Protecting your mental health during IVF treatments
BRIEFING: It has been acknowledged for decades that infertility affects mental well-being. However, the fact that fertility treatments may add stress and further impact the mental health of fertility patients is less acknowledged. Our “Feuilleton” article this month offers advice on how the process of going through in vitro fertilization (IVF) – likely the most stressful fertility treatment –with just a few considerations can be better tolerated.
In vitro fertilization (IVF) can take a toll on a patient’s mental wellbeing. Research shows that IVF can often intensify an individual’s feelings of anxiety and depression as well as negatively affect self-esteem and confidence. These can be difficult issues to cope with while simultaneously experiencing the potential physical side effects of IVF.
Selected routes patients can take going through fertility treatments to protect and nurture their mental health, however, exist as their bodies cope with the course of fertility treatments. Below are some suggestions to keep in mind if you are one of the millions of infertile women turning to IVF to grow your family.
Make sure you have a support system
Loved ones who support you through life’s obstacles can be such a beacon during difficult times. If you are struggling as you go through

treatments and have loved ones you can confide in, try to talk out your worries with them. Speaking with a partner, family member, or friend instead of letting your worries go unspoken can make a world of difference.
If you are going through IVF with a partner, be careful to not shut him/her out. The quite lengthy experience of IVF can put strains on a partnership because of the pressures of the logistics behind continuing prior established patterns of sex and the anxiety IVF sparks over whether the treatment will succeed. The one partner physically going through treatment, moreover, can easily feel resentment toward the other, even if subconsciously. Odds are that your partner is also experiencing a range of emotions during this time. Being aware of that fact and “checking in” can help you to stay connected as you go through this process together with your partner.
Turn to the IVF community
The Centers for Disease Control and Prevention (CDC) report for the U.S about 4 million births per year, with 1-2 percent of those occurring via IVF. Consequently, many thousands of women have gone through IVF, meaning that ample resources exist to connect with their stories and experiences.
Blogs like Stirrup Queens, podcasts like The Fertility Podcast and Big Fat Negative, and groups who connect on social media—plus countless articles, essays, books, shows, and movies in the cultural digest are out there and freely available. Reviewing these resources can help you to feel more seen as you relate to others who have Continued
The V oice | 5 Continued on page 6
6
on page
Continued from page 5

“Talking out your experiences, concerns, and stressors with a qualified mental health professional can be key when one is going through the motions of IVF treatment.”
gone through the same experiences you are facing. This can also help to feel less isolated, - should be what you are experiencing.
Seek out a therapist
Talking out your experiences, concerns, and stressors with a qualified mental health professional can be key when one is going through the motions of IVF treatment. Therapists can offer their objective opinions on your situation and help you unravel your thoughts and understand your emotions, which you might be pushing off without even realizing while focusing on trying to have a baby. Therapy for infertility patients has become a well-defined sub-specialty among therapists. The CHR will gladly make recommendations if you are looking for a qualified therapist. Many now also offer virtual therapy sessions, which appear to be just as effective as in-person sessions.
Practice meditation and mindfulness
Apps, podcasts, and playlists full of guides to meditation and mindfulness practices are also widely available. If you need to escape from ruminating thoughts about your treatment, you for instance can turn to an episode of the Calm app, allowing your brain to focus on “something else.” Learning the basics of embracing a mindful attitude can be helpful in overcoming obstacles you might face along your fertility journey.
Keeping a journal about the experience
The welcome empty pages of a journal can be a source of comfort during trying times. As with confiding in loved ones or speaking with a therapist, writing down your fears and anxieties
can help to free your mind from stress and even to better understand your emotions. This is especially helpful if you are lacking a support system or are unable to access professional counseling.
Take care of your physical health
Taking care of your physical health during IVF will only strengthen your mental wellbeing. Make sure you are eating a balanced diet, drinking enough water, and not letting selfcare fall by the wayside as you go through IVF treatments. You should also be sure to get enough sleep.
Though you may no longer feel up to your usual strenuous exercise once you are advancing in your IVF cycle, don’t abandon low-impact exercise, especially walking, yoga etc. Continuing to move can help to keep your headspace in a wholesome place.
Ask your physician whatever you want to know
Don’t be scared “to bother” others as you undergo IVF; and this includes your fertility nurse as well as your treating physician. Communicating clearly with your medical staff is key. We have a saying at the CHR: “We always prefer you ask too many rather than too few questions!” Such open communications will help alleviate concerns you may have about IVF and ultimately will ensure that you and your doctor are always on the same page. As you through your path to fertility, this is, of course, key to avoiding any confusion and/or crossed wires, leading to potential treatment mistakes.
6 | The Voice

The V oice | 7


8 | The Voice ADVERTISEMENT ADVERTISEMENT
BRIEFING: CDC and SART publish annual U.S. IVF cycle outcome reports of most (though not all) IVF clinics in the nation. Because those reports are not patient-specific (i.e., not adjusted for individual patient’s characteristics, including age, functional ovarian reserve (FOR), prior failed IVF cycles, etc.), they lack any potential utility for the public in offering correct outcome comparisons between clinics. Acknowledging this fact, both registries point out that their data should not be used for comparisons between IVF clinics. But one then must ask, what then would be the purpose of their publication?
These reports adversely affect the behavior of IVF clinics by disincentivizing them from improving patient-specific IVF cycle outcomes. This is reflected - unfortunately only rarely acknowledged in the infertility literature - in since 2010 mostly stagnating and, often even declining, worldwide pregnancy and live birth rates.
Rapid changes in IVF practice ownership from private to equity investor-control has also changed management priorities in IVF clinics from achieving best IVF outcomes to improving revenues and profits (see also the November-December issue of the VOICE). Valid outcome comparisons between IVF clinics appear more important than ever. We here present a proposal on how this could be done on relatively short notice; that is, - if IVF clinics really would want to know!

The Centers for Disease Control and Prevention (CDC) and the Society for Assisted Reproductive Technology (SART) have significantly improved their respective reporting systems over the years and are continuing to do so (as have international reporting bodies, like ESHRE). A primary purpose of “informing the public,” must acknowledge that all current national reporting systems are basically failures, as none can offer patients the information they need to choose a “best-suited” fertility provider for their specific needs.

Current reporting systems, since first mandated by the U.S. Congress in 1992, do actually exactly the opposite: While pointing out that they should not be used for outcome comparisons between clinics, they are nothing else but hidden “winks” to the public “to do exactly that.” If the intent were what is claimed by CDC and SART, both organizations, at minimum, would explain to the public how seriously misleading their reports can be because of built in biases.
Continued on page 10 The V oice | 9
Continued from page 9
It appears time to speak out and explain, how current reporting systems could be greatly improved with relatively minor efforts, in the CHR’s opinion, a much more important step toward fair outcome reporting to the public than much of the minutia every year added to the systems without adjustments to the systems’ main problem - patient selection biases.
Historical background
The establishment of SART as a special interest group of (then called) the American Fertility Society (AFS) has since led to SART becoming a daughter-society of the American Society for Assisted Reproductive Medicine (ASRM) - so-renamed from the AFS. SART’s establishment in 1985 was, not the least, motivated by the young IVF field’s desire to collect voluntarily submitted IVF outcome data from reporting clinics on as large of a scale as possible.1 In 1987, an article by several prominent IVF experts in Fertility and Sterility shook up the still young IVF field by asking the rather provocative question, “are we exploiting the infertile couple?.”2 In combination with increasing consumer complaints about the lack of formal IVF outcome data from clinics, this paper lead the U.S. Congress in 1992 to pass the Fertility Clinic Success Rate and Certification Act, mandating the annual reporting of IVF clinic (i.e., assisted reproductive technology, (ART)) success rates to the CDC 3 To this day, (fortunately) this mandate has remained the only federal reporting mandate Congress has passed for all of medicine.
Voluntary reporting to SART in the early IVF days was basically limited to cycle numbers, pregnancies and miscarriages. SART then compounded the data and published an annual report (with over two years delay) in Fertility and Sterility. With passage of reporting to the CDC, reporting changed from cycle to clinic-levels under responsibility of the CDC. From that point, the U.S. had two annual national ART outcome reporting systems, both slightly differing in content and style of reporting.
Limitations of this kind of reporting were obvious to the field from the very beginning. However, it took almost a decade for another group of prominent experts to voice publicly the opinion that better reporting platforms were required to “afford the public with credible and understandable estimates of conception per initiated cycle.”4 But despite indisputable progress, both systems to this day have failed to adjust reported cycle outcomes for patient characteristics in individual IVF clinics. Instead, improvement in both systems have concentrated on better (more detailed) differentiation between IVF cycle types, while continuing to ignore patient characteristics.
SART and CDC have competing priorities for their respective reporting systems: SART rightly sees in it an important potentially research tool (t would help further if SART would only make its registry easier available to researchers), while the CDC sees its obligation primarily in offering the public an outcome assessment of ART cycles at reporting IVF clinics. Unfortunately, not only in their annual reports, but also in several publications in the literature, the CDC staff responsible for ART outcome reporting to the public has over the years demonstrated surprising ignorance about how outcome data should be reported in statistically correct ways.
The more complex data collection and data analyses become, the more difficult are results to explain to the public. That clinic A has
a 15% and clinic B a 27%, live birth rate is easy to communicate; but it is much more difficult to explain that this difference may not be statistically significant in favor of clinic B because clinic B has a much younger patient population with much lower FSH and much higher AMH than clinic A. Consequently, clinic A may actually have the better IVF program, even though this clinic has a lower overall live birth rate. Reporting systems to the public have to be simple to be understandable, a subject we will return to.
Why patient characteristics matter so profoundly
Clinical outcome reports mimic clinical research studies in the need for an accurate definition of study populations. As often before noted in the VOICE during reviews of published papers, almost nothing is more important in a properly presented study than definition of study population. The same also applies to outcome registries in clinical medicine. For example, cardiac surgeons will never compare outcomes for bypass surgery between patients with small and large vessel disease because favorable outcomes are much more difficult to achieve with small vessel disease.
Yet, in association with IVF, patients are usually stratified in age groups, - but no attention whatsoever is paid to their functional ovarian reserve (FOR) as defined by FSH and AM. Though both of these hormones are by now well-defined in their respective age-specific levels, whether a woman has normal, low, or high age-specific FSH and/or AMH, is completely ignored. LFOR, diagnosed based on abnormally high age specific FSH and abnormally low AMH, is, therefore, ignored even though such a finding is, of course, associated with poorer IVF outcomes.
Just as patients with small coronary artery disease have poorer outcomes than those with large vessel disease, so will IVF cycle outcomes at a clinic with many LFOR patients, therefore, have poorer IVF cycle outcomes than a clinic with only few such patients. It, therefore, appears obvious that outcome comparisons from registries must be adjusted for all eventual compounding factors,in this case the clinics’ prevalence of patients with LFOR or the two groups’ mean FSH and AMH values. Only if this kind of adjustments (and adjustments to other patient characteristics linked to outcomes) are made to individual clinic reports (as done in every well -executed clinical study), can clinics really be compared. There is no reason why both U.S. IVF registries should not be able to adjust all reported outcomes appropriately.
10 | The Voice
The CHR offers a good example: For example, we just learned that in 2023, for the first time, the median age of the center’s IVF patients reached 44 years (see Figure 1 below). This means that more than half of all patients were above age 44 years. In the preceding five years, ages had slowly but steadily risen from 43 years. For contrast, during the same time period, the national median age of IVF patients at U.S. clinics had remained stable around 36 years (considering that women above age 40 nationally are the quickest growing age group having children,5 a finding that can only be explained by women above ages 42 and 43 in U.S. IVF clinics being, mostly automatically, advanced into third-party egg-donation). Based on the most recent (2021) CDC report, in the U.S. only 19.6% of all fresh IVF cycles were performed in women over the age of 40, and only 10.1% in women above age 42, and almost none above age 43.6
Not only is the CHR’s patient population undergoing IVF, which is dramatically older than at any other reporting U.S. IVF clinic, but these women also had significantly more prior failed IVF cycles at other IVF clinics before reaching treatment at the CHR. This also applies to 16% of the CHR’s patients who during 2023 were under age 40. Also, they almost uniformly had LFOR and had failed prior IVF cycles elsewhere. How then can cycle outcomes at the CHR be compared to cycle outcomes elsewhere?

44 years
first time. As the figure demonstrates, only 16% of the CHR’s patients were under age 41 and, even these women uniformly reached CHR only after multiple failed IVF cycles elsewhere and usually had exceedingly low FOR.
But all of this does not only apply to the CHR. All IVF clinics have different patient populations. Some clinics will be above, while others will be below the national median age of 36 years. The latter should have better outcomes than clinics at or above the national median. After appropriate statistical adjustments for age (and other co-variables, a process routinely performed in studies), this variability should mostly disappear if clinics perform at similar levels. If there still are differences, they may be due to other variables that either were missed in adjustments or, more likely, they reflect true performance differences between clinics.
All the wrong incentives
As current reporting systems do not statistically adjust cycle outcomes in IVF clinics based on the adversity to success represented by different patient populations, currently reported data are basically uninterpretable and should be considered worthless for the public. This is unfortunately hardly ever noted in the literature with the same clarity as here, and an unhealthy situation for IVF clinics as well as the public.
The inability to correctly compare performance levels between IVF clinics also removed the principal incentive for IVF clinics to care about how well (or how poorly) they perform. At a time when, because of changes in clinic ownership from physician-owned to private equity-owned IVF clinics, incentives in IVF increasingly emphasize earnings and profits, physicians should be especially motivated in defending the best IVF cycle outcomes as the principal goal of IVF practice. After all, achieving a healthy delivery is also the principal goal of every infertility patient.
Solutions
What is then the best solution? It seems reasonable to assume that, at least in the long term, artificial intelligence (AI) will provide us with the tools to develop multi-functional models in IVF that will allow for the practice of highly individualized “precision medicine.” This means that considering the patient’s specific past medical history, we will be able to determine what treatment offers an individual patient the best chance of success. However, such AI programs are still likely several years away. In the meantime, there is something that can be done within a reasonably short timetable, and that “something” can be learned from golf - yes golf!
To allow individuals with different talents and experience levels to play with each other, golf, ingeniously, invented the “handicap.” Similarly, based on the characteristics of a clinic’s patient population every clinic can be assigned a “handicap,” which periodically can change as patient populations shift in their characteristics. This handicap is then used to adjust every IVF clinic’s reported outcomes. Like in golf, we then all can play together in the rapidly changing field of IVF and, most importantly, can then be fully transparent which centers will serve patients with specific problems best.
Considering how quickly IVF is becoming an “industry,” we feel that transparency in IVF practice has never been of greater importance. Let’s see how IVF clinics really compare, once all reporting clinic’s outcomes are “handicapped” in reflection of their specific patient populations. Boy, will there be surprises!
REFERENCES
1. Toner et al, Fertil Steril 2016;106(3):541-546
2. Blackwell et al., Fertil Steril 1987;48(5):735-739
3. United S . Fertility Clinic Success Rate and Certificate Act of 1992. Washington: U.S. G.P.O. : Supt. of Docs., U.S. G.P.O., distributor; 1992 (Public Law No. 102-493, October 24, 1992)
4. Williams RS, et al., Am J Obstet Gynecol 2015;212(2):157-162
5. Gleicher et al.,J Endocrinol 2016230(1):F1-F6
6. CDC. 2021 Assisted Reproductive Technology. Fertility Clinic and National Summary Report 2021. https://www.cdc.gov/art/reports/2021/ pdf/Report-ART-Fertility-Clinic-National-Summary-H.pdf
FIGURE 1: The pie chart demonstrates the age distribution of women undergoing fresh autologous IVF cycles at the CHR during 2023 when the center’s median age was
for the
The V oice | 11
Continued on page 12
12 | The Voice

BRIEFING: We here offer brief notes regarding news that in preceding months caught our attention that are relevant to the practice of reproductive medicine and infertility.
Alabama Supreme Court offers a truly absurd decision regarding human embryos
If a decision the Alabama Supreme Court on February 20, 2024, made would apply to New York state, the CHR would now suddenly no longer be the custodian of thousands of human embryos, but the caretaker of many thousands of children. After wrongly concluding that all life begins at fertilization, regardless of location, on that day, this court incorrectly designated un-implanted human embryos to be children.
For an array of good reasons, this is an absurd decision that not only contradicts all logic, but is biologically incorrect. Establishing an embryo through fertilization of an egg with a spermatozoon, simply, does not create a potential of life. To have a potential of life, such an embryo must be allowed to implant in a uterus and, even in nature, a majority of naturally produced embryos, never have the chance of implanting. This chance even at peak fertility of a woman in her early 20s is only roughly 30% and declines as women are getting older to less than 5% after age 45 for each embryo. This means that between 70% and ca. 95% of embryos nature produces during regular human intercourse, will never be given the chance to implant. Therefore, the judgment of the Alabama Supreme Court simply makes no sense and should be reversed on evidentiary grounds.
Unsurprisingly, all related professional organizations, from ACOG to ASRM and its daughter societies and interest groups (SART, SRBT, etc.) have condemned the court’s decision. At the time of this writing two
Continued on page 14 The V oice | 13
Continued from page 13
Alabama-based hospitals, however, already announced a pause in their IVF programs, - even though Alabama’s attorney general announced that his office was not even considering steps that in any way might restrict the practice of IVF. That some alleged “proponents of life” want to deprive infertile couples from having families, is beyond credulity and, indeed, demands condemnation. It appears that wherever we are looking in contemporary society, it is the extremists who are running the show. The time is, therefore, ripe for society’s center to unite and to show extremism on both sides of the political spectrum the door!
Alabama’s Supreme Court decision regarding the “personhood” of embryos stemmed from a lawsuit over the accidental loss of embryos which, considering the huge and rapidly growing utilization of IVF around the world, has remained reassuringly low. Unfortunately, the media, as is so often the case these days, however, could not help themselves in greatly exaggerating the problem. The Alabama lawsuit was just too big an opportunity to steer the pot. The New York Times was a good example when claiming that, “the clinic accident at the center of the Alabama case echoed a pattern of mistakes in the reproductive health industry.”1
Especially in the U.S., where IVF clinics, unprecedented for any other area in medicine, under federal law, must report every IVF cycle outcome to the federal government (the CDC) and the FDA tightly regulates (and regularly inspects) the clinical safety of all IVF clinics, this statement by one of the country’s leading media voices was, of course, blatantly incorrect.
Until fully resolved, the legal environment for IVF clinics in Alabama unfortunately may remain precarious. For the CHR this means that Alabama–based infertility patients for some time to come may find themselves in some limbo regarding their treatments. Because especially female infertility in many cases can be strongly age-dependent, delays can have significant adverse consequences. The CHR for that reason offers a “hotline” to Alabama infertility patients who amid treatments or for other reasons may have questions and/or require immediate help. Because of its national and international clientele, the CHR routinely works with long-distance patients from all over the U.S. and the world. Please call the CHR at (212) 994 4400 or e-mail us at arata@thechr.com and let our staff know you are calling from Alabama. Our staff will make every possible effort to get you in touch with one of our physicians within 24 hours.
The same applies to our colleagues at Alabama IVF clinics: If you have patients who need immediate attention, please contact us in the same way. One of our physicians will on the same day be made available for a (free) physician-to-physician conversation.
Finally, the CHR is also exploring third-party sources that may make available travel reimbursements for Alabama patients who, because of current circumstances, have to come to NYC for treatments.
REFERENCE
1. Ghorayshi A, Kliff S. The New York Times, February 23, 2024;pA18
CooperSurgical’s legal troubles
According to another e-mail from Griffin Jones, founder-owner of Fertility Bridge, on January 24, 2024, CooperSurgical’s legal problems regarding one of the company’s embryo culture media are far from over. In an attached article, Ron Shinkman noted that two couples are currently suing CooperSurgical for the destruction of their embryos by “faulty” embryo culture media.
The lawsuits were filed in Los Angeles County Superior Court through the local law firm, Pfeiffer Wolf, claiming that the company did not sufficiently test the media before sales, resulting in a formal recall notice on December 5, 2023, for three lots of media. The lawsuits further alleged that those lots of culture media were “toxic” to human eggs, sperm, and embryos. They also alleged that the company’s recall “intentionally did not immediately disseminate notice of the recalled lots publicly or throughout the IVF community.” The company, basically acknowledged this in its recall notice, noting that it had received a large number of complaints regarding these three lots and warned about “impaired embryo development before blastocyst stage.”
As of February 17, 2024, according to The New York Times, at least eight patients have filed lawsuits over two months around the U.S., involving the loss of more than 100 embryos. Based on a recall notice by the FDA for almost 1,000 bottles of culture media, the article estimates that as many as 20,000 patients could have been affected.
The CHR does not routinely use CooperSurgical’s embryo culture media and was not affected by this recall.
REFERENCE
1. Kliff S, Ghorayshi A. The New York Times. February 17, 2024, p3
Several IVF clinics have stopped offering monitoring for outside patients
Ever since IVF clinics came to be, it was understood that they would make themselves available for monitoring visits in IVF cycles of patients from other cities, if their treating local REIs so requested. Monitoring clinics were fully expected to charge for their services, but making this service available for traveling patients was an automatically extended courtesy to colleagues and their patients.
However, with so many other “not-for-the-better” changes in the IVF field, we have been witnessing in recent years, this courtesy is now increasingly denied. Unsurprisingly, this new trend is led by several investor-owned clinic networks. Examples of such clinic networks are Boston IVF – Eugen (recently purchased by KKR on behalf of IVIRMA Worldwide) and the Shady Grove networks (a part of the large U.S. Fertility network that just closed its NYC office after adding RMA-NY with all of its locations to its network).
The CHR considers this a disturbing development, and not only because increasing numbers of the CHR’s patients (who in over 60% reside outside of the larger NY- tristate area) and, therefore, often depend on these services, but because we see it reflective of collegiality and medical professionalism in the evolving “IVF industry” being increasingly replaced by a highly competitive
14 | The Voice
commercialization of the field by non-medical and purely financially-driven (extensively reviewed in the November-December 2023 issue of the VOICE) investor interests, which already control over half of U.S. IVF cycles.
The CHR decries that so many colleagues, after being routine practice for decades, decided to abandon this courtesy service and continue to offer this service to colleagues and their patients during visits to NYC seven days a week and 365 days a year, even if they, themselves, have stopped offering these services.
Mount Sinai sued for reducing services at the Mount Sinai Beth Israel Hospital and New York Eye and Ear Infirmary as part of a plan to sell their assets and real estate
According to a report in Becker’s Hospital Review, a coalition of community organizations filed a lawsuit against NYC’s Mount Sinai Health System alleging that the health system, after its merger with Continuum Health Partners, deliberately reduced services and staff at Mount Sinai Beth Israel and New York Eye and Ear Infirmary to sell the two hospitals’ assets and real estate.1 The lawsuit claims that, “Mount Sinai Beth Israel has been intentionally creating ongoing, dangerous conditions at its hospital to bolster its ability to sell off the hospital’s real estate portfolio.” Due to increasing losses, Mount Sinai, as we previously reported in the VOICE, announced in September of last year that it was planning on closing Beth Israel completely. The lawsuit also claims that Mount Sinai on purpose closed profitable units, such as Labor and Delivery, the neonatal ICU, and almost all ENT services at the Infirmary to have a reason for closure of the hospitals which requires the local government’s approval. A judge since temporarily blocked Beth Israel’s closure.2
REFERENCE
1. Diaz N. Becker’s Hospital Review. February 7, 2024. https://www. beckershospitalreview.com/legal-regulatory-issues/lawsuit-claims-mountsinai-cut-services-to-sell-real-estate.html#:~:text=The%20lawsuit%2C%20 obtained%20by%20Becker’s,department%20rules%2C%20the%20state%20 constitution
2. Cass A. Becker’s Hospital Review, February 12, 2024. https://beckershospi talreview.com/finance/judge-temporarily-blocks-beth-israel-closure.html
Is Kindbody in trouble?
Kindbody, a roughly 6-year-old company with headquarters and clinical services in NYC, described itself in a recent press release as “the leading fertility clinic network and global family-building benefit provider for employees,”1 and in 2023 claimed a $1.8 billion market valuation. It now appears to be going through some rough waters, with everything recently documented in three articles By Jackie Davalos in Bloomberg. 2-4
On February 1, 2024, those three articles were moreover summarized by Rosemary Scott in one of Griffin Jones’ periodic e-mails from Fertility Bridge under the article title, “Kindbody and Bloomberg. What started the three-article series and what journalists expect next.” Davalos’ three articles appeared on October 13,2 November 29,3 and December 22, 2023.4 After interviewing over 30 current and past employees of the company, the first article
reported on substantial understaffing in many Kindbody clinics and inconsistency in applying safety protocols. The company subsequently disputed to be understaffed but acknowledged (at least in one case) the mislabeling of embryos. Paradoxically, according to Scott, the company despite this acknowledged incident, still claimed that “no Kindbody laboratory has had an incident, accident, or other issue that is unusual to what occurs in IVF laboratories in general.”2
This statement is completely inconsistent with an acknowledgment of mislabeling of embryos and, likely was a factor in Davalos expanding her investigation of the company. In her second article in November, she reported that Kindbody significantly (by 22.5%) reduced its 2023 revenue forecast from $240 million to $186 million and was seeking to raise in financial markets an additional $50 million before the year’s end. Davalos claimed evidence that the company, contrary to earlier statements, until mid-2024 would not reach profitability, in the meanwhile through 2023 losing ca. $7 million every month.
Davalos also reported that Kindbody was planning a change in CEO, replacing Annbeth Eschbach once a search firm recruited (for a fee of $750,000) a suitable candidate. Eschbach is the founder of Exhale Enterprises, a spa and fitness business she sold to Hyatt Hotel in 2017. In May 2019, She replaced Gina Bartasi as CEO, a co-founder of Kindbody, and a very successful serial entrepreneur in the fertility field. in addition, among other administrative management changes, Gregory Poulos, who was the company’s President, stepped down from his position last September.
In her third article, Davalos reported increasing pressure on physicians from management to increase their monthly IVF cycle numbers by at least 12 to increase income and facilitate the plans of the company to go public. She also noted resistance from physicians who described these demands as “unreasonable” and expressed concerns that such pressure could lead to the performance of unindicated IVF cycles.
As Scott also reported, this may not have been Davalos’ last article on Kindbody. Should other sources come forward with new information, we can expect to hear from her again.
REFERENCES
1. Kindbody News Release, October 16, 2023, https:///www. prnewswire.co/news-releases/kindbody-continues-sci...%20 announced20ththe,HCLD%2C%20as%20Chief%20Scientific%20Officer.
2. https://www.bloomberg.com/news/articles/2023-10-13/ kindbody-fertility-clinic-embryo-errors-spotlight-ivf-business-risks
3. https://www.bloomberg.com/news/articles/2023-11-29/startup-kindbodyseeks-to-raise-50-million-cuts-sales-outlook?embedded-checkout=true
4. https://www.bloomberg.com/news/articles/2023-12-22/kindbody-fertili ty-clinic-pushes-doctors-for-more-egg-retrievals
Continuing problems for the genetic testing industry; Invitae and 23andMe
As we have repeatedly reported in these pages – especially regarding PGT-A testing, troubles in the genetic testing industry are nothing new. By now serious problems involve even some of the major genetic testing companies like Invitae and 23andMe. Based
The V oice | 15
Continued on page 16
Continued from page 15
on reports in the media at the time of this writing, the former is preparing to file for bankruptcy,1,2 while the market values of 23andMe have with surprising speed gone from $6 billion to almost nothing.3 The company, according to media reports, is considering a restructuring into two separate companies, though even this potential resolution will depend on the ability to raise additional investment funds from outside sources.4
These two companies serve quite different genetic testing markets. Invitae, backed by the (by now somewhat infamous) SoftBank Group, has become a substantial player in the PGT-A testing market. For the infertility field, Invitae’s ultimate fate will be much more relevant than that of 23andMe. Standby for further news, as they develop.
REFERENCE
1. Business Briefs, The New York Post, February 6, 2024 (sources Reuters, Dow Jones, AP)
2. Biswas S. The Wall Street Journal., February 5, 2024; https://www.wsj. com/articles/softbank-backed-medical-genetics-company-invitae-pre pares-for-bankruptcy-d468f120
3. Winkler R. The Wall Street Journal, January 31, 2024; https://www.wsj. com/health/healthcare/23andme-anne-wojcicki-healthcare-stock-913468f4
4. Winkler R, The Wall Street Journal; February 8, 2024, page B5
Where have all the physician-scientists gone?
A recent report in Medscape addressed the precipitous drop over 30 years by two-thirds in physician-scientists in the U.S., from 4.7% to 1.5%.1 This is even though residency and fellowship programs have added research years to many training programs.
Nowhere more apparent than in REI fellowships
REI fellowships several years ago added a ridiculous third year to the prior two-year fellowship in the hope of producing more physician-scientists in the field. However, this change achieved exactly the opposite, as almost all graduating fellows after three years of fellowship (with ridiculously low salaries and often significant outstanding student loans) couldn’t get quickly enough into private practice.
That this three-year fellowship has not worked out as expected by now should be very obvious; some colleagues in academia, still resist shortening the fellowship back to only two years. Even that in the CHR’s opinion is too long to train an OB/GYN after four years of residency if all she/he is looking forward to is a career in clinical fertility practice. In such cases, a single year of clinical fellowship appears more than adequate. For those few wishing to become physician-scientists in REI, a second research year can then be attached, but three years of REI fellowship when probably less than five percent of fellows remain in academia is not only wishful thinking, but also a total waste of time and resources, serving nobody.
Why the general disinterest in science?
What are then the reasons for this radical decline in interest in becoming a physician-scientist? There, likely, are several, and, as the next discussed item well demonstrates, academia has not only become very unpopular as a goal, but dissatisfaction about academia is also very high among those already in academia.
The above-quoted article suggested that one reason may be how difficult grant funding has become: Only roughly 12% of NIH applications are funded currently on average,1 but the percentage was not much better 30 years ago, and, yet satisfaction in academia was much higher. The answers, therefore, are much more complex and reflective of much larger societal changes: For example, 50 years ago, the top of every college class went into medicine but that hasn’t happened in decades. Starting in the 1960s and 1970s, these students instead went to Wall Street, and in more recent years they have been going into high-tech and start-ups.
Then there are other major societal changes: Thirty years ago, females were a still relatively small minority among medical students; nowadays they are in the majority. When it comes to reproductive medicine, 40 years ago female residents in OB/ GYN started to be accepted (before that, OB/GYN – like surgery - paradoxically was considered an in principle male specialty, and female residents were, at best, only a small minority) Today it is the other way around: If a male is accepted into an OB/GYN residency, that is the exception. Due to this, females only in more recent years also started to fill leadership positions in medicine.
Finally, one also must acknowledge that not only the type of student choosing medicine as her/his career has changed, but medical schools, like other schools of higher learning, also changed their acceptance criteria in comparison to 30 or more years ago. As this subject, especially recently, has become visibly more controversial than in decades, this is not the spot or the time to address this subject further. Only so much: Currently, individuals with different personality characteristics and social interests choose medicine as their career than even 30 years ago. Medical schools moreover purposefully, like other teaching institutions, have over recent years increasingly deemphasized meritocracy in favor of other social considerations, while 30 years ago meritocracy still largely dictated student selection.
This is not to judge one way as better or worse. As noted, we leave this important discussion to another occasion. However, one cannot deny that all of these social changes impact the people who nowadays practice medicine in comparison to those who practiced medicine ca. 30 years ago. Therefore, it should not be a surprise that these differences end up affecting practice choices. If society wants more physician-scientists than society currently produces (and the CHR strongly believes that this is essential if U.S. medicine is to maintain its currently already slipping leadership role in the world), then society must find ways to incentivize the current generation of young physicians to become physician-scientists. The old methods and motivations no longer seem to work!
REFERENCE
1. Chaudhuri A. Medscape, January 26, 2024; https://www.medscape.com/ viewarticle/99985
The “great resignation” from academia
A recent article in Nature magazine1 rekindled the discussion the magazine had raised earlier when suggesting that the great resignation that had started in 2021 with the COVID-19 pandemic
16 | The Voice
had by 2022 also hit academia. According to this more recent article, this trend has been continuing through 2023, with faculty turnover continuing higher than in pre-COVID-19 years and changed motivations: According to a career consultant interviewed, academic flight used to be caused by the unavailability of academic jobs; now, however, even tenured academics walk away, “because they, simply, can’t stand it anymore.” As noted in the preceding commentary, people have changed over the last 30 years. They have different appreciations and desires in life.
REFERENCE
1. Nature 2023;62(4):461-463
CHR news
The CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, on December 17, 2023, upon invitation gave a plenary lecture on, “Using science to enhance precision medicine in IVF,” at the annual Ovarian Club – Asia scientific meeting in Hong Kong.
He was also invited to present on February 8, 2024, at Lenox Hill Hospital in NYC a Journal Club for the REI division and REI fellowship program of Northwell Health (see photograph) that was concomitantly electronically transmitted to the program’s Long Island campus. The subject was “Precision Medicine in REI.”
The Northwell Health REI program has a new Chief in Tomer Singer, MD, MBA, who, years ago, as a resident at Lenox Hill, rotated through the CHR and published some papers with the CHR staff. We congratulate him on his new appointment and welcome him back to his original institution.

The CHR’s Norbert Gleicher, MD upon completion of the Journal Club for the Northwell REI program. Next to Dr. Gleicher (in white coat) the new Chief of the Northwell REI division, Tomer Singer, MD, MBA Both are surrounded by fellows and embryologists from the Northwell program.
Long COVID, - the new cash cow?
An article in JAMA 1 recently noted that clinics/businesses that used to sell unapproved stem cell and exosome therapies for COVID-19 are now targeting individuals with post-COVID conditions and/or long COVID-19. Neither treatment has been approved by the FDA. Most clinics function in the U.S., but an almost identical number of clinics serving primarily the U.S. market were located in Mexico. Patients with long COVID are especially vulnerable to such schemes that, according to the article go for anywhere between $2,950 to $25,000.
REFERENCE
1. Eastman Q. JAMA 2023;330(24):2326-2327
The financialization of healthcare
A recent article in the New England Journal of Medicine offered what we believe is a new term in its title, “The Financialization of Health in the United States,” 1 contrasting the new term, “financialization” from “corporatization” which according to the article, has been the focus of health care markets since the 1980s. The article further defines the new term as the “transformation of public, private, and corporate health care entities into salable and tradable assets from which the financial sector may accumulate capital,” in the process generating short-term profits which then are distributed to financial interests outside of health care and general citizenship.
In the process, companies are loaded up with substantial debt and become subject to quick (often repeated) buy and sell cycles, with private equity investment funds making a quick profit for their partners/owners. For example, we in the NovemberDecember issue of the VOICE noted that the Boston IVF chain of IVF clinics within a few short years had three ownership changes.
The central question the article likely tries to address is whether, considering the increasing influence the financial sector is exerting over national health care, the U.S. is getting “a good deal.” Though not ready to offer a final answer, a significant degree of skepticism appears to abound.
REFERENCE
1. Bruch et al., N Engl J Med 2024;390(2):178-182
The first at-home sterile insemination kit approved by the FDA

Image source: https://www.pherdal.com/
A company called PherDal Fertility Science, Inc, founded by Illinois biologist Jennifer Hintszsche, PhD, received recently approval from the FDA for the marketing of a sterile at-home insemination kit after 34 babies were born from the first 200 proof-of-concept kits from the company,1 17% live birth rate. Hintszsche in the article by Fox News Digital was quoted to have commented that, “even saying that still gives me goosebumps,” which is somewhat bizarre since self-inseminations – without
The V oice | 17
Continued on page 18
Continued from page
commercially available kits – have been very common for decades and the live birth rate of 17% reported by the company in a self-selected patient population with alleged infertility is by no means surprising.
What pregnancy and live birth rates will be after at-home self-inseminations will, of course, depend on whether a couple has a fertility problem, what that problem is, and how old they are. A 2017 study for example reported that in 67% of cases of unconsummated marriage – a quite frequent background to home-inseminations, the underlying cause was vaginismus in the female, 22% of cases were erectile dysfunction cases in the male, and 11% of cases were premature ejaculation of the male. Even in this best-prognosis group of patients, as one would expect, clinical pregnancy rates, however, varied with age: 69% at ages 20-33, 43% between ages 3336, and 25% above the latter age.2
This does not mean that a sterile, easily available self-insemination kit does not have advantages over a self-improvised set-up, but that will at least to a degree depend on the cost difference.
REFERENCES
1. Stabile A. Fox News Digital, January 26, 2024. https://www.foxnews.com/ health/fda-approves-first-home-sterile-insemination-kit-help-infertili ty-goosebumps
2. Banerjee K, Singla B. J Hum Reprod Sci 2017;10(4):293-296
AI for embryo selection?
This time, Marc Siegel, MD, one of Fox News’ principal medical commentators was the one who exaggerated1 and misrepresented a report from an Israeli start-up, called AI-IVF, which now, for some time, has been marketing its AI program under the claim that it could select non-invasively aneuploid embryos during IVF, thereby improving IVF outcomes by 30%.
However, simple logic establishes beyond reasonable doubt that this is pure nonsense because once eggs are retrieved in an IVF cycle, their cumulative pregnancy and live birth chances can no longer be improved. The effect of post-retrieval management indeed can only be neutral and, if there is a post-retrieval effect, it can only be a negative one from poor embryology.
Siegel may have been misled by his affiliation with NYU (where he is a professor of medicine) since NYU’s fertility center has for many years been an outspoken proponent of chromosomal testing of embryos (PGT-A). Even though the program has significantly progressed toward a more correct understanding of PGT-A and now, finally, at least supports the transfer of selected so-called “mosaic” embryos,2 this clinic still appears to fail to understand that, once a cohort of oocytes has been retrieved in an IVF cycle, that cohort’s cumulative pregnancy and live birth chances can no longer be positively affected.
REFERENCE
1. Stabile A. Fox News, January 26, 2024. https://www.foxnews.com/health/ fda-approves-first-home-sterile-insemination-kit-help-infertility-goose bumps
2. Kelly et al., Fertil Steril 2023;120(4, Suppl.): E185
 Photo Credit: New Scientist
Richard Horton, OBE, FRCPCH, FMedSci
Photo Credit: New Scientist
Richard Horton, OBE, FRCPCH, FMedSci
, The Lancet’s longstanding editor-in-chief, is a person of considerable influence, not the least because The Lancet currently holds the highest impact factor ranking of any journal in the world. Though a medical journal, The Lancet – even before Horton’s editorship – never hesitated to wade into worldwide political controversies. Upon ascending to the editorship, Horton (politically left of center) only further enhanced the journal’s involvement in political issues and especially started expressing an, often, rather anti-Israeli tone in The Lancet, which had some critics even accusing him of fostering antisemitism.
In 2014, during the last big military conflict between Israel and Hamas (“Operation Protective Edge”) before the current war initiated last October 7 by the murderous attack of Hamas terrorists and abduction of hundreds of living, wounded, and dead Israeli and international citizens, Horton was severely criticized for publishing in The Lancet a rather blatantly antisemitic article by a group of Arab public health experts. Amidst that criticism, Horton, who never before had visited Israel, was invited by a group of Israeli physicians from Haifa’s Rambam Medical Center to visit Israel.
In what he later described as an “intensive visit, which offered opportunities for discussions with Arab Israeli physicians and medical ethicists” he was confronted “with a new awareness of Israel’s positive aspects that did not reach Britain.”1 Interestingly, The Lancet’s tone regarding Israel since then has changed and while still trending more to the left (and toward the Arab positions) became more balanced.
A recent personal commentary by Horton in his weekly “Offline” page in The Lancet amid the current Israel-Hamas war confirmed this assessment and deserves notice:2 In this article, he was direct in criticizing the worldwide protests in support of Hamas and minced no words when accusing Hamas of blatantly lying when claiming that its members had not deliberately killed, raped, and tortured civilians. He also categorically rejected Hamas’ claim that the October 7 events represented “legitimate resistance” and described it as an act of “singular barbaric violence” and “terror- pure and simple.” He also was correct when noting “that those marching in the streets in the West on behalf of Hamas don’t understand the terrorist culture that is projected by Hamas.”
As someone who earlier had acknowledged that seeing things with his own eyes (even for just a few short days) had significantly changed his understanding of the Israeli-Palestinian conflict, he understood well how uninformed many, if not most, of the protestors are who at times cause havoc in our streets (and those of other
18 | The Voice
The Lancet’s Richard Horton on the Israel-Hamas war
17
countries), - a point also well-documented by media after interviewing protesters here in the U.S., but also in other countries who were protesting under the banner “from the river to the sea,” without even being able to name the river or the sea they were talking about. Suffice it to say that their knowledge of the history of the region is often equally lacking.
Still clearly at the left of the political spectrum, Horton by no means can be viewed as a neo-Zionist. Very much to the contrary, even in the above-noted piece we here found it important to acknowledge,2 he, unsurprisingly, also noted the destruction, killing, and suffering in Gaza, and expressed concern that the many deaths among Gazans will only breed a new generation of radical terrorists, and called for dialog in place of violence, a message he expressed in even more urgent language in another “offline” article in The Lancet more recently.3
While we here at the CHR have frequently disagreed with Horton in the past, disagree with him also on some of his opinions regarding the current Israel-Hamas-Hezbollah war and, likely, will continue to disagree with him on many more issues into the future, we have at the same time to acknowledge our growing respect for his understanding of how closely interwoven medicine often is with politics, for his documented openness to change his opinion if confronted with appropriate evidence and, most of all, for his willingness to point out barbarism by whoever such acts are performed.
REFERENCES
1. Siegel-Itzkovich J. The Jerusalem Post, October 12, 2014. https://www.jpost.com/israel-news/health/ lancet-editors-visit-to-israel-still-causing-stir-378665
2. Horton R. Lancet 2023;40210424):15
3. Horton R. Lancet 2024;403(10425):420
Katsuhiko Hayashi, one of Nature magazine’s 10 Who Shaped Science in 2023
Everybody in reproductive medicine knows Katsuhiko Hayashi, PhD, who recently moved his lab in Japan to Osaka University (see photo) because of his spectacular achievements in reproductive biology. In 2016 his lab reported reconstitution in vitro of the entire cycle of the mouse female germ line.1 The authors in that paper produced mouse eggs from mouse stem cells, fertilized the eggs, and produced multiple generations of healthy pubs from those embryos.

His most recent achievement, published in 2023, and the reason why Nature magazine named him among its annual 10 Who Shaped Science in 2023, was his group’s paper that reported mouse egg production from male mouse cells.2 These experiments produced only seven live pubs from 630 embryos, but that was more than enough to produce a milestone in reproductive biology, pointing to almost unimaginable possibilities in producing parental genetic compositions of human embryos in the future. Congratulations Katsuhiko!
REFERENCES
1. Hikabe et al., Nature 2017;539:543
2. Murakami et al., Nature2023;615:900-906
Yes, some authors are too productive!

Commenting on a recent preprint,1 a news article in Nature magazine recently summarized increasing concern about “over-productive” authors. Can that be, you may ask? Though it may be hard to believe, there exists a good number of authors who produce over 60 papers annually, basically publishing a new paper every five days.2 Moreover, the number of prolific authors like that has almost quadrupled over the last decade.1
In all areas of scientific exploration, medicine was the by far most prolific field with over 1,000 such authors, with the second-in-line having only roughly 600. Among countries, quite surprisingly, Saudi Arabia was the leader with almost 70 “over-productive” authors, followed by Italy (slightly over 60), and India (slightly over 50). Then comes nothing for quite some time, followed in declining order by South Korea, Spain, Thailand, Pakistan, and Russia, all between ca. 10 and 25. This is just another sign of the publication crisis in medicine we previously discussed in the November-December issue of the VOICE in more detail and are also addressing further in this issue of the VOICE in the Literature Review section.
REFERENCES
1. Ioannidis et al., bioRxiv 2023; https://doi.org/k9b3
2. Conroy G. Nature 2024;625:14-15
Another opinion on private equity investments in medicine
Without wanting to be repetitive after having addressed this issue also in detail in the November-December 2023 issue of the VOICE, just a brief note about another warning opinion about increasing costs and, likely, poorer quality of health care as the consequence of purchases by private equity interests of health care providers with the by-far most provocative title so-far. The author, a physician in Laboratory and Computer Sciences at Massachusetts General Hospital in Boston, MA,1 chose as the title of his article, “Private equity and medicine: A marriage made in hell,” and this title alone quite clearly reflects his sentiments on the subject.
REFERENCE
1. Bruch et al., N Engl J Med 2024;390(2):178-182
Photo Credit: Kyushu Univeristy
The V oice | 19
Prof. Katsuhiko Hayashi, Professor Osaka University, Osaka, Japan
Building on the success of the 2023 conference, the FRMC over three conference days will once again present a unique program in reproductive medicine, connecting in a single lecture hall between basic science and clinical practice, in the process facilitating translational connections between bench and clinic. As in preceding years, the principal purpose is demonstrating to clinicians what is possible and to scientists what is needed. The intent is not to dream about the future, but to demonstrate what can already be achieved.
“To think differently” has been the principal motto of the FRMC since the beginning and will remain that, as questioning mainstream thinking has been at the core of the conference’s success since its beginning. The FRMC in addition also frequently premieres new treatment paradigms.
As new findings are reported in basic science and clinical journals, the conference content evolves over the preceding year. Since the embryo contains universal information about almost everything in human biology genetically, - life, death, regeneration, immune tolerance, etc., the earliest stages of embryo development never fall out of fashion and have always occupied an important place on the program of the FRMC. While several big themes, such as reproductive genetics, the aging of infertile patient populations, “add-ons” to IVF practice, difficulties in IVF cycle outcome reporting, the relevance of the female immune system to fertility, and others that have been addressed before will return with hopefully new data, brand-new subjects can also be expected. For example, obesity is a rapidly growing worldwide health problem also adversely affecting female and male fertility as well as fertility treatment success. Very successful, newly-to-market anti-obesity drugs must be integrated into routine infertility care of obese patients. Another big theme in the 2024 FRMC conference will be the ethics of infertility practice because of the rapidly expanding takeover
of infertility practice by outside financial interests; a subject gaining in urgency by the day.
The FMRC can proudly point out to have affected engrained, ineffective, and, at times, harmful daily practice patterns in IVF long before other conferences even noticed. This included preimplantation genetic testing for aneuploidy (PGT-A) and, more recently, the long-standing concept of embryo selection in general, single embryo transfer for everybody, and blastocyst culture for everybody. Worldwide declines in IVF live birth rates since 2010-2013 have still not attracted the attention they deserve. Never bashful in addressing controversies, FRMC 2024 will stay the course in attempting to define the underlying causes for this observation.
The publication crisis in medicine will also have to be addressed, considering the constantly increasing number of paper retractions, even in very prominent journals, involving very prominent individuals. Related is also the recognition that what is considered evidence-based medicine must be accompanied in parallel by “real world data” studies, as carefully planned prospectively randomized studies can never fully reflect what happened in “real-world” applications of treatments.
In short, following the annual lightening of New York City’s famous Christmas tree at the Rockefeller Center that formally opens the city’s Christmas season in only several days, the 2024 FRMC will not only offer what, likely, is the most interesting professional conference in reproductive medicine anywhere in the world, but also a unique time to visit New York City in one of the city’s most beautiful periods. Registration has opened at https://whova.com/portal/registration/frmc_202412/. Please go to https://www.foundationforreprodmed.com/ for further information.
ADVERTISEMENT 20 | The Voice



28 years old; I had three miscarriages in a row, and now can’t get pregnant for over 18 months. My gynecologist says I’m too young to worry, but I do worry.
Your gynecologist is, unfortunately, very wrong and you, fortunately, are very right in worrying. It is impossible to reach a diagnosis for you simply based on the little we so far know about you, but three consecutive miscarriages fulfill even the criteria for “repeated pregnancy loss.” This means that, simply for this reason, you should have had a diagnostic work-up because there, likely, is a reason behind your repeat miscarriages.
Without testing, in most cases, it is impossible to say what the underlying cause may be; but as you describe your history, we already have a strong suspicion which will have to be confirmed.
You also pointed out a second very important circumstance, namely that for over 18 months you have been unable to conceive. This, even at your very young age, defines you as a so-called secondary infertility patient, which means that you

became infertile after initially being fertile. The occurrence of secondary infertility after prior repeated miscarriages in almost all cases is a presentation typical for so-called immunologic pregnancy loss.
The natural history of immunologic pregnancy loss is characterized by women, first, experiencing (often more than one) pregnancy loss(es) and then, at some point, no longer can get pregnant. When at that point undergoing a diagnostic investigation, these women often demonstrate evidence for what is called premature ovarian aging (POA), by some also called occult primary ovarian insufficiency (oPOI). This means that they have fewer eggs left in your ovaries than ca. 90% of women of your age. Like repeated miscarriages, POA is also closely associated with immune problems.
Your diagnoses likely, are (i) repeat-immune aborter and, already at a relatively young age, (ii) POA, a diagnosis that affects ca. 10% of all women. We recommend that you see a fertility specialist who also has expertise in immunologic infertility.
Experts in the latter are called reproductive immunologists and there are only relatively few such experts around. The CHR is lucky in that its Medical Director and Chief Scientist,
Continued on page 22
The V oice | 21

Continued from page 21
Norbert Gleicher, MD, is one of the best-known reproductive immunologists in the country and is known as one of the fathers of reproductive immunology in the country. He in 1979 was among the founders of the American Society for Reproductive Immunology (and the society’s first VP) and, for ca. 20 years, was also the editor-in-chief of the society’s official journal, the American Journal of Reproductive Immunology (AJRI).
POA is unfortunately a progressive condition that we have not yet learned to arrest. Time may not be on your side and we recommend that you don’t waste time in seeing somebody with appropriate qualifications. Remember, simply based on your history we can only suspect your multiple diagnoses. They now must be confirmed with a few simple tests which do not have to cost a fortune. Because of your young age, with a little help you, likely, should still have no problems conceiving and, with proper treatments, should also have no problems in avoiding yet another miscarriage.1
REFERENCE
1. Sung et al., J Reprod Immunol 2021;148:103369
My husband and I are older. We got married when I was 42 and he 53. We want a child-, but now are scared of having one with Down’s Syndrome or Autism
We hear you and, almost daily, many others with similar fears. A little information is sometimes more dangerous than no information and your question is a good example of this. We hope that the source of your information was not a physician



because physicians, even if not in reproductive medicine, should know better. Here is a little bit of information that, hopefully, will reduce your concerns about having a baby with chromosomal abnormalities at your current age.
Let’s start with warranted concerns: It is true that chromosomal abnormalities in eggs increase with advancing female age (though not with advancing male age) and, therefore, chromosomal abnormalities in parallel also increase in embryos. However, this does not mean that chromosomal abnormalities in parallel also increase in pregnancies and the reason is simple: nature is smart, and nature does not want us to have “abnormal” offspring. Nature has built-in three well-working defenses as women get older: The first is that a large majority of human embryos with significant chromosomal abnormalities are not allowed to implant. Only a relatively small number of chromosomal “abnormal” embryos slip through this first line of defense and do implant. But that “defeat” of nature’s defense usually does not last very long before the second defense kicks in and that is usually a quite early miscarriage before fetal heart, either as a so-called chemical pregnancy (before pregnancy becomes visible on ultrasound) or an early clinical pregnancy (visible on ultrasound but before fetal heart). Only relatively recently discovered,1 there, indeed, exists also a third natural mechanism in early-stage embryos that prevents the birth of chromosomal-abnormal embryos and that is the ability of embryos to “self-correct.” What that means is that embryos at those early stages can get rid of chromosomal-abnormal cells, which allows them to continue to develop as chromosomal-normal euploid fetuses.
Because of these three defenses, nature puts up against abnormal pregnancies, when one looks at the risk of, for example, having an ongoing pregnancy with Down’s syndrome (the most frequent human chromosomal abnormality) is at age 20 only 1/1667 and only 1/526 for all chromosomal abnormalities combined, - and even at age 40 it is only 1/106 (less than 1%) and for any chromosomal abnormality 1/66 (1.51%) (see also the Table):
Table: Chromosomal abnormalities in pregnancies with advancing maternal age _______________________________________________
Maternal age Down’s Risk for all chromosomal abnormalities
20 ...……………………….. 1/1667 1/526
30 …………………………. 1/952 1/385
35 …………………………. 1/378 1/192
40 …………………………. 1/106 1/66
45 …………………………. 1/30 1/21
49 …………………………. 1/11 1/8
These numbers are based on miscarriage assessments of products of conception. For several reasons, especially miscarriage assessments, mostly performed after cell cultures were established from trophoblast (extraembryonic cell lineage) lead to somewhat exaggerated assessments of aneuploidy since, in contrast to the embryonic cell lineage that forms the fetus, the extraembryonic cell lineage does not have the same capability to self-correct from aneuploidy.1
_______________________________________________
_______________________________________________
22 | The Voice




The risk of an ongoing, chromosomal abnormality with advancing maternal age goes from incredibly low only to very low. Moreover, so-called non-invasive prenatal blood testing (NIPT) in very early pregnancy detects even those small risks in over 90% of cases and 99.9% of cases with a little later performed chorionic villous biopsy (CVS) or amniocentesis.
The story with advanced male age is quite different. As already noted, male age does not affect the risk of chromosomal abnormalities. Advanced male age is, however, associated with increased autism risk. Unfortunately, a reliable way of testing a pregnancy for autism does not exist. But once again, the increase in risk is small: In the absence of a known risk in a pregnancy for the fragile X syndrome (a rare condition in offspring that can be diagnosed), the risk of having a child with autism to parents in their 20s has been reported in the literature at about 1.5%; the risk to parents in their 40s (mostly representing paternal age risk) in comparison will be only ca. 1.6%.
In summary, while at your older ages, your risk to have a child with a chromosomal abnormality and/or autism is, indeed, higher than at younger ages, we don’t see it as substantial enough a risk not to have children with your eggs and semen at your ages. To reduce your risk, you, of course, have the option of working with young donor eggs and/or young donor sperm; but we do not believe that the risks outlined here really warrant such a decision.
REFERENCES
1. Yang et al., Nat Cell Biol 2021;23:314-321
I was diagnosed with systemic lupus erythematosus (SLE) and have been in full remission since age 32. Now 35, I have been unable to conceive for over two years and have failed two IVF cycles. Could there be a link with my history of SLE?
Coincidentally you are addressing in your question a very important issue in reproductive medicine, - the close link between female fertility and autoimmunity, which is also the subject of our Case Report of The Month below. After this answer to your question we, therefore, suggest you also read the below-presented case report which demonstrates in more detail how autoimmunity often mingles with female fertility/infertility. Since you are a patient diagnosed with a classical autoimmune disease (SLE), even though you are in remission from your disease, this does not mean that your autoimmunity no longer affects your fecundity (i.e., ability to conceive). It, indeed, very likely still does and it, moreover, also still, likely, increases your miscarriage risk once you do conceive. Autoimmunity and pregnancy have one very important thing in common: they are very dependent on each other, - though on an inverted scale.
Both are dependent on the immunologic tolerance of the host; The human’s immune system must be tolerant to “self” (i.e. all biological structures making up our bodies). Every time this tolerance is broken, our immune system will start reacting against components of our bodies, in most severe cases causing autoimmune diseases, for example including SLE and rheumatoid arthritis (RA). In pregnancy, the maternal immune system must

ADVERTISEMENT
The V oice | 23 Continued on page 24

Continued from page 23
be initially tolerant to the implanting embryo and, later in pregnancy, to the complete fetal-placental unit. In the absence of such tolerance, and because pregnancy is a semi-allograft (like an organ transplant or nowadays with the use of donor-oocytes even a full 100% allografts), pregnancies would in very early stages be destroyed by the maternal immune system if it had not developed tolerance toward the products of conception.
The induction of tolerance pathways by mothers in pregnancies must be similar to the pathways that guarantee in most people immunological invisibility for “self” antigens because, once the initial risk of rejection of a new pregnancy is overcome, starting in the second trimester of pregnancies many autoimmune diseases, including SLE and RA, actually clinically tend to improve.1 The explanation for this observation is that tolerance pathways induced to protect the fetus and placenta also protect from immune responses to “self”-epitopes. In other words, whatever helps to prevent rejection of pregnancy by the maternal immune system, also weakens existing immune responses against “self.”
Overall, autoimmune diseases, including SLE and rheumatoid arthritis (RA), are, however, not a good thing in pregnancy because, especially at the beginning and end of pregnancy, autoimmune disease flares are common. They, indeed, rise by ca. 60% over non-pregnant periods.2 At the beginning, such flares are, among several other conditions, associated with miscarriages, at the end of pregnancy they are associated with premature labor/delivery and preeclampsia/ eclampsia. The by far largest risk of autoimmune flares, however, exists in the immediate postpartum period and up to 5 months postpartum, when autoimmune diseases often are also for the first time diagnosed.
Whether SLE is specifically associated with female infertility is unclear; but autoimmunity in general very clearly has such an association. Moreover, SLE and other autoimmune diseases are often also associated with other autoimmune diseases. Individuals who develop an autoimmune disease, therefore, lifelong are at increased risk for other autoimmune diseases. That you were diagnosed with SLE, clearly demonstrates that you have a hyperactive immune system, and such an immune system, even when you are in remission from active SLE, still means increased flare risks at the beginning and end of pregnancy, including the postpartum months, likely increased miscarriage risk, increased risk for premature labor and delivery, increased preeclampsia/eclampsia risks, higher chances of a Cesarean section delivery, and other later pregnancy complications.
You, moreover, should not only receive treatment at a fertility clinic that also has special expertise in managing women with autoimmune diseases, but you should also maintain an ongoing relationship with a rheumatologist throughout pregnancy and into the postpartum period, preferably with admitting privileges at the same hospital where you are planning on delivering.
Similarly, you should also choose an obstetrician and/or perinatologist to take care of you during your pregnancy who also understands the close interplay between pregnancy and autoimmunity. Please continue to the Case Report for some additional explanations.
REFERENCES
1. Adams Waldorf KM, Nelson JL. Immunol Invest 2008;37(5):631-644
2. Merz et al., Dtsch Ärtzte Bl Int 2022;119(9): PMC9201458

TRYING TO REACH THE INFERTILITY COMMUNITY?
Have you thought about advertising in the VOICE?
This newsletter every month goes electronically to ca. 80,000 infertility patients, medical professionals in the field, and members of the media, with over 25% (an unusually high number) also opening the VOICE.
For further information, please contact: Ms. Alexandra Rata (212) 994-4400 or e-mail to arata@thechr.com
ADVERTISEMENT
24 | The Voice

BRIEFING
• Attempting to offer a teachable moment, every month we present in this section of the VOICE an anonymized case report from the files of the CHR.
• This case involves a 34-year-old woman who presented with a principal diagnosis of “unexplained” secondary infertility to the CHR after she had failed two IVF cycles at a different IVF center.
• We are presenting this case to point out how closely female autoimmunity intermingles with pregnancy.
• We offer special emphasis on how the CHR considers the presence of autoimmunity in infertile women in their treatments.
Case-presentation
A 34-year-old G4P0 presented to the CHR with a history of secondary infertility. She reported two voluntary terminations before age 20 and two spontaneous miscarriages between ages 28 and 30, one at ca. 6 weeks gestational age, and the other after detection of fetal heart at ca. 8 weeks. She then experienced secondary infertility since age 30.
Her past medical history was negative except for a diagnosis of juvenile idiopathic arthritis (formerly called juvenile rheumatoid arthritis1) somewhere between ages 3-4 years, for which she received undefined “treatments” for approximately one year. Some children have symptoms only for several months, while others may suffer for much longer. Many, if not most children with juvenile arthritis later become adult patients with rheumatoid arthritis.2
However, since approximately age 5, she had been off medications and had not encountered a recurrence of the disease or what she considered to be significant symptoms, except for mild arthritic pains for a few weeks in small joints of her hands after both of her two spontaneous miscarriages. Those, however, were not significant
Continued on page 26 The V oice | 25
Continued from page 25
enough to seek out medical care. Neither of her two spontaneous miscarriages required any follow-up treatments. Ploidy of products of conception was not determined, nor did the patient’s obstetrician-gynecologists initiate a diagnostic workup after either the first or second miscarriage but encouraged the patient to continue pregnancy attempts.


After the patient failed to conceive for over 18 months after her second miscarriage, she returned to her gynecologist who, without further investigations, referred her to a fertility clinic. Now almost 33 years old, there she underwent basic infertility testing which, based on abnormally high FSH for age (11.8mIU/mL) and abnormally low AMH for age (0.85ng/mL) led to the finding of low functional ovarian reserve (LFOR) for age. Based on a rather irrational) treatment guideline of her insurance company, the clinic had to treat her with three intrauterine insemination (IUI) cycles under clomiphene citrate stimulation before the insurance company would cover IVF. She failed those cycles and was at that point advanced into IVF. Two IVF cycles under gonadotropin stimulation followed, which resulted in 5 and 11, retrieved oocytes, and 1 and 2 blastocyst-stage embryos, respectively, which by PGT-A were determined to be chromosomal-“abnormal” and were not considered transferrable. Paradoxically with a sign-out diagnosis of “unexplained” infertility from her clinic, by that point, this 34-year-old patient consulted with the CHR.
CHR diagnoses and conclusions
Reviewing the patient’s history, the CHR immediately concluded that she was not a patient with “unexplained” infertility. As repeatedly before noted in the pages of the VOICE, the CHR considers this diagnosis an oxymoron because whether an infertility diagnosis can or cannot be reached, of course, depends primarily on how deeply an investigation is pursued. Based on her LFOR, she very obviously suffered from premature ovarian aging (POA), by some also called occult primary ovarian insufficiency (oPOI). Furthermore, we were intrigued by four findings: (i) Her history of juvenile idiopathic arthritis as a child, (ii) by her two consecutive miscarriages, with at least one occurring after fetal heart; (iii) by her developing mild arthritis in both hands after both miscarriages, and (iv) by her secondary infertility after those miscarriages. What all four findings had in common was a potentially strong link with the likelihood of having a hyperactive immune system, including evidence of autoimmunity.
The link with her history of juvenile idiopathic arthritis was obvious. Two consecutive miscarriages, with at least one occurring after fetal heart, suggested the possibility of repeat immune-mediated pregnancy loss. Moreover, flares of autoimmune diseases occur typically most often upon termination of pregnancy (whenever that may happen) and she experienced mild arthritic flares after both miscarriages; and, finally, secondary infertility following repeat immune-pregnancy loss is a common step in the natural course of immune-pregnancy loss. Based on her past medical history alone we, therefore, suspected that this patient may have so far overlooked subclinical autoimmunity which then, indeed, was quickly confirmed in an initial diagnostic work-up.
Even though she apparently had no clinical symptoms suggestive of an autoimmune condition, her testing revealed a positive ANA (1:160, speckled), a positive rheumatoid factor, and positive anti-phospholipid antibodies in IgG isotype. Aside from that, she also demonstrated the typical laboratory picture of a woman with deteriorating POA, with her FSH already at 14.0 mIU/mL and her AMH at 0.45ng/mL). As is also typical with POA/oPOI, she demonstrated severe hyperandrogenism, characterized by low testosterone, DHEA, and DHEAS, and elevated sex-hormone binding globulin (SHBG).2
Whenever we see a history of repeated pregnancy loss and of POA in the same patient, the common denominator is usually, as in this case, a hyperactive immune system, and especially autoimmunity. The underlying problem is that hyperactive immune systems are often not able to develop the required tolerance pathways properly that render the embryo (a semi-allograft) immunologically “invisible.” This invisibility is essential for implantation and early tolerance until additional and more expanded tolerance pathways are developed through fetal-maternal microchimerism and, possibly, other pathways.
26 | The Voice
Stock-photo of an 18-months-old girl with acute arthritis in her right knee
https://emedicine.medscape.com/
Treatments and outcomes
As this patient’s cause of infertility was not “unexplained,” what she really suffered from was a very insufficient diagnostic evaluation before coming to the CHR. Having a diagnosis of POA as well as repeated pregnancy loss due to a hyperactive immune system, she did not only need help to conceive but, also required support in remaining pregnant once a pregnancy had been established.
Because she was found to be hypo-androgenic, she was placed on androgen supplementation with DHEA (25mg, TID; PLEASE NOTE THE POTENTIAL CONFLICT STATEMENT BELOW). After approximately six weeks of DHEA supplementation, she was started in an IVF cycle in which five oocytes were retrieved, three were fertilized, and two day-3 embryos were transferred. With the IVF cycle start, she also was started on a baby aspirin (81mg) daily and a prednisone regimen (10mg/40mg x 4 days with hCG-trigger/20mg till pregnancy test. She conceived in her first cycle and delivered a healthy female by vaginal delivery at 38 weeks.
STATEMENT OF POTENTIAL CONFLICT
The CHR and some of its staff members own shares in a company (Fertility Nutraceuticals, LLC, doing business under the name Ovaterra), which produces a DHEA product to supplement androgen levels in hypo-androgenic infertile women. Since this case report notes that the CHR pioneered androgen supplementation in hypo-androgenic, infertile women readers are advised that opinions expressed about androgen supplementation in infertile women may be biased by potential financial conflict.
Conclusions
• This case report is a perfect example of the argument the CHR has been making for decades that the female immune system only too often in infertility practice does not receive the attention it deserves.
• This case also very clearly demonstrates the logic of treating a suspected immune problem as an integral part of treating multifactorial infertility (when an infertile couple demonstrates more than one infertility diagnosis concomitantly).
• Unless multiple-factor infertility – whether only in females or also caused by a male factor is addressed concomitantly, even one diagnosis left untreated can prevent pregnancy.
• Repeatedly previously noted in the VOICE, in contrast to many (if not most) other fertility centers, the CHR views pregnancy as an in principle immunologic rather than endocrine phenomenon. The reason is the indisputable fact that the establishment of maternal immune tolerance toward the fetal semi-allograft (in donor egg cycles even a complete allograft) precedes any other maternal contribution to implantation and the establishment of pregnancy.
REFERENCES
1. https://www.mayoclinic.org/diseases-conditions/juvenile-idiopathic-arthritis/symptoms-causes/syc-20374082
2. Gleicher et al., Hum Reprod 2013;28(2):294-297

ADVERTISEMENT

The V oice | 27
28 | The Voice

BRIEFING
• As the world around us has been changing, medical and scientific training has remained mostly unchanged for decades.
• This article argues against continuous ossification of medicine as well as related research.
• Current specialty-based training no longer makes sense, as sub-specialties become smaller and smaller, yet also deeper and deeper, and collaborative efforts across traditional specialty areas are becoming increasingly necessary if big issues are to be resolved.
• Whether in the training of physicians or scientists, the pursuit of initially, widely differing interests is advocated to allow individuals to determine the combination of interests they wish to pursue in their careers, allowing them to develop their own “micro-specialties.”
Have you ever asked the question of why medical specialties exist, how they came into existence, and whether they still make sense? If not, you may want to start pondering this question because our current medical system of rigidly defined specialty areas (and, of course, sub-specialties and sub-sub-specialties) may have lost its initially favorable cost-benefit equation.
Expert opinions
That medicine evolved along traditional specialty lines was a natural evolution based on the basics of “expert” development: Distinctions based on individual organs and/or organ systems in research and clinical medicine made all the sense in the world if basic knowledge and basic practice were to be developed. However, as a plethora of behavioral studies have in all areas of expert development convincingly demonstrated, expert opinions not only offer advantages. They often also lead to significant problems, a point very acutely reemphasized by the many misdirections the management of the COVID-19 pandemic took based on so-called (and often highly selective) “expert” opinions.
As previously on several occasions discussed in these pages, “experts” tend to “fall in love” with their area of expertise and, often, end up ignoring the fact that their area of expertise does
Continued on page 30 The V oice | 29
not exist in isolation but is closely interwoven with many other areas of expertise, - with all of influencing each other. Ignoring those influences will often significantly negate the accuracy of an expert opinion.
Nowhere is this more obvious than in medicine: While cardiology expertise is essential in a woman with mitral stenosis, if this woman wishes to conceive and must be safely managed through pregnancy, obstetrical expertise becomes not less important than cardiologic expertise and, under certain, circumstances maybe even more important. And that does not even consider that additional medical specialty areas may, at times, play equally or even more important roles, including, for example, anesthesia, intensive care medicine, pharmacology, etc.
The importance of redundancies
The same applies to the development of new knowledge through research. Here, too, science has taught us (and is still teaching us daily) how primitive our thinking at times has been (and, often, still is) when we assumed only a few decades ago that every gene has only one function; or when new knowledge in immunology led us to discover the importance of the immune system in development, progression, and treatment of cancers, and medicine in the 1970s and 1980s, and medicine started believing that immunology was on the verge of curing cancer through this new immunology knowledge.
Other examples of too simplistic past thinking in medicine, of course, abound and many are still driving forces in, both, research as well as clinical practice. Likely one of the most profound misdirections in medical “expert” opinion is the basic assumption that any A to B leading effect is singular; that is if we discover (and experimentally prove) that A leads to B through a factor C and that the withholding of C prevents A from going to B, this represents the end of the story.
Biology must be fully dependent on redundancies.
This still widely-held opinion (currently the basis for innumerable scientific publications) is in many (and likely most cases) too simplistic and would be equal to sending a rocket to the moon without backup systems in place to prevent a catastrophe for A
failing in transfer to B and a system, thus, going down. Just as rocket systems in a flight to the moon must have redundancies to prevent catastrophes in case A to B processes break down, so must biology have redundancies to most (if not all) biological processes. If for some reason A to B does not function properly, there must be an A to B1 and a B 1 to B (and probably several other redundancies) because, considering how complex a process reproduction is, we all would not be in this world without the existence of such redundancies. Yet, we all are daily still taught that A always leads straight to B (or not at all), an incredibly simplistic view of biology and nature in general.
The advantage of having special expertise in unrelated areas
Having expertise in completely unrelated areas for several reasons can have great advantages: First, even seemingly unrelated areas of medicine often have shared meeting points of overlap. They, often, just may not become obvious to individuals without special expertise in both of those areas. In addition, special expertise in seemingly unrelated areas has a very good chance of remaining rare among colleagues and, therefore, often offers special opportunities with little opposition and naysayers.
My own experiences are good examples: The unexpected opportunity of an unusually intensive training in cardiology during my rotating internship following graduation from medical school, significantly helped during my early academic career in general obstetrics and gynecology in developing special expertise in studying and clinically managing pregnant women with often unusual and/or severe medical problems during pregnancy. Special expertise relating to general internal medicine and obstetric practice was further fostered when I was given the additional opportunity of a reproductive immunology fellowship at Mount Sinai Medical Center in a six-month break between my rotating internship and the start of my obstetrics and gynecology residency.
As noted above, those were important (and overly optimistic) days for the field of immunology and, especially, cancer immunology. My early academic career during residency and a subsequent full-time academic appointment at what then was the Mount Sinai School of Medicine of CUNY, therefore, was in principle characterized by clinical work and research regarding medical problems in pregnancy, while my research laboratory mostly worked on what then was a brand-new subspecialty area in obstetrics and gynecology, reproductive immunology. In vitro fertilization (IVF) did not exist and that practically meant that what was considered infertility practice was only a minor appendix to general gynecology.
Greatly supported by my then department chairman, Saul B. Gusberg, MD (see photo), I was already able to get outside grant support for my research laboratory during residency. Upon graduation from residency, I was appointed head of the
Continued from page 29 30 | The Voice
first subspecialty division of reproductive immunology in an academic obstetrics and gynecology department in the country. I also became the founding editor-in-chief of the American Journal of Reproductive Immunology (AJRI), a position I held for approximately 20 years.
My special knowledge in general medicine and hands-on benchwork in the laboratory was also extremely helpful when, only two years after graduation from residency at the young age of 33 years, I was appointed Department Chair of Obstetrics and Gynecology at Chicago’s Mount Sinai Hospital (unrelated to New York’s Mount Sinai) and decided to establish in my new department the first IVF programs in Chicago and the Midwest (and one of the first in the country).

Saul, B. Gusberg, MD, Chairman, Department of Obstetrics and Gynecology at Mount Sinai Medical Center in NYC during Dr. Gleicher’s fellowship in reproductive immunology, residency, and faculty appointment
Simply based on a residency in obstetrics and gynecology, I would never have been able to pull this off because, in those very early IVF days, one could not just hire IVF experts, as hardly any existed. Together with the Chief of my department’s REI division, Jan Frieberg, MD, PhD, I once more had to self-train in a brand-new field of medicine, and the rest is by now history. However, that last re-training would not have been possible without my two earlier training experiences outside of my primary OB/GYN field.
Reproductive medicine interplaying with other fields
The CHR in those Chicago days was not only an IVF pioneer (the first ever vaginal egg retrieval, for example, was performed at the CHR in Chicago, in those days still hospital-based at Mount Sinai Hospital in Chicago1), but also pioneered other treatments, for example, transvaginal tubal catheterizations under x-ray control. Here, the idea again came from cardiology, where the progress in catheter
technology in coronary catheterization had been amazing and produced the idea at CHR to try out these cardiac catheters in fallopian tubes, and it worked.
Through a multicenter prospective study in women with obstructed tubes, we were able to establish the concept long before our radiology colleague started offering tubal catheterization.2 In the following years, the CHR (and increasingly others), performed hundreds, if not thousands, of such catheterizations for occluded tubes because the principal alternative in those days was major tubal microsurgery. However, as IVF results got better and better, surgery and catheterizations became rarer and rarer because both were only very temporary solutions since tubal occlusions usually recurred within six months, - often more severe than before.
Approximately seven years ago, the CHR finally shut down its catheterization unit under x-ray for good. Nowadays, if there exists a rare indication for a tubal catheterization, it is usually done by radiologists (though we here at the CHR still insist on reading our films).
Other areas of interphase with other specialties, and often even more contentious, have been rheumatology and/or immunology. It is quite astonishing that, to this day, even some very prominent fertility centers deny any link between the establishment of pregnancy and the maternal immune system. As elsewhere discussed in two locations in this issue of the VOICE, there can no longer be any doubt that the first step that must be accomplished to lead to pregnancy is the successful establishment of maternal tolerance vis-à-vis the implanting embryo (a paternal semi-allograft). Unfortunately to this day, the number of obstetricians-gynecologists, reproductive endocrinologists, and rheumatologists/immunologists with knowledge of immunology as well as reproductive medicine is by far too small. The consequence has been a rather significant stagnation in our understanding of pregnancy as an immune-mediated condition in principle.
Another important specialty area with which reproductive medicine increasingly interphases is genetics. Readers of the VOICE are aware of several disagreements the CHR has expressed with clinical practices heavily promoted by the genetic testing industry, primarily involving PGT-A and, more recently, also what is called polygenic risk scoring (PGRS) of embryos, and to a lesser extent, non-invasive prenatal genetic testing (NIPT). We do not wish to be repetitive and will not address these disputes any further, except for the fact that on both sides of the argument, ignorance of basic physiological realities appears to be the reason why so many geneticists still actively promote these tests, and so many colleagues in IVF still overuse them.
Reassessing medical specialties
As overlapping knowledge between specialty areas has become increasingly important in clinical practice, the same also applies to investigations and basic research. Once more, a brief personal
A PIECE OF MY MIND
Continued on page 32 The V oice | 31
experience is an illustration for this statement. As earlier noted, during my residency and early full-time academic career, I ran my research laboratory dedicated to reproductive immunology research. The first subject that fascinated me while still in my residency, was common denominators between pregnancy and malignancy, with the hypothesis being that immune pathways that allow tolerance of the fetal-placental semi-allograft in pregnancy are “misused” by malignancies to overcome rejection by the host’s immune system. My laboratory’s work was at the time published in three consecutive papers in what then was the leading medical journal in the specialty, the American Journal of Obstetrics and Gynecology 3-5
Paradoxically, after several studies that demonstrated the importance of aneuploidy in solid cancers for their invasiveness and metastatic spread, this hypothesis is more alive than ever, as preimplantation-stage embryos have been demonstrated in a very high percentage of cases to demonstrate mosaic aneuploidy, which in the fetus often self-corrects, but in the placenta remains present until birth.
On a very personal level, the circle of life has been closing. As I started my research career in the laboratory trying to pursue the hypothesis of common denominators between pregnancy and malignancy and, currently, have amazingly been presented with the opportunity, through collaboration with colleagues at Rockefeller University and MSK Cancer Center, to hopefully confirm this hypothesis.
So, what does all of this then mean regarding the need to redefine medical specialties?
The above-outlined hypothesis would only very unlikely be pursued by me alone in my primary specialty of obstetrics and gynecology, nor would it likely be pursued alone by my cancer-researcher colleague at SKM Cancer Center, and, most certainly not by my biologist colleague at Rockefeller University.
What this circumstance demonstrates is that many remaining big issues in biology and medical research transcend current medical specialties and research areas in laboratories. Just as they transcend specialty boundaries in basic research, so do they also often transcend clinical practice areas. As areas of special expertise grow in complexity, they in parallel must shrink in size. What then is the purpose of training physicians over four years in general obstetrics and gynecology, when a big portion of such-trained physicians will never practice again general obstetrics and gynecology after residency?
Or, what is the purpose of training RE fellows for three full years (a third year was added to “induce them to do research”), when the clinical skills required from an average REI who does not perform complex surgeries (as almost none do) can be safely taught in one or, at most, two years? Wouldn’t our specialty be much better off if candidates who are interested in
pursuing research, instead of wasting three years for unserious research in irrelevant REI fellowships, spend a year in a real research lab at Rockefeller University or a SKM Cancer Center? Concomitantly, wouldn’t research labs be better off by, instead of having postdocs suffer for years in the same lab, sending them into a clinical setup related to the investigator’s or the lab director’s research interests?
In short, while science, technology, and societal habits have drastically changed, our medical and scientific training methods have remained mostly the same, caught in a rigid system of specialty areas that no longer make much sense in the broadness of intent as well as execution, yet are unable to satisfy purposes and/or individual desires of trainees.
Specialties should be determined by demand in the market and the desires of physicians and scientists. If I wanted to become the world’s best “expert” for the small left toe, I should be able to pursue this goal in a rational and economic way, just as I would do if I wanted to remain a general obstetrician-gynecologist or a regular clinical REI. A system like that would allow us to change our careers as the world changes around us and vice versa. Most importantly, it would also allow the worlds of medicine and science to change alongside the best qualified and most satisfied staff in the most economical approach for all sides.
REFERENCES
1. Gleicher et al., Lancet 1983;2(8348):508-509
2. Confino et al., JAMA 1990;264(16):2079-2082
3. Gleicher et al., Am J Obstet Gynecol 1979;133(4):386-390
4. Gleicher et al., Am J Obstet Gynecol 1980; 136(1):126-131
5. Gleicher et al., Am J Obstet Gynecol 1980;136(1):5-10

from page 31 A PIECE OF MY MIND
Continued
ADVERTISEMENT 32 | The Voice
BRIEFING: Obesity has become a major societal health problem. It is now well established that obesity adversely affects female as well as male fertility and reduces treatment success in infertility. Yet it has so far not found the deserving recognition in infertility practice. This section of the VOICE, therefore, is dedicated to filling this gap by offering relevant information about nutrition, pharmacological interventions to fight obesity, and, where applicable, supplements as integral contributions to a comprehensive treatment approach toward female as well as male infertility.
For the many long-distance patients of the CHR who often spend considerable time in NYC and, of course, also for local patients who are interested in this information), we in this section also offer a listing of our favorite restaurants in the city. In at least some of them, advising them that the CHR referred you may even help with reservations that are at times difficult to get. As in other sections of the VOICE, we welcome comments and suggestions, which are to be sent to arata@thechr.com.
Continued on page 34

Finally bringing anti-obesity drugs into infertility practice
New anti-obesity drugs like Wegovy,® Ozempic,® and Rybelsus (all semaglutide products), and Mounjaro® (a tirzepatide product) are among several prescription medicines that appear destined to change medicine by offering virtually guaranteed weight loss at highly significant proportions to everybody who starts injecting these medications.
Semaglutide acts as an agonist to the so-called glucagon-like peptide (GLP1) receptor and thus it pretends to be the GLP-1 hormone which makes us less hungry by sending signals of feeling full to the brain.
Mounjaro® is a little more complicated because it is made up of two effective substances that induce weight loss, - one again a GLP-1 receptor agonist but, now added to it, a so-called glucose-dependent insulinotropic polypeptide (GIP) and, thus
The V oice | 33
Continued from page 33
mimics the GLP-1 as well as the GIP hormone in their activities on their respective receptors. Like GLP-1, GIP triggers a feeling of fullness. These drugs likely also affect the brain’s control of food intake and this function has also in general been associated with anti-addictive behavior, a reason why these drugs now are also investigated for their potential effectiveness in drug – and other addictive behaviors.
Other medications, alleged to be even more effective in inducing weight loss, appear on the way to market. Remarkably, these medications have relatively few and usually easy-to-overcome side effects, and, considering that these drugs have already for several years been in relatively long-term use in diabetic patients, unexpected longterm side effects appear unlikely.
Even more remarkably, this family of new weight loss medications does not only affect blood sugar levels and causes significant weight loss but, likely because of secondary benefits from significant weight loss, has substantial secondary health benefits, with most not yet even recorded. Mounjaro® has been shown to reduce systolic blood pressure1 and semaglutide beneficially affects heart health in diabetic patients.2 In mice, semaglutide’s cardioprotective effects exceeded effects obtained from dietary weight loss, thereby suggesting that beneficial effects may not only come from weight loss.3
No wonder producers of this family of anti-obesity drugs are taking all kinds of unusual steps in attempting to boost production of these medications which are all in short supply.4 Moreover, Eli Lilly’s – the producer of Mounjaro®- and of other weight loss products that are on the way - market capitalization surpassed Tesla’s market cap, causing The Wall Street Journal to suggest that the company deserves to become one of the “magnificent seven” companies which control the stock market. The article suggests that manufacturers of obesity drugs, and not manufacturers of electric vehicles, can be expected to show the kind of revenue growth in coming years that warrants inclusion in this elite group of companies.5
Because obesity has so many secondary negative effects on health, potential secondary beneficial effects have been also suggested on neurodegenerative diseases like Alzheimer’s and Parkinson’s disease, depression and anxiety, osteoarthritis, fatty liver, inflammation, and others. A very recent study demonstrated weight loss from this family of drugs reduced all cause-mortality among patients with knee and hip osteoarthritis.6,8 Most recent data also suggest beneficial effects on inflammation,
Even though obesity is by now well established as a contributing factor of infertility in both sexes, the potential effects of these drugs on female as well as male infertility have so far not been explored. The likely reason is that mouse (and other) data suggested that these medications when used during early pregnancy can cause birth defects and small for age fetuses. This, however, should not be a reason for not using these drugs before pregnancy as part of a strategy to improve pregnancy chances with later fertility treatments. Weight loss has been for decades known to improve the effectiveness of practically all fertility treatments. There were in principle only two major reasons why this knowledge has only so rarely been applied to infertility patients: (i) Weight loss very frequently was unsuccessful;
and (ii), - even if successful, weight loss took a very long time to achieve, - time many infertility patients do not have, especially if older.
However, what this new family of weight loss drugs now has established without any remaining doubt is that these drugs allow for substantial weight loss in a relatively short time. This is important because studies have repeatedly demonstrated that loss of as little as 5% to 7% of body weight (representing only 10-20 pounds) will already significantly improve treatment chances in obese infertile women and men. This goal in many patients can be achieved with as little as three months of treatments with these new medications. Time appears to be ripe to start integrating drugs like Vegovia ®and Munjaro® into fertility treatment algorithms for obese infertility patients! The CHR has started to do this, and we will address this issue in more detail in the May issue of the VOICE. In the meantime, if you feel that you may benefit in your attempts to lose some weight, come and see us at the CHR.
REFERENCES
1. Lingvay et al., Cardiovasc Diabetol 2023;22:66
2. Lincoff et al., N Engl J Med 2023;389:2221-2232
3. Withaar et al., J Am Coll Cardiol Basic Trans Science 2023;8(10):1298-1314
4. Loftus P. The Wall Street Journal. February 6, 2024
5. Wainer D. Wall Street Journal, February 7, 2024, page B12
6. O’Mary L. WebMD Health News, February 9, 2024. https://www.med scape.com/s/viewarticke/study-suggests-mind-body...0_daily_240209_ MSCPEDIT_etide6300414&uac=223637CN&implID=6300414
7. Lenharo M. Nature 2024;626:246
8. Wei et al., Arthit Rheum 2023; doi: 10.1002/art.42754. Online ahead of print.
The CHR’s favorite NYC restaurants
All listed restaurants are in Manhattan unless otherwise noted. Like all opinions about restaurants, ours are subjective and are to be understood as such. If you visit one of them, let us know whether you agree with our ratings. We value your feedback.
HOW WE RATE
PRICES
$ Inexpensive or Not worth a trip
$$ Moderately expensive
$$$ Expensive
$$$$ Very expensive
SPECIAL COMMENTS
+ ………. Overall favorite restaurant in NYC
v ……….. Special vibe
M ………. Michelin-starred
• Good
•• Very good
••• Excellent
•••• Uniquely delicious
FOOD QUALITY
34 | The Voice
NAME & CUSINE ADDRESS TELEPHONE COMMENTS AUSTRIAN Koloman +/•••/$$/v 16 W 29th Street (212) 790-8970 V; Excellent deserts Wallsé +/•••/$$/v/* 344 W 11th St (212) 352-2300 V; Excellent deserts CHINESE
Yuan Szechuan +/•••/$$/v 42 East Broadway (212) 966-6002 V; Authentic Szechuan Mr. Chow Downtown/Uptown +/••/$$$/v 121 Hudson St., Tribeca (212) 965 9500 V 324E, 57th Street (212) 751 9030 V CONTINENTAL 425 ***/$$$/v 425 Park Avenue (212) 751 6921 V; Gorgeous restaurant FRENCH
Gratin ••/$$ 5 Beekman St. (212) 597-9020 V; Try the gratin potatoes Le Charlot +/•• /SS 19 E 69th St. (212) 794-6419 V; Best steak au poivre and Thai mussels; great deserts Le B •••/$$$ 283 W 12th St (212) 675-2808 V Le Bernadine +/••••/$$$$/ MMM 155 W 51st St (212) 554-1119 V; Mostly seafood. Likely the best in NYC restaurant GREEK Elias Corner (Queens) ••/$ 24-02 31st St. (718) 932-1510 Mostly seafood HAMBURGERS Jackson Hole Burgers (the “original”) +/••/$ 232 E 64th St. (212) 371-7187 Not a place for vegetarians ITALIAN Cipriani Downtown/Uptown +/••/$$/v 376 West Broadway (212) 343 0999 Great food and beautiful people 781 5th Avenue (212) 753-5566 Great food and high society Elio’s +/•••/$$/v 1621 2nd Ave. (212) 772-2242 Best Italian home cooking and where everybody meets Principe ••/$$/v 50 West Broadway (212) 335-0509 V; mostly seafood but one of the best chicken dishes Sistina •••/$$$ 24 E 81st St. (212) 861-7660 V; Amazing wine list JAPANESE SUSHI Sushi Ann +/••• /$$$$ 8 E 51st St. (212) 755-1780 V; Best quality fish; make reservation at the bar GENERAL Sakagura +/•••/$$ 211 E 43rd St. (212) 953-7253 V; Amazing food; Best sake selection Yakitori Torishin +/+++/$$$M 362 West 53rd Street (212) 757 0108 Unique and amazing skewer restaurant KOREAN Jungsik •••/$$$$/ MM 2 Harrison St. (212) 219-0900 Where NYC’s Korean restaurant revolution was born … The V oice | 35 Continued on page 36
Hwa
Le
Continued from page 35
Oiji Mi +/•••/$$/v / M
MIDDLE EASTERN-ISRAELI
17 W. 19th St. (212) 256-1259 …. and has continued
Dagon ••/$$ 2454 Broadway (212) 873-2466 Best humus in NYC
NEW YORK JEWISH DELI
P. J. Bernstein’s Deli •/$ 1215 3rd Avenue (212) 879-0914
PERUVIAN
Mission Ceviche •••/$$
PIZZA
1400 2nd Avenue (212) 650-0014
All the great classics; pastrami, chicken soup
If you like Peruvian – the best
San Matteo Pizzeria e Cuccina ••/$ 1559 2nd Avenue (212) 861-2434 True Napoli
POLISH
Karczma (Brooklyn) +/•/$ 136 Greenpoint Avenue (718) 349-1744
UKRAINIAN/RUSSIAN
Great authentic Polish food – and dirtcheap
Caviar Russe +/••••/$$$$/ M 538 Madison Avenue (212) 980-5908 V; Most underrated restaurant in NYC
Russian Samovar •/$/v
256 West 56th St. (212) 757-0168
Any suggestions and/or comments, please write to arata@thechr.com
Great Russian/Ukrainian Food and music

36 | The Voice
David Gregory Bouley, likely the most talented and most important chef of his generation in the U.S., died from a heart attack unexpectedly on February 14, 2024, in his house in Connecticut. He is survived by his wife of almost 20 years, Ms. Nicole Bartelme, independently known as an artist and as a founder of the TriBeCa Film Festival. I and all the staff of The CHR offer our deepest condolences to Ms. Bartelme and Bouley’s five siblings and 14 nephews and nieces.
Considering his importance in the New York food scene, it was not surprising that his death made the frontpages of most newspapers and headlines of many electronic media, giving him among many other attributes the title of “Pioneering Chef of New American Cuisine” (The New York Times), “Legendary Chef” (Eater NY), and pointing out the many outstanding restaurants he owned over decades, almost always located in TriBeCa, and only a few blocks from each other. They included his namesake, Michelin-starred Bouley in its final location on the corner of Hudson and Duane Streets, Brushtroke, a pioneering Japanese restaurant he operated in partnership with one of the leading Japanese culinary schools in
Osaka just across the street to the south from Boule, at a time when authentic Japanese restaurants were not yet on every other NYC corner. Then there was Bouley Botanical where the CHR held several GrandRounds and other events and Bouley’s Bakery in the space Bouley had previously occupied. His last venture, Bouley at Home, as all of his restaurants pioneering, was a test kitchen, a working restaurant, and an event space all at once, serving exceptionally great food on short kitchen counters. It was literally like eating in the kitchen at home, just so much better! I also celebrated my 70th birthday in the event place.
This is not where my decades-long relationship with David started. That happened in the late 1970s when I was still a resident at Mount Sinai and David was the sou chef at a new Austrian restaurant on East 79th Street, called appropriately Vienna 79. It was NYC’s first Austrian restaurant and quickly became this ex-Austrian’s steady hangout until it became almost impossible to get reservations because Mimi Sheraton, at the time the New York Times’ (still anonymous) food critic, awarded the place an almost unheard of four stars. Predating the Internet, her New York Times’ weekly restaurant
The V oice | 37 Continued on page 38
Continued from page 37
review was the bible for the restaurant industry and barely a handful of restaurants had ever gotten a four-star review from Ms. Sheraton. At that time still an unknown, her awarding of four stars to this small new restaurant in the middle of nowhere should have “warned” the world that culinary greatness was on the way in the person of an at the time still very young David Gregory Bouley.
Our personal relationship rekindled after Boulet had already become a superstar through his restaurant Bouley, this time not only because of New York Times stars, but Michelin stars. However, it wasn’t Bouley that made me again “hang out” regularly where David was in the kitchen; it was a small restaurant, across from the original Bouley, on Duane Street, up steep stairs on the second floor, above his small bakery, appropriately called “Upstairs” which to this day, considering its pricing structure, I consider by far the best restaurant I have ever experienced in NYC and probably in the world. It was a tiny, packed space with two separate kitchen areas taking up the west- and north-sides of this small space, a Japanese (staffed by two incredible chefs, and Bouley’s first toe dips into Japanese cuisine) on the north, and a Continental-French kitchen on the western wall. There was no tasting menu, all was a-la-cart, and one could combine food from both kitchens, the western one often manned by Bouley himself. Though I usually am not a big fan of lamb meat, I will never forget David’s small lamb chops, marinated in milk for 24 hours before going on the grill. I have ever since tried to find them elsewhere, unfortunately to no avail!
Interestingly, none of the many obituaries I read mentioned either Vienna-69 or Bouley Upstairs, nor did any of the obituaries mention Boule’s restaurant, Danube, which resided in the same space where several years later Brushstroke moved in. Danube was one of the most “grandee”- appointed restaurant spaces in NYC and the Austrian food it served was even better than at Vienna-79. It is evidence that Bouley not only built on his French cooking heritage acquired during several years of training at some of the most famous French chefs’ kitchens, but also on Austrian traditions acquired in his younger years.
What always fascinated me about David was his constant desire to learn and to teach. I don’t know whether his collection of cookbooks is the largest in the world, but it would not surprise me. He constantly brought great chefs to wherever he was, in an effort to learn new things and pass them on to others. Had he been a physician, he would definitely been an academic researcher: he thought that way and acted that way. Somewhere around 15-20 years ago, besides being interested in how people cook around the world, he also became interested in the idea of food as medicine. Around 2013 he started to organize dinners around this concept, always inviting a similarly minded physician to give a talk and called the series of special dinners, “The Chef and the Doctor.” As always, he was ahead of the “Zeitgeist.”
We have been missing David since he closed several years ago Bouley at Home, his last restaurant, always hoping that he would return with a new idea and yet another new restaurant. Now we will miss him forever; but what a memory!
Norbert Gleicher, MD
NEW RESTURAUNT REVIEWS
NEW RESTAURANT REVIEW: 425 ***/$$$/v This updated review is based on four visits.
This gorgeous new restaurant named after its address on Park Avenue, is the latest addition to the restaurant empire of JeanGeorge Vongerichten who is now responsible for over 60 restaurants worldwide, among those 13 in NYC. Though probably among the most successful French super-chefs in the world, we have never been big fans of his cooking style or, to be more specific, of his palate which, years ago, we came to understand when he, personally, manned the kitchen at The Mark, only a few blocks away from the CHR.
Located in the new skyscraper at 425 Park Avenue, a beautiful ground-floor bar is also serving a limited food menu. Accessible by staircase or elevators, a gorgeous main dining room on the second floor is in its grandeur and modernity almost breathtaking, featuring a to the floor fully visible kitchen behind a glass wall. The dining room is reminiscent in shape, vibe, and emotional “Gestalt” to the iconic pool room of the former Four Seasons restaurant in the Mies van der Rohe – designed Seagram Building down the block on Park Avenue, - just more modern, of course, and missing the iconic central pool.
As promised, we went back for two more visits, and we are pleased to report that the food has greatly improved. The Chef de Cuisine is Jonathan Benno, a chef we very much appreciate from his two restaurants at the Evelyn Hotel on 27th Street, where he also received a well-deserved Michelin star, appears to have found his footing in the gorgeous kitchen, observable from every table in the restaurant. It often takes time for a new restaurant kitchen to get settled. This restaurant has become worth a visit.

NEW RESTAURANT REVIEW: Café Boulud -/$$ This review is based on two visits.
When star-chef Daniel Boulud’s moved his first restaurant, the Michelin-starred namesake Daniel, from 76th Street between Madison and Fifth Avenue to its current location on the corner of 65th Street and Park Avenue, its prior location became in 1998 Café Boulud, a slightly less formal and less expensive restaurant than
Photo credit: 425 Park Avenue
38 | The Voice
before, but for many years a deserving continuous destination for the Upper East Side crowd.
Unfortunately, as so often happens, as Boulud ascended to his chef-stardom and started opening a steady stream of new restaurants all over the city and around the world, both of his initial flagship restaurants started a steady decline in food quality, best demonstrated by Daniel losing a Michelin star and no longer belonging to the small elite-gang of three-starred restaurants in NYC (the restaurant still has two stars). The decline at the Café, named after Boulud’s family’s original café in Lyon, France, was even more pronounced and its closure did not surprise us.
It now reopened in a new spot on the corner of 63rd Street and Park Avenue in a not-very-lucky restaurant space which over the years housed Vosin, Périgord Park, the Park Avenue Café, and, most recently, Vaucluse. So far only partially completed, the restaurant, as in its prior itineration Vaucluse, occupies two wings, with the western wing toward Park Avenue housing a very modern-elegant classical and somewhat tightly packed restaurant space (with some surprisingly interesting art) and the eastern wing still under construction and planned to house a large bar area that will also serve a limited bar menu.
This brings us to the food and the news is not equally good. To a degree, that is not surprising because the Executive Chef is Romain Paumier, who worked at the Café at its prior location and as noted before, ruled over what we considered a declining kitchen at that location before becoming Executive Chef at Daniel, where the kitchen witnessed a similar fate. Interestingly, it stands in contrast to another restaurant the Boulud organization recently took over, Le Gratin in the downtown Beekman Hotel (the former Augustine), where we like the food. This Boulud restaurant even made it into our most favorite restaurant list (see above).
The menu in the Café’s main dining room is offered as a two or three-course tasting menu in four categories: La Tradition (French classic), Las Saison (currently winter flavors), Le Potager (from the

farmer’s market), and Le Voyager (currently cuisine from Thailand), with individual appetizers, main courses, and deserts freely interchangeable between the categories. The first three categories were between tasteless and mediocre. The cuisine from Thailand was pretty awful (and we like Thai food). On one visit, the service was atrocious. During a second visit, the main culprit was nowhere to be seen and the service was much better. As of this point, we cannot recommend this restaurant for a visit, but we will continue to check. It often takes time to get things running, but there is much to fix here.

The V oice | 39
Photo credit: Café Boulud




The VOICE in this section of the newsletter offers commentaries on a broad survey of recent articles in the English literature, which the CHR found of interest, even if, at times, not immediately applicable to daily clinical practice. Articles are mostly chosen for their translational value to clinical medicine, often helping in determining where clinical practice will likely go.
Translational research is one of the CHR’s principal goals and has over the years produced some milestone discoveries and a good number of U.S. patents since its founding in 1981. Such research has also propelled the CHR into its current status as a worldwide center of last resort for infertile patients who have failed treatments elsewhere. This section of the VOICE, demonstrates and makes public the process through which the CHR for decades has been following and interpreting the published literature, a process always at the very core of how research and clinical practice have evolved at the CHR.
Primarily directed at physicians and basic scientists, this section of the VOICE to our surprise has also attracted many of the CHR’s patients, from which we assume that it also has found a readership among the public. The VOICE strives through its writing style, to make this section also accessible and understandable for a general audience.

Ethics & Law
Considering the possibility of bipaternal progeny
Three very important individuals in reproductive sciences (though with very different scientific backgrounds) offered recently in Nature Medicine their combined opinion about ethical and legal challenges in assisted same-sex conception through in vitro gametogenesis:1 Eli Y. Adashi, a well-respected reproductive endocrinologist, past research scientist, and medical school dean (and longstanding friend of the CHR), Katsuhiko Hayashi, one of the leading reproductive biologists in the world (see also a short report about him and his recent work in the News Section of this issue of the VOICE), and I. Glenn Cohen, a well-known law professor at Harvard Medical School and Director of the Petrie-Flom Center for Health, Law Policy, Biotechnology, and Bioethics.
The impetus for this opinion piece was, likely, a recent paper from Hayashi’s laboratories at Kyushu University in Fukuoka, Japan, and Osaka University, Osaka, Japan, which by Nature magazine was listed as one of the 10 most important science contributions of 2023.2 The authors suggested so much by stating in the introductory paragraph that, “it has become clear that bipaternal progeny may soon be technically possible thanks to in vitro gametogenesis (IVG),”
referring to another breakthrough paper by Saitou and Hayashi in 2021.3 In that earlier study, mouse oocytes were established from stem cell lines, fertilized, embryos were transferred, establishing pregnancies and deliveries of healthy pubs, with the cycle being successfully repeated over several generations.
What made the more recent paper even more remarkable was the fact that the pluripotent stem cells from which oocytes were generated came from a male mouse, thus converting an XY chromosomal set to an XX counterpart, with the modified iPS cell then guided toward oocyte fate. Without going into technical details, it is important to note that this process was still highly insufficient.
That this breakthrough may become clinically applicable and allow in the relatively near future the establishment of bipaternal progeny may be somewhat optimistic, though the authors’ optimism appeared more directed at achieving the technical abilities, while at the same time, being maybe too skeptical about potential ethical, legal, and governmental obstacles.
In our opinion, the article appears to look a little too far into the future, paradoxically making the subject appear more futuristic than it may actually be. We suspect that, once the whole process
40 | The Voice
in humans comes closer to realization, appropriate avenues will open at professional, ethical, and government levels to find out how such complex issues can be brought into an ethically acceptable experimental human framework. Starting the discussion too early just may foster a return to the pre-IVF experience, where even professionals within the infertility field were issuing exaggerated warnings that IVF would produce “Frankenstein monsters.” For those who enjoy looking beyond currently realistically achievable horizons, this is a very well-written paper.
REFERENCES
1. Adashi et al., Nat Med 2024; https://doi.org/10/1038/s41591-023-02689-7; Online ahead of print.
2. Murakami et al., Nature 2023;615:900-906
3. Saitou et al., Science 2021;374:eaaz6830
The moral justification for “add-ons” As is widely appreciated in the specialty, the CHR has for years been preaching against many, if not most, “add-ons” to IVF. We could not resist the temptations, when we came across a paper in RBMOnline, titled “Moral justification for use of “add-ons” in ART.”1 The paper tried to describe what the factors are that IVF practitioners consider when deciding to offer “add-ons” to their patients, but tried to do this by interviewing only 31 IVF providers.
That behavioral scientists believe they can obtain worthwhile data from such small study populations is always amazing, but so much behavioral science is based on such small-volume studies. As one, therefore, would expect, the study ended up offering only platitudes. Interestingly, nobody among the study participants mentioned the increased revenue for their clinics from the utilization of “add-ons,” which probably is rather telling about the honesty of the responses of study participants or, under a more favorable interpretation of those responses, their lack of insight into their decision-making processes. That fact alone should have demonstrated to the authors the scientific worth of their data. By publishing their paper, they now, instead, have the dubious honor of being a prize paper in this issue of the VOICE as a “worst” paper.
REFERENCE
1. Gallagher et al., Reprod Biome Online 2024;48(2):103637; PRIZE PAPER: A worst paper of the issue.
More on polygenic risk scoring of embryos
Repeatedly a subject of criticism in these pages and elsewhere as ineffective and unethical, polygenic risk scoring (PGRS) in the U.S., nevertheless, is rather unabashedly advertised by several IVF clinics as well as genetic testing laboratories. Now some Belgian social scientists queried (paradoxically again 31) healthcare providers in reproductive medicine and genetics in Europe and North America about their attitudes toward PGRS.
Unsurprisingly, the interviews revealed significant concern about the utilization of PGRS in association with IVF but, as noted in discussing the preceding paper, we do not understand how 31 individuals can be considered to properly represent the IVF field. Moreover, the authors did not even differentiate between clinicians and geneticists. In other words, it is a well-meaning paper, but with execution that offers nothing new.
REFERENCE
1.
Siermann et al., Scial Sci Med 2024;343:116599
General infertility
Assisted reproduction, including IVF GONADOTROPINS. The start of gonadotropin administration practically defined the beginning of modern infertility care and in association with IVF represented the turning point, when the procedure went from being experimental to becoming a clinically highly effective mainstay of infertility practice. Yet surprisingly little research has been done ever since on the clinical utilization of exogenous gonadotropins in female infertility. This is why a recent paper by Chinese colleagues in Scientific Reports (an increasingly frequent source of interesting papers in reproductive medicine) caught our attention.1
In this study, the authors attempted to better understand the relationship between FSH dose and live birth rates (LB) in infertile women (excluding PCOS patients) which, due to varying results reported in different studies, has remained controversial. Investigating 11, 645 patients at one institution who had undergone IVF cycles with and without ICSI, the authors reported several interesting findings: (i) LBs increased with every increase in FSH by 1,000IUs for as long as the total FSH dosage remained lower than 1,410 IU; (ii) Once total FSH exceeded 1,410 IU, the association turned negative. (iii) This interaction changed with advancing patient age. Overall, the study suggested a non-linear relationship between FSH dosage and live birth outcomes which, moreover, was age-dependent.
Even though the study suffers from several shortcomings (to be discussed further below), these are for several reasons interesting and, likely, important results: (i) They to a degree may explain contradictory findings on this subject in the literature, once more reemphasizing the importance of proper patient selection in studies to be able to work with as “cleanly” defined patient populations as possible. Here, the authors at least excluded PCOS patients from their center’s patient pool. (ii) The data reemphasize the importance of patient age in choosing a patient’s stimulation protocol and support the CHR’s now over seven years old practice of highly

Continued on page 42
The V oice | 41
Continued from page 41
individualized age-dependent cycle management. (iii) The data support the “toxic” effects of exogenous gonadotropins, which has been an increasingly visible subject in the literature (please see also page 50; Are excessive gonadotropins toxic to ovaries?) Finally, (iv) the data potentially also support the notion that these “toxic” effects on follicle development may increase with advancing female age, which is a conclusion the CHR recently also has reached based on clinical and laboratory observations, resulting in increasingly milder stimulations at the CHR with advancing female age and in parallel to the CHR’s by now well-known HIER program of progressively earlier oocyte retrievals with advancing female age.
At the same time, these data should not be overinterpreted and require further clarification. As a retrospective study, it is difficult to know how many biases still exist in patient selection as well as cycle management. The authors, for example, point out that they did not differentiate between different FSH products. Nor did they, as it appears, use hMG products (mixed FSH and hMG). Overall, this is an important paper.
RESCUE IVM. We recently mentioned in these pages two publications that confirmed the benefits of another long-standing practice at the CHR, - namely so-called “rescue in vitro maturation” (rIVM) of immature oocytes, which has been routine practice at the CHR for over 10 years. Now the Colorado Center for Reproductive Medicine (CCRM), finally, has also caught up to the idea.2 Hopefully, they now will also catch up to other longstanding CHR practices that contradict CCRM practices, like only selected extended embryo culture to blastocyst stage and as little as possible PGT-A.
PROGESTIN PRIMING. Another treatment that has suddenly gained popularity is progestin-primed ovarian stimulation (PPOS) in IVF. Now a group of Chinese investigators published a paper in the JCEM, once more, making the point that new treatments proposed by one or two papers in the literature (and often of rather poor quality) should always be viewed with caution. These authors now report that in good-prognosis patients (that distinction alone

makes this paper a worthwhile contribution) PPOS appears to adversely affect cumulative live birth rates in comparison to women who were in GnRH–stimulated cycles. The reason appeared to be poorer blastocyst quality (i.e., likely poorer oocyte quality).3 Congratulations to our Chinese colleagues on an important paper!
PRIZE PAPER. If we are already talking about good as well as bad ideas, then how about the idea that, instead of planning with patients a “cycle-by-cycle strategy,” let’s go right away to “multicycle treatment planning.” Yes, this is not a joke! The joke is on us, the readers, and it is fully deserving of the title “most absurd article reviewed in this issue.” First-time IVF cycles allow for often highly significant new findings that prior to those IVF cycles, even with extensive diagnostic testing, are unavailable. To propose long-term treatment plans before the completion of at least one IVF cycle appears to be not only impractical, but unethical.
A recent “Inkling” article, something like an “editorial” in Fertility and Sterility, by a group of Italian colleagues (more about them below) amazingly, described the concept of going from a “cycle-by-cycle” to a “multicycle treatment plan” as “the next relevant shift in perspective needed in assisted reproductive technology” and then further described this new paradigm as,” possible and desirable, based on each professional’s ethics.”
But that is - to say it politely - pure hogwash. First of all, one must ask how anything in medicine can be “ethical” if it is dependent “on each physician’s personal ethics?” If that were how medicine was to be practiced, the world of medicine would be in chaos (some may argue that the world of medicine in Italy may, indeed, be in chaos).
Nothing in IVF is more important in fully understanding a patient’s infertility than her first IVF cycle because that cycle offers information that any other testing, otherwise, cannot predict. The argument that a patient’s infertility plan should be established for multiple cycles is, simply, absurd. However, it is also abusive just as any multiple-cycle package is abusive before one has acquired enough detailed knowledge about a patient to be able to predict whether she really will need multiple cycles.
That this opinion piece comes from the two senior authors on the paper, Filippo Maria Ubaldi, MD, MSc, PhD, and Laura Rienzi, MSc cannot be a surprise. Borrowing with some minor modifications a quote from Robert Gates, a past U.S. Secretary of Defense, Ubaldi and Rienzi “have not stopped being wrong for 20 years” of holding important positions in Europe’s IVF community. In contrast to most European colleagues, they have been at the forefront of promoting PGT-A and many other useless and, at times, harmful medical practices (“add-ons”) in IVF, all, of course, to significant degrees generating additional revenue for IVF clinics. What generates more revenue than, a-priori locked-in, and prepaid multiple-cycle IVF packages? One wonders who shepherded this article through peer review.
ARTIFICIAL INTELIGENCE
(AI). One cannot escape AI when discussing IVF-related papers these days. Here is an Israeli paper for change claiming to have demonstrated that a
42 | The Voice
machine-learning model for best ovulation trigger timing improved IVF cycle outcomes in antagonist protocols across all age groups in fresh and all-freeze cycles.5 These conclusions were reached after comparing actual trigger timing with timing (considered “concordant”) suggested by the system, with cycles where there was no correlation (“discordant” cycles) and after “concordant” cycles in several cycle sub-groups demonstrated bigger oocytes and embryo numbers in the “concordant” group.
It is hard to decide where to start to criticize this paper because so much is wrong with it (retrospective uncontrolled patient selection, no adjustments, etc.) but one must acknowledge that we are just at the beginning of AI utilization in IVF. It will have to get better if it is to be taken more seriously. At its current levels, we do not see how it can, or will, improve IVF outcomes.
SOCIAL EGG-FREEZING.
It has been known for some time that only a small fraction of women who freeze their oocytes to extend their potential fertile lifespan return and use their frozen eggs. But, most reported percentages were in the 20s. Now investigators from Boston, MA, reporting on 47, 363 patients undergoing 67,893 freezing cycles between January 2014 and December 2020, reported that to this point, only 2.5-3.0% of patients returned.6 Among those, 2.3% of women with normal ovarian response during stimulation returned but the rate was 4% in women with poor response. This difference was most notable among women between ages 30 to 34 at the time of egg-freezing, where the percentages were 16.7% and 8.4%, respectively, and between ages 35-39, where they were 21.1% and 14.9%. Time to return did not differ between normal and poor responders. Adjusted for age, multivariate analysis suggested that having fewer than five cryopreserved oocytes was associated with higher utilization of frozen eggs.
This is an important study that offers new information regarding social egg-freezing, which is so widely propagated by many clinics: (i) Return rates appear to be even lower than have been already reported before. (ii) Women with small egg numbers (especially if under five) returned at a higher frequency, likely because they suffered from low functional reserve (LFOR) and likely from premature ovarian aging (POA) and infertility. (iii) It appears that freezing eggs of women under age 30 makes little economic sense, - unless they suffer from POA. Finally, (iv) and not noted in the paper, women on average froze only eggs from 1.4 retrieval cycles, an abominably low number if women do wish to extend their reproductive lifespan and/ or are planning on multiple children.
Unfortunately, in most provider organizations, social egg-freezing can no longer be considered a medical procedure because women, quite obviously, do not even receive appropriate counseling as to how many oocytes they must freeze to produce at least a reasonable pregnancy chance for the desired number of pregnancies and children. Like so much else in reproductive medicine, social egg-freezing, primarily, appears to have become a business.
MORE TWINS WITH OBESITY? There exists a still unexplained paradox in infertility practice: Obesity in women as well as men is associated with decreased fertility and usually lower success rates for practically all fertility treatments. Yet, paradoxically twin birth rates increase in women in parallel with increasing BMI.
This was now once again confirmed in a study of Canadian and British investigators who in a cohort of 524,845 births reported a clear increase in twinning with increasing BMI, with the highest rates observed in women >BMI 40.7 Between BMIs 20 and 39.9 (Classes 1 & 2 of obesity), one-quarter of the increase could be attributed to more utilization of IVF, but that was no longer the case > BMI 40, where rates were the highest (see Table 1). The cause or causes are still unclear.
Table 1. Adjusted risks for twins based on weight in comparison to women with normal weight
REFERENCES
1. Xu et al., Sci Reports 2024;14:1462
2. Yuan et al., Fertil Steril 2024;121
3. Zhou et al., J Clin Endocrinol Metab 20014;109:217-226
4. Faustini et al., Fertil Steril
5. Reuvveny et al., Reprod Biomed Online 2024;(481):103423
6. Fouks et al., JAMA Network Open 2024;7(1):e2349722
7. BONE ET AL., JAMA Network Open 2024;7(1):e2350934
Polycystic ovary syndrome (PCOS)
That adipose tissue plays an important role in PCOS is well known. What is less well known, is that there is something called “adipose tissue dysfunction” (ATD), which appears to play an important role in the pathophysiology of PCOS, and not only in obese, but also in lean PCOS patients (phenotype D under Rotterdam criteria). As readers of this newsletter by know already know, there is almost nothing that interests the CHR currently more than the D-phenotype of PCOS.
A recent “mini-review” in The JCEM right away attracted our attention since, as an additional point of interest, its senior author (among nine authors) was Ricardo Azziz, MD, - “Mr. PCOS” himself.1 We were surprised in how many different ways ATD can express itself. Though the paper is at times somewhat confusing (even contradictory) and, clinically, adds relatively little to the current understanding of PCOS, it nevertheless is a worthwhile read.
The authors concluded that ATD appears to contribute more to metabolic and inflammatory abnormalities of PCOS than even adipose tissue distribution does. This is, in itself, an interesting finding for the CHR since, as recently reviewed in an earlier issue of the VOICE, published CHR research has concluded that PCOS, likely, is not a condition of four phenotypes (as suggested by Rotterdam criteria), but is more likely an amalgam of only two presentations, one “metabolic,” and the other “immunologic.”2 Interestingly, Azziz’s female counterpart as “Ms. PCOS,” Andrea E. Dunaif’, MD, from NYC’s Icahn School of Medicine at Mount Sinai and her group of
Continued on page 44
BMI RISK RATIO Simple overweight 1.14% 25-29.9 Obesity class I 1.16% 30-34.9 Obesity class II 1.17% 35-39.9 Obesity class III 1.41% >40
The V oice | 43
Continued from page 43
investigators reached similar conclusions,3 and will be addressing this subject as the CHR’s guest speaker of the CHR’s March GrandRounds on March 26, 2024.
Related, but addressing pediatric aspects of PCOS, investigators from Harvard University recently published an interesting article in the JCEM reporting pediatric features of genetic predisposition to PCOS,4 noting that genetic risk factors were associated with changes in several traits in children affecting metabolism, growth, and development. These findings offer a brand-new understanding of PCOS, suggesting that the condition does not only affect females post-menarcheal, but affects both sexes already in early childhood.
This is an important study, though it unfortunately perpetuates one shortcoming of too many PCOS studies, namely that all presentations (phenotypes) of PCOS are bunched together. And since, as already noted above, recent clinical data from the CHR2 and genomic data from NYC’s Mount Sinai3 strongly suggest that the current PCOS diagnosis includes two very distinct phenotypes, we have to repeat an argument here, which readers of the VOICE by now will be very familiar with: In PCOS, studies it appears high time to “clean-up” the patient selection process, if progress is to be made.
REFERENCES
1. Bril et al., JCEM 2024109:10-24.
2. Gleicher et al., Biomedicines 2022;10:1505
3. Dapas et al., PLoS Med 2020;17:e1003132
4. Zhu et al., J Clin Endocrinol Metab 2024;109:380-388 – PRIZE PAPER: Most absurd article reviewed in this issue.
Pregnancy &Obstetrics
Preeclampsia
Are estradiol levels (E2) in early pregnancy associated with preeclampsia risk? This is what Chinese investigators recently claimed in a paper in Frontiers in Endocrinology. They reported that E2 levels at week five of gestation were significantly higher in the 3rd and 4th quartiles of E2 than in the 1st and 2nd quartiles.1 The underlying hypothesis for this study was that preeclampsia has been associated with abnormal remodeling of spiral arteries and (though still controversial) that E2 plays an important role in placentation. Animal data also have suggested a role for estradiol in placentation.
Data were retroactively retrieved and came from a single University program in China in artificially built frozen-thawed embryo transfer cycles (FETs). Since results were adjusted for alleged confounders, one has to assign the obtained results some credibility despite the retrospective nature of data collection. This is also supported by the fact that FET cycles have repeatedly been associated with increased preeclampsia risk, especially in comparison to natural cycle FETs.
Comparing 447 infants with biliary atresia with 2,912 controls, the paper reported associations between E2 in week 5 of pregnancy (ca. week three after implantation) with preeclampsia. Since some IVF clinics carry estradiol supplementation into
early pregnancy, this finding could, therefore, be explained by still ongoing E2 support. We are somewhat skeptical about this report: E2 is just too omnipresent periconception and, if involved, in the pathogenesis of preeclampsia that early in pregnancy, should cause a much higher prevalence of preeclampsia than is observed in clinical practice.
Metformin in pregnancy
Among the most frequently used medications during pregnancy, metformin is generally considered a mostly safe drug in pregnancy, achieving similar glycemic control to insulin in pregnancy for all but the most severe diabetics. A recent review by European colleagues attempted to summarize the literature on the subject. They reported that its maternal utilization does reduce neonatal hypoglycemia and does not affect the prevalence of birth defects and low APGAR scores, and NICU admission. Metformin has been associated with premature labor and lower birth weight, though these associations may be more reflective of underlying medical problems in women who require metformin treatment rather than the drug itself. The literature also suggests that the drug may be associated with altered fetal programming, predisposition to childhood obesity, and metabolic syndrome in adulthood, though it is again difficult to separate these complications from underlying obesity and/or diabetes for which metformin was prescribed.
More worrisome, though less frequent, is the recently reported association of maternal prenatal infections with subsequent biliary atresia in offspring.2 Comparing 447 infants with biliary atresia with 2,912 controls, mothers of infants with obstruction reported significantly more urinary and gastrointestinal infections prenatally. Why that would be is presently still unclear.
Finally a breakthrough for hyperemesis gravidarum and beyond?
Though mild cases of hyperemesis gravidarum affect many (roughly two-thirds of) pregnancies and by some experts are considered a good prognostic sign in early pregnancy, the condition at times can be debilitatingly severe and extend into late pregnancy. A new finding, suggesting that maternal sensitivity to a hormone produced by the fetus may be the underlying cause, offers hope for potentially better treatment for this condition.3
The hormone GDF15 (Growth-Differentiating Factor-15), also often called macrophage inhibitory cytokine-1, is a divergent member of the transforming growth factor ß superfamily. It is rare in most tissues, but present in very high concentrations in the placenta. It increases with age and in response to inflammatory processes, and also serves as an immune checkpoint inhibitor, making it a potential target for cancer immunotherapy.4
That it is present in large quantities in the placenta and that it in absolute amounts increases in parallel with placental growth, suggests that it may play an important role in the placenta’s function of preventing the fetal-placental allograft from being rejected by the maternal immune system.
Excessive Cesarean section rates
That Cesarean section rates in the U.S. are too high has been widely bemoaned for decades,1 yet they have only continued to increase. However, nowhere have they so far reached the stratospheric level Puerto Rico has reached.2 Between 2010 and 2018, the rate ranged from 46.3 to 48.4%, afterward increasing every year even further and
44 | The Voice

ADVERTISEMENT The V oice | 45
Continued from page 44
reaching 50.5% of all births by 2022, which approaches Brazil’s rates, for decades considered the country with the highest Cesarean section rates of ca. 30% in public and 70% in private hospitals. Amazing!
REFERENCES
1. Gleicher et al., N Engl J Med 1988;319(23):1511-1516
2. Osterman MJK, Juiz Gallego MM. NCHS Data Brief. No 486; January 2024; https://www.cdc.gov/nchs/products/index.htm
Peripartum cardiomyopathy
This condition can lead to severe degeneration of cardiac function up to clinical heart failure and is characterized for occurrence during pregnancy or, up to five months, postpartum. It has several typical features of an autoimmune disease, though it is not (yet) accepted as such by cardiology. It has been reported to complicate ca. 1 in 2,000 births, though we would not be surprised if this turned out to be an underestimation since especially milder cases are not recognized as such and, are often misdiagnosed as preeclampsia.
An excellent review of this condition was recently published in The New England Journal of Medicine,5 even though we were seriously disappointed with how little attention a possible autoimmune etiology received in the article in a single sentence that suggested that supportive data for an autoimmune etiology are only very limited. We disagree because, as noted before, the timing of the condition follows the typical timing of autoimmune diseases. Moreover, like in autoimmune diseases, there exists a recurrence risk in following pregnancies.
REFERENCES
1. Hsieh et al., Front Endocrinol 2023; 14. https://doi.org/10.3389 fendo.2023.1223181
2. Wang et al., JAMA Network Open 2024;7(1):e2350044
3. Fejzo et al., Nature 2024;625:760-768
4. Wischhusen et al., Front Immunol 2020;11:951
5. Arany Z. N Engl J Med 2024;390:154-164

















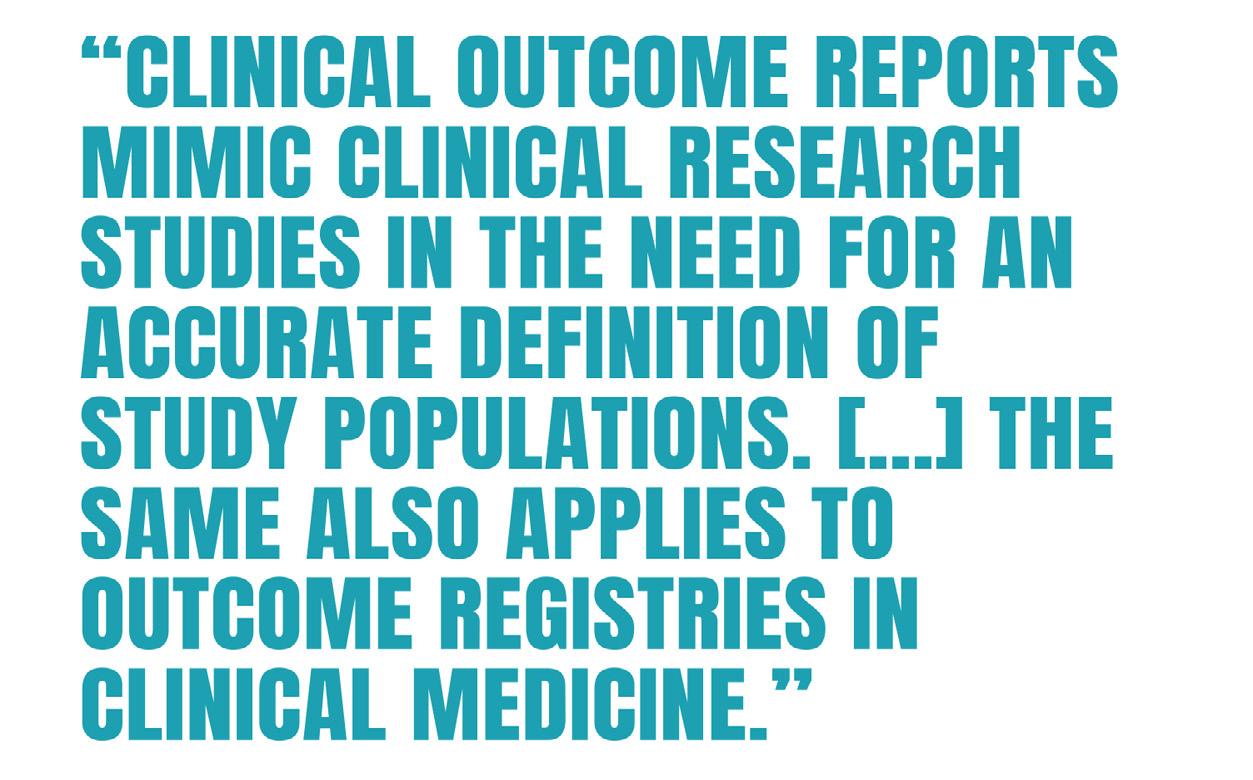

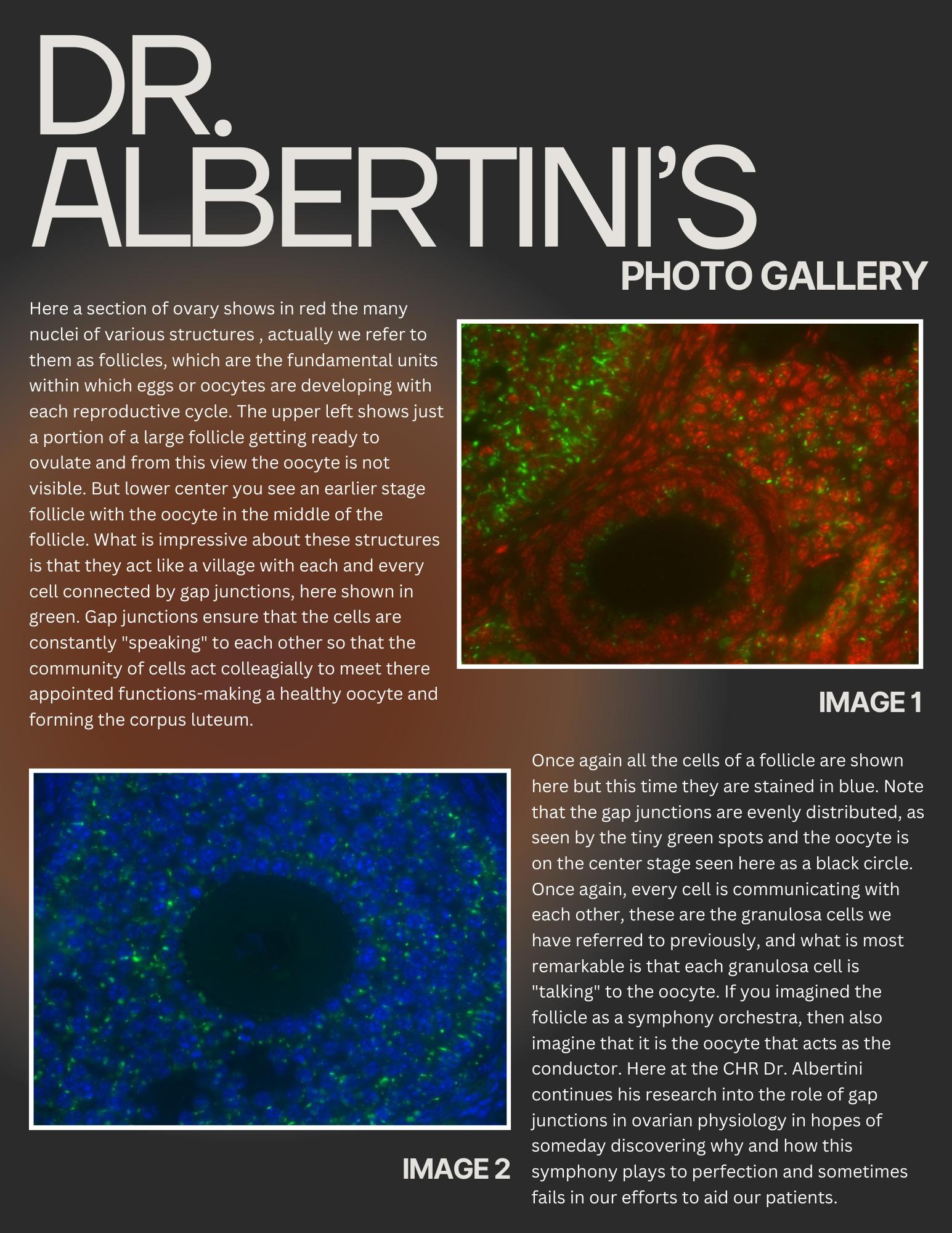



 Photo Credit: New Scientist
Richard Horton, OBE, FRCPCH, FMedSci
Photo Credit: New Scientist
Richard Horton, OBE, FRCPCH, FMedSci