THE DECEMBER 2022 in this month’s issue The CHR Letter Endometriosis: The Condition Nobody Knows Much About, Part II Questions Patients Ask A Piece of My Mind: What Made Us Physicians Believe We Know Better Than Patients What is Good for Them? The CHR’s Interpretation Of Recent Medical Literature Relevant To Reproduction 03 04 09 15 22
The CHR is known as a “fertility center of last resort,” primarily serving patients who have previously failed treatments elsewhere. Among CHR’s areas of special expertise are treatments of “older” ovaries, whether due to advanced female age or premature ovarian aging (POA), immunological problems affecting reproduction, repeated pregnancy loss, endometriosis, polycystic ovary syndrome (PCOS), tubal disease, male factor infertility, etc.

Missed the last issue of The VOICE?

Access previous issues on thechr.com



AT THE CHR
BOARD-CERTIFIED RE-I AT ASSOC. PROF/PROFESSOR LEVEL

The CHR is looking for another senior board-certified RE-I (or international equivalent) to join our growing national and international practice. Though private, our center is organized along academic principles in that physicians are expected to excel not only as clinicians but also as researchers. The center’s uniquely structured compensation package, therefore, incentivizes both activities. We are looking for an individual with documented excellence in both areas, commensurate with associate professor/professor level. Besides a competitive salary, incentive bonus structure, and excellent benefit package, the CHR also offers partnership along either a 3-year or 5-year equity track and, ultimately, part or complete ownership, as the current leadership is expected to retire within that time-period.
If you feel qualified for the position and share our philosophy of being a physician-scientist, please let us know by submitting your C.V. and a brief letter of interest to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position can be filled immediately. All submissions are considered confidential.


CONNECT WITH THE
CHR
www.thechr.com @CHRNewYork @CHRNewYork @CHRNewYork 2 | december 2022 | The Voice
hirinG
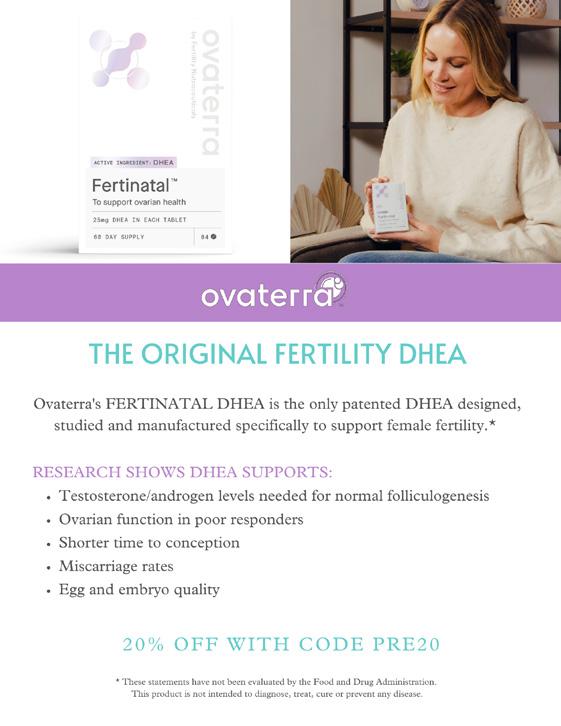
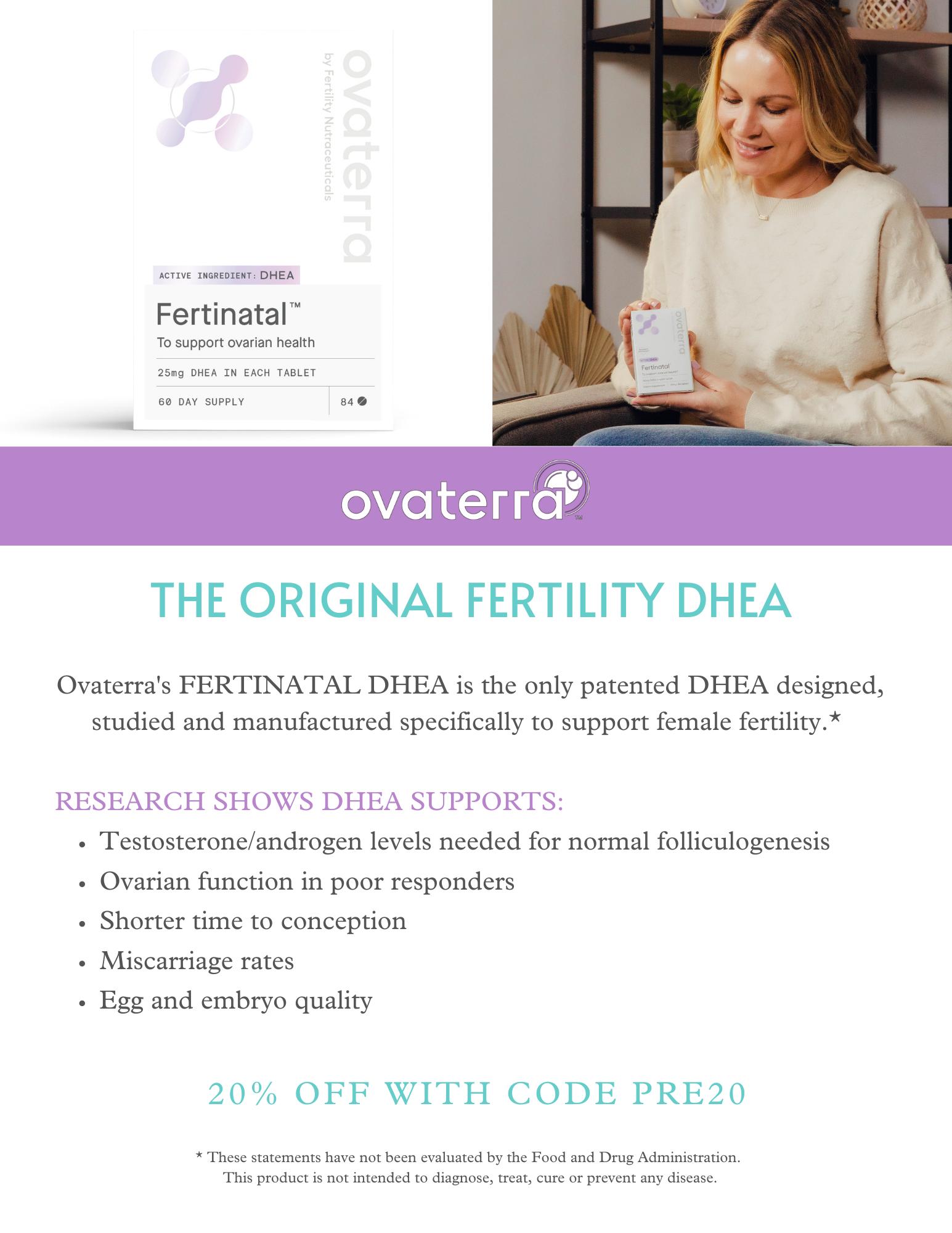
ADVERTISEMENT
the Voice
With the year 2002 is almost behind us, it is easy to conclude that it on many different levels was an unusually tumultuous year. It, however, also was the year that, finally, moved COVID-19 into the rear mirror, though, as was learned, this virus can be very unpredictable. It, of course, is not completely gone, - we just had to learn to live with the virus and with its likely many future mutations, just as we have learned to live with an annual influenza season caused by always changing influenza virus strains.
Because New York state has renewed the COVID-19 emergency, we are maintaining most (though not all) of the restrictions in access to the CHR over the holiday season. Should we be able to avoid another severe COVID-19 wave over the year-end and the beginning of the new year, our intent is to scale those restrictions radically down or even completely remove them by the end of January 2023. We are in the meantime maintaining them not only because of concerns about a winter wave of COVID-19, but because New York is currently under a quadruple threat: Fortunately, Monkeypox seems to be declining; but hospitals are now concerned about the trifecta of COVID-19, Influenza, and the Coxsackie viruses, with the latter already overwhelming pediatric hospitals in their occupancy. Coxsackie infections primarily affect young children; but can also become another dangerous respiratory disease for older people. All three of these viral diseases present with similar symptoms and are, therefore, often difficult to hold apart. As we have noted repeatedly before, despite all alleged controversies, the CHR recommends COVID-booster vaccinations as well as the annual flu shot, which is available at the CHR.
And then there was a record-breaking inflation to deal with, as this country has not witnessed in decades which, unfortunately, is predicted by many economics experts to lead into a recession sometimes during 2023. Let’s hope that these experts are wrong (it would not be the first time); but we will know early because CHR investigators, then quoted in the New York Post, reported after the last big recession in 2008 that drops in national IVF cycle numbers were an early indicator for an upcoming recession. So-far we have not seen such evidence, but we will let you know when we do.
As always, the CHR remains open over the holidays to primarily serve our many long-distance patients who often choose this time to pursue treatment cycles. We, therefore, during this time period are also available to patients from other IVF centers that have closed for the holidays (as most do) who experience emergencies. Which leaves us with wishing all of our readers a Joyous Holiday Season and a Happy, Healthy, Prosperous and Recession-free New Year. We are looking forward to seeing you again in 2023,
The Editorial Staff of the VOICE and the staff of the CHR
DECEMBER 2022 The V oice | december 2022 | 3
ENDOMETRIOSIS
ENDOMETRIOSIS
THE CONDITION NOBODY KNOWS MUCH ABOUT PART
II
Only FEW subjects in female medicine are surrounded by as much “mystique” as the condition known as endometriosis. Because endometriosis clinically affects women especially during reproductive years, it is erroneously widely perceived as mostly a reproduc tive disease, causing infertility. It often, however, also causes pelvic pain and several other symptoms. Endometriosis is, however, a much more complex condition than that, and in many women greatly affects quality of life. After in the november issue offering Part I in a series of articles on endometriosis, we here continue with Part II giving our readers a detailed view of how clinicians and scientists at the CHR currently view this condition. Further segments will follow in the new year.
Introduction
We started this series of articles in the November issue of the VOICE with an introduction that emphasized how surprisingly little is known about endo metriosis, even though this condition (or should we call it a disease after all?) is by many not only considered one of the most frequent causes of female infertil ity but also as often severely disabling. In here presented section we are more practical by addressing several clinically relevant issues, women with endometri osis usually face.
The importance of timely diagnosis Everything, of course starts with diag nosis, - which immediately raises several important questions because there is good reason why this condition has been often described as a diagnostic chameleon: The diagnosis of a disease usually starts with symptoms that raise suspicion and is then often confirmed with laboratory tests. Unfortunately, neither applies here, however, because even severe endometriosis may exist without any symptoms, may have many rather non-specific symptoms, like mild dysmenorrhea (menstrual discomfort), bloating, pelvic and/or abdominal dis comfort, and discomfort during sexual
intercourse, or it may be so severely symptomatic that women functionally become disabled peri-menstrual or even for longer times, while also being unable to consummate intercourse because of excruciating pain (dyspareunia), espe cially with deep penetration. In other words, endometriosis is unique in that symptoms often do not correlate with severity of disease: mild disease may cause severe symptoms and severe disease can be completely asymptom atic. Consequently, even severe disease may go undiagnosed into advanced age, often to be recognized only unexpect edly during unrelated surgeries or as a result of a hysterosalpingogram (HSG) demonstrating tubal disease, a very fre quent consequence of endometriosis.
A timely diagnosis of endometriosis is even further hampered by the wide age-range when the disease has been diagnosed, which reaches from adoles cence1 up into menopause.2 Ultrasound is now the most widely used tool to diagnose the condition3l but has obvious limits in diagnosing mild disease and can be considered as diagnostic only if the ultrasound detects endometrio mas in ovaries, which denotes at least stage III disease. MRIs of the pelvis are
generally considered superior to ultra sound examinations but, to the best of our knowledge, no direct comparisons have been reported between these two instrumentations. In detecting rectal endometriosis, investigators noted no significant advantage of MRI studies;4 Japanese investigators also reported no obvious advantage for MRIs in the diag nosis of endometriosis with retroflexed uteri.5 Consequently consensus exists that the most reliable method of diag nosing (and staging) endometriosis is by laparoscopy with concomitant multiple peritoneal biopsies.6 Multiple biopsies of suspicious peritoneal areas are a requirement because endometriosis can be microscopic, - not even visible to the naked eye during the procedure.
CHR physicians, who have extensive experience in reading hysterosalpingog raphies (HSGs) and never rely on radio logical reports without looking at the original films, frequently also can reach quite accurate endometriosis diagnoses from 3-4 typical HSG findings: (i) the deviation of the uterus from the midline to one side; (ii) a retroverted uterus; (iii) a uterus with a Müllerian abnormality; and a typical tubal occlusion pattern, characterized by distal phimoses and
4 | december 2022 | The Voice
Continued on page 5
hydrosalpinges. Already in the 1990s CHR investigators reported that tubal endometriosis usually starts with a distal phimosis of tubal fimbriae, which leads to distal tubal occlusion and fluid accu mulation in the tube, forming a so-called hydrosalpinx. As a reflection of tubal damage, the process often also leads to increased intratubal pressure.7 For years there have been attempts made to find accurate less- or fully non-invasive means to diagnose endo metriosis. CHR investigators already in 1995 published such attempts.8 Recently polygenic risk scoring has been proposed for non-invasive diagnosis.9,10 For the CHR’s October GrandRounds, we welcomed Christina N Metz, PhD and Peter K. Gregersen, MD from Long Island’s Northwell Feinberg Institute who devel oped a single cell RNA-assay with the intent of diagnosing endometriosis from menstrual fluid.11 But to this day, laparos copy is considered the gold standard in the diagnosis of endometriosis
REFERENCES:
1. Russel et al., BMJ Case Rep 2021;14(3):e238547
2. Secosan et al., Diagnostics (basel) 2020;10(3):134
3. Bäumler et al., Horm Mol Biol Clin Investig 2022;doi: 10.1515/hmbci-2021-0082; Online ahead of print.
4. Poordast et al., Int J Gynecol Obstet 2022; doi: 10.1002/ijgo.14554. Online ahead of print.
5. Matsuda et al., J Nippon Med Sch 2022; doi: 10.1272/jnms.JNMS.2023_90-106
6. Signorile et al., In Vivo 2022; 36(1):430-438
7. Karande et al., Fertil Steril 1995; 64(6):1070
8. Gleicher et al., Hum Reprod 1995;10(4):923-926
9. Svensson et al., BMC Womens Health
2022;22(1):208
10. Kloeve-Mogensen et al., Front Reprod Health 2021;3:793226
11. Shih et al., BMC Med 2022;20(1):315
Endometriosis as a gynecological condition
Though the CHR confronts endometri osis primarily as a fertility-causing con dition, its importance as a gynecological disease is probably affecting many more women. As already reviewed in Part I of this series of articles, endometriosis can be found almost anywhere in pelvis and abdomen. It has also been reported to
CHR’s Medical Director, Norbert Gleicher, MD, already in 1987 raising the question whether endometriosis should not, in itself, be considered an autoimmune disease.8 The association with other autoimmune diseases can at times create a confusing symptomatology, further complicating diagnosis.
invade the umbilicus up to the skin,1 the diaphragm into the lungs and/or thorax cavity,2 the bladder to cause hematuria,3 and the rectum to result in rectal bleed ing during menstruation4 among many other locations. Consequently, symp tomatology can greatly vary and mimic other diseases. In addition, endometri osis is, as will be discussed separately in the future, highly associated with autoimmunity5 and other autoimmune diseases, for example Sjögren’s syn drome 6 and rheumatoid arthritis.7 with
The by far most frequent presenting symptom, ultimately leading to a diag nosis of endometriosis is, however, often greatly varying pain. The most frequently encountered symptomatology leading to diagnosis is the combination of dysmenorrhea (pain with menses) and dyspareunia (pain with inter course). Whenever especially a younger woman in reproductive years presents to the gynecologist with these two symp toms, endome triosis must lead the differential diagnosis. Once a diagnosis is confirmed, then, however, arises the question how to treat the patient. And, unfortu nately, we to this day do not have a good treatment; indeed, we have no treatment at all, - if we consider a treatment as an attempt at cure of a disease. All currently available treatments of endometriosis, at best, only on a temporary basis improve the disease and/or its symptoms. As soon as treatments are paused, endometriosis very often returns.
The reason is that all treatments are based on Sampson’s theory of retrograde men strual flow through the fallopian tube being responsible for endometriosis because all
The V oice | december 2022 | 5
Continued on page 6
“Though the CHR confronts endometriosis primarily as a fertility-causing condition, its importance as a gynecological disease is probably affecting many more women.”
recent and current treatments are based on the interruption of the menstrual cycle and preventing menstruations. By interrupting the hormonal cyclicity that supports proliferation of endometrial tissues and subsequent shedding wheth er from endometrium or from implants in pelvis or abdomen, endometrial im plants are “starved” and prevented from expanding. The consequence is fibrosis of the lesions and scarring, producing a “burn-out” of endometrial lesions. Such treatments, therefore, only make sense in women in active distress who wish to receive quick relieve from pain, - even if only temporary, but are willing to accept the risk of recurrence. Such treatment can also be the bridge to surgical treatment of endometriosis, though pretreatment may make identification of by endometriosis affected areas more difficult during ablative surgery.
Aside from treatment improvements being temporary, since all treatments are based on interrupting the menstrual cycle, women cannot conceive while
in treatment. Moreover, prolonged suppression of ovaries by GnRH ag onists and/or antagonists (the most common drugs used to treat endome triosis) especially in infertile women with low functional ovarian reserve may cause irreversible further suppression of ovaries. Consequently, pregnancy is by many physicians considered the best of all temporary treatments of endometriosis especially in women with infertility because it, of course, interrupts cycle cyclicity, though without ovarian suppression. One, finally, cannot address the treatment of endometriosis without mentioning the introduction of an anti-inflammatory diet as a highly effective intervention in women with se vere endometriosis. Though largescale studies in support of such an approach are lacking, the CHR has seen dramat ic responses in highly symptomatic patients and, therefore, recommends an anti-inflammatory diet that excludes wheat, lactose, and sugar to all symp tomatic endometriosis patients. This is, indeed, a subject important enough to receive in the new year its
own more detailed discussion.
REFERENCES:
1. Deng et al., Clin Nucl Med 2022;doi: 10.10.1097/RLU.0000000000004459
2. Kardaman et al., Ann R Coll Surg Engl 2022;104(4):e109-e112 3. Soares et al., J Minim Invasive Gynecol 2022;S1553-4650(22)00961 4. Akborzi et al., Front Surg 2022;9:978326 5. Vila Boas et al., Hum Immunol 2022;83(1):70-73 6. Chao et al., Front Immunol 2022;13:845944 7. Zervou et al., Rheumatology (Oxford) 2022;61(11):4252-4262 8. Gleicher et al., Obstet Gynecol 1987;70(1):115-122
SELECTED FUTURE ENDOMETRIOSIS
TOPICS
- What is the place of surgery in endometriosis?
- Is endometriosis an immunological disease?
- The importance of diet endometriosis as a fertility diagnosis.
Ribbon for endometriosis awareness

6 | december 2022 | The Voice Continued from page 5
AT THE CHR
ONE or TWO-YEAR CLINICAL FELLOWSHIP in RE-I

If you failed in securing a formal fellowship position in RE & Infertility or simply want a change out of general OB/GYN practice, the CHR offers a fellowship position in RE-I which after 1 year will greatly improve competitiveness for a formal fellowship position and in 2 years establishes independent competence for establishing an infertility practice. The center’s last 1-year fellow was accepted into the NIHfellowship program after failing to secure a position in the preceding year.
Qualified candidates must be OB/GY board-eligible or certified, be eligible for hospital privileges and for a New York state license to practice medicine. As CHR maintains a very active research program in affiliation with Rockefeller University, CHR fellows gain substantial research experience, with great likelihood resulting author- or co-authorships in peer-reviewed publications. Board eligible candidates who still must accumulate surgical cases will be given the opportunity to do so.
Chosen candidates will receive a very competitive salary and a generous benefit package, including health and malpractice insurance as well as paid vacation time. If you feel that you qualify and are interested in a career in RE & I, please submit your CV and a brief application letter to our COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available as of January 1, 2023. All submissions are considered confidential.
ADVERTISEMENT hirinG
The V oice | december 2022 | 7 ADVERTISEMENT
Very great service, very knowledgeable doctors and nurses I really recommended it.
- A Patient
PATIENT TESTIMONIALS
PATIENT TESTIMONIALS PATIENT TESTIMONIALS PATIENT TESTIMONIALS

“
“They are group of phenomenal human beings, knowledgeable, professional, caring, honest, approachable, kind, and compassionate. Dr. Gleicher and Dr. Barad are skilled, experi enced, and honest physicians that keep communication as one of the key elements in their relationship with the patient. Even when things did not go as expected, they made sure to comfort me and maintained a positive attitude without being unrealistic.”
- CHR Graduate
8 | december 2022 | The Voice
“
QUESTIONS PATIENTSASK

Is the CHR open during the holiday season?
Yes, we are open because many of our long-distance patients, especially those from overseas, often use this time to come to NYC for IVF cycles. Because most IVF centers shut down over the holiday, the CHR has also made it a tradition to offer those centers back-up for their patients during this time period if emergencies require that a patient must be seen.
As a patient, please contact our center in such a case by calling 212-994 4400 and advise our staff which fertility center you usually attend, who your principal physician is at that center, and why you need help. Our staff will then give you an emergency appointment in accor dance with your needs.
As a physician or fertility center, please call our center at 212-994 4400 and ask to be connected to a physician on call, who then will handle all administrative matters regarding your patient.
Will drinking alcohol during the holiday season impact my IVF treatments?

That depends on the definition of “drinking alcohol:” If it’s only a glass of red wine here and there, there should be no impact on your IVF cycles (can you imagine women in, Italy, France, or Spain not having a glass of wine once in a while?). But if it means substantial and reg ular hard liquor intake, we, of course, recommend against. Once presumed pregnant (that is after embryo transfer), all alcohol consump tion should cease until the baby is delivered and/or stops breast-feeding.
Should we eat pineapple core after an embryo transfer to improve the chances of implantation?
That we received this question repeatedly should not surprise because this idea has recently made the rounds on the Internet.1 The idea behind this latest fad appears to be that a substance, found especially concentrated in pineapple core, called bromelain because of its anti-inflammatory effects offers improvements in embryo implantation rates. A literature search we conducted revealed only 1 paper that mentioned bromelain under the heading of IVF, and that involved camels.2 One additional paper referred to its anti-inflammatory
Continued on page 22 The V oice | december 2022 | 9
effects as a natural proteolytic for intraabdominal adhesion prevention.3
Though bromelain, thus, may be a valuable anti-inflam matory and, as we have repeatedly noted in these pages, CHR does not “like” evidence of inflammation in our IVF patients, the concept of adding one “shot” of an anti-inflam matory to an IVF cycle after transfer, appears like a highly naïve approach from an immunological standpoint and only very unlikely could have any kind of effect on implantation. We, therefore, do not see any rational to eat pineapple core after an embryo transfer, - that is, of course, unless you like pineapple.
REFERENCES:
1. Fenimore C. https://www.ovulifemd.com/pineapple-fertility/
2. El-Bahrawy et al., Anim Reprod Sci 2017;187:100-108
3. Sahbaz et al., Int J Surg 2015;14:7-11
Does daylight saving time affect female fertility?



The Internet never disappoints in allowing us to discover “interesting” new alleged medical knowledge. Another item making the rounds as we found out recently is the idea that daylight savings time (DST) increases for pregnant women the risk of miscarriages for a period of approximately two weeks. When comparing pregnancy rates and pregnancy losses between Spring and Fall, no significant differences were detected. When DST occurred after embryo transfer in the Spring, the rate of miscarriages was allegedly significantly higher and was especially pronounced in women with a prior history of spontaneous pregnancy loss.1

Published as a serious medical research project by Bostonbased colleagues, involving 1,654 autologous IVF cycles for whatever reason performed between 2009 and 2012 (we hope the reason was not that it took them so many years to find a medical journal that would publish this article) the article was already in 2017 published in a rather obscure journal (where it belongs) but only now was discovered by the Internet.2 And, then, there is not much more to say about this paper and the subject it claimed to address!
REFERENCES:
1. Liu et al., J Biol Med Rhythm Res 2017;34(5):571-577
2. Science Daily. 2017; https://www.sciencedaily.com/releas es/2017/02/170208111607.htm
How useful are home-insemination kits?
Increasing numbers of home insemination kits have been hitting the marketplace, and we are often asked, which are the best? Whether there are better or worse home insem ination kits being offered to single women or gay female couples, who are the principal users of these kits, we frankly do not know because we have not tested different products
and also have not heard much commentary on the available kits. Like with everything else for purchase, it appears reasonable to suspect that there must be differences. But considering how relatively simple the technical process of self-insemination is (with or without help), differences cannot be major. A little bit of investigating different brands before purchase, however, of course still makes sense.
The important issue, though, is of course not the insemina tion device, but the semen specimen that goes into the de vice. Unfortunately, the Internet increasingly propagates and offers “private” semen donations of untested semen. THIS IS DANGEROUS because it is impossible for the woman to know whether her semen donor is infected with a potentially conta gious disease, including HIV. The semen donor, himself, may, indeed, not even know if he is still in asymptomatic stages of the infection.
There is a good reason why the FDA and local state departments of health maintain strict rules regarding the use of donor semen. Under professional guidelines and under many states’ laws, se men from men with whom a woman is not sexually active must be quarantined for at least six months before use. Only once the donor has been retested following the end of this quarantine period, can this semen sample then legally be used for insemi nations at fertility centers. All semen samples available in frozen sperm banks have already undergone such quarantine and, therefore, are safe. Tough regulations and on-site inspections of fertility centers and sperm banks by the FDA make sure of that; - PRIVATE DONATIONS, HOWEVER, DO NOT OFFER THIS SAFETY!
We, therefore, strongly urge women who are considering self-in seminations with donor semen from males with whom they are not sexually active to do it only with help from a commercial semen bank or f a fertility center which will quarantine the

Continued from page 9 10 | december 2022 | The Voice
donor’s semen samples for them. This is not only a legal re quirement but in the best interest and for the protection of the woman, - even if it means waiting for the insemination speci men for six months!
How is Tacrolimus used in female infertility?


This is an increasingly relevant question as more and more pregnant women have been exposed to tacrolimus not neces sarily for infertility purposes but in its main function in cur rent medicine as an immunosuppressive calcineurin inhibitor used to prevent the rejection of transplanted organs or to quiet autoimmune diseases. With increasing numbers of pregnant women in both of these clinical situations exposed to this drug, its safety in pregnancy appears by now quite well established which, in turn, has led to the suggestion that this drug could also be used to achieve immunosuppression for fertility-related clinical circumstances.1
As an immunosuppressive drug, tacrolimus, however, has the usual warnings attached, - that it may increase risks of getting serious infections and develop cancers, especially lymphomas, both risks which increase with length of use and increases in dosage.2 The drug is usually orally administered. To treat cer tain inflammatory, allergic, and autoimmune skin conditions, it, however, can also be administered topically as a cream. There are different brands of tacrolimus on the market under different names (Astagraf XL®, Envarsus XR®, Prograf®). Since their dosing varies, they cannot be used interchangeably! The drug also interacts with many different medications as well as supplements that must be stopped before initiating treatment. A detailed patient history about medication and supplement use of patients considered for tacrolimus treatment is, there fore, essential. Because of expanding plasma volume and, likely,
TRYING TO REACH THE INFERTILITY COMMUNITY?
Have you thought about advertising in the VOICE?
This newsletter every month goes electronically to ca. 80,000 infertility patients, medical professionals in the field, and members of the media, with almost 20% (an unusually high number) also opening the VOICE. For further information, please contact: Ms. Alexandra Rata (212) 994 4400 or e-mail to arata@thechr.com
also because of immunological changes in pregnancy, the dosage of tacrolimus in pregnancy usually must be adjusted up if patients were on the medication before conceiving.

Under US FDA pregnancy rating, tacrolimus is still considered a category C drug, which means that animal studies have shown adverse effects on fetuses and that there are no adequate and well-controlled studies available in humans to define potential ad verse effects adequately. The drug, however, may potentially benefit patients, which may warrant its use despite known risks.

In female infertility tacrolimus has been used in a variety of differ ent indication, widely considered indication for suppression of the female’s immune system. Aside of preexisting conditions requiring this treatment, that has been suggested to include, especially in women with elevated Th1/2 helper cell ratios, repeated implantation failure (RIF), 3,4 and presumed repeat immunological pregnancy loss (RPL), where immune responses to tacrolimus treatment in RIF patients apparently differed based on whether they did or did not have a history of RPL.5
Despite the still very sparse literature on the subject, many other reproductive immunology programs have in recent years incorpo rated tacrolimus almost universally into their treatment protocol for treating these two conditions. As a category C FDA drug, and because of the sparsity of available data, the CHR, however, uses tacrolimus only as a last resort drug, and describes it to patients as a still experimental medication.
1.
2. https://medlineplus.gov/druginfo/meds/a601117.html 3. Nakagawa
4.
5.
Continued on page
REFERENCES:
Le et al., Ther Drug Monit 2020;42(5):518-531
et al. Am J Reprod Immunol 2014;https://doi.org/10.1111/ aji.12338
Bahrami-Asl et al., Geburtshilfe Frauenheilk 2020;80(8):851-862
Hisano et al., Hum Fertil 2021; https://doi.org/10.1080/14647273.2021.1955 415
12
The V oice | december 2022 | 11 ADVERTISEMENT
How is Valtrex (Valacyclovir) used in female infertility?
Valtrex is, of course used to treat selected viral infections, especially including herpes infections. It, therefore, is a so-called anti-viral drug. Since 2004, the drug has been associated with a decrease in NK cells in infertile women. Because of this alleged effect on the female immune system, the drug has been in use at some fertility centers. For what purpose, has, however, not been very clear to us here at the CHR since the sparse literature asserting the NK cell effects,
involved NK cell counts in peripheral blood, which have clearly been demonstrated to differ from endometrial NK cell counts and, indeed, in relevance to female infertility. Bluntly spoken, peripheral NK cell counts are worthless in assessing real functional NK cells in endometrium. Consequently, they really have no predictive mean ing for anything regarding pregnancy and should not be used for any treatment hypotheses. The CHR, therefore, never used Valtrex to treat infertile women, and also does not support such treatments for any reproductive purposes. This, of course, does not mean that Valtrex should not be used in pregnancy for its anti-viral qualities.
REFERENCES:
1. Thomas et al., Am J Reprod Immunol 2004;51(3):248-255
RESERVE THE DATES for the foundation for reproductive medicine conference
(FMRC)
in New York City December 1-3, 2023

The New York Intercontinental Hotel Times Square 111 East 48th Street, New York, N.Y. 10017 TEL: (212) 755-5900
Translational Reproductive Biology and Clinical Reproductive Endocrinology

The mottos: Think differently! and Paradigms you will not hear elsewhere!
FORMAL REGISTRATION WILL START IN EARLY 2023. FOR FURTHER INFORMATION AND/OR PRE- REGISTRATION, PLEASE CALL Alexandra Rata at (212) 994-4400 OR E-MAIL TO arata@thechr.com
If you are interested in exhibiting at the FRMC or if your company is interested in potentially sponsoring conference events, please call Alexandra Rata at (212) 9944400 or e-mail to arata@thechr.com
ADVERTISEMENT Continued from page 11 12 | december 2022 | The Voice
You are a small to mid-sized company in the NYC Tristate area and your current benefit package’s health insurance does not include infertility coverage including IVF because either your insurance company does not offer such coverage or adding it would bust your company’s health insurance budget. Yet, because of difficulties in recruiting and retaining staff, you must become more competitive. We may have the solution: Consider contracting with one of the region’s most accomplished infertility center, serving a world-wide clientele,- The Center for Human Reproduction (CHR) in NYC.
Known as a leading fertility center of last resort all over the world after other centers have failed, imagine by how much more, and earlier, the CHR could be successful if patients reached out to the CHR even earlier in their infertility journey. This is what you now can offer your current and future employees by contracting with the CHR. Instead of coming by air or train, your staff would, in addition, also only have to use the subway.
Based on the company’s employee characteristics and its financial limitations, the CHR of fers highly customized contracts to small and mid-sized companies with 10 to 1000 employees. WOULD YOU NOT WANT TO BE ABLE TO TELL ALL OF YOUR CURRENT AND FUTURE EMPLOYEES THAT YOU NOW CAN OFFER THEM FERTILITY SERVICES AT ONE OF THE WORLD’s MOST ACCOMPLISHED FERTILITY CENTER? If interested in exploring this possibility further, please contact the CHR’s COO, Ms. Jolanta Tapper at (212) 994 4400/ext. 4406 or at jtapper@thechr.com. Like our patients receive highly individualized care, you then will receive for your company a highly individualized offer that meets your company’s needs, while remaining affordable.

A
RECRUITING AND/OR RETAINING EMPLOYEES? CONSIDER GIVING THEM INFERTILITY COVERAGE ! The V oice | december 2022 | 13 ADVERTISEMENT
HAVING
HARD TIME
DR. ALBERTINI’S
Image 1
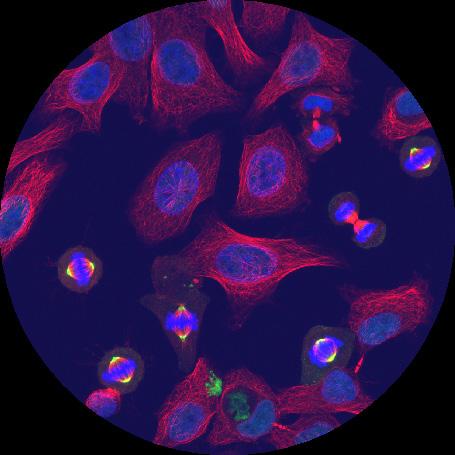
In vitro, literally “in glass”, is a phrase that scientists have used for decades to describe life outside the body of any living multicellular organism. Among some of the first human cells to have been successfully maintained for extended periods of time “in vitro” were those pictured here in an image taken by Professor Albertini many years ago. The cells you see are in very different stages of dividing by the process of mitosis. The DNA of chromosomes is stained with a fluorescent dye (blue), while two other cell components are stained in red (microtubules) or yellow (centrosomes). These cells were first taken from a woman named Henrietta Lacks in 1951 and are known as HeLa cells. They are widely used by cell biologists to study the process of cell division given their prolific growth “in vitro.”

Image 2
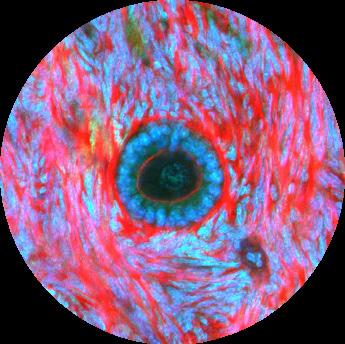
Deep within the structure of the human ovary reside the many so-called ovar ian follicles from which oocytes are obtained during so-called “egg re trievals.” Here is shown an image of one such ovarian follicle but in its earliest stages of development, something we refer to as a primary fol licle. If you look closely, you will notice the circle of blue dots repre senting the nuclei of individual granulosa cells surrounding an inner red circle representing the boundary of a single oocyte; within the oocyte you can see the DNA of the oocyte nucleus that after some 90-100 days of devel opment in the ovary will be ready to retrieve and fertilize. Notice also the dense tissue stained in red that protects and nourishes the follicle during its long journey to eventual ovulation.
At the CHR and other fertility centers, patients that have undergone stimulation and oocyte retrieval next await the re sults of having fertilized their oocytes either by ICSI or IVF. The day after re trieval is known as PN check day when the embryologists examine each egg for the presence of two pronuclei, one representing the DNA from mom and one from dad. Here is shown one of the things that can go wrong during the process of fertiliza tion. Notice two equal sized nuclei and one smaller one which sometimes happen when the oocyte fails to completely eject some of the female chromosomes into, in this case, the second polar body. Such an dysfunctional zygote would be discarded by the embryologists given this abnormal ity in genetic composition.
Image 3
The V oice | no V ember 2022 | 19
Photo Gallery
14 | december 2022 | The Voice
OF
MY
PIECE MIND
 By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.
By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.
As this newsletter noticed on the introductory page, we lived through an unusually tumultuous year during 2022. We, indeed, have been living through unusually unsettling times for at least three years (the start of COVID-19 in late 2019) and , probably, for at least as long as 6 years (the election of President Trump in November of 2016). Which of these time periods ultimately has been responsible for the many changes the world has been experiencing as of this point does not really matter. As history tells us, seeds for historical develop ments often go back for considerable time. But consequences, of course, do matter as they affect all aspects of our current lives.

Continued on page 16
A
What Made us physicians believe we know better than patients what is good for them?
The V oice | december 2022 | 15
I will here only concentrate on certain medical developments,fully recognizing that there, of course, have been innumerable other non-medical developments which in importance may far outweigh the here discussed subjects (i.e., millions of deaths from COVID-19, the Ukraine war, inflation, internal as well as external national security, etc.). But, as many of those other de velopment affecting the country attract most attention, it is also important to note how much the practice of medicine has been and is continuing to change; and I don’t only refer to the intro duction of telemedicine which to significant degrees interrupted the face-to-face contact between patient and physicians and, likely, never will return to the intimacy of the pre-pandemic area.
Economic trends leading to the disempowerment of physicians within the medical industry as a whole have been long in coming, mostly starting with transfer of hospital management from physicians to professional managers several decades ago, the logical formation of hospi tal systems in place of individual independent hospitals in order to be competitive with the in creasing purchasing power of a consolidating health insurance industry. On the physician level, we have witnessed as part of these mega trends secondary trends that saw diminish ing power for department chairs in hospitals and medical schools, as well as a dramatic decline in the importance of private practice physicians in especially teaching hospitals, increasingly moving patient care responsibilities from pri vate practitioners to hospital-employed physicians. Since the 1990s, these develop ments were accompanied by an increasing financial interest of non-medical equity investors in accumulating assets in several private practice-friendly medical specialties (including reproductive medicine and, especially, the IVF field) in competi tion with hospital systems which aggressively have been pur suing the same goal. As a result, most physicians nowadays are employed, as a recent study of the American Medical Association (AMA) reported, while only a few decades ago, a majority owned their own practices and/or were partners in small group practices.1
physicians experienced when owning and managing their own private practices. This stands in contrast to what has been happening in other developed countries, especially in Europe, Israel, Canada, and Australia, which for decades of fered comprehensive national health insurance coverage and where, therefore, private practice represented only a very small percentage of the overall health care system. In most of these countries, private practice has in recent decades, however, significantly grown, often again driven by equity investors (rather than independent physicians) entering the private medical practice marketplace.
In many ways so-called “socialistic” medical systems, therefore, are growing into hybrid “socialistic-market-driv en” systems, while the classical capitalistic health care system of the U.S. increasingly mimics “socialistic’ systems, concentrated in huge bureaucratic organizations of hospital networks or equity-owned clinic networks, recently also joined by medical insurance companies which have also started buying up physi cian networks. In their modus operandi and bureaucracy these huge provider organizations then, paradoxically, end up not much different from government-driven health care plans, and in many cases functioning even worse, as COVID-19 well demonstrated.
“Physicians, thus, increasingly are employed by either large hospital systems or large physician practice networks, either way depriving them of the independence.” earlier generations of physicians experienced when owning and managing their own private practices.
Physicians, thus, increasingly are employed by either large hospital systems or large physician practice networks, either way depriving them of the independence earlier generations of
All of this is, however, only background to what in recent years has changed more than anything else in medicine, - the practice of medicine itself. In parallel to the very obvious loss of physician power in defining our medical system on a national-administrative level, medicine has progressively regressed regarding the likely most important core-pillar of medical practice in the U.S., - the patient-physician relationship which, accord ing to the AMA, to this day is supposed to dictate medical practice.2 This column in the November issue of the VOICE discussed how commercial third party interests increasingly dictate how medicine is practiced. Those intereests, how ever, could not do this without the help of physicians who support these interventions into the traditional patient-phy sician relationship by either issuing professional opinions on which medical insurance companies, hospital systems, or clinical practice networks then base their clinical practice
Continued on page 16 16 | december 2022 | The Voice
guidelines which, of course, usually are primarily driven by economic and not medical considerations. Unfortunately, once again with the help of willing (and well-paid) physi cians, they then are camouflaged as based on “best clinical practice.”
Best clinical practice, of course, exists as a constant desired ideal target of medical practice but, as also discussed in this column before, it is never achieved (as for example a very re cent heart study in JAMA again so well demonstrated3), it is never static, and should never be primarily based on balance sheet considerations of mega-corporate entities. And, theo retically, even truly “best clinical practice,” cannot be imposed upon patients but must, first, receive their appropriately obtained informed consent, unless for obvious reasons that is not possible in certain emergency situations.3
But, to an at times almost absurd degree, many colleagues among us have come to believe that they know better than their patients “what is good for them.” How organized med icine has handled the COVID-19 pandemic in this country and in many other places around the world represents a good example if one analyzes how the medical establish ment went from being “advisors” to the public to being their “dictators.” Politicians would not have failed the COVID-19 management in this country as badly as they did, had they not received bad medical advice from physician-experts who believed that they – and only they - knew “what was best for all Americans.”
To demonstrate how poorly we have managed things here in the U.S. when it comes to the COVID-19 pandemic, Japan, which started grand-scale vaccinations only almost a full year after the U.S., never fully shut down the country, as the U.S. did, never shut down schools, as the U.S. did, and has an older population than the U.S. Nevertheless, the country experienced barely 15% of the U.S. COVID-19 mortality rate.4 Though, considering that no other major developed nation in the world came even close to the Japanese experi ence – it appears truly astonishing how little U.S. media and government appear interested in this observation and one really must wonder why? Could it be that nobody wants to acknowledge that, ultimately, nobody can tell their neighbor what’s best for them when it comes to medical treatments?
The first rule of ethical medical practice is “to do no harm.” After acknowledging these numbers, can medical and government establishments really still deny having done unmeasurable harm to the country and its population? If we do not work on figuring out where we went wrong, we, of course, are destined to repeat the same mistakes.
The trend away from being “advisors” to becoming “dicta tors” to our patients, has been increasingly bothering me for many years because what we have witnessed during the COVID-19 pandemic on a gigantic scale is happening in routine daily medical practice as well. I am here not talking about the extremes, like the allegations we have seen recently in the media that physicians (and major health care insti tutions) treat minors without consent from their parents.5

I am talking about daily routine medical care; and, yes, also in reproductive medicine and infertility: We, for example, pretend to know with certainty that not having twins is good for all of our patients, ignoring not only that having twins is a natural phenomenon but, even more importantly, that infertility patients have a right to wish for twins and that wanting twins can, under certain circumstances, be an em inently rational decision.6 What this subject furthermore in addition teaches us is that one cannot only look at upsides of an intervention; one also must look at its downsides before ultimately judging the value of a procedure (of course also a major lesson of COVID-19 management).
Or we pretend to know that all of our patients’ embryos must be cultured to blastocyst-stage and, of course, must undergo preimplantation genetic testing (PGT-A). This is at least what many patients are telling us they were told without being given an alternative after prior consultations elsewhere. They are, thus, not give any choice, even though nobody has ever demonstrated factual outcome benefits from either practice in anybody but best-prognosis patients. I, of course, could go on with a litany of other “add-ons” to IVF we are literally imposing on our infertility patients because we believe that “we are doing good” for our patients, while imposing on them our preconceived biases. And this is the best-case scenar io because, if for example our recommendations of these treatments were based on financial consideration, the ethical breach would, of course be even more pronounced.
I cannot end this argumentation without also raising the widely disseminated opinion in this country that the best and likely, only acceptable infertility treatment for women above 42-43 years is third party egg donation rather than trying with their own eggs. That this indeed, represents the “common wisdom” of the field is reflected in the minute numbers of autologous IVF cycles performed in women above this age in the U.S. based on CDC and SART regis tries. There are not many women who come to infertility centers to be treated with third-party donor eggs, and I, therefore, never understood how it was possible that we fertility providers do not consider the need for donor eggs a treatment failure. Instead, we find that many infertility cen ters literally “force” patients into egg donation with grossly inaccurate outcome predictions for alternative treatments.
Continued from page 16 The V oice | december 2022 | 17
We here at the CHR always considered third-party egg donation an absolutely last resort and have not only advised and treated our patients accordingly but have also tried to convince our colleagues through publications7,8 that this is how egg donation should be ethically presented to patients. We have also pointed out repeatedly in the literature that outcomes in properly selected women above age 43, while obviously relatively poor, are by no means as low as we constantly hear patients are advised, especially if cumulative pregnancy chances from several cycles are considered.9 We, therefore, were delighted to recently see a publication from our colleagues at Weil-Cornell, reaffirming this point.10
As physicians most of us attempt very hard to serve our pa tients to the best of our abilities. Like every human being, we are, however, subject to biases and, therefore, to often unrec ognized misrepresentations. This recognition alone, should foster humility in our interactions with patients and restrict us to the position of “advisors” rather than “dictators.” We, moreover, also must always recognize a patient’s right to self-determination. In other words, a patient always must be given the last word in determining what she/he considers to be her/his best interest. Our purview ends with explaining to patients their options with all of their respective pros and cons; It is, however, not our responsibility to make decisions for them; it, indeed, appears to me to be unethical to do so and/or to manipulate information in a way that purposefully biases a patient’s information track with the goal of achiev ing a particular outcome. Even if we believe “we know best,” what is “best” for us, is not necessarily “best” for our patients. If we all could agree to this, the practice of IVF would im mediately change dramatically to the better and, considering how pregnancy- and live birth-rates have been declining worldwide, IVF practice would definitely benefit from such a reform.

REFERENCES:
1. https://www.ama-assn.org/press-center/press-releases/ama-analy sis-shows-most-physicians-work-outside-private-practice#:~:tex t=Employed%20physicians%20were%2050.2%25%20of,2018%20 and%2053.2%25%20in%202012
2. https://www.ama-assn.org/delivering-care/ethics/ patient-physician-relationships
3. Jollis et al., JAMA 2022;doi:10.1002/jama.2022.20149
4. https://pandem-ic.com japan-and-us-are-worlds-apart-on-pandemic-mortality/
5. https://thenationaldesk.com/news/americas-news-now/ac cess-to-hormone-therapy-without-parental-consent-increases-teensuicides-study-says
6. Gleicher N. Reprod Biomed Online 2022;44(1):1-4
7. Gleicher et al. J Assist Reprod genet 2020;37(7):1583-1588
8. Gleicher et al J Endocrinol 2016;230(1):F1-6
9. Gleicher et al., Reprod Biomed Online 2018;37(2):172-177

10. Romanski et al., Obstet Gynecol 2022;140(5):743-750
TRYING TO REACH THE INFERTILITY COMMUNITY?
Have you thought about advertising in the
This newsletter every month goes electronically to ca. 80,000 infertility patients, medical professionals in the field, and members of the media, with almost 20% (an unusually high number) also opening the VOICE
For further information, please contact: Ms. Alexandra Rata (212) 994 4400 or e-mail to arata@thechr.com
Continued from page 17 18 | december 2022 | The Voice
ADVERTISEMENT
EMBRYOLOGY LABORATORY SUPERVISOR FOR RESEARCH

The CHR is searching for a candidate for the newly created position of Embryology Laboratory Supervisor for Research. The CHR’s em bryology laboratory, under a single laboratory director, is in the process of being reorganized into three distinct areas with separate supervisory responsibilities: (i)clinical, (ii)administrative, and(III)research.


Supervisors in all three areas must hold PhD degrees (or equivalent) and be fully trained human embryologists with sufficient historical professional experience to hold a supervisory position.


While such human embryology experience is preferred for this new position as well, priority qualifications are a record of excellence in reproductive biology research, documented by publications in prestigious peer-reviewed journals and, in absence of human IVF experience, at least substantial animal IVF experience allowing for relatively quick in-house training in human IVF.
Besides a competitive salary and benefit package, the CHR also offers in this position a unique financial incentive-structure linked to the success of the center’s research activities, as demonstrated by publications in prestigious peer-reviewed journal. Moreover, this position will also be eligible for the opportunity to earn shared ownership in research-driven new start-up companies and the center itself.
If you feel that you qualify for this position, please submit your CV and a brief application letter to the CHR’s COO, Ms. J. Tapper, at jtapper@thechr.com. The position is available immediately. All submissions are considered confidential.
hirinG
ADVERTISEMENT
Center for
The V oice | december 2022 | 19
AT THE CHR
Learn more by accessing our library of educational videos: https://www.centerforhumanreprod.com/contents/video-gallery
Human Reproduction
THE FOUNDATION FOR REPRODUCTIVE MEDICINE YEAR-END DONATIONS

Coming to CHR after having received treatments at other fertility centers, patients are often surprised how differently CHR approaches their fertility problems. This does not happen by accident but is heavily data-driven and, therefore, dependent on ongoing research. CHR’s research budget over the last decade has, indeed, grown more rapidly than any other budget items.
For all of those years The Foundation for Reproductive Medicine, a notfor-profit research foundation, has generously supported parts of CHR’s research efforts and CHR, in turn, has generously financially supported the foundation. Exclusively dedicated to research in reproductive biology and reproductive clinical endocrinology and the dissemination of state-of-thearts knowledge to colleagues, it has been my honor to serve as the founda tion’s president.
I, therefore, today ask you to consider a year-end gift to support the mis sions of The Foundation for Reproductive Medicine. Because CHR is com mitted to cover all of the foundation’s overhead costs, 100 percent of your donation will go straight to research-related activities. The foundation at times also supports research at other institutions. For example, with the help of CHR, the foundation supports a shared research position between Rockefeller University and CHR. The foundation’s largest commitment is an annual international conference on translational reproductive biology and reproductive endocrinology in New York City. As a not-for-profit foundation, your donation is tax-deductible according to law.
We live in very exciting times, where major progress in the field seems to lie just around the corner. Your generosity will help us take advantage of existing research opportunities to further advance scientific knowledge and treatment outcomes in infertility.

ADVERTISEMENT scan to donate! 20 | december 2022 | The Voice
Norbert Gleicher, MD

The V oice | december 2022 | 21
the chr’s interpretation of RECENT LITERATURE, relevant to REPRODUCTIVE MEDICINE
Mostly placed into a clinical context, we in this section of the newsletter offer a survey of articles in the English literature, usually published in the preceding month, which the CHR found of interest to the current practice of clinical reproductive endocrinology and infertility, - even if at times not immediately applicable to daily clinical practice. These articles, however, nevertheless often point out where clinical practice will likely go and, therefore, serve an important translational purpose. Translational research has been the CHR’s principal research goal since its founding in 1981, has produced a significant num ber of U.S. patents over the years, and has propelled the CHR into its current position as a worldwide center of last resort for infertile patients who have failed treatments elsewhere.
Pregnancy
The long-term effects maternal medical conditions can have on offspring are increasingly coming into focus. Using Danish national health registers, Chinese and Danish investigators used 2 437 718 Danish citizens between 1978 and 2018 born alive as their study population, trying to elucidate the impact of maternal hyperten sive conditions (MHC) on offspring, with the primary outcome being all causes of death up to age 41, statistically considering several confounders Among the total population studies, 102 095 mothers experienced a MHC, - the overwhelming majority (n=67 683) preeclampsia, 679 eclampsia, and 33 733 hypertension of pregnancy. In 41 years of follow-up (median 19.4 years) 781 death were recorded (58,94/100 000 person years), among those with
preeclamsia 17 (133.73/100 000), 22 to eclampsia (133.73/100 000), 223 to hypertension (44.38/100 000), while only 19 119 deaths in women without MHC resulted only in a death rate of 41.99/100 000 live years, for a significant difference in mortal ity between MHC- and non-MHC-exposed mothers (95%CI 0.11% to 0.64%). Significant increased risks were observe for the following causes: death in perinatal period, cardiovascular diseases, digestive system diseases, and endocrine, nutritional, and metabolic diseases combined. Risk were, moreover, more pronounced with early onset severe preeclampsia, MHC + diabetes, or MHC + low educational level.
These are, of course, a highly disturbing findings because mor tality is an extreme outcome, suggesting that milder adverse outcome consequences very likely are even more substantially present in offspring of mothers with MHC in pregnancy. Not only do these findings, therefore, call for further investigations of such effects but they also demonstrate an urgent need for prevention of MHCs, wherever and whenever possible. The
22 | december 2022 | The Voice
Effects on mortality to young adulthood from birth to mothers with maternal hypertensive disorders of pregnancy
Continued on page 23
next paper we discuss, indeed, addresses the prevention of chron ic diseases in offspring.
REFERENCES
1. Huang et al., BMJ 2022;379:e072157
Investigators form the Harvard TH Chan School of Public Health in Boston, MA, in a recent paper estimated the impact of prenatal supplementation with iron and folic acid , multiple micronutri ents, and calcium at 50%, 75%, or 90% coverage on future non communicable diseases by age and sex for the year 2015. Using secondary data sources from 132 countries, they estimated the impact of prenatal supplementation on diabetes, hypertension, and death from noncommunicable diseases, reaching fascinating conclusions: At 90% coverage, over 51 000 noncommunicable dis ease deaths, 6 million cases of hypertension, and 3 million cases of diabetes could be prevented per birth cohort if mothers were prenatally supplemented at 90% coverage. For iron and folic acid, the numbers would be roughly half of that and calcium supple mentation at 90% would delay 51 000 per birth cohort as well.
Putting these two papers together in their respective effects on birth generations, one is left wondering why it took us so long to understand the importance of the intrauterine environment on the future health of offspring. After all, we have now known for decades that the nine months we spend in utero in our mothers from an epigenetic point of view are the most important months in our existence. It appears increasingly obvious that we are miss ing a huge public health opportunity by not learning to maximize the intrauterine environment during this time period.
REFERENCES
1. Blasted et al., Am J Clin Nutr 2020;116():1291-1302
To continue the theme of how the intrauterine environment affects the postdelivery life of chil dren, few subjects have re mained as controversial as the consumption of coffee during pregnancy by preg nant women. Even rather modest consumption
of coffee has been in the literature associated with lower birth weights.1 One factor implicated was lower birth length.2 The same group of investigators, therefore, now followed up on their earlier paper by directly associating maternal caffeine consump tion during pregnancy with shorter child growth between ages 4 and 8 years. Somewhat unexpected there were this time no clear patterns of weight or body mass index changes. In early childhood maternal coffee consumption, even in small amounts, therefore, per the authors, appears associated with shorter stature in off spring up to age 8. 3 Whether this observed shortening of stature also continues into older age, was not investigated.
To be honest, we have always been somewhat skeptical about all the allegations against coffee in pregnancy. After all, Italians, French, and Austrians, all three local cultures addicted to coffee, do not appear particularly different from other European natures with other preferences in ether weight or height. But then hold on for a moment, haven’t we all been wondering why Italians, despite all the pasta they are consuming, are rarely overweight? Maybe we just found the answer: it’s all the espressos their moth ers drank during pregnancy! (JUST JOKING!)
REFERENCES
1. Chen et al., BMC Med 2014;12(1):174
2. Gleason et al., JAMA Netw Open 2021;4(3):e213238
3. Gleason et al., JAMA Netw Open 2022;5(10::e2239609
–but this time good news
That women of African descent in general have lower IVF preg nancy and live birth rates than Caucasian and Asian women has been reported for decades.1 Though the underlying causes have remained unknown, CHR investigators years ago demonstrated significantly differing distributions in the repeat CGG pattern of the FMR1 gene between women of African descent and Caucasian as well as Asian (Han Chinese) women, which, at least in part, could explain this difference.2
Now, however, come colleagues form Lenox Hill Hospital’s Perinatology Division here in NYC with a very interesting related study that suggests that, when it comes to maternal and neonatal complications in pregnancies con ceived through IVF, the picture goes the opposite way, with women of African descent demonstrating significantly lower complication rates.3 Using the CDC’s natality based between 2016-2018 of as non-Hispanic Black and non-Hispanic White self-iden tified women (n=8 485 531,
The V oice | december 2022 | 23
Can micronutrients given to pregnant women in pregnancy prevent chronic diseases in offspring?
Does maternal coffee consumption in pregnancy shorten the stature of her offspring?
More evidence for differences in IVF outcomes for women of African descent
Continued on page 24
Black 1 788 197, 21%; White 6 697 334, 79% ). Black women had sig nificantly lower risks for gestational diabetes, hypertensive disorders of pregnancy, and eclampsia in comparison to white women. On the neonatal side, the need for immediate and prolonged neonatal ventilation was also significantly lower, even though Black women demonstrated significantly more APGAR scores below 7. There were no differences in several other maternal as well as neonatal parameters.
These are surprising, though very welcome findings, considering all the bad news over many years about lower pregnancy and live birth rates after IVF in women of African descent. Though the authors of this research letter in the American Journal of Obstetrics & Gynecology are to be congratulated for discovering a very important and previously unknown finding, we must politely disagree with part of their conclusions, which interpreted their findings as further evidence in support of social factors being the primary culprits in observed outcome differences. Considering that the findings went in exactly the opposite way to well-established finding regarding IVF cycle outcome and, considering that social factors usually affect out comes toward the negative, we would argue that this study actually further strengthens those who suggested that biological (i.e., genetic) factors dominate in affecting IVF cycle- as well as pregnancy-out comes, with social factors mostly only playing minor roles.
This conclusion is also supported by several other observations: Once the effects of a fresh IVF cycle are removed from consider ation, as is the case in frozen embryo transfer cycles, all IVF out come differences between Caucasian and African American women disappear, even if Black women present with more fibroid uteri.4 Moreover a just presented abstract at the 2022 ASRM Scientific Congress and Expo in Anaheim, CA, demonstrated that race, and not neighborhood deprivation, predicted IVF success.5
REFERENCES
1. Humhries et al., Am J Obstet Gynecol 2016;214(2):212.e1-212.e17
2. Gleicher et al., PLoS One 2011;6(4):e18781
3. Bar-El et al., Am J Obstet Gynecol 2022;227(4):661-664
4. Csokmay et al., Fertil Steril 2011;95(1):89-93
5. Andre et al., ASRM Scientific Congress & Expo; oct. 22-26, 2022, Anaheim, CA
Cardiomyopathy in pregnancy
A cardiomyopathy (CM) is defined by structural and functional abnormalities of the ventricular myocardium in absence of other causes of myocardial disease. British investigators now published a systematic review and meta-analysis regarding pregnancy outcomes in women affected by a CM and the picture they ended up drawing is not a very attractive one: Unsurprisingly, women with CM more likely delivered by Cesarean section than women without cardiac disease or women with heart diseases other than CM. They were also at significantly increased risk for severe cardiovascular events during pregnancy (~7-fold) and had significantly higher in-hospital mortal ity than controls and other cardiac patients (~4-fold).1 The maternal risks of so-called peripartum CMs (PPCMs), as already the name indicates, can carry over into the postpartum
period.2 In practical terms this means that women with CM must be informed of these risks before deciding on conception and may even have to be protected from conceiving. If such a patient nevertheless conceives, seeks to conceive, or is for the first time diagnosed in pregnancy, she must be considered an extremely high-risk patient who should only be delivered in a tertiary care center with an appropriate multi-specialty team of physicians being pulled together to manage such patients. For whoever is interested in more detail on the subject, we recommend the 4th edition of “the bible” of textbooks on cardiac disease in pregnancy by our friend Uri Elkayam, MD, professor of cardiology at USCLA, Cardiac Problems in Pregnancy 3
REFERENCES
1. Eggleton et al Am J Obstet Gynecol 2022; S0002-9378(22)00524-5. doi: 10.1016/j.ajog.2022.06.048. Online ahead of print.
2. Davis et al., J Am Col Cardiol 2020;75(2):207-221
3. https://www.wiley.com/en-us/ Cardiac+Problems+in+Pregnancy,+4th+Edition-p-9781119409793
More bad news on cannabinoids and pregnancy
That cannabinoids have become a regular topic in this newsletter in recent months and years is no accident but is directly linked to their increasing legalization around the country that has led to an explosion in use as well as abuse. A new review article by col leagues from the Oregon Health & Science University in Portland, Oregon,1 where cannabis was first legalized, therefore, is not only timely but also urgently needed because this drug is, of course, especially popular among people of reproductive age. This, as the authors point out, is especially concerning because cannabis exposure has been unequivocally demonstrated to exert adverse effects on female as well as male reproductive health. Continuing above raised subject of maternal effects on the long-term health of their offspring, there, however, is also increasing evidence in the literature that maternal cannabis exposure of mothers in pregnan cy has adverse effects on the fetus as well as longer-term offspring health and developmental trajectory.
In males use of cannabis has not only been reported with adverse effects on fertility but also with erectile dysfunction, abnormal spermatogenesis, and testicular atrophy. In women, it has not only been associated with infertility but also with abnormal implanta tion and development of embryos. Its main psychoactive com ponent, delta-9-tetrahydrocannabinol, also crosses the placenta into the fetus and can also be found in breast milk, explaining why adverse effects on offspring have been reported, including small-for-gestational-age infants, premature births, neurodevel opmental changes, and impaired socio-behavioral and cognitive development.1
Considering the explosive growth in cannabis consumption in the U.S., we strongly recommend this review article, which gives comprehensive insights into a subject, likely for political reasons, clearly not getting the attention it deserves.
Continued from page 23 24 | december 2022 | The Voice
REFERENCE
1. Lo et al. Am J Obstet Gynecol 2022;227(4):571-581
Gestational diabetes
Another subject that does not get adequate attention in our opinion is the increase in diabetes mellitus (DM) prevalence in the population and, with it of course, the increase in prevalence of gestational DM (GDM). A comprehensive review article by Australian and British colleagues in Endocrine Reviews, there fore, is also timely.1 We strongly recommend this article for its thoroughness and attention to detail but, at the same time were disappointed that, in explaining the rapidly rising prevalence of DM and GDM, the authors once again only hold epidemi ological facts, mostly the increase in obesity in modern societ ies, responsible. They, like the literature in general, completely ignoring that with the introduction of insulin supplementation, mankind has interrupted the evolutionary barrier nature had set up to reproduction that prevented the genetic risk for the polygenic disease of DM to be passed on to future generations by preventing almost all diabetic patients from conceiving and/ or causing miscarriages after conception. With diabetic patients now having identical delivery rates to non-diabetic women, they are supercharging the inheritance of polygenic diabetes risk and, hardly ever acknowledged, greatly contributing to the rapid growth of DM and GDM prevalence. In contrast to this very obvious omission, the paper, however, does point out well that the consequence of GDM is not only DM but also for cardio-vas cular disease (i.e., metabolic syndrome).
REFERENCE
1. Sweeting et al., Endocrine Rev 2022;43:763-793
Gynecology
Endometriosis news
An abstract by Harvard researchers out of Boston, MA, reported at the annual ASRM conference in Anaheim, CA attracted con siderable attention1 but had already in August been reported in Human Reproduction. 2 The study focused on proteomic plasma profiles in endometriosis patients and found an association with 15 plasma proteins. Using data from the Nurses Health Study II, researchers analyzed 200 blood samples in women with laparo scopic ally confirmed endometriosis and matched controls for 1,305 biomarkers for immunity, angiogenesis, and inflammation and found 15 to be associated. Considering the long-known association between endometriosis and hyperactive immune systems, it was surprising that the investigators claimed to be surprised to find multiple pathways related to migration of in nate immune cells upregulated in endometriosis.3 This and more is, indeed, exactly what we would have expected.
REFERENCE
1. Sasamoto et al., Fertil Steril 2022;116(Suppl)
2. Hum Reprod 2022;37(9):2042-2053
3. VanDewater K. https://www.healio.com/ news/womens-health-ob-gyn/20221024/ endometriosis-associated-with-plasma-protein-levels
Polycystic ovary syndrome (PCOS) news
A recent Chinese paper in Endocrine claimed to have discovered 8 genes, among those the hub gene GNB3 as “the most important regulatory gene in PCOS.”1 Considering that PCOS patients were not properly identified and, as unfortunately is usually the case in PCOS studies, apparently no differentiation was made between PCOS phe notypes, we have a hard time in accepting this study. One can only wonder why investigators of PCOS, who supposedly are experts on this condition, do not understand the importance of differentiating between different phenotypes. We have made this point repeatedly before in these pages, unless PCOS research starts all over again with “clean” patient populations, the current decades-long stagnation in our understanding of this condition will continue.
REFERENCE
1. Qiao et al., Endocrine 2022;78:615-627
Hypoactive sexual desire disorder
Female hypoactive sexual desire disorder (HSDD) is to this day a poorly understood, - yet quite frequently encountered condition in gynecology as well as infertility practice. Currently only two medi cations have been improved for this condition, both only minimally effective and probably not worth the money. Now increasing evidence is appearing in the medical literature that suggests that kisspeptin, a hypothalamic activator of the reproductive hormone axis, may be more effective. When intravenously injected. It was in a prospective ly randomized study well tolerated and was associated with brain processing of erotic stimuli and facial attractiveness. This study may, indeed, open new options for the treatment of HSDD
REFERENCE
1. Thurston et al., JAMA Netw Open 2022;5(10):e2236131
Infertility
In vitro maturation of immature oocytes
In vitro maturation of immature oocytes is by most IVF centers not considered a particularly urgent need and they, therefore, usually pretty automatically discard GV oocytes. At the CHR the situation has, however, for years been quite different because, considering, the center’s highly unusual and very unfavorable patient population, every lost egg must be at all costs avoided. Consequently, under our motto, “we fight for every egg and embryo,” attempts at in vitro matu ration of immature oocytes have been routine for years.1
This is why a recent paper by C. Yiding Andersen’s group in Copenhagen, Denmark caught our close attention in which he reported that oocyte diameters predict the maturation rate of hu man immature oocytes.2 In their study they found oocyte diameter
Continued on page 26 The V oice | december 2022 | 25
positively associated with MII stage, with MIIs demonstrating a significant larger diameter than MI and GV oocytes as well as degenerated oocytes. The mass of a follicle’s cumulus cells was, furthermore, significantly asso ciated the MII stage. These findings reemphasize the mutual depen dency of the follicle and egg on its surrounding microenvironment made up of mostly cumulus cells and suggests that the diameter of the oocyte to a degree is indicative of nuclear maturation, a poten tially important predictor of which immature oocytes may benefit from in vitro maturation and may ultimately lead to pregnancy. Within this context, we also need to acknowledge that CHR’s investi gators already in 2015 among several oocyte parameters only found oocyte diameters to be predictive of IVF outcomes.3
At the same time, we have to call for a cautious assessment of these very interesting data because the authors did not pay attention to pa tient-ages in their analyses. CHR investigators, however, in a study, currently submitted for publication and under review, reported that the outcomes of in vitro maturation of MII, MI, and GV oocytes significantly change with advancing female age, and do so in rather unexpected ways (which currently cannot yet be reveal since the manuscript is under review). Stay tuned, we predict interesting new developments on this subject!
REFERENCES
1. Lee et al., Endocrine 2016;52(1):165-161
2. Pors et al., J Assist Reprod Genet 2022;39(10):2209-2214
3. Lazzaroni-Tealdi et al., PLos One 2015;10(12): e0143632
Pregnancy chances with IVF in very poor prognosis patients
Likely the strangest advice many of our new patients tell us they had before received at other IVF centers is that their live birth chances were in the 0-2% range. Most patients who reach out to the CHR after receiving such advice, are either women above ages 42-43 years or younger women with very low AMH levels. We, of course, know that only very few women, usually above age 45-47 really have such low chances; most others, even if their chances are low, have sig nificantly better chances than in the 0-2% range. Moreover, if such poor prognosis patients enter their treatment with eyes wide open,
recognizing their small chances per cycle, but experiencing, of course, accumulating chances with repeated cycles, their futures are by no means as bleak as most IVF centers present them to be in their usual attempts to push pa tients into third-party egg donation.1,2
We now were pleasantly surprised when not ing a paper from our Weill-Cornell colleagues that basically made the same point:3 In this paper the authors reported IVF cycle outcomes of women with very low AMH levels of 0.3ng/ mL or lower, stratified for age. They then compare outcomes with reference live birth to the national SART reports for the same time period.
Results were for several reasons fascinating: As they first demonstrated (in Figure 1) in every age group their study group significantly underperformed national SART data for the same age groups by over 50%. This, of course, does not sur prise since most IVF centers in the US will advance a patient with AMH of <0.3ng/mL very quickly into egg donation. The national data, therefore, represent a much more favorably se lected patient population. With study and SART data declining with advancing female age, live births above age 42 years were in 1st cycles in the Cornell population only at 1.2% and only at 4.1% in SART. When, however, all cumulative treatments were considered (Figure 2 in the paper) differences between the Weill-Cornell study group and SART data disappeared at all ages, with live birth rates being 4.0% and 4.1%, respectively (and CHR’s rates above age 42 are, moreover, even better). In short, our Weill-Cornell colleagues are to be congratulated on a very interesting study that confirms that currently widely distributed practice of sending women above age 42 pretty automatically into third-party egg donation deserves reconsid eration, even if patients are considered to have poor prognosis.
REFERENCES
1. Gleicher et al. Reprod Biomed Online 2018;37(2):172-177
2. Gleicher et al., J Assist Reprod Genet 2020;37(7):1583-1588
3. Romanski et al., Obstet Gynecol 2022;145(5):743-750
Reproductive immunology
Intravenous
There are very few issues in infertility that are as controversial as the concept of immunological pregnancy loss. To this day, many colleagues in the field, still, simply do not want to believe that the maternal immune system must play a major role in the establishment of pregnancy because the implanting
26 | december 2022 | The Voice
gamma-globulin (IV-Ig) treatment in women with repeated pregnancy loss
Continued from page 25
embryo, unquestionably, is a semi-allograft and, therefore, under most-basic ground rules of immunology should be rejected by the maternal immune system. That this does not happen in normal pregnancies is a principal reason why all of us are in this world, and basically establishes that the maternal immune system must change its activities, so that the implanting embryo is not rejected. As we also know, practically every physiological process in our bodies can mal function. One, therefore, with considerable certainty can assume that whatever tolerance pathways the maternal immune system induces to prevent rejection of a normally progressing pregnancy, induction of these pathways may on some occasions go awry. And this brings us to a subject that may be even more controversial in the field of infertility than the issue of repeated immunological pregnancy loss, and that is its prevention and/or treatment.
It is rare to be able to bring to our readers’ attention a publication in reproductive medicine that offers answers to two highly controversial subjects that have remained unresolved for decades. We, therefore, are delighted to be able to report on an important clinical study conducted and published in the prestigious general medical journal eClinical Medicine (a Lancet family journal) which usually is not on the reading list of most infertility specialists. We, therefore, in this issue of the VOICE will dedicate a little extra space to this important paper.1 Here is a summary:
After a literature search that confirmed for the investigators that there was no accepted universal definition of “unexplained recurrent pregnancy loss, they chose a properly conservative definition for patient selection for their study (four or more losses, with chemical pregnancies not counted). They also correctly concluded that, therefore, no standard treatment existed and that, whatever prospectively randomized studies had been published, they found no supporting evidence for paternal lymphocyte immunization, predni sone, low dose aspirin, and/or anti coagulant treatment, and progester one support. Regarding IV-Ig, they noted no convincing prior evidence in the literature for medium dose treatment (20-50gm), - though in our opinion some studies have suggested a positive effect. They, therefore, decided on a more rigorous patient selection than any prior study had chosen that included four or more miscarriages among which at least one had to show evidence of chromosomal-normal
products of conception. Besides a more rigid patient selection, they also decided to test the effectiveness of IV-Ig at high dosage (100gm). Finally, and likely their most controversial choice, they chose to initiate treatments post-conception at 4-6 weeks gestation al age. Some prior studies suggested that earlier treatments prior to implantation had better outcomes.2
They then initiated a well-designed double-blind prospective study in which they compared administration of 400mg/kg of IV-Ig with administration of a placebo over five consecutive days (20gm/day). The primary outcome was ongoing pregnancy rate at 22 weeks, while live birth was the secondary outcome. Analysis was based on intention to treat. Excluded were only women who miscarried and were found to have miscarried chromosomal-abnormal pregnan cies. The study was, moreover, registered with ClinicalTrials.gov with number #NCT02184741.
After exclusion of three study subjects, 50 women assigned to the treatment arm and 49 to placebo made up the study population. At 22 weeks, pregnancy rates were 29/50 (62.0%) and 17/49 (34.7%), respectively (OR 3.07, 95%CI 1.35-6.97, P=0.009) in favor of IV-Ig. The live birth rates were 29/50 (58.8%) and 17/49 (34.7%, OR 2.60, 95%CI 1.15-5.86, P=0.03. If only women who received IV-Ig in weeks 4 and 5 were assessed (excluding women who received the medication in week 6), outcome advantages for IV-Ig were even higher (P<0.001 and P=0.003. respectively), supporting the conten tion that earlier administration, as noted above, may produce even better outcomes.
The study, however, also produced somewhat worrisome findings which clearly demand further clarifications: four newborns in the IV-Ig group and zero among controls were born with congenital abnormalities. Those included one case of atrial septal defect, a case of cleft lip/palate, a case of congenital hearing loss, and a case of ventricular septal defect/cerebral cyst. This not only a clinically worrisome finding but also makes one wonder whether repeated unexplained pregnancy loss by immune system activation cannot also in at least some cases been seen as an evolutionary protec tion mechanism from birth of congenitally abnormal offspring. One also wonders why the authors did not address the difference in congenital abnormalities and how come the editors of the journal allowed this omission.
Also important to note but, in contrast to above noted congenital abnormalities, not necessarily unexpected, IV-Ig patients demonstrated earlier gestational age at delivery (36w1d vs. 39w2ds, P=0.004) and preterm before 37 weeks ( 10, 34.5%, vs. 1, 5. 5.9%, P=0.007), and more fetal growth restriction (10, 38.0% vs 0, 0%, P=0.008), leading to small for gestational age births. These
Continued on page 28 The V oice | december 2022 | 27
are, as repeatedly discussed in this newsletter before, findings for decades associated with immune problems in pregnancy and explainable by early termination of tolerance in “rescued” pregnancies.
As so many times in medicine and science in general, a good study frequently generates more questions than it answers. What we deduct from this study are, however, a few import ant conclusions, some more likely to be correct than others: (i) Unsurprisingly, so-called unexplained repeated pregnancy loss does, likely, not represent a homogenous group of patients: Many among them, indeed, suffer from immunological causes, and among those treatment with IV-Ig improves delivery chances, though with increased risks for late pregnancy complications and, possibly, congenital abnormalities. (ii) Timing of IV-Ig ad ministration must occur before five weeks of gestational age, and based on earlier studies, may, indeed, be best timed shortly be fore implantation. (iii) Patients receiving IV-Ig must be advised of a possible increase in fetal risks for congenital abnormalities, premature labor and delivery as well as growth restrictions. Not noted in the paper, but the CHR’s experience for decades, women with repeated immunological miscarriages who are well managed beyond their miscarriage risk, remain at higher risk for intrauterine fetal death in the 3rd trimester, as well as preeclamp sia and gestoses of pregnancy. They, therefore, must receive close maternal as well as fetal surveillance, starting at 26 weeks.
We do not believe that this study established 100gm as the ideal dosage for IV-Ig treatment. It, however, suggests that at 25gm, 40gm, and 60gm, the latter dosage in women with active auto immune diseases, we here at the CHR may currently under-dose some patients (CHR has been using IV-Ig in selected repeat aborters for almost 40 years). Because IV-Ig is expensive and, if administered only for fertility purposes (miscarriages included), often is not covered by insurance, we will continue to use IV-Ig only for patients who have failed less costly treatments and/or have severe immune system activation. We, however, will aban don the lowest 25gm dosage and start with 40gm, go to 60gm in more severe and to 100gm in most severe cases.
REFERENCES
1. Yamada et al., eClin Med 2022;50:101527
2. Yang X, Meng T. J Immunol Res 2020; 2020:6672865
The importance of sexual intercourse (i.e., exposure of the female immune system to semen) for the development of the immune system in young women
To stay with the topic of tolerance induction to the fetal semi-al lograft by the maternal immune system, another potentially important paper just appeared in a prominent general science journal called eLife, 1 like the previously noted eClinical Medicine not usually on the reading list of fertility specialists. But to bring such papers, otherwise frequently overlooked by the field of
reproductive medicine, to the attention of reproductive endocrinolo gists and other clinical staff in the field, is exactly the purpose of here presented literature reviews.
In this paper researchers from the U.S., Africa, and Europe inves tigated adolescent girls and young women at high risk for sexually transmitted infections with the intent of determining whether the onset of sexual intercourse leads to a change in immune mediators in the cervicovaginal tract. Though the purpose of this paper was to determine risk factors for infections, we are interpreting the impor tance of this paper from a more reproductive immunology viewpoint, asking what this paper potentially teaches us about the longstanding hypothesis that exposure to semen represents a female’s first exposure to the partners HLA and, therefore, likely represents a first signal to a future mother’s immune system that allows the immune system to “familiarize” itself with paternal antigens, potentially, start an appro priate induction process for tolerance pathways.
Assessing 20 immune mediators through cervicovaginal lavage before and after first penile-vaginal intercourse and, in addition, combining the results of their study with previously reported data by meta-anal ysis. Consistently 19/20 of those immune mediators increased after first intercourse. Moreover, concentrations of these immune medi ators increased cumulatively over time, roughly doubling every 5 months. The authors’ systematic review identified two other eligible studies with similar results.
Our principal conclusion from this study, thus, is that first (and subsequent) intercourse clearly activates the female immune system. One can further argues that this would not happen unless there was a physiological reason for it. One such reason undoubtedly is the defense against invading organism during intercourse. But in view of infections with certain helminths we have previously discussed in these pages 2 which were shown to induce tolerance pathways against helminths that apparently also favored tolerance of a fetal semi-al lograft, these data can also be interpreted as supporting the notion that sexual intercourse induces immune changes in the female that later-on potentially favor implantation and successful pregnancy.
REFERENCES
1. Hughes et al., eLife2022;11:e78565
2. Blackwell et al., Science 2015; 350(623):970-972
Reproductive genetics
More on Preimplantation genetic testing for aneuploidy (PGT-A)
Let us start by saying that there is really nothing new at the PGT-A front: PGT-A does not improve IVF outcomes and in some women, actually, reduces pregnancy and live birth chances (that is especial ly true for patients who produce only few embryos). That PGT-A improves IVF outcomes in older patients is not only logically absurd, practically impossible, and only the result of blatant ignorance about statistical processing of data. A recent so-called systematic review by
Continued from page 27 28 | december 2022 | The Voice
Chinese colleagues in Obstetrics & Gynecology 1 is, therefore, absurd and reminds of the old IBM tenant, - “garbage in, garbage out.”
Yet the commercial exploitation with PGT-A continues at IVF centers worldwide, wile the genetic testing industry is already on the way to expand this exploitation even further, as increasing numbers of test ing laboratories in the US are starting to offer polygenic risk screen ing (PGRS) of embryos. Since we discussed this subject repeatedly in the past, we do not wish to be repetitive, even though CHR finds it astonishing that so many genetics laboratories (and IVF centers) are pursuing PGRS, even though a major European society of geneticists declared this an “unethical procedure.”2 However even more surpris ing, neither ASRM nor FDA have been commenting on this newest abuse of IVF patients. But who can be surprised, considering their decades-long inactivity in regard to PGT-A.
But not all news is bad news, considering that most of the IVF world until relatively recently either did not use or even discarded every embryo that demonstrated even only a smidgen of aneuploid DNA in a trophectoderm biopsy. Fortunately, that is no longer the case, as two recent guidelines from professional societies regarding the manage ment of so-called “mosaic” embryos demonstrate. 2,3
Though mentioned in the same sentence and addressing the same issue of what to do with mosaic embryos, these two guidance documents are not comparable. The first document issued by the Preimplantation Genetic Diagnosis International Society (PGDIS) is basically not worth the paper it is written on.2 It is within itself contradictory and full of totally incorrect statements, lacks all trans parency as to the obviously conflicted status of the PGDIS and the authors of the document who practically all make their living from PGT-A. Moreover, the document really makes no real recommenda tion, though hints at the possibility of transferring “mosaic” embryos. The second document, just recently released by ESHRE, 3 though also far from perfect, at least recognizes most of its shortcomings and is, in contrast, a true guidance document offering all the requisites expected from practice recommendations issued by a professional society. It also clearly supports the transfer of “mosaic” embryos. Both societies, thus, more-less, reflect the fact that increasing num bers of embryos, which just a few years ago would never have been transferred, now often are transferred. And this is good news because it means that huge numbers of perfectly good embryos that used to be discarded now are given a chance of pregnancy.
We, however, always wonder how our colleagues feel after for so many years promoting the discarding of huge numbers of perfectly fine embryos, when now recommending the transfer of exactly the same embryos? We also wonder how they feel about the large number of additional IVF cycles they, therefore, unnecessarily conducted on their patients? And how about all those women who finally went with donor eggs, while they could have gotten pregnant with their own? We are still waiting for their “mea culpa!”
With the transfer of selected “mosaic” embryos being declared “ko sher,” we now see a plethora of reports in the literature from all over
the world trying to tell us which “mosaic” embryos should or should not be transferred.4-6 Together with both of above noted formal society guidances they all, however, still suffer from the fact that PGT-A laboratories all over the world continue to define “mosaicism” incorrectly. For as long as the PGT-A laboratory community does not switch to the worldwide recog nized correct definition of mosaicism which is, “presence of two or more cell lineages in one organism,” and sticks to their false definition of “mosaicism,” which is, “presence of two or more cell lineages in an on average 5-cell embryo biopsy from trophec toderm,” the field will over-diagnose normal and aneuploid, and underdiagnose mosaic embryos. And as a consequence, good embryos with normal pregnancy potential will continue to be disposed of or not used.
REFERENCES
1. Cheng et al., Obstet Gynecol 2022;140(5):769-777
2. Leigh et al., Reprod Biomed Onlien 2022l45(1):19-25
3. ESHRE Working Group on Chromosomal Mosaicism. Hum Reprod Open 2022;hoac044
4. Yakolev et al. Reprod Biomed Online 2022;45(1):88-100
5. Ai et al., Reprod Biomed Online 2022;45(1):54-62
6. Chen et al., Reprod Biomed Online 2022;45(1):2634
Why the first mitotic division is so important in an embryo
Now that even proponents of PGT-A have to accept that most aneuploidies of preimplantation stage embryo are of mitotic origin, it has become difficult to argue that a 5-cell trophecto derm biopsy (TEB) can be representative of a clonal form of aneuploidy, characterized by little islands of aneuploid cells that can be anywhere among 200-300 cells of a blastocyst. Mitotic errors can, of course, happen in every mitotic cell division, of which there are innumerable, while there is only one meiotic cell division preceding all mitotic divisions. But as a recent paper in Nature Communications now very well demonstrates, the first mitotic division in a human embryo is playing an unexpected big role in embryo aneuploidy because this mitotic division is highly error prone.1
The British authors demonstrated this fact beautifully via live cell imaging of chromosome segregation. What they discov ered was that an extended prometaphase/metaphase in the first mitotic division demonstrates phenotypes that cause nondis junction, including multipolar chromosome segregations and lagging chromosomes that lead to the formation of micronu clei, as also seen in cancer cells that become aneuploid. Most importantly for IVF, and also returning to the PGT-A subject, the authors traced phenotypes in 2-cell embryos to two births, demonstrating that errors in this first mitotic division contrib ute to frequent mosaicism in preimplantation-stage human embryos but are tolerated by human embryos since they can give rise to normal births.
REFERENCES
1. Currie et al., Nat Comm 2022;13:6755 Continued on page 30
The V oice | december 2022 | 29
Basic science
More evidence for the importance of cumulus cells for oocytes
The importance of cumulus cells, a sub-lineage of granulosa cells that encircle the oocyte, for oocyte support has over the last de cade become increasingly obvious. That cumulus cells, therefore, may relate to ultimate oocyte competence, therefore, appears like a logical putative hypothesis and this is exactly what Spanish and Australian investigators tried to confirm in a recently published paper in Reproductive Sciences 1 Individual oocytes (n=130) were assessed in quality by a so-called cumulus cell DNA fragmenta tion index (CCDFI) using a variant of the chromatin dispersion test. Among those 90 developed into embryos, and significant differences in CCDFI were found between oocytes that fertilized and did not fertilize, with oocyte quality negatively correlating with CCDFI. Moreover, a ROC analysis suggested a cut-off at 24% CCDFI discriminated the ability of the oocyte to result in syngamy with specificity of 75.6% and 65.0%, respectively. Based on these cut-offs the authors concluded that CCDFI could be used as a potential index to assess in advance the reproductive potential of an oocyte.
We, frankly, don’t think so: First, the testing procedure appears too cumbersome for daily routine embryology practice; and sec ond, we very much doubt that sensitivity of 75.6% and specificity of 65.0% can beat out the experienced eye of a good embryologist. We, however, appreciate the paper nevertheless, because it offers further support for the importance of cumulus cells in “feeding” oocytes. This has, indeed, been a subject in intense interest at the CHR for several years and, especially recently, appears to come into increasing focus under the leadership of David F. Albertini, PhD, Editor-in-Chief of the JARG, a former director of CHR’s laboratory division, and now a senior Visiting Scientist at the CHR. We hope to be able to offer interesting news on this subject in the very near future.
REFERENCES
1. Baratas et al., Reprod Sci 2022;29:3194-3200
Blobs that rule biology?
Medical writer Elie Dolgin recently penned a very interesting feature article in Nature magazine, titled, “The shape-shifting blobs that rule biology.”1 We recommend this article because it summa rizes brand-new developments, suggesting a completely new cell biology, and he does it superbly. To quote his summary: “More than a decade ago, scientists started finding peculiar droplets inside cells. Now researchers are trying to work out how these ubiquitous beads form and what they do.”
As he notes, everywhere in cells, as now has become apparent, throngs of proteins and DNA are sticking together, producing “pearl-like” droplets that allow cells to conduct some of the most
essential functions, including gene control, DNA repair, stress responses, and even waste disposal. In contrast to for example mitochondria which are enclosed by membranes, these “pearls” have no membranes and disappear once they have concluded their job. A researcher in this field interviewed by the writer con cluded: “There isn’t a cellular process hat’s been studied that is not now known to involve these condensates.; - it involves damn near everything.” It appears that the next biological revolution is upon us, and we thought our readers should be made aware of it!
REFERENCES
1.
General aspects of medicine
Marketing to the medical profession
Though mostly directed at equipment sales (sic., embryoscope), genetic testing (sic., PGT-A, polygenic risk scoring of embryos), or other lab tests (sic., ERA testing), how abusive marketing to the medical profession can be, has been repeatedly the subject of this newsletter. Now comes Troyen Brennan, MD, MPH, currently an Adjunct Professor at the Harvard Chan School of Public Health and former Executive Vice President and Chief Medical officer of CVS-Caremark and pens an article on pharmaceutical marketing that is must-read.
There are several good reasons for reading this paper; but what for us exploded off the pages was how wasted all the rulemaking has been, medicine has suffered under in recent years, which has made it almost impossible for educational events to receive com mercial sponsorships.
Does anybody really believe that physicians change prescribing patterns because a salesperson drops off a few pens and coffee mugs at a medical office; or because a drug maker sponsors an event or the food at a medical conference without having in fluence on who speaks and what is said? What this article quite clearly demonstrates is that, even these days, if indus try really wants to bribe
Dolgin E. Nature 2022;611:24-27
Continued from page 29 30 | december 2022 | The Voice
physicians, even under the boatload of existing, often stupid govern ment rules meant to prevent such abuses, not only will industry find the appropriate opportunities but – and this is really what we find most disturbing – they will find a receptive audience among some of the most prominent physicians, a picture we, unfortunately, have only too often witnessed in reproductive medicine in recent years. The victims are the vast majority of honorable physicians who be lieve their “expert” brethren, having no idea that their professional heroes are nothing more than paid sales staff for industry.
REFERENCES
1. Brennan T. N Engl J Med 2022;387;(18):1631--1633
The end of anonymous egg and sperm donations?
We have previously in this newsletter addressed the quickly in creasing risk of breach of donor anonymity for egg as well as sperm donors due to social genetic testing offered by several companies, obviously led by 23andMe. Now come two prominent academics: a lawyer, and CHR’s friend and colleague, Eli Y. Adashi, MD, MS, for decades has been one of the leading academic voices in reproductive medicine, and pen in an article for JAMA in which they raise the very appropriate question of whether a new Colorado law soon will not only end the anonymity of sperm donation in that state, but be a forerunner for the whole country, likely, also meaning an end to anonymous oocyte donation.
Whether anonymous gamete donation should remain possible is a difficult subject to parse apart because it involves so many contra dictory rights and interests, starting with the increasing demand (and right) of offspring from donations to know who their biological parent is, the contradictory right to privacy of parents who chose to build their family through gamete donations, and the right to privacy of donors whose numbers will dramatically shrink once anonymity is removed (this is known from counties
like the U.K., where anonymity was removed).
REFERENCES
1. Cohen, et al. JAMA 2022; doi: 10.1001/jama.2022.19471. Online ahead of print.
The really bad papers section
Our readers’ response to the first “really bad paper section” in the November issue of the VOICE was so rewarding, we decided to give it its own regular spot in our monthly literature review. This month we chose two papers from the same issue of the same journal; and, no, we do not go after preselected journals in choosing those pa pers, even if it may appear that way, - since our first two really bad papers also came from one journal. Here are this month’s winners, by coincidence, both, from issue 1 of volume 45 of Reproductive Biomedicine Online:
Claiming to be a regular research article, a group of British re searchers in an article claimed to have studied, “how fertility clinic medical directors view IVF.”1 And guess how many questionnaires they analyzed to get the information? The answer is a total of 10 from among 93 that were originally sent out to UK IVF clinics. That editors would accept such a manuscript for publication, therefore, is truly remarkable and warrants the inclusion of this paper among this month’s “winners.”
In another paper in the same journal, this time by Turkish col leagues, the criticism once again is the inadequate number of study subjects.2 This study claimed to have investigated, “whether COVID-19 disease does cause ovarian injury to women of reproduc tive age?” The authors conclusion that, fortunately, there is no injury from COVID-19 infections, while likely correct based on other reported data in the literature, can, however not be deducted from
Continued on page 32 The V oice | december 2022 | 31
this paper. Basing their conclusions on pre- and post-values of FSH, LH, the ratio between both of these hormones, and AMH values, and offering no pre-study power analysis that would explain what outcome difference would be expected, they enrolled into the study 132 women between ages 18-40. That this very likely is an inade quately small sample size to rule out a type II error is, for example, demonstrated by their conclusions about AMH levels demonstrat ed no difference between pre- and post-COVID-19 periods. The P-value they claim in support of this conclusion was, however, 0.097, therefore suggesting a trend toward significance, which with larger patient numbers very well may have reached significance. Unsurprisingly, the authors also did not acknowledge this weakness of their paper in their discussion, suggesting that this issue did not even come up in the journal’s review process.

REFERENCES
1. Iacoponi et al., Reprod Biomed Online 2022;45(1):169-179
2. Madendag et al., Reprod Biomed Online 2022;45(1):153-158
Continued from page 31 The
Fighting
ADVERTISEMENT 32 | december 2022 | The Voice
CHR
for every egg and embryo


The Center for Human Reproduction Fighting for every egg and embryo c onnect with us! www.thechr.com social@thechr.com 212.994.4400 21 e 69th s t n ew York, n ew Y ork 10021 ADVERTISEMENT





























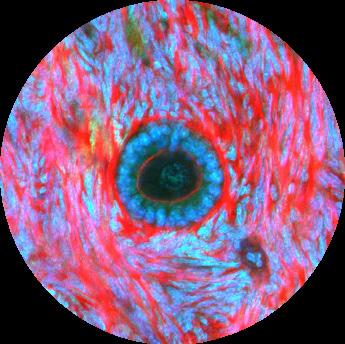
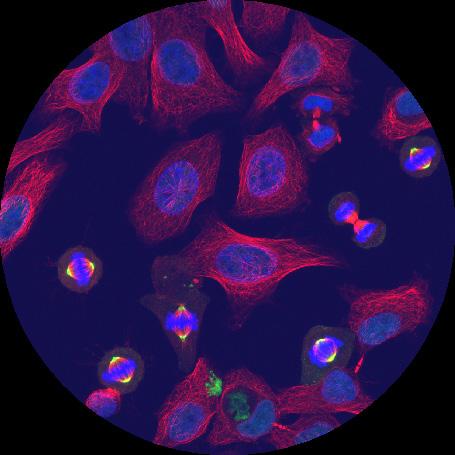
 By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.
By Norbert Gleicher, MD Founder, Medical Director and Chief Scientist The CHR, New York, N.Y.