We welcome all of our readers to the March issue of The CHR VOICE, which, as usual, in the new and expanded format offers a broad potpourri of articles for patients and laypeople as well as professional physicians and scientists working in reproductive medicine and biology. Due to so many interesting papers with relevance to reproductive biology and medicine being published in February, our literature review section will, indeed, be even more exhaustive than usual.
With an over 35% opening rate and an average reading time of eight minutes for the February issue, the response to our new format for The VOICE has been nothing but spectacular. As marketing experts will attest, both of these numbers are beyond expectations. That the new format of The VOICE appears timely and seems to satisfy a strong demand in the community is not only demonstrated by the above-noted marketing statistics but also by the number of individual responses we are receiving from readers, suggesting colleagues to be placed on the mailing list for The VOICE, commenting on articles, or even ordering the print version of the newsletter that for the first time became available with the February issue. To re-emphasize, the marketing and distribution team can be reached by sending an e-mail to arata@thechr.com.
Topics discussed in this issue of The VOICE are shared risk programs offered by IVF centers and other corporate entities, chromosome genotypes that, as is now increasingly understood, are not as “fixed for life” as was believed in the past, and ethical issues in reproductive medicine that are increasingly surfacing (March is National Ethics Awareness Month). As always, we have also selected a few questions we recently received from the public regarding “needle-free IVF” and surrogacy (gestational carriers), as well as human excessive embryos donated for research, so-called “compassionate” embryo transfers, and the increasing use of antioxidants, especially, CoQ10. Moreover, The CHR’s Norbert Gleicher, MD, additionally contributes his monthly column, “A Piece of My Mind.”
Suffice it to say, the above already-noted literature review this month is unusually broad, covering a wide section of subjects, though, remarkably, this month did not find any articles for the by now rather infamous “Real Bad Paper Section,” – clearly a positive finding reflective of the fact that this section is meant to present the most interesting papers in the literature potentially relating to reproductive medicine, whether in the good or bad.
We hope you will enjoy the March issue!
The Editorial Staff of the CHR VOICE• The CHR, as of 2/13/23 has modified prior COVID-19 rules, as here defined.
• There no longer exists a universal masking requirement for either staff or patients, A masking requirement, however, continues until further notice for the following exceptions:
- All individuals, whether staff or patients who access The CHR’s facility, with even minimal upper respiratory tract symptoms and/or fever, even if COVID-19 and/or Influenza testing was negative.

- Individuals, whether staff or patients, with positive COVID-19 and/or Influenza testing, are still pro hibited from access to The CHR, unless and/or until such access is granted by The CHR’s Medical Director and/or designee.
- Children under age 16.
- We will allow only one accompanying person per patient.
- When in doubt about one’s status, contact The CHR before coming to The CHR by calling the main line at 212-994 4400, and you will be advised of your status at The CHR after consultation with The Medical Director and/or designee.
• Upon patient request, the CHR once again offers face-to-face in-office consultations with physicians, though teleconsultation will remain routine.
• The CHR, still, strongly recommends full vaccination against COVID-19 as well as Influenza for all CHR staff and all patients trying to conceive.
• The CHR welcomes all staff members and patients who, still, wish to continue wearing face masks while in the facilities of The CHR.
• Health and well-being of our patients and members of the CHR community and all of their families remain our top priority. We will continue to monitor local transmission levels — especially as we approach the end of respiratory virus season in the spring — and will share news should our requirements change in the future. All decisions will be made in line with guidance from professional organizations as well as state and federal agencies.
Norbert Gleicher, MD Medical Director February 13, 2023As so-called “shared risk programs” in IVF are proliferating, offered by some IVF centers directly but, increasingly also by independent finance companies, the time appears right to provide some transparency to this practice. Google describes the process as IVF clinics and/or financial agencies “sharing the financial risk for unsuccessful IVF cycles” (sic, therefore the term “shared risk” program). Yet, such programs share risks with you, the patients, only in the same sense as your car insurance shares the risks with you for having a car accident or your health insurance shares with you the risk of getting sick. In reality, insurances do not “share” risk; they “insure” against risks, in this case, the IVF center or finance company insured you against the risk of not conceiving in several IVF cycles, - dependent on the shared risk program you choose. Also, like insurance contracts, these shared risk contracts are the results of carefully developed actuarial financial models, developed with only one goal in mind, - making money for the commercial entity that offers these plans. IVF centers and/or financial companies offering shared risk programs are not benevolent not-for-profits; like in all insurance businesses, their principal goal is to make a good profit for their investors.
By subscribing to a shared risk program, a patient, therefore, is still paying the IVF center’s regular fees (or at least close to it). In addition, however, a second commercial entity, whether the IVF center itself or an unrelated finance company, must make additional profit. That fact alone already demonstrates that the zero-sum game does not favor the patient who, either as an individual or as part of a larger community, ends up paying the bill not only for the IVF cycle but also for the additional profit of whoever covers the shared risk.
In practical terms, this means that assuming infertility patients do not have coverage through medical insurance that also includes IVF, they have two options: The still most common is to pay the fees for the needed IVF cycle out of pocket. The alternative is to join a shared risk program. In making this choice, the first important point to understand is what it really means to select a shared risk program:
(1) A commitment to one vs. multiple IVF cycles: When infertility patients for the first time are advised that their treatment should be IVF, many are understandably hesitant. To be at that point asked to commit to more than one cycle, therefore, may not only be unexpected but, for several reasons, in The CHR’s opinion inappropriate: The CHR, therefore, usually recommends against signing multiple cycle package commitments or shared risk cycle commitments before a first cycle has been completed.
The CHR views a first IVF cycle as a crucially important additional diagnostic test that almost always reveals new information about patients that, simply, cannot be gleaned otherwise. Unless a center plans to rigidly follow the one same protocol, whatever a cycle reveals, the CHR’s physicians before a first cycle, therefore, often simply do not feel to be in a position to assess well what a patient’s longer-term pregnancy chances may be and what number of IVF cycles, therefore, may be required.
(2) Paying IVF market costs or paying market costs plus insurance costs: If a woman conceives in her 1st IVF cycle, her costs in an out-of-pocket payment will always be significantly lower than her costs (even after partial refunds) after joining a shared risk program. The reasons are obvious: The woman who paid cash and conceived in her cycle paid for only one cycle. Everyone in a shared risk program paid a significant additional premium which the insurer partially uses to pay for additional cycles of women in the shared risk program who did not conceive. Most shared risk programs balance costs out for patients after approximately two cycles. In a third cycle, a shared risk patient may already be mildly ahead in comparison to having paid for three cycles out-of-pocket; and by a fourth cycle, the shared risk patient will be financially clearly ahead.
(3) You may not even be eligible for a shared risk program: Shared risk programs are usually highly selective in who is eligible to join and/or significantly increase participating costs for poorer prognosis patients. Once again, the analogy to other insurance contracts is obvious: No insurance company will, for example, insure an individual already diagnosed with cancer; or a 45-year-old with heart disease will have to pay a much higher premium than a 45-year-old without.
Continued on page 6
Continued from page 5
(4) How do you know you will like your infertility center long enough to go there through repeated cycles: It is an almost daily occurrence at The CHR that new patients, after a consultation, tell us how much they would switch to our center, - but that they have still one or two cycles in their prepaid shared risk package, from which they cannot escape.
(5) Be aware of extra charges: Even for infertility patients with insurance coverage, many widely used so-called “add-ons” to IVF are not covered by insurance and therefore, are often excluded from shared risk programs. If patients want one of those treatments in a shared risk cycle, they end up paying for those extra. The most widely such “add-on” is, of course, preimplantation genetic testing for aneuploidy (PGT-A), an often-covered subject in this newsletter. Such charges can be significant and, often, also are not included in refunds that patients receive who have not conceived upon completion of a predetermined number of cycles under the shared risk agreement. Many other charges can also apply.
Offering a succinct summary, a nurse not too long ago summarized the pros and cons of shared risk programs as shown in the table below.1
- UNUSUAL PARTIAL REFUND IN IVF
- MAINTAINS ADOPTION OPTION
FINANCIALLY
- “PEACE OF MIND”
- FEWER TREATMENT DROPOUTS
- RESTRICTED ACCESS TO BETTER PROGNOSIS PATIENTS ONLY
- EXCESSIVE COST WITH QUICK CONCEPTION
- ADDITIONAL FUNDS MAY BE NEEDED
- CONTRACTS MAY BE FULFILLED EVEN IF PREGNANCY IS MISCARRIED
However, what is rarely discussed in the literature and in patient counseling are the incentives created by these programs and when they are brought up, they, unfortunately, are often misrepresented. One for example, in many advertisements, is given the impression that a shared risk program creates strong economic incentives for IVF centers to produce good pregnancy and live birth rates since the fewer services they have to provide, (i.e., the quicker in a multiple-cycle commitment a patient conceived) the more profitable will this patient be.
Though on first impression, a seemingly logical conclusion, in reality, the incentives may go in exactly the opposite direction. Since IVF centers base their pricing for all packages on their past outcome experiences, if anything, multiple cycle packages encourage repeat protocols and disincentivize individualization of care. Patients coming to The CHR from programs with large numbers of shared risk cycles, therefore, almost uniformly complain about just having gone through cycle after cycle without barely any changes.
Those centers also regularly revisit actuary tables and if outcomes have declined, they simply adjust their fee structure accordingly. Although not formally investigated so far, it would not surprise if this fact has also been contributing to the declining live birth rates in autologous IVF cycles in the U.S.
Finally, shared risk programs are also increasingly offered in egg-donation cycles. Indeed, donor-egg banks have gotten into the business of offering them in collaboration with several fertility centers (some egg banks, indeed, share ownership with several IVF centers). All of this, of course, creates additional potential financial conflicts patients must be aware of. Moreover, donor-recipient cycles are supposed to have the highest pregnancy and live birth rates among all IVF cycle types by far. Shared risk programs involving young donor eggs, therefore, should be the least expensive shared risk cycles. However, that is surprisingly not what the market in general demonstrates.
1. Gurevich R. https://www.verywellfamily.com/what-are-ivf-refund-or-shared-risk-programs-1960050
The CHR is looking for another senior board-certified RE-I (or international equivalent) to join our growing national and international practice. Though private, our center is organized along academic principles in that physicians are expected to excel not only as clinicians but also as researchers. The center’s uniquely structured compensation package, therefore, incentivizes both activities. We are looking for an individual with documented excellence in both areas, commensurate with associate professor/professor level. Besides a competitive salary, incentive bonus structure, and excellent benefit package, the CHR also offers partnership along either a 3-year or 5-year equity track and, ultimately, part or complete ownership, as the current leadership is expected to retire within that time-period.
If you feel qualified for the position and share our philosophy of being a physician-scientist, please let us know by submitting your C.V. and a brief letter of interest to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position can be filled immediately. All submissions are considered confidential.
If you failed in securing a formal fellowship position in RE & Infertility or simply want a change out of general OB/GYN practice, the CHR offers a fellowship position in RE-I which after 1 year will greatly improve competitiveness for a formal fellowship position and in 2 years establishes independent competence for establishing an infertility practice. The center’s last 1-year fellow was accepted into the NIH-fellowship program after failing to secure a position in the preceding year.


Qualified candidates must be OB/GY board-eligible or certified, be eligible for hospital privileges and for a New York state license to practice medicine. As CHR maintains a very active research program in affiliation with Rockefeller University, CHR fellows gain substantial research experience, with great likelihood resulting author- or co-authorships in peer-reviewed publications. Board eligible candidates who still must accumulate surgical cases will be given the opportunity to do so.
Chosen candidates will receive a very competitive salary and a generous benefit package, including health and malpractice insurance as well as paid vacation time. If you feel that you qualify and are interested in a career in RE & I, please submit your CV and a brief application letter to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available as of January 1, 2023. All submissions are considered confidential.
I just had my initial consultation with Dr. Norbert Gleicher last week. It went really well. He was very patient to answer all my questions and concerns. More importantly, he is digging deeper on my overall health to find out or exclude any health issues that prevents me from achieving my family expansion goal. That’s what I have been looking for. I believe in Dr. Gleicher, and I also believe with his help I will succeed in the near future. My confidence in him started me viewing all his Youtube videos. They are very helpful. I already liked him since then. Strongly recommend Dr. Gleicher to anyone who hasn’t found out the reasons and corresponding solutions. He provides customized plans, just for you! - YS

Besides his great expertise and high scientific knowledge, Dr. Barad is compassionate, kind, patient. He supported me in the worst moment of taking the decision to transfer my poor quality embryos on Day 3 holding my hand and genuinely caring for my wellbeing. Because of the pandemic, I had to wait a couple of years before being treated at CHR - I definitely recommend Dr. Barad and hope to get his advise also in the next future.
-BZ

Assessing a couple’s chromosomes, also called determining the karyotype of an individual through a blood draw, is almost a routine test in most infertility evaluations. And, like other genetic tests, this test is generally believed to be good for a lifetime: i.e., if done once, the result is good for ever and the test, therefore, does not have to be repeated. As with so many other things we have in the past gotten wrong about our genes here, too, we, however, viewed things in somewhat simplistic ways.
But let us start from the beginning. Normal human beings have 23 pairs of chromosomes, of which 22, the so-called autosomes, are always identical (i.e., we all have 22 identical pairs of chromosomes, numbers from #1 to #23, with each either coming from our mother or father. In addition, we all have two socalled sex-chromosomes, which in females are identical (XX) and in males differ (XY). A normal female, therefore, has a karyotype of 46, XX, while a normal male has a karyotype of 46, XY and, therefore, are considered “euploid.” A normal, euploid karyotype is, however, not universal. Indeed, abnormalities, diverting form normal 46, XX or 46, XY karyotypes, are surprisingly frequent and can take different directions: some individuals may have three in place of two copies of a chromosome (called a trisomy), others may be missing one chromosome from a pair (called a monosomy) if affecting autosomes. If sex chromosomes are numerically affected, it is called a sex chromosome abnormality and can also mean an extra sex chromosome (X or Y) or a missing sex chromosome ( a female, for example, may be missing one of her two X chromosomes, exhibiting an X0 karyotype called a Turner syndrome). In addition, chromosomes can have segmental abnormalities, usually either deletions or duplications. Segmental abnormalities are, indeed, quite frequent and, often, have no phenotypical or clinical meaning.
Once human chromosomes were discovered, a dogma evolved assuming that an individual’s karyotype is stable for life. In other words, once your karyotype has been established as normal -euploid, it will stay so for life. Obviously, that also applies to abnormalities; once diagnosed, they will be there forever. While these assumption in principle have been proven correct, it has also become obvious that DNA repair mechanisms decline in efficacy with advancing age, resulting in increasing numbers of somatic mutations in practically all tissues of the body.1
As patients with myelodysplastic syndrome, an age-dependentonco-hematologic disease, however, demonstrate numerical as well as structural changes in karyotypes can also
occur, including +8, +15, +17, +21, -X as well as polygenic clones.
Studies furthermore suggest that sex chromosomes undergo mosaic events more frequently than autosomes.3 That X chromosomes go missing with advancing female age should, therefore, not surprise. X0 (Turner syndrome) mosaicism, for example increases almost four-fold between ages 59 and 75, from 0.11% to 0.45%. Women with detectable X0 mosaicism also demonstrate an increased likelihood of harboring autosomal mosaicism.3 And autosomal mosaicisms have, of course, been associated with several solid malignancies and, indeed, have been suggested as possible early markers of disease.4
The subject of X0/XX mosaicism recently attracted The CHR’s attention when, within a few weeks, two new infertility patients on initial diagnostic work ups were reported to be X0/XX mosaics with high single digit percentages of X0 peripheral lymphocytes; yet their laboratory reports dismissed the mosaicism as “age-dependent” and, therefore, as clinically irrelevant. This was the first time we became aware of the fact that X0 mosaicisms may appear (and increase) with advancing age. Subsequently, searching the literature, it was disappointing to see how little has been published on the subject. It is somewhat reassuring that mosaic Turner syndrome appears to show reduced penetrance in adults.5
But at the same time the literature suggests that age-dependent mosaicism is usually at best in the low single digits, while both of The CHR’s patients’ mosaicism was clearly higher. Genetic laboratory guidelines do not even address the issue.6 Interestingly, a 2010 study in the European Journal of Endocrinology suggested that any Turner syndrome mosaicism over 6% was, likely, clinically significant.7 One then must wonder how genetic laboratories can just blow off the clinical significance of mosaicism above 6% as age-dependent and, therefore, clinically insignificant?
The CHR is on the outlook for more cases. Colleagues who have experienced similar reports from genetics laboratories, suggesting insignificant age-dependent Turner mosaicism, are encouraged to contact The CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD (ngleicher@thechr.com) if they are willing to contribute their cases to a registry for such patients
REFERENCES
1. Gorbunova et al., Nucleic Acids res 2007;35(22):7466-7474
2. Luiz Ribeiro et al., Sci rep 2021;11:2783
3. Machiella et al., Nat Commun 2016;7:11843
4. https://dceg.cancer.gov/news-events/news/2017/mosaicism-early-marker#:~:text=%E2%80%9CThese%20 studies%20provide%20evidence%20from,a%20risk%20factor%20for%20cancer
5. Tuke et al., Genet Med 2019;21(4):877-886
6. Wolff et al., Genet Med 2010;12(1):52-55
7. Homer et al., Europ J Endocrinol 2010;162(3):617-623

In a Viewpoint article published on January 30 online in JAMA, Donald M. Berwick, MD, MPP, from the Institute for Health Care Improvements in Boston, MA, penned a highly appropriate piece for the National Ethics Awareness Month under the title, “Salve Lucrum: The Existential Threat of Greed in US Health Care.”1 And this article says it all, unvarnished as things stand these days in all of medicine and, likely, nowhere more so than in reproductive
medicine: Greed has become an existential threat to the ethical practice of medicine.

The author chose “Salve Lucrum,” the Latin title of the article, after the slogan in the mosaic of an opulent house excavated at Pompeii buried under 16 feet of volcanic ash, which translates to, “Hail Profit” in order to reflect that “the grip of financial self-interest in US health care is becoming a stranglehold, with
dangerous and pervasive consequences, with no sector of health care being immune from the immoderate pursuit of profit, neither drug companies, nor insurers, nor hospitals, nor investors, nor physician practices.”
He, of course, is correct, that the whole U.S. system of medicine is evolving into rapidly growing monopolies with almost unlimited control over pricing and almost no concerns beyond the profit

motive. Insurers are getting bigger and bigger and, as repeatedly pointed out in recent months in these pages, are getting progressively more aggressive in reducing payments to physicians and, even more so, in directly, and without license, intervening in the practice of medicine by manipulating what services they cover or do not cover.
Hospital systems grow in parallel to be able to withstand payment pressures from insurers, in the process acquiring medical practices in their drawing areas to lock in referral patterns (even though directed referrals based on a profit motive in most states are considered illegal). Once part of a hospital system, the same office and the same physician charges are instantly increased because

repeatedly addressed in recent months in these pages, nothing is changing infertility practice as quickly and profoundly as the rapidly growing number of investor-owned fertility clinic networks. Now already mostly entering the second stage of acquisition of such practices, when the original founders of those centers either retire or retreat from management positions. This is when then new professional managers swoop in and cashflow and profitability become the dominant drivers of business. Investors usually work short-term schedules, requiring quick improvements in profitability to reach greatly improved evaluations when the asset is either sold off or taken public, often with no longer than a five-year horizon. Consequently, once professional man-
“add-ons” in this newsletter and in articles in the medical literature for years. Because of preimplantation genetic testing for aneuploidy’s (PGT-A’s) obvious negative impact on fertility treatments of so many women, no “add-on” has been subject to as many columns in The VOICE and in published articles than PGT-A, and it is pleasing to now notice that ethical, and not only the economic, dimensions of these developments are increasingly recognized and written about in the medical literature.3,4
With infertility practice increasingly becoming a multifaceted industry, involving not only infertility providers in their fertility centers but, horizontally and vertically integrated, also testing laboratories, pharma, and various manufac-
in-hospital charges are reimbursed at better rates than charges from freestanding private practice set-ups. Though, therefore, clearly not in the best interest of the general public since instantly raising medical costs, the process, nevertheless, is tolerated by government and, of course, further accelerates the rapid disappearance of private practice in the country because nobody can compete if the competition in hospital employment can charge and get reimbursed at significantly higher rates for the same services?
But, as noted above, the “salve lucrum” principle also applies to private practices, and this brings us from addressing issues relevant to all of medicine to specifically fertility-practice. As also
agement takes over, the initial “honeymoon” between buyer and “the bought” often ends.
It is also when clinical outcomes, once the principal criterion based on which IVF centers competed with each other, become less and less important and drift into the background, while maximum revenue generation becomes the priority. How else is the very rapid growth in utilization of IVF “add-ons” to IVF since approximately 2010 to be understood, considering that almost all have failed to demonstrate positive outcome effects on IVF.2
The CHR, of course, has been criticizing the increasing utilization of these
turers, all often representing cross-ownerships hidden from the public (or at least not transparently disclosed), we can only support Berwick’s conclusion that, ”health care providers need to become nosier about conflict between unchecked greed and the duty to heal.”
Several clinical practice patterns in the opinion of The CHR urgently require revisions, starting with the concept of third-party egg donation. We previously noted in these pages that The CHR does not understand why the infertility field does not perceive the need for egg donation as a “last-resort” treatment. The CHR, therefore, considers the need for egg donation a professional “failure” of current infertility treatments. To refuse
IVF treatment with autologous oocytes after ages 42-43 rather automatically, as is currently practice at many fertility centers, appears to us to represent age discrimination and to be unethical. Do not almost all women entering infertility treatments do so with the desire of not only biological but also genetic maternity?
But then there, of course, again come economic interests into play: Donor egg cycles are the most profitable IVF cycles for IVF centers and we, in addition, once again run into often undeclared other conflicts of interest like, for example, cross-ownerships of frozen egg-banks and IVF centers.
As previously repeatedly discussed in these pages as well, The CHR also does not support the trend of all-freeze cycles for everybody, which avoids all fresh embryo transfers. While that may be a more “practical” way to manage patients for IVF programs and add revenue through additional delayed thaw cycles, several excellent studies in recent months and years demonstrated beyond reasonable doubt that such an approach does not improve pregnancy chances, as

claimed by the original proponents of this “add-on.” It, indeed, just lengthens time to pregnancy and increases costs for the patient.5,6
But clearly the most unethical treatment pattern in IVF practice today is PGT-A in association with routine extended embryo culture to blastocyst-stage.7,8 That almost all IVF cycles in the US today utilize blastocyst-stage culture and, as of 2022, more than half involve PGT-A (including donor egg cycles using oocytes from young healthy females) is difficult to understand. The likely only remaining explanation why utilization of PGT-A still appears to increase in IVF clinics is a context several months ago suggested by an economist on Wall Street who suggested that, hypothetically assuming that PGT-A were to be outlawed by the Food and Drug Administration (FDA), up to a third of US IVF centers would have to close or at least restructure since all of their profitability is currently linked to PGT-A, as an “add-on” usually not covered by insurance, - even if IVF is otherwise covered. This additional cash income, therefore, significantly augments poorly reimbursed insurance-covered
IVF cycles for IVF centers. If there is anywhere in reproductive medicine a very obvious conflict between unchecked greed and the duty to heal, - it, therefore, can be found in the increasing utilization of PGT-A, resulting in non-use of huge numbers of perfectly fine human embryos on a daily basis and, therefore, not only not improving IVF outcomes but, actually, for many women causing significant harm to their chances of conceiving. If there exists an urgent ethical conundrum anywhere in reproductive medicine, then there is no better example than PGT-A!
1. Berwick DM. JAMA 2023; doi: 10.1001/ jama.2023.0846. Online ahead of print
2. Harper et al., Hum Reprod 2017;32:485-491.
3. Zemjarska MS. J Med Ethics 2019;45:346-350
4. Paes de Almeida et al., JBRA Assisted reprod 2022;26(3):371-373
5. Maheshwari et al., Hum Reprod 2022;37(3(:476-487
6. Wong et al., Cochrane Databse Syst rev 2017;3(3):CD011184
7. Gleicher et al., Nat Med 2022;28(3):442-444
8. Gleicher N. Trends Mol Med 2021;27(8):731-742
The CHR is looking for another senior board-certified RE-I (or international equivalent) to join our growing national and international practice. Though private, our center is organized along academic principles in that physicians are expected to excel not only as clinicians but also as researchers. The center’s uniquely structured compensation package, therefore, incentivizes both activities. We are looking for an individual with documented excellence in both areas, commensurate with associate professor/professor level. Besides a competitive salary, incentive bonus structure, and excellent benefit package, the CHR also offers partnership along either a 3-year or 5-year equity track and, ultimately, part or complete ownership, as the current leadership is expected to retire within that time-period.
If you feel qualified for the position and share our philosophy of being a physician-scientist, please let us know by submitting your C.V. and a brief letter of interest to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position can be filled immediately. All submissions are considered confidential.


Have you thought about advertising in the VOICE?
This newsletter every month goes electronically to ca. 80,000 infertility patients, medical professionals in the field, and members of the media, with over 25% (an unusually high number) also opening the VOICE.
For further information, please contact: Ms. Alexandra Rata (212) 994 4400 or e-mail to arata@thechr.com

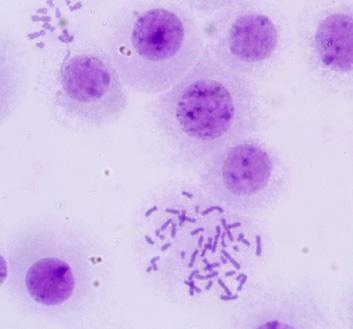
Granulosa cells in the ovarian follicle are central to the production of good quality oocytes. Here at CHR, several ongoing research projects use the granulosa cells left over from egg retrievals to study just how these cells support and maintain the oocyte during the long road to ovulation. This image shows one such cell that has been kept in culture for 5 days after retrieval. Aberrations in the structure of the DNA-containing nucleus, shown in blue are evident as irregular projections, a sign that this cell is undergoing stress outside of its normal environment.
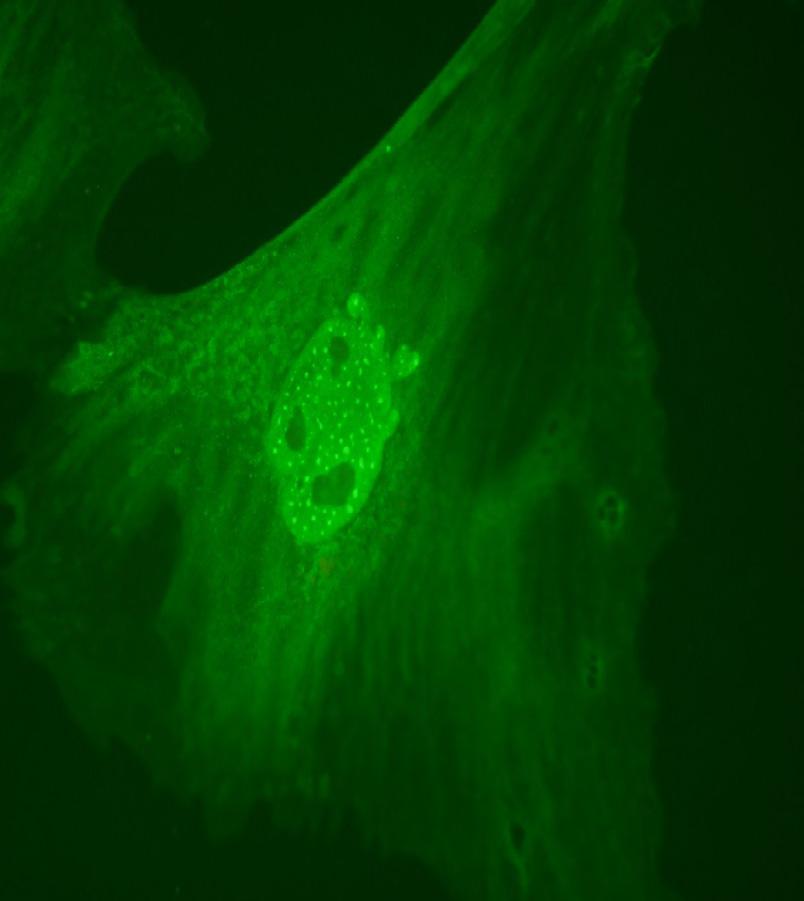
This image is of the same cell shown above but in this case we used an antibody-staining technique to ask whether or not the stress of culture was causing damage to the DNA. Shown as yellow/ green speckles, we can see many sites of DNA damage as the cell tries to repair what are known as double strand breaks, actual cuts in the DNA that can lead to mutations or even death of the cell. Dr. Albertini and the CHR research team continue their investigations into the factors that control the health and well-being of the genome in the eggs, embryos, and granulosa cells we are grateful to have access to from our patients.
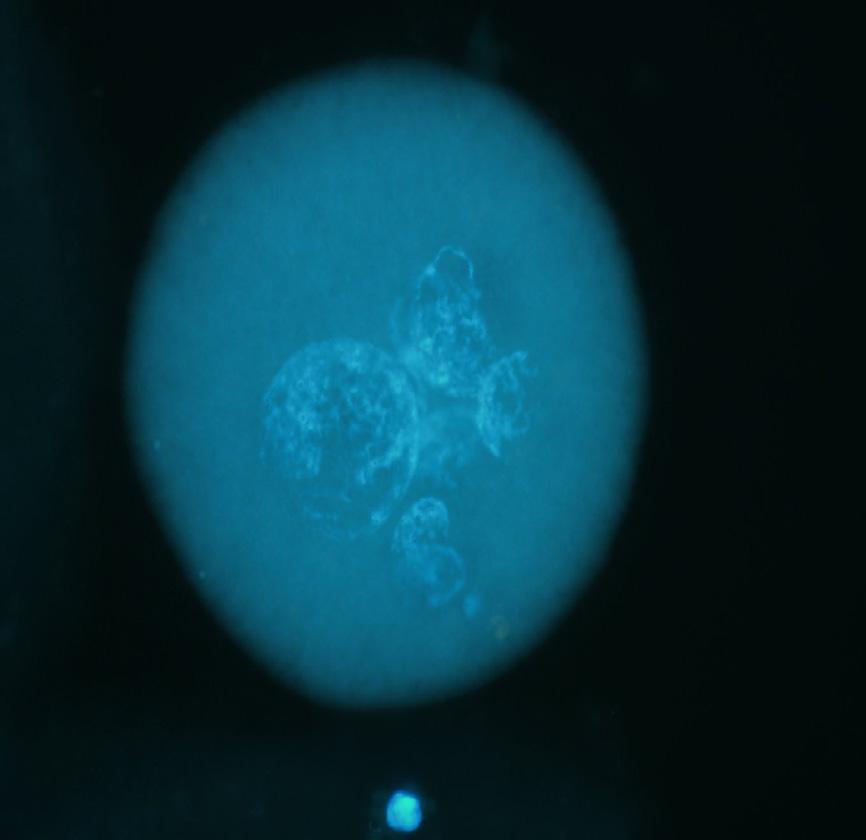
In a collaboration with Dr. Pasquale Patrizio when he was at Yale Medical School, CHR scientists had the opportunity to study the abnormal embryos from a patient whose eggs showed abnormal changes in nuclei following ICSI fertilization. Sadly for this patient, all of her eggs showed the same abnormality after two IVF cycles so she was unable to get pregnant with her own eggs, a puzzle we are still trying to solve for this patient. The figure here shows one of her eggs containing multiple nuclear structures (blue) we believe reflect a defect in coordinating the first cell divisions required to make a healthy embryo. A search for genetic defects that might underscore this pathology has not yet yielded clues that could explain this unfortunate behavior.
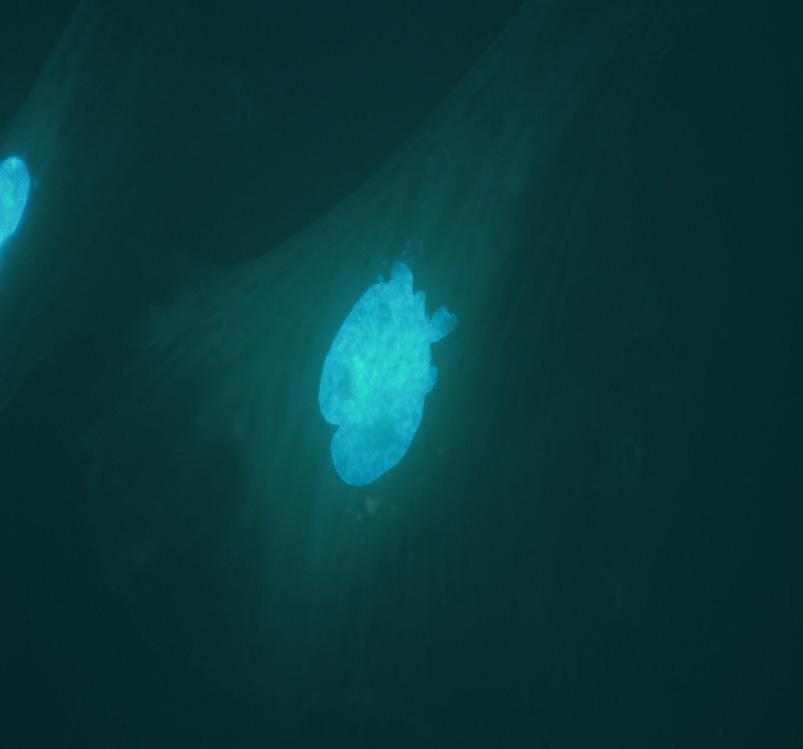 Image 2
Image 3
Image 2
Image 3
 By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.
By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.

Even though quantum computing already appears on the verge of practical realization, terms like quantum entanglement to most laypeople still sound foreign, and even to physicists it has remained a fascinating phenomenon. Here is one of the simplest explanations I have read: “Quantum entanglement occurs when a pair of particles become so closely intertwined that one can no longer be described without the other, even if they are light years apart. A change in one of the particles, therefore, will automatically and instantly trigger a change in its partner particle, even if this partner-particle is on the other end of the universe. What this, potentially, means for computing can only be described as miraculous because, if one were to encode the changes in the states of these two particles with 1s and 0s, this should allow communications at speeds faster than light.”1

Deeply counterintuitive to most of us simple human beings, the concept even confused Albert Einstein who described it as, “spooky action at a distance.” Yet, many experiments have established quantum entanglement as a fact and this phenomenon, therefore, now is the basis for newly emerging technologies, such as quantum computing and quantum networks. Observations of entanglement historically were made only between pairs of photons and electrons but, just recently, researchers for the first time reported a new form of entanglement involving pairs of dissimilar particles and, thereby, offering new insights into the inner workings of atoms, governed by the “bizarre” laws of quantum mechanics.1
Quantum theory, of course, potentially applies to every aspect of our existence, including our biology as humans, as all matter – and that includes living matter – is subject to the laws of physics. Biological processes constantly involve the transport of particles and are only maintainable if the involved systems – for example a cell or a macromolecular system – exchange energy with their surroundings through molecular vibrations and phonons. Phonons sare definite discrete units of quantum of vibrational mechanical energy and at the same time also a quantum of electromagnetic or light energy). Where such exchanges take place, such systems are called “open quantum systems.” In contrast, the universe, as currently understood, is, for example, believed to be a “closed quantum system.” Consequently, our bodies are made up of our universe’s particles and, apparently, not of particles beyond (if a beyond were to exist).
Certain processes that are essential for all functioning living systems require quantum mechanics to explain them.3 Good examples are photosynthesis, vision, and enzyme catalysis. Phenomena in the past believed to only exist in atomic or subatomic systems at extremely low temperatures, now have been identified in systems responsible for life. The field of study encompassing all of these phenomena has, indeed, become a well-defined specialty area, called quantum biology, which explores the application of quantum theory to aspects of biology that cannot be accurately described by classical laws of physics.2

One of the more fascinating examples is quantum tunneling, which is considered a very well-studied archetypical quantum effect. Some proteins apparently perform redox reactions using long-range electron tunneling over distances up to 30Å, which even in a vacuum would be impossible. Some enzymes also use quantum tunneling within molecules to transfer protons as part of catalytic reactions and, maybe most interestingly, tunneling also plays a role in the occurrence of DNA mutations through opposing nucleobases exchanging in this way protons.3 To quote Jenny Morber in the June 4, 2022 issue of Hard Science, “The ease of proton tunnelling and the longevity of these intermediate states might even be relevant to studies on the origin of life because the rate of early evolution is linked to the mutation rate of single-stranded RNA. Thus, though the quantum world might seem
weird and distant, it might have played a role in giving us life — and also taking it away.”4
Einstein concluded that the “spooky action at a distance” in quantum mechanics must be an incomplete picture of reality, with hidden variables missing. Physicist John Bell then proposed in 1964 the theorem of super-determinism, now called Bell’s theorem that exposed the nonlocality of quantum mechanics. John Horgan in Scientific American on March 10, 2022, noted that Bell in a 1985 interview suggested that “the puzzle of nonlocality vanishes if you assume that the world is super-deterministic, with not just inanimate nature running a behind-the-scene clockwork, but with our behavior, including our belief that we are free to choose to do one experiment rather than another, absolutely predetermined.” 5 Further expanding on this though, Horgan quotes Sabine Hossenfelder, a contemporary physicist, as calling free will “logically incoherent nonsense,” though he personally (and other prominent physicists and philosophers) disagreed with this opinion.
As readers of this column you, rightly, at this point may be asking what all of these “crazy” ideas have to do with the practice of medicine, which, after all, is supposed to be the overruling purpose of this column. The answer is actually quite simple: All the preceding information quite clearly pointed out that we live in a world that is much more complex than we all are able to perceive in our daily lives, and that, of course, also applies to the practice of medicine. Indeed, I would argue that our current inability as humans to perceive our physical realities better is, likely, more harmful in medicine than in other areas of human existence because naiveté in reaching conclusions in medicine often has seriously negative consequences.
Also, there is of course, no lack of naiveté in medicine: Consider the fact that only a few decades ago, we believed that every gene has only one function, - that A always leads to B or that A+B always produces C. We have learned and have come to understand our bodily systems better, but the principal purpose of this column is to point out that our current understanding of biology and medicine is still too simplistic. To better understand the complexities below the surface of current knowledge, it appears important to acknowledge that mankind would not exist if biology was as simplistic as we view it. The causation of everything is multifactorial and, just because A may lead to B does not mean that C to F may not influence how well (or poorly) A to B works. And the opposite is true as well: just because we have witnessed that A may lead to B, does not mean that there isn’t redundancy built in that allows A to go to B via, for example, C, D, and E in case A to B has broken down.
Consequently, we in science often observe only the superficial pathways and then attribute all activities to them, without considering what lies beneath and creates all the redundancies
Continued on page 19
Continued from page 18
that allow life to continue even during catastrophic events and, even more importantly, allows the survival of the species.
What quantum physics has revealed is that beyond the visible to us and perceivable world of biology and medicine, inanimate nature is running behind-the-scenes a clockwork of unrecognized connections and interplays which, as of this point, we can only imagine in their complexities and interdependencies, but mostly unperceivable by our senses and intellect. Maybe artificial intelligence (AI) will reveal some of these multicentric connections but, considering that quantum physics has taught us the realities of quantum entanglement and, from that, the shortcomings in our ability, short of highly complex experimental set-ups, to make true observations, one is almost left in despair, recognizing how hopeless medicine is in claiming absolute truth. If there is indeed one conclusion to all of this, then it is the need for humility in recognizing how little we know, with, despite enormous strides, little hope for sufficient quick progress since we haven’t even started yet to really fully understand what makes our bodies function and misfunction.

1. Puiu T. New Physics. https://www.zmescience.com/science/physics/ physicist-just discovered-a-new-type-of-quantum-entanglement/
2. https://royalsociety.org/blog/2019/02/ the-future-of-quantum-biology/
3. https://www.azolifesciences.com/article/What-is-Quantum-Biology. aspx
4. https://bigthink.com/hard-science/quantum-biology-mutation/
5. https://www.scientificamerican.com/article/ does-quantum-mechanics-rule-out-free-will/
The CHR is searching for a candidate for the newly created position of Embryology Laboratory Supervisor for Research. The CHR’s embryology laboratory, under a single laboratory director, is in the process of being reorganized into three distinct areas with separate supervisory responsibilities: (i) clinical, (ii) administrative, and (III) research.
Supervisors in all three areas must hold PhD degrees (or equivalent) and be fully trained human embryologists with sufficient historical professional experience to hold a supervisory position.

While such human embryology experience is preferred for this new position as well, priority qualifications are a record of excellence in reproductive biology research, documented by publications in prestigious peer-reviewed journals and, in absence of human IVF experience, at least substantial animal IVF experience allowing for relatively quick in-house training in human IVF.
Besides a competitive salary and benefit package, the CHR also offers in this position a unique financial incentive-structure linked to the success of the center’s research activities, as demonstrated by publications in prestigious peer-reviewed journal. Moreover, this position will also be eligible for the opportunity to earn shared ownership in research-driven new start-up companies and the center itself.
If you feel that you qualify for this position, please submit your CV and a brief application letter to the CHR’s COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available immediately. All submissions are considered confidential.
Of the top 25 worldwide ranked general fertility specialists, 3 are located in New York City and 2 in New Jersey; and 2/3 in NYC are at The CHR
EXPERTSCAPE (https://expertscape.com/) describes itself as “finding the world’s top expert for any medical problem, ranking people and institutions by their expertise in more than 29,000 biomedical topics.” It further describes the process in 4 steps:
1. Get topic articles — EXPERTSCAPE searches the PubMed database to find all the medical journal articles published about the topic in the past ten years.
2. Score articles — It assigns a score to each article, based on the article’s year of publication (recent is better), the article’s type (guidelines and reviews, for example, count more than letters to the editor), and the journal in which the article appeared (some journals are better than others). It also assigns a score to each author of the article (first author scores higher than second author).
3. Determine institutions — It determines the institution, if possible, from which the article appeared.
4. Tabulate results — It tallies the scores for all articles, authors, institutions, cities, regions, and countries.
The company just published its first worldwide expert listing for “infertility” bunching male (urologists & andrologists) and general infertility specialists (gynecologists) together under the “infertility” heading. Among 67 WORLDWIDE top-ranked experts based on their publication history, and excluding andrologists and urologists, only 3 were NY-based fertility specialists: Zeev Rosenwaks, MD, head of the Weill-Cornell IVF program, at overall position #40 (gyn + urology), the CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, at #46 and the CHR’s Director of Clinical IVF and Head of the Research Division, David H. Barad, MD, MS, at #54. Excluding andrologists and urologists, the worldwide positions for these three physicians were #19, #23, and #39, respectively. Two additional regional colleagues are based in New Jersey, Jason Franasiak, MD at 52/23 and Emre Seli, MD at 41/20, both physicians at IVI/RMA.

Remarkably, the CHR’s Norbert Gleicher, MD, and David H. Barad, MD, MS, thus were among only three NYC-based, and only among 10 total U.S.- based general infertility experts ranked worldwide in the top grouping. Moreover, except for Weill-Cornell, no gyn-faculty member of another NY-based medical school and/or major teaching hospital made it into the list of the top fertility specialists worldwide. That a relatively small private and independent fertility center, like The CHR, succeeded in placing two of its physicians into this elite group, is unprecedented and is an acknowledgment of the CHR’s stellar research effort in the infertility field over the last decade. Within this context, it is also important to reemphasize that the whole U.S. placed only 10 general infertility experts in the top group.

The CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, appeared on Griffin Jones’ Inside Reproductive Health Podcast, - a Fertility Bridge podcast
Norbert Gleicher, MD, on February 13 joined Griffin Jones on his 173rd weekly Inside Reproductive Health Podcast (https://podcasts.apple.com/us/podcast/inside-reproductive-health-podcast/id1447306896) which his company describes as follows: “Inside Reproductive Health is your source for information about the growing field of fertility. Inside Reproductive Health features an active blog and weekly interviews with leaders from the clinical, investment, patient relations, and pharmaceutical corners of reproductive medicine.”
The editorial staff of The VOICE has found many of these podcasts very informative, frequently cites them for relevant information, and has in the past recommended subscriptions to the podcast for those interested in learning background information about the infertility field in the U.S. The podcast is also finding increasing interest outside of the U.S. and recently offered a review of IVF in India.
Jones and Gleicher discussed a whole array of subjects affecting infertility practice and medicine in general, starting with the important subject of information misrepresentations in medicine which, of course, leads to inappropriate medical practices. At the time of this writing, the exact date of when the podcast will go public in March is not yet determined but it will be made available at the above-noted link. The link will also be featured in the April issue of The VOICE
Tocci A, Barad DH, Lukaszuk K, Orvieto R, and the International Do No Harm Group in IVF (IDNHG-IVF). Routine double-ovarian-stimulation (Duo Stim) in poor responders lacks rationale, evidence, and follow-up. Hum Reprod 2023; dead002. doi: 10.1093/humrep/dead002. Online ahead of print.

This publication is a product of the International Do No Harm Group in IVF (IDNHG-IVF), which several years ago was founded by The CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, with the goal of gathering colleagues worldwide who are unsatisfied with practice patterns that, obviously, harm (rather than help) in achieving best IVF outcomes. This informally coalesced group of physicians and biologists in the IVF field was several years ago incorporated as a not-forprofit foundation in New York City and offers free membership to any member of the worldwide IVF community who shares in the opinion that the introduction of new practice patterns in IVF in recent years has often occurred without proper prior validations and, therefore, must be opposed.
As an informal group, the IDNHG-IVF offers every member of the organization the opportunity of generating manuscripts addressing IVF practice for formal sponsorship by the organization. The decision on whether a paper should be sponsored is then up to the Executive Committee of the organization. If sponsorship is approved, the IDNHG-IVF is listed as a co-author of the paper. Moreover, the primary author is given the opportunity (if desired) to invite co-authors from the group’s membership. This process was followed in this case, with the primary author being Angelo Tocci, MD, from the Reproductive Medicine Unit of the Gruppo Donnamed in Rome, Italy. CHR’s David H. Barad MD, MS, was a co-author of this “opinion” article, which wisely argued against another (among many) “fashions of the moment,” introduced into the IVF field without proper rational and/or validation before introduction to clinical practice.
Those interested in joining the IDNHG-IVF or submitting a paper for possible sponsorship should write to Norbert Gleicher, MD, Executive Director, IDHNG-IVF, at ngleicher@thechr.com


would you like a copy of the voice mailed to your door?
we are excited to announce that the voice is now available in print!
To sign up for a print subscription, please reach out to social@thechr.com and specify how many copies you’d like to receive each month. Our team will follow up with a payment and address inquiry



The CHR is searching for a candidate for the newly created position of Embryology Laboratory Supervisor for Research. The CHR’s embryology laboratory, under a single laboratory director, is in the process of being reorganized into three distinct areas with separate supervisory responsibilities: (i) clinical, (ii) administrative, and (III) research.
Supervisors in all three areas must hold PhD degrees (or equivalent) and be fully trained human embryologists with sufficient historical professional experience to hold a supervisory position.

While such human embryology experience is preferred for this new position as well, priority qualifications are a record of excellence in reproductive biology research, documented by publications in prestigious peer-reviewed journals and, in absence of human IVF experience, at least substantial animal IVF experience allowing for relatively quick in-house training in human IVF.

Besides a competitive salary and benefit package, the CHR also offers in this position a unique financial incentive-structure linked to the success of the center’s research activities, as demonstrated by publications in prestigious peer-reviewed journal. Moreover, this position will also be eligible for the opportunity to earn shared ownership in research-driven new start-up companies and the center itself.
If you feel that you qualify for this position, please submit your CV and a brief application letter to the CHR’s COO, Ms. J. Tapper, at jtapper @thechr.com. The position is available immediately. All submissions are considered confidential.


To what extremes some IVF centers go to promote services is becoming increasingly outlandish and well reflected in the question we recently were confronted with: does The CHR offer “needle-free” IVF? First, to be honest, we didn’t even know what was meant by “needle-free” IVF, thinking that somebody may have, perhaps, invented a high-pressure transdermal-administered new method of delivering gonadotropin hormones to patients instead by needle. However, once we looked up what was meant by this term, it immediately became apparent that what we were queried about, was nothing new, and was just another ridiculous marketing campaign, selling to the public yet another unvalidated treatment which, on top of everything else, makes absolutely no clinical sense.
A recent article by Story Studio1 (apparently the PR arm of an NYC-based fertility center that now offers a service it calls “needle-free” IVF) propagates the allegedly new concept with unsupported claims and lacking any data from prior research. The concept, indeed, even lacks a good new hypothesis. Moreover, as the nation’s longest proponent of the so-called mild stimulation in IVF, this center has already been practically practicing “needle-free” IVF for over 20 years by hardly using gonadotropin stimulations of ovaries (usually replaced by clomiphene citrate) in following the old Japanese so-called Sato protocol of mild ovarian stimulation, blastocyst-culture of embryos and elective single embryo transfer.2 This in Japan dominant IVF protocol is also widely credited for IVF live birth rates in Japan for the last 20 years persistently having been by far the lowest among developed countries, a truly surprising finding considering that Japanese investigators are leading the world in many aspects of reproductive research.
As it turns out “needle-free” IVF is supposed to replace “daily blood draws and potentially painful injections of high-dose medications that cause your body to create an excess number of eggs.” That, of course, sounds like conventional IVF is really a terrible thing that at all costs must be circumvented by offering as an alternative “gentle stimulation of ovaries with oral and nasal fertility medicines instead of injection,” but is a nonsensical argument primarily for two reasons: (i) Since, after female age, the number of available embryos for transfer in an IVF cycle is the second-most important predictor of pregnancy chance, mild stimulations of ovaries, which a-priori accepts lower egg yields, as a principle, make no sense. (ii) Consequently, every single study of mild stimulation ever published demonstrated lower pregnancy and live birth rates than conventional stimulations. This even includes studies by the “inventor” of “needle-free IVF,”3 of course, a fact never
Continued from page 27
pointed out when propagating the concept of mild stimulation in one or the other clinical framework. Cleverly, the results are then described as producing “very acceptable” pregnancy rates,3 which, of course, does not mean that they are equal to or better than conventional stimulations.

“Needle-free” IVF is, therefore, nothing else but a rebranding of a by now decades-old concept of mild stimulation of ovaries which, as frequently previously discussed in these pages, for most infertility patients makes little sense, - either clinically or based on costs because, if pregnancy rates are clearly lower, it usually means that more cycles are needed, and more cycles are cumulatively usually also more costly. Mild ovarian stimulations, thus, not only produce poorer cycle outcomes but are also not more cost-effective. The only patient population where mild stimulation may make marginal economic sense, are young good-prognosis patients who, even with mild stimulation, will produce large egg and embryo numbers, such as patients with PCOS.
The above-noted article then continues with more false information by stating that, “scientific research shows that taking high-does fertility drugs during a conventional IVF cycle results in poorer-quality eggs and more difficulty getting pregnant,” both categorically false statements with not a shade of real evidence in support in the literature, - yet a repetitive theme of proponents of mild stimulation. The article furthermore claims that “needle-free” IVF has “a similar pregnancy success rate to conventional IVF,” as already noted above, an outright misrepresentation, even contradicted by data published from the same IVF center.3 Finally, the article, as expected, claims ca. 50% lower costs per cycle which, as also already noted above, is a misrepresentation, considering much lower pregnancy and live birth rates.
In short, a lot of false advertisements, and we thought that ASRM4 and ACOG4 have policies against such false advertisements!
REFERENCES
1. https://storystudio.greenwichtime.com/2022/12/14/ needle-free-ivf-new-hope-fertility/
2. Kato et al., Reprod Biol Endocrinol 2012;10:35
3. Zhang et al., Reprod Biomed Online 2010;21(4):485-495
4. Ethics Committee of the American Society for Reproductive Medicine. Fertil Steril 2013; 1 0 0:334-336
5. Committee on Ethics of American College Obstetricians and Gynecologists. ACOG Committee Opinion No. 510: Obstet Gynecol 2011;118:1195-7.
Kim Kardashian did it twice, and now Paris Hilton did it for the first time (with advice from Kim). And what is the big ”it”? Foregoing nine months of carrying a baby and letting a gestational carrier do all the work. In many, but not all
countries, the use of a gestational carrier is legal. In the U.S., the process is legal, though closely regulated by the FDA and state health departments.

Using a gestational carrier means that a volunteer woman – usually somebody who already had children on her own, is willing to carry a pregnancy which, upon completion, will be the formal (and legal) child of somebody else. That somebody else can be a single woman or man or a heterozygous or same-sex couple. Consequently, where the egg and sperm are coming from to produce the embryo(s) that is/are implanted in the gestational carrier can vary.
Gestational carriers traditionally were used only in infertility situations. The term “surrogate” was, indeed, initially applied to women who not only carried a pregnancy for (usually) another couple but also contributed their own egg to the pregnancy. In other words, the original “surrogates” were only inseminated with the male partner’s semen of a couple that then became the legal parents of the so-created pregnancy. Only in more recent years and in association with the evolution of IVF, did “surrogates” increasingly morph into “gestational carriers” by no longer contributing their own oocytes but, instead, becoming a vessel for a complete embryo.
And with it – who can be surprised – the idea of carrying a pregnancy for somebody else went from, in most cases, mostly being a charitable activity, to becoming a business, mostly still serving infertile patients or women for whom pregnancy would be too dangerous, but in increasing numbers also just serving the convenience of businesswomen, actors, and other wealthy
celebrities who, simply, no longer wanted to be pregnant, but still wanted to have additional children.
The growing industry around this process, of course, welcomed the growing marketplace with open arms; but the picture for infertile couples for several reasons, especially since COVID-19, got progressively bleaker. They found longer and longer waiting periods because not enough women wanted to be gestational carriers and, with it, already exorbitantly high costs skyrocketed even further. In addition, similarly, to what we previously reported in these pages regarding egg donors, the medical qualifications of gestational carriers in The CHR’s experience have significantly deteriorated over the last three years.
The CHR always suggested that the center’s patients who chose to use a gestational carrier book their chosen candidate for a medical consultation with one of The CHR’s physicians to make sure that the candidate was well-qualified for the job. Before COVID-19, it was a rarity for CHR physicians to recommend against the use of a gestational carrier. More recently, it has become common.
Recent research pointing out the importance of epigenetic influences not only on the pregnancy itself but also on the later health of the child,1 has only reemphasized the importance of choosing a good gestational carrier. Regarding third-party egg donation, The CHR, therefore, more than ever, sees the use of gestational carriers as an absolute last resort. At the same time, The CHR, however, fully endorses the right of a woman to self-determination and, therefore, to free choice in choosing whether she wants to carry herself or use a gestational carrier. Before putting down a payment to an
agency for a gestational carrier, we, however, strongly recommend an independent review of the carrier. The physicians of The CHR are always available for such a review.

One more related, though clearly somewhat unusual point: A recent article in COSMOPOLITAN magazine2 attracted considerable buzz on the Internet because it reported on a paper by a Norwegian philosopher at the University of Oslo who suggested in an accepted publication by a bioethics journal,3 the ludicrous-sounding idea that the bodies of brain-dead women could be used as “gestational carriers.”
She developed this “brilliant” idea after apparently learning that some women who, because of accidents became brain-dead while pregnant, had been successfully maintained on life-support for several weeks to allow their pregnancy to mature toward viability. From that observation, she extrapolated that, like organ donors can proclaim themselves as organ donors while alive, women may proclaim themselves a “whole-body donor”, in which embryos may be implanted and then carried to delivery. Considering the very obvious “brilliance” of this idea, we became curious as to who this philosopher-genius was and, low and behold, she turned out to have a distinguished publication list in the bioethics field, with several articles, indeed, addressing ectogenesis (the growth of a human fetus outside the mother’s body).4
1. Andrawus et al., Int J Molec Sci 2022;23(2):12698
2. https://www.cosmopolitan.com/uk/body/health/a42771871/ brain-dead-women-surrogate/

3. Smajdor A. Theor Med Bioethics2022; doi: 10.1007/s11017-022-09599-8. Online ahead of print.
4. Räsänen J, Smajdor A. Bioethics 2020;34(4):217-221
The CHR has a sizable research program, much in collaboration with laboratories here in NYC, the rest of the country, or even outside of the U.S. Most of this research does not require human embryos; yet, research laboratories never have enough human embryos for research. The CHR, therefore, very much welcomes embryos donated for research by our own patients but, at times, also receives embryos from other IVF centers in the U.S. which do not have research programs and, therefore, when receiving from their patients for research purposes donated embryos, don’t have any use for those themselves. In addition, The Foundation for Reproductive Medicine (FRM) which at times also receives research-donated embryos from other IVF centers, maintains those embryos at The CHR. The CHR also accepts research-donated embryos directly from patients at other centers, as long as those patients make the arrangements to have these embryos moved to The CHR.
Every embryo donated for research that ends up frozen and housed at The CHR is logged in with all of its details being recorded. Every donated embryo, therefore, can be accounted for at every moment
and is traced longitudinally to whatever research project the embryos are finally assigned. Every study receiving embryos from The CHR must be IRB-approved, and researchers must account for every single embryo they receive. These rules are so rigid because there is rare consensus in the research community that human embryos deserve “special consideration.” 1 This is, indeed, a subject the ASRM has published on one of its best ethics opinions.2
Also, in compliance with the “special” ethical standing of human embryos, like still in clinical use cryopreserved embryos, embryos donated to research are kept in large liquid nitrogen tanks, secured from failures by redundant security alarms. In summary, like all other human embryos, those donated to research receive close attention and their use in research projects follows well-delineated ethical rules.
REFERENCES
1. Negro et al., Clin Ter 2021;172(4):358-362
2. Ethics in Embryo Research Task Force, Ethics Committee of the ASRM. Fertil Steril 2020;113(2):270-294
The term “compassionate embryo transfer” always seemed somewhat awkward to us. It is widely defined as a procedure wherein in vitro-created embryos are placed into a patient’s cervix, vagina, or uterus at an infertile period in the menstrual cycle where they are expected to perish.1 The procedure is often chosen by patients who for religious reasons object to laboratory disposal of excessive embryos. Other patients chose the procedure as more “natural” than a laboratory disposal and yet others claim that it offers an opportunity to grieve for a potential pregnancy.

Even though we do not like, the term “compassionate” in this framework and, for example, would greatly prefer to name such transfers “natural,” “spontaneous,” or, maybe “mis- timed” transfers. The CHR, of course, offers these transfers to desirous patients. Interestingly, the ASRM also published a comprehensive ethics opinion on this subject.2 IVF centers apparently deal with this issue in greatly varying ways.3
1. Riggan KA, Allyse M. Hum Reprod 2019;34(5):791-794
2. Ethics Committee of the ASRM. Fertil Steril 2020;113(1):62-65
3. Hairston et al., Fertil Steril 2020; 114(3):552-557

CoQ10 is the primary lipophilic antioxidant molecule endogenously produced by cells.1 It is naturally present in living cells where it acts as an essential cofactor for ATP production and performs as an important antioxidant. It has very low toxicity and, therefore, is widely used as a food supplement, including
in female2 as well as male infertility,3 though available studies are of poor quality and efficacy appears limited.4,5 Acceptable daily intake has been suggested to lie around 1200mg/kg/day, roughly 720mg/day for a person with an average weight of 60kg.6 Depending on weight, The CHR, therefore, usually prescribes between 600-800mg daily to females and between 600-1000mg daily to men.
It has been suggested that CoQ10 improves age-related deterioration in oocyte quality, though mechanisms for this activity have remained unclear. In males, six months of CoQ10 supplementation appear to improve semen parameters in oligoasthenospermia.8
However, as noted in February’s VOICE, antioxidants (and their metabolites) can also reach toxic levels,9 which can cause adverse effects on infertility. This fact has raised concern at The CHR because we see increasing numbers of patients who are on multiple different antioxidants at the same time. It would appear that one – at the right dosage – is enough.
1. Santoro MM. Cell Metab 2020;31(1):13-15
2. Ben-Meir et al., Aging Cell 2015;14(5):887-895
3. Lucignani et al., Nutriets 2022;14(21):4585
4. Showell et al., Cochrane Database Syst Rev 2020;8(8):CD007807
5. Sharma et al., Urology 2022;161:4-11
6. Hidaka et al., Biofactors 208;32(1-4):199-208
7. Yang et al., Frnt Endocrinol (Lausanne) 2022;13:813772
8. Alahmar AT, Naemi R. Andrologia 2022;54(5):e14385
9. Bast A, Haenen GrMM. Environ Toxicol Pharmacol 2002;11(3-4):251-258
Mostly placed into a clinical context, we in this section of the newsletter offer a survey of articles in the English literature, usually published in the preceding month, which the CHR found of interest to the current practice of clinical reproductive endocrinology and infertility, - even if at times not immediately applicable to daily clinical practice. These articles, however, nevertheless often point out where clinical practice will likely go and, therefore, serve an important translational purpose. Translational research has been the CHR’s principal research goal since its founding in 1981, has produced a significant number of U.S. patents over the years, and has propelled the CHR into its current position as a worldwide center of last resort for infertile patients who have failed treatments elsewhere.
In a recent “editorial,”1 Nature magazine recently discussed a paper that was published in the preceding month2 which concluded that papers and patents that changed the course of science by leading to paradigm shifts in science have become less “dominant.,” and what this observation may mean for the quality of produced science in the world. Studying the time period between 1945 and 2010, the authors concluded that, despite an explosion in the number of published papers and patents that could be qualified as “disruptive remaining approximately the same, their share of overall volume has been diminishing. The concern arising from this observation was that innovation may be slowing, thereby raising fundamental questions about the “science enterprise” in the current world.
In preparation for the editorial, its writers spoke to several scholars and received diverging feedback: While some were concerned, others did
Continued on page 32
not share this feeling, arguing that the overall number of paradigm-changing papers and patents remained similar. Yet others wondered whether these findings were not indicative of how poorly science is organized. One particular concern increasingly heard all-over science is that super-specialization and the resulting division of science into ever narrower units of knowledge is detrimental to new discoveries that may require broader expertise.
This is a concern also very widely distributed in medicine, where the separation into ever smaller sub-specialty units has been increasingly criticized. We have in The VOICE, repeatedly addressed this concern when especially discussing the shortcomings of expert opinions in medicine, which during the COVID-19 pandemic on so many occasions have been obvious. Criticism of expert opinions by philosophers and others has for decades centered on experts’ limitations in recognizing the interconnectivity of their area of expertise with other, seemingly unconnected knowledge areas which, however, despite being invisible to them, do share interconnectivity.
Our concentration on “the obviously visible” and dismissal of the
important and connected “invisible” is this month also the subject of Norbert Gleicher, MD’s “A Piece of My Mind” column. This level of ignorance, indeed, increasingly appears to affect progress in medicine and science in general.
1. Editorial. Nature 2023;614:7-8
2. Park et al., Nature 2023;613:138-144
Harvard University investigators recently published in JAMA a review of the organization and performance of U.S. health systems with the objectives of (i) identifying and describing health systems in the U.S.; (ii) assessing differences between physicians and hospitals in and outside of health systems; and (iii) comparing quality and cost of care delivered by physicians and hospitals in and outside of health systems,1 and the findings were not what the medical establishment, likely, expected: As of 2018, (where the data derived from) physicians in health systems and hospitals by that point have already delivered a large part of medical services (they by now can be expected to control even a significantly larger share). Performance on clinical quality and patient experience was marginally better in systems, but spending and prices were substantially higher, especially when compared to small practices. The authors concluded that health systems on average have not met the expectations of better care at equal or lower costs.
An accompanying editorial offered further interesting commentary:2 The author pointed out that, for better or worse, independent medical practices and solo community hospitals are disappearing, often by being acquired by hospital-based health systems (a point repeatedly in recent months discussed in The VOICE). His conclusions were that: (i) Little if any difference in the quality of patient care between system and non-system physicians and hospitals. (ii) Prices paid to hospitals for commercially insured patients were, however, 31% higher in system hospitals and 20% higher for system physicians. Overall costs in systems for commercial as well as Medicare patients were 5% higher. Health system patients, moreover, were slightly less likely to be enrolled in Medicaid (so much for providing care to the poor).
Prices were the highest in academic systems (though they also offered the best patient experience), followed by large nonprofit
and, finally, for-profit systems. One really must wonder whether we are on the right track or, whether through ever larger private insurers and ever larger private provider systems, we are not just mimicking all the negative practice patterns of big government-run systems.
1. Beaulieu et al., JAMA 2023;329(4):325-335
2. Casalino LP. JAMA 2023;329(4):293-294
This is what a recent piece in The Wall Street Journal, indeed, suggested,1 after a whole bunch of leading medical schools withdrew participation in the U.S. News ranking. The reason per Icahn School of Medicine at Mount Sinai in NYC is, “the U.S. News rankings undermine the school’s commitment to anti-racism and outreach to diverse communities.” Other schools issued almost identical communiques.
According to the opinion piece, the context for these developments (which are also happening in leading law schools) is the expected disqualification by a Supreme Court majority in a pending case of current selection processes in medical schools which downgrade test scores and grades in the name of diversity. The article also noted that, when some colleges made the SAT optional for admission, the response was muted “for as long tests for would-be brain surgeons would not be eliminated.” However, that appears to change now, “that the battle lines in the meritocracy wars have shifted, as it is precisely would-be brain surgeons whose test scores the medical school want to conceal.”
Whether meritocracy should outweigh concern for equity is, of course, debatable; but we previously pointed out in these pages that medical schools since the 1980s no longer attracted the top graduating college students they pretty much automatically recruited in earlier years. Those, since the late 1980s, first went into MBA programs and to Wall Street, only to abandon those choices in droves since then, in order to join the start-up world. Medicine survived the brain drain, though it, undoubtedly affected those who nowadays choose to become a physician. Whether those changes are to be better or worse for medicine overall, remains to be seen. Today’s brain surgeons are, however, clearly different from their brethren a few decades ago.
1. Stoll I. https://www.wsj.com/articles/medical-schools-bail-on-academic-merit-and-intellectual-rigor-us-news-rankings-diversity-equity-inclusion-race-students-11675005330., January 30, 2023, pA17
Though frequently critical of medical journals’ editorial offices, we have persistently defended them for being hampered by understaffing and underfunding. The rot of conflicts of interest may, however, go deeper than was ever imagined, as a recent report in Nature magazine suggests.1 The case involved whistle-blowers who accused authors of a series of papers of having used “doctored” photographs in their publication. But, as it turned out, those whistle-blowers did not disclose their own very obvious conflicts of interest in the matter.
Some of the allegations involved papers about an experimental Alzheimer’s drug, simufilan, a drug developed by a company by the name Cassava Sciences, based in Austin, TX. What the whistle-blowers failed to disclose is that they had been short sellers of the shares of the company.
The matter has remained unresolved, with the whistle-blowers claiming that their profits were negligible (but, of course, could have been bigger), while some of the papers have been withdrawn, raising the possibility that there really was maleficence in published manuscripts. However, what makes this case important is that it demonstrates how much financial interests nowadays are enmeshed in medical publishing, and how naïve (or blind to the matter) editorial offices often are. There clearly exists an urgent need for assessing economically motivated biases in submitted manuscripts (and review processes). And it seems high time for editorial offices to wake up to this threat to the integrity of medical publishing. And, yes, breaches of integrity also exist in reproductive medicine journals!
Though not even close in potential significance, here is a very recent example: Fertility&Sterility, the flagship journal of the ASRM, recently got a new editor, who we for several reasons welcomed with open arms. One of the main reasons was a constant stream of self-publications by one of the two former co-editors-in-chief, at times even involving papers with very obvious economic interest for him and/or co-workers.
Editors publishing in their own journals (other than opinion commentaries, of course) has been a subject of controversy for a long time, even though it has not been categorically prohibited if editors excused themselves from the review process of their own manuscripts. Yet, everybody who was ever part of an editorial office knows that, practically, such separation is almost impossible to achieve. A recent systematic review of the subject, indeed, confirmed this and reached the following five key conclusions:2
- There is concern that scientific journal editors submitting papers to their own journals may receive preferential treatment.
- The systematic review showed that the prevalence of editors publishing in their own journals varies greatly between journals.
- Results did not show that biased review practices benefitting editors publishing in their own journals are widespread.
- Journal guidelines should include clear information about the handling procedure for submissions authored by editors.
- Overall, it is preferable that at least editors-in-chief strive to avoid publishing research papers in their own journals.
In each monthly issue of Fertility&Sterility, the journal publishes one paper, tagged as “Seminal Contribution,” obviously chosen by the editorial team for its outstanding quality. In the February issue of the journal, the article chosen was a paper in which the new editor-in-chief was the senior author:3
We, of course, expected better from the new editorial team. It didn’t seem unreasonable to expect relief from the practice of self-publishing with the new editorial team coming on board, especially since we were not the only ones who raised concerns about the practices of the prior editorial team.
Our criticism here is not about the quality of the published paper, - we, indeed liked it. But did the new editor-in-chief, who has a distinguished publication list (we, in the February issue of The VOICE, described one of his prior papers as “important,” really need to submit this paper to his own journal? And, even if he saw no other choice, was it really necessary to select his own paper as the “seminal” article of the issue (even if he thought it was)? We don’t believe so and see such, on the surface seemingly relatively minor transgressions by editors, as a principal reason why the credibility of medical journals is increasingly questioned. We also refer readers to the discussion of a recently published article in Nature magazine in this issue’s literature review section (under “The business of medicine”) which revealed that one-quarter of academic editors publish 10% of their own papers in the journals they edit.4
1. Else H. Nature 2023;613:618-619
2. Helgesson et al., Wiley Online Library 2022; https://doi.org/10.1002/ leap.1449
3. Steinberg Weiss et al., Fertil Steril 2023;119(2):186-194
4. King MM. nature 2023;613:445-446
The February issue of The VOICE featured an article on cardiovascular diseases in pregnancy, pointing out that this disease group represents the most frequent cause of maternal death in pregnancy. How timely our article was had become apparent from the literature published last month. A “consensus statement” from the so-called Alliance for Innovation on Maternal Health, indeed pointed exactly the same issue out and, furthermore, stressed that mostly Hispanic and Black women are affected.1 The statement also pointed out that most causes of death from cardiac conditions in pregnancy or postpartum were undiagnosed at the time of death. However, this was not even the worst indictment of current obstetrical care in the U.S.: Over 80% of all pregnancy-related deaths, irrespective of cause but including cardiac causes, were judged as preventable.
A second major point made in this consensus statement was the fact that pregnancy complications, like preeclampsia and diabetes, were predictive of future cardiovascular disease risk. This risk especially regarding preeclampsia was, indeed, the subject of a series of recent
papers: A paper in the European Journal of Preventive Cardiology reported that within as little as seven years from delivery of a first pregnancy with preeclampsia, women were at increased risk for myocardial infarction and/or ischemic stroke. At 10 years after delivery, the risks were four- and three-fold, respectively for both conditions. Both risks almost doubled in comparison to women without a history of preeclampsia within 20 years of delivery. Looking at the same data age-stratified, women between ages 30-39 with preeclampsia had five- and three-fold higher risk of myocardial infarction and ischemic stroke.2
As recently also pointed out in the commentary,3 similar data had also been reported two years earlier by US investigators,4 and last month again by Swedish investigators, using coronary computed tomography, which is highly sensitive in the detection of coronary heart disease.4 After examining 10,528 women with a median age of 57 years, on average 30 years after a first pregnancy, they found that 19% had a history of adverse pregnancy outcomes. In comparison to the remaining 81% of women with no adverse outcome, these women demonstrated a 3.8% absolute increase in coronary arteriosclerosis (32.1% vs. 28.3%). With prior preeclampsia, the increase was 8.0%, with similar findings for gestational hypertension in general, corresponding to increased severity of coronary heart disease by 4-11 years. The commentary mostly addresses these findings within the context of known differences in coronary artery disease between women and men and concludes that the strong associations found with especially hypertensive diseases of pregnancy warrant risk reclassifications of these women, though racial differences, while not fully understood yet, will also have to be considered.
1. Hameed et al., Am J Obstet Gynecol 2023; 141(2):253-263
2. Hallum et a., Eur J Prevent Card 2023;doi: 10.1093/eurjpc/zwad003
3. Bello NA. JAMA 2023;329(5):373-375
4. Davis et al., Am J Obstet Gynecol 2021;77(14):1763-1777
5. Sederholm Lawesson et al., JAMA 329(5):393-404
A recent study in PLoS One by US and European investigators reported interesting findings regarding the length of pregnancy, generally assumed to be 40 weeks from the first day of the last menstrual period (factually implantation and, therefore, the initiation of pregnancy occurs ca. 14 days later; the true average length of pregnancy, therefore, is ca. 38weeks).1 That in the U.S. average pregnancy length has shortened has been suggested before but why that was happening has remained controversial.
Some evidence pointed toward underlying physiological changes, while other investigations suggested that obstetric intervention’s, especially early inductions may be the cause. By comparing pregnancies in the U.S. with pregnancies in the U.K. and The Netherlands, authors now appear to have found the answer.
They found that gestational lengths in the U.S. between 1990 and 1920 declined by more than half a week, from 39.1 weeks to 38.5 weeks. Among hospital births, distribution before 40 weeks
in the U.S. (76%) was clearly different from the U.K.’s (60%) and The Netherland’s (56%), while the distribution of homebirths was similar in all three countries. Interestingly, home births peaked in the early morning hours (2:00 am to 5:00 am) but, while in the U.K. and The Netherlands vaginal hospital births followed a similar pattern, in the U.S., the pattern reversed: most vaginal births occurred between 8:00 am to 5:00 pm.
These findings, thus, rather convincingly answer the question as to why U.S. pregnancies have been getting shorter. It seems obvious that, as the authors in polite language expressed, organizational priorities in the U.S. appear to prevail over the natural course of delivery. This finding, of course, raises additional questions, the most important being whether this observation contributed to the poorer perinatal outcomes in the U.S. in comparison to most European countries. Wouldn’t that be a shame!
1. Declercq et al., PLoS One 2023;18(1):e0278856
As the most frequent autoimmune disease in women during reproductive years, thyroid disease in infertility and pregnancy is a frequent topic in The VOICE. Now comes a paper from Chinese investigators in the Journal of Clinical Endocrinology and Metabolism (JCEM) which offers a comprehensive view on the subject, based on 1903 mother-infant pairs and the results were beyond clear: maternal thyroid disease in pregnancy mandates our close attention.1
Specifically, maternal overt hypothyroidism, subclinical hypothyroidism, and hyperthyroidism, as well as hypothyroxinemia during early pregnancy were clearly associated with weekend neuropsychological development in infancy. Interestingly, some of these effects may be sex-specific, with both sexes affected more in varying parameters. These findings reemphasize the need to monitor thyroid function in infertile women closely before pregnancy and throughout especially the first trimester.
1. Chen et al., J Clin Endocrinol Metab 2023;108:339-350
We in these pages have repeatedly pointed out the risks of Cannabis use during pregnancy. Considering its legalization in most states, the number of pregnant women using the drug has significantly increased. Concomitantly, the number of adverse pregnancy effects reported in the literature has also grown.1 Exactly what causes those adverse effects has, however, not been determined.
A recently reported study of cannabis use in early pregnancy now offers some answers. Since the endocannabinoid system regulates placental implantation, the placental function can be expected to be a primary target. And this is exactly what this recently published study appears to suggest.2 Using a composite outcome that included small for gestational age, preterm birth medically indicated, stillbirth, and hypertensive disorders of pregnancy, early pregnancy use of marijuana was statistically
significantly associated with adverse composite outcomes primarily mediated by the placenta. More specific investigations of the effects of pregnancy timing of cannabis exposure are announced.
1. Logue et al., J Matern Fetal Neonatal Med 2022;35(26):2128658
2. Metz et al., Am J Obstet Gynecol 2023; 228(1.Suppl): S3-S4
In the fashion industry, “fashions of the moment” are, of course, expected. Short lifespans of fashion trends, which is indeed a characteristic of fashion, are expected to change from season to season. However, this is not so in medicine, where newly introduced treatments are expected to have an underlying rationale, to have been validated before introduction, and, therefore, to last.
With the introduction of many new so-called “add-ons” to IVF, all of these assumptions have, however, largely disappeared: “Fashions of the moment” just appear to come and go, depending on the season, at times not even lasting a season because many – if not most – were not previously validated and, often, did not even have a logical underlying premise. Double-ovarian stimulation – an immediate second stimulation round in the luteal phase following routine follicular-phase–stimulation – was initially proposed as an opportunity to maximize egg yields in a single month - in young women who required surgical removal of ovaries and/or toxic chemotherapy for ovaries, diagnosed with cancers was, without rational or prior validation studies, quickly misappropriated as an idea for routine fertility treatments. Unsurprisingly, as the first studies appeared in the literature post-factum, the results were disappointing.
In an article, also briefly addressed under “CHR Publications,” a group of investigators from The International Do No Harm Group in IVF (IDNHG-IVF), among them also The CHR’s David H. Barad, MD, MS, published an opinion piece that “blasted” the concept. The article is
good reading, not only because it correctly analyses the subject, but also because it demonstrates well how the IVF field over and over again repeats the same mistakes in introducing hypotheses into routine practice without a proper underlying hypothesis, physiological understanding of potential adverse consequences, and prior validation studies. In short, here is yet another good example of a “fashion of the moment.”
1. Tocci et al., Hum Reprod 2023; dead002. doi: 10.1093/humrep/dead002. Online ahead of print.
In recent issues of The VOICE, we on repeated occasions reported on somewhat concerning findings in children born after IVF. In the February issue, we wondered after a recent paper was published 1 and commented on,2 whether IVF children as adults, because of significant epigenetic effects in offspring of IVF cycles, will be as healthy as spontaneously conceived offspring.
Now come investigators from the University of California, San Francisco and reported on metabolomic profiles of children conceived by IVF, non-IVF fertility treatments, or spontaneously conceived offspring and found little differences, - though differences between IVF and controls were more significant than between non-IVF offspring and controls.3 The authors described their findings as “overall reassuring” because few differences in metabolites they found in IVF offspring in comparison to controls were of questionable clinical relevance. That there were differences at all, and that these same differences were not seen in association with non-IVF infertility treatments, however, still appears to a degree as disconcerting. We, therefore, fully agree in this case with the authors’ conclusions that further studies of the subject are urgently required.
1. Wang et al., Nat. Med 2022;28:2646-2653
2. Brison DR. Nat Med 2022;28:2476-2477
3. Tolani et al., JCEM 2023;108:315-322
Myoinositol has especially become a supplement in many infertility centers and is almost automatically given to infertile women with polycystic ovary syndrome (PCOS). A recent review article by a Hungarian colleague in Reproductive Biology and Endocrinology, therefore, appears timely and is recommended to our readers. The article, however, omits one important issue, unfortunately usually left out in almost all PCOS–related papers,which PCOS phenotypes are addressed?
Everybody, of course, knows that, under Rotterdam Criteria, PCOS is made up of four phenotypes (A, B, C, and D). We do not wish to regurgitate here what the alleged differences are between
them and also do not, once more, want to raise the issue of whether defining PCOS by these four phenotypes still makes sense. However, we want to repeat an important point, discovered several years ago by CHR investigators 1,2 and, to these days, overlooked by most colleagues: While all PCOS phenotypes are hyperandrogenic between menarche and roughly age 25, only phenotypes A, B, and C remain hyperandrogenic into advanced ages. Phenotype D, in contrast, however, starts dropping adrenal androgen production, starting approximately at age 25, then goes through a decade of normal-range androgens, only to drop into the hypo-androgenic territory by ca. age 35.
Why is this important? Because the inositols, besides their effectiveness in treating insulin resistance (of course, a frequent feature of many PCOS patients), also lowers androgen levels. And, since phenotype-D PCOS patients above age 35 are already hypo-androgenic, supplementation with inositols further lowers their already low androgens, which makes them infertile and treatment-resistant to IVF in the first place. In practical terms, this means that the inositol counteracts androgen supplementation, whether with DHEA or testosterone directly.3
1. Greff et al., Reprod Biol Endocrinol 2023;21:10
2. Gleicher et al., J Steroid Biochem Mol Biol 2017;167:144-152
3. Gleicher et al., Endocrine 2018;59(3):661-676
4. Gleicher et al., Biomedicines 2022;10:1505
Worldwide declining sperm counts continue at an accelerated pace
The fact that sperm counts have been declining worldwide has been known for years and, indeed, already in 2018 was by experts described as a major worldwide health concern.1 However, the data was incomplete because they did not include proper representation of South/Central America, Africa, and Asia. Now, a consortium of investigators produced a worldwide literature review and meta-analysis on the subject which also included these previously left-out regions of the world, and the results were rather devastating.
Between 1973 and 2018, declines in sperm concentrations were obvious. Among unselected men from all continents, the mean sperm concentration declined by 51.6%, with the decline accelerating after the year 2000. The decline in total sperm count was similar at 62.3% among unselected men.2
This data is obviously concerning and calls for immediate and intensive research in order to determine the causes for this decline in human male reproductive health which, if continuing, can, of course, seriously threaten the survival of the human species, as the authors correctly noted.
1. Levine et al., Basic Clin Androl 2018; 28:13
2. Levine et al., Hum Reprod Update 2022; dmac035.doi:10.1093/humupd/ dmac035. Online ahead of print.
A recent paper in Cell Reports Medicine pointed out that fertility has become a priority in transgender health research.1 Transgender women usually seek out gender-affirming hormone therapy (GAHT), which interrupts the production of semen. Authors from The Netherlands and Australia now reported on nine transgender women who ceased GAHT, resulting in renewed sperm production and, thereby, reaffirming the transient nature of testicular suppression by GAHT. Those are, of course, not unexpected findings but, nevertheless, important findings for the counseling process of the female transgender community regarding their future fertility.
Also relating to the female transgender community, another study in the JCEM offered new information on serum testosterone (T) and adrenal androgen levels with and without surgical removal of testes. Once again, the findings were not surprising in that they reaffirmed that, after an initial drop, T levels remain stable. Adrenal androgens decreased in the first year of treatment with cyproterone acetate plus estrogen and remained steady after gonadectomy. Moreover, androgens did not change after gonadectomy and discontinuation of cyproterone acetate.
1. Yau M, Safer JD. Cell Rep Med 2023;4:100835
2. De Nie et al., Cell Rep Med 2023;4(1):100858
3. Collet at al., CCEM 2023;108:331-338
Congenital adrenal hyperplasia (CAH) is a group of autosomal recessively inherited disorders caused by several different enzyme deficiencies in the steroidal pathway of adrenal glands. Culprits are pathogenic variants in specific genes of adrenal steroidogenic enzymes, the most common being 21OH deficiency. So-called non-classical CAH is a milder form of 21OH deficiency and more common than the classical form. It is mostly diagnosed in hirsute women with infertility and, is often, misdiagnosed as polycystic ovary syndrome (PCOS). Therefore, this is an important diagnosis in female infertility and is the motivation for recommending an excellent recent “seminar” on the subject in The Lancet 1 Besides offering a detailed review of the subject, the article also offers information on novel treatment
approaches, aiming to mimic physiological circadian cortisol rhythms or to reduce adrenal hyperandrogenism independent of suppression with glucocorticoids.
1. Auer et al., Lancet 2023;401:227-244
More on preimplantation genetic testing for aneuploidy (PGT-A)
Focus on Reproduction, the official monthly magazine of ESHRE in its most recent issue published on January 30, 2023, an unsigned article under the tile, “Cumulative LBR in PGT-A falls below routine IVF in new SART analysis.”1 What this article referred to was a paper by U.S. investigators in JARG and reviewed in these pages in the February issue of The VOICE,2 which, as the Focus article reported that PGT-A, among all patients with blastocysts available for transfer or screening, was associated with lower live birth rates per cycle (as well as cumulatively) than IVF cycles that did not use PGT-A. Interestingly, this cumulative deficit was especially pronounced in women under age 35, a fact CHR researchers recently also discovered in a still unpublished analysis of national CDC data (Patrizio P et al., unpublished data).
As the commentary, however, also pointed out, not everything regarding PGT-A was necessarily bad: Early pregnancy loss was lower (7% vs. 12.5%) and twin deliveries were lower under age 42 (by a big part of the medical community considered an adverse IVF outcome but by many infertile patients considered a desirable outcome. That this effect was not seen above age 42 may indeed, suggest that these twin pregnancies were electively allowed only in younger women without PGT-A, which The CHR would, indeed, consider appropriate treatment). Then, in discussing the increasingly heated debate in recent years between proponents and opponents of routine PGT-A utilization, the Focus article indeed referred, to The CHR by noting that in a “characteristically provocative editorial in Human Reproduction,3 Gleicher and colleagues proposed that PGT-A had now reached a dead end, with a (recent Chinese) trial’s results’4 a final nail in the coffin of the PGS/PGT-A hypothesis.”
Interestingly, ASRM as well as ESHRE are currently circulating draft texts regarding updated PGT-A statements, with, of course, nothing set in stone until stakeholder comments are received, reviewed, and integrated. However, if changes in the two drafts will be symmetrical, we will see very different opinions with ESHRE more or less following the UK’s HFEA traffic-light opinion that PGT-A remains fixed on red because of “no evidence from RCTs that PGT-A will improve the chance of having a baby,”5 while ASRM continues to avoid saying anything of significance for fear of antagonizing the genetic testing industry.
Returning to the above-noted claim that PGT-A utilization may reduce early pregnancy loss, colleagues from the Oregon Health and Science University in Portland just published a paper in Fertility & Sterility Reports demonstrating that women with recurrent pregnancy loss have similar aneuploidy rates in their embryos and similar IVF outcomes as controls.6 Reduced miscarriage rates were also not
found in the previously noted clinical trial,4 and in a relatively recent meta-analysis of PGT-A outcomes.7
1. ESHRE. Focus on Reproduction 2023; https://www.focusonreproduction. eu/article/News-in-Reproduction-PGTA-LBR
2. Kucherov et al., JARG 2023;40:137-149
3. Gleicher et al. Hum Reprod 2022;37:2730-2734
4. Yan et al., N Engl J Med 2021;385:2047-2958
5. https://www.hfea.gov.uk/treatments/treatment-add-ons/ pre-implantation-genetic-testing-for-aneuploidy-pgt-a/
6. Siegel Kornfield et al., Fertil Steril Rep 2022;3(4):342-348
7. Cornellisse et al., Cochrane Database Syst rev 2020;9(9): CD005291
An interesting article suggesting an epigenetic basis of evolution was recently published in Progress in Biophysics and Molecular Biology, in which the author proposed that evolution occurred over two levels: (i) Flow of RNA-based information, mostly small regulatory RNAs released from somatic cells exposed to environmental stimuli, which are taken up by spermatozoa and fertilization delivered to the oocyte; and (ii) a highly permissive and to “errors”-prone environment of zygotes and totipotent early-stage embryos. The author, indeed, suggested that under this viewpoint, random genetic mutations, nor natural selection are needed, as sperm acts as a phenotypical inducer” of environmentally acquired traits. One only wonders why the author concluded that it is either one or the other; why not all these processes together?
1. Spedafora C. Progr Biophys Mol Biol 2023;30:S0079-6107(23)00011-1. doi: 10.1016/j.pbiomolbio.2023.01.005. Online ahead of print
The immunology of repeated implantation failure (RIF)
Implantation failure is, likely, the most speculative diagnosis in IVF because nobody really knows what it means. If one further adds the term “repeated,” the matter becomes even more complicated because nobody also knows at what number of failed IVF cycles a “repeated” implantation failure (RIF) should be diagnosed.
The confusion surrounding this subject is well demonstrated by a recent review of the subject in Reproduction which starts with the definition of RIF as “absence of pregnancy despite the transfer of 3 or more good-quality blastocyst-stage embryos.” But what if a patient has embryo transfers at the cleavage stage, as many especially older women will experience? How about age in general? Do three good blasts define an implantation problem, independent of age? We don’t believe so and therefore, The CHR is highly skeptical of almost all published literature on the subject, and this includes the above-noted recent review by Canadian colleagues.1
Once there exists no clear definition of diagnosis, we then also do not understand how treatments can be retrofitted to what does not really exist. Yet, this is exactly what the above-cited paper does by reviewing what the manuscript calls immunomodulatory therapies for RIF. Whether what the paper describes as therapies for RIF are really functioning immunomodulatory treatments within a presumed context of failed
implantation, of course, remains unresolved in this manuscript. We, nevertheless, recommend this paper to our readers because it describes very well several widely used immunological treatments for patients in their respective efficacies and side effects. It, however, does not convince us that any one of them really improves implantation and, therefore, live birth chances. In order to figure that question out, we, first, must learn to better define what really represents RIF in a given patient at different ages and/or with varying functional ovarian reserve.
1. Genest et al., Reproduction 2023;165:R39-R60
We in the February issue of The VOICE noted that the frequency of rheumatoid arthritis (RA) in women of reproductive years warranted steady updates on the management of the disease. The same argument holds up for a recent “review” article in The New England Journal of Medicine that offers a very compelling presentation about common origins but divergent mechanisms among RA patients.1
As the article notes, in contrast to, for example, psoriasis, which largely depends on one pathway of IL23 and I-17, RA can occur through multiple paths, - all leading to the same clinical presentation. Yet, in the process of disease progression, the dominance of pathways varies between patients. That is the reason why responses to treatments are so variable among RA patients. The disease occurs also 2-3 times more frequently in women than men.
Though this article offers a very detailed update on current knowledge regarding this disease, it also once again demonstrates how much more remains to be discovered, especially when it comes to achieving complete remissions, which are still very rare. Also quite disappointingly, this otherwise very detailed article not even once mentioned the management of RA in association with pregnancy.
As we in these pages repeatedly addressed especially in discussions of the COVID-19 pandemic, our immune system in an evolutionary sense is really made up of two distinct components, the so-called innate (also called “general” or “nonspecific”) and adaptive (also called “specialized”) parts. As the evolutionary earlier part of the immune system, it is the first line of defense against, for example, invading bacteria but reacts always in, more-less, the same way. The adaptive immune system evolved later in evolution and has, in contrast, the ability to mount highly specific immune responses involving lymphocytes and antibodies.
Within this context, it is important to recognize that the innate immune system usually goes to work when the skin and mucosal barriers are breached by bacteria and/or tissue damage ensues; in other words, whenever inflammation occurs. It is by now well documented that inflammatory reactions have the purpose of amplifying innate resistance to invaders and enhance tissue repair. In the process of inflammation, the so-called acute-phase proteins are produced as what in clinical medicine are widely called “inflammatory markers”, with C-reactive protein being a prototype and, to these days, together with others, serving as very valuable clinical tools in monitoring inflammatory conditions.
Innate immunity has a cellular and a humoral arm, with the former having the function of sensing microbial moieties and tissue damage, while the humoral arm is made up of molecules that act as ancestors of antibodies and activate complement, opsonizing microbes as well as damaged cells, agglutinating or neutralizing microbes, and regulating inflammation. All of this and much more can be learned from a recent review article in The New England Journal of Medicine, 2 which specifically addresses how acute phase proteins act as part of humoral innate immunity.
Readers of this newsletter will recall how we during the earlier stages of COVID-19 repeatedly lamented the absence of research regarding the innate immune responses against the SAR-CoV-2 virus, with almost all published papers solely concentrating on antibody responses by the adaptive immune system. The importance of overall immunity of the innate immune system has, however, since those early days of the pandemic repeatedly demonstrated. Therefore, we find this superficially unrelated review to be of importance, nevertheless. This is also well demonstrated by the first article discussed here in the next section.
1. Firestein GS. N Engl J Med 2023;388(6):529542
2. Mantovani A, Garlanda C. N Engl J Med 2023;439-451
Updates on COVID-19
The adaptive immune response to COVID-19
The last month produced an unusually large number of interesting articles regarding COVID-19, considering how far into the pandemic we are. The first article we decided to present in this section is a summary that appeared in the BMJ on the adaptive immune response to COVID-19.1 As already noted in the preceding section, for to these days rather unclear reasons, the COVID-19 research community appears to favor research on the adaptive immune response over research on the innate immune response, - but we, of course, are happy to discuss whatever interesting information we can get out of the literature on the subject of COVID-19.
In this article, the freelance medical writer Chris Stokel-Walker takes the reader through a detailed explanation as to how the adaptive immune system (for definition, please see the previous section) creates longer-term immunity to the SARS-CoV-2 virus. After briefly explaining the differences between innate and adaptive parts of our immune system, the article also points out the close interaction between both, presenting as an example that non-neutralizing antibodies produced by the adaptive immune system (its neutralizing antibodies have the function of “neutralizing” a virus) mark pathogens for destruction by the innate immune system. This is, of course, a crucially important process especially when it comes to the evolution of new variants of a virus.
He then points out that it is still unknown for how long adaptive immunity, generated by an individual’s B and T lymphocytes, lasts. Since T cell immunity is long-lasting and ca. 90% of patients post-infections demonstrate T cell immunity, the adaptive immune system should produce at least some long-term immunity.
Referring to another study, the author noted that B cell immunity (production of antibodies) likely lasts for at least 11 months. Since respiratory viruses usually initially infect mucous membranes eliciting only a relatively short IgA response, a more important question is how well this immunity protects against severe COVID-19 disease (generally defined by hospitalization and death). This question returns us to the distinction between mild and severe COVID-19 disease and the observation that neutralizing antibodies prevent infections and, mostly, only mild disease. However, severe disease as was noted is prevented by non-neutralizing antibodies which activate the innate immune system against the virus by painting it for recognition by the innate immune system and by T cell immunity. Like viral infections, vaccines very clearly activate an adaptive immune response in inducing T cell responses that are primarily geared at non-mutating regions of the SARS-CoV-2 virus. Stronger T cell responses, as has already been confirmed in mouse experiments, therefore may offer better long-term protection against new viral mutations. How much protective cross-reactivity is created against new mutations is, however, still unclear, and subject to intensive investigations. Based on what has been discovered regarding B cell immunity following the 1918 influenza pandemic, there is hope that we may be developing longstanding adaptive immunity that may last for up to 90 years.
A major issue raised mostly by critics of the worldwide administrative and medical response during the COVID-19 pandemic has been that the development of “natural” immunity in large parts of the population was mostly ignored by experts. Some recently evolving data on long-term innate as well as adaptive immunity would support this criticism.
Another major criticism of the management of the COVID-19 pandemic, repeatedly discussed in these pages, has been the failure to develop drugs to treat the disease in its early stages, while almost exclusively only focusing on prevention through vaccines. The failure to develop drugs is, indeed, difficult to understand and has even led to conspiracy theories, suggesting that Big Pharma on purpose held back such research since such drugs would, of course, have cut into the industry’s boom in vaccine sales.2
If the COVID-19 pandemic has taught us one thing, it was the fact that a pandemic like this one cannot be defeated by vaccines alone. The reasons appear obvious: (i) We will never be able to vaccinate enough people quickly enough to interrupt a pandemic via adequate community immunity. (ii) We (probably rightly so) will never be able to convince enough of the public to get vaccinated. (iii) Viruses mutate quickly, generating new strains with improving abilities to escape vaccine protection. (iv) At least so far, even new technologies in vaccine development and production are lagging behind mutation rates. (v) Vaccines have significant (often initially unrecognized) side effects, including effects on the recipient’s immune system.
As an excellent recent article in Nature magazine pointed out,3 though updating mRNA vaccines to new strains now appears to be quite easy, it appears increasingly questionable whether so-tailored new vaccines will really improve protection against infection. The reason is a process known since the 1918 Spanish flu pandemic,
called “imprinting,” which describes the fact that the first strain of a virus causes a much more severe immune response than subsequent strains. Consequently, such individuals can still be infected by newer strains (though may be, as noted above, protected from severe disease). This does not mean that boosters should be rejected; but it definitely means that expectations for their efficacy should be limited, which, of course, must affect risk/benefit and cost/benefit considerations as to who should receive them. It also explains why bivalent COVID-19 vaccines introduced to the marketplace did not do any better in producing antibody responses than mono-valent responses, as a recent “perspective” article in The New England Journal of Medicine noted.4
A recent article in Wall Street Journal, however, pointed out that not all vaccines are equal. Specifically, the article noted that a single-shot vaccine developed by Johnson & Johnson induced better and longer-lasting immunity than Pfizer’s and Moderna’s mRNA vaccines. Moreover, its T cell response appeared stronger as well, with its NK cell response being 5-10 times stronger than both mRNA vaccines.5 Interestingly, its response with neutralizing antibodies also was 5 times stronger and the mono-vaccine passed the protection of the Pfizer vaccine after 4 months, and that of the Moderna vaccine after 8 months. The FDA, nevertheless, announced a “new COVID-19 vaccine strategy” involving single annual booster shots, mimicking the annual flu strategy. Somewhat difficult to understand, the FDA also suggested that all COVID-19 vaccines should, going forward, have the same bivalent composition, targeting the original Wuhan strain and Omicron subvariants BA.4 and BA.5.6 Considering what we above noted the recent literature on the subject suggests, these new FDA recommendations very obviously make little sense. Why is that not surprising?
The Wall Street Journal article also reported, the current administration “threw the better J&J vaccine under the bus,” when in April of 2021 a minimally increased thrombosis risk was reported for the J&J vaccine, even though it was lower than the since reported risks for the mRNA vaccines, including myocarditis in young men and pulmonary emboli and strokes in older men.
To improve future anti-SARS-CoV-2 vaccine boosters in the hope of not only preventing severe disease, but preventing all disease grades, the blocking effects of imprinting must be overcome and, as the above-noted Nature article explained, various strategies are already
under investigation.3 But what all of this only furthermore points out is the fact that we in the future cannot only rely on vaccines in fighting COVID-19 (and other potential pandemic viruses).
When it comes to medications to treat already existing COVID-19, there is good and bad news: In a potentially significant breakthrough a large group of investigators recently reported excellent treatment results in a randomized controlled adaptive platform trial in mostly adults with severe COVID-19 (in Brazil and Canada) within seven days from the onset of symptoms. They received either pegylated interferon lambda (189 μg, s.c.) or a placebo. The primary composite outcome was hospitalization or an emergency department visit due to COVID-19 within 28 days after randomization: 931 patients received interferon, 1,018 placebo, and 83% had been vaccinated. Primary outcome events occurred in 25/931 study patients (2.7%) and 57/1018 controls (5.6%). The difference was 51% (RR, 0.57; 95% CI 0.33 to 0.95). Analyses of secondary outcomes were compatible. Thus, even only a single dose of this interferon resulted in a significant positive effect in this group of COVID-19 patients.7
However, as an article in The New York Times pointed out, this very promising new treatment approach faces considerable market hurdles, even though the drug rivals the results of Paxlovid, currently the only anti-COVID-19 drug on the market.8 Moreover, this study made observations that were independent of the viral strain, suggesting that this treatment approach may also be effective against flu viruses and potentially other viral pandemics.
Interferons have been known to have anti-viral properties for quite some time, mostly mediated by their ability to activate the general firstline innate immune response by promoting cytokine production, NK cell function, and antigen presentation. That the use of an interferon in the treatment of COVID-19 was not already considered earlier, we find somewhat surprising, but further supports the above-noted contention that treatments of COVID-19 have fallen victim to the obsession of governments in favor of vaccines. Although the FDA has shown little hesitance in authorizing the emergency use of Pfizer and Moderna mRNA vaccines, they so far refused consideration of this treatment on the same basis since the trial did not have an American site (it was conducted in Canada and Brazil) and was conducted by academic centers
rather than its manufacturer, a company called Eiger. 8 We, of course, would argue that a study performed by economically uninterested academics, probably, has more credibility than a Pharma-produced study.
Experts quoted in the New York Times article were, moreover, unanimous that the drug’s most important future function may lie in the prevention of disease, especially in high-risk populations.
A study of Fluvoxamine, basically a psychiatric medication but in early reports suggested to beneficially affect COVID-19 patients throughout the course of their disease, however, failed to demonstrate the alleged benefits a study of U.S. investigators reported in JAMA 9 An accompanying editorial suggested in searching for reasons for the discrepant result with earlier reports that the efficacy may have changed of the drug as new variants of the SARS-CoV-2 virus evolved.10 Whatever the reasons, Fluvoxamine will not very likely become part of COVID-19 treatment.
As in prior months discussed on several occasions on these pages, monoclonal antibody therapy also has remained controversial in association with COVID-19. Now comes, however, a very interesting new study in Nature magazine by investigators from Rockefeller University that attempted to define how (monoclonal) antibodies affect the immune system.11 The authors pointed out that already in 1909 investigators noticed that antibodies through feedback can inhibit humoral immunity. Later it became apparent, that antibodies can, indeed, either enhance or inhibit humoral immunity. To understand the underlying mechanisms better, they investigated how pre-existing antibodies influence the development of so-called memory B cells.
After receiving two high-affinity anti-SARS-CoV-2 monoclonal antibodies and subsequently two dosages of an mRNA vaccine, they discovered that study subjects produced antigen-binding and neutralizing titers only fractionally lower than in controls. Memory B cells, however, differed: They mostly only expressed low-affinity IgM antibodies. Building on these observations in humans and exploring things further in a mouse model, they found that pre-existing high-affinity antibodies bias germinal center and B cell selection in two ways: The activation
threshold is lowered, allowing lower-affinity clones to become part of the immune response, and through direct masking of epitopes. The authors concluded that these findings may in part explain why, as alluded to earlier above, memory antibodies present with shifting target profiles after booster vaccinations. What, however, was not noted was the possibility that these findings could also explain the varying results of treatments with convalescent monoclonal antibodies in COVID-19.
An article in Nature magazine suggested that China’s most recent COVID-19 wave probably has peaked.12However, the article very clearly notes that a lack of data (as, of course, is expected from this country) makes it practically impossible to assess the true impact of the outbreak that started when the Chinese government basically overnight terminated all COVID-19 related restrictions.
Another interesting paper in Nature magazine investigated discriminatory attitudes against unvaccinated people during the COVID-19 pandemic.13 Unsurprisingly, the worldwide study demonstrated significant levels of discriminatory attitude from vaccinated toward unvaccinated citizens everywhere except in Hungary and Romania at levels usually only reserved for immigrant and minority populations. Unvaccinated people, in contrast, showed no evidence of discriminatory behavior toward vaccinated people, except in Germany and the U.S., where concomitantly discriminatory attitudes arose in support of the removal of fundamental rights.
A large prospective observational study involving 41 hospitals in 18 countries reported in The Lancet enrolled between November 2021 and June 30, 2022 (the first six months of the Omicron variant’s dominance) 4618 pregnant women with COVID-19 diagnoses. These women experienced increased maternal morbidity and mortality, especially among symptomatic and unvaccinated women. Women with complete or boosted vaccine doses had reduced risks for severe symptoms, complications, and deaths.14
This outcome data, of course, is nothing new and reaffirms prior vaccination recommendations by practically all authoritative bodies in the profession. They, of course, also concur with The CHR’s current still valid recommendation that infertile women in treatment and pregnant women, as quickly as possible, should get fully vaccinated.
1. Stokel-Walker C. BMJ 2023;380:p19.doi: 10.1136/bmj.p19
2. https://rumble.com/v1hu7xr-the-truth-about-ivermec tin-a-new-short-documentary-by-plandemic-filmmaker-m.html
3. Brazil R. Nature 2023;613:428-430
4. Offit PA. N Engl J Med 388 (6):481-484
5. Finley A. https://www.wsj.com/articles/how-biden-officials-bungled-a-bet ter-vaccine-virus-covid-public-health-antibodies-immunity-boost ers-risk-11675003017
6. Couzin-Frankel J. Science 2023;379(6631):425-426
7. Reis et al., N Engl J Med 2023;388(6):518528
8. Mueller B. The New York Times, February 9, 2023. https://www.nytimes. com/2023/02/08/health/covid-drug-eiger-interferon.html
9. Mc Carthy MW, et al., JAMA 2023;329(4):296-2305
10. Bhimray A, Gallagher JC. JAMA 2023;329(4):291-292
11. Schaefer-Babajew et al., Nature 2023;613:735-742
12. Lewis D. Nature 2023;613:424-425
13. Bor et al., Nature 2023;613:704-710
14. Villar J, et al., Lancet 2023;401(10375):447-457
It appears that the COVID-19 pandemic affected the whole world’s immune systems, promoting all kinds of viral diseases to resurface. After polio, monkeypox, the syncytial virus, and, of course, the annual flu season appears all to have mostly faded, here is the next generation of warnings: First to be noted, an expanding bird flu outbreak (a new variant of the H5N1 influenza virus) in mink and other mammals sparked concern about possible spread to humans.1 That has so far apparently not happened yet.
Then there is the most recent warning from the CDC about a current wave of Norovirus in the U.S., a very contagious virus causing often severe GI symptoms, including vomiting and severe diarrhea. Infections happen from direct contact with infected people, consumption of contaminated food or water, touching of contaminated surfaces, and unwashed hands in the mouth.
Finally, Human Immunodeficiency Virus (HIV) infections in infertility practice and obstetrical care are now almost routine, with current viral treatments allowing safe reproduction for almost all infected females and males. An estimated 1.3 million persons living with HIV infections become pregnant annually, among which roughly 1.1 receive antiretroviral treatments according to a recent review article in The New England Journal of Medicine, addressing the potential association of antiretroviral therapy with adverse pregnancy outcomes. This article, therefore, is very timely, and we recommend it to everybody who is treating HIV-positive patients (as The CHR does routinely).
1. May Sidik S. Nature 2023; 614:17
2. CDC., https://www.cdc.gov/norovirus/index.html
3. Eke et al., N Engl J Med 2023;388(4):344392
The recognition of the human microbiome as a co-determinant of human health is one of the major discoveries in medicine in recent years. Now comes an international group of researchers and reporters on the transmission within and across populations of these microbiomes.1 In investigating over 9,700 human metagenomes and computational strain-level profiling, they – we would say unsurprisingly – detected significant bacterial strain sharing with strong mother-to-infant gut microbiome transmission, remaining stable during infancy and remaining detectable into older ages. Transmissions of the oral microbiome, however, happened more horizontally and depended on the length of sharing a home. Gut and oral microbiomes were shared at 12% and 32% median strain-sharing rates, respectively, more so than age and genetics. The authors concluded that such sharing data may inform on non-infectious, microbiome-associated diseases.
REFERENCE
1. Valles-Colomer et al., Nature 2023;614:12-135
We only found one study in the literature last month with potentially important relevance to reproductive medicine and that was a study by U.S. investigators that established a primate model for the in vitro study of human gametogenesis in a primate model using induced pluripotent stem cells from Marmosets to efficiently generate primordial germ cell-like cells.1
Marmosets have in recent years become the preferred primates to model reproductive processes with relevance to the human experience. This study, as the authors pointed out, now offers such a comparative tool, thereby creating a foundation for the preclinical modeling of human gametogenesis.
1. Seita Y, et al., Elife 2023;12:e82263
How much ovarian aging and general somatic aging correspond in timing and underlying physiological processes is still largely undetermined; but that both must share common denominators, is difficult to dispute and is the reason why we follow studies on general somatic aging. Within this context, we found several studies we considered of interest. Leading among those is a review article in Cell, outlining the hallmarks of aging.1 Even though this article does not directly address ovarian aging it is likely the most comprehensive recent coverage of the aging process in the literature and, therefore, is a must-read for anybody interested in human aging.With exactly 300 references, it also can serve as an excellent reference source for further reading.
The authors basically described the aging process as resting on 12 “hallmarks:” genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, disabled macroautophagy, deregulated nutrient sensing, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, altered intercellular communication, chronic inflammation, and dysbiosis. One can easily imagine that all 12 also apply to ovarian aging.
All of this is not only of importance because factors leading to somatic aging may also be involved in ovarian aging, but because it has been suggested that early ovarian aging in women may also be predictive of premature somatic aging.2
Endogenous retroviruses (ERVs) are leftovers of long-ago infections which were integrated as stable genomic DNA elements into primates, now comprising ca. 8% of the human genome.3 Ca. six million years ago, the so-called ERV-K (HML-2) group is believed to have been the most recent integration. The dormant human ERVs can, however, be awakened and have been implicated in various disease states. Another recent paper in Cell now demonstrated that such reactivation of ERs in old age can induce senescence, as the awakening is associated with epigenetic derepression, contributing to age-associated chronic inflammation.4 Living results in increasing entropy, manifesting as a loss of genetic and epigenetic information. Yet another paper in Cell
demonstrated convincingly that loss of epigenetic information can be the cause of mammalian aging, concluding that these findings are consistent with the so-called information theory of aging which claims that a reversible cause of aging is loss of epigenetic information.6
1. López-Otin et al., Cell 2023;186:243-278
2. Cedars MI. Semin Reprod Med 2013;31(06):443-451
3. Dasgupta N, Adams PD. Cell 2023;186:233-235
4. Liu et al., Cell 2023;186:287-304
5. Yan et al., Cell 2023;186:305326
6. Blokh D, Stambler I. Prog Neurobiol 2017;157:158-173
In an e-mail from Griffin Jones (Inside Reproductive Health) to IVF clinics, Ron Shinkman reported that after 11 months of waiting for government approvals, KKR & Co, the private equity giant located in New York City, finally closed on the purchase of an 80% stake in IVI-RMA Global, headquartered in Spain for a record price of US $3.25 billion, which represents an enterprise valuation of US $4.0625 billion. IVI, which originally started in Spain, already had a worldwide presence when in 2019 it entered the U.S. market through the purchase of RMA-NJ, a chain of IVF clinics mostly located on the East Coast (originally announced as a “merger”), leading to the name change to IVI-RMA Global 1
As the article also notes, KKR & Co. already owned another major company providing IVF service in multiple countries by the name GeneralLife which operates 16 IVF centers in Spain and many more in Italy, Sweden, the Czech Republic, and other European countries. Spanish government regulators, therefore, required that KKR & Co. agreed to divest holdings by that company in the Spanish provinces of Seville, Murcia, and Zaragoza operating under the name Ginemed and also restricted some other activities for the company.
As the article also points out, not everything went smoothly in executing this purchase. Once KKR & Co won the quite heated competition for IVI-RMA, it obtained financing from a consortium of banks, including Morgan Stanley, Credit Suisse AG, Bank of America, and Deutsche Bank, AG, who, according to a Bloomberg report last April, beat out a consortium of private investors. Those banks, however, just a few months later apparently got cold feet regarding this deal and dumped their loan obligations at a significant loss. KKR & Co. nevertheless decided to go ahead with the deal, apparently confident in their quite remarkable valuation. It will be interesting to see whether, going forward, this high valuation will impact the individual valuations of IVF centers. Considering that IVI-RMA currently operates 75 individual locations worldwide, this would represent an average enterprise value of US $5.5 million per location.
1. https://www.ivirma.com/press/ivi-arrives-at-america-hand-in-handwith-rmanj-and-consolidates-as-the-largest-group-of-assisted-repro duction-in-the-world.html
The VOICE has in recent months repeatedly reported on various reproductive genetics laboratories closing their doors. Now Inside Reproductive Health, Griffin Jones’ regular e-mail service to IVF clinics, also picked up on the subject. Pointing out the various genetic laboratories that discontinued testing in reproductive medicine, Alexandra Frost, the author of the report, also had the opportunity to interview some experts in the industry who, somewhat surprisingly, did not appear surprised, pointing out that companies that went under were almost exclusively women’s reproductive health testing enterprises. A principal reason seemed to have been overcharging for tests, with insurance carriers no longer offering demanded reimbursements by the laboratories and, instead, to everybody’s surprise, consolidating these tests to selected preferred lab-services providers. Blue Cross Blue Shield, in addition, discovered in an audit that Sema4 had overcharged them between 2019 and 2022 by US $30 million. No wonder, Sema4 had to leave the field.
That academic editors publish editorial opinions is nothing new and can, indeed, add an interesting twist to a medical journal, as the almost weekly page in The Lancet by Richard Horton OBE, FRCP, FMedSci, and the monthly editorial in JARG by David Albertini, PhD, well demonstrate. While Horton’s contributions by many may be considered ideologically too biased for a medical journal, nobody can argue with the validity of Albertini’s monthly comments. Feelings, however, change dramatically when the discussion turns to academic editors who publish their own papers.
We briefly raised this issue elsewhere in this issue of The VOICE, but here have the opportunity to go a little more into detail based on a recently published article by Molly M. King in Nature magazine,1 who commented on a paper in Nature Human Behaviour 2 that addressed this apparently growing concern with truly surprising statistics. Studying 103,000 editors of 1,167 journals (all published by the publisher Elsevier). As it turns out, a full quarter of academic editors publish at least 10% of their own scientific output in the journals they edit. Indeed, 12% publish at least 20%, and 6% at least a third of all of their papers in their own journals. The most senior editors, editors-in-chief, do so at the highest rate. Moreover,
men demonstrated a higher increase in the rate of self-publishing soon after becoming editors than women editors (who, apropos, are still underrepresented).
If anybody still doubted that editorial offices deserve more scrutiny, what other evidence is there still needed?
1. King MM. Nature 2023;613:445-446
2. Liu et al., Nat Hum Behav 2023; doi: 10.1038/s41562-022-01498-
1. Online ahead of print
We are very pleased to report that this month, none of the papers we reviewed was chosen for this section.
The CHR VOICE is the newsletter of The Center for Human Reproduction (CHR), an independent, academically affiliated infertility and research center located at 21 East 69th Street in Manhattan, New York, N.Y 10021. www.centerforhumanreprod.com. Telephone +212 994 4400.
The CHR VOICE attempts to inform and engage a global community of infertility patients, infertility service providers, and researchers in reproductive medicine, physiology, and biology. The mission of The CHR is clinical care, research, and education, all at highest standards, with empathy, honesty, integrity, and equity.The newsletter is published 10 times a year (except July and August). Copyright © 2023 by The CHR. All rights reserved. Print ISSN 2836-3086. Online ISSN 2836-3094. Copyright © 2023 by The CHR. All rights reserved.
For letters to the editor, comments, and suggestions, please contact Micah Elias at melias@thechr.com. For all advertisements or sponsorships in The VOICE , please contact Alexandra Rata at arata@thechr.com. Advertisements appearing in The CHR VOICE do not necessarily reflect the opinions of The CHR. .R