

VOICE
October 2024
To our readers,
Welcome to the October issue of the VOICE. With the summer behind us, everything around us seems to be speeding up and, before we know it, we will fnd ourselves in the midst of the holiday season. Time is really relative: when much is happening, the world appears to speed up, but it seems to drag when nothing is going on and, in appropriate symbolism, time appears to stand still.
But that is most certainly not something anybody has to worry about this year. What is happening in our country—and in most parts of the world—these days basically assures no boredom. After all, October 7 marked the one-year anniversary of likely the most callous political mass murder and rape since the end of WWII. And over 100 hostages are still in the hands of Hamas, with the world seemingly having forgotten and doing absolutely nothing about it.
And shortly after that date comes November 5 (for those just visiting from another planet, this is Election Day in the U.S.) and, whichever side loses, will hate the other half of the country even more than before.
Here is one more relevant observation: both candidates have been such lucky bastards that they have started believing in divine interventions. Who knows how many assassination attempts candidate Donald Trump will still have to survive to even make it to Election Day. Considering an assassin’s bullet grazed his right ear, missing his skull bone by only millimeters, he understandably attributed surviving this frst attempt at his life “to God’s
intervention” (one becomes religious in such situations!). And that a Secret Service agent from relatively far away identifed a gun barrel in the bushes surrounding the golf course where Trump was playing a Sunday round just one hole away, can also be viewed as a small miracle.
And then there is, of course, the always cheery Kamala Harris, current V.P. and potential future frst female President of the U.S., who must as well have become a believer in miracles because, there is no other explanation but divine intervention for her sudden rise to being the Democratic presidential candidate—to gain this position without even winning a primary, having become V.P. after President Biden promised the American people he would choose a female running mate. But most remarkably, she became the presidential candidate without anybody knowing what she really stands for. And—as things stand at this writing—she may be elected President without anybody knowing what she stands for. If there ever was a true political miracle, this is it!
Once the election is over (and if we are not yet in Civil War II or WWIII), there is Thanksgiving; and the week after that, the CHR co-hosts with the Foundation for Reproductive Medicine (FRM) the annual FRM Conference (FRMC) here in NYC, with over 30 of the world’s most prominent clinicians and scientists offering a true example of what it means to, in a positive way, “think differently,” a longstanding motto of the FRMC, but also of the CHR in its daily clinical activities. And then it is already Christmas and Hanukkah and the New Year, and we all will be a year older in an increasingly diffcult world to manage.
Economic diffculties so many people in this country have been encountering over the last few years have taken an obvious toll. This is the point where this welcome note to this month’s VOICE more directly reconnects with the fertility feld, which for so many obvious reasons, is always greatly affected by the economic environment: when people have a hard time paying bills and live from paycheck to paycheck, the last thing they are thinking about is having children. That is also the usual response to political instability and wars and now it seems we have it all together in one big mess.
First came COVID, and following that a period of almost unprecedented infation in our lifetimes, and now fears of an economic slow-down with declining employment and, maybe, even a recession in 2025. Who then can be surprised by plummeting birthrates all over the world (including the U.S.) but—interestingly—most in developed countries, like Italy, Japan, and Korea which can most afford—and indeed need—more births (again including the U.S.). This is a subject repeatedly discussed in theVOICE in recent months and is again a topic in this issue, which reviews a book with the provocative title,What Are Children For?
And on the other extreme, in countries that can’t even afford their current population numbers, growth is just speeding up, with little need for fertility clinics. Though these days there are fertility clinics almost everywhere,
they obviously are primarily in more developed countries. The growth of the infertility industry in the world’s two most populated countries, China and India, has been remarkable. In China, where live birth rates have dropped to catastrophic low levels, the government now is offering strong incentives to have more children (which the population, interestingly, does not appear interested in). South Korea, Japan, Italy and other European nations are also facing astonishing low birth rates, signifcantly below replacement rates. One, therefore, senses an increasing appreciation for IVF in improving in birth rates.
Infertility practice is to a major degree dependent on a population’s desire to have children. Individuals who are not desirable of parenthood, of course, do not need fertility services. Consequently, it should not surprise that in the U.S.—as CHR investigators demonstrated in association with the 2008 recession—lower consumption of fertility services (especially IVF cycle numbers) served as early indicators of recessions.1 The next few weeks should, therefore, be telling!
And—yes—before we forget, you have just started browsing through a very diverse issue of theVOICE , as usually offering a potpourri of signed articles (amongst those a very interesting article on PGT-A, our frst submission by Russian colleagues from Moscow), general medical news items, our usual food and nutrition section and, of course, our literature review of new articles that have appeared with potential relevance to reproduction. Let us know if you like or dislike something and don’t forget, we invite contributions. If interested, please write to us at social@thechr.com.
The Editorial Team of the VOICE

1. Crudele J. December 14, 2015, New York Post. https://nypost.com/2015/12/14/can-less-baby-making-mean-bad-news-for-us-economy/
BASICS ABOUT FERTILITY & INFERTILITY
UNDERSTANDING CHROMOSOMAL ABNORMALITIES IN EARLY-STAGE EMBRYOS BETTER
By Ilya Volodyaev, PhD., et al., (Anna Ivanova, Elena Korchivaia, Ilya Mazunin), Senior Researcher,
Laboratory of Developmental Biophysics, Department of Embryology, Faculty of Biology, Moscow State University, Russia; and Russian national representative (basic science) to ESHRE. He can be contacted though Te Reproductive Times or directly at ivolodyaev@gmail.com or ivolodyaev@emcmo.
Reprinted and edited with permission of authors and Te Reproductive Times.
BRIEFING: Especially in human embryos, chromosomal abnormalities in early embryonic development are a routine fnding. However, they can also be found in some other mammals. Tey can involve all cells of an embryo or be mosaic, and they can afect one or more complete chromosomes or be segmental, afecting only small pieces of chromosomes (Figure 1). In testing embryos for such chromosomal abnormalities, the technology matters. Some reported abnormalities are defnitely


artifacts of current testing technologies, but their exact efects on the accuracy of testing—in the fertility feld called preimplantation genetic testing for aneuploidy or PGT-A—are still largely unknown. In this article, we address the distinction between true biological aneuploidies and false-positive diagnoses based on technical errors and also discuss what the prevalence and dynamics of chromosomal abnormalities and the role of embryo self-correction.



WHOLE-CHROMOSOMAL ABNORMALITIES, A KNOWN ENTITY
Whole-chromosomal abnormalities (WCAs) in human oocytes and embryos are well-documented. A mother’s age plays a critical role, with women under age 35 experiencing WCAs in approximately 20–30% of eggs, with an additional ca. 6% increase in aneuploidy for every year after that (Figure 2). These abnormalities are observed both in natural and stimulated cycles1 and remain consistent across diferent studies. Interestingly, sperm WCAs show age independence, and afect only about 3% of sperm cells.2
Figure 2. Proporton of euploid human embryos as a functon of female’s age (autologous oocytes). Note the linear trend in the advanced maternal age. Data from 5
Whole-chromosomal abnormalities, particularly in human embryos, are largely attributed to the instability of the oocyte’s meiotic spindle, which lacks microtubule-organizing centers and certain molecular motors, and thus appears much more error-prone than in most other species.3,4 Interestingly, besides humans, such intriguing properties of meiotic spindle have been documented across several other species, namely pigs, horses, and primates.5-7
SEGMENTAL ANEUPLOIDIES (SA): VARIABILITY AND CHALLENGES
Unlike WCAs, segmental aneuploidies (SAs) display signifcant variability in reported prevalence, ranging from less than 3% in some studies1 to as high as 30% or more.8,9 Although these estimates vary, one consistent fnding is that SAs are independent of age and WCAs. These abnormalities are often platform-dependent, meaning their detection rates fuctuate with the technology used.10 For instance, studies reporting fewer SAs tend to have more concordant results in repeated biopsies, suggesting that many SAs reported in other studies may be artifacts.
The reported incidence of SAs is around 3–10% in oocytes, 5–20% in sperm, 15–25% in cleavage-stage embryos, and 7–15% in blastocysts.8,11,12 SAs are associated with relatively poorer development of embryos, which, moreover, more frequently arrest than euploid embryos.13 However, the true signifcance and nature of an SA diagnoses in an embryo is still debated and may often be associated with technical artifacts. The frequency of
misdiagnoses of SAs is at least one potential reason why among all chromosomal abnormalities, embryos with SAs, if nevertheless transferred - demonstrated the best pregnancy and live birth rates among transfers of embryos with any chromosomal abnormality.
MOSAICISM: A CONTROVERSIAL DIAGNOSIS
Whole-chromosomal mosaicism (WCM), like SAs, exhibits a wide range of reported rates — from less than 3%14,15 to over 30%16,17 and is age- and WCA-independent. It apparently is the consequence of a range of phenomena, from real biological issues to technical artifacts and misinterpretations. Their true distribution still remains to be determined and is among the most hotly debated issues in reproductive medicine.
Some authors believe that most reported cases of mosaicism are artifacts due to variability in testing platforms and yet unresolved issues of single-cell DNA testing.18-20 Several among them, moreover, then argue that true mosaicism likely affects only about 5–15% of blastocysts. Based on single-cell studies,21 others consider the real mosaicism rate to stand at ca. 80% of all blastocysts Whatever one wishes to believe, to minimize false diagnoses, PGT-A platforms must be optimized as much as possible and the seemingly amazing plasticity of embryos and, therefore, their ability to self-correct must be further explored,
One must also remember that, while the correct defnition of mosaicism is the presence of two or more cell lines with different karyotypes in a whole organism (in this case, a blastocyst), typical PGT-A reports refer to mosaicism only based on a 5—10-cell biopsy of trophectoderm. This incorrect defnition of mosaicism by PGT-A laboratories will, therefore, only refect a small fraction of the actual mosaic aneuploidy in the tested human embryo. Consequently, the diagnosis of a full aneuploidy will be incorrect if only a small island of aneuploid cells was at random biopsied (while the embryo contains both aneuploid cells and euploid cells). Similarly, an embryo may be incorrectly identifed as euploid if by chance only euploid cells have been biopsied, while surrounding tissues contain aneuploid cell islands. Underdiagnosis of mosaicism is also supported by ca. 80% of blastocyst-stage embryos in single cell analyses demonstrating aneuploid cells.21
With ca. 20% of all embryos afected by meiotic aneuploidy (afecting all cells in an embryo) and all other aneuploidies being mitotic (and, therefore, present in islands of cells) - if ca. 80% of all embryos demonstrate at least some aneuploid cells by single cell analysis - ca. 60% of all embryos must be to diferent degrees mosaic.
The diagnosis of mosaicism is also affected by PGT-a laboratories using arbitrary thresholds in defning mosaicism: An embryos in many PGT-A laboratories in the U.S and Europe can be defned as euploid with <20%, <40%, or even <50% aneuploid DNA in a trophectoderm biopsy of 5- 6 cells. Which of these defnitions a laboratory uses to defne euploidy will, of course determine the percentage of mosaic embryos because they will represent either the range of 20-80%, 40-80%, or even 50-80%. The cut-off for aneuploidy, in contrast, has remained consistent at 80%. It is, however, important to remember that under the correct biological defnition of “mosaicism,” any presence of a second cell lineage in the organism, from 0.1% to 99.9% in theory represents “mosaicism.”
Consequently, most embryos currently signed out by PGT-A laboratories are biologically mosaic and many embryos signed out as aneuploid also are in reality mosaic. This, however, does not negate that percentages of aneuploid cells in a mosaic embryo matter because we know from animal models that the ability to self-correct declines with increasing percentages of aneuploid cells in an embryo.22
That mosaic embryos more likely arrest than euploid embryos,13 may also be a reason for underestimation of mosaicism at the blastocyst stage. Mitotic errors occur mainly during the frst and second divisions of the zygote. The proportion of embryos at the cleavage stage affected by mosaicism- including possible artefacts - is, therefore,
higher than at the blastocyst stage.
All of this, paradoxically, however, also does not exclude overdiagnosis of mosaicism when “noisy NGS profles” are overinterpreted as mosaic instead of being marked as “unreadable.” This, of course, can also contribute to laboratory-specifc differences in prevalence of mosaicism diagnoses in the same patient populations.19 We below offer a short introduction to the potential mathematical estimation of chromosomal artifacts in PGT-A technologies.
UNDERSTANDING THE MATHEMATICS BEHIND CHROMOSOMAL ARTIFACTS
When it comes to assessing chromosomal abnormalites, whether whole-chromosomal or segmental, a critcal challenge is diferentatng true biological events from technical artfacts introduced during testng. Technical artfacts have atracted too litle atenton in the medical literature. Understanding how these artfacts arise requires not only biological insight but also a mathematcal perspectve. Below, we provide a brief overview of the formulas used to estmate the probability of artfacts in whole-genome amplifcaton (WGA) technologies, such as Next-Generaton Sequencing (NGS), and Fluorescence In Situ Hybridizaton (FISH).
Artfact Probability in Whole-Genome Amplifcaton Technologies
In WGA technologies, artfacts arise from such factors as DNA degradaton or “loss” and non-uniform amplifcaton. The probability of encountering such artfacts can be mathematcally estmated using the following formula:

where: α is probability of degradaton of 1 DNA copy; pk , probability of 1 DNA copies degraded; N, number of DNA copies in the sample; n, number of DNA copies required for a stable signal; G, number of “independent genome segments” (which is a conditonal division of the genome into fragments to account for their independent degradaton processes).
This equaton illustrates how the probability of artfacts decreases as the number of DNA copies in the sample increases. Simply put, the more DNA is present for analysis, the more reliable will the results be because of fewer artfacts being introduced during the testng process.
Artfact Probability in FISH
For FISH, which is used to detect specifc chromosomes, artifacts arise from hybridization failures, chromosome overlap, and “false signals”. The probability of encountering an artifact in FISH can be approximated using the following formula:

where: φ is probability of false signals; β, probability of hybridizaton failure for a single chromosomal type; s, average relatve area occupied by one chromosome at FISH on which the next chromosome must not overlap; m, number of chromosomes labeled in one cell; n, number of chromosomal types labeled in one cell; N, number of cells in the biopsy sample. Note that this formula is approximately true for small n and becomes false for large n.
Unlike WGA, the probability of artfacts in FISH increases with the number of cells in the sample. This fundamental diference makes FISH and WGA assessments of chromosomal abnormalites inherently incomparable. Even when the two methods yield similar results, variatons in the number of cells tested (unavoidable in real practce) will cause signifcant discrepancies.
WHAT THESE FORMULAS TELL US
The diferences in the mathematical estimations of artifacts between WGA and FISH underscore the complexities of detecting chromosomal abnormalities accurately. While WGA improves reliability with more DNA copies, FISH becomes less reliable as the sample size increases. Although this may seem like a currently unimportant issue considering FISH is basically no longer used in PGT-A, one faces these discrepancies every time when PGT-A data from diferent stages of embryo development are compared. The PGT 1.0 to PGT 2.0 shift included changes of technology and of stage of embryo biopsy. A large majority of PGT-tested cleavagestage embryos underwent FISH testing, while blastocysts have been mostly subjected to aCGH or NGS.
CAN EMBRYOS SELF-CORRECT?
One of the most intriguing and still controversial topics in embryonic development is the promising evidence that mammalian embryos, as well as human embryonic stem cell models and cultures can self-correct.21-23 Thousands of healthy births have followed the transfer of mosaic embryos, challenging our understanding of embryo biology.21-27 The signifcantly lower rates of mosaicism among fetuses and children suggest that either current testing methods are misidentifying euploid embryos as mosaics, or that some embryos have the ability to correct chromosomal errors during development.20,-22,25,28-30 The frst question is more technical and seemingly uninteresting, while the second option involves deep insights into embryonic development and the true beauty of regulatory processes and self-organization. However, it is the frst “uninteresting” technical issue that must be scrupulously optimized not to be trapped by above noted technical artifacts.

The self-correction issue has recently gotten strong support from a study by Danish investigators31 who reported ESC-derived mouse primitive endoderm lineage (producing the trophectoderm and placenta from the so-called extraembryonic cell lineage) to have so much plasticity and potency that it can regenerate a complete blastocyst which continues post-implantation development. Though this, of course, does not imply genetic self-correction and does not explain how aneuploid cells are removed, it appears reasonable to assume that an epiblast that can regenerate the extraembryonic cell lineage, also can replace its own chromosomal abnormal cells (interestingly, the extraembryonic cell lineage in mouse20 and human embryos 21 does not appear to have the same plasticity and ability to self-correct). A better understanding of the embryo’s ability to self-correct has, however, still to be pursued.
CONCLUSION
While whole-chromosomal aneuploidies are relatively well-understood, segmental aneuploidies and mosaicism remain more open to discussion, largely due to the limitations and artifacts of the current testing technologies. The role of mosaicism in embryo development, and the possibility of embryo self-correction represent critical questions in the feld of reproductive medicine that warrant further examination and changes in current reporting schemes in PGT-A.
After the very recent statement of the Practice Committees of the American Society for Reproductive Medicine (ASRM) and the Society for Assisted Reproductive Technology (SART), noting absence of any outcome utility for the PGT-A procedure for in vitro fertilization (IVF),32 the future of PGT-A appears at a crossroad. If PGT-A is to remain in continued use in association with IVF, a clear outcome utility for the procedure must be found and current laboratory methodologies must be further improved. In practical terms this means a better understanding of technical artifacts, a signifcant decrease in overdiagnoses, potentially the addition of new types of diagnosable anomalies due to more in-depth diagnostic techniques and technologies,33 and improvements in the ability to separate embryo plasticity and self-organization from technical artifacts. .
REFERENCES
1. Labarta et al.,. J Clin Endocrinol Metab 2012;97:E1987-E1994
2. Bell et al.,. Nat 2020;583:259-264.
3. Holubcova, et al., Science 2015;348:1143-11477.
4. So et al., Science 2022;375.
5. Hornak et al., Plos One 2012;7:e30335.
6. Hornak et al., CytogenGenome Res 2016;150:60-70.
7. Dupont, et al., Fertil Steril 2010;93:2545-520.
8. Babariya et al., Hum Reprod 2017;32:2549-2560.
9. Navratil et al.,Molec Hum Reprod 2020;26:269-76.
10. Treff NR, Franasiak JM. Fertil Steril 2017;107:27-31.
11. Treff NR, Marin DT. Fertil Steril 2021;116:1205-11.
12. Magli eet al.,Hum Reprod 2020;35:759-69.
13. McCoy et al., Genome Med 2023;15(1):77
14. Katz-Jaffe et al., FertilSteril 2017;108:e87-e8.
15. CCRM 2017. . CCRM Reports the Lowest Chromosomal Mosaicism Rates in the U.S. At Less Than Three Percent Across
16. the CCRM Network. In: Peel J, ed. CCRM Fertility, 2017.
17. Escudero et al., Fertil Steril 2016;105:e20-e21.
18. Munne et al., Am J Hum Genet 1994;55:150-159.
19. Treff et al., Hum Reprod 2010;16:583-589.
20. Kullyev et al., In: Preimplantation Genetic Diagnosis International Society PGDIS 2023. Paris, France, 2023
21. Swain EJ. Reprod BioMed Online 2019;39:599-607
22. Yang et al. Nat Cell Biology 2021;23:314-321.
23. Viotti et al. Fertil Steril 2023;120(5):957-966
24. Barad et al., Hum Reprod 2022;37(6):1194-1206
25. Bolton et al., Nat Commun 2016;29(7):11165
26. Coticchio et al., Hum Reprod Update 2021;27:848-865.
27. Munne et al., Eur J Med Genet 2020;63:103741.
28. Yakovlev et al., Reprod Biomed Online 2022;45:88-100.
29. Capalbo et al., Hum Reprod 2017;32:492-8.
30. Esfandiari et al., J Assist Reprod Genet 2016;33:14391444.
31. Popovic et al., , Hum Reprod Update 2020;26:313-334.
32. Linnenberg-Agerholm et al Cell 2024;S00928674(24)00595-
33. Practice Committee of the ASRM and SART. Fertil Steril 2024; 122(3);421-434
34. Essers et al., Nat Med 2023;29:3233-3242.


THIRD-PARTY REPRODUCTION IN NON-INFERTILE PATIENTS
Building Mono-parental and Shared-motherhood Families
By
Sònia Gayete Lafuente, MD, PhD, who is a Foundation for Reproductive Medicine (FRM) postdoctoral research fellow at the CHR and can be reached through The Reproductive Times at hello@reproductivetimes.com or directly at sgayete@thechr.com. Reprinted and edited with permission of authors and The Reproductive Times
BASICS ABOUT FERTILITY & INFERTILITY
Increasing numbers of women and men with no evidence of traditonal infertlity problems are seeking out standard infertlity treatments, either desirous of fertlity preservaton into older ages, single parenthood, or because of being in same sex relatonships. The author of this artcle ofers some important insights into the individualized treatments such patents require.
INTRODUCTION
As reproductve technologies have evolved, the use of egg and sperm donaton has broadened beyond outright clinical indicatons to encompass fertlity optons in a variety of non-clinical scenarios. These include supportng uniparental families, diverse LGBTIQ+ family structures, and adjustng medical and technical aspects of fertlity assessment and treatments to these predominantly non-infertle populatons. Understanding these highly individual circumstances and their respectve treatment implicatons is of great importance in order to properly manage third-party reproductve practces.
While access to fertlity treatments for single mothers and same sex couples has been improving in many parts of the world, legal, cultural, religious, and other systemic societal factors stll greatly vary. In the U.S. and in many other countries with more advanced health care systems, medical insurance coverage stll ofen quite distnctvely diferentates between coverage of infertlity in heterosexual couples and coverage of medical services to achieve pregnancy for non-infertle individuals who need treatments because of being single and/or being in same-sex relatonships. Though such coverage has also been improving in recent years in the U.S., other countries, such as Spain, the U.K., and especially Belgium, are considerably ahead of the U.S.
Non-infertle women requiring fertlity-related medical services also include women seeking what is widely called social or planned egg freezing in atempts to preserve their fertlity chances with their own eggs into more advanced ages. While this is generally not a covered beneft in most health insurance plans, some typically larger companies – especially those in very compettve industries for staf recruitments – have started to ofer fnancial contributons for such services, though usually not full or unlimited coverage. This area of fertlity practce, therefore, represents an evolving landscape of changing policies, deserving of review.
STRIVING FOR MONO-PARENTAL and LGBTIQ+ FAMILIES
Several studies have demonstrated that a strong primary motvaton for social egg-freezing is the concern of single women about not fnding a suitable partner in tme. At the same tme, especially in the U.S., young women have also been exposed to at tmes hard-driving marketng campaigns by a quickly developing eggfreezing industry, which ofen argue that every young
woman (and man) should cryopreserve gametes at peak fertlity in their mid-twentes.
Whether this, because of potental risks (as small as they may be) and quite signifcant costs, is an ethically defensible positon, is not the subject of this communicaton, though it may be one day because the subject has remained controversial. As here at the CHR we do not believe that there exists any medical treatment that should be applied to “everybody,” this, in our opinion, also applies to fertlity preservaton through egg-freezing. But the choice, of course, should always be the patent’s!
At the same tme, becoming a single mother with the help of (in most cases in the U.S. stll anonymous) semen donatons has become socially more acceptable and is, therefore, quickly increasing. Studies on the subject suggested that single women proceeding with donor sperm either though intrauterine inseminatons (IUIs) or in vitro fertlizaton (IVF) rather than freezing their eggs, tend to have a historically longer desire for motherhood, live closer to family, and report stronger social support compared to those choosing egg freezing. Men, interestngly, opt for single parenthood through egg donaton and use of a gestatonal carrier (ofen mistakenly called a surrogate) much less frequently.
Lesbian female couples must also rely on sperm donaton to build their families, while gay male couples, of course, require donor eggs and the availability of a gestatonal carrier, with the later being extraordinarily expensive, unless one is lucky enough to recruit a friend or family member who does it for free. The use of donor gametes and gestatonal carriers, moreover, in several even otherwise medically very advanced countries, is stll forbidden. Laws usually only change once adoptons by gay couples are allowed.
Though in the U.S. all these optons are available, it is important to note that third-party gamete donaton is very closely regulated by the FDA. IVF clinics, therefore, have to follow very strict rules and are regularly inspected by FDA inspectors in surprise visits.
THE TREATMENTS
In countries where third-party gamete donaton for single and same-sex female couples are allowed, about 25% of sperm donaton cycles occur in single women, 50% by same-sex female couples, and only 25% by heterosexual couples with male factor infertlity. In other words, a large majority of donor sperm cycles are
actually performed in absence of what traditonally has been defned as “infertlity.”
Single women undergoing fertlity treatments are signifcantly older than same-sex female couples (aged around 37 vs 32 years) and more ofen chose IVF as their inital treatment, while lesbian couples more ofen prefer donor sperm IUI, partcularly in natural cycles. Despite these diferences, afer adjustng for age, live birth rates in those groups are comparable.
… donor sperm IUI vs. IVF in non-infertle women
Simple logic suggests that fertlity clinics must approach non-infertle women in here discussed circumstances diferently from obviously infertle women where the assumpton is that there exists a medical problem that must be overcome. In non-infertle women – at least at relatvely young ages – such an assumpton does not exist. The assumpton, indeed, must be (unless, of course, there exists history that suggests otherwise) that, once egg and sperm are allowed to meet in presence of a uterus, pregnancy should happen at agedependent speed.
A recently published study demonstrated that the cumulatve clinical pregnancy rate of up to 4 donor sperm IUIs in a non-infertle populaton is approximately 45%, with most pregnancies occurring within the frst two atempts. Interestngly, this pregnancy chance also did not difer between age-comparable women with AMH ≥ 1.1 ng/mL and < 1.1 ng/mL.
Non-infertle patents even with low functonal ovarian reserve – unless, of course at extremely diminished levels – therefore, stll deserve at least several IUI cycles before IVF is initated. A widely accepted consensus exists that in more depth fertlity evaluatons in preparaton for IVF should only be considered afer up to 4 failed IUI atempts.
As with infertle women, ovarian stmulaton protocols and other IVF strategies should be individualized in non-infertle patent populatons based on age, ovarian reserve, and other hormonal as well as uterine parameters.
… the ROPA method in shared motherhood IVF
Among same-sex female couples, a new opton for shared motherhood is becoming increasingly popular,
the so-called Reciprocal IVF or ROPA (Recepton of Oocytes from Partner) method. It allows for both female partners to be actvely involved in the concepton and birth of their children. With ROPA one of the two female partner undergoes ovarian stmulaton to produce eggs which, afer retrieval, are inseminated with donor sperm, producing embryos for transfer into the uterus of the other female partner, who technically now becomes the gestatonal carrier for the transferred embryo(s). She has no genetc connecton to the fetus growing in her (the genetc mother will be the partner who produced the eggs), but she will be the biological mother of the child. In other words, both female partners can claim motherhood of the newborn child.
Among female couples using ROPA, the gestatonal carriers tend to have had more previous fertlity treatments and be generally more parous than the egg providers, who generally have slightly higher ovarian reserve markers. In non-infertle females, ROPA has comparable success rates to fully autologous IVF. It is, therefore, a safe and efectve treatment with reassuring obstetric and perinatal outcomes.
Afer we have navigated fertlity treatment optons for single mothers and same sex female couples, we would love to be part of yours. Whether you are exploring donor sperm IUI, IVF, or the innovatve ROPA method, at CHR our expert team is here to guide you through your journey to motherhood, commited to ofering comprehensive and tailored fertlity solutons to meet your wishes and needs. Visit us to discuss your familybuilding optons!
CONCLUSIONS
Non-infertle individuals seeking out fertlity treatments – whether women or men – ofen fnd themselves in an unexpected framework, akin to a healthy individual entering an emergency room. This feeling of “notbelonging” is ofen further accented by fertlity clinics treatng these individuals as if the treatments they were receiving were not really fertlity treatments.
But they, of course are exactly the same treatments truly infertle patents receive and they, therefore, must be appreciated as such. An IUI or IVF cycle is the same IUI or IVF cycle in heterosexual and samesex couples. Under both circumstances, treatments dispensed by fertlity clinics, therefore, have the same obligatons of maximizing outcomes for their patent
in every treatment cycle. In other words, even though an egg-freezing cycle in a 25-year-old will not include fertlizaton of her eggs and/or immediate transfer of an embryo as a regular IVF cycle usually entails, her cycle stll requires a careful assessment of her overall health ahead of cycle start, determinaton of how her ovaries are best stmulated to safely obtain the largest possible egg numbers for cryopreservaton, administraton of intravenous sedaton by certfed anesthesiologists for the egg retrieval, and a needle entering (under ultrasound vision) her pelvic cavity. In other words, she receives real treatment, with potentally real (though fortunately rare) complicatons, and is for all of these reasons a real patent.
Patents who are not perceived to be considered “real” patents and/or do not receive the appropriate atenton they feel they deserve as patents, therefore, may be best of by looking for an alternatve clinic.
READING LIST

Bodri D, Nair S, Gill A, Lamanna G, Rahmat M, Arian-Schad M, Smith V, Linara E, Wang J, Macklon N, Ahuja KK. Shared motherhood IVF: high delivery rates in a large study of treatments for lesbian couples using partner-donated eggs. Reprod Biomed Online. 2018;36(2):130-136. doi: 10.1016/j.rbmo.2017.11.006.
Brandão P, Ceschin N, Cruz F, Sousa-Santos R, Reis-Soares S, Bellver J. Similar reproductve outcomes between lesbian-shared IVF (ROPA) and IVF with autologous oocytes. J Assist Reprod Genet. 2022;39(9):2061-2067. doi: 10.1007/s10815-022-02560-7.
Brandão P, Ceschin N, Sandvik B, Paolelli S, Doblinger J, Reis-Soares S, Sousa-Santos R, Bellver J. Female couples undergoing assisted reproducton - choices and the importance of pregnancy and genetcs. JBRA Assist Reprod. 2023;27(3):442-452. doi: 10.5935/15180557.20230007.
Diego D, Medline A, Shandley LM, Kawwass JF, Hipp HS. Donor sperm recipients: fertlity treatments, trends, and pregnancy outcomes. J Assist Reprod Genet. 2022;39(10):2303-2310. doi: 10.1007/s10815-022-02616-8.
García D, Vassena R, Rodríguez A. Single women and motherhood: right now or maybe later? J Psychosom Obstet Gynaecol. 2020;41(1):69-73. doi: 10.1080/0167482X.2019.1669018.
Gayete-Lafuente S, Moreno-Sepulveda J, Sánchez-Álvarez J, Prat M, Robles A, Espinós JJ, Checa MÁ. Ant-Müllerian hormone does not predict cumulatve pregnancy rate in non-infertle women following four IUI cycles with donor sperm. J Assist Reprod Genet. 2024 Jul 10. Epub ahead of print. doi: 10.1007/s10815-024-03188-5.
Matorras R, Perez-Fernandez S, Hubel A, Ferrando M, Quintana F, Vendrell A, Hernandez M. Perinatal outcomes in lesbian couples employing shared motherhood IVF compared with those performing artfcial inseminaton with donor sperm. Hum Reprod. 2023;38(5):895-907. doi: 10.1093/humrep/dead035.
Peigné M, Bernard V, Dijols L, Creux H, Robin G, Hocké C, Grynberg M, Dewailly D, Sonigo C. Using serum ant-Müllerian hormone levels to predict the chance of live birth afer spontaneous or assisted concepton: a systematc review and meta-analysis. Hum Reprod. 2023;38(9):1789-1806. doi: 10.1093/humrep/dead147.
Wrande T, Kristjansdotr BH, Tsiartas P, Hadziosmanovic N, Rodriguez-Wallberg KA. Live birth, cumulatve live birth and perinatal outcome following assisted reproductve treatments using donor sperm in single women vs. women in lesbian couples: a prospectve controlled cohort study. J Assist Reprod Genet. 2022;39(3):629-637. doi: 10.1007/s10815-022-02402-6.
RECURRENT IMPLANTATION FAILURE (RIF): Does it really exist, and can it be treated?
By David H Barad, MD, MS, who is a Senior Scientist and head of Clinical IVF and Research at the CHR. He can be reached at social@thechr.com.
Reprinted and edited with permission of authors and The Reproductive Times.
BRIEFING: Recurrent Implantation Failure (RIF) is a widely used diagnosis in reproductive medicine, yet it has remained controversial, with an increasing number of investigators questioning whether such a diagnosis even exists. The hypothesis of RIF basically suggests that failure to achieve pregnancy with a certain number of good-quality embryos (usually n=3-4), automatically suggests that –because of the good quality of transferred embryos – the failure to conceived must be caused by an implantation problem, an assumption based on
Few things are more frustrating for physicians and patients than the repeated transfer of highquality embryos without achieving a pregnancy. Repeated implantation failure (RIF) is typically defned as the inability to achieve pregnancy after the transfer of three or four high-quality embryos. Yet there exists no universally accepted defnition of RIF. If the expected implantation rate for a high-quality embryo is ca. 30%, then there is a 70% probability of failed implantation. After transferring two such embryos, the chance that both will fail to implant is 70% squared, or 49%. With three embryos, the probability that all will fail is 70% cubed, or approximately 34%, and this pattern continues with each additional embryo. Thus, even after transferring seven embryos, there remains a signifcant 8% chance that none will implant (70% raised to the seventh power equals about 8%). In scientifc terms, an event is not typically considered rare unless its probability is less than 5%.
In other words, even after seven embryos have failed to implant, that failure may simply be due to chance. To consider somebody to have a diagnosable medical problem (i.e., implantation failure) as cause of their infertility after the failed transfer of only three to four embryos makes little sense.
the observation that at peak-fertility (in one’s 20s) a single embryo offers a ca. 30-35% pregnancy chance per month. Since the chance of conception per embryo, however, quickly declines with advancing female age, the hypothesis of RIF is not really sustainable for a large majority of infertility patients. The author further mathematically explains its shortcomings, however, also noting that this does not mean that efforts to improve implantation chances should not be pursued and then details what such efforts may include.
Even so, it is important to identify and address factors beyond chance over which we have some control. Unfortunately, these factors can be numerous. Factors that can contribute to the failure of a healthy embryo to implant include structural issues like fbroids, polyps, uterine scarring, hydrosalpinxes (fuid-flled fallopian tubes), and, likely, adenomyosis of the uterus; lifestyle factors such as stress, smoking, obesity, or excessive alcohol use; immunological factors; poor timing of embryo transfers; and problems with the uterine lining leading to poor endometrial receptivity.
While many of these issues can be identifed and treated through a thorough diagnostic work-up, endometrial receptivity problems often remain among the most challenging to address. Endometrial receptivity refers to the ability of the endometrium to support embryo implantation, making it in IVF treatments a critical factor for achieving a successful pregnancy.
Many treatments have been proposed to address poor endometrial receptivity. Hormonal support with sequential estrogen and progesterone is commonly used to prepare the endometrium for an embryo transfer. If there is evidence of fbroids, polyps, or
endometriosis, they can be surgically removed or treated to improve the environment of the uterus.
Sildenafl citrate, commonly known as Viagra ®, has been explored as a treatment option to improve endometrial blood fow and thickness in women undergoing fertility treatments. The underlying idea is that enhancing blood fow to the uterine lining may improve its receptivity to embryo implantation. Research on sildenafl’s effectiveness for improving endometrial receptivity has shown mixed results. Some small-scale studies report positive outcomes, while others fnd no signifcant beneft. Sildenafl is, therefore, not universally accepted for this purpose. Its use is considered off-label, and more extensive clinical trials are needed to establish effcacy and safety conclusively.
Endometrial scratching is a medical procedure involving a minor injury or “scratch” to the endometrium, which is the lining of the uterus. This procedure is often considered for women who have experienced repeated implantation failures during in vitro fertilization (IVF) treatments or other assisted reproductive technologies. The procedure can be painful and can cause some vaginal bleeding. It also creates a small risk of infection. The exact mechanism by which endometrial scratching might enhance implantation is not fully understood, but several theories exist: The scratch may induce a mild infammatory reaction, releasing growth factors and cytokines that may improve the receptivity of the endometrium; the procedure may alter the expression of genes involved in implantation, making the endometrium more hospitable to an embryo; the injury might promote the shedding of older endometrial cells and the growth of new cells that are more receptive. Initially proposed by Israeli investigators early studies, indeed, seemed to confrm that endometrial scratching may improve implantation rates. Then, however, several larger randomized clinical trials did not fnd signifcant effects. Most recently, a quite well executed metaanalysis demonstrated clear benefts, leaving the question about effcacy of this treatment again wide open.
Granulocyte Colony-Stimulating Factor (G-CSF) has been proposed as a treatment option for women experiencing thin endometrium, which can be a signifcant barrier to successful embryo implantation during in vitro fertilization (IVF) cycles. G-CSF is a glycoprotein that
stimulates the bone marrow to produce granulocytes, stem cells, and release them into the bloodstream. It is commonly used in medicine to boost white blood cell counts in patients undergoing chemotherapy. G-CSF may stimulate the proliferation of endometrial cells, leading to a thicker uterine lining. It might improve blood circulation within the endometrium, providing a more supportive environment for embryo implantation. G-CSF could also infuence the immune environment of the uterus, making it more receptive to an embryo. At CHR we found that G-CSF was effective to promote endometrial growth in women with thin endometrium, but we were not able to show any beneft when G-CSF was given to women with normal endometrium to try to improve embryo implantation. G-CSF is typically administered directly into the uterus via a catheter. This targeted approach aims to maximize its effect on the endometrial lining. Though G-CSF is well tolerated and has few reported side effects there is insuffcient highquality evidence to conclusively support the routine use of G-CSF for thin endometrium. More extensive, randomized controlled trials are necessary to determine its effcacy and safety defnitively.
Platelet-Rich Plasma (PRP) therapy has emerged as a potential treatment for thin endometrium in women undergoing fertility treatments like in vitro fertilization (IVF). Thin endometrial lining can be a signifcant obstacle to successful embryo implantation, and PRP therapy aims to enhance the receptivity of the uterine lining. It is a fraction of the patient’s own blood with 4-5 times enhanced platelet concentration which is rich in growth factors including platelet-derived growth factor (PDGF), endothelial growth factor (EGF), transforming growth factor (TGF), vascular endothelial growth factor (VEGF), insulin-like growth factor (IGF), connective tissue growth factor (CTGF), hepatocyte growth factor (HGF), and cytokines (both anti-infammatory and proinfammatory), such as several interleukins, TNF-α, IFN-α, and stromal cell-derived factor 1-α, which promote tissue regeneration through cell activities like migration, growth, differentiation, and angiogenesis. Originally introduced in sports medicine, because of alleged anti-infammatory and regenerative effects, PRP is presently also widely used in orthopedics, dentistry, urology, surgery, wound healing, cosmetic procedures, and in female infertility.
PRP is prepared by centrifuging a sample of the patient’s
own blood to concentrate the platelets, which release growth factors and cytokines. Since PRP is derived from the patient’s blood, the risk of allergic reactions or immune rejection is minimal. PRP is believed to enhance the endometrial environment by promoting angiogenesis (the formation of new blood vessels), reducing infammation, and improving tissue repair. This treatment is thought to improve endometrial thickness and quality, which are crucial for successful implantation. The procedure is generally well-tolerated, although some women may experience mild cramping or spotting after the injection.
PRP is typically administered into the uterine cavity 48 hours before a planned frozen embryo transfer or in a fresh IVF cycle. Sometimes more than one administration of PRP is used. The procedure is generally considered safe although some patients may experience signifcant cramping with intrauterine administration.
Studies of PRP for RIF are hard to compare as there is little standardization in PRP preparation or administration. Some preliminary studies and case reports have shown that PRP therapy can increase endometrial thickness in women who have not responded to conventional treatments like estrogen supplementation. Improved pregnancy rates have also been reported in some cases. While early results are promising, the number of high-quality studies is limited. Some research has methodological weaknesses, such as small sample sizes and lack of control groups. Larger, randomized
READING LIST
controlled trials are necessary to conclusively determine the effectiveness and safety of PRP therapy for thin endometrium. PRP therapy for thin endometrium is still considered experimental and is not a standard treatment in fertility clinics.
PRP therapy offers a promising avenue for treating thin endometrium by potentially enhancing the uterine lining’s thickness and receptivity. While early studies show encouraging results, more extensive research is needed to establish its effcacy and safety conclusively. In summary: RIF is challenging to defne, and even when a defnition is established, diagnosing a specifc cause or prescribing an effective treatment remains diffcult. Initial steps should involve diagnosing and treating underlying conditions such as polyps, fbroids, or uterine scarring. Additionally, lifestyle modifcations like reducing stress, quitting smoking, maintaining a healthy weight, and limiting alcohol consumption can be benefcial. While a well-timed embryo transfer during a natural menstrual cycle can be successful, providing hormonal support to the endometrium with sequential estrogen and progesterone is often a primary approach to treating a thin endometrium. Further medical treatments such as the use of sildenafl (Viagra), endometrial scratching, intrauterine administration of Granulocyte Colony-Stimulating Factor (G-CSF), and intrauterine Platelet-Rich Plasma (PRP) remain promising, but the mechanisms of action and effectiveness of each of these measures need to be validated in future well-structured randomized trials.
Cutting ER, Abdallah KS, Mol BW. Is there a treatable cause of repeated implantation failure, or isit simply treatment failure by chance? Reprod Biomed Online 2024;48(6):103845
Tao Y, Wang N. Adjuvant vaginal use of Sidenafl Citrate in hormone replacement cycle improved live birth rates among 10,069 women during frst frozen embryo transfers. Drud Des Devel Ther 2020;14:5289-5279
Van Hoogenhijze NE, Lahoz Casarramona G, Lensen S, Farquhar C, Kamath MS, et al., Endometrial scratching in women undergoing IVF/ICSI: an individual participant data meta-analysis. Hum Reprod Update. 2023; 29(6):721-740
Gleicher N, Kim A, Michaeli T, Lee H-J, Shohat-Tal A, Lazzaroni E, Barad DH. A pilot cohort study of granulocyte colony-stimulating factor in the treatment of unresponsive thin endometrium resistant to standard therapies. Hum Reprod 2013;28(1):172-177

THE PROBLEM WITH...
Reprinted and edited with permission of authors and The Reproductive Times
BREIFING: This feature will point out in a short format signifcant problems we have identfed within reproductve medicine that deserve atenton. Once introduced here, some of the raised issues may later be expanded by other members of the editorial team into more detailed presentatons of the subjects. If you have something to say about a subject you feel deserves menton, let us know by writng to social@thechr. com. We are always looking for new contributors. This feature comes from Norbert Gleicher, MD, the Medical Director and Chief Scientst at The Center for Human Reproducton in New York City (ngleicher@thechr. com). A Visitng Research Scientst at Rockefeller University, Dr. Gleicher can also be reached at ngleicher@ rockefeller.edu.
… THIRD-PARTY GAMETE DONATIONS
It suddenly looks like the business of egg donaton is getng out of control, and, yes, a business it has become:

indeed, an increasingly big one! Let’s start with egg donors: Have you ever heard of egg donors receiving in excess of $100,000 per donaton? We have, and the last one we saw was, on top of it, a truly lousy donor. We suspected so much afer her inital interview and testng round; but the (obviously very well-of) couple that had selected her with help of a donor agency (we never could fnd out what the agency fee was) insisted on startng a cycle anyhow. The cycle then got cancelled because the donor completely screwed up her gonadotropin dosage. So much for her Ivy League educaton!
And how about $20,000 semen donatons per single sample, that is, if you are a well-trained athlete and have the abs to show it? We have seen this too, within weeks of the above -described egg donaton atempt. Again, this was only the fee the donor received; what the sperm bank charged was obviously extra. In contrast to oocyte donors, we do not interview sperm donors (the

assumpton has been for decades that frozen sperm banks can be trusted in their donor selecton processes). That this star athlete’s specimen demonstrated only 1% morphology, therefore, came as quite the surprise. And the infertle couple stll purchased all of this donor’s specimens that the sperm bank had in storage.
Third-party gamete donatons, consequently, increasingly raise serious ethical as well as medical issues. With the quickly rising demand for donor eggs and donor semen, simple market dynamics can be expected to lead to price increases. But from a recent average of roughly $8,000 for an egg donaton to over $100,000, and from a few hundred dollars to $20,000 per semen donaton, this appears beyond reasonable.
So, what is going on? Let’s call it the mega-yacht phenomenon: if you are the Russian oligarch Roman Abramovich and can aford the superyacht Eclipse at an estmated

cost of $1.5 billion (and even if you are a litle less rich), why wouldn’t you spend $100,000 (or even more) on super donors? Frankly, it makes sense, because there do stll exist people who believe that their future children are their most important possessions.
But is it ethical?
We don’t think so. But this does not mean that we have recommendatons as to how this obvious ethical confict may be resolved. Future parents, of course, are fully expected to select what they consider to be the best possible gamete donors for what will, afer all, be their future children. Any controlling infrastructure – as when it comes to organ donatons –therefore will have to be efectve at the distributon point, in this case (in most instances) frozen egg, embryo, and sperm banks, and they, too, unfortunately appear increasingly out of control.
… FROZEN EGG, EMBRYO, AND SPERM BANKS
The concept of frozen gamete banks started with frozen donor sperm banks afer the frst HIV cases were reported from fresh sperm donatons in the early 1980s. Freezing and quarantning of sperm allowed for eliminaton of all HIV risks, as use of fresh donor sperm was for all practcal purposes forbidden.
Cryopreservaton of embryos then preceded cryopreservaton of oocytes since embryos proved easier to freeze than eggs. The frst frozen donor egg bank was only announced in 1998, with frozen egg banks then especially over the last 20 years becoming a major industry. The principal reason was that, technically, egg freezing greatly improved following a switch from so-called slow-freezing to
vitrifcaton, a quicker and less workintensive method of cryopreservaton.
Before the establishment of frozen egg banks, egg donaton relied on most IVF clinics maintaining their own egg-donor pool. Once a donor match was made, the donor went through a fresh egg retrieval cycle, with soobtained eggs distributed between one or more recipients who had been in parallel prepared for the transfer of fresh embryos. Their embryos were produced through fertlizaton of the fresh donor eggs with either partner or donor semen. If a donoregg cycle produced more embryos than were immediately needed for fresh transfer(s), excess embryos were cryopreserved by the IVF clinic for future use by those same recipients. In other words, those frozen embryos became the patents’ property.
Logistcally and administratvely, it was a complex, expensive process in fresh donor cycles to manage the donors and recipient in parallel. With the establishment of frozen donor egg banks, IVF clinics, therefore, quickly discovered how this process could be managed with more ease and cost-efectveness by simply ordering already-frozen oocytes from a frozen donor-egg bank. This new opton allowed them to abandon in-house egg donor recruitment and avoided the need to parallel coordinate donor and recipient cycles. IVF clinics, therefore, increasingly terminated their own fresh egg-donor pools, increasingly relying on frozen donor eggs from an ever-increasing number of commercial frozen donor-egg banks.
Patents also derived clear benefts from these developments because they suddenly had so many more donor choices. If one egg bank did not have eggs from a donor they liked, they could just look up on the Internet
what was available at another. Nor was there any longer a need to wait for the donor to go through her full retrieval cycle, since that stage of the process was already past her. Eggs were already frozen, and they could be shipped to any IVF clinic within 24-48 hours. And to make this choice even more atractve for patents, donor egg banks also priced their eggs very compettvely in comparison to eggs from fresh cycles.
With this opton ofering so many improvements for patents as well as IVF clinics, nobody can be blamed that a large majority of donor egg cycles in the U.S. (and elsewhere in the world) now utlize already-frozen eggs. This trend has accelerated considerably in recent years, even though strong arguments can also be made favoring fresh over frozen oocyte donatons; the most important one is beter pregnancy and live birth chances with fresh eggs.
Though at tmes rather aggressively denied by the egg-freezing industry, the evidence by now appears indisputable that fresh in this regard is beter than frozen: While inital studies suggested a single digit diference, more recent studies suggest that the diference may, indeed, be in the 12-14%-range. But even considering this diference, most IVF clinics and their patents stll prefer the logistcs of using already frozen donor eggs. Consequently, only a very small minority of IVF clinics stll maintain their own, independent egg-donor pool. The reason why our center, despite signifcant difcultes in recouping costs, decided to maintain its own donor pool, is also one of the main issues we are presentng in this artcle: Overall, we have come to trust our own eggdonor selecton more!
More specifcally, we fnd increasing
reason to distrust: (i) donor selecton by frozen gamete-banks and their tributaries of IVF clinics which most banks employ to stmulate and retrieve their donors; (ii) the quality of oocytes and semen those banks dispense to their clients’ fertlity centers; and (iii) the convoluted sales conditons frozen gamete-banks impose on patents.
Here are a few more examples of why it is becoming increasingly difcult to trust commercially motvated partes in gamete-donor and similar third-party selectons. Another increasingly common thirdparty patent selecton occurs in the selecton of gestatonal carriers (incorrectly sometmes also called surrogates). Similar to gamete donors, the demand for these carriers has also greatly increased in recent years. As with oocyte donors, we usually suggest to our patents to let us interview their carriers before commitng to them fnancially. Untl COVID, we very rarely recommended against a choice; by now it has almost become routne. We just recently recommended against a gestatonal carrier because she demonstrated evidence of signifcant autoimmunity, a fnding that in pregnancy can cause miscarriages and other pregnancy complicatons, but also can afect the carrier’s health.
But not only does the quality of third-party egg-donors (and gestatonal carriers) appear to be declining, the same – unsurprisingly of course – then also afects their products, with egg quality being a good example, and by now a real problem at our Center. In an extreme example of poor quality, a prominent egg bank in a recent shipment sent three out of fve straws to us empty (frozen embryos are kept and transported in glass straws, usually
containing one or two embryos each). The egg-bank, in other words, sent only about half the number of embryos the patent had purchased.
Which brings us to the legal jungle of paperwork patents are forced to sign when purchasing oocytes from a frozen egg-bank: In trying to fnd the balance between successful marketng and protectng themselves from unwanted claims, most banks sell oocytes in small groups of fve to six, guaranteeing at minimum one or two blastocysts. If that minimum is not reached, the egg bank will replace the originally purchased number eggs. However, as we only recently learned to our surprise when fnding us in such a situaton with a prominent frozen donor-egg clinic, replacement oocytes, surprisingly, do not come with such a replacement guarantee.

Unsurprisingly, therefore, they are frequently worse than the original set of oocytes which, of course, also means lower pregnancy and live birth chances.
Commercial reproductve thirdparty medical services, whether gamete or embryo donatons or use of gestatonal carriers, uniformly appear to have a problem in maintaining quality and, therefore, treatment outcomes. It seems tme to take notce!
REFERENCES
1. Ombelet W, Van Robays J. Facts Views Vis Obgyn 2015;7(2):137143
2. GILEAD HIV. 2024. htps:// www.gileadhiv.com/landscape/ history-of-hiv/?gclid=EAIaIQ obChMI67KXgo6WiAMV6HF HAR31zxCLEAMYASAAEgLdr vD_BwE&gclsrc=aw.ds

Political Tribalism in Medicine Kills
All Common Sense; gender-affrming care is an example
Reprinted and edited with permission of authors and The Reproductive Times.
This is, of course, best seen in the national debate over abortions and the question of when human life begins. A central issue in the upcoming November elections, this is not today’s subject of discussion, but, undoubtedly, will become a theme of the VOICE sometime in the near future. Today’s subject is another highly politicized subject, gender-affrming medical care in children and adolescents, unsurprisingly also an issue in the upcoming elections. Moreover, it has recently become subject of intense confict (one can no longer call it a debate) within the medical feld. And, as with in the abortion debate, political extremism appears to rule the day.
BRIEFING: Controversies surrounding gender affrming medical care for children and teenagers were expected to abate following publication of the Cass Review in the U.K., widely lauded as a unique and fair product of four years of work. Instead, the report has reinfamed the controversy, driven by political ideologies rather than evidence and common sense. We here discuss this subject as an example of how damaging the intrusion of politics is to the practice of medicine and how it often leads to the suspension of all logical thinking.
One would assume that the negative effects on public health and society from how government and medical experts managed the COVID-19 pandemic would have been convincing enough to warn everybody about allowing national politics to enter medical practice. Current schisms in society, likely the most profound since the early 1930s in Europe and the McCarthy period in the late 1940s and early 1950s in the U.S., however, even outbid the obvious. And when- and where-ever this happens, medicine and society appear to suspend all common sense.
It from the start is important to note that we, here, are not addressing gender-affrming care in adults. The subject of this editorial is exclusively gender-affrming care in young children and adolescents up to age 18 years. In other words, the subject here is such care for minors who society–for good and logical reasons–has throughout history limited in their ability to make medical decisions without parental input.
It does not take much scientifc insight to understand that our brains must mature before they allow us to make (more or less) logical decisions. This is why in practically all states a school nurse under law must call parents for permission before giving their child a Tylenol capsule for headache, and physicians need to get parental consent before performing an appendectomy on a child.
But now, a recently passed law in California prohibits schools and school districts from adopting parental notifcation policies requiring teachers (or other school employees, like nurses, and psychologists) to inform parents if their under-age child asks to use a name or pronoun different from the one given at birth or if they engage in activities and use of spaces designed for the other sex.1 In other words, under current California law, the above-noted school nurse must get consent from parents to give their child a Tylenol for headache but may be prohibited from communicating with the child’s parents that their child suddenly demonstrates clinical signs of gender dysphoria. One cannot but wonder, where is the common sense?



With the rapidly increasing demand for genderaffrming medical care, very quickly a provider industry arose around it. And while it started with offerings to adults, it quickly expanded to genderaffrming care for children and adolescents. Moreover, it went far beyond just name changes and pronouns, including serious medical treatments with potential lifelong irreversible effects, including puberty blockers and major surgical procedures, often advocated by and offered at major medical centers and prominent academic institutions.
And here is one paradox: At a time when the medical feld decries “medicalized female genital mutilation” in an unsigned formal editorial in The Lancet, 2 the British Medical Association (BMA) called for the lifting of a ban on puberty blockers for transitioning children with gender dysphoria (under age 18) in the U.K. which the British High Court had upheld.3
All of this, of course, has been happening after the publication of the initially widely-lauded Cass Review which had warned that the use of puberty blockers and hormones for patients under the age of 18 really relied only on a “shaky foundation.” 4 The report was based on four years of gathering available evidence and did not claim that there was evidence that puberty blockers did cause permanent and often irreversible damage to individuals so-treated as children (as claimed by some) but specifcally noted that convincing evidence in favor of such treatment did not so far exist. Contrast that to the statement of the chair of council of the BMA who in support of the BMA’s motion noted that the ban on puberty blockers was “unsubstantiated” and “discriminatory.”2
The difference between these two statements offers an excellent example for an often-overlooked paradox at such controversial medical decision points: medical ethics demand that treatments not be allowed to enter routine clinical practice unless previously validated in their claimed effectiveness and relative safety. In practical terms this means that whoever wishes to introduce new treatments into routine clinical practice has the obligation to frst demonstrate the treatments’ effectiveness as well as safety.

Prof. Hilary Cass, MD, a British pediatrician and former president of The Royal College of Pediatrics and Child Health was Chair of the Cass Review. The Review’s conclusions not only affected British transgender practice in children and young adolescents but changed practice in almost all European countries. Originally published on April 10, 2023, the report was politically endorsed in the U.K. by the two leading political parties - Conservative and Labour - and by several medical societies. Regarding the behavior of individual physicians, the fnal document noted in diplomatic language that “some professionals were overshadowed by an unhelpful polarized debate around conversion practice.”
This is usually done in properly designed prospectively randomized studies, where participants are appropriately consented about the fact that the treatments they are receiving are part of a study and have not yet been established as effective and/or safe. Within this context, the Cass Review correctly pointed out that for the use of puberty blockers in children, appropriate evidence for effectiveness and/or safety currently still does not exist. A recommended ban on unrestricted use of puberty blockers in children and adolescents under the age of 18, therefore, was clinically as well as ethically the correct recommendation. The Cass Review document, moreover, did not attempt to prevent or prohibit such treatments–and, indeed, encouraged them–if offered under controlled experimental protocols with appropriate informed consents.

Contrast this logical position of the Cass Review with the above-noted statement of the BMA spokesperson: he, of course, was unable to offer clinical validation and safety data in favor of puberty blockers in children and, therefore, resorted to the oldest trick in medicine proponents of unproven treatments–starting with snakeoil salesmen–have utilized for centuries, transferring the responsibility of establishing proof of utility and safety from the proponent to the opponent of a given treatment.
Accusing the Cass Review of having no (or not suffcient) data to prove that puberty blockers do not work and/or may cause long-term harm to so-treated children and adolescents, the BMA spokesperson resorted to exactly the above-described switch and bait tactic of snake-oil salesmen in selling their wears to an ignorant public, completely ignoring the fact that the responsibility for proof of effcacy and safety lies exclusively with proponents of puberty blockers (and other gender-affrming treatments).
To see such irresponsible behavior from only too often poorly informed physicians and/or obviously economically interested parties is, of course, not surprising, considering that this trick has been around since medicine has existed as a defnable professional activity. But to hear it from a representative of a highly regarded medical society like the BMA is nothing but astonishing and deeply regrettable. It can only be explained by politization of the BMA, a process which in recent years, unfortunately, also has involved several prominent medical societies in the U.S., including, regrettably, societies in the reproductive feld.
As effective as the Cass Review was in affecting clinical practice in Europe, it received much less attention in the U.S., even though the case load involving children and adolescents in the U.S. increased more rapidly than in Europe and also involved much more frequently the irreversible surgical removal of body parts. Nevertheless, in contrast to Europe, one heard almost no critical medical voices and saw almost no articles in the medical literature questioning these aggressive medical practices involving children and adolescents.
One exception has been for some time the journalist Jesse Singal, who came to the attention of the public regarding this subject already in 2018 when he wrote a cover story on the subject for The Atlantic.5 And he deserves credit for not letting go to this day. He, indeed, just published another highly informative series of two articles on the subject on August 19, 2024, and September 1, 2024 (corrected), in his newsletter on Substack, in which he accused the Yale University “Integrity Project” of spreading misinformation about the Cass Review document.6,7 And more on the subject is coming because he just announced he was taking most of September off from his newsletter to fnish a book on the subject.

Singal is a Princeton University-educated American journalist who has written for New York magazine, The New York Times, and The Atlantic and publishes a successful newsletter on Substack. He frst addressed the issue of gender affrming treatments in 2018 in a cover story in The Atlantic under the title “When Children Say They’re Trans,” which at the time received considerable attention. He is now fnishing a book on the subject.
Singal correctly pointed out in his writing that, if something was publicly written on the subject, it often only involved online political activists and their followers on the pro-intervention side and, therefore, did not represent objective information. As an example, he now recently presented in detail a (non-peer-reviewed)
Jesse
white paper published by a group of Yale University physicians (and one lawyer), paradoxically called “The Integrity Project,” which, as he well demonstrated in his scathing review, demonstrated little integrity in criticizing the Cass Review.6,7
In the two-part series of articles under the title, “Yale’s ‘Integrity Project’ Is Spreading Misinformation About the Cass Review and Youth Gender Medicine,” he quite devastatingly demonstrated the often naked selfinterests that have driven this feld–especially involving many of its surgical operatives, often strongly supported by their institutions, as gender-transitioning surgeries have become big business in the U.S.

Demonstrating a little black humor, he noted in the subheading to the frst part of his article, that his writing “will not increase the reader’s confdence in highly credentialed (medical) experts,” a very relevant point to be made, especially after the world’s recent COVID experience.
A demonstration in the U.K. against the ban on puberty blockers. Source: Jesse Singal. Substack. September 1, 2024. 7
And then there was Lydia Polgreen, a columnist at The New York Times (where else, of course?), who on August 18, 2024, went to war against the Cass Review. Under the heading, “The Strange Report Fueling The War on Trans Kids,” her conclusion regarding the Cass Review was that it was presented “as a supposedly scientifc
document but, in fact, was subjective and political.” 8
But this description is, indeed, a very good conclusion of her unusually long article (The New York Times allotted her two full pages of the paper). How Polgreen described the Cass Review, indeed, revealed itself as a highly biased, subjective, and politicized product: exactly what Singal referred to when making the point that whatever was published on the subject in the media was usually biased toward political activists and their followers on the pro-intervention side.
The Cass Review, of course, is not a perfect document; but that is not for lack of trying. Because scientifc truth constantly changes, perfection is diffcult to achieve. The Cass Review is, however, as good a document as its subject currently allows. And on top of that, it is excellent evidence for the increasing politicization of medicine, because why else would the very liberal “newspaper of record” dedicate two full pages to a political (rather than science) writer to cover this subject and trash a detailed, scientifcally-conducted medical review that took four years to perform?


Here is just one example of why political writers for scientifc topics may not be the best of all choices (there, of course are several more examples in her unusually long piece): one of Polgreen’s criticisms of the Cass Review was that it unfairly criticized the lack
Lydia Polgreen, a columnist at The New York Times, used to be editorin-chief at the HuffPost. Source: The New York Times

of available data on puberty blockers. And in support of her argument, she claimed (what else?) that this was discriminatory since so many other medical treatments also are constantly introduced into medical practice without suffcient prior validations.
She, of course, is correct that too many medical treatments (including in reproductive medicine) are introduced into routine medical practice without proper prior validation studies, and this is deplorable. Her argument, however, also demonstrates her lack of knowledge about ethical ground rules in medicine, especially since she cited as an example, treatments in the past given to very immature neonates without knowing potential outcomes of such treatments.
To compare risk-beneft between trying to save the life of a very immature neonate and offering minors potentially irreversible life-changing treatments, is simply absurd. Moreover, when very immature neonates were treated with experimental treatments, this usually happened with informed consent from the parents. Comparing giving puberty blockers to children with treating very premature infants to give them an opportunity for life, therefore, makes simply no sense and can only be explained by either complete ignorance about ethical human research or very obvious political biases. Which of the two explanations in this case applied really does not matter because both are unacceptable. Accusing the Cass Review “of fueling war on trans kids,” therefore, must be seen as highly inappropriate and as an indisputable example of the politization of medicine, in this case in the alleged “paper of record,” The New York Times.
There, moreover, exists yet another very good reason why the Cass Review should be considered an important document, and that reason is that the Review simply makes sense. It is logical in its arguments, while its opponents, very obviously, are not! Similar sentiments were recently also expressed by 900 U.K.based physicians who signed a letter urging the BMA to abandon its announced inquiry into the Cass Review.9
What the New York Times article, however, also demonstrates is that bringing politics into health
care may increasingly occur by intent. Regarding the abortion issue, this has, of course, already been obvious for many years. The similarities between the abortion debate and controversies surrounding gender-affrming care come further into focus through a recent report by Jennifer Block in The Free Press on August 7, 2024, in which she reports that Planned Parenthood apparently has started a new business: The nation’s largest abortion provider is now also one of the largest suppliers of the hormone testosterone to transitioning women.10
REFERENCES
1. Associated Press. July 16, 2024. https://www. npr. org/2024/07/16/nx-s1-5041437/californiabans-school-rules-requiring-parents-notificationof-childs-pronoun-change#:~:text=Hourly%20 News-,California%20bans%20school%20rules%20notifying%20parents%20of%20kids’%20pronoun%20 change,person%20without%20the%20child’s%20 permission.
2. Editorial. The Lancet August 3, 2024. The lancet 2024;404:405
3. Feinman J. BMJ 2024;386:q1722
4. Cass Review. https://cass.independent-review.uk/ home/publications/final-report/
5. Jesse Singal. The Atlantic. July/August 2018. https:// www.theatlantic.com/magazine/archive/2018/07/ when-a-child-says-shes-trans/561749/
6. Singal J. Substack, August 19, 2024. https:// jessesingal.substack.com/p/yales-integrity-projectis-spreading
7. Singal J. Substack (Corrected) September 1, 2024. https://jessesingal.substack.com/p/yales-integrityproject-is-spreading-ba7
8. Polgreen L. The New York Times. August 18, 2024. https://www.nytimes.com/2024/08/13/opinion/ cass-report-trans-kids.html
9. Feinmann J. BMJ 2024;386. Doi: https://doi. org/10.1136/bmj.q1772
10. Block J. The Free Press. August 7, 2024. htps://www. thefp.com/p/how-did-planned-parenthood-become
The increasing challenges to publication integrity in medicine and basic sciences

By Norbert Gleicher, M.D., who is the Medical and Laboratory Director as well as Chief Scientst at the Center for Human Reproducton.
Reprinted and edited with permission of authors and The Reproductive
Times
.
BRIEFING
As this artcle will demonstrate, there is increasing concern in science circles about the integrity of the academic publicaton process. Over the last month the subject appears to have reached new levels of atenton, as suggested by several important artcles in prominent journals. This artcle summarizes those opinions.
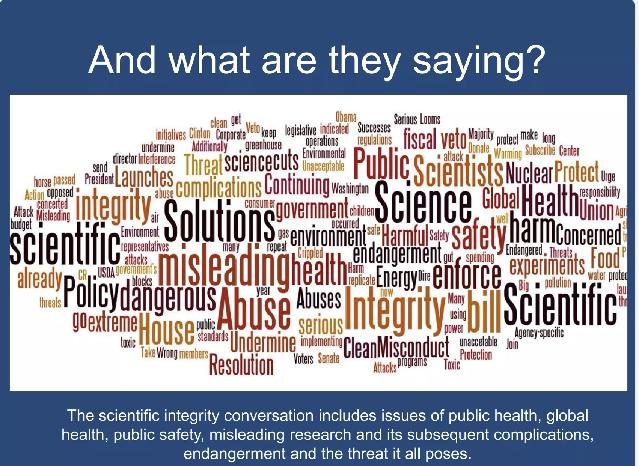

It surely looks like things are getng worse by the month, maybe even by the week, as medical and basic science journals are full of artcles lamentng a large variety of problems with scientfc publishing. Nature magazine, for example, recently noted that “investgatons by journals of potental unreliable research are ofen superfcial, opaque, and prolonged.” 1 The artcle further suggested that “changing the guidance of the Commitee on Publicaton Ethics could tghten up the process.”
An artcle in the BMJ suggested that “urgent steps must be taken to reduce misconduct, restore trust, and protect patents.” The artcle also noted that many countries have no laws or legally enforceable standards that govern research integrity, therefore, relying on natonal voluntary codes of conduct, quite obviously not sufciently efectve. An artcle in JAMA suggested that proposals from the Ofce of Research Integrity (in the U.S. Department of Health and Human Services) should prepare the academic community for more regulatory directves and less autonomy in reviewing data integrity allegatons. 3
The Wall Street Journal recently covered the subject on its frontpage by reportng extensively about a debunked cancer study. 4 Under the leadership of a very prominent physician scientst from a reputable academic insttuton, it was published several years ago in Nature magazine (likely the world’s most prestgious science journal) and reverberated through oncology as well as microbiology because it claimed that cancers have distnct microbial signatures, which should permit diagnoses through blood tests. It also reverberated through the fnance community because a start-up company (Micronoma) raised $17.5 million under the assumpton that – based on the artcle – blood tests could, indeed, be developed to diagnose specifc cancers.
Unsurprisingly, the paper was cited in other publicatons in the ensuing four years no fewer than 600 tmes before fnally being retracted in June of this year. As one scientst was quoted in the Nature artcle, “this paper polluted the literature.” The fall-out was considerable: journals have started reviewing eight other studies published since the original paper was published because they all, of course, relied on the original paper. Further retractons can be expected. And the startup shut down!
Another recent artcle in Nature reemphasized the point that bad science ofen gets propagated through the literature. 5 The author – described by the magazine as a “scientfc sleuth” and professor of computer science
at the University of Toulouse, in France, in his artcle suggested that readers ofen are not aware when a paper cannot be trusted, a point we, of course, fully agree with. He furthermore suggests that adoptng some easy-to-use technological solutons can help researchers, publishers, and referees “to clean things up.” For example, he points out that nonsensical phrases in papers can sound alarm bells.
And demonstratng how seriously Nature these days is taking this subject, another artcle in this magazine that pointed out how blind some journals (or their editors) are to citatons of already retracted papers.6 Heavily building on some of the suggestons in previously cited paper, 5 the authors put together a list of the 10 published papers with the highest percentages of withdrawn papers cited in their list of references: Astonishingly, it went from 21% to 65% of the respectve papers’ reference list.
And then there was yet another, even harder-to-believe news item that crossed the wires and it, again, appeared in Nature magazine: research integrity “watchers” recently discovered schemes that sell fake citatons, which allows researchers to artfcially infate their citaton counts, which academic insttutons increasingly consider in promoton assessments.7
Related and clearly refectng the same disturbing mindset is also the subject of ever increasing so-called predatory scientfc conferences. This, too, has recently been a repeated subject of concern in the literature. Again, an artcle in Nature magazine – this tme even in the format of an unsigned editorial –addressed this issue in some detail, making the point that these kind of exploitatve meetngs especially target vulnerable early-career researchers and warrant much more awareness by the scientfc community and possibly even legal redress. 8
In short, the scientfc enterprise must start cleaning house.
REFERENCES
1. Grey et al., Nature 2024;632:26-28
2. Bouter L. BMJ 2024;386 doi://htps://doi.org/10.1136/bmk.q1595
3. Caron et al., JAMA 2024;332(3):193-194
4. Subbaraman N. The Wall Street Journal. August 31-September 1, 2024. htps://www.wsj.com/health/healthcare/cancer-studyretracted-research-fallout-9573f842
5. Cabanac G. Nature 2024; 632:977-979
6. Van Noorden R, Naddaf M. Nature 2024;633:13-15
7. Singh Chawla D. Nature 2024;632:966-967
8. Editorial. Nature 2024;632:7
DR. ALBERTINI’S PHOTO GALLERY
As our senses get bombarded by the multmedia frenzy of the 21st century, getng informaton in a tmely and accurate fashion seems to consistently important. This is also the case when it comes to processing informaton for the eggs in a women’s ovary. As we here demonstrated last month, eggs spend the tme within the confnes of the ovarian follicle where they are nurtured for many years before being called upon at the tme of ovulaton in a process called recruitment. How is informaton conveyed from a woman’s body to the eggs in her ovaries? The mainstay of these communicaton pathways are delicate structures known as “transzonal projectons” or TZPs. Dr Albertni and others have spent decades studying these specialized structures in hopes of understanding what drives the development and maturaton of eggs in many mammalian species. Here are a few examples of how complex the landscape is at the interface of follicles and oocytes.
IMAGE I IMAGE II

IMAGE I - depicts an immature egg cell, within the cumulus complex showing striatons or stripes emanatng from the egg, all of which consttute the elaborate communicaton network of TZPs.

IMAGE II - is similar but in this case some cumulus cells have been dislodged from the zona pellucida revealing both the TZPs (yellow stripes) and the egg periphery labeled to demonstrate the presence of contractle proteins to stabilize the egg cell membrane. Note the germinal vesicle (GV) at 3 o’clock. 3



IMAGES III & IV again demonstrate an immature human egg with cumulus cells on the outside anchored to the zona pellucida. At an even higher magnifcaton in the 4th image, one can see small partcles, known as exosomes and likely transmitng informaton from cumulus cells to the egg for further processing.
MONTHLY NEWS MONTHLY NEWS MONTHLY NEWS
BRIEFING: The VOICE in this secton ofers opinions about news which in preceding months atracted our atenton and which we believe are relevant to the practce of medicine. As these are opinions – in medicine widely recognized as the lowest level of evidence – we fully recognize their limitatons due to inherent and unpreventable biases of our writers and their respectve privileges (or lack thereof). Unable to ofer consistent “truth” (assuming that something like that really exists), the VOICE, however, strongly believes that coming at least as close as possible to the most likely “truth of the moment” mandates openness to a widespread ofering of opinions. We, therefore, welcome submissions from our readers that address opinions voiced here even, or especially, if they contradict our own. They should be submited under the heading “opinion” to social@thechr.com.
Partially reprinted and edited with permission of authors and The Reproductive Times
Getting fairly covered as patients and fairly paid as providers by insurance companies
The introductory paragraph of a KODIAK RCA benchmarking analysis published in August under the intriguing ttle “Death by a thousand requests” began with the following:1
“Nothing is more frustratng, perplexing, and needlessly expensive for a provider than an inital request for informaton claim denial from a payor. Inital RFI (request for informaton) claim denials are rising and, along with them, providers’ administratve costs at a tme when they can least aford it. It’s tme for providers to take the fght to payors.”
And inital RFI claim denials are constantly increasing. Between 2022 and 2024 alone, denials increased by 8.8%. These data are in line with increasing unhappiness among medical service providers regarding how they are treated by their payors. Well-known ethicist at NYU, Arthur L. Caplan, PhD, in one of his recent commentaries for Medscape Business of Medicine put it this way: “I don’t think I’ve seen any-
thing screwier from a moral point of view than the system we have that allows preauthorizaton by third-party payor, or insurers, in order to give care to patents. It’s prety clear that a third-party payor has a confict of interest. It’s simple: They don’t want to spend money.”2
And it seems that things now may get even worse because insurers are considering the integraton of A.I. into the review and approval process. Caplan considers the whole idea to be ethically “nuts,” arguing that only (treatng) physicians really can know what a patent needs.
We, of course, agree in principle but also have to acknowledge that, just as insurance companies have been squeezing physicians and hospitals more and more, so have at least some physicians abused insurance companies with an onslaught of bills for unnecessary and/or ofen unindicated medical services. Some bad apples can do considerable damage and insurance companies have clearly overreacted: they for all practcal purposes are now actvely practcing medicine which, under the law, they are prohibited from doing.
Some of the insurance companies appear to sense the potental (legal) danger. CVS Health’s Aetna, the country’s third-largest insurance company, for example, recently announced that it would widen coverage for fertlity services, regardless of sexual orientaton or partner status.3 The changes are, however, stll inadequate. Practcally the company just removed the defniton of infertlity as one year of unsuccessful exposure to semen, from lesbians and transgender individuals who – up to this point – had to pay for one year of inseminatons out of pocket before they became eligible for infertlity coverage. The decision, therefore, does not refect Aetna’s positon that it shows the company’s commitment to women’s health across all communites, including LGBTQ+ and unpartnered individuals.
The company made this decision because Blue Cross/Blue Shield of Illinois was legally forced to make this decision.
And then – everything goes in circles – afer the HMO craze of the 1980s and 1990s which shifed fee-for-service to all-inclusive capitaton services under which a certain patent volume was assigned for all-inclusive services to a provider organizaton. In other word, providers received a certain amount of payment per patent in that sub-insured group. Providers were paid whether that member received services or not. The system, therefore, clearly incentvized less (and poorer-quality) care because the less service the provider had to give, the more proftable the contract.
Unsurprisingly, this system collapsed on itself because patents revolted due to too litle and too poor medical care. And now basically an almost identcal system is introduced under the new name, Value-Based-Care (VBC) because it allegedly focuses on patent outcomes rather than the volume of services provided, aiming for (i) Improved patent health outcomes; (ii) Reduced costs of healthcare; and (iii) Enhanced patent satsfacton.4
Good luck! Exactly the same goals were claimed for the HMO-madness in the 1980s and 1990s. And just like in those HMO days physicians were complaining about too low capitaton rates per patent, so have they started lamenting about so-called Relatve Value Units which determine provider reimbursements and, of course, are determined by insurance companies.4 Our health care system is going in circles!
REFERENCES
1. KODIAK RCA Benchmarking Analysis, August 2024. htps:// statc1.squarespace.com/statc/65d790c56a64c0761fd9171e/t/66ad47fe0c92b05e206ef424/1722632192313/ K1005+KPI+Benchmarking+Report+Aug+Q3+2024.pdf
2. Caplan AL. Medscape Business of Medicine. July 31, 2024. htps://www.medscape.com/viewartcle/insurers-rules-and-ai-preautorizaton-ethically-nuts-says-2024a1000dql
3. Japsen B. Forbes, August 27, 2024. htps://www.forbes.com/ sites/brucejapsen/2024/08/27/aetna-widens-coverag-of -fertlity-services-amid-politcal-uncertainty/
4. Vargas B. Medscape Medical News. August 22, 2024. htps:// www.medscape.co/viewartcle/physicians-lament-over-reliance-relatve-value-units-survey-2024a1000fe2?form=fpf
California may no longer want private equity-fnanced health deals
This is for two reasons a potentally important issue for the infertlity feld: First, because this is happening in California and what happens in California usually is quickly also
introduced in most other blue states. Second, private equity in the U.S. already controls more than half of the IVF cycle market and related procedures.
Gov. Gavin Newson, according to an artcle in The Wall Street Journal 1 has not yet announced whether he will sign Assembly Bill 3129 which passed the Senate by a vote of 49 to 14. If we had to guess, we would suspect that he may not sign the bill. Private equity just provides too much money to his fundraising eforts. But who knows; maybe he will surprise us. Such a law would, likely, overnight signifcantly reduce the value of existng equity investments in medicine because these investments are made with a cash-out horizon of 5-7 years. Who will then be the buyers if private equity is not permited to invest?
REFERENCE
1. Cumming C. The Wall Street Journal, September5, 2024. htps://www.wsj.com/artcles/california-senate-passes-bill-toclamp-down-on-private-equity-healthcare-deals-118a2134
How private-equity drained fnances of a hospital, putting it into bankruptcy
That – because of increasing numbers of reported negatve efects of private equity investments in medicine – such investments deserve more scrutny and, maybe as California’s above noted new law suggests, may not be in the public’s best interest, is further supported by the recent bankruptcy of a for-proft hospital (Steward Health Care System in Dallas, TX) which, according to an artcle in The Wall Street Journal on September 12, 2024, was (at least to as signifcant degree) caused by a dividend payment of $790 million by the hospital to its private-equity owner at the tme, Cerberus Capital Management. According to the artcle this payment “drained” the hospital’s fnances and it, consequently, never recovered. A spokesperson for Cerberus denied the allegaton, commentng that the company at that tme “had more than sufcient capital and liquidity.”
Whatever the underlying causes may have been for this bankruptcy, what happened to this hospital afer acceptng a substantal private-equity investment is just one more example demonstratng that such private equity investments for the investor are planned for a very short tme frame only, after which the investor – really at all costs – has to exit a deal. And under such circumstances, a proftable exit is, of course, more important for the investor than the well-being and/or survivability of the company the investor leaves behind. Un-
surprisingly, therefore, increasing numbers of experts have started to queston whether private-equity investments are appropriate for health care.
REFERENCE
1. Weil J. The Wall Street Journal, September 11, 2024. htps:// www.wsj.com/fnance/how-a-private-equity-payday-drained-ahospital-chain-of-cash-35a5cb35
The FDA updates mammography regulations
Women with dense breast on mammography will now have to be told. The reason is that dense breasts to signifcant degrees increase the risk of false-negatve mammography. Once notfed, women then have the opportunity to ask for follow up examinatons with ultrasound of MRI, with especially the later ofen not covered by insurance.
This follows a recent announcement by the American Cancer Society notng that women startng at age 40 should be given the opton of annual mammograms. It recommended annual screening startng at age 45.2 This stands in contrast to an April 30, 2024, recommendaton by the U.S. Preventatve Service Task Force which recommended that women be screened afer age 40 every two years.
REFERENCES
1. Abbot B. The Wall Street Journal. September 6, 2024. htps:// www.wsj.com/health/wellness/dense-breast-tssue-mammogram-breast-cancer-704604be
2. American Cancer Society. 2024. htps://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detecton/ american-cancer-society-recommendatons-for-the-early-detecton-of-breast-cancer.html
3. U.S. Preventatve Services Task Force Breast cancer Screening Guidelines 2024. htps://www.google.com/search?q=US+Preventatve+Task+Force+on+mammography&rlz=1C5CHFA_enUS1083US1083&oq=US+Preventatve+Task+Force+on+mammography&gs_lcrp=EgZjaHJvbWUyBggAEEUYOTIICAEQABgWGB4yDQgCEAAYhgMYgAQYigUyCggDEAAYgAQYogQyCggEEAAYgAQYogQyCggFEAAYgAQYogQyCggGEAAYgAQYogTSAQoyMjQwNWowajE1qAIIsAIB&sourceid=chrome&ie=UTF-8
An example of “fake” medical news in The New York Times picked up by many other news outlets
Why Black women in the U.S. would have 25% “unneeded” Cesarean sectons in comparison to White women would, indeed, be an important queston to fnd out; that is, if one
assumes this informaton is, indeed, correct.
But before we get to addressing this queston, a litle bit of interestng background: On September 6, 2024, Sarah Klif reported in The New York Times1 on a study by Janet Curts, PhD, et al., the Henry Putnam Professor of Economics and Internatonal Afairs at the Princeton University School of Public and Internatonal Afairs, which – based on a large study of almost 1 million births in 68 New Jersey hospitals – found that Black women demonstrated a 25% excess in Cesarean secton deliveries compared to White mothers. In additon – and important to note – the headline of the Klif artcle noted that these excessive Cesarean sectons were “unneeded.”
Within 24 hours her artcle had become the basis for several reports, including by CBS News, 2 even though Klif referenced no peer-reviewed study in her artcle and a quick literature search we conducted for such an artcle under the authorship of Janet Curts was unsuccessful.
In other words, here was The New York Times – based on no source data whatsoever – reaching the conclusion that Black women in the U.S. undergo 25% more “unneeded” Cesarean sectons and distributed this informaton as a fact and, since it was The Times, everybody picked up the message without asking where all of this informaton was coming from.
As we are writng this commentary, we have absolutely no idea what kind of informaton Curts apparently ofered Klif for this artcle. We, however, know one thing for sure: unless we see data or at least are reassured that a writen manuscript underwent competent peer review, the informaton provided by Klif is not only worthless but also irresponsible. Even if Curts as an economist is assumed to understand the subtletes of defning what is a “needed” vs. “unneeded” Cesarean secton – even competent obstetricians ofen disagree on this issue – it appears irresponsible to disseminate a not only medically unproven allegaton but, in this case also an unproven allegaton of racism.
Black women have consistently, and globally, worse pregnancy outcomes than White women.3 This fact alone not only explains higher Cesarean secton rates in Black women, but mandates them. Shame on The New York Times and every other media outlet that reprinted this – as of this point – totally unsupported allegaton of “unneeded” Cesarean sectons in Black women!
REFERENCES
1. Klif S. The New York Times. September 11, 2024. 2024. htps://www.nytmes.com/2024/09/10/health/cesarean-sec-
tons-black-women.html
2. Stahl S. September 11, 2024, CBS News. htps://www.cbsnews. com/philadelphia/news/new-research-black-women-unnecessary-c-sectons/Janet Curts, Cesarean Sectons
3. Natonal Insttute for Health Care Research. May 25, 2023. htps://evidence.nihr.ac.uk/alert/black-women-around-theworld-have-worse-pregnancy-outcomes/
Is all the commotion surrounding A.I. just a marketing scam?
We do not recall ever before to have been inspired by an advertsement to write a commentary; but there is a frst tme for everything. The Dawn Project was founded by Dan O’Dowd, who describes himself as ‘the world’s leading expert in creatng sofware that never fails and can’t be hacked.’ He created the Dawn Project which “is dedicated to making computers truly safe for humanity.”1 He describes the problem in this way: “Connectng the power grid, hospitals, and millions of cars to the Internet with sofware riddled with millions of bugs and security defects has turned these systems into weapons of mass destructon. Hackers can use these systems to kill more people than an intercontnental nuclear bomber. We must convince the CEOs and Boards of Directors of all the companies that build systems that our lives depend on to rewrite all their sofware, so it is as safe and secure as if it were for an intercontnental nuclear bomber. And we must do it now. The clock is tcking down to Cyber Armageddon.”

The Dawn Project’s full-page advertsement in The Wall Street Journal on August 14, 2024, suggestng that the world is falling victm to a gigantc scam by the high-tech industry and that the Magnifcent Seven’s defectve A.I. systems are useless for anything beyond trivialites. 2
The Dawn Project recently took out full-page advertsements in many leading newspapers, including The Wall Street Journal (see Figure above), addressing this tme a related though quite diferent issue: the unprecedented commoton throughout the world regarding Artfcial Intelligence (A.I).
What atracted us this opinion presented to the public in the format of a quite original marketng campaign is the image of the snake oil salesman.
REFERENCES
1. The Dawn Project. htps://dawnproject.com/about-us/#soluton
2. The Dawn project. htps://dawnproject.com/dan-odowd-discusses-the-ugly-truth-about-silicon-valleys-artfcial-intelligence-systems-in-internatonal-policy-digest/
Ethics still count in …
… gender affrming care: It is good to see that ethical issues in medicine stll fnd atenton. Here are a few examples: The VOICE in this and in previous issues addressed the professional (and politcal) diferences that currently divide medicine on the subject of medical care for transgender and nonbinary youth. But, as a recent Viewpoint artcle in JAMA correctly noted,1 those diferences of opinion should not divert from the fact that – now more than ever – transgender and nonbinary youth not only exist in much larger numbers than, likely, ever before, but also from the fact that – more than ever before – they need good-quality medical and psychological treatment programs.1
The authors suggested that pediatric hospitals may be the best places for such programs. Though good arguments can be made for placing such programs into pediatric hospitals, especially here in the U.S., where some leading insttutons in the past have developed clearly over-aggressive interventonal programs, such an approach raises serious questons. Indeed, wherever such programs are, past experiences have clearly demonstrated that they require close supervision for obvious politcal biases and, it must be said, economic exploitaton and fnancial conficts.
… study recruitment: A strong motvaton for the partcipaton in prospectve studies in medicine has been the widely held belief that this benefts patents in their clinical outcomes.2 More recent data, however, raise questons as to what degree that, indeed, may be the case and whether such benefts are not exaggerated during consent procedures in atempts to recruit more study partcipants. A physician lawyer from Singapore recently addressed this issue in another Viewpoint artcle in JAMA3 and concluded that
“the problem arises when researchers turn from the ethics of clinical care to the ethics of research.” In other words, the physician’s priority no longer is the patent but the answer to a research queston. He has a point!
… the wellness industry: Well-known NYU ethics professor, Arthur L. Caplan, PhD, in a Commentary in Medscape Business of Medicine let loose on the wellness industry, describing it as “fnancially toxic.”4 And he has a point, because – as he noted – the world is supposedly spending $1.8 trillion on “wellness” which he describes as wasted to “cover bunk, nonsense, and charlatsm,” while those funds could go to much beter use elsewhere to really improve health. His criticism goes “to everything from gut probiotcs sold in sodas to probiotc facial creams and the Goop industry of Gwyneth Paltrow, where people buy things like wellness mats or vaginal eggs that are supposed to maintain gynecologic health” and he considers this whole industry to be “out of control.”
… genetic screening: And how can a subsecton on ethics be concluded without a word about genetc testng? A recent unsigned editorial in the highly prestgious medical journal Nature Medicine was presented under the heading, “Every baby deserves access to genetc screening.”5
Quite unexpectedly considering the importance of this journal, we found this editorial in some ways to be “schizophrenic.” One, of course, must agree with “genomic-based newborn screening having the potental to revolutonize health care,” and one also cannot disagree with the demand for “new solutons to ensure “that derived benefts are equitably available.” One, however, also must be extremely concerned about the potental implicatons on society from somewhere in the cloud a signifcant amount of genetc informaton on all of our children lurking, just waitng to be stolen like all of our other informaton is stolen on a daily basis from allegedly most secure electronic storage systems.
That our genetcs colleagues always advocate for more genetc testng can, of course, not surprise and, likely, will never end. But that does not mean that the rest of the world should, blindly, accept every recommendaton by the genetc testng industry for ever increasing prospectve genetc data accumulatons. The editorial acknowledges security concerns and concerns about the impact of such data on the baby’s lifetme. It even recognizes that parental consent afer birth may be contradictve to the individuals own wishes later in life.
But startng with a heading that suggests that every newborn should undergo a comprehensive genomic evaluaton, and that such informaton “is likely to provide immediate
lifesaving informaton for children” appears incorrect and is, therefore, disturbing. First of all, how much immediate lifesaving informaton such routne testng would produce – at least as of this point – is very questonable and actually contradicts the editorial’s own later statement that how availability of such data will afect the baby’s lifetme and the baby’s family remains to be seen.
What we, however, fnd most disturbing is that somewhere in the bowels of the genetc testng industry – using this editorial in a highly prestgious medical journal - somebody is already putng together the next start-up company that will ofer parents full genome testng of their newborns, - and many parents will buy it, - believing that they are actng in the best interest of their ofspring. At least as of this moment, - they are not!
REFERENCES
1. Santos et al., JAMA 2024;332(7):529530
2. Natonal Insttute for Health and Care Research. September 2, 2016; htps://evidence.nihr.ac.uk/alert/partcipaton-in-healthresearch-may-be-linked-to-beter-care-and-performance/
3. Menikof J. JAMA 2024;332(3):195196
4. Caplan AL. Medscape Business of Medicine. htps://www. medscape.com/viewartcle/wellness-industry-fnancial-toxic-says-ethicist-2024a1000fc6?form=fpf
5. Editorial. Nature Medicine 2024;30:2095-2096
Do you know what an “Absolute Uterine Factor” is?
Do you know what an Absolute Uterine Factor is? If not, we believe you are not alone! An “Absolute Uterine Factor”— clearly also deserving of an acronym (i.e., AUF), is nothing but an absent uterus. Yes, an absent uterus and an AUF are one and the same! Then why all of the semantcs? One explanaton is because an absent uterus would not sound important enough as an indicaton for the performance of uterine transplants.
One can only admire the impeccable stepwise research over many years by Swedish investgators under the amazing leadership of Mats Bränström, MD, startng with years of animal studies before taking the procedure to a human trial and achieving in 2012 not only long-term tolerance of the transplant (a frst human uterine transplant that had to be removed was performed already in 2000 in Saudi Arabia) but in 2014 also the frst delivery of a healthy ofspring in Australia.
At the same tme and from the very beginning several experts in the infertlity made the argument that just because
something can be done, does not mean it should be done, as certain things may just not be worthwhile doing. And— at least within reproductve medicine—there is no beter example for such a circumstance than the amazing ability of achieving successful uterine transplants which then allow recipients of these transplants to go through pregnancy and delivery. A recently published report of several U.S. centers on the IVF practce in patents with AUF undergoing uterus transplants only further reafrmed this positon on ethical, clinical, and fnancial grounds.1
The study included 31 transplant recipients at mean age of 31.0 ± 4.7 years who before their surgery completed between 1 and 4 oocyte retrievals, banking 3-24 by PGT-A untested embryos or 2-10 by PGT-A as euploid reported embryos. Additonal post-transplant retrievals were required in 19% of patents for a total of 16 cycles (2-4 per patent). PGT-A was used in 74% of patents.
A total of 72 autologous embryo transfers occurred in 23 women, with 70 using frozen and 2 cycles using fresh embryos. The live birth rate per cycle was 25/72 (34.72%) afer 1st embryo transfer; it was 13/23 (56.52%) and rose to 17/23 (73.91%) afer the 2nd transfer. In comparison to matched non-transplant IVF patents, there was no diference in obstetrical outcomes, nor were there any outcome diferences between uterine transplants from living or deceased donors.
Those, of course, are outstanding IVF cycle outcomes, even considering the young age of the patent populaton. However, it took an accompanying Refecton artcle2 to point out the following: 8/31 (25.81%) had a uterine graf failure. Per intent to treat, above noted live birth rates, therefore, would only have been 41.94% afer a 1st transfer and 54.84% afer the 2nd transfer, though stll very respectve outcomes. More importantly, however, the authors of this commentary also pointed out that most recently available U.S. data for IVF cycles using gestatonal carriers reported a 52.4% live birth rate.3
In practcal terms this means as the authors correctly stated that the use of a gestatonal carrier—the current standard method of helping women with AUF to have autologous children—stll represents the most optmal treatment for them. And that does not even at all considers the morbidity for living uterus donors, morbidity from removal surgery of the transplanted uterus once a patent has completed childbearing and, of course, the dramatcally higher costs of uterine transplantatons, which stll greatly exceed by many multples the quite signifcant costs of a gestatonal carrier.
Therefore, it seems worth repeatng: Just because we can do something does not mean we should do it!
REFERENCES
1. Walter et al., Fertl Steril 2024;122(3)-404
2. Pereira N, Lindheim SR. Fertl Steril 2024;122(3):435-436
3. Traub et al., Am J Obstet Gynecol. 2024. S0002-9378(24)005532.doi: 10.1016/j.ajog.2024.04.027. Online ahead of print.
Are we ready for what may come after IVF?
If you believe a recent guest essay in The New York Times by Ari Schulman, editor of The New Atlants, “a journal of technology & society,”1 the world is not ready for what comes afer IVF. What he appears mostly concerned about is in vitro gametogenesis, the producton of new eggs and new sperm, most likely from stem cells. Schulman, moreover, expects society to “turn against reproductve technology” in the very near future because he perceives Silicon Valley to represent the focal point of much of today’s critcism and, as everybody knows, Silicon Valley “is getng more involved” in reproductve medicine (boy, is he right on that point!)
Presentng himself as a “classical-liberal critc of assisted reproductve technology,” he claims to talk for so-characterized individuals when arguing that it would be “unethical to turn the arrival of a child – which should be considered a gif – into a project in satsfacton of our own ambitons.” In short, infertlity treatments are probably unethical and should be abandoned.
And we thought that it was the politcal right the IVF feld had to be concerned about; but now it turns out that in our topsy-turvy world that was exactly wrong. What the infertlity feld really has to worry about are what the author, himself, described as classical liberals on the lef. This, however, on second thought should not be too much of a surprise: Afer all, most of the right loves children; and much of the lef, less so!
Have we really reached the point on the lef when, if pregnancy doesn’t happen on its own, doing something about it is perceived as “unethical?” Schulman presents his artcle as a demand “to set limits now” to the “designing of children.” We, however, would argue that almost nothing would elicit more moral resistance in the infertlity feld than atempts at “designing babies.”
Some outliers exist in any group and the infertlity feld, for sure, is no excepton. Polygenic risk scoring (PRS) of embryos, unfortunately propagated by some such outliers, indeed, could be misunderstood as “designing babies;” but while by no means an excuse, PRS at the current tme is more a busi-
ness of selling snake-oil than of “designing babies.”
Not being known as defenders of PGT-A, we nevertheless have no choice but to in this instance defend PGT-A since Schulman included PGT-A among procedures used for “designing babies.” While chromosomal analyses of embryos, of course, allow for the determinaton of sex, to argue that PGT-A is used to select in China an “overclass” of boys and an “underclass” of girls is nonsense because China prohibits PGT-A laboratories from reportng the sex of embryos, exactly to prevent sex selecton. And in contrast to many Western countries, in China laboratories follow government advisories to the dot.
Moreover, already years ago, CHR investgators demonstrated that, while in the U.S. (where sex selecton is legal) certain minority populatons (Chinese and other Asians, as well as couples from Middle Eastern countries) for cultural reasons, indeed, preferred selectons for male, a large majority of Caucasians and other minorites actually preferred selectons for females.2
How politcal this artcle basically is becomes apparent not only from the fact that it was invited and appeared on the opinion pages of the very liberal New York Times, but also by the author apparently not being able to help himself from bringing Elon Musk into the picture and describing him as having “pronatalist ambitons,” among those, “his desire for ‘smart people’ to have more children, his reported extensive use of IVF and surrogacy” (the author likely cannot diferentate between use of a gestatonal carrier and a surrogate3), “and his serving as a sperm donor” (we wonder about the sources for all of this informaton).
In short, just another example for the increasing politzaton of medicine and science in general! With reproductve medicine at the cutng age of producing and maintaining life, this medical specialty may, indeed, have to get beter prepared for increasing future controversy.
REFERENCES and NOTES
1. Schulman A. The New York Times. September 9, 2024. htps:// www.nytmes.com/2024/09/09/opinion/ivf-debate.html
2. Gleicher N, Barad DH. Hum Reprod 2007;22(11):3038-3041
3. A gestatonal carrier just carries a pregnancy produced with an embryo produces by an unrelated couple. Asurrogate contributes her wone eggs to the pregnancy for an unrelated couple)
with bird fu with no apparent contact with animals,1 now a follow-up report suggested that someone who lived with the inital patent also got ill.2 A CDC ofcial was quoted as saying that there currently was no epidemiological evidence to support person-to-person transmission of the H5N1 virus but his comments suggested that this must be considered a possibility and further research would be pursued. Since frst discovered in dairy catle in March, the virus has been reported in 14 people, 13 of whom had direct contact with infected catle or chickens.
REFERENCES
1. Aleccia J. AP News. September 6, 2024. htps://apnews. com/artcle/bird-fu-human-missoiri-769d0a52bae2f97a5a 0df13f9e733619
2. Mandavilli A, Anthes E.The New York Times. September 13m 2024. htps://www.nytmes.com/2024/09/13/health/ bird-fu-missouri.html
FDA WARNING regarding Veozah® (fezolinetant); may cause liver injury
Veozah®, the only FDA-approved non-hormonal medication for hot-flashes in menopause (Astellas Pharma), according to a recent warning by the FDA can cause rare but serious liver injuries. According to the warning, stopping the medicaton if there are potental signs or symptoms of liver injury, could prevent worsening of the injury and potentally return liver functon to normal. This warning was posted afer only one post-marketng report of a patent with elevated liver functon tests and signs and symptoms of liver damage afer taking the medicaton for approximately 40 days. The FDA, therefore, does not discourage women from using this efectve treatment but recommends more frequent liver functon testng.1
REFERENCE
1. Manalac. T. BioSpace. September 13, 2024. htps://www. biospace.com/fda/astellas-hot-fash-drug-veozah-slappedwith-another-fda-warning-for-liver injury#:~:text=The%20 FDA%20on%20Thursday%20added,rare%20but%20serious %E2%80%9D%20liver%20injury.
Summer Olympics in Paris, a COVID “success story”
Is it time to worry about H5Ni, the bird fu?
Afer inital reports of a Missouri patent who was diagnosed
According to the WHO, at least 40 athletes tested positve for COVID during the Games in Paris (not including the Paralympic Games) but that is considered an improvement over Tokyo and Beijing. One additonal feature supportng
the relatve irrelevance of COVID in comparison to the 2021 Summer Games in Tokyo and the 2022 Winter Games in Beijing—which both had strict restrictons—the Paris games had absolutely no formal requirement for testng or reporting.1
REFERENCE
1. Kekatos M. ABC News. August 15, 2024. htps://abcnews. go.com/Health/summer-olympic-games-paris-covid-successstory/story?id=112829794
Alabama IVF clinics still concerned
The New York Times reported that despite a new law meant to protect IVF clinics in Alabama, patent and physician concerns persist, driving some doctors and their patents to move their embryos out of state and/or destroy them. There appears to be litle trust between the state’s public and its legislature, which is somewhat surprising, considering that, following the now-infamous Alabama Supreme Court decision equatng human embryos with “life,” both major partes supported a new law that was supposed to keep IVF where it was before the court decision.
Though the reported concerns appear exaggerated, the CHR will gladly accept frozen embryos from Alabama and promised they will stay on the center’s premises (many IVF clinics increasingly sub-contract long-term cryopreservaton out). New York City, according to the artcle, is a popular shipment destnaton.
REFERENCE
1. Chorayshi A, Klif S. The New York Times. August 13, 2024. htps://www.nytmes.com/2024/08/12/health/ivf-embryos-alabama.html
Making pregnancies safe for surgeons (and obstetricians/ gynecologists)
Published data suggestng signifcantly larger pregnancy risks and complicatons among surgeons (probably including obstetricians and gynecologists) than in control populatons have become very convincing. A surgeon, an obstetrician/ gynecologist, and public health specialists from the University of Wisconsin in Madison, WI, now got together and wrote an interestng review on the subject that should be very helpful to who either is trying to go through pregnancy as a practcing surgeon or supervises especially surgical training
programs.1
REFERENCE
1. Glazer et al., JAMA Surg 2024. doi:10.1001/jamasurg.2024.0979
Watch your facial temperature; it reveals age and disease
We usually like the weekly Commentary of Yale’s F. Perry Wilson, MSCE, MD under the name “Impact Factor,” published by Medscape. He pointed us in a recent issue 1 toward a paper in the journal Cell Metabolism 2 which went beyond the increasingly ubiquitous presence of facial recogniton sofware in our environment to reporting on algorithms that from a picture of a face can also obtain the age of the individual.
Unsurprisingly performed in China (considering how pervasive facial recogniton already is there), the study involved 2,811 facial images of Han Chinese at age 20-90 years. What they called their “ThermoFace” deep learning model had a mean absolute deviaton for age of about 5 years in cross-validaton and of 5.18 years in validaton with an independent cohort. The diference between predicted and chronological age—according to the authors—was highly associated with metabolic parameters, sleeping tme, and selected gene expression pathways for DNA repair, lipolysis, and ATPase in blood transcriptome, as well as exercise. A ThermoFace disease predictor, consequently, was able to forecast metabolic diseases. Faty liver, for example, was predicted with considerable accuracy (AUC >0.80).
The investgators could also with considerable accuracy determine who ate seafood (they usually looked younger than their age) and who ate meats (who looked older than their age); they could predict who was getng more sleep (they looked younger), and who ate more yogurt (also looked younger). These paterns also allowed recogniton of those with higher BMI, higher blood pressure, and higher fastng glucose. Moreover, two weeks of rope-jumping makes one look fve years younger.
Can you imagine where all of this may end up?
REFERENCES
1. Wilson FP. Medscape July 2, 2024. htps://www.medscape. com/viewartcle/how-facial-temperature-revelas-age-and-disease- 2024a1000c73
2. Yu et al., Cell Metab 2024;36(7):1482-1493
The Lancet describes direct-to-consumer medical testing as built on fear
In an unsigned editorial regarding direct-to-consumer medical testng, The Lancet did not hold back recently, demanding tghter regulaton of the industry. The editorial, however, also called for “a honest conversaton” with the public about benefts, risks, and potental economic value of asymptomatc screening tests. Is a pleasure to – for once – agree with The Lancet!1
REFERENCE
1. Editorial. The Lancet.2024;404:991
The politization of the nation’s top medical schools.
In an opinion piece in the New York Post on September 15, 2024, Jay P. Greene, who is a senior fellow at Do No Harm, a natonal associaton of medical professionals that describes itself as “combatng the atack on our healthcare system from woke actvists,” reports on a study he conducted which strongly suggested that “the naton’s top medical schools prioritze lef-wing actvism over science.” Instead of classes on anatomy and physiology, they are forced to take classes on justce and diversity.1
Why does that not surprise? The subject has been addressed in the VOICE repeatedly in recent months. It is not only our medical schools that have gone woke; so have most of our medical societes (just visit the website of ACOG as an example). Looking at the inclusion of “ideology” into curricula in the country’s 10 highest-ranked medical schools (per US News and World Report ranking) based on publicly available course catalogues, he searched through content analysis for specifc keywords, eight politcized words and eight scientfc or medical terms (examples: race/racism and equity vs. chemistry and physiology) Across all course catalogues, politcized words appeared over 2,400 tmes; scientfc and medical terms only 1,900 tmes. Among the top 10 schools, only Duke and Washington University skewed more toward science than politcs, though also not by much. Stanford led the pack of wokeness with ideological terms beatng science more than two to one. Thank God A.I. is coming to help these future doctors make diagnoses!
So, what then are we to do with college and university campuses where wokeness rules? For at least some answers
to this highly complex issue we refer our readers to a quite remarkable recent artcle by Jennifer Schuessler, who is a reporter for the Culture Secton of The New York Times. Her artcle atempts to negotate between the Republican (or beter described non-woke) viewpoint that colleges should embrace “viewpoint diversity” (the president of Wesleyan University apparently prefers the term “intellectual diversity”) by hiring more conservatve faculty members (most colleges nowadays, of course, have an overwhelming majority of liberal and very faculty members). The woke lef on the other hand “sees such eforts as breaking the current status quo and, thereby, weaponizing academic values against itself.”
This artcle is defnitely worth a read, and not only because it, amazingly, appeared in The Times. The paper even printed the following quote from a prominent psychologist: “When universites have lost the trust of centrists and moderates, you can’t blame it on the right.” Wow!
REFERENCES
1. Greene JP. New York Post. September 15, 2024. htps://nypost. com/2024/09/15/opinion/new-study-fnds-medical-schools-value-actvism-over-science/
2. Schuessker J. New York Times. September 14, 2024. htps:// www.nytmes.com/2024/09/14/arts/viewpoint-diversity-universites-conservatves.html
The discussion of antisemitism and DEI in colleges and universities continues
And since we are already talking about college educaton, interestngly once again in the opinion pages of The New York Times, two senior Stanford University academics (one a former dean of the university’s law school) concluded that programs at the university were too ideological, which only exacerbates problems on campus. In other words, “DEI is not working, and new approaches are needed,” paraphrasing the ttle of their artcle.
The original impetus for their artcle appears to have been the rise of antsemitc incidents afer October 7, 2023, at the Stanford campus. Both authors were appointed to a subcommitee “on antsemitsm and ant-Israeli bias, which (what a surprise!) concluded that, “many Jews and Israelis have experienced bias and felt insecure on campus.” In the following sentence the authors–not even appreciatng its absurdity–note that a parallel commitee formed to address ant-Muslim, Arab, and Palestnian bias reached similar conclusions.
In other words, when Stanford University – like many other leading universites and colleges much too late – notced that it had a signifcant antsemitsm problem, it apparently also felt that it had an at least similar ant-Muslim problem. Why would it, otherwise, have established two subcommittees in parallel to investgate antsemitsm and ant-Muslim biases? Yet, in contrast to the innumerable, and very obvious antsemitc events that took place on the Stanford campus, has anybody heard about even a single ant-Muslim event prior to establishment of these subcommitees? Of course not, - because there were no such events; yet, interestngly, as the artcle noted, the ant-Muslim bias commitee “reached similar conclusions to the antsemitsm subcommitee.” Seriously?
The authors then noted that the antsemitsm subcommittee felt pressured by many of the 300 people they “listened to” during 50 listening sessions “to recommend adding Jews and Israelis” (an interestng Freudian distncton!) “to the identtes currently recognized by Stanford’s DEI programs, so that their harms would be treated with the same concerns as those of people of color and LGBTQ+ people, who are regarded as historically oppressed.” And it is at this point – when there was pressure to add Jews and Israeli’s to traditonally oppressed minorites, the two authors (and we assume other academic leaders) suddenly notced that DEI does not really work!
Are you getng the point? Here is just one more example for how what widely for decades has been considered “kosher” (or – to demonstrate our objectvity – “halal”) for everybody, once it comes to the Jews (forgive us for throwing Israelis in with Jews; there, of course, also exist Muslim, Christan, and other believers among Israelis), things no longer apply. And isn’t this exactly what one would defne as antsemitsm? So, what led two leading sages among Stanford’s academic leadership to come to the conclusion that DEI no longer works? Coming from such two prominent voices, the answers are disappointng, though not surprising, because they have been obvious for quite some tme. It just took the no-longer deniable antsemitsm on campuses to make things so obvious that even liberals, like the two authors of The New York Times’ op-ed, no longer can deny the obvious: “Rather than correctng stereotypes, diversity training too ofen reinforces them, breeds resentments, and impedes students’ social development,” the two authors apparently only very recently discovered. And they went on, “overall, these programs may undermine the very groups they seek to aid by instlling a victm mind-set and pitng students against one another.”
To the objectve observer these words sound like plattudes because they are plattudes. They just state the obvious, what every clear-minded and not ideology-contaminated college professor should have deduced from what was happening on college and university campuses for years. And especially at a school like Stanford – which prides itself on being one of the essental intellectual hubs of this country, if not the world – it is not only astonishing that it took these two authors so long to reach these conclusions but, as they noted in their artcle, that only now “an increasing number of educators are coming to these conclusions.”
And what are the recommended solutons? Unfortunately, here, too, all the two authors have to ofer are more plattudes: “Confictng viewpoints must be brought into conversaton with one another in a constructve way, to form a picture that is more complete and reliable than we would have were we to look at only the dominant perspectve or only at subaltern perspectves,” to quote another academic “thinker” the artcle refers to (does this not sound exactly like a Kamala Harris answer?) A Harvard “thinker” on the subject is quoted as suggestng – what else – a new term, “confdent pluralism,” defned as “honoring our own values while making decisions together.”
We could go on with examples of further plattudes in the artcle but do not want to challenge the patence of our readers. Only so much: to demonstrate the absurdity in the thinking process of too many current academic intellectuals, here is the artcle’s closing paragraph: “The current system is not good for Jews at Stanford and other universites. It’s not good for Muslims, either. And it’s certainly not good for society as a whole.”
We, of course, fully agree that DEI is not good for society as a whole; but to once more, feel obliged to compare antsemitsm to ant-Muslim biases is absurd; and to use the recent surfacing of antsemitsm on campuses to DEI, is beyond absurd. Antsemitsm is as old as the Jewish religion and DEI is/was just one of the most recent fashionable ideological manifestatons of radical socialism.
Unfortunately, the intellectual dishonesty of this New York Times artcle only confrms the contnuing intellectual dishonesty of academic leaders at almost all leading colleges and universites who apparently to this day have not learned anything from their failures in dealing with the consequences of what happened on their campuses following October 7, 2023.
REFERENCE
1. Brest P, Levine EJ. The New York tmes, August 30, 2024. htps:// www.nytmes.com/2024/08/30/opinion/college-dei-programs-diversity.html
Membership uproar at the British Medical Association (BMA)
Elsewhere in this issue of the VOICE, we in the form of an Editorial lament the politzaton of medicine, with the example chosen to demonstrate the point being the controversy surrounding the Cass Review on gender identty services and treatments of children and adolescents published to initally quite thunderous applause afer four years of investgaton in the U.K. We there also noted that – afer initally being very well received – to everybody’s surprise the BMA (out of all organizatons!) suddenly turned hostle and voted against the Review.
Now the BMA appears in the midst of a major crisis because a signifcant membership opposes its stance and have initated a “not in our name campaign.” According to a Lancet report,1 comments accused the BMA of lack of transparency and disregard of evidence (we suggest you peruse our above noted editorial elsewhere in this issue of the VOICE). Words like “disappointed,” “shocked,” and “appalled” were recurrent comments.
Interestngly, since the BMA’s rejecton of the conclusions of the Cass Review, the Academy of the Medical Royal College reiterated its support of the Review.
Though all of this happened in the U.K., why is this of importance for the U.S.? Because, unfortunately, in the U.S., in contrast to the U.K. and other European countries, academia and organized medicine have been very quiet regarding gender-afrming care of children and young adults for much too long. In many ways, remaining quiet in the face of poor medical and ethical practces, however, speaks for itself. Which brings us to the second reason why those occurrences in the U.K. can teach us something here on the other side of the Atlantc: as members of professional organizatons, nobody forces us to accept all the crap that they ofen serve up on their membership without proper prior consultaton.
REFERENCE
1. Thornton J. Lancet 2024;404:1004-1005
What to do if you get plagiarized?
As if we would need further evidence of the deterioraton in publicaton integrity (see also the earlier artcle on
publicaton integrity by N. Gleicher, MD, in this issue of the VOICE), Dan Garisto published in Nature magazine the story of a scientst who was asked to review a paper for a journal because it was in his area of expertse. As he pursued the review, he noted a fgure identcal to what he had published on the subject.1 He advised the journal, and the paper was rejected. Low and behold, it nevertheless a few weeks later appeared in print in another journal. Afer being informed, the journal, Proteomics, retracted the paper.
As it turned out, the paper was the product of a Moscow-based paper mill (yes, not only China has those!), and the paper was retracted, eith four of the listed authors claiming to have had no knowledge of the paper and its submission. Unbelievable; and strikingly bad luck for the perpetrator of this scam because imagine somebody else was the original reviewer. This scam would, likely, never have been detected, leaving one wondering how many other such fake-papers are out there and are being widely cited.
REFERENCE
1. Garisto D. Nature 2024;633:260-262

ADVERTISEMENT
A.I. vs human intelligence - who wins in extracting data from medical records?
So-far physicians are doing beter than generatve artfcial intelligence in extractng data from medical records a recent study by investgators from New York’s Columbia University demonstrated.1 One, however, wonders how long this advantage will last, considering how many medical providers are in the process of bringing more order traditonally ofen by hand-writen medical records.
REFERENCE
1. Burford et al., JAMA Network Open 2024. 7(8):e2425981
What differentiates IgE from antibodies of other isotypes?
The answer is that IgE -producing plasma cells are transcriptonally and functonally distnct from other isotypes, as a recent paper in Science Immunology suggested. The CHR has a longstanding interest in IgE since observing some case of complete absence of IgE in infertle women. Ever since the queston has been circulatng at CHR, what -besides being a mediator in allergic reactons – does IgE do? Or stated even beter, how come complete absence of IgE does not have any clinically obvious consequences? Unfortunately, this paper also does not ofer an answer.
REFERENCE
1. Vecchione et al., Sci Immunol 2024;9(99). DOI: 10.1126/ sciimmunol.adm8964
An interesting example for the unpredictability of assumptions: Will free medical school attendance boost diversity?
Medical schools thought so; indeed, it was a main argument when NYU as a frst medical school became tuiton-free. Why did they think so? Because of the hypothesis that the cost of going to medical school – in other words the accumulaton of tuiton (and other) debt – represents the principal reason why minorites are incapable to equal opportunites.
A recent artcle in Medscape Hospital Medicine, however set the record straight, using the NYU experience of going tuiton-free as the study subject:1 Afer announcing that the school had gone tuiton-free, applicatons went up by almost 50%. Among desired previously underrepresented groups the increase was even more pronounced, fully doubling. But here come the ultmately most telling results: At 3%, the acceptance rate for underrepresented minorites remained the same as before. Moreover, the GPA on the MCAT (the test required to get into most medical schools) went up for admission to NYU’s medical school. While students from low-income backgrounds used to represent ca. 12% of every incoming class before the change in tuiton policy, since the change it has been only in the 3% to 7% range.
What are, therefore, the conclusions? First, of course, tuitons have been proven not to represent a principal problem, - one more hypothesis (this tme a social hypothesis) that seemed so obvious, and in practce failed to deliver, a fnding medicine, of course, should not be surprised about, considering how ofen hypotheses in medicine fail in clinical practce. But the principal conclusion must be that in trying to achieve more diversity in medical schools, two important goals for society are currently clashing, the noted desire for more diversity and the desire of most societes to build on meritocracy.
So, what is then the soluton if more diversity remains the goal? The artcle, unfortunately, ofers only the usual clichés: Outreach and equal opportunity from early on in life and mentorship through K-12 and college, MCAT prep, etc. These are, of course, all good ideas; but they do not consider the likely most important factor that, ultmately, makes our children succeed or fail, - and that is what they are taught at home!
The home not only maters, - it is essental! There is a reason why poor Asian immigrants not only have no difcultes in being accepted into our best colleges and universites but – if not discriminated against by admission commitees – would by-far exceed their expected proportonal representaton. They to a large degree stll have two-parent homes with demanding parents. This is the reason why the two sons of one of the CHR’s Chinese billers who spoke only broken English were accepted into every single Ivy League school and within one generaton will achieve full integraton and economic success in the U.S. And neither one went to fancy private K-12 schooling; both went to public schools.
These are by not new conclusions. Indeed, already in 1965
the so-called Moynihan Report [so named afer Senator Daniel Patrick Moynihan (1927-2003) from New York] in calling for natonal acton to combat Black poverty, identfed family structure as “the fundamental problem” of Black society and argued for federal interventons with the goal of establishing “a stable Black family structure.”2
And since 1965, things have, indeed, even been gettng progressively worse, with single-parent households steadily increasing, heroic single mothers ofen simply not being able to control especially their male ofspring (a principal reason why females do so much beter in college admissions than males3) The truth of the mater, therefore, is that – unless and untl – society does not take signifcant steps to combat and reverse the break-up of the family unit and instlls in family units (and that, of course, includes if possible two parents and grandparents) the value of educaton, throwing more and more money at a non-performing educaton system will not stop the steady decline in the quality of educaton of our children – especially in poorer inner cites. As The Washington Post noted, especially “public educaton is facing a crisis of epic proportons,”4 and while schools and teachers’ unions to a large degree are responsible for the decline from bad to worse, parents, government, and society as a whole share in the blame.
REFERENCES
1. Patel AS. Medscape Hospital Medicine. August 6, 2024, https://www.medscape.com/viewarticle/free-med-schoolalone-wont-boost-diversity-2024a1000eb3?form=fpf
2. The Moynihan Report. 1965. https://www.blackpast.org/ african-american-history/moynihan-report-1965/
3. Nietzel MT. Forbes. August 7, 2024; https://www.forbes. com/sites/michaeltnietzel/2024/08/07/women-continue-to-outpace-men-in-college-enrollment-and-graduation/ Meckler L. The Washington Post, January 2022. https:// www.washingtonpost.com/education/2022/01/30/public-education-crisis-enrollment-violence/
More on the politization of medicine: boycotting practitioners for their alleged political believes?
Hard to believe, - but out all medical specialty felds, it had to be a therapist who publicly promoted the boycotng of colleagues for their personal politcal believes. Her name is Heba Ibarahim-Joudeh, a Professional Counselor, with Illinois license number 2024-02634, who announced to the Facebook group “Chicago Ant-Racist Therapists” that she “put together a list of therapists and/or practces with Zi-
onist afliatons that we should avoid referring clients to.” And as psychiatrist, Sally Satel, MD, furthermore, reported in The Free Press, 1 she then added to the message, “please feel free to contribute additonal names, as I’m certain there are more out there.”
The list of 26 therapists had only one common denominator: they all were Jewish! And how do you think the response from Ant-Racist Therapists was upon receiving this message? They, of course, responded enthusiastcally to the idea and – though, of course, not very becoming for a group of professionals with that name. They, indeed, also added further names and practces to the list, - some were surprisingly non-Jewish colleagues – though not for trying to project at least a degree of objectvity - but because they had Jewish-sounding names.

Satel sees this behavior as typical for a troubling trend within the world of psychotherapy, where more and more clinicians consider psychotherapy to primarily be a politcal rather than clinical enterprise. Doesn’t that sound surprisingly similar to what prominent journalists have called replacing the century-old obligaton of journalists’ to “neutral objectvity” with “moral clarity,”2 which within just a few years has succeeded in largely ruining the credibility of most news media.
Is this the beginning of choosing your doctor based on her/ his politcal believes? Never underestmate our ability to make stupid decisions!
REFERENCES
1. Satel S. American Enterprise Institute. The Free Press, August 13, 2024. https://www.aei.org/op-eds/inside-the-campaign-to-blacklist-zionist-therapists/
1. Welch M. Reason. June 24, 2020. https://reason. com/2020/06/24/journalists-abandoning-objectivity-for-moral-clarity-really-just-want-to-call-people-immoral/
Sally Satel, MD, is a practcing psychiatrist in Washington, D.C. a lecturer at Yale University School of Medicine in CT, and a resident scholar at the American Enterprise Insttute.

ANNOUNCEMENT
THE ANNUAL pre-Christmas FOUNDATION FOR REPRODUCTIVE MEDICINE CONFERENCE (FRMC) in New York City, December 6-8, 2024* on Newest Developments in Translational Reproductive Biology, Clinical Reproductive Endocrinology, and Infertility
*Te most beautiful time of the year in NYC

CONFERENCE VENUE: CONVENE Conference Center
Accessible at 237 Park Avenue, east of the Helmsley Building on Park Avenue on 46th Street or at
466 Lexington Avenue, between 45thand 46th Street, - up the escalator. It is near subway stations 4,5,6,7, and S. If coming by subway into Grand Central Station, use exit Northeast.
TARGET AUDIENCES
Medical students – free attendance
Residents, fellows, postdocs – discounted attendance
Obstetricians & Gynecologists
Endocrinologists & Infertility Specialists
Reproductive Biologists - discounted attendance
Embryologists - discounted attendance
Geneticists
Ethicists
Fertility nurses and nurse practitioners - discounted attendance
Sonographers - discounted attendance
Science journalists – free attendance
Investors & administrators in the feld
Industry interested in the feld
Lawyers interested in the feld
CONFERENCE SPONSORS
A Not-For-Proft Research Foundation www.foundationforreprodmed.com
The Center for Human Reproduction (CHR) An International Fertility and Research Center www.centerforhumanreprod.com
STATEMENT OF NEED
(i) To demonstrate to clinicians in the feld what ongoing bench research can contribute to better understanding of physiological processes relevant to clinical practice.
(ii) To demonstrate to basic scientists in the feld what the basic knowledge needs of clinicians are.
(iii)To learn to “think diferently” by critically assessing current clinical practice patterns in attempts to improve clinical outcomes PROGRAM OBJECTIVES
• To present most up-to-date basic science as well as clinical knowledge to lead to a better understanding between basic scientists and clinicians in reproductive medicine.
• To demonstrate how improved cooperation between basic science and clinical medicine can improve patient care.
• To outline an alternative thinking pattern that allows for the critical evaluation of clinical practice patterns in their respective efectiveness.
CME CREDITS
Te conference will award up to 20 CME credits.
Trebron Management, Inc. New York, N.Y. ComtecMED Medical Congresses, Israel The Foundation for Reproductive Medicine (FRM)
CONFERENCE HOTELS – all within 2 blocks of




A Book Wort Reading
Book Review: What Are Children For? On Ambivalence and Choice by Anastasia Berg and Rachel Wiseman (St. Martin’s Press, 2024).
By H. Duncan, M.F.A.,
who is a writer and copy editor of The VOICE.



2024 has been marked by a predominant mood of anxiety surrounding childlessness, from headlines sounding the alarm about declining birth rates—which reached a record low in the United States last year—to the seemingly unending fallout from Republican VicePresidential candidate J.D. Vance’s comments decrying “childless cat ladies.”
Seen only in the big-picture framework of economics and politics, questions of family-building tend to obscure the swirl of motivations that go into this deeply personal decision a woman must make, a choice that touches on the most profound philosophical questions
about what gives life its meaning.
Why are women delaying or forgoing motherhood? How should a person struggling with whether to start a family begin to approach this decision? Can one separate so-called “external factors”—whether one has enough money or the right partner—from the murkier trappings of one’s own wants and fears?
Enter What Are Children For? On Ambivalence and Choice, an engaging and often surprising new work of nonfction by Anastasia Berg and Rachel Wiseman. Both authors are editors of The Point, a magazine of
What Are Children For? On Ambivalence and Choice by Anastasia Berg and Rachel Wiseman (St. Martn’s Press, 2024).
philosophical writing, and Berg teaches philosophy at Hebrew University of Jerusalem.
What Are Children For? seeks to “penetrate to the core the contemporary mood of ambivalence” toward parenthood. The tools are wide-ranging: survey data; an exploration of the roots and evolution of feminist discourse on motherhood; thoughtful probes into the role of attitudes toward dating, love, and personal fulfllment. The book quotes from sources as diverse as Angela Davis, Philip Larkin, Shulamith Firestone, and David Benatar. It is as much an explanation of “how we got here” as it is a guide for women suffering from “analysis paralysis.”
The authors also cast a refreshingly skeptical eye at common media narratives surrounding millennial and Gen Z women shirking motherhood. Regarding prophylactic or “social” egg freezing, the authors cite research showing many women choose egg-freezing not primarily as a way to delay childbearing for the purpose of career advancement, as it is usually framed, but more often, to buy more time to fnd the ideal romantic partner with whom to raise kids (a point noted by CHR research fellow Dr. Sònia Gayete Lafuente in her piece on egg-freezing in the September VOICE).
In another example, they investigate the notion that childless women face external pressure to become mothers, as exemplifed by the trope of the mother nagging: ‘When are you going to give me grandkids?’ In fact, most of those surveyed reported facing no or little pressure from people in their lives and in the cases of some career felds, like academia, felt pressure not to have kids. (It is worth noting that most of the women Berg and Wiseman surveyed are more highly educated than the general population.)
The authors also dig deeper into the string of media headlines that cite the threat of climate change as a reason people aren’t having kids. Beyond the chatter, fear of ecological instability, they found, is rarely the primary or decisive factor in forgoing parenthood. Are people really concerned with the ethics of bringing children into a burning world, or can it be that it’s easier or more socially acceptable to couch one’s hesitancy in terms of environmental concern
than to acknowledge one’s ambivalence?
A particularly interesting chapter examines the trend of so-called “motherhood ambivalence literature,” the spate of bestselling novels and memoirs of the past few years in which female narrators pore over the decision of whether to have kids in an “endless recursive” cycle. Often in these works, the question of motherhood is faced in “solitude and bewilderment.” Yet Berg and Wiseman point out that in a relationship, it is not only a woman’s decision to contend with; it can be unhelpful for men to simply remove themselves from the deliberations until their female partner makes her choice.
What Are Children For? is an illuminating read for anyone grappling with the question of whether to become a parent. It acknowledges the fraught reality of ambivalence while affrming that there are paths through it. And it states the urgency of fnding that path; in Berg’s words—and as fertility doctors know all too well—“A decision delayed long enough makes itself.”
ADVERTISEMENT



A Piece of My Mind
An Example for How a Whole Specialty Can Lose Hard-to-Recover Credibility:
Reproductive Immunology as an Example for Genetics and Other Expertise
Norbert Gleicher, MD
Is the Medical Director and Chief Scientist of The CHR
BRIEFING: Reproductve immunology evolved as a distnct subspecialty area within reproductve medicine in the late 20th century and quickly was recognized as an area of special expertse with potental for signifcantly contributng to improvements in various areas of reproductve medicine. The good will extended by reproductve medicine to this new medical specialty was, however, quickly wasted by some leading reproductve immunology “experts” who overpromised and under-delivered and, in additon, by becoming vendors of diagnostc tests – ofen despite obvious economic conficts – aggressively promoted them. As a consequence, reproductve immunology to this day is (erroneously) widely dismissed as irrelevant for reproductve medicine. We here make the point that the premature and unvalidated introducton into fertlity practce and commercializaton of several genetc and other tests promoted by “experts” in highly specialized areas of reproductve medicine most practcing physicians in the feld are not familiar with, now creates the same risk for other subspecialty areas, especially when it comes to genetc testng.
One reason why reproductve immunology to this day has litle credibility in the fertlity feld, is a history of false scientfc claims, poor-quality studies, and commercial exploitaton, especially in the late 1980s and early 1990s. One of the more telling examples was the marketng of antphospholipid antbody testng by some prominent reproductve immunology “experts” as a panacea for almost everything in reproductve medicine, in those days associated with the relatvely new
sub-specialty of reproductve immunology.1 Aside from autoimmune diseases, this included implantaton failure in IVF, pregnancy loss, endometriosis, pregnancy complicatons like preeclampsia, etc.
It in retrospect was also the beginning of the recogniton that “experts” in a small subspecialty area, otherwise not well understood by most colleagues in the larger feld of reproductve medicine, had the opportunity to establish a successful and prosperous clinical practce in their medical feld of allegedly special expertse. And establishing practce, among other determinatons, meant that they were given the opportunity to defne allegedly useful tests in managing clinical practce. Moreover, “experts” also quickly discovered that by being the authorites who establishing testng paradigms, they had a unique opportunity to also become the source for such testng.
Staying with the above-noted example, several prominent reproductve immunologists became in the U.S. the primary purveyors of antphospholipid antbody testng and other immunological tests and, with it, of course created a very obvious economic confict of interest. Ever since, these kinds of conficts – these days even to much larger degrees – spread with considerable vengeance into several other subspecialty areas of reproductve medicine (more on that below).
In reproductve immunology this mana from heaven, however, did not last for very long because exaggeratons and misrepresentatons by the newly established testng industry within a relatvely short tme period became quite obvious, resultng in a backlash to the other extreme, with many reproductve endocrinologists (REs) declaring all reproductve immunology to be irrelevant for reproductve medicine.2 The failure of this new testng industry to live up to exaggerated promises was also considered reason enough to almost completely exclude reproductve immunology from the RE feld.
As a consequence, clinicians and serious investgators really never got together to utlize – considering the enormous progress immunology research had made – what the big immunological questons are that reproductve medicine must tackle. Reproductve immunology – which really should be an integral part of reproductve endocrinology and infertlity (REI), therefore, at best has remained only a peripheral entty within REI. That to some degree it stll does not deserve much beter, is from tme to tme reafrmed by ofen poor-quality papers in the literature, with a very recent one actually becoming the “inspiraton” for this opinion artcle. The artcle referred to is a paper recently published in Early Human Development 3 generally considered a beter journal than its impact factor would suggest.
How this paper made it through the journal’s peer review, therefore, is unclear. Its three authors claim as a fact that human pregnancies established with “unrelated” embryos (i.e., egg donaton and use of gestatonal carriers) are “riskier” than normal semi-allogeneic pregnancies, where the birthmother contributes the egg. Where the evidence for such a claim is coming from is unclear because valid evidence for such a claim simply does not exist. Nor do increasing percentages of aneuploidy necessarily support more pregnancy complicatons on a theoretcal level, since at least one hypothesis of allogeneic tolerance argues exactly the opposite, namely that poor allogeneity of the male reduces reproductve ftness of a couple and may lead to increased miscarriage risks.4
But neither of these argument prevented the authors – all three biologists without clinical training – from building their own biological hypothesis around an alleged increased risk of a 100% allogeneic pregnancy in comparison to an only 50% natural allogeneic pregnancy.
It is exactly this kind of unsupported grandiosness in pronouncements that has led reproductve immunology into medical exile. The artcle, therefore, is here, presented to demonstrate how things should not be done: All three authors are reputable biologists (not physicians) at reputable insttutons; but, as their paper demonstrates, really project litle understanding of clinical medicine; yet – without any hesitaton – the paper even ofers in its conclusions “several medical proposals.”
And we quote: “First, egg donors and surrogates should be informed of the increased health risks they would face.” In consideraton of this alleged (and in our opinion really unproven increased risk), these young, fertle women should not be compared to older, infertle women undergoing IVF (as if anybody would do that); the proper comparison group is other young, fertle women. Second, contrary to some medical advice, perhaps genetcally related egg-donors and surrogates should be preferred, all else equal (the lack of any reality in this sentence should be obvious to everybody). An
immunological matching scheme, like what is used for organ transplants, could improve surrogate pregnancy outcomes (undoubtedly one of the most absurd statements that ever made it through peer-review). Third, more research is needed on microchimerism, sperm exposure, and long-term impact of allogeneic pregnancies on maternal and child health.”
The absurdity of this publicaton, however, does not only refect on the medical journal that published the paper. It unfortunately also – once again – refects on the feld of reproductve immunology, projectng once more upon reproductve immunology the impression of complete unseriousness. One also wonders who the reproductve immunologists might have been who reviewed this paper? Or was this paper only reviewed by “alibi reviewers”? One also wonders how litle appreciaton for reproductve immunology there really is in reproductve medicine for a journal, like Early Human Reproducton, to publish such a paper.
Which brings us back to the important subject of “experts” in a small niche of a much larger feld of medicine. As the COVID pandemic so well demonstrated, “experts” in our current natonal medical enterprise appear to represent one of the weakest points. Above discussed experience of reproductve immunology within reproductve medicine, does not stand on its own and/or alone. To the contrary, reproductve immunology was “revealed” for what it really was with relatve ease and in relatvely short tme. Contrast this, for example, with preimplantaton genetc testng for aneuploid (PGT-A) of embryos in associaton with in vitro fertlizaton (IVF), frst introduced to IVF practce in the late 1990s and since then steadily growing in popularity. It is by now utlized worldwide (in the U.S. in over half of all IVF cycles) despite the fact that in over 25 years nobody was ever able to demonstrate clinical efcacy for the test, as fnally only very recently also for the frst tme acknowledged in a combined statement by the American Society for Reproductve Medicine (ASRM) and the Society for Assisted Reproductve Technology (SART).5
Or take the concept of endometrial receptvity testng, which, like PGT-A, made all kinds of promises about how it would improve IVF outcomes without fulflling them and–also like PGT-A–gave rise to multmillion dollar testng companies that ofered these tests. HEFA, the U.K.’s Human Fertlisaton & Embryology Authority rates the test for most patents as red “because the fndings from moderate/high quality evidence shows that this add-on (to IVF) may (actually) reduce (IVF) treatment efects.”
Like “experts” in reproductve immunology misled the reproductve medicine community and the public about the efectveness of immunological tests and, in doing so, ruined reproductve immunology’s credibility for decades to come, so must genetcs “experts” be held responsible for the huge number of human embryos not used and/or the huge numbers of embryos with excellent pregnancy potental that were simply discarded. Unnecessary prolongaton of infertlity, considerable additonal costs, and unnecessary use of third-party donor eggs were the consequences for large numbers of infertle patents; all because of poorly validated tests introduced into fertlity practce at recommendaton of genetcs “experts.”
Excessive reliance on “experts” has been for centuries critcized by philosophers, historians, and writers in the humanites with the argument that “experts” are, of course, essental in receiving advice; they, however, should not allowed to be the decision makers and – most certainly – should not be allowed to beneft fnancially from advice they provide. The incentve to adjust advice according to such fnancial incentves, otherwise, would be too large.
REFERENCES
1. Hatasaka et al., J Reprod Immunol 1997;34(2):137-153
2. Hill JA, Scot RT. Fertl Steril 2000;74(3):439-442
3. McCoy et al., Early Hum Development 2024;196:106072
4. Oikonomou et al., Cureus 2023;13(3):e36584
5. Practce Commitees of the ASRM and SART 2024; . Fertl Steril 2024; May 18: S0015-0282(24)00241-3. doi: 10.1016/j.fert stert.2024.04.013. Online ahead of print.
6. HEFA. htps://www.hfea.gov.uk/treatments/treatment-add-ons/endometrial-receptvity-testng/#:~:text=Endometrial%20receptvity%20 testng%20involves%20taking,receptve%20to%20an%20embryo%20implantng. Next review date: 10/9/25
Te CHR’s favorite NYC restaurants
All listed restaurants are in Manhattan unless otherwise noted. Like all opinions about restaurants, ours are subjective and are to be understood as such. If you visit one of them, let us know whether you agree with our ratings. We value your feedback.
SYMBOLS WE USE IN OUR RATINGS
PRICES
FOOD QUALITY
SPECIAL COMMENTS
$ Inexpensive - Not worth the trip + Overall favorite of the CHR
$$ Moderately expensive
$$$ Expensive
$$$$. Special event expensive
• Good v Special vibe
•• Very good M Michelin starred
••• Excellent V Vegetarian/vegan dishes on •••• Uniquely delicious the menu
ADDRESS TELEPHONE
COMMENTS
AUSTRIAN
Koloman +/•••/$$/v 16 W 29th Street (212) 790-8970 V; Excellent desserts
Wallsé +/•••/$$/v/* 344 W 11th (212) 352-2300 V; Excellent desserts
CHINESE
Hwa Yuan Szechuan +/•••/$$/v 42 East Broadway (212) 966-6002 V; Authentic Szechuan Mr. Chow Downtown +/••/$$$/v 121 Hudson St., Tribeca (212) 965 9500 V Uptown 324E, 57th Street (212) 751 9030 V
CONTINENTAL
425 •••/$$$/v 425 Park Avenue (212) 751-6921 V; Gorgeous restaurant FRENCH
Le Gratin ••/$$ 5 Beekman St. (212) 597-9020 V; Try the gratin potatoes
Le Charlot +/•• /SS 19 E 69th St. (212) 794-6419 V; Best steak au poivre & Tai mussels; great desserts
Le Bernadine +/••••/$$$$/ MMM 155 W 51st (212) 554-1119 V; Mostly seafood. Likely the best NYC restaurant
ITALIAN
Cipriani Downtown +/••/$$/v 376 West Broadway (212) 343 0999 Great food, beautiful people & Uptown 781 5th Avenue (212) 753-5566 Great food and high society
Elio’s +/•••/$$/v 1621 2nd Ave. (212) 772-2242 Best Italian home cooking and where everybody meets
Principe ••/$$/v 50 West Broadway (212) 335-0509 V; mostly seafood but one of the best chicken dishes
Sistina •••/$$$ 24 E 81st St. (212) 861-7660 V; Amazing wine list FRENCH-ITALIAN
Café Carmellini •••/$$$$/v 250 Fifh Avenue (212) 231 9200 V; Gorgeous place, top service; sophisticated and adventurous food
JAPANESE
SUSHI
Sushi Ann +/••• /$$$$ 8 E 51st St. (212) 755-1780 V; Best quality fsh; make reservation at the bar
GENERAL
Sakagura +/•••/$$ 211 E 43rd St. (212) 953-7253 V; Amazing food; Best sake selection
Yakitori Torishin +/+++/$$$/M 362 West 53rd Street (212) 757-0108 Unique and amazing skewer restaurant
KOREAN
Jungsik •••/$$$$/ MM 2 Harrison St. (212) 219-0900 Where NYC’s Korean restaurant revolution was born …
Oiji Mi +/•••/$$/v / M 17 W. 19th St. (212) 256-1259 … and has continued
GREEK
Elias Corner (Queens) ••/$ 24-02 31st St. (718) 932-1510 Mostly seafood HAMBURGERS
Jackson Hole Burgers (the “original”) +/••/$ 232 E 64th St. (212) 371-7187 Not a place for vegetarians
MIDDLE EASTERN-ISRAELI
Dagon ••/$$ 2454 Broadway (212) 873 2466 Best hummus in NYC NEW YORK JEWISH DELI
P. J. Bernstein’s Deli •/$ 1215 3rd Avenue (212) 879-0914 All the great classics; pastrami, chicken soup PERUVIwAN
Mission Ceviche •••/$$ 1400 2nd Avenue (212) 650-0014 If you like Peruvian –the best
PIZZA
San Matteo Pizzeria e Cuccina ••/$ 1559 2nd Avenue (212) 861-2434 True Napoli POLISH
Karczma (Brooklyn) +/•/$ 136 Greenpoint Avenue (718) 349-1744 Great authentic Polish food – and dirt-cheap ROMANIAN-JEWISH
Sammy’s Roumanian Steak House** $$ 112 Stanton St. (212) 673 0330 Authentic JewishRomanian Steak House, with entertainment
UKRAINIAN/RUSSIAN
Caviar Russe +/••••/$$$$/ M 538 Madison Avenue (212) 980-5908 V; Most underrated restaurant in NYC
Russian Samovar •/$/v 256 West 56th St. (212) 757 0168 Great Russian/ Ukrainian food and music
Any suggestions and/or comments, please write to social@thechr.com.



N
W S F
O M N Y C ’
R E S T A U R A N T S C E N E

More Michelin-starred restaurants for NYC?
S o i t s e e m s ! T h e c o m p a n y o n S e p t e m b e r 1 1 a n n o u n c e d
t h a t i t i s c o n s i d e r i n g 1 2 a d d i t i o n a l r e s t a u r a n t s f o r i t s
2 0 2 4 a w a r d s , a f t e r i n A p r i l a l r e a d y a n n o u n c i n g a l i s t o f
p o t e n t i a l l y n e w a w a r d e e s . W e m u s t s a y , w e a r e n o t
i m p r e s s e d . T h e A p r i l l i s t i n c l u d e d B a n g k o k S u p p e r C l u b ,
w h i c h w e f o u n d s o d i s a p p o i n t i n g o n a s i n g l e v i s - i t t h a t
w e c a n c e l l e d a p l a n n e d s e c o n d v i s i t T h e s a m e a l s o
a p p l i e d t o v e r y w e l l - d e s i g n e d I l i s , a r e s t a u r a n t i n
G r e e n p o i n t , B r o o k l y n , b y D a n i s h c h e f , M a d s R e f s l u n d ,
c o - f o u n d e r o f C o p e n h a g e n ’ s f a m o u s N o m a r e s t a u r a n t ,
w h i c h w e , b a s e d o n a r e l a t i v e l y s m a l l m e n u a n d r e a l - l y
u n i n t e r e s t i n g f o o d , a l s o d i d n o t f i n d w o r t h a s e c o n d
v i s i t I n t h i s c a s e , o u r j u d g m e n t w a s a l s o s u p p o r t e d b y
o n l y a – w h a t w e w o u l d c o n s i d e r t o b e a v e r y p o l i t e a n d
g r a c i o u s – 2 - s t a r r e v
And then there is suddenly the not so new Le B. by Angie Mar on Michelin’s candidate list. Where has Michelin been for so long? This is a typical restaurant Michelin reviewers usually would like. It, indeed, was on our most favorite r e s t a u r a
be one of the best chefs in the city – if she wants to; but, unfortunately, it appears she does not always want to. In other words, the restaurant was uneven: On good days it was spectacular; on bad days it was still good, - but not really worth the considerable cost of every visit (it is quite expensive). This, as we noted after its removal from our most favorable restaurant list, was, however, not the problem. W e r e m o v e d
group, the wait staff blatantly overserved shared portions, wine bottles, and even mineral water. We simply felt abused and that is the last thing one wants to feel, even in a very good restaurant.
So, we are anxiously waiting for the final Michelin list for the year There are always interesting surprises, even though we often may not be in full agreement.

Flambéing at tableside at LeB
La Grenouille finally closed
One of NYC’s all-time classical great French restaurant –maybe, indeed, the city’s last – has finally closed its doors. I t h a s b e e n c o m i n g f o r s o m e t i m e , a n d n o t o n l y b e c a u s e of circulating rumors The restaurant had just lost its relevance. The place was still elegant, the food was still reasonably good; but it no longer offered a reason to go back. It was no longer a to-see or to-be-seen place (think Cipriani downtown), the food was mediocre, - neither gourmet nor bistro but somewhere undefinable in-between. Founded in 1962, it finally expired. May it rest in peace.
What is going on at three-Michelin-starred Per Se
Thomas Keller’s Per Se is closed – again After being closed over the summer for renovation, then supposedly reopened, only to close again on September 11, noting that it “continued to address unexpected kitchen maintenance for the safety and well-being of our team and guests.” That t h i s a p p e a r s t o b e a n o n l
scheduled permitted kitchen maintenance in August has taken slightly longer than anticipated to complete; the
into the main dining room as soon as possible The private dining room remained open ” Strange! Apparently the city turned off the restaurant’s gas line
Pete Wells left as the New York times’ food critic

Recent medical literature relevant to reproductive medicine
BRIEFING: The VOICE in this section offers commentaries on a broad survey of recent articles in the English literature which the CHR found of interest, even if, at times, not immediately applicable to daily clinical practice. Articles are mostly chosen for their transla- tional value to clinical medicine, often helping in determining where clinical practice will likely go
Though the New York Times food critic these days is no longer very important for the public and the city’s restaurant industry (several decades ago the NYT critique could make or break a restaurant), it is still one of the more important positions among food critics in the city and the competition to follow Wells – we are sure – is intense. Considering the dramatic changes the restaurant industry has undergone in recent years – especially since COVID - we would not be surprised if the newspaper would be looking for somebody who could report on the restaurant scene beyond just food criticism (think Steve Cuozzo of the New York Post)
Even though, we very clearly have quite a different palate from Pete Wells, we liked the professionalism in his criticisms. He very obviously “new his stuff.” New York will miss his voice.
Translational research is, since its founding in 1981, one of the CHR’s principal goals and has over the years produced some mile- stone discoveries and a good number of U.S. patents. Such research has also propelled the CHR into its current status as a worldwide center of last resort for infertile patients who have failed treatments elsewhere. This section of the VOICE demonstrates and makes public the process through which the CHR for decades has been following and interpreting the published literature, a process always at the very core of how research and clinical practice have evolved at the CHR.
Primarily directed at physicians and basic scientists, this section of the VOICE to our surprise has also attracted many of the CHR’s patients, from which we assume that it also has found a readership in the more general public. The VOICE, therefore, strives in its writing style to make this section also understandable and, therefore, accessible to a general lay audience not necessarily familiar with scientific lingo
Pete Wells, formed New York Times restaurant critic

O B E S I T Y & N U T R I T I O N N E W S
BRIEFING
In this still relatively new section of the VOICE, we are t r y i n g t o i n f o r m a b o u t t h e i m p o r t a n c e o f f o o d f o r g e n e r a l h e a l t h a n d r e p r o d u c t i o n , w i t h a l
lighter fare dispersed between pages. Food can have p o s i t i v e e f f e c t s , - a
condition in women and men closely associated with infertility and lowered success rates for fertility treatments. With the availability of ever more-effective GLP-1 drugs for the treatment of obesity, weight loss with this family of drugs has, therefore, assumed the
sense can also be understood as the first substantial new family of drugs the pharma industry has provided to the infertility field in decades.
Obesity and
Obesity has become a public health challenge in women and men. In women it is associated with reduced fertili- ty and infertility as well as with an increased miscarriage risk. In men it is also associated with decreased fertility and infertility. A recent study in JAMA Network Open now reported on the association between preconception BMI in both partners with time to pregnancy and/or miscarriage.1
c o m p a r e d w i t h w o m e n w i t h n o r m a l w e i g h t . M o r e o v e r ,
c o m p a r e d t o n o r m a l w e i g h t , u n d e r w e i g h t , o v e r w e i g h t ,
a n d o b e s i t y w e r e a s s o c i a t e d w i t h i n c r e a s e d o d d s o f
s u b f e r t i l i t y . I n m e n t h i s a p p l i e d o n l y t o o b e s i t y . I n
a d d i t i o n , w o m e n w i t h o v e r - w e i g h t a n d o b e s i t y a l s o
d e m o n s t r a t e d i n c r e a s e d m i s c a r - r i a g e r i s k i n c o m p a r i s o n
t o n o r m a l w e i g h t w o m e n .
All of this is, of course, nothing new It, however, reinforces the concept of weight loss as a fertility treatment, which we at the CHR have started emphasizing since GLP-1 receptor agonist drugs have come to market. Much more on all of that below REFERENCE
1 Boxem et al , JAMA Network Open 2024;36157
Does maternal
fish intake during pregnancy reduce autism risk in offspring?
Not necessarily a new suggestion, but this is what a recent study in the American Journal of Clinical Nutrition recently again reported.1 The study confirmed earlier reports that increased fish consumption during pregnancy appears associated with lower numbers of autism cases and a more modest reduction in autism-related traits. The reason was always assumed to be the omega-3 intake that comes from fish. While this study confirmed the association with fish consumption, it did not support an association with gamma-3 levels. The so-called SRS scores on the Social Responsibility Scale, however, did demonstrate a modest increase with better Omega-3 levels. The authors concluded that
always assumed to be the omega-3 intake that comes from fsh. While this study confrmed the associaton with fsh consumpton, it did not support an associaton with gamma-3 levels. The so-called SRS scores on the Social Responsibility Scale, however, did demonstrate a modest increase with beter Omega-3 levels. The authors concluded that fsh consumpton in pregnancy should be encouraged.
REFERENCE
1. Lyall et al., Am J Clin Nutriton 2024;120(3):5830592
GLP-1 receptor agonists –revolutionizing health care
2024 Lasker Awards 2024 go to GLP-1 receptor agonist researchers
One of “The Laskers” – after the Nobel Prize the most prestigious science awards and, often, foreshadowe recipients of a Nobel Prize, this year went to several scientists responsible for the still evolving health revolution induced by the new family of weight-loss drugs, called GLP-1 receptor agonists.
The Lasker-DeBakey Clinical Medical Research Award went this year to three recipients who made essential contribution to the development of these drugs: Joel Habener, MD, is an endocrinologist and Professor of Medicine at Harvard Medical School, who had a research interest in diabetes, - specifcally the hormone glucagon – hoping that discovery of its gene would allow shutting glucagon down, thereby reducing glucose levels. In the process he in an animal model discovered a protein that resembled glucagon, shortly thereafter by another researcher who had discovered the same protein in a diferent animal model given the name glucagon-like-peptide-1 (GLP-1).

the time at Massachusetts General Hospital in Boston and now a professor at Rockefeller University in NYC and they succeeded in producing the frst biologically active form of GLP-1. It, however, was clinically not usable because it had too short a lifespan before being metabolized. This is where Lotte Bjerre Knudsen, PhD, a scientist at the by now wellknown Danish pharma company, Novo Nordisk in Copenhagen came into the picture and solved the problem by attaching the new GLP-1 compound to a fatty acid which extended the time of its function, - and the rest is history.1 As in detail reviewed in last month’s VOICE, this new family of weight loss drugs not only started a revolution in treating obesity, but it is also becoming increasingly clear that they also exert benefcial efects on many other medical conditions. We suspect that the Nobel Prize cannot be far behind!
Deceptive promotion of GLP-1s
Repeated articles in The Wall Street Journal have called attention to what The Journal considers deceptive promotion of GLPs on platforms such as TikTok, YouTube, and Instagram.2 The newspaper now reports that a newly introduced bill in the Senate targets infuencers and telehealth companies for misleading promotions of weight loss and other drug promotions.2 If passed by congress, the bill would allow the FDA to fne individuals and companies up to $500,000 for posting false information inline about, for example, Ozempic and Wegovy, - still the bestsellers among GLP-1s.
Good news: GLP-1s help not only through weight loss – and other benefts
Evidence that GLP-1s have benefcial efects far beyond just weight loss are accumulating. Here are a few examples. They, for example, reduce alcohol consumption,3 incidence and relapse with cannabis use disorder,4 compulsive behavior,5 and seemingly even the drive to smoke (so-called tobacco use disorder).6 They benefcially afect heart failure,7,8 and appear to reduce dementia risk in adults.9 And, yes, they also appear to improve sleep apnea,10,11 all-cause mortality, etc.
Especially important for the fertility feld is increasingly well documented real-world evidence that GLP-1s – when used preconceptionally and in early pregnancy - do not increase pregnancy complications. Because data on inadvertent early pregnancy use are still sparse, a one-month wash-out period before fertility treatments, however, still appears appropriate.
Habner
with a biochemist, Svetlana Mojsov, PhD, at
Finally, two excellent reviews on use of GLP-1s for weight
From left to right: Joel Habener, MD, Svetlana Mojsof, and Lotte Bjerre Knudsen.
Credit Nature magazine.
worked
loss deserve attention,12,13 and a recent study confrmed that among GLP-1 receptor agonists on the market the eficiency to result in weight loss varies. As earlier data already suggested a direct comparison now confrmed that in adults with overweight and obesity tirzepatide (Mounjaro®, Zepbound®) resulted in significantly greater weight loss than semaglutide (Ozempic®, Wegovy®) And even more effective drugs are announced and already in trials.
REFERENCES
1. Lenharo M. Nature, September 19, 2024. https://www.nature. com/articles/d41586-024-03078-x
2. Loftus P, O’Brien SA. The Wal Street Hournal., September 12, 2024. https://www.wsj.com/health/healthcare/senators-target-influencers-telehealth-firms-for-misleading-weight-lossand-other-drug-promotion-81dbaf40
3. Quddos et al., Scientifc Reports 2023;:20998
4. Wang et al., Mol psych 2024;29:2587-2589
5. Arillotta et al., Brain Sci 2024;14(6):617
6. Wang et al., Ann Int Med 2024; 177(8): https://doi.org/10.7326/ M23-2718
7. Kosiborod et al., Lancet 2024;404:949-961
8. Hage C. Lancet 2024;404:909-911
9. Shin et al., BMJ 2024386:e079475
10. Blum D. The New York Times, Jue 21, 2024. https://www.nytimes.com/2024/06/21/well/sleep-apnea-weight-loss-drug. html
11. Malhotra et al., Contemp Clin Trials 2024;141:107516
12. Kusminski et al, Cell 2014;187:3829-3876
13. Gudzune KA, Kushner RF. JAMA 2024;332(7):571584
What is new regarding diets? Are Western diets killing us?
Two Austrian academic internists published an interesting paper in Nature Medicine in which they argue that Western diets basically kill us. More specifcally, they suggest that “westernization,” defned as industrial, cultural, and dietary trends, has paralleled the rise on non-communicable diseases around the world. After reviewing the literature in support of their thesis, they conclude that healthcare professionals and societies must react today to the detrimental efects of the Western diet to bring about sustainable change and improved outcomes in the future.
Not in any way desirous of defending Western diets, one is left wondering why - If it is only Western diets? Japanese diets, for example, have a much higher incidence of gastric cancers (attributed at least in part to more cases of gastritis),2 which they lose once they immigrate to the West. Chinese diets seem to overwhelm China’s health system, with
over a ffth of adults being overweight and experiencing large increases in hypertension, stroke, and adult-onset diabetes.3 In other words, it is not only the Western diet!
And how about intermittent fasting?
“Time-restricted eating,” as these diets are also called have become very popular. A new study in the Annals of Internal Medicine now, however, suggests that the possible efectiveness of these diets may have diferent causes than previously assumed: It may not be directly due to time-restricted eating but may be the consequence of smaller calory-intake when people restrict eating to only certain time periods.4
This in other words was a purely mechanistic study which tried to determine whether times when people ate their meals mattered, with no attempts to control for calories of those meals. Preliminary, one of the most interesting conclusion from these fndings, therefore, is that, while these kinds of diets do not lead to bigger weight loss than other diets, they appear to save individuals from having to count calories,5 - which may be one reason why these diets have become so popular. In the end, it always comes down to calory-intake (and, of course exercise, etc.). Though this kind of diet did not proof to be more efective than other diets, it, therefore, may be more patient friendly.
REFERENCES
1. Adolph TE, Tilg H. Nat Med 2024;30:2133-2147
2. Naylor et al., Gut 2006;55(11):1545-1552
3. Popkin BM. Healt Af. (Millwood). 2008;27(4):1064-1076
4. Lin et al., Ann Int Med 2024;176(7): https://doi.org/10.7326/ M23-0052
5. Varady KA, Oddo VM. Ann Intern Med 2024;177(5):672-673
The subject of excessive weight in infertility is gaining popularity
Overweight and obesity are suddenly hot issues in the infertility literature. Fertility and Sterility dedicated one of its monthly Views and Reviews series of articles to this issue under the heading, “A weighty issue,” discussing primarily the impact of GLP-1s on in vitro fertilization (IVF) cycle outcomes.1 the introductory article in this series reviewed well the impact of overweight and obesity on reproductive health and female metabolism, describing obesity as a “highly prevalent chronic disease that impacts over 40% of reproductive-age women.”2
A second interesting paper addressed weight bias in fertility medicine.3 That especially severely obese patients are discriminated against in fertility practice is dificult to deny. At the same time, it, however, is dificult to determine where good medical care ends and discrimination starts. For example, to suggest that morbidly obese women and men lose some weight before starting an IVF cycle, – especially now with availability of GLP-1s, allowing for relatively quick weight loss – would appear to represent excellent medical advice. But it is excellent advice, of course only if the patient is not too old or has very low functional ovarian reserve.
Such advice, of course, also depends in its appropriateness on how much weight a patient is expected to lose and in how long a time period. Older studies have suggested that relatively small weight loss will already improve fertility outcomes in IVF; but studies of what represents “best” weight loss at diferent starting points – which in the past were practically impossible to execute – with the quick weight loss of GLP-1s should now be possible and would appear urgently needed.
We also agree with the authors call to avoid body mass index restrictions for IVF treatments. In the end, it - of course always with patient safety at the forefront - always should be the patient who decides what treatment she/he receives.
And fnally, a fourth article in the series just ofered a somewhat superfcial and in some respects repetitive review of GLP-1s in association with infertility.4 Still a worthwhile read, - but clearly the least interesting article in the series.
The most interesting article on the subject in the same issue of Fertility and Sterility was, however, a systematic review and meta-analysis of preconception weight loss interventions on fertility in women.5 The study confrmed that pregnancy rates were higher in women who had undergone weight loss interventions before conception but also suggested no impact from such interventions on live
birth rates and miscarriages. These are, of course, contradictory fndings because –considering better pregnancy rates after prior weight loss, one would expect higher live birth rates unless, of course, miscarriage rates were increased (which they weren’t). We attribute these fndings to the very obvious shortcomings of systematic literature reviews which – frankly speaking –almost always include not only papers of poor quality but papers with greatly difering patient populations. What this study, therefore, reafirms for us is the urgent need for prospective studies using GLP-1s in obese patients before IVF cycle starts. We urgently need to know how much weight loss is enough to show outcome benefts in subsequent IVF cycles and – if possible – how much weight loss ofers the most improvements.
And to complicate this subject even a bit more, in the same issue of Fertility and Sterility investigators from several U.S. institutions also published a research letter trying to determine the efects of improved metabolic syndrome parameters (of course, including obesity) on live birth following intrauterine insemination (IUI) cycles.6 Somewhat surprisingly, women who improved their metabolic syndrome parameters through lifestyle interventions prior to their IUI cycles, did not demonstrate improvements in their fertility or live birth outcomes.
The authors, themselves, pointed outs several weaknesses in their study, which must be appreciated. This study, however, only further demonstrates the urgent need for properly conducted studies in this rapidly growing patient population which by 2030 is expected to represent half of all patients presenting to infertility clinics.
REFERENCES

1. Widra EA. Fertil Steril 2024;1222(2);193
2. Schon et al., Fertil Steril 2024;122(2):194—203
3. Boots et al., Fertil Steril 2024;122(2):204—210
4. Goldberg AS, Boots CE. Fertil Steril 2024;122(2):211-218
5. Caldwell et al., Fertil Steril 2024;122(2):326-340
6. Spitzer et al., Fertil Steril 2024’122(2)373-375
T h i s i s a n i n c r e a s i n g l y r e l e v a n t q u e s t i o n a n d , o f c o u r s e , i n p r i n c i p l e a l s o i n c l u d e s t h e t e s t i n g o f e m b r y o s
M o l l y M c D o n o u g h , A s s o c i a t e E d i t o r o f H a r v a r d M e d i c i n e , a t t e m p t e d t o a d d r e s s i t i n i n t e r v i e w i n g V a r d i t
R a v i t s k y , P h D , w h o i s n o t o n l y o n e o f t h e w o r l d ’ s p r e e m i n e n t r e p r o d u c t i v e e t h i c i s t s , b u t a l s o a l i t t l e o v e r a
y e a r a g o
A screening test during her pregnancy revealed that she had a 1-in-40 chance that her child could be born with Down’s syndrome. In an interview published in the Harvard Medicine Magazine, the two discussed this experience within the context of ever more prenatal genetic testing, especially socalled NIPT (non-invasive prenatal testing)
Also speaking from personal experience, McDonough felt “empowered” by having the information that NIPT offered. But once she started thinking about the implications at a societal scale, things started “to feel more problematic.”

Vardit Ravitsky, Ph.D
Ravitsky was very clear in her position when stating that, “it always must be about choices and knowledge and should not slip into the goal of eliminating certain types of conditions or even certain traits, syndromes, or types of people.” She went on, “what child to have should always remain a personal decision, free of societal pressures.”
Regarding NIPT, which basically very early in pregnancy uses the same technology to determine the fetuses’ DNA from maternal blood that is used in preimplantation genetic testing for aneuploidy (PGT-A) through a biopsy of the embryo, it, therefore, has similar unreliability built into its process as PGT-A. As Ravitsky noted, the context matters if the result of the test suggests that the pregnancy may be at high risk for a specific chromosomal abnormality, raising the question, what justifies more invasive follow-up testing with chorionic villous sampling (CVS) or amniocentesis?
d v o c a t e s a r g u e a g a i n s t i n c l u d i n g t h e m .
The ethics of “serious” genetic conditions in reproduction
Related to the above-described interview, Ravitsky was also the senior author of a recent paper in the European Journal of Human Genetics which discussed reproductive decision-making when it comes to “serious” genetic conditions (2). The article notes that the definition of a genetic condition as “serious” has defined importance because the term is often used to define and/or delineate permissibility and access to new reproductive genomic technologies. The paper, however, also pointed out that the term also lacks clarity, leading to inconsistent use, and then tried to address this gap
In the process, within the context of prenatal (and, though not mentioned, PGT-A) and reproductive genomic technologies they identifed three areas of ‘tension:” (i) Clinical care and population health; (ii) The impact of designating something as ‘serious;” and (iii) the perception of quality of life. The frst basically involves the issues discussed in above-described interview. Defning something as ‘serious,” is, of course, highly subjective and requires appropriate mindfulness and, regarding the issue of quality of life, it is important to note that the widely held notion that anybody afected by a “serious” genetic condition must have a poor quality of life has been proven incorrect.
The authors conclude that “the concept of seriousness in reproductive decision-making represents one of the most ethically complex uses of the term, as it infuences not only prospective parents’ reproductive decisions and family planning, but also has a direct infuence on societal decisions around who is born.”
Are we saving enough very premature babies?
A recent article by Liz Essley Whyte in the Wall Street Journal asked two questions: frst, why most hospitals do not try to save very premature babies, even though babies—starting already approximately at 21-22 weeks gestational age— now demonstrate increasingly better odds of survival; second, if hospitals cannot do this, why don’t they inform parents that other hospitals can (3)?
As we discerned after listening to an interview she gave to a radio station regarding her article, she obviously meant well in writing it. But as unfortunately is so often the case, medicine is more complicated than lay people are able to understand, unless they are really willing and able to dig deep into a subject and that was defnitely not the case here. Essley Whyte correctly noted that some neonatal intensive care units (NICUs), indeed, are getting better and better in achieving good survival of very immature infants starting at roughly 21-22 weeks. These units in the U.S. are so-called Level IV NICUs and are located in regional perinatal centers and are referral centers for so-called level III NICUs which are equipped to manage critically ill newborns who need intensive care but do not have the ability to provide level IV services (see table below).
*A Level IV NICU designation must meet all Level III capabilities, plus have the ability to care for infants born earlier than at 32 weeks of gestation and weighing less than 1,500 grams, provide life support, perform advanced imaging including MRI and echocardiography, as well as provide a full range of respiratory support
In short, like with all medical care, not all hospitals can provide all of it. If a higher level of care is required, the patient (in this case the baby) is transferred to an appropriate provider who ofers a higher level of care. The truth, therefore, is not, as the article appears to suggest, that “most hospitals don’t try,” but that most hospitals are not expected to try. The real question is also not whether the parents are told that other hospitals are ofering such highly specialized care but, whether hospitals are fulflling their obligation within perinatal networks to transfer the patient (in this case the baby) to an appropriate level NICU if the baby’s needs exceed the hospital’s capabilities. And hospital usually do this rather automatically in all medical specialties.
One diference from many other medical specialties, however, is that the occurrence of a very premature deliveries cannot always be predicted. In a majority of cases it, indeed, will occur unexpectedly, with the patient ending up in the closest and not necessarily best hospital for her situation.
And then there is another crucially important point the science reporter for the WSJ apparently did not understand. In her interview, when asked whether other countries did better than the U.S., she described Japan and Sweden as especially successful with survival rates in the high-50% range. But that means that in the high 40% range babies do not survive. She also noted that surviving babies may have mild learning disabilities, but many surviving babies may, indeed, end up with quite severe lifelong disabilities, and nobody can at 21-22 weeks with accuracy predict which baby will survive, or survive with only mild or with severe disabilities. The treatment ofered to parents of such very premature infants, therefore, often must be considered “experimental,” and, therefore, requires their specifc consent.
In short, another rather superfcial article critical of medical care, maybe meaning well, but essentially just trying to be provocative by falsely accusing hospitals of “not even trying” to save very immature babies.
The ethics of working with embryo models
We have in these pages on several prior occasions pointed out the increasing use in human embryo research of stem cellderived human embryo models. Nature magazine—we believe also rather superfcially and quite uncharacteristically for this highest-ranked science journal—described this efort recently as “uncharted ethical territory (4).” The author, Smriti Felicitas Mallapaty, an Asia reporter for Nature News, should know better because this subject has become highly “charted” territory, maybe even too charted, as some scientists working in the feld would say. Interestingly, Mallapatty correctly quoted in her article such a scientist making the point that, aside of the fact that so many diferent embryo models have by now been reported, none of them has led to “scientifc discoveries of any societal value.”
This is important because she also correctly pointed out that ethical issues would become relevant only once one of the embryo models could be viewed as becoming “equivalent” to a human embryo; and that appears still miles away. It appears to us, therefore, that the very visible drive by many toward regulation of embryo models, also demonstrated in publication of the recent “code of practice” for human embryo models grown from stem cells organized by Cambridge Reproduction (4) may turn out to be more hindrance than beneft for the feld but it, most defnitely, cannot any longer be described as “uncharted territory.” One can also only hope that Roger Sturmey, a professor of reproductive medicine in the UK, was correct in suggesting, also in Nature, that the above-noted code of practice aims to ensure ethical research, while demonstrating enough fexibility to allow for progress in a rapidly moving feld. As he also noted to establish unifed limits to all types of embryo models would seem impractical (5).
Two steps forward, one step backwards in improving research integrity
Science magazine recently reported that the Ofice of Research Integrity (yes, there is such a thing!) in its frst regulatory overhaul in 20 years is taking “modest steps toward greater transparency (6).” What this means according to the article is that the U.S. agency responsible for investigating research misconduct by federally funded biomedical scientists (where has this agency been for the last 20 years?) has actually dropped “controversial proposals” intended to speed up investigations and increase transparency.
The agency apparently “listened to concerns expressed by attorneys representing several major research institutions.” One wonders whether that is a good omen?
REFERENCES
1. McDonough M. Harvard Medicine Magazine 2024;htps://magazine.hms.harvard.edu/artcles.ethics-prenatal-genetc-testng
2. Kleiderman et al., Europ J Hum Genet 2024; htps://doi.org/10.1038/s41431-024-01681-0
3. Essley Whyte L. Wall Street Journal. August 7, 2024. htps://www.wsj.com/health/healthcare/premature-babies-hospitals-pregnancyfa1f091f
4. Mallapaty S. Nature 2024; 633:269-271
5. Cambridge Reproducton July 2024. htps://www.repro.cam.ac.uk/scbemcode/governance-stem-cell-based-embryo-models-g-scbemproject
6. Sturmey R. Nature 2024;632:639
7. Mervis J. Science 2024;385(6715):1263
GENERAL INFERTILITY
Surprising risks with gestational carrier pregnancies: a game changer?
Despite rapidly increasing costs, the use of gestational carriers (GCs) – by some also erroneously called “surrogates” (a surrogate also contributes her own egg) –is steadily gaining in popularity and, indeed, has become its own “industry,” with new agencies popping up almost daily. The underlying assumption for most GC cycles is that the genetic mother because of medical reasons cannot or should not carry a pregnancy and, therefore, chooses a GC to carry a pregnancy in her place. A second and rapidly increasing indication for the utilization of GCs is in ofering fatherhood to single men and/or male same-sex couples.
Especially in more recent years, the utilization of GCs has, however, expanded beyond just medical and biological indications. Increasingly – and often even widely publicized by celebrities – the indications are social, and we have also noticed an uptick in GC utilization among female business executives.
Whatever the indication for the use of a GC may be, an underlying assumption in choosing a GC, of course, will always be that a GC is fertile (to ofer the best chance of pregnancy with transfer of embryos) and healthy (to ofer the best chance for a normal pregnancy outcome). GCs, therefore, must be very carefully selected and not only have a clean past medical history and family history but, ideally, should have given birth before, should neither be too young or too old, and be socially responsible individuals.
Assuming a proper GC selection process, one should therefore also be able to expect that GCs not only should conceive quickly but almost universally should also experience uncomplicated pregnancies. But is this really true? And if not, why not?
Interestingly, this had never before been systematically investigated. A very recent paper by Canadian colleagues on the subject appeared, out of all places, in the Annals of Internal Medicine (1). And this paper likely made it into this prestigious general medical journal because it surprised! From among all eligible singleton births the Canadian colleagues investigated, 846,124 (97.6%) occurred through unassisted conception, 16,087 (1.8%) through IVF, and only 806 (0.1%) using a GC. The risk for severe maternal
morbidity was 2.3% with unassisted conception, 4.3% with IVF, and 7.8% in GC cycles. Weighted relative risks generated through modifed Poisson regression models were 3.30 (95% CI, 2.59 to 4.20) comparing GC cycles with unassisted conception and 1.86 (CI, 1.36 to 2.55) comparing GC cycles with IVF. Respective risks for severe neonatal morbidity were 5.9%, 8.9%, and 6.6%, generating weighted relative risks of 1.20 (CI, 0.92 to 1.55) for GC pregnancies versus unassisted conception and 0.81 (CI, 0.61 to 1.08) for GC pregnancies versus IVF. GCs also demonstrated more hypertensive disorders, postpartum hemorrhages, and preterm births at less than 37 weeks in comparison to both comparison groups. Though GCs demonstrated more preterm births, the evidence of severe neonatal morbidity was less than the evidence for severe GC morbidity and adverse pregnancy outcomes.
The authors concluded that potential mechanisms for higher maternal morbidity among GCs require elucidation and that GC cycles require development of “special care plans.”
They are to be congratulated on having published a very important study which will likely have a great impact on who uses GCs and how GCs are selected. Women who for medical reasons have no choice and men who need a woman to carry their child, of course, have also no choice. Both groups will, therefore, continue using GCs. But we can see social indications for GC utilization somewhat declining. And while the authors, of course, are correct in that underlying causes for poorer outcome of GC cycles should be further investigated, we fnd this argument a little bit too correct politically.
There, indeed, is no big mystery hiding behind the fndings pointed out by the paper. In principle, we know of two reasons. One is poor GC selection, a subject we will return to, and the other is the GC’s immune system. And here is why: When a woman spontaneously conceives, the pregnancy is a so-called 50% allograft. This means that half of the genetic background of the pregnancy is maternal, and the other half is paternal and, therefore, allogeneic. In a GC pregnancy the situation difers: For the GC, the pregnancy is 100% allogeneic because the GC has zero genetic contribution to the pregnancy. And 100% allogeneic pregnancies (other examples are pregnancies established with donor eggs and
the father’s semen or with donor eggs and donor sperm) are well known to experience increased pregnancy complications for the person carrying the pregnancy and the ofspring of such pregnancies, as recent paper well reviewed (2).
One, of course, can also not preclude that women who for medical reasons may need a GC may be producing “poorer” eggs than most other women, but women undergoing IVF should have represented an appropriate control for such a possibility in the recent paper. Moreover, if egg quality was the reason, the diference, likely, would have been primarily seen in neonatal morbidity and not GC morbidity, as the study suggested.
In a sense, this paper, however, did not surprise. Especially since COVID, the quality of GCs appears to have signifcantly declined. The CHR therefore recommends to all patients that they allow for an interview of their GC with a CHR physician before making any downpayments to an agency. Though we noticed a rise even before COVID, rejecting GC candidates was then a relatively rare event; but after COVID, rejections have almost become the norm. For example, very
SOURCE: Business Insider. https://www.businessinsider.com/ photographers-stunning-portrayal-of-surrogacy-went-viral-hereswhy-2023-10
One commentator on Facebook said the silhouette was a “photographic representation of the inherent beauty of the human spirit.” Courtesy of Melissa Wilson
recently we discovered that a proposed GC was a diabetic.
With patients in a large majority of cases fnding their GCs through GC agencies, one must hold the GC industry at least partially responsible. Young, fertile, healthy, and socially responsible GCs should, themselves, have lower than average complications in a pregnancy and should have lower—not higher—complication rates in pregnancies than unselected control populations. Though as noted above, carrying a 100% allogeneic pregnancy undoubtedly increases risks to GC and ofspring, the observed rate in increase still appears excessive and, therefore, very likely also includes a GC selection contribution.
Does this mean—as the authors suggested—that special care plans must be developed for GC cycles?
To a degree probably yes, but one plan that fts all, of course, makes little sense, considering what all can be wrong with a GC. What defnitely has to change, however, are four aspects of current GC practice: (i) As already noted, GC selection must be tightened; (ii) The informed consent given to patients using GCs must include the new recognition that GC cycles do not necessarily produce

low-risk pregnancies; (iii) GCs must be informed that GC pregnancies likely carry higher risk than the pregnancies they already experienced with use of their own eggs; and (iv) obstetricians must also be made aware of the fact that GC pregnancies must be expected to be more complicated than prior pregnancies of the GC with her own eggs.
And, yes, the rapidly growing GC industry must acknowledge all of these new observations and must recognize that growing demand for GCs cannot be satisfed by lowering the criteria for GC selection. To the contrary, with growing demand, the responsibility of GC agencies in selecting only the best qualifed GCs actually increases. Their eforts at GC selection, therefore, must be tightened.
REFERENCES
1. Velez et al., Ann Intern Med 2024; doi: 10.7326/M240417. Online ahead of print.
2. McCoy et al., Early Hum Development 2024;196:106072
Preventing chemotherapy-induced ovarian damage
The literature has suggested various modalites to minimize or even completely prevent chemotherapy-induced ovarian damage. Now investgators from the University of Chicago reported in a mouse model that pretreatment of ovaries with mesenchymal stem cell exosomes prevents chemotherapy-induced ovarian damage (1).
The idea for this study came from the observaton that mesenchymal stem cells and exosomes derived from them may be able to restore ovarian functon in preclinical models of primary ovarian insufciency (POI) by restoring damaged cells and inhibitng apoptosis. Whether these observatons were, however, also applicable to preventng ovarian damage was unknown. The authors concluded that using exosomes from mesenchymal stem cells could represent a simple new treatment of ovaries to prevent chemotherapy damage.
REFERENCE
1. Park, eta., Am J Obstet Gynecol2024;231:111.e1-e18
Some basic news on PCOS
It is widely believed that ca. 20% of all women sufer from one form or the other form of PCOS. Despite this very obvious importance, progress in our understanding of PCOS has been painfully slow. Every piece of new scientfc informaton that can contribute to a beter understanding,
therefore, is valuable. Britsh and Australian investgators now published a preprint in eLife which may do this (1). As it is only a “reviewed preprint” without revisions, the data should be consumed with cauton, but we are notng the paper here because of the potental importance of reported fndings. The study also involved mouse models and “mice are not men” (in this case women).
It is also widely believed that in PCOS the so-called arcuate kisspeptn (ARNKISS) neurons making up the GnRH pulse generator are dysfunctonal. Using highly sophistcated methods and technologies, the authors in this paper in two diferent mouse models atempted to defne the generator’s behavior. What they discovered is a complex phenotype demonstratng various defcits at multple levels of the hypothalamic-pituitary axis. In other words, PCOS is a highly variable conditon and one, indeed, has to start asking whether it isn’t tme to no longer consider it one conditon.
REFERENCE
1. Zhou et al., htps:/doi.org/10.7554/eLife.97179.1
Is cancer increased in women with primary ovarian insuffciency (POI)?
Both POI and cancer have been associated with DNA damage/repair gene variants. In a populaton-based casecontrol study investgators from the University of Utah now report that POI and certain reproductve cancers share common genetc risk. The cancers involved were breast cancer and, to a lesser degree, ovarian cancer. Relatves were associated with colon and prostate cancers. The authors concluded that the common risk between POI and primarily reproductve cancers may have relevance to postmenopausal hormone replacement therapy.
REFERENCE
1. Allen-Brady et al., J Clin Endocrinol Metab 2024; 12:dgae480. doi: 10.1210/clinem/dgae480. Online ahead of print.
Does noise and air pollution affect fertility?
These were the questons Danish investgators recently explored in the Britsh Medical journal (BMJ) and yes, they found evidence that the risk of infertlity appears associated with long-term exposure to trafc noise as well as air polluton (1). Specifcally, they reported the following: (i) Partculate air polluton was associated with
an increased risk of infertlity in men. (ii) Trafc noise was associated with a higher risk of infertlity in women above age 35 and, likely, men above age 37. If confrmed, it of course raises the queston, what could be done about it?
REFERENCE
1. Sørensen et al., BMJ 2024;386:e080664
GnRH agonist vs. antagonist in ovarian stimulation
Like most U.S. fertility centers—approximately 25 years ago after the first GnRH antagonist was approved for use in infertility—the CHR, in those days still in Chicago, succumbed to the manufacturer’s marketing efforts and started using the antagonist in place of the GnRH agonist the center had ben using for years. The results were remarkably disappointing, as pregnancy rates clearly declined. Because the CHR in those days served a very large and unselected patient population performing roughly 2,000 IVF cycles a year, we felt the results were very credible and, in contrast to most other IVF clinics, which to this date prefer the conveniences of GnRH antagonists over agonists, basically stopped using them except in very rare exceptional situation. And once the CHR fully switched to NYC and increasingly started concentrating on poorer prognosis patients rather than the typical patient population of most fertility clinics, using antagonists—obviously having a suppressive effect on ovaries—made even less sense.
Now, an international consortium of investigators published an important study in Human Reproduction , basically fully reaffirming the CHR’s conclusions over 25 years ago (sometimes it may take a little too long; but, ultimately, in medicine the truth always prevails). 1 Administering in a prospective, randomized multicenter trial of an obviously unselected patient population individualized follitropin delta dosages to patients, though randomized between antagonist and agonist during first stimulation cycles, the study offered the following results: 437 women from IVF clinics in Austria, Denmark, Israel, Italy, The Netherlands, Norway, and Switzerland were randomized, 221 to agonist and 216 to antagonist. Mean age was 32.3 ± 4.3 years and mean AMH was 16,6 ± 7,8 pmol / L (2 . 3 ± 1 . 1 ng / mL) . The study group, in other words, was relatively young and had relatively normal functional ovarian reserve .
Agonist patients produced significantly more oocytes (11.1 ± 5.9 vs. 9.6 ± 5.5; P=0.0185). Unsurprisingly, greater differences were observed in younger women under age
35 and with better AMH values above 15.0 pmol/L (2.1 ng/mL). Both groups had similar cycle cancellation rates, though trends favored agonists (2.0% vs 3.4% for cycle cancellations and 13.4% vs. 14.7% for fresh blastocyst transfer cancellations). The ongoing pregnancy rate was also higher with agonist (35.8% vs. 28,7%), though this difference also did not reach significance (P=0.1002). The same applied to live birth rates (35.8% vs. 28.7%; P=0.1265).
In looking at these data it is important to recognize that neither pregnancy nor live birth rates represent cumulative rates. Having more eggs, however, usually means having more embryos, and more embryos usually mean higher cumulative than first-cycle numbers. In other words, the data of this study strongly suggest that cumulative pregnancy and live birth rates can be expected to further improve over the obvious—statistically non-significant trends—in favor of agonists the study produced, probably reaching statistical significance. Moreover, these data were produced in relatively young women with relatively normal functional ovarian reserve. In poorer prognosis patients and with advancing age, the observed trends in favor of agonists over antagonists, therefore, can also be expected to strengthen.
Does this mean that the field will show an impact from this (in our opinion very important) study? We don’t think so! When antagonists first entered fertility practice, one of the principal arguments of antagonist proponents was the convenience and shorter time period of antagonist over agonist cycles for patients and providers. 2 Those are, of course, important and appropriate considerations but only as long as IVF cycle outcomes are not adversely affected. Proponents of antagonist treatments, therefore, from the beginning claimed that there were no outcome differences between agonists and antagonists, even though in 2002 a Cochrane review suggested outcome advantages for agonists. 3 In other words, already then— somewhat surprisingly—the field chose convenience over outcomes. There is little reason to believe that now it will respond differently.
REFERENCES
1. Lobo et al., Hum Reprod 2024;39(7):1481-1494
2. Albano et al., Hum Reprod 2000;15(3):526-531
3. Al-Inany H, Aboulghar M. Hum Reprod 2002;17(4):874-875
More animal evidence in a mouse model that DHEA supplementation improves ovarian function
CONFLICT STATEMENT: The CHR and some of its employees were awarded certain U.S. patents claiming treatment benefts from supplementing hypo androgenic infertile women with the male hormone DHEA. The CHR and these employees, therefore, receive license fees from use of DHEA in hypo-androgenic infertile women. Readers of this article should be aware of this fact since it may bias opinion expressed by the authors of this commentary regarding androgen supplementation in hypo-androgenic infertile women.
Though by now used in fertlity practce worldwide, DHEA as a fertlity enhancer in infertle women has remained controversial. The principal reason has been the absence of well-powered and designed prospectvely randomized studies, as atempts to execute such studies repeatedly have run into recruitment problems because infertle women—understandably—ofen are reluctant to be randomized to placebo for prolonged tme periods. The use of DHEA has, therefore, primarily relied on either underpowered and poorly controlled small clinical trials or studies of lower evidence levels.
What is, however, ofen overlooked when this issue comes up in discussion, is the fact that animal models, small and large, have by now not only clearly defned why good androgen levels are essental for good follicle growth and maturaton especially at small growing stages between primary and small-antral follicle stages but have also demonstrated improved ovarian functon afer androgen supplementaton in androgen-defcient animals.
Yet another such study was recently published by Chinese investgators in Reproductve Biomedicine Online in which DHEA (the precursor of testosterone) was demonstrated to promote angiogenesis and improved ovarian functon in a rat model premature ovarian insufciency. The study moreover also demonstrated that this efect was achieved by upregulatng HIF-1 alpha/VEGF signaling (1).
REFERENCE
1. Zhao et al., Reprod Biomed Online 2024;49(3):10391

ASSISTED REPRODUCTIVE TECHNOLOGY (ART)
A true
“milestone”
study: Cleavage- vs. blastocyst-stage culture and transfer
Especially after publication of this study by Dutch investigators (another among several such “masterpieces” the collaborative effort of the IVF community in The Netherlands appears to produce every few months) (1), one must conclude that, likely, only very few papers in the history of IVF have caused as much damage to IVF practice as the original paper by Gardner et al ., promoting the use of blastocyst-stage embryo transfer under the very enticing heading, “Culture and transfer of human blastocysts increases implantation rates and reduces the need for multiple embryo transfers (2).”
That this was unintended can be assumed; nevertheless, it must serve as a warning for how a single deeply flawed paper can not only affect, but dominate, medical practice for almost a quarter of a century. Not that there hasn’t been criticism of the very general concept that extended embryo culture to blastocyst-stage was “the thing to do” because it (universally) improved IVF outcomes. Indeed, there was considerable criticism based on biased patient selection in the original study, including from the author of this article (and colleagues) (3). Only very good prognosis patients were included; yet that went not only unnoticed, but the results of the study were presented—and promoted—as
applicable to every IVF patient.
That a level of discomfort persisted with how blastocyst-stage transfers were promoted was witnessed by attempts at meta-analyses by Glujovsky et al ( 4,5). trying to compare cycle outcomes after cleavage- and blastocyst-stage transfers; but those were, of course, dependent on previously published studies and, if those were equally or even only similarly biased to the original Gardner et al. study, it should not surprise that they were unable to offer clear answers.
Here addressed recent Dutch study, therefore, is deserving of applause. Once more, this time under the leadership of two veterans in the field, Simon Cornelisse, MD and Sebastian Mastenbroek, PhD , the unique collaborative research effort
The Netherlands’ academic IVF centers have been able to establish has again born plenty of fruit in answering a crucially important question for the IVF community: Does it really matter in good-prognosis patients whether their embryos are transferred on day-3 (cleavage-stage) or days 5 or 6 (blastocyst-stage) if the desired outcome is not live birth chance in first transfer cycle but cumulative pregnancy and live birth chances? And the answer the study provided was very clear: Cleavageand blastocyst-stage transfers achieved similar cumulative live birth rates in women who after one retrieval had at least 4 blasts available for transfer.
And, importantly, the methodology
of this study was solid: it involved 21 hospitals and clinics during August 2018 and December 2021. Though it is unclear why publication of this study took almost three years— speaking from personal experience and, obviously, speculating—it would not surprise if the message of the paper had run into resistance during the peer review process and, therefore, required repeated submissions to different journal, and that takes time. The infertility field, unfortunately, has a history of often refusing publications which argue against what is considered the common wisdom of the moment.
The study recruited 1202 women, with 599 randomized to cleavagestage and 603 to blastocyst-stage transfer. Primary analysis took place based on intention-to-treat, with secondary analyses based on protocols. Primary outcome was cumulative live birth rate per oocyte retrieval, including all frozen embryo transfers of excessive embryos within one year after randomization if a first transfer had failed (it is important to remember that inclusion into the study required at least 4 transferrable embryos). Secondary outcomes included cumulative pregnancy rates, pregnancy loss, live birth after fresh transfer, number of embryo transfers needed, number of frozen embryos, and obstetric and perinatal outcomes.
As already noted, the cumulative live birth rate did not differ (cleavagestage 58.4%; blastocyst-stage 58.9%). After fresh embryo transfer (i.e., 1st transfer)—as one would
expect—blastocyst-stage transfer had a slightly higher live birth rate (CI 1.26, 1.00-1.58) and a lower pregnancy loss rate (CI 9,68, 0.510.89), and a lower number of required transfers required for a live birth (CI, 1.55 vs. 1.82, P<0.001). The incidence of moderate preterm birth (32-36 weeks) was, however, higher in the blastocyst group (CI, 1.87, 1.05-3.34).
These are fascinating results that go far beyond just the finding of no difference in cumulative live birth rate and include the following:
(i) These are—as in the original blastocyst-transfer study of Gardner et al (2).—findings that in principle only pertain to (very) good-prognosis patients because the requirement of 4 blastocysts for inclusion in the study at all ages clearly selects out only best-prognosis patients. This selection bias, moreover, increases with advancing patient age and declining functional ovarian reserve of a patient because both of these cycle characteristics are obviously directly linked to the chance of producing at least 4 blastocysts in an IVF cycle.
(ii) These findings, however, also suggest that, since in this bestprognosis patient group there was no difference in cumulative live birth rates, in poorer prognosis patients (i.e., in older women and younger women with low functional ovarian reserve), blastocyst-stage embryo transfer will do poorer. In other words, at a still to be determined age and / or lower than normal age-specific ovarian reserve (i.e., in women with premature ovarian aging, POA) affected women will actually do more poorly with blastocyst-stage transfer, an important point that should lead to significant changes in how, for example, ASRM and SART judge
when blastocyst stage-transfers are indicated (6).
(iii) The same also implies to secondary outcomes. Though this study demonstrates mildly lower miscarriage rates and quicker time (fewer embryo transfers) to viable birth, these relatively minor advantages at some point will also disappear as women get older or advance in their POA. They, indeed, at some point may reverse to an advantage for cleavage-stage transfer. Moreover, increased prematurity risk with blastocyst-stage transfer may, indeed, further increase.
(iv) The principal conclusion of this study, therefore, is that blastocyststage embryo transfer is greatly overused in current IVF practice and its increasing utilization (7), therefore, should not only be stopped but reversed.
But this is not all: One also must consider unrelated consequences of excessive utilization of extended embryo culture on IVF. A good example is the concept of almost universal elective single embryo transfer (eSET), by Gardner et al (and later by many others) already in their initial paper touted as a major secondary benefit of extended embryo culture (2). That 2-embryo transfer (2ET) offers higher pregnancy and live birth rates than eSET is undisputed. What this study, therefore, strongly suggests is that the current worldwide policy which in most IVF cycles calls not only for blastocyst-stage embryo transfers but also for eSET must be reevaluated.
And then there is, of course, also to consider the still rapidly growing practice of preimplantation genetic testing for aneuploidy (PGT-A) which is automatically linked to
blastocyst-stage culture because current PGT-A technologies require extended embryo culture, whether for trophectoderm biopsy or for use of so-called non-invasive PGT-A, which uses spent media from blastocyststage embryos to detect fetal DNA (and has even been suggested to extend embryo culture by one day).
The IVF field, therefore, as of this moment in time not only faces the fact that ASRM and SART only just recently reaffirmed that PGT-A, still has not demonstrated any significant beneficial utility for IVF cycle outcomes (8). As a consequence of here discussed BMJ publication, the IVF field finds itself, therefore, at an important crossroad, suddenly confronting the reality that several of the most basic practice patterns at most IVF clinics have been determined to serve no useful purpose or may for some patients even be harmful.
It will be interesting to see how the field will react to this news. Logical consequences will, of course, not only require significant clinical practice changes but will have also considerable economic repercussions. But patients should benefit because less unnecessary treatments will mean lower IVF costs; and if IVF needs one thing to become available for more patients, it is affordability.
REFERENCES
1. Cornelis et al., BMJ 2024;386:e080133
2. Gardner et al., Feril Steril 1998;69(1);84-88
3. Gleicher et al., J Assist Reprod Genet 2016;33(4):455-459
1. Glujovsky et al., Cochrane Database Syst Rev 2016;30(6):CD002118. doi: 10.1002/14651858.CD002118. pub5.
2. Glujovsky et al., Cochrane Database Syst Rev 2022;5(5):CD002118. doi: 10.1002/14651858.CD002118. pub6.
3. Practice Committees of ASRM & SART. Fertil Steril 2018;110(7):1246-1252
4. Andrew C, Doody K. Fertil Steril 2023;120(1, Suppl) E 15-E 16
5. Practice Committees of ASRM & SART. Fertile Steril 2024;122(3):421-434
More on rescue in vitro maturation (rIVM)
The literature has been full of reports in recent months about so-called rescue in vitro maturation (rIVM) which involves the overnight culture of immature MI or GV oocytes in the hope they mature into fertilizable MII oocytes. Now comes a potentially interesting paper from an interesting group of investigators (interesting because led by a startup in NYC called Gameto Inc., which counts Harvard’s George Church, PhD , among its scientific advisers) in eLife. 1

The study built on the now wellestablished observation that oocytes and the surrounding cumulus/ granulosa cells in the follicle maintain a bidirectional conversation during maturation and hypothesized that, therefore, that oocytes stripped off their cumulus calls and socalled “ovarian support cells” (OSCs are further defined below) from mature oocytes would establish such a conversation in the Petri dish during rIVM, thereby improving the
maturation process.
The study involved denuded oocytes from 47 female, 25- to 45-year-old fertility patients undergoing IVF. Oocytes were randomly assigned to standard overnight rIVM or OSC-IVM culture. The latter was defined as 100,000 OSCs in suspension culture with hCG, FSH, androstenedione, and doxycycline added. Standard rIVM culture contained the same add-ons to the media as in OSC-IVM except for the OSCs. The primary endpoint of the study was the percentage of immature oocytes that had matured to MII oocytes overnight.
OSCs were derived from humaninduced pluripotent stem cells (hiPSCs), as previously described in a paper from Church’s laboratory at the Wyss Institute at Harvard University that described the direct differentiation of hiPSCs to functional ovarian granulosa-like cells via the overexpression of transcription factor (10,772 views, 1,282 downloads, 31 citations). 2 How this is done is important to understand the paper in JARG 1 because the process is only inadequately explained.
Here is how the eLife digest summarized this referenced paper: “Ovaries are responsible for forming the eggs humans and other mammals need to reproduce. Once mature, the egg cell is released into the fallopian tube where it can be potentially fertilized by a sperm. Despite their crucial role, how eggs are made in the ovary is poorly understood. This is because ovaries are hard to access, making it difficult to conduct experiments on them.
To overcome this, researchers have built artificial ovaries in the laboratory using stem cells from the embryos of mice which can develop into all cell types in the adult body. By culturing these embryonic stem cells
under special conditions, researchers can convert them into the two main cell types of the developing ovary: germ cells which go on to form eggs, and granulosa cells which help eggs grow and mature. The resulting labgrown ovary can make eggs that produce live mice when fertilized.
This approach has also been applied to human induced pluripotent stem cells (iPSCs), adult human cells which have been reprogrammed to a stemlike state. While this has produced human germ cells, generating human granulosa cells has been more challenging. Here, Pierson Smela, Kramme et al. show that activating a specific set of transcription factors (proteins that switch genes on or off) in iPSCs can make them transition to granulosa cells.
First, the team tested random combinations of 35 transcription factors which, based on previous literature and genetic data, were likely to play a role in the formation of granulosa cells. This led to the identification of a small number of factors that caused the human iPSCs to develop features and carry out roles seen in mature granulosa cells; this includes producing an important reproductive hormone and supporting the maturation of germ cells. Pierson Smela, Kramme, et al. found that growing these granulosalike cells together with germ cells (also generated via iPSCs) resulted in structures similar to ovarian follicles which help eggs develop.
These findings could help researchers build stable systems for studying how granulosa cells behave in human ovaries. This could lead to new insights about reproductive health.”
The Editor’s evaluation of the manuscript said the following: “ This manuscript addresses a
Prof. George Church
fundamental issue in ovarian biology of deriving granulosa cells from human iPS cells. These findings are important to treat female infertility in the future and may prove valuable in the Ob and Gyn clinical practice. The authors provide compelling evidence by developing and validating their model using in vitro ovaroids. This study provides a novel resource for transcriptomic signatures of ovarian somatic cells derived in vitro.”
The JARG manuscript then claimed that OSC-IVM resulted in statistically significant improvement in MII formation with no negative effects on oocyte morphology or spindle assembly. Moreover, oocytes from OSC-IVM demonstrated closer transcriptomic maturity signatures to IVF-MII control oocytes than MII oocytes from standard rIVM. Considering the same group recently reported that hiPSC-derived OSCs are capable of improving MII and euploid blastocyst formation after abbreviated gonadotropin stimulation, 3 here discussed study appears like a logical follow-up.
Though the results of this study are, of course, very interesting – which is the reason we are giving it so much space here – and even though we find especially the transcriptomic improved similarity very intriguing, we, nevertheless maintain a degree of skepticism regarding their study conclusion which were – and we quote – we “strikingly” observed a 1.7-time improvement in maturation in comparison to the control group (62.00 ± 5.57% vs. 37.00 ± 8.96%; P<0.0138).
Our skepticism has several reasons, especially regarding the lack of information about who the patients were who provided the oocytes for this study. We are here, moreover, speaking from very
personal experience because our (unpublished) experience with using cumulus cells for co-culture during rIVM were unsuccessful. In addition, the CHR’s researchers only very recently published a paper in iScience which very well demonstrated how age-dependent rIVM was on the age of the patient at the time of oocyte retrieval. Especially for GV oocytes, advanced female age, paradoxically greatly improved rIVM results with advancing age to similar percentages reported in this paper here for OSCIVM. 4
Clearly an interesting paper, but we would like to see more data before OSC-IVM becomes a commercially available product.
And since we are already talking about rIVM, the Colorado group in a Correspondence article in Fertility and Sterility Reports reported on their center’s experience with oocytes that had undergone rIVM before cryopreservation and, later, at some point were warmed and transferred. 5 The study ended up including 110 patients and 134 IVF cycles and basically demonstrated that such oocytes had similar outcomes up to cleavage stage but had lower blastocyst development and euploidy. Otherwise, the article is loaded with detail that becomes irrelevant because subgroups become too small to reach conclusions. In short, what the publication unsurprisingly says is that if an immature oocyte matures during rIVM, it can and should be used.
REFERENCES
1. Paulsen et al., J Assist Reprod Genet 2024;41:2021-2036
2. Pierson Smela, et al., eLife. 2023 https :// doi . org / 10 . 7554 / eLife 83291,sa0
3. Piechota et al., Hum Reprod 2023;38:2456-2469
4. Nicholas et al., iScience 2023;26:107308
5. Schlenker et al., F S Reports 2024; 5(3):333337
Contrasting “endometrial failure” and “endometrial receptivity testing”: an interesting hypothesis but a very poorly executed attempt at confirmation
Even though endometrial receptivity testing (ERT) is still widely practiced, it is as of this point really hard to understand why that is. Based on well designed and executed clinical trials, the literature on the subject – as repeatedly discussed in these pages – appears clear: ERT does not improve IVF cycle outcomes and in some patients may actually adversely affect outcomes.
Holding this opinion, we were almost ready to discard a paper from European colleagues because it involved several well-known past proponents of ERT and in its heading announced a new “biomarker signature” (i.e., what we thought would be yet another endometrial gene expression signature). But then our scientific conscience kicked in requiring at least a quick and unbiased look at the paper after all and – low and behold – we found the paper to be full of surprises: Most importantly, it did not promise to define the implantation window better (as ERTs attempted to do) but the hypothesis here was “to identify endometrial disruptions independent of the endometrial luteal phase.” 1
In other words, this paper offered a very different hypothesis from
prior ERTs; no longer was there the goal of shifting the timing of the embryo transfer into an allegedly better defined implantation window (which to us appears to be a somewhat outdated concept), but to ask the question whether the expression of 404 genes in the mid-secretory endometrium could identify endometria with poorer and better ability to lead to pregnancy— conceptually and clinically, of course, a very different question.
And not only is the hypothesis different, but so is also the underlying rational for a patient undergoing a test: While with ERTs the rational is purely mechanistic (i.e., embryo transfer earlier or later), here the rational becomes diagnostic, with the question no longer being when to transfer her embryos but why isn’t she getting pregnant? In other words, assuming this newly announced test, indeed, can differentiate between “good” and “bad” endometria, it would offer a first step toward understanding why the endometrium prevents in some patients embryos from implanting, converting the concept for doing a test from being mechanistic to potentially being truly diagnostic in the sense that an identified cause could lead to a specific treatment.
With the CHR now for some time has promoted the concept of “precision medicine” in infertility, such a test and the resulting patient-specific treatment would then represent exactly the kind of progress the infertility field must strive for in contrast to what we have been witnessing over the last two decades with the premature introduction of poorly validated tests and treatments given the by now derogatory term “add-ons.”
So, how was this study done and
what
did it reveal?
Unfortunately, the description of study’s design turned out to be almost paradoxically inadequate: The study is described as “prospective” but was performed between 2018 and 2021 involving 281 patients who were scheduled for endometrial evaluation “due to medical indications or 2 or more implantation failures of idiopathic origin.” But the authors don’t tell us what those medical indications were and how they defined implantation failure due to idiopathic origin. Based on these shortcomings one already wonders how this paper made it through peer review without even minimally defining the study population. Then the authors note that the patients “underwent hormone replacement therapy for a single embryo transfer” (a term usually reserved for postmenopausal women) but here –we assume – meant to suggest that patients underwent embryo-thaw cycles with artificially built cycles (once again, one wonders about a peer review process that ignores absence of such basic information).
What the paper does tell us is that age range of patients was 18-50 years and BMI of 19-30 kg/m 2, both obviously very wide ranges and, apparently, ignored in data analysis, as if the expected difference in transcriptomic profiles between age 18 and age 50 would not be highly relevant. The paper also informs on many other patient and cycle characteristics but in principle appears to have retroactively resurrected old data from prior studies on ERT to investigate the new concept of “endometrial failure.” This appears confirmed by the paper referencing how endometrial biopsies were obtained and processed with a prior publication. 3
The paper then claims that the new
data analysis allowed stratification of the study population into a poor (n = 137) and good (n = 49) endometrial prognosis groups on the basis of their clinical and transcriptomic profiles. The differences were as follows: Pregnancy rates (44.6% vs. 79.6%), live birth rates (25.6% vs. 77.6%), clinical miscarriage rates (22.2% vs. 2.6%), and biochemical miscarriage (20.4% vs. 0%). The relative risk of endometrial failure for patients predicted as a poor endometrial prognosis was 3.3 times higher than those with a good prognosis. The differences in gene expression between both profiles were proposed as a biomarker, coined the endometrial failure risk (EFR) signature. Poor prognosis profiles were characterized by 59 upregulated and 63 downregulated genes mainly involved in regulation (17.0%), metabolism (8.4%), immune response, and inflammation (7.8%). This EFR signature had a median accuracy of 0.92 (min = 0.88, max = 0.94), median sensitivity of 0.96 (min = 0.91, max = 0.98), and median specificity of 0.84 (min = 0.77, max = 0.88).
The authors’ conclusion of their paper was that “the EFR signature represented a promising biomarker for endometrial evaluation and –inspired by what in breast cancer research has been called the MammaPrint risk signature, they suggested that the EFR signature could become a next-generation (after ERT) tool to classify patients on the basis of endometrial prognosis.” Transparently, the Declaration of Interests of the paper discloses a pending patent application.
After spending an unexpectedly long time on the review of this manuscript, what then is the message?
The answer is complex because the new hypothesis presented
by the authors that endometrial transcriptomic profiles – if done and analyzed correctly – may be able to identify IVF patients who have an endometrial cause for not conceiving sounds logical and deserves further pursuit. But the here presented paper is completely inadequate to even lay claim to represent a preliminary step in developing such a test. What, however, is even more shameful is the fact that one of the infertility field’s most prominent medical journals accepted this paper. That a paper with so many most basic shortcomings could make it through the journal’s peer review process is nothing but astonishing.
In the following month’s issue the journal published a Letter to the Editor by four prominent colleagues, two from France and two from the U.S., which raised some of the issues we noted here but, in addition, pointed out incongruities between prior publications of this group apparently involving the same patient population. 3 As is customary, the medical journal then allowed the authors of the original paper to respond. Interestingly, only three of the original 12 authors signed this letter of response and – even more interestingly – those three authors were the only one among the original 12 who in the paper’s Declaration of Interest had acknowledge a planned European patent. Suffice it to say, their letter offered no real rebuttals of the criticisms in the Letter to the Editor or – for that matter – of what we have criticized here. 4
REFERENCES
1. Diaz-Gimeno et al., Fertil Steril 2024;122(2):352363
2. Diaz-Gimeno et al., Hum Reprod 2022;37:284-296
3. Pirtea et al., Fertil Steril 2024;122(3):549-550
4. Diaz-Gimeno et al., Fertil Steril 2024;122(3):551
Does using embryos
from frozen donor eggs in fresh or in frozen-thawed embryo transfers make a difference?
This time it is a Research Letter in Fertility and Sterility that attracted our attention in which investigators pursued an in principle interesting study by asking whether it makes any difference whether embryos produced from frozen donor eggs after warming and fertilization should be, if possible, transferred fresh or could be frozen for later thaw and transfer. They attempted the answer through a sibling oocyte study and reported that there was basically no difference in cycle outcomes. In other words, there was no reason to be concerned about double cryopreservations. 1
But once again, for several reasons, we were not very happy with the peer review of this paper and those reasons, once again, first and foremost involved patient selection. It this time, however, was not a lack of information on the oocyte donors (here the study population) because they were in principle well-defined with mean age of 25.5 years and mean BMI of 23.0 kg/m 2. Their mean AMH level of 5.9 ng/mL and mean antral follicle count of 28.3, however, told a different story: those values, of course, were anything but “normal” for an average group of egg donors.
Both of these values defined the investigated egg donor population as highly selected for unusually good functional ovarian reserve. Indeed, a majority must have been PCOS patients. The claims made by the authors of this research letter,
therefore, do not apply to average egg donors who usually have lower functional ovarian reserve. The second reason for our unhappiness with the peer review of this Research Letter also relates to number of eggs retrieved from an oocyte donor because what ultimately defines the “value” of an egg donor is not the pregnancy/live birth rate achieved from a first embryo transferred using her eggs, but the cumulative pregnancy/live birth rate the donor cycle produces.
A single cycle sibling oocyte study, therefore, can really not offer an answer to the question the authors attempted to answer. A donor cycle’s first two oocytes chosen for this sibling study may be the best of the cycles’ total oocyte cohort. Results of remaining oocytes may be very different since better oocytes freeze and thaw better than poorer oocytes.
Finally, there is one more rather indisputable reason why this brief study cannot be taken seriously: every time we freeze either oocytes or embryos, we automatically lose cumulative pregnancy and live birth chances because at every thaw some eggs or embryos will not make it. The basic concept of this study, therefore, simply does not make sense as it is presented, and is just another example of deteriorating peer review in our specialty journals.
REFERENCE
1. Barrison et al., Fertil Steril 2024;122(3): 536-537
Do co-transfers of poor embryos impact
the
results of good embryos?
Whether co-transferred embryos
impact each other’s chances of implantation has been a question for decades, with studies offering different results. Considering the large variety of possible combinations of embryos, this should not surprise. Now investigators from China contributed another answer in a typical Chinese study of huge cycle numbers (n=11,738).
All cycles involved vitrified warmed blastocyst-stage transfers (between 2015 and 2022) and basically underwent single good-quality embryo transfer (n=9,338) or a double embryo transfer in which a good- quality blast was combined with a poor-quality embryo (2-ET, n=2,400).
Unsurprisingly, the live birth rate was significantly higher in the 2-ET group (65.6% vs 56.3%; P<0.001). Multivariable logistic regression demonstrated that 2-ET was an independent predictor of live birth rate (OR 1.55, 95%CI 1.41 to 1.71; P<0.001). Moreover, while a higher twinning rate was, of course, expected with 2-ET, the degree of difference was astonishing (1.8% vs 41.4%, P<0.001).
While it appears safe to stop worrying about combining poorer with better embryos, the study raises serious additional questions regarding its credibility: First, to achieve in a general population of this size a 56.3% live birth rate either means an unbelievably good IVF program or— we, of course, do not wish to accuse our Chinese colleagues of any willful wrongdoing—incorrect outcome data presentation.
That 2-ET would produce a ca. 10% improvement in life birth rate to 65.5% would be within expected range. But a ca. 40% increase in
twinning rate with only a ca. 10% improvement in live birth rate is again highly suspicious. It also raises questions about how the authors defined good- and poor-quality embryos
Simply based on the numbers it is, moreover, obvious that this was not a prospectively randomized study, but that good-prognosis patient usually received a single embryo, while poorer prognosis patients received a 2-ET. If confirmed, the study, therefore, also may suggest that the program may not very well differentiate between good- and poor-prognosis patients and between good and poor embryo quality. And if the program has these difficulties, how it would generate above-noted superb live birth rates is difficult to understand.
We, therefore, have serious questions about the reported outcomes in this publication and wonder whether the journal’s editors requested submission of primary materials to the editorial office before acceptance of this paper. If not, one must ask, why not?
REFERENCE
1. He et al., Reprod Biomed Online 2024;49(3):104104
More disappointment in IVF with A.I.
If it didn’t involve A.I., we very much doubt that the paper we are discussing here would have been published in the very highly rated general medical journal Nature Medicine ; but it does involve A.I. and, therefore, we have the opportunity to review this paper here in which investigators from Australia, New Zealand and several European countries attempted embryo selection in IVF in a randomized,
double-blind noninferiority trial by comparing deep learning with standard manual morphology. 1
We, of course, recently on several occasions have here in the VOICE described the concept of embryo selection in an IVF cycle as a biologically false and, therefore, implausible dogma that has ruled IVF practice since the earliest days of this procedure. That the here reported multicenter investigation – using deep learning – was unsuccessful to beat manual morphology with endpoint clinical pregnancy (not even live birth) for a noninferiority of only 5%, for us was, therefore, not surprising (and rather pleasing).
This result, moreover, proves in addition another argument made in these pages in recent months repeatedly regarding the in our opinion oversold potential use of A.I. in medicine in general, namely for A.I. to find a difference between options, there must exist such a difference in the first place. As we believe that such a differences do not really exist to significant degrees in cumulative pregnancy and live birth rates of one oocyte and/or embryo cycle cohort, we do not expect A.I. to ever have a significant impact on embryo selection in IVF.
To all those start-ups which still believe otherwise and – even more so – to all those start-ups which already know better but still are trying to sell their A.I services to IVF clinics, we suggest you preserve your resources and start looking for other, and hopefully better, targets for A.I.
REFERENCE
1. Illingworth et al., Nat Med 2024; Nat Med (2024). https :// doi org / 10 1038 / s41591-024-03166-5

GENETICS IN REPRODUCTION
In the end, nothing seems to change with
preimplantation genetic testing for aneuploidy (PGT-A)
THE RECENT ASRM/SART PRACTICE COMMITTEE OPINION:
Yes – as previously noted in the VOICE afer an electronic preprint was published – ASRM and SART fnally published in print their new Commitee Opinion on PGT-A,1 and there is good news and bad news: The good news is that the document for the frst tme clearly states that, “the value of PGT-A as a routne screening test for all patents undergoing IVF has not been demonstrated.”
This statement alone, clearly distnguishes this Commitee Opinion from its 2018 predecessor document and –unquestonably – represents signifcant progress, for which ASRM as well as SART are to be congratulated. This sentence alone renders routne utlizaton of PGT-A in all IVF cycles –as is currently practce in a substantal number of IVF clinics – no-longer defensible.
The bad news in all of this is, however, that above noted sentence – more or less – was the beginning and the end of the clear and evidence-based part of the document because an appropriate follow-up was very obviously missing. An as important statement as the above noted sentence afer
over 20 years of ever increasing PGT-A utlizaton in U.S. IVF clinics (including the tme period when the procedure had diferent names), one would expect to be followed by the queston, “… and what now?” Moreover, ASRM and SART would also be expected to answer this queston.
Instead, the fact that PGT-A as a screening tests in IVF has in over 20 years failed to establish even one-single clinical utlity, is just lef hanging out there for IVF providers and their clinics to decide on how to react to this statement. That is not only unfair to providers and clinics but is also ethically challenging because, like other professional societes, ASRM and SART are not only expected to analyze and advise on what should be done in fertlity practce, but also on what should not be routnely done.
What should not be done seems obvious: If something does not work and, therefore, does not produce a beneft that warrants its use, it should no-longer be done in routne clinical practce. This means that, based on this new ASRM/ SART document performing PGT-A routnely in every IVF cycle no-longer appears to represent “standard-of-care.” This conclusion then, however, immediately raises the second queston: under which circumstances is PGT-A then stll indicated? And this is where the ASRM/SART document gets into further troubles because – not only does it not provide an answer – but the document appears to struggle in atempts to fnd such indicatons. An example of this struggle is the following “word-salad” already in the abstract: “The value of PGT-A to lower the risk of clinical miscarriage is also unclear, although these studies have important limitatons.”
What this sentence in simple English is, likely meant to communicate is that reducton in miscarriages – by proponents of PGT-A now frequently proposed as a new primary indicaton for PGT-A afer improvement if pregnancy and live birth rates have become impossible to defend – is also no longer defensible. So, what is then lef?
One increasingly hears that PGT-A shortens tme to pregnancy. The literature suggests this may be true, though only to very minor degrees and only in good prognosis patents who produce large embryo numbers. The smaller the embryo number, the smaller this beneft, of course, will be. And even assuming such a marginal beneft, is this really worth the efort and additonal costs?
In short, the ASRM/SART document1 represents important progress in defning the utlity of PGT-A in associaton with IVF. The two Commitees, interestngly, also responded in writng to a critcal Leter-to-the-Editor which, among other
issues raised how troubling it was that—despite increasing reports about the inefectveness of PGT-A in IVF—utlizaton of the procedure has been increasing.2 In their response, the two Commitees agreed that “it was troubling that the use of PGT-A in the U.S. is increasing, despite the lack of evidence to support this practce.”3
But since their document failed to go beyond that in spelling out the rather automatc conclusions one must reach from this most recent Practce Commitee opinion, we summarize them here in three points.
Since PGT-A has not been demonstrated to have any clinical value as a routne screening test for all patents undergoing IVF, the following changes in IVF practce appear to represent logical conclusions:
• PGT-A should no-longer be ofered as a routne addon to IVF cycles.
• PGT-A should only be ofered for specifc clinical circumstances where the benefts outweigh costs and risks. Examples are parental inheritable chromosomal abnormalites (i.e., balanced translocatons), repeated miscarriages with abnormal karyotypes, medical need or social desire for sex selecton, anxiety, etc.
• Based on the right to self-determinaton, patents should be allowed to request PGT-A in associaton with IVF, though they must receive informed (writen) consent which clearly states that PGT-A so-far has not demonstrated any benefcial outcome benefts in IVF and, therefore, - except in situatons as outlined above - stll must be considered an experimental procedure.
PGT-A IN FRESH vs. FROZEN DONOR OOCYTE CYCLES: Related, a recent paper by investgators from several U.S. insttutons recently analyzed 28,562 donor oocyte cycles reported to the SART registry and found that – among patents who had at least 1 blastocyst available for transfer (i.e., in relatvely good prognosis patents), utlizaton of PGT-A was actually associated with a decreased live birth rate afer 1st transfer in fresh oocyte donor cycles (58.4% vs 66.6%: P<0.001), thereby reafrming prior recent reports suggestng that in younger patents PGT-A in 1st cycles may, indeed, adversely afect IVF cycle outcomes.4
This diference disappeared, however, in frozen-thawed oocyte donor cycles with PGT-A, where PGT-A cycles nominally (though afer adjustments not signifcantly) produced higher live birth rates (48.3% vs. 40.5%, N.S.).
That PGT-A is frequently used even in donor-recipient cycles, which already produce the highest pregnancy and
live birth rates among all cycles, is only further evidence for the abusive utlizaton of PGT-A in the U.S.
NON-INVASIVE PGT-A (niPGT-A): The current hypothesis of why many colleagues pursue niPGT-A is that PGT-A has failed to improve IVF outcomes because due to increased manipulaton a biopsy adversely afects an embryo’s ability to later implant and to lead pregnancy. First suggested by Richard F. Paulson, MD,5 this hypothesis and the hope for a simpler PGT-A procedure have led to an onslaught of reports using diferent methodologies, though all based on using spent media from blastocyst-stage embryos to detect fetal DNA. The test basically follows the same principles that has been successfully implemented in obstetrical practce with the use of non-invasive prenatal testng of maternal blood (niPNT).
A recent review artcle in Human Reproducton summarized this experience, concluding that, “like traditonal PGT-A, niPGT-A must atain the high standards of precision and reliability expected of any genetc testng platorm used in clinical setngs before it can be adopted into routne protocols of IVF.”6
We, of course, fully agree with the sentment expressed, and also agree that the quick implementaton of niPGT-A by several IVF clinics in the U.S. and overseas appears premature. But that, of course, should not surprise, considering that PGT-A has been sold to the public for over 20 years and—just now—was fnally “discovered” by ASRM/ SART not to improve IVF outcomes (see above).1
This artcle, however—somewhat unsurprisingly, considering the artcle’s three authors have been strong proponents of PGT-A for many years—missed what is likely the most important argument against niPGT-A which is that it stll pursues the same (by now badly debunked) PGT-A hypothesis which suggested that a blastocyst-stage embryo from a small DNA sample can be reliably diagnosed in its chromosomal make up.
In other words, PGT-A has failed for over 20 years not because of poor techniques and technologies (those have greatly improved and yet PGT-A, stll fails in this efort) but because the biology of early-stage embryos has been widely misunderstood. This biology, however, remains the same, whether fetal DNA is obtained from a 5-6-cell trophectoderm biopsy or from spent media.
And then there are our Spanish colleagues who have brought us so many original tests, procedures, and instruments over the years that failed to deliver what they
initally promised, somewhat surprisingly in collaboraton with Boston colleagues who usually are more cautous in their pronouncements.7 They collaborated in a study— this tme in Fertlity and Sterility—where they decided to extend routne embryo culture from 5 to 6 days in the hope to get more and beter spent media for their niPGT-A assay (seemingly unconcerned about several recent reports on increasing epigenetc changes observed in embryos with prolonged culture tmes).
But this is not the main reason why we are mentoning this paper here. That is the fact that the authors reported high concordance between niPGT-A and PGT-A by embryo biopsy, as the authors “cautously” concluded, “possibly limitng the need for invasive PGT-A and making it available for an (even) wider range of patents.” Now, does that make sense afer above noted ASRM/SART Practce Commitee Opinion?
But this is, of course, not all yet: The same group (in different order of authors, of course) published another paper on the same subject, this time in Human Reproduction (why putting all together when you can get two papers out of it?), where the authors looked for potential damage the embryos may have encountered as a result of longer blastocyst culture. And—unsurprisingly and note the wording—“the implementation of an embryo culture protocol to accommodate iPGT-A had no impact on blastocyst viability or pregnancy outcomes.”
To summarize, here patents reported in these two studies were by determined, we presume by their physicians, to need a test called PGT-A which by ASRM/SART, fnally, afer over 20 years of clinical (ab)use was declared useless (and in some cases even harmful to IVF cycle outcomes). 1 They, however (rather poorly controlled, but that is a separate issue) chose not to ofer some patents the established PGT-A test but instead an experimental and in general reported to be less “accurate” PGT-A test in niPGT-A, prolonging embryo culture without knowing the efects from these changes on embryo quality, implantaton and pregnancy rates, and—as already noted above— epigenetcs, potentally afectng an individual for her/ his whole life. Wow, one is only lef wondering how the informed consent for this study was worded?
AND A FINAL WORD: Afer over 20 years of various forms of PGT-A, it likely that as of 2024 a substantal majority of IVF cycles in the U.S. include PGT-A at an average added costs to usual costs of IVF of at least $5,000. Moreover, this added cost come out of the patent’s pocket, even if she has full insurance coverage for IVF, because insurance companies (in this case smartly) do not cover PGT-A. Also smartly, IVF
clinics and PGT-A laboratories roughly split the fees for PGT-A (that is unless clinics have their own in-house PGT-A laboratory, which especially clinic chains now increasingly establish, in which the clinic gets the whole fee).
IVF clinics, therefore, have become dependent on PGT-A fees which in contrast to increasing insurance coverage for IVF cycles is usually received in cash and undiscounted. Therefore, it appears very unlikely that the recent ASRM/ SART document on PGT-A will even make a small dent in PGT-A utlizaton. Indeed, with rapidly growing introducton of niPGT-A, we would not be surprised to see overall utlizaton of PGT-A to expand even further.
REFERENCES
1. Practce Commitees of the ASR and SART. Fertl Steril 2024;122(3):421-434
2. Orvieto R. Fertl Steril 2024;122(3):555
3. Practce Commitees of ASRM and SART. Fertl Steril 2024;122(3):556
4. Gingold et al., Fertl Steril 2024; DOI: 10.1016/j. fertnstert.2024.08.315. Ahead of print.
5. Paulson RF. Fertle Steril 2017;108(2):228-230
6. Volovsky et al., Hum Reprod 2024;39(9):1899-1908
7. Ardestani et al., Fertl Steril 2024; 122(3):465-473
8. Sakkas et al., Hum Reprod 2024;39(9):1952-1959
CAUTION, UNREVIEWED
PREPRINT: What aneuploidy does to preimplantation-stage embryos, explaining self-correction?
We only rarely present unreviewed preprints, but we found a recent one by Belgian investgators, published by bioRxiv on September 14, 2024,1 interestng enough to make an excepton since it is highly relevant to a stll somewhat controversial subject, the queston of whether embryos at early stages can self-correct from chromosomal abnormalites.
That this may, indeed, be happening was frst suggested in the mouse2 and more recently in a paper CHR’s investgators published in collaboraton with colleagues from Rockefeller University.3 This preprint is the product of research the Belgian investgators initated to potentally beter understand this self-correcton mechanism.
They now reported that aneuploidy triggers proteotoxic stress, autophagy, p53-signaling, and apoptosis independent from DNA damage. The consequence was lower total cell numbers in aneuploid embryos. Lower cell numbers in trophectoderm were atributable to apoptosis, while in
the embryonic cell lineage (epiblast/primitve endoderm) aneuploid apparently impaired second lineage segregaton and, especially, formaton of the primitve endoderm.
Summarizing their fndings, these authors thus claimed that aneuploidies in human preimplantaton-stage embryos trigger autophagy and p53-mediated apoptosis and impairs the second lineage segregaton, thereby leading to embryo arrest in many aneuploid embryos but, also, potentally contributng to the ability of embryos to self-correct in the embryonic cell lineage (fetus), while this ability is strongly diminished in the extraembryonic cell lineage (trophectoderm and placenta).
REFERENCES
1. Regin et al., bioRxiv preprint. Doi: htps://doi. org/10.1101/2022.08.31.506009, posted September 14, 2024
2. Bolton et al., Nat Commun 2016;7:1-12
3. Yang et al., Nat Cell Biol 2021;23:312-321
Ovarian aging—among other
things— also refects cancer risks
Ovarian aging as a model for general aging has become a prominent subject in the medical literature, but now an internatonal group of investgators have taken these studies a step forward: Afer human genetc studies of common variants have informed well about biological mechanisms that govern ovarian aging, a consortum of internatonal investgators now reported in Nature magazine analyses of rare protein-coding variants in 106,973 women from the UK Biobank study,1 demonstratng with approximately fve-tmes larger efects than had been previously found for more common variants, specifcally ETAA1, ZNF518A, PNPLA8, PALB2, and SAMHD1, with the later associaton reinforcing the link between ovarian aging and cancer susceptbility, previously reported.2 Damaging germline variants of SAMHD1 were furthermore associated with extended reproductve lifespan and increased all causes of cancer risk in women and men. On the other hand, proteintruncatng variants in ZNF518A were associated with shorter reproductve lifespan (i.e., earlier menopause by a whopping 5.61 year) and later menarche age (by 0.56 years). The study also revealed that common genetc variants associated with earlier ovarian aging also associated with an increased rate of maternally derived de-novo mutatons, though the authors were unable to replicate this result with another database.
An accompanying commentary by Anne Goriely summarized these fndings as follows:3 “By mining large-
populaton genetc data sets, the researchers identfed the key factors controlling menopause tming, and revealed a close connecton between reproductve longevity, cancer risk and new mutatons in children.” She also concluded that “these fndings could also provide avenues for developing treatments to delay ovarian aging,” though hopefully without increasing cancer risk.
REFERENCES
1. Stankovic et al., Nature 2024;633:608-614
2. Ruth et al., Nature 2021;596:393-397
3. Goriely A. Nature 20224;633:530-531
Novel genetic risk locus on X chromosome found which is linked to Alzheimer’s
Based on a meta-analysis of 1,252,284 (females 57.7%, males 42.3%) individuals in genetc associaton studies in various data cohorts in diferent places, among which 138,558 had Alzheimer’s, investgators recently reported in JAMA Neurology and associaton between SLC9A7 –located on the X chromosome – and Alzheimer’s disease. The associaton was modest (~5%) and the strongest among six independent genetc loci the study linked to Alzheimer’s which met the threshold for X chromosomewide signifcance.
An accompanying commentary summarizing the involvement of the X chromosome with Alzheimer’s,2 reemphasized that four of these loci demonstrated escape from X chromosome inactvaton, a fnding that may contribute to the understanding of why Alzheimer’s is more frequent in females. Moreover, SLC9AC is involved in regulatng pH homeostasis in Golgi secretory compartments, suggestng that it may have downstream efects on betaamyloid accumulatons.
REFERENCES
1. Belloy et al., JAMA Neurol 2024. doi:10.1001/ jamaneurol.2024.2843
2. Buckley RF, Seto M JAMA Neurol 2024. doi:10.1001/ jamaneurol.2024.2831
Five genes linked to postpartum hemorrhage, the leading cause of maternal death in the world
Danish investgators identfed fve genetc loci linked to postpartum hemorrhage in a meta-analysis. Functonal annotaton analysis indicated candidate genes HAND2, TBX3 and RAP2C/FRMD7 at three loci and showed that at each locus, associated variants were located within binding sites for progesterone receptors. They also found strong genetc correlatons with birth weight, gestatonal duraton and uterine fbroids. In contrast to postpartum hemorrhage, bleeding in early pregnancy yielded no genome-wide associaton signals but showed strong genetc correlaton with various human traits. The later fnding suggested a potentally polygenic etology.
These fnding suggest a potental progesterone connecton to postpartum hemorrhages, as the authors furthermore suggested, possibly linked to signaling dysregulaton.
REFERENCE
1. Westergaard et al., Nat Genet 2024; htps://doi.org/10.1038/ s41588-024-01839-y; ahead of print

Pregnancy and obstetrical management
The amazing changes to the mother’s brain in pregnancy
Because of the obvious associaton of pregnancy with neurological and psychiatric changes—as Nature magazine recently noted1—what happens to the brain in a woman during pregnancy has for the longest tme been neglected. Liam Drew, the author of the artcle is telling one of these always fascinatng stories, how something unexpected happening out of the blue one day changes science. The story this tme involved in November of 2008 a car ride of three postdocs in neurosciences to a party, with one of them notng that she was thinking about having a baby. The ensuing discussion about what that would do to her brain became so intense that the three gave up on the party and drove back to their lab at the Autonomous University of Barcelona (where all of this happened) to search the literature.
What they found was a litle bit of animal work but absolutely nothing about the human experience. And this is where the revoluton started: It took eight years before a frst paper was published using magnetc resonance imaging (MRI) of the brain before, during and afer pregnancy.2 Two of the three original passengers in the car, Susana Carmona and Elseline Hoekzema, are stll driving the feld forward, one stll in Spain, the other in The Netherlands.
As Drew notes, 50% to 80% of pregnant women report obvious efects on the brain from pregnancy, - from memory defcits, brain-fog, and other cognitve complaints. Almost everybody has heard the term “pregnancy brain” to describe those occurrences. By now we, moreover, know that they are biological and not mental because they are associated with highly signifcant changes in sizes of diferent brain regions. The impact is, however, most pronounced in the cerebral cortex and there especially in areas that integrate informaton from other areas of the brain. The

entre cortex shrinks by ca. 5%, only to fully reverse this shrinkage quickly afer birth of the child.
Though not yet absolutely confrmed, the shrinkage is not perceived as necessarily negatve. It, indeed, appears to correlate with the depth of maternal-child bonding that evolves. Moreover, shrinkage does not necessarily also mean loss of neurons. Most researchers, indeed, believe it refects a refnement of neural functon during a demanding tme period.
Another issue the artcle of Drew raises is the associaton with a heightened risk for mental health issues, mostly immediately postpartum. What used to be called postpartum depressions and is now called peripartum depression, is clearly in some ways associated with pregnancy. Pregnancy also has been demonstrated to have long-term effects on the brain; indeed, it may keep the brain younger.3
REFERENCES
1. Drew L. Nature 2024;632:2224
2. Hoekzema et al., Nature Neurosci 2017;20:287-296
3. De Lange, et al., Proc Natl Acad Sci USA 2019;116:22341-22346
Have we forgotten about preeclampsia?
This is what The Wall Street Journal thinks. On September 3, 2024, it published a frontpage artcle describing preeclampsia as a deadly disorder that is threatening new mothers since it seems to be on the rise in the U.S., and nobody is researching it.
Though describing preeclampsia these days as “deadly” is an obvious exaggeraton, more marketng of the artcle than factual reportng, there is some truth to what the artcle says otherwise: Preeclampsia, indeed, is increasing in prevalence and it is not very clear why that should be. In additon, and quite obviously linked to our stll unexplainably poor understanding of the conditon, this is only one – among innumerable others – for how unsatsfying the research in perinatal medicine has now been over decades.
What have we really learned over the last 40 years? We stll don’t know what the signal is that induces labor either pre-, at-, or post-term. We stll don’t understand how the maternal immune system tolerates the fetal semi-allograf (and with egg-donaton or use of a gestatonal carrier a full allograf). And, yes, we stll don’t understand why some women are getng preeclampsia.
We in these pages have repeatedly made the point that all of the answers for these pregnancy-associated conditons with great likelihood are linked to each other by sharing the immune system of the mother as the principal culprit. But isn’t it really tme to fnd out?
And of course, related, we do have two publicatons to menton which did address immune system-related issues regarding preeclampsia. First among them is a paper from China in eLife, which reveals a preeclampsia-specifc immune cell network in placentas.
CAUTION, UNREVIEWED PREPRINT: The eLife assessment before revisions was that the paper represented a valuable study investgatng the maternal immune system’s role in preeclampsia. The study mapped the immune cell landscape of the human placenta, notng an increase in macrophages and Th17 cells in cases of preeclampsia. Th17 cells are a subset of T cells which produce IL17, granulocyte/ monocyte colony stmulatng factor (GM-CS), and Interferon-gamma, all proinfammatory cytokines. From mouse experiments they furthermore concluded that the IGF-1 – IGF-1R pathway may be involved in how macro -
phages infuence T cells, potentally driving the pathology of preeclampsia. This paper is not yet accepted and will have to undergo quite signifcant revisions and additons if it is to be accepted; but it certainly presents an original concept.
The second paper, in contrast, appeared already in print but is a systematc review under the ttle, “Immunologic aspects of preeclampsia.”3 It is writen by French physicians and basic scientsts who have a long traditon of interest in reproductve immunology. That, however, does not always mean they are correct.
Though supposedly a systematc review, we would more call it a selected review, concluding that decidual immune cells, including regulatory T cells (Tregs) NK cells, macrophages (se also above) and decidual nonimmune cells, such as stromal cells, are critcal for trophoblast invasion and vascular remodeling. From these observatons they then concluded that dysfunctons in these cells or of their interacton with trophoblast cells, or decreased expression if immune checkpoints, such as HLA-G, can lead to defects in placental vasculature and, ultmately, to preeclampsia.
We do believe that the biological observaton described in this paper are likely factual and characteristc of preeclampsia but in all the years these facts have been presented as causal for preeclampsia, we have seen no convincing evidence. To the contrary, the beter we have come to understand ground rules of tolerance, the less-likely we perceive the probability that the tolerance by the maternal immune system of a logarhythmically growing parasitc tumor (which the fetal-placental unit is) being the consequence of a primarily local immune process to be an even possible explanaton. Similarly, it does not make sense, that local anatomical conditons in the uterus months later suddenly are causal in initatng a systemic disease like preeclampsia (and how would this local source of the disease cause postpartum preeclampsia?). Much more likely, preeclampsia refects in a way abnormal terminaton of tolerance by the maternal immune system. Like the conditon of preeclampsia, this hypothesis ofers at least a systemic explanaton for an obviously systemic disease.
REFERENCES
1. McKay B.. Wall Street Journal, September 3, 2024l htps:// www.wsj.com/health/preeclampsia-rise-united-states-pregnancy-20115589
2. Fei et al., eLife. htps://doi.org/10.7554/eLife.100002.1
3. Boulanger et al., AJOG Global Reports 2024l4(1):100321

How do polycystic ovary syndrome (PCOS) pregnancies fair obstetrically?
Two recent papers atempted to answer this queston: In a frst study by investgators in Norway that appeared in JAMA Network Open, the conclusion was that maternal PCOS was associated with lower birth weight, shorter birth length, and smaller head circumference in ofspring. Growth restricton correlated with BMI.1 The second paper announced in its ttle informaton on an alleged correlaton of PCOS phenotypes with pregnancy and neonatal outcomes.2 Unfortunately, however, the paper did not address classical PCOS phenotypes (only normo- or hyper-androgenism). The overall prevalence of prenatal complicatons and neonatal outcomes, however, to quote the authors – “precluded a meaningful comparison between the two groups.”
The only conclusion the paper really ofered was that women with hyperandrogenic PCOS achieved lower pregnancy and live birth rates than normo-androgenic PCOS patents. Interestngly, both patent groups were very young (28.5 ± 4.2 and 28.3 ± 4.2). Why is this important? Because under Rotterdam criteria, only PCOS phenotype D is not hyper-androgenic and this phenotype until approximately age 35 has normal androgen levels and is normally fertile. Women with this phenotype develop infertility only once they become hypoandrogenic after age 35. 3 The study, therefore, misinforms.
REFERENCES
1. Aaserud Talmo et al., JAMA Network Open 2024;7(8):e2430543
2. Chan et al., Obstet Gynecol 2024;144(4):543549.
3. Gleicher et al., Biomedicines 2022;10(7):1505

NEWS IN GYNECOLOGY …
… on polycystic ovary syndrome and endometriosis
HYPERANDROGENISM and PCOS: Since we above already ofered informaton on how pregnancies in PCOS may difer from other pregnancies, here are some new papers about PCOS in general, startng with a worthwhile review artcle in Endocrine Reviews by Chinese authors which describe the genetc and epigenetc landscape for drug development in PCOS.1
They correctly point out that all currently available treatments for PCOS are, in principle, only symptomatc and, quite remarkably, not even a single drug has been approved so-far by the FDA specifcally for the clinical indicaton of PCOS. They furthermore again correctly argue that a beter understanding of genetcs and epigenetcs – both increasingly important in new drug developments – therefore may be helpful in the development of PCOS-specifc new pharmacological interventons and make this the basic assumpton of their review. Since we do not remember a similar angle in any recent PCOS-related artcle, this is defnitely a worthwhile read.
Another in many ways related artcle in the same issue of Endocrine Reviews ofers a history of how causes of common hyperandrogenism were elucidated between 1965 and ca. 2015.2 The single author of this artcle was Robert L. Rosenfeld, MD, from the Department of Pediatrics and Medicine at the University of Chicago, who was unquestonably one of the most important contributors to the literature during that tme period regarding PCOS and hyperandrogenism in general. His opinions were always worth listening to.
Since only recently addressed in the VOICE, most of our readers by now should be familiar with so-called microRNAs (miRNAs) which are single-stranded, non-coding RNAs which regulate mRNA expression on the post-transcripton level. Some observatonal studies suggested possible involvement of serum microRNAs in PCOS. Austrian investgators now started to expand on these observatons by testng serum expression of miR-23a-3p and miR-425-5p in the classical Roterdam phenotypes of PCOS (A, B, C, D).3
As is ofen the case in PCOS studies the patent populaton was quite young (for all patents 27.78 ± 3.69 years). Among individual phenotypes, B was the oldest (mean 25.09 years) and A the youngest (mean 26.42 years) and – interestngly – control patents were the oldest of them all (29.15 ± 3.57 years). This is very important because at least the D phenotype signifcantly changes with advancing age. At mean age of 27.51 years, it is expected to be in normal androgen range, demonstrate a normal, regular menstrual patern, and stll be normally fertle, as D phenotypes become hypo-androgenic and infertle usually only afer approximately age 35.4
Unsurprisingly, the D phenotype, however, already had even lower mean DHEA than controls (1.2 vs. 1.37ug/mL), while classical PCOS phenotype A demonstrated the by far highest levels at 23.33 ug/mL. Similarly, the D phenotype also demonstrated the lowest free and total testosterone levels among all PCOS phenotypes, though mildly higher ones than control patents. The study, therefore, does something unfortunately only very few PCOS studies in the literature usually do: it investgated the diferent phenotypes of PCOS separately, for which it deserves special recogniton. Unfortunately, however, the study was underpowered and, therefore, really failed to ofer useful results.
For example, the authors report that the serum expression of miR-23a-3p was upregulated in phenotype B and discriminated it from phenotype s B, C, and D at a signifcance of P<0.006, but the conclusion was reached on only 10 phenotype As and only 11 Bs, Cs, and Ds, respectvely, without apparently controlling for age. The expression of miR-425-5p was downregulated in phenotype C (with only 11 study subjects) and was alleged to discriminate it from the other three phenotypes (again apparently without age adjustments). Likely the one fnding of some statstcal value was the downregulaton of MiR-9305p in all PCOS phenotypes (n=42) versus controls which again only included 8 individuals. In short, a valiant atempt but with very inadequate executon and, therefore, no real progress in our understanding of PCOS.
EXTRACELLULAR VESICLES in PCOS and ENDOMETRIOSIS: And then there is one more review artcle worth mentoning
which addresses a currently very popular subject in medicine in general, so-called extracellular vesicles (ECVs, and their content) which now are reported practcally everywhere in the body, appear to have important functons in communicatng between cells, and have been reported as altered in PCOS and endometriosis. Canadian investgators from Toronto published this review in the Journal of Ovarian Research
ECVs, including exosomes and microvesicles, have been reported in follicular fuid and in tubal fuids. The review included nine PCOS studies, with 2 miRNAs being identfed in PCOS, miR-379 and miR-200.
Because of their presence in tubal fuid, they are suspected of playing a role in embryo maturaton, as the fertlized egg descends through the tube toward the endometrial cavity while developing to a blastocyst. Because of their suspected impact on embryo growth and development, studies are underway in several laboratories, considering vesicle content for use in in vitro embryo culture.
In the same paper, the authors also look at the efects of extracellular vesicles in endometriosis: Here the paper notes that peritoneal fuid in endometriosis patents contains molecules that modulate the immune response and -actually – support establishment and maintenance of endometriosis. Having reviewed 11 endometriosis studies, the authors were, however, unable to elucidate any observed paterns common to patents.
And, since we are already addressing endometriosis, some interestng news from the largest cardiology conference in the world (this is not a misprint), the European Society of Cardiology (ESC) Congress 2024 in London, UK, where investgators reported that women with endometriosis have a 20% greater risk of heart atacks and strokes than controls.
Women of average age 37.3 years were on average followed for a median of 16 years and a maximum of 45 years. Besides increased risk for myocardial infarctons and ischemic stroke, endometriosis women also demonstrated increased risk for cardiac arrhythmias and heart failure. A prior review artcle atributed such an associaton to systemic hormonal, pro-infammatory, pro-angiogenic, immunologic, and genetc pathways.7 As previously noted in these pages, the noton that endometriosis is a systemic rather than localized disease, frst propagated by Yale’s gaining increasing acceptance.
REFERENCES
1. Chen et al., Endocrine Rev 2024;45(4):437-459
2. Rosenfeld RL. Endocrine Rev 2024;45(4):553-592
3. Trummer et al., Int J Mol Sci 2024;25:3205
4. Gleicher et al., Biomedicines 2022;10(7):1505
5. Duval et al. J Ov Res 2024;17:160
6. Havers-Borgersen et al., European Society of Cardiology (ESC) Congress, London, England August 30-September 2, 2024
7. Marchandot et al., Eur Heart J Open 2022;2(1):oeac001 Corrigendum 4(1):oead137
8. Taylor et al., Lancet 2021;397(10276):839-852



… on lifespans of females with early menopause
That women outlive men by on average 5.8 years is by now well established. The gap has, indeed, been growing from 4.8 years in 2010. Now two investgators from Florida, using propensity score matching analysis, investgated sex diferences in all-cause mortality and life span between women undergoing premature menopause and men. Propensity scores matching analysis created matched cohorts of women and men using a 1:1 rato. The adjusted hazard rato (HR) values (95% CI) for women and men to survive to the 75th percentle of life span was not statstcally signifcantly diferent and there was no signifcant diference in the mean life span between deceased women and men in the matched cohorts. In a subgroup analysis, the mean life span did not difer signifcantly between deceased women taking hormone therapy and men. Life span of women never using hormone therapy was, however, signifcantly longer than that of men (78.3 ± 11.6 vs 76.6 ± 11.9 years, P = 0.0154).
There were at various levels interestng results: (i) Life span of women never using hormone therapy was signifcantly longer than that of men (78.3 ± 11.6 vs 76.6 ± 11.9 years, P = 0.0154), suggestng an adverse efect on female lifespan from hormone therap. (ii) Women experiencing premature menopause had lower risks of all-cause mortality than men, but the advantage that women had in terms of life span was lost, suggestng that women lose lifespan in associaton with early menopause.
REFERENCE
1. Xing Z, Kirby R.S. Menopause 2024. 31(10):p 887-896
… on sexual dysfunction in women
Not a commonly discussed subject in major general medical journals, it is worth mentoning that The New England Journal of Medicine did present the case of a 54-year-old woman with sexual dysfuncton in its weekly Clinical Practce case report and discussion.1 Because of its excellent discussion, we recommend this paper to anybody who wants to get an update on the subject.
REFERENCE
1. Davis SR. N Engl J Med 2024;391(8):736-745
… on Rapamycin, preventing cyclophosphamide-induced ovarian follicular loss and more
That certain chemotherapies induce abnormal actvaton and depleton of the pool of primordial follicles in ovaries is wellestablished. A breakthrough in understanding the process was achieved when it was discovered that cyclophosphamide induced follicle loss by actvatng the so-called rapamycin (mTOR) pathway and resultng in complete follicle burn out.1 Other investgators then built on this observaton and shortly thereafer reported that mTOR inhibitors exhibited a protectve efect against such follicle loss,2 a fnding several other groups have since confrmed. Now Japanese investgators atempted to elucidate these mechanisms in more detail in a mouse model. Reportng in Human Reproducton, 3 they demonstrated that daily administraton to mice or rapamycin together with a cyclic regimen of cyclophosphamide (sufciently potent as a single cancer drug against breast cancer in this model), suppressed cyclophosphamide-induced primordial follicle loss while also demonstratng an inhibitory efect against tumor proliferaton. The potental benefts of such an approach in breast cancer patents appear obvious and seem deserving of a clinical trial.
REFERENCES
1. Adhikari D, Liu K. Cell Cycle 2010;9:1673-1674
2. Goldman et al.; Proc Natl Acad Sci USA 2017;114:3186-3191
3. Tanaka et al., Hum Reprod 2024;39(7):1519-1532
… on the effects of gender-afrming testosterone treatment in trans men on the immune system
Females wishing to transiton routnely undergo gender-afrming hormone therapy with testosterone (trans men). An interestng study by Swedish investgators asked the queston of what this treatment does to their immune system. That this is an important queston is quite obvious, considering the rather profound diferences between female and male immune

systems, with infectous, infammatory, and autoimmune conditons, therefore, presentng quite diferently between the two sexes.
They longitudinally investgated 23 trans men in this study and found that testosterone modulates the immune system through a cross-regulated axis between type-I interferon and tumor necrosis factor. This is, of course, a discovery that is relevant for cis populatons as well, as it adds important new knowledge to our understanding of why female and male immune systems difer so signifcantly.
REFERENCE
1. Lakshmikanth et al., Nature 2024;633:155-164
2.
… on postmenopausal vulvovaginal symptoms.
Interestngly, out of all medical journals, it was the Annals of Internal Medicine which recently dedicated two review papers to what is widely called the genitourinary syndrome of menopause, which includes vulvovaginal complaints (dryness, irritaton, pruritus), urinary symptoms (urgency, frequency, dysuria, repeat infectons), and symptoms related to sexual intercourse (dyspareunia, poor libido, arousal difcultes, and failure to reach orgasm).
The frst systematc review found that most studies in the literature were too small to allow for meaningful results and, therefore, did not ofer any meaningful results. The other review suggested that vaginal estrogen, vaginal DHEA, oral ospemifene, and vaginal moisturizers improve some symptoms in the short term, but long-term data are really missing. In short, really not very much evidence that anything really works.
REFERENCES
1. Ullman et al., Ann Int Med 2024; htps://doi.org/10.7326/ANNALS-24-00603; ahead of print.
2. Danan et al., Ann Int Med 2024; htps://doi.org/10.7326/ANNALS-24-00610; ahead of print.
… on innovative ovarian cancer treatments
So-called homologous recombinaton defciency (HRD) is frequent in cancers and is a major reason of genomic instability and aneuploidy of cancer cells. It can be found in ca. 50% of ovarian cancers. Investgatng over 100 high grade serous ovarian cancer samples, neoadjuvant monotherapy with the PARP inhibitor niraparib achieved impressive response rates. Efector regulatory T cells (eTregs) were identfed as key responders to HRD and neoadjuvant therapies, co-occurring with other T cells reactve to tumor, especially exhausted CD8+ T cells. Moreover, interferon signaling correlated with cancer cells upregulatng MHC class II and co-inhibitory ligands, potentally driving Treg and CD8+ cells fates. In a mouse model, depletng eTregs with or without PARP inhibiton (a PARP inhibitor is a substance that blocks an enzyme in cells called PARP which helps DNA repair) suppressed tumor growth without toxicity. These fndings open the door to eTreg-focused therapied for ovarian cancer as well as other HRD-associated cancers.
REFERENCE
1. Luo et al., Cell 2024;187:4905-4925

INFECTIOUS DISEASES
And the COVID story continues
Even though the COVID pandemic is over, COVID news is as prevalent as ever and afects several important issues. One of the clearly dominating subjects is long COVID, recently well-summarized in a Review artcle in Nature Medicine 1 The artcle describes long COVID as a “complex, multsystem disorder that can afect nearly every organ system and can be severely disabling.” It is believed to afect globally ca. 400 million people and to have an economic impact of ca. $1 trillion, representng approximately 1% of the world’s economy. The conditon does not appear to have a single cause but – more likely – involves several possibilites and/or hypotheses, startng with viral persistence, immune dysregulaton, endothelial infammaton, and microbiome dysbiosis. A recent NIH study of over 10,000 patents from 83 clinic sites fell short in fnding diferences in laboratory parameters between patents with long COVID and those who had regular short COVID.2
A concern expressed by several authors in several papers, among those one in The New England Journal of Medicine, 3 decried that we have not learned the right lessons from the COVID pandemic. Concerns arise especially because of how the spread of the H5N1 avian fu infuenza virus is handled (more on H5N1 later).
Though the COVID pandemic is over, the virus has established itself endemic all around the world, which means that we can expect to experience waves of the disease for the foreseeable future. We just went through such a wave in the later part of the summer and the next one is expected in late fall, more or less in parallel to the annual fu
wave at that tme of the year.
Here in the US, the CDC stll tracks the SARS-CoV-2 virus through multple data collecton systems, among those the Natonal SARS-CoV-2 Genomic Surveillance System, the Natonal Wastewater Surveillance System, and the Traveler-based SARS-CoV-2 Genomic Surveillance Program.4
On a more positve note, COVID vaccines do apparently not raise the risks for congenital anomalies in ofspring.5 This conclusion was reached using Scandinavian data on almost 350,000 children. And as a reminder, if you are pregnant or planning on being pregnant (i.e., if you are in fertlity treatments) we strongly recommend you take a COVID booster shot. It reduces severity of disease in pregnancy (which is higher than in the non-pregnant state) and it also protects the newborn.
MULTISYSTEM INFLAMMATORY
SYNDROME IN CHILDREN is a severe, post-SARS-CoV-2 infecton sequela in children where the pathophysiology of the conditon was unclear. Now in a multcenter efort of US investgators, the problem has been solved: As it turned out, afected children develop a characteristc immune response to the viruses’ nucleocapsid protein which, due to molecular mimicry, appears to cross-react with the self-protein SNX8, thereby explaining the range of possible post-infectous autoinfammatory diseases seen with this infecton.6
REFERENCES
1. Al-Aly et al., Nat Med 2024;30:21482164
2. Erlandson, et al., Ann Int Med 2024;177(9): DOI: 10.7326/M24-0737
3. Sinha et al., N. Engl J Med 2024;391(6(:481486
4. CDC. https://www.cdc.gov/covid/ php/variants/index.html
5. Peluchon R. Medscape Medical News. August 26, 2024. https://www. medscape.com/viewarticle/covidvaccine-does-not-raise-risk-congenital-anomalies-2024a1000fj
6. Bodansky et al., Nature 2024;632:622-629
And let’s not forget the fu
As already noted above, fu season is just around the corner, and if you have not goten your fu shot yet, we have the vaccine available at the CHR. As with the COVID booster the fu vaccine is recommended for women already pregnant or planning on pregnancies (therefore including women in fertlity treatments). It reduces the woman’s and her ofspring’s risk from getng the fu.
A large recent study in JAMA Network Open confrmed the safety of seasonal fu vaccines over two successive pregnancies and reemphasized it use in pregnant women.1
And then let’s not forget the bird fu or beter called the bovine H5N1 infuenza virus. The number of reported cases in humans is increasing. Though most can be traced to bovine contacts, there also have already been a small number of cases where human to human infecton may have occurred. A recent artcle in Nature magazine, moreover, demonstrated that the currently very widely distributed bovine HPAI H5N1 virus possesses features that may facilitate infecton and transmission in mammals which includes us humans.
REFERENCE
1. Getahun et al., JAMA Network Open 2024;7(9):e2434857

THE IMMUNE SYSTEM IN REPRODUCTION
The relevance of adjuvants for vaccines
Adjuvants are supposed to boost the adaptve immune response. The process by which a vaccine enhances immunity against infectous agents or other diseases is complex and involves many diferent cell types. A recent preprint – CAUTION PREPRINT – tried to inform on these processes. The Chinese investgators demonstrated in a mouse model a potental mechanism by which adjuvants impact the exogenous peptde repertoire presented by MHC II molecules.1
A commentary then noted that by altering which peptde antgens are presented to CD4+ T cells, adjuvants afect the specifcity of the immune response.2
REFERENCES
1. Li et al., eLife , July 16, 2024. Reviewed reprint. https:// elifesciences.org/reviewed-preprint/99173
2. Rapaka RR. eLife August 13, 2024. https://elifesciences. org/articles/101259?utm_source=content_alert&... um=email&utm_content=fulltext&utm_campaign=14August-24-elife-alert
Progress in autoimmune diseases
EULAR 2024 (European Alliance of Associatons for Rheumatology), which this year took place in Vienna, Austria, promised interestng and very welcome new developments regarding the treatment of several major autoimmune diseases ofen seen in women during reproductve years. Systemic lupus erythematosus (SLE) is one very good example. Apparently at least 17 phase-2, and 14 phase-3 trials are expected to start in the near future, including B-cell-targetng agents, plasma cell-targetng agents, and drugs with novel mechanisms of acton.
A very “hot” issue for many autoimmune diseases at the conference were treatments with CAR-T cell therapy, and not only in SLE. A recent paper in Cell, for example, reported on three patents who received CR-T therapy for severe myosits and systemic sclerosis.2 Healthy-donorderive CD19-targetng CART cells were engineered using CRISPR-Cas9 to address immune rejecton and infused into the three patents. Infused cells persisted for over three months. Complete B cell depleton was achieved within two weeks. A 6-months follow-up, patents went into deep remission, without complicatons (like cytokine storm). The patents also demonstrated reversal of infammaton
and fbrosis. These preliminary results suggested that this treatment—introduced to human practce of course in oncology—appears relatve safe and strong immune modulatory efects.
Maybe most importantly, the study suggests that the cells for CAR-T treatment no longer must be autologous but that they could be ordered “of the shelf.” What this also starts to suggest that such treatment may also be used during pregnancy.
Going to another promising treatment, it is important to return the discussion to CD4+FOXP3+ regulatory T cells (Tregs) which are known to play a central functon in preventng autoimmunity. When they dysfuncton, autoimmunity can occur but the molecular processes underlying this are unknown. And internatonal consortum of researchers now ofered some clarity: in multple sclerosis (MS) patents they looked for essental transcripton programs regulatng autoimmunity in these patents. What they found was an aberrant PRDM1-S/SGK1 axis which led to destabilizaton of forkhead box P3 (FOXP3) and Treg dysfuncton. And most interestngly, they also found this abnormal axis in other autoimmune diseases. Emergence of PRDM1-S and epigenetc priming of AP-1/RF may, thus, be a key driver of dysfunctonal Tregs leading to autoimmune diseases.3
Considering the close interconnectvity of autoimmunity and pregnancy (a state not only of considerable self-tolerance but also of allogeneic tolerance), one wonders what these fndings potentally may mean for pregnancy abnormalites driven by tolerance defects?
REFERENCES
1. Freeman S. Medscape Medical News. August 1, 2024. https:// www.medscape.com/viewarticle/multiple-investigationalapproaches-show-promise-treatment-2024a1000e5y
2. Wang et al., Cell 2024;187:4890-4904
3. Sumida et al., Sci Transl med 2024;16(762):eadp1720
At least some humans can fght (most) infections even in absence of tumor necrosis factor (TNF)
Here is one example for how science constantly ofers unexpected results, and we are talking about tumor necrosis factor (TNF), a key signaling molecule in our immune system (untl recently called TNF-alpha). In response to an antgen,

it is primarily produced by actvated macrophages and induces infammaton. It may boost a person’s immune response but may also cause cell necrosis and cell death.1 It is a so-called cytokine and, through a variety of mechanisms involving the regulaton of infammaton and cell death, protects many species from infectons.
And here is the paradox: Roughly 50 years ago, TNF was discovered in mice infected with mycobacterium, the microorganism causing tuberculosis.2 Considering TNF’s central role in fghtng infectons and its evolutonary conservaton, the widely held opinion has been that mutatons of the gene encoding TNF that eliminate its functon would prevent afected individuals from reaching adulthood. This conclusion was reached based on several animal models and the observaton that ant-TNF treatments which have become very popular in treatng chronic infammatory diseases are ofen complicated by life-threatening infectons, especially from Mycobacterium tuberculosis.3
Now, however, a very large internatonal consortum of investgators reports on two patents (cousins) who lack all TNF actvity, are surprisingly healthy, which means that they are able to prevent most infectons, but are susceptble to tuberculosis.4 Gene-expression analyses and other studies of the two individuals revealed nothing unusual in regarding their immune cells, or gene-expression profles in absence of tuberculosis. They, indeed, responded completely normal to other cytokines.
Those are, of course, fascinatng fndings which – as always in science – raise many more questons. The principal one, of course, is why are these two cousins immunologically competent against all other infectous agents (the study suggested that there may be also mildly diminished protecton against Listeria monocytogenes)? Discovering what kind of redundancies may be efectve in protectng these two cousins from other infectons in complete absence of a TNF response would, of course, allow the development of new ant-infectous treatments, a very urgent need at a tme of ever-increasing drug resistance to available treatments.
REFERENCES
1. National Cancer Institute. https://www.cancer.gov/ publications/dictionaries/cancer-terms/def/tumor-necrosisfactor
2. Carswell et al., Proc Natl Acad sci USA 1975;72:3666-3670
3. Pyle CJ, Tobin DM. Nature 2024;633:293-294
4. Arias et al., Nature 2024;633:417-425
Some good news regarding recurrent
or refractory chronic graft-versushost disease (GvHD) and why it may matter for reproductive medicine
Chronic graf-versus-host disease (cGvHD) is a very frequent complicaton of allogeneic hematopoietc stem cell transplantaton, the only curatve treatment for bone marrow failure. The pathophysiology is based on infused allogeneic stem cells viewing the recipients cells as a threat and start atacking them. The clinical presentaton of cGvHD mimics an autoimmune-like infammatory disease, afects 50% of long-term bone marrow transplant patents, and is fatal in 20-40% of cases.1 First line treatment is stll high dose systemic cortcosteroids, but several biologicals are also increasingly used, as is the mammalian target of rapamycin (mTOR) and other drugs. No standard secondline treatment has, however, so-far been established.2
Both acute and chronic GvHD result from an inital insult that triggers an exaggerated infammatory cascade of events, with frst symptoms usually involving the skin and oral mucosa in the form of a maculopapular rash.3 Because such rashes also occur in pregnancy – especially in the third trimester – the specter that pregnancy may be complicated by GvHD-like conditons has been raised.
More specifcally, acute GvHD can occur in neonates as consequence of a maternal-fetal and in mothers due to fetal-maternal transplacental transfusions during pregnancy and can develop into cGvHD if going unrecognized. This –of course – should not surprise because the fetal-placental unit is during normal pregnancy a seemingly well-tolerated semi-allograf (and full allograf in cases of egg donaton or gestatonal-carrier pregnancies) within the maternal environment, untl it no longer is well-tolerated.
That a recent paper in The New England Journal of Medicine, therefore, recently reported that a drug, called Axatlimab, is quite successful in treatng recurrent or refractory cGvHD4 is, therefore, of interest for reproductve medicine. It is well known that colony-stmulatng factor 1 receptor (CSF1R) – dependent monocytes and macrophages are essental mediators of cGvHD. Axatlimab is a CSF1R-blocking antbody.
REFERENCES
1. Berger et al., Bone Marrow Transplant 2008;42(suppl 2):S101-S105
2. Shiratori et al., Int J Hemat 2024. https://doi.org/10.1007/ s12185-024-03850-9
3. Ramachandran et al., Dermatol Clin 2019;37(4):569-582
4. Wolf et al., N Engl J Med 2024;391:1002-1014
Basic science research
A refreshing new look at men and mice
One can hardly fnd a beter introductory artcle for this secton of our monthly medical literature review than here discussed artcle in Cell1 because it is not a scientfc report or even a review; it instead tells the personal story of one scientsts, Brian S. Kim, MD, Vice Chair of Research in the Department of Dermatology at Icahn School of Medicine at Mount Sinai, here in NYC (he has 4 additonal insttutonal appointments). And the artcle is not only inspiratonal, but describes why the pursuit of research, if

done correctly, can be one of the most rewarding professions in our crazy world. Lacking the space to go into detail, we can only recommend this artcle for its essental insights and quote the author’s own words:
“In defying conventonal views that dismissed ‘itch’ as trivial, I persisted in studying basophils and ILC2s in human skin and atopic dermatts. May research on JAK inhibitors for itch ultmately led to FDA- approved drugs. This is my story of disregarding categories and defnitons – a story about an unconventonal path in science that emphasizes innovaton over conformity.”
Finding out that a mouse model did not correctly refect the human reality since phenotypes did not match and that he even had no clear hypothesis, he came to the “bitng conclusion” that humans are unreliable models of mouse disease (a point ofen also missed in reverse), he nevertheless contnued:
“Stubborn persistence to keep delving into this biology, even in the face of confusion, dogma, and misfortune, informed a new area of neuroimmunology (a new feld for him) borne out of a study in a few patents with an inborn error of immunity.”
We applaud his career approach not only because it led to remarkable achievements, but also because it mimics the CHR’s approach to research especially over the last 20 years that allowed a relatvely small, private and independent fertlity center like the CHR to repeatedly produce practcechanging research in the fertlity feld, ofen rather viciously atacked by opposing voices representatve of “common wisdom,” erroneously dominatng practce.
REFERENCE
1. Kim BS. Cell 2024;187:4815-4817
The value of embryo models

In this case natural (right) and synthetc (lef) mouse embryos side by side to show comparable brain and beatng heart formaton. Image credit: Amadei and Handford. Laboratory credit: Magdalena Zernicka Goetz, et al., Cambridge University, UK, Department of Physiology. htps://www.cam.ac.uk/stories/model-embryo-from-stem-cells
Under the argument that there aren’t enough human embryos available for reproductve biology research, reproductve biology is awash in artfcial embryo models produced from stem cells. Now comes Prof. Dr. Guido Pennings, Professor of Ethics and Bioethics at
Brian S. Kim, MD
Ghent University in Belgium, who argues that that this overwhelming interest in what he calls embryo-likestructures is largely based on two misconceptons: the belief that there is a shortage of available human research embryos and the further belief that such research would make research on natural embryos redundant.1
We believe he is mistaken!
Just as it is by now quite well established that “mice are not men,” we see no evidence in the literature that any of the authors who have published artfcial embryo models would really advocate that these models are meant to replace research on natural human embryos. Like animal models, they are meant to establish background, which then allows to skip preliminary investgatons in human embryos and, by doing so, gives human embryos the special consideraton the worldwide science community agrees they deserve, among other criteria defned by using as few human embryos as possible for every experiment.2 Coming from an ethicist, this is an unexpected opinion!
REFERENCES
1. Pennings G. Reprod Biomed Online 2024;48(6):103886
2. Ethics Commitee of the ASRM. Fertl Steril 2020;113(2):270294
The frst human organoids with an immune compartment
Before there were artfcial human embryos, there were organoids originatng from adult stem cells. They are, however, basically only epithelial structures, while organs are multlayered and multcompartmental, also including— among others—immune cells which, of course, play crucially important roles. Now Swiss investgators reported a frst intestnal immune-organoid which allowed them to identfy the Rho pathway as a new target for mitgaton of immunotherapy-associated intestnal infammaton. The authors correctly concluded that such models could be used to study tssue-resident immune responses in the context of tumorigenesis, infectous diseases, and autoimmune diseases. Interestngly, they forgot to menton what, at least for reproductve biology, is likely, the most interestng applicaton: embryo implantaton in the endometrium, which for far too long has been viewed as an endocrine process, while—as we discussed in the VOICE a few months ago—it really should be viewed as an immunological process.
REFERENCE
1. Recaldin et al., Nature 2024;633:165173
Lineage segregation in the mammalian preimplantation-stage embryo
The subject of lineage segregaton in preimplantaton stage embryos has been very well elucidated over the last decade in basic science journal but has found litle atenton in more clinical journals in the feld. A review artcle updatng the subject in Human Reproducton can, therefore, be viewed as tmely, even though it does not contribute new informaton for the already educated reader.1
Unfortunately, the artcle completely omits a discussion of the diferences between embryonic and extraembryonic cell lineages in their respectve abilites to self-correct from aneuploid cells. Since this is a subject repeatedly discussed in recent months in these pages, we do not want to be repettve but since the diference in self-correctng ability is a very important point in the stll raging discussion about the clinical utlizaton of preimplantaton genetc testng for aneuploidy (PGT-A), this is an almost inexcusable shortcoming, which characterizes this artcle as a bit too superfcial for basic scientsts and devoid of what likely is the most important relevance of the addressed subject for clinicians.
REFERENCE
1. Skory RM. Hum Reprod 2024;39(9):1889-1898
At least in the mouse, embryonic genome instability may happen in waves
We are delighted to present another interestng paper by Japanese colleagues regarding preimplantatonstage embryos. At least in a mouse model, they recently demonstrated in a paper published in Nature magazine that at 1- and 2-cell stage embryos lacked a replicaton tming program for DNA, with the complete genome replicatng slowly through slow-moving replicaton forks. Such a program, however, started abruptly somatc-cell-like, though with stll slow fork speed, extended S phase, and appearance of markers of replicaton stress, DNA damage as well as repair. Especially during the 4- to 8-cell division breakpoints became enriched in late replicaton regions, with errors rescued by nucleoside supplementaton, which accelerated fork speed and reduced replicaton stress. By 8-cell stage forks had gained speed, S-phase was of normal length, and chromosome aberratons decreased again.1
Why another Japanese study that was just published demonstrated the process to be more gradual,2 remained unexplained.
REFERENCES
1. Takahashi et al., Nature 2024;633:686-694
2. Nakatani et al., Nature 2024; 625:401-404
Rejuvenating aged oocytes through exposure to a young follicular microenvironment?
It is these days, unfortunately, quite popular for many IVF clinic to advertse ovarian “rejuvenaton” procedures. What is referred to in most cases, is the injecton of platelet-rich plasma (PRP) into ovaries, something we would not call a rejuvenaton process; but that to a degree is semantcs. But now come Chinese investgators who claim to have really found the “fountain of youth”—at least in a mouse model—in a very simple experiment. They took “old” eggs from follicles of older females and, basically, exchanged the follicles for follicles from younger females. In other words, they gave older eggs the environmental support of younger eggs and—lo and behold—those older eggs were signifcantly improved in maturaton rates, blastocyst formaton, and live births afer IVF. Moreover, this “rejuvenaton” was also associated with enhanced interacton with somatc cells, transcriptomic and metabolomic remodeling, improved mitochondrial functon, and higher fdelity of meiotc chromosome segregaton. A switch into the opposite directon—placing younger oocytes into older follicles—had the opposite efects.
If confrmed—and especially if confrmed in humans— this, as the authors note, opens the door for future somatc follicular cell-based therapy for age-based female infertlity. But there is more to these results if confrmed: likely the most important conclusion then would be that oocytes at restng stage do not age afer all. This was before suggested, mostly based on the fact that primordial follicles before recruitment show almost no metabolic actvity. The suggeston made then, was similar to what here reviewed paper suggests, namely that what ages as women get older is the somatc microenvironments in the ovary in which follicles mature following recruitment out of restng stage in primordial follicles. If confrmed, indeed, a very excitng fndings that may really allow rejuvenaton of ovarian functon in older women.
REFERENCE
1. Wang et al., Nat Aging 2024;4:1194-1210
Human stem cells in regenerative medicine
Related to the previous subject, a review of the increasing use of human stem cells in regeneratve medicine afectng many diferent medical specialtes was recently addressed in a Review artcle in The American Journal of Medicine. 1 the authors in this artcle noted that, “medicine now has the potental of improving many human diseases by introducing adult somatc stem cells that can repair and/or replace defectve or damaged tssue.” Though we feel that this statement is somewhat of an exaggeraton, it was to a degree mitgated by the authors also notng that these treatments are stll “in an early phase of development” and, therefore, must be introduced into clinical practce with maximal safety and only afer proper validaton.
Unfortunately, this is not happening in many medical felds, reproductve medicine included. Adult stem cells are already injected into ovaries without – to the best of our knowledge – any safety studies in animal models ever performed. The ovaries are a highly cancerogenous organ and must be treated with great cauton. We, therefore, as of this moment would cauton women against allowing stem cell injectons into their ovaries.
REFERENCE
1. Goetzl et al., Am J Med 2024;137:805-809

ADVERTISEMENT


