested positive for a minor learning disability on a mandated school test, administered without parental preapproval. The recommended response to the result by the school was to start my daughter on medical treatment (yes, with prescription drugs!).
When I refused to sign the relevant consent forms, arguing that my daughter was too young for these medications and that I did not want to sentence her for life to dependency on these drugs, the stigma of a learning disability, and the
possible consequence of lifelong “victimhood,” I became an “enemy” for the school administration. Rumor had it that administrators were even discussing whether to report me to the authorities for child abuse.
Luckily, mostly because I was a physician, I was able to withstand this (let’s assume well-meaning) encroachment on parental authority. One, however, can imagine how much more difficult it must have been for other parents. As I later learned, at one point almost two-thirds of my daughter’s classmates had been classified as learning-disabled and a majority among those had been placed on psychotropic medications. My daughter, fortunately, was given the opportunity to learn to overcome her alleged shortcomings and successfully completed graduate school.
As my daughter’s class experience so well demonstrated, diagnostic tests have the function of identifying outliers from the norm; but as often applied, these tests are frequently used to identify extremes on normal distribution spectrums. Biology has taught us the evolutionary wisdom and absolute necessity of such spectrums which, often, are the basis for normal physiological functions through redundancies, even if abnormalities exist. In other words, we exist because our existence is not based on perfection, but on our bodies’ ability to overcome imperfection through redundancies. And – as in my daughter’s case – by putting our children on too many medications, we practically prevent them from learning how to circumvent their imperfections. As a consequence, the U.S. has become the most overmedicated nation in the world.
Unfortunately, the medical field does not seem to have sufficiently acknowledged this fact yet, but – interestingly after the COVID-19 experience – the political process has started to pay attention. However, it would be rather unbecoming for medicine as well as society as a whole if, because medicine cannot sufficiently self-regulate, medical practice became dictated by politics. And the overmedication of society is not the only warning sign. Another subject where the medical field has failed to self-regulate, resulting already in highly targeted government interventions in almost all European countries (and probably soon under the incoming Trump administration also in the U.S.) has recently been genderaffirming care in children and young adults, which has been subject of discussion repeatedly in these pages. And, as also repeatedly discussed in these pages before, the infertility field, of course, also does not lack practice patterns where medical self-regulation has failed and government interventions will become unavoidable if medicine does not learn to do better.
In short, a compromised education system is always a forerunner of societal crises – and, if the last year has demonstrated one thing beyond any reasonable doubt,
the U.S. education system from kindergarten to colleges and universities is in the midst of an educational crisis, in its intensity not matched by anything seen since the end of WWII. And since our medical schools and law schools are in crisis, unsurprisingly medicine and the practice of law are in crisis. In short, the country is in crisis, and the expression of antisemitism in society is by historians widely appreciated as a canary in the coalmine.
You at this point likely understand what the educational experiences of my two daughters may have to do with antisemitism which, of course, since October 7, 2023, has seemingly exploded in the U.S., in Canada, Australia, New Zealand and all over Europe. To summarize in a very Jewish way, they have everything and nothing to do with the recent surfacing of worldwide antisemitism, depending on where you look
As already noted, one very obvious link is the seemingly completely out of control educational system that at times appears closer to how Hamas and Hezbollah indoctrinate their children than how liberal democracies are supposed to educate children. And the worst indoctrination, of course, occurs in our colleges, with our most famous colleges and universities consciously actually having been driving this outrage.
A second and not less paradoxical link is the increasing presence of radical Muslim populations in the Western world (including the U.S. and Canada) who left their countries of origin for a better life in the West and – once here – refuse to integrate into Western society. Instead, they are attempting to turn Western society into the same kind of destructive environment they or their parents fled in the first place. Though these groups have existed in Western societies for decades, they in more recent years greatly increased in numbers, whether through legal or illegal immigration. They consequently have also become more visible, more outspoken, and more demanding. Since October 7, 2023, they, moreover, have also led the massive pro-Palestinian demonstrations all over the world, including in the U.S., which, of course, frequently have vile antisemitic overtones – even if they claim to be only anti-Zionists and not antisemites.
How ridiculous a statement that is, can be well demonstrated by my family’s history: After my parents’ decision to flee Communist Poland when I was one year old, our Jewish ancestral home in Israel, despite its chaotic conditions at the time, was really their only option (I noted before that I would return to this subject). The connection to our ancestral Jewish home that almost every practicing Jew for all her/his life
constantly feels is best demonstrated by one sentence every Jewish community in the world – from Europe, the Americas, Australia, Asia, and even Africa– daily expresses in prayer and in common language. This sentence is - and has been for thousands of years – ask any Jew in the world – “next year in Jerusalem!” and has been at the core of the Jewish people’s survival over thousands of years of diaspora, even though most of the people lived as tiny and persecuted minorities all over the world.
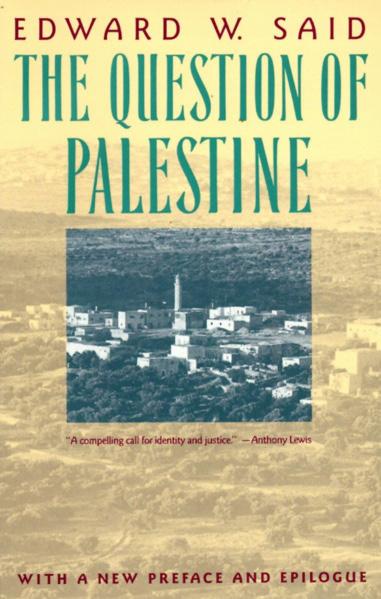
Though the term colonialism in conjunction with Israel’s founding even circulated among early Zionists prior to the creation of the state of Israel, if one person can be tagged as the original academic source in more contemporary times for mislabeling Israel as a colonial project, it was Prof. Edward Wadie Said (1935-2003), described by Wikipedia as a Palestinian American academic at (where else?) Columbia University in NYC. He can be viewed, since the founding of Fatah as a political movement in 1959 and as a political fraction in the Palestine Liberation Organization (PLO) in 1964, as the principal theoretician and ideologue of Yasir Arafat’s (1929, Cairo – 2004, Paris, France) PLO. A professor of literature, Said is also widely considered a founder of the fields of so-called postcolonial and Middle Eastern studies.
Though Said has been widely described as of Palestinian American background, one at this point also must note that a Palestinian state – or for that matter any other societal structure described as “Palestinian” never before in history had existed in the Middle East. Yasir Arafat one day in 1964, allegedly enticed by the Soviet Union, just made it up, claiming to represent this newly presented people/nation through the PLO.
In establishing the PLO, he presented himself as the son of a never existent state of Palestine based on a false claim to have been born in Palestine (he was really born in Egypt to Egyptian-Arab parents). The PLO and Arafat, moreover, from the beginning claimed that their alleged Palestinian state reached “from the river (Jordan) to the sea (Mediterranean),” thereby – from 1964 on – disputing the right of Israel to exist.
Arabs living in this area until then never identified as Palestinian but simply described themselves as Arabs. As we all have witnessed since October 7 of last year, the slogan “from the river to the sea” now has become the anthem of pro-Palestinian supporters, even though it has no historical backing, contradicts original U.N. resolutions that led to the creation of the state of Israel in 1948, and denies the Jewish people their right to their ancestral homeland. How else can one describe such a denial after thousands of years of exile and discrimination but as institutional antisemitism.

And it is, therefore, also no coincidence that the uproar on college and university campuses after the October 7, 2023, atrocities committed by Hamas in Israel, started at Columbia University in NYC. This university has singlehandedly over decades promoted the Palestinian statehood myth by training faculties all around the country (and the world), like several other leading universities (Harvard, University of Pennsylvania, etc.) to a significant degree financed by Muslim countries, like Qatar.

While the uninterrupted Jewish presence and history in these lands – as noted above – is well documented for thousands of years, Said and a small initial group of other academics of often Middle Eastern and Arab background succeeded in planting the seeds for a never before existing historical Palestinian people with a right to their own ancestral home of Palestine (he, therefore, described himself as Palestinian) and led the academics efforts in defining Jews returning to their ancestral homeland as colonizers.
Initially not more than an underground academic fringe movement, the concept caught on in academia in a coalition with the political left (Arafat is by many historians considered to have started his career as a paid agent of the Soviet Union), and has grown dramatically over the decades, as Israel progressively became a highly successful country. While in 1963, at the beginning of the Six Day War, still seen as the
weaker party (an impression that quickly started to fade after the decisive Israeli victory), Israel -with increasing economic success – became the suppressor of Palestinians, ignoring the fact that the Palestinian leadership repeatedly rejected offered peace deals proposed by U.S. presidents Carter, Clinton, and Trump. An alliance with the left, therefore, was for Palestinian supporters a logical evolution, even though Israel until 1963 was still widely considered a socialist state.
But that has since dramatically changed, as mainstream academia now presents an until recently never existing alleged Palestinian people as the victim of an increasingly dominant colonial Israel. And here is another interesting analogy: Like the surprising sympathy expressed in certain mostly leftist circles toward the recent coldblooded murderer of the CEO of United Healthcare on the streets of NYC by often highly educated students and some of their professors, more or less the same circles of actors also expressed sympathy and often outright support for the atrocities committed by Hamas on October 7, 2023. Both of these upside-down value judgments demonstrates how badly our Western education system has been performing over several decades. Only relatively few years ago, one could have assumed that most of our smarter students would conclude that planned political assassinations of CEOs and the sadistic rape, murder, and live-burning of women, men, babies, and children are despicable and inexcusable acts against humanity. Nowadays they are often, however, applauded at our college and university campuses by students as well as faculty.
Dogmas, however, work only in ideologies and religions (and even there not very convincingly). They certainly don’t work in politics and state craft, and they most certainly have no place at any level in education, from kindergarten to graduate degrees.
What we have witnessed in the streets of the U.S., Canada, New Zealand, Australia, and all over Europe may have been financed by Qatar and similar sources but it was bred over decades in our colleges and universities. The initial purpose may not have been to generate antisemitism, but original purposes in revolutions almost typically are quickly replaced, as revolutions tend to “eat their children” (Jacques Mallet du Pan, 1749-1800). The antisemitism we have witnessed over the last year on innumerable prominent campuses like Columbia, Harvard, UCLA in the U.S. and, of course elsewhere as well, like at Oxford University in the UK), would have been unthinkable only 10 years ago. It must become unthinkable again!
And how the world – including the U.S. - reacted
The shock of October 7, 2023, affected me in several waves, from the unimaginable inhumanity of Hamas murderers who not only slaughtered innocent babies, children, women, and men in Israel’s southern communities but often, first, sexually abused them, tortured them, and then burned them alive, to the failure of Israel’s security systems to warn the nation ahead of the Hamas attack, and finally, to the unimaginable failure of the Israeli army, which since has performed miraculously well, to respond for hours and hours to the Hamas attack. All three of these shocks, however, were even exceeded by how the world reacted to the events of October 7, 2023. Space here does not allow for a detailed review but there is room for a few key points: And so did practically all major international women’s organizations. Contrast this with how outspoke they usually are when women get raped and/or killed, - as long as it does not involve Jewish victims, of course.
I. In the U.S., Barack and Michelle Obama remained mum. Contrast this, for example, to Michelle’s campaign for the abducted Nigerian school girls several years earlier.
II. And so did practically all major international women’s organizations. Contrast this with how outspoke they usually are when women get raped and/or killed, as long as it does not involve Jewish victims, of course.
III. The International Red Cross did not even make attempts at visiting the Israeli hostages held in Gaza and/or express concern about their general or medical well-being. Contrast that to the constant comments by the Red Cross about alleged atrocities of the Israeli military forces in Gaza and of the Israeli prison system, to both of which the Red Cross has full access.
IV. The International Criminal Court in the Hague issued arrest warrants for Israel’s Prime Minister and Secretary of Defense alleging war crimes. Contrast this to the lack of any action against too many countries producing routinely atrocities which are, moreover, run by lists of murderous dictators too long to cite here (one mass grave just discovered in ex-President Asad’s Syria alone contained over 100,000 bodies).
V. And then there is, of course, the United Nations (UN), and what can one say about an organization originally created to maintain peace in the world, which now – and not for the first time – has a blatantly antisemitic Secretary General in António Guterres, the ninth person in this position. Of course, there were other antisemites before him in this position, among those Dag Hjalmar Agne Carl Hammarskjöld , the UN’s 2nd General Secretary, and , of
course, Austrias’ Kurt Waldheim, a former SS-officer in The Third Reich, and later President of Austria who – in full disclosure – awarded me the country’s Highest Honor in Arts and Science. The UN in its history issued more than twice as many condemnations of Israel’s conduct than of the conduct of all other member states combined, has an agency called UNWRA which not only indoctrinates Palestinian children in its school system in Hamas doctrines but whose employees openly participated in the atrocities of October 7, 2023. And now the U.N., as the employer of these murderous sadists, argues in U.S. court that – as employees of the UN– they enjoy diplomatic immunity from prosecution for the crimes they committed on October 7, 2023. Can you believe that?
Considering that all of this represents only a miniscule example of how obviously biased much of the world reacted to the events of October 7, 2023, one is only left with a single very obvious and very regrettable conclusion: The world has not changed; a highly significant degree of hatred against the Jewish people has been maintained even after the Holocaust. The events of October just brought this hatred to the surface.
But there is also good news: At least in most Western countries, anti-Semites are only a relatively small minority and populations in most Western countries (if one excludes the Muslim populations in those countries) and in a majority support Israel against Hamas and Hezbollah, in the U.S., for example, based on several polls, always almost 80%. But there are exceptions in traditionally antisemitic Ireland and Slovakia (you may want to read up on these countries’ respective histories during WWII).
But the picture is, of course, very different at college and university campuses, and not only among students but also among faculty. The columnist and lawyer Nils A Haug from the Gatestone Institute, recently noted in an article with the provocative title, “Rebottled Jew-hate: The boycott of Jewish genius,” that “there is a systemic and widespread global agenda to erase Jewish influence in academia, science, technology, and culture.”7 As the article suggested, after October 7, 2023, a sort of quiet boycott of Israeli researchers has begun as never before has been seen. It is reflected in cancellations of invitations to medical conferences, rejections of articles by medical journals, and refusal to grant Israeli projects.
If true – and not difficult to believe considering the various formal boycott proposals made by students and faculty at various colleges and universities against Israel – this would, of course, be not only antisemitic but pure racist. The author furthermore noted that these attempts of boycotting Israel are systemic and indicative of a global agenda to erase Jewish
influence in academia, science, technology, and culture, for me reminiscent of what happened in the city of my childhood, Vienna, as antisemitism steadily increased with increasing Jewish influence in the last stages of the Austrian-Hungarian Empire and – in a much shrunk country – between the two world wars, leading to the acceptance of Nazism after the Anschluss to the German Reich (see also below).
Haug made similar associations by suggesting that these activities reflect deep-seated Jew-hatred (he interestingly does not use the word antisemitism) within various Western societies, for the longest time “concealed within a façade of tolerance and social niceties,” while then quoting Steven Spielberg as saying that “antisemitism is no longer lurking, but standing proud,” – as it did during the 1930s in Austria and Germany. He also quoted in the article well-known investigative journalist and columnist, Daniel Greenfield, as saying, it’s not about Israel but has everything to do with the Jews (i.e., cultural and academic ostracization is simply rebottled Jew Hate).
At my alma mater, the medical school in Vienna, dismissal from their positions of the heavily Jewish faculty after the Anschluss (incorporation of Austria into Hitler’s German Reich) in March of 1938 resulted in the end of the university’s scientific and medical prominence in the world. Those countries and institutions currently driving away their Jewish faculties will come to regret it, like the city of Vienna came to regret the loss of its Jewish physicians, lawyers, artists, scientists, writers, composers, architects, etc. Almost 100 years later, the city still has not recovered from the losses of the 1930s.
In the U.S., Congress appears to have not only recognized the problem but successfully traced it to the education system, especially, however, colleges and universities, As Dion J. Pierre in a recent article in The Allgemeiner noted, a recent U.S. House report on the subject condemned universities for their insufficient response to rising antisemitism.8 Unfortunately, it appears that mostly only the Republican side of the House considers these issues in academia as really problematic. Especially the left wing of the Democrat party appears increasingly contaminated by developments like the UK’s Labor Party experienced already several years ago, when – especially the party’s left wing including the party’s then leader himself – demonstrated blatant and basically irrefutable antisemitism (a term I still prefer over Jew-hate).
What, as The New York Sun recently pointed out, is, however, especially painful regarding the Democrats’ left wing’s antisemitism, is that Chuck Schumer, the Jewish leader of the currently still Democratic majority in the Senate, has been single handedly responsible for preventing even consideration
in the Senate of the Antisemitism Awareness Act, a piece of legislation that had passed the House with overwhelming bipartisan support already months ago.9 The reason was telling: the Democrats’ left wing opposed the definition of antisemitism used in this law which equated anti- Zionism with antisemitism, and Schumer, who in his decade-long political career always presented himself - in a wordplay to his name - as the “Shomer” (defendant) of Jews (he represents Brooklyn in the Senate) shamefully caved.
With antisemitic incidents spiking by hundreds of percent following October 23, 2024, it practically appears obvious that there also must have been an impact on the healthcare system. A recent paper by a group of academic Jewish physicians from several leading medical institutions in the U.S., then, indeed, confirmed this hypothesis in a paper published in the Journal of General Internal Medicine.10
Surveying 645 self-identified Jewish healthcare professionals (30.2 % response rate), 253 (39.2%) reported exposure to antisemitism within their professional and/or academic environment, and 170 (26.4%) described themselves as feeling somewhat or to a great degree threatened or at least unsafe. On an interesting side note, while 474 (73.5%) responded that their institutions required anti-bias training, only 12 (1.9%) noted that this training also addressed antisemitism. To a degree, this latter point appears even more telling in demonstrating the obvious participation of medical institutions in the current wave of academic antisemitism that so very obviously has been engulfing even some of the most prominent academic institutions.
Jewish healthcare professionals also reported on cases of almost unbelievable systematic discrimination, including refusal of medical treatments for “Zionists.” In the Canadian health system, the discrimination appears to be even more profound: According to a study of the Jewish Medical Association of Ontario (JMAO), 80% of Jewish medical workers experienced antisemitism in their workplaces since October 7, 2023.11 This stands in contrast to before October 7, 2023, when only 1% of Jewish Canadian physicians reported antisemitism in their work environment. Now those numbers are 29% in community practices, 39% in hospitals, and – interestingly but not surprisingly – 43% in academic environments.
Medical antisemitism appears in Canada, especially pronounced in the province of Ontario, where Jewish medical professionals reported antisemitism in 60% of hospitals and in 73% of academic institutions. For Jewish medical students the picture was even worse: the percentage more than doubled
from 25% before October 7, 2023, to 63% after that date.
That the province of Ontario is especially affected is no coincidence, considering that over half of all Canadian Jews are living in the province, of course the highest prevalence in any Canadian province.
So where does this leave us? Very obviously with a heavy heart and much work to do. With antisemitism a scourge of the world since at least the fourth century, it would be naïve to even consider the possibility that it could – somehow –suddenly disappear.
What, however, is especially troublesome, is the recent success radical Islam has been able to muster following October 7, 2023, in establishing a very aggressive coalition with the political left, which now manifests itself in almost daily, often extremely well-attended street demonstrations all over the world. Under the main slogan “From the river to the sea,” these demonstrations have become increasingly assertive and at times, indeed, violently antisemitic.
It appears likely that under the second Trump administration things will change. Colleges and universities will risk loss of significant financial support from the federal government, unless they more aggressively attack their in-house expression of antisemitism, whether by students or faculty. And similarly, the media landscape appears to be shifting in parallel. But the ultimate conclusion from the last year remains that the scourge of antisemitism is still deeply embedded in societies in many – if not most – countries in the world. The best we can do is just to suppress it to the best of our abilities, knowing very well that – when given the opportunity – it will always immediately raise its ugly head. But we will NEVER AGAIN be helplessly led to the gas chambers!
1. Zukeran P. https://probe.org/judaism/
2. Denova R. https://www.worldhistory.org/article/1785/theseparation-of-christianity-from-judaism/
3. Gleicher B. Im Schatten der Kornblume (German). September 18, 2018. https://www.amazon.com/SchattenKornblume-German-Beatrice-Gleicher-ebook/dp/ B07HM6L81D
4. Traynor I. The Guardian April 27, 2012. https://www. theguardian.com/world/2012/apr/27/vienna-row-legacyantisemitic-karl-lueger
5. Kolirin L, Halasz S. CNN. June 5, 2023. https://www.cnn. com/style/article/austrian-antisemite-statue-scli-intl/ index.html
6. Encyclopedia Britannica. https://www.britannica.com/ biography/Karl-Lueger
7. Haug NA. December 12, 2024. https://worldisraelnews. com/rebottled-jew-hate-the-bycott-of-jewish-genius/
8. Pierre DJ. The Algemeiner. December 20, 2024. https://
worldisraelnews.com/we-need-accountability-ushous-report-condems-universities-response-to-risingantisemitism/
9. Zhukovsky N. The New York Sun. December 24, 2024. https://www.nysun.com/article/ congress-poised-to-close-without-passing-anymajor-legislation-on-antisemitism-is-chuckschumer-to-blame?lctg=1654546113&recognized_ email=ngleicher%40thechr. com&utm_source=MG&utm_medium=emailnewsletter&utm_campaign=Morning%20Sun%20%20 2024-12-24
10. Michelson et al., J Gen Intern Med DOI: 10.1007/s11606024-09159-x. Ahead of print.
11. Jewish Breaking News. December 18, 2024. https:// worldisraelnews.com/disturbing-study-finds-jewishhealthcare-workers-face-rampant-antisemitism-inamerica/


By Promila Rao, MD, MHA, an internist and hospital executive. She can be contacted through the VOICE.
BRIEFING: A large majority of the CHR’s patients are not local to NYC, but often travel long distances to receive treatments at the CHR. One such patient is the author of this unsolicited article, which was unexpectedly received one day in the editorial office of the VOICE. What makes this communication even more unique is the fact that the author—as will quickly become apparent—is a practicing physician in internal medicine and, in addition, has considerable managerial experience as a senior administrative officer in a general hospital in her home state. We felt that her view of the infertility world was insightful and worth sharing.
I would like to give a shoutout to the CHR and Dr. Gleicher (the CHR’s Medical Director and Chief Scientist) and others who are similarly dedicated in their pursuit of science and truth and to delivering individualized, patient-focused care rather than relegating everything to an algorithmic approach based on dubious data.
Evolution has programmed us to say and do things that are widely accepted by society because acceptance is the most fundamental of human needs. Our very survival and wellbeing depend on being accepted. However, progress cannot be made by conforming to the status quo. Discerning and brave voices that deviate from the mainstream narrative, such as Dr. Gleicher’s, are necessary for bringing into focus the issues that require further scrutiny. For example: success rates for blastocyst vs. cleavage stage embryo transfer, fresh vs. frozen embryo transfer, the pitfalls of preimplantation genetic diagnosis for

aneuploidy (PGT-A) testing for patients, the pitfalls of embryo grading based on blastomere symmetry, the pitfalls of “discarded per protocol,” and the recognition that egg and embryo quality may very well suffer if exposed to excessive hormonal stimulation—just to name a few. Dr. Gleicher stands out as a singular person who has the unwavering courage and intellectual authority to shed light on these issues in a relentless pursuit of science and quest for the truth throughout his career. As such, he and those like him are the bastions of hope for patients and incubators of future innovations.
People who conform to the status quo and focus on the bottom-line seldom make history. The future heroes of the fertility industry will be the ones who see a way to break away from the lure of a volume-based approach that targets the lowhanging fruit in a narrow age range and recognize that new advances are needed because it is no

longer enough to replicate variations of what was done in 1978 with mixed results. The future of humanity may very well be at stake.
Has Reproductive Endocrinology stagnated like Physics, where endless debates on Einstein’s ‘Theory of Relativity’ and the ‘String Theory’ have been the norm since the 1970s with little further innovation? Is it not time for a quantum leap to break out of the time warp and meaningfully address today’s issues?
Fortunately, we don’t live in a hyper-regulated society which rations care. This allows us to leverage current research and apply it to provide better outcomes by exploring novel options and technologies.
As physicians, we all took the Hippocratic oath, whose principal premise is “Primum non Nocera” (first, do no harm). Aside from the obvious implicit in that oath, is the recognition that we as physicians possess consequential knowledge and are tasked with guiding patients towards outcomes that are better than what would occur without our intervention.
Today, physicians are called upon to solve problems that are not just simple “diseases” with well-understood etiologies such as polycystic ovary syndrome (PCOS). We are living through a time where multiple factors play a role. An increase in chronic illness and cancer in the US is a manifestation of what is wrong with our food and environment.
In addition, the very structure and dynamics of society have been upended. Due to decimation of the family structure and of traditional values, people are more disconnected than ever before. Masculinity itself has reached a crisis point as society has lost the art of imbuing men with a sense of pride, integrity, and purpose by providing male role models. This is the reason why reproductive endocrinologists are seeing a rising number of successful and healthy women who are childless not by choice but rather due to societal conditions. Hopefully, advances in science can bridge the gap for women, as we undertake the herculean task of improving society and resolving the crisis of masculinity.
Let us examine the current definition of infertility as it has evolved to become more inclusive to cover those who are not truly infertile. The traditional definition used to be ‘the inability of a couple to conceive after unprotected intercourse for 12 months under 35 or 6 months > 35 years.’ (Definition of infertility: a committee opinion (2023) | American Society for Reproductive Medicine | ASRM).
It would be interesting to see what percentage of the populations in fertility clinics is made up of successful, well put together, healthy women without fertility issues who are on this journey due to purely societal issues. Disempowerment of men and the decay of masculinity has led to suffering not just for men but also for the very women who crave normal, monogamous, and stable relationships with men.
While it may be the case that reproductive medicine helps those who suffer from infertility, it is not at all clear that, when it comes to normal non-infertile women in difficult social situations, it offers any outcomes approximating what nature provides if left uninterrupted. Additionally, there is potential harm due to invasive procedures and exogenous hormone exposure.
The prevailing messaging encourages healthy women to freeze their eggs to preserve fertility with scant data to help them decide where to seek care and no insight into the various pitfalls of oocyte vitrification. This allows for a false sense of security for women who are generously and lovingly trying to buy time to spare men from the pressures of the biological clock. However, these brave and generous women need to know that their live birth outcomes would be far better with nature, as the widespread protocols currently in use have significant limitations.
Should we leave any stone unturned to ensure that these strong, intelligent, independent, empathetic women become mothers and shape the future of humanity?
Furthermore, I would like to point out the obvious— the survival and non-extinction instinct is as strong in women as it is in men. Donor eggs do not offer survival and propagation of the gene pool for women.

I feel that my specialty (Internal Medicine) has become somewhat of a “manager of disease” with no cure in sight and a good bit of blame shifting towards the patient—often implying that if only the patient had a better genetic makeup, complied better with lifestyle measures, and with medicine, their disease could be better managed. Healthcare systems are rated on a Leapfrog scale (the Leapfrog Hospital Safety Grade is the only hospital rating focused exclusively on hospital safety. Its A, B, C, D or F letter grades are a quick way for consumers to choose the safest hospital to seek care) and have learned to manipulate data for financial gain.
It is incredibly easy to go from a Leapfrog score of C to an A. For example, in order to show lower mortality rates, inpatient hospice admissions are encouraged as they don’t count towards mortality. Instead of addressing root causes of patient safety incidents (PSIs), nurse managers are incentivized to ask doctors to not order C. difficile or urine culture with indwelling foley catheters, etc. End result: fantastic scores with no net improvement in the quality of care rendered! I see a parallel in the Reproductive Endocrinology field, wherein several clinics amass vast numbers of patients in the desirable age demographic. This is followed by slicing and dicing data, eliminating outliers etc., to show amazing results. These results are then proudly advertised to attract even more patients and compete with other conglomerate clinics. The resulting high volumes are managed using protocol driven, assembly-line approaches with no focus on excellence of care or the individual patient.
I experienced this myself when I vitrified 15 oocytes at age 41 in July 2014 with a SC clinic rated among the top 10 in the US based on CDC live birth rate data as no vitrification data was available at that time. This was an age at which multiple women from both sides of my family conceived and gave birth to healthy children naturally. I felt confident in my choice as this clinic had a Donor Egg Bank Certification and several published studies demonstrated 95% thaw survival. Aside from that, my colleagues experiencing fertility struggles had success with this clinic. My estradiol peaked at 8898 pg/ml causing me to be concerned about OHSS and it kept me from
considering additional retrievals. I was told that my ovaries were the size of grapefruits but in spite of my requests, no immature oocytes/ GVs were vitrified and my suggestions were treated with indulgent humor instead of being taken seriously. Following vitrification I felt I had bought time and felt fortunate that I had options previously unavailable to women that could ensure 95% thaw survival rate of oocytes and ensure that I had preserved my fertility. However, in 2021 upon thawing my eggs 3-4 at a time at a leading clinic in NJ, the thaw survival was a dismal 30% instead of 95%. In addition, embryologists of questionable competence and qualifications blindly discarded my blast-stage embryo “per protocol” with no input from my reproductive endocrinologist and, of course, I was kept in the dark and only found out retrospectively. I was not given the option for cultivating to cleavage stage but opted out of PGT testing due to mosaicism and my understanding of auto correction. Now at age 50-51 I have made 7 cleavage stage embryos (most Grade B) which in itself is a miracle and speaks to the fact that my confidence in my family history was not unfounded. However, my confidence in my own profession and science has taken a huge hit as my achievable dreams suddenly feel out of reach. In addition, I have had to subject myself to additional exogenous hormones and invasive procedures due to the limitations of science. If someone with my level of fertility and knowledge can experience this, what is the hope for other women?
Our intuition/common sense is the result of millions of years of evolution and has ensured our survival and propagation. Prospective double blinded cohort studies are not needed to validate what we instinctively know to be right. We intuitively know that oocytes and embryos will do better if we reduce freezing/thawing stress, avoid inhospitable culture media, plastic culture dishes, etc. This is the only way to improve upon natural outcomes of the general population. Otherwise, assisted reproductive technology (ART) will always lag behind nature.
Hopefully, we can build on existing research from people like Professor Mitinori Saitou, MD, PhD, at Kyoto University in Japan, Professor Shoukhrat Mitalipov, PhD , at OHSU in Oregon, and others to offer hope for the future of humanity.
1. We are all driven by a need for acceptance and belonging to a group; however, let’s not forget that we have instincts, a free will and a conscience that can guide us and has never

led our species astray.
2. The future belongs to the bold, the innovative and upright. The pursuit of truth through science necessitates that we eliminate subversion and manipulation for personal gain. Data manipulation does not equal advances in fertility outcomes.
3. Let’s remember and re-avow to the Hippocratic oath: ‘Primum non Nocera.’ It should be possible to provide outcomes better than nature even for non-infertile women who are childless due to societal issues.
4. Women who are childless due to societal issues must be treated as a distinct population. These women need to know the limitations of science and current protocols such that, if they subject themselves to IVF, their live birth outcomes would be no better than those reflected by ART data for infertile women. They might be better off if they let nature take its course and just procreate as God intended.
5. Let us recognize the limitations of Evidence Based Medicine (EBM). Let us keep in mind that EBM does not mean we have to ignore common sense and our instincts or move away from individualized approach to patient care.
6. Let’s not forget that all of us, including—of course—our patients, are created equal in the eyes of God. Patients should be allowed full transparency, including time-lapse pictures of embryos. Decision-making regarding discarding an embryo or egg must include the patient and physician.
7. Future innovation must aim at minimizing invasive procedures and hormonal stimulation so that women, especially those who are in this situation due to societal issues, don’t have to sacrifice their health for a chance at having a baby.
8. This is a call to all my reproductive endocrinology colleagues to become the bastions of hope, the defenders of truth even when it is unpopular, and the protectors of women and thereby the future generations. Educated and compassionate women raise stable and productive children who can change the course of humanity for the better.
9. Let it not be said that reproductive endocrinologists stood by and allowed the world to be overrun by other species such as mice, monkeys, cloned dogs, sheep, beauty camels, and even the wooly mammoths, while many wonderful women were admonished based on age, failed by medicine when they tried to preserve fertility, judged for the shortcomings of men and society, and, ultimately, led to extinction as no one could figure out how to do things better. Please help save this valuable endangered species that is
at the brink of extinction.
10. Finally, let’s consider the future with AI. If AI is fed erroneous/manipulated data through large language models, what would the future of our species be? AI has the potential to be the only God-like entity without morals and emotions. To what extent can we appeal to AI? While God is capable of love and compassion and forgave humanity without us bearing the burden of proof, the same cannot be said of AI or its creators.
11. Our hope lies in future generations possessing bravery, intelligence, and integrity passed on to them by mothers who possess these qualities. The pursuit of truth that is shared by both religion and science needs to be the primary quest for humanity. This requires freedom of thought and speech and individual autonomy. In conclusion, whosoever ensures that good mothers propagate and are not led to extinction will save the world!
BRIEFING: The unfortunate embryo mix-up between two infertile couples several years ago in a Los Angeles area in vitro fertilization (IVF) clinic was just resurrected by The New York Times Magazine in a terrific cover story on December 1, 2024 (see figure below) 1 . There are several reasons why this article deserves special attention. First, though considering the millions of IVF cycles performed in the U.S. since the birth of the first U.S. IVF offspring in 1981, fortunately, it is an extremely rare event, it never hurts, from time to time, to steer-up easily setting-in administrative complacency to minimize such occurrences. But what really makes this article so special are the writer’s descriptions of the discovery of the mix-up and what then followed. And, yes, some incorrect comments cited in the article by—who else—malpractice lawyers, are also addressed here.
Everything started in 2019, when two infertile couples in short succession celebrated the births of their respective second child, in both instances the result of a successful IVF cycle in a small Los Angeles area IVF clinic. Obviously delighted to have brought a healthy second child home after the often-arduous IVF process, both couples settled into their new routines, which in both households, of course, included the introduction of the new sister to her older sibling, allowing for parents and siblings to proceed through their natural bonding
processes.
But in one of the couple’s households something was apparently amiss: In expression of increasing concern that he “was reluctant to voice,” the father started joking about the fact that their daughter showed no physical similarities to either one of her parents. He was Italian (but with fair hair and light brown eyes) and his wife was Ashkenazi Jewish with bright red hair. And he even joked that the IVF clinic might have mixed up embryos. And their daughter had deep dark hair.
Behind those jokes, the father had, however, developed increasing concern which also started affecting his wife. And it was she who in the end set into motion what would turn

the couple’s life completely upside down. Unclear what she was supposed to do, she called her husband’s best friend for advice, and he did his job by leaving no doubts that he was convinced that at least one of the parents was genetically not really a parent (with the suspicion, of course, falling on the husband).
This is when in November of 2019 the couple sent off genetic DNA home tests to a commercial laboratory. The results arrived three weeks later in December and reported that with over 99% certainty neither husband nor wife were the genetic parents of their daughter. These reports ended up reshaping the lives of two Los-Angeles-area families forever. Coincidentally, they

lived only minutes apart from each other.
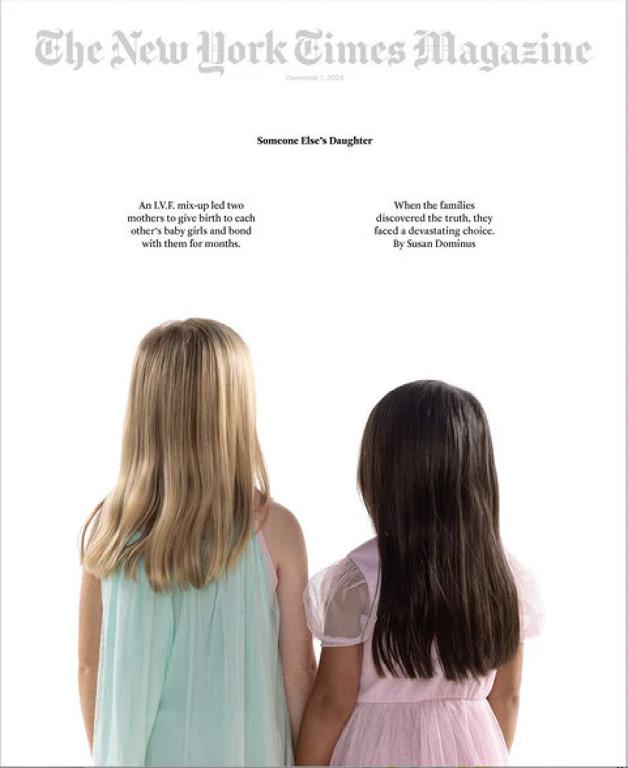
The December 1 cover page of The New York Times Magazine 1
With those test results in hand, the first family informed their small fertility clinic which, after reviewing their records, concluded that on the day of the couple’s embryo transfer at the clinic a mix-up of embryos must have occurred with one other couple which also had their embryo transfer on that day. After informing this second couple of this likely conclusion, their DNA testing confirmed it, leading to the heartbreaking recognition for both couples that they for months had raised and bonded with a daughter which wasn’t theirs.
The rest of the beautifully written article then tells in detail how these two obviously deeply shell-shocked couples not only found the strength to overcome the situation by, in a carefully and delicately managed transition process, introducing themselves to their genetic daughters (and their older siblings) before formally switching parenthood (legally the births of both girls ended up being defined as “birth by gestational carrier”) and, in the
process, establishing a new, combined family unit that allowed all four children of these two families to consider themselves as siblings.
How in modern-day IVF practice embryo switching can – and on, fortunately, only exceedingly rare occasions does – still occur is, indeed, difficult to understand, considering the various safety rules every certified IVF laboratory in the U.S. must follow. One prominent embryologist when recently asked about this subject offered an interesting analogy: “If babies can and—on similarly rare occasions—are still mixed up in neonatal hospital nurseries, who can be surprised that, despite so many well-working precautions in embryology laboratories, on very rare occasions such errors still occur.”
Though this of course, is, not an excuse for something that, simply, never can be allowed to occur, it is likely the most reasonable explanation for why errors still do occur. When system failures under all circumstances must be avoided, nature as well as industry—interestingly— resort to the same rather simple solution: both increase
redundancy processes until safety is virtually 100%. There really are no good reasons why embryology laboratories (and neonatal nurseries), through redundancies in safety procedures, should not be able to avoid such mix-ups with at least 99.99% certainty.
And it appears not too farfetched to assume that—at least in the U.S.—if this goal has not already been reached, considering how rare such reported occurrences have been in millions of IVF cycles in over 40 years of IVF practice, we, at least, must be very close to reaching the goal. A 2021 paper in the Journal of Assisted Reproduction and Genetics (JARG ) confirmed this fact and, moreover, also demonstrated that the extraordinary media attention each one of such cases attracts, makes numbers of cases appear to be much bigger than they in reality are. 2
There, of course, have been other cases reported in the U.S. since above-described California events, including a relatively recent one involving a New York City (NYC) couple undergoing IVF at another small California IVF clinic 3 , which because of financial difficulties, has since been acquired by another fertility clinic in the Los Angeles area. And then there was also a relatively recent case in NYC proper, which in contrast to the two Los Angeles cases, led to the closure of the IVF clinic where the mix-ups happened 4 . Like the two Los Angeles clinics, the NYC clinic was also

a relatively small program, leading to the suggestion that the availability of fewer financial resources at smaller IVF clinics may contribute to risk. This hypothesis, however, based on a recent similar occurrence in one of the largest IVF laboratories in Israel (a country with one of the world’s most sophisticated IVF clinic systems) likely does not apply. 5
One cannot address embryo mix-ups without a word on the legal consequences of such events. Moreover, whenever something happens in medicine that with proper medical care is considered preventable and, therefore, under no circumstances should be allowed to happen, there exists in almost all cases an “owner” for what happened. And this “owner” has legal liability. There exists also societal consensus that victims of such transgressions in medical care are entitled to payments in compensation for practical and often mental damages that have resulted from such events. That, of course also applied to the above-described California case which, as usually happens, was settled between the parties before reaching trial. By allowing several lawyers to comment on IVF in general rather than keeping their comments restricted to
embryo-switching, the article in The New York Times Magazine , however, unfortunately and inappropriately, allowed the plaintiff malpractice Bar to offer some rather biased cliché opinions about IVF, giving the wrong impression that malpractice suits in the IVF field are common (which in comparison to most other medical practice fields is not at all the case).
One of the two couples’ lawyers in article, unsurprisingly “specializing in suing fertility clinics,” for example, thumped his chest by noting a plaintiff’s case he filed which had absolutely nothing to do with embryo-switching (an incorrect genetic testing result was reported to an IVF patient; of course such an error is not necessarily typical of IVF alone, as embryo switching clearly is). He also cited a case of alleged failure of an IVF clinic to respond to alarms of freezers where embryos were stored (as if that occurs only in IVF labs) and expressed unhappiness about some IVF clinics still relying “on pen and paper labeling systems” (again, quite obviously not an issue restricted only to IVF laboratories, if that, indeed, does represent an issue at all).
A law professor with alleged focus on bioethics (whatever that means) is quoted as making what is likely the most frequently made false claim by malpractice lawyers—widely used in their advertisements 6 —namely
that IVF “is underregulated in comparison to most other medical procedures.” In reality, IVF is among the most—maybe even the most—regulated procedure in medicine. We, for example, know of no other procedure in medicine which under Congressional mandate (the so-called Fertility Clinic Success Rate and Certification Act) has to report every single event to the Food and Drug Agency (FDA), as IVF is obliged to do. 7
Unsurprisingly, above-noted plaintiff’s attorney beats the same dead horse by claiming that, if it weren’t for the malpractice plaintiff’s Bar, “nobody else would hold the IVF field responsible.”
One final note: In the U.S. legal precedent has established that in case of an embryo mixup as in the here-discussed case, genetics rule the day. In other words, the genetic parent(s) is/are becoming the legal parents of any born child. This is, however, not the case everywhere else in the world: In Israel and several other countries, for example, unless otherwise settled by the involved parties, any born child is assigned to the birth mother.
In conclusion, mix-ups of embryos among infertile couples in IVF clinics are exceeding rare events. Our quick review of the literature suggests that, likely, only somewhere between 15-20 cases have been reported in the literature.

This is very obviously an underestimation even for the developed world; but, considering that so-far over 12 million IVF babies have been born worldwide, these numbers suggest that embryo mix-ups indeed are extremely rare, even though, as The New York Times Magazine article again so well demonstrated, each case is one case too many.
1. Dominus S. The New York Times Magazine. December 1, 2024. https:// nytimes.pressreader.com/the-newyork-times-magazine-8326/textview
2. Rasouli et al. J Assiste Reprod Genet 2021; 38:1101-1107
3. Boniello K. New York Post. December 30, 2023. https://nypost. com/2023/12/30/metro/nyc-couplein-twin-embryo-mix-up-settles-suitagainst-california-clinic/
4. Manno A. Dailymail.com. April 3, 2022. https://www.dailymail. co.uk/news/article-10681315/ Massachusetts-couple-says-mothercarrying-wrong-embryo-mix-NewYork-clinic.html
5. The Times of Israel.. November 28, 2024. https://www.timesofisrael.com/ slow-and-clumsy-health-ministryreport-pans-tel-aviv-hospital-over-ivffoul-ups/
6. Fertility Advocates for Justice. https://www.fertilitylawsuits. com/?gad_source=1&gclid=EAIaIQo bChMIsqjXkrGHigMVL2hHAR28shN PEAAYASAAEgKYefD_BwE; accessed 12/1/24
7. CDC.https://www.cdc.gov/art/ nass/policy.html#:~:text=In%20 response%20to%20concerns%20 about,government%20in%20a%20 standardized%20manner.
David H Barad, MD, MS, is Director of Clinical IVF and Research and a Senior Scientist at the CHR. He can be reached through the editorial office of the VOICE.
BRIEFING: In contrast to preimplantation genetic testing for monogenic diseases (PGT-M), where the status of a single gene is determined, and preimplantation genetic diagnosis for aneuploidy (PGT-A), where allegedly the status of an embryo’s 46 chromones is evaluated, polygenic testing of embryos (PGT-P) allegedly assesses the risk of developing so-called polygenic diseases, which are diseases which occur if several different gene constellations work together to establish disease risk. Because of the ongoing controversy surrounding PGT-A, we intentionally ascribe to PGT-A an “alleged” purpose, while, as the literature demonstrates, indications for use of PGT-M and PGT-P are clear. In contrast to PGT-M which has been validated in having very high accuracy, PGT-P’s accuracy has remained largely unknown and will likely remain so for the foreseeable future.
In J.D. Salinger’s novel The Catcher in the Rye , Holden Caulfield envisions himself as someone who saves children from falling off a cliff, a metaphor for his desire to protect children from the hardships of growing up. So too do some of us, as modern catchers, imagine ourselves as protecting future generations by means of genetic screening of embryos.
Over the past two decades, the process of embryo selection in IVF has shifted from simple morphological assessments—based on factors like cell number and symmetry—to chromosomal screening aimed at detecting aneuploidy as a means of improving IVF outcomes by deselecting embryos with abnormal chromosomal complement before transfer into the uterus (called PGT-A). However, despite widespread clinical adoption in U.S. IVF clinics over the last 20 years, PGT-A has failed in enhancing live birth rates, as a recent combined Committee Opinions of the two most relevant professional U.S. societies in the IVF field recently finally made clear. 1
Now, the field is, however, poised to take yet another, even more daring step into genetic preimplantation embryo selection, moving from targeted single gene (PGT-M) and chromosomal (PGT-A) genetic assessments to whole-genome screening (PGT-P) using so-called polygenic risk scores (PRSs). This approach aims to estimate an
embryo’s predisposition to polygenic traits and diseases, such as eye color, heart disease, or diabetes.
Though the introduction of PGT-P to IVF is in marketing campaigns usually presented as “progress,” this new practice offered by a small number of laboratories and in vitro fertilization (IVF) clinics in the U.S. has raised significant medical as well as ethical concerns. Among the former is an almost complete lack of scientific validation of PRS as a legitimate embryo selection method, while ethical concerns should be very obvious, like the risk of (as happened with PGT-A) overpromising benefits, the potential for exacerbating societal inequities between poorer and richer segments of society, and, of course, a concern about eugenics. As such, it remains highly questionable whether these emerging technologies represent meaningful clinical advancements or merely add new complexities and cost to an already challenging and too expensive IVF process.
PGT-P involves the use of PRSs derived from large-scale observational studies in affected adult populations to estimate the potential future risk of disease in a child born from a given embryo. Unlike traditional genetic testing that identifies single-gene mutations (PGT-M) or chromosomal abnormalities (PGT-A), PGT-P assesses the cumulative effect of multiple genetic variants across the genome, each contributing a small amount to
the overall risk of complex, polygenic diseases such as heart disease, diabetes, or certain cancers. By analyzing these polygenic profiles, the goal is to provide prospective parents with additional information about the relative risk associated for each embryo.
The predictive value of these scores is, however, inherently probabilistic and influenced by numerous factors, including population-specific genetic variations, gene-environment interactions, and the limitations of current genomic databases, which are, of course, based on already born individuals and, therefore, may not fully capture the diversity of human genetic backgrounds in preimplantation-stage embryos, as was learned in association with PGT-A, when it was discovered that embryos with chromosomal abnormalities at blastocyst-stage often can self-correct downstream from that stage. 2,3 Since PRSs provide a relative risk estimate, they do not offer definitive predictions. Consequently, patients – for example - may misunderstand a 20% increased risk for a disease as a 20% chance of developing the disease, leading to either overconfidence in the results or unnecessary anxiety. The determination of single gene mutations (PGT-M), such as sickle cell disease or Tay Sachs disease, in contrast, have clear and unequivocal outcomes; an embryo either is or is not affected.

Explaining the distinction between absolute and relative risk to patients can be particularly challenging, especially given that the predictive accuracy of polygenic risk scores (PRSs) varies widely depending on the trait in question and the nearly limitless variables involved. For example, PRSs predictions of adult height or an embryo’s future BMI are far more reliable than PRSs attempts to predict future autism or schizophrenia.
PRSs are, moreover, derived from studies of adult populations where the traits or diseases of interest have already manifested. Their applicability to embryos is, therefore, fraught with challenges, as practically all polygenic traits and diseases are influenced by developmental, environmental, and epigenetic factors that accumulate over a lifetime. An embryo’s genetic predisposition, therefore, may not directly translate into the same risk levels observed in adults.
These limitations significantly complicate the interpretation of adult-derived risk scores when applied to embryos and may, in fact, call into question the entire concept of PGT-P. The practical impossibility of conducting prospective studies that span the developmental journey from the preimplantation-stage embryo, through pregnancy (a period where epigenetic modifications play a crucial role), and into adulthood undermines the scientific validity of these predictions. Without such studies, the utility of PGT-P remains speculative at best.
Further adding to the concerns about the already offered clinical utilization of PGT-P is the limited predictive accuracy of PRSs even in adults for whom they were developed because they often explain only a small fraction of the variance in disease risk. Adult PRSs, moreover, are frequently based on genome-wide association studies (GWAS) conducted in cohorts predominantly of European ancestry. The data generated in European populations are, however, not equally applicable to other populations, like for example Chinese Han. This is one reason why, even in adults, PRSs are still considered experimental. Their clinical utilization in embryos, therefore, has been questioned, 4,5 and even declared unethical by some professional genetic societies. 6
Ethical concern also arises from the possibility to apply PRSs to selection of non-health related traits, such as height, eye color, intelligence, or athletic ability. Eye color selection is, indeed, already offered in the marketplace. 7 Information about nonmedical traits could, of course, also reinforce certain societal stereotypes and prioritize cosmetic traits over choice of embryos more likely to lead to successful pregnancy.
That PGT-P at this point is not ready for primetime should, therefore, be obvious. That it, indeed, even in the foreseeable future will become a clinically and ethically viable offering as part of an IVF cycle, also appears unlikely, - but can, of course, not be ruled out. Any integration of polygenic risk scores (PRS) into reproductive decision-making forces us, however, to confront profound ethical, scientific, and societal questions about our capacity to use this information responsibly. We must ask ourselves if we possess the wisdom to navigate the inherent uncertainties and limitations of PRSs, while ensuring that its application truly aligns with the wellbeing of our patients and their future children. PRSs offer probabilistic data rather than definitive predictions, raising concerns about how this information might be misinterpreted or misapplied in the emotionally charged context of IVF. Are we prepared to communicate the nuances of relative risk in a way that empowers patients without overwhelming or misleading them?
Finally, as clinicians and scientists, we must openly confront the gaps in our current scientific understanding of polygenic traits, the limitations of risk prediction models, and the ethical boundaries of our interventions. Are we truly ready to wield such complex information in ways that prioritize the long-term well-being of patients over the allure of technological innovation?
As guardians and stewards of this field, we bear a profound responsibility to approach the questions surrounding PRSs with careful consideration and humility. The potential to apply this technology in ways that shape the genetic future of humanity places us in a delicate and morally charged position. Are we the proverbial “Catcher in the Rye,” standing at the
edge of the metaphorical cliff, striving to protect others from unknowingly stepping into harm’s way?
Like Holden Caulfield, who wrestled with the desire to preserve innocence and shield others from an uncertain future, we too face a similar internal struggle. Our role is to balance the promise of innovation against the risk of unintended consequences, safeguarding the patients and families who entrust us with their hopes for the next generation. The complexities here are staggering. PRS data, probabilistic and incomplete, forces us to tread a thin line between empowerment and coercion, between advancing medicine and overstepping ethical bounds. We must ask ourselves whether we are truly equipped—not just with knowledge, but with the ethical clarity—to guide others safely through this uncharted terrain. To be the “Catcher” in this context is not to prevent progress but to ensure that it is pursued thoughtfully, ethically, and with a clear-eyed understanding of both its potential and its limits. If we lose sight of this, we risk falling into the very abyss we seek to protect others from.
1. Practice Committees of ASRM and SART. Fertil Steril 2024;122(3):421-434
2. Bolton et al., Nat Commun 2916;7:11165
3. Yang et al., Nat Cell Biol 2021;23:314-321; CORRECTION: Idem 2021;23:1212
4. Gleicher et al., Nat Med 2022;28(3):442444
5. Sierman et al., Social Scie Med 2024;343:116599
6. Forzano et al for the European Society for Human Genetics. Eur J Hum Genet 2022;30:493-495
7. The Fertility Institute. https://www. fertility-docs.com/programs-and-services/ pgd-screening/choose-your-babys-eyecolor. Accessed December 21, 2024

By Norbert Gleicher, MD, Medical Director and Chief Scientist at The Center for Human Reproduction
in New York City. He can be contacted though the VOICE or directly at either ngleicher@thechr.com or ngleicher@rockefeller.edu.
BRIEFING: An excellent paper that just appeared in Nature Medicine , accompanied by an equally good, signed Commentary, put another nail into the sarcophagus of the dying dogma that embryo selection (ES) beyond embryo morphology will improve IVF cycle outcomes.
In comparing embryo selection (ES) in IVF (in vitro fertilization) between a deep learning artificial intelligence (A.I.) program and manual morphology, an excellent just-published study in Nature Medicine found no difference. 1 Because we have been arguing for years that beyond morphology, ES is biologically illogical, to us this result was not a surprise. To many others in the field, however, it apparently was. It, otherwise, would not have been accepted in such a prominent medical journal and, in addition, given an accompanying commentary. 2
The concept of embryo selection is almost as old as in vitro fertilization (IVF) itself and, therefore, has to be considered a founding dogma of IVF. It assumes that in a cohort of embryos produced in a single IVF cycle, there must be a “best” – or at least several “best” – embryos. While embryo cohorts, indeed, vary in quality (defined by pregnancy and live birth chances), none among several widely practiced ES methods in IVF have ever been demonstrated to exceed the efficacy of manual morphology assessments.
A concept first explored when embryo morphology was recognized to predict IVF cycle outcomes, it has since been the single most investigated subject in IVF, with no other subject in the fertility field receiving more funding. Yet hardly any other major investment has produced fewer rewarding results. No wonder then that all the search for ES over more than 40 years achieved, was the introduction of to this day unvalidated clinical IVF practices, such as routine embryo culture to blastocyst stage, time lapse closed incubation systems, preimplantation genetic testing for aneuploidy (PGT-A), and
others. All of these ES practices have been demonstrated not to improve IVF outcomes and, in certain patient populations, to even adversely affect outcomes. 3,4
With A.I. being everywhere (and not only in medicine), it also cannot surprise that most recent attempts at ES have involved deep learning systems. with start-ups from all around the world having reported alleged claims of superiority over standard embryo morphology. Our review of these claims has, however, left us skeptical; none in our opinion, indeed, properly validated their statements. A recently published prospectively randomized multicenter study, just published in Nature Medicine , moreover, actually refuted this claim, demonstrating no significant outcome differences between an A.I. – driven ES and standard manual embryology.
One can only hope that this recently published study 1 and its equally excellent accompanying commentary 2 will, finally, convince the IVF field that the continuous pursuit of ES beyond basic embryology makes biologically little sense and has already wasted too much effort and investments. Resulting useless IVF practices have just continued to increase the costs an already far too expensive and for many unaffordable IVF process.
If a clinically relevant difference in embryo quality were to really exist, good manual embryology is highly efficient in selecting out “best” embryos. That was recently also demonstrated by several papers which reported no outcome differences between embryo transfers at cleavage and blastocyst-

stages in general populations but suggested some outcome advantages for cleavage-stage transfers in poorer prognosis patients (mostly older and/or women with small embryo numbers).
To return to economics, one can only imagine how much cost could be saved for providers and patients in IVF if fertility clinic would not culture every embryo to blastocyst-stage, but transferred at least a majority of embryos already at cleavage-stage on day-3 after fertilization, as used to be routine until one single study in a highly biased and favorably patient population alleged outcome benefits from blastocyst-stage embryo transfers for all –by now clearly refuted.
The only outcome benefit after embryo morphology has been established that blastocyst culture potentially offers is a minor shortening of time to pregnancy if there is more than one obviously “best” embryo. But so what, if the first embryo does not implant? One tries in the following month again; and, if this was really the better embryo, the patient will be pregnant one cycle later. And, as the literature suggests, even this tiny benefit applies only to goodprognosis patients.
Is this worth the effort and additional costs of blastocyst-stage culture for everybody? We don’t think so!
And how about PGT-A for everybody, as many IVF clinics have established as almost a mandate for patients? No longer able to hold back the conclusion that PGT-A in general populations offers not a single established outcome benefit in IVF (though it may harm outcomes in some sub-populations), the most recent opinion paper of the Practice Committees of ASRM and SART, finally acknowledged publicly what everybody who can read the literature already figured out quite a while ago, such mandate or even recommended – utilization of PGT-A no longer seems feasible (the recently filed class action suits regarding this subject may also turn out to be helpful).
Just imagine the cost savings for clinics as well as patients that an IVF cycle would bring without a need for automatic blastocyst-stage culture and PGT-A. And then there is so much more junk science being practiced in association with IVF; but that remains on the docket for another time.
1. Illingworth et al., Nat Med 2024; 30:31143120
2. Kieslinger et al., Nat Med 2024;30:3059-3060
3. Gleicher et al., Nat Med 2022; 28::442-448
4. Kieslinger et al., Lancet 2023;401:1438-1446
BRIEFING: This article about third-party egg donation is presented as an Editorial because it represents the institutional opinion of the CHR and – where applicable – is reflective of the CHR’s practice patterns when it comes to third-party egg donation. Witnessing rather substantial changes in how third-party egg donation has been offered to the public over the last 20 years, the CHR has become increasingly concerned about the commercialization of the process, best characterized by two key events: (i) the 2016 settlement by the ASRM of a class-action lawsuit brought by several egg donors (or should we say their attorneys) in which the ASRM agreed to remove recommended pricing caps for egg donors from its ethics guidelines 1 and, (ii) the establishment of a plethora of commercial frozen egg banks. Both of these developments for the first time led to the definition of oocytes as marketable “products” of specific value and fostered a new coalition of economic interests between IVF clinics (especially in parallel rapidly growing clinic networks), frozen donoregg banks, and egg-donor agencies, in the process significantly contributing to the de-privatization and commercialization of infertility practice.
The first IVF pregnancy and delivery from use of third-party donor eggs occurred in Australia in 1983; the U.S. saw the first American offspring from use of donated oocytes the following year. Ever since, third-party egg donation has been an integral part of IVF in the U.S. and in most countries (though in some countries egg donation to this day is not permitted). We have over the years repeatedly criticized egg donation for one principal reason best demonstrated by the very small number of U.S. IVF cycles in women above age 42: A large majority of U.S. IVF clinics (as well as elsewhere) in our opinion are often much too quick in referring infertile women to egg donation.
The argument is usually that above age 42, pregnancy chances with autologous oocytes are too low to make IVF worthwhile, an opinion which we for several reasons categorically reject: the first reason is that, at least up to age 45, pregnancy and live birth rates – while of course declining with age – are still objectively reasonable for many, or even most, people. A more important point, however, is that what is “reasonable” for one person is not necessarily also “reasonable” for the next patient. And this dichotomy is also obviously applicable to physicians and their patients: what a physician
considers to be reasonable may not coincide with the definition of her patient and some patients will be more and others less in line with the physician’s obviously very personal opinion of what is and is not “worth it.”
After age 45, pregnancy and live birth rates reach levels where an argument of universal unreasonableness makes increasingly sense; but even at those ages many women – having a right of self-determination – should, after receiving correct informed consent, have the right to choose much lower outcome chances with own over much better outcomes with thirdparty donor eggs. Yet, while the right to selfdetermination of patients is universally cited as a basic ethical law for all of medical practice, infertile women are almost routinely denied choosing autologous IVF cycles after age 42.
That after age 42 most women are still automatically strongly “encouraged” to use donor rather than autologous eggs must, therefore, have other motivations. Likely not accidentally, donor egg – recipient cycles are also the most profitable IVF cycles in IVF clinics.
Though repeatedly refuted by several studies over the years, the frozen egg-banking industry still maintains that live birth rates are “comparable” between fresh and cryopreserved
donor eggs. That this was not the case was, indeed, first demonstrated in 2015, 2 and has since been repeatedly confirmed. 2021 CDC data, for example, reported a national fresh donor-egg live birth rate of 53.35 vs. frozen donor-egg rate of 45.8% (-7.7%). The overall difference between various published studies was between ca. 7% to ca.12% in favor of fresh donor eggs. 2,3
But frozen donor eggs do not only offer disadvantages. They indeed also offer many advantages to patients as well as IVF clinics, starting with the fact that they have basically eliminated long waiting periods for donor eggs. The rapidly increasing number of donor-egg banks also has substantially expanded donor choice, as individual egg donor pools in IVF clinics used to be small and limited numbers of donors almost always resulted in long waiting periods for patients. Clinics, moreover, hated the administration of their own donor pools which, in addition, was expensive and, therefore, adversely affected the bottom-line of what otherwise is the most profitable IVF cycle in IVF clinics.
In attempting to answer this question, one is almost tempted to answer with only one word: everything! Though such an answer would, of course, be an exaggeration, it unfortunately is not far from the truth. Let us, therefore, answer this question in some detail, starting with how we now, here in the U.S., obtain eggs for donation.
As already noted above, egg donation changed radically with the legal settlement of a class action suit the ASRM reached in 2016 with a group of egg donors which led the Society to

No wonder then that frozen donor eggs nowadays are used in a large majority of donor-egg cycles in the U.S. and fresh donor egg cycles have become a rarity. But this is not where the story ends because with steadily increasing demand for donor eggs and increasing numbers of commercial frozen donor-egg banks opening –it seems almost daily – a real donor-egg industry has arisen, characterized by features 20 years ago would have been unthinkable. So we were not surprised when The Free Press , likely the most impressive recently established “new-world” news outlet founded by Bari Weiss , published an article by Rina Raphael , titled “ The ‘Wild, Wild West’ of the American Egg Donor Industry .” 4 And, boy, was she on point and should be read by everybody thinking about becoming an egg-donor or thinking about purchasing donor eggs from wherever!
withdraw recommended payment caps to egg donors which it, previously, had published in regular time intervals as part of its clinical guidance program for clinical practice, basically accepting the plaintiffs’ argument that those priced caps restricted trade. This step – largely unmentioned then and to this day – instantly and radically changed the definition of egg donation from up to that point representing a selfless voluntary act for which donors were “reimbursed” for time and effort only (with the ASRM’s guidance representing a formal assessment of what this “reimbursement” should be in various markets), to a formal business agreement under which egg donors are free to sell their eggs, like in any other business transaction, to the highest bidder.
In other words, the ASRM’s decision to settle the
class action suit for the first time defined eggs as a legal property of egg donors that could be freely bought and sold, an idea which up to that point was considered unethical, even though men had been “selling” their semen for decades (of, course at a tiny fraction of the price donor eggs demanded, considering the much larger effort women had to undergo in making a gamete donation). That the concept of human eggs being for sale raises major ethical concerns is also demonstrated by the fact that – to the best our knowledge – no other country has followed this U.S. example. Very much to the contrary, most countries to this day restrict egg donor “reimbursements” to even significantly lower amounts than ASRM caps had been prior to 2016.
The consequences are two-fold: (i) Practically everywhere else where permitted, third-party egg donation, because of lower donor payments, ends up being much cheaper than in the U.S. (leading to large numbers of U.S. patients traveling outside the U.S. for egg donation); (ii)
Some U.S. clinics and – yes – allegedly also frozen donor egg banks, have started to “import” frozen donor eggs, or even “egg donors” themselves, from abroad who fly in for donations, both questionable practices for several clinical as well as legal reasons. However, what makes both of these practices even more repulsive is the fact that clinics (and frozen egg-banks) often are not transparent to patients about the “importing” of eggs and donors and, usually, also do not pass on the cost-savings to patients.
from clinics not only has quality based on oocyte morphology decreased, but also based on thaw and fertilization rates. And we have also heard about deliveries of empty straws and incorrect egg numbers, all signs of decreasing quality control at frozen egg banks. In parallel, we have come to question egg-donor selection by some of these egg banks, as at least one clinic found donors refused by its donor selection process, later in lists of frozen egg banks.

As also already noted above, frozen donor banks have greatly proliferated and, today, must be described as an industry with considerable power to influence practice policies in the infertility field. And this power derives from several facts, the most important one being that most fertility clinics – as noted earlier – have stopped maintaining their own egg donor pools and exclusively rely on cryopreserved donor eggs for their patients. As a consequence, the market these banks are serving has greatly expanded and service quality – according to observations in at least one clinic we talked to – has at multiple levels unfortunately decreased, while costs for oocytes are at times reaching obscene levels.
Why do we believe that egg quality has decreased? Because, based on what we hear
And then there are the purchase contracts for eggs, with often have become so complicated that one must wonder whether that reflects purpose. The complications arise from all kind of outcome guarantees which patient can purchase and which, in most cases, means that the egg bank promises additional eggs in replacement if a given number of purchased eggs does not produce – for example – at least one transferrable (blastocyst-stage) embryo. And these contracts are complicated because they, often, become “negotiable” and, probably not surprisingly, egg banks frequently “must be convinced” to really come forward with replacement oocytes when these minimal goals are missed.
In other words, under most of these purchase agreements as they have evolved, patients in principle purchase a certain number of eggs (usually a minimum of 5-6) at an average cost per egg of $3,500 approximately without any outcome guarantee. If they do want a minimal outcome guarantee as described before, there are significant additional charges, raising the cost per egg even beyond $3,500.
Consider what this means: Assume an egg donor produces 10 freezable eggs (a very small number; most donors can be expected to produce over twice that number) these eggs will produce $35,000 in revenue to the egg bank (and even more with insurance payments), with average payments to egg-donors in NYC currently at $8,000 (in other locations they frequently are lower). Moreover, clinics “importing” eggs and/ or donors, usually have even significantly lower donor costs.
Current egg pricing by egg donor banks can, therefore, only be called abusive. That this judgment is well-earned is further demonstrated by the fact that the egg-freezing industry – as a major argument why patients should choose
frozen over fresh eggs, from the beginning has been promoting frozen eggs as “significantly less costly.” So much then for this argument. Only a small group of IVF clinics still maintain their own egg donor pools. One reason is that they, often, trust their own egg donor selection. Some clinics also do not consider themselves to be in the business of “selling eggs” and, therefore, do not consider the production of donor eggs as a profit center. Such clinics then, often, price eggs obtained from inhouse egg-donors at cost. Some clinics with in-house produced eggs, therefore, offer lower per oocyte charges than most egg banks, even if freshly retrieved.

But this is not where our criticism of the current egg-donation industry ends. The excesses go far beyond that and are, indeed, starting to attract the attention of several media outlets, as two very detailed recent articles in the general press well demonstrated. One is previously noted article by Rina Raphael in The Free Press 4 and the other is an article by Jackie Davalos and Sophie Alexander in Bloomberg Businessweek , which tells an almost unbelievable story. 5
The first article – among other subjects – offer insights into what it takes to be an egg donor and rightly criticized the absence of research on the long-term effects of being an egg donor, often many times over. Addressing this issue, she quotes one donor as saying, “it’s [being an egg donor] sold as an easy way to make money and help others. Nobody mentions the longterm risks. I never saw this coming” (referring to infertility she experienced later in life, allegedly attributed to her egg donations).
Another issue the article addresses is the psychological effects of knowing that –somewhere there, likely, are children running around who are the product of the donors’ eggs. A donor whose experiences enliven almost the whole article now experiences “psychological distress” because she has started wondering whether those children might be curious about her, as she, is now very curious about them. The accusation, in short, is that egg donors do not receive proper informed consent before committing to being a donor.
Considering that most U.S. IVF clinics now use an extra-long ASRM-designed consent (or at least work off it), this cannot be considered a valid accusation for as long as donors are really encouraged to read the whole consent before signing and to ask questions. The article, however, does have a point when describing the egg-freezing industry in the U.S. as largely unregulated and, often, exploitative and even unethical. It cites misleading advertisements in recruiting financially vulnerable candidates on TikTok, and how some egg donor payments have really reached a stratospheric amount. The article claims that donors of Asian ancestry, because in increasing demand (egg donation in China is forbidden), can charge up to $50,000 for a single donation. But even that is nothing in comparison to one recent patient at a NYC clinic who, through an agency, paid $120,000 for a donor (who, as a side note, the clinic recommended against, but the patient insisted on), and who ended up producing only one single embryo.
And, if that is not already crazy enough, the same couple recruited right afterwards another donor from the same agency, and for roughly the same money; except this time, she turned out to be a very good donor.
The second article appeared in a business magazine because it involved a (legally) disgraced business tycoon billionaire who literally “built a network of egg donors and gestational carriers” (by some also incorrectly called surrogates). Many were young fashion models. One of them in the article given the name Anya because she was a native of Kazakhstan, was promised $1.5 million for posing at a Chicago IVF clinic as an acquaintance of his who she wanted to donate her eggs to for the standard fee of $10,000. In 2019, one year later, a gestational carrier gave birth to a boy conceived from one out of 20 of Anya’s eggs that had been retrieved. Five years later (now 33 years old), she hasn’t seen her biological son even once because her “exboyfriend” had her sign papers that cut her out of the boy’s life (and, as she never received the $1.5 million, she likely did not have the means to fight for him in court).
The exclusive father, according to the article, is a disgraced insurance tycoon who once had a net worth exceeding $1 billion but, now after two
convictions in federal court for bribery is facing up to 30 years in jail (he already spent two years in jail and was released upon appeal). By now he has at least (nobody knows for sure) 12 children, with nine among them born over the last five years form arrangements as the one described for Anya. He is the sole parent for eight, and he lives with them near Tampa in Florida; another 4 live with his ex-wife and a business associate, possibly also his fiancée. According to the article at least six of his children were born through a network of egg donors and surrogates including at least 25 women.
What makes this story so remarkable is that all of these activities were, at least at the medical practice level, perfectly legal. Though one clinic apparently turned him away (see below), most did not! Interestingly, he initially was very supportive of the planned article and collaborated with the two writers for hours in telephone and sit-down interviews. Shortly before publication, however, he cut off all contact and actually filed a lawsuit against them, alleging defamation, slander, and interference in his relationship with one of the gestational carriers.
Coming back to his model girlfriends, another one – this time from Los Angeles – ended up with him at the Duke University IVF program. The Duke staff, this time, was, however, told the truth about the promised $1.5 million and this time the potential model-donor got cold feet and Duke also said no.
But pretty much every other IVF clinic he approached said yes, and he had donors go through egg donation cycles in California, Illinois, and Nevada, as well as outside of the U.S. at the single IVF clinic in Barbados. The large majority of cycles were, however, performed at HRC Fertility in Los Angeles and Kindbody in Chicago, two of the largest private equity IVF clinic chains in the country.
Does this mean that chain clinic networks financed by private equity are more unscrupulous than physician and academically owned IVF clinics? We cannot say this with certainty but there is, of course, reason to believe so; these commercial entities work on an on average 5-7year schedule, in which they have to turn over an asset with significant profit. That can only happen if they massively grow revenue over this
time and, of course profit follows. A just recently, so-far only electronically published study of U.S. investigators in JARG which demonstrated that – based on nationally reported data – private equity-owned clinic networks utilize significantly more PGT-A than physician and academicallyowned clinics. 6 The literature is also full of reports of increasing pressure on physicians to maximize utilization of all kinds of treatments once private equity assumes ownership of a medical enterprise. The heavy involvement of the Kindbody network with the above-described billionaire, therefore, does not bode well for this company’s image in community as well as public, which recently has already been damaged by missed announcements of public listings, unmet other forecasts, and a major management shakeup.
This Editorial – as by now should be obvious –very clearly is meant to reflect dissatisfaction and even a degree of embarrassment about the current status of egg-donation in the U.S. This sentiment, moreover, also extends from frozen donor-egg banks to agencies which supply patients with “fresh” egg-donors (i.e., donors who go through a fresh stimulation cycle) which, therefore, makes it possible for donor-egg recipients to have a fresh-fresh cycle (fresh eggs and fresh embryos), and with gestational carriers (by many also falsely called surrogates because surrogates also contribute their own eggs). Among gestational carriers we have since the COVID-19 pandemic also noticed a rather steep decline in their clinical quality, finding ourselves much more frequently than in older times, recommending against use of proposed carriers. Moreover, the pricing of agencies for fresh donors and/or gestational carriers has, at times, reached truly absurd levels, especially when it comes to certain ethnicities.
In short, the state of the union is not great when it comes to egg donation (or gestational carrier pregnancies). Recognizing this fact is an important first step; doing something about it is a very different – and more difficult – issue, and not the least because egg-donation has become such a big business.
What we have been witnessing with eggdonation is, therefore, just one more symptom of a more general malaise in infertility practice
which is caused by the “industrialization” of everything, from the practice of medicine itself, now increasingly owned by Private Equity and Wall Street, and a support- industry around this practice including testing, pharma, and supply services, as well as frozen gamete banks and various service agencies, all united in one common goal: to increase utilization of fertilityrelated respective services.
Because the overwhelming goal for all of these interest groups is more revenue and bigger profits, the primary traditional goal of good medical practice – outcome improvements in practice – have fallen by the wayside and are just receiving lip service and, even that, only rarely and then generally only in attempts to safe costs. No wonder IVF has, based on outcomes, actually made no significant progress in over a decade and, to a degree, has even regressed.
References
1. International Fertility Law Group. February 11, 2016. https://www.google.com/search?q=ASRM+settels+clas s+action+lawsuit&rlz=1C5CHFA_enUS1083US1083&oq= ASRM+settels+class+action+lawsuit&gs_lcrp=EgZjaHJvb WUyBggAEEUYOdIBCjE0MDQxajBqMTWoAgiwAgE&sour ceid=chrome&ie=UTF-8
2. Kushnir et al., JAMA 2015;314(6):623-624
3. Souza Setti et al., Fertil Steril 2029;112(3):e120-e121 (abstract)
4. Raphael R. The Free Press, Wednesday, December 4, 2024. https://www.thefp.com/p/fertility-industrypreys-on-female-egg-donors
5. Davalos J, Alexander S. Bloomberg Businessweek. December 2, 2024. https://www.bloomberg.com/ news/features/2024-12-02/us-fertility-clinics-helped-adisgraced-billionaire-deceive-women
6. Patrizio et al., J Assiste Reprod Genet 2025; Ihttps:// link.springer.com/article/10.1007/s10815-024-03340In press.


In the above picture, Norbert Gleicher, MD giving his Plenary Talk on breaking dogmas in reproductive medicine. In the next picture from left to right at a faculty dinner in Hong Kong’s famous Hong Kong Club:
Prof. Claus Yding Andersen, PhD, from the University of Copenhagen in Denmark; Prof Cii-Ruey Tzeng MD, MPH (standing), former Chair and now Honorary Professor, Taipei Medical University, Taiwan, and Secretary General of the Asia Pacific Initiative on Reproduction (ASPIRE); again, the CHR’s Norbert Gleicher, MD; and Prof. Zeev Shoham, MD, from Israel, one of the founders of the Ovarian Club conferences in Europe and Asia, with his Hong Kong partner Milton Leong, MD who hosted the Conference and amazing dinner serving an international not shown in the picture.
This issue of the VOICE is a double issue for January and February of 2025 but, considering the production schedule, really covers early December of 2024 to mid-February of 2025. We, therefore, start the CHR News section with the annual Foundation for Reproductive Medicine Conference (FRMC) held from December 6-8, which, one by now can say “as expected,” was once again a smashing success, as always welcoming a faculty and audience from all over the world, but also, for the first time, streaming to the whole world.
And then there has been a lot more news around the CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD,
who after three exhausting days of overseeing the FRMC boarded a 15-hour flight to Hong Kong to present a Plenary Talk at the annual Asian Ovarian Club under the title “Breaking Some Longstanding Dogmas in IVF.” As well, sometime in-between, he was notified by Doximity that his over 500 peer-reviewed published papers had been cited over 11,100 times, which places him among the top 5% of all members in the worldwide Doximity community. 1
REFERENCE
1. https://www.doximity.com/ insights/citations_reports?_eda_ link_uuid_=32...insights::citations_ report&utm_source+doximityeda&utm_medium=email
Gleicher N, Barad DH. New insights into the effects of endometrioisis on in vitro fertilization (IVF). Reprod Biomed Online. 2024; ahead of print. https://www.rbmojournal.com/article/S14726483(24)00671-0/fulltext;.
Based on a recently published paper by Italian colleagues on the effects of endometriosis on IVF, the two authors in their Commentary article offered additional insights on the subject they gleaned from the data in this publications. We here quote the abstract: “It is not uncommon that a published paper offers unintended insights, - not noticed by its
authors. This to substantial degree was the case with a recent publication addressing the effects of endometriosis on in vitro fertilization (IVF). Utilizing donor-recipient cycles as study population to isolate recipient effects, the wellexecuted study demonstrated only mildly adverse outcome effects of endometriosis on IVF cycle outcomes, to a significant degree laying to rest this still controversial issue. In the process the study, however, also offered very interesting – and left unmentioned – insights into a host of other issues with considerable relevance to endometriosis and IVF practice in the U.S and U.K. Those are the subject of this communication.”
Orvieto R, Gleicher N. A simple and practical approach to elective egg freezing to control costs and expand access to care. J Ovarian Res 2024; 17:213.
As the title of this paper already indicates, the authors in this manuscript suggest a simple and cost-effective approach to routine elective (also called) social egg-freezing cycles in uncomplicated patients.
Patrizio P, Darmon S, Barad DH, Gleicher N. Greater PGT-A utilization in IVF clinics does not improve live birth rates but relates to IVF center ownership: a preliminary report. J Assist Reprod Genet 2024; ahead of print. https://doi.org/10.1007/ s10815-024-03340-1
In this study the investigators demonstrated two separate and important findings in a national data set of IVF cycles: First, the study demonstrated that
IVF clinics with higher PGT-A utilization did not demonstrate any improvements in IVF cycles in comparisons to clinics with lower PGT-A utilization, - further supporting the increasingly accepted conclusion that PGT-A does not improve IVF cycle outcomes in general populations.
Second – and, because never before reported to a degree even more important, – the study provided the first evidence that PGT-A utilization in IVF clinics significantly varied depending on clinic ownership. Specifically, clinics owned by private equity (and similar outside financial interests) demonstrated significantly higher utilization of PGT-A than physician-owned and academic IVF clinics.
Though this finding must still be confirmed in a larger study over a longer time span, this is, of course, a worrisome finding because it suggests that financial incentives may come into play when patients are advised to utilize PGT-A in their IVF cycles.
In April 2021, our practice had the privilege of consulting with a male couple who hoped to start a family through gestational surrogacy and egg donation. Both partners, diagnosed with HIV-1 several years prior, had achieved
undetectable viral loads through antiretroviral therapy. Despite advances in reproductive medicine that allow HIV-positive individuals to safely contribute gametes, New York State regulations initially prohibited the use of semen from individuals with a history of HIV for surrogacy.
We advised the couple to seek help from the Bedford Research Foundation’s Special Program of Assisted Reproduction (SPAR) in Massachusetts, which specializes in preparing virusfree semen specimens for assisted reproduction. Their specimens were thoroughly tested and confirmed free of any detectable virus. However, New York’s stringent tissue bank regulations presented a significant hurdle, requiring us to advocate for an exception to the existing rules. After extensive correspondence with the New York State Department of Health (NYS DOH), including highlighting the safety of SPAR’s protocols, the Department carefully considered this unique case.
Following this discussion, in March 2023, the NYS DOH updated its policies, reflecting the “Undetectable = Untransmittable” (U = U) principle. This new guidance allows exceptions for individuals living with HIV to contribute reproductive tissues under strict conditions, including maintaining undetectable viral loads, comprehensive counseling for an intended gestational carrier, and adherence to rigorous safety protocols. Most recently, in January 2025, the NYS DOH granted an exception for our center’s above-noted couple’s,
enabling the CHR to use their embryos in gestational surrogacy.
This milestone highlights the progress made in ensuring that individuals living with HIV can safely pursue parenthood through assisted reproduction. The approval demonstrates the importance of updated medical policies that reflect current scientific understanding and advances in reproductive technology. By addressing these barriers, this case has helped create a clearer pathway for others. We are proud to have supported this couple in overcoming barriers and paving the way for future families in New York state.
On December 23, 2024, at 6:30pm, Anja von Schondorf – Gleicher, JD, the older daughter of the CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, delivered exactly at term a healthy daughter, Ajla Adela Seferi (see below), finally making him a grandfather. Mother, father (Zim Seferi) and daughter are doing extremely well!



Building on the CHR theme of “fighting for every egg,” this month’s image gallery is all about the starting point for IVF treatment: the egg. The development of a human egg cell involves a long journey within the cozy confines of the ovarian follicle, with most estimates being around 100 days in duration to move from the earliest stages (Figure 1) to a fully activated state (Figure 4).

Figure 2 gives us a glimpse into the growing egg, biding its time by building up the stockpiles of materials needed to support embryo development, here the chromosomes of the egg are shown in blue with the outer blue nuclei representing those of the follicle granulosa cells.
Figure 1 shows one of the secrets of the egg cell in its early stages of development, the green stain shows a special molecule that allows the egg to talk to the cells of the follicle residing outside. Its technical name is GDF9, and we consider it to be the conductor of the symphony that will lead the follicle all the way up to the time of ovulation.


Figure 3. shows what happens during the time of ovulation when the egg positions its chromosomes (seen in white) on the meiotic spindle (blue, center) and in the moment captured by this image, one can appreciate the forces pulling the chromosomes apart from one another as the egg goes through maturation.

Figure 4. shows the finished product of ovulation-the mature egg with its polar body at twelve noon (blue bubble) and the egg’s chromosomes remaining in the cytoplasm awaiting the opportunity to undergo fertilization, should a willing and capable sperm be introduced after IVF or ICSI. So ends the journey of an egg from its beginnings through to ovulation!

BRIEFING: The VOICE in this section offers opinions about news which in preceding months attracted our attention and which we believe in some ways are relevant to the practice of medicine. We separate them into subheadings: (i) Local, National, and International News; and (ii) General Medical News not directly related to Reproduction (direct medical news are reported in a later section of this VOICE). Since outside opinions and CHR’s positions on various issues can obviously be biased, it is important to reemphasize that we are fully cognizant that “expert” opinions in medicine are considered the lowest level of evidence and should be viewed as such by our readers. Unable to offer, therefore, consistent “truth” (assuming that something like that really exists in science), the VOICE strives to come in its selection of topics and in its content as close as possible to the most likely “truth of the moment.” We, therefore, especially welcome from our readers contrarian submissions to our own opinions. They should be submitted under the heading “opinion” to social@thechr.com.
*Do you know what preprints are?
If the answer is no, you are not alone; only about one-third of survey respondents (an obviously evenly favorably selected group) correctly described preprints as unreviewed research findings. 1
It appears that at NIH you can just go on leave forever: Facing according to a report in Science allegations of workplace misconduct, 2 Rena D’Souza, Director for the National Institutes of Health’s National Institute of Dental and Craniofacial Research has been on involuntary paid administrative leave since last April. And now she is suing the agency for discrimination! We don’t envy the incoming new NIH boss!
*And more on the NIH
The NIH is, indeed, getting a new boss. His name is Jay Bhattacharya, MD and he used to be rather unpopular in leading NIH circles, especially during the COVID-19 pandemic, when he refused to follow the politically-correct
opinions of – then – big NIH boss, Francis S. Collins MD , a geneticist who really did not know very much about pandemics but, of course, was a brother-in-arms with by now quite notorious Anthony Fauci, MD (who, indeed, is an infectious disease expert).

Jay Bhattacharya, MD, PhD (in economics) a professor at Stanford University School of Medicine in the Department of Health Policy and formerly in the Department of Medicine.
Those two bigshots were very upset when three prominent public health experts—among them Bhattacharya— disagreed with their public policy on lockdowns during the COVID-19 pandemic and formally criticized it in an open letter, known as the Great Barrington Declaration.
In a recent editorial in The Wall Street Journal , John Sailer , a Senior Fellow at the Manhattan Institute, noted that the NIH has been creating career pathways built on race rather than merit and expressed hope that Bhattacharya—who really seems to be an unusually nice and smart guy—“can
bring science back to the NIH.” 3 We are quite certain he will! What makes us believe that he, indeed, will is the fact that he announced plans to link NIH grants to gauges of academic freedom at academic institutions. This, for example, for Harvard University could have quite devastating consequences, considering it has in recent years always come out dead last among leading universities on this gauge.
A recent paper and commentary in Nature Magazine reported that deep sleep helps the heart to heal. 4,5 It appears that after a heart attack, immune cells travel to the brain and induce sleep with the purpose of suppressing inflammation in the heart and aid in its recovery. If sleep is disrupted, excessive inflammation worsens cardiac function and slows healing. One wonders whether that does not also apply to other injuries of the body. So much for the 6AM wake up calls in hospitals!
*Finally, somebody speaks out about the absurd flood of systematic reviews in medical journals
It is high time that somebody says it: worthless b.s. systematic reviews have been flooding the medical literature but that is not even the main problem, as a recent article in Science magazine
points out; we are dealing with a chain of corrupted events. 6 Fake papers, often produced by papermills, are flooding the literature. The only study a fake scientist can produce at his desk without ever planning and executing a real study is a meta-analysis of published literature. But if the data on the subject is fake, even the best research synthesis will be unable to discover a really valuable result. And the combination of fake papers and b.s. systematic reviews become a deadly threat for medical publishing. But here is one more point to consider; this is also the material that currently trains all the A.I. programs for medicine. God may help us!
Yes, hard to believe there is a “dark proteome,” driven by thousands of new human genes. So-far overlooked segments of the human genome, as it turns out, code for a multitude of tiny but important proteins. 7 Quoting a scientist from the Salk Institute for Biological Studies in la Jolla, CA, the article notes that “unless we know what the proteins in the dark proteome are, and how they contribute, our ability to treat diseases will remain limited.”
*Is the risk of metastatic disease with cancers inherited?
This is what—per Rockefeller University’s News Highlights —a new study scheduled to appear in Cell suggests. 8 Roughly 90% of cancer deaths are due to metastatic spread of the cancer and not due to the primary tumor. For the longest time such metastatic spread was considered dependent on selected cells within the primary tumor. Now this paper suggests that there may be a potential second mechanism by which metastatic disease occurs, a hereditary disorder where the cancer’s hosts own tissue – and not the primary cancer – is the culprit. Their still preliminary data in breast cancer suggest that patients with a variant PCSK9 gene have a 22% risk of metastasis over 15 years, while the risk in cancer patients without this variant is only 2%. These findings, quite obviously, open up
some interesting potentially new treatment options.
The Cass Report in the U.K., extensively discussed in the VOICE in prior issues, now has legislative consequences, with the U.K. banning the use of puberty blockers in potential transgender minors. 9 As we have repeatedly pointed out in discuss ing this subject, we strongly feel that this is the right decision, though we, of course, remain concerned when governments make medical treatment decisions.
This decision by the UK government is of special interest for the U.S., considering that the U.S. Supreme Court is currently considering the same subject and is expected to come down with a similar opinion. As we also have repeatedly pointed out, government and/or court interventions – as in this case – usually happen only if the medical profession fails to self-control medical practice. In the treatment of alleged transgender youth, the medical establishment has bitterly failed on both sides of the Atlantic. The U.K, however, at least recognized the problem, which several years ago led to establishment of the Cass investigation. The medical establishment in the U.S. has, in contrast, mostly remained mum, with leading academic institutions actually having led the excesses in treating alleged transgender youths.
need better
We of course strongly believe that this is the case since – as we have noted repeatedly in raising this issue in the VOICE – corporations are not yet licensed to practice medicine, which they, however, practically speaking, do on a daily basis, when insurance companies deny coverage or administrators of clinic chains develop practice guidelines in place of physicians. Now an Opinion article in The New England Journal of Medicine suggests that independent physician associations could be “a bulwark against corporate control.” 10 Whatever keeps corporations away from practicing medicine is good for us!
*Mark
One cannot but love Eric Topol, MD ’s blog Ground Truth. The subjects and individuals he chooses for interviews are always interesting and, most recently, it was Mark Cuban , business magnate and self-made billionaire, star of the hit-TV show Shark Tank, past NBA owner and still GM of an NBA team, as well as political dilettante with suspected future political aspirations (on the Democratic party’s side), who sometimes can say really stupid things, as we found out shortly before the recent election, who was the interviewee. 11
In January of 2022 Cuban launched a new company called Cost Plus which, according to Topol, “transformed how many Americans can get their prescriptions filled at a fraction of the prevailing prices, bypassing pharmacy benefit managers (recently in the headlines for really representing an unusually high percentage of excessive U.S. costs for pharmaceuticals) which control 80% of U.S. prescriptions.”
And, as we learned from this interview, this is only Cuban’s first step in disrupting the overpriced U.S. healthcare system through “creative destruction.” So far there exists Cost Plus marketplace and Cost Plus Wellness but much more is expected. Very much worth the read!
*If you really want to read something very special
The Free Press in 2023 announced its first-ever high school essay contest for teenagers in which they were challenged to describe a problem troubling American society and how they would fix it. As the editors noted, “over 400 teenagers responded but one really stood out”: 17-year-old Ruby LaRocca from Ithaca, New York, a homeschooled senior. You will not believe what you will read. 12 It is simply too beautiful to describe; it must be experienced!

*Will updated FDA labeling of “healthy” food make us healthier?
We don’t think so! The new rules on labeling foods as “healthy” basically only tighten limits for sugar, sodium, and saturated fats. 13 But isn’t there so much more to “healthy foods”?
Unsurprisingly, the inflation the country has been experiencing also affects health care costs which, of course, in comparison to other developed countries, already have been exorbitantly high. As a recent article in The Wall Street Journal pointed out, rising wages of hospital fees are the main causes. 14 Key points were: (i) Healthcare spending in the U.S. reached $4.867 trillion in 2023, a 7.5% increase from the previous year. (ii) Americans spent about $4,000 on health insurance in 2023, up nearly 20% from five years earlier. (iii) Hospitals and doctors’ offices are paying more for workers, in large part due to worker shortages, rising wages and high turnover.
Shared theocentric perspectives between orthodox Jewish and Muslim patients A group of authors from the Division of Medical Ethics at Weil Cornell Medicine in NYC recently addressed this rather unusual but certainly interesting subject in a paper. 15 For those practicing in NYC or in any other city where both of these two religious groups are prominently represented, this paper offers interesting and useful insights.
It has been known for quite some time that cell-free DNA (cfDNA) used in early prenatal testing for fetal aneuploidy (NIPT) can incidentally detect maternal cancers. Now the group that initially made this observation reported on 107 pregnant women with unusual clinical cfDNA sequencing results on NIPT but no hint at cancer and had them undergo detailed cancer screening. Occult cancer was detected in 52 (48,6%), with lymphoma being the most frequent diagnosis (31 out of 52) 16 . Interestingly, neither the paper nor an accompanying Editorial 17 commented on the fact that cfDNA may, therefore, likely also be used for diagnostic purposes in non-pregnant states and in men to detect occult cancers. Certainly worth a trial!

*David
So, who is this guy, you may ask, especially if you are not familiar with the anti-aging world of medicine. In that world – you better believe it – everybody knows DAS because he, unquestionably, can be considered one of the field’s “gurus,” as The Wall Street Journal recently described him in a front-page article with the not too friendly headline “A reverse aging guru’s trail of failed businesses.” 18 A tenured geneticist and professor at Harvard, he has become known for his highly controversial believe that aging is a disease that can be reversed.
And like many other geneticists (we fully acknowledge an inherent bias against by geneticists offered commercial testing), he may be a better salesman than scientist since none of the many companies he has founded over the years – though having raised for them over $1 billion according to the Wall Street Journal article - ever succeeded in developing a worthwhile product. Four companies have gone bankrupt or halted operations, among those – yes there is a link to reproductive medicine – in 2011 a company called OvaScience, which became infamous in the field of infertility for a totally absurd hypothesis how older ovaries could be rejuvenated. Based on D.A.S.’ and an (at the time prominent) biologist’s representations, the company in March of 2015 reached a market cap of $1.3 billion (!!). By March 2018 the stock traded below $1, and the company was acquired in a reverse merger for basically nothing.
Another four of his companies have not yet tested any drugs or gene therapies in humans or have, according to the article in the Wall Street Journal , initiated only smallscale trials that are unpredictive of
their potential effectiveness. We recently had also the opportunity to see and hear D.A.S. debate Rockefeller University’s Ali Brivanlou, PhD on the question whether aging is a disease in a sold-out venue in Brooklyn Harbor and he was, indeed, a great salesman; but Brivanlou clearly won the scientific debate (In full disclosure, - we may be biased because we have maintained closed collaborations with Brivanlou over many years).
And Eric Topol, MD, in his above-noted Ground Truth blog, is no exception, when in another recent post he interviewed Kevin Dennis Hall, PhD , 19 Senior Investigator and Section Chief at the Integrative Physiology Section in the Laboratory of Biological Modeling in the Intramural Research Program at the National Institutes of Health (NIH). The interviewee is widely recognized for his rigorous randomized human trials as well as animal model studies in advancing the understanding of nutrition and metabolism.
Here are a few key points from the conversation we found interesting: (i) The link between ultra-processed foods and higher risk of cancer, cardiovascular disease, type 2 diabetes and neurodegenerative disease are “pretty darn strong.” (ii) Vegan as well as ketogenic diets have a positive effect on the immune system, indeed, both, on innate and adaptive immune functions which, of course, has special relevance in autoimmune diseases (and in reproductive medicine, likely, in endometriosis/adenomyosis). (iii) Adiposity is somewhere between 40% to 70% polygenetic heritable. (iv) GLP-agonists are associated with loss of muscle mass and patients on these medications, therefore, should be encouraged to use resistance exercises.
*Is
bird flu (H5N1) another pandemic threat for the country and the world?
So at least argued Zeynep Tufekci, PhD , a professor of sociology and public affairs at Princeton University and columnist of The New York Times in a recent Op-Ed, urging Biden
in his final weeks in office “to get serious“ about the bird flu and avoid a foreseeable catastrophe. 20 She may be right according to comments by former Coronavirus Response Coordinator under President Donald Trump, Deborah L. Birx, MD , who feels that “we (again) have our heads in the sand.” 21 Also worrisome is the finding that the H5N1 sample from a very ill patient – according to the CDC – demonstrated concerning mutations, which make the virus more contagious for humans. 22
In a warning shot to the bow of other medical journals that may be considering a switch to the novel publishing model of the eLife journal, Clarivate, the company which publishes the metric of the “impact factor,” announced that simply performing a peer review after publication and neither accepting or rejecting papers, “does not meet the standard of a peer review journal,” to which an eLife ’s Executive Director, Damian Pattinson, PhD , responded that “the journal impact factor is a very corrosive metric, one that we’ve never supported or publicized.” 23
A general surgeon in Texas named Eithan Haim, MD , may, as The Free Press reported, end up in prison for it. 24

such services had been paused. By being charged by the U.S. Department of Justice with four felony counts, he is threatened with up to 10 years of prison for blowing the whistle on the hospital. And all of this started when he was still a surgical resident. One can only hope that the new Justice Department under the Trump administration will quickly withdraw the threat to a young physician at the beginning of his career who fulfilled his first obligation as a physician: to prevent harm to patients!
1. Science 2024;386(6722):603
2. Wadman M. Science 2024;366(6722):609610
3. Sailer J The Wall Street Journal. November 20, 2024. pA15
4. Hunyh, et al., Nature 2024;635:168-177
5. Rowe R. nature 2024;635:4546
6. Else H. Science 2024;386(6725):955
7. Pennisi E. Science 2024;386:6725:951952
8. The Rockefeller University. December 9, 2024. https://www.rockefeller.edu/ news/36964-researchers-discover-agenetic-disposition-in%20increasing-riskof-breast-cancer-metastasis/
9. Zhukovsky N. The New York Sun. December 11, 2024. https://www.nysun.com/article/ unacceptable-afety-risk-uk-governmentannounces-indefinite-ban-on-pubertblockers-for-minors
10. Zhu et al., N Engl J Med 2024;391(24):22832285
11. Topol E. Ground Trust. December 20, 204. https://erictopol.substack.com/p/markcuban-a-master-disrupter-for
12. LaRocca R. The Free Press. August 31, 2024. https://www.thefp.com/p/free-press-highschool-essay-contest-winner
13. Jewett C. The New York Times. December 19, 2024. https://www.nytimes. com/2024/12/19/health/fda-healthy-foodslabel.html
14. Torry H. The Wall Street Journal. Updated December 18, 2024. https://www.wsj.com/ health/healthcare/american-healthcarespending-charts-explained-adaa0e23
15. Hossain et al., Cambridge Quarterly of Healthcare Ethics 2024.:1-17. Doi:10.1017/ SO963180124000379
16. Turriff et al., N Engl J Med 2024;391(22):2123-2132
17. Vora NL. N Engl J Med 2024;391(22):21682169
18. Marcus et al. The Wall Street Journal. December 5, 2024. https://www.wsj.com/ health/wellness/david-sinclair-reverseaging-failed-business-8bc4a43d
19. Eric Topol. Ground Truth. November 30, 2024.https://erictopol.substack.com/p/ kevin-hall-what-should-we-eat
20. Tufekci Z. The New York Times. November 29, 2024. https://www.nytimes. com/2024/11/29/opinion/bird-flupandemic.html
21. Tirrelll M. CNN. December 27, 2024.
The federal governmentin the Biden administration was accusing him of a HIPAA violation when he revealed that Texas Children’s Hospital was providing gender transition treatments to minors after the hospital had announced that
22. Mueller B. The New York Times. December 27, 2024. https://www. nytimes.com/2024/12/27/health/bird-flumutations-louisiana.html
23. Brainard J. Science 2024;386(6724):839
24. Bartlet T. The Free Press. December 3, 2024. https://www.thefp.com/p/bidenprosecution-eithan-haim-gender-care-
Nobody can deny that birth rates are declining in almost all economically advanced countries and, to lesser degrees, even in many developing countries as well. Declining birth rates, however, do not automatically mean declining fertility rates, even if the public (including media) unfortunately uses those two terms often interchangeably (just Google the question “Are fertility rates declining?”).
A recent article in The Wall Street Journal attributed in its title a decline in “fertility rates” to everyday chemicals. 1 The anecdotal case report offered as an example, however, reveals the whimsiness of the claim: A 30-year-old nurse anesthetist failed for a few months (!!!) to conceive, and her doctors told her that her ovaries “weren’t functioning properly” (???). A Facebook group – and scientific papers (???) she subsequently looked up convinced her that synthetic chemicals found in everyday consumer products were likely to blame.
As a consequence, she decided to reduce her exposure to such chemicals and – lo and behold – she conceived two years later (!!!) with help of an intrauterine insemination (!!!). What a surprise! And we hope that our readers will understand the symbolism of the exclamation and question marks in parentheses, pointing out the absurdity of the alleged associations.
So, what is really going on? Birth rates, indeed, are almost universally declining. In the U.S. this has been the case since 2007, reaching historical lows again in 2024. According to the CDC, they declined in only one year from 2022 by 3%. The average U.S. female, therefore, currently has only 1.6 children, when a country needs a birth rate of 2.1 children per woman to maintain its population. And having birth rates below replacement levels, of course, creates considerable economic problems because it means a shrinking workforce and a relative increase in the aging population, resulting in fewer working people having to take care of more already retired people (now you know why Elon Musk is planning to produce humanoid robots!). The world’s total birth rate has fallen from 4.8 children in 1950 to 2.2 today, with the only continent still producing a birth rate above replacement being Africa.
Like almost always, Musk, therefore, has been absolutely correct: the world does not suffer from over- but from under-population!
Why the drop? Likely the principal cause is the close inverse association between development and prosperity and birth rates. But other causes may, of course, also contribute. Likely the most important among those is significant delay in childbearing by women who, now, are usually in the work force. Such delays have two potential consequences. First, to spontaneously conceive takes increasingly longer and more often fails with advancing female age. And second, the remaining reproductive lifespan of women is shortened, allowing for fewer pregnancy attempts.
Though declining fertility rates of women and men may obviously also contribute their effects on overall birth rates it is—at worst—only small. Which brings us to the
main point of this commentary: While fertility rates in the world may also be declining, this development is relatively insignificant in comparison to the decline in birth rates. To clearly differentiate between birth and fertility rates, therefore, is essential. In contrast to birth rates, a decline in fertility means that either a woman or a man does not spontaneously conceive within a defined time period and whether—considering this definition—we are becoming less fertile is somewhat unclear. There exists, indeed, at least some evidence that certain environmental agents may be culprits in adversely affecting female and/or male fertility (more on that below).
As The New York Times article points out correctly, many of the suspected substances are so-called “endocrine disruptors,” so-called because they mimic and/or block hormones responsible for reproductive functions (one reason why we here at our IVF center do not like Chinese herbs in women receiving fertility treatments, which often contain especially estrogen measurements-affecting substances). But they can also be found all over our environment, with especially plastic packaging having attracted lots of attention recently, but also cosmetics, toys, sofa coverings, etc. PFAS (manmade polyfluoroalkyl substances) have been tagged by the U.S. Environmental Protection Agency as “possible” (!!!) interference with reproduction, and they are everywhere, from drinking water to non-stick cookware, and takeout containers in every home.
The article further noted that higher levels of PFAS in blood were associated by researchers at New York’s Mount Sinai Institute for Climate Change, Environmental Health, and Economics with significant reductions in likelihood of pregnancy and live births. Trying to track down this paper, we were unsuccessful beyond finding a note from the National Institute for Environmental Health Sciences of June 29, 2023, which funded the Mount Sinai center, reporting these alleged findings of the Mount Sinai investigators in a study of women of reproductive age in Singapore. 2
Without offering any detail, the article also claims that studies have demonstrated that PFAS can delay puberty, and increase the risk for PCOS and endometriosis, while so-called phthalates allegedly reduce oocyte yields in IVF cycles.
Returning to the nurse anesthetist featured in Wall Street Journal article, we would not only argue that her case offers absolutely no evidence for infertility caused by any of above discussed environmental substances but – if there, indeed, was an environmental effect at all – it likely came from the gases nurse anesthetists are, of course, exposed to at all times in the operating room, and even that is questionable.
REFERENCES
1. Chaudhuri S. The Wall Street Journal. December 14, 2024. https:// www.wsj.com/health/fertility-chemicals-science-bc0964a1
2. National Institute of Environmental Health Sciences. June 29, 2023. https://www.niehs.nih.gov/research/supported/centers/core/ spotlight/fertility#:~:text=The%20team%20reported%20that%20 higher,who%20were%20trying%20to%20conceive.
*How lab tests can be misleading by relying on population-based reference
Returning once more to Eric Topol’s Ground Truth , in his December 14 posting 1 he addressed a subject in clinical medicine which probably applied to reproductive medicine almost more than to any other specialty: the much too common reliance on population-based reference ranges for blood tests. This has, of course, been a subject repeatedly discussed in these pages in the past, explaining that reproductive hormones for individual patients are not adequately reflected in what laboratories often publish as “normal” ranges. And the principal reason is obvious: what is normal significantly changes with age. General population-based age ranges, in contrast, involve all age groups in one very big basket and, therefore, do not inform on age-specific levels.
In his posting Topol specifically addressed a recent paper in Nature magazine, which used CBC data (the most frequently obtained lab test with over 2 million such tests being processed per day – or 500 million per year). 2
And here the reasons why population-based reference values are not telling are different: What the investigators discovered is that 9 indices of a CBC turned out to be very stale over 20 years, fluctuating in a very narrow range and, therefore, demonstrating a very low coefficient of variation (CV). Indeed, inter-individual vacation was far greater than intra-individual variation for each of the CBC metrics, and long-term (15-year+) variation were at the individual level similar to short-term variations (see Figure 1 below).
corpuscular volume (MCV) with osteoporosis and there was again consistency in direction and magnitude of hazard (up or down) for most of these associations between 2 tested cohorts. 1

Topol also pointed out that A.I. hasn’t been applied yet in the current study to interrogate a person’s setpoints. Such studies of an individual’s lab test trends in pancreatic cancer, such as bilirubin even within the normal range, have already been suggested as indicative of a higher risk. And this is a diagnosis rarely made at early stages.
Can you imagine what kind of prognostic diagnostic information A.I. will be able to generate for medicine from large available data sets!
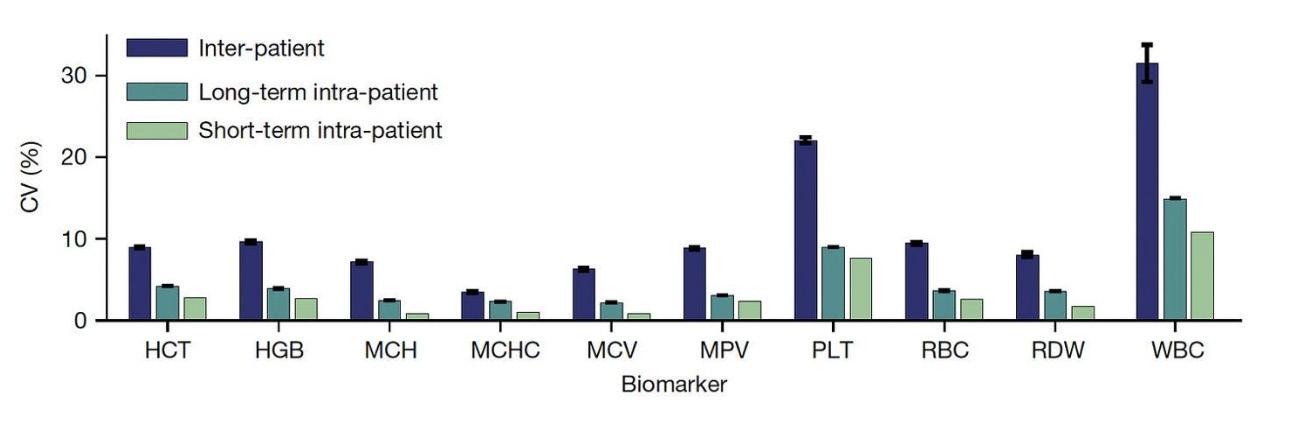
The paper then addressed how mortality for all causes in a large study population could be predicted based on the 9 setpoints of a CBC and, once again, the Figure below reflects the very interesting results: For predicting risk of all-cause mortality, individual setpoint (in orange) performed in general far better than population-level reference level (in blue). Indeed, 20% of the cohorts had an increase up to 5% in the chance of dying in the next 10 years, a partitioning which could help in differentiating high-risk status for tighter surveillance and prevention. 1
Moreover, many of the setpoints showed association with diseases: Red cell distribution width (RDW) with atrial fibrillation; hematocrit (HCT) with chronic kidney disease; the white blood cell count (WBC) with Type 2 diabetes; mean corpuscular hemoglobin concentration (MCHC) with major adverse cardiovascular events; red blood cell count (RBC) with myelodysplastic syndrome (MDS); and mean
1. Topol E. Ground Truth. December 14, 2024. https://erictopol. substack.com/p/your-lab-tests
2. Foy et al., Nature 2024. December 11, 2024.. doi: 10.1038/s41586024-08264-5. Online ahead of print.
As we already noted in the short piece on Harvard University’s Professor Sinclair, the question of what human aging really represents has remained highly controversial, with Sinclair likely being the most controversial “expert” for claiming it to represent a reversible disease. Now comes research from the Laboratory of Single Cell Genomics and Population Dynamics of Junyue Cao, PHD at Rockefeller University in NYC which offers important new insights on
tracking organ development at the single cell level. Singlecell sequencing is not easy but has become a specialty of the Cao laboratory at Rockefeller. This technology makes visible the genetic expression and molecular dynamics in individual cells, while at the same time showing the exact identity of each cell. Cao recently for this achievement was awarded the Science & SciLifeLab Prize For Young Scientists. 2

The laboratory originally developed the technique for studies of aging in the brain but now expanded it to every single major organ in a mouse (quite an accomplishment!). 1 In a recent Science magazine essay, Cao started explaining his work by noting that every human, of course, develops from a fertilized egg (i.e., a single cell) which divides into two cells, which then divide over and over again until a complete organism is created, made up of trillions of cells of hundreds of cell types. 2 Now scanning in a mouse millions of cells from every organ across five stages of life, he created the world’s largest cellular atlas in a single study and reported amazing observations: Certain cell population undergo the same changes, at the same time, in every organ during very specific stages in life.
In other words, it appears that aging is not, as widely perceived, a gradual linear process, but – based on the timing of certain molecular signals – affects all organs at the same time. Aging, therefore, appears to happen stepwise and Cao argues that those individual aging steps, therefore, may be delayable or even completely avoidable by reprogramming of those molecular signals.
Using cells from more than 600 female and male mouse samples at the above-noted five different stages of life, the laboratory discovered 10 main cell types and roughly 200 subtypes which consistently depleted or expanded at a certain age. Age 3-12 months (early adults in mice) very specific subtypes, for example, dropped significantly in numbers in fat, muscle, and epithelial tissues, while at 12-23 months (advanced adults) immune cells increased hugely. Especially B lymphocyte subtypes were affected by this expansion, potentially explaining the increase in inflammatory and autoimmune diseases with advancing age.
How important the immune system appears to be in aging was demonstrated in immunodeficient mice that lacked these B lymphocyte subtypes as well as T lymphocytes affected significant changes in other cell types associated with aging.
We would argue that not unexpectedly (others feel differently 1 ), the researchers also found significant sex-based differences, in turn potentially explaining why women dem -
onstrate a much higher prevalence of autoimmune diseases than men (though men, often, have more severe disease).
If these periodic changes in different cell populations are also confirmed in humans, the potential therapeutic applications are, of course, enormous. And, while this periodic aging pattern cannot be considered a disease – and may not be reversible (but who knows?), it would at least appear delayable and maybe even preventable to a degree.
1. Science News. The Rockefeller University. December 11, 2024. https://www.rockefeler.edu/news/36993-study-reveals-howunexpected-...ell-populations-are-revising-our-understanding-of-theaging-process/
2. Cao J. Science 2024. https://www.science.org/doi/10.1126/science. abf1686
The only blog we are paying as much attention to as Eric Topol’s Ground Truth is the Impact Factor, the amazing blog of Yale’s F. Perry Wilson MD, MSCE. In his December 17, 2024, posting he once again offers a masterpiece in statistical clarity by explaining the curious reasons why taxi drivers apparently are protected from Alzheimer’s disease. And –yes – this is not a misprint; they really appear protected! 1 His blog starts with an explanation of how important the hippocampus in the brain is for converting short-term into long-term memories and for forming spatial memory, the basis for our ability to navigate in complex ways. And when Alzheimer’s starts to become clinically apparent, the hippocampus is the first brain region affected and, with it, memory and orientation.
Already in the year 2000 a British study of London cab drivers reported that their hippocampi were much larger than normal and the longer they had been in the profession, the larger they were. 2 And the only explanation for this finding was that cab drivers’ hippocampi had to work overtime to orient themselves in a city as complex as London (the obvious follow-up study one now would be expect is a determination whether the introduction of computerized navigation systems to the taxi industry may reverse this finding and make taxi drivers again more susceptible to Alzheimer’s).
The blog was motivated by a more recent paper that had appeared in the BMJ3 and assessed disease mortality from Alzheimer’s among taxi and ambulance drivers, which demonstrated – this time in a very large patient population of 8,972,221 – that taxi and ambulance drivers, indeed, demonstrated the lowest death rate from Alzheimer’s among 443 professions during the period of January 1, 2020, and December 31, 2022 3 (see figures on next page).
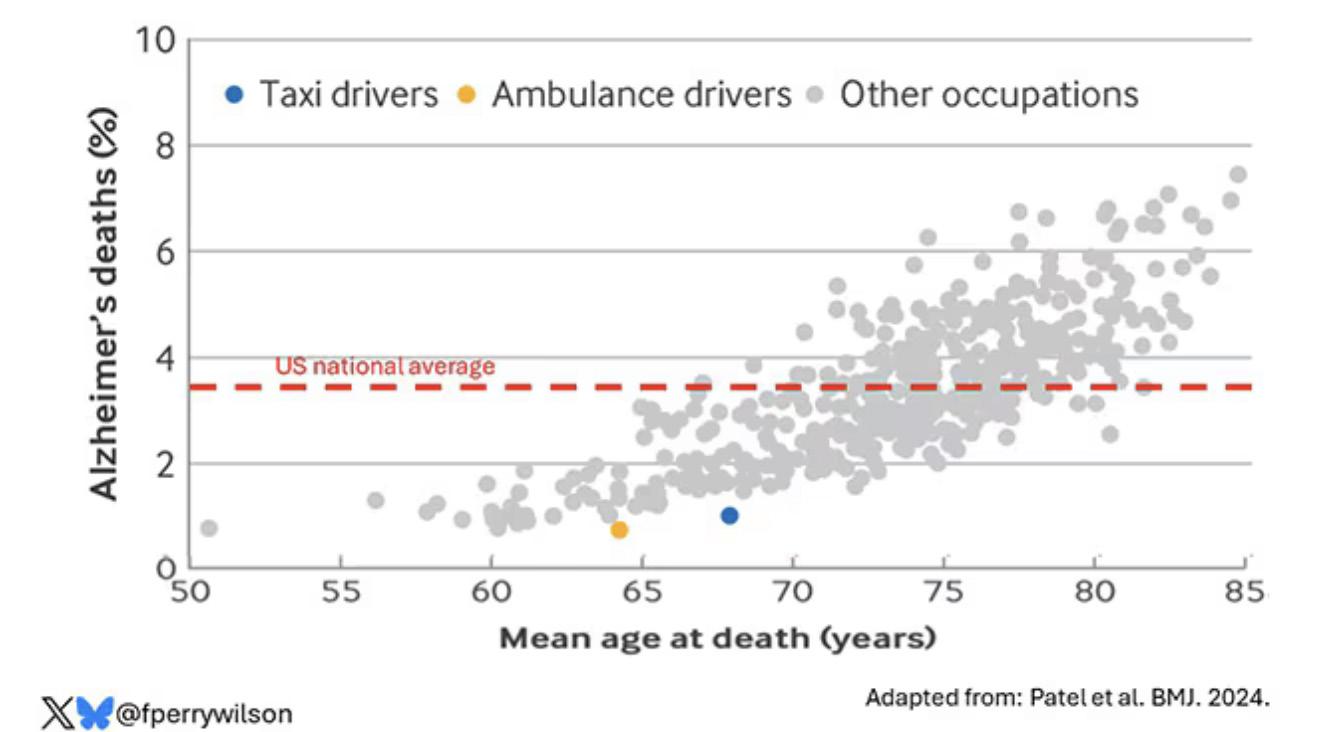
This figure demonstrates as expected a rise in Alzheimer’s in the general population with advancing age (gray circles); but the low death rate from Alzheimer’s (though at relatively young age) of taxi (blue circle) and ambulance drivers (orange circle) is remarkable.
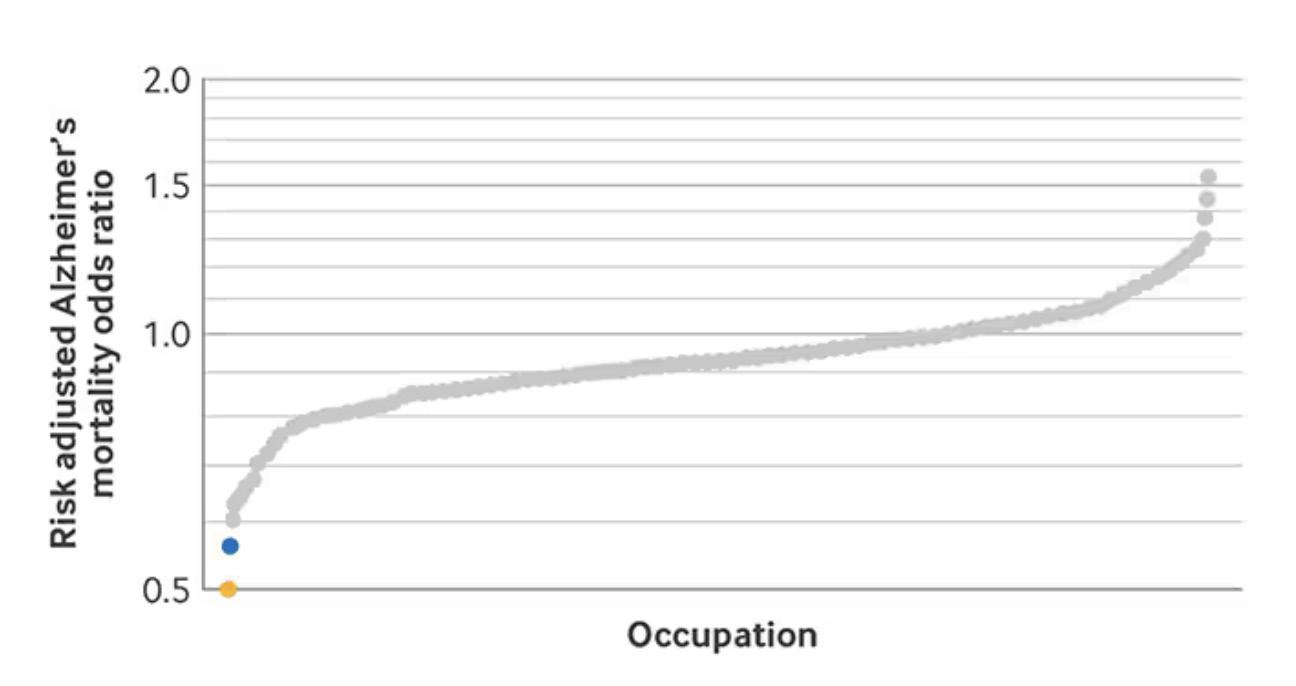
This figure demonstrates that these two professions demonstrated the lowest adjusted risk for death from Alzheimer’s from among 443 professions.
Source: Impact Factor
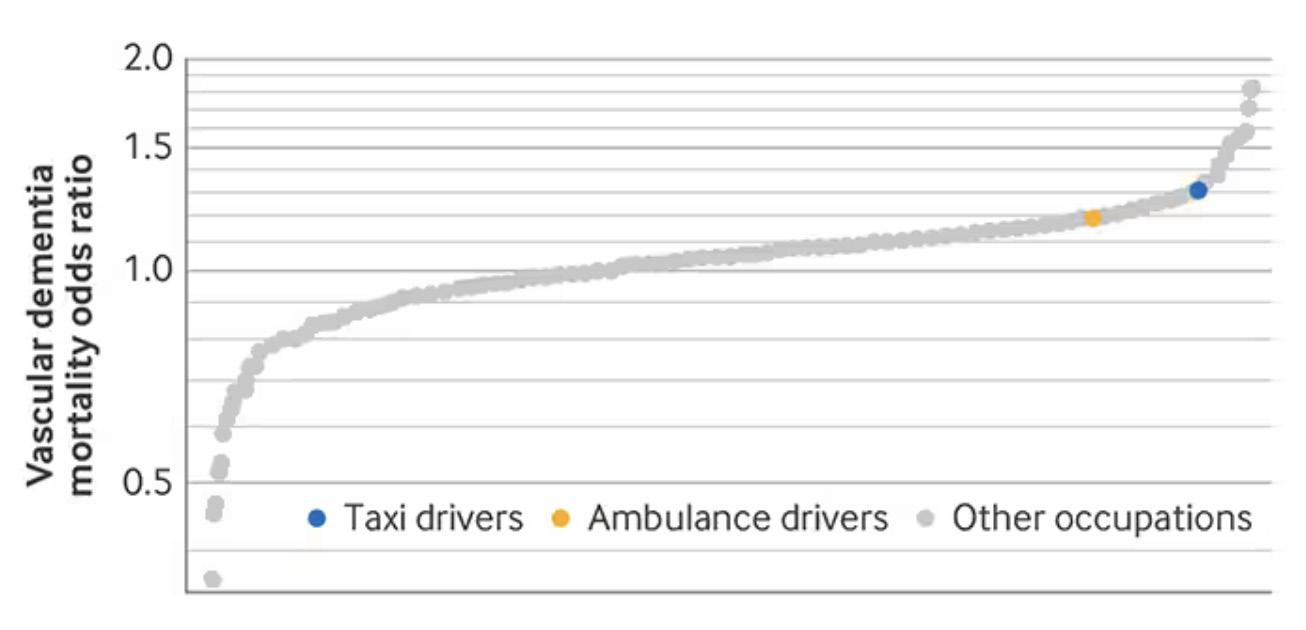
But this figure demonstrates that both professions do not protect from other than Alzheimer’s, offering support to the hypothesis that size of the hippocampus has specific protective effects for Alzheimer’s disease.
Source: Impact Factor
REFERENCES
1. Wilson FP. Impact Factor. December 17, 2024. https://www.medscape.com/viewarticle/curious-reason-taxi-drivers-are-protectedalzheimers-2024a1000n9h
2. Maguire et al., Biol Sci 2000;97(8):4398-4403
3. Patel et al., BMJ2024;387:e082194
A recent article by Andrew Wang, MD, PhD , in Healio attempted to address this question. 1 He noted in his article that ca. 24 million Americans (roughly 5%) are afflicted by autoimmune diseases, 8 million alone by psoriasis, 4 million by Sjögren’s, and 3 million by inflammatory bowel disease. In the U.K estimates are even higher: approximately one in 10. In less than 30 years, the prevalence of positive ANA
tests has in the U.S. apparently increased by almost 50%. And this, of course, has major relevance for reproductive medicine because it means more infertile and pregnant women with autoimmunity.
The causes for this very obvious increase are not very clear. Everybody is, of course, these days talking about U.S. nutrition and the environment, but autoimmunity is now widely perceived as a polygenic transmitted and highly familial inheritance pattern, but with environmental, epigenetic factors controlling which autoimmune disease is then phenotypically expressed against such a polygenic background.
Another reason, according to the article, is that so many different pathways can lead to autoimmunity. Causality, therefore, is almost impossible to establish. Consequently, etiologies of individual diseases are mostly still unclear and an increasing consensus is developing around the concept of a “multi-hit-hypothesis,” involving genetic susceptibility, stress, and poor diets.
Stress appears to work primarily through IL-6 being the dominant cytokine, which is also associated with anxiety and depression, of course two other conditions we have witnessed explode in prevalence over recent years. This and more is all noted in Wang’s article, which is definitely worth the read. Also, you may also want to look up “The relevance of autoimmunity to infertility, and vice versa,” in our Literature For The Fertility Clinic section.
1. Wong A. Healio. March 25, 2024. https://www.healio.com/ news/rheumatology/20240321/source-of-surging-autoimmunity-may-lie-i-a-thousand-cuts

BRIEFING: That “food is medicine” is an increasingly frequently heard phrase in medicine. It, of course, also applies to fertility. With obesity in women and men also increasingly recognized as an infertility diagnosis of its own, especially weight loss from the use of GLP-1 receptor agonist drugs is promising to revolutionize at least this aspect of infertility treatments. The CHR has, indeed, been among the first fertility centers to make active use of this new family of drugs in selected severely obese patients. This section of the VOICE, moreover, caters to the concept of “food as medicine” in a wide variety of ways, from discussing serious nutritional science to offering critical reviews of nutritional supplements in fertility practice, which to a degree has reached almost absurd proportions and, often, not only don’t help, but even hurt pregnancy chances. With a large majority of the CHR’s patients residing outside of the New York City tristate area—many indeed outside the U.S.— this section also attempts to cater to those patients’ nutritional needs when in NYC by offering the CHR’s obviously biased view on the city’s restaurant scene. We hope you enjoy this section of the VOICE.
A quite lengthy Feature article in Nature magazine recently drew our attention because of its title and subtitle: “How ‘miracle’ weight-loss drugs will change the world” and “Models suggest societal upheaval from anti-obesity medicines – but their impacts are hard to predict.” 1 As steady readers of the VOICE by now already likely know, the CHR has been among the first fertility centers to integrate these drugs into routine fertility treatments for severely obese women and men because severe obesity— in either or both partners—not only can be associated with infertility but also with resistance to treatments of infertility.
The author started the article with a relatively short glance into the future to 2030, quoting anonymous analysts as predicting that heart attacks and strokes will be down 20%. A drop in food consumption will leave more money in people’s wallets. Lighter passengers will be saving airlines 100 million liters of fuel each

year. And billions of people will be enjoying a better quality of life, with improvements to their mental and physical health. A Columbia University gastroenterologist is quoted as saying that “short of some crazy unfortunate side effect, these drugs are going to change the world.” And the world needs such change because otherwise, more than half of the world’s population is by 2035 expected to be seriously overweight and/or have diabetes.
And they are already hard at work, in the process changing the world indeed: 12% of U.S. adults – per that article – have already used GLP-1 agonists (see figure below).
Forecasts of potential economic effects are almost mind-blowing; a global market already worth $47 billion is by 2032 to have grown tenfold. US calorie consumption may by 2035, according to experts, drop by 1.3%, severely worrying the food industry. Other industries are also worried. For example, medical devices, such
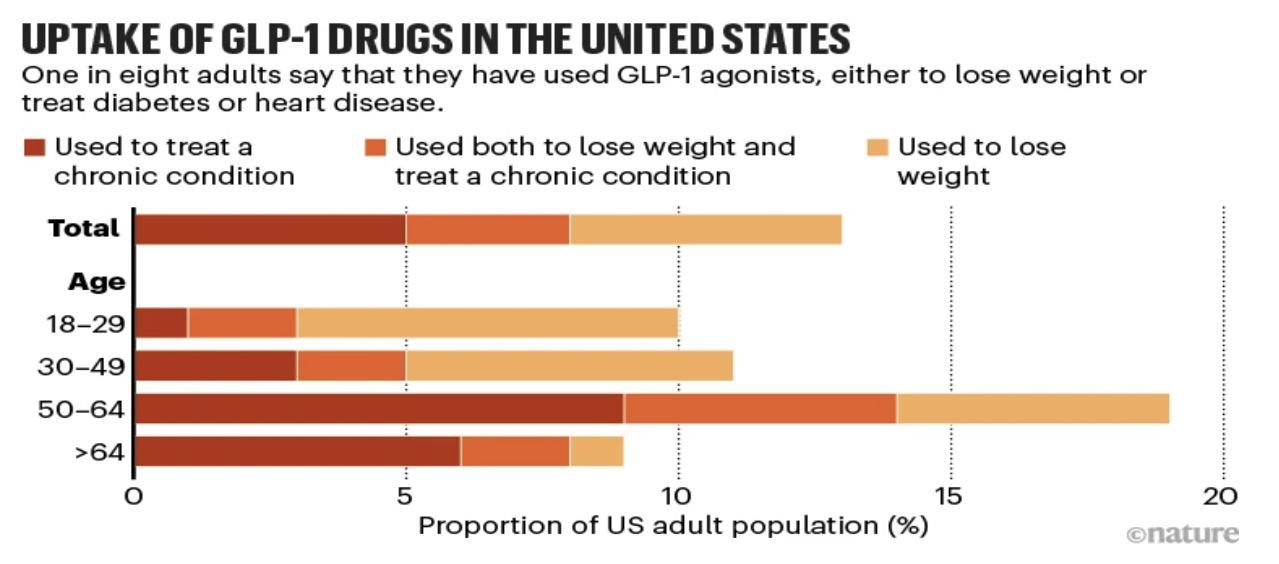
Source: KFF & US NCHS/CDC
as knee implants or treatments for sleep apnea, and car manufacturers expect more demand for smaller cars, etc.
Sister journal Nature Medicine in an unsigned Editorial asked the question of whether GLP-1 drugs are really for everybody? And the answer was that these drugs have emerged as treatment options for medical problems going far beyond diabetes and obesity, it becomes essential to differentiate how genetic, clinical, and sociodemographic differences impact their effects on weight loss (and other medical conditions). 2
Is there an impact on
receptivity and implantation?
This is the question a Review article in Acta Obstetricia et Gynecologica Scandinavica 3 pretends to address but without really offering any significant new information to the reader besides the cliché “key message” that GP-1s hold promise for improving female fertility, especially in obese or PCOS patients. Because of limited evidence, their use should, however, be approached with caution, and no word on either endometrial receptivity (whatever that means) and/or implantation. Clearly a paper worth a “ WORST PAPER AWARD. ”
REFERENCES
1. Reardon S. Nature 2024;635:22 -24
2. Editorial. Nat Med 2024;30:3029
3. SOLA-LEYVA et al., Acta Obstet Gynecol Scand 2024;00:1-9. DOI: 10.1111/AOGS.15010

BMI and PCOS – a self-fulfilling prophecy! A recent study by Chinese investigators in the JCEM ended up being nothing but a self-fulfilling prophecy with the conclusion that a Mendelian randomization analysis produced evidence of a causal relationship between elevated BMI and risk of PCOS, suggesting in addition that severity of PCOS may contribute to elevated BMIs. 1 Really? And how about differentiating between PCOS phenotypes? Isn’t the D-phenotype also called the “lean” phenotype? How many of those were in the study population? Unfortunately, just another example of one of the many worthless “desk-studies” from China flooding our medical journals.
REFERENCE
1. Fabg et al., J Clin Endocrinol Metab 2024;110(1):41-47
Fat cells unfortunately have memory
Maintaining weight loss is quite a challenge, even with GLP-1s. Why that is, has remained mostly unknown. Overcoming this barrier for longterm treatment success is difficult because the molecular mechanisms leading to the rebound in weight have remained largely unknown. Now, however,
in a recent paper by European and U.S. investigators in Nature, an interesting explanation is being reported. 1 Using single-nucleus RNA sequencing, they in human and mouse adipose tissues discovered retained cellular transcriptional changes after appreciable weight loss and persistent obesity-induced alterations in the epigenome of mouse adipocytes that negatively affect their function and response to metabolic stimuli. Mice carrying this obesogenic memory show accelerated rebound weight gain. Moreover, epigenetic memory can explain future transcriptional deregulation in adipocytes in response to further high-fat diet feeding. These findings, at least to a degree, can explain the socalled “yo-yo” effect often accompanying dieting. These observations obviously demonstrate potential directions to overcome rebounding weight gains.
REFERENCE
1. Hinte et al., Nature 2024; 636:457-465

So, the 2024 awards are out and the trend of over- and underrated restaurants by the Michelin awards we have witnessed in recent years continues. And while every rating system is subjective, this year’s awards again raise the question of who these “unknown” Michelin reviewers are and what their review criteria are. That Michelin once again completely overlooked KOLOMAN and kept OJIMI at one star is just as absurd as the two-star overrating of CÉSAR. And how about over 40 years of ignorance of ELIO’s, one of the most amazing Italian restaurants in NYC, with a public which packs the place every day of the year – obviously demonstrating better judgment than the Michelin judges.
And since we already are talking about Italian restaurants, ignoring CIPRIANI Soho and CIPRIANI Uptown is also a shame, even if Michelin does usually not award chain restaurants and the Cipriani restaurants by now can be considered that, as good as they are. But if the CIPRIANIs are chain restaurants, how come the growing number of Daniel Boulud restaurants are not considered that and he – combined – (undeservedly) has probably the largest number of Michelin stars of any chef-owner in NYC.
Boulud is, indeed, an interesting example for the unevenness of the Michelin rating system because his original three-star Daniel restaurant – still considered his crown jewel – used to be a perennial three-star

at almost the level of LE BERNADINE, was rightly downgraded, initially to two and more recently to only a single star. Yet his relatively recently opened Café Boulud – with really poor food and service – also got one star. If a world-famous chef loses two of his three stars either involuntarily or because he no longer gives a damn, it says something. Another way to say it is that real two- and three-star Michelin restaurants usually depend on the permanent presence of their master-chef. Once that master-chef becomes a celebrity chef who opens every year a few restaurants (mostly financed by others) around the world, he ceases being a master-chef and really becomes a manager who runs chain restaurants and should be excluded by Michelin. The same, apropos, also applies to Chef Jean-Georges who also has lost his once three-Michelin star reputation at his crown jewel JEAN GEORGE.
But not everything is bad about this year’s Michelin ranking; we were very pleased to see that JUNGSIK, NYC’s first gourmet Korean restaurant, was finally awarded a third Michelin star. Not only does this restaurant deserve this honor more so than some of the other three-stars, but it also deserves it as the original founding source for the Korean fine dining bonanza NYC is currently experiencing. Everybody expected ATOMIX to get the third start but were it not for the training the chef of ATOMIX received a JUNGSIC, ATOMIX, likely, would not even exist. So, congrats to JUNGSIK, the first new three-star in NYC in 12 years.
All listed restaurants are in Manhattan unless otherwise noted. Like all opinions about restaurants, ours are subjective and are to be understood as such. If you visit one of them, let us know whether you agree with our ratings. We value your feedback.
SYMBOLS WE USE IN OUR RATINGS
$ Inexpensive - Not worth the trip + Overall favorite of the CHR
$$ Moderately expensive
$$$ Expensive
$$$$. Special event expensive
• Good v Special vibe
•• Very good M Michelin starred
••• Excellent V Vegetarian/vegan dishes on
•••• Uniquely delicious the menu
AUSTRIAN
Koloman +/•••/$$/v 16 W 29th Street (212) 790-8970 V; Excellent desserts
Wallsé +/•••/$$/v/* 344 W 11th (212) 352-2300 V; Excellent desserts
CHINESE
Hwa Yuan Szechuan +/•••/$$/v 42 East Broadway (212) 966-6002 V; Authentic Szechuan
Mr. Chow Downtown +/••/$$$/v 121 Hudson St., Tribeca (212) 965 9500 V Uptown 324E, 57th Street (212) 751 9030 V
CONTINENTAL
425 •••/$$$/v
FRENCH
425 Park Avenue (212) 751-6921 V; Gorgeous restaurant
Le Gratin ••/$$ 5 Beekman St. (212) 597-9020 V; Try the gratin potatoes
Le Charlot +/•• /SS 19 E 69th St. (212) 794-6419 V; Best steak au poivre & Thai mussels; great desserts
Le Bernadine +/••••/$$$$/ MMM 155 W 51st (212) 554-1119 V; Mostly seafood. Likely the best NYC restaurant
ITALIAN
Cipriani Downtown +/••/$$/v 376 West Broadway (212) 343 0999 Great food, beautiful people & Uptown 781 5th Avenue (212) 753-5566 Great food and high society
Elio’s +/•••/$$/v 1621 2nd Ave. (212) 772-2242 Best Italian home cooking and where everybody meets
Principe ••/$$/v 50 West Broadway (212) 335-0509 V; mostly seafood but one of the best chicken dishes
Sistina •••/$$$ 24 E 81st St. (212) 861-7660 V; Amazing wine list
FRENCH-ITALIAN
Café Carmellini •••/$$$$/v 250 Fifth Avenue (212) 231 9200 V; Gorgeous place, top service; sophisticated and adventurous food
JAPANESE
SUSHI
Sushi Ann +/••• /$$$$
8 E 51st St. (212) 755-1780 V; Best quality fish; make reservation at the bar
GENERAL
Sakagura +/•••/$$
211 E 43rd St. (212) 953-7253 V; Amazing food; Best sake selection
Yakitori Torishin +/+++/$$$/M 362 West 53rd Street (212) 757-0108 Unique and amazing skewer restaurant KOREAN
Jungsik •••/$$$$/ MM 2 Harrison St. (212) 219-0900 Where NYC’s Korean restaurant revolution was born …
Oiji Mi +/•••/$$/v / M 17 W. 19th St. (212) 256-1259 … and has continued
GREEK
Elias Corner (Queens) ••/$ 24-02 31st St. (718) 932-1510 Mostly seafood
HAMBURGERS
Jackson Hole Burgers (the “original”) +/••/$ 232 E 64th St. (212) 371-7187 Not a place for vegetarians
MIDDLE EASTERN-ISRAELI
Dagon ••/$$ 2454 Broadway (212) 873 2466 Best hummus in NYC
NEW YORK JEWISH DELI
P. J. Bernstein’s Deli •/$ 1215 3rd Avenue (212) 879-0914 All the great classics; pastrami, chicken soup PERUVIAN
Mission Ceviche •••/$$ 1400 2nd Avenue (212) 650-0014 If you like Peruvian –the best PIZZA
San Matteo Pizzeria e Cuccina ••/$ 1559 2nd Avenue (212) 861-2434 True Napoli POLISH
Karczma (Brooklyn) +/•/$ 136 Greenpoint Avenue (718) 349-1744 Great authentic Polish food – and dirt-cheap
ROMANIAN-JEWISH
Sammy’s Roumanian Steak House** $$ 112 Stanton St. (212) 673 0330 Authentic JewishRomanian Steak House, with entertainment
UKRAINIAN/RUSSIAN
Caviar Russe +/••••/$$$$/ M 538 Madison Avenue (212) 980-5908 V; Most underrated restaurant in NYC
Russian Samovar •/$/v 256 West 56th St. (212) 757 0168 Great Russian/ Ukrainian food and music
Any suggestions and/or comments, please write to social@thechr.com



760 Madison Avenue (between 65th and 66th Street)
Phone: (212) 207-1902
After moving the restaurant and store from their old location on Fifth Avenue to new grounds in the brand-new Armani building, the new restaurant is only a few weeks old but already pretty busy. We have visited twice for dinner and, therefore, cannot comment on lunch service which, due to the restaurant’s location, may actually turn out to be the restaurant’s busiest time.
One enters the restaurant to the north of the store at street level through its own private entry straight into the bar adjacent to the two-story main dining room (see above). The restaurant has a smaller second room at ground level and a second-floor dining area above the bar.
The décor is functional, modern-elegant; one can say, typical Armani-style! Tables are covered by white linen which is, of course, immediately ironed once placed. The restaurant very obviously perceives itself as a fine dining establishment.
But this is unfortunately where the good news ends. Our first visit took place in the first week after the opening, and the extremely incompetent service could be attributed to the newness of everything (the incompetence was really striking). And, though during our second visit the service had greatly improved (most of the original waitstaff had apparently been replaced), the food, unfortunately, had not changed. It was still pretty awful.
And here is where things get a little complicated because the food is difficult to describe. It’s supposed to be Italian and to a degree it, of course, is. Executive chef Antonio D’Angelo’s home was Naples, but we sensed surprisingly little Neapolitan influence in his cooking. Seemingly a very friendly and nice guy, if he is responsible for the menu, he appears to be lost. He, moreover, is trying much too hard to cook fancy-Italian.
Some cuisines simply don’t lend themselves as much to “fancy” like the French or Japanese cuisines. Korean restaurants have shown us in recent years how spectacularly “fancy” Korean food can be. Italian food, especially in the south, seems to a degree incompatible with “fancy,” paradoxically strongly contributing to its worldwide popularity. There is, of course, a reason for Elio’s being our favorite Italian restaurant in NYC; it is anything but fancy, but every dish is usually delicious.
Some Italian restaurants succeed in upscaling, but they are usually the ones that understand the limits in upscaling the Italian cuisine allows. Armani Ristorante exaggerates its upscaling efforts to such a degree that flavors and plate compositions at times become almost absurd. The risotto was drowning in an overbearing and also oversalted mushroom broth. A primi of seafood was, in contrast, overcooked and really tasteless, and a pasta was again drowning in sauce, except that this time the dish was tasteless.
The menu is small, and one of those menus where one has a hard time deciding what to order, not because one wants to taste everything, but because nothing really looks interesting or familiar. In short, no stars so far for Armani/Ristorante and we, therefore, do not recommend a visit.
964 Lexington Avenue (between 70th and 71sth Street) (•/$ ). Phone: (212) 390-8106
What a contrast in comparison is this new (we’ll come back to this term) restaurant, right across from one of our favorite NYC Italian places, Bella Blue (yes, we don’t only like Elio’s!) in a long empty street-level space, in its last occupation a seafood restaurant, and a coffee bar before that.
And it is everything Armani/Ristorante is not: Though obviously a brand-new restaurant, it proudly pronounces on its facade “Since 2008,” which is when Chef-owner Harold Moore opened his first Café Commerce in the West Village. This restaurant, however, did not last too long. The current reincarnation, therefore, is not only a new restaurant in its location but, after a long absence, in many ways also a new concept.
It is a small space with allegedly only 55 quite cramped seats (including a long bar where the full menu is served). It does not try to build up expectations by its simple pseudo–Art Deco décor, its atmosphere, and its menu. It definitely does not want to be fancy; all that it apparently wants to be is a new neighborhood place (based on how many new restaurants have opened since the fall it seems that the restaurant industry has rediscovered the Upper East Side). The restaurant describes itself as a French Bistro, with several dishes attesting to Moore’s past French training with such celebrity chefs as Daniel Boulud and Jean-Georges Vongerichten , and his residency as Chef at Montrachet.
And rather than disappoint, it surprises. We basically really liked all the French dishes we tasted, including desserts, but what we liked most had very little to do with French cuisine and would have much better fitted into a Jewish deli, an excellent chicken soup, so thick with meat and vegetable, it almost could be a main course, and a real chicken schnitzel, like I thought one could find only in really good Israeli restaurants.
So this place we really liked on both of our visits and, therefore, very much recommend. We are not yet willing to elevate this place into our most favorite restaurant elite list yet, but would not be surprised if this were to happen after a few more visits.
BRIEFING: The VOICE in this section offers commentaries on a broad survey of recent articles in the English literature which the CHR found of interest regarding the practice of clinical infertility, even if, at times, not immediately applicable to daily clinical practice. Articles are mostly chosen for two reasons: their potential translational value for immediate clinical practice or to help in determining where clinical practice might evolve to. Translational research has been at the center of the CHR’s success since its founding in 1981.
*Further evidence that the time has come to individualize the timing of ovulation triggers and egg retrieval
There are not too many clinical practices left in IVF that have remained unchanged from the earliest days of the procedure. One of those is the worldwide practice of triggering IVF cycles at lead follicle sizes of 18-22mm on average. Moreover, if deviations occur, they usually occur upwards to larger sizes, rather than downwards to earlier retrievals at smaller sizes. The latter fact is likely driven by the earliest stages of IVF, when IVF cycles were still stimulated with clomiphene citrate, and best trigger sizes were considered to be approximately 22-24mm.
The switch to 18-22 mm occurred only with the introduction of gonadotropin stimulation to IVF in 1981 by the first IVF clinics in the U.S. 1 and Australia. 2

And that trigger range has since 1981 become a dogma of IVF practice all around the world, only challenged by investigators at our clinic in NYC, the Center for Human Reproduction (CHR, founded in Chicago in 1981), when we in molecular studies of older patients above age 43 discovered that follicles luteinize progressively earlier as women age 3,4 and, therefore, concluded that with advancing female age egg retrievals— and, therefore, ovulation triggers—had to be administered earlier and earlier. And it is now indeed the 10-year anniversary of the radical step we took at the CHR in 2015 to age-adjust the timing of ovulation triggers in first IVF cycles to the age (and functional ovarian reserve, representing ovarian age) of patients in a process we have named Highly Individualized Egg Retrieval (HIER).
This step has been central to the CHR’s success in treating older patients, with women above 43—and especially above age 45—routinely being triggered at lead follicle sizes as small as 10-12mm. This step was also crucial in discovering additional age-dependent changes in folliculogenesis which had not been known before 5 (more on that below).
This lengthy introduction is necessary to understand the importance of a recently published paper by a consortium of British investigators in Nature Communications, which— with the use of artificial intelligence (A.I.)— demonstrated that best follicle sizes are not the same for everybody. 6
In a multi-center study, the investigators used data from 19,082 women (before any fertility treatments) from 11 European IVF centers and harnessed explainable A.I. to identify follicle

sizes that contributed most to relevant clinical IVF outcomes. And especially considering our 10-year experience with HIER, their results were interesting because what they discovered was that follicle sizes at retrieval mattered. Specifically, intermediate-size follicles were— for example—most important in determining the number of mature oocytes subsequently retrieved. Maximizing these mid-size follicles by end of ovarian stimulation also led to an improved live birth rate. Unsurprisingly they also found that larger follicle sizes, especially those over 18mm, were, based on premature progesterone elevations, obviously—as we had reported in older women 3 —associated with premature luteinization. Also, unsurprising and previously reported by us in older women, 3,4 the diagnosis of premature luteinization negatively impacted live birth rates in fresh embryo transfer cycles.
Unfortunately, the investigators in this study only differentiated between patients under and above age 35, thereby not really allowing for the detailed age associations we reported with increasingly declining best follicle sizes at ovulation trigger in older infertility patients. Even though their data, therefore, do not directly confirm the CHR’s HIER data in older women, they nevertheless appear to support them. For example, that best oocytes—regarding maturity as well as quality—are not necessarily in the biggest follicles became obvious years ago in older patients. Some very tiny follicles at times produced perfectly mature metaphase 2(M2) oocytes, while bigger ones in the same cycle cohort might yield still immature M1 or even more immature germinal vesicle (GV) eggs. The CHR’s investigators are, therefore, currently attempting to identify markers on follicles during vaginal ultrasound examinations that may help in identifying mature follicles even at very small sizes.
Moreover, CHR’s practice of HIER more recently, as alluded to above, allowed its investigators to discover yet another previously unknown physiologic phenomenon of human oocytes that breached yet another dogma in reproductive medicine. The three major maturity grades of oocytes M2, M1, and GV, since the establishment of IVF have been considered fixed in their respective clinical potentials: Mature M2 oocytes have been widely considered the overreaching
goal of all IVF cycles, while the most immature GV oocytes in most IVF clinics to this day are mostly automatically discarded because maturation attempts in vitro have in general been very unsuccessful.
Because the CHR serves a unique, very poorprognosis patient population, in which every fertilizable oocyte is disproportionally valuable, we have been performing so-called rescue in vitro maturation (rIVM) on all immature oocytes retrieved for over 10 years. 7 In this process, we started to suspect that the clinical efficiency of M2, M1, and GV oocytes to produce good quality embryos did not appear to remain stable with advancing female age. A formal prospective study then very recently confirmed this observation. 5 It demonstrated that mature M2 oocytes lost significant ability to produce good-quality embryos with advancing female age, while very immature GV oocytes greatly improved in their ability, further supporting the hypothesis that evolution favors increasingly earlier retrievals as women age.
That this hypothesis is likely correct can be also deducted from the observation that practically all fertility-related biological processes are controlled by inhibition. Luteinization and ovulation of follicles are good examples: As women age, inhibitory controls progressively weaken, resulting in above-noted earlier and earlier premature luteinization and premature progesterone rises and, ultimately, in shorter and shorter menstrual periods. In IVF cycles, this development is reflected in their shortening length with advancing female age. Another observation pointing at disinhibition as a sign of follicular stress is the well-known observation that follicle growth increases with premature luteinization based on increases in progesterone levels. 8
In other words, premature luteinization elicits a stress response in the affected follicle, resulting in increasing disinhibition, with the follicle demonstrating a growth spurt. Follicles at similar sizes in the same follicle cohort, therefore, may be under different stress levels. Here discussed paper by Hanassab et al., therefore, reaffirms by demonstrating the importance of early rises in progesterone at all ages the importance of premature luteinization in harming egg quality at all ages.

The single most important message this paper offers, however, is that the dogma of a uniform 18-22mm trigger sizes of leading follicles in all IVF cycles should be considered a bygone. Individualization of trigger and, therefore, retrieval timing is not only important in older women but affects oocytes and, therefore, embryo quality at all ages.
REFERENCES
1. Jones et al. Fertil Steril, 1982, 38 (1) 14–21
2. Trounson et al., Science 1981;212(4495):681-682)
3. Wu et al., J Endocrinol 2015;226(3): 167-180
4. Wu et al., J. Ov Res 2018;11:23
5. Nicholas et a., iScience 2023;26:107308
6. Hanassab et al., Nat Commun 2025;16:296
7. Lee et al., Endocrine 2016;52:165-171
8. Cortés-Vasquez et al., JBRA Assist Reprod 2022;26(3):531-537
cryopreservation cycles?
This is the question investigators from the Mount Sinai IVF program in NYC recently addressed in a paper in RBMOnline , 1 in which they compared young women undergoing social (sometimes called “planned”) egg-freezing who had used contraceptives before their cycles with women who had not used any contraceptives. Outcome criteria was number of obtained oocyte-cumulus complexes retrieved and mature MII oocytes that were cryopreserved in a cycle. And after adjustments for confounders, a multivariate analysis found no difference between study and control groups or individual contraceptives.
Though this study has several shortcomings, including its retrospective nature and mostly reliance on patient memory, the finding can be considered as reassuring, on a practical level suggesting that prior utilization of especially hormonal contraceptives does not seem to require a prolonged washout period.
REFERENCE
1. Hernandez-Nieto et al., Reprod Biomed Online 2024(3):104105
IMPROVING EMBRYO QUALITY DURING RESCUE IVM Though this study still must be considered to be preliminary since it was only published as an abstract at the annual ASRM meeting, 1 it nevertheless deserves attention and follow-up. Investigators from Penn State University reported that in vitro maturation of immature oocytes (also frequently called “rescue” maturation) improves oocyte and embryo quality in older women (age 38 and older) if culture media are supplemented with nicotinamide mononucleotide (NMN) and this effect may be mitochondriamediated, as mitochondria demonstrated improved morphology and function.
While in vitro maturation, normal fertilization, and cleavage of immature oocytes from older women at ages 38 and above were not enhanced, there were substantial improvements in effective embryos (53.3% vs. 29.4%), high-quality embryos (31.7% vs. 8.8%), blastocyst formation (31.2% vs. 6.2%), and high-quality blastocysts (70.0% vs. 23.5%) (all P < 0.05). Transmission electron microscopy revealed increases in number of mitochondria with intact inner and outer membranes and clear cristae (P < 0.05). Moreover, fluorescence signal quantification analysis demonstrated significantly higher Tetramethyl rhodamine ethyl ester (P < 0.05) and mitochondrial activity and membrane potential by MitoTracker (P < 0.05), and fluorescence intensities. Single-cell transcriptome analysis identified 277 significantly upregulated genes and 183 significantly downregulated genes in the supplemented group. Gene Ontology (GO) analysis of differentially expressed genes showed significant enrichment in mitochondrial-related terms such as “positive regulation of protein targeting to mitochondrion” and “mitochondrial matrix.” Real-time quantitative PCR results confirmed the upregulation of oxidative phosphorylation genes (ATP6V1D, ATP5MC1, PPA1, NDUFC1, CYC1, NDUFA12, and NDUFB3) in IVM oocytes of the principal aged study group, validating the accuracy of the RNA-seq data.
Though numbers are small, the data are interesting, not the least because they make physiological sense. As the authors noted, declines in oocyte quality are a primary factor in reduced fertility in women of advanced maternal

age. Older women have also been demonstrated to exhibit an increased prevalence of abnormal mitochondria and reduced nicotinamide adenine dinucleotide (NAD+) levels. Restoring and enhancing oocyte NAD+ levels could, therefore, be a promising intervention.
The peer review process at Human Reproduction is usual quite good in comparison to most other medical journals in the fertility field. But this time, the journal really got a black eye for publishing one of the most ridiculous papers in some time. The heading of the paper already says it all: “Empirical use of growth hormone (GH) in IVF is useless: the largest randomized controlled trial.” 2
The study basically investigates whether supplementation with GH in a general population of infertile women in an antagonist IVF cycle improves outcomes. The absurdity of this study design is the same as in a hypothetical study of aspirin use which tests in a prospectively randomized study of a general population (i.e. a population that may or may not have a headache) whether aspirin, indeed, does improve headache. Simply idiotic!
A medical treatment can show effectiveness only if the target population is affected by the medical problem the treatment is supposed to take care of. In an IVF cycle this means that GH supplementation makes sense only if insulin growth factor-1 (IGF-1) levels are abnormally low because GH acts on small growing follicles during folliculogenesis synergistically with FSH through IGF-1. And since abnormally low IGF-1 levels in infertile women are very rare, this study—with great likelihood—treated in a large majority women with GH who did not need it. Who can then be surprised about the conclusion of the study that GH showed no effects!
We, indeed, in these pages have repeatedly pointed out that the persistent controversy regarding GH supplementation in IVF is likely exclusively due to the fact that the different studies with varying outcomes just reflect the different prevalence of abnormally low GH levels in study populations.
This article, however, also raises another important point, namely positive biases affecting the peer review processes assuming that every prospectively randomized study represents a pinnacle of evidence. And that is not only false but there is literature that demonstrates the dangers of poorly executed and/or interpreted clinic trials because their results are so overestimated. 2 This paper has a special gall trying to blow up its importance even further by claiming to be the biggest trial of GH use in IVF ever. In other words, this makes it the biggest screw-up on a GH hormone study in infertility ever. Not a great compliment!
Related, another recent paper is worth mentioning. Investigators from several countries attempted to determine how the IGF system participates in the midcycle surge in women. 3 As noted above, IGF-1 signaling is well known to affect follicular function during especially small growing follicle stages, but also to a lesser degree beyond. How it is involved in the ovulatory peak which greatly affects granulosa cell function is still largely unknown. What this study now suggests is that downregulation of IGF signaling at that time is mediated by increases in the expression of the inhibitory protein, STC1, which then is instrumental in the sudden cessation in GC proliferation and onset of differentiation during the ovulatory peak.
1. Mourad et al., Hum Reprod 2024; doi: 10.1093/ humrep/deae251. Online ahead of print.
2. Kis D. Medthority. March 30, 2023. https://www. medthority.com/news/news-trends/clinical-trials/ how-can-flaws-in-clinical-trial-design-conduct-andreporting-impact-clinical-decision-making/
3. Bøtkjær et al., J Clin Endocrinol Metab 2024;110(1):e160-e167
*DO ARTIFICIAL
(A.I.).
So claims the industry that is selling A.I. products and closed incubation systems with time-lapse— which, of course, has commercial interests— and, unfortunately, so do some colleagues and institutions, which often spend fortunes on this equipment and software. 1 But, as we have repeatedly noted in these pages, major recent studies on A.I. 2 and time-lapse 3 have demonstrated no outcome benefits for IVF cycles

(while, of course, further increasing costs for already widely unaffordable IVF).
1. Singer T. Northwell Health. https://r1.marketingpages.com/p/7N0G-6LW/q424-improving-ivfoutcomes-with-ai-and-time-lapse-monitoring-?dm_ i=7M0G,6WXA,1E6J9V,U3J6,1
2. Kieslinger et al. Nat Med 2024;30:3059-3060
3. Bhide et al., Lancet 2024;404(10449):P256-265
One would think that the question whether fresh or frozen-thawed embryo transfers in subsequent cycles were better treatment options, was finally resolved, but no: F S Reports 5(4):2666-3341 decided to publish another study on the subject after accepting a retrospective single center study involving 8,319 autologous first blastocysts (in absence of PGT-A). Among those 6,755 transfers were fresh and 1,564 were FETs (frozen-thawed transfers) after freeze-all cycles. 1
Considering the retrospective nature of this study, one cannot be surprised by significant differences in patient populations between the two study groups (Table 1 of study). Though the authors apparently made appropriate statistical adjustments, this finding alone, however, raises serious questions about the validity of the study results because one, furthermore, must assume that there were good clinical reasons why patients ended up in one or the other group.
Moreover, without explanation, the study retrospectively investigated IVF cycles only between January 1, 2015, and December 31, 2020. Considering how much IVF practice has changed since 2015 – and even since 2020 – the meaning of any results from such a long time ago for practice now must be seriously questioned. After all, the concept of freeze-all cycles was born around 2014, 2 and by 2020 was already by many refuted. 3
Though the paper’s conclusion that there is no major difference between both approaches cannot be denied, this still does not allow for the conclusion the authors reached that a final decision about which approach should be taken should be left to patients and physicians. While that in medicine should probably in all circumstances be the rule, assuming both options are really equal, why would anybody choose a
more expensive option which, in addition, would delay time to pregnancy? The correct medical recommendation from physician to patient— unless there exist special circumstances— therefore should be fresh transfers.
1. Pavlovic et al., F S Reports 2024; 5(4):2666-3341
2. Shapiro et al., Fertil Steril 2014;102:3-9
3. Ben Rafael Z. Hum Reprod 2020;35(10):2179-2184
Even though the ASRM has by now already acknowledged that PGT-A does in a general population not improve anything in IVF cycles (and, indeed, in certain subgroups affect outcomes adversely), it is always amazing to read some of the stuff some colleagues are coming up with to, still, make claims of outcome improvements for PGT-A and offer reasons to continue utilizing PGT-A in association with IVF. The two most prolific now finally got together and – somehow – convinced a BMJ-group genetic journal to publish their Opinion article, which they base on “mining the SART database.” 1
And, as expected, the article can only be described as pathetic, offering repeatedly by now widely rebutted data interpretations and comments that simply do not make sense. We understand that it is difficult to have been so wrong for such a long time as these two gentlemen, especially if—as in the case of one of the two authors for the longest time having been considered the “Wunderkind” of PGT-A (the other author was a relatively late convert)— never really knew what he was talking about.
It is also telling that this article appeared in the genetics and not the infertility literature. And it, indeed, apparently is the third article in this brand-new journal, suggesting that the article was likely (rightly) already repeatedly rejected by other journals. One characteristic of what now can be described as “the PGT-A disaster” was the ignorance of basic biological facts the genetics community has exhibited when it comes to chromosomal testing of preimplantationstage embryos. They, indeed, don’t even appear to know how to correctly define “mosaicism.” And, since the infertility field viewed them as “the experts” the field was relying on, there was nobody with authority around to stop the disaster from continuing.

Clearly this paper is almost a demonstration project for a WORST PAPER AWARD in the VOICE
A Fertility and Sterility publication in vivid contrast, indeed, addressing the mosaicism diagnosis in human embryos, comes from Russia, with Ilya Volodyaev and collaborators, by training a physicist, and in practice a senior embryologist, who actually contributed a wonderful article to the November/December issue of the VOICE . As in his article for the VOICE , this article for F&S also offers some clarity between true biology and artefacts in chromosomally testing of embryos. Though he in our opinion still maintains a too rosy viewpoint of PGT-A, his argumentation—in contrast to the prior paper—is sharp and logical. A worthwhile read!
And here is a technically interesting news item: Researchers in a basically interesting research letter in Fertility and Sterility reported blastocyst re-expansion at 1 hour after trophectoderm biopsy may be for an embryo predictor of live birth. 2 Once can only hope that proponents of PGT-A now take this as another indication to recommend PGT-A to their patients!
Less interesting was another PGT-A paper in the same journal issue in which investigators produced what we have come to call a “selffulfilling prophecy paper” (i.e., a paper where the answer a study is supposed to find is too obvious to even waste the effort). Here the investigators from California were apparently surprised to find out that aneuploidy rates in cycles where embryos underwent PGT-M and PGT-A had the same age-specific aneuploidy rates as women undergoing only PGT-A. 3
Really?! Did they really ever believe that PGT-M could affect aneuploidy rates in any potentially conceivable way? Too absurd!
And, finally, another technically interesting paper from the U.S. Juno-Genetics Laboratory and others which reported that certain PGT-A platforms may be able to detect inherited small copy number variants (CNVs) with very high specificity without prior knowledge of parental status and were either confirmed as benign, likely benign, or a variant of uncertain relevance. Since the study involved basically couples with no known pathological CNVs, the authors correctly
noted that the fact that no pathological or likely pathological CNVs were detected does not mean that these platforms may not also be able to detect those. 4
1. Munné S. Griffin DK. BMJ Connections Clin genet Genomics 2024;1:e000003 [WORST PAPER AWARD]
2. Elkhatib et al., Fertil Steril 2024;122(6):1147-1149
3. Martel et al., Fertil Steril 2024;122(6):993-1000
4. Itturiaga et al., Fertil Steril 2024;122(5):789-798
Here is for a change an interesting paper in RBMOnline. 1 Chinese investigators in a retrospective cohort study of Chinese numbers (n=11,738) of women, investigated what happens if only 1 good blastocyst is transferred or this good blastocyst gets for the transfer a poor-quality second blast as co-traveler. And the results were not surprising but still quite remarkable: Two embryos did better than one embryo, as the live birth rate was higher with good/poor embryo double transfer than with only one single good blast. Moreover, this higher pregnancy rate was also associated with a higher twinning rate (41,4% vs. 1.8%).
There are two important lessons to learn from this paper: (i) As already noted, two embryos are always better than only one in establishing pregnancies and achieving deliveries. (ii) But there is also a second important lesson: while we don’t know how good or bad our Chinese colleagues were in evaluating the quality of their embryos (especially considering the very high twinning numbers), one must wonder whether they did not underrate their embryos by morphology. The ultimate lesson, however, is an old one: even pretty ugly embryos at times still give you perfectly fine pregnancies and deliveries. So, don’t be too generous in discarding embryos!
And here is a second paper in which embryos were mixed up on purpose. Here the question was whether there was a difference in outcome after a fresh 2-embryos transfer on day 3 or a fresh single day-3 embryos plus a subsequent frozen-thawed blast. And the answer was, in women under age 38 the combination of 1 fresh day-3 and one frozen-thawed blast produced a higher live birth rate and lowered the twinning rate in comparison to 2 fresh day-3 embryos being transferred.

To be honest, we have our doubts about this paper. Even the authors acknowledge some quite important limitations to their data. So, we would not put too much onto this manuscript’s conclusions; but it certainly attempted to address an interesting question.
REFERENCE
1. He et al., Reprod Biomed Online 2024;49(3):104104
2. Wanh et al., Hum Reprod 2024;39912):2702-2710
Everybody, of course, knows that female age represents the single, likely, most crucial factor in determining IVF cycle outcomes and male age plays comparatively only a very limited role. How both partners’ ages interact, however, so-far has not been investigated until recently, when UK investigators tried. What they found was quite interesting: In fresh IVF cycles, male age mattered more than one might have expected starting at age 40 if the female was between 36 and 39 years old but did not matter at all if the female was under age 35 or over age 40. 1
The authors of the paper failed to explain these findings, and we have to acknowledge that we also thought hard how these female agedependent differences could be potentially explained without coming up with a potential explanation. The only possible explanation that comes to mind is that at both female age extremes—very young and older—IVF cycle outcomes are poorer than in-between these two extremes. Maybe the male at these extremes does not matter as much anymore because egg issues prevail. But since finding even a workable hypothesis for the age-related findings in this study are difficult, a degree of skepticism regarding this paper appears in place.
The authors must be given credit for, themselves, offering a substantial list of shortcomings of their study, which likely—combined—have to be considered responsible for an “accidental” and, therefore, likely irrelevant finding. The likely conclusion, therefore, has to be that our understanding of the effects of female and male age on IVF cycle outcomes has not changed much as a consequence of this study.
REFERENCE
1. Datta et al., Hum Reprod 2024;39(1):2491-2500
In the journal’s Fertility Battle series, Fertility and Sterility recently addressed the question of whether egg sharing is ethical, with two proponents and three opponents contributing to the discussion. 1 Considering the explosive growth the donor egg bank industry has been experiencing, to us this question has become mute. Isn’t what frozen egg banks do, egg sharing?
Diane Tober , an associate professor of Anthropology at the University of Alabama and the Institute for Social Science Research, just published a 2025 edition of her Google Book “Eggonomics” (see figure above), which offers an interesting and, at times, controversial perspective on egg donation.
The VOICE would be interested in a review of the book, if anybody is interested in writing one (up to 500 words). 2
Also worth mentioning here, was the actually 2 nd oral presentation at the 2024 ASRM meeting in Denver, 2 in which Sarah Holley, PhD, a psychologist at the University of California, San Francisco, presented very interesting data on how egg donors apparently feel after donations. 3
The abstract summarized the study as follows: The average age of the studied donors was 34.9 years old (range: 24 – 47 years). Participants had donated an average of 2.8 times (range: 1 – 8). A large majority (88.3%) felt positively (i.e., proud,
good, happy) about having been a donor. Most (58.3%) were not concerned about their health or future fertility, though a minority (23.6%) voiced concerns. Most donors (73.6%) were curious about the child(ren) born from the donation, though only 10.3% reported thinking repeatedly about the experience or the potential children from their donations. Interestingly, about half (46.8%) expressed a desire to someday meet the child(ren), while two thirds expressed willingness to meet if requested. Regarding release of their identity to a child (age 18 or over) upon request, 62.2% expressed willingness to have their identity disclosed and an additional 21.7% expressed uncertainty; only 16.1% reported they would not be willing to have their identity disclosed.
And finally, the practice committees of ASRM and SART published an updated opinion guidance document on gamete and embryo donation. 4 Always worth the read!
1. Shah et al., Fert Steril 2024;122(6):984-990
2. https://books.google.com/books?hl=en&lr=&id =YuEfEQAAQBAJ&oi=fnd&pg=PT11&dq=Holley+S R.+Egg+donors.+Fertil+Steril.+2024&ots=xRAQT oN-qV&sig=Iu1GalufZDjudZ2VEVDb9Pr-qoI#v=onepage&q&f=false
3. Holley et al., Fertil Steril 2024; DOI: 10.1016/j. fertnstert.2024.07.072. Abstract O-2
4. Practice Committees of ASRM and SART. Fertil Steril 2024;122:5(:799-820



A recent Danish paper in Cell Reports Medicine may really turn out to be game changing for at least some males with oligospermia, 1 and here is why: Sperm production is dependent on proper Sertoli-germ cell interaction. For several reasons, the Danish investigators hypothesized that receptor activator of nuclear factor κB ligand (RANKL) activity in Sertoli cells, therefore, may influence spermatogenesis.
A RANKL inhibitor called denosumab (brand name Prolia and others) is already an FDA approved human monoclonal antibody to treat osteoporosis. The investigators, therefore, explored its use. Basically, as they had hypothesized, treatment increased testicular weight, inhibin B, and germ cell proliferation in ex vivo testis cultures and in vivo in a humanized RANKL mouse. Moreover, germ cell proliferation was positively associated with baseline serum concentrations of anti-Müllerian hormone (AMH). Denosumab also increased germ cell proliferation in ex vivo human testis cultures with low/ moderate but not severe impairment of Sertoli cell function.
In a placebo-controlled randomized clinical trial, denosumab showed no effect on semen quality but increased sperm concentration in a subgroup of infertile men with serum AMH ≥38 pmol/L at baseline. A high serum AMH may, therefore, increase the probability of a beneficial response to denosumab treatment in infertile men.
REFERENCE
1. Andreassen et al., Cell Rep Med 2024:5:101783
This is what Brazilian investigators have apparently come to believe after observing men with moderate to severe COVID-19 showed that their gametes released extracellular traps (in a process called ETosis) in response to the infection. This immune response is common for macrophages and neutrophils but has never
before been observed in mammalian reproductive cells. 1
1. Moura J. Medscape Medical news. October 14, 2024. https://www.medscape.com/viewarticle/sperm-appearhave-nonrepoductive-function-2024a1000ipl?form=fpf
There is lots of news on this front. An article in Science magazine summarized the work of two different teams which independently came to a similar conclusion. It has been known for some time that two sperm proteins and the egg receptor had to interact to join both cells. How that happened was, however, unclear. Both groups, therefore, utilized the recently developed Multimer tool of AlphaFold (for which a Nobel Prize was awarded) to determine how different proteins in this case may slot together based on their structures. And what the A.I. predicted was a formation of a three-protein complex (trimer) – instead of only 2 proteins – noy only including Izumol and Spaca6, but also the protein, TMem81, never before associated with fertilization. An Austrian research group then demonstrated that deleting Tmem81 in zebrafish and mice caused the same sperm defects as deletion of Izumol or Spaca6. In other words, all three proteins were needed. To further confirm this Triade of proteins in their importance not only as an A.I. prediction, they added antibodies to these three proteins to zebra fish sperm, confirming that always all three proteins together were pulled out. This represented formal experimental evidence. 1
Remarkably, the sperm complex has remained the same along vertebrate evolution, while the egg receptors change. Suffice it to say, these discoveries may have opposing translational relevance for the development of new male fertility treatments and/or for development of male contraceptives.
REFERENCE
1. Leslie M. Science 2024;386(6720):363-364
The mammalian testis contains one of the most complex transcriptomes of any tissue as well as abundant RNA binding proteins.

To provide insight into the biology of male fertility, Chinese investigators now examined mouse male germ cells at different stages of development to generate an atlas of RNA binding proteins and their roles in sperm development. They then identified major evolutionarily conserved RNA binding proteins and regulatory elements and demonstrated their roles in mouse spermatogenesis. Their relevance to clinical practice was then demonstrated by collecting data from hundreds of human males in treatments for male infertility and demonstrating the relevance of the mouse findings to human health. This paper, thus, represents an important step in decoding the genetic and molecular basis of male fertility. 1
REFERENCE
1. Li et al., Science 2024;386(6720):397
The VOICE reported in the spring of 2024 on the sudden closing of a Nashville IVF clinic in April of that year. Some patients shortly thereafter presented to the CHR, wanting to transfer cryopreserved gametes and/or embryos to the CHR. To move gametes or embryos into New York State, very strict criteria apply regarding how those gametes and/or embryos had been obtained. Unfortunately, as it turned out, the way the Nashville center had done it was not sufficient, and the CHR could not bring the patients’ embryos to NYC.
As it now turns out, other centers had similar difficulties because the Nashville clinic apparently had failed to follow even some of the most basic rules. A recent article by Rae Nudson in The Cut offered some detail: 1 On April 26, the attorney general of Tennessee, Jonathan Skrmetti, filed a lawsuit against the physician owner and the clinic, as well as the labs and embryo adoption program the physician had run, alleging that physician failed to provide patients with services they had already paid for; that the clinic endangered frozen eggs, sperm, and embryos; and that it was not able to provide continuity in care for patients, including not providing medical records. Under the Tennessee Consumer Protection Act, the physician, therefore, was
alleged to be liable for these “deceptive and unfair acts,” which the physician denied.
In quoting Nudson’s article, the American Embryo Adoption Agency, which the physician had founded and owns, promised prospective parents a chance “to experience the love they have always desired through adopting an embryo child — ultimately bringing hope and happiness into this world.” The program claimed it would take care of all the legal aspects and screening for donors to provide a “secure, responsible, and honorable” option for families. The article also notes that the clinic used donor eggs proportionally much more frequently than national averages would suggest, implying that the clinic inappropriately pushed patients toward donor eggs.
1. Nudson R. The Cut. November 20, 2024. https://www. thecut.com/article/center-for-reproductive-healthclosing-ivf-patients-stories.html
That we at CHR don’t like many systematic reviews and following meta-analyses is no secret because they are suffocating the medical literature. We, therefore, really do not see much reason for the here presented paper by Canadian colleagues that reports on return rates and pregnancy outcomes after oocyte cryopreservation based on articles that already have provided all of these answers many time over. 1 Totally unsurprisingly, the paper’s conclusions, therefore, are exactly as one would have expected, that individuals considering social egg-freezing should be counseled regarding the low return rate of patients (i.e., most never use their frozen eggs). And that wasted 15 valuable pages in Fertility and Sterility
And, yes, then there is, of course, one of those Reflection commentaries attached to the article, which give the reviewers an incentive to recommend acceptance of an article because – if they reject it – they, of course, will not have the opportunity to write a nice commentary for their C.V. 2
REFERENCES
1. Kirubarajan et al., Fertil Steril 2024;122(5):902-916
2. Diego D, Hipp HS. Fertil Steril 2024; 122(5):825-826

And if we are already talking about the flood of meta-analyses in medical journals, here is another one and – this time – it is not simply a meta-analysis of reported papers but an “umbrella review” of meta-analyses. In other words, it is practically a meta-analysis to the square, but it is now called a review. 1 And suffice to say, the same group, only a few years ago, of course published their own meta-analysis on the same subject. 2
And what were the conclusions? The new superanalysis noted an association between ovarian cancer (including borderline ovarian tumors) and fertility treatments (clomiphene citrate as well as gonadotropins), but no with breast, endometrial, and cervical cancers. The authors recognized that this association remains a contentious topic because meta-analyses have been contradictory. Yet this umbrella review concluded that a statistically significant increase in the incidence of ovarian cancer and borderline ovarian tumors is associated with fertility treatments.
The authors also reemphasize that association does not mean causation and that further and bigger, preferably prospective studies will be required to reach a confident answer.
1. Saso et al., Fertil Steril 2024; doi: 10.1016/j. fertnstert.2024.09.023. Online ahead of print.
2. Barcroft et al., Hum Reprod 2021;36(4):10931107
The Ethics Committee of the ASRM updated its 2019 guidance on the management of poor prognosis patients and patients whose treatment situation is considered futile. In the process the definition remains the same: “Futility” is defined as >1% chance of live birth. A “very poor prognosis” is defined as a 1% to 4.9%. 1
Also unchanged is the opinion that physicians can deny treatment to very poor prognosis and futile patients, but refer to physicians offering such services (i.e., the CHR as probably the only one in NYC and one of only a handful worldwide).
1. Ethics Committee of the ASRM. Fertil Steril 2024;122(6):1002-1006
A laudatory shout-out to Ann Z. Steiner, MD as well as Fertility and Sterility for an amazing example of what transparency should look like, but unfortunately rarely does
To start with the good news, something truly unusual – and really amazing – happened in the December issue of Fertility & Sterility : Ann Steiner, MD, MPH , Professor of Reproductive Endocrinology and Infertility at UNC School of Medicine, and herself an editor-in-chief (of F&S Reviews ) was apparently a reviewer for a paper submitted to the mothership, Fertility and Sterility

The paper came from a Scottish group and had a very accomplished first author. 1 Steiner – for several good reasons–did not like the paper and (we are here only guessing) likely recommended rejection. Whether due to other reviewers having a different opinion or the prominence of the first author of the paper, the editorial office of Fertility and Sterility at some point decided to accept the manuscript despite Steiner’s opposition. And then the amazing thing happened as Steiner noted in the introductory sentences of her Reflection commentary to the Scottish paper she was asked to write by the editorial office. 2
And she minced no words in her commentary about what she felt were inaccurate results and conclusions and, of course, very obvious (and disclosed) commercial conflicts of interest.

Already in her introductory paragraph she identified five of the six authors of this paper on anti-Müllerian hormone (AMH) as employees, founder (and stockholder), or consultants for a company called Modern Health which sells AMH tests to women as an alleged infertility test. And data as well as financial support for the study reported in the submission was provided by Modern Health.
But she really went to work after that – at least for us – demonstrating beyond any reasonable doubt that this paper should have been for a variety of procedural as well as analytical reasons categorically rejected. She was also correct when stating that there is convincing evidence since 2015 that AMH is a poor reflection of natural fertility. The use of AMH in a home test of fertility, as apparently marketed by Modern Health, would, therefore, be inappropriate.
That Steiner was allowed by the editorial office of Fertility & Sterility to make her points to the readership is a great step forward from where Fertility and Sterility was under prior editorial leadership, where the journal at times very obviously allowed inappropriate and misleading commercial promotions of all kinds of products in its pages. The editorial office is, therefore, to be congratulated to allow for full transparency in this case. There, indeed, is an argument to be made that allowing publication of this very obviously misleading paper with Steiner’s critique next to it, is more transparent for the readership than would have been rejection of the paper since the paper, undoubtedly, would have been published somewhere else anyhow and, likely, without Steiner’s terrific comments.
Great job ladies and gentlemen! And, hopefully, a new beginning for Fertility and Sterility in recognizing its responsibility as one of the two leading journals in the infertility field.
And now to the – let’s say – not so good: We here at the CHR, strongly believe that editors should never publish in the journals they are editing, except in rare cases in a signed editorial. But, like authors, editors of course, are subject to conflict of interest rules and those do not only apply to financial conflicts but of course also apply to intellectual conflicts. Consequently, an editor should never use his own journal to repudiate an article in a different medical journal
because it contradicts something the editor believes and previously published about.
What we are talking about here is a 2021 Fertility and Sterility paper reporting on a prospectively randomized study of I.M vs. intravaginal progesterone supplementation of the luteal phase in IVF cycles, which suggested a significant benefit of I.M over intravaginal progesterone. 3 Now comes the editor-in chief of F&S Reports and published a length “Editorial” in his journal, basically accusing above noted prospectively randomized study of being wrong and using his own 2014 paper in JCEM as evidence. 4 Unsurprisingly these days, the story is picked up by a writer at Conexiant. 5
The issue we are trying to raise here is not who is right and who is wrong in regard to the disputed issue (our subjective opinion at the CHR is that it, likely, makes no difference whether women are treated with I.M or vaginal progesterone except, maybe, in older women with corpus luteum deficiency), nor do we question the editor’s right to present his opinion on the subject to the public. But the one journal where he should not do it is the journal where he controls acceptance. Why not, for example, send it to the journal where the original article was published? It, after all, is a sister journal! It, moreover, will not raise suspicions that the paper was rejected elsewhere.
It is simply time to eliminate all suspicions of biases, conflicts of interest, and lack of transparency in medical publishing!
1. Nelson et al., Fertil Steril 2024;122(6):11141122
2. Steiner AZ. Fertil Steril 2024;122(6):1020
3. Devine et al., Fertil Steril 2018;116:633-643
4. Paulson et al., J Clin Endocrinol Metab 2014;99:4241-4249
5. Miller K. Connexiant. December 16, 2024. https://conexiant.com/obgyn/articles/arevaginal-progesterone-findings-misleading/

Surprisingly many mammals can pace down their development around the blastocyst stage, thereby temporarily uncoupling conception from delivery. In mice, this is achieved by decreasing the activity of the mTOR signaling pathway. A group of international investigators from Europe no reported in Cell that decreasing the activity of the mTOR signaling pathway induces human pluripotent stem cells (hPSCs) and blastoids to enter a dormant state with limited proliferation, developmental progression, and capacity to attach to endometrial cells. 1 These in vitro assays further demonstrated that, similar to other species, the ability to enter dormancy is active in human cells around the blastocyst stage and is reversible at both functional and molecular levels. These findings, of course, have potentially enormous implications for in vitro fertilization (IVF).
REFERENCE
1. Iyer et al., Cell 2024;187(23):6566-6583.e22
Austrian investigators recently published in Reproductive Biology and Endocrinology a fascinating paper, which opens up many potentially translational considerations. They basically investigated the crosstalk between maternal immune cells and the developing embryo by investigating the immunogenic properties of human blastocyst spent media (SM) on dendritic cells. SM were collected after blastocyst formation, grouped based on successful or unsuccessful implantation. They were also analyzed by protein array or used to stimulate monocyte derived dendritic cells (moDC). The immunomodulatory properties of SM on moDC were then investigated by analyzing changes in phenotype, cytokine secretion, indoleamine 2,3-dioxygenase (IDO) activity, and ability to activate T cells. 1
The study revealed a plethora of cytokines and growth factors secreted from preimplantation embryos. Exposure to embryo SM altered the
phenotype of moDC in a manner dependent on the implantation outcome. Specifically, SM from non-implanted embryos increased the expression of co-stimulatory molecules and activation markers on moDC. SM treated dendritic cells secreted low levels of cytokines and growth factors and were able to stimulate naïve T cells. Activation of IDO was decreased in moDC after stimulation with SM. Human preimplantationstage embryos, thus, secrete a surprising abundance of molecules with the ability to significantly affect and even regulate immune cells in their environment.
1. Kyvelidou et al., Reprod Biol Endocrinol 2024;22:150
This is what Akshhay Syal, MD from NBC News recently asked in an article on NBCNews.com. 1 Among women, interest in testosterone is primarily driven at ages 40 to 50. A chief medical officer at a national telemedicine company described it as “almost like an epidemic.” Testosterone levels in women are, of course, much lower than in men (ca. 1:15), just like estrogen levels are much lower in men than women.
“Low T” does not only exist in males; in females it also can lead to low energy levels, lethargy, depression, and very depressed libido. It can be remedied by straight testosterone supplementation, usually given transdermal. In the form of a testosterone gel, or in the form of dehydroepiandrosterone (DHEA) – the precursor hormone of testosterone.
A gynecologist at Stanford Medicine in Palo Alto is quoted in the article as having—especially with the onset of menopause symptoms—witnessed “a dramatic rise in recent years in middle-aged women asking for testosterone.” She further observed that this trend “took off” only over the last two years, with women asking for testosterone when offered estrogen replacement therapy. Yet another cited gynecologist noted that the demand comes from several problems, but mostly, to improve mood, energy, sex drive, get rid of brain fog, and improve muscle mass.

How effective a remedy for all of these conditions androgen therapy really is, remains, however, to be seen and professional opinions differ.
REFERENCE
1. Syal A. NBC News.co,. November 20, 2024. https:// www.nbcnews.com/health/women-health/ testosterone-women-hormone-replacement-therapywhat-know-rcna179380
women who carry germline mutations in BRCA1 and BRCA2 have increased breast cancer risk from hormonal contraceptives?
A recent paper in the Journal of Clinical Oncology suggested exactly that! 1 Using pooled observational data from four prospective cohort studies, associations between hormonal contraceptive use and BC risk for unaffected female BRCA1 and BRCA2 mutation carriers and using then Cox regression analyses, hormonal contraceptives were, indeed, significantly associated with increased breast cancer risk, though only for BRCA1 mutation carriers. This risk was especially increased with longer use. The authors’ correct conclusion, therefore, was that the risks of hormonal contraception use in BRCA1 carriers must be carefully weighed and individualized.
REFERENCE
1. Phillips et al., J Clin Onc. 2025. Uploaded from ascopubs.org by 198.179.71.164 on January 7, 2025 from 198.179.0714. Ahead of print.
A revolutionary new potential treatment breakthrough for preeclampsia
The condition of preeclampsia here in the VOICE , of course, requires no detailed introduction. Most of our readers know that preeclampsia and its more severe form of eclampsia are still responsible for approximately 75,000 maternal and ca. 500,000 infant deaths annually around the world. 1
This fact alone makes one wonder how come this obviously very important complication of pregnancy is still only poorly understood. A
currently prominent hypothesis of the condition is based on certain mechanistic placental observation in association with preeclampsia but – still – do not physiologically explain why preeclampsia/eclampsia happen (more on that below). This mechanistic explanation of the condition claims that in an early first stage incomplete placental development (whatever that means) compromises blood flow through the placenta and leads to hypoxia. In a second stage, the placenta then starts to release so-called vascular toxins, among those the protein sFlt1, which is an inhibitor of vascular endothelial growth factor (VEGF), a well-known signaling protein. According to this hypothesis, these released circulating toxins make endothelial cells lining maternal blood vessels dysfunction, which then directly leads to the phenotypic expression of preeclampsia, including maternal hypertension.
As this alleged pathophysiology has been elucidated, several blood tests involving levels of sFl-1 and related other biomarkers have been published in the literature with claims that they allow for the early diagnosis of preeclampsia and/or predictions of who may be at risk for developing the condition. The expected next step, therefore, unsurprisingly would be a therapeutic intervention to counteract the causing VEGF signaling deficiency now presumed to cause preeclampsia. A very recent paper in Nature magazine by investigators from the University of Pennsylvania, now claimed to have achieved this goal, at least in a mouse model of preeclampsia. 2
They achieved this by delivering to the placenta messenger RNA encoding the VEGF protein using lipid nanoparticles which can carry quite large molecules, including mRNA or molecules that can interfere with RNA functions (this delivery method has, for example, been used in COVID-.19 vaccines).
Testing their delivery systems in two different mouse models for preeclampsia – one induced by inflammation and the other by hypoxia – they now reported that a single injection of their product (an encapsulated VEGF mRNA, called LNP 55) interrupted maternal hypertension until end of pregnancy. They furthermore as a results observed improved fetal health and improvements in placental vasculature, in local and systemic immune function (more on that

later), and in serum levels of soluble Fms-like tyrosine kinase-1, widely accepted as a clinical marker of preeclampsia. The authors summarized their findings as suggesting that they successfully developed a mRNA LNP platform for treating placental disorder including preeclampsia.
We, of course, fully agree and find ourselves fascinated by the potential of “treating” the placenta during pregnancy in this way, and not only for preeclampsia; but there is more to contemplate after publication of this interesting paper. First, to be cautious, humans and mice are not the same. That means what works in mice may not work equally in humans. Second, assuming the investigators’ findings can be repeated in human pregnancies, we must return to the fact that the here presented hypothesis of preventing and/or treating preeclampsia is purely mechanistic: This means that we are told that preeclampsia is the consequence of a vascular insufficiency of the placenta, and that resulting relative anoxia in the placenta. But this just describes the mechanics of the process and does not explain the underlying cause(s). In other words, it does not explain, what is/are the cause(s) for this to happen in some patients—but not in most, why this—unless a new paternity steps—occurs mostly only in first pregnancies, why if mechanistically set early in gestation, it mostly becomes clinically apparent only in late pregnancy, and a million other still unanswered questions.
That preeclampsia, as the authors note, is a disease of the placenta and not of the fetus is also of great interest because it corresponds with another hypothesis which recently has gained popularity, namely that the placenta not only provides nutrition for the fetus but also represents the protective immunological shield of the fetus against rejection by the maternal immune system.
Two observations in principle point toward this fact: First, the placenta grows in size in parallel with the fetus. Since pregnancy tolerance in contrast to tolerance after most solid organ transplants must in normal pregnancies, therefore, be maintained for nine month with an exponentially growing fetal “tumor,” any shield against rejection—whatever it may be—must be able to deal with the rapidly growing antigenic mass of the fetus. Only the placenta experiences
similar growth and, therefore, appears capable of being the shield against rejection for this rapidly growing “tumor.”
The second potential piece of evidence for a placental function in establishing immune tolerance for the fetus is the extensive persistent aneuploidy maintained in the placenta until delivery even in chromosomal perfectly normal pregnancies. Products of conception—made up of fetus and placenta—thus represent a usually euploid fetus with a usually aneuploid placenta. This dichotomy in maintaining aneuploidy in the placenta but not in the fetus must have a physiological purpose, and—like in solid cancers—this physiological purpose is increasingly suspected to be the ability of aneuploidy to circumvent rejection at immune checkpoints. In other words, what may allow tolerance of the fetal semi-allograft by the maternal immune system may during evolution have been appropriated by cancer as a survival strategy to prevent destruction by the host’s immune system. Now it only remains to be determined how exactly the aneuploid placenta does it.
As we by now are coming to better understand the mechanics of what does prevent the placenta from functioning normally (in this paper in preeclampsia), if—as a next step—we could learn how to prevent placental damage from occurring in the first place, or – if it already exists – how to fix it!
1. Thadahani R, Karumanchi A. Nature 2025;637(8045):273-274
2. Swingle et al., Nature 2025;637:412-4121
This is what a recent article in the JCEM suggested; and – if true, this would represent a very significant problem since roughly 40% of pregnant women are suffering from (too) short sleep duration (SSD). 1 The Chinese authors followed 7059 mother–child pairs collecting sleep data during pregnancy via the Pittsburgh Sleep Quality Index at weeks 24 to 28 and 32 to 36. Neurodevelopmental outcomes from 6 to 36 months postpartum were then assessed via the Denver Developmental Screening Test-II. They

then investigated the link between maternal SSD and neurodevelopmental delay risk in offspring.
Mothers with SSD during mid-pregnancy demonstrated a neurodevelopmental delay in boys (adjusted HR 2.05, 95% CI 1.29, 3.25). Cord blood marker analysis revealed a positive relationship between cord blood serum C-peptide levels and neurodevelopmental delay in offspring (RR 0.04, 95% CI 0.00, 0.08). The proportion of the association between SSD and neurodevelopmental delay mediated by cord blood C-peptide was 11.05%. We found the difference between the two sexes of special interest. The authors speculated that higher levels of C-peptide in fetuses may be responsible
1. Zhang et al., J Clin Endocrinol Metab 2024. dgae569, https://doi.org/10.1210/clinem/dgae569
Eczema is a quite frequent problem in infertile women as well as in early pregnancy. Dupimulab – a dual IL-4 and IL-13 inhibitor in 2017 approved as a very effective treatment for eczema. In addition, the drug has since been approved by the FDA for the following additional indications: atopic dermatitis, chronic rhinosinusitis, asthma, eosinophilic esophagitis, and prurigo nodularis. We, therefore, can expect a steadily increasing exposure to this biological in women in fertility treatment and early pregnancy.
A recent presentation at the annual meeting of the European Academy of Dermatology and Venerology In Vienna, Austria, on September 22-24, 2024, suggesting no adverse pregnancy outcomes with use of the drug is, therefore reassuring. The data, indeed, suggest – and we must say not really surprisingly if one considers that the medication very obviously is antiinflammatory – that this treatment may decrease risks of adverse pregnancy outcomes. Matched controls (who did not receive the drug) ended up with significantly greater risk of preterm labor (P=0.001), gestational hypertension without proteinuria (P=0.003), preeclampsia (P=0,005), and gestational diabetes (P=0.001). All adverse outcomes were added up, the significance even further increased to a P<0.0001.
These are rather amazing outcome differences in a rather small study of only 702 matching
pairs and we are, therefore, anxiously waiting for a hopefully soon published full-length paper confirming these findings in print. If confirmed, the potential consequences could be substantial:
The data would then suggest a very strong contributing immune component in preterm labor, hypertensive diseases of pregnancy, including preeclampsia, and even gestational diabetes. While the two first would, of course, not surprise – after all, every autoimmune disease is associated with premature labor risk 1 and preeclampsia has been linked to the maternal immune systema for decades but 2 ; gestational diabetes is, however, somewhat of a surprise. And the data would also suggest that all three of these major complications of pregnancy may be preventable with dupilumab treatment, - a very exiting potential!
1. Campbell P. HCP Live. October 4, 2024. https:// www.hcp;ive.com/view/matched-analysis-finds-nolink-between-dupiluab-use-and-adverse-pregnancyoutcomes
2. Gleicher N. Clin Rev Allergy Immunol 2010;39(3):194206
HS is a weird disease and the reason ism – we still don’t know what is causing this skin condition. It is a painful, chronic skin condition often seen in obese PCOS patients. This is also the reason why we are addressing it here. It causes skin abscesses and skin scarring, and we saw recently a patient at the CHR who several years ago went into sepsis from one of her abscesses and almost died.
A paper in JAMA Dermatology 1 now looked at the effects of this disease on pregnancy, and especially on maternal and neonatal pregnancy outcomes, and the finding were anything but great: In ta cohort study of 1.3 million pregnant patients with up to 16 years of follow-up, HS was associated with 30% to 60% greater risk of adverse pregnancy complications, including hypertensive disorders, gestational diabetes, and severe maternal morbidity. The risks, indeed, continued into the postpartum period. After pregnancy, HS was associated with up to 2.5 times the long-term risk of metabolic, infectious, and other morbidity in mothers and offspring.

what causes this not uncommon disease. Until the pathophysiology is better understood, there will no effective prevention and/or treatment. Pregnancy has historically been described as a “research animal” or “stress test” for many different conditions. What the risk profile of this disease in pregnancy suggests is that this is a systemic disease.
REFERENCE
1. Li et al., JAMA Derm 2024;160(12):1297-1303
How can we do without PGT-A? We actually can’t!
So, once more, as Spanish group of investigators is presenting a retrospective PGT-A stud, this time including not less than 64,071 embryos. And what was the question? What is the influence of biological, technical and clinical factors on embryo outcomes in preimplantation genetic testing for aneuploidies (PGT-A) and what is the recurrence pattern?
And if you don’t understand the question, you are not alone; but -maybe – the question will become clearer if we present the answers and conclusions: The authors reported that the aneuploidy rate was 67.75%, higher in women aged over 35 years than in women aged 35 years or less (71.76% versus 47.44%), and higher in day 3 embryo versus blastocyst biopsies (77.51% versus 58.62%). 1
That aneuploidy increases with female age is, of course, not a revelation and neither is the fact that aneuploidy is higher in day-3 than blastocyststage embryos, even though these authors apparently did not understand the meaning of percentage because on day-3 this means 1-2 aneuploid cells out of a 5-6-cell embryo, while at blastocyst stage it usually means a handful of aneuploid cells out of a ca. 250-cell embryo. So what percentages are we comparing here
And then comes further nonsense: The trisomy to monosomy ratio was 1.01 for blastocysts versus 0.84 for day 3 embryos, and is this really meant to mean anything?. Trisomy 21 was present in 4.9% of embryos. Woe, is this day-3 embryos, blastocysts or both? In aneuploid embryos, the probability of having one or more involved
chromosomes followed a decreasing exponential pattern, and what else would one expect with increasing cell umbers.
The probability of an embryo being euploid was constant at around 30% (40% in blastocysts, 20% in day 3 embryos). The cumulative probability of having one or more euploid embryos after 10 biopsied embryos was 94.79% in blastocysts and 80.61% in day 3 embryos. AMA was associated with a much higher aneuploidy rate than all other indications, which among them had similar aneuploidy rate and chromosomal involvement.
The banality of this paper is nothing but astonishing. We decided not to give it the honor of a “worst paper” designation because the paper is not “bad;” it is just totally banal in reporting absolutely nothing of any importance and –disappointingly - neither authors, nor reviewers, or editors obviously noticed this fact. What a shame! It also demonstrates how poorly the basics of human embryology are understood in the infertility community.
1. Matorras et al., Reprod Viomed Online. 2024;49(5):103979
So here is an interesting question: How much does infertility treatment (of an obviously infertile woman) affect the later onset of systemic autoimmune diseases among women giving birth, which a recent paper by Canadian investigators in Human Reproduction recently attempted to answer. And the answer was somewhat surprising: Women who experienced infertility but did not use fertility treatment had a higher incidence of later autoimmune diseases for up to nine years after delivery than those who did not experience infertility, even after accounting for a higher rates of preeclampsia, spontaneous preterm birth, and stillbirth.
The study included 568, 053 singleton births among 465, 078 women aged 18–50 years without known pre-existing autoimmune diseases

and involved all 2012-2021 data for the Canadian province of Ontario. And here is some detail: The median follow-up was 6.5 (4–9) years. The incidence of autoimmune diseases was 9.3 per 10 000 person-years in women without infertility, 12.5 per 10 000 person-years in those with infertility and no fertility treatment, 10.9 per 10 000 person-years following non-invasive fertility treatment, and 10.9 per 10 000 personyears after invasive fertility treatment. Infertility without treatment was associated with an elevated risk, even after accounting for adverse pregnancy outcomes. Neither non-invasive nor invasive fertility treatments were associated with increased autoimmunity. 1
So, what do these findings mean? The authors suggest that they mean that Infertility in the absence of fertility treatment may be an important risk marker for the development of autoimmune diseases in the future in women who give birth. Though this conclusion seems obvious and, therefore, should not be underestimated in its importance, we feel that this paper informs on significant additional issues: A first is the mere fact that female infertility appears highly associated with autoimmunity. Doesn’t this represent an even more important conclusion of this paper? That autoimmune findings in infertile female populations are more frequent than in noninfertile female populations has been for several decades claimed by several authors – including investigators at the CHR. 2 But we are unaware of any study which documented this fact as clearly as this study did. And doesn’t this, therefore, not also suggest a strong pathophysiological and, therefore, etiological connection between autoimmunity and infertility?
So much for our colleagues who still believe that the female immune system has nothing to do with female infertility!
And, last but not least, shouldn’t we ask the question why and how fertility treatments apparently reduce the risk of autoimmune diseases? Isn’t this, likely, the most important issue this paper raises?
Unfortunately, the paper addresses none of these issues in any depth and, indeed, raises in addition serious questions about its overall validity. One the authors note themselves:
Neither non-invasive nor invasive fertility treatments were associated with occurrence of autoimmune diseases. So which treatments did? The association between untreated infertility and later autoimmune diseases only persisted in analyses restricted to women under age 38 and in those without endometriosis or other autoimmune diseases.
The incidence of autoimmune diseases was 12.5/10,000 person years with untreated and 9.3/10,000 person years in controls without infertility. Though statistically a significant difference because of the huge study size one must ask whether this is really – clinically a relevant difference? We, frankly, doubt it. The authors, moreover, pointed themselves out other limitations and reasons for caution: For example, the study used published algorithms in health administrative data with unknown or imperfect sensitivity and specificity. Data on individual-level social and lifestyle factors and underlying causes of infertility were not available and thus were not included in the analysis.
In short, a potentially interesting study but of questionable clinical value. Its principal benefit may after all be a strong reemphasis of the connection between autoimmunity and female infertility (see also, “Why autoimmune diseases are surging” in the General Medical News section).
And, finally, and only somewhat related, a recent study in BMC Rheumatology linked early menopause before age 45 with increased risk for rheumatoid arthritis. Based on a meta-analysis from 11 observational studies (and we don’t like many meta-analyses as our readers by now well know) they found that: (i) postmenopausal women experienced more rheumatoid arthritis than menstrual women, and – even more interesting – women with early menopause (before age 45) had an even greater risk [OR 2.97, 95%CI 1.73-4.22]. 3 Again, not a surprising but interesting finding because, after all, all autoimmune diseases increase with age, and autoimmunity is, of course, one of the most prominent associations with primary ovarian insufficiency.
REFERENCES
1. Scime et al., Hum Reprod 2025;40(1):157-166
2. Gleicher N, Hum Reprod Update 1998;4(2):169-176
3. Namavari et al., BMC Rheumatology 2024;8:48

The idea of an APS was first presented in 1983 by an internist in New Zealand who on his ward noticed the accidental presence of several pregnant women who shared in three phenotypical findings: thrombosis, miscarriages, and presence of the so-called lupus anticoagulant (LA). 1 Its definition has since repeatedly been modified, expanding presence of a LA to presence of antiphospholipid antibodies (aPLs) and autoimmunity in general. CHR investigators, indeed, played a quite significant role in the initial expanded understanding of the syndrome. 2
A recent review, however, describes it as an “autoimmune disease” characterized by the presence of antibodies and recurrent thrombosis or fetal loss, 3 a definition we have a hard time accepting considering that in the next sentence the authors acknowledge that, “while there is no diagnostic criterion for APS, the clinical diagnosis requires both laboratory evidence with the presence of an aPL antibody (anticardiolipin, anti-B2-glycoprotein, or LA) which is positive on two consecutive occasions at least 12 weeks apart and clinical evidence of a thrombotic event or obstetric complication.” How an entity can be a ”disease” without having diagnostic criteria is difficult to understand and we, therefore, prefer to continue considering the APS – as its name suggests - as a “syndrome.”
Overall, the review is disappointing because all it presents are longstanding clinical cliches really lacking a deeper physiological understanding what links pregnancy with autoimmunity in general. This is well demonstrated by the concluding sentence in the paper’s abstract, which reads: ”While APS is a relatively rare condition, the effects this disease can have on maternal and fetal outcomes even with available therapies demonstrates the need for more highquality, evidence-based research.” This is the kind of concluding sentence when a review really has nothing new to say.
In contrast, a paper from Utah and Oregon based investigators reported interesting data by presenting a study of novel antiphospholipid antibodies previously not investigates in pregnancy and assessed their adverse effects on pregnancy outcomes. 4 Specifically, they
investigated anti-beta-2 glycoprotein01 domain 1 (aD1) and the anti-phosphatidylserine -prothrombin antibody in predicting adverse pregnancy outcomes in a high-risk population. The purpose of the study was to determine whether these novel antibodies could replace the lupus anticoagulant (LA) as the most predictive marker of adverse clinical outcomes in the obstetric antiphospholipid syndrome.
And the answer was, - nit really. While both antibodies proved to be independent predictors of risk, they did best in combination with the LA. Too bad, to get Las is always somewhat of a pain, and we always wonder how congruent results are between different commercial labs.
1. Hughes GR. Br Med K (Clin Res Ed) 1983;287(6399):1088-108
2. Gleicher N, Friberg J. JAMA 1985;253(22):3278-3281
3. He L, Sims C. Semin Reprod Med 2024;42(03):197-208
4. Moyle et al., Obstet Gynecol 2025;145(1):55-64
humanized mouse model with
How the maternal immune system tolerates the fetal semi-allograft (complete allograft after egg donation) is still not well understood and – of course – is very likely a highly complex process involving a multitude of processes. Historically, most research has been based on the early stages of invasion, - i.e., the local immune response where the embryo implants. What, however, has been widely overlooked in this research is the fact that in vitro studies have clearly established that for up to 10-14 initial days, the implanting embryo develops completely independently from any maternal influences. 1 And it appears obvious that -assuming the maternal immune system would respond to this invasion as it would be expected – in this time period an anti-embryo, anti-allogeneic immune response would be initiated by the maternal immune system, Yet – such an immune process does not occur in a normal pregnancy.
Moreover, in contrast to an allogeneic solid organ transplant which in general maintains its size (only liver transplants grow in size and volume to a degree) the allogeneic fetus grows exponentially to a huge size and – yest – still is not rejected in most pregnancies.

A very exiting recent paper by Chinese investigators now offers some new insights 2 : As the paper pointed out, most of the current understanding regarding human maternalfetal immunity is based on conventional rodent models which, based on the substantial evolutionary divergence may not precisely represent human immunological processes. They therefore developed a pregnant human immune system (HIS) mouse model through busulfan preconditioning, which hosts multilineage human immune subset reconstitution at the maternal-fetal interface. And here is what this model detected: At roughly mid-gestation, the human maternal-fetal immunity exhibits a tolerogenic feature in the decidua. However, at a later stage, the immune system switches to an inflammatory profile. The study, moreover, based on single cell RNA-Seq analyses, revealed a cellto-cell interaction network which contributed to the observed changes at the maternal-fetal interphase in which macrophages played an important role by secreting several immune regulatory mediators.
The study also reaffirmed the known importance of Treg cells by demonstrating that their depletion at early implantation stages resulted in severe early inflammation and outright rejection of the fetus. This model, thus, offers the potential for very interesting additional studies in the future.
REFERENCES
1. Deglincerti et al., Nature 2016;533:251-254
2. Dong et al., JCI Insights 2024;9(20):e176527
Quercetin in NLRP3-associated inflammation
Quercetin is an important flavonoid widely represented in fruits and vegetables. It also has multiple potential therapeutic effects, including as an antioxidant, as an antiinflammatory agent, anti-viral activity,, other immunomodulatory, and even analgetic properties. Its antioxidant activity comes from regulating glutathione, enzyme activity, and the production of reactive oxygen species (ROS), while its substantial anti-inflammatory effects come from acting on the Nod-like receptor protein 3 (NLRP3) inflammasome. A very good review by Chinese scientists now summarized these anti-inflammatory effects on the NLRP3 inflammosome. 1
Since we have noticed that increasing numbers
of infertility patients are receiving quercetincontaining supplements, we felt that this paper makes a worthwhile read for patients as well as providers of fertility services interested in this flavonoid.
REFERENCE
1. Wu et al., Inflammopharmacol 2024; 32:3585-3610
IL-23 inhibition with biological monoclonal antibodies inhibits hyperactive cytokine signaling that drives chronic inflammation. Consequently IL-23 inhibitor drugs have become important in the treatment of psoriatic skin as well as joint disease. A well-written recent review article in The Lancet informs on this family of drugs, 1 and is a worthwhile read for everybody interested in this subject. Moreover, it would not surprise if this family of drugs would also turn out to be effective in other inflammatory diseases. How, for example, a trial in endometriosis?
REFERENCE
1. Jairath et al., Lancet 2024;404:1679-1692
What reflects a so-called “normal” immune system has never before been attempted to be defined, - that is until a recent paper by a large consortium of U.S investigators published in Nature Medicine. 1 Also accompanied by a Commentary in the same issue of the journal, 2 the study utilized a wide array of “-omics” and artificial intelligence (AI) to define what is normal and abnormal. And there was a surprise: Among 228 patients with 22 monogenic conditions that impact key immune pathways and 42 age and sexmatched controls, healthy immune systems vary much more than was expected.
In general, the immune health metrics obtained were concordant between two types of analyses and distinguished between normal and polygenic autoimmune and inflammatory conditions through mostly signs of inflammation and cell signals of innate immunity in 10 independent data sets. The discrimination was better than for established markers of inflammation, like CRP and IL-6 which we use at the CHR as general inflammatory markers. Among all cells, NK cells

frequency was the best discriminator between health and disease. Immune health metrics varied more between individuals that longitudinally in individuals (even if in treatments).
Where these findings may lead diagnostically and potentially therapeutically, is as of this point still difficult to assess; but we would not be surprised if these kind immune system assessments in the not-too-distant future would become an integral part of diagnoses in precision medicine.
REFERENCES
1. Sparks et al.,Nat Med 2024;30:2461-2472
2. Vinuese et al., Nat Med 2024;30:2411-2412
Are “poo milkshakes” in the future of babies delivered by Cesarean sections?
It is by now well accepted that newborns who because of a Cesarean section delivery missed out on passing through the maternal birth canal and, therefore, lack exposure to the maternal vaginal microbiome are immunologically disadvantaged. As a News article in Nature magazine now reported, feeding such babies milk containing a tiny bit of their mothers’ feces –thereby introducing beneficial microorganism to their guts – might improve their immune function and prevent diseases during childhood an later life according to a clinical trial reported orally at a recent infectious disease meeting in Los Angeles. 1
All of this sounds a little far-fetched to us; but the funny thing is, this concept is given serious consideration. It, however, of course, should not be tried at home! Moreover, the investigators pointed out that they had to exclude among 90 women 54, because of their fecal matter contained pathogens.
Not a concept we would invest in, - but what do we know? We also would have not invested in fecal transplants, and they have become routine treatments in hospitals for Clostridium difficile GI infections.
REFERENCE
1. Lenharo M. Nature 2024;635:17-18
CRISPR-modified immune cell therapy – so-called chimeric antigen receptor (CAR-T) therapies in
CAR-T therapies, which have become routine treatments in oncology, now are also entering the treatment of autoimmune diseases. As a News article in Nature magazine recently reported three treatment successes in China – all with engineered donor rather than autologous cells –are, as the article, notes a first stage in the mass production of such heterologous cell therapies. All three patients remained in remission with their autoimmune diseases six months after receiving the treatment. A women had an autoimmune myopathy, and two men had severe cases of systemic sclerosis. Side effects often seen in using the treatment in oncology, were not seen in any of these three patients. CAR-T therapies may be on the verge of revolutionizing the treatment of severe autoimmune diseases! 1
Autologous CAR-T therapy has been going on for some time. German investigators already at the beginning of 2024 reported on 15 patients with SLE, scleroderma, or myositis, with the 8 SLE patients among them ending all up were in drugfree remission 4-29 months after the treatment. 2 The first person to become a successful SLE CAR-T patient in Germany was a 20-year-old Vietnamese former hip-hop dancer and gymnast, later ravaged by the disease (see her surrounded by her doctors at the University Hospital Erlangen in Germany in the picture below. 3

Vu-Thi Thu-Thao (center) smiles with the doctors at University Hospital Erlangen who helped her become the first person with SLE to get chimeric antigen receptor T-cell therapy. SOURCE: Kind/University Hospital Erlangen3
REFERENCE
1. Mallapaty S. Nature 2024;634:519-520
2. Couzin-Frankel J. Science 2024;387(6727):1215
3. Couzin-Frankel. Science 2024;386(6723):719-723

More on COVID-19
LONG COVID It appears every organization dealing with COVID-19 is publishing their own definition of Long COVID. Now it was the turn of the National Academies of Science, Engineering, and Medicine in The New England Journal of Medicine . 1 We, frankly, fail to understand the purpose, and the many different definitions –we would argue – support our view. Much more important seems what Harvard investigators did and recently published in Med : 2 They attempted precision phenotyping to define individual research cohorts of patients with unexplained post-acute sequelae of COVID-19. As the authors noted, this approach accounts for infection related chronic conditions as well as differential diagnoses and demonstrated superior accuracy in identifying post-acute sequelae compared to existing ICD-10CM code U09.9, while also mitigating biases in diagnosis. This approach allows the definition of a specific research cohort to explore genetics as well as metabolics of Long COVID.
Related, most recent research confirms that Paxlovid, likely, protects to a degree form Long COVID. 3 And, finally, likely the best review on Long COVID we have read was published in Cell. 4 It's definitely worth a read. And if you want to learn more about the so-called COVID Brain, we recommend Eric Topol, MD’s Ground Truths of September 26, 2024, where he reported a paper that demonstrated cognitive deficits in patients requiring hospitalization for COVID-19to be equivalent to 20 years of ageing. In addition, the study he discussed also demonstrated objective evidence brain injury and reduced gray matter volume. 5
A question that has been asked for some time, why protection from COVID infections and vaccines wanes so quickly, has finally at least one answer: It appears that a so-far little investigated immune cell subpopulation in bone marrow, called long-lived plasma cells (LLPCs), which produce long-lived antibodies may lead to the production of longer-effective vaccines. As recently discussed in a News article in Science , 6 a
recent study suggested that the SARS CoV-2 virus apparently does not produce these cells in bone marrow as frequently as other viruses with longer post-infection and post-vaccination immunity. Now vaccine producers have to figure out how to overcome this fact.
A recent CDC announcement updated information on COVID-19 – associated hospitalizations and maternal vaccinations among infants below age 6 months. 7 As it turns out, infants under age 6 months have a relatively high COVID19-associated hospitalization rate and are not eligible for vaccination. The rate is, indeed, the highest among all age groups, except for individuals above age 75 and comparable to hospitalization rates for 65–74-year-olds. Among ca. 1000 hospitalized infants at such young ages, 22% were admitted to an ICU, and 9 died. If mothers had been vaccinated, the percentage was only 18% during October 2022-September 2023 and to <5% during October 2023-April 2024. Maternal vaccination, therefore, appears clearly protective for offspring into the neonatal period.
Another very disturbing finding is that COVID-19 apparently greatly increases within 6 months the diabetes risk in children and teens. 8 In comparison to children and teens with other respiratory infections, those with COVD-19 demonstrated a 50% increase in diabetes incidence. Interestingly, this involved type 2 diabetes and not type I diabetes, as one might have suspected, considering the strong association of COVID-19 with autoimmunity. A very recent paper in JAMA Dermatology , indeed, reported in a study of not less than 6.9 million Korean people - half of whom had experienced COVID-19 -that a past COVID infection significantly increased the risk of alopecia, vitiligo, Crohn’s disease, ulcerative colitis, rheumatoid arthritis, and SLE. 9
1. Wesley Ely E et al., N Engl J Med 2024;391(18):17461753
2. Azhir et al., Med 20256:1-11
3. Rubin R, JAMA. 2024;332(13):1040-1042
4. Peluso MJ, Deeks SG. Cell 2024;187:5500-5529
5. Topol E. Substak. September 26, 2o24. https:// erictopol.substack.com/p/covid-brain
6. Cohen J. Science 2024;386(6719):255-256
7. CDC. https://www.cdc.gov/mmwr/volumes/73/wr/

mm7338a1.htm
8. O’Mary L. WebMD. October 15, 2024. https://www. webmd.com/covid/news/20241015/coivd-greatlyincreases-diabetes-risk-kids-teens
9. Anderere A. JAMA 2025;333(2):
We have before in these pages raised the question whether infectious threats have increased in the world in recent years. It at least seems that way, raising the obvious question why that may be? Here are just a few examples which – all – of course may occur in pregnancy: BIRD FLU is likely the biggest threat, as the virus has now expanded not only from birds to cows, but also to pigs, 1 and humans, where it on January 6, 2025, also has led to the announcement of a first human death from the H5N1 virus causing the bird flu, as announced by the Louisiana Department of Health. 2 Spillover infections have affected increasing numbers of farm workers and a recent Nature paper reported that a human isolate of the bovine H5N1 virus in such a worker from his eye was transmissible to and lethal in small animals (ferrets). 3
Somewhat unsurprisingly, one hears and reads increasingly about concerns of a pandemic threat from the bird flu, with calls to start developing vaccines, should a pandemic indeed arise. 4 Concerns are further aggravated by increasing evidence that the prevalence in humans may be already much bigger than has been estimated because infected individuals have been found who were completely symptom-free. Moreover, a recent paper in Science reported that a single mutation in bovine influenza H5N1 hemagglutinin switches specificity to human receptors. 5
MONKEPOX VIRUS (mpox) A recent news article in Nature magazine reported that an analysis of a clade Ia strain of the virus in Central Africa demonstrated genetic mutations suggestive of sustained human-to human spread. 6 Because the virus has significant adverse effects in pregnancy, an article in the New England Journal of Medicine, therefore, appeared timely in reviewing risks, vertical transmission, prevention, and potential treatments in pregnancy. 7 The
WHO has, in the meantime, declared the mpox outbreak a public health emergency of international concern. 8
MARBURG VIRUS This deadly virus spreading in Rwanda, Africa, causes an Ebola-like hemorrhagic fever, for which there are no approved treatments, though vaccines are on the way. 9
PARVOVIRUS B19 in children also known as Fifth disease. In contrast to measles, mumps, and chickenpox, this virus – because of its usual benight course - is not a reportable disease and the CDC, therefore, cannot as accurately track the disease. 10 Immunity is long-lasting and, even getting the disease in pregnancy is usually not a major risk to either mother of pregnancy.
PERTUSSIS Whooping cough has also been surging this year as a recent News article in JAMA pointed out. The article also noted that causes for this resurgence are still unclear, - but one cause appears to be a waning protection from current vaccines. 11 Bordetella pertussis is spread via airborne droplets and may be changing to resist vaccines. Attempts at making a better vaccine are underway
REFERENCES
1. Sun LH.washington Post. October 30, 2024. https:// www.washingtonpost.com/health/2024/10/30/bird-flupig-virus/
2. Louisiana Department of Health. January 6, 2025. https://ldh.la.gov/news/H5N1-death
3. Gu et al., Nature 2024;636:711-718
4. Goodman et al., JAMA 2024;332(190:1609-1610
5. Lin et al., Science 2024;386(6726):1128-1134
6. Kozlov M. Nature 2024;635:13-14
7. Nachega et al., N Engl J Med 2024;391(14):1267-1270
8. WHO. August 14, 2024. https://www.who.int/news/ item/14-08-2024-who-director-general-declares-mpoxoutbreak-a-public-health-emergency-of-internationalconcern
9. Callaway E. Nature 2024;634
10. Rubin R. JAMA 2024;332(15):1226-1227
11. Rubin R. JAMA 2024;332(19):1597-1598

Unsurprisingly, this has now become a repeated subject in these pages, as the progressive legalization of cannabis, of course, not only has increased general use but, likely, also use during pregnancy. Just to make certain that increasing use in pregnancy was not coincidental and/or artificial due to changes in cannabis screening methods, U.S. investigators attempted to determine whether the new permissive legalization in California was directly associated with changes in prenatal cannabis use, based on self-reporting and urine toxicology testing. And low and behold the results were abundantly clear: The new recreational cannabis legislation in California was clearly associated with an increase in rates of cannabis use during early pregnancy,both by self-reporting and toxicology testing. 1
But this is by no means the end of the story. A paper in JAMA Pediatrics asked the question whether prenatal cannabis exposure is associated with poorer executive function and more aggressive behavior among preschool-aged children, - as some evidence had suggested? And, once again, low and behold in a cohort study of 200 children, prenatal cannabis exposure was associated with worse attention (i.e., inhibitory control) and planning ability on select laboratorybased assessments, and with more aggression based on behavioral observations. 2
And to further demonstrate the obvious effects of cannabis on young brains, in another paper
in JAMA Pediatrics , investigators investigated cannabis use in adolescence and young adulthood on academic achievements and – unsurprisingly – in a meta-analysis of by now 63 studies of 438,329 individuals concluded with moderate certainty (a pretty respectable certainty level for such a study!) showed a likely association with lower school grades, less likelihood of high school completion, university enrollments, and postsecondary degree attainment. Moreover, school drop-out rates and school absenteeism were increased, while evidence of association with increased unemployment was lower. 3
An excellent analysis of the problem was presented on October 4, 2024 in The New York Times. 4 An article from which above Figure 1 was modified.
That the country relaxes cannabis controls and, thereby, encourages its use at a time when the nations deteriorating health is increasingly appreciated is yet another absurdity of the country’s political system. In which the drive toward election and reelection of politicians seemingly by far outweighs all other considerations. The only solution to this problem - if any - are term limits.
1. Young-Wolff et al., JAPA health Forum. 2024;(5):11):e243656
2. Keim , et a l., JAMA Pediatr. 2024;178(12):1316-1325
3. Chan et al., JAMA Pediatr.2024; 178(12):1280-1289
4. Twohey et al., The New York times. October 4, 2024. https://www.nytimes.com/2024/10/04/us/cannabismarijuana-risks-addiction.html

Figure 1. Rates of almost daily cannabis use at ages 18-25 (top line), 26 and over (middle), and 12-17 (bottom)
The Y-axis represents 2%-14% of survey responders.
SOURCE: KARL RUSSED, The New York Times, October 5, 2024, based on an analysis from the federal government’s National survey of Drug Use and Health conducted






The CHR VOICE is the newsletter of The Center for Human Reproduction (CHR), an independent, academically affiliated infertility and research center located at 21 East 69th Street in Manhattan, New York, N.Y. 10021. www.centerforhumanreprod.com. Telephone +212 994 4400. The CHR VOICE attempts to inform and engage a global community of infertility patients, infertility service providers, and researchers in reproductive medicine, physiology, and biology. The mission of The CHR is clinical care, research, and education, all at highest standards, with empathy, honesty, integrity, and equity. The newsletter is published 10 times a year (except July and August). Copyright © 2025 by The CHR. All rights reserved. Print ISSN 2836-3086. Online ISSN 2836-3094. Copyright © 2025 by The CHR. All rights
For letters to the editor, comments, and suggestions, please contact jgreenberg@thechr.com. For all advertisements or sponsorships in The VOICE , please contact jgreenberg@thechr.com.
the opinions of The CHR.