






















When you start a chief executive job, particularly when you are joining a new sector, your first priority is to try to get to know the new community you are joining. When I became legal ombudsman, I spent my first six months on the road, meeting and greeting, talking and listening. From an efficiency perspective, it made little sense and, to be honest, there was more than one evening when I would wonder why I was spending a wet Tuesday night in Stoke or Swansea. But the effort paid off: not only did I understand the profession far more at the end of that six months, all those train journeys had been a visible desire to learn. Sadly, that strategy has not been possible at the AOP – I started during the second wave of the pandemic. Since things have opened up again, I have started to try to get out more, making sure I have had a presence on the ground in Northern Ireland, Scotland and Wales, for example. Yet I am all too aware that I have only met a fraction of the AOP membership – and whatever the formal governance structures, the membership is the authority in the AOP. This is why events like 100% Optical are so important. But I recognise that while the conversations I had at 100% Optical, though useful, I have still a long way to go to fully understand what different members think and feel. This is why I am so anxious to see the results of our recent member survey, in which over 3000 of you gave your views. The part of the survey I am most anxious to see is where we asked you to talk about your future ambitions and aspirations in your career. As this edition of OT discusses, the dayto-day reality of work as an optometrist is changing rapidly. Not only is the profile of individuals joining the profession very different from what it was two decades ago, so is the shape of the potential career path for them. My hope is that, by better understanding what members want and feel, we can develop our services to provide greater support, and use our (growing) influence with policymakers to try to shape the future in members’ favour. One of my key memories of those wet Tuesday nights in Stoke and Swansea was of listening to solicitors venting their belief that their representative body did not understand the issues they were facing. It is vital the same is not said of us.


Adam Sampson, AOP chief executive

“By better understanding what members want and feel, we can both develop our services to provide greater support, and use our (growing) influence with policymakers to try to shape the future in members’ favour”


The news in digest
Picture this
Professor Bruce Evans receives the AOP’s Lifetime Achievement Award OT reports
Concerns patients on waiting list will be lost in the system
The edit
Optics in 16 stories
100% Optical
OTreviews the 2023 show which welcomed more than 10,600 visitors across the three days
Industry profile
Senior consultant at Euromonitor International, Natasha Cazin, on three consumer trends affecting optics
AOP round-up
100%Respectcampaign one year on, the policy team’s consultation responses, and the AOP’s myopia resources
“We need to work collaboratively and remain open to the tough conversations that move us forward”
Serena Box, AOP PR manager PAGE 16
The trends, launches and looks
OT focuses on...
Eyewear at 100% Optical
Me and my glasses
Hakim Group head of buying, Lorna Robinson
Get the look // Anatomy of a frame
With Lizzy Yeowart
The shortlist
The April/May selection
Behind the brand
Exeter Eyewear





31-35
THE IP SPECIAL REPORT
In part two of OT’s ongoing IP:an upskillingworkforcespecial report series, we explore the qualification in practice, with optometrists across the four nations sharing their views and experiences
“I THINK IT’S VERY IMPORTANT TO WORK COLLABORATIVELY WITH THE LOCAL PRIMARY AND SECONDARY CARE TEAMS SO THAT THE CARE IS JOINED UP AND FLOWING IN BOTH DIRECTIONS”
Marc Drake, specialist IP optometrist and partner at Osmond Drake Opticians



OT and its wrapper are produced on paper from European mills meeting the highest quality and environmental standards. The journal and paper wrapper are fully recyclable.
Professional development for optometrists, DOs and CLOs CPD
65 CPD welcome
66 Making sense of the macular
72 Environmental quality and ocular surface health


79 Optical Consumer Complaints Service annual report – a goldmine of insight
86 Another day in the hospital eye clinic
88 Vitreoretinal cases

























Business insight and career development
The roundtable
OThosted a roundtable discussion exploring solutions for vitreous floaters, in partnership with VivaQuity
How I got here
Optometrist, Christian Dutton
How do I...
Support those returning from parental leave?
What I have learned
The value of mentoring
Pre-reg focus
Rochelle Anderson and Akshay Shah
IP and me
IP optometrists discuss managing trauma-induced anterior uveitis
Becoming a business owner
Donna Lowther
Eyes on wellbeing
A look at managing burnout


From green spaces and flexible working to discrimination, OT explores how optometrists can foster positive working environments today. Plus: clinicians share insight into the items that enhance their working environment and why
OTvideo highlights OT’s highlights from 100% Optical 2023
Watch the video on www.optometry.co.uk
Listen to The OT Podcast today
Our first three episodes, featuring Professor Nicola Logan, Ian Cameron and Keith Valentine, are available to listen to on all main podcast platforms
END NOTES
Career advice
Duncan and Todd’s Frances Rus and Julie Mosgove on why flexible working is key for the group I could not live without...
”LOCSU leadership and training,” says optometrist, Reena Anand Last word Professor Ed Mallen’s secret life
Contact OT with your experiences and observations from practice: newsdesk@optometry.co.uk








































































































12 100% OPTICAL
OTshares some highlights from the 2023 show, which saw over 10,600 visitors
14 INDUSTRY PROFILE
Euromonitor’s Natasha Cazin on the consumer trends set to impact this year
16 AOP UPDATE
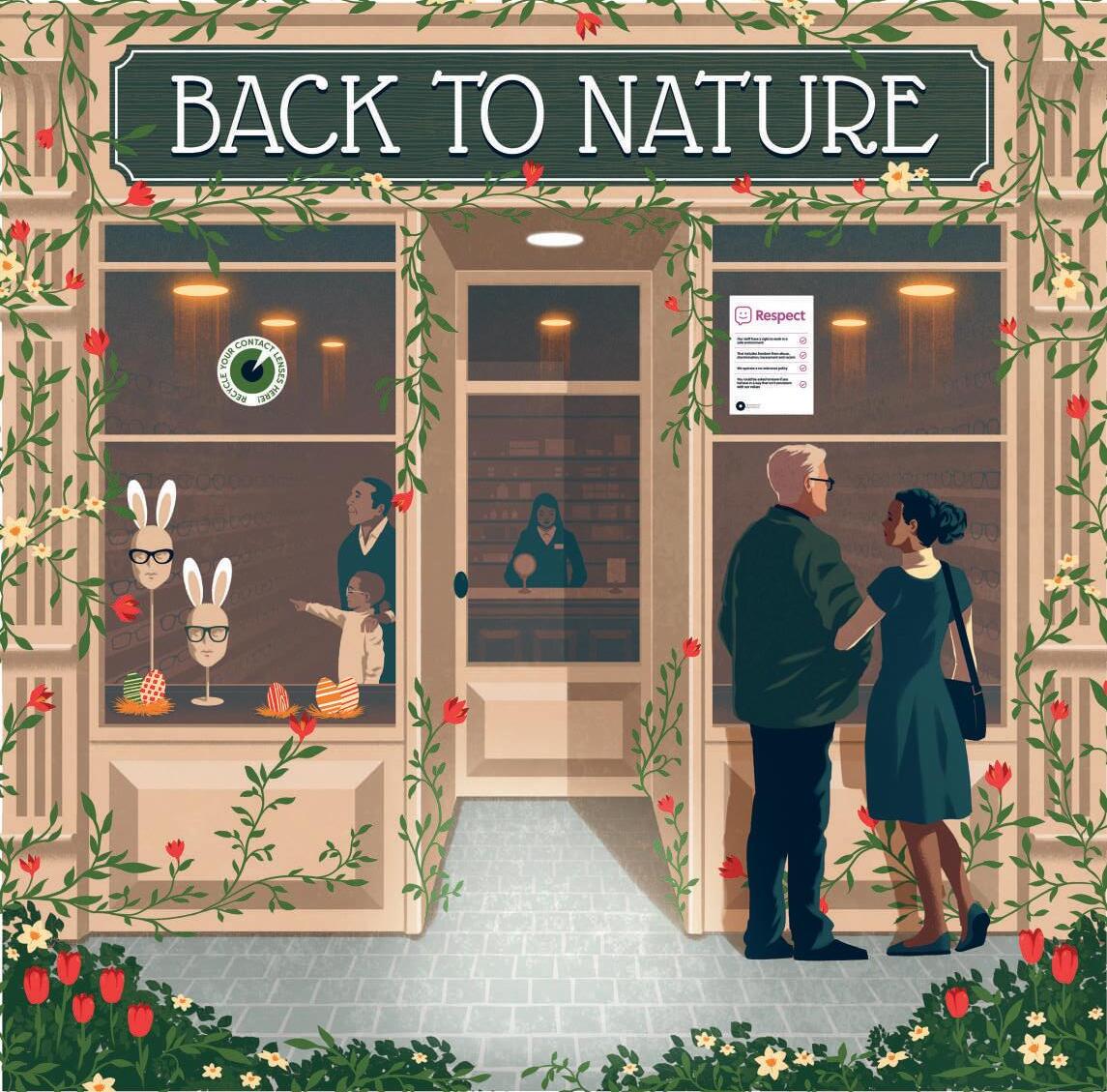
OTupdates on the AOP’s 100% Respect campaign one year on

Optometrist Professor Bruce Evans has received the AOP’s Lifetime Achievement Award, in recognition of a career that has spanned three decades
Professor Bruce Evans was presented with the AOP’s Lifetime Achievement Award, sponsored by CooperVision, at the AOP’s Excellence in eye care event, hosted on the Sunborn Yacht, London on 26 February.
On receiving the award, Evans told OT: “It is a real surprise, a huge honour, and a slight sense of impostor syndrome, because I know lots of people in the profession who I think deserve it much more than me. A huge sense of gratitude, because it is really a reflection of the teams that I’ve worked with and of the people that have inspired me.”
During the event, the AOP also recognised excellence across a number of areas of the profession, with the
Association announcing the winners of three award categories that focus on sustainability, research and community-led care. These included: Recognising sustainable excellence, awarded to Simon Berry; Recognising excellence in community-led care, awarded to Cardiff and Vale University Health Board Primary Care Optometry and Secondary Care Glaucoma Teams; and Recognising research excellence, awarded to Professor James Wolffsohn.
Read more about the AOP’s Excellence in eye care award recipients on the OT website: bit.ly/3JghR2D
April/May 2023

Volume 63:02 Issn 0268-5485
ABC certificate of circulation 1 January 2021–31 December 2021
Editor: Emily McCormick emilymccormick@optometry.co.uk
Deputy editor: Lucy Miller lucymiller@optometry.co.uk
Features editor: Selina Powell selinapowell@optometry.co.uk
Senior reporter: Kimberley Young kimberleyyoung@optometry.co.uk
Web content and social media manager: Leah Boyle leahboyle@optometry.co.uk
Clinical editor: Dr Ian Beasley ianbeasley@optometry.co.uk
Clinical editor for multimedia: Ceri Smith-Jaynes cerismithjaynes@optometry.co.uk
Video production editor: Laurence Derbyshire laurencederbyshire@optometry.co.uk
CPD enquiries: 020 7549 2076 CPDhelp@optometry.co.uk
AOP membership and OT subscription team: subscriptions@aop.org.uk
Advertising: Matt Hall 020 3771 7257 matt.hall@thinkpublishing.co.uk
Advertising production: aop@ccmediagroup.co.uk
Art director: Grant Pearce
Senior designer: Juanita Adu
Associate director: Anna Vassallo
Executive director: Jackie Scully
Published bimonthly for the Association of Optometrists by Think Media Group
20 Mortimer Street, London, W1T 3JW
Printed by Acorn Web, Normanton Ind Estate, Loscoe Close, Normanton, West Yorkshire, WF6 1TW
All rights in and relating to this publication are expressly reserved. No part of this publication may be reproduced in any form or by any process without written permission from the AOP or the publisher.

NHS England has confirmed that 323 patients have been placed on active monitoring following the roll out of new waiting list management guidance
There are concerns that patients will be lost in the system following the implementation of new guidance for managing waiting lists by NHS England.
The guidance, which was published at the end of October, permits clinicians to remove patients from the NHS elective waiting list after they have declined two offers of treatment and place patients on ‘active monitoring.’
In response to a Freedom of Information (FOI) Act request by OT, NHS England confirmed that 323 patients were placed on active monitoring between October 2022 and the end of January 2023.
Speaking to OT when the guidance was first published, a spokesperson for the Royal College of Surgeons highlighted that while the guidance seemed sensible at face value, how it is executed would be key.
“NHS trusts and clinicians will need to ensure that patients do not feel bullied into moving off the waiting list, and into active monitoring,” the spokesperson highlighted.
“NHS England will also need to ensure that trusts are not tempted to use the guidance to game waiting lists, making them appear shorter than they are in reality,” the spokesperson emphasised.
Concerns were also expressed about the practicalities of implementing the new guidance.
The Royal College of Surgeons stated: “It may be wholly appropriate that a patient is moved to active monitoring, if they agree with that approach. But, will NHS systems be able to cope with moving patients on and off waiting lists?”
At the end of January, only 27 out of 533 NHS providers had placed patients on active monitoring.
Seven of the providers placing patients on active monitoring were NHS trusts, while the remaining 20 were independent hospitals.
The Royal College of Surgeons shared: “Used responsibly, these new guidelines could give us a more streamlined picture of patients waiting for treatment, and patients a more realistic idea of how long their waits might be. Used poorly, it could see patients lost in the system, or banished to waiting list purgatory.”
A hidden waiting list?
Waiting list consultant, Rob Findlay, of data and elective pathway management company Insource, highlighted the importance of a clinical decision being made when patients are placed on active monitoring.
“If clinicians are making clinical decisions that are in the best interests of the patient, then there is no problem,” he said.
However, he expressed concern that clinicians could come under pressure to remove patients from the waiting list, or that administrators rather than clinical staff could have responsibility for the decision.
In its response to OT’s FOI request, NHS England highlighted that patients were placed on active monitoring following a “clinical conversation that has determined it is clinically appropriate for a patient to choose to delay their treatment.”


#SightWontWait
Find out more about the AOP’s #SightWontWait campaign that has gained national media coverage: www.aop.org.uk/ sightwontwait

“Used poorly, it could see patients lost in the system, or banished to waiting list purgatory”
Royal College of Surgeons spokesperson
Insource colleague, Karen Hyde, questioned the degree of patient choice that is present within the new guidance – for example, if a patient is repeatedly offered an appointment in a location that they cannot get to.
“Ophthalmology contains quite a lot of elderly patients. They may not have transport or someone to take them to another area,” she shared.
A frequently asked questions document seen by OT did not provide specific parameters for what would be considered a reasonable location for an appointment.
“A reasonable offer will be determined by each region based on the geography of the region,” the document stated.
Hyde shared her concern that patients would be lost in a “hidden waiting list” as a result of the guidance.
“I always think about mums and aunties, grandads and best friends. These are patients – this should not be about making waiting lists look more palatable,” she said.
Lessons from Scotland
Findlay suggests that NHS England should look to Scotland for an example of the risks of creating exceptions to the reported waiting list.
In Scotland, there was a large increase in the use of social unavailability codes between 2008 and 2011. Social unavailability codes can be used when a patient is unavailable for treatment and are not included in the patient’s overall waiting time.
An Audit Scotland report in 2013 found that the use of this code increased from 11% to 31% over the four-year period.
The report concluded that the focus on waiting time targets led to insufficient scrutiny of how these targets were being achieved.
The proportion of patients coded as socially unavailable was higher in specialties with high patient numbers and pressure on capacity, such as ophthalmology and orthopaedics.
For example, in 2011, 40% of patients on the waiting list for ophthalmology outpatient treatment at Southern
General Hospital in Scotland were coded as unavailable.
Audit Scotland also found limits on the choice that patients had when offered alternative appointments.
“We found little evidence to suggest that NHS boards are taking account of patients’ individual circumstances, such as access to transport, mobility or additional support needs, before offering them treatment at a location outside the board area,” the report highlighted.
Dr Peter Hampson, AOP clinical and professional director, shared that the guidance may appear to be a pragmatic solution on the surface.
“But the difficulty here is that once recategorised these patients may fall off the radar and as a result would not receive the care and treatment they require. We’re already seeing thousands of people experience delays to treatment due to the backlog in hospital eye care and there is a very real concern that this new approach allows even more patients to fall through the cracks. Given that ophthalmology patients are often elderly and the reasons they cannot attend may be practical and even financial it’s essential that trusts exercise prudence,” he said.

“At milestones like these, we reflect on our history and take pride in our heritage”

Ryan Leighton, CEO of Leightons Opticians and Hearing Care, reflected on the history of the company as it celebrates 95 years in 2023. The business opened as a dispensing practice in Southampton in 1928 and has grown into a clinically led optometry group, in its third generation as a family business.
41,000
Approximately 41,000 visually impaired people under the age of 25 are “at risk of inequitable education leading to reduced employment opportunities,” the Royal National Institute of Blind People (RNIB) has said, warning of a “worrying” attainment gap between visually impaired (VI) children and their fully sighted peers. RNIB research found that three quarters of local authorities in England have cut or frozen VI education service budgets at least once in the last four years, while there has also been a 10% increase in the number of children recorded as having vision impairments in these authorities.


Stepper Eyewear has launched a new logo and strapline focusing on ‘The Perfect Fit’ as part of a brand refocus. Peter Reeve, managing director of Stepper UK Limited, said: “The first frames, designed in 1970 by Hans Stepper, were manufactured in a new material and process to provide an exceptional standard of fit. This motivation remains true today.”
Chancellor of the Exchequer, Jeremy Hunt, unveiled a Spring Budget with the theme of ‘education, employment, enterprise, everywhere,’ on Thursday 15 March. The Chancellor laid out measures that he said will help to ‘level up,’ decreasing economic inactivity and encourage investment. Plans included an overhaul of disability support to make it easier for those with disabilities who want to work to do so. OT set out the key points from the Budget and shared the reactions from charities in the eye care sector. Read more at: bit.ly/3FCtQFw.

“20 years of Nocturnal is special to me”
Specsavers has introduced myopia management products into its practices across the UK and Republic of Ireland. Practitioners and retail staff across the multiple have completed myopia management training and the national launch of myopia management includes a contact lens and a spectacle lens option for patients. Specsavers confirmed it has worked closely with CooperVision and Hoya to ensure staff are able to communicate effectively about the products.
10,000
Bird Eyewear will plant more than 10,000 trees in the next two years as part of its Bird Forest initiative. The brand is working closely with Devon County Council and The Devon Wildlife Trust as part of a wider innovation project, supporting Bird’s drive towards carbon zero. The Bird Forest is located across three main sites in Devon: Haytor, Pinhoe and Slapton.

Scott Brown, optometrist and clinical director of Scotlens, looked back on 20 years of the company’s Nocturnal orthokeratology product. In celebration of the milestone, the company has launched a new advert forming part of Scotlens’ ‘#nightlenses revolution,’ which seeks to utilise “easy to use and remember night lenses terminology” to increase public awareness.
Research in JAMA explored the effect of low-concentration atropine eye drops on myopia incidence. The Chinese University of Hong Kong Eye Centre trial saw 474 nonmyopic children randomly assigned to apply 0.05% atropine, 0.01% atropine or placebo drops once nightly in both eyes over two years. It concluded that nightly use of 0.05% atropine drops resulted in a significantly lower incidence of myopia compared with the placebo.
University Valli Opticians, at the University of Huddersfield, is raising awareness of children’s eye health, particularly the early diagnosis and treatment of amblyopia, as part of a new study that will offer free vision screening for over 1000 primary school children in Kirklees. Read about the research at: bit.ly/3LKfiav
Researchers have restored vision in a mouse model of retinitis pigmentosa (RP) using a new form of CRISPR gene editing. Published in JournalofExperimental Medicine, research outlines how the gene editing system can be programmed to correct many different types of genetic mutation – irrespective of the location on the genome.

SpaMedica Chelmsford has received the Alzheimer’s Society’s ‘Working to Become Dementia Friendly’ award. Feedback from the charity highlighted how the facility, which provides NHS cataract surgery, YAG laser capsulotomy, and wet age-related macular degeneration treatment, worked closely with the charity and Chelmsford Dementia Friendly community. As an organisation SpaMedica has introduced a Dementia Action Plan across all 46 of its UK hospitals.
The Optometric Fees Negotiating Committee has said that its evidencebased bid for an increase to GOS fees and grants has been “disregarded” by NHS England. A 4.5% rise, which is below inflation, was imposed to GOS and pre-reg training grants, and a freeze to CPD grants was confirmed.
“This development in the US is a huge milestone for patients living with dry AMD”
The Macular Society’s Geraldine Hoad, on the news that Pegcetacoplan had received US Food and Drug Administration approval for the treatment of geographic atrophy secondary to AMD.
“Even a simple acknowledgement to say Ramadan Mubarak – meaning have a blessed Ramadan – is a great way to make your Muslim employees and colleagues feel included”
Optometrist, Shamina Asif, reflected on the significance of Ramadan 2023 and the ways practices can support their Muslim colleagues. Read Shamina’s insights on OT: bit.ly/3LpVU2x
“I was shocked to see what I suspected to be a retinoblastoma”
Optometrist, Laura Leafe, talked to OT about the concerning photograph of her niece’s eye that led to an urgent appointment and referral. Find the full story on OT: bit.ly/3JAvZUn

Isha Saghir, pre-registration optometrist at Bennett & Batty, a Hakim Group independent practice in Liverpool, shared her journey so far for OT’s Pre-reg focus, including balancing work with study and successfully achieving all her required competencies for Visit 1. Read Isha‘s latest update on the OT website: bit.ly/4035OLD


















The 2023 edition of 100% Optical saw a record breaking number of visitors






“This has been our best show yet,” Nathan Garnett, show director for 100% Optical, told OT at the close of the optical trade show.
revealed key themes around treating dry eye, the impact of new technologies and artificial intelligence, and the everincreasing focus on sustainability.
In dry eye, Positive Impact launched the TearRestore Thermal Mask (pictured left bottom), described as the “first and only” open-eye warm compress.
BIB Ophthalmic Instruments showcased a variety of devices, including the Optopol Revo FC130, described as the fastest Optopol OCT, while Cerium Visual Technologies presented the Intuitive Colorimeter Wave, and Australian-based Cylite presented its multi-functional diagnostic device, the Cylite Hyperparallel OCT.
A number of exhibitors celebrated anniversaries at the show, including a 10-year anniversary for Glasklar UK, and a 30-year celebration for Cerium Visual Technologies
From 25–27 February, eyewear brands, equipment manufacturers, contact lens companies, and community ophthalmology service providers took to ExCeL London.
More than 10,000 people attended the three-day event, representing a 10% year-on-year increase on the previous record.
Exhibitor activity
The show saw strong representation from companies in every sector, including the return of international independent eyewear brands after pandemic restrictions limited travel for many in 2022.
The number of contact lens companies at the show also grew, with CooperVision joining for the first time, launching its FreshThinkingcampaign (pictured left centre) with activities that included a giant 2.7m ‘buzz wire’ game.
Observing conversations and exhibitor plans across the show floor
Bird Eyewear launched its new ophthalmic range, designed for UK optometry practices and developed from a mix of bioplastics and recycled materials in a lowcarbon production process, and Coral Eyewear showcased its new cellulose acetate collection in an exciting range of colours.
Meanwhile, Johnson & Johnson Vision went paperless – turning marketing materials into digital resources and calculating the number of paper sheets saved for every download, visualised as a ‘living tree.’ The company ended the show with 1100 paper sheets saved.
The catwalk saw a number of new features, with The Eyewear Stylist, Dan Scott, offering pointers on styling and choosing frames and lenses. Panel discussions on the catwalk covered
100% Optical 2023 saw 10,657 ATTENDEES
More than 140 CPD SESSIONS

Maddie, who was eight when she became myopic.”


sustainability in eyewear, myopia management and consumer trends.
Garnett said: “We’ve been working with Euromonitor who delivered a session on trends and we hosted a discussion afterwards about how opticians on the High Street can talk to the different groups out there, whether Millennials, Gen Z and so on.”
The event also received a visit from presenter, restaurateur and broadcaster Dame Prue Leith, who launched Specs by Prue with MAC Eyewear in 2022.
Main stage highlights
As the official UK partner for 100% Optical, the AOP developed a packed programme of continuing professional development (CPD) for delegates.
Garnett said: “We’re really pleased to be working with the AOP. The relationship just gets stronger and stronger.”
A session titled Drawing on the skills of the entire eye care sector to reduce avoidable sight loss saw Specsavers’ clinical services director, Giles Edmonds, and director of professional advancement, Paul Morris, discuss key challenges affecting eye care in the UK, and the role of optometry as part of the solution.
They were joined by Anthony King, a consultant ophthalmologist at Nottingham University Hospital, and chair of Glaucoma UK, who described the pressure on ophthalmology services. Speaking to OT, King shared the importance of the whole eye care community having insight into the importance of early diagnosis, adding: “The way glaucoma is detected in this country is through opportunistic detection, and that’s primarily undertaken by optometrists, so what better place to raise this as an issue.”
Reflecting on the show, AOP head of education, Dr Ian Beasley, said: “We’re thrilled with the results of this year’s event,” adding: “Heading into our landmark 10th year, that speaks volumes about how much practitioners appreciate the opportunity to come together, meet hundreds of exhibitors, and consume education from world class speakers.”
As the official media partner for 100% Optical, find all of OT's interviews at www.optometry. co.uk/optical2023
The programme included more than 140 sessions of CPD across a variety of topics and domains.
Elizabeth Lumb, director of global professional affairs for myopia management at CooperVision, presented a lecture on Driving change to put the brakes on myopia. She reflected on how far the profession has come in myopia management since she delivered a session on the topic at 100% Optical in 2017, telling OT: “There’s lots of talk about in just a short space of time.”
She added: “I was able to frame the conversation around the experiences of my niece,
Verification of CPD attendance was sent to delegates by email on 8 March. Registrants who have not received this are reminded to check their spam folders, or contact events@ aop.org.uk with any queries.
The optical trade show will return to ExCeL London from 24–26 February 2024, which will also mark the 10th anniversary of 100% Optical. Show organisers already have plans for the milestone event. This includes a dedicated ophthalmology section
and education programme, working with key partners, suppliers and the NHS to deliver the content for ophthalmologists.
Looking towards the 2024 event, Garnett told OT: “We’re very excited about some of the plans we’ve got for that already.”
Jakob Sveen, Johnson & Johnson Vision managing director, Northern Europe and general manager UK and Ireland commented: “These shows are critical for this industry, not just bringing a lot of innovation from the suppliers, but it’s also about that partnership between suppliers and customers, with the patient in mind.”
Tim Baker, group CEO of BIB Ophthalmic Instruments, reflected that 2022 saw more of a tentative approach to shows, whereas: “This year has proven to be more relaxed, the footfall has been fantastic and more importantly, the interest in the technology has been noticeably different.”
Luke Wren, head of business development for Hakim Group, noted: “It’s been a much more normal show this year,” remarking on the high numbers of attendees, and “great conversations” had at the event.
Doug Bairner, country manager, UK and Ireland for CooperVision, shared: “Being at 100% Optical is amazing for us, because it is everyday practitioners who are here, so it’s great to be able to talk with such a broad scope of people who have different priorities in their practice, to really understand what’s going on in their world.”
Jason Kirk, managing director of Kirk & Kirk, described the show as “really exciting.” He highlighted: “The thing that has been very interesting was to see international people coming and buying at the show.”

100% Optical visitors enjoyed a Q&A with Dame Prue Leith
Coral Eyewear’s George Bailey described the importance of the show for the team: “Where we have regional reps in Scotland and Wales, and across the UK, it’s really nice for everyone to come together, meet in one hub, and feel the buzz of the industry and see those sustainable developments come together.”
Natasha Cazin, senior consultant at Euromonitor International, picks out the three biggest consumer trends set to affect eyewear and optics in 2023


Euromonitor International highlights the new normal in its Global Consumer Trends 2023. The biggest impact we see is consumers cutting back on spending and not going out as much as initially thought.
‘Budgeteers’ is a consumer trend you can’t avoid in any industry. 2023 will be about bracing for a lean year ahead: nearly half of consumers plan to increase efforts to save money according to Euromonitor‘s Voice of the Consumer Lifestyles survey 2022. We have consumers that are more cautious than ever before, with economic uncertainty and rising costs like energy prices, driving the consumer to budget and think about how they spend their money.
Some consumers are budgeting to live well. They might budget for a holiday but perhaps have less to spend on eyewear. Then there are the consumers who have got no choice – they are struggling and are budgeting to live.
Independent practices might want to think about how they can add value to make sure the consumer purchases in their practice. I would advise practices show them the added value – the
customer experience, the product, and the overall package. One example is a loyalty scheme – adding a bit of value to retain clients who might be thinking about cutting costs.
The ‘Here and Now’ consumers really want to get out there. They are fed up of the pandemic, and they want to spend some money and do something special, but they possibly don’t have a lot of money. For this consumer, it’s about affordability.
“I don’t think it’s possible for businesses to ignore consumer trends”
I would recommend that businesses think of how they can help the consumer to make payments. There are split payment methods, like buy now, pay later finance company, Klarna. It could be hundreds of pounds they are spending, and perhaps they could pay that over several months –giving them the option so that they can buy the product in your store. There are also options like discounts or loyalty cards. It doesn’t have to be complicated.
Euromonitor’s top 10 consumer trends for 2023
1. Authentic Automation
2. Budgeteers
3. Control the Scroll
4. Eco Economics
5. Game On
6. Here and Now
7. Revived Routines
8. She Rises
9. The Thrivers
10. Young and Disrupted.
The third key trend affecting the industry is ‘Young and Disrupted.’ Generation Z, the 12–27 year olds, are not young children any more. They are gaining financial independence; they might have their own homes and they have jobs. Their education has been disrupted by the pandemic: they had a tough time and want to be buying again.
How can businesses respond to this? They have to be aligning with the values and expectations of the young consumer. This consumer stands up for their beliefs; they are into social responsibility and inclusion. For example, they are likely to choose a sustainable product over something else, so consider having a sustainable line. I would also say: consider being online if you want to communicate with this generation. Social media platforms, like TikTok or Instagram, are a good way to get online.
I don’t think it’s possible for businesses to ignore consumer trends. It is imperative to think about, ‘who is my consumer?’ ‘How old is my consumer?’ ‘Am I targeting the older generation, or the younger generation?’ You have to think about your consumer carefully.
The Euromonitor International report is available to download for free from www.euromonitor.com

















tUsing measuredand modeleddata, pooledacrossages(8-17), MiSight®1 day slowedmyopiaprogressionby an averageof approximately50%. t12 months post-treatment, evidenceindicatesthat no accumulatedmyopia control benefitswere lost following 3 or 6-years of MiSight®1 day wear (on average,for childrenaged8-15 at start of wear). Instead,eye growth revertedto expected,age-normalrates. 1. ArumugamBet al.ModellingAge Effectsof Myopia Progressionfor the MiSight 1 day ClinicalTrial.Invest.OphtholmolVisSci.2021; 62(8): 2333. 2. ChamberlainPet al.A 3-year RandomizedClinicalTrialof MiSight Lenses for MyopiaControl.Optom VisSci.2019; 96(8): 556-567. 3. ChamberlainPet al.Long-term Effect of Dual-focusContact Lenseson Myopia Progressionin Children:A 6-year MulticenterClinicalTrial.Optom VisSci.2022; 99(3): 204-212. 4. ChamberlainPet al. Myopia progressionon cessationof Dual-Focuscontact lenswear: MiSight 1 day 7-yearfindings. Optom VisSci.2021; 98(E-abstract): 210049. 5. ZadnikKet al. FactorsAssociated with RapidMyopia Progressionin School-agecChildren.Invest.Ophtholmol.Vis.Sci.2004; 45(13): 2306. 6. HammondD,ArumugamB,et al.Myopia ControlTreatmentGainsare Retainedafter Terminationof Dual-focus Contact LensWearwith no Evidenceof a ReboundEffect. Optom VisSci.2021; 98(E-abstract): 215130. © 2022 CooperVision.CooperVision®and MiSight®are registeredtrademarksof The CooperCompanies,Inc.and its subsidiaries.

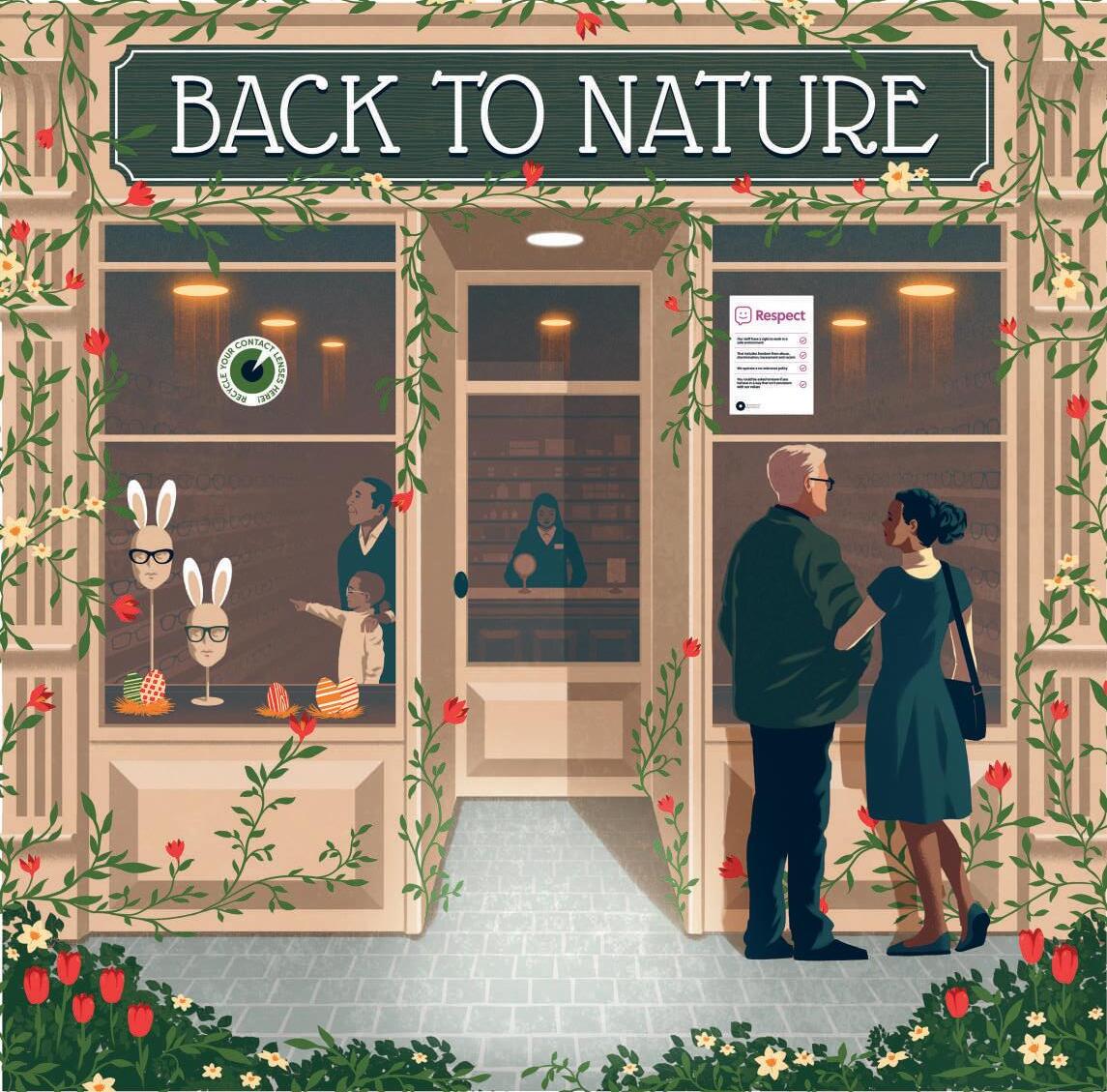
“100% Respect is designed to be a long-running programme of work”
One year on from the launch of the AOP’s 100% Respect campaign, Serena Box, PR and media manager for the AOP, reflects on the initiative and what comes next

Launching our 100% Respect campaign at 100% Optical in spring 2022 gave us an incredible platform to speak to members directly about the equality, diversity and inclusion (EDI) work we’re doing. As part of the campaign, we developed a range of advice for both employers and employees, including a suite of resources that promote inclusivity, from our expert legal and employment team.
In our research, members indicated that in 80% of cases the discrimination they faced in practice was “perpetrated” by patients, so we created resources, such as practice posters, that highlight a zero-tolerance approach, alongside digital assets.
The AOP’s Anti-racism and equality team (ARET), made up of AOP staff optometrists, also provides emotional and practical support where an individual is facing discrimination.
There is a huge amount of support for the campaign from members – and particularly those who have been affected by discrimination. Some have gone on to share personal stories through OT’s Time to Speak series. Sharing powerful and relatable stories builds trust and helps others feel safe to share their own experience and to also take action. But the responsibility shouldn’t fall to the individual – at the AOP we have always recognised that there is wider work to be done with employers in the sector. Our survey results reflected that, with 54% of our members calling for the AOP to work with employers to tackle discrimination and 51% asking for more guidance and support. We’ve built on this with a new template equal opportunities policy and CPD on the Equalities Act
100% Respect is designed to be a long-running programme of work. None of the challenges highlighted in our survey are going away and through the work we do we can really make a difference to members on the ground. We recently explored with the AOP Policy Committee how to enhance our EDI support and the next step is to plot out this activity over the coming 12–18 months.
Fundamental to this work is putting our members at the centre, to help build inclusive workplaces where they can thrive. It will require a whole host of approaches, whether that be guidance, service offering or campaigning, to support long-term cultural change.
Our initial campaign activity focused on race discrimination as this was reported by members more than any other form (60%). But we saw levels of discrimination across a range of characteristics and it is vital that our members who fall within these groups feel safe and protected – primarily through the advice of the AOP’s employment team, or the AOP guidance for employees, but also by the AOP being an advocate for change on key areas such as women’s equality, disability and LGBTQ+ issues.
Complementing this work is our advocacy outside the sector. We’ve recently become a partner of the We Are Able campaign – designed to support
Resources and further reading
AN AOP SURVEY OF OVER 1000 MEMBERS FOUND REPORTED INCIDENTS OF DISCRIMINATION RELATING TO:
Religion – 36%
Sexism – 35%
Age – 33%
Disability – 7%
Pregnancy – 7%
Other forms of discrimination reported included being married or in a civil partnership (4%), sexual orientation (4%), and gender reassignment (2%).
Source: AOP Equality, diversity and inclusion survey 2021.
people to lead safe and independent lives at home.
EDI is an incredibly complex area to navigate – with disadvantage and exclusion rooted in so many factors – social, economic, and cultural to name a few. Now we have a baseline, from our research, the next step is to measure meaningful progress and deep-dive into particular issues and challenges. To do that effectively, I think we need to work collaboratively and remain open to the tough conversations that move us forward.
Find practice resources, template policies, and guidance for employees: www.aop.org.uk/advice-and-support
Take the Discrimination Law and the Equality Act CPD: www.optometry.co.uk/cpd
Learn about the We Are Able campaign: https://weareable.uk/
Read the Time to Speak series on OT: www.optometry.co.uk/time-to-speak
Find more information on the 100% Respect campaign: www.aop.org.uk/respect

OT heard from Kathy Jones, AOP policy adviser, about the AOP’s work in responding to consultations that shape the future of the profession

What consultations does the AOP respond to?
A small part of what the AOP does for members is to keep a look out for consultations about changes that could affect our members or the future of the profession. These consultations could be launched by government, the General Optical Council (GOC) or the NHS.
Sometimes the proposed changes are huge, such as the GOC’s Education Strategic Review, that took place between 2015 and 2020, or their new consultation on the future of the Opticians Act. The changes can be short-term, such as the GOC’s temporary changes to their procedures during COVID-19 lockdown, or longterm, such as the Government’s consultation on the future of healthcare regulation as a whole, or the latest set of NHS reforms.
While some of these issues may seem very remote from the day-to-day experience of our members in the testing room, they could have a huge impact on their future working lives, and those of the optometrists of the future.
What goes into forming a response?
The AOP responds to between 10 and 20 consultations a year, and we post most of our responses on our website.
Consultation responses are normally led by the AOP’s small policy team, but they often involve many other people. It is not unusual for the legal and regulatory teams to play a strong advisory role.
politics and at the GOC. The biggest challenge ahead is the ongoing review of the Opticians Act. We already know that it could involve threats to the protected functions that only optometrists can carry out, potentially undermining the profession. When put alongside the threats from online sales, legal and illegal, this could make a huge difference to our members’ roles and incomes, so it’s essential that we make the strongest arguments possible, backed by evidence.
How can members get involved?
the
We also usually involve the AOP’s Policy Committee and the virtual policy group, which is an open group of members who have expressed an interest in helping. For the really big consultations, we involve the whole AOP Council. We often involve members to let us know their views, via emails and the website forums. When we know the topic is likely to provoke strong views among our members, such as the Department of Health and Social Care consultation on making COVID-19 vaccination a mandatory condition for being able to carry out patient-facing care, we undertake member surveys to find out what our members think.
Sometimes we don’t get much warning of a consultation, but usually we know what’s on the way through our ongoing monitoring of what is happening in
The AOP’s voice is greatly strengthened by our membership. When we can quote our members, or give figures for their support for topics, it makes our arguments stronger. We also find that many members can offer specific information and opinions from their experience. We have a virtual policy group which is made up of members who have agreed to be consulted by email on topics that might be of interest. There is no obligation to send their views, but the members have been really helpful in commenting on things within their experience and areas of interest. Members who don’t want to be involved can still contribute by reading the occasional AOP policy update emails and responding to questions they are interested in, or by participating in our occasional surveys designed to measure member opinion. Anyone considering joining the AOP virtual policy group can express interest via policy@aop.org.uk.
published consultation responses at www.aop.org.uk/ consultations SAVE THE DATE
From education to guidance, the AOP has developed resources to support members in this evolving area of practice
The AOP has developed a day of education and refreshed resources to help members keep up to date with the field of myopia management.
Sunday 21 May marks the AOP’s second MAYopia Day.
The inaugural event saw more than 2300 attendees. Dr Ian Beasley, AOP head of education and OT clinical editor, confirmed that the programme for the 2023 event will be even bigger.
“It is very clear that myopia management is the topic of the moment, and because it is rapidly changing, it is important for practitioners to continually keep up to date with changes in the field.
MAYopia Day is there to serve that purpose,” Beasley said.
MAYopia Day will be delivered in partnership with headline sponsor, CooperVision, and is supported by EssilorLuxottica, Topcon, Johnson & Johnson Vision, Hoya, and Eyerising International.
The full day of webinar content will cover a range of different topics relating to myopia, approaches to myopia management and communication with patients.

Day will take place on Sunday 21 May. Look out for details about the full day of virtual education at www.aop.org.uk/events-and-education
The AOP has also recently refreshed a suite of myopia management resources to recognise changes within the “rapidly changing clinical landscape,” Beasley said. This includes guidance for members on myopia management.
Refreshed patient-facing resources includes a leaflet on myopia management along with a consent form to inform parents of children with progressive myopia, or those who are at risk of developing myopia, on current myopia management options. Resources for practices, including patient leaflets, can be found at: www.aop.org.uk/advice-and-support




To all members of the Association of Optometrists (AOP). This year the AGM of the AOP will be at the AOP’s office: 2 Woodbridge Street, London EC1R 0DG on Wednesday 7 June, commencing at 9am.
Agenda for the Association of Optometrists’ Annual General Meeting 2023
1. Introduction by the chairman
2. To receive and approve the minutes of the last Annual General Meeting held on 8 June 2022
3. Roll of deceased members
4. To receive the chairman’s report
5. To receive the chairman of Finance Committee’s report
6. To approve the Annual Financial Report and Accounts for the year ended 31 December 2022
7. To consider and, if thought correct, approve the proposal of the Board that BDO LLP be re-appointed as the Association’s auditors
8. Any other business.


PEER SUPPORT LINE FROM THE AOP
Supporting members at all career stages
In 2022, volunteers of the AOP’s confidential, free-phone Peer Support Line received 207 calls.
Launched in May 2017, the service, which is available to members and non-members, will mark its sixth anniversary next month. Since launching, it has received over 1350 calls from practitioners looking for a safe space to discuss any problems they may be experiencing.
Averaging over 17 calls per month last year, the three main reasons given for calling for support were: mental health (27%), employment (17%), and stress (16%). The service aims to provide practitioners at any stage of their optical career, including students,
with the opportunity to talk with a trained, empathetic peer who recognises the pressures of optical practice. Those accessing the service for mental health reasons has increased substantially since 2021 when it accounted for 15% of calls, up 12%.
What is the Peer Support Line?
Speaking to one of the AOP’s
36 Peer Support Line volunteers enables practitioners to talk through their problems in a dedicated non-judgemental space. Volunteers are trained AOP members who will not give advice, but will offer other possible sources of support and, where relevant, help callers to reach a resolution. Importantly, the volunteers understand the benefits of having someone listen who is impartial and has no personal agenda.
Calls can be on a range of issues, including workplace pressure, bullying, ill health, financial worries, bereavement, or anxiety about exams. No issue is too small or too trivial. Calls are completely anonymous and only a first name or alias will be requested.
Views from a volunteer
Speaking about the purpose and importance of the Peer Support
By Order of the Directors. Adam Sampson, chief executive, 2 Woodbridge Street, London EC1R ODG
1. Please note that a full set of the 2022 accounts will be available at www.aop.org.uk in advance of the AGM
2. A member entitled to attend and vote at the meeting convened by the notice set out above is entitled to appoint a proxy to exercise all or any of his or her rights to attend and speak and vote in his or her place. A proxy need not be a member of the Association
3. A form of proxy is available on the AOP website: www.aop.org.uk To be effective, the instrument for appointing a proxy must be deposited with the Association’s chief executive at the Association’s office (janicephillips@aop.org.uk) no later than 3.45pm on Friday 2 June 2023. Completion of the proxy does not preclude a member from subsequently attending and voting at the meeting in person if he or she so wishes.
The AOP’s Annual Report will be available at: www.aop.org.uk
Line, a volunteer, who has supported the line since 2017, shared: “The Peer Support Line is important because it provides the professional with a safe and confidential space to express their concerns.”
She explained that the volunteers to the line are experienced optometry professionals, which is “an added bonus” as “we really understand when they mention and talk about clinical things.”
The volunteer told OT listening is vital, before they discuss the options available to caller: “We don’t give advice, but if necessary we signpost the callers. It is a discussion for the caller to give them a safe space to talk.”
“We’re there to listen, and to show empathy, and be compassionate to people who need it,” she added.
The Peer Support Line IN NUMBERS
CALLS RECEIVED IN 2022
207 1350
MORE THAN 1350 CALLS RECEIVED SINCE ITS LAUNCH IN MAY 2017
NUMBER OF CALLS RELATED TO MENTAL HEALTH HAS INCREASED BY 12%
SINCE 2021
The number Call 0800 870 8401. Calls are answered 24 hours a day by an external answering service, with volunteers on duty to return calls between 8am and 8pm.






























Two decades in partnership Mondottica highlighted new Ted Baker frames at 100% Optical, as it celebrated 20 years of partnership with the brand. In the spotlight was ‘Vincent’ in ‘green tort’ – a retro-inspired shape for the new season. The signature Ted Baker ‘T’ is hidden within the hinges, while the brand’s magnolia flower emblem can be found on the inside of the end tips, providing what the brand described as a “spring-like flourish.” www.mondottica.com

Active eyewear
Bollé has revealed its new ecofriendly ophthalmic collection, with five models made from bio-acetate. The frames are equipped with the Bollé signature flex hinge, which the brand says has a resistance two times better than normal acetate and, in rotation tests, performed four times better than the norm.
Bollé’s demo lenses are made with 100% recycled material and the brand logo has been printed directly onto the lens to prevent the unnecessary addition of labels. The company’s intention to move towards a more sustainable approach is encapsulated in its ReactforGoodcampaign. www.bolle.com/gb/
Festival ready
Marcolin has spotlighted a new style from its collection with Guess Eyewear, designed for the festival season. The geometric acetate frame, ‘GU2968,’ stands out from the collection, with thin rims and an angular design embellished with gems to provide extra sparkle. Described as “bold and unapologetically feminine” Marcolin suggests the frame has a “distinctive personality.” www.marcolin.com/en/





Vintage inspiration
Eyespace showcased its 17-piece Cocoa Mint Sunwear collection, which takes inspiration from vintage fashion, modernised by runway trends and celebrity style influences. A highlight from the collection, the ‘CMS 2115’ sees sides made from bioacetate and a unique pressing technique that creates a crocodile leather effect surface pattern. The Cocoa Mint branding is etched onto a metal plate for a designer-feel. The model features category three polarised lenses in a warm grey graduation. www.eyespace-eyewear.co.uk



Optometrist and lifestyle blogger, Lizzy Yeowart, shares eyewear with a colour pop
Embracing the new season with bold eyewear in uplifting zesty colours.

Light and soft
‘Giggle’ has a youthful, light-hearted, soft-octagon silhouette in a choice of three uplifting colours. www.etniabarcelona.com
Head of buying for Hakim Group on colourful frames and taking patients on an eyewear journey
1
I have a thorough process for choosing my own frames. If I like a frame, and I think it looks good on me, I will then consider in which scenarios I would reach for that frame: whether a particular occasion, outfit, or mood. I don’t want a frame that is going to play the same role for me as one I already have.
2
I love all my frames. It depends on my mood on the day, what I’m wearing, how I’m feeling and where I’m going. I wouldn't ever be able to pick one pair. It’s no secret that Kirk & Kirk is probably my personal favourite brand. I’m known for my co-ordination, so it's important to me to have vibrant colours that I can then match to my outfits.
3
I think, particularly in the independent space, a role we play is to help take people on that journey. New glasses day –granted it happens a bit more in my house than in most – is still a really exciting day. You get them back from the lab and think: what am I going to wear tomorrow so I can wear my new glasses?
4
I’ve been stopped in the street by people asking where my glasses are from. Colour enables you to show your personality and stand out. If I inspire just one person to be a bit more colourful or choose something a bit bolder the next time they choose their glasses, then I think that is a really positive thing.

and joy
Inspired by the capital city of the US, this ‘Washington’ frame in tantalising tangerine celebrates freedom, power and joy. It is handmade in Slovenia. www.laibach-york.com

Apple of your eye
‘Hana,’ pictured in Apple, is a wellbalanced cat’s eye frame, designed in Brighton and fabricated in France from the highest quality acetate. www.kirkandkirk.com





















































The new Elle collection, by Charmant, fuses urban Parisian elegance with design flourishes. Models include rounded, retro looks, squares and, cat’s eye styles, and are adorned with horizontal and vertical French pleats and geometric forms. From the collection, the light ‘EL13533’ acetate frames have a soft cat’s eye style front. A curvy, pleated metal decoration with contrasting colour highlights is a key design feature. The frame is available in green, brown, grey and red. www.charmant.com

Silhouette has unveiled the latest addition to its Titan Minimal Art (TMA) range, with the La Ligne collection. The special edition, four-piece collection sees frames inspired by the editorial makeup that graces catwalks, fashion shows and photoshoots, with neonaccents, graphic shapes and bold lines. The brand’s high tech titanium material has been utilised in the oversized cat’s eye style, combined with accent rings. The frames also feature the TMA hingeless technology. www.silhouette.com



From
Spectrum Ophthalmics has introduced a new range of dry eye products, including the OptiClear IPL (below) and a 3nethra classic HD fundus camera. The OptiClear IPL uses light energy to stimulate and unblock meibomian glands, while the fundus camera captures high-resolution, undistorted images of the retina and surfaces such as the cornea, to assist with accurate dry eye disease diagnosis. www.spectrumophthalmics.uk


LOOK has released its new LOOK Bold line with three masculine and one unisex frame. The front is made of natural injection light polymer and the sides are made of Xinox steel. In additional to classic colours like traditional Havana or blue and black, four special edition options see an asymmetrical colourway where the left side of the frame is a canary yellow, deep blue, bright green or bright orange. lookocchiali.it


Cutting-edge
BIB Ophthalmic Instruments has partnered with Visionix to distribute its Essential Line product range in the UK optical market. Products in the range include both desktop and hand-held wavefront autorefractors and keratometers, an auto-phoropter, LCD Chart Displays, wavefront auto-lensmeters, a fundus camera, clinical and digital slit-lamps, and dedicated furniture solutions. www.bibonline.co.uk

To feature in OT’s Hit list, contact kimberleyyoung@ optometry.co.uk


The latest in lens tech
At 100% Optical, Nikon Lenswear UK launched Pure Blue UV (pictured), a new material offering enhanced protection against UV and blue light, without compromising the lens aesthetics and without any blue reflection. The Pure Blue UV is available exclusively with SeeCoat Next, the latest advancement in Nikon’s premium lens coating portfolio. SeeCoat Next has been designed with a unique diamond booster technology to ensure the topcoat sustains its highest levels of durability even after prolongued use. www.nikonlenswear.com/uk
Caron Eyewear has introduced its spring/summer 2023 collection of optical frames and sunglasses, with inspiration drawn from precious stones, bold retro styles and colourblocking. Described as the statement sunglasses of the season, the ‘Wild Thing’ is an aviator shape with a futuristic twist. The frame features contrasting front laminations that follow through to the angular sides. The model is available in black with fluorescent pink, black with Caron red, and black with bone. www.caroneyewear.com




























































EXETER EYEWEAR
Rob Barrow, director of Exeter Eyewear
1 2 3
Rob Barrow bought Spec-Care Ltd, the business that repaired his broken frames as a child, 20 years ago
The TR range was developed for Barrow’s nine-year-old son who needed securely-fitted spectacles that were comfortable
We have developed an accidental damage policy to keep playful children’s eyewear in great condition.

Unpicking a standout frame, by OT columnist Lizzy Yeowart

What led to the launch of Exeter Eyewear?

I was initially motivated to produce universally-fitted frames for young people that are fashionable and affordable. Exeter Eyewear has been a development of mindset. It was never really planned, but it did become a natural evolution of my work and changing role within optics.
What are the latest collections?
We have two very exciting collections releasing in 2023. Firstly, we have the TR range, a very light and robust collection offering enhanced fitting characteristics. These frames are perfectly suited to the increasing necessity of myopia management and have been placed with Norville, to be part of the new Blitz Kids range.
The second big release is with Bondeye Optical and is the first young person optical range they have catalogued, so we are very energised to support this development with such a dynamic business. The iPlay range is a highly adjustable product made from a newly sourced polyamide, that offers the practitioner superior quality and exceptional savings on comparative products on the market.
Are there any new products in development that customers should be aware of?
We have some great ideas planned. Some fantastic clinics have already trialled our new developments, and feedback and responses indicate they will be a huge success. Our product developments will be focused on supporting current collaborations and enhancing the unique features their ranges will become associated with.
Deconstructed cat’s eye shape

in three conversationstarting colourways: pink, yellow and orange
Loved by celebrities including Cameron Diaz and Jennifer Lopez
In the second part of a special report series on the IP workforce, OT overviews projects, pilots and practice models
Independent prescribing (IP) optometrists tell us that the benefits of the qualification convey clinical, professional and personal enhancements, but the logistics of using the qualification to its fullest extent can be a challenge.
In the second part of a report on IP – present and future – OT looks at the scope for IP in the community currently, what it means for practices, and some of the considerations for this growing workforce.
Collaborative working
During the COVID-19 lockdowns, Independent Prescribing Optometry Services (IPOS) drew on the skills of IP optometrists to manage complex eye conditions in primary care in areas of Wales. One such scheme was established in Cardiff and Vale, where an electronic patient record platform supported the safe transfer of patient data and images, as well as referral between practices.
Marc Drake, specialist IP optometrist and partner at Osmond Drake Opticians in Penarth, manages a rota of IP optometrists in the scheme locally.
Drake became IP-qualified in 2019, and in 2020, Sharon Beatty, the optometric adviser to the Cardiff and Vale University Health Board at the time, reached out to ask if he would consider being a part of an IP service. Within days IPOS launched and

of the pathway. Drake said: “We all hate it when we get no response from secondary care, so I always write to the referring practice.”
Drake suggested that, having delivered the service through the pandemic, trust between practices, and the relationship with secondary care, has grown.
Osmond Drake Opticians was one of four practices to start providing the service.
“The patients loved it, secondary care loved it, and it has kept going,” he said.
Now Drake dedicates two days of the week to IPOS. He said: “Day to day, we have a normal contact lens and refraction clinic running in one of my rooms and IPOS in the other.”
Drake, and his colleagues, take referrals from other practices across Cardiff and the Vale. Patients are triaged, seen and treated, and booked in for follow-up appointments. The hospital eye clinics will also refer patients to finish their treatment and monitoring in the community.
The practice does not market itself to patients attending through IPOS, and maintaining communication with the referring practice is a key part
Considering the scope of IP currently, he reflected: “IPs want to be able to manage the majority of anterior segment cases up to a point, and I think it’s very important to work collaboratively with the local primary and secondary care teams so that the care is joined up and flowing in both directions.”
Change is on the horizon for optometrists in Wales, following the agreement of contract reforms in 2022. In a statement announcing the plans, Eluned Morgan, minister for health and social services in Wales, said the changes seek to enable patients to access eye care services “delivered by the right professional, in the right place across the entire eye care pathway.”
With the new contract rolling out, Drake said: “Hopefully it should open up a lot of opportunities to expand what we do, or to fine tune what we do, to make it work better for everybody.”












Providing a picture of the scope for IP in Northern Ireland, Brian McKeown, vice-chair of Optometry Northern Ireland (ONI), AOP Councillor and an IP optometrist, told OT: “The scope for IP is slowly developing. IP optometrists can get their prescription pad after they pass their exams and then it’s up to them what they use it for. If you’re proactive you can use it to deliver a higher level of care.
“There certainly is a lot of good will with ophthalmologists who witnessed first-hand what IP optometrists in the community could manage during the pandemic.”
Considering the ambitions the professional body might have for the future, he said: “We feel optometry as a whole has a vital role to play in helping a congested NHS. ONI is working closely with the SPPG to ensure that optometrists always have a voice for future services.”
A pilot is just about to begin in Belfast that would see patients redirected from eye casualty to IP optometrists. At the time of writing, discussions with stakeholders are being finalised. It is hoped the pilot will be launched in the coming weeks.
McKeown explained: “Patients will be redirected from a casualty triage system to their nearest IP optometrist. The patient, suffering from iritis, foreign bodies or keratitis, will be managed in the community and a discharge letter, outlining diagnosis and treatment, will be sent to their own optometrist. The service will then be audited to establish whether it will be extended further.”
As of February 2023, there were 40 IP optometrists in Northern Ireland, with more undertaking the training. Looking ahead, what will this growing workforce mean for optometry?
“We need more IP optometrists working in the community to enable a regional IP service. Once we have that, then Northern Ireland will be extremely well-placed to offer a higher level of eye care in the community,” McKeown said.
“The big consideration is geographic coverage for any regional scheme. Also, are all the IP optometrists interested in working in a new service? When there is a willing workforce then appropriate remuneration needs to be discussed. The fee needs to cover the optometrists’ time and the enhanced skill level, as well as creating good value to the commissioner,” McKeown said. The fee for the new pilot is £90, he explained.
With optometrists the first port of call for patients presenting with eye concerns in Scotland, Eilidh Thomson,
A survey carried out by LOCSU in April 2021 showed that only 27% of Clinical Commissioning Groups who had commissioned either Minor Eye Condition Services or COVID-19 Urgent Eye care Services had also enabled access to FP10 pads for the local IP optometrists within the service.
Reflecting on the audit, Zoe Richmond told OT that progress has been made in the past two years, explaining: “Our purpose in performing the audit was to raise awareness and encourage local systems to consider solutions, working with their LOCs and primary eyecare companies.”
vice chair of Optometry Scotland and an optometrist for Black & Lizars, reflected that the balance is starting to shift towards more provision in primary care optometry practices.
Between 30–40% of the optometry profession in Scotland is made up of IP optometrists. Having the IP workforce as part of community optometry allows that provision to remain in primary care, Thomson suggested.
This means that patients can be treated closer to home, while secondary care can focus on cases that cannot be managed in the community. Thomson said: “I think that it makes it all more streamlined for the patient. That’s the main thing we are trying to do – make the patient journey better,”
This spring sees a pilot of the Community Glaucoma Service launch in Glasgow, through which IP optometrists who have completed the NHS Education Scotland Glaucoma Award Training (NESGAT) will support the safe discharge of glaucoma patients from the hospital to community optometry practice.
Once the pilot has been delivered, the next step would be to review the learnings and consider what is needed to roll it out across the country.
Meanwhile, plans are in development for a new scheme in Scotland that would outline a list of conditions that could be managed in the community, and would support referral between practices with and without an IP optometrist.
Thomson shared: “It is hoped that the new scheme will adequately remunerate IP optometrists to encourage business owners to support the service.”
Frank Munro, a founding member and clinical adviser for Optometry Scotland, has been involved in designing the new specialist supplementary
General Ophthalmic Services (GOS) examination – building on work carried out in Glasgow to design treatment ladders for anterior eye conditions.
The model, funded through GOS will focus on specific, complex areas of care, with 10 specialty supplementary GOS scenarios defined at present.
Munro, of Munro Optometrists, explained: “There will be a list of IP optometrists in that area who are willing to see those patients on behalf of non-IP colleagues. The IP colleague would see the patient, treat them, and feedback the results to the non-IP optometrists.”
With the plans for an intra-referral pathway in the works, Munro suggested this would be “another big step change in service development in Scotland, and establishing optometry as the main player for dealing with eye problems in the community.”
A variable outlook
In interviews with OT, optometrists seemed to agree that the opportunity in England to utilise the IP qualification to its fullest extent is variable.
Providing context, Dr Peter Hampson, AOP clinical and professional director, explained that the opportunity to use the full scope of IP “really depends on where you are prescribing.”
“There are a handful of practitioners who have built really quite developed business models around quite a wide
“The scope for IP is slowly developing”
Brian McKeown, vice-chair of Optometry Northern Ireland, AOP Councillor and IP optometrist
range of conditions,” he said, but pointed out that there are those who have the qualification, but feel they are not using it widely.
Funding and availability of FP10 pads is also an issue, he noted.
“Budget for the FP10 pad has to come from somewhere. Normally this comes from one of the local prescribing budgets; the GP prescribing budget, for example,” Hampson said, adding that this requires a balancing of budgets and a level of assurance – something that takes time to develop.
Zoe Richmond, clinical director of the Local Optical Committee Support Unit (LOCSU), told OT: “Within LOCSU we are well aware there is an interest from primary care practitioners to deliver a wider scope of clinical care, to better meet their patient needs, upskilling and taking on higher qualifications where needed.”
“At the same time, we hear significant frustration from practitioners with higher qualifications that they do not always have the opportunity to fully utilise these skills when working solely within primary care,” Richmond continued. “Even where there are appropriate local commissioning arrangements, empowering primary care clinicians to work in an enhanced clinical role, we often hear that this does not always extend to FP10 pads for IP optometrists.”
Local commissioning can lead to fragmentation and variation, but Richmond shared that consistency in the delivery of locally commissioned services has been increasing in recent years, pointing to the work of Local Optical Committees (LOCs) with LOCSU and the sector bodies to develop and publish national pathways and pathway guidelines, used by LOCs across England.
“My ideal would be a national extended eye care service delivered from networks of practices making optimal use of our collective clinical expertise –including those with high qualifications – and equipment and providing timely accessible care in local communities,” Richmond said, adding that LOCSU and sector bodies have “long called” for a national solution for England.
In 2022, CCGs ceased to exist and Integrated Care Systems (ICS) became legal entities in England. There are 42 ICSs in England, made up of Integrated Care Boards (ICBs), and Integrated Care Partnerships (ICPs).
With the new structure in place, Richmond suggested: “The move from local commissioning to large ICB commissioning footprints should help to reduce current unwarranted variation.”
Specsavers has seen prescribing as a norm in Australia and New Zealand for some time already. In England, however, Paul Morris, director of professional advancement for Specsavers, identified a “patchwork quilt” effect: “There isn’t one strategy for it. Optometrists have got to plough their own furrow, by offering private services, or I know some who have moved locations so they can more freely practise with the skills they’ve obtained.”
Michael Bradbury, clinical operations communications manager for Specsavers and an IP optometrist, also noted the variation across the country, but added: “I do think there’s been a positive move forward over the last couple of years, with the big uptake of CUES that came as a response to the pandemic. Hopefully there will be a positive legacy of that, a momentum to get more widespread access to those sorts of minor eye care services.”
Despite the variable approaches, IP will be a part of the future, as Morris suggested: “Whatever happens with the health economy in England, IP is absolutely enshrined in the psyche of optometrists and how they wish to develop.”
There were 40 IP optometrists in Northern Ireland as of February 2023
In targeted areas where IP forms part of the fabric of the health economy, the company is sponsoring IP courses.
Morris reflected: “Whenever I speak to people who have gone through the IP learnings, they all tell me that they’ve become more confident as clinicians, and that should not surprise us.”
How IP is incorporated into practice depends on services in the local areas, but colleagues are encouraged to use designated slots. Morris said: “Setting up and maintaining an appropriate diary over multiple consulting rooms can be complex. Our local directors and clinicians are best placed to understand their own health economy, having some sort of provision to meet the need, by using the data you have of previous clinics that have run, to predict what you'll need in the future and set yourself up accordingly.“
Forging a path
Leightons Opticians & Hearing Care is considering what its patient journeys might look like as optometrists seek out higher qualifications such as IP.
Kiki Soteri, head of clinical services for Leightons Opticians & Hearing Care, explained: “A lot of people think of IP as being related to providing NHS services, and our strength is in our private eye care provision.
“What we’re doing at the moment is looking at how we can deliver IP at a scale, and not waiting for the NHS to provide it. NHS England hasn’t
got to the same place as NHS Wales, NHS Scotland, or in Northern Ireland. Therefore, we kind of have to lead the way for private eye care, and IP, and how that fits in.”
Diary management and funding are key considerations to be balanced. Andrew Bridges, director of professional services at Leightons Opticians & Hearing Care, emphasised that without NHS funding, the fees have to be appropriate to sustain the practice, while Soteri added: “Emergency presentations or consultations may need follow up and review in a short timeframe, and that’s a very different way of working to routine eye examinations with long recall intervals. That would be one of the practicalities – thinking about how practice infrastructure and fee structure can support that.”
Supporting the learning of optometrists is key, Bridges shared, noting that more than 30% of optometrists in the company either have, or are studying for, a higher qualification. This is not limited to IP, of course, and the group is looking into how optometrists can be enabled to support local enhanced services, particularly in glaucoma.
Describing how he sees the scope for IP, Ian Cameron, managing director of Cameron Optometry, a Hakim Group practice in Edinburgh, said: “Patchy. If you’re in some practices or settings, there is significant scope to use your IP – even close to its fullest extent. I would say that is the case in our practice.”
Prescribing has always had some presence in his practice through the
30–40% of the profession in Scotland are IP-qualified
local GP, and so the IP qualification felt like a “natural extension,” and is now an integral aspect of the practice. Cameron said: “It’s part of everything we do.”
For the practice, Cameron explained, the ethos is: “Where possible, you keep the patient in practice, and you don’t refer them on or clog up NHS clinics unnecessarily. IP is essential to that if you are trying to manage eye problems and keep them out of other places.”
“That’s why, in my practice when I’m taking on somebody new, they need to be IP-qualified. Because it’s absolutely built into the fabric of how we run the place and how we expect optometrists to deal with the patient in front of them,” he added.
Having a high number of IP-qualified optometrists in the practice means the team can share learnings, or ask questions and gain a second opinion.
Evolving practice models
Dr Peter Frampton, practice owner of Aaron Optometrists, a Hakim Group independent practice in Ashington, Northumberland, told OT: “I find it difficult to imagine working without IP. It’s absolutely fundamental to all aspects of our business – not only ocular emergencies – IP is essential for our contact lens business and general optometry services.”
Frampton was one of the first 30 optometrists through the IP qualification. He told OT: “I am very proud to have been in the vanguard pushing the clinical envelope: 30 IP
A key focus for LOCSU is Optometry First, which seeks to utilise the core competencies of optometrists, supported by practice teams and higher qualified primary care practitioners, across a network of local optometric practices. Optometry First recognises the increased scope of care that can be delivered in teams including optometrists with IP, Richmond said, telling OT: “In the future we won’t look to our own practice team capability in isolation, but will work across a network of practices, recognising and fully utilising
optometrists, many in the hospital system, did not leave a lot to expand general community 'eye casualty’ services. However, it did allow time to evolve slowly and try a plethora of practice logistics to accommodate this new skill base.”
“Even now, there is no single recipe on how to incorporate IP into community optometry. Every practice has different sets of logistical, educational and service coverage challenges,” he shared.
In 2022, the practice introduced a new fee-based system for general eye exams. Under the new model, patients can see non-IP optometrists for a certain fee or via the NHS, or can opt to pay a top-up fee to see an independent prescriber.
“We think it’s a very fair system,” Frampton said, emphasising that the practice has not become completely private. While he initially had concerns around pricing, he described the uptake as “outstanding,” adding that it would appear “because we charge for this now but give people the choice, they value it more.”
He acknowledges, however, that the shift to the new model required the practice to have the reputation in prescribing to support it.
The cost to value ratio
IP optometrists described the value of the qualification, with Cameron sharing: “It makes my patient interactions and clinical work more enjoyable because I can use my skills and help people where I can. What I want to do as an eye care practitioner is look after people’s eyes and this helps me to do that,” he added, “I think it’s a practice builder.”
However, the profitability of IP can be a trickier part of the equation.
the skills in the wider team to best meet patient needs within local communities.” While this happens in ‘pockets of excellence,’ the approach seeks to make this commonplace. Making the best use of these skills, Richmond emphasised: “Practitioners should not be required to hold the same higher qualifications, but should be able to identify an area of personal interest and integrate care across a network of practices, based on local need, to make full use of their skills and maintain confidence and clinical exposure.”

“Seeing people for IP appointments is not as profitable as selling them a pair of glasses,” Cameron said, but added: “I think it’s important for the practice, and to progress the practice, and my optometrists, to give them and me job satisfaction, and to benefit my patients.”
“Even if financially, it is not the most profitable thing I can do with my time, I think it is overall sufficiently profitable in other ways that it is worth doing,” he summarised.
Frampton suggested: “General 'emergency eye’ management is more financially challenging, especially when many schemes, such as MECS and CUES, come pre-budgeted.”
“You have to restructure what you do and think outside of the box, developing practice processes that work to the budget” he advised, but recognised the hurdle this can present: “Managers tend to think in terms of replacement theory: they see it replacing the sales of spectacles, which does not necessarily make sound business sense. What you have got to try to do is come up with a business strategy where it is an alternative, additional supply – not a replacement one.”
He explained his view that a “different paradigm” is needed for IP optometry: “I think of them as two different businesses under one roof. The IP business may not be as profitable as our traditional core model, but practice processes ensure, ideally, it represents an auxiliary revenue stream rather than replacement.”
Reflecting on the ways IP optometry has changed, Frampton adapted the adage of ‘educate then legislate’ to ‘educate then instigate.’ For practices just starting out with prescribing services, the journey may be tougher.
“In my opinion, we have done it the correct way, but that has been a financially stressful process, because we had to commit to the educational and
“I think that it makes it all more streamlined for the patient”
Eilidh Thomson, vice chair of Optometry Scotland and an optometrist for Black & Lizars
logistical processes before we offered a valuable service. Here I am, 12 years on, and it is coming to fruition.”
Morris suggested that practitioners interested in higher qualifications shouldn’t wait for a service to train, explaining: “What I’ve learned over years and years of working with commissioners in audiology, as well as optometry, is that if the skillset is there, people will use it.”
With numbers of IP optometrists growing, Hampson explained that looking at the spread of the workforce, as well as the distribution of workload, would be important.
He suggested: “There is definitely an argument for – if you’ve got the workforce already, it makes it easier to then commission something.”
This is particularly true when taking into account that the IP qualification is an approximately two-year process.
“However, having the workforce in place is more complicated than simply having the IP optometrists – it is the distribution of them as well,” he continued, highlighting existing recruitment challenges, such as ensuring IP optometrists are established in more remote and rural places.
“Where are we going with all this? I think it’s about the new contract and good communication between primary and secondary care,” Drake told OT “Independent prescribers need to be able to do what it is that they want to do, but they also need to fit into the big scheme of things as well. I think there’s lots of scope for expansion, as long as it’s done in a collaborative way.”
Thomson reflected that the demand for IP training is already there amongst graduating optometrists, sharing: “If I’m undertaking an interview with a
relatively newly-qualified optometrist, one of the questions I always ask is what their career aspirations are for the future. I can’t remember the last time that somebody didn’t mention IP.”
Cameron also noted that Scotland has a significant cohort of IP optometrists, suggesting: “I feel the pendulum shifting towards that being part of the culture here.”
With the glaucoma service, and referral between optometry practices in the pipeline, he said: “If you want to be a player in any of those things, you’re going to need your IP.”
Looking at the current scope for independent prescribing, and considering the future, Soteri reflected: “I think we need to think more widely about the scope of contribution that optometry can play into helping people receive care closer to home, more conveniently, in a more timely manner, and that optical practices in the community do that at a time when our patients otherwise would have to go to a secondary care setting or hospital, wait a long time to see an appropriate professional, and those services are really overburdened right now,”
Considering what an expanded IP workforce might mean for optometry, and healthcare more broadly, Richmond reflected: “There is a need to better understand the current eye care workforce, as well as future workforce requirements of our new models of care. I’ve no doubt there’s a role for an increased number of optometrists with higher qualifications and IP in England, as we move to delivering more eye care locally and releasing capacity within hospitals for those with the most complex health needs.”
To read the first part of our special report on IP, which explored training and funding, scan the QR code here: 0


























42 How do I...
Supporting staff returning from parental leave, with AOP head of employment, Liz Stephenson
44 What I have learned Optometrist, Don Williams, and consultant, Professor Peter Shah, on the value of mentoring
46 Pre-reg focus
Pre-reg at Vision Express, Rochelle Anderson, on patient interactions and supervision
48 IP and me OT’s panel of IP optometrists discuss managing traumainduced anterior uveitis

In a roundtable discussion, hosted in partnership with VivaQuity, OT investigates how floaters are managed in practice, and explains the research behind a daily supplement that could have significant benefits for patients’ quality of life
While floaters may reduce quality of life as well as visual performance, many optometrists will be acutely aware that discussing treatment with patients is not always straightforward
– whether because of cost, hesitation around private treatment, or the potential side effects of surgery. Now, the answer could be found in a nutritional supplement that is new to the UK market – but that has
been used successfully in Germany for a decade. Designed to be taken daily, VitroCap N uses ingredients including vitamin C, grape seed, and citrus fruit extract, as well as L-Lysin and zinc, and has been found to
Dr Frank Eperjesi, optometrist and EyeTools co-founder
Dr Scott Mackie, optometrist and owner of Mackie Opticians
Dr Thomas Kaercher, ophthalmologist
Professor John M Nolan, Nutrition Research Centre
Ireland at South East Technological University.
decrease the quantity of floaters in 77% of patients across a double-blind, placebo-controlled study. The six-month Floater Intervention (FLIES) Study demonstrated significant improvements in subjective visual disturbances, as well as vitreous opacity density and contrast sensitivity. During a roundtable hosted in partnership with VivaQuity, OT spoke to two
FLIES in context: key numbers
343
The number of patients screened ahead of the FLIES study
61
The number of participants recruited onto the trial
6
The number of months taken to see a benefit to those taking VitroCap N
20%
The average shrinkage of floaters in 70% of patients taking the VitroCap N
67%
The subjective improvement success rate of the FLIES study 77%
The objective success rate (reduction in floater quantity) of the FLIES study.
UK optometrists about their current management of floaters in practice, discussed 10 years of experiences of VitroCap N with a German ophthalmologist, and heard from an Irish vision scientist about the years of research that have gone into confirming the supplement’s viability.
Identifying vitreous floaters in the testing room
In Scotland, Dr Scott Mackie finds that he rarely goes a day without encountering a patient who is being troubled by floaters – in fact, he identifies around 10 instances of posterior vitreous detachment (PVD) every month. He initially asks the question as part of his history and symptoms, and follows up by identifying how much the floaters impact on quality of life. “I move on to ask if their floaters are getting worse, regarding duration or intensity,” Mackie, owner of Mackie Opticians, a Hakim Group practice, explained. “I ask when it troubles them the most. Night driving with floaters is a nightmare.”
For Mackie, coming across a retinal detachment is much rarer than it is a PVD – allowing quality of life to be the main discussion point. As well as night driving, he sees reading as something that can be vastly impacted by floaters. He demonstrates the effect that floaters are having via a low contrast chart, which he finds “a bit of a game changer” for patients.
The Scottish requirement to dilate every patient means that Mackie sees more floaters than he might in another location – especially in myopes, as the vitreous
starts to deteriorate after the age of 21.
In the West Midlands, optometrist Dr Frank Eperjesi finds that floaters tend to present in one of two ways: the patient identifying the condition themselves and seeking out help, or through history and symptoms.
In the first instance, Eperjesi moves on to identifying whether the patient has a retinal tear or detachment, or whether there is one impending.
“When they present and volunteer that information, I get concerned, and obviously that opens up a whole raft of tests that I would do,” he explained.
When floaters are discovered, Eperjesi said, “I further investigate that by asking, ‘How long have you noticed them for? Do you have many of them? Do they trouble you in your everyday life?’”
He believes that VitroCap N can provide a treatment option for those patients
“You can improve a person’s quality of life by advising them to use VitroCap N”
Dr Frank Eperjesi
who are troubled by floaters, but do not have a retinal tear, where there might not have been a solution previously.
“Because now we’ve got VitroCap N available, there’s a possibility of treating those people whose quality of life is affected by their floaters,” Eperjesi said. “That’s not something I used to ask much in the past, because,
other than vitrectomy or laser vitreolysis, there really wasn’t anything available for a person who had floaters that were troublesome to them. “Now there is this alternative, I think it’s incumbent on the optometrist to further pursue and ask questions of the patient who says they have floaters,” he added.
Making the case for capsules
Although Eperjesi believes that VitroCap N will allow him to treat his patients in a different way, he still raises a note of caution around persuading patients to invest in the treatment.
Making the tangible benefits to the individual’s day-to-day life clear is key, he said: “Either they have to volunteer that there is trouble in their everyday life, or have it pointed out to them through a thorough history and symptoms and low contrast sensitivity charts.

“People don’t buy into something unless they’re going to get some benefit. So, I need to point out to them the potential benefits of using something like VitroCap N. I think it’s important to find out why that person would invest that time and money,” he added.
Mackie believes that patients are wary of taking
oral tablets when prescribed by an optometrist. This is something he has seen during his time as an independent prescriber. With a preference for “conservative management” over “something as invasive as surgery,” Mackie finds it helpful to balance the pros and cons of oral treatments when discussing with patients.
“There are a couple of points that you have to discuss with people,” he said. “One thing we should let people know is the daily recommended limit. If you look at the daily recommended limit for zinc, or for vitamin C, the tablets are well within that, for men and women.”
In Heidelberg, Germany, ophthalmologist Dr Thomas Kaercher finds that his patients expect a full explanation of the treatments that they are being offered.
He shared a recent scientific paper, in which an elderly gentleman with Parkinson’s had tried to remove his floaters with water, causing erosion of the cornea.
“This indicates how severely affected the patient can be,” Kaercher said. “Not realising that the floater is inside the eye can cause injuries. This gives us good impression of how the patient feels. We should modify and correct this wrong impression.”
Incorporating into optometry practice Eperjesi said that the key message he will take from the FLIES study is the improvement in quality of life that VitroCap N can give to patients. “You can improve a person’s quality of life by advising them to use VitroCap N,” he said.
Nolan on why floaters should not be thought of as “just a nuisance”
Alongside FLIES, various papers have been peer reviewed and published over the past six years, including a major review of the nutrients and enzymatic and non-enzymatic antioxidants of the vitreous, and a study into why micronutrient intervention would benefit patients with vitreous floaters.
Nolan explained: “One of our first publications was to demonstrate that, in a patient with the presence of floaters, regardless of stage of disease, all the way up to PVD, contrast sensitivity was reduced by about 65%. The effect that has on their visual function is remarkable. We demonstrated that very clearly.
“It confirms that we shouldn’t look at the person’s floaters as just a nuisance. They’re not just bothersome opacities in the way of the patient’s vision. They are something that greatly affects visual function, and therefore eye care should be attentive to finding ways to try and reduce the burden for patients. That is the job of eye care.”
“You’ve got to set them up properly. I think the science speaks for itself. I think it’s how you then take that and go forward with it”
Dr Scott Mackie
He added: “Optometrists sometimes say, ‘I’m not a salesperson, I’m not selling tablets, I’m not selling glasses. I’m a clinician.’ But we need to get beyond that and focus on the quality of life. That’s a big message: that they will be doing the right thing for a large proportion of their patients who are struggling with floaters.”
Mackie agrees that quality of life needs to be the point that is emphasised. In paying for the capsules, he suggests setting up Direct Debits.
“We give them six months of tablets up front, and they’re always paying in arrears, because you don’t want a patient trying it for a month and saying it didn’t do anything for them and that’s enough,” he explained. “You’ve got to set them up properly. I think the science speaks for itself. I think it’s how you then take that and go forward with it.”
Professor John M Nolan wants to stress that the micronutrient is “not a silver bullet at this point in time,” but rather

something that patients need to understand the value of complying with.
“It represents a lifestyle change,” he said, adding that “you have a very easy experiment every time a patient makes the decision following the information you give them to try this. If it doesn’t work, they’ll stop doing it.
“But what we’re seeing is, that’s not the case. The people in the trial have stayed on it, and the people that have tried it after a recommendation from their clinic have stayed on it too.”
He added: “The patients know a lot about this now. Eye care professionals have a duty of care to be alert, because people who are suffering do their own research. They want to know. So, I think it’s a new approach: a patient-led discussion. They want to know about it, and they want the information.”

“Eye care professionals have a duty of care to be alert”
Professor John M Nolan 0

“I’m very optimistic about the future of the profession”
Optometrist Christian Dutton on how his interest in medical technology has brought new opportunities
My father is a dentist, and was supportive throughout the careers process. I was keen to do something clinical. Medicine took too long, and I wasn’t keen on needles, so dentistry was out. Optometry seemed like a clean and interesting career. As a spectacle wearer, I’d already experienced the benefits first-hand.
I studied at the University of Manchester Institute of Science and Technology from 1995–1998. The tutors were excellent, and I made a number of lifelong friendships. I enjoyed learning with a range of students of different ages, backgrounds and cultures in a large, vibrant, but rather rainy, city.
I joined Boots Opticians’ Undergraduate Summer Work Experience Programme in 1996. I remember coming home exhausted after my first few days of ‘proper work.’ This led to a pre-reg with Boots, which had a great reputation and a fantastic team of ‘tutor practitioners.’ I qualified at 21 and looked like I’d just left school.
The first years of my career were spent at Vision Express. Upon qualification, colleagues and patients suddenly had quite different expectations of me. I enjoyed building rapport with my patients and providing staff training for the first time.
A role came up with Asda Opticians, which had branched out into optics and opened a practice in Farnborough. While there, I had the opportunity to write clinical guidelines and policies, which piqued my interest in professional services. I also maintained an interest in postgraduate education and completed a Master’s in clinical optometry through City, University of London, which gave me a clinical edge.
I had been interested in Tibetan culture since completing a module on ‘the philosophy of science’ at university. Asda Opticians granted me leave to set up the Tibet Eyecare Project, helping several thousand people see more clearly without charge. Over the following years, I designed and fundraised for a
purpose-built clinic in Yushu to improve the quality and volume of care provided. I led groups of volunteer UK optometrists and broadened the scope of the project to incorporate dentistry and midwifery. We trained local people and sponsored students. I travelled to Tibet five times, and met my future wife there.
In 2016 I moved to a professional services role with Evolutio Care Innovations, a community ophthalmology provider. My focus was on education and training, quality improvement, and triage.
In 2019, I completed an independent prescribing diploma and a higher professional certificate in glaucoma, both of which required me to be in hospital under the mentorship of a lead consultant. These qualifications have given me the knowledge required to manage a greater proportion of patients autonomously.
“I qualified at 21 and looked like I’d just left school”
It would be nice to be able to develop a medical record system, not necessarily for optometry, but any healthcare discipline. The efficiency of this is crucial to optometrists, because they need to get through a decent volume of patients. If you’ve got a system that works with rather than against them, everything is much smoother.
“My Plan B?”
Computer science and data analytics.
Having read and triaged over 100,000 ophthalmology referrals, I recently launched a YouTube channel, Dutton Optometry, where I offer my tips on writing referrals for a wide range of conditions as well as jargon-free patient education videos.
My next move is to the Specsavers clinical performance consultant team. I will be developing community practices and clinicians, so patients have access to the eye care they need now and in the future. Each consultant has a regional responsibility, tailoring their support to the needs of local optometrists, the health service and patients. My patch is in the south of England. Specsavers’ purpose is to improve lives through better sight and hearing, and I’ll be helping to make that positive difference.
COVID-19 has been the catalyst for change, and I feel that it’s time for us to come together to drive the profession forward in a unified way, making the most of our skillset. Optometrists shouldn’t be afraid to develop themselves. I consider optometry and the hospital eye service to be one big team; we’re supporting one another for the benefit of our patients. It’s a good time for us to demonstrate how we can help them. I’m very optimistic about the future of the profession.
0














Registerfor the free educationalplatform whichoffers engaging,innovative,and up to the minutetrainingfor all. Whetheryou are a student, retail associate,store manageror seasonedopticalprofessional,there will be somethingthere to interestyou.
Features to explore:
• Check out the News section for details regarding live CPD events
• Listen to latest research and scientific information from leading optical experts
• Support your practice staff with their learning
• Gain top tips for success from other optical professionals and share your own
• Find tools to help your contact lens practice and information to aid your business to grow
• CPD modules always available and developing, with new content monthly
• Build your personalised learning portfolio complete with downloadable and printable certificates.
Join us and become part of the CooperVisionlearningcommunity.


Register now by scanning ~, .::,::·g;~~;the QR code.

AOP head of employment, Liz Stephenson, explains how employers can comply with their obligations towards those returning from maternity, paternity, and shared parental leave
Returning from maternity, paternity or shared parental leave can be a nervewracking time for employees, so it is in everyone’s interests that any possible issues are discussed and addressed as soon as possible.
During maternity leave
You should ensure the employee is kept informed of any changes in the business, particularly:
Any jobs being advertised
Any promotion opportunities. They should also be included in any workplace consultation for redundancy or re-organisation.
Someone on maternity leave can carry out up to 10 ‘keeping in touch’ days without bringing the leave to an end, and similar rights exist for shared parental leave. More information on keeping in touch days is available via Maternity Action.
Working hours
It is a good idea to have a flexible working policy that is publicised to all staff. If a request is going to be
made it is helpful to know in good time, as there are statutory requirements regarding how you deal with such requests. More information can be found via the AOP’s Managing flexible working page. There is no right to have it granted, but the employee could have legal remedies if the flexible working request is not dealt with properly, or if it is dealt with in a discriminatory way.
Working arrangements
Before or when they return, it may be wise to allow the employee to ease themselves back into the workplace by, for example, offering training on any equipment before they start testing patients. You should be prepared to offer slightly longer testing times, for example, if they indicate that this would be helpful.
Health and safety
You have a duty to provide a safe workplace, and to carry out risk assessments in respect of pregnant employees, as well as those who are breastfeeding or have given birth in the past six months. More information is available via the Health and Safety Executive.
Breastfeeding mothers

for an employee to rest if they’re breastfeeding. You’re not legally required to provide somewhere for employees to breastfeed or express milk, but they may ask if you can organise something – for example, a private room and a fridge to store the milk.
It may help to highlight to staff any policies you have around dependent leave. You can highlight how and when you should be informed of the need to take any such leave. Be aware, though, that the nature of it means their need may be urgent or unexpected. You may also ensure that employees who need to be contactable during working hours (for example by nursery or care providers) are allowed to check their phone and to provide the practice phone number to the relevant people.
Future changes
The law is constantly changing. Some things to look out for include:
Read more articles from our extensive How do I... series on our website www.optometry.co.uk/ how-do-i
to those who have returned from maternity leave within the past six months.
Changes to flexible working rules
It was announced in December 2022 that the law (in England, Wales and Scotland) is due to change as follows, although it is unclear precisely when this may happen:
The right to make a flexible working request will be a day one right, as opposed to the current arrangement where employees need 26 weeks’ continuous service
Employees will no longer need to explain the effect their request might have on their employer
Employees will have the right to make two flexible working requests every 12 months instead of one
0 0 0
Employers will be required to consult with their employees on other options before rejecting a flexible working request
The deadline for an employer to decide if they will approve or reject a flexible working request will be shortened from three months to two months.
“The employee could have legal remedies if the flexible working request is not dealt with properly” Get
As an employer you must provide somewhere suitable
Changes to redundancy protection for new mothers Currently, if an employee is made redundant during pregnancy or maternity leave they must be offered any suitable available vacancy. This right is to be extended
For help, contact the AOP’s employment team on: employment@aop.org.uk












WHAT I HAVE LEARNED

Optometrist, Don Williams, and consultant ophthalmologist, Professor Peter Shah, explain the mutual benefits of their mentor-mentee relationship
Don Williams (DW), optometrist and director at Edgbaston Eye Clinic
When did your mentorship with Professor Shah start?
DW: Over the years, I’ve been tutored and mentored by various brilliant consultants. You can’t put a price on the experience you gain.
When I started my practice, in 2017, I had Professor Shah and others to help. We supported each other. Then, Professor Shah took a lead role in mentoring.
That relationship has got stronger over the past few years. I’ve just finished my diploma in glaucoma, and he mentored me through that. Every Sunday morning at 8am we had an hour’s Zoom, where we discussed complex cases and how to get through the exams. It’s great, because you don’t feel isolated.
How long have you known mentoring is important?
DW: When I started my career, I was a locum. I realised, after about a year, that my knowledge was not as good as I thought. That’s when I said to myself, ‘I need more experience. I need someone to really guide me here.’ So, I left High Street practice after about a year and a half and started hospital work. I knew that to learn, I needed
someone who knew more than me. I’ve been lucky enough to work alongside helpful, friendly consultants. I cannot stress enough the importance of mentoring.
How has mentoring improved your workplace?
DW: The more you broaden your comfort zone, the better it gets. With experience and knowledge, you become more comfortable as a clinician. For me, that’s the main value: the experience and comfort of managing my patients.
What is the most significant lesson you have learned from your mentor relationships?
DW: You have to listen to your patients. Don’t assume you know everything. Always ask. I cannot stress enough the importance of listening to every patient.
Do you have advice for other optometrists on finding a mentor?
DW: When you come out of university and your pre-reg year, you think you know everything. But you should realise your knowledge is fairly basic. To improve on your knowledge and experience, it’s important to find someone who is willing to tutor you.
Finding that person is not easy. You have to put yourself out there. Hospital work is a good start. When I first started doing hospital work, I wanted the clinical benefit: the experience and knowledge. I was thirsty for that at the start. You have to enjoy learning.
Professor Peter Shah (PS), consultant ophthalmologist and glaucoma specialist How long have you been aware of the value of mentoring?
PS: When I look at my whole career, 42 years in the NHS, I’ve had a stream of great mentors. So, I knew the power of mentoring through direct experience as a mentee. I started mentoring people when I was at registrar level, but when you become a consultant, you’ve got a much bigger team and you interact with more people. So, when I became a consultant in 1999, I really threw myself into mentoring.
What do you think the key benefits of mentoring are?
PS: Becoming a mentor enriches your own life as well as that of your mentees. There are huge benefits that you accrue for yourself, not least of which is that you have a great network of people that you can call on to work with. You future-proof yourself, because many of the people you’re mentoring might be a lot younger than you. In interacting with them, you’re going to learn new skills yourself. Mentor because it’s the right thing to do, but don’t forget that it benefits you as well. Mentoring is a two-way relationship. You’ve got knowledge flowing both ways.
The AOP provides a professional development mentoring programme that is free to use and is designed for pre-registration, newlyqualifed and locum optometrist members. For more information and to sign up to be matched with a mentor, visit: www.aop.org.uk/ mentoring
Any advice on finding a mentor?
PS: Finding a mentor is tough. The number one piece of advice is to avoid isolation. If you’re isolated, and you’re not part of a network, it’s going to be very hard for you to find the kind of people who would want to help you. Your first step might be to build networks, maybe with other optometrists or with secondary care, or through social media. They’re not just going to walk into your life. It’s an active process.
How do you think the mentor/mentee relationship can positively influence the workplace environment?
PS: If as many of us as possible become mentors, we’re creating a more nurturing workplace, where people can be listened to and express their ideas. It moves us away from bullying cultures. Mentoring allows you to influence the culture of an organisation, a business or a profession, in a very positive way.
AOP mentoring scheme 0
Share your story
Get in touch if you would like to share your experience with OT lucymiller@optometry.co.uk









































































































































PRE-REG FOCUS
“Obtaining a second opinion has been invaluable”
Pre-reg optometrist at Vision Express in Chiswick, Rochelle Anderson, on the value of her placement supervisors
My pre-reg placement has helped me become a more well-rounded, independent clinician. It has given me hands-on experience, which has increased my skills and my depth of knowledge. Through increasing my confidence when dealing with certain patients, such as young children or those with binocular vision abnormalities, I have become much more competent. I have also learnt to appreciate the extended amount of testing time I am able to have during this pre-reg period, as opposed to that which some qualified optometrists have. This year has shown me the areas I feel most confident in, and the areas I still need to improve on. Obtaining a second opinion has been invaluable: I have used other optometrists for personal growth, clinical opinions and maintaining professional standards. This has enriched my experience and provided a solid foundation of knowledge necessary to


become a safe practitioner. During this placement, I have worked effectively as a new team member within an established team at my practice. I have learnt how to communicate well with work colleagues regarding dispensing queries, seeking advice on how to dispense high prescriptions, sorting out vouchers, and ordering lenses. When I worked in previous practices, I always acknowledged the need for

what type of patients will come through the door. Emergency patients, those with acute eye problems, or those who have mixed up their appointment time, can walk in on the same day, and all have to be seen. These unplanned patient episodes can be fascinating. I love any patient-clinician interaction where I can make people feel comfortable enough to open up about concerns regarding their health, lifestyle, or sight.
“I really do appreciate the patience and courtesy people have offered me”
everyone to play their role, as that is vital to ensure the day and the patient experience run smoothly. Now I am a pre-reg, I appreciate the patience people have offered me, allowing me time to organise my patient records and care.
My day-to-day experience has varied. There have been times when I have not known
Working on the practice floor has made me aware of the daily struggles patients have with broken or faulty glasses. This has given me an opportunity to give great customer service, and to resolve issues patients have had, both big and small.
My supervisors are supportive, and are on hand to double check any
Education Library. OT’s Education Library contains CPD and Skills guides on 31 topics www.optometry.co.uk/ cpd/education-library
abnormalities, queries or concerns I have with patients. They have all tried to make me feel comfortable and show me the interesting cases that don’t present often. I have discussed and had support with different pathology. That has underpinned my approach to care, and has helped me to articulate my management to the patient. I have one supervisor who encourages me to ask questions and knock on her door if I am unsure of anything. This support is invaluable, and should be available to all pre-regs. Standout moments include the numerous instances of alternating exotropia that I have seen in the past few months. Also, the number of appreciative patients who have offered me chocolates and kind words in the consultation room. I enjoy receiving positive patient feedback at the end of an examination. It makes me feel valued and appreciated, and confirms that I am giving good care.
0
My favourite part of the pre-reg is... gaining handson experience in a diverse clinical setting. We get to learn and practise a wide range of skills, from basic patient care to complex diagnosis and management of eye conditions. Working in a teaching hospital offers an opportunity to be close to leading research in the field, from developing technologies to innovative new treatments.
My least favourite part of the pre-reg is... the difficulty of balancing the demands of clinical practice with the intense studying and training that is required in order to gain the qualification. Being a pre-registration optometrist means embracing a steep learning curve, and striving to perform at the same level as highly qualified colleagues.
Before I started my pre-reg, I wish I’d known... about the level of organisation required in order to deal with the large number of administrative tasks. This is something I have adapted well to, but you need to ensure to make time for it on a daily basis so you don’t get overwhelmed.
AkshayShahisapre-registration optometristatMoorfieldsEye Hospital,London Akshay says…



































OT presents a clinical scenario to three of its resident IP optometrists. This edition: managing unilateral, trauma-induced acute anterior uveitis
Ceri Smith-Jaynes, OT clinical multimedia editor, IP-qualified: 2018
Farah Topia, AOP clinical adviser, IP-qualified: 2016
Kevin Wallace, AOP clinical adviser, IP-qualified: 2012.
The question: Recently, a patient presented at my practice with unilateral, trauma-induced acute anterior uveitis. Dilated examination revealed a few inflammatory cells in the anterior chamber, however the vitreous and fundus were healthy. I’m interested in hearing how you would manage this patient?
OT’s panel says...
Ceri Smith-Jaynes (CSJ): The first thing I would do is establish what happened and when. Are we talking squash ball at high-speed, or someone’s finger poked in their eye? A history would include questions about vision, pain, photophobia and diplopia.
a corneal abrasion or a biff on the sclera?
Farah Topia (FT): You might want to ask specifically about any auto immune conditions or prior infections. The onset and the duration of symptoms is important in trying to ascertain the underlying cause. If it’s not trauma related, an underlying systemic disease has to be considered, particularly if the patient mentions previous episodes. A full history is key and, as Ceri has said, if it does seem to be trauma-related, the type of trauma will help give an idea of what else you need to be looking out for.
CSJ: I assume we checked motility, looked at the pupils, and measured visual acuity before dilating.
FT: Even if the trauma is to one eye, it’s important to check both eyes as the inflammatory response can affect both.
CSJ: I’d have a look for any synechiae or even the imprint of the iris in the anterior lens from the force of a blow. I’d also check for hyphaema, keratic precipitates and hypopyon.
I like to use the Standardisation of Uveitis Nomenclature (SUN) Working Group grading scheme to record cells or flare, so I can quantify any improvement (or the ophthalmologist can, if I am referring).
“The onset and the duration of symptoms is important in trying to ascertain the underlying cause”
Farah Topia, AOP clinical adviser
FT: I agree with Ceri’s management. If there is trauma involved, you have to consider other pathology compared to a simple anterior uveitis. With anything impacting the eye, you should counsel the patient on retinal detachment signs and symptoms just so they know what to look out and what to do if their symptoms change.
0 0 0 0
Also, I’d ask about previous iritis and health conditions, for instance, what if this wasn’t caused by the trauma? Is the anterior chamber reacting because of
CSJ: Intraocular pressure (IOP) is important for two reasons: it can go up or down in trauma, and if I do end up prescribing a steroid, I’ll want a baseline measurement.
FT: The IOP is also helpful to rule out angle closure as a differential diagnosis.
In my area, we have an agreement with the local eye clinic that independent prescribers will assess iritis, start treatment and refer to the hospital for follow-up. I’d give the eye clinic a call first, but if there is no corneal abrasion, it’s likely I’d prescribe 1% cyclopentolate three times a day and 1% prednisolone four times a day and refer on for followup in a few days. The patient may need to take their usual over-the-counter painkillers. Traumatic iritis tends to respond more quickly to steroids and can be tapered more quickly than usual acute iritis. I’m not able to do gonioscopy, which I think is important in some trauma cases to rule out angle recession, so I’d be glad for the ophthalmologist’s view. They can be on the lookout for trauma induced glaucoma and take a second look for any retinal breaks too.
CSJ: Oh, and don’t forget to give the patient advice about eye protection before they leave.
Kevin Wallace: I agree with Ceri and Farah’s comprehensive options already presented and would manage my patient in the same way. I am glad that the patient was dilated, as it’s important to assess the internal eye in cases of a significant impact. It is always good practice to finish by recommending appropriate safety eyewear to reduce the chance of this sort of injury happening again.
For more information
If you are unsure about managing a scenario in practice, email: regulation@aop.org.uk
If there is a scenario that you would like to hear our IP optometrists’ views on, email: lucymiller@optometry.co.uk








Six months after becoming co-owner of the independent where she had worked as practice manager and optical assistant (OA) for 18 years, Donna Lowther has not come to terms with what she has achieved.
Her slight state of shock is understandable: after nearly two decades at County Durham independent, Sight Ltd, 2022 saw her career move up a gear with a dispensing optician (DO) course via Bradford College.
The results confirming her DO qualification came through on 30 September 2022, and on 1 October, she officially became the practice’s co-owner.
“I was practice manager and then went on to do the DO course so that I could go into directorship,” she explained. “I put it off for years. I never thought I could be a DO. But the previous optometrist said, ‘you can do this.’ He kept pushing and I was like, ‘okay. I’ll give it a go.’ I ended up with a distinction, so I thought, ‘Oh, I knew something then.’”
She shares the business with the resident optometrist, whom she already worked alongside.
“It was an opportunity: rather than [the previous owner] sell to somebody we didn’t know, we got our heads together,” she said.
In terms of branding, she said, “we’ve kept everything the same. We are a good community. Our patients know us on first name terms. It didn’t make sense to make
“It is the goal, when you
go into optics, to do something
like this”

realising that minor tweaks –like putting lights in practice windows – can have a bigger impact than she had expected.
“To be given the opportunity is beautiful. I just love it”
Donna Lowther, new co-owner of Peterlee independent practice, Sight Ltd, on why she never expected to succeed in her ‘pipe dream’ of business ownership
it look like a new business, because it’s not. It was founded in 1984, so it’s got a personal patient base.”
Speaking about her route into ownership, she said: “It was a pipe dream. I’ve still got impostor syndrome. I feel like it’s someone else’s life that I’m living right now.
“It is the goal, when you go into optics, to do something like this. To be given the opportunity is beautiful. I just love it.”
She added: “I always knew I wanted to go bigger than what I was doing, so I could make the decisions on what was best for patients. Since doing the DO course, I’m quite big on low vision. I’ve got together with [visual aid supplier] Associated Optical and we’re hosting events. It’s something I wouldn’t have been able to do before. Now, I can support the community in different ways.”
The value of relationships Her move into management has seen her make an effort to prioritise relationships with her staff. “If I’ve got a
happy team, I know patients are going to get looked after,” she said, adding: “The girls know that they can text or ring, at any time. It’s a bit tricky to go from friend to boss, but I’ve made sure that they know that I’m still me. If I’ve got any concerns, we’ve got a really good relationship, where I can take it to them too.”
Lowther explained that in the longer-term, she is planning to bring in MiyoSmart to ensure that she can serve younger patients, and will be focusing on ensuring that all her staff have the knowledge to talk about it confidently. For now, though, she is
She explained a recent conversation that, based on the fact that the practice has been in its current location since 2000, surprised her.
“The first day I put the lights in the window, I had a guy come in and say, ‘When did you open? I’ve never seen you before,’” Lowther said. “I asked, ‘Well, how have you seen me today?’ He said, ‘because you’ve got lights on.’ They are little things, but they are making a big difference.”
Has her confidence improved through her new venture? Lowther’s answer is clear: “Absolutely. Now, if I’m asked a question, I’m confident with my answer, and I’m confident to support somebody else with similar situations. My confidence is great now, because of this.”
She added: “The flexibility of becoming a business owner is becoming more apparent. Putting my own spin on our practice and being able to juggle work and family life is easier by the day. I’m loving this experience and I’m so grateful I’ve got this amazing opportunity.”
0
Donna’s three tips for aspiring business owners
1 Get connections beforehand. Optics is such a small world: you don’t realise who you know. If you can find somebody to help you, it’s definitely worth it
2 Have faith in yourself. That’s the one thing I didn’t have. My confidence was asking, ‘how am I doing this? I’m a little colliery girl. How do I do things like this?’ I wasn’t born with money or knowledge. Nobody is, really. It’s surreal
3 Go for it. Just go in there and do it. Don’t doubt yourself.




























April is Stress Awareness
Month, an event that has been taking place for 21 years – although the conversation around the causes of stress and its impact in both the short and long-term has become more pronounced over the past decade, and even more so recently as a result of COVID-19.
It might be a common topic of conversation – who hasn’t pressed a hand to their temple and muttered “I am so stressed out” on a hectic Tuesday afternoon? – but the reality and nuances of stress make it a broad subject, and one that can often feel too nebulous to practically contend with.
In order to try and address at least part of this huge subject, the AOP and OT have turned their attention to a particular consequence of stress: burnout, which the World Health Organization (WHO) defines as an “occupational phenomenon.”
By classing it in this way, the WHO categorises burnout as a factor that influences health status or contact with health services, but not as a medical condition. It further defines it as “a syndrome conceptualised as resulting from chronic workplace stress that has not been successfully managed.”

Burnout is the WHO-defined “occupational phenomenon” that has the potential to drive us to exhaustion. Here is what you need to know
overwhelmed, trapped, defeated, detached or alone, having a cynical or negative outlook, experiencing feelings of self-doubt, and procrastinating or taking longer to get things done, to the list of common signs.
Mental Health UK also emphasises that burnout is not something that goes away if ignored – in fact, it is likely to worsen if the underlying issues aren’t addressed.
DID YOU KNOW?
One in five people feel unable to manage stress and pressure in the workplace
(source: Mental Health UK)
Ignoring the signs could “cause further harm to your physical and mental health in the future” and could lead you to “also lose the ability and energy to effectively meet the demands of your job, which could have knock-on effects to the other areas of your life,” the charity said.
feelings of overwhelm that you might have about completing things that seem unmanageable
Use self-help cognitive behavioural therapy (CBT) techniques: the NHS has a page that can give further information on how CBT might be beneficial to you
Speak to someone: in the first instance, it is likely to be friends or family that you turn to to discuss how you are feeling – but as burnout is work-related, speaking to colleagues or your manager about workload and particular
pressure points is the only way to address what you are dealing with head-on. Mind, the mental health charity, also lists advice for avoiding and dealing with burnout. They include: Making sure you get enough sleep
Finishing work on time
Ensuring you take all your annual leave
Taking time off while experiencing burnout, rather than trying to power through
Asking for help.
If you are an employer or practice owner who is mindful of the impact of burnout on staff, Mental Health UK advises creating a wellbeing plan, which can be downloaded from the charity’s website, and sharing it with the team. A resource to help create a stress risk assessment, which could avoid instances of burnout occurring, can also be downloaded from the same place.
Trevor Bibic, host of the AOP’s May webinar on burnout, says...
Burnout, the WHO goes on to say, is defined by “feelings of energy depletion or exhaustion,” “increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job,” and “reduced professional efficacy.”
Mental Health UK adds feeling helpless, or of being
With the accepted definition unequivocally tying burnout to work and workplace pressures, the AOP will be running a webinar on 16 May, entitled Burnout to balance: recognise, prevent and recover from burnout
Ahead of the webinar, here are three tips from the NHS on managing stress and burnout:
Split up big tasks: this will help break down

In our upcoming workshop, we will focus on three areas: identifying symptoms, preventing, and recovering from burnout.
To identify symptoms, we can pay attention to physical and emotional signs, notice changes in our behaviour, and keep a stress diary in order to help recognise the patterns that may lead to burnout.
To prevent burnout, practice regular self-care (for example, getting enough sleep), set boundaries, prioritise your workload, and build a strong support network.
To recover from burnout, take time off to rest and recharge, seek professional help and identify lifestyle changes to reduce stress.
Burnouttobalance:recognise,preventand recoverfromburnout, will take place on 16 May at 1pm: www.aop.org.uk/events
















20 Individually Wrapped Pre-Moistened Towelettes








From green spaces to flexible working and tackling discrimination, OT explores how optometrists can foster positive workplace environments today






When Dr Peter Frampton was growing up in Brisbane, Australia, he remembers the day an ancient gum tree was cleared to make way for a new school football pitch.


Frampton recalls looking around and thinking his reaction was different to that of his peers.
“All of us boys were standing around watching this tree go down and as it fell, the others cheered,” he said.
“I felt really upset. It offended me to see this magnificent tree, that had been there before colonisation, come down,” Frampton observed.
This formative sense of respect for the environment is now imbued in the practice that Frampton owns in Northumberland.
Aaron Optometrists recycles contact lenses and blister packs, and donates second-hand spectacles to charity. The practice uses repurposed packaging for deliveries, alongside corn starch and paper packaging that can be composted.
When Frampton is not cycling around town, he uses his practice’s electric vehicle, which is charged from solar panels on the roof of his home. He thinks of single-use contact lenses as daily recyclables, rather than daily disposables.
Frampton told OT that sustainability informs all the decisions that he makes as a business owner. A practice mantra that he repeats to staff is: “Unscrupulous profit today means cost tomorrow.”
This principle is true both from a customer loyalty perspective and an environmental standpoint, Frampton emphasised.
“If you don’t think about the upshot of what you are doing, there will be a cost further down the line,” he shared.
Times have changed since Frampton completed his first degree in environmental studies in Brisbane. “Suddenly being an environmentalist has some level of kudos. During the 80s, it wasn’t like that at all – people thought I was just some weird dude,” he said.
Alongside the sustainability initiatives at Aaron Optometrists, Frampton makes an effort to engage with patients on the issue. He organised a practice visit for 18 members of the Ashington (St Andrew’s) Brownie Unit to learn about difficult-to-recycle plastics. Frampton also contributed written answers to questions about sustainability from a nine-yearold patient ahead of her meeting with a local MP.
During COVID-19, when Aaron Optometrists was operating on an appointment-only basis, patients could still tap on the door and hold up their bag of used contact lenses for recycling.





“CONSUMERS ARE DEMONSTRATING AN ENDURING APPETITE FOR SUSTAINABLE PRODUCTS”
Jayne Abel
Frampton highlighted that there are limits to the impact a single practice can have. “While always striving to source ethical product, it is difficult, as a single practice with finite resources and funds to absolutely authenticate the environmental provenance of every product,” he shared.
Now that Aaron Optometrists is part of Hakim Group’s family of independent practices, Frampton is optimistic about the potential to catalyse broader change within the profession.
“With Hakim Group’s commitment and power base we can do a lot more,” he said. “Everyone should try and do what they can. I think that sometimes it is too easy to close your eyes and think that it is too big a problem to contemplate. It is not – we can all help,” Frampton shared.
“Just start; achievable small steps lead to seismic change. Environmental awareness must define your practice ethos,” he emphasised.
In March, the Optical Suppliers Association’s sustainability committee launched its Green Charter, outlining a “practical and achievable roadmap” for optical businesses to reduce their environmental impact.
Founder and chair of the sustainability committee, Jayne Abel, told OT that the Green Charter began with a growing awareness of climate change and a sense of urgency for every industry to take action. “Many businesses are willing but just don’t know where to start,” she said.
Optical suppliers across all sectors can sign up to the charter – from frames and lenses to practice



equipment and health services. Abel observed that there has been an “accelerated interest” in sustainability within the optical supplier industry over the past six months.
“Consumers are demonstrating an enduring appetite for sustainable products in other sectors and there is evidence that wearers seeking out ecofriendly eyewear will become an established and growing market share over the next two years.”
Abel emphasised that it is no longer enough to talk about sustainability.
“We need to act now if we are to become a key player in instigating a positive change,” she said.
Abel, who is the co-founder and chief executive of British eyewear company, Eyespace, shared that she has “road-tested” many of the actions outlined in the charter within the Midlands-based business.
“They have been positive, satisfying and completely compatible with day-to-day operations. It starts with small incremental changes, but they add up and together we can all make a big difference and feel good about how our businesses are treating the planet,” she said.
She added that incorporating sustainability can have a positive impact on the work culture, by helping to attract and retain progressive thinkers within a business.
Abel shared that over the past two decades, the effects of neglecting the environment have begun to be felt in “undeniable ways.”
This has caused her to reflect on what will be passed on to her younger family members and colleagues.
“The effects of climate change are accelerating and will become a part of daily life in ways we can’t yet conceive, but we can substantially lessen their impact during our working lives. We can also evolve the industries we work in to become vehicles to a solution,” Abel highlighted.
Within optometry practices, Abel highlighted simple wins can be made by switching to renewable energy sources, reducing waste and integrating sustainable products through the business.
Practices can choose to review their product portfolio and assess whether they are selecting the most environmentally-conscious suppliers.
Abel added that checking for independent certification, such as ISO standard accreditation, is important to avoid greenwashing. “For example, carbon offset initiatives help repair and restore the planet but are not a solution to unsustainable supply chain processes,” she explained.
Abel shared that suppliers are launching
and refining more sustainable service lines – such as frames and cases made with bio-acetates or recycled materials.
“Ask your suppliers what sustainable products and services they offer; the more they are asked, the more they will grow these parts of their business,” she recommended.
Lastly, Abel highlighted that consumers and businesses need to become comfortable with a minor surcharge on sustainable products – which is negligible when viewed in the context of inflationary pressures.
“It has quickly become the norm for customers to pay for a bag at a supermarket and not think twice about it and this is much the same,” she said.
“Sustainable products and packaging are more competitively priced than ever and will become more so, but only if we increase the volumes we buy,” Abel concluded.
When consultant medical ophthalmologist, Dr Nima Ghadiri, was working as a doctor in Auckland, New Zealand, he became increasingly aware of the impact of green spaces on his wellbeing.
The hospital wards and cafeteria had a view of a large lake where Ghadiri’s colleagues would sometimes go windsurfing after work.
“It affected me in subtle ways that I couldn’t quite quantify then. I gradually realised what I was feeling and noticed the reduction in stress from being able to see nature, water and sky,” he said.
Moving between different hospitals in the UK as he completed his training, Ghadiri chronicled his favourite healing gardens through a photo essay published on The Guardian website (bit.ly/3Zcoys8).
“ACHIEVABLE


Dr Peter Frampton

He told OT that the latest NHS survey found that around half of staff are experiencing work-related stress.
“For nurses, doctors and optometrists, anecdotally we have found that there is reduced burnout when there is a green space. Plants can provide psychological comfort and awaken your senses. They provide a chance to practise mindfulness,” he shared.



The Local Optical Support Committee Unit has published a report examining equality, diversity and inclusion within local optical committees (LOC) The report is based on survey data from 205 LOC members who answered questions on protected characteristics as well as how effectively EDI is currently promoted within committees Most respondents said they did not face barriers in joining a LOC and they felt empowered to contribute to discussions However, one in four respondents did not believe their LOC was representative of the local population. Recommendations made as a result of the report, included removing barriers to joining the LOC, supporting diverse leadership and actively creating a culture of equal opportunities.
The Local Optical Support Committee Unit has published a report examining equality, diversity and inclusion within local optical committees (LOC). The report is based on survey data from 205 LOC members who answered questions on protected characteristics as well as how effectively EDI is currently promoted within committees. Most respondents said they did not face barriers in joining a LOC and they felt empowered to contribute to discussions. However, one in four respondents did not believe their LOC was representative of the local population. Recommendations made as a result of the report, included removing barriers to joining the LOC, supporting diverse leadership and actively creating a culture of equal opportunities.
The full report can be viewed online: bit.ly/3JofuLh
The full report can be viewed online: bit.ly/3Jofulh
A 2018 study, published in the American Journal of Critical Care, found that taking daily work breaks in a hospital garden could help to mitigate the risk of burnout among nurses.
Ghadiri also advocates for the benefits of artwork in clinical spaces. While working as a junior doctor in the east of England, he recalled the impact of seeing illustrations and paintings.
“As I was rushing between wards or clinics, I started appreciating how much my own mood improved and my stress levels went down when I saw some art on the walls,” he said.
Ghadiri acknowledged that optometry practices have greater restrictions on space than a hospital environment. However, he emphasised that ring fencing even a small area can have a significant impact on staff and patients.

“Even single plants can make a lot of difference. They provide a link to nature and integrate the natural world into what might otherwise be a sterile environment,” he said.
Wall art, frame displays or a mini historical exhibition can be used to enhance the atmosphere of a practice, Ghadiri added.
“Art can provide a pleasant distraction from the stress and anxieties of work. It can be something to think about or quickly practise mindfulness with,” he said.
In January, Dr Keith Diaz and colleagues at Columbia University published new research investigating the effect of small
“YOUR BODY WASN’T DESIGNED TO BE IDLE FOR LONG PERIODS OF TIME”
Dr
Keith
Diaz




“exercise snacks” during prolonged periods of sitting. For five days, a group of 11 older and middle-aged adults completed periods of light intensity walking over an eight-hour day where they were otherwise sitting down.
On each day, the group would take a different type of walking break: either every 30 minutes for one minute, every 30 minutes for five minutes, every 60 minutes for one minute or every 60 minutes for five minutes.
On the fifth day, the group spent the eight hours sitting down with no walking breaks.
Speaking to OT from New York while walking, Diaz shared that walking breaks had a significant effect on blood pressure and blood sugar levels.
“I think we expected to find that walking breaks would have some health benefits, and that it would offset some of the harm of sitting. I was surprised by how much of an effect there was,” he said.
Taking a walking break for five minutes every half hour reduced the surge in blood sugar after eating by 60% – the same kind of reduction you would see with a diabetic receiving an insulin injection. This type of walking break also reduced blood pressure by four to five points, an effect that you might see after going for a run, swim or cycle.
The other unexpected result that Diaz observed was the benefit of very low doses of walking. For example, taking a one minute walk every hour still reduced blood pressure by four to five points.

While the most effective dose was a five minute walk every half hour, Diaz acknowledges that this type of break may not be practical for people in many workplaces.
The next study will investigate the effectiveness of 25 different strategies, with the aim of providing tailored solutions that will work for most individuals.



“WE
Jennie Fowler


“If you are someone who is a truck driver, your job will not allow you to take a walking break every half hour. What do we do for those situations?” Diaz shared.
“Our belief is that there is not going to be one solution for everyone – there will be multiple solutions. A person would be able to pick and choose based on their lifestyle and workplace,” he said.
Turning to his advice for employers, Diaz highlighted that there is a growing body of evidence showing that sitting for extended periods is an occupational hazard.
“The simplest thing is to structure your workers’ day so that it allows them to have movement and walking breaks away from their desk,” he said. He emphasised the importance of managers within the workplace leading by example, as they are the ones that set the social norms.
Diaz observed that during previous interventions encouraging employees to incorporate movement into their working day, one of the common barriers was a sense of awkwardness.
“When we ask people why they did not act on a reminder to take a walking break, one of the things that people say is that it would have been uncomfortable or it is not socially acceptable,” he said. “You have to work to build that workplace culture where it is socially acceptable to have a walking meeting or you can stand up in the middle of a conversation,” Diaz added.
Diaz highlighted that people who have sedentary jobs and then complete periods of intensive exercise still need to consider how to incorporate activity into their working day.
“It is not as simple as ticking off a box and saying ‘Oh I exercised today – I’m done.’ The reality that we are learning is that your body wasn’t designed to be idle for long periods of time,” he said.
“What we are realising is that exercise is the tip of the iceberg. Even if you did 30 minutes a day, that is 2% of the day. What you do with the rest of your day, the other 98%, also matters,” he said. There is office furniture that can help employees to become

active – such as treadmill or cycling desks. Simpler interventions may be to take a smaller water bottle to work requiring more frequent refills or to get up from your desk to ask a colleague a question rather than sending an email.
Even though Diaz is an expert in the science behind sedentary behaviour, he also has days where he struggles to incorporate as much activity as he would like to.
Part of this is driven by a culture where sitting is the default position.
“Since the time you are old enough to go into school, our culture has said ‘You are supposed to sit’,” he observed.
“But when we are kids that is not our default position – we like to move and we can’t sit still. We have trained our bodies to think that sitting is the natural state and it can be hard to break free of that,” he said.
Across many professions and industries, there was a shift to flexible working following the COVID-19 pandemic.
Working patterns that were initially introduced to stem the spread of infection have lingered following the easing of restrictions.
Within optometry, there are roles and tasks that are incompatible with home working, while there has traditionally been an expectation to work weekends in many practices.
Hakim Group talent acquisition manager, Jennie Fowler, shared with OT that the pandemic has seen team members assess their priorities.
“We believe the pandemic acted as a great reset for the candidate market, with multiple employee wellness surveys finding that staff value work-life balance above salary,” she said.
Post-pandemic, Fowler has observed an increase in people discussing work patterns that suit their lifestyle at recruitment stage.
“We’ve also seen an increase in people looking for part time opportunities at all stages of their career,” she said.
Ross Campbell, an optometry partner with Specsavers practices in Northallerton and Swaledale, described COVID-19 as a “seismic event” when it came to work-life balance, but his practice has always promoted a balanced approach.
Staff at Specsavers in Northallerton and Swaledale work full-time, part-time, school hours only, term-time only, and variations in between.
“We’ve always engaged optometrists on contracts that work for them,” he said.
Optometrist, James Carolan, works from Wednesday to Saturday at Specsavers Wilmslow.













opticians and optometrists is Muslim (18%). Close to four in 10 (38%) optometry students are Muslim.
The MDA was established in 2004 as a small community organisation. It has since expanded to undertake regional, national and international projects with a focus on health promotion, health policy and promoting equality, diversity and inclusion within the NHS.
As well as doctors, a range of healthcare professionals are included within the MDA membership – including dentists, optometrists, psychologists and pharmacists.
“ANECDOTALLY WE HAVE FOUND THAT THERE IS REDUCED BURNOUT WHEN THERE IS A GREEN SPACE”
Dr Nima Ghadiri
Having a three-day weekend enables the Cheshire optometrist to visit his family in Northern Ireland regularly without taking annual leave. “For me, flexible working is one of the benefits offered by optometry and I've found it generally makes for better career satisfaction,” he said.
Retail manager at Specsavers Wilmslow, Rob Cox, shared that some staff within the practice work Monday to Friday to fit in with other family members’ schedules, while other staff only work at weekends to align with childcare commitments.
In 2021, the Muslim Doctors Association (MDA) published a report exploring the experiences of 150 healthcare professionals.
Excluded on the Front Line: discrimination, racism and Islamophobia in the NHS reported that four in 10 survey respondents had received verbal abuse linked to their religion, while eight in 10 had experienced negative assumptions related to their religion. Four in 10 respondents felt like they needed to compromise in practising their faith at work. Almost half of those surveyed said that they had considered leaving the profession.
“These were really concerning findings – that colleagues felt they had no option but to leave,” chair of the MDA, Dr Hina Shahid, shared with OT. “In the current climate, of workforce crisis and shortages, retaining staff is something that we need to focus on,” Shahid emphasised. Within optometry, around one in five dispensing




Following the pandemic, the MDA wanted to understand what healthcare workers were going through on the frontline.

“We did quite a lot of work to look at how Islamophobia was showing up during the pandemic,” Shahid said.
“We wanted to understand what these chronic daily stresses and experiences of Islamophobia were like,” she elaborated.
Experiences uncovered through the 2021 survey range from workers feeling overlooked or isolated because of their religion, to physical and verbal abuse. “In general, the report showed that Muslim healthcare professionals face prejudice and microaggressions that targeted multiple aspects of their religion and beliefs,” Shahid shared.
Respondents reported hearing derogatory remarks about different aspects of their faith –from prayer breaks and fasting, to saying no to alcohol and pork.
Shahid emphasised that Islamophobia presents on a spectrum within the workplace.
There are more obvious aspects – such as direct discrimination, harassment, bullying and abuse – but there are also more subtle forms of Islamophobia, including stereotypes, prejudices, assumptions and biases.
“A lot of the day-to-day experiences of Islamophobia are under the surface. They are not visible,” Shahid shared.
“Colleagues may say they do not feel included and welcome when they start a new job. A lot of networking may take place in environments where alcohol is served and that can influence career progression,” Shahid said.
She highlighted that experiences of discrimination can make healthcare workers feel like they do not belong. “Time and time again there is the feeling that you have to go over and above to prove yourself, because there





Directaction:directly intervene, for example, by asking the person to stop. Call out negative behaviour, explaining why it is not appropriate.
Direct action: directly intervene, for example, by asking the person to stop. Call out negative behaviour, explaining why it is not appropriate.
Distraction:indirectly intervene, for example, by interrupting to change the focus or subject.
Useful if direct intervention could be harmful to the target or bystander.
Distraction: indirectly intervene, for example, by interrupting to change the focus or subject. Useful if direct intervention could be harmful to the target or bystander.
Delay:wait for the situation to pass and check in with the individual. Take action at a later stage when you have had time to consider what occurred.
Delay: wait for the situation to pass and check in with the individual Take action at a later stage when you have had time to consider what occurred.
Dele~ation:inform a more senior member of staff who has the social power and authority to manage the situation.
Delegation: inform a more senior member of staff who has the social power and authority to manage the situation
Source: Imperial College London
Source: Imperial College London
is an assumption that you are not competent. The burnout and the stress that this causes is a recurrent theme,” Shahid observed.
Shortly after Shahid began wearing a head scarf, she was walking back from a home visit when a patient poured alcohol over her.
She contacted the police about the attack but ended up dropping the case. “You feel like you have a duty of care for patients but then you end up being mistreated – how do you balance those two aspects?” Shahid shared with OT.
The 2021 survey found that three in five respondents had experienced discrimination from patients.
Respondents described patients who would refuse to be seen by a Muslim healthcare professional.
“I THINK YOU CAN ASK QUESTIONS WITH COMPASSIONATE CURIOSITY”
Dr Hina Shahid
Four in 10 respondents felt like they needed to compromise in practising their faith.
Shahid highlighted that there is a mental burden if people have to hide parts of their identity when they come to work.
“We want people to bring their whole self to work – to thrive and flourish in a job that they love. It takes the joy out of working if you have these experiences of discrimination,” she said. Within the 2021 MDA report, a 12-step action








plan (bit.ly/3xDzWkJ) details practical advice for employers in reducing Islamophobia within their workplace.
Recommendations include implementing an Islamophobia zero tolerance policy, reforming recruitment policies and celebrating diversity within the workplace.
“How inclusive is the social culture in the workplace? Can Muslim colleagues take time off for prayer and religious festivals? These are some of the things that employers and organisations can think about,” Shahid shared.
On an individual level, Shahid highlighted the importance of being aware of assumptions that people may have about Muslim staff and challenging those assumptions.
Shahid is happy to answer questions about her faith as long as there is respect and openness on both sides of the conversation.
“I have had colleagues who are genuinely interested in my faith and why I do certain things – why do I wear a headscarf? Why do I fast?” Shahid shared.
“The last thing I would want is for people not to ask out of fear of being politically incorrect. I think you can ask questions with compassionate curiosity,” she emphasised.
Shahid encouraged optometrists who are Muslim who experience discrimination to prioritise their own wellbeing and seek out support – either formal or informal – if needed. “It is important to understand that those experiences, even if they are covert, are real,” she said.





Selected by optometrist, Peter Frampton
“After the local Brownie Unit visited our practice to find out about recycling, they gave each member of staff an honorary Brownie badge. I wear mine with pride on my Sea Shepherd cycling jersey. In return, we gave each Brownie a recycled environmental key ring”



Selected by optometrist, James Carolan
“This lovely pen was a leaving present from a team I worked with until last year. It’s engraved with my name and is a thoughtful memento of my time working with them. Not only that... it’s a great pen I use every day”







Selected by optometrist, Claire Ranger
“This is a picture I have on the wall in my office that I bought when I went travelling in 1993. It is so colourful that it lifts my spirits every time I look at it. It makes me smile when I enter and leave my office and my stresses just melt away”
Selected by optometrist, Patrick Friis
“I work in multiple settings and my phone allows me to keep in contact with the different teams I work in, wherever I am physically sat that day. I know how everyone is doing, who has passed exams, whose birthday it is, when we have had good days or challenging days, and this allows us to support each other which is the biggest factor, for me, in a positive work environment”
















OT asked clinicians to curate the items that enhance their working environment

Selected by ophthalmologist, Dr Nima Ghadiri
“This plant has followed me around for five years and travelled with me to four UK cities. I kept it in my registrar’s office and my fellow’s office making sure it had enough light and humidity to survive. Wherever I take it the shield leaves get bigger and bigger. For me it symbolises resilience, which comes with time and experience”







Selected by Muslim Doctors Association chair, Dr Hina Shahid
“My portable prayer mat is always with me at work. I find it so comforting and rejuvenating to pause my busy day and re-connect with God for a few minutes to fill my cup through my daily prayers”

















C-104462
LEARNING OUTCOMES
Practitioners will be able to elicit relevant details from patients presenting with macular disease Practitioners will be able to identify key features of common macular conditions and manage the patient accordingly.
C-104506
LEARNING OUTCOMES
Practitioners will be able to advise patients on how to modify environmental conditions to benefit the ocular surface Practitioners will understand how environmental conditions can affect the ocular surface.
REMEMBER TO UPLOAD YOUR CPD POINTS TO YOUR MYGOC
C-104688
LEARNING OUTCOMES
Practitioners will understand the importance of communication to avoid and manage complaints effectively Practitioners will understand the role that the OCCS plays in complaint mediation.
C-104353
LEARNING OUTCOME
Practitioners will be able to assess hospital clinic cases and determine management within their scope of practice.
LEARNING OUTCOME
Practitioners will be able to interpret a range of retinal images and understand the likely causes and management options.
QUESTIONS, REFERENCES & DECLARING CPD POINTS
MCQs for OT’s CPD appear online at www.optometry.co.uk/CPD. Exams in this issue will be live from 15 April to 7 July, 2023. When taking an exam, the MCQs may require practitioners to apply knowledge that has not
been covered in the article. Visit www.optometry.co.uk/CPD, and click on ‘Related CPD article’ to view the article and references in full. In the new CPD cycle, registrants are responsible for declaring their CPD
points viatheir MyGOC account. If you pass an exam with OT,you will receive a certificate to use as evidence when declaring your CPD points. Certificates will be available to download in your MyAOP.
Sarah Butterworth BSc (Hons), PGDip,
IN BRIEF This article reviews the anatomy and physiology of the normal macula and examines the presentation and management of four common macular conditions.
The number of UK residents over the age of 75 is predicted to rise from 4.9 million in 2010 to 8.9 million in 2035.1 An inevitable consequence of this is a subsequent rise in the number of patients with ophthalmic disease. It is predicted that there will be a 64% rise in cases of neovascular age-related macular degeneration (nAMD) between 2015 and 2035.2 With an increasing number of practices using optical coherence tomography (OCT) as part of an eye examination, practitioners are now able to identify, and potentially diagnose, conditions at an earlier disease stage as well as make a more accurate assessment of disease severity. When considering macular disease, it is helpful to recall the anatomy and physiology of this region of the retina. The key players in the normal functioning of a healthy macula are the neurosensory retina itself, the retinal pigment epithelium (RPE), Bruch’s membrane and the choriocapillaris. The macula is the 5.5mm central region of the retina. The fovea is a depression of the central 1.5mm of the macula, composed purely of cone photoreceptor cells. Photoreceptor cells convert photons of light into electrical impulses; however, this comes at a cost. To function properly, these cells need constant regeneration of the outer segment and
subsequently have an enormous metabolic demand. In fact, photoreceptor cells have the highest level of oxygen consumption per gram of any cell type in the body.3
The RPE is a single layer of hexagonal cells found between the neurosensory retina and the choroid. RPE cells are known as ‘phagocytic cells’; this means that they ingest waste material and dead or dying cells to support the continuous renewal of the outer segment of photoreceptors.4 The inner side of the RPE is made up of microvilli which interdigitate with the outer segment of photoreceptors, while the basal side of these cells form strong attachments to the underlying choriocapillaris, forming the innermost layer of Bruch’s membrane. The RPE is only weakly attached to the neurosensory retina and the potential space between the two structures is the subretinal space.5 The RPE and the surrounding tight junctional complexes form the blood-retinal barrier. This barrier prevents extracellular fluid leaking into the subretinal space from the choriocapillaris and also works to actively pump ions and water out of the subretinal space.4
Bruch’s membrane separates the RPE from the choriocapillaris. It is used to transport metabolic waste from the retina and is also thought to play an important role in suppressing choroidal neovascularisation.6

The choriocapillaris is the innermost structure of the choroid. Its role is to supply the outer retina with metabolites and remove waste products; this is particularly important at the macula, where there is no inner retina circulation. Subsequently, the density and width of the vessels of the choroid are greatest in the area beneath the macula. Figure 1 shows a schematic of the outer retinal layer, the RPE, Bruch’s membrane, and the choriocapillaris. There are a number of conditions that can cause a change to the structure of the macula, the most common of which is age-
related macular degeneration (AMD). Patients with acute macular disease will often present with sudden unilateral painless loss or change to their vision. This article will consider four common macular conditions that may present in primary care, outlining their presentation and management.
As we age there are a number of ocular changes that occur, which make the eye more susceptible to AMD. There are decreases in choroidal thickness, circulation within the choroid and choriocapillaris density.3 Changes to collagen and proteins in Bruch’s membrane cause it to increase in density, and as a result, it becomes more resistant to the passage of waste materials.7 The RPE has reduced phagocytosis of waste materials and RPE density decreases with age.8 The consequence of these ageing changes is the formation of drusen between the RPE and Bruch’s membrane. The exact composition and mechanics behind the formation of drusen is unclear but it is known that they are deposits of biomaterials under the RPE.8 Although the presence of small drusen (<63μm in diameter) in the absence of pigmentary changes are considered a normal ageing change, they are a risk factor for the development of AMD.9 Drusen are rare prior to the age of 40 years but commonly found in patients over 70 years. Table 1 (see page 69) shows a classification system for AMD.9 Risk factors for the development of AMD include:
• Age (three-fold risk in over 70s)
• Family history of AMD
• Caucasian
• Light irides
• Genetics
• Smoking
• Obesity
• Hypertension
• Poor diet
• Lack of exercise.
Dry AMD is the most common type of the condition accounting for 85 to 90% of cases.10 It presents as a gradual loss of vision, often affecting both eyes, although one eye may be worse than the other. Vision may fluctuate but is often better in bright light. Fundus examination will show visible drusen. OCT can confirm the presence of drusen, increased hyper-reflectivity, and in advanced cases, reverse shadowing caused by RPE atrophy and photoreceptor cell death. Unfortunately, there is currently no treatment for dry AMD, but patients should be counselled on appropriate advice for reducing their risk of the progression of AMD, and if appropriate, a referral to low vision services or signposting to an eye clinic liaison officer (ECLO) may be helpful. nAMD, otherwise known as wet AMD, occurs as a

result of choroidal neovascularisation (CNV). Vascular endothelial growth factor (VEGF) is one substance among many enzymes and growth factors that promotes the formation of new blood vessels within the macula. VEGF is upregulated in response to ischaemia, hypoxia, inflammation and trauma.11 With regards to nAMD, it is thought that the accumulation of oxidised lipids in Bruch’s membrane and ischaemia caused by the atrophy of the choriocapillaris, drive the upregulation of VEGF leading to the formation of CNV.11 These new vessels penetrate through Bruch’s membrane and proliferate between Bruch’s membrane and the RPE or in the subretinal space. They are fragile and can leak proteins and lipids or haemorrhage.
Patients with nAMD will typically present with a sudden onset of reduced vision in the affected eye. They may be aware of metamorphopsia or a scotoma but might only offer this information when asked directly. A fundus examination will often show a visible subretinal or intraretinal haemorrhage (see Figure 2) and/or exudates. However, it is worth being aware that a CNV complex may exist and the patient could have symptoms without an obvious haemorrhage.



Figure 4 Fundus photo and OCT showing retinal vein occlusion. ImagecourtesyofGloucestershireRetinal EducationGroup
If assessing a patient presenting with a marked reduction in visual acuity and it is difficult to get an adequate view of the macula, then it is worth dilating them. With a dilated, stereoscopic view, CNV may be visible as a grey-green submacular lesion. OCT is an invaluable tool for assessing patients with macular disease. The presence of subretinal fluid (SRF), intraretinal fluid (IRF) or a pigment epithelial detachment (PED) in the presence of acute symptoms is often enough to form a likely diagnosis of nAMD.
Although nAMD usually presents as an acute loss of vision, it is surprising how many patients can be unaware of unilateral vision loss that is only detected during a vision check at the start of a routine sight test. A marked drop in vision should always be treated with suspicion and a dilated fundus examination is recommended.
Patients presenting with nAMD require urgent referral to secondary care. Most regions have a rapid access referral pathway in place, so practitioners should be familiar with arrangements in their local area. Patients are typically treated with anti-VEGF intravitreal injections. Traditionally this was with Lucentis (ranibizumab) or Eylea (aflibercept); however,
in 2020 the UK Court of Appeal ruled that Avastin (bevacizumab) could be used off label to treat nAMD and in circumstances where patients would not otherwise meet the treatment criteria (if vision is better than 6/12 or worse than 6/96).12 The National Institute for Health and Care Excellence (NICE) guideline 82 (NG82) provides a comprehensive overview of the treatment of nAMD.13 Vabysmo (faricimab) is another anti-VEGF injection that was approved by NICE for the treatment of nAMD in June 2022. In addition to targeting anti-VEGF, it also targets the angiopoietin-2 pathway.14
It is worth discussing modifiable risk factors with patients, including smoking cessation and the benefits of a healthy diet and lifestyle. The Royal College of Ophthalmologists advise a healthy diet rich in fresh fruit, vegetables, eggs and oily fish.15 Dietary supplements following the age-related eye disease study (AREDS) 2 formulation may reduce the five-year risk of developing late AMD by up to 25%; however, NICE guidelines acknowledge the limitations of the AREDS 2 study design, and highlight that further research is required to assess the effect of AREDS 2 on disease progression.15
It is also important to explain self-monitoring to those with AMD. Practitioners should advise patients with AMD to report any new symptoms or changes of a blurred or grey patch in their vision, distortion, or objects appearing a different size to normal. Providing patients with an Amsler chart is a cheap, simple and effective way to allow them to monitor their vision.
Adult vitelliform dystrophy is a type of pattern dystrophy, a genetic disease, that may be discovered by chance during a routine sight test. The patient may present with a gradual reduction in their central vision or can be asymptomatic. It typically occurs in patients over 40 years of age. Clinical signs include a symmetrical, round, yellow deposit visible on ophthalmoscopic examination in one or both eyes. The appearance is similar to Best disease, but the lesion is typically smaller and presents later in life. An OCT examination may show subretinal material and atrophy in the area of the lesion (see Figure 3).
There is currently no treatment for adult vitelliform dystrophy. Although its appearance on an OCT can look alarming, adult vitelliform lesions without CNV do not necessarily require referral to secondary care. NG82 classifies a vitelliform lesion without significant visual loss (best corrected visual acuity better than 6/18) as early AMD at high risk of progression and it should be managed as such.15 If the visual acuity is 6/18 or worse, NG82 classifies the condition as late AMD (dry). Visual acuity is often preserved or only mildly affected despite the presence of vitelliform material in the subretinal space.16 However, as there is
“PATIENTS PRESENTING WITH A SUDDEN, UNILATERAL, PAINLESS LOSS OF VISION WILL OFTEN HAVE MACULAR DISEASE. A CAREFUL HISTORY INCLUDING THE DESCRIPTION, ONSET AND DURATION OF VISUAL SYMPTOMS WILL AID IN MAKING A DIFFERENTIAL DIAGNOSIS”
an increased risk that the patient will develop CNV in their lifetime, these patients should be monitored in primary care on an annual basis and given an Amsler chart to monitor for any change to vision or onset of distortion. If the patient does go on to develop CNV they should be referred to secondary care for the commencement of anti-VEGF treatment.
Central serous chorioretinopathy (CSCR) is a condition predominantly affecting men of working age and is characterised by a localised serous detachment of the sensory retina and the presence of subretinal fluid. It can be acute – typically resolving within three to six months – or chronic. The pathophysiology of this condition is poorly understood. It is thought that in CSCR, hyperpermeability of the choroid causes ischaemia and increased hydrostatic pressure. This in turn leads to damage of the RPE and the breakdown of the normal function of the blood-retinal barrier, leading to the accumulation of fluid in the sub-retinal space.17
Patients with CSCR may present with unilateral blurred vision, a reduction in contrast sensitivity and colour vision, metamorphopsia and a hyperopic refractive shift. Often, they will complain of an awareness of a scotoma and may compare it to a feeling of having looked at a light for too long. Vision
Category
No apparent ageing changes
Normal ageing changes
Early AMD
Intermediate AMD
Late AMD
may only be slightly reduced in spite of the presence of SRF, with studies finding an average best corrected logMAR visual acuity of approximately 0.20 (Snellen 6/10).18,19 Dilated fundus examination may show a round elevated clear lesion; however, often there may be no visible sign of CSCR on a fundus image. OCT will show an elevated dome where the sensory retina has detached from the RPE. Risk factors for the development of the condition include:
• Male
• Between fourth and sixth decades of life
• ‘Type A’ personality and/or psychological stress –possibly causing elevated corticosteroids
• Pregnancy
• Sleep apnoea
• Systemic corticosteroids
• Exogenous testosterone exposure.
There is a known relationship between the use of glucocorticoid steroids (for example, prednisolone, betamethasone, dexamethasone) and the presence of CSCR. Cortisol, a naturally occurring steroid hormone, can be elevated in response to high stress and during pregnancy. It is thought that the elevated level of cortisol may be the trigger for the development of CSCR in pregnancy.20 A detailed history is essential. It can be helpful to ask specifically about steroid
Definition (lesions within two disc diameters of the fovea)
No drusen
No AMD pigmentary abnormalities
Small drusen (<63μm)
No AMD pigmentary abnormalities
Medium drusen (>63um but <125μm)
No AMD pigmentary abnormalities
Large drusen (>125μm)
Any AMD pigmentary abnormalities
Neovascular AMD and/or geographic atrophy
Ischaemic
Visual acuity (VA) worse than 6/60
Relative afferent pupillary defect (RAPD)
Multiple dark deep intraretinal haemorrhages
Multiple cotton wool spots
Macular oedema
Severe venous tortuosity
Marked optic disc swelling
New vessels elsewhere
New vessels at disc
New vessels at iris (usually after two to four months)
inhalers, nasal sprays or topical creams as many patients might not think of these as medicine and may forget to mention them when asked about medication. Consider the patient’s overall demeanour and their occupation. Enquiring about their general stress levels can often lead to patients reporting that they have had an abnormal amount of recent stress and/or anxiety.
In the vast majority of cases, CSCR is self-limiting and will resolve without treatment within four months. In a small percentage of cases, SRF and serous retinal detachment persists. CSCR is chronic if it has not resolved after four to six months. Chronic CSCR may be treated with photodynamic therapy (PDT).
The College of Optometrists’ guidelines recommend referring central serous retinopathy urgently;21 however, some regions may have local schemes in place. For example, Suffolk LOC recommend urgent referral if the optometrist is unsure about the diagnosis, particularly if they do not have access to an OCT, or cannot rule out other causes, for example nAMD. However, if the optometrist is confident in their diagnosis, Suffolk LOC recommend routine referral alongside advice to the patient should their condition fail to improve, or worsen, and the patient should be given an Amsler chart for self-monitoring.22 Practitioners can check if there are guidelines within their local area. Differential diagnosis of CSCR includes: CNV, AMD, polypoidal choroidal vasculopathy, hypertensive choroidopathy and optic pit maculopathy.
Retinal vein occlusion (RVO) is the second most common retinal vascular disease after diabetic retinopathy23 and occurs as a result of obstruction of
Non-ischaemic
VA 6/30-6/60
No RAPD or mild RAPD
Mild to moderate dot, blot and flame haemorrhages
Mild cotton wool spots
Mild venous dilation and tortuosity
Mild macular oedema
the venous system due to thrombus formation. The thrombus formation associated with the development of a retinal vein occlusion is often as a result of atherosclerosis (where arteries develop plaque). The most common associations of RVO can, therefore, be defined as risk factors for atherosclerosis.24 Other systemic considerations include conditions that cause hyperviscosity or affect blood flow through retinal veins. Risk factors for RVO include:25
• Age
• Hypertension
• Hyperlipidaemia
• Hyperviscosity syndromes
• Blood dyscrasias
• Inflammatory vasculitis, for example, systemic lupus erythematosus
• Open-angle glaucoma
• Ischaemic optic neuropathy
• Optic nerve head changes including disc drusen and tilted optic nerve heads
• Some medications including oral contraceptives and diuretics.
RVO is classified according to where the occlusion occurred. In a central retinal vein occlusion (CRVO), the occlusion typically occurs posterior to the lamina cribrosa. In a hemiretinal vein occlusion, the occlusion occurs in a hemicentral vein affecting the entire superior or inferior retinal hemisphere. In a branch retinal vein occlusion (BRVO), the occlusion typically occurs at an artero-venous crossing.
Retinal vein occlusions have a distinctive appearance (see Figure 4). In a central retinal vein occlusion there will be extensive, widespread dot, blot and flame haemorrhages in all four quadrants of the retina (‘blood
and thunder appearance’), there will also be cotton wool spots, dilation and tortuosity of retinal vessels, along with possible disc and macular oedema. Patients may go on to form collateral vessels at the disc. In a hemiretinal vein occlusion, this will affect either the superior or inferior retina, respecting the horizontal demarcation. In a BRVO, signs will occur in the affected venous segment, often in a wedgeshaped pattern.
The most common cause of visual loss as a result of a vein occlusion is macular oedema.25 When an occlusion occurs, increased vascular pressure can cause failure of the capillary endothelium blood-retinal barrier, causing fluid and small molecules to leak across the vascular wall resulting in oedema. This oedema can then lead to the presence of inflammatory mediators including VEGF. Macular oedema can occur in ischaemic and non-ischaemic CRVO (see Table 2). In ischaemic RVO, increased venous pressure causes decreased capillary perfusion, meaning the retina does not receive enough oxygen; the retina becomes hypoxic and permanent cell damage or death can occur.26 Ischaemia can lead to neovascularisation at the retina or iris (rubeosis iridis), increasing the risk of neovascular glaucoma, tractional retinal detachment or vitreous haemorrhage. In an ischaemic vein occlusion, cotton wool spots will be more prominent, and haemorrhages may appear deeper and more extensive. Fundus fluorescein angiography (FFA) will show capillary non-perfusion. The prognosis for an ischaemic retinal vein occlusion is generally poor.
The College of Optometrists’ guidelines recommend that retinal vein occlusions should be referred urgently to ophthalmology (to be seen within at least two to four weeks) andthey should be referred urgently to their GP for medical management and investigation for underlying systemic conditions, specifically for cardiovascular risk factors.27 In secondary care, patients may be treated with anti-VEGF or an intravitreal steroid such as Ozurdex (dexamethasone) therapy to treat macular oedema and/or neovascularisation. Patients with neovascularisation of the retina, disc or iris may also require pan-retinal photocoagulation (PRP) laser treatment.
When confronted with an unfamiliar macular condition, it can be difficult to know whether to refer it and how urgently it needs to be seen. Practitioners should check their local pathways to see what guidance is in place. The College of Optometrists’ clinical management guidelines are useful tools when making decisions. If in doubt, refer, particularly if fluid is present at the macula.
In the referral letter it is helpful to describe what the patient’s visual symptoms are, or whether they are asymptomatic and the duration of the symptoms, particularly whether it is an acute onset. Include a description of what can be seen on the fundus image or OCT; this is often more helpful than a tentative diagnosis and helps to triage the patient. Ideally, an image of the OCT and fundus photo should be provided alongside the letter. Including previous visual acuities in the referral letter is also useful where available. It is also helpful to advise the patient that they will likely have dilating drops at their hospital appointment and should not drive to it.
Patients presenting with a sudden, unilateral, painless loss of vision will often have macular disease. A careful history including the description, onset and duration of visual symptoms will aid in making a differential diagnosis. Remember to consider the patient’s age, medical and family history, and the presence of risk factors. Although OCT is a valuable tool, its absence should not be a barrier to assessment; an Amsler chart and a dilated fundus examination can provide the information needed to guide appropriate management. Any sudden loss of vision, distortion or scotoma should be regarded with a high degree of suspicion even in the absence of an obvious haemorrhage and should warrant further investigation.
There are a number of materials available for practitioners looking to further their knowledge, but in particular, NG82, the Royal College of Ophthalmologists’ guidance, and the College of Optometrists’ clinical management guidelines are all free, easily accessible, valuable resources.
0

Sarah Butterworth is a specialist optometrist working at Gloucester and Cheltenham hospitals, predominantly in medical retina clinics. She also supervises third year optometry students in their primary care clinics at the University West of England (UWE) and has recently completed her postgraduate diploma in clinical optometry at Cardiff University.
Dr Katrina Schmid BAppScOptom (Hons), PhD, Grad Cert Higher Ed, Grad Cert Ocular Therapeutics, SFHEA, AFHEA (Indigenous)
IN BRIEF This in-depth article considers the outdoor and indoor environment, including air quality and climatic factors, and how this affects the tear film and ocular surface health.
Poor outdoor and indoor environmental quality, including both air quality and climatic factors, can detrimentally affect the tear film leading to symptoms of ocular irritation. These effects can be acute or chronic depending on the duration and extent of the adverse environmental conditions. Air pollutants include those from natural (for example, wildfire smoke) and man-made sources (such as building materials, consumer products, and cooking) that emit strong sensory irritants, corrosive chemicals, and combustion-related pollutants (for instance, particulate matter and nitrogen dioxide). The quality of the outdoor environment can alter people’s daily habits, where often poor conditions lead people to spend greater time indoors; this increases the importance of indoor air quality (IAQ) and the indoor climatic conditions. Knowledge in this area is important for eye care practitioners (ECPs) so they can understand the impact of environmental quality on ocular surface health, both for their own wellbeing and that of their patients. The goal is to protect the ocular surface from the adverse effects of air pollutants combined with the negative influence of thermal factors, such as dry air and high temperatures.
Outdoor air quality
People who live in countries with poor outdoor air quality (OAQ) are acutely
aware of the detrimental health effects of polluted air1 and the ocular irritation this can produce.2 In Australia, reports show that measured particulate matter (PM) and ozone levels in Sydney can at times exceed the health standards.3 In the UK, the levels of roadside PM have reduced over the past 10 years as fuel efficiency has improved and emissions have reduced.4 In urban areas, residential combustion of wood in stoves and open fires contributes to elevated pollution levels during winter months.4 Poor OAQ affects the liveability of cities and people’s ability to enjoy the outdoor environment. The air quality index (AQI) provides information on daily air quality in cities around the world. The AQI is the average concentration of pollutants, but those included may vary (for example, carbon monoxide, lead, nitrogen dioxide (NO2), ozone, particulate matter, and sulfur dioxide (SO2)).

ENVIRONMENTAL FACTORS


Particles, eg from combustion
Reactive air pollutants
Low humidity
High temperature
Draft (airflow)
HUMAN FACTORS


Gland function
Table 1 Recommended actions and UK health advice based on outdoor air pollution band (DAQI).6 *Adults and children with heart or lung problems are at greater risk of symptoms. It is possible that very sensitive individuals may experience health effects even on low air pollution days
Air pollution band Value
Low 1–3
Moderate 4–6
High 7–9
Accompanying health messages for at-risk individuals*
Enjoy your usual outdoor activities
Adults and children with lung problems, and adults with heart problems, who experience symptoms, should consider reducing strenuous physical activity, particularly outdoors
Adults and children with lung problems, and adults with heart problems, should reduce strenuous physical exertion, particularly outdoors, and particularly if they experience symptoms. People with asthma may find they need to use their reliever inhaler more often. Older people should also reduce physical exertion
Accompanying health messages for the general population
Enjoy your usual outdoor activities
Enjoy your usual outdoor activities
Anyone experiencing discomfort such as sore eyes, cough or sore throat should consider reducing activity, particularly outdoors
Very high 10
Adults and children with lung problems, adults with heart problems, and older people, should avoid strenuous physical activity. People with asthma may find they need to use their reliever inhaler more often
It can be calculated in several ways. One method is to take the average of readings from air quality sensors of each pollutant over a stated time frame, the values are divided by the national quality standard, and multiplied by 100, with the highest value used as the AQI. The mathematical function used to convert from air pollutant concentration to AQI varies by pollutant.
The AQI is provided in real time, can be searched by location, and people can use this information to make judgements about the OAQ, and if they should alter their behaviour (for instance, not go outside). The lower the AQI, the better the air quality; a value of less than 50 is considered good, greater than 100 poor and greater than 150 hazardous to health. Countries with a very high AQI, and thus very poor air quality are numerous, and include Bangladesh, Chad, Pakistan, Tajikistan, and India.5 There are multiple websites that provide AQI information. Air quality data in the UK, including the AQI and PM level are available.5 AQI in the UK is
Reduce physical exertion, particularly outdoors, especially if you experience symptoms such as cough or sore throat
considered good, although the reported 2021 average PM concentration was 1.8 times the World Health Organization (WHO) annual air quality guidelines value. The UK Department for Environment Food & Rural Affairs UK-AIR converts the AQI to a daily score for use in public health messaging.6 The daily AQI (DAQI) is numbered one to 10 and divided into four bands, low (1–3) to very high (10), to provide simple information about air pollution levels (see Table 1). OAQ can be poor in countries relatively close to the UK such as Bosnia, Bulgaria, Italy, Poland, Serbia and Turkey.7 Depending on weather conditions, including the direction of the prevailing winds, the quality of UK air can be detrimentally affected from sources originating outside the UK. It is also known that during bushfire events, the AQI will be greatly increased.8 Extra care should be taken at this time. The UK is not immune to the effects of wildfires and the health hazard they create.9 For example, in August 2022,
Table 2 How people’s habits can affect indoor (IAQ) and outdoor air quality (OAQ) and potentially the ocular surface.* Selected examples have been provided, note that this is not an exhaustive list.
Changed activity Effect on air quality
Less outdoor time
Less commuting, less vehicle (air and ground) travel
Increased exposure to indoor air of variable quality
Increased exposure to dry indoor air
Home schooling or work from home
Increased use of alcoholbased cleaners
Corrosive cleaning product aerosols
Quaternary ammonium chlorides
Chlorine from bleach
Recommendation to improve indoor ventilation
Avoid dry air conditions
Avoid high room temperature
Avoid draft
Recommendation to use air filters
Mask wear
Dependent on current quality of outdoor air
Reduced emissions, decrease pollution
Greater exposure to environmental tobacco smoke
Greater exposure to dry air if heating (in cold climates) or air conditioning (in hot climate) systems required
Increased screen time, decreased blinking, exacerbation of detrimental effects of poor air quality, drafts
Likely none for cleaners used in the home. Issue with direct eye contact
Use of spray cleaners elevates exposure Uncertain effect of other cleaners
Reduced indoor contaminants
Improved air flow
Reduced indoor contaminants
Localised change to air flow around the eye
Contact lens wear May exacerbate effect of detrimental air quality factors on ocular surface
Suggested to avoid spectacle fogging due to mask wear
Health and ocular surface effects Literature*
Poorer mental health
Exacerbation of myopia in children
Reduced sunlight exposure and vitamin D
Reduced pollution related deaths and improved life expectancy
Reduced asthma exacerbations
Reduced ocular surface irritation and immune response
Exacerbation of asthma, airway irritation, dry throat, dry skin, dry eye
Links to refractive error
Exacerbation of asthma, airway irritation, dry throat, dry skin, dry eye
Digital eye strain, exacerbation of dry eye
No evidence that standard indoor cleaners are detrimental to human health.
Uncertain as to whether harmful aerosols are produced.
Poor evidence regarding whether ocular surface is affected, and if so, likely only with protracted use and/ or direct contact
Improved general well-being and health
Improved ocular surface
Improved general well-being and health
Improved ocular surface
Exacerbates dry eye, particularly when poorly fitting
Interacts with mask wear to decrease contact lens comfort
Huang et al, 202128
Wang et al, 202129
Larson et al, 202230
Novaes et al, 201031
Venter et al, 202027
Mandell et al, 202015
Domínguez-Amarillo et al, 202026
Wolkoff, Azuma, Carrer, 202132
Wolkoff, 201820
Wolkoff, Azuma, Carrer, 202132
Nielsen et al, 200833
Sheppard and Wolffsohn, 201819
Clausen et al, 202034
Shetty et al, 202035
Zhang et al, 202036
Domínguez-Amarillo et al, 202026
Hadrup et al, 202237
Megahed and Ghoneim, 202138
Wolkoff, Azuma, Carrer, 202132
Engineer et al, 202139
Megahed and Ghoneim, 202138
Moshirfar etal, 202040
Krolo etal, 202141
Mastropasqua etal, 202142
Martinez-Perez et al, 202143
the AQI in Greenock, Scotland was greater than 150 due to summer fires. Thus, the key is to reduce the likelihood of fires, and if they occur, ensure that the poor OAQ does not subsequently lead to poor indoor air quality (IAQ).
Indoor air quality
IAQ is the air quality within and around buildings and structures, that is to say, within the internal environment.10 As this varies locally, and must be individually monitored within each building, IAQ values are not reported. New air pollution sensing methods are being developed to measure IAQ,11 which could provide useful information in real-time.
As people spend most of their lives indoors (up to 90% of all time), the quality of the indoor environment has the potential to have a very large effect on human health. Poor IAQ has been linked to sick building syndrome, reduced productivity and impaired learning in schools.12 Along with the incursion of outside air pollutants, contaminants are also produced within the indoor environment. These can include emissions from building products and furnishings, and from activities like heating, cooling and cooking. Common indoor pollutants include second-hand tobacco smoke, air pollutants from indoor combustion, PM, moulds and other allergens, volatile organic compounds, carbon monoxide and carbon dioxide, and ozone.
Climate changes can translate into altered indoor environments; this is related to heat exposure, flooding, and chemical and biological contamination in buildings.13 It has been suggested that increased health burdens related to more extreme heat and cold, indoor exposure to air pollution derived from outdoor sources, and mould growth, will occur and that mechanical ventilation with heat recovery and air filtration will be required.13 Source control, filtration and the use of ventilation to dilute contaminants are the primary methods for improving indoor air quality in most buildings.
The potential adverse effects of air pollution on the eye have received much attention.14,2 Both poor OAQ and IAQ, can impact the ocular surface health, particularly if it is already compromised, leading to further exacerbation of ocular symptoms. Various degrees of inherent gland disease will contribute to the overall disturbance,15 and this may be worsened by a broad list of medications known to alter the tear film and cause dry eye.16 The tear film, which protects the ocular surface, is exposed directly to the air and hence affected by air quality.17,18 For instance, the tear film can be impacted by processes that increase tear evaporation and decrease its stability (for example, low humidity, high temperature, air current, that is to say, drafts). Inadequate ventilation can exacerbate the effects of dry air and high temperature, producing even drier air and further deterioration of the
ocular surface. Tear film stability is further destabilised by a reduced blink frequency or increased portion of incomplete blinks during extended screen-based work involving digital devices or inadequate lighting conditions.19 For instance, during visually demanding work where the tear film is compromised, it becomes more vulnerable to external stimuli. People with unrecognised or mild to moderate dry eye disease may further experience exacerbation of dry eye symptoms during and after visually demanding screen-based work in an environment with poor IAQ and aggravated microclimatic conditions.20 Thus, the ocular surface becomes more vulnerable to the inadequate IAQ in the home environment, and even more so after extended screen-work.
Aggressive chemicals in combustion particles (environmental tobacco smoke, wildfire smoke, traffic emissions) are harmful to the ocular surface. For example, ambient levels of vehicle induced air pollution have been shown to alter conjunctival goblet cell density and increase MUC5AC mRNA levels; 21 these may be adaptive responses to long-term exposure to pollution. The exposure to high levels of PM may also increase the risk of meibomian gland dysfunction (MGD) and blepharitis. 22
Elevated concentrations of certain oxidative agents, mostly strong sensory irritants like formaldehyde or acrolein, can cause chemesthesis and sensory irritation. Pollution-induced irritation in the trigeminal distribution can cause sensory irritation to the eye, nose and throat. 23 Furthermore, chemicals in certain surfactants present in cleaning or disinfection products are potentially harmful.
A key question from the perspective of managing the IAQ in residential environments, is how indoor air pollution, the microclimatic parameters (temperature, indoor air humidity, ventilation, and draft), and the workstation conditions (such as screen-based digital device work and position) may deteriorate the ocular surface health (that is to say, tear film stability). Figure 1 shows a pictorial representation of how environmental factors which affect air quality interact with human factors that affect ocular surface health, thus further exacerbating the reduction in tear film quality.
Ocular surface diseases, in particular dry eye, are very common, often chronic, can be severe, cause ocular irritation and pain, and can reduce visual and work performance.17 The lockdown events as a result of COVID-19, and subsequent lifestyle changes,24 have exacerbated ocular surface issues and led to the proposed term ‘quarantine dry eye’.25 Domínguez-Amarillo etal describe a vicious cycle whereby increased time spent in the home deteriorates IAQ due to increased pollutant emission from activities (for example, cooking), increased cleaning, and steps undertaken to improve the home’s comfort (for instance, increased heating, reduced ventilation).26
People’s daily activities and behaviours can thus alter the environmental conditions they are exposed to. For example, when groups of people in cities commute less, there is a reduction in outdoor air pollution due to reduced vehicle emissions.27 At an individual level, the amount a person commutes to work, how much time is spent indoors, what tasks are carried out and whether air filters are used in the home will all vary environmental quality and duration of exposure to adverse conditions. Table 2 provides a summary of how alterations to a person’s activities can potentially affect air quality, general health and the ocular surface. Some of these might have positive ocular effects, while others can exacerbate dry eye and other ocular surface problems.
Many studies have confirmed the important influence of traffic-related pollutants, for example, PM, NO2 (proxy of traffic and combustion), and SO2, on the development and exacerbation of dry eye disease and symptoms.15 Environmental exposure during commuting to and from the workplace might influence the ocular surface stability. It has been speculated that the reduction in dry-eyesymptom-scores measured during periods of lockdown could be due to reduced exposure to outdoor air pollution from not commuting to work.44
A positive outcome has been the many reports of reduced air pollution during periods of lockdown, with improvements in OAQ in many parts of the world.27 Analysis has shown that after accounting for meteorological variations, lockdown events reduced the population-weighted concentration of NO2 and PM levels by approximately 60% and 30%, respectively.27 Decreases in global transport emissions are largely responsible for the NO2 reductions. Improvements in OAQ during periods of lockdown have been reported both in Australia and the UK.45,46 The reported reductions in pollution levels in Australia were smaller than elsewhere and not always at significant levels.45 In the UK there was a large reduction in traffic, and this translated to a reduction in both NO2 and PM levels at urban traffic monitoring sites.46
A lifestyle of less time outdoors and more indoor time increases the risk from indoor environmental pollutant exposure.47 The assessment of IAQ factors impacting the ocular surface is the same whether the indoor environment is a home or office. These IAQ factors include thermal factors (temperature and indoor air humidity), a host of various kinds of pollutants, both volatile inorganic (NO2 and ozone), and volatile organic compounds (VOCs), and PM. While there are WHO global air quality guidelines48 and IAQ guidelines,49 most countries do not have IAQ standards.
The impact of indoor air pollutants, including VOCs and particles, has been reviewed.12,15,17 To summarise, only situations with high concentrations of strong sensory
eye and airway irritants like formaldehyde and acrolein may result in acute sensory irritation by trigeminal nerve stimulation. These exposures are activity-dependent, for example, cleaning-related activities with fragrance-based consumer products in ozone enriched environments. However, the risk is low, and fortunately, VOCs have thresholds for sensory irritation orders of magnitude higher than those typically measured indoors in both office and home environments. Construction products, electronic devices and other polymer-based products found in the home can result in elevated concentrations of endocrine disrupting compounds (semi-VOCs), both in the indoor air and in dust particles, of which some may be associated with an elevated risk in dry eye.50
Indoor temperature and humidity
Other factors important for a stable ocular surface are the room temperature and the indoor air humidity. Elevated temperature and low indoor air humidity increase water evaporation, which can result in desiccation of the ocular surface. Furthermore, both high room temperature and/or low indoor air humidity compromise work performance.32 The lacrimal secretion is retarded during reduced stimulation of cold receptors by elevated ocular surface temperature and this will further alter the composition and basal flow of the tear film.51 Conditions of draft, that is to say, air flow across the ocular surface, may also increase the complaint rate of dry eye symptoms, possibly by elevated water evaporation from the ocular surface and consequently a sensation of cooling.
Exposure to environmental tobacco smoke
Indoor PM2 5 is the most reliable marker for the presence of tobacco smoke; the level of PM2.5 can be 10 times higher in houses of smokers versus those of non-smokers. Recent studies have demonstrated that PM2.5 levels are closely correlated with chronic lung diseases,52 highlighting the damage that can be caused by prolonged exposure to poor IAQ. Tobacco smoking can cause symptoms of itchiness and irritation, along with conjunctival redness. Changes to the ocular surface associated with smoking include a reduction in tear film break-up time, changes in the tear film lipid layer, reduction in tear secretion, corneal and conjunctival sensitivity, and tear lysozyme concentration.53 Exposure to secondary environmental tobacco smoke is associated with similar effects.54
Increased working and studying from home
Since an already compromised ocular surface may be more vulnerable to further insult from external stimuli, an important question is how occupational (office) working conditions, work habits and lifestyle may differ from conditions when working from home. It is important to consider that the potential ocular surface impact of IAQ can be exacerbated by many work-related factors, for example, duration of screen/reading work and other visually demanding tasks. Studies have found
associations between the extended screen/reading hours after the lockdown and elevated prevalence of dry/irritated eye symptoms.24,55 Similarly, for students, online lectures have been associated with worsening of dry eye symptoms.56,57 It is well known that blinking frequency decreases during use of digital devices and this will further exacerbate the ocular surface dryness experienced in dry air.
Infection control measures, including wearing face masks, physical distancing, regular cleaning of surfaces, hand hygiene (including alcohol-based sanitisers), and increased ventilation have been recommended.
Indoor ventilation
One possible major difference between the office (occupational) and home environments is the conditions of ventilation and the use of combustion-related activities at home like cooking and the use of (kerosene) heaters, fireplaces and infiltration of vehicle emissions from near-by traffic. The home activities might result in elevated PM concentrations relative to offices.27 Combustion particles are associated with an elevated acute risk of dry eye symptoms.17 Thus, adequate ventilation is essential to control the room temperature and the indoor air humidity within recommended limits of comfort and safety.32 However, ventilation may also impact the IAQ negatively during the cold dry air winter season because the incoming dry air becomes even drier in the heated indoor environment, thus, further exacerbating the desiccation of the ocular surface. Natural ventilation at the levels required to improve IAQ may be unachievable as the outdoor air is too hot, too cold or too polluted.
Cleaning of surfaces and hands
Indoor dust and moulds are potentially harmful to humans, can degrade furnishings and equipment, and need to be removed from surfaces. Dust can contain pollen, mould spores, fungus, bacteria, viruses, dust mites and dead skin cells. Other PM that may be present include degraded plastics, concrete dust, pesticides and fuel residues. Vacuuming and wiping surfaces with a damp cloth is the best way to remove dust PM. Infection control procedures also require the use of surface cleaners. There are reports that the intensity and frequency of the use of household cleaners has increased and newer cleaners containing hypochlorite and biocides utilised.26 Anecdotal reports state that ECPs alcohol wipe frequently touched items (PIN pads, keyboards, pens) and spray counters, chairs and doorhandles with surface cleaners proven effective against COVID-19 (for example, containing hydrogen peroxide, benzalkonium chloride (BAK)). These cleaners are stated to be safe with no harmful fumes, though safety instructions include use of gloves and eye protection. There is some indication of BAK in cleaning products inducing asthma,37 and of course, BAK is well known as an ocular surface irritant when used as a preservative in eye drops. 58 In terms of the ocular surface, the greatest risk is with direct contact, although there is little information on effects of aerosols on the ocular surface. For example, there are reported cases of ocular surface irritation caused using alcohol-based spray hand sanitisers, and as such, it is recommended to spray below eye level.35 Although it is well known that if alcohol comes in direct contact with the cornea, it will debride the epithelium, there is no current evidence of an ocular surface effect when in aerosol form.
Clausen etalreport that the evidence for respiratory effects after inhalation of quaternary ammonium compounds (QACs) found in cleaning spray products is
Table 3 Suggested advice relevant to air quality and the ocular surface, including actions relevant to the environment and activities
Environmental factors
Contribute to global sustainability and reduced emissions
Lobby for clean air and reduced pollution.
Increase outdoor time if OAQ is of good quality
Take steps to improve IAQ
Ensure adequate indoor air ventilation
Use air filters if IAQ is poor
If IAQ is too dry, humidify the air
Human factors
Take steps to avoid digital eye strain by taking micro-breaks when performing extended cognitive visual activities
Carefully consider which cleaning products are best, avoid using spray cleaners at eye level
If required, wear a correctly fitting face mask
Use ocular lubricants or contact lens rewetting agents as needed
Treat meibomian gland disease
Be aware that many medications can detrimentally affect the tear film quality
ambiguous.34 They also report that solvents including glycols and glycol ethers as well as propellants are only very weak airway irritants and not expected to induce sensitisation in the airways (and thus not the ocular surface either); this does not preclude the fact that there may be people with a higher-than-normal sensitivity to these chemicals. Others suggest that only particular agents have asthma inducing potential (for example, chloramine, BAK) and there is much equivocal data.37 In any case, to reduce the risk, chemical free products should be used if possible, applied with a damp cloth rather than spraying a mist into the air. The aim is not to introduce additional aerosols into the air when cleaning.
Air filters (purifiers)
IAQ can often be improved by having good ventilation, that is to say, having outdoor air flow inside. However, when the OAQ is poor it may be better to lower the natural ventilation rate. IAQ can then be improved by using air filters which are designed to filter pollutants out of the air. Some filters (for example, MERV-13, HVAC systems, HEPA) can capture fine smoke particles and viruses. It is suggested that if the CO2 levels are above 800ppm, HEPA air filters should be installed. The benefits of air filters in improving IAQ have been reviewed.59 The key features are good air flow to ensure adequate ventilation, ability to filter out a range of small particle sizes, and easy-to-complete, cost-effective maintenance. There is currently a lack of good evidence for claims that household HEPA systems remove all small particles including airborne bacteria and viruses.60 While there are studies showing the positive effects of air filters/purifiers that reduce air pollution on cardiorespiratory health59 and ocular allergy,61 there are no comprehensive studies of effects on the ocular surface.
Mask-associated dry eye (MADE)
There are now many reports of mask use increasing dry eye symptoms;40 this includes increased corneal staining, representing increased epithelial cell desiccation and sloughing, in staff who wore masks all day.40 Although dry eye symptoms and ocular surface inflammation increase, changes in goblet cell density were not observed and corneal dendritic cell density only increased in participants that already had dry eye disease.42
It has been proposed that ocular surface dryness, and hence symptoms, occur because the exhaled air flows
upwards towards the eyes’ surface when the mask is not fitted tightly across the bridge of the nose. This repeated warm air draft (36–37℃) causes tear film instability and dry spot formation and is thus termed mask-associated dry eye (MADE). 62 Relief of dry eye symptoms may occur by taping down the upper aspect of the mask. Primary management includes ensuring the mask fits well, particularly across the nose bridge, and secondly, rewetting eye drops are used as required.
CLINICAL ADVICE RELEVANT TO AIR QUALITY AND OCULAR SURFACE HEALTH
Tips to consider for improving air quality with potential beneficial ocular surface health are summarised in Table 3. ECPs should consider how they can contribute to global sustainability and reduce their own emissions, and lobby for the importance of clean air and reduced air pollution. If the OAQ is of good quality, suggest patients increase their time outdoors. Take steps to improve IAQ; this might mean ensuring adequate indoor air ventilation, using air filters if the IAQ is poor and humidifying the air adequately. ECPs can advise patients to take frequent micro-breaks from screen use and consider their workstation design. Everyone should carefully avoid use of spray cleaning products at eye level. Wear a correctly fitting mask and use ocular lubricants, or contact lens rewetting agents in dry environments to reduce ocular surface desiccation. Be aware of medications that are known to alter the quality of the tear film.
ECPs should consider which of these recommendations might benefit individuals and thus what to focus on in the advice they provide to each patient. This advice is particularly important for patients that already have a compromised ocular surface.
This article highlights the critical importance of both OAQ and IAQ on the health of the ocular surface. ECPs should consider people’s environments and habits, the effect of these on the ocular surface and individualised advice provided.
This CPD article was developed from discussions with Professor Peder Wolkoff, Denmark, an expert on indoor air quality and its impact on the ocular surface.

Dr Katrina Schmid is associate professor in the School of Optometry and Vision Science, Queensland University of Technology. Her teaching expertise includes ocular pharmacology, and in particular, the mechanisms, uses and side effects of ocular therapeutic agents. Her research interests include assessment of the ocular surface, including meibomian gland dysfunction and dry eye, and its treatment.
Richard Edwards BSc, MCOptom
IN BRIEF This article provides an overview of the types of complaints received by the Optical Consumer Complaints Service (OCCS) to highlight trends and help practitioners identify common issues that can be avoided in clinical practice.
Each year the OCCS presents its annual report to the General Optical Council (GOC). The discussion following the report is always highly engaging and the insight provided by GOC council members helps to stimulate the development of the future plans for the service. Nevertheless, the majority of registrants are unlikely to find time to digest the full report with the same curiosity that council members consistently demonstrate, despite the fact it provides real insight into the trends and patterns of how the optical consumers in the UK are thinking and behaving. This article shares a bitesize summary of the trends and data from the OCCS 2021–2022
report1 to provide readers with key insights from this goldmine of information on consumer trends. Shaped by the mood of society, the work carried out by the OCCS adapts to the current challenges faced by patients and optical practices. Indeed, since the beginning of COVID-19, the work and mediations carried out by the OCCS have been impacted by the sharp shock that the pandemic had on society and the relationship between optical practices and consumers. From social distancing to economic uncertainty, the sector, and therefore the OCCS team, has had to be nimble and adapt effectively to help overcome a series of novel difficulties that came to define the height of the

Table 1 Executive summary of OCCS caseload 2021–2022 including data relating to GOC FTP complaints and OCCS cross referrals
pandemic. As previous reports and outputs demonstrate, the OCCS has developed proven strategies that have supported patients during a particularly tumultuous time.
The lasting effects of the pandemic are now being felt as the UK economy struggles with rising living costs and is something that is already feeding into the complaints that the OCCS are asked to mediate. While there is no question that these conditions have created the perfect storm, there is also no doubt that the past two years have provided the OCCS with a renewed strength to navigate such choppy waters.
The following sections summarise the work by the OCCS over the past reporting year, providing a rich amount of insight and data that form the foundations for existing and future trends.
As part of the GOC’s remodelling of the fitness to practise (FTP) triage process and implementation of acceptance criteria, the GOC FTP and OCCS teams have worked closely to develop and refine an effective approach which balances the fundamental public protection role of the FTP process with proportionate resolution and a complainant-focused approach. From an OCCS perspective, their key aim is to support
proportionate and effective complaint resolution, and the specificity of the FTP process. The new collaborative approach by the GOC to triage cases has been hugely successful in channelling complaints to the most appropriate body. Fully redacted case synopses are presented from which the OCCS can easily define the appropriate channel for a complaint. The process has been consistently uncontentious and easy to secure unanimous support for a course of action.
A headline summary of the 2021–2022 report shows that:
• The OCCS received a total of 1734 enquiries between 1 April 2021 and 31 March 2022, an increase of 21.5% on the previous year
• 95% of enquiries received were consumerrelated issues which fall under the remit of the OCCS. Of those that were out of remit, five were referred by the OCCS to the GOC FTP committee; this represents 0.2% of all enquiries where three cases involved behaviour and attitude of a GOC registrant and two related to clinical diagnoses
• Concerns which were initially received by the GOC and subsequently referred to the OCCS as they did not amount to allegations of FTP, totalled 5% (89) of all enquiries; this
is an increase of 117% on the previous year and demonstrates the growing effectiveness of the collaborative working relationship between the GOC FTP triage team and the OCCS.
A breakdown of cases in each year from 2018 to 2022 is provided in Table 1 along with a summary of outcomes comparing the past two reporting years in Table 2. The main driver of the overall activity increase is the number of enquiries which require support at a local level, both from consumers contacting the OCCS for preliminary mediation and practices reaching out for support. An overview of the types of complaints received in the past two reporting years is provided in Table 3 (see page 82). The year-on-year variation reflects the increased activity in the optical sector compared to the 2020–21 pandemic period where practices operated in ‘red’ and ‘amber’ conditions. The proportion of complaints relating to the goods and services received in 2021–2022 is consistent with pre-pandemic years. Figure 1 provides data on timescales from the time of enquiry to the conclusion of OCCS involvement. Through the remodelled FTP process, proportionate and effective triaging has helped to ensure that concerns are considered and handled within the most appropriate forum. GOC FTP data indicates that of the concerns received by the GOC, 75% did not fall within the acceptance criteria, and therefore, an investigation was not
appropriate. Of those 75%, 27% were referred to the OCCS for complaint mediation and resolution, where effective, proportionate management of the issue, underpinned by a reassurance that should any FTP matter emerge then the OCCS will refer such rare cases back to the GOC. This arrangement demonstrates the importance of cross-organisational work, and the supportive role of the OCCS in relation to the GOC’s statutory function of public protection and maintaining confidence in the profession.
In addition to direct referrals by the GOC FTP team to the OCCS, and complainants given details of the OCCS, there are also complainants who will self-triage via the GOC or the OCCS websites. There is ongoing collaboration between the OCCS and the GOC to improve this pathway.
A critical aspect of the OCCS’s role is to ensure that any complaint involving potential allegations of impaired FTP are referred to the GOC in order to protect the public. While these events are rare, it is essential that this monitoring and safeguarding aspect of triage and mediation management is effective. The OCCS team has a good understanding of the issues and concerns which may amount to impaired FTP; this is reinforced through training and interaction with the GOC FTP team with both organisations having a detailed understanding of how the roles differ and support each other to deliver timely and effective resolution. The OCCS team combines optical sector
experience with mediation resolution skills to provide effective support and guidance at the initial point of contact by the consumer. If the complaint has exhausted local resolution, it will progress into full mediation. In 66% of contacts within the OCCS remit, the complaint remains in local resolution, that is to say, with the practice. The OCCS will explore with the consumer:
• The details of the complaint
• What has been done to try to resolve the matter so far
• If no contact has been made with the practice, how the complaint should be presented, and the focus needed to help aid swift and local resolution
• Why the input by the practice so far has not resolved the complaint
• The basis, and root cause of the complaint and the desired outcome, to assist the consumer in formulating and articulating a reasonable and focused interaction with the practice.
As a result of this guidance, 95% of these interactions are successful and the complaint does not need to return to the OCCS. In 2021–2022, the OCCS saw a 22% year-on-year increase in the number of complaints assisted at this stage; this is to be expected given the increase in activity across the sector in 2021–2022 compared with 2020–2021 when tighter
restrictions were in place across all four nations and the pandemic impacted on practice capacity. The OCCS continues to analyse complaints to share real-time updates and guidance for practices to access, to help minimise recurrence and proactively adjust ways of working.
Where local resolution has been exhausted, the OCCS will engage with the consumer and the practice to mediate the complaint. The OCCS conducted 8% more mediations in 2021–2022 compared with 2020–2021, with a consistent year-on-year resolution rate. The assigned OCCS resolution manager mediates between the consumer and the practice to assist in finding a resolution acceptable to both parties. There is little variation in the outcomes or the need for full mediation in different types of complaint, except for complaints relating to charges and offers, which are more likely to be resolved at an earlier stage without the need for full mediation. The resolutions mediated within the OCCS process range from:
• Supporting the consumer to return to the practice for a further consultation, adjustment or replacement product
• Partial or full refunds
• Apologies
• Explanations and conselling of the patient
• Supplementary and complimentary product supplied
• NHS voucher reinstatement.
In the 2021–2022 reporting year, the OCCS saw a significant increase in diagnosis-driven complaints reflecting more activity within the sector and increased confidence in older members of society returning to their opticians. The largest year-onyear increase related to cataract where concerns increased from eight to 22 cases. No clinical concerns were noted in these cataract cases, rather, the issues were primarily that of communication and patient understanding of referral criteria. As such, in most cases, the OCCS was able to address the concerns swiftly in early phases of the process. Where required, the consumer was supported by the OCCS working with the practice, or directly, to ensure they had an explanation of the decision or the referral criteria and process. However, it is a salient reminder to registrants of the need to ensure patients understand their condition and to keep good records of advice given.
Overall, in this category, the OCCS saw the majority of these complaints referred to the practice with preliminary mediation, advice and local resolution support. This reflects the increasing capability and confidence of the resolution manager in this arena, and the effective use of GOC acceptance criteria concerning single clinical issues. The complaints falling outside of remit were a combination of consumers wanting to refer the matter to the GOC or complainants who were adamant they wanted to pursue legal avenues for redress and were signposted accordingly.
Overall insights
Refractive surgery
In 2021–2022, the OCCS saw an increase of 30% in year-on-year complaints relating to refractive surgery, driven by an uplift in activity in this specialist clinical area as COVID-19 restrictions were eased. Most cases in this area are addressed as ‘advice only,’ with OCCS resolution managers using their expertise to guide consumers regarding their options in pursuit of a resolution. In 2021–2022, this included four enquiries relating to providers of refractive surgery who were not GOC registrants, and therefore, fall outside the remit of the OCCS. The effectiveness of mediation in these complaints has dipped year-on-year. Last year’s higher successful mediations were aided by ‘lower hanging fruit’ of complaints relating to deposit returns for customers during the pandemic. Mediation success rates are lower in elective surgery cases than ‘core optical’ cases, which
reflects the increased complexity of such complaints. Many cases relate to a disappointment in the refractive outcome and the OCCS would encourage any potential patients to be vigilant and cognisant of the detailed consent process in the area of elective surgery.
The OCCS has seen an increase in the proportion of cases supported at the local resolution stage with advice and preliminary mediation, along with increased signposting to other avenues when mediation was deemed inappropriate.
In the latter half of the year, anecdotal analysis indicates that the OCCS has seen the impact of financial pressures starting to flow through into optical complaints. This takes many different forms but includes an increase in pricing-related issues and practices perceiving complaints to be related to consumer regret. This pattern is likely to increase further in 2022–2023 as the cost-of-living crisis puts pressure on household and practice finances.
Communication in clinical complaints
The root cause of clinical complaints is consistently due to communication issues leading to misunderstanding of risks, the need for treatment or referral, and a lack of understanding from patients on the clinical progression of their condition; this demonstrates the benefits of developing professional confidence and expertise in this area to minimise unnecessary patient anxiety.
Provision of prescription
Previous annual OCCS reports have highlighted a rising trend in complaints relating to the provision of a prescription by the practice. The OCCS has undertaken some communication insight-led work on this matter. Stakeholder engagement has also referenced this issue, including feedback reports with multiples and professional bodies. In 2021–22, the OCCS saw a decrease in the number of complaints relating to this issue, reducing from 48 in 2020–2021 to 28 in 2021–2022.
Domiciliaries
Domiciliary work is an area of practice which comes with an elevated risk around patient capacity, while balancing this against a patient’s right to make their own independent decisions. Given the vulnerability of consumers in the domiciliary sector, the OCCS has always analysed complaints arising in this area to monitor how these particular
“SET AGAINST A SECTOR THAT PERFORMS UPWARDS OF 22 MILLION EYE EXAMINATIONS A YEAR, THE WORKLOAD OF THE OCCS REFLECTS A SECTOR IN TUNE WITH CONSUMER DEMANDS”
consumers can access support, and also to monitor trends in complaints arising. In recent years, the OCCS has seen an ongoing commitment by larger service providers to improve consent procedures, capacity assessments and complaint handling with consumers and where appropriate, their families or representatives.
There is oversight in this area in terms of NHS performance controls, and of course, GOC standards of practice.2 The OCCS also has visibility of the private consumer interactions which occur in this part of the sector.
Over the last 12 months, the OCCS has seen an emerging trend of rising complaints involving smaller providers of domiciliary eye care. The numbers of complaints referred to the OCCS in 2021–2022 remain low (38) but the increase from 2020–2021 (18) is significant. The impact of the pandemic and restrictions during 2020–2021 may be a factor, but the OCCS continues to monitor this sensitive area. The typical complaint issues can be categorised as follows:
• Concerns around consent being obtained for an eye examination by a provider who is not the consumer's usual optometrist
• Concerns and inconsistency around assessing capacity, and then its relevance to data protection within complaint handling
• Complaints where the consumer or their family considers the change in prescription or the visual acuity achieved with the dispensed spectacles does not justify or explain the recommended purchase.
These issues may be addressed with reference to records which note sufficient detail of findings of the eye examination and refraction. Where this information is not recorded or is minimal, it is difficult to justify the clinical judgment and

recommendations when faced with a consumer who considers they have been inappropriately or unnecessarily advised to purchase spectacles or a particular type of product. While GOC registrants are accountable for the care they deliver, some providers are not GOC registrants themselves, and therefore, currently fall outside the GOC's standards of practice for business registrants. The OCCS continues to monitor this matter so insight can feed into the legislative reform agenda if appropriate.
The future for our sector is exciting. For instance, technological advances to improve diagnostic capabilities, the emergence of myopia management, which has the potential to transform the impact of the myopia epidemic, and the opportunity for optometry to step further into the eye health space. Interestingly, the OCCS sees very few concerns relating to shared care activity in the sector currently. However, there will be challenges – the lasting impact of the pandemic and the rapidly emerging cost of living crisis will undoubtedly shape the work of the OCCS in the coming years. For all of us engaged in customer-facing work, this will present ever greater challenges; however, as the latest OCCS annual report highlights, the optical sector has shown itself to be a nimble and adaptable industry. There is every reason to believe we can meet the future challenges in the way we have met every challenge in the recent past. We should be proud of the work we do and largely the manner in which we do it. Set against a sector that performs upwards of 22 million eye examinations a year, the workload of the OCCS reflects a sector in tune with consumer demands and committed to delivering great service. Readers may be interested to note that the OCCS 2022–2023 report will be published in July 2023.
Richard Edwards qualified as an optometrist in 1987 and was director of professional services at Boots Opticians before launching OPTOMiSE Consulting in 2014. He is professional adviser to the OCCS and is a former member of the General Optical Council (GOC) companies committee. Edwards has worked on a consultancy basis for the GOC policy team and presents widely in the area of complaint resolution.
0
IN BRIEF
This feature presents a series of clinical cases seen in the hospital eye clinic. Readers are invited to review the images and use additional resources where necessary to answer the questions.

A 32-year-old female patient complains of left eye discomfort, photophobia, redness and reduced visual acuity. She admits fatigue as she has two young children. She has no previous ocular history
01 What is the most likely diagnosis?
a) Herpes simplex virus
b) Herpes zoster ophthalmicus
c) Keratoconjunctivitis sicca
d) Acanthamoeba keratitis
02 The College of Optometrists’ clinical management guidelines advise the practitioner to perform a dilated fundus examination when they suspect this condition – why?
a) To rule our viral retinitis
b) To help to reduce the intraocular pressure
c) To check for Shafer’s sign
d) To reduce patient discomfort
03 Which of the following is leastlikely to be a treatment option at the hospital eye clinic?
a) Topical cyclosporin
b) Epithelial debridement
c) Topical steroid
d) Topical antiviral
CPD POINT

A 73-year-old patient with primary open angle glaucoma is seen for routine review
04 Which slit lamp mounted investigation is shown in the image?
a) Goldmann applanation tonometry
b) Perkins applanation tonometry
c) Gonioscopy
d) Pachymetry
05 The reading that is being taken will be inaccurate – why?
a) The instrument is placed too superiorly
b) The instrument is placed too inferiorly
c) The instrument has not been calibrated accurately
d) Too much fluorescein sodium has been instilled
06 Which of the following statements about the readings obtained with this instrument is true?
a) A thin central corneal thickness will cause the intraocular pressure measurement to be underestimated
b) A thick central corneal thickness will cause the intraocular pressure measurement to be underestimated
c) If the patient holds their breath during measurement, the readings will be underestimated
d) Corneal abnormalities do not significantly affect the results

A 45-year-old male patient is referred to the hospital glaucoma clinic by their optometrist who noted raised intraocular pressure with a visual field defect
07 What is the most likely diagnosis?
a) Pigmentary glaucoma
b) Iris hyperplasia
c) Pigment dispersion syndrome
d) Posner-Schlossman syndrome
08 This condition is defined by a triad of clinical signs. Which of the following is not one of them?
a) Amyloid-like material in the trabecular meshwork
b) Kruckenberg spindle
c) Iris transillumination defects
d) Hyperpigmentation of the trabecular meshwork
09 Which of the following statements about this condition is true?
a) The patient may describe episodes of blurred vision associated with exercise
b) Patients often report pain when performing near vision tasks
c) Axenfeld-Rieger syndrome is a risk factor
d) It is more common in people of Afro-Caribbean descent


A 64-year-old female patient presents with a gradual reduction of visual acuity in the left eye over a period of one week. The previous VA was 6/5 and is now 6/36
10 What is the diagnosis?
a) Full thickness macular hole
b) Adult vitelliform dystrophy
c) Central serous chorioretinopathy
d) Bull’s eye maculopathy
11 Which of the following is not a risk factor for this condition?
a) Stargardt disease
b) Prolonged cystoid macular oedema
c) Trauma
d) High myopia
12 Which of the following tests would be leastuseful when investigating this condition?
a) Ishihara
b) Amsler
c) Watzke-Allen test
d) Visual acuity
Dr Deborah Armstrong graduated from Aston University. She worked as an optometrist in primary care and the hospital eye service before completing the IOVS glaucoma course at the University of Manchester and a PhD at the University of Bradford. Armstrong works as a specialist optometrist in glaucoma for East Lancashire Teaching Hospitals NHS Trust, teaches at the University of Bradford, and is an examiner for the Royal College of Ophthalmologists.
Dr José Ares Gómez PhD, MSc, OD (EC), DipTp (IP), Prof Cert Glauc
IN BRIEF This feature presents a series of ultra-widefield retinal images. Readers are invited to review the cases and use additional resources where necessary to answer the questions.

A 63-year-old asymptomatic male patient presents for routine examination
01 What is the peripheral retinal degeneration shown in the image?
a) Degenerative retinoschisis
b) White without pressure
c) Lattice degeneration with associated atrophic holes
d) Retinal detachment with associated fluid
02 What is the aetiology of this condition?
a) Degeneration of the neural elements of the retina leading to atrophy of the tissues with lipid deposits in the internal retinal layers
b) Due to an area of unusually strong attachment between the vitreous and retina
c) Localised inner limiting membrane thinning, overlying vitreous liquefaction and marginal vitreoretinal adhesion
d) Microcystoid degeneration of the neurosensory retina with splitting at the outer plexiform layer of the retina
03 What is the most likely type of treatment to be applied?
a) No treatment is required
b) Laser photocoagulation to the area of degeneration
c) Cryotherapy to the abnormal area of the retina
d) Scleral buckling

A 72-year-old asymptomatic female patient presents for routine examination
04 What is the peripheral retinal anomaly shown in the image?
a) Serous retinal detachment with associated subretinal fluid
b) Degenerative retinoschisis
c) White without pressure
d) Horseshoe retinal break
05 What is the most likely type of treatment for this case?
a) No treatment is required
b) Localised laser photocoagulation to seal the break
c) Cryopexy treatment
d) Pneumatic retinopexy
06 What does the pigment found in the far temporal retina indicate?
a) A fresh retinal break that requires emergency referral for vitrectomy and serous retinal detachment repair
b) Migration of pigment from the retinal pigment epithelium
c) Chronicity of this peripheral microcystoid degeneration of the neurosensory retina with splitting at the outer plexiform layer of the retina
d) Previous laser treatment for an old retinal break

07 What is the posterior segment anomaly shown in the image?
a) Honeycomb degeneration associated with vitreous floaters
b) Degenerative retinoschisis
c) Retinal detachment with associated subretinal fluid
d) Horseshoe retinal tear secondary to posterior vitreous detachment
08 What type of retinal detachment can this finding lead to?
a) Rhegmatogenous as this retinal tear is associated with posterior vitreous detachment
b) Tractional as this lesion has been caused by neovascularisation
c) Exudative as this lesion has been caused by accumulation of subretinal fluid from a mass lesion
d) Rhegmatogenous as this retinal lesion is associated with an intraocular foreign body
09 What type of treatment is shown in the image?
a) Scleral buckling
b) 360⁰ argon laser retinopexy to seal the tear
c) No treatment has been undertaken
d) None of these options

0

10 What is the temporal retina finding shown in the image?
a) Operculated retinal hole
b) White without pressure
c) Lattice degeneration with associated atrophic hole
d) Paving stone retinal degeneration
11 What is the likelihood of the finding in the image resulting in a retinal detachment?
a) 14 to 35% of cases
b) It is inevitable during a patient’s typical expected lifetime
c) It is a benign degeneration and is not usually associated with complications such as retinal detachment
d) 33% in males and 75% in females
12 Which of the following statements regarding the finding shown in the image is correct?
a) Usually located between the ora serrata and equator with a size of one to several disc diameters
b) More commonly located in the infero-nasal and temporal quadrants
c) The prevalence of this finding is approximately 4–28%, usually bilateral, no sexual predilection and increasingly common with age
d) All of these options
Dr José Ares Gómez was awarded a MSc in optometry in 2002. He returned to the University of Bradford the same year and was awarded a PhD in in 2007 which investigated retinal ganglion cell function in both normal and glaucomatous patients. He has held a position as a visiting research fellow in clinical optometry at the University of Bradford School of Optometry and Vision Science since September 2007 and has worked as a specialist optometrist at York Teaching Hospital NHS Foundation Trust since September 2008 with responsibilities in the glaucoma screening, cornea, specialist contact lens and medical retina treatment clinics.

MY CAREER ADVICE
Frances Rus (pictured), managing director at Duncan and Todd, and Julie Mosgrove, retail director, on why flexibility is key at the Scottish independent optometry group
If someone wanted to work for Duncan and Todd, what is the first piece of advice you would offer?
Frances Rus (FR, pictured): We have fairly stable teams. Often people say that the first thing they notice is that the staff know all the patients by their names as soon as they walk through the door. It makes them feel that they have to up their game, to have that much knowledge about their patients. We give them time to get to know their patients. The biggest piece of advice is to take your time in the test, to understand your patients’ needs.
When shortlisting candidates, what is the first thing that you look for?
FR: Someone who wants to work in an independent practice, and understands that difference. Also, longevity: that they are looking to stay somewhere for a while.
How important is the cover letter?
Julie Mosgrove (JM): Cover letters give a bit of personality, rather than a CV, which is just a list of experience. It allows you to find out a bit more about the person.
What is the biggest mistake that someone can make in an interview for Duncan and Todd?
FR: Someone who is totally focused on the benefits. I would expect people to focus on the kind of environment they’ll be working in: testing times
and the size of the team, for example. If I was interviewing somebody who didn’t show interest in the business, I think that would be a problem.
If you had a new employee preparing for their first week, what would you say to them?
FR: If they haven’t already, visit the practice, and meet the team and manager they will be working with.
JM: We have regular check-ins when someone is getting ready to start. Some people have a three-month notice period, so it can be a long time. We have touch points over that journey, so they feel engaged and ready to begin their role. We share information about what will happen on their induction day. We try to give as much information as possible, and advise on what to bring on their first day.
How do you approach flexible working?
FR: Duncan and Todd has always supported flexible working. The profession is predominantly female, so we are used to managing maternity
“Optics lends itself to flexible working. It just makes sense. If your people are happy, that’s a big part of work-life balance”
Frances
Rus
How important is employee wellbeing at Duncan and Todd?
FR: Really important. I joined during my pre-reg year, as did Julie. Now that it is my business, I try really hard to hold onto what I loved about it. It is a caring profession. As a management team, we all know each other really well. It’s a very approachable business. Whenever we have had external companies in, they tell me they have never had such honest and open feedback. We do exit interviews, and we’ll all sit down and discuss if there is anything there.
leave and people potentially wanting something different afterwards. Optics lends itself to flexible working. It just makes sense. If your people are happy, that’s a big part of work-life balance. Our percentage of part-timers must be 40%. It’s nearly half the workforce.
JM: We’ve always done certain things: for example, some lunches might be half an hour. Some colleagues work longer hours, but do fewer days. It is variable across practices. Some people do shifts: two weeks on, two weeks off. Everyone gets a weekend off.
FR: We try to accommodate everybody. We have had people take a month or two off to go travelling. We even had a netball player who went to the Commonwealth Games.




It couldbe, if you're lookingfor a role that'sfocusedon clinicalcare and providinga high-quality serviceto NHS patients. Due to our recent expansion, we have vacancies in multiple locations, where you'll have the opportunity to work with some of the UK's leading ophthalmologists, nurses and HCTs. You'll benefit from fantastic training and professional development opportunities too.
We're patient-focused, providing clinical expertise and support for all our patients throughout every step of their patient journey.
We're busy-as the UK's largest provider of NHS cataract surgery, we have thousands of patients choosing our services and are proud to be able to support them in improving their sight and, ultimately, their quality of life.
Our patients really value the service we deliver-we've received 5-star reviews from more than 10,000 NHS patients across our 47 hospitals -you can read these on NHS UK.
CONTACTUS TODAY:
This is a great opportunity to join one of the UK's leading ophthalmology service providers. Please call or email us today if you're interested in joining our team.
You'll be GOC registered, with at least 12 months' post-registration experience -we provide full training so previous hospital experience isn't required.
You'll be someone that enjoys variety, is calm under pressure, great at problem solving and is willing to go the extra mile to provide the best service and advice for our patients.
Telephone:0330 058 4280


'' As a member, I know that my views count
I





have a voice on the issues affecting my profession. The AOP stands up for me as an individual practitioner, and represents my profession as a whole to government and the general public.
ASIFTUFAIL
OPTOMETRIST AND AOP MEMBER


Association of Optometrists



Hi! We're Ace & Tate Opticians and we make glasses. It sounds fairly simple, and that's the whole point. We're here to inject a good dose of common sense into our industry by making well-designed, quality eyewear accessible to everyone. Great fits that last, for all eyes.
With many new stores on the way, we're expanding in the UK and seeking new colleagues.
Scan the QR and find out about our job openings. Or plan a coffee or a chat with our UK team.




















Lead the way with the UK's most flexible, adaptable and affordable OCT & Visual field solutions.






















OPHTHALMIC INSTRUMENTS 01438 740823 I sales@bibonline.co.uk

EDUCATION
Discover UCL's Optometry and Ophthalmology programmes, covering the academic component of the accredited College of Optometrists Higher Qualifications in Medical Retina and Glaucoma.
You will be taught by expert clinicians working at Advanced Practice level alongside world-leading researchers and consultants from the UCL Institute of Ophthalmology and Moorfelds Eye Hospital. UCL is ranked 1st in the world for studying ophthalmology (CUWR 2017).
Our programmes
• Optometry and Ophthalmology MSc / PG Cert
• Optometry and Ophthalmology (Advanced Clinical Practice) MSc
• Optometry and Ophthalmology (Enhanced Clinical Practice) PG Cert
• Advanced Clinical Practice in Ophthalmology (integrated degree apprenticeship) MSc
Advanced Clinical Practice programmes:

Contact us

For community and hospital-based optometrists, you may be able to fund your studies through the Apprenticeship Levy via your employer or if hospital based, through NHS England, also via your employer.
Applications close on 30 June.
Learn more or begin your application by visiting: bit.ly/ioo-programmes
Email: ioo.admissions@ucl.ac.uk Website: ucl.ac.uk/ioo
Scan the QR code to visit our website:


















UK's largest provider of NHS cataract surgery, with 47 hospitals across the country
NHS appointments available within four weeks of referral
Free transport for patients
Patients return to community optometrists for post-op assessment
SUPPORTING YOU & YOUR PATIENTS
Regular communication from SpaMedica at every stage of the patient journey
Specialist advice to community optometrists to support you with your patients/referrals
24-hour emergency hotline for your patients
Telephone:0330 058 4280
Email:contact@spamedica.co.uk
Clinical research optometrist, Reena Rani Anand, explains how a LOCSU-funded leadership skills course has transformed both her confidence and her career
Last March, I undertook the Leadership Skills for Optical Professionals course at Cardiff University, funded by the Local Optical Committee Support Unit (LOCSU). I applied after completing the LOCSU induction course and developing an interest in how to make the Walsall Local Optical Committee (LOC) more effective. LOCSU had 10 places available, and I was awarded one of these.
I COULD NOT LIVE WITHOUT...

The course improved my interpersonal and leadership skills, and has facilitated closer working relationships with staff. I gained clarity on people’s roles and now understand the qualities of good leadership. I have since been able to work with others more effectively. I have found myself analysing the workplace from a different viewpoint: what type of leadership am I seeing? Is this an effective environment and does the team feel valued?
I developed a closeness with the leadership cohort through interactions online and contact days. The instructors were knowledgeable, friendly, and helpful. Meeting in person over two days in London was my favourite aspect. Sessions involved workshops and team building exercises. Following this, I knew I was moving towards being the type of leader I wanted to be.
“As optometrists, our roles are constantly evolving and expanding, and self-directed lifelong learning is important to keep our knowledge and skills up to date”
pushing each other to progress. I am grateful to have this acceptance and support from colleagues within the profession.

We still talk on WhatsApp, celebrating our achievements and
I could not recommend the course enough. It helped me gain selfconfidence and develop understanding of my working environments and the positions within them. The leadership content enables you to view things from different perspectives. You learn about leadership styles, influencing, and persuasion techniques.
The course required weekly blogs and a final essay, improving my writing skills. Before this, I had not
undertaken any formal writing since university. The blogs allowed me to reflect on my leadership style in a non-judgemental way, to determine what was going well and where improvements could be made. They helped me focus on where I wanted my career to progress. As a result, I have learnt to seize new opportunities.
As optometrists, our roles are constantly evolving and expanding, and self-directed lifelong learning is important to keep our knowledge and skills up to date. The course has allowed me to discover and address gaps in my knowledge.
I am motivated to continue to learn and improve my practice. I am now enrolled on a glaucoma postgraduate module at Aston University.
Our LOC is more effective with participation from all members. As part of my final essay, I set up a team building activity, which acted as a vehicle for conversations about our strengths as individuals and as a team, helping us achieve our desired outcome of increased engagement and active participation among all committee members. We are far more effective and proactive now.
I have since progressed within my LOC, becoming its continuing professional development officer. I also gained employment at Aston University as a clinical research optometrist. A lot has changed in the past 12 months. I learned a lot from the course. I would urge others to consider leadership skills training.

Professor Ed Mallen tells OT why bell ringing is his form of meditation
There was a call from the Central Council of Church Bell Ringers in 2017 for people to train for the Ringing Remembers initiative, which aimed to replace the 1400 bell ringers who were killed during World War I.
I began ringing in memory of my grandfather, Arthur Wester Mallen, who was severely injured at the Battle of the Somme.
I went to Haworth Church, which is just along from where I live in the Worth Valley, said hello and asked if I could come and learn.
I have probably rung bells in around 70 towers across the UK and Ireland now. If I hear bells ringing and I’m not busy, I will go and tap on the tower door. A warm welcome is always waiting.
You learn about the heritage of the bells. At St Bartholomew’s Tower in London, the bells are from the 1500s. It makes you wonder who has heard those bells. The people who have heard that same sound is incredible really.
“If you have worries or concerns, you leave them at the tower door”
The bells at Haworth Church were put in by Patrick Brontë in 1845. The Bronte sisters would have heard those bells while they were writing – that same sound that we hear today punctuated the writing of Wuthering Heights. Bells bring people together. You get a sense of belonging and a sense of usefulness. You ring beside people of every profession, every trade and every age. I have seen people learning who are nine or 10, and I have rung with someone who is 100.
My secret life Do you have a personal passion to share with readers? Get in touch with selinapowell@ optometry.co.uk
When you are ringing and it is working well –you are catching the rope in the right place, you are putting the right amount of effort in – suddenly, the bell becomes almost weightless. What I like about ringing, is that if you have worries or concerns, you leave them at the tower door.
All you can think of when you are ringing is the control of your bell, remembering the method – the music we follow when ringing – and staying in time with your fellow ringers. It is my version of meditation really. During the pandemic, ringing was immediately suspended. It was the first time they had stopped. ringing since World War II. There was an online platform that was developed called Ringing Room where people could meet virtually and ‘ring’ together – there was no physical bell, you would hit a button on your computer. It kept people together as a community during that difficult time.
I am all for technology, but I certainly hope computers never take over bell ringing. When I was a PhD student at Aston University, I used to walk back to the train past St Philips Cathedral where they ring a three-hour performance most Monday nights.
It sounded so perfect, I thought it must be a recording. But it is not – it is 12 human beings, each with a rope in their hand, connected to a tower bell.
0
Patient is at risk of frequent changes of prescription for reasons not requiring medical referral or for reasons already known to a medical practitioner.
2 Patient has pathology likely to worsen, for example age-related macular degeneration, cataract, corneal dystrophy or congenital anomalies.
3 Patient has presented with symptoms or concerns requiring ophthalmic investigation: 3.1 resulting in referral to a medical practitioner; or 3.2 resulting in issue of a changed prescription; or 3.3 resulting in either no change or no referral (the patient's record should indicate any symptoms shown to support this category of claim if necessary).
4 4.1 Patient needing complex lenses; or 4.2 with corrected vision of less than 6/60 in one eye.
5 Patient has: 5.1 presented for a sight test at the request of a medical practitioner; or 5.2 is being managed by an optometrist under the GOC referral rules, for example suspect visual fields on one occasion which is not confirmed on repeat, or abnormal IOP with no other significant signs of glaucoma; or 5.3 identified in protocols as needing to be seen more frequently because of risk factors.
6 Other unusual circumstances requiring clinical investigation.





















has increasedits parameter range to cover 95% of the astigmatic population~ The only one-day toric lens that offers around-the-clock axes across all cylinder powers and a core range from +8.00 to -1 o.ooos_t Powered by Aquaform®Technology.
Torie Lens Geometry'."
















