THE CENTER FOR HUMAN REPRODUCTION FEBRUARY 2023 in this month’s issue The CHR Letter Once Adults - Will IVF children be as healthy as spontaneously conceived offspring? A COVID-19 Update - With all that uncertainty, what we want patients to know! A Piece of My Mind: How do we protect ourselves from medical misinformation? The CHR’s Interpretation Of Recent Medical Literature relevant to reproduction 03 05 09 17 27 Cardiovascular Diseases are the #1 cause of deaths in pregnancy 13 Questions Patients Ask 23 Happy Valentine’s Day CHR Publications 22
The CHR is known as a “fertility center of last resort,” primarily serving patients who have previously failed treatments elsewhere. Among CHR’s areas of special expertise are treatments of “older” ovaries, whether due to advanced female age or premature ovarian aging (POA), immunological problems affecting reproduction, repeated pregnancy loss, endometriosis, polycystic ovary syndrome (PCOS), tubal disease, male factor infertility, etc.


hirinG

AT THE CHR
BOARD-CERTIFIED RE-I AT ASSOC. PROF/PROFESSOR LEVEL

The CHR is looking for another senior board-certified RE-I (or international equivalent) to join our growing national and international practice. Though private, our center is organized along academic principles in that physicians are expected to excel not only as clinicians but also as researchers. The center’s uniquely structured compensation package, therefore, incentivizes both activities. We are looking for an individual with documented excellence in both areas, commensurate with associate professor/professor level. Besides a competitive salary, incentive bonus structure, and excellent benefit package, the CHR also offers partnership along either a 3-year or 5-year equity track and, ultimately, part or complete ownership, as the current leadership is expected to retire within that time-period.

If you feel qualified for the position and share our philosophy of being a physician-scientist, please let us know by submitting your C.V. and a brief letter of interest to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position can be filled immediately. All submissions are considered confidential.



CONNECT WITH THE CHR
the last issue of The VOICE? Access previous issues on thechr.com
Missed
www.thechr.com @CHRNewYork @CHRNewYork @CHRNewYork 2 | february 2023 | The Voice
ADVERTISEMENT
the VoiCe
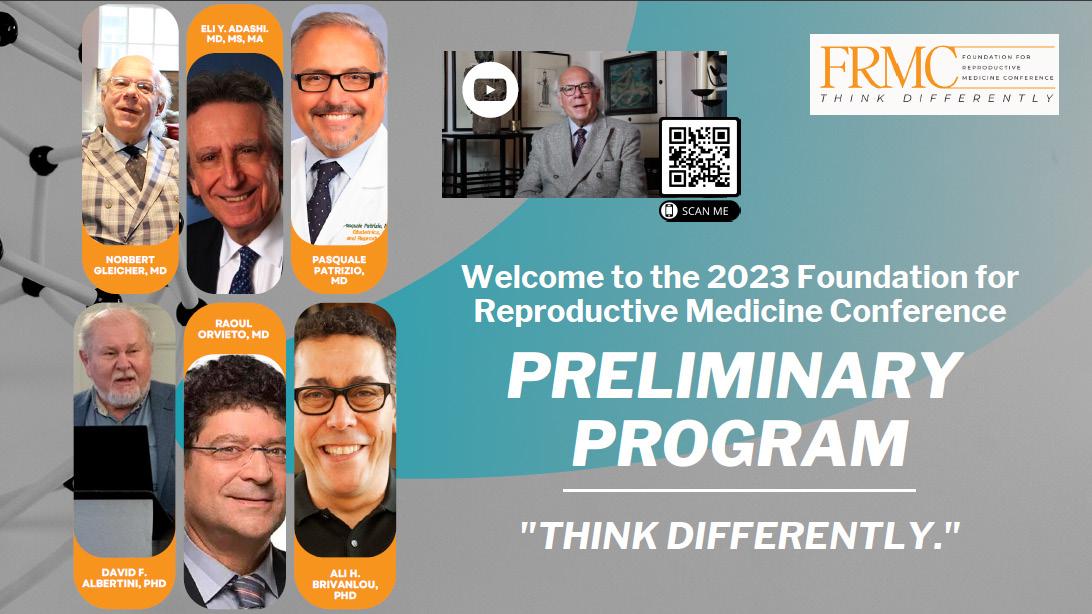
We are very pleased to offer the February 2023 issue of The CHR VOICE and want to take the opportunity of this introduction to direct the attention of our readers to the fact that, after a three-year break due to COVID-19, The CHR this year, once again, proudly co-sponsors in New York City (NYC) the annual Foundation for Reproductive Medicine Conference (FRMC) in Translational Reproductive Biology and Clinical Reproductive Endocrinology between December 1 and 3, 2023. The new and even better conference venue and hotel will be the InterContinental New York, Times Square, on 300 West 44th Street, right in the Broadway theater and restaurant district, and the timing is two weeks closer than in the past to Christmas and Chanukkah (this year December 7-15), offering attendees even more exposure to the unique atmosphere in NYC during these few weeks, which usually reaches a peak with lightening of the Christmas tree at Rockefeller Center on November 30, just in time to welcome all the attendees to the FRMC.
As most readers of this newsletter, likely, already know, the FRM is a not-for-profit research foundation, supporting much of The CHR’s research and, therefore, as the main sponsor of the FRMC, the ideal partner for The CHR.
In the years preceding the COVID-19 pandemic, the FRMC earned for several very obvious reasons considerable applause and a very special reputation among attendees for being “different” from practically all other conferences in reproductive medicine: (i) The Conference is unique in how it brings together leading basic science and clinical infertility medicine, thereby, facilitating and speeding up the translation of discoveries in basic science into new treatments. (ii) In addition, the presence of leading basic scientists and clinicians over three days in the same environment, listening to each other’s presentations, as we quickly learned during these earlier meetings, always leads to new collaborations. And, as we all by now know, nothing is more important in advancing progress in fertility treatments than for basic scientists to understand where new basic knowledge is required in serving infertility patients, and for clinicians to understand where such knowledge can be obtained (and in many cases already may exist). Unfortunately, still, only too often, neither side knows what the other side is doing. As frequently noted in evaluations, the FRMC, therefore, was eye-opening for many attendees.
But what really made the FRMC “famous” were its two main mottos: “to think differently” and “what you, likely will not hear elsewhere.” We in the pages of this newsletter often point out how, in many different ways, treatments at the CHR have over the years come to significantly differ from “group-think” in the field. And most of these differences have, in fact, been the result of CHR’s investigators and clinicians having made it into a routine to “think differently.” The CHR sees this as the most essential and most basic component of the center’s research attitude and the main reason why The CHR for decades has been so successful in advancing fertility treatments.
Centering the FRMC around the motto “to think differently” has, therefore, been an essential contribution of The CHR to the Conference since its founding and, of course, will also be reflected in this year’s Conference and its large pool of invited speakers from around the world.
We are also pleased to announce that registration for the Conference has opened. Please visit https://www.foundationforreprodmed.com/frmc-2023. Our brand-new registration system will, in one swoop, allow you to register for the Conference and make room reservations at the Conference venue InterContinental New York, Times Square hotel. Please note that, because of the high room demand in NYC in the pre-Christmas period, we could secure for the three days of the Conference only a limited number of rooms at reduced pricing. If you plan on staying in NYC for some extra days, the hotel also agreed to extend those discounts for a limited number of registrants to extra days before or after the Conference. Because room numbers are limited, we recommend early reservations. Should the need arise, registrations, as well as room reservations, can be cancelled without penalty until one month before the

FEBRUARY 2023 The V oice | february 2023 | 3
Scan the QR code to watch the FMRC 2023 introduction video!
Continued
Conference start. Early registration also offers significant cost savings.
For questions regarding the FRMC, please contact info@foundationforreprodmed.com. Though the Conference is meant primarily for clinicians and basic scientists in the field, we also in past years have been able to welcome some of the CHR’s patients as well as patients (and other lay people) from elsewhere. To also facilitate their early registration, the FRMC again offers “day-only” passes at reduced registration rates. Attendance by media is free but must be registered in advance at https://whova.com/portal/registration/frmc_202301/. Considering the long COVID-19 break and all the new knowledge that has accumulated in reproductive medicine over this time period, we are looking forward to record attendance, and who does not want to Christmas shop in NYC?

Coming back to this issue of The VOICE, readers will, again, find the usual sections: In his monthly “A Piece of My Mind” column, The CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, addresses the problem of medical misinformation. Like elsewhere in daily life, because of “old” and social media, misinformation has become a topic of considerable national interest and, of course, can also involve medical information, as the COVID-19 pandemic so well demonstrated. That is, however, only part of the story since medical misinformation can also be produced “in-house” (i.e., by the medical profession itself). Other headers of articles are listed on the front page, and, as always, the newsletter ends with a review of the published literature. We hope you will enjoy the read!
The Editorial Staff of the VOICE
would you like a copy of the voice mailed to your door?
we are excited to announce that the voice is now available in print!
To sign up for a print subscription, please reach out to social@thechr.com and specify how many copies you’d like to receive each month. Our team will follow up with a payment and address inquiry

4 | f ebruary 2023 | The Voice
from
3
page
ADVERTISEMENT
Once adults - will IVF children be as healthy
as spontaneously conceived offspring?
The literature suggests that so far over 8 million humans on this earth were conceived through In Vitro Fertilization (IVF), and the numbers are, of course, growing. Considering the at times highly exaggerated concerns expressed about IVF going as far as predicting the birth of “monsters,”1 innumerable studies have compared birth outcomes between IVF - and naturally-conceived offspring and, in general, have found no adverse effects caused by IVF. When slight differences were found, they usually were attributable to infertile IVF patients often having underlying associated medical conditions that explained observed discrepancies.
More recently, however, a series of studies have started to raise additional questions. Those questions started with the recognition of the importance of epigenetic effects on embryos pre-entry into the endometrial cavity and post-entry during nine months of gestation. A very recent Chinese study in the prestigious journal, NATURE MEDICINE, has now raised these concerns to new levels and provided the impetus for this article.²
Introduction
Contrary to widely held beliefs, the history of IVF did not start with the world’s first reported IVF birth in the United Kingdom on July 25, 1978.³ This birth was, indeed, preceded by years of research and failed attempts by Patrick Steptoe, MD, and Robert Edwards, PhD, who in 1978 finally succeeded,but also by others. What also is often forgotten is that in those days this kind of research, often, had to take place in relative secrecy because the public, media, and even academia, were strongly opposed to such research on medical, ethical, and religious grounds, not only arguing that such research was amoral but also expressing fears that the end products of IVF would be the birth of “monsters” or, at least, the birth of medically “abnormal” offspring.1 The prominent British magazine Nova in the spring of 1972 ran a story arguing that, what then was called “test-tube babies,” represented, “the biggest threat (for mankind) since the atom bomb.”4
Likely in academic medicine representing this mindset best at the time, was a 1973 incident at Columbia University, in New York City, where Landrum Brewer Shettles, MD, at the time a prominent faculty member and researcher of the OB/GYN department, who had co-authored the bestseller, “How to Choose the Sex of Your Baby,” which sold over 1
million copies, attempted a first human in vitro fertilization of a woman’s egg with her husband’s semen. His department’s chairman, Raymond L. Vande Wiele, MD, himself at the time a famous infertility specialist, became aware of the experiment and took it upon himself to destroy it. Columbia accused Shettles of “ignoring acknowledged guidelines for human experimentation and acting in an unsafe and unethical manner,” and he was forced to leave the institution. Doris and John Del-Zio, the couple that had donated their gametes for the experiment, then sued the university for damages, with the trial that ultimately awarded the couple only $50,000 (they had sued for $1.5 million), paradoxically, occurring in July of 1978, exactly when the first IVF baby was born five years later.⁵
From experimental procedure to mainstay among fertility treatments
After the first IVF birth, newly established IVF centers, initially, operated under experimental protocols supervised by Institutional Review Boards; but progress was rapid and, within a few short years, IVF went from being an experimental procedure to becoming a mainstay among infertility treatments. This progression was, however, responsibly guided by a research community that, from the very beginning, was concerned
about the potential of adverse effects of IVF on offspring. Considerable efforts were, therefore, invested into investigations of newborn follow-ups conceived through IVF, almost uniformly demonstrating no outcome differences between IVF and spontaneously conceived offspring.⁶-⁸ When differences were noted, they, usually were explainable by underlying medical and, therefore, dismissed.⁹
A retrospectively very precinct opinion paper on the subject appeared in 2013 penned by the current Editor-in-Chief of Fertility & Sterility, Kurt T. Barnhart, MD, in which he made the point that a preponderance of evidence, indeed, does suggest that IVF is associated with significantly increased perinatal consequences, “even though the vast majority of children conceived with ART are healthy.”10 Following a detailed discussion of methodological limitations of published studies, he concluded that “the association of IVF with perinatal morbidity does appear to be real,” citing as examples associations between ICSI and certain (urological) congenital abnormalities, of extended embryo culture to blastocyst-stage with preterm delivery, and of more low birth weight after fresh than frozen-thawed embryo transfer all, of course, since further defined.
More recently, however, studies started surfacing that suggested that IVF may affect embryo quality and that even a proven healthy uterine environment may
The V oice | february 2023 | 5
Continued on page 6
not overcome those.¹¹ In other words, the IVF process in itself, may be responsible for increases in adverse perinatal/ neonatal outcomes like preterm births, low birth weight, etc., in comparison to spontaneous conceptions. In addition, studies started to appear reporting differences in epigenetic control of transposable elements and imprinted genes in newborns between IVF and spontaneous pregnancies, even in absence of underlying infertility.¹² Other observations suggested that embryo culture media affect perinatal pregnancy outcomes.¹³ Moreover, while maternal diseases in pregnancy have been known to affect pregnancy outcomes for decades, it recently has also become increasingly obvious that maternal disease affects not only can affect pregnancies but can carry over into effects manifesting at adolescent and even adult ages. Good examples are influenza¹⁴ and gestational diabetes.¹⁵
The most recent findings
All of this, of course, raises concerns because the many studies over the decades that, more or less, dismissed concerns about significant adverse effects of the IVF procedure itself on offspring, at least until recently, never looked at potential long-term effects because even the world’s oldest IVF baby is currently only 44 years old. We, simply, have not had in the past, and still do not currently have the historical experience that would allow us to predict what the effects of IVF, for example, on longevity may be. Not only can we not predict long-term effects on the first generation of IVF children, but we, of course, can be only even less certain about the effects of epigenetic changes induced into embryos during IVF that later may be inherited into future generations.
This is why a recent paper in Nature Medicine ² by Chinese investigators attracted so much attention because they investigated the initial leukocyte telomere length (LTL) of 1,137 individuals from 365 families, including 2002 children conceived by IVF and 205 conceived spontaneously. As a well-known
indicator of age-related phenotypes in later life, LTLs offer exactly the kind of look into the future, which we currently do not have regarding the consequences of being born as an IVF baby. The results were concerning: At age one year IVF children had significantly shorter LTLs than spontaneously born children, and this finding was maintained after adjustments for confounding factors. Moreover, the finding was much more pronounced after the transfer of blastocyst-stage than cleavage-stage embryos. The association was then further validated in 586 children conceived by IVF from five centers using different LTL quantitation methods and blastocyst-stage transfers in mice postnatally of day-1 and statistically marginally (P=0.042) at six months. Mouse embryos cultured did not demonstrate suppressed telomer shortened telomere length at late cleavage stage but did suppress telomerase activity at early blastocyst stage. The authors concluded that, in offspring conceived by IVF, there exists a need to evaluate the long-term consequences of IVF on aging-related phenotypes.
For IVF practice these findings, however, raise some additional, and more immediate questions regarding almost routine extended embryo culture to blastocyst-stage in most IVF centers: The CHR has, of course, for years in these pages and in many articles in the literature argued against this practice. Here discussed paper’s raised concerns are probably not enough for most IVF centers to curtail current practice patterns to significant degrees, but all IVF practitioners, at minimum, should now be more cognizant that there must be a good reason why a patient’s embryos are cultured to blastocyst-stage. In other words, a switch in practice patterns from, when in doubt - go with blastocyst-stage culture to, when in doubt go with cleavage-stage embryo transfer, appears now to have much more support.
In the same issue of Nature Medicine, Prof. Daniel R. Brison, PhD, FRCPath, a Consultant Clinical Scientist in the British
NHS and Scientific Director of a clinical Department of Reproductive Medicine offering infertility treatments, from the University of Manchester at the Manchester Academic Health Sciences Center in Manchester, UK, offers a very well-written brief commentary ¹⁶ to the paper by Chinese investigators.² His concluding paragraph is worth citing verbatim:
“Ultimately the aim of such research is not to discourage the use of ART (IVF) but rather to make it as safe as possible. The current ART industry represents a profound experiment in human reproduction, one that has brought joy to millions of people, but as with any medical intervention, the use of ART also carries risks. Researchers and clinicians owe it to the millions of future children who will be conceived via ART to identify the modifiable risk factors that will optimize their lifelong health, while at the same time caring for extant offspring as they age.” The time appears right to revisit the “extended embryo culture for all “– mantra!
REFERENCES:
1. Mulkay M. Scinec, Technology & Human Values 1996;21(2):157-176
2. Wang et al., Nature Med 2022;28:2646-2653
3. https://www.history.com/this-day-in-history/ worlds-first-test-tube-baby-born#:~:tex t=On%20July%2025%2C%201978%2C%20 Louise,parents%20Lesley%20and%20 Peter%20Brown
4. https://research.mcdb.ucla.edu/Goldberg/ HC70A_W04/pdf/SciAmer:PandoraBaby:2003. pdf
5. https://www.library-archives.cumc.columbia. edu/obit/landrum-brewer-shettles
6. Wennerholm et al., Lancet 1998;35(9109):1085-1090
7. Litzky et al., Epigenetics 2017;12(8):653-661
8. Halliday et al., Fertil Steril 2014;101(4):1055-1063
9. Fauser et al., Reprod Biomed Online 2014;28(2):162-182
10. Barnhart KT. Fertil Steril 2013;99(2):299-302
11. Woo et al., Fertil Steril 2017;108(6):993-998
12. Choux et al., Hum Reprod 2018;33(2):331-340
13. Sacha et al., Fertil Steril 2022;117(6):1246-1254
14. Song et al., BMC Infect Dis 2020;20(1):502
15. Hammond et al., Diabetologia 2018;61(5):1037-1045
16. Brison DR. Nat Med 2022;282476-2477
6 | february 2023 | The Voice Continued from page 5
TRYING TO REACH THE INFERTILITY COMMUNITY?
Have you thought about advertising in the VOICE?
This newsletter every month goes electronically to ca. 80,000 infertility patients, medical professionals in the field, and members of the media, with almost 25% (an unusually high number) also opening the VOICE.
hirinG
AT THE CHR
For further information, please contact:
Ms. Alexandra Rata
(212) 994 4400 or e-mail to arata@thechr.com
ONE or TWO-YEAR CLINICAL FELLOWSHIP in RE-I

If you failed in securing a formal fellowship position in RE & Infertility or simply want a change out of general OB/GYN practice, the CHR offers a fellowship position in RE-I which after 1 year will greatly improve competitiveness for a formal fellowship position and in 2 years establishes independent competence for establishing an infertility practice. The center’s last 1-year fellow was accepted into the NIH-fellowship program after failing to secure a position in the preceding year.


Qualified candidates must be OB/GY board-eligible or certified, be eligible for hospital privileges and for a New York state license to practice medicine. As CHR maintains a very active research program in affiliation with Rockefeller University, CHR fellows gain substantial research experience, with great likelihood resulting author- or co-authorships in peer-reviewed publications. Board eligible candidates who still must accumulate surgical cases will be given the opportunity to do so.
Chosen candidates will receive a very competitive salary and a generous benefit package, including health and malpractice insurance as well as paid vacation time. If you feel that you qualify and are interested in a career in RE & I, please submit your CV and a brief application letter to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available as of January 1, 2023. All submissions are considered confidential.
The V oice | f ebruary 2023 | 7
ADVERTISEMENT ADVERTISEMENT ADVERTISEMENT
Everyone that works at CHR is so kind and professional. - JB
PATIENT TESTIMONIALS

PATIENT TESTIMONIALS PATIENT TESTIMONIALS PATIENT TESTIMONIALS
Very professional and efficient. Straight forward and informative!
8 | f ebruary 2023 | The Voice
“ “
- GL
A COVID-19 UPDATE
With all that uncertainty, what we want patients to know!
Messages in print, on television, and from social media regarding the COVID-19 pandemic are, at times, quite confusing; but that is of course nothing new and, likely, contributes to the almost laissez-faire attitude that appears to have settled upon the U.S. and, really, most of the world, most surprisingly, including China.
Where we are
In some ways, the pandemic appears behind us in that almost nobody masks up any longer and social distancing is a thing of the past. The public’s utilization of anti-COVID-19 vaccine boosters has significantly dropped, as have sales of antiseptic solutions and wipes. Yet, in other ways, the pandemic is clearly not over, - in an epidemiological sense we, indeed, are still in the midst of it and are, at the time of this writing, likely, on the downhill slope of yet another winter wave, the fourth since COVID-19 started late in the fall of 2019.

We hardly notice because currently circulating viral strains, while highly infective and, indeed, getting constantly better at evading our immune systems even if boosted, cause only relatively mild disease. Why that exactly is, remains to be determined but appears to reflect the natural history of viral pandemics, over time tending to become less lethal. That the currently dominant XBB.1.5 strain of the SARS-CoV-2 virus usually causes only mild disease, this, however, does not mean that high-risk, especially older and/or immune-suppressed individuals, do not end up hospitalized or are not still dying. Hospitalization and death rates are just much lower than they used to be, especially during earlier waves during the pandemic. XBB.1.5, therefore, only very unlikely will become a global threat.1
What we need to be concerned about
Another part of the natural history of viral pandemics is that, rather than being pandemic and infecting populations in sequential waves, the virus becomes endemic, which means it causes infections only sporadically and usually in quite restricted areas. Due to vaccinations in large portions of the population in the U.S. and elsewhere, there was some hope that by now we would have reached an endemic state; but, as already noted, that is clearly not the case. Though the current state of affairs in the U.S. and Europe appears tolerable, the question, however, remains whether things will continue this way or get worse again.
Continuation is not guaranteed because new mutations to the virus do not have to follow old habits: nothing guarantees that they will only continue to become more infectious but less virulent. The picture would obviously change overnight if a future variant accelerated in infectivity as well as clinical virulence.

And there is serious concern that this may, indeed, happen. Most of the new concerns stem from the unexpected changes in COVID-19 management that have in recent weeks taken place in China. Overnight, the country switched from the world’s most oppressive shut-down policy to the other extreme, - a no-control whatsoever policy, causing unprecedented consequences
Continued on page 10
The V oice | f ebruary 2023 | 9
inside China. Consequences will, however, not only affect China but, undoubtedly, will also, once again, affect the whole world. Millions of new COVID-19 cases among 1.4 billion Chinese citizens, with the Chinese government, suddenly, removing any and all travel restrictions for the first time in three years and allowing unlimited flights in and out of the country, simply, allows for no other conclusions.
Concerns further increased because of how the Chinese government, suddenly changed policy,reaching the decisions in secret and without prior collaborative preparations with the rest of the world. In addition, China is (as on many prior occasions during this pandemic) hiding the consequences of the policy change by publishing outrageously low infection and death rates which border on the absurd, considering how overburdened Chinese hospitals very obviously are and considering the long lines in front of crematoria, the principal method of burial in China.
Most concerning, however, is that the Chinese government never acts without a purpose: Especially its move toward “open skies,” is very reminiscent of what China did in late 2019, when the country discovered the first cases of COVID-19 in Wuhan (and later in other cities) and, instead, of alarming the world, kept all of this a secret until the whole world was infected by travelers from China. Considering the country’s past behavior, one cannot dismiss the notion that the Chinese government, finally recognizing that its three-year-old COVID-19 policy was no longer sustainable, and aware of the tremendous consequence of its sudden change in COVID-19 policy in a severely under-immunized 1.4 billion population, decided on repeating its 2019 strategy and, once again, getting the world reinfected in parallel to China. Allowing only China’s economy to suffer from the current gigantic COVID-19 outbreak in China would, of course, adversely impact China’s competitiveness with the U.S. and the rest of the Western world. But if Western competitors had the same problem, China would lose out too much lesser degrees.
In attempts to prevent the export of the disease into their countries, Western governments, including the U.S., have instituted testing mandated for travelers from China. Those are, however, only political alibies for politicians, with everybody very well understanding that, once flight routes are opened, the virus cannot be controlled through 48-hour pre-testing of passengers. Once again, the world has already started importing COVID-19 from China. One among many questions immediately arising is, what variant or what variants?
Media reports from China currently claim that the same XBB.1.5 variant, currently dominant in the U.S. and Europe, is at this time also the dominant variant in China. Yet, as with all other COVID-19 information coming out of China, one must be skeptical. Even under the assumption that XBB.1.5 is really currently China’s dominant variant, which other variants are already “brewing” to lesser degrees in China’s huge currently infected population, likely involving hundreds of millions of citizens?
The big threats, of course, are new variants and, as the world has gotten used to most new influenza virus strains every year coming out of China, it would not surprise if most future strains of the SARS-CoV-2 virus would follow this example.

There is yet another major concern surrounding this topic from which many media sources are shying away: Considering the past behavior of the Chinese government in suppressing investigations of where the SARS-CoV-2 virus came from, can we even be certain that the Chinese government may not, first, modify the viruses it is sending out into the world? After all, after years of denial, even The Lancet now to a degree acknowledges the possibility that a (Chinese military) research center (in Wuhan) may have been the source of where we got the virus in the first place. Remarkably, The Lancet Commission in its 2022 report acknowledged, “that there are two leading hypotheses: zoonotic spillover from wildlife or a farm, possibly through a wet market or from a research-related incident.”³ Considering that The Lancet for the longest time has been carrying water for the Chinese government in insisting that only the zoonotic hypothesis was realistic, this represents progress. These two opposing hypotheses have, however, co-existed since almost the beginning of the pandemic,⁴ and not only represented by proponents of conspiracy theories, as much of the media initially wanted us to believe.

Continued from page 9 10 | f ebruary 2023 | The Voice Continued on page 11
Are we ready for another round of more severe COVID-19?

The answer is a clear, no, we are not! And this is true for several reasons: First, our available vaccines against COVID-19 are losing effectiveness by the hour; every day that passes, they prove to be less effective against currently circulating strains. As we will discuss further below, that does not mean that selected individuals should not be vaccinated. We still believe that the best evidence supports booster vaccinations for at least high- and moderate-risk patients since boosters as of now, still, do reduce the severity of disease. For how much longer such a positive risk-benefit ratio will still hold up for existing vaccines is, however, unclear. Why industry and government are not producing improved vaccines at an accelerated pace is, therefore, difficult to understand.
What is even more difficult to understand, however, is the inactivity of industry and government in developing effective treatment modalities for infected patients with COVID-19. As Max Kozlov recently in a Nature article noted,² Paxlovid, initially considered a “game-changing” oral anti-viral drug, reducing severe COVID-19 cases by almost 90% if taken early after infection, has fallen victim to insufficient investments in the drug (by Pharma and government) and fear about a widely reported rebound effect, causing a return of disease symptoms (as, for example, experienced by President Biden as well as his wife). The drug is a combination of two anti-virials, nirmatrelvir and ritonavir, reducing hospitalization and death risk by as much as 89%.
Though the drug is, indeed, very effective, it cannot be taken with many other drugs and may affect taste buds, making foods taste bad. Together with the alleged, and still unexplained, rebound effect, the drug, therefore, has not been very popular. But, interestingly, there, apparently is no urge to develop other drugs to fight the virus and that is puzzling but probably financially motivated. On the contrary, monoclonal antibody treatments have been basically removed from use, leaving Paxlovid as the only realistic treatment option for already infected patients. We, therefore, do not consider the nation well-prepared for another round of more severe COVID-19.
What to do?
Which leaves us with the question, what should individuals do going forward? In principle, we advocate getting immunized and the reasoning, as noted above, is that risk-benefit considerations still favor immunization for moderate- and high-risk individuals. These considerations do include increasing concerns about serious side effects from current vaccines, including myocarditis especially in young men, thrombotic phenomena, including strokes, and others. Due to all of these risks, even if real and extremely rare, the benefits of vaccines in moderate- and high-risk populations still clearly outweigh the risks, Considerations, however, differ in low-risk patients, which basically includes all healthy, normal-weight young adults and most children. In those populations, anti-COVID vaccinations have become very questionable.
We also do not recommend universal masking. - but do recommend masking in higher-risk situations, like in medical facilities, in large indoor crowds where ventilation is poor, and, considering the significant increase in Chinese air travel, on all plane rides.
For those who plan a pregnancy or are already pregnant, we also recommend maximal vaccination, the reason being that, as noted in these pages repeatedly before, COVID-19 in pregnancy is a more severe disease than in the non-pregnant state. A recent study just confirmed this, reporting significant increases in maternal mortality and severe morbidity as well as considerable adverse outcome effects on neonates.⁵
We hope this short update on COVID-19 was helpful.

REFERENCES:
1. Callaway E. Nature 2023;613:222-223
2. Kozlov M. Nature 2023;613:224-225
3. Sachs et al., Lancet 2022;400:1224-1280
4. Relman DA. Proc Natl Acad Sci USA 2020;117(47):29246-29428
5. Smith et al., BMJ Global Health 2023;8:e009495
Continued on page 12
The V oice | f ebruary 2023 | 11 Continued from page 10
hirinG
AT THE CHR
BOARD-CERTIFIED RE-I AT ASSOC. PROF/PROFESSOR LEVEL
The CHR is looking for another senior board-certified RE-I (or international equivalent) to join our growing national and international practice. Though private, our center is organized along academic principles in that physicians are expected to excel not only as clinicians but also as researchers. The center’s uniquely structured compensation package, therefore, incentivizes both activities. We are looking for an individual with documented excellence in both areas, commensurate with associate professor/professor level. Besides a competitive salary, incentive bonus structure, and excellent benefit package, the CHR also offers partnership along either a 3-year or 5-year equity track and, ultimately, part or complete ownership, as the current leadership is expected to retire within that time-period.

If you feel qualified for the position and share our philosophy of being a physician-scientist, please let us know by submitting your C.V. and a brief letter of interest to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position can be filled immediately. All submissions are considered confidential.


TRYING TO REACH THE INFERTILITY COMMUNITY?
Have you thought about advertising in the VOICE?
This newsletter every month goes electronically to ca. 80,000 infertility patients, medical professionals in the field, and members of the media, with almost 25% (an unusually high number) also opening the VOICE.

For further information, please contact:
Ms. Alexandra Rata
(212) 994 4400 or e-mail to arata@thechr.com
ADVERTISEMENT 12 | f ebruary 2023 | The Voice
ADVERTISEMENT ADVERTISEMENT
CARDIOVASCULAR DISEASES ARE THE #1 CAUSE OF DEATHS IN PREGNANCY
Since this is the “American Heart Month,” we felt it was time to address the fact that cardiovascular diseases are the most frequent cause of maternal death in pregnancy. Because ever older women are now conceiving, often with donated eggs from younger women, we have started to see cardiovascular diseases in pregnant women - especially after fertility treatments – which, only a few decades ago, were practically unknown.
It is important to initiate this brief review by being very clear that, just because a woman suffers from a cardiovascular disease does not mean she cannot or should not conceive. A large majority of women with such disorders, indeed, can safely go through pregnancy, though there are a few conditions that are, usually, considered contraindications to pregnancy. Those are primary pulmonary hypertension and the so-called Eisenmenger syndrome, characterized by a cardiac septal defect and resulting secondary pulmonary hypertension. Some of the earliest publications of The CHR’s Medical Director and Chief Scientist, Norbert Gleicher, MD, were, indeed, on Eisenmenger
syndrome in pregnancy.1,2 In both of these conditions maternal mortality in pregnancy used to be so high that both conditions were considered absolute contraindications to pregnancy and, if pregnancy occurred, medical termination was considered indicated. But cardiac medical treatment greatly improved since the late 1990s, and now a more measured approach appears indicated. A very recent Chinese study, for example, offered new food for thought regarding pulmonary hypertension in general because these investigators were able to accumulate data on 154 affected women, a very large number for a very rare condition in pregnancy: In this study population, 3.9% had idiopathic pulmonary arterial hypertension (iPAH) 26.6%
The V oice | f ebruary 2023 | 13
had pulmonary arterial hypertension (PAH) associated with congenital heart disease (CHD-PAH), 29.2% had PAH related to other diseases (oPAH), and 40.3% had PH related to left heart disease (LHD-PH).
Only 3.2% of these women- less than 10% of what the mortality, likely, would have been in the 1990s – died within one week from delivery (this time frame is important because most deaths in association with this condition happen shortly after delivery). This number may, however, be misleading because among iPAH patients 3/6(50%) died, - a very similar number to 1990s rates. At 35.1%, ICU admissions were, overall, surprisingly low since patients with PH in the 1990s would in almost all cases have been delivered in an ICU setting. Moreover, congestive heart failure (CHF) was also unexpectedly low at 14.9%. Unsurprisingly, 70.1% of women delivered by Cesarean section, even though in the old days operative delivery was actually considered a risk factor.
As one would expect, offspring were also affected: 42.0% of pregnancies had premature deliveries; 28.6% had low birth weight, 13.0% had very low birth weight, and 3.2% had extremely low birth weight infants; 61.0% had small for gestational age infants, and 1.9% of offspring succumbed.
the Indian study were diagnosed with Eisenmenger only while already pregnant.
This potential explanation also points out one of the most important principles in the management of maternal diseases in pregnancy: Correct diagnosis before pregnancy is essential if the best outcomes are to be achieved. First diagnosis in pregnancy almost universally will produce poorer results, with two reasons contributing: First, early diagnosis allows for proper preparation of the patient, so conception can be planned when she, considering her medical problem, is in the best possible physical and mental shape. Cardiac problems are a very good example: If, for example, a cardiac patient constantly veers on the verge of CHF, this is not the time to conceive. Indeed, acute CHF is also considered a contraindication for pregnancy. But once a woman’s hemodynamics have been appropriately controlled, she will be in a much safer condition to conceive.
THOUGH THE NUMBERS OF IPAH PATIENTS WERE RELATIVELY SMALL, THE FACT THAT THEY EXPERIENCED SO MUCH HIGHER MORTALITY THAN OTHER FORMS OF THE DISEASE, LED THE AUTHORS TO THE RECOMMENDATION THAT, IN IPAH PATIENTS, PREGNANCY
A second reason is that medical treatments will always be better if the need for treatment is expected than when it comes as a surprise. In other words, it is, of course, always better to be prepared than to be surprised.
Though the numbers of iPAH patients were relatively small, the fact that they experienced so much higher mortality than other forms of the disease, led the authors to the recommendation that, in iPAH patients, pregnancy should, still, be considered as contraindicated. However, without explicitly saying so, this also means that in other conditions accompanied by PH, including Eisenmenger syndrome, pregnancy may be considered. Another very recent study, this time from India, however, in a much smaller group of 12 pregnancies with Eisenmenger syndrome reported a 37% maternal mortality rate in the postpartum period,4 - not very different from rates reported in the 1990s. This much higher mortality in this group than in the Chinese study may be due to the fact that almost 80% of patients in
If these ground rules are followed, most women with cardiovascular problems will sail safely through pregnancy, - even if older. They, of course, should be managed by a team made up of gynecologists, infertility specialists, perinatologists, neonatologists, anesthesiologists, and, of course, cardiologists that, is ideally assembled before the patient conceived. The responsibility for the assembly, therefore, usually falls on the patient’s general gynecologist or fertility specialist. Suffice it to say, cardiac patients should deliver in a tertiary medical center with ICU and advanced neonatal care, at which all members of the assembled team have privileges.
REFERENCES
1. Gleicher et al., Obstet Gynecol Surv 1979;34(10):721-741
2. Gleicher N, Jaffin H. N Engl J Med 302(13):751-752
3. Lv et al., BMC Pregnancy Childbirth 2023;23(1):16
4. Sharma et al., Cardiol Young, 20231-5. doi: 10.1017/ S1047951122004152. Online ahead of print.
“ “ 14 | f ebruary 2023 | The Voice Continued from page 10
SHOULD, STILL, BE CONSIDERED AS CONTRAINDICATED
https://www.centerforhumanreprod.com/contents/video-gallery


hirinG

EMBRYOLOGY LABORATORY SUPERVISOR FOR RESEARCH
The CHR is searching for a candidate for the newly created position of Embryology Laboratory Supervisor for Research. The CHR’s embryology laboratory, under a single laboratory director, is in the process of being reorganized into three distinct areas with separate supervisory responsibilities:


(i) clinical, (ii) administrative, and (III) research.
Supervisors in all three areas must hold PhD degrees (or equivalent) and be fully trained human embryologists with sufficient historical professional experience to hold a supervisory position.

While such human embryology experience is preferred for this new position as well, priority qualifications are a record of excellence in reproductive biology research, documented by publications in prestigious peer-reviewed journals and, in absence of human IVF experience, at least substantial animal IVF experience allowing for relatively quick in-house training in human IVF.
Besides a competitive salary and benefit package, the CHR also offers in this position a unique financial incentive-structure linked to the success of the center’s research activities, as demonstrated by publications in prestigious peer-reviewed journal. Moreover, this position will also be eligible for the opportunity to earn shared ownership in research-driven new start-up companies and the center itself.
If you feel that you qualify for this position, please submit your CV and a brief application letter to the CHR’s COO, Ms. J. Tapper, at jtapper @thechr.com. The position is available immediately. All submissions are considered confidential.

AT THE CHR ADVERTISEMENT Learn more by accessing our library of educational videos: The V oice | f ebruary 2023 | 15
for Human Reproduction ADVERTISEMENT ADVERTISEMENT
Center
Research at the CHR has for years made important contributions to our understanding of the human ovary especially as related to the changes that occur during maternal aging. Among the projects CHR has engaged in are ones designed to get a glimpse into why oocytes from older women seem to have become impaired in their ability to mature and/or correctly fertilize and develop as embryos. While the field of reproductive medicine continues to focus on chromosome misbehaviors to explain age-related problems, we at CHR continue to see this as a problem of the ovarian follicle and its various cellular components. Accordingly, many studies at CHR use granulosa cumulus cells taken from patients to explore various parameters of cell function. This image is an example of what a patients cumulus cells look like after a few days in culture and reveal to us defects in nuclear structure as shown by the blue stained objects in this field of view.
DR. ALBERTINI’S
Photo Gallery
As we pass through the COVID pandemic not entirely unscathed, we find reasons to regain a sense of optimism that will carry our collective efforts to bring the dream of family building to our patients here at CHR. Among Professor Albertini’s interests has been gaining a deep understanding of what makes an oocyte the most highly potentiated, and likely the largest, of all the cells in the human body. Using a variety of microscopic techniques, his work at the CHR has brought to light many fine details of human oocyte structure such as the one shown here. In this case, an immature GV stage human oocyte has been stained with a fluorescent dye to label mitochondria represented as the fine particles seen within this oocyte but also within and at the surface of the zona pellucida. When filters are adjusted on the CHR imaging system to view this living oocyte, both the signal conveyed by the mitochondria (yellow speckles) and the red halo appear creating this visual effect.
Patients know well that once they receive word from the nurse coordinator that they should take their trigger injection, the next day will be a telling one when they will receive word from the embryologists as to how many and of what quality their retrieved eggs were. This image typifies what the embryologists will be looking for at the time of egg retrieval. Again, CHR research has been attempting to classify egg quality prior to removal of the surrounding cumulus cells owing to our personal recognition of how important these cells are to the overall quality of oocytes. This image taken at the CHR reveals the oocyte in the center of the expanded cumulus mass and our ongoing research efforts are making headway towards understanding just what factors and molecules cumulus cells are providing to the oocyte that will improve a patients chances of becoming pregnant.


 Image 2
Image 3
Image 2
Image 3
16 | february 2023 | The Voice
Image 1
MY A OF
PIECE MIND

How do we protect ourselves from medical misinformation?
 By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.
By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.
In last month’s issue of The VOICE, I addressed how and why patients often are misinformed, and how that can be prevented. This month’s subject is related, - but affects a much wider audience because it is general medical misinformation, of course, also –and maybe primarily - including us physicians and other health care providers, often being the source of such misinformation. The impetus for this column came from a very brief one-page article in Nature Medicine1 by Carl T. Bergstrom, PhD, a theoretical and evolutionary biologist, and professor of biology at the University of Washington and, with Jevin D. West, PhD, associate professor in the Information School at the University of Washington, co-authors of the astutely named book, “Calling Bullshit,” The Art of Skepticism in a Data-Driven World [2020, Penguin Random House].

on page 16
Continued
The V oice | february 2023 | 17
The introduction to this book, indeed, is also a good introduction to this column and goes like this: “It’s increasingly difficult to know what’s true. Misinformation, disinformation, and fake news abound. Our media environment has become hyper-partisan. Science is conducted by press release. Startup culture elevates bullshit to high art. We are fairly well equipped to spot the sort of old-school bullshit that is based in fancy rhetoric and weasel words, but most of us don’t feel qualified to challenge the avalanche of new-school bullshit presented in the language of math, science, or statistics.”
With so-far 5,989 citations, the book has revealed an obviously growing need for discussion of this subject, and Bergstrom now offered a shortened summary in his recent paper, entitled “Eight rules to combat misinformation.” 1

If the tone and sentiment expressed here will appear familiar to readers of The VOICE, it is no accident because last month’s issue’s literature review started with the discussion of another brilliant piece of writing from three European scientists who had coined the term “health nonsense” for much of the current medical literature that suffocates medicine with misinformation.2 Whether “health nonsense,” or even “bullshit,” the intensity of name-calling for the degree of misinformation that is permeating medicine nowadays appears to suggest that a critical mass may finally have been reached, and scientists are, finally, taking a stand.
Though not in equally harsh language, here at the CHR, we, of course, have expressed similar opinions about “groupthink” and misinformation in reproductive medicine for a good number of years. Largely because the medical literature no longer controls medical practice, what to do about it has, however, remained unresolved. What overwhelmingly does control medical practice these days, on first impression, appears to be the Internet (Mr. Google) and social media. But they too, do not really exert control; that honor goes to corporate might, represented by industry, large hospital networks, medical insurance companies, and of course, Big Pharma and Wall Street, which all use the Internet and social media not only to influence the public but, in association with economic incentives and disincentives, also physicians (and other medical providers) and their professional organizations. There are good (economic) reasons why our professional organizations have not taken a firmer stand against the increasing utilization of preimplantation genetic testing for aneuploidy (PGT-A), for example. Just look at which companies nowadays have the biggest exhibition spaces at their annual meetings. Replaced by the genetic testing industry and rapidly growing investor-financed IVF clinic networks, it no longer is Big Pharma. The genetic testing industry and IVF clinic network are, of course, also the biggest benefactors of PGT-A overuse.
“Replaced by the genetic testing industry and rapidly growing investor-financed IVF clinic networks, it no longer is Big Pharma. The genetic testing industry and IVF clinic network are, of course, also the biggest benefactors of PGT-A overuse.”

Nobody these days seems to have any more time (or attention span) to read medical journals, even though even prominent journals now offer brief summaries. Even abstracts appear to have become too long reading for our short attention spans. We all are increasingly left consuming summaries of summaries and, consequently, becoming dependent on who summarizes and interprets papers for the next level of diminution. Not only are we, therefore, unable to evaluate the quality of the original information but we are also losing the ability to assess quality by entering a social echo chamber of constantly self-reinforcing opinions, without having the practical and intellectual resources to even question the message. Consequences then follow automatically: We physicians lose control of the message and become followers rather than leaders, ultimately controlled by the P.R. process of major economic interests.
Bergstrom in his brief communication appears hopeful that there are still enough colleagues out there in the medical-scientific universe to right the ship. For those who still write and read, he offers eight rules to combat medical misinformation: (i) Be aware of the environment into which we release information. (ii) Avoid hype and tenuous claims of significance. (iii) Recognize the importance of visualization in making figures stand on their own. (iv) Try to envision and head off in advance abuses of one’s findings, (v) If submitting an unreviewed preprint, consider its reception by the public. (vi) Take responsibility for any press release regarding your work. (vii) Interact responsibly with traditional
Continued on page 17
Continued from page 15 18 | february 2023 | The Voice
Continued from page 16
media by helping them understand the material. (viii) Do engage on social media, even though it can be complex, and be realistic by recalling Brandoline’s asymmetric principle: “The amount of energy needed to refute bullshit (here is the word again!) is an order of magnitude larger than to produce it.”

I must acknowledge being more pessimistic than Bergstrom about the future of medicine. I, indeed, have come to believe that medicine is in the midst of a “revolution,” with medicine as we knew it becoming a phantom of the past. From a physician-driven profession, medicine is changing before our eyes into a management-driven industry, not different from other major industries. The consequences, of course, are clear: an increasing depowering of physicians and, therefore, a radical change in the patient-physician relationship. How, for example, can the current physician-patient relationship be maintained, if medical insurance companies and or clinic network administrators can tell physicians how to treat patients and which medications to prescribe?
The depowering of physicians within medicine started several decades ago in hospitals and pharma companies, where physician leadership was increasingly replaced by professional managers. It continued with the increasing power of ever larger medical insurance companies and quickly growing hospital networks in determining which medical treatments physicians could or could not prescribe, and more recently expanded with the increasing success of investor-driven clinic networks, where administrative-economic interests, ultimately, often win over strictly medical considerations.3, ⁴ As a consequence, we have reached a point in the U.S., where, for the first time, a majority of physicians are employed.5
I am, therefore, skeptical whether Bergstrom’s eight rules can really make a significant difference in our new, almost apocalyptic world of medical misinformation. Moreover, I, of course, have here interpreted and abbreviated Bergstrom’s eight rules and, therefore, potentially misinformed readers of this column. But then our readers always have the option of reading the original article because it is referenced.1 His paper is also briefly discussed in the Literature Review Section of this issue of The VOICE.
REFERENCES:
1. Bergstrom CT. Nat Med 2022;28:2468
2. Stein et al., BMJ 2022;379:02932
3. Patel et al., JAMA Ophtalmol 2019;137(6):601-602
4. Geyman J. Int J Health Serv 2022;207314221134041
5. https://www.ama-assn.org/press-center/press-releases/ ama-analysis-shows-most-physicians-work-outside-pri vate-practice

hirinG
EMBRYOLOGY LABORATORY SUPERVISOR FOR RESEARCH
The CHR is searching for a candidate for the newly created position of Embryology Laboratory Supervisor for Research. The CHR’s embryology laboratory, under a single laboratory director, is in the process of being reorganized into three distinct areas with separate supervisory responsibilities: (i) clinical, (ii) administrative, and (III) research.
Supervisors in all three areas must hold PhD degrees (or equivalent) and be fully trained human embryologists with sufficient historical professional experience to hold a supervisory position.

While such human embryology experience is preferred for this new position as well, priority qualifications are a record of excellence in reproductive biology research, documented by publications in prestigious peer-reviewed journals and, in absence of human IVF experience, at least substantial animal IVF experience allowing for relatively quick in-house training in human IVF.
Besides a competitive salary and benefit package, the CHR also offers in this position a unique financial incentive-structure linked to the success of the center’s research activities, as demonstrated by publications in prestigious peer-reviewed journal. Moreover, this position will also be eligible for the opportunity to earn shared ownership in research-driven new start-up companies and the center itself.
If you feel that you qualify for this position, please submit your CV and a brief application letter to the CHR’s COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available immediately. All submissions are considered confidential.

ADVERTISEMENT
AT THE CHR ADVERTISEMENT The V oice | february 2023 | 19

20 | february 2023 | The Voice ADVERTISEMENT


Continued from page 20 The V oice | february 2023 | 21
CHR Publications
Barad DH, MD., PGT-A “perfect” is the enemy of good. J Assist Reprod Genet 2022;40:151-152
This is the second month in a row that The CHR’s Clinical Director of IVF, Director of Research, and Senior Scientist, David Barad, MD, published an invited commentary (by the editors) in a leading medical journal in the field regarding a PGT-A paper published in the same issue of the journal, this time The Journal of Assisted Reproduction and Genetics (JARG), in more detail discussed in our monthly literature review section.1 While last month’s commentary in Fertility & Sterility Reports reflected on the transfer of embryos, by PGT-A reported to be “abnormal,” this month’s commentary in JARG addresses more fundamental aspects of utilization of PGT-A in IVF practice.
In very clear and easily understandable language, Barad explains extremely well why routine utilization of PGT-A in IVF does not make much sense. Though a small group of best-prognosis patients with, anyhow, best pregnancy chances may gain a small additional benefit from PGT-A, a vast majority of patients derive absolutely no outcome benefits, and many, indeed, will reduce their pregnancy and live birth chances by utilizing PGT-A. We have not read or heard the explanation for these conclusions ever expressed with more clarity than in this short commentary and, therefore, recommend it to everybody interested in the subject.

Like any CHR publication, we gladly will send you upon request a reprint. Please address reprint requests to melias@thechr.com
REFERENCES:
1. Kucherov A, et al., J Assist Reprod Genet 2023;40:137-149
CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR CHR
22 | february 2023 | The Voice
QUESTIONS PATIENTSASK
How do cortisol levels affect fertility and infertility?

Cortisol is one of several hormones produced by the adrenal glands, sitting on top of both kidneys. Adrenals produce several families of hormones under regulation of a pituitary hormone called adrenocorticotropic hormone (ACTH). These groups of hormones are derived from three so-called zonae and an area called the hilus of the adrenal gland.

Cortisol, a steroid hormone, is the main product of the zona fasciculate (zF), which produces the so-called glucocorticoid hormones (also called corticosteroids) and is the body’s main stress hormone. In other words, adrenal glands produce the hormone cortisol in response to stress. But, like every producer of a product, adrenals can produce only so much of this stress hormone. If stress is too severe and/ or lasts for too long, the adrenals may, simply, run out of cortisol and adrenal glands may become insufficient (i.e., cortisol may become abnormally low or can almost completely disappear). Some physicians use the term “adrenal fatigue” to describe milder cases of adrenal insufficiency, while others strongly dislike the term and consider it misleading and inappropriate.
Cortisol has multiple roles to play: It to a degree controls blood sugar levels, supports the breakdown of carbs, proteins, and fats, affects blood pressure (high levels raise blood pressure), suppresses inflammation (i.e., is an excellent suppressor of the immune system), is involved in the regulation of the sleep-wake cycle, and raises glucose in response to stress.

The other two zonae are the most outer zona glomerulosa (zG) and most inner zona reticularis (zR), adjacent to the hilus of the adrenals. The zG produces the so-called mineral-corticosteroids, with the principal one being the hormone aldosterone which is essential in the control of bodily fluids by causing water retention, increasing the sodium in the GI tract, and disposing of excess potassium through urine. Finally, the zR produces androgen hormones, all in roughly 50/50 partnership with ovaries, except for one androgen hormone, DHEA-S, which is only produced by adrenals.
There is one additional characteristic of the adrenals of potential importance, though not widely known even among fertility specialists: Ovaries and adrenals share a common embryonic primordium. In other words, ovaries and adrenal glands are derived from the same
Continued on page 20

The V oice | february 2023 | 23
stem cell lineages. This, of course, can have major relevance to female infertility but has hardly been explored yet. Another widely unknown fact is that adrenals after ovaries, have the highest density of AMH-hormone receptors. The presence of hormone receptors in a tissue usually denotes a function for this hormone in this tissue. While AMH of course, has major functions in ovaries, no function on adrenals has been, however described so far.
The only direct function the adrenals so far have been demonstrated to exert on ovaries is through their androgen production by the zR. Interestingly, as mostly only the CHR’s investigators have reported, the frequently observed hyperandrogenism in infertile women in association with various infertility diagnoses,1-3 almost universally is due to adrenal rather than ovarian androgen insufficiency and has become the basis for androgen supplementation for many female infertility patients.
But as noted before, all the adrenal zonae are under ACTH control, it, therefore, should not surprise if low adrenal androgen production may also be accompanied by dysfunction in the other two zonae. And the CHR’s investigator, indeed, in 2016 reported that infertile women with low functional ovarian reserve, who almost uniformly are hypo-androgenic,3 also demonstrate a degree of hypocortisolims.4,5
Coming back to the immune-suppressive effects of corticosteroids, they, of course, represent a mainstay of medical treatments with all kinds of hyperactive immune systems, from long-term asthma treatments in inhalers to autoimmune diseases and inflammatory diseases as well as allergies. But when we receive treatment with corticosteroid and levels,
therefore, rise in our bodies, a message gets back to the pituitary gland (a so-called “feed-back”) that says, enough ACTH already As ACTH stops stimulating the adrenals, androgen production can stop, as we recently saw in 2 infertile women who came to The CHR after years of failed IVF cycles in multiple centers and having been labelled as suffering from “unexplained infertility.” Both were on long-term corticosteroid treatments and fully recovered, once taken off steroids and supplemented with DHEA to raise their testosterone levels back into a normal range. (A paper describing these two cases was just submitted for publication).

One final point on cortisol measurements: they should be obtained early in the morning because levels rise after 10 am.

REFERENCES
1. Gleicher et al., Endocrine 2021;72(1):260-267
2. Gleicher et al., Endocrine2018;59(3):661-676
3. Gleicher et al., Hum Reprod Hum Reprod 2013;28(4):1084-1091

4. Gleicher et al., Reprod Biol Endocrinol 2016;14:23
5. Gleicher et al., J Steroid Biochem Mol Biol 2016;158:82-89
Can we prevent the transmission of infections from mother to fetus?


This, is indeed, a very interesting question that does not allow for a simple yes or no answer. In principle, the placenta protects the fetus and most infectious agents will not be transmitted during pregnancy. Yet, there are exceptions. For example, the SARS-CoV-2 virus, in principle, does not cross from mother into the fetus; but a handful of cases have been reported where this, nevertheless, happened. Such cases are believed to occur when the placenta is damaged and, therefore, no longer can maintain size-filtration.
That maternal bacterial infections move during pregnancy into the fetal department, therefore, is in principle very rare. But here, too, are exceptions: Listeriosis is such an example. Listeria monocytogenes is a bacterium that in mammals acts as an intracellular parasite. Humans usually become infected through contaminated food items. The bacterium appears to have specific affinity to trophoblast (placenta) and amniotic fluid and, after infecting the amniotic cavity, will not only induce pregnancy loss but can lead to a life-threatening septicemia in the mother.1,2
Another devastating example presented itself several years ago with the Zika epidemic in Brazil when thousands of microcephalic newborns bore evidence for a virus’s ability to cross the placental barrier and cause severe damage in the fetus. Another example is Toxoplasmosis, transmitted from cat litter and, of course, several more. Once a mother is infected by an organism with the ability to overcome the placental barrier to cause a cross-infection, we usually have few, if any, treatment options left.

Continued from page 19 Continued on page 21 24 | february 2023 | The Voice
Interestingly, this is, however, not the only way, how offspring can get infected by the mother. A likely much more frequent occurring way of causing infections in newborn is through passage of the maternal (infected) birth canal. This is how hepatitis and other viral diseases were routinely transmitted from mother to offspring, Such contaminations can be avoided by cesarean section or, even more cost-effectively, often through timely vaccination of mothers whose humeral immunity in form of antibodies is passed through the placenta to the fetus and renders him/her immune. We witnessed during the COVID-19 pandemic how vaccinated mothers gave birth to offspring with anti-COVID-19 immunity.
REFERENCES
1. Quereda et al., Virulence.2021;12(1):2509-2545


2. Dunphy et al. BMJ Case Rep 2022;15(10):e249989
Embryoscope time-lapse systems, - do they work?
Almost a decade has passed since the concept of constant visual monitoring of human embryos entered clinical embryology with the first “embryoscope” coming to market. As so many other hypotheses, the IVF field immediately embraced the idea under the believe that constant observation of embryos during development from single cell (zygote) to transferrable embryo (usually at blastocyst-stage), without doubt, would finally allow for selection of “best” embryos from among a cycle’s cohort of embryos and, therefore, improve IVF outcomes. But, as with so many hypotheses that have since 2010 been implemented in IVF prematurely and without proper validation studies, to almost everybody’s

– except The CHR’s – surprise, the experiment failed: To this day, not a single study in the medical literature has been able to demonstrate valid outcome benefits from continuous visual observation of embryos during their life in the embryology laboratory.1-4
Despite early warnings about prematurely implementing this concept into routine embryology,5 the utilization of time -lapse systems in embryology laboratories, nevertheless, exploded, indeed, resulting in inclusion of this concept into the growing list of useless (and sometimes even harmful) so-called “add-ons” to IVF that have been littering the IVF landscape sine 2010. As always, and as has been our practice for many years, The CHR acted more cautiously and, before purchasing the required equipment, first, decided to test it out. Testing out changes in how The CHR manages its clinical and embryology practice are always made only very carefully and, usually, only after internal pilot studies. This has been policy at The CHR for many years because we learned years ago that what works in many other IVF centers with very different patient populations, often, does not work at The CHR, with its much less-favorable prognosis patients.
Testing the earliest embryoscope model that had come to the market for several months in two distinct patient populations, - young egg donors and our regular poorer-prognosis infertility patients, we were rewarded for our caution because we, very early, learned that, considering The CHR’s patient population, we would do better continuing traditional embryology than switching to the new closed incubation systems with time-lapse monitoring.6 More specifically, in poor-prognosis patients outcomes were identical between both approaches but, to our great surprise, we learned that the new system doubled embryology staff-time, while proponents of the system were marketing it with, actually, exactly the opposite claim. Moreover, when embryos produced with young donor-eggs were randomized to closed and standard incubation, morphologically embryos cultured manually gave much better results.
This does not mean that time-lapse systems have no use; they, of course, do because they clearly have added to our knowledge about how embryos behave between zygote- and blastocyst-stages and, therefore, are valuable research instruments. We, however, do not use them in The CHR’s clinical embryology laboratory for routine culture of embryos and continue in that regard to trust in the manual work of our excellent embryology staff.
REFERENCES
1. Polanski et al., Ultasound Obstet Gynecol 2014;44(4):394-401

2. Goodman et al. Fertil Steril 2016; 105(2):275-85.e.10
3. Bhide et al., Hum Fertil (Cambridge) 2017;20(2):74-79
4. Reignier et al., Reprod Biomed Online 2018;36(4):380-387
5. Armstrong et al., Hum Reprod 2015;30(1):3-8
6. Wu Y-G. Reprod Biol Endocrinol 2016;14(1):49
Continued from page 20 The V oice | february 2023 | 25

26 | f ebruary 2023 | The Voice ADVERTISEMENT
the chr’s interpretation of RECENT LITERATURE, relevant to REPRODUCTIVE MEDICINE
Mostly placed into a clinical context, we in this section of the newsletter offer a survey of articles in the English literature, usually published in the preceding month, which the CHR found of interest to the current practice of clinical reproductive endocrinology and infertility, - even if at times not immediately applicable to daily clinical practice. These articles, however, nevertheless often point out where clinical practice will likely go and, therefore, serve an important translational purpose. Translational research has been the CHR’s principal research goal since its founding in 1981, has produced a significant number of U.S. patents over the years, and has propelled the CHR into its current position as a worldwide center of last resort for infertile patients who have failed treatments elsewhere.
The business of infertility
Continuing consolidation of IVF clinics in the U.S.
Griffin Jones, founder and owner of Fertility Bridge, 1 offered interesting reading in two recent e-mails to fertility centers. In a first on January 12, 2023, Rachel Leland reported that the U.K.’s largest fertility clinic network, CARE Fertility, made its first clinic purchase in the U.S. by buying the former Integramed (which in 2020 declared bankruptcy and was liquidated) clinic REACH in Charlotte, NC. Though financial conditions are not known, experts estimated that the purchase price was, likely, in the “low double-digit of EBITDA.”
In a second e-mail from Griffin Jones on January 19, 2023, an even more interesting article by Michael Barbella summarized the rapid consolidation that is taking place among fertility centers in the U.S. If interested in reading both of these reports, we suggest that you contact Griffin Jones directly via his company’s e-mail.2 Since he offers a stream of steady insights into the infertility field, it may be worthwhile joining his mailing list.
The report notes that at least 25 fertility clinics were sold during 2022, listing them and their respective buyers. The report also notes
Continued on page 28
that, after an initial post-Covid boom, patient care volume in the field declined in later 2022, resulting in a decline in valuations from buyers and more risk aversion. Overall investors in the field, however, remain very optimistic, expecting the global market for IVF services to increase by 37.5% by 2028, reaching a whopping US$36.25 billion.
Here are some further “pearls” from the report: Through the purchase of the Vios Fertility Institute founded by Angeline Beltos, MD, Kindbody became a “unicorn,” reaching a $1.15 billion valuation (roughly a third of the sales price IVI/RMANJ recently fetched).3 After this purchase, Kindbody now owns 26 clinics and offers in-house genetic testing through Phosphorus Labs, its own surrogacy agency through Alternative Reproductive Resources, and financing options for patients, as we briefly reported in the January issue of The VOICE.
The Prelude Network, currently owned by Inception Fertility, which has been following a similar vertical integration strategy, continued its expansion into the Canadian market by purchasing a second center, this time in Alberta. Interestingly, the report, however, noted that, according to Axios, Lee Equity Partners is seeking a buyer for the company, representing
The V oice | f ebruary 2023 | 27
somewhat of a deviation from the, overall, very optimistic acquisition attitude that prevails in the field.
Lee Equity Partners were among the first investors in the fertility field when funding serial entrepreneur Martin Varsavsky in 2015 with US$ 200 million to start Prelude. 4 Their decision to sell may be just a reflection of standard equity investing strategies, usually limited to only several years. As currently very high valuations in the industry, at least for the foreseeable future, have likely reached their peak, this may, indeed, be the right time to sell.
On the other hand, considering above noted slowdown in the field in the latter half of 2022 and persistent rumors in the industry of almost uniformly disappointing profitability, Lee Equity Partners’ apparent desire to exit the field, may be a warning signal that widely held business expectations about the infertility field have been too optimistic. Of course, only the future will tell; we clearly live in interesting times when it comes to the business of infertility,
REFERENCES
1. https://www.linkedin.com/in/grifjones
2. griffin@fertilitybridge.com
3. https://www.fiercehealthcare.com/digital-health/ kindbody-hits-unicorn-status-vios-fertility-institute-acquisition-new-lead ership
4. https://www.forbes.com/sites/miguelhelft/2016/10/17/prelude-fertili ty-200-million-startup-stop-biological-clock/?sh=5b6c5f417260
What is going on with the conference business in infertility?
The COVID-19 pandemic, of course, practically terminated all traditional conference activities for almost two years, literally overnight popularizing the virtual “electronic conference” which, without the need for travel, and in most cases for free, can be attended from one’s office or even bed. Unsurprisingly, attempts at returning to traditional “attendance conferences” have, therefore, been experiencing significant headwinds, as generally disappointing lower attendance numbers during 2022 clearly demonstrated.
The ASRM’s January 13, 2023, announcement that the annual “2023 Best of ESHRE and ASRM” joint conference (usually alternating between a European and U.S. location) on March 2-4, 2023 in Orlando, FL, because of insufficient numbers of registrants had been cancelled,1 nevertheless,
came as a shock. On further consideration, the ASRM, as this year’s organizer, should, however, have demonstrated more foresight in how the meeting was prepared. After all, the experience with many other scientific conferences during 2022, including the annual ASRM meeting (this year in Anaheim, CA), and, despite claims to the contrary also characterized by very poor attendance (a very prominent invited plenary speaker on the last day of the meeting had an audience of 4 (!!) in an auditorium for over 1,000 attendees) flashed clear warning signals.
But those warning signals were, quite obviously, overlooked. A conference that really offered no good reason to pack up bags and travel to Orlando, therefore, had to be cancelled. Just announcing a conference is, thus, no longer good enough, - not even for ASRM and ESHRE, the two largest professional societies in our specialty in the world. Registrants must be given good reasons to make the effort and spend the money.
All, of course, still starts with the content of the conference: What are the subjects? Who are the speakers? Will I gain new knowledge, or will I hear more of the same? Is information provided objectively, or is it still the frequent “echo chamber,” more driven by industry interests and personal relationships in choosing speakers and topics than the need to know about new developments in basic science and their potential translational clinical applications, and diversity of opinion? And then one, of course, also has to consider the social factors, starting with the chosen venue city. Is Orlando really an interesting enough place to visit? Do attendees of a state-of-the-art conference really want to go to Disney’s Magic Kingdom or Universal Studio after all day sitting in lectures? We sincerely doubt that!
The size of conferences also matters. Do we really all day long want to speed along endless convention center corridors from one lecture room to the other? Again, we don’t think so. Instead, we want to learn, to have the opportunity to discuss things with colleagues, and yes, want the opportunity to question so-called authorities to find out whether we can really trust them. Not only among the lay population, the COVID-19 pandemic has also done almost irreparable damage to the reputation of the medical-scientific establishment. Physicians as of this point often do not feel very differently. If so-called “authoritative voices” in medicine, therefore, want to recoup some of the during the COVID-19 pandemic lost good-will, they must be ready to face immediate inquiry from an audience, which is one thing virtual conferences, still, cannot do well.
We want to be challenged to think critically and that does not happen in long hallways
Continued from page 27 28 | f ebruary 2023 | The Voice
but in single rooms where the attendees of a conference are given the opportunity to question speakers and to hear the questions and concerns of peers. In other words, the format of conferences must change if we want to attract attendees. There really are only two remaining motivations for travel to medical conferences that electronic attendance in a medical conference cannot offer, - previously noted immediate interaction with speakers and colleagues and the social experience of meeting up with colleagues from other places and having a good time.
And here is a little self-promotion: Suffice it to say, after a three-year COVID-19 break, the again resurrected annual 2023 FOUNDATION FOR REPRODUCTIVE MEDICINE CONFERENCE (FRMC), co-sponsored by the CHR, fulfills all of these needs. Like always taking place in wonderful pre-Christmas New York City (this year on December 1-3, 2023) only a few blocks from its world-famous Christmas tree at Rockefeller Center on Fifth Avenue, which will be lit for the first time the evening before the Conference start, it addresses the most relevant topics in translational reproductive biology and clinical reproductive endocrinology under the main motto, “think differently!” Experiencing the Conference will in three days confront attendees with the most complex clinical issue in the field and, at the same time, offer updates on the underlying state-ofthe-art science, - all presented by many of the world’s leading experts who are not afraid of being confronted by their audience.
REFERENCE
1. https://www.sart.org/news-and-publications/news-and-research/announce ments/2023-best-of-eshre-and-asrm-cancellation-announcement/#:~:tex t=It%20is%20with%20a%20heavy,March%202%2D4%2C%202023.General medical importance
Where has the physician authority gone in medicine?
This newsletter has in recent months repeatedly addressed the steady decline in physician authority over the practice of medicine. It, therefore, is good to see that we are not alone in decrying this development for its adverse impacts on the quality of care. We, therefore, found two recent papers in JAMA of interest because, both, addressed unionization of the medical profession as, likely, the only remaining remedy for physicians to maintain at least some measure of influence over how medicine is practiced. A first paper, describing trends in labor unionization among U.S. healthcare workers in general1, offered the opportunity for a well-written and even more interesting accompanying editorial by a lawyer (Duke University, NC) and a physician (Stanford University, CA) under the title, “Restoring Physician Authority in an Era of Hospital Dominance.”2
The authors note that, even though currently only 6-8% of physicians currently are union members, “given the changing power dynamics between physicians and health care administrators, unions might provide attractive opportunities for physicians to improve their status while also improving the health care system.”
This article is, of course, not the first to acknowledge the increasing loss of physician authority within the medical field. There, indeed, is no better confirmation than the fact that over the last decade alone,
the percentage of non-physician-owned medical practices has grown substantially: While in 2012 60.0% of medical practices were physician-owned, by now 52.1% of physicians are employed by hospitals and 21.8% by other corporate entities.2 Becker’s Hospital Review, indeed, recently reported that UnitedHealth Group has become America’s largest physician employer.3 Most large healthcare insurance companies now, indeed, own healthcare delivery units, as the article also notices, potentially further threatening the clinical autonomy of physicians.
In other words, private medical practice is dying in the U.S., the alleged beacon of capitalism. That the proposed response to this development and the suggested solution is the unionization of physicians, further demonstrates the generational shift in thinking among physicians especially over the last two decades, away from being a spiritually independent profession made up of fiercely individualistic physicians, to more or less, a generation of medical practitioners comfortable with (by others) set employment rules (and, therefore, by others determined medical practice patterns), willing to forego the potential for higher income in return for a secure paycheck and work hours that allow for a satisfying social life.
Whether this is a purely generational shift is, however, doubtful because we have not witnessed similar developments in finance (Wall Street) and especially not among start-up companies. However, what nobody is talking about is the fact that medicine used to attract top college graduates. Approximately three decades ago that started to change, when Wall Street became their first choice, - just to be replaced in more recent years by the promises and the excitement of start-ups.
One, therefore, could very well argue that the unionization of physicians will not restore physician authority in health care. What would do it, however - though much more difficult to achieve –would be a way to make medicine again more attractive to top students in college classes. But, as we do not see that happen, would we, still, want our children and grandchildren to become physicians?
REFERENCES
1. Ahmed et al., JAMA 2022;328(24)2404-2411
2. Richman BD, Schulman KA. JAMA 2022;328(24):2400-2401
3. https://www.beckerspayer.com/payer/meet-americas-largest-employ er-of-physicians-unitedhealth-group.html
Are government subsidies for IVF a solution for low birth rates?
For many years Israel has been the country with the by-far largest number of IVF cycles per capita of the population. The very obvious reasons have been unusually generous government subsidies for IVF cycles, covering almost unlimited cycle treatments until women have successfully delivered three children. The publicly stated motivation for these to this point, elsewhere unprecedented, and unusually generous subsidies for IVF has been the government’s desire to increase the country’s population.
The V oice | f ebruary 2023 | 29 Continued on page 30
As The New York Times now, however, reported on January 22, 2023, China has picked up on the idea.1 Having just experienced the first year since the Cultural Revolution in which the country’s population shrunk, China’s government is, very obviously, becoming concerned about significant declines in birth rates and a quickly aging population. According to the article, China promised at least one IVF center for every 2.3 -3.0 million citizens by 2025. Serving a population of approximately 1.4 billion, the country has currently only 539 IVF clinics, a number barely larger than the number of U.S. IVF centers with a population of less than 400 million; yet these Chinese centers already perform over 1 million IVF cycles annually, triple the numbers of IVF cycles in the U.S.
Since Chinese women, simply, don’t want to have more children, though potentially helpful, experts agree that this initiative will not solve China’s insufficiently slow population growth. Having abandoned its decade-long “one-child policy” for already several years, first advocating two, and more recently three children per household (as has been Israel’s policy), the success of recently announced subsidies for IVF in China will have to be seen. The big difference between Israel and China regarding this issue is not how the subsidies are offered but that Israel’s women do want multiple children, while Chinese women over the many years of the “one-child policy” appear to have lost their appetite for large families.
REFERENCE
1. Stevenson A, Wang Z. Eager to subsidize I.V.F. to ease a crisis. The New York Times, January 23, 2023, ppB1&B7
Ethics
When does life start?
When life starts is a still unresolved ethical, religious, and biological question, - as old as mankind. Some religions consider life to start with the fertilization of the egg by sperm, whether that happens in vivo (in the body) or in vitro (outside the body, as in IVF). Others, consider the detection of a fetal heart as the milestone; and, yet others, consider the moment to be reached by birth. Though it is difficult to imagine how an in vitro-produced human embryo without chance of implantation can represent human life, we will, here, not resolve this question and neither did an article by Elizabeth Dias, a National Correspondent for Religion and Politics of The New York Times in a frontpage article on January 2, 2023.
The recent Supreme Court decision regarding Roe v. Wade, however, actualized the question and brought it back into the daily discussion. Considering that many states are in the midst of passing laws to replace Roe v. Wade in their states, often with the question of when life starts dominating the debate as to the gestational age at which abortions should be prohibited, it should not be surprising that the question made the front page of the newspaper.
Even though Dias, of course, cannot offer an answer to the
question, we strongly recommend this article for several reasons: First, because when life begins, indeed, is an important ethical, religious, and biological question of enormous complexity, a fact this article very well demonstrates in language easily understandable even to laypeople. Secondly, however, as Dias also notes, an answer to the question, “pushes past science.” As she correctly concludes, “it is tied to a society’s values, a person’s sense of self, and a cultural understanding of what it means to be human, requiring social choice and interrogation of our ethics.”
REFERENCE
1. https://www.nytimes.com/2023/01/02/briefing/when-does-life-begin.html
Issues of general medical importance
Are new hunger-quashing drugs harborers of a medical revolution?
On first impression, it sure looks like it, if one considers the serious consequences of obesity on human health and wellbeing,1 the billions spent on the long-term mostly unsuccessful weight loss regiments and, if one in addition adds the costs of treatments of obesity-associated/induced health problems and assumes that these new hunger-quashing drugs really can turn us again into our skinny self of younger years. Whatever area of human medicine we may consider, if we effectively can reduce the BMI of our patients, every diagnosis, and every treatment will come away with benefits from serving a less obese patient population. That obesity affects reproductive health in both sexes is, of course, understood.2,3
McKenzie Prillaman, under the heading, “The Showstopper Obesity Drugs That have Stunned Researchers,” recently offered a very insightful review of the subject in Nature magazine.4 To define the problem and outline the opportunity, she points out that worldwide obesity has tripled since 1975. By 2016 the WHO estimated that 40% of adults were overweight and 13% outright obese.
She then offers a very insightful history of how this new family of drugs, which mimic a group of hormones called incretins, which are known to lower blood sugar and curb the appetite of people. Most of the early drugs were developed for treating type 2 diabetes and, as of this point, only one or two are FDA-approved for weight loss. Yet, researchers were astonished by the speed and amount of weight loss they observed in practically all studies without almost any adverse side effects.
The story started in 1987 with the discovery of glucagon-like peptide 1(GLP-1) and its role in controlling blood sugar. In 1994, leptin was reported to keep mice lean. In 2002 the gut hormone glucose-dependent insulinotropic polypeptide (G1P) was demonstrated to prevent obesity in mice. By 2005 the FDA approves Exenatide for type 2 diabetes which targets the GLP-1 receptor. In 2014, the FDA approves the first drug targeting the GLP-1 receptor for weight loss, liraglutide (Saxenda) shown to induce approximately 8% weight loss. In 2017 semaglutide (Ozempic), a new GLP-1 drug was approved by the FDA for type 2 diabetes. By 2021 the same semaglutide, branded as Wegovy,
30 | f ebruary 2023 | The Voice Continued from page 29
was approved for weight loss after a trial demonstrated 15% weight loss. In 2022 tirzepatide (Mounjaro) was approved for type 2 diabetes, the first drug to target GLP-1 as well as GlP. It was shown to result in 21% of weight loss.
Several experts interviewed by Prillaman pointed out the symbolic importance of the success of these drugs in inducing significant weight loss, as proving that obesity was a disease and not only, as widely perceived, the inability to control one’s food urges. Others are concerned about the fact that weight, of course does not alone (or even primarily) reflect health and that the success of these drugs, therefore, may mislead the public into ignoring other important aspects of health.
As is practically always the case in medical research, progress only leads to new questions. One most often asked is, are those drugs for life if one wants to maintain weight loss? One study suggested that after one year, patients who stop treatment will regain roughly twothirds of their prior weight.5 There is still much to be learned but one thing is clear, most people struggling with their weight for almost their whole life, find it miraculous to lose 20% of their body weight in half a year by just injecting a few drops of medicine under their skin once a week. Yes, medicine still creates miracles!
REFERENCES
1. Blüher M. Nat Rev Endocrinol 2019;15(5):288-298
2. Legro RS. Fertil Steril 2017;107(4):860-867
3. Thong EP, Burden C. Semin Reprod Med 2020;38(6):333-341
4. Prillaman MK. Nature 2023;613:16-18
5. Wilding et al., Diabetes Obes Metab 2022;24:1553-1564
Wasted time and effort in medical research
Most physicians, and especially those who are not only clinicians but also pursue research, feel overextended. Demands seem to constantly increase from all directions: see more patients, get more grants, write more papers, review more papers for journals; and then, there are, of course, also the growing administrative responsibilities. Is there really a physician left who does not hate the time needed to satisfy the hospital’s EMR?
No worry, this is not yet another of these commentaries on physician burn-out which, suddenly, appear to be everywhere. To the contrary, we here want to offer advice on how not to waste our obviously very valuable time by piggybacking upon a recent article by a Dutch investigator in Nature magazine, who correctly, makes the point that, “we routinely wait until peer review -after a study has been done – to identify flaws that can’t then be corrected.”1 Coming from an academic background, he sees this as only an academic problem, solvable by, “universities ensuring that study design can actually answer their research questions.”
The problem is, however, much bigger, - it is all of our problem in how much useless “garbage” we all are producing in our research efforts. Consider the time wasted on many of the useless studies published in the literature (and with enough persistence, almost every paper, ultimately, will get published somewhere, somehow!). Just this month, among here discussed papers, how many would not have been missed by a single soul in the world if they had never seen the light of day?
Think how much time the authors (and their secretaries) would have spared; think how many fewer papers journals would have to review (and mostly reject); think how many fewer papers would end up in our e-mails as reviewers for many different journals and, finally, think about how much time we could be saving by not having to read those papers. Like great artists do not always produce masterpieces, great researchers do not always produce worthwhile papers. We all who are in this academic race for knowledge and glory should pay more attention to the fact that time is our most pressured possession. Let’s not waste it on worthless garbage and this is, therefore, a job for all of us and not only for universities.
REFERENCE
1. Lakens D. Nature 2023;613:9
Talking about research in reproductive health and disease
Continuing the conversation about research, a recent paper in eLife argued that research into reproductive health and disease is underpopulated and needs to be expanded.1 We have made this point a The CHR for many years. It is absolutely shameful how much, for example, the IVF field has grown over the decades and how little important research is performed by the field. IVF in 2023 is at most IVF centers, basically, practiced in almost exactly the same ways as 20 or even 30 years. And many changes made, especially since 2010, have not helped but hurt.2
Based on an analysis of PubMed, the authors report that the number of articles on non-reproductive organs are 4.5 times higher than articles published regarding reproductive organs. Indeed, even in the two most-researched reproductive organs,
The V oice | f ebruary 2023 | 31 Continued on page 32
the breast and prostate, the emphasis is on non-reproductive issues, mostly cancer. Moreover, grant awards in Canada, as well as the U.S., are 6-7 times higher for non-reproductive than reproductive health issues. The researchers concluded, and we quote: “There are too few researchers working in the field of reproductive health and disease, and the funders, educators, and the research community must take action to combat this longstanding disregard for reproductive science.”
REFERENCES
1. Mercuri ND, Cox BJ. eLife 2022;11:e75061
2. Gleicher et al., Hum Reprod Open 2019(3):hoz017
“The mathematics of danger”
This is how Richard Horton, for many years Editor-In-Chief of The Lancet, recently headlined one of his weekly columns. Though because of his, at times, rather radical viewpoints usually often not one of our favorite commentators, he with this column did hit the nail:1 The subject was mathematical modelling, a subject repeatedly discussed in The VOICE, especially during the early months of the COVID-19 pandemic. Modelling studies, however, also can constantly be found in specialty journals, including in reproductive medicine, frequently being treated as equals to formal studies.
What we mean by that is that, like in studies based on actual facts, the results of mathematical modelling studies, by definition are not based on facts but on assumptions. These are, however, misrepresented as facts. In quoting from a recently published book, Horton notes, “models are never only about mathematics. Assumptions and value judgments permeate every model, although they are rarely made explicit.” We better remember that when the next mathematical modelling paper tries to convince us once again about offering “the truth.” Like fiction, at times, can be more truthful than reality, mathematical modelling can, however still, be useful in medicine, - as long as we remember that it is fiction.
REFERENCE
1. Horton R. Lancet 2023;401:91
Combating medical misinformation
Maintaining a similar theme, we would like to point our readers to a commentary in Nature Medicine1 by a biologist from the University of Washington who is known as the co-author of a widely cited book on medical
misinformation, also known for its blunt language. Since this article was the impetus for CHR’s Medical Director and Chief Scientist’s “A Piece of My Mind” column in this issue of The VOICE, we, here, will not offer further detail but strongly suggest at least a quick peak at this column. Combating medical information is, of course, currently a crucially important goal for all of medicine, including in reproductive medicine, where so much misinformation is driving current clinical practice, especially in association with IVF.
It is also timely, considering that California’s new “Misinformation Law,” demonstrates exactly how misinformation in medicine should not be addressed. California’s new Assembly Bill 2098, indeed, “silences physicians and enshrines government as the monopoly on scientific truth,” as a recent article from the Pacific Legal Foundation so well explained.2 One can only hope that this absurd law will be found unconstitutional because the last thing medicine needs after COVID-19 is for governments to determine what opinions physicians and/or scientists are allowed to express.
REFERENCES
1. Bergstrom CT. Nat Med 2022;28:246
2. https://pacificlegal.org/californias-new-law-silences-doctors/?gclid=EAIaI QobChMIh_yXq9Lg_AIVz_rICh38ywX0EAAYASAAEgI4sfD_BwE
Pregnancy
Gestational age at birth affects cognitive outcomes in adolescence
Premature deliveries represent the single largest adverse outcome in obstetrical care, being the leading cause of perinatal mortality and morbidity, responsible for up to 75% of perinatal deaths.1 Moreover studies have demonstrated that early deliveries before 40 weeks were associated with long-term reduced cognitive outcomes. These studies, however, usually had not adjusted their data to potential confounders. Scandinavian investigators now, however, report a study that did exactly that and, still demonstrated cognitive impairments in children with gestational age below 34 weeks, specifically when it comes to mathematics and intelligence tests. Interestingly, they also were able to demonstrate that deficits above 34 weeks were primarily explainable by family history, and unrelated to gestational age.2
In an accompanying editorial, two Canadian colleagues pointed out that currently, likely, approximately 15 million infants are born annually under 37 weeks worldwide. Moreover, 95% of such preterm infants survive into adulthood, undoubtedly causing significant and broad consequences to societies.
32 | f ebruary 2023 | The Voice Continued from page 31
REFERENCES
1. Ananth CV, Vintzileos., Am J Matern Fetal Neonatal Med 2006;19(12):773-7782
2. Husby et al., BMJ 2023;380:e072779
3. Ahmed A, Yang A. BMJ 2023;380:p70
Reproductive Endocrinology & Infertility
We, in recent issues of The VOICE saw repeatedly the need to criticize papers and commentaries that had appeared in the medical journal Reproductive Biomedicine Online. We, therefore, are especially pleased to extend this month a compliment to the journal. Its last two issues contained a large number of interesting articles, many subjects of review in this section.
What happens to eggs and embryos as women age?
An interesting paper from the New York from the Weill Cornell program reported age-stratified oocyte and embryo data for women of advanced ages.1 The paper is interesting for several reasons: First, very few IVF centers treat older women above age 42-43 with the use of their own (autologous) eggs and, therefore, any data on older women is very welcome. The Weill Cornell program is one of the very few that still treats older women with autologous eggs, an effort they must be appreciated for. Second, their data offer some interesting insights, especially if one looks a little deeper than the authors did at times.
Their analysis involved a total of 3,362 patients going through embryo cryo-preservation cycles. The median mature oocyte rate was 81.8% and the median fertilization rate was 81.8%. Interestingly, both rates for all years up to age 44 remained stable; above age 44 mature oocyte rates, however, increased further and fertilization rates declined. These findings are, of course, entirely compatible with findings The CHR’s investigators reported already several years ago, demonstrating that premature luteinization in ovaries progresses with advancing age, which since has become the basis for The CHR’s highly individualized egg retrieval (HIER) the progressively earlier retrieval of oocytes with advancing female age.2,3 Had our colleagues retrieved especially their patients above age 44 earlier (though we start earlier retrievals in selected patients even below age 44), they, very likely, would not have experienced more mature (which in these cases really means over-mature) oocytes and, therefore, lower fertilization rates.
A similar conclusion can be reached from the reported blastocyst rates which remained comparable through age 40, from where on they started to significantly decline with advancing female age. Interestingly, mature oocyte and fertilization rates were not impacted until age 44. The discrepancy between this observation at age 44 and the earlier noted decline in blastocyst rates after age 40, however, tells a very interesting story, which
CHR’s researchers recently discovered (a paper has been submitted for publication), demonstrating that the ability of mature MII oocytes to make good quality embryos to very significant degrees deteriorates with advancing age.
Though this may also be a consequence of early luteinization after age 40 which also may be improvable through earlier egg retrievals, these numbers basically support the CHR’s longstanding policy of not culturing embryos of women above age 40 to blastocyst-stage.
REFERENCES
1. Romanski PA., et al Reprod Biomed Online 2022;45(3):432-439
2. Wu eta l., J Endocrinol 2015;226(3):167-180
3. Wu et al., J Ov Res 2018;11(1):23
Ethnic differences in AMH
Especially in the U.S., we are used to treating racially and ethnically highly diverse patient populations in our fertility centers. We, however, test them with the same test kits and expect results in the same ranges. Now two recent studies demonstrated the obvious: There are differences that must be considered!
British and Indian investigators discovered significant discordance between European and Asian-Indian women; Fertile healthy Indian women had at all ages significantly lower AMH values than their European counterparts, and, as one would expect, infertile Indian women, depending on underlying medical issues, had varying AMH levels from fertile healthy Indian counterparts.1 A Chinese study, on the other hand, published age-specific random day AMH values in a Chinese Han population,2 and their curves were practically identical to published U.S. and European curves.
REFERENCES
1. Gromski et al., Reprod Biomed Online 2022;45(5):979-986
2. Hao et a., Am J Obstet Gynecol 2022;227:883.e1-18
Does the quality of sleep impact IVF results?
Another recent study, this time in Fertility & Sterility, believes this to be the case for women under the age of 35 years.1 Clinical pregnancies (69.3% vs. 65.1%) and live birth rates (50.5% vs. 45.7%) appeared associated with “good” in comparison to “poor” sleep but we are, frankly, suspicious of these data. Definitions of “god” and “poor” sleep are always rather unprecise (the authors used the Pittsburgh Sleep Quality Index, PSQI), confidence intervals were marginal, and cofounders were not adjusted for.
That, of course, does not mean IVF patients should not try to sleep well; but we, frankly, would not even know how to quantitate good sleep: Does that mean good sleep every night or only the night before retrieval or embryo transfer? One sometimes really wonders what ends up in our medical journals.
REFERENCE
1. Liu et L., Fertil steril 2023;119(1):47-54
The V oice | f ebruary 2023 | 33 Continued on page 34
Some good news regarding Multiple Sclerosis
(MS) and ART
IVF cycles in women with MS have been associated with disease flairs.1 Consequently, it appears not unreasonable to raise the possibility that IVF cycles may increase the risk of developing MS. Fortunately, that does not appear to be the case, as a recent Danish study suggested.2 Studying 585,716 women of which 63,791 had at least one IVF cycle, at least within two years of an ART cycle, there was no evidence of an increased MS risk. Based on small numbers a non-significant trend toward increased risk was, however, present with increasing cycle numbers.
Though the latter observation suggests that a link cannot be completely ruled out, even a significant association with an increasing number of IVF cycles would not necessarily denote causation because autoimmunity is well known to be associated with increased infertility and autoimmunity may, therefore, be the cause for more IVF cycles. What comes first, - chicken or egg?
REFERENCES
1. Michel et al., J Neurol Neurosurg Psychiatry; 2012;83(8):796-802
2. Kopp TI, et al., Fertil Steril 2022; S0015-0282(22)01977-X. doi: 10.1016/j. fertnstert.2022.10.027.Online ahead of print.
Can endometrial and vaginal microbiota predict recurrent pregnancy loss?
According to Finish and British investigators, the answer is yes. They observed an association between repeated pregnancy loss and reduced L. crispatus and increased G. vaginalis abundance in the endometrium as well as increased abundance in the vagina. Moreover, vaginal, and endometrial microbiota corresponded. Though these data to some degree are reaffirming of earlier published data, they leave many questions unanswered. The most important one as of this point is, of course, whether the observed association is reflective of causation or, potentially, only a secondary event. And assuming that causation exists, how would changes in bacterial flora, especially in endometrium affect miscarriages? It appears easier to imagine an impact on implantation, - but repeat miscarriages? Especially considering that microbiota are not very stable, this appears like a very questionable proposition.
REFERENCE
1. Peuranpää et al., Reprod Biomed Online 2022;45(5):1021-1031
Androgen pretreatment in poor responders?
CONFLICT STATEMENT: Readers of this section should be aware that The CHR and some of its principals have been awarded several US user patents, claiming treatment benefits from supplementation with DHEA and other androgens in some infertile women. CHR and its principals receive licensing fees from these patents and are shareholders in OVATERRA by Fertility Nutraceuticals LLC, a company that produces a DHEA product called Fertinatal.
A group of investigators published a systematic review and meta-analysis suggesting higher live birth rates following transdermal testosterone supplementation in poor responders during IVF.
Considering how bad the published data on testosterone supplementation are, the authors did a heroic job. By concluding that the probability of pregnancy is increased in poor responders pretreated with transdermal testosterone, they, likely, reached a correct conclusion. Since we reviewed androgen supplementation in The VOICE last month, we here will not be repetitive. Only so much. The CHR does not like androgen supplementation with testosterone because it, easily, allows for over-supplementation into toxic ranges for ovaries. Too high testosterone is even worse for ovaries than too little of the hormone. Supplementation with DHEA may take a little longer but is far safer and is, therefore, how The CHR supplements women with low functional ovarian reserve.
REFERENCE
1. Katsika et al., Reprod Biomed Online 2023;46(1):81-91.
Endometriosis
An international consortium of investigators just published a first single-cell transcriptomic analysis of endometriosis in Nature Genetics. 1 This is a very important piece of work, on which investigations of the condition can build in the future. The study profiled transcriptomes of in excess of 370,000 cells from endometriomas, endometriosis, eutopic endometrium, control (unaffected) ovary, and control (unaffected) peritoneum, in the process generating a cellular atlas of endometrial type epithelial cells, stromal cells, and microenvironmental cell populations across different tissue sites.
Endometrial-type epithelium demonstrated significant differences in cellular and molecular signatures across tissues, suggesting cellular restructuring and transcriptional reprogramming in endometriosis. In endometriomas, epithelium, stroma, and proximal mesothelial cells demonstrated dysregulation of inflammatory pathways and upregulation of complement. Interestingly, they also found enriched signatures of ciliated epithelial cells in ovarian cancer which they suggested may “reinforce” suggested epidemiological associations between endometriosis and ovarian cancer.
A second interesting paper on endometriosis was published in the JAMA Network Open journal for the first time demonstrating epidemiologic as well as genetic associations between endometriosis and mental health co-morbidities, such as depression, anxiety, and eating disorders.2 The study population involved 202,276 unrelated females. Genotypic and phenotypic information was retrieved from the UK Biobank and combined with genome-wide association statistics available in several data international from five countries.
The population was, however, surprisingly aged: 8,276 women with endometriosis had a mean age of 51.3 years (194,000 controls, 56.7 years). Accounting for age, BMI, socioeconomic status, chronic pain-related phenotypes, irritable bowel syndrome, and psychiatric co-morbidities, endometriosis was found to be associated with increased odds of depression, eating disorders, and anxiety, all also supported by significant
Continued from page 33 34 | f ebruary 2023 | The Voice
genetic correlations. A genome-wide analysis of pleiotropic associations was identified after multiple corrections 1 locus (DGKB rs12666606) with evidence of pleiotropy between endometriosis and depression.
We have to acknowledge a serious degree of skepticism, in accepting this paper’s reported facts, considering that recruitment ages were in the menopausal range and diagnoses of endometriosis mostly depended on self-reporting. If one then adds that, even at younger ages, endometriosis diagnoses are known to be highly inaccurate, one must question the likelihood that here reported associations can really be considered too seriously.
REFERENCE
1. Fonseca et al., Nat Genet 2023; doi: 10.1038/s41588-022-01254-1. Online ahead of print.
2. Koller et al., JAMA Net Open 2023;6(1):e2251214
Should we stop screening for endometritis?
Three Belgian colleagues in an opinion piece in Reproductive Biomedicine Online recently advocated ending screening for endometritis. The article published under the heading “countercurrent” basically laments how little is known about this condition. We agree that this condition deserves further scientific inquiry but that, of course, does not mean we should stop looking for it. On the contrary, we should encourage more efforts to diagnose the condition accurately, followed by appropriate treatment trials.
What, moreover, the authors failed to consider is the well-known fact that endometritis may be bacterial or sterile-inflammatory, with cases being approximately evenly distributed between these two etiologies. Both, quite obviously, need different treatments.
REFERENCE
1. Darici et al., Reprod Biomed Onlien2023;46(1)3-5
Embryology
More on closed incubation and time-lapse
A seemingly well-executed multicenter study from China involving 1224 very young participants who underwent 1182 IVF cycles prospectively and randomized either with the use of a time-lapse system or a standard incubator. The results were interesting because this study demonstrated significantly better implantation rates in the first cycles with time-lapse (52.35% vs. 47.11%; P=0.014; after adjustments at P=0.02). However, cumulative implantation rates, live birth rates in first as well as cumulative live birth rates did not differ.1 In short, time-lapse systems are still searching for a reason to exist.
Another study in the same journal issue from China as well suggests that there is value in studying the morphology of the inner cell mass (ICM).2 Retroactively investigating 8946 singleton deliveries from vitrified-warmed single blastocyst transfers, what the authors described as Grade C ICMs ended up with a higher adjusted birth weight (of course in the literature in general
attributed to frozen-thawed embryo transfer cycles3). The authors then present a potpourri of alleged statistical calculations reaffirming this association between CME type C and large infants but do not in the paper describe how CME types A, B, and C were defined. They just provide a reference for the CME grading system they used which is not even developed by the authors. In short, not a very credible study.
In an attempt to further clarify why more males than females are born, Spanish investigators analyzed data from 646 women undergoing 921 PGT-A cycles in which 548 “euploid” blastocysts were warmed and transferred in elective single embryo transfers.4 They reported that 53.1% of embryos were males and only 46.9% were females for a sex ratio of 1.13. After adjustments “euploidy” was more common in females (ad, OR 1.29, 95% CI 1.08-1.55). Euploid blastocysts were, however, comparable between the sexes. Moreover, the investigators found no significant differences between sexes in implantation, miscarriage, and live birth rates. They concluded that more male embryos reach the blastocyst stage but exhibit higher “aneuploidy,” though both sexes did not differ in implantations and in live births. (Please note that chromosomal diagnoses were in parentheses because the authors used standard PGT-A definition which, erroneously, judges embryos only with reference to a 5-6-cell trophectoderm biopsy. Consequently, mosaicism is undercounted and euploidy and aneuploidy are overcounted)
REFERENCES
1. Zhang et al., Reprod Biomed Online 2022;45(5):858-866
2. Zhu et al., Reprod Biomed Online 2022;45(5):890-897
3. Siijkers et al., Gynecol Obstet Invest 201;82(6):538-546
4. Carraasco et al., Reprod Biomed Online 2022l45(5):851-85
Menopause
Does perimenopausal hormone replacement therapy protect against Alzheimer’s?
Hormone replacement therapy (HRT) in perimenopausal women has for several reasons remained a controversial issue, with the risk/benefit situation for such treatment being the principal issue of contention. Women, however, have a higher risk for
Continued on page 36 The V oice | f ebruary 2023 | 35
age-dependent dementia than men. Assuming a beneficial effect of HRT on this risk could greatly affect the current risk/benefit considerations. Now come British investigators and reported evidence for improved delayed memory and larger entorhinal and amygdala volumes in APOE4 carriers (at increased risk for Alzheimer’s).1 If confirmed in additional studies, this observation would support more aggressive use of perimenopausal HRT in at least APOE4 carriers, a large population of women at increased risk for Alzheimer’s.
REFERENCE
1. Saleh RNM, et al., Alzheimers Res Ther 2023; 15(1):10
Viruses and bacteria
Updates on COVID-19
COVID-19 is not over; indeed, as an editorial in the new year notes, “it is far from over.”1 As of mid-January, things are, however, apparently getting better: Even though the omicron XBB1.5 variant, representing almost 50% of all COVID-19 cases, is the so-far most infectious variant by far, it is also clearly less virulent. The winter wave appears to have peaked; hospitalizations and death rates were never very high and already appear to decline. In a way, most reassuring is the recent FDA announcement that, in analogy to an annual influenza vaccine, the FDA will in the future recommend one booster against COVID.
The FDA thus recognizes that COVID-19, based on the risk of severity of societal impact has become the “new flu.”2 Like in current practice with annual flu vaccines, scientists in the spring will travel to China to see which mutations are the most active and then produce, with these mutations in mind, the appropriate COVID vaccines for the Western hemisphere for the following fall and winter. In other words, what goes into those vaccines is to a considerable degree a guess. Efficiencies of such vaccines, therefore, barely ever reach 50%. Exactly the same efficacy is, therefore, what we can expect from this newly proposed FDA strategy. One can only hope that future strains maintain low virulence.
COVID-19 convalescent plasma (CCP) in the early days of the pandemic, when vaccines were still in development, was viewed as a potentially lifesaving remedy. The treatment however, has since fallen out of favor and, especially the COVID-19 infamous World Health Organization (WHO), indeed, in December of 2021 recommended against the use of this treatment even in immunocompromised patients.3 A recent systematic review and meta-analysis just published in JAMA Network Open, however, contradicted the WHO recommendation by demonstrating clearly decreased mortality following CCP in immunocompromised individuals.4
A rather scathing article supporting the use of CCP followed, very well outlining not only the supportive facts but also why the dismissal of CCP, considering the increasing ineffectiveness of Omicron variants of the SARS-CoV-2 virus and availability of basically only one FDA-approved anti-viral drug against the virus, mandates the continued availability and clinical use of CCP at least in immunocompromised individuals.5 There was a time when WHO (CDC and FDA) used to be the first to discover these things, but those days appear gone. What is left are unfortunately often rudderless organizations, not only incapable of protecting public health but, at times, endangering public health.
The British Medical Journal Global Health (BMJ-GH) just published an important individual participant data meta-analysis regarding maternal, fetal, and newborn outcomes among pregnant women with SARS-CoV-2 infections that offered significant new insights.6 The conclusions were that the virus at all times of pregnancy increases the risk of maternal death, of severe maternal morbidity, and neonatal morbidity, but not of stillbirths or intrauterine growth restriction. Only more reason to get vaccinated before or in pregnancy, - as little as this may help - it is better than nothing!
There has been considerable hope among investigators that a nasal anti-COVID vaccine will, finally, end the COVID-19 pandemic, even hopefully preventing endemic maintenance in the population akin to the influenza virus. Unfortunately, these hopes were shattered when a phase 1 trial at Oxford University in the UK only
36 | f ebruary 2023 | The Voice Continued from page 35
produced disappointing results.7 A recently published survey of nasal candidate vaccines found over 100 in development worldwide and 20 in clinical trials and, therefore, allows for hope for better results. The so-called ChAdOx1 intranasal vaccine tested at Oxford had, however, produced excellent results in inducing mucosal and systemic immune responses in mice, hamsters, and non-human primates and, still, failed in humans.
REFERENCES
1. Editorial. The Lancet 2023;401:79
2. https://www.npr.org/sections/health-shots/2023/01/23/1150032238/ fda-considers-major-shift-in-covid-vaccine-strategy
3. https://www.who.int/news/item/07-12-2021-who-recommends-againstthe-use-of-convalescent-plasma-to-treat-covid-19
4. Senefeld et al., JAMA Network Open 2023;6(1):e2250647
5. Franchini et al., Life (Basel) 2023;13(1):134
6. Smith et al., BMJ Global Health
7. Carvalho T. Nat Med 2022;28:2439-2440
Yes, Zika is still of concern
Though the Zika virus has disappeared from the headlines as quickly as it ascended, the CDC still records cases and warns women and men who are planning pregnancies or already have an established pregnancy from visiting areas with still active disease.1 Now comes, however, a paper in Cell which identified a Zika virus-specific in pregnancy elicited monoclonal IgM antibody (DH1017.IgM) which exhibits ultrapotent neutralization of the virus.
What makes this finding so remarkable are three observations:
(i) That this antibody is produced in pregnancy; (ii) That this antibody is of the IgM and not IgG isotype (i.e., a product of the immediate humeral response during 30 days from infection); and (iii) that IgM antibodies, because of their large size, do not cross the placenta. Consequently, these antibodies – in contrast to maternal IgG antibodies – therefore, cannot protect the fetus. The authors propose the so-identified IgM antibody as a safe and potentially effective treatment modality but in their discussion fail to notice that administration to the mother, likely, will not protect the fetus.
REFERENCE
1. Singh et al., 2022;185:4826-4840
Genetics of reproduction
Preimplantation genetic testing for aneuploidy (PGT-A)
There have been several papers published over the last month on PGT-A, but none of them have significantly added to the literature or are worth our attention. One of only three exceptions was a paper in JARG that, based on the SARS CORS database, investigated the cumulative national U.S. impact of PGT-A on IVF outcomes.1
Analyzing 133,494 autologous IVF cycles from the registry that produced at least one blastocyst for either an embryo transfer of
PGT-A. Among those and including those who after PGT-A had no embryos to transfer, the cumulative live birth rate (CLBR) after PGT-A was at all ages lower than in non-PGT-A controls (P<0.001), except in women above age 40. This negative association was especially pronounced under age 35 (where most PGT-a cycles are performed). Unsurprisingly considering that this was not a randomized study, and choice or non-choice of PGT-A was obviously influenced by the patient’s medical conditions and personal choices, multiple gestations, preterm births early pregnancy losses and low birth weights were all greater in non-PGT-A patients.
CHR’s David Barad, MD, MSc, was asked by the editor-in-chief to write a commentary on the paper (see also “CHR Publications” in this issue), which he did well under the brilliant title, “PGT-A ‘perfect” is the enemy of good.”2 What he meant to say with this title is that, as through PGT-A we strive to provide our patients with “perfect” embryos, we risk elimination many “good” embryos with still significant pregnancy potential.
The second exception was another paper by U.S. authors that compared the reported PGT-A results from four national PGT-A laboratories and appeared surprised that some labs reported significantly different euploid and mosaicism rates in blastocyst-stage embryos as well as subsequent pregnancy rates.3 That PGT-A results from identical embryos significantly varied between laboratories CHR investigators already reported in 2015.4
While their claim of being the first to ever compare cycle outcomes (i.e., pregnancy rates) between PGT-A laboratories is, likely, correct, the reason, however, is not that the idea for the study was overdue but, indeed, exactly the opposite: The assumption that such a comparison should be attributed to the quality of the PGT-A lab, is with overwhelming likelihood incorrect, even though the study population was seemingly very uniform young egg donors. When, however, definitions of euploidy and mosaicism differ between PGT-a laboratories, as they do to very significant degrees, comparisons are, of course, impossible because what in one lab is a euploid embryo in the other lab may be a mosaic. Some laboratories, indeed, have returned to only binary reporting of euploid and aneuploid.
Though a contribution from laboratory techniques cannot be ruled out, they are only very unlikely significant for cycle outcome. The quality of embryos, as determined by ovarian stimulation, the timing of retrieval, embryo culture, and, finally, embryo biopsy are much more likely significant contributors to clinical outcomes. Moreover, centers with better egg donor selection, better simulation protocols, and better embryology will, of course, have better outcomes.
How this paper, therefore, sailed unchallenged through peer review is somewhat surprising. this paper will be subject at the CHR’s February Grandrounds, February, 21, 2023.
The third paper comes from The Netherlands and claims to
The V oice | f ebruary 2023 | 37 Continued on page 38
present a cytogenetic comparison of trophectoderm (TE) and inner cell mass (ICM) in 46 surplus embryos.5 By the time we, however, come to Figure 3, a schematic comparison between TE and ICM in the same embryos, out of 10 comparisons, 6 had only between 1 and 3 embryos. The authors then reached one of these almost bizarre conclusions, in themselves contradictory when stating:
“Despite the low cytogenetic concordance rate due to chromosomal mosaicism, a single TE biopsy could correctly predict whether the ICM consists of mostly normal or abnormal cells in the majority of case.” If anybody can decipher what this sentence is meant to mean and how it can inform on how TE and ICM correspond in ploidy, may they step forward! Once again, wonders how such a wishywashy statement gets through peer and editorial review. It, after all, says absolutely nothing.
REFERENCES
1. Kucherove et al., J Assist Reprod Genet 2023;40:137-149
2. Barad DH. J Assist Reprod Genet 2023;40:151-152
3. Bardos et al., Fertil Steril 2023;119(1):2934
4. Gleicher et al. Fertil Steril 2015;104(3Suppl)E59
5. Chavli et al., Reprod Viomed Online 2022;45(5):867-877
Non-invasive prenatal testing (niPT) for monosomy X (Turner syndrome)
The American Journal of Obstetrics & Gynecology finally has published an interesting and rewarding review paper worth some comments. It is a clinical opinion under the signature of quite a large number of authors from varying institutions in the U.S. and offers very interesting insights into the complex issue of X-chromosome monosomies and the management of suspected maternal and/ or fetal Turner syndrome in early pregnancy.1 We noted only one omission in this, otherwise, very comprehensive review of the subject. The authors did not address so-called age-associated Turner mosaicism, a rarely discussed phenomenon in the literature which, however, is not infrequently encountered in laboratory reports of peripheral karyotypes in older infertility patients as a result of so-called somatic mosaicism, an inevitable consequence of human aging.2
REFERENCES
1. Dowlut-McElroy et al., Am J Obstet Gynecol 2022;227(6):862-870
2. Evans MA, Walsh K. Physiol Rev 2023;103(1):649-716
Immunology
Everybody is by now aware of CAR T cells, engineered modified autologous T cells that have become life-changing in many human cancers. Now first reports are appearing in the literature describing the application of the same techniques in treating autoimmune diseases, especially systemic lupus erythematosus (SLE),1 a disease mostly affecting young women of reproductive age. It is this latter fact that makes this development noteworthy to our readership. Understanding CAR T cells is complex, but a recent article in Nature magazine is so well written and explains things so well, we felt it should be featured here,- so our in the subject interested readers could look it up.
REFERENCES
1. Mackensen et al., Nat Med 2022;28:2124-2132
2. Tsokos GC. Nature 2022;611:-458
the really bad paper section
More on drug use (including Cannabis) in pregnancy
In two papers investigators from the Division of Research of Kaiser Permanente Northern California offer additional insights into current drug use in pregnancy. A first paper addressed perceptions among prenatal cannabis users about cannabis following legalization (in California).1 Unsurprisingly, users described easier access, greater acceptance (including less stigma among healthcare providers), and improved trust in retailers. Responses were described as more “mixed’ regarding whether marketing and advertising impacted prenatal cannabis use and whether legalization decreased concerns about involvement from Child Protective Services. One really wonders why anybody would expect anything else but these results and, if that is the case, why waste effort on this study?
In a research letter, the same group reported on trends in self-reporting and biochemically verified cocaine and methamphetamine use in pregnancy in Northern California between 2011-2019.2 They found that annual relative rate increases for cocaine use were estimated as greater through toxicology testing than self-reporting. In contrast, methamphetamine usage did not increase, as measured by toxicology screening, and, actually, declined by self-reporting.
In other words, both comparisons demonstrated – again rather unsurprisingly - that self-reporting is, likely, not as discriminatory as toxicology testing. One wonders again, what else than this outcome the investigators expected? If investigators want to waste time and resources on obvious “self-fulfilling” studies, that is, of course, their prerogative; but don’t the JAMA journals have better use for the valuable space in their journals?
REFERENCE
1. Young-Wolff et al., JAMA Netw Open 2022;5(12):e2246912
2. Young-Wolff et al., JAMA Netw Open 2022;5(12):e2248055
Additional information on thyroid disease in infertility and pregnancy?
Thyroid autoimmune disease is the most frequent autoimmune disease in women of reproductive years. it frequently presents with anti-thyroid autoantibodies before clinical thyroid function is affected. Especially thyroid peroxidase antibodies (TPO ABs) are frequently present and are known to often predispose to later function abnormalities. British and Singaporean investigators now reported on the development of abnormal
Continued on page 39
38 | f ebruary 2023 | The Voice Continued from page 37
thyroid function among initially euthyroid women who were TPO ABs – positive between ages 16-40 with a history of miscarriages or subfertility, were planning on pregnancy, and were randomized to 50mcg daily of levothyroxine or placebo. Approximately 7% of originally euthyroid TPO Ab-positive women developed subclinical or overt hypothyroidism within one year of preconception time or in pregnancy. Conception rates in these women were lower than in women who did not become hypothyroid, though live birth rates were similar.1
The here investigated patient population came from a secondary analysis of the TABLET trial that had investigated the effects of prophylactic levothyroxine treatment on pregnancy in TPO AB-positive though euthyroid women and had not found any positive effects of such treatment.2 The question mark at the end of the heading for this sub-section, therefore, is based on our question about what the additional purpose for this secondary analysis may have been because as the authors themselves noted in this paper, their 2019 paper also reported that 7.4% of women within one year developed hypothyroidism. The only news from this paper was the totally unsurprising “revelation” that treated women with hypothyroidism had a higher failure to conceive rate in comparison to euthyroid women (adj. RR 2.02[1.56-2.262]; P<0.001). The authors, however, then did not even ask why then live birth rates did not differ.
We, of course, do not know the answer; but the first logical thought when pregnancies are lost between conception and delivery is, of course, miscarriages. And here the difference was, indeed, 31% in euthyroid women and 0% in hypothyroid women. It does not take a genius to understand that women who remained euthyroid, for whatever reasons, had higher miscarriage rates. Obviously, those diagnosed with hypothyroidism within a year of observation received some treatment that prevented miscarriages that the other group did not receive. Where were the reviewer’s editors?
The CHR
Fighting for every egg and embryo
REFERENCE
1. Gil et al., J Clin Endocrinol Metab 2023 108;124-134
2. Dhillon-Smith et al., N Engl J Med 2019;380:1316-1325
Does single embryo transfer imply the quality of care in IVF?
They call it a “review” but, because of being highly selective in which references to cite, it in reality was nothing but (a very bad) opinion piece when Belgian colleagues recently penned an article in Reproductive Biomedicine Online propagating the idea that elective single embryo transfer (eSET) implies the quality of care in reproductive medicine.1
Since we have addressed the eSET issue in The VOICE on many occasions before, we will not regurgitate the subject but we felt strongly that this paper deserves inclusion in this month’s price winners as “really bad papers.” One only needs to read the authors’ key message to understand: “This review highlights that single embryo transfer (SET)complies with important aspects of quality of care in reproductive medicine by encompassing safety, effectiveness, patient-centredness (is this really a word?) and efficiency, which leads to equity. SET, therefore, should be the standard of care in assisted reproductive technology.” Why does this sound more like an ideological, political statement than the summary of a medical opinion piece? Because it is!
REFERENCE
1. De Neubourg et al., Reprod Biomed Online 2022;45(5):899-905
The CHR VOICE is the newsletter of The Center for Human Reproduction (CHR), an independent, academically affiliated infertility and research center located at 21 East 69th Street in Manhattan, New York, N.Y 10021. www.centerforhumanreprod.com. Telephone +212 994 4400.
The CHR VOICE attempts to inform and engage a global community of infertility patients, infertility service providers, and researchers in reproductive medicine, physiology, and biology. The mission of The CHR is clinical care, research, and education, all at highest standards, with empathy, honesty, integrity, and equity.
The newsletter is published 10 times a year (except July and August). Copyright © 2023 by The CHR. All rights reserved.
For letters to the editor, comments, and suggestions, please contact Micah Elias at melias@thechr.com. For all advertisements or sponsorships in The VOICE , please contact Alexandra Rata at arata@thechr.com. Advertisements appearing in The CHR VOICE do not necessarily reflect the opinions of The CHR. .R
The V oice | f ebruary 2023 | 39



The Center for Human Reproduction Fighting for every egg and embryo Conne C t with us! www.the C hr. C om so C ial@the C hr. C om 212.994.4400 21 e 69th s t n ew y ork, n ew york 10021 ADVERTISEMENT




































 Image 2
Image 3
Image 2
Image 3

 By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.
By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.