THE CENTER FOR HUMAN REPRODUCTION JANUARY 2023 in this month’s issue The CHR Letter Endometriosis: The Condition nobody knows much about, Part III Polygenic Risk Scoring - The next commercial scam involving embryo testing in association with In Vitro Fertilization (IVF) A Piece of My Mind: What made us physicians believe we know better than patients what is good for them? The CHR’s Interpretation Of Recent Medical Literature relevant to reproduction 03 04 09 15 22 23 Frozen Donor Egg Banks - What we want The CHR’s patients to know 11 CHR publications 22
The CHR is known as a “fertility center of last resort,” primarily serving patients who have previously failed treatments elsewhere. Among CHR’s areas of special expertise are treatments of “older” ovaries, whether due to advanced female age or premature ovarian aging (POA), immunological problems affecting reproduction, repeated pregnancy loss, endometriosis, polycystic ovary syndrome (PCOS), tubal disease, male factor infertility, etc.

Missed the last issue of The VOICE?
Access previous issues on thechr.com



AT THE CHR
BOARD-CERTIFIED RE-I AT ASSOC. PROF/PROFESSOR LEVEL

The CHR is looking for another senior board-certified RE-I (or international equivalent) to join our growing national and international practice. Though private, our center is organized along academic principles in that physicians are expected to excel not only as clinicians but also as researchers. The center’s uniquely structured compensation package, therefore, incentivizes both activities. We are looking for an individual with documented excellence in both areas, commensurate with associate professor/professor level. Besides a competitive salary, incentive bonus structure, and excellent benefit package, the CHR also offers partnership along either a 3-year or 5-year equity track and, ultimately, part or complete ownership, as the current leadership is expected to retire within that time-period.
If you feel qualified for the position and share our philosophy of being a physician-scientist, please let us know by submitting your C.V. and a brief letter of interest to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position can be filled immediately. All submissions are considered confidential.


CONNECT WITH THE
CHR
www.thechr.com @CHRNewYork @CHRNewYork @CHRNewYork 2 | january 2023 | The Voice
hirinG
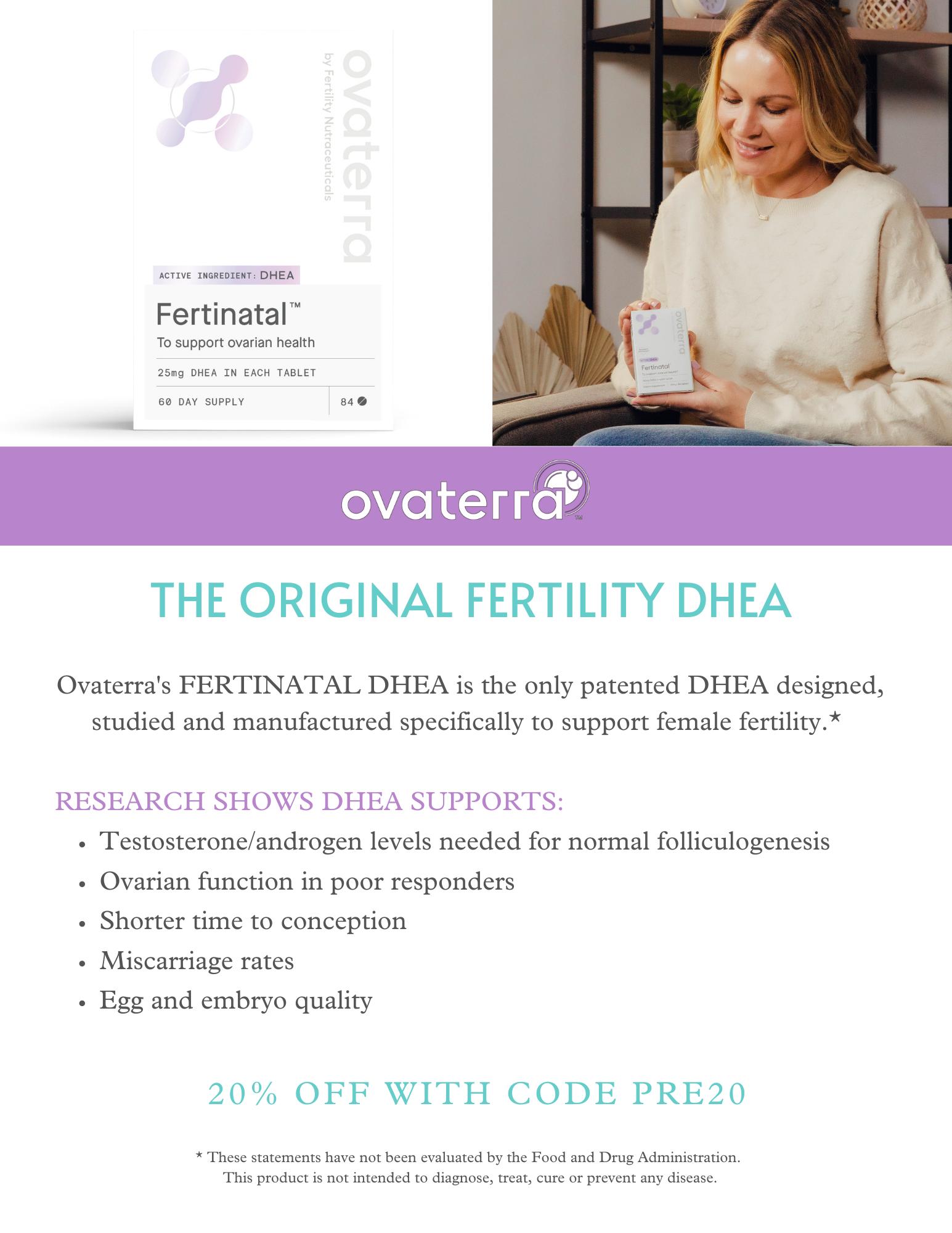
ADVERTISEMENT
the VoiCe
With this January issue, we are very pleased for the year 2023 to welcome back to The VOICE, the monthly newsletter of the CHR, - you, our reader. In this newsletter, we are trying to inform you about what we, here at the CHR, consider relevant and important information for reproductive medicine. Our rapidly increasing, very diverse readership includes lay people (often potential or already active infertility patients), physician colleagues practicing reproductive endocrinology and infertility, basic scientists working in reproductive biology, especially embryology, as well as clinical embryologists, carrying the enormous daily laboratory burden of in vitro fertilization (IVF). Not to be forgotten, we also mail this newsletter to a substantial list of science and medical writers/ journalists interested in reproductive medicine.
With an e-mailing list of over 80,000 individuals and close to an almost unbelievable 25% opening rate, almost 20,000 reproductive medicine interested individuals currently read at least parts of our monthly newsletter. As we are expanding our mailing list, we, of course, plan on expanding the readership further during 2023 and encourage other fertility centers to consider their distribution of this newsletter with the option of personalizing The VOICE to their practices. If you are interested in a potential licensing agreement for individual articles, sections, or complete issues of The VOICE, please contact Micah Elias at melias@thechr.com for further details.
Though we, of course, are trying to be as objective as possible in presenting medical facts, we cannot deny that The CHR, at times, disagrees with widely held opinions in the infertility field which then, of course, is reflected in the newsletter. This is not different from any newsletter, magazine, newspaper, or social medium that differentiates between news and editorials, except that we, hopefully, come across as more transparent, when representing primarily CHR’s opinions rather than consensus in the infertility field (which, of course, these days exists only rarely). Moreover, we also want to point out what we have noted many times before on these pages, - we always welcome opposing responses to any article that appears in The VOICE, whether in a response to a CHR opinion or a news article.
As always, this issue of The VOICE in the front part caters primarily to patients and laypeople by offering general knowledge patients frequently ask about. We in this issue continue our Endometriosis series of articles with Part III. But we also try to inform the public about developments in the field that may be more practically related to fertility treatments. We, therefore, in this issue, for example, discuss observations about egg quality in donor egg banks and advise our readers how to be selective in purchasing frozen donor eggs. We also address in more detail the so-called polygenic risk scoring of embryos, an additional embryo testing procedure now being offered by increasing numbers of IVF centers in the U.S., - and not necessarily to the advantage of most infertility patients.
The back part of the newsletter, as always, contains our “relevant” literature review of published papers in preceding months, which among colleagues and researchers in the field quickly has become the most popular section of The VOICE. In between both of these sections of the newsletter there, of course, are lots of additional materials for everybody, and we, as always, are very much looking forward to your comments.
JANUARY 2023 The V oice | january 2023 | 3
The Editorial Staff of the VOICE
ENDOMETRIOSIS
ENDOMETRIOSIS
THE CONDITION NOBODY KNOWS MUCH ABOUT PART III
Only a FEW subjects in female medicine are surrounded by as much “mystique” as the condition known as endometriosis. Because endometriosis clinically affects women especially during reproductive years, it is erroneously widely perceived as mostly a reproductive disease, causing infertility. It often, however, also causes pelvic pain and several other symptoms. Endometriosis is, however, a much more complex condition than that, and in many women greatly affects quality of life. After in the november issue offering Part I in a series of articles on endometriosis, we here continue with Part II giving our readers a detailed view of how clinicians and scientists at the CHR currently view this condition. Further segments will follow in the new year.
What is the place of surgery in endometriosis?
We noted in earlier parts of this series of articles that endometriosis is not only a major cause of female infertility but also a major gynecological problem, strongly associated with pelvic pain and other symptoms which frequently adversely affect the quality of life. Consequently, when addressing the place of surgery in endometriosis, one must differentiate between surgery to improve fertility and surgery to improve clinical symptoms, mostly pain.
Infertility surgery Surgery with the primary purpose of improving spontaneous fertility and/ or the chances of pregnancy with infertility treatments, including IVF, is the most controversial subject when it comes to treating endometriosis surgically. Nobody, of course, can argue against the need for surgical interventions if endometriosis causes excruciating pain or other debilitating symptoms in general gynecological practice. But when it comes to surgery in efforts to improve the fertility of a
woman, considerations are much more complex and, therefore, more controversial because in such cases surgery can also have very detrimental effects on future fertility chances.
The CHR in such circumstances, therefore, follows a very conservative philosophy that requires that the evidence of potential outcome benefits either is overwhelming or medical circumstances offer no possible choice but surgery. Let us explain further: Assume a patient who due to endometriosis has severely damaged fallopian tubes filled with large amounts of fluid (so-called hydrosalpinges). Since these fallopian tubes are unsalvageable and backflow of the tubal fluid into the endometrial cavity can harm embryos, we may recommend the removal of such tubes before the initiation of an IVF cycle. The risk/benefit consideration here appears obvious: the tubes have become useless, - indeed, may increase the risk of tubal pregnancies) and may harm pregnancy chances in subsequent IVF attempts. Moreover, their removal creates no significant new future risks for the patient.
Or take another situation: A woman presents with severe acute abdominal pain and upon physical examination demonstrates so-called “peritoneal signs,” suggestive of peritonitis. On ultrasound, she is found to have a large endometrioma in her right ovary and the suspicion is that she may either be leaking from this endometrioma or may have twisted her ovary on its stump because of the additional weight of the endometrioma. Both possibilities represent potentially life-threatening emergencies and, of course, mandate surgery.
In contrast, an infertility patient who on initial investigation is found to have endometriomas in both ovaries but exhibits no related symptoms. Even if these endometriomas are of equal size as the endometrioma in the preceding case, we here at the CHR would strongly recommend against surgery to remove them in this case because, even in the best surgical hands, still healthy ovarian tissue is removed, in resection of an endometrioma and that, very well, may put a patient with already low functional ovarian reserve into full menopause. Such a patient
4 | january 2023 | The Voice
Continued on page 5
was, of course, not helped but harmed by her surgery.
It is important to reemphasize that opinions on this subject can differ and that not everybody in the field agrees with CHR’s conservative approach. Especially so-called reproductive surgeons, colleagues who specialize in complex surgeries on reproductive organs, very often advocate for more aggressive surgical approaches, mostly emphasizing their “special surgical skills.” We, however, have unfortunately seen too many women who, even in the best surgical hands, have come out of surgeries castrated and in menopause. There is a saying in surgery that, “once one goes in (i.e., into surgery), one never knows where one comes out.”
The most controversial issue in infertility-related endometriosis surgery is, however, paradoxically not the severe case of disease but so-called mild endometriosis (i.e., Stage I of disease) because here, too, reproductive surgeons often advocate aggressive pre-treatment surgery in attempts to fulgurate and/or excise as much visible endometriosis as possible. They argue that this improves spontaneous pregnancy rates as well as IVF success, first
suggested by Canadian investigators in 1997 after performing a prospectively randomized study,1 and later supported by a 2014 Cochrane Review that later was withdrawn without explanation.2 Unsurprisingly, the concept of surgery for mild endometriosis has, therefore, remained controversial,3 and CHR in most cases does not support it. The CHR also does not support the performance of automatic laparoscopy/hysteroscopy in advance of IVF cycles to rule out the presence of mild endometriosis, as is a practice in many IVF centers, because, even if mild endometriosis is confirmed, this diagnosis does not change IVF treatments in any way. Why then do the surgery?
REFERENCES:
1. Marcoux et al., N Engl J Med 1997;337(4):217-222
2. Jacobson et al., Cochrane database of Systematic Reviews. https://doi. org/10.1002/14651858.CD001398.pub3
3. Daniilidis A, Pados G., Reprod Biomed Online 2018;36(1):84-87
Endometriosis as a fertility diagnosis

This then raises the question, of whether and/or how endometriosis affects female fertility and, as essential as this question is to the understanding of
endometriosis as well as female infertility, the likely, surprising answer is that, as of this point, there really is no good overall answer to this question, - aside of a circumstance where endometriosis has irreversibly destroyed a woman’s fallopian tubes and in vitro fertilization (IVF) remains the only realistic chance to achieve pregnancy. And even this circumstance is not the universal answer because The CHR’s first ever IVF pregnancy (in Chicago) in 1981 was established in a woman after three failed major surgeries by the world’s leading tubal surgeons, who after her first birth went on to deliver two children after spontaneous conception.
This case, indeed, greatly influenced The CHR’s longstanding opinion that endometriosis to significant degrees is an unpredictable condition that, therefore, requires careful individualization in management. Tubal disease often involves scar tissue formation between fallopian tubes and surrounding anatomic structures and such scar tissue can “separate” in pregnancy, as the uterus grows and ascends out of the pelvis, thereby stretching, at times, loosening scar tissue and, thereby, freeing fallopian tubes.
Individualization of treatment is further essential because of what endometriosis does to ovaries, and specifically to egg quality, has remained a controversial issue: While there is agreement that intraovarian endometriosis can, and often does reduce functional ovarian reserve (the number of eggs in an ovary), what it does to egg quality has remained unresolved. Some studies have suggested that the condition reduces the quality of oocyte morphology,1 other studies suggested that it has little or no effects on egg quality.2 The likely correct answer, therefore, is that effects on egg quality, therefore, may vary, - yet another strong rationale for individualization of care, by now a focus and for several decades another main characteristic of infertility treatments at The CHR.
REFERENCES:
1. Robin et al., Reprod Biol Endocrinol 2021;19(1):160
The V oice | january 2023 | 5
Continued on page 6 Continued from page 4
2. Garcia – Velasco JA, Arici A. Hum Reprod 1999;14Suppl 2:77-89
Is endometriosis an immunological disease?
Another main issue of controversy has been the underlying pathophysiology of endometriosis, - whether it is an inflammatory disease or even an outright autoimmune condition. This is an important question because, if appropriate treatments are to be developed, one, of course, must, first, understand the underlying pathophysiology. There is consensus that endometriosis is associated with inflammation.3 This, however, does not settle whether inflammation is local, surrounding endometrial islands of cells, systemic, or both. This differentiation is important because, assuming inflammation is systemic, it may be a contributing factor to the establishment of endometriosis by preventing the expected rejection of endometrial cells that attempt to implant after retrograde menstruation into the peritoneal cavity. In other words, endometriosis is a classic example of the ancient question, what comes first, the egg or the chicken? In this case, this means that we still don’t know whether a female immune defect leads to endometriosis by allowing the implantation of endometrial cells or whether endometriosis leads to immune system abnormalities, including inflammation.
We would argue that until this question has been resolved, the pathophysiology of endometriosis will remain unexplained. That endometriosis is significantly associated with immune abnormalities has not been in dispute for decades.1 The CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, indeed, already in 1987 suggested that endometriosis may be an autoimmune disease.2 One of the classical features of autoimmune diseases is a significant association with other autoimmune diseases, - a
characteristic endometriosis shares.3 Also supportive of such a notion is the increased miscarriage risk in association with endometriosis,4 which is seen in all medical conditions associated with a hyperactive immune system, including autoimmune diseases.5 Individualized medical care of endometriosis, therefore, not only mandates attention to female fertility but also consideration of increased miscarriage risk.
REFERENCES:
1. Giudice LC, Kao LC. Lancet 2004;364(9447):1789-1799
2. Gleicher et al., Obstet Gynecol 1987; 70(1):115-122
3. Shigesi et al., Hum Reprod Update 2019;24(4):486-503
4. Farland et al., Obstet Gynecol 2019;134(3):527-536
5. Javinani et al., J Clin Rheumat 2022;28(1):e166-e170
The importance of diet
A much more recent evolution in our understanding of endometriosis has been the importance of diets,1 and especially of an anti-inflammatory diet in treating endometriosis. Though available studies as of this point are sparse and of limited quality, The CHR’s staff is convinced of the benefit of an anti-inflammatory diet for endometriosis symptoms. Though so far mostly an anecdotal experience, we have seen significant improvements
in symptoms following a switch to exclusion diets for gluten, dairy, and sugar. Further studies are, of course, still required; but The CHR’s physicians very often recommend such a diet to patients affected by endometriosis. Simply based on that endometriosis unquestionably is associated with inflammation, such a diet empirically makes sense.
REFERENCES:
1. Aslaug Sverrisdottir et al., Eur J Obstet Gynecol Reprod Biol 2022;271:245-249
Conclusion of this series of articles
In this series of three articles, we attempted to summarize important aspects of endometriosis that we feel often are not well understood by the public. Endometriosis, affecting approximately 10% of women of reproductive age and often still undiagnosed for many years, is by many considered the most frequent cause of female infertility.1
For those interested in more detail, we recommend a very recent review in the British literature, also discussed in our monthly literature review in this issue of The VOICE 2
REFERENCES:
1. Mercuri ND, Cox B J., Elife 2022;11:e75061
2. Ye et al., BMJ 2022:379. https://doi. org/10.1136/ bmj-2021-068950
6 | january 2023 | The Voice Continued from page 5
“One of the classical features of autoimmune diseases is a significant association with other autoimmune diseases, - a characteristic endometriosis shares”
Have you thought about advertising in the VOICE?
This newsletter every month goes electronically to ca. 80,000 infertility patients, medical professionals in the field, and members of the media, with almost 25% (an unusually high number) also opening the VOICE.

For further information, please contact: Ms. Alexandra Rata (212) 994 4400 or e-mail to arata@thechr.com
AT THE CHR
ONE or TWO-YEAR CLINICAL FELLOWSHIP in RE-I


If you failed in securing a formal fellowship position in RE & Infertility or simply want a change out of general OB/GYN practice, the CHR offers a fellowship position in RE-I which after 1 year will greatly improve competitiveness for a formal fellowship position and in 2 years establishes independent competence for establishing an infertility practice. The center’s last 1-year fellow was accepted into the NIHfellowship program after failing to secure a position in the preceding year.
Qualified candidates must be OB/GY board-eligible or certified, be eligible for hospital privileges and for a New York state license to practice medicine. As CHR maintains a very active research program in affiliation with Rockefeller University, CHR fellows gain substantial research experience, with great likelihood resulting author- or co-authorships in peer-reviewed publications. Board eligible candidates who still must accumulate surgical cases will be given the opportunity to do so.
Chosen candidates will receive a very competitive salary and a generous benefit package, including health and malpractice insurance as well as paid vacation time. If you feel that you qualify and are interested in a career in RE & I, please submit your CV and a brief application letter to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available as of January 1, 2023. All submissions are considered confidential. The V oice
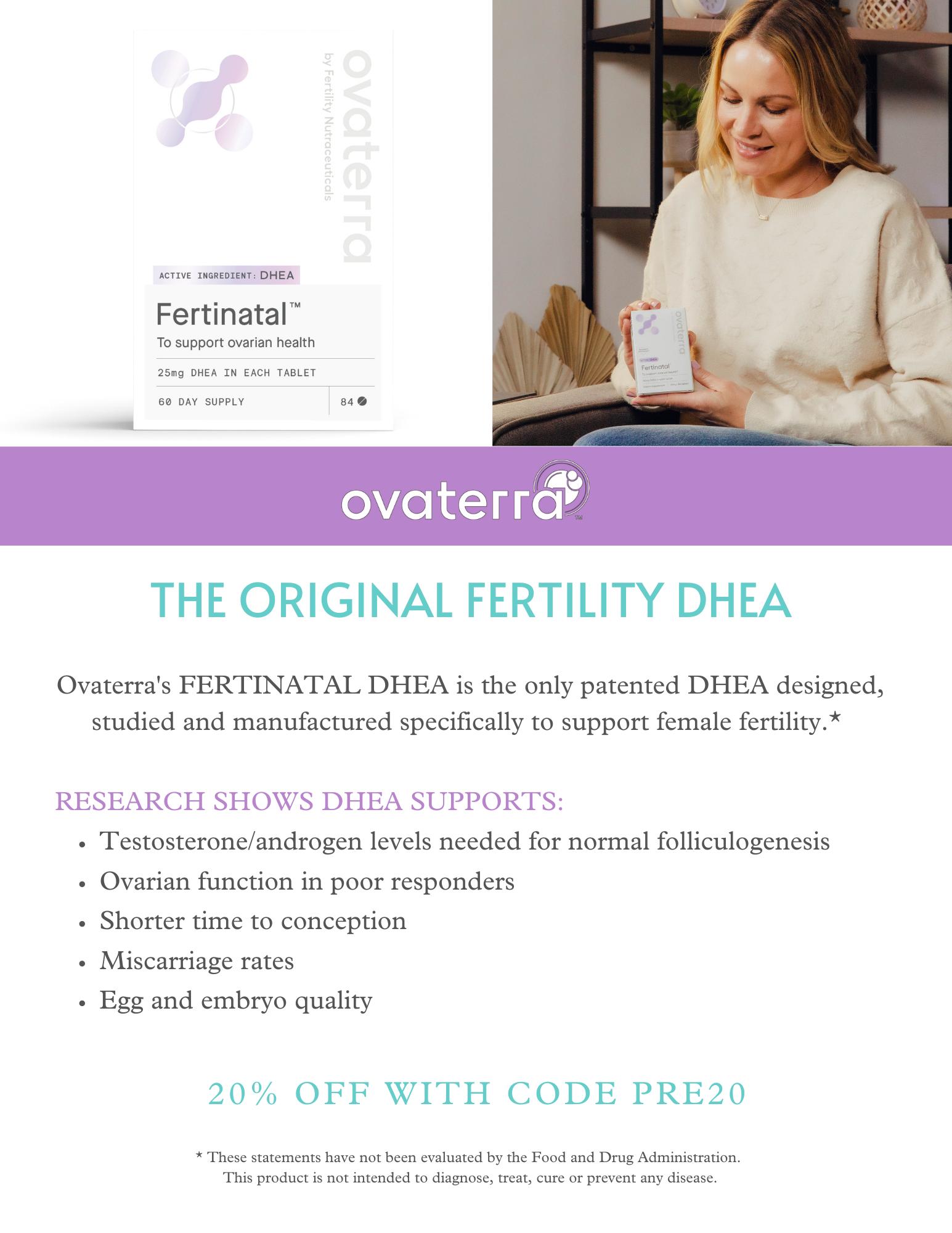
ADVERTISEMENT
hirinG
| 7 ADVERTISEMENT
| january 2023
TRYING TO REACH THE INFERTILITY COMMUNITY?
ADVERTISEMENT
Amazing experience. Dr Gleicher is really great, explains everything in detail. He asks you about the smallest details regarding your health and looks at the problem holistically. The staff at CHR is great, very friendly and professional.

- TG
PATIENT TESTIMONIALS
PATIENT TESTIMONIALS PATIENT TESTIMONIALS PATIENT TESTIMONIALS
“
There’s no real words do describe how caring, informative, knowledgeable, and helpful Dr. Barad is for the mind and fertility! There’s no better hands to be in! - SO
8 | january 2023 | The Voice
“
POLYGENIC RISK SCORING
the next commercial scam involving embryo testing in association with in vitro fertilization (IVF)
In association with IVF, the concept of embryo testing prior to transfer into the uterus has been around for over 25 years. It started with what was then called PGD (preimplantation genetic diagnosis) and involved embryo biopsy at the cleavage stage of 1-2 blastomeres (1-2 cells of a 6-8-cell embryo) in attempts to diagnose embryos that carried single gene diseases with nested PCR.1 PGD from the very beginning was highly accurate and has survived as an almost unchanged concept ever since, though the name of the procedure has been changed to PGT-M (preimplantation genetic testing for monogenic diseases) and embryo biopsy is now routinely performed at blastocyst-stage, allowing for more DNA to be obtained.
Had embryo testing remained restricted to PGD/PGT-M, the concept of embryo biopsy likely would never have become controversial. That was, however, not the case because geneticists in the U.S.2 and later in Europe3 expanded embryo testing to what initially was called PGS (preimplantation genetic screening) at cleavage stage (PGS 1.0), later like PGD moved to blastocyst-stage (PGS 2.0) and renamed PGT-A (preimplantation genetic testing for aneuploidy). In contrast to PGD/PGT-M, this expansion of embryo testing to PGS/PGT-A from the very beginning was controversial and opposition to this procedure’s utilization in IVF has, indeed, greatly increased over the years. Since PGS/ PGT-A has been the subject of many articles in The VOICE, we here will not be repetitive. Only so much: The CHR considers PGS/PGT-A to be a useless test that, contrary to decades-long claims, does not improve IVF outcomes. PGS/PGT-A is, indeed, actually harmful for many infertile women/couples by reducing cumulative pregnancy and live birth chances for them. The CHR, therefore, except in very rare instances recommends against the utilization of PGS/PGT-A and its researchers have extensively published on the subject over the years.4-9 Over the years, prominent colleagues also have increasingly shared in this opinion.10-13
Continued on page 10 The V oice | january 2023 | 9
The genetic testing industry which, mostly because of PGS/ PGT-A, has grown into the likely most powerful interest group in reproductive medicine (even replacing “Big Pharma”), has continued to (in economic terms) successfully market PGS/ PGT-A to colleagues as well as the public. Not only is the clinical utilization of embryo biopsies for these reasons, therefore, in the U.S. still growing, but some of the most prominent supporters of PGS/PGT-A over the decades now have doubled down on the concept of embryo biopsy prior to embryo transfer by recommending the testing of embryos for so-called polygenic risk scores (PRS). And what makes things even worse, some IVF centers in collaboration with some genetic testing laboratories (yes, the same labs also performing PGS/ PGT-A testing) already have started offering such testing in clinical practice.

To understand how absurd and truly unethical this is, the concept of polygenic risk scoring must be explained. We noted above the accuracy of PGD/PGT-M in detecting single-gene diseases in embryos. Most medical conditions are, however, not caused by single gene abnormalities but are polygenic (i.e., predisposition is inherited by a combination of genes and/or environmental factors). Instead of evaluating the risk of a single gene in association with single-gene diseases (which, as noted above, is simple and accurate) PRS, based on whole genome analyses statistically evaluates the polygenic risk of an individual to develop disease.14 In contrast to assessing single gene risks, the assessment of PRS is much more complex mathematically, - but also, as noted above, strongly affected by environmental factors which, of course, have their own highly significant complexities.
In principle even in adult medicine still an experimental concept, mostly used to determine the risk in older individuals to develop diseases like diabetes mellitus, hypertension, or heart disease, it even in adult medicine has remained a controversial subject of many ethical, legal, and social debates.14 It, therefore, does not take an expert to understand that in embryos PRS must be considered even more “experimental.” That is, of course, exactly the case, - not the least because, currently, it is impossible to predict how accurate prediction models in embryos really are, - even if a recent study attempted to claim exactly that with a genotype accuracy of 99.0-99.4%.15
One also wonders how the accuracy of such predictions will ever be determined, considering that any embryo tested must on the first implant, become a normally developing pregnancy, deliver and then grow up to develop or not develop diabetes, hypertension, heart disease, or any other medical condition over 40 or 50 years. And all of this does not yet even consider the above-noted environmental influences. The only thing that is certain because of PRS is that even more perfectly fine embryos with excellent pregnancy and live
birth potential will end up discarded and pregnancy chances from IVF will be further reduced.
Unsurprisingly, the clinical utilization of PRS in association with IVF has, therefore, been widely criticized as premature, and was even rejected and declared unethical by the European Society for Human Genetics 9,16-18 That U.S. genetics laboratories and IVF centers already offer PRS is, therefore, in The CHR’s opinion outrageous, and that neither ASRM nor FDA are doing anything about it, is a scandal. One, of course, also cannot forget that, at least theoretically, PRS can also be used to choose blue eyes in an embryo (already being advertised!!), intelligence, and – who knows – maybe also Michael Jordan’s basketball talents. Do we really want to live in such a world? That should at least be discussed before implementation! REFERENCES:
Ray PF, Handyside AH. Methods Mol Med 1996; 5:245-258
Verlinsky Y, Kuliev A. Hum Reprod 1996;11(10):2076-2077
Ginaroli et al., Fertil Steril 1999;72(5):837-844
Gleicher et al., Fertil Steril 2008;106(1):75-79
Gleicher et al., Trends Mol Med 2021;27(8):731-742
Gleicher et al., Clin Chem 2022;68(4):501-503
Barad et al., Hum Reprod 2022;37(6):1194-1206
Barad et al., Hum Reprod 2022;37(5):2216-2218
Gleicher et al., Nat Med 2022;28(3):442-444 10. Cornelisse et al., Cochrane Database Syst Rev 2020; 9(9):CD005291
Mastenbroek et al., N Engl J Med 2021;385(22):2096-2100
Schattman GL. Fertil Steril 2019; PMID: 31843076 13. Orvieto et al., Hum Reprod 2021;36(5):1186-1190 14. Chapman CR. J Commun Genet 2022; doi: 10.1007/s12687022-00625-9. Online ahead of print. 15. Kumar et al., Nat Med 2022;28(3):513-516 16. Costello JF, Fisher SJ. N Engl J Med 2021;385(1):87-89 17. Polyakov et al., Hum Reprod 37(10):2229-2236 18. Forzano et al. Eur J Hum Genet 2022;30(5):493-495
1.
2.
3.
4.
5.
6.
7.
8.
9.
11.
12.
Continued from page 9 10 | january 2023 | The Voice TRYING TO REACH THE INFERTILITY COMMUNITY? Have you thought about advertising in the VOICE?
This newsletter every month goes electronically to ca. 80,000 infertility patients, medical professionals in the field, and members of the media, with almost 25% (an unusually high number) also opening the VOICE
ADVERTISEMENT
For further information, please contact: Ms. Alexandra Rata (212) 994 4400 or e-mail to arata@thechr.com
For several reasons the demand for third-party donor eggs is worldwide steadily increasing: One major contributing factor is obviously the “graying” of infertility patients, - i.e., infertility patients are getting progressively older. Here at The CHR, we are seeing this trend, likely, at the extreme since our center serves the by far oldest patient population among reporting U.S. IVF centers (and likely in the whole world), with the median age, year-by-year, slowly advancing toward 44 years. For over three years, the median age has already been above 43 and is steadily climbing, meaning that over half of the center’s patients in recent years have been over the age of 43 years.
Especially in the U.S. (but increasingly elsewhere as well) IVF practice patterns favor in almost all women above ages 42-43 third-party egg donation over attempts at conception with autologous oocytes and, therefore, are a second major reason for increasing donor-egg cycles. That only too few IVF centers are willing to give women above that age realistic tries with the use of their eggs, has been repeatedly lamented in the pages of The VOICE and shall, therefore, here not be as subject of further discussion. But, in The CHR’s opinion, it cannot be overstated, how many infertile women, because of this practice, are unfairly deprived of chances of genetic motherhood.
FROZEN DONOR EGG BANKS
AND WHAT WE WANT THE CHR’S PATIENTS TO KNOW
And then comes the subject of this article, - the establishment and rapid evolution of frozen commercial egg banks which, unquestionably, have improved egg donor selection options for patients and have simplified the process of egg donation for patients as well as medical providers. In the process, they also have made frozen donor egg cycles even more profitable for IVF centers than they were before egg banks existed when IVF centers had to maintain their egg-donor pools (a very expensive process for IVF centers).

It consequently was no surprise that with quick growth in the number of commercial frozen egg banks, the IVF field started seeing parallel declines in the number of IVF centers that still maintained their own egg-donor pools. Consequently, also unsurprisingly, frozen donor-egg cycles in the U.S. are now significantly more common than fresh donor cycles. Already by 2017, per Google, 3,452 frozen cycles beat out 3,324 fresh donor egg cycles.1
But just because the IVF field in a majority is clearly favoring the use of frozen donor eggs does not mean that the use of frozen donor-bank eggs is necessarily the best choice for every infertility patient considering egg donation. There, indeed, are several good reasons why patients (and their physicians) may prefer fresh over frozen eggs.
Continued on page 12 The V oice | january 2023 | 11
Continued on page 12
One very good reason, for example, is that fresh eggs offer better pregnancy chances than frozen eggs, a point first demonstrated by The CHR’s investigators several years ago,2 and rather aggressively disputed by representatives of the then still-evolving egg-freezing industry,3 reaffirmed a few years later by The CHR’s investigators in a larger follow-up study,4 and recently once again confirmed with an even larger margin of difference by a third group of investigators, suggesting a ca. 12% live birth difference in favor of fresh over frozen donor eggs (66.7% vs. 54.2%).5
Even this difference in outcome may, however, not be reason enough to automatically reject the use of frozen donor-bank eggs. Better convenience for patients and treating physicians, greater donor selection, and, possibly, also cost advantages for patients are, all, good reasons to consider such an option in an individualized recommendation given to patients. Yet, as with all information physicians offer to their patients, the information provided should be all-inclusive and unbiased and this, as we hear from many patients, is, often, not the case.
We here, therefore, want to clean up some of the biased opinions patients appear to receive from counselors at some frozen egg banks and from physicians at selected IVF centers: Within this context, we above already pointed out the by now well-established outcome differences between fresh and frozen donor oocytes, which to this day are frequently denied by representatives of the egg-banking industry and at IVF centers. Interestingly, the argument in the early days of egg banking was that results with frozen donor eggs would improve, as more IVF centers would familiarize themselves with using frozen rather than fresh eggs.3 The opposite, however, happened: as the use of frozen eggs moved from research centers into general practice, the gap in outcomes, indeed, approximately doubled.4,5

Once again this, however, should not surprise and, indeed, was predicted by the CHR’s investigators based on long-established facts in IVF and on simple logic: Donor egg banks in a majority receive oocytes from different IVF centers, with greatly varying IVF practices. Even if IVF cycle protocols are “equalized” between centers, outcomes will vary in full analogy to a dish executed by different chefs in different kitchens will taste differently, even if derived from the same recipe. Egg-banks, therefore, by definition, must offer eggs of different quality, a fact commercial egg-banks are not denying, while trying to compensate for with “thaw-out guarantees” (i.e., minimum guaranteed well-thawed out oocytes producing embryos). Especially over more recent months, we at the CHR, however, noticed a clear decline in egg quality from
some egg banks and, in parallel, a reluctance by some to compensate patients properly if oocyte thaw-out rates fell below promised minimums.
Most telling was, however, an unexpected coincidence when two of the center’s patients, independently, selected eggs from the same egg-donor cycle at the same commercial donor egg bank. When investigating why both demonstrated unexpectedly poor cycle outcomes, we found out that they shared a donor, who had produced in her cycle in excess of 40 eggs that went to at least three different recipients (and possibly even more), with our center’s patients being two of them. That egg quality is adversely affected in women producing excessively large egg numbers (in this case an obvious PCOS patient)6 should have been obvious to the egg bank. It, therefore, should have been more selective in determining which of the donor’s eggs would be offered for purchase by patients.
This occurrence in addition, however, raised at The CHR additional concerns about (conscious or subconscious) purposeful overstimulation of young egg donors for financial gains from large egg yields, benefitting IVF centers and/or commercial egg banks: more eggs produced, of course, means more oocytes are available for sale. That this suspicion must be considered was demonstrated approximately a decade ago when this issue for the first time surfaced in IVF. Several prominent infertility specialists in Israel were then accused of purposefully having overstimulated some of their egg donors for commercial gains and, in the process, of course, exposing them to significant risks of developing ovarian hyperstimulation syndrome
Continued from page 11 12 | january 2023 | The Voice
Continued on page 13
(OHSS).7 Some of these cases went to court and some of the physicians lost their medical licenses and academic positions.
In summary, like most IVF centers, the CHR, mostly because of patient choices, has in recent years been increasingly using commercial donor-egg bank oocytes in donor-egg recipient cycles. In contrast to other IVF clinics, the CHR, however, has not dissolved its fresh donor pool; very much to the contrary, because of the above outlined problems, the center recently decided on an expansion. In addition, one of the larger egg banks just announced a significant price increase for frozen eggs, further raising questions about the claim made by the egg-banking industry that the use of frozen eggs “saves money.”
Obviously worried about some of the developments we have been observing, we, as noted, are at the same time also very cognizant of the many advantages frozen donor
eggs offer patients and IVF centers. This article, therefore, is not meant to in any way denigrate the utilization of frozen donor eggs. The CHR, indeed, maintains its own small frozen donor-egg pool, made up from those fresh donor cycles where recipients did not purchase all freshly retrieved oocytes. We, however, also do not ignore the associated negatives when working with frozen donor-bank oocytes and strongly feel that our (and other centers’) patients deserve objective disclosure when considering third-party egg donation.

REFERENCES 1. https://tinyurl.com/2d2cv245 2. Kushnir et al., JAMA 2015;314(6):623-624 3. Grifo et al., JAMA 2015;314(23):2569-2570 4. Kushnir et al., J Ovarian Res 2018;11(1):2. doi: 10.1186/ s13048-017-0378-4. 5. https://tinyurl.com/2kwwkhfd 6. Patel SS, Carr BR. Semin Reprod Med 2008;26(2):196-2013 7. Siegel-Itzkovich J. BMJ 2000;320(7247):1425
AT THE CHR
BOARD-CERTIFIED RE-I AT ASSOC. PROF/PROFESSOR LEVEL
The CHR is looking for another senior board-certified RE-I (or international equivalent) to join our growing national and international practice. Though private, our center is organized along academic principles in that physicians are expected to excel not only as clinicians but also as researchers. The center’s uniquely structured compensation package, therefore, incentivizes both activities. We are looking for an individual with documented excellence in both areas, commensurate with associate professor/professor level. Besides a competitive salary, incentive bonus structure, and excellent benefit package, the CHR also offers partnership along either a 3-year or 5-year equity track and, ultimately, part or complete ownership, as the current leadership is expected to retire within that time-period.
If you feel qualified for the position and share our philosophy of being a physician-scientist, please let us know by submitting your C.V. and a brief letter of interest to our COO, Ms. J. Tapper, at jtapper@thechr.com The position can be filled immediately. All submissions are considered confidential.
The V oice | j anuary 2023

13
|
ADVERTISEMENT Continued from page 12
hirinG
ADVERTISEMENT
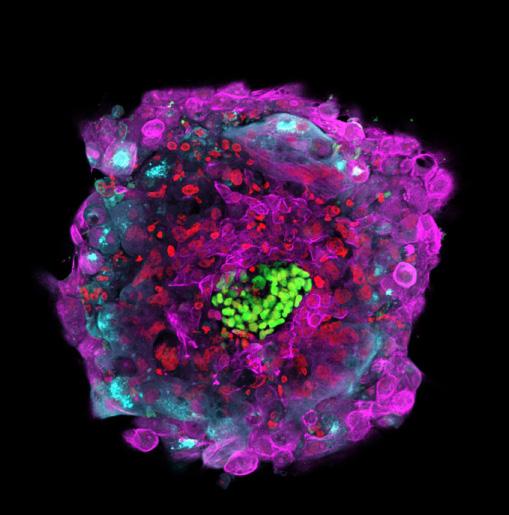
Among the many collaborations the CHR undertakes with worldwide experts studying human development is that with the Brivanlou laboratory at Rockefeller University. This image was taken by scientists in the Brivanlou laboratory who were studying several years ago whether human embryos donated for basic research could develop beyond the typical 3 or 5 days they are cultured before embryo transfer in an IVF cycle. This remarkable image depicts a human embryo after 10 days in culture and shows many different cell types have formed based on the staining patterns. Inner cell mass is shown in yellow, magenta shows one type of placental cell and blue illustrates placental cells responsible for producing the hormone of pregnancy, hCG.
DR. ALBERTINI’S
Image 2
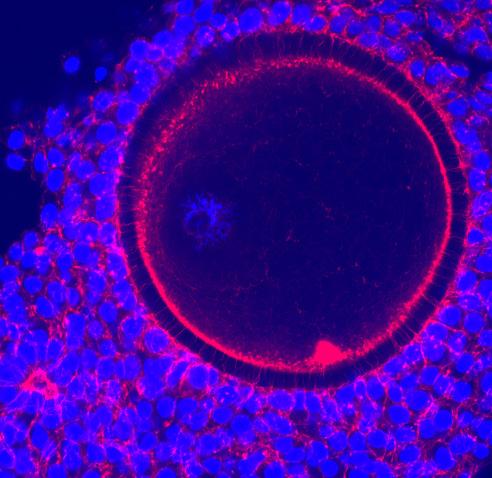
As part of a routine IVF cycle, patients receive notification when it is time for them to take an injection two evenings before egg retrieval will take place. The injection, known as the ovulation trigger, will initiate events in the follicle that prepare the oocyte for its final maturation in preparation for IVF or ICSI. The image here shows what the oocyte and its surrounding cumulus cells look like before the ovulation inducing trigger. The mass of blue shows the cumulus cells that have been nurturing the oocyte during its prolonged journey in the ovarian follicle. The inner red circle denotes the oocyte itself, and looking outwards, one sees a black circle (the zona pellucida) and a second red domain representing the connections between the cumulus cells and the oocyte. Without the support of the cumulus cells the oocyte would not be able to complete its designated mission-to generate a healthy embryo!
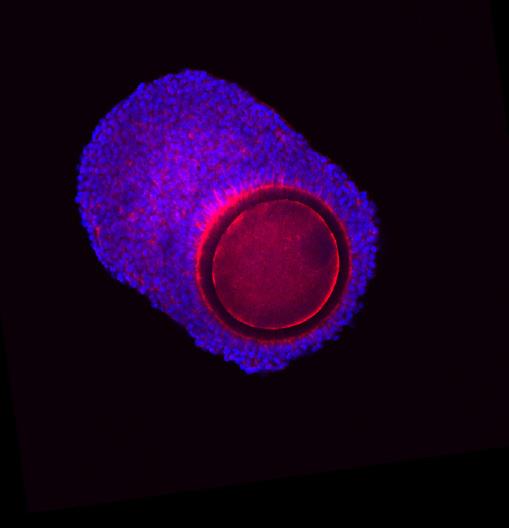
How do the cumulus cells support the livelihood of the oocyte? This is a higher magnification image of the above one where now you can see the many thousands of contacts cumulus cells make with the oocyte surface (note the spots on the oocyte surface in the upper left quadrant). Spanning the zona pellucida (black) are many projections known as transzonal projections (TZPs), a favorite research subject of Professor Albertini throughout his career. His work and that of many others has now made it clear that nutrients and signaling molecules made by the cumulus passage through the TZPs to supply the oocyte at various stages of its development.
The V oice | no V ember 2022 | 19
Photo Gallery
Image
3
Image
14 | january 2023 | The Voice
1
MY A OF
PIECE MIND
 By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist
By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist

The CHR, New York, N.Y.
That The CHR for a very long time has been sincerely concerned about how patients receive their medical advice (and not only in fertility practice) should by now, be very obvious to every reader of The VOICE. Elsewhere in this issue, the newsletter, for example, points out how misinformed infertility patients often are when it comes to choosing between fresh and already cryopreserved third-party donor eggs. In earlier issues, we addressed widely distributed misinformation about major aspects of current routine infertility practice, from routine extended blastocyst-stage culture to universal elective single embryo transfer, autologous versus third-party donor eggs after ages 42-43 years, and – who can forget – the continuously increasing utilization of preimplantation genetic testing for aneuploidy (PGT-A), despite overwhelming evidence that it does not improve IVF outcomes and for many patients reduces pregnancy and live birth chances.

Continued on page 16
The V oice | january 2023 | 15
Looking only for the upside - how patient advice becomes biased
My personal interest in how patients are “informed” (or should we say “misinformed”) arose early in my academic career, years before the first IVF birth, when my principal academic research interests were still primarily reproductive immunology and medical problems in pregnancy. Reproductive immunology was then already a very controversial subject and mostly represented by two equally extreme opposing camps, - on the one side, a newly arising subspecialty of reproductive immunology believing that the science of immunology would cure everything from miscarriages to cancer. And on the other side of the debate – unchanged till today – the nay-sayers who simply rejected the notion that pregnancy must be primarily an immunologically-mediated state because, otherwise, the fetal semi-allograft of pregnancy would have to be rejected by a seemingly normally functioning maternal immune system. Similarly, the late 1970s were the time when Cesarean section rates started to explode, yet another development that has not abated since then, even though, as a young academician at Mount Sinai in New York City, I simply could not detect real scientific reasoning for these rapidly increasing rates.
What I, indeed, found most surprising was the fact that much of the pressure for the performance of Cesarean sections came from patients. In trying to understand this phenomenon better, it took me not very long to understand what was to a large degree driving this patient desire, - information patients received from their obstetricians. I still remember the very prominent private attending who had a cesarean section rate of over 90%, more often than not, citing as an indication for his Cesarean sections “the patient’s desire.” It then quickly dawned on me that patient desires very often only really reflected their physicians’ desires. From this point on, it didn’t take a genius to understand the
consequences: those who provide patients with information establish the frameworks that then determines the patients’ viewpoints. Who provides patients with informed consent, even if informally, therefore, matters. Since there is not a single physician in the world who is not at least to a degree biased in her/his opinions (this writer included), we must acknowledge our influence on how our patients reach their decisions. “Groupthink” among physicians, a subject I recently discussed in this column, then, of course, also very quickly permeates into social media, creating a second “contaminated” source for the lay public.

Recruited in 1981 as department chair at Mount Sinai Hospital and professor at Rush Medical College in Chicago, the opportunity presented itself to turn what I had learned into practice by attempting to reduce the Cesarean section rate at my new department. Like most hospitals at the time, it had seen year after year higher Cesarean section rates. By introducing a second-opinion mandate, offered by specially trained obstetricians on how to “inform” patients about their options before non-emergency Cesarean sections, the department, literally overnight, significantly reduced its Cesarean section rate. The decline was so remarkable that the prestigious New England Journal of Medicine accepted our report for publication.1
Analyzing how the newly required second opinion achieved the desired goals of reducing the department’s Cesarean sections we, moreover, learned interesting additional details about how obstetricians in the department had prepared their patients for the possibility of a Cesarean section
“By introducing a second-opinion mandate, offered by specially trained obstetricians on how to ‘inform’ patients about their options before non-emergency Cesarean sections, the department, literally overnight, significantly reduced its Cesarean section rate.”
Continued on page 17 16 | january 2023 | The Voice
Continued from page 15
delivery: They did not necessarily mislead their patients about the possible indications for a Cesarean section; unconsciously or consciously. Patients were, however, only informed about the upsides of surgery (less labor pain, quicker delivery, better outcomes for babies, etc.), while information about potential downsides (longer hospital stay and recovery, potential post-operative sequelae, increased infertility, greater cost, etc.) were often withheld. This is where the mandated second opinion came into play because physicians who were authorized to offer these second opinions had been trained to do both.
This experience at young stages in my career has stayed with me ever since: How we inform patients about their treatment choices greatly matters, and the information patients to these days frequently receive from their physicians has, unfortunately, often remained biased by a primary emphasis on only the benefits of interventions, without concomitantly also advising patients on potential downsides, including adverse outcomes. Such biases are, of course, seriously destructive for appropriate decision-making processes of the patient, whether they affect relatively minor decisions, like medication choices or whether to undergo certain tests, or whether it involves major national policy decision like the governments had to make during the early days of the COVID-19 pandemic. I have noted in these pages before that for the first three months of the pandemic all we heard from government spokespersons was how important distancing was, why businesses and schools must be closed, and about other restrictions to normal life, which, since, have mostly been found to have been useless; not once did I, however, during those first three months of the pandemic hear a government spokespersons address the potential downsides of all of these recommended and/or mandated interventions. Today we know better, with China just learning the hard way how wrong it is to look only at potential benefits from interventions while ignoring their potential pitfalls.
In daily medical practice, we are all guilty in our interaction with patients of exactly these kinds of biases. We, however, also must acknowledge that the same biases also often dominate the discourse among physicians and, therefore, affect the establishment of standards of care; and that, of course, applies to the infertility field as much as to other specialty areas. The British Medical Journal, in my opinion for many years the most daring and intellectually honest major general medical journal in the world, just published under the title, “Global health nonsense,” a fascinating opinion piece by Norwegian and British scientists,2 in which they define “nonsense” as, “global health discourse that either underperforms or misinforms its audience.” They further argue (in my opinion absolutely correctly) that, “such nonsense is widespread, and (actually) jeopardizes improvement in global
health governance.” This paper in my opinion is a must-read because it, better than anything I have read in a long time, explains what increasingly pains current medical practice.
It would exceed the purpose of this column to go here into further detail regarding this extraordinary piece of writing; but for those who are interested in more detail, it is further discussed in this month’s newsletter in the literature review section.
There are, of course, many different reasons for all that “nonsense” that current-day medicine manifests. Pretending to be “good-doers” without considering the negative consequences of one’s actions these days, indeed, does not only appear restricted to medicine. It, in principle, is not different from Bankman-Fried’s benevolent capitalism that led millions to lose their investments, and, in many ways, unfortunately, appears to represent a sign of our times. It is, however, one thing when politicians or criminals falsely pretend “to do good” without really caring about adverse consequences. We physicians and scientists should know better and not fall into the trap of promoting “nonsense” to our patients!

REFERENCES
1. Myers SA, Gleicher N, N Engl J Med 1988;319(23):1511-1516
2. Stein et al., BMJ 2022;379:02932
ADVERTISEMENT
Continued from page 16 The V oice | january 2023 | 17
Learn more by accessing our library of educational videos: https://www.centerforhumanreprod.com/contents/video-gallery Center for Human Reproduction

EMBRYOLOGY LABORATORY SUPERVISOR FOR RESEARCH

The CHR is searching for a candidate for the newly created position of Embryology Laboratory Supervisor for Research. The CHR’s embryology laboratory, under a single laboratory director, is in the process of being reorganized into three distinct areas with separate supervisory responsibilities: (i) clinical, (ii) administrative, and (III) research.

Supervisors in all three areas must hold PhD degrees (or equivalent) and be fully trained human embryologists with sufficient historical professional experience to hold a supervisory position.
While such human embryology experience is preferred for this new position as well, priority qualifications are a record of excellence in reproductive biology research, documented by publications in prestigious peer-reviewed journals and, in absence of human IVF experience, at least substantial animal IVF experience allowing for relatively quick in-house training in human IVF.
Besides a competitive salary and benefit package, the CHR also offers in this position a unique financial incentive-structure linked to the success of the center’s research activities, as demonstrated by publications in prestigious peer-reviewed journal. Moreover, this position will also be eligible for the opportunity to earn shared ownership in research-driven new start-up companies and the center itself.
If you feel that you qualify for this position, please submit your CV and a brief application letter to the CHR’s COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available immediately. All submissions are considered confidential.
hirinG
ADVERTISEMENT
AT THE CHR
18 | january 2023 | The Voice
QUESTIONS PATIENTSASK
If the plan is a new baby in the new year, how should we prepare?

The answer to this question is, that depends: If you are still at young reproductive age (female under age 38), have no reason to believe that, as a couple, you may have a fertility problem, and if you have no medical problems, then there is not much preparation needed. If you are a little overweight, take the opportunity to lose a few pounds; if you are out of shape after the holidays, it may be a good idea to renew the gym membership. The better shape you are in overall when attempting pregnancy, the better will be the chances of a quick and healthy pregnancy. Diet, of course, matters, and The CHR usually recommends a balanced diet and staying away from any of the fad-of-the-moment diets. As recent studies again confirmed,1,2 a Mediterranean-like diet is, likely, the healthiest diet for mother as well as offspring., even though Mediterranean countries, paradoxically, appear to be switching away from such a diet.3
The answer, however, changes if you are older, have medical problems, or are aware of potential infertility problems. If any of these circumstances apply, we recommend that you make an appointment at a fertility center. The general rule is that unprotected regular intercourse for one year without conception should be considered a likely sign of an infertility problem. If the woman is over 38 years old, the recommendation is that a fertility expert should be consulted already after six months of failed intercourse.
Also, remember that having a baby is a quite frequent resolution in a new year. In January and February fertility centers, therefore, are often heavily booked, and waiting times for an appointment may be considerable.

REFERENCES
1. Flor-Alemany et al., Matern Child Nutr 2022;;e13454
2. Miller et al., BMC Pregnancy Childbirt 2021;21(1):558
3. Obeid et alEur J Nutr 2022;61(7):3327-3344
The drug Berberine for polycystic ovary syndrome (PCOS)?
With PCOS being a very frequent cause of female infertility, its prominence on the Internet cannot surprise. Unfortunately, PCOS is also one of the worst-understood and, therefore, only a very poorly investigated condition in reproductive medicine, and published studies
Continued on page 20 The V oice | january 2023 | 19
claiming to address this condition, therefore, have to be viewed with caution. This also applies to treatment recommendation, with the medication attracting recently the most attention no longer being Metformin or Myoinositol, both medications, which in the past have dominated the PCOS chat, but a drug called Berberine. It is an isoquinoline-derivative alkaloid herb extract, which is alleged to improve insulin sensitivity and, like Myoinositol, reduces hyperandrogenism (high male hormone levels).
And this is where one of the main problems lies with this drug; PCOS is a syndrome, under current international consensus still made up of four so-called phenotypes: A, B, C, and D. PCOS, therefore, is not one disease but a hodgepodge of four separate conditions or, as the CHR’s investigators recently suggested, really two distinctively different conditions, one made up of phenotypes A, B, and C, and the other representing phenotype D.1 All PCOS patients at young ages after menarche are considered o be hyperandrogenic (demonstrating high male hormones). Phenotypes A, B, and C maintain high androgens into advanced age. Phenotype D, however, differs and experiences, starting approximately at age 25, declining androgen levels. They, however, for ca. 10 years remain in the normal range and by approximately age 35 drop below the normal range into the hypo-androgenic range. This decline in androgen levels is due to insufficiency of adrenal androgen production in these women, with ca. half of a female’s androgens coming from adrenals and ovaries, respectively. Ovaries, however, require good androgen levels in order to make good eggs. Consequently, phenotype D PCOS patients with low androgens produce poor egg numbers and poor egg quality and, indeed, therefore require androgen supplementation after age 35.1
Most PCOS studies in the literature, however, do not differentiate between phenotypes and include all four phenotypes
in studies. This means that most patients (phenotypes A, B, and C, all hyperandrogenic), indeed, may benefit from drugs that lower androgen levels, like Myoinositol and, yes, Berberine. But if these medications are given to phenotype D PCOS patients after age 35 who already have low androgen levels, they will make things even worse. The CHR, therefore, strongly recommends against the use of either Myoinositol or the newly fashionable drug, Berberine, in PCOS patients, unless they have been, indeed, found to be phenotype A, B, or C patients with high androgen levels. Since most PCOS studies, however, do not differentiate between phenotypes of PCOS, these studies must be viewed with caution. This, of course, also includes the most recent study supporting the use of Berberine over Metformin and Myoinositol.2 Unfortunately most colleagues do not even test androgen levels in their PCOS patients and, therefore, don’t even know which PCOS phenotypes they represent.
REFERENCES
1. Gleicher et al., Biomedicine 2022;10:1505
2. Mishra et al., Cureus 2022;14(1): e21781
Is artificial intelligence (AI) really on the verge of revolutionizing IVF?




This time it is not only the Internet that appears obsessed with AI revolutionizing IVF but also our medical literature. One cannot open a medical journal in the field without finding glowing testimonials about how AI will revolutionize the practice of IVF.1-4 While we, of course, hope that all of these prophets are correct in their predictions, we must admit we are skeptical.
AI undoubtfully will revolutionize the world and will have an enormous impact on medical care. We, however, doubt that AI will have a significant impact when it is applied to find differences where no significant differences exist. Indeed, it does not take a data expert to understand that all the AI in the world cannot detect what does not exist. And here is what we mean by that: Innumerable companies have been founded and have been successful in raising funds with the promise of finally achieving through AI what in over 40 years the field has been unable to achieve successfully: embryo selection, - i.e., the best embryo from among an embryo cohort generated in a single IVF cycle. If beyond basic embryology assessments, embryo selection was a viable proposition, why has time-lapse failed in improving embryo selection or why has PGT-A proven to be ineffective in doing so? Or is it realistic to assume that AI will select spermatozoa for fertilization with enough superior efficiency over an experienced embryologist to warrant the expense? We don’t think so!
As long as promises are made and investors are willing to risk capital in supporting research, we, of course, have no problem with attempting to develop AI that sometimes in the future may or may not beneficially affect IVF outcomes. This is, of course, one of those circumstances where nothing would please us more than having been wrong in our assessment of AI in association with IVF. The field of IVF has stagnated for over 20 years and needs help. We, however, are skeptical that it will come from
Continued from page 19 20 | january 2023 | The Voice Continued on page 21
AI and, if it does, it will not be through embryo or spermatozoa selection but through the analysis of huge data sets to define with better accuracy patients’ pregnancy and live birth chances in advance.
What we, however, are concerned about are, once again, companies that already sell AI products to IVF clinics and patients that have not been sufficiently validated. The introduction of unvalidated practices in IVF has been the subject of many articles in The VOICE. This is, however, the first time that we address the premature introduction of AI “add-ons” to clinical practice. One company, FutureFertility (Toronto, ON, Canada), for example, in an AI product already sold to IVF clinics under the name VIOLET™, claims to be able to quantitate oocyte quality by determining oocytes that support the development of embryos to blastocyst-stage.5 The product is sold in support of selecting oocytes for cryopreservation. A parallel product, called MAGENTA™, is advertised as “evaluating and scoring oocyte quality to help inform decision-making, assess cycle outcomes, and plan for future cycles.” We wonder how well this AI system would do in comparison to the oocyte assessment CHR investigators recently reported in two published papers.6,7 FutureFertility, moreover, “drives impact for clinics” that purchased its AI products (per their website 4) with marketing efforts directly to patients.

As the company’s website notes. its claims are based “on two validation studies,” both only presented in oral presentations at scientific meetings.8,9 They, therefore, have not passed peer review for a published paper. One wonders why?
The insufficient validation of commercial tests in IVF has in recent years become a serious quality problem and, as we also repeatedly have pointed out in these pages, likely carries significant responsibility for declining IVF live birth rates worldwide,10 while adding unnecessary cost to an already often unaffordable IVF cycle. Another test that “conquered” the IVF field worldwide despite insufficient validation and, indeed, despite several reports invalidating its results, was
hopefully finally buried after a well-performed prospectively randomized study failed to support its claims.11 This study is further discussed in the literature review section of this newsletter.
REFERENCES
1. Diakiw et al. hum Reprod 2022;37(8):1746-1759
2. Sfakianoudis et al. Biomedicines 202210(3):697
3. Curchoe CL. J Assist Reprod Genet 2022;39(7):1493-1496
4. Chow et al., Reprod Fertil 2021;2(3):C29-C34 5. https://futurefertility.redox-dev.com/violet/
6. Hu et al., Fertil Steril 2021;116(2):431-443
7. Hu et al., Fertil Steril 2021;116(5)1330-1340
8. Nayot D., Meriano J., Casper R., Krivoi A. An oocyte assessment tool using machine learning; Predicting blastocyst development based on a single image of an oocyte. Oral Presentation - 36th Annual Meeting of ESHRECopenhagen 2020.
9. Campbell A., Nayot D., Krivoi A., Barrie A., Jordan K. et al. Independent a ssessment of an artificial intelligence-based image analysis tool to predict fer tilization and blastocyst utilization potential of oocytes, and comparison with ten expert embryologists. Oral Presentation - Fertility Online 2021 Conference; British Society.
10. Gleicher et al., Hum Reprod Open 2019(3):hoz017
11. Doyle et al., JAMA 2022;328(21):2117-2125
hirinG
AT THE CHR
EMBRYOLOGY LABORATORY
SUPERVISOR FOR RESEARCH
The CHR is searching for a candidate for the newly created position of Embryology Laboratory Supervisor for Research. The CHR’s embryology laboratory, under a single laboratory director, is in the process of being reorganized into three distinct areas with separate supervisory responsibilities: (i) clinical, (ii) administrative, and (III) research.
Supervisors in all three areas must hold PhD degrees (or equivalent) and be fully trained human embryologists with sufficient historical professional experience to hold a supervisory position.


While such human embryology experience is preferred for this new position as well, priority qualifications are a record of excellence in reproductive biology research, documented by publications in prestigious peer-reviewed journals and, in absence of human IVF experience, at least substantial animal IVF experience allowing for relatively quick in-house training in human IVF.
Besides a competitive salary and benefit package, the CHR also offers in this position a unique financial incentive-structure linked to the success of the center’s research activities, as demonstrated by publications in prestigious peer-reviewed journal. Moreover, this position will also be eligible for the opportunity to earn shared ownership in research-driven new start-up companies and the center itself.
If you feel that you qualify for this position, please submit your CV and a brief application letter to the CHR’s COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available immediately.
All submissions are considered confidential.
Continued from page 20 The V oice | january 2023 | 21
ADVERTISEMENT
CHR Publications
Barad DH, MD. REFLECTION:
Preimplantation
euploidies screening is not diagnostic.
Fertil Steril Rep 2022;3(4):294
In this invited editorial, The CHR’s Clinical Director of IVF, Director of Research, and Senior Scientist, David Barad, MD, addressed a case report published by colleagues from the University of Rochester Medical Center in Upstate New York in which they reported a healthy live birth after transfer of a so-called “chaotic” embryo. What PGT-A laboratories define as “chaotic” unfortunately greatly varies and can go from 2 chromosomal abnormalities up to 6 or more aneuploidies in a single embryo. As the authors note in their paper, IGENOMIX, a leading national PGT-A laboratory located in Florida, recently circulated a mailing among IVF centers warning from automatically discarding “chaotic” embryos because their studies discovered that embryos, they found on testing to be “chaotic,” in ca. 40% upon re-biopsy were found to be “euploid-normal.” The company, therefore, recommended a re-biopsy of all “chaotic” embryos and transfer if the re-biopsy is “normal-euploid.”
This recommendation, however, very obviously
does not make any sense because why should a second biopsy be more accurate than a first one? Moreover, a second biopsy requires thawing, repeat biopsy, and re-freezing, - certainly not improving an embryo’s pregnancy chances. Finally, all of this, of course, adds costs and time. Barad made all of these points and many more in his commentary, basically explaining to the reader why this highly unusual case report only adds further credence to the CHR’s position on PGT-A which for many years has described PGT-A as a useless test which, however, in addition, for many women can actually reduce pregnancy and live birth chances, especially if embryos with good pregnancy potential are either not used or even disposed of.
REFERENCE
1. Lin et al., Fertil Steril Rep 2022;3(4):301-304
CHR CHR
CHR CHR CHR CHR CHR CHR
CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR
22 | january 2023 | The Voice
genetic testing for an
the chr’s interpretation of RECENT LITERATURE, relevant to REPRODUCTIVE MEDICINE
Mostly placed into a clinical context, we in this section of the newsletter offer a survey of articles in the English literature, usually published in the preceding month, which the CHR found of interest to the current practice of clinical reproductive endocrinology and infertility, - even if at times not immediately applicable to daily clinical practice. These articles, however, nevertheless often point out where clinical practice will likely go and, therefore, serve an important translational purpose. Translational research has been the CHR’s principal research goal since its founding in 1981, has produced a significant number of U.S. patents over the years, and has propelled the CHR into its current position as a worldwide center of last resort for infertile patients who have failed treatments elsewhere.
General medical importance
nonsense”
A recent opinion paper in The British Medical Journal (BMJ), interestingly authored by two Norwegian environmentalist and a British anthropologist, likely represent the most authentic and comprehensive criticism of current global health care in many years. They in the process also added a succinct new term to the medical literature, - “health nonsense,” which perfectly describes many of the often-absurd practice patterns that, paradoxically, have evolved in medicine during a time when the practice of “evidence-based medicine” has become something of a holy grail in how organized medicine perceives itself.
There is no better way to summarize the authors’ argument but to cite them verbatim in their three key messages: (i) Spin, hyperbole, meaningless buzzwords, and technocratic jargon have become increasingly common in global health discourse. They are part of a broader
phenomenon labeled “global health nonsense.” (ii) Three main forms of global health nonsense are obfuscation, misrepresentation, and omission of relevant information. (iii) Global health nonsense must be called out because it stifles collective efforts to understand, critically assess, and improve global health governance.
We, here at The CHR, of course, could not agree more, and readers of The VOICE, of course, know this already for a long time from the many diverging opinions The CHR espouses in contrast to what must be viewed as generally advocated practice in routine infertility care, whether it is routine extended embryo culture to blastocyst, elective single embryo transfer, of course, preimplantation genetic testing for aneuploidy (PGT-A), and many other practices. Because in the CHR’s opinion, we simply do not understand how many of these practice patterns can still be defended considering current literature evidence, we also love the term “health nonsense” to describe them.
The above-noted three key messages, of course, only represent summaries. The authors in their manuscript offer much more
A genius new term in medicine, - “health
Continued on page 24 The V oice | january 2023 | 23
detail, and we, therefore, consider their paper an absolute must-read for everybody interested in improving how we currently practice medicine and, of course, not only in reproductive medicine.
REFERENCE
1. Stein et al., BMJ 2022;379:02932
About journal editors
The importance of journal editors in the practice of medicine is enormous and, therefore, has also been the subject of repeated discussion in these pages. They, of course, are the individuals who ultimately not only decide which articles are and are not published but also, with help of the expert reviewers, choose how a manuscript must be modified before publication. The latter is clearly the more complex responsibility because a paper can have overall value even if it contains shortcomings or even falsehoods, which often are overlooked by editors if not pointed out by reviewers.
Expert reviewers, as we also have repeatedly pointed out in this newsletter before, by definition are biased in their reviews when it comes to the specific subjects in which they are considered experts, favoring how they view the subject and opposing contradictory opinions. As a consequence, they will tend to overlook falsehoods that support their viewpoints but, of course, will be critical of opinions by representatives of the opposition. If editors do not consider this fact in assessing peer reviews before making decisions on a manuscript, they fall short of their responsibility and will bias what is published in their journal toward prevailing opinions, while discriminating against original thoughts. This is a phenomenon that, unfortunately, is very prevalent in medical journals (more so than in basic science journals) and unfortunately also exists in the infertility literature, often contributing to the “health nonsense” addressed in the preceding paper here discussed.
As also repeatedly noted before in these pages, medical journal editors these days are often overburdened by an onslaught of submissions and, especially if not full-time editors (as most still are), simply do not have the time to give detailed attention to every paper. Consequently, they become more dependent on the opinions of peer reviewers, and the vicious cycle of biased reviews is further enhanced. How limited editors’ abilities are these days to assess submitted papers was recently demonstrated in another interesting article in the same issue of The BMJ by editors of the journal, who were tested in their ability to predict the citation potential of manuscripts submitted to The BMJ. As it is reasonable to assume that citation indices relate
to the importance of a paper, the editors tested their ability to predict the importance of a paper. One also must acknowledge that, because this assessment was done under study conditions, they, likely, reviewed those articles at least as closely as they would review other articles that go through peer review (and, likely even closer).
Yet, to quote their conclusions, “editors weren’t good at estimating citation potential of manuscripts individually or as a group; there is no wisdom of the crowd when I come to BMJ editors.” Considering the importance of the peer-review process for how medicine is practiced, this article, therefore, offers further evidence for the urgent need to find ways to improve the decision-making process of what is and is not published.
REFERENCE
1. Schroter et al., BMJ 2022;379:e073880
Legalities and ethics
Several recent articles of note addressed legal and ethical issues. CHR’s colleague and friend, Eli Y. Adashi, MD, MSc., for decades a leading reproductive endocrinologist and physician-scientist who in more recent years has become one of the country’s most prolific writers for many prominent journals on general medical (and often legal) issues, together with Harvard law professor and frequent co-author, Glenn Cohen, JD, addressed a recently arising important issue for physicians, the criminalization of medical errors. This is, of course, an important issue for every practicing physician but also for nurses and, as the two authors correctly pointed out, ultimately also for patients. The legal analysis of a case involving a nurse accused, and by a jury convicted of criminally negligent homicide and gross neglect of an impaired adult, served as the impetus for the article.
When and whether a medical error, as the authors noted, is appropriately treated as a homicide, is, of course, a difficult question. It is reasonable to assume that the medical system as a whole, not the least because of legal threats, but also because of medicine’s primary ethical responsibility of “not doing harm,“ is in most cases doing its utmost to prevent undue harm to patients. To prevent the reoccurrence of preventable adverse events, such a system requires full transparency in reporting, investigation, and subsequent remedial actions. In absence of such transparency, events will repeat themselves. As has been well demonstrated especially in prevention efforts in the airline industry, threats of excessively severe punishment result in an increasing absence of transparency, mostly because of underreporting of events. Criminalization, as the authors, point out, therefore, does not prevent medical errors and, indeed, may enhance their likelihood.
Continued on page 25 24 | january 2023 | The Voice
If the system fails in this obligation, patients, in contrast to many other legal victims, moreover, have relatively easy access to the court system since a horde of malpractice law firms all over the country are accepting promising cases on a contingency basis. Related, the Physicians Insurance A Company in Seattle, WA, recently announced a criminal defense reimbursement coverage for physicians and hospitals for defense costs arising from criminal allegations from patient care.2
A conviction for any form of homicide, as the authors point out, requires intent. Negligence, in contrast, does not. The legal system must be careful about what it wishes for!
On a different legal subject, Progyny Inc , the largest company in the U.S. selling fertility benefits to employers (NASDAQ: PGNY), according to an announcement by Griffin Jones (Inside Reproductive Health) on December 14, 2022, is being investigated by several national shareholder rights law firms after a December 7, 2022 report by (the anonymous) Jehoshaphat Research under allegations “of deceiving the investor community via its financial reporting practices,” and, “actually being unprofitable but masking this problem with accounting games.” The initial report allegedly was based on information received from a competitor, KINDBODY, a national investor-driven chain of fertility and wellness clinics) which denied having spoken to the research firm and refused to weigh in on the report. Investment banks following Progyny Inc, have so far not issued any reports. Supposedly, at least one law firm is preparing a class action lawsuit (The Rosen Law Firm, New York, N.Y.) and encourages investors in Progyny Inc. to inquire about its securities class action investigation.3 The competition in the infertility industry is apparently increasing and becoming nastier.
A legal, but foremost ethical, issue in medical practice is the question of when and how a physician may refuse treatment because of personal moral, ethical ,and/or religious believes. This is, of course, a subject of increasing controversy not only in medicine, as especially the question of refusing services because of religious beliefs has kept courts busy in recent years, with some cases even reaching the Supreme Court. In reproductive medicine this issue has for decades been, primarily linked to the performance of voluntary abortions, due to the recent Dobbs v. Jackson et al Supreme Court decision that reverted the abortion issue from a federal right into a local state-by-state decision, it, however suddenly again surfaced.
One of the principal functions of the World Medical Association (WMA) is to resolve complex ethical issues for the medical field. This is exactly what a recent meeting in Jakarta, Indonesia did, which was well summarized in a recent editorial in JAMA. Documents like this always are compromises, and this document was no exception. But for everybody worried about this issue, it offers clear guidance.4
REFERENCES
1. Adashi EY, Cohen G. Nat Med 2022;28:2241-2242
2. https://www.prnewswire.com/news-releases/physicians-insurance-introduc es-criminal-defense-reimbursement-coverage-to-medical-professional--hos pital-liability-insurance-policies-301634080.html
3. https://www.globenewswire.com/news-release/2022/12/16/2575781/0/en/ NATIONALLY-RANKED-ROSEN-LAW-FIRM-Encourages-Progyny-IncInvestors-to-Inquire-About-Securities-Class-Action-Investigation-PGNY. html
4. Parsa-Parsi RM. JAMA 2022;328(20:20182021
The nation’s increasing drug problem
It is impossible not to conclude that the nation faces a rapidly increasing drug problem. What, however, is not properly addressed by the media is how multifaceted this problem has become. The abuse of illicit drugs is, of course, nothing new for the U.S., and has been accepted as a national scourge at least since the 1960s (and probably from even earlier on). It, however, in recent years has literally exploded, first through the opioid crisis brought on by the promotion of excessive prescribing of addictive opioids for unwarranted analgesic indications by the pharma industry, large pharmacy chains, and physicians,1 and more recently through the fentanyl crisis, caused by huge amounts of inexpensive fentanyl being illegally brought mostly from Mexico into the U.S. Because of its potency, Anne Milgram, the DEA’s administrator, described this drug as, “the single deadliest drug threat our nation has ever encountered.“ She went on: “Fentanyl is everywhere, from large metropolitan areas to rural America, no community is safe from this poison. We must take every opportunity to spread the word to prevent fentanyl-related overdose death and poisonings from claiming scores of American lives every day.”2
Among pregnant and postpartum women drug overdose mortality increased by approximately 81% between 2027 and 2020.3 Considering the increased influx of fentanyl over especially the last three years, it is easy to imagine how much further mortalities increased since then. A recent study further confirmed the obvious: If more mothers abuse drugs, more of their offspring will show neonatal effects.4
Yet, at the same time, more and more states are paradoxically legalizing “pot” (marihuana) and it is just a matter of probably months until the federal government will legalize “pot” in the whole country, even though today’s “pot” is significantly more potent than it was only a decade ago and, because of its increased potency, has become addictive. A recent study of pregnant women in the U.S. not only confirmed increased use of cannabis while pregnant but demonstrated that a quarter of users qualified for the psychiatric diagnosis of cannabis use disorder and, therefore, for substance abuse treatment.5 Similar to offspring after maternal opiate abuse, a recent study by the Canadian National Cannabis Working Group recently reported that newborns of cannabis users in pregnancy had almost identical neonatal consequences: preterm birth, low birth weight, small-for-gestational age, and major congenital abnormalities. Moreover, female infants demonstrated increased susceptibility,6 and accumulation in fetuses during pregnancy and in neonates who breast-feed is now an established fact.7
In a recent article in The New York Times the writer Maia Szalavitz under the title, “It’s not just pot. Our entire drug policy needs a rewrite,” addressed some of the contradictions and warned that just changing marihuana policies is not sufficient since, for example, psychedelics are already presenting similar regulatory issues.8 We recommend this article. How far we have come in this country in missing the boat when it comes to addiction is also well demonstrated by the anticipated approval of over-the-counter naloxone dispersion by the FDA.9
REFERENCES
1. https://www.cdc.gov/drugoverdose/epidemic/index.html
Continued from page 24 The V oice | january 2023 | 25
2. https://www.dea.gov/fentanylawareness
3. Bruzelius E, Martins SS. JAMA 2022;328(21)2159-2161
4. Umer et al. J Pediat 2022;S0022-3476(22)01114-3
5. Wicken et al., AJOG Glob Rep 2022;2(4):00095
6. Luke et al., PLoS One 2022;17(11):e0276824
7. Monfort et al., Front Pharmacol 2022;13:919630
8. https://www.nytimes.com/2022/12/11/opinion/marijuana-drugs-us-pol icy.html
9. https://www.fda.gov/news-events/press-announcements/fda-announc es-preliminary-assessment-certain-naloxone-products-have-poten tial-be-safe-and-effective
Pregnancy
Effects of
vs.
transfer on obstetric and neonatal outcomes
Under the hypothesis that everything beyond singleton deliveries, represents adverse and, therefore, undesired IVF cycle outcomes, initiated in the Scandinavian countries, the aggressive pursuit of elective single embryo transfer (eSET) for almost all IVF cycles has, now for many years, become a major theme of the worldwide IVF field. Embraced by most major professional organizations in the field, including ASRM and ESHRE, as well as perinatology and neonatology societies, their main argument for considering twins and higher multiples adverse IVF outcomes have been alleged increased outcome risks for mothers and, especially, neonates. To prevent these increased risks, as we have repeatedly discussed in these pages before, a consensus arose that the only way to prevent all multiple pregnancies was through mandated eSET for almost everybody.
The CHR does not share this opinion and has documented the reasons over many years in multiple publications, the last only relatively recently.1-3 This means that we agree that triplets and higher multiples must be avoided. We, however, strongly disagree that twin pregnancies must also be avoided.
Our opposition has, in principle been based on the following arguments: (i) We have for years claimed that data demonstrating clinically significantly increased outcome risks for mothers and offspring were based on incorrect statistical methodologies in studies used to support an eSET policy (for detail, we refer to above cited references). Assuming that such risks do not exist, what would then be the purpose of such a policy? (ii) It is indisputable that eSET reduces pregnancy chances in comparison to a double-embryo transfer (2-ET). It, indeed, takes an eSET plus at least one frozen-thawed cycle to pull even. If there are no outcome improvements from eSET when it comes to outcome risks, what is then the compensatory benefit from eSET for lower pregnancy and live birth chances? (iii) Patients have an almost absolute right to self-determination and studies have clearly demonstrated that many women/couples are desirous of twins, even if fully aware of (often exaggerated) alleged outcome risks. Moreover, this desire is associated with increasing maternal age and length of infertility, all supportive of the argument that a desire for twin pregnancies is often very rational.
Now come once again Scandinavian colleagues (from Sweden), publishing an important paper in JAMA Pediatrics, in which they in a large Swedish patient population, investigated obstetric and perinatal outcomes of single births following either eSET or 2ET.4 Though the study reveals interesting observations, the conclusions are, unfortunately, once again partially flawed because of statistical biases that were not considered.
The authors concluded that 2ET cycles were associated with a higher risk of adverse outcomes in singleton pregnancies than eSETs, with these adverse outcomes mostly observed in 2ETs after frozen-thawed cycles at blastocyst-stage. More specifically, neonatal death after 2ETs were allegedly statistically higher and in frozen-thawed cycles 2ETs 2ETs were also associated with higher risk for low birth weight and, after blastocyst transfer, with very preterm births and low birth weight.
Though the study, of course, demonstrates all these supposedly statistically significant findings, the data for several reasons make no sense: First, the study was retrospective, which means there, likely, were good reasons why some patients had eSETs and other 2SETS, a fact very likely strongly biasing outcome. Also, frozen, and/or blastocyst-stage transfers have historically not been associated with low but with high birth weight.5
At the same time the authors, however, deserve considerable credit for the final paragraph of their paper which we, therefore, here quote in full: “Although neonatal death is a serious detrimental outcome, the absolute risk after 2ET is still very low, especially in relation to the general risk of assisted reproductive technology and twin pregnancies (we, of course, disagree with the latter point). We conclude that, although the results support the use of eSET, the observed higher risk after 2ET should not, in itself, deter from use of 2ET in women who are older or have otherwise low reproductive potential. “
We, of course, fully agree with the last sentence because it is fully applicable to the whole eSET vs. 2ET debate, thereby reaffirming the longstanding position of The CHR on this highly controversial subject. That this conclusion is coming out of Sweden, where much of the eSET hypothesis originated, is doubly satisfying, pointing out the sincerity of Swedish colleagues in tackling this very complex issue.
REFERENCES
1. Gleicher et al., BJOG 017;124(5):755
2. Meldrum et al., Fertil Steril 2018;109(2):223-229
3. Gleicher N, Orvieto R. Reprod Biomed Online 2022;44(1):1-4
4. Rodriguez-Wallberg et al., JAMA Pediatr 2022;doi:10.1001/jamapedi atriccs.2022.4787. Online ahead of print.
5. Trobo et al., Reprod Sci 2022., doi: 1007/s43032-022-01075-x
Medical problems in pregnancy
Chronic maternal inflammatory bowel disease has been for years known to affect pregnancy outcomes. Whether those risks vary depending on histological activity of the disease was, however, unknown, and was subject of a recently published study.1 The study suggested that inflammatory bowel disease, and especially ulcerative colitis, were, indeed, risk factors for preterm births which does not surprise since hyperactivity of the maternal immune system, and especially autoimmune conditions, have in general been associated with premature labor and delivery for many years.2
single-
double-embryo
Continued on page 27 26 | january 2023 | The Voice
Complete congenital fetal heart block is associated with anti-Ro/La (SSA/SSB) antibody-positive pregnancies, easily diagnosed by fetal echocardiography. A new study just reported at ACR Convergence 2022 now, however, reported that a timely diagnosis is often missed because echocardiograms in pregnancy are often not performed in timely fashion.2 This study, therefore, basically suggests that obstetricians do not pay enough attention to the known association between autoimmunity (in presence of these autoantibodies), especially in association with systemic lupus erythematosus (SLE), and risk for congenital fetal heart block. Recognizing this risk in timely fashion is important for prevention which rheumatologists are attempting through the treatment of mothers with Plaquenil, an anti-malarial anti-inflammatory drug, and/or intravenous immunoglobulin.
Related, SLE in pregnancy is, of course, associated with significantly increased risks for several pregnancy complications. Now investigators from several U.S. universities reported a large study indicating that cardiovascular complications go far beyond only congenital fetal heart block and include many maternal complications like preeclampsia, peripartum cardiomyopathy, heart failure, various arrhythmias, acute kidney injury, stroke, and venous thromboembolism. 4 While by no means a surprising finding, this is, likely, the most comprehensive ever published study addressing this issue.
Also, regarding preeclampsia, the Society for Maternal-Fetal Medicine (SMFM) just published a “special report” on this still only poorly understood condition.5 Disappointingly, the document once again documents how little progress has been made in better understanding the underlying pathophysiology. In the CHR’s opinion, one of the main reasons has been the unwillingness of the perinatology community to recognize preeclampsia as, primarily, an immunological condition reflective of inadequate tolerance levels of the maternal immune system toward the fetal semi-allograft, a position advocated by the CHR for decades.6,7
Also related to immune responses, a recent study in Nature
Communication by Dutch and British investigators reported that whether an infant is delivered vaginally or by Cesarean section matters for the neonate’s immune system:8 Infants delivered vaginally demonstrated significant better immune responses to immunizations after birth than infants born by Cesarean section. Further assessments
of the newborns’ microbiota suggested that mode of delivery affects the newborn’s microbiota which, in turn, likely affects its immune system. Interestingly, CHR’s Medical Director and Chief Scientist, already in 2006 in women with autoimmune diseases in pregnancy pointed out the possibility that mode of delivery may influence the immune system of the newborn.9
We have in these pages repeatedly pointed out that COVID-19 in pregnancy is a much more sever disease than in nonpregnant females. Now a study in Cell Reports Medicines offers a potential explanation by demonstrating, by utilizing human expanded potential stem cells (hEPSCs), susceptibility of ACE2+ early syncytial-trophoblasts to SARS-CoV-2 virus variants by blocking syncytiotrophoblast maturation which can be rescued by antivirals.10
Considering how frequently miscarriages occur, a recent study from Australia investigating whether for decades held consensus that another pregnancy should not be attempted before three months following a miscarriage or induced abortion came as a surprise, when it demonstrated no difference in pregnancy outcomes if a subsequent pregnancy was established within three months in comparison to 6-11 months.11 That risk of large for gestational infants was decreased in the earlier pregnancy group and a statistical trend toward more small for gestational births may suggest that a shorter time interval may, however, have a small effect on fetal weight.
A milestone in in-utero treatments of some genetic diseases was recently reported in The New England Journal of Medicine by US investigators when a fetus afflicted by infantile-onset Pompe disease was apparently (at least temporarily) cured by in utero enzyme replacement therapy 12 By 13 months of age, the infant developed completely normal and, hopefully, will continue to develop normally. Infantile-onset Pompe disease is a lysosomal storage disease that usually causes organ damage already in utero. Treatment, therefore, ideally should start in utero.
The American Journal of Obstetrics and Gynecology recently published a challenging systemic review by Italian investigators of studies about pregnancies with confined placental mosaicism, concluding that such pregnancies were associated with increased risk for impaired fetal growth.13 They, therefore, suggested that such pregnancies deserved increased antenatal surveillance. Superficially these conclusions and recommendations make sense; but that assumes that the placental studies correctly identified confined placental mosaicism which is highly unlikely because we now know that confined placental mosaicism for decades has been greatly underestimated.14 Consequently, many presumed control placentas without confined mosaicism must be assumed to still have had such mosaicism, thus invalidating the study and the authors’ conclusions of effects on fetal growth. We have discussed this subject in this newsletter repeatedly and, therefore, will not be repetitive. For those who, however,
Continued from page 26 The V oice | january 2023 | 27
question our assessment of this paper, we strongly recommend that they review the above cited paper by Coorens et al, also frequently previously noted in these pages.
Finally, as several recent studies have pointed out, obstetrical care in the U.S. is not doing well: A first reason is rising preterm birth rates, with the country receiving only a D+ grade from the March of Dimes, nine states even receiving an F-grade, and only one (Vermont) an A-grade. 14 Moreover, maternal mortality is rising as well,15 with 4 in 5 maternal deaths recently judged as preventable.16 A disproportionate number of these adverse outcomes, of course, occur in minority populations and, therefore, are not necessarily the result of inferior medical care but a reflection of social inequalities that require very different solutions.
REFERENCES
1. Mårild et al., EClinMed 2022;53:101722
2. Gleicher N. Clin Rev Allergy Immunol 2010;39(3):194-206
3. https://www.healio.com/news/rheumatology/20221115/most-screenings-forfetal-congenital-heart-block-do-not-occur-by-recommended-time
4. Zahid et al., JAMA Network open 2022;5(11): e2243388
5. SMF, Louis et al., Am J Obstet Gynecol 2022; https://www.smfm.org/ publications
6. Gleicher N. Am J Obstet Gynecol 2007;196(1): 5.e1-7
7. Gleicher et al., J Assist Reprod Genet 2017;34(4):425-430
8. de Koff et al., Nat Commun 2022;13(1):6638
9. Gleicher et al., J Autoimmun 2006;27(3):161-165
10. Ruan et al. Cell Rep Med 2022;3.100849
11. Brhane Muts et al., PLoS Med 2022;17(9): e0275155
12. Cohen et al., N Engl J Med 2022;387(23):2150-2158
13. Spinillo et al. Am J Obstet Gynecol 2022; https://doi. org/10.1016/j.ajog.2022.07.034
14. Howard j. Nov. 15, 2022. https://www.news8000.com/i/usgets-d-grade-for-rising-preterm-birthrates-new-report-finds
15. https://www.commonwealthfund.org/ blog/2022/us-maternal-mortality-cri sis-continues-worsen-internation al-comparison, December 1, 2022
16. Kuehn BM. JAMA 2022;328(19):1893-1897
Reproductive
Endocrinology & Infertility
General aspects
To continue the subject of social inequalities, colleagues from Yale University recently published an interesting study, demonstrating that racial disparities persist in fertility
treatments even in presence of insurance mandates in states.1 More specifically, adjusted odds rations for live births were the same in mandated and non-mandated states for non-Hispanic Blacks , non-Hispanic Asians, and for Hispanics. Though minorities demonstrated no significant differences in relative IVF utilization increases between states with and without mandates, whereas there were substantial differences compared to non-Hispanic white women who over the study period, overall, increased the number of IVF cycles per 10,000 women by more than double (minorities, 23.5/10,000 vs non-Hispanic Whites 56.2/100,000).
Are our IVF patients’ cycle outcomes affected by the quality of their sleep? According to a study by Italian investigators in the prestigious journal Scientific Reports, the answer is a clear YES!2 Though statistically significant differences were found in sleep quality between women who did and did not conceive, the relative low levels of significance and the relatively small study size leave us with some doubts about the reported findings by the authors that poor sleep quality in IVF patients is common and may influence IVF outcomes. It however, cannot hurt to stress to our patients the importance of appropriate rest.
A paper we missed during the summer break that appeared in PLoS One already last August was brought to our attention by a reader of this newsletter who asked what we thought about this publication?
Upon reading the paper, it became obvious why the question arose: The study, simply, did not appear to make sense! Chinese investigators set out to investigate the question whether women with prior ectopic pregnancies were at increased risk for ectopic pregnancies after IVF? Their findings then suggested that women with prior recurrent ectopic pregnancies had a lower risk if ectopic pregnancies in association with IVF than women who had experienced only one prior ectopic. But can that make sense?
The authors suggested that this outcome may be caused by repeated prior surgeries for ectopic pregnancies, preventing tubal pregnancies after IVF. However, that explanation also does not make much sense because ectopic pregnancies after IVF often are cornual. What appears clear is that patients with prior ectopic pregnancies are, as has been known for decades, at significant risk for repeat ectopics; and this risk extends to IVF cycles. That more prior ectopics reduce this risk, is, however, somewhat difficult to believe.
The monthly editorials of David F Albertini, PhD. Editor-in-Chief of JARG, introducing every issue of the journal, are almost always short vignettes very much worthwhile the read, both, for their scientific insights as well as heir literally escapades. The November 2022 issue was no exception and, indeed, deserved special attention, as Albertini
Continued on page 29 28 | january 2023 | The Voice
attempted to address the subject of embryo selection or, as he put it, “why do some human embryos of varying genetic constitution make it to the finish line as healthy euploids, while others fail?”4
The Sunday, December 24, 2022 issue of The New York Times contained an article by Alisha Haridasani Gupta and Dani Blum, ‘Just Part of Life’: Experiences With Egg Freezing, for which they interviewed hundreds of women.5 They noted that many among those women expressed joy and hope, while others communicated crushing disappointment, even finding the experience “illusionary.” We were impressed by the objectivity of the piece and recommend it to everybody who is thinking about freezing their eggs or has family members and/or friends who do. As we have repeatedly noted in The VOICE, the egg-freezing industry, unfortunately, often offers a distorted picture of oocyte cryopreservation to potential customers. This article offers the desired balance.
REFERENCES
1. Correia et al., Am J Obstet Gynecol 2022;S0002-9378(22)02158-5
2. Reschini et al., Sci Rep 2022;12:17477
3. Xue et al., PloS One 2022;17(8):e0272949
4. Albertini DF. J Assist Reprod Genet 2022;39(11):2437-2438
5. https://www.nytimes.com/2022/12/23/well/family/egg-freezing-fertility.
html
The end of receptivity testing as we know it?
Different days across the menstrual cycle demonstrate, as one would expect, varying transcriptomic pictures of gene expression. First in some detail described by Spanish colleagues,1,2 they used this finding to develop a diagnostic test, called endometrial receptivity assay (ERA), which classified endometrial biopsy samples as “pre-receptive,” “early-receptive,” “receptive,”, “late-receptive,” and “post-receptive,”3 with the alleged goal of identifying the maximal 6-hour implantation window in which to perform a patient’s embryo transfer.4
For several reasons, The CHR has been skeptical about this test from the very beginning (and, therefore, never integrated it into its routine patient management, though does offer it at patient request). (i) As repeatedly noted in the pages of The VOICE, the CHR rejects the view of pregnancy as primarily an endocrine condition and, instead, considers especially implantation as primarily an immunologically determined event. As such, a 6-hour “best” implantation window, simply, makes no sense. This was later also supported when a competing company offered an expanded array that included immune genes.5 (ii) Careful review of published data regarding the test furthermore raised serious questions about the reliability of presented data, their interpretation and, as unfortunately is only too often the case with newly introduced tests into IVF practice these days, their clinical validation efforts. (iii) This concern was further strengthened by the fact that critically important papers in support of ERA almost exclusively only appeared in a journal in which one of the authors and, therefore, proponents of the test was editor-in-chief. 1,4,6 (iv) Considering how transcriptomes are expected to change under varying environmental conditions, we could not see the logic how a transcriptome obtained in a preceding cycle could represent with enough accuracy a later cycle. Our mostly empiric concerns quickly were, however, reaffirmed
when studies of ERA by independent investigators rather uniformly were unable to confirm the clinical utility of this test, none of which, interestingly, appeared in above noted journal that had published most of the ERA-favorable papers.7,8 Now, however, a group of U.S. investigators published what, likely, for some time to come will be the definite study on ERA.9 A double-blinded, randomized clinical trial at 30 study sites by the Shady Grove chain of IVF clinics compared receptivity-timed frozen embryo transfers with progesterone adjustments(n=381) with control cycles (n=386) independent of ERA results. Primary outcomes were live births and secondary outcomes were chemical and clinical pregnancy rates. Importantly, all patients in both study arms also underwent PGT-A and had only “euploid” embryos transferred. ERA offered no outcome benefits!
REFERENCES
1. Diaz-Gimeno et al., Fertil Steril 2011;95(1):50-60
2. Horcajadas et al., Hum Reprod Update 2007;13(1):77-86
3. Ruiz-Alonso et al., Biochim Biophys Acta 2012;1822(12):1931-1942
4. Ruiz-Alonso et al., Fertil Steril 2013;100(3):818-824
5. Enciso et al., Hum Reprod 2018;33(2):220-228
6. Diaz-Gimeno et al. Fertil Steril 2017;108(4):703-710.e3
7. Bassil et al., J Assist Reprod Genet 2018;35(7):1301-13-03
8. Cohen et al., Syst Biol Reprod Med 2020;66(6): 347-354
9. Doyle et al., JAMA 2022;328(21):2177-2125
Polycystic ovary syndrome (PCOS) and Endometriosis
We are putting PCOS and endometriosis under a single heading because both subjects have recently generated basically almost no interesting literature, even though they are considered the two most frequent causes of female infertility.
Rather unsurprisingly, therefore, there is really not much new to report regarding PCOS, as over almost 30 years the field appears stuck when it comes to this diagnosis. As often noted in these pages, we consider the Rotterdam classification into four phenotypes (A-D) to represent a major reason for this lack of progress because, on the one hand, we separate PCOS patients into these four phenotypes but, on the other hand, PCOS studies usually throw all PCOS patients into the same study pool, thereby, likely mutually obfuscating differences between subgroups of patients.
We, therefore, have to go with what is available, and within such a framework two recent publications, both reviews, deserve some attention. One is an article by Indian investigators in JARG on etiology, genetics and immunology of PCOS,1 and the other is an update on animal models of PCOS by a Swedish scientist in Endocrinology. 2
Like PCOS, endometriosis, too, appears to be stuck in how we understand and treat the condition (reviewed in this and two preceding issues of The VOICE). We do, however, recommend a recent review by a Scottish and an American colleague in the BMJ, which systematically addresses pathophysiology, diagnosis, and management of endometriosis in well-organized fashion.3 Another review article, this time from Korean colleagues, addresses an aspect of the condition, we have not seen previously reviewed in the literature, - namely the link between endometriosis and adiposity.4 This review was based on the recognition in the literature that lower body mass indices predispose to endometriosis. The authors fail to explain this association which, at
Continued from page 28 The V oice | january 2023 | 29
least superficially, appears counterintuitive since, like endometriosis, obesity, but not low BMI, is inflammatory. They, however, succeed in reemphasizing how little we really know about the pathophysiology of endometriosis.
REFERENCES
1. Siddiqui et al., J Assist Reprod Genet 2022;39:2439-2473
2. Stener-Victorin A. Endocrinol 2022;163:1-11
3. Horne AW, Missmer SA. BMJ 2022;379:e070750
4. Hong J, Yi K-W. Obstet Gynecol Sci 2022;65(3):227-233
Some interesting news about the FMR1 gene
The FMR1 gene has been subject to research at The CHR since approximately 20091 and has since, according to PubMed, been subject of 39 peer-reviewed publication from CHR investigators. The gene attracted our attention because it is one of only a small number of expansive genes, characterized by nucleotide repeats (in this case C-G-G) which in subsequent generations can increase (i.e., “expand”). So, for example, if the FMR1 gene expands to beyond 200 CGG repeats, an individual suffers from the so-called fragile X syndrome, especially in males a devastating condition associated with mental retardation and/or autism. If expansions reach 55-200 CGG repeats, the condition is called a pre-mutation, in women highly associated with primary ovarian insufficiency (POI), also called premature menopause, and in males with a neurodegenerative disease that usually becomes symptomatic at middle-ages, the so-called fragile X neuro-ataxia syndrome.
It was the statistical association with POI, that led CHR’s investigators to suspect an important function of the FMR1 gene on the ovary, which led to the discovery that normal ovarian function was represented by 26-34 CGG repeats, and everything below and above had to be considered “abnormal.” However, while all attention regarding this gene for understandable reasons had been only directed toward larger CGG repeat numbers, CHR’s research for the first time demonstrated that, regarding ovarian function, especially low CGG counts (<26) were closely associated with negative fertility outcomes in women, both spontaneously and during IVF cycles. Why that is, has, however, not been elucidated.
Now come Israeli investigators, including CHR’s longstanding friend and collaborator, Raoul Orvieto, MD, from Tel-Aviv University and report findings that suggest that in women with premutation-range CGG repeats and, therefore, poor ovarian response to stimulation, granulosa cell dysfunction due to Sam68 sequestration may be an underlying cause.2 These data, therefore, shed additional light on the CHR’s now longstanding argument that the FMR1 gene is a key gene in ovarian function that deserves further exploration.
REFERENCES
1. Gleicher et al., Fertil Steril 2009;91(5):100-1706
2. Boustanai et al., J Clin Endocrin Metab 2022;107:3000-3009
Important insights regarding oxidative stress and reproductive function
If there is a supplement in female infertility that has captured the field’s imagination, then it is the administration of antioxidants. Oxidative
stress as a key factor in etiology of infertility was, however, originally established almost 100 years ago with the recognition how important alpha-tocopherol was in male reproduction.1
By now we know about the importance of oxidative stress from earliest stages of development of spermatozoa as well as oocytes, through fertilization and into early embryo stages, and exquisitely summarized in a recent special issue of Reproduction. While we recommend the complete issue for those interested in detail, we definitely recommend the introductory editorial by Robert John Aitken, 2 which exquisitely summarizes how oxidative stress affects reproductive function. One very important clinical point he emphasizes is that imbalance in the redox system in the other direction (i.e., too much antioxidant) may be also harmful, creating a state of “reductive stress,” as harmful as oxidative stress.
So, watch out for too much antioxidant therapy! We are now increasingly seeing women (and men) who are supplementing with multiple antioxidants at high doses concomitantly.
REFERENCES
1. Masson KE., J Exp. Zool 1926;45:159-229
2. Aitken RJ. Reproduction 2022;E5-E8
Ovarian aging
Glycosylation variants of FSH Naturally produced FSH in women is made up of in principle two glycosylation forms, so-called FSH21/18, dominant at young ages, and FSH24, steadily increasing in proportionality with advancing female age. A recently published very interesting mouse study by British and US investigators in Endocrinology now demonstrated how these variants distinctively modulate pre-antral follicle growth and survival by initiating different FSHR signal pathway activations, which likely determines how they exercise different effects on follicle growth and survival. The authors also conclude that these differences may underpin the increasing ovarian resistance to FSH observed during aging, characterized by increase follicle apoptosis and decreased steroidogenic- and folliculogenic-associated gene expression.
The finding, of course, have significant potential translational connotations: Specifically, FSH biosimilars currently used in fertility treatments are mostly made up of fully glycosylated FSH (similar to FSH24). These data, however, suggest that a mix of FSH21/17 and FSH24 may have better effects. Though it is dangerous to extrapolate mouse data automatically to the human experience, the idea of commercial gonadotropin products that differ in their glycosylation patterns from currently available medications is not new and has been previously discussed in this newsletter. The original gonadotropins used for ovarian stimulation were extracted from menopausal urines mostly produced by nuns and, therefore, were mostly FSH24-like. Later biosimilars, therefore, unsurprisingly were similar in glycosylation patterns to these menopausal gonadotropins. Why Pharma has not picked up yet on the idea of producing “younger” gonadotropin medications is, indeed, surprising.
Continued on page 31 30 | january 2023 | The Voice
Early menopause and early aging
We also want to point out a recent paper by Joop S.E. Laven, MD from The Netherlands who, in RBM Online under the somewhat confusing heading “countercurrent” in this case, addressed a typical “egg or chicken” question, increasingly subject of discussion in the medical literature: Does early menopause cause general premature ageing or is early menopause the result of premature general ageing? Though there, of course, is no final answer to this question, he presents succinct arguments for the latter. Above noted shifts in glycosylation patterns with advancing female age would also support this conclusion.
In a recent opinion piece in Reproduction, Australian investigators recently addressed a related subject by suggesting that endogenous cellular processes subject oocytes to significant ssDNA damage. Though dsDNA repair capacity has been well recognized as important within the context of genome stability in female gametes, the authors feel that ssDNA repair capacity, especially in older women, must also be fundamental to the survival and maintenance of follicles and oocytes.3 To us this appears like a reasonable argument. The question now, however, is, what to do about it?
REFERENCES
1. Johnson et al., Endocrinol 2022;163:1-16
2. Laven JSE., Reprod Biomed Online 2022;45(3): 421424
3. Giridharan ey al., Reproduction 2022;164:V15-V18
Interesting news on DHEA
CONFLICT STATEMENT: Readers of this section should be aware that The CHR and some of its principals have been awarded several US user patents, claiming treatment benefits form supplementation with DHEA in some infertile women. CHR and its principals receive licensing fees from these patents and are shareholders in OVATERRA by Fertility Nutraceuticals LLC, a company that produces a DHEA product called Fertinatal™.
The study we here want to bring to our readers’ attention is again a mouse study and, therefore, not automatically transferrable to the human experience. Moreover, it is a study in male mice. Nevertheless, we found it informative because it apparently is the first study ever that measured androgen levels in different organs following DHEA supplementation.
Because male mice do not have ovaries, this study does not inform on testosterone levels in ovaries, which is, of course, what would be most relevant to current DHEA supplementation schedules widely in use in female infertility. The paper, however, offers one important piece of information which, likely, is transferrable to the clinical experience of supplementing infertile women with DHEA: Post-supplementation testosterone and dihydrotestosterone levels in most organs increased but varied between organs. At least in the male mouse, DHEA supplementation did not increase androgens in muscle tissue and brain, while demonstrating unusually high concentration in the liver.
What is, therefore, to learn from this study in supplementing infertile women with DHEA? Our conclusions are as follows: (i) DHEA,
indeed, raises testosterone levels but does so, likely, to varying degrees, depending on dosage administered, preexisting levels, target organ, micronization and, therefore, possibly manufacturer. (ii) DHEA should only be supplemented if a patient demonstrates abnormally low androgen levels. (iii) Starting dosage is usually 25mg TID. (iv) After 30 days of DHEA supplementation, androgens should be reevaluated; if too high, the dosage should be reduced. (v) In patients with liver problems, liver function should be monitored, and DHEA should be discontinued if liver enzymes significantly rise. (vi) If androgen levels are kept in normal, physiological range, DHEA supplementation to ovaries can, likely, be considered adequate as well as safe, even though direct studies of ovarian androgen levels following DHEA supplementation do not exist.
REFERENCE
1. Colldén et al., Endocrinol 2022;163:1-7
Reproductive immunology
Autoimmunity
Autoimmunity and pregnancy are in such a close symbiotic relationship (to the good and the bad) that almost any news in autoimmunity has relevance to reproduction. Consequently, the news that clonal IgA and IgG autoantibodies from individuals at risk for rheumatoid arthritis have been found to identify an arthritogenic bacterium (Subdoligranulum) is potentially important news for several reasons.1 First, the finding points out once more the importance of the gastrointestinal biome for human health. Second, that one of the antibodies is a mucosal IgA antibody is very relevant because IgA antibody levels in infertile women are often abnormal, without any explanation available so-far why that would be. Mice colonized with this bacterium developed arthritis similar to rheumatoid arthritis.
In support of the concept of bacterial causes of autoimmune diseases, another new study of inflammatory disease of the spine supports the idea that an immune response to microbes may also have cross-reactivity with normal human proteins (in this case in the spine or eye, causing autoimmune disease. Specifically, human leukocyte antigen B*27 (HLA-B*27) is strongly associated with inflammatory disease of spine and pelvis (ankylosing spondylitis) as well as eye (uveitis). How HLA-B*27, however, causes this
Continued from page 30 The V oice | january 2023 | 31
to happen was unknown. This study now provided experimental supportive evidence for the hypothesis that microbial and self-antigens, indeed, in this way could play a pathogenic role in HLA-B*27associated autoimmune diseases.
REFERENCES
1. Chriswell et al., Sci Trransl Med 2022;14(668):eabn5166
2. Yang et al., nature 2022;612(7941):771-777
Pregnancy has been alleged to protect against ovarian, endometrial cancer and, possibly, breast cancer. In a recent min-review researchers from New Zealand and China put together the various explanation for such a possibility.1 They, of course, were unable to offer a final explanation but the various proposed hypotheses make interesting reading, nevertheless. Should such protection really exist, it must be multifactorial to offer enough redundancy to be successful in cases one pathway or the other fails.
REFERENCE
1. Main et al., Endocrinol 2022;163:1-6
One of the big surprises of sequencing of the human genome was that what initially was considered “junk DNA” with no functionality, actually dominates the genetic code and, in itself, is dominated by endogenous retroviruses (ERVs) and other genomic parasites, “domesticated” by a host genome over millions of years of evolution. This and many other interesting facts about human evolution were noted in a commentary in Science1 that accompanied a paper in the same issue of the journal,2 in which investigators from the U.S., Spain,
and Scotland reveal fascinating new findings regarding evolution of antiviral activity of a human protein of retroviral origin. The authors report in their manuscript the discovery of hundreds of such transcribed retroviral envelope genes primed for co-option and describe one, called Suppressyn, which restricts viral infections of human placental trophoblast, a tissue where another domesticated envelope gene, called Syncytin, promotes fusion of cells which, of course, lies at the basis for formation of syncytiotrophoblast and the placenta.
As the commentary noted, domestication of a viral envelope gene over 100 million years ago, creating the Syncytin gene, was a milestone innovation for mammals because it led to emergence of syncytiotrophoblast and the placenta, creating a barrier between fetus and mother that allowed passage of nutrients but prevented passage of viruses into the fetus. But, as evolutionary progress may also have adverse consequences, Syncytin-1 mediated cell fusion at the same time created a strong vulnerability of syncytiotrophoblast to ASCT2tropic viruses, including certain retroviruses. In searching for a possibility to block these viruses, the researchers presumed that a protein occupying ASCT2 could block entry of the virus by interfering with envelope proteins expressed by certain retroviruses and screened the human genome accordingly, identifying over 1500 fitting open reading frames (ORFs) that could encode viral envelope proteins, many with tissue-specific transcription. One of these ORFs was above noted Suppressyn, which regulates the fusion activity of Syncytin-1.
Since many, if not most embryonic genes, are transcribed only in selected time-windows of development, it was somewhat of a surprise that Suppressyn is expressed throughout human development. This finding was interpreted as meaning that Syncytin-1, beyond any developmental cellular function it may have, must have a separate essential function for the developing embryo, which the authors identify as antiviral defense. This work, therefore, suggests that Suppressyn, an endogenously expressed viral envelope gene, restricts viral replication in humans.
REFERENCES
1. Padilla Del Valle R, McLaughlin Jr. RN. Science 378(6618):356-357
2. Frank et al., Science 2022;378(6618):422-428
Can pregnancy protect against certain cancers?
Genetics
“Stolen” genes with antiviral activity, over 60 million years ago forming the first syncytium and, therefore, the placenta
Continued on page 33 32 | january 2023 | The Voice
The effect of maternal aging on oocyte aneuploidy
No laboratory in the world currently, likely, knows as much about oocyte aneuploidy as Melina Schu’s Department of Meiosis at the Max Planck Institute for Multidisciplinary Sciences in Göttingen, Germany. Moreover, nobody has ever published as beautiful photos and videos on the subject. To, therefore, have the opportunity to read a review article from this group on the impact of maternal aging on aneuploidy in mammalian oocytes, as offered recently in Nature Reviews Molecular Cell Biology, 1 is, therefore, a very special treat and should not be missed by anybody interested in aneuploidy (and who isn’t these days?).
As a very comprehensive review article, a detailed discussion of this paper would exceed the framework of this literature review. But we, nevertheless, want to point out some highlights: That chromosomal segregation errors in oocytes increase with female age is well known. But, at the same time, not all factors leading to segregation errors are age-related. The paper, therefore, separates between two principal areas that contribute to oocyte aneuploidy. It concentrates on recent discoveries that reveal new error-causing pathways and also attempt to present a framework for therapeutic strategies to extend the span of female infertility, though those clinical parts are clearly the weakest in the paper (Box 2).
The authors also provide interesting information on environmental and lifestyle factors implicated in promoting aneuploidy (Box 1). Especially emphasizing the adverse effects of obesity and exposure to environmental toxins, both factors, likely, too often overlooked in clinical practice of infertility. Overall, this paper is clearly a tour-deforce of the subject of oocyte aneuploidy, highly recommended to everybody interested in aneuploidy of oocytes and embryos.
Related, another interesting paper regarding oocyte aneuploidy came from Chinese investigators who reported new findings regarding the mechanism of acentrosomal spindle assembly in human oocytes.2 Specifically they reported that, similarly to rodents, human oocytes also possess an acentriolar microtubule organizing center (aMTOC), called the human oocyte microtubule organizing center (huoMTOC). It serves as a major site of microtubular nucleation and is essential for spindle assembly. Compared to mouse aMTOC, the huoMTOC greatly varies in numbers, localization, and composition. Mutations in TACC3, moreover cause defects in spindle assembly in humans by disrupting the structure of the huoMTOC, leading to oocyte maturation arrest. The authors furthermore conclude that these findings may have clinical significance since evaluation of the huoMTOC may allow for conclusions about oocyte quality.
REFERENCES
1. Charalambous et al., Nat Rev Mol Cell Biol 2023;24(1):27-44
2. Wu et al., Science 2022;378(6621):745
mRNA nanomedicine
Until two messenger RNA (mRNA) vaccines became the most successful anti-SARS-CoV-2 virus vaccines during the COVID-19 pandemic, there was very little talk about mRNA vaccines. That has now changed because similar mRNA nanomedicine technology can
also be applied to other medical uses. A recent review article in Nature Medicine offers a state-of-the-arts update on where the field on mRNA nanomedicine now stands.1 Besides quickly spreading applications in vaccines against infectious diseases, applications now also include at least three trials of anti-cancer vaccines (melanoma and head and neck cancer) as well as four trials for protein replacements in solid tumors, deficiencies, and autoimmune diseases, and at least one gene-editing trial for hereditary amyloidosis. Readers interested in more detail, especially the fascinating technology behind these new developments, we refer to the above-cited publication.
REFERENCE
1. Padilla Del Valle R, McLaughlin Jr. RN. Science 378(6618):356-357
Preimplantation genetic testing for aneuploidy (PGT-A)
The preceding few weeks offered an above-average number of published papers on PGT-A, especially since the November issue of JARG published several papers of interest, - some for good and others for bad reasons. Here is a brief summary:
A group of Austrian fertility experts published a critical commentary on the recent Position Statement on the Transfer of Mosaic Embryos (2021) by the Preimplantation Genetic Diagnosis International Society (PGDIS), 2 which we in the December 2022 issue of The VOICE already had severely criticized. We, of course, fully agree with the Austrian colleagues but actually wish they had been even more critical because, considering its very obvious biases and omissions, this document should never have been accepted for publication.
A very important paper was published by British colleagues who offered an analysis of how a “naive” analysis of aggregated UK assisted reproductive technology (ART) data held by the Human Fertilisation and Embryology Authority (HFEA is the UK counterpart of the CDC in the US in accumulating national IVF outcomes) can be severely misleading when PGT-A outcomes are analyzed.3 Being British and, therefore, civilized-polite, the authors did not even refer in their manuscript to the paper of another group of British investigators which in 2021, in the same journal, had, indeed, published such a “naïve” analysis of HFEA data that reached all the wrong conclusions.4 The paper was at the time heavily criticized not only for misrepresentations of HFEA data but also because of the failure of the authors to disclose commercial conflicts in relation to the PGT-A testing industry.
Suffice it to say the recent study of HFEA data completely contradicted the conclusion of the earlier paper by obtaining estimates of the effect of PGT-A with proper statistical considerations that suggested an overall modest reduction in treatment success with IVF as a result of PGT-A, while the earlier study had claimed “very obvious” improvements in IVF outcomes. Darren K Griffin, a Professor of Genetics at the University of Kent, School of Biosciences, in the UK, who was the senior author of the former paper 4 apparently, still, has not gained the necessary insights to understand how PGT-A results should be evaluated because coincidentally co-timed with the above cited recent publication in JARG, he just published an opinion paper (under the rubric “countercurrent”) in RBMOnline under the title, “Why PGT-A, most likely, improves IVF success, ”5 which in this issue of The VOICE
Continued from page 32 ADVERTISEMENT The V oice | january 2023 | 33
will be mentioned twice since it received the honor of being this month included in the “ Really Bad Paper Section” of this literature review. More about this paper, therefore, there!
How PGT-A results are correctly analyzed was also the subject of another recent paper in JARG, this time by the British colleague Paul N. Scriven, who, repeatedly before, has contributed important comments to the literature on this subject.6 He in this commentary demonstrates why marginalizing the detriment relegates the benefit when assessing the falsely alleged benefit of PGT-A in reducing miscarriages.
Surveying the literature on PGT-A, one must start wondering why so much of the well-supported criticism about the clinical utilization of PGT-A comes from overseas, especially Europe, and so little from the U.S.? Unsurprisingly, the utilization of PGT-A is low in countries where criticism is voiced (UK, The Netherlands, Sweden, Denmark, Austria, Japan) and high where one does not hear much criticism (U.S., Italy, Spain, Czech Republic).
In another JARG article in the November issue, Chinese investigators report that there is no purpose in performing PGT-A in cases where a parent is a carrier of a chromosomal inversion PGT for structural rearrangements, PGT-SR). Though this is, of course, exactly what one would expect empirically, it was nice to see that the incidence of parentally originating aneuploidy in inversion carrier couples was even lower than statistically expected.7
Finally, we only very rarely review case reports on these pages but here is one that does for several reasons deserve our attention: First, it is to our best knowledge the first reported transfer of a by PGT-A as a “chaotic” defined embryo that led to a healthy birth.8 And, yes, this was not an embryo transfer of an “abnormal” embryo at The CHR as many readers might have suspected, but a transfer by colleagues at the University of Rochester Medical Center in Upstate New York for which we congratulate them. We, indeed, wish, more IVF centers would start transferring properly selected so-called “abnormal” embryos, rather than keep them frozen or even discard them.
The second reason is that the editors of the journal where the paper appeared asked The CHR’s David H. Barad, MD, MSc., the center’s IVF program’s Clinical Director, to write an accompanying editorial,9 in which he very well explained why this occurrence was even possible and why, therefore, selected “abnormal” embryos should be transferred. We, of course, strongly recommend this commentary to our readers and also comment on it a little further under the heading “CHR Publications.”
REFERENCES
1. Murtinger et al., J Assiste Reprod Genet 2022;39:2563-2570
2. Leigh et al., Reprod Biomed Online 2022;45:19-25
3. Roberts et al., J Assist Reprod Genet 2022;39:2547-2554
4. Sanders et al., J Assiste Reprod Genet 2021;38(12):3277-3285
5. Griffin DK. RBMOnline 2022;45(4):633-637
6. Scriven PN. J Assist Reprod Genet 2022;39:2475-2481
7. Tong et al., J Assist Reprod Genet 2022;39:2573-2579
8. Lin et al., Fertil Steril Rep 2022;3(4):301-304
9. Barad DH. Fertil Steril Rep 2022;3(4):294
Sperm chemotaxis
Here is also some news regarding male infertility: To direct sperm toward the egg sperm chemotaxis is required. Chinese investigators now identified such a physiological sperm chemoattractant as DEFB19/119.3 Interestingly, this attractant is secreted by the female reproductive tract as well as the cumulus-oocyte complex. In mice, manipulation of DEFB19/119 concentrations determined the amount of sperm that reaches the egg. The investigators, moreover, identified in women with idiopathic (“unexplained”) infertility low levels of the attractant in follicular fluid.
If confirmed, this paper in Cell Reports Medicine is a potentially very important discovery with diagnostic as well as potential therapeutic translational implications for female as well as male infertility.
REFERENCE
1. Li et al., Cell Reports Med 2022;3:100825
Since when do Ashkenazim exist?
A paper recently published in Cell garnered unusual attention, the most important being that everybody was surprised the study could have even been performed. The question to be answered was when did the founder event happen that created the Ashkenazi genetic identity? Genetic studies of Jewish ancestries have been practically impossible because Jewish law strictly forbids the disturbance of buried human bodies. When 33 Ashkenazi graves dated to the 14th century were discovered at the medieval Jewish cemetery in Erfurt, Germany, a Solomonic rabbinical decision that allowed the use of loose teethes for genetic analysis, rather unexpectedly, allowed the recently reported study to go ahead. Interestingly, those 14th-century Jews were found to be genetically similar to contemporary Ashkenazim, but they demonstrated more variability in Eastern-Europeanrelated ancestry than today’s Ashkenazim do. A third carried a mitochondrial lineage (inherited only through the female) common in modern Ashkenazim; eight carried pathogenic variants known to affect Ashkenazim today. These findings suggest that the Ashkenazi founder effect and acquisition of main sources of ancestry must have occurred before the 14th century. They, moreover, suggest that Ashkenazim then were genetically more diverse than they are today.
Viruses and bacteria
Persistence of the SARS-CoV-2 virus
A recent report in Nature magazine offered results of autopsies of 44 patients who died of COVID-19 in an effort to determine the presence of the SARS-CoV-2 virus in different parts and organs of the body. Especially in patients who died with severe disease, the virus was found to be widely distributed including in the myocardium, lymph nodes, sciatic nerve, ocular tissue, and already in early infection in all parts of the brain except the dura mater. The persistent virus was found in multiple anatomic sites as late as 230 days following the onset of symptoms, including
Huang et al., Nat Med 2022;28:2273-2287
REFERENCE 1.
34 | january 2023 | The Voice Continued on page 35
throughout the brain. Outside the respiratory tract, the investigators, however, found little evidence of inflammation or direct cytopathology. Somewhat disappointingly, the study, however, could not further our understanding of long-COVID-19 disease.
REFERENCE
1. Stein et al., Nature 2022;612:758763
Finally, - a vaccine against all known influenza virus subtypes?
A recent study in Science magazine by US investigators1 suggested that a multivalent nucleoside-modified mRNA vaccine may, finally, offer a breakthrough toward a universal anti-flu shot. Since seasonal influenza vaccines offer only poor protection against pandemic influenza strains, the search for a universal vaccine has been underway for some time. The U.S. investigators, using mRNA vaccine technology, now reported such a multivalent vaccine that elicited concomitantly high levels of cross-reactive and subtype-specific antibodies in mice and ferrets which reacted against 20 encoded antigens. Similar approaches may also work against other viruses, as the authors pointed out. A race toward a multivalent anti- SARS-CoV-2 virus vaccine is, of course, also underway, considering the rapidly declining effectiveness of current vaccines against new virus variants.
REFERENCES
1. Arevalo et al., Science 2022;378(6622):899-904
you heard about “viral interference?”
The media have written extensively about the so-called triple-threat, or as some called it, “Tripledemic,” caused by the convergence of COVID-19, the annual influenza season, and respiratory syncytial virus (RSV), which this year appears to have an unusually pronounced presence in the population, mostly in young children. But as a recent article by science writer, Jon Cohen, in Science magazine suggests, things may not be as bad as they look, and the reason is “viral interference.”
As it turns out, viruses, and especially respiratory viruses, often “interfere” with each other. A good example was the first two years of the COVID-19 pandemic which almost completely shut out influenza infections. Epidemiologists, therefore, consider it unlikely that all three viruses will circulate widely at the same time. But ultimately nobody can be certain because how much the virus circulates always depends on so many different factors, including population immunity, when the virus last circulated, and, of course, vaccination rates in the population.
Already in 1975 virologists identified interferon as the agent that makes interference possible. In other words, what protects us in such cases is our innate immune system. As Cohen reports, studies have shown that an organoid model rhinovirus interfered with SARSCoV-2, and in a different experiment, influenza A and SARS-CoV-2 blocked each other out.
REFERENCE
1. Cohen J. Science 2022;378(6622):814-815
The gut microbiome and exercise craziness
All of us now understand that we have an additional, highly involved organ in our gut microbiome that represents pounds of bacteria and more cellular units than our bodies consist of. It also affects most, if not all, of our body’s function, including the brain through what is now called the gut-brain- microbiota- axis. Now medical writer Elizabeth Pennisi reports that “exercise-crazy mice have their gut microbes to thank.1
But men are not mice and, therefore, this tentative microbiome function in humans must still be confirmed. Some supportive evidence already exists in that the microbiome of marathon runners differs from that of non-runners and some scientists in the field are already working on probiotics for humans that would favor exercise.
REFERENCE
1. Pennisi E. Science 2022;378(6625):1157
Basic science
Though the recent few weeks have been relatively slow on reproduction-connected published research, a few papers deserve mention: An article in Cell reported on the embryonic origins of adult pluripotent stem cells (aPSCs) which can be found in many cell lineages but how they form during embryogenesis has remained unknown. Harvard investigators now in this paper identified cellular mechanisms and a molecular trajectory for aPSC formation that, as they suggested, opens the door for in vivo studies of aPSC regulation and evolution.1
U.S. and Chines investigators also published a paper in Nature magazine utilizing 8-11 cynomolgus monkeys (56,636 single cells) and performed an in-depth transcriptomic analysis of major perigastrulation cell types, shedding light on the development of the primitive streak somatogenesis, development of gut tube, neural tube patterning and neural crest differentiation. The study, in addition, involved comparisons of mouse embryos and human embryoids which revealed conserved and divergent features of perigastrulation between species. The authors described their work, as filling the knowledge gap in non-human primates but also as a
Have
The V oice | january 2023 | 35 Continued from page 34
resource for understanding human embryogenesis and developmental disorders.
REFERENCES
1. Kimura et al., Cell 2022;185:4756-4768
2. Zhai et al., Nature 2022;612:732-738
The really bad paper section
Though there were several more, three paper we felt definitely qualified this month for this section, and here they are: The first price goes definitely to Prof. Griffin’s recent opinion piece in Reproductive BiomedOnline, which we already criticized in the preceding Genetics section of this literature review under the sub-heading PGT-A.1 So, let’s add on a bit: This is an opinion piece that basically says nothing. It, therefore, is difficult to understand how editors are willing to even consider a paper that makes “most likely” claims. The title of the paper basically says it all: “why PGT-A, most likely, improves IVF success.” Seriously?
After over 20 years of PGT-A (or PGS as it was called before 2016) to write a paper claiming that PGT-A “most likely” works is absurd. And what does “most likely” really mean, - in 30%, 50%, 90%? Since when does medicine propose treatments on such a basis, especially if denial of transfer of embryos unequivocally reduces pregnancy chances for IVF patients? There is, however, some progress to be noted in comparison to his earlier by now rather infamous paper in JARG on the subject,2 recently so well rebutted by other British colleagues:3 At least he now acknowledges his economic interests in the subject when noting financial support from Cooper Surgical and Igenomix. likely the two largest PGT-A laboratory providers in the world, outside of China. He did not do that in his prior paper. Moreover, in his prior paper in 2021, he was still certain that PGT-A improved IVF success; now it’s only “most likely.” Let’s see what he is coming up within 2023?
And then there was another PGT-A paper, this time from Turkish colleagues who wrote a paper in JARG under the title: “What to advise to patients with only one good quality blastocyst, PGT-A or not?”4 This is also an astonishing piece of work that really should
never have been accepted for publication because this manuscript, as so many before it on the subject, breaks all the accepted rules of data presentation, from, still, reporting pregnancy rates with reference embryo transfer and, therefore, ignoring patient selection biases. We really thought that by now we were beyond this point in the discussion on PGT-A; but we, obviously, were incorrect. Like Griffin’s paper in 2021,1 This paper will undoubtedly elicit responses. And they will not be supportive!
Finally, likely the least offensive of here selected three papers, that claim to have investigated the impact of endometriosis on IVF outcomes, except that it did anything but what it promised: It pretends to be a retroactively matched study of women with and without endometriosis. How they were matched is unclear, as is how a diagnosis of endometriosis was affirmed and/or refuted. What stages of disease women with endometriosis had is also unclear. Inclusion into the study was dependent on an AMH level of at least 1.1 ng/mL, but this kind of AMH is low at age 20 but exceptionally high at age 40. Moreover, this measure, likely, excluded really poor prognosis patients with low functional ovarian reserve. We, indeed, could go on with many additional reasons why this paper also should never have been accepted for publication, - but we have mercy!
REFERENCES
1. Griffin DK. Reprod Biomed Online 2022;45(4):633-637
2. Sanders et al. J Assist Reprod Genet 2021;38:3277-3285
3. Roberts et al., J Assist Reprod Genet 2022;39:2547-2554
4. Kahraman et al., J Assist Reprod Genet 2022;39:2555-2562
5. Invernici et al., Reprod Biomed Online 2022;45(2):275-281
The CHR
Fighting for every egg and embryo
36 | january 2023 | The Voice Continued from page 35

The Center for Human Reproduction Fighting for every egg and embryo Conne C t with us! www.the C hr. C om so C ial@the C hr. C om 212.994.4400 21 e 69th s t n ew y ork, n ew york 10021 ADVERTISEMENT













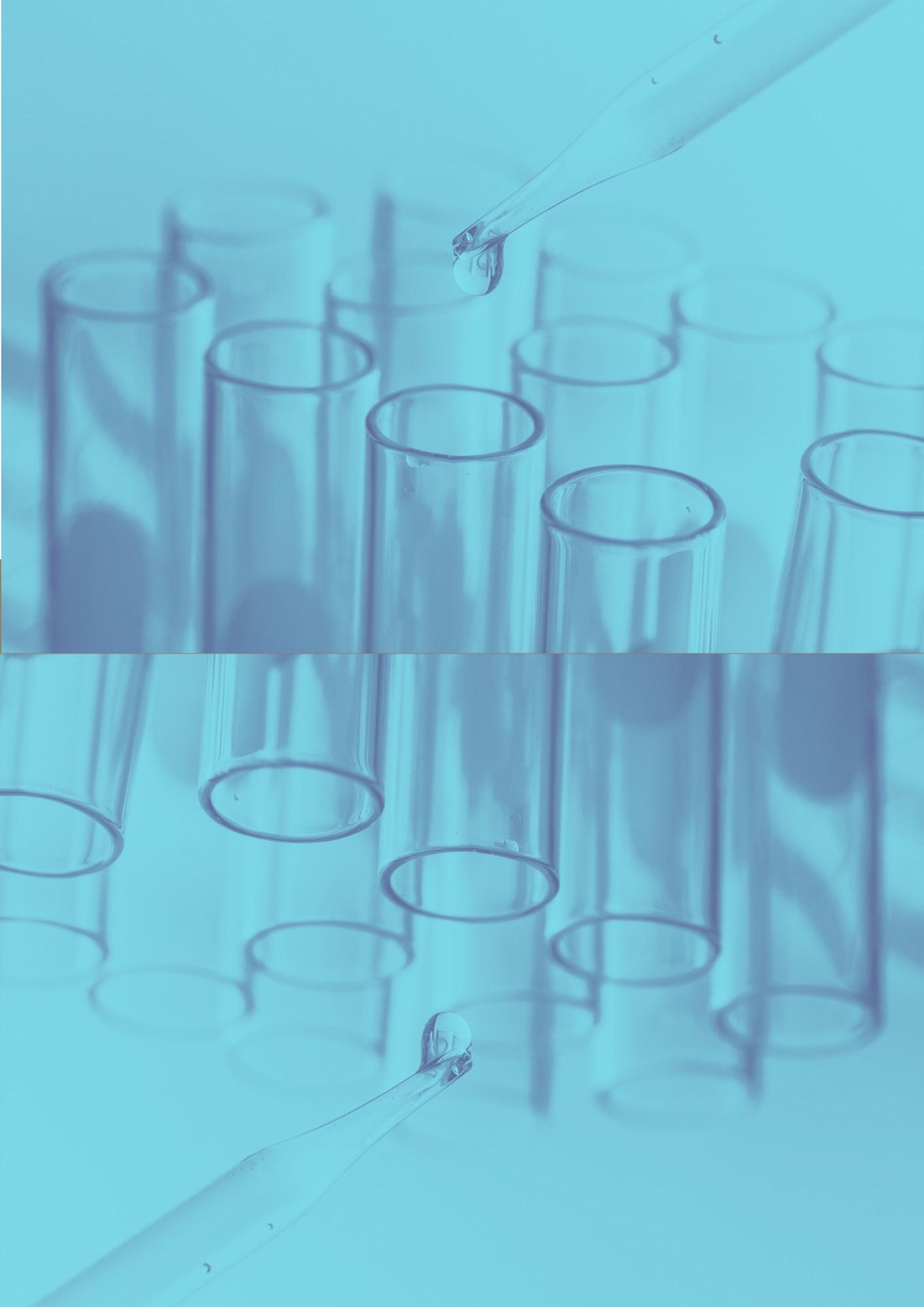





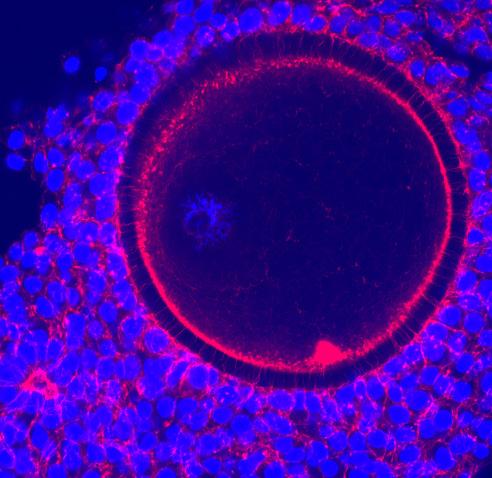
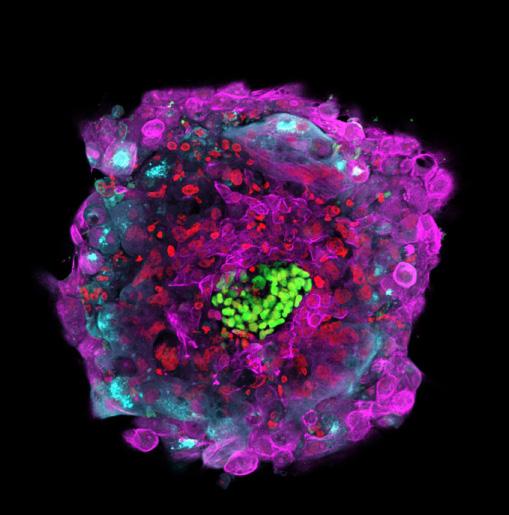
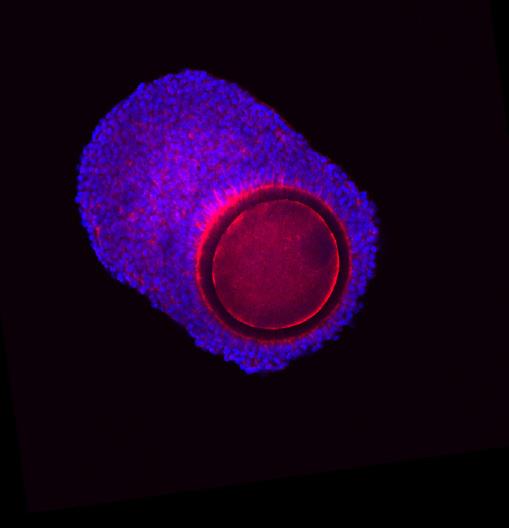
 By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist
By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist