




Myopia management: setting expectations100% Optical 2024 in numbersPresbyopic patients and contact lenses









Myopia management: setting expectations100% Optical 2024 in numbersPresbyopic patients and contact lenses







There is no single model for future success,

Admitting I am wrong is never easy for me – or for anybody. But when I was an academic, it was particularly hard. Not for reasons of shame: failure is part of the academic process. Sadly, that tendency to be wrong did not stop when I left academia. When I was legal ombudsman, I predicted that rising costs, changes in consumer behaviour and the increasing use of artificial intelligence (AI) in legal services would lead to the disappearance of solicitor firms from the High Street within two decades. While there has been a significant decline in the number of High Street firms, the High Street solicitor model is still very much alive. And so it is with some caution that I approach the issue of the future of High Street optometry.
On the one hand, there is no doubt that the High Street retail model is under threat. The Mintel data about consumer attitudes to online purchasing continues to show an inexorable increase in consumer preference for remote fulfilment. At the same time, the GOC has reported that over a quarter of practices are planning to increase investment in AI in the near future and that, overall, more optometrists are pessimistic than optimistic about the long-term future of the profession. At the same time, there are good reasons not to write off High Street optometry. The very Mintel surveys that extol the popularity of online retail also show that consumers/patients value the High Street experience for reasons other than mere ease and price. More significant will be the impact of the trend confirmed by the GOC survey of the growth in clinical activity on the High Street. The conspicuous failure on the part of government to respond to the growing secondary care waiting lists by moving more clinical work into primary care optometry should not be allowed to mask the fact that clinical activity is continuing to increase. What is clear is that, as with other sectors, there is no single model for future success. Yes – the number of High Street solicitors has declined and the business model is not the same as it was, but it has remained robust. If knowledge is based on learning from failure, I have learned my lesson. I am leaving the predictions game to others to play.




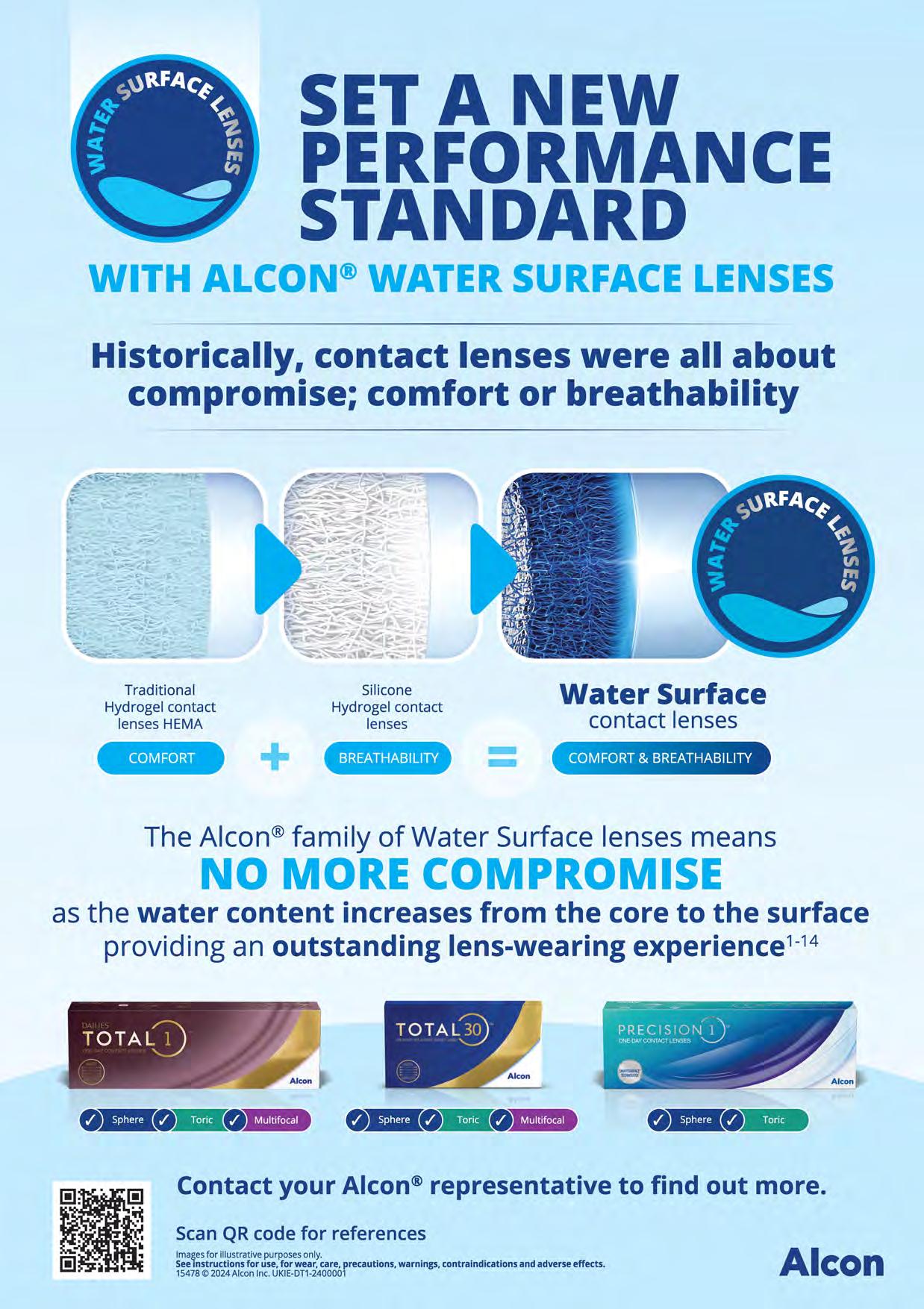
Historically, contact lenses were all about compromise; comfort or breathability








OT features a range of expert contributors who share their optometry expertise and insight. Here are some of those who helped us put this edition together

The roundtable Meeting the needs of presbyopic patients
In partnership with Alcon, OT hosted a roundtable exploring the needs of presbyopes, and how Alcon’s portfolio is supporting the needs of this growing patient group
June/July 2024
Volume 64:03 Issn 0268-5485
ABC certificate of circulation 1 January 2023–31 December 2023
Editor: Emily McCormick emilymccormick@optometry.co.uk
Deputy editor: Lucy Miller lucymiller@optometry.co.uk
Features editor: Selina Powell selinapowell@optometry.co.uk
Senior reporter: Kimberley Young kimberleyyoung@optometry.co.uk
Web content and social media manager: Leah Boyle leahboyle@optometry.co.uk
Clinical editor: Dr Ian Beasley ianbeasley@optometry.co.uk
Clinical editor for multimedia: Ceri Smith-Jaynes cerismithjaynes@optometry.co.uk
Video production editor: Laurence Derbyshire laurencederbyshire@optometry.co.uk
CPD enquiries: 020 7549 2076 CPDhelp@optometry.co.uk
AOP membership and OT subscription team: subscriptions@aop.org.uk
How should remote care be utilised by High Street optometry?
Karen Gennard, optometrist at Norville Independent Eyecare I could not live without…, page 85PAGE 40 -

“For appropriate low risk patients, ECPs may wish to consider conducting parts of the fitting process remotely, for example post-fit follow-up or a check in on contact lens handling”
Nicky Latham, professional affairs lead for myopia management at CooperVision Supplier insight, page 82


“The key is optimising outcomes for patients. Access to technology should aid, not impede, our daily practice. We must blend advanced tech with robust clinical skills.”

“When it comes to remote care in the future, overall, I would like to see it being used appropriately for those cases where it’s safe to do so”
Ankur Trivedi, IP optometrist and AOP Councillor A final thought, page 90
Advertising: Jamie Dawson 020 3771 7201 jamie.dawson@thinkpublishing.co.uk
Advertising production: aop@ccmediagroup.co.uk
Art director: Grant Pearce
Client engagement director: Kieran Paul Executive director: Jackie Scully
Published bimonthly for the Association of Optometrists by Think Media Group 20 Mortimer Street, London, W1T 3JW
Printed by Acorn Web, Normanton Ind Estate, Loscoe Close, Normanton, West Yorkshire, WF6 1TW
All rights in and relating to this publication are expressly reserved. No part of this publication may be reproduced in

claritr 1 day
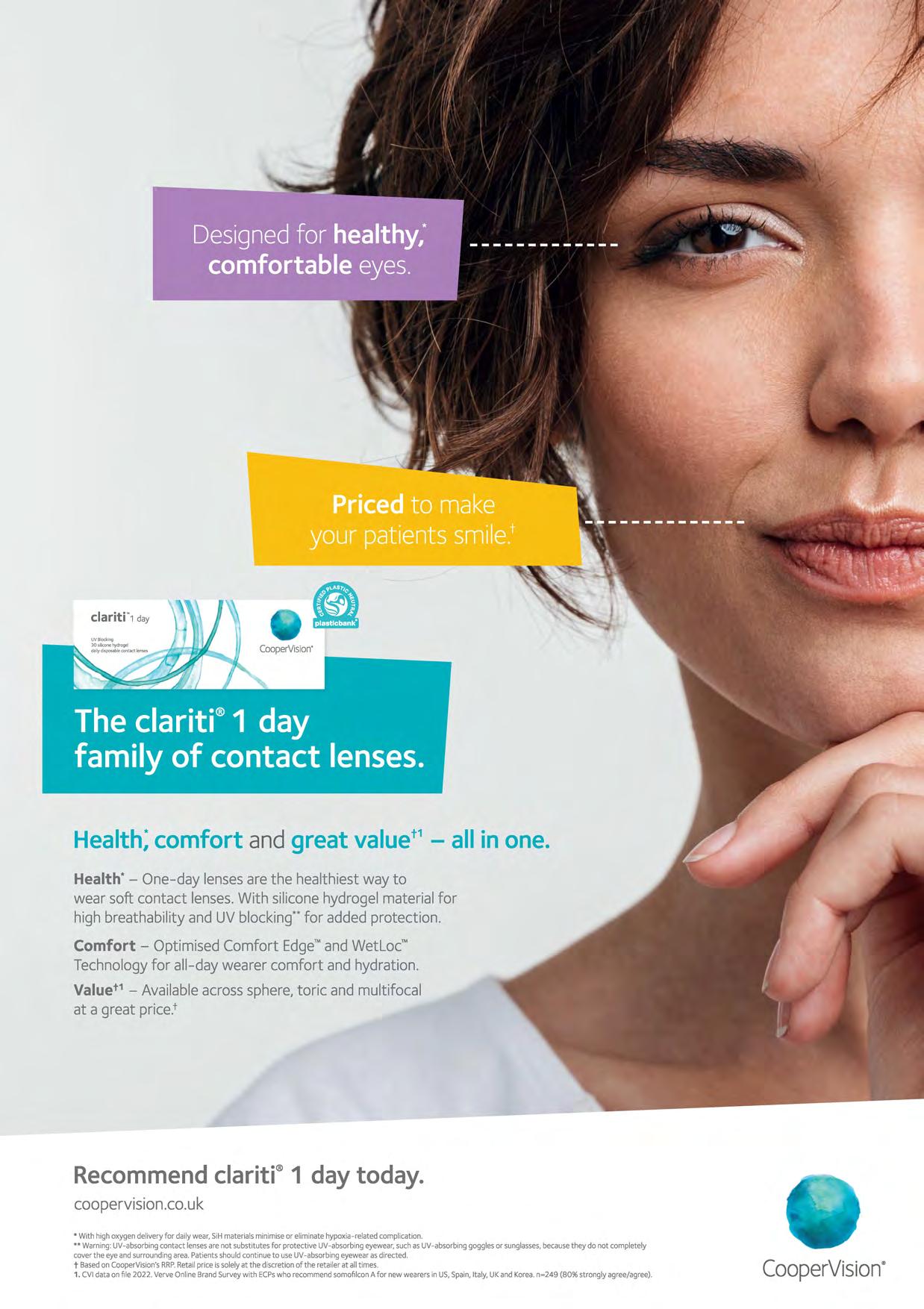
Health;comfort and great valuet 1 - all in one.
Health* - One-day lensesare the healthiest way to wear soft contact lenses.With siliconehydrogel materialfor high breathability and UV blocking··for added protection.
Comfort - Optimised Comfort Edge'"and Wetloc"' Technologyfor all-day wearer comfort and hydration.
Valuet 1 - Availableacrosssphere,toric and multifocal at a great price.t

Milestone moments
OT’s Laurence Derbyshire met with the owners of A J Rawlings, Catherine Sims and Emma Smith, to discuss the practice’s secrets after 100 years on the High Street www.optometry.co.uk/videos

You and your practice team
Read our latest content, updated daily online: www.optometry.co.uk
1
Contact lens skills guides
OT’s latest video skills guides delve into specialist contact lens fitting www.optometry.co.uk/skillsguides
We have begun filming our next Practice team training modules. The first two explore products behind the reception and personalised recommendations for contact lenses, to be released at the end of June www.optometry.co.uk/practiceteamtraining
Professor Lyndon Jones


A press event in London provided OT’s Kimberley Young and Leah Boyle with the opportunity to learn more about Transitions’ new Gen S lens www.optometry.co.uk

OT’s Laurence Derbyshire and Ceri Smith-Jaynes met with laser eye surgeon, Allon Barsam, at OCL Vision to film our next CPD video, which will be released in July www.optometry.co.uk/CPD
3
The view from the CEO
The AOP’s Adam Sampson shares insight on a range of optometry topics in his monthly OT blogs www.optometry.co.uk/blogs 2
4
Celebrating Eid
In the latest instalment of The OT Podcast, we sit down with Professor Lyndon Jones www.optometry.co.uk/podcasts
OT speaks to members about how they celebrated the end of Ramadan www.optometry.co.uk/ramadan
Tracing the history – and future – of the UK High Street by talking with staff at longstanding practices
_ WORDS: SELINA POWELL
PHOTOGRAPHY: ALEX LLOYD JENKINS, DAVID CORDNER




When a person is lucky enough to live to 100, alongside the steady procession of baked goods, flowers and a card from the King – there is one inevitability.
Questions. What is the secret to a long life? Was it the morning tai chi or the long walks through the dales? The daily crossword or a positive outlook? Perhaps a nightly whisky is the key to a birthday cake that treads the line between celebratory treat and fire hazard.
For this edition, OT explores the question of High Street longevity by speaking with staff from longstanding optometry practices across the UK about what they believe has contributed to their practice’s success. The future of the High Street is also examined by investigating how technology is changing care – and how the optical regulator is working to catch up with the changing landscape of online sales.
The centenarians
Harris Rundle Optometrists was originally established in 1905 as a network of practices throughout Ireland by Harris Rundle, the son of a sea captain from Liverpool.
Harris started his optical career at Wood Abraham in Liverpool before moving to Ireland and meeting his

wife. After enduring recessions, two World Wars and The Troubles, the remaining practice, close to Belfast City Hall, continues to provide eye care to the people of Belfast.
Optometrist and Harris’ greatgranddaughter, Lucy Rundle, took over the helm of the practice following the retirement of her father, optometrist Alan Rundle, two years ago.
When asked for her thoughts on the longevity of the business, Lucy observed that both her and her father have demonstrated a commitment to retaining personal service.
“We’re quite grounded people – we like to be involved in every aspect of the patient experience and feel that our reputation for service ensures that new patients continue to seek us out,” she said.
When the business had four practices, Alan would take a drive each Sunday to check that everything was running smoothly at branches outside Belfast.
The optometrist duo worked alongside each other for 11 years before Alan’s retirement.
“We had a very gradual transition period, trying to get to a point where the we were ready and the patients were ready,” Lucy shared.
As a newly-qualified optometrist, Lucy observed that there can be a temptation to get through the different elements of the sight test quickly. But through observing her father, she learned the importance of taking time. “When dad and I were working together, I would see him bringing in his patients. And then I would happen to pass the corridor around 20 minutes in to hear him say, ‘So, how are your eyes?’,” she said.
Alan shared with OT that he never cut corners with the time allocated to the eye examination.
“You need to take the time to listen to what they have to say,” he said. “If you try and rush through you will not get that picture of the individual you’re dealing with,” Alan highlighted.



If you try and rush through you will not get that picture of the individual you’re dealing withAlan Rundle
Alan remembers how his father, Cecil, would come home after a day examining eyes to do a further hour of work at a card table.
“He was a very honest gentleman, always very well dressed,” Alan recalled.
The pair worked together for a decade before his father’s retirement, with Cecil remaining actively involved until the age of 78.
As the first chairman of Optometry Northern Ireland, Alan has welcomed the evolution of optometry over the course of his career to provide more care in the community and relieve pressure on secondary care. “Those who are currently training to
become optometrists have arrived at a great time now that we’re much more recognised as a primary care provider. That was not always the case,” he said.
Alan qualified in 1976 after completing his training at City, University of London and his pre-registration year at the London Refraction Hospital.
He returned to Belfast to begin work at the family optometry practice during The Troubles.
“It was a strange experience. I spent four years in London, and came back into the middle of what might have been described as a war zone,” Alan shared. A former practice in Bangor was obliterated after a
bomb was placed outside the door. No one was in the practice at the time and there were no injuries.
The incident that sticks out in Alan’s mind occurred at the Belfast city centre practice one night after the shutters had been drawn and the business was closed for the day.
The practice bookkeeper was sitting at a desk by the window, and Alan had just sat down in his consulting room chair when a bomb went off on the other side of the city hall.
“All of a sudden, I was lifted off my seat and landed on the floor,” he said.
While neither were injured, Alan remembers his bookkeeper picking glass out of her hair. “When we pulled up the shutters, I heard an English accent from one of the soldiers across the other side going ‘Blimey, there’s somebody in there’,” he said.
The history of the practice can be traced through boxes at Alan’s home, with optical instruments dating back to the late 19th century, ingenious century-old advertisements, and around 50 pairs of vintage frames.

On a holiday two years ago, Alan and his wife came across a black and white photo in a practice that was previously the Cork branch for Harris Rundle for more than half a century before being sold by Cecil to Patrick Crowley. “I thought, ‘Oh my goodness, it’s my grandfather’,” he shared.


“There’s a nice sort of symmetry in that the practice is now run by his grand-daughter,” Alan observed.
While Harris Rundle was travelling the length and breadth of Ireland to oversee his many practices, across the Irish Sea in Wales, two brothers established Phillips Opticians in 1922 in Pontywaun.
Wilf Phillips, an optometrist, and Percy Phillips, a jeweller, developed a network of practices in the South Wales Valleys – with five remaining practices now run by dispensing optician and director, Lee Price.
Price originally joined the practice in 1996, attracted by the idea of working for a traditional South Wales Valley company with a premier reputation.
“There’s a real sense of community here,” he shared. “Almost every day a patient will bump into a friend at the practice.”
Price took over sole directorship of Phillips Opticians in 2019, less than a year before the first COVID-19 lockdown.
All but a small group of staff were placed on furlough – dubbed by their colleagues the ‘The Fab Five.’
Reflecting on the responsibility of steering the practice and his 21 team members through the pandemic, Price described the experience as a learning curve. “It was a baptism of fire,” Price shared.
“We didn’t know what would happen next. We had to do whatever we could to keep ahead,” he said.
During lockdown, Caroline Jenkins was the sole optometrist working at Phillips Opticians – which acted as an eye care hub for the Caerphilly region. She saw patients with everything from severe hayfever and gardening injuries to retinal tears and orbital cellulitis.
Jenkins shared that reflecting on that time period feels surreal.

Ò
a patient

“It feels almost like another world,” she shared with OT.
“I was glad to keep busy and have a purpose. I didn’t want to let down the patients,” she shared.
After completing her preregistration year with Phillips Opticians in 2001, Jenkins worked for a variety of independent and multiple practices before returning to the business in 2019.
“It was nice and straightforward. I slotted back in like I had never left,” she reflected.
Jenkins appreciates being able to spend time with patients – some of whom have record cards dating back to the 1940s.
“There’s definite loyalty. Often patients are quite proud that they’ve never been anywhere else,” she said.

When asked about the success of the practice, Price pays tribute to the value of longstanding employees. Practice administrator, Sue Winnel, has worked at the business for 50 years.
While staff are spread across five practices, they come together for birthdays and the annual Christmas party.
“We have very high staff retention. There are lots of people who have

been here for over a decade,” Price explained.
As a 14-year-old, Thomas Walls travelled from the Orkney Islands to Edinburgh. He initially apprenticed as a cabinet maker before becoming a scientific instrument maker, specialising in magic lanterns and ships instruments.
His ophthalmic and scientific instrument business, Thomas J Walls, was established in 1888.
Optometrists, George Rodger and Lyn Smalridge, who studied together at Glasgow Caledonian University, now lead the 136-year-old business.
Although the original Forest Road practice has now transformed into a coffee shop, it has kept the Thomas J Walls name – which is worked in marble on the front step and above the window – and interior features.
Smalridge, who started at the practice in 1983, recalls a dimly lit building with the floor space separated into testing cubicles by wooden panelling.
There was no advertising in the window – only a black vase, which often did not contain flowers.
A heavy velvet curtain separated the public area at the front from the

offices at the back. “People would be waiting out front and suddenly staff would emerge from behind this red curtain as though they were coming from stage left,” Smalridge recalled.
Rodger, who joined the practice as a pre-registration student in the late 1970s, described his first impression of the practice as “Dickensian.”
He encouraged staff to introduce new equipment – such as a slit lamp and keratometer.
Smalridge, who had become accustomed to the bright lights and frame displays of Dollond & Aitchison in his previous role, was also a proponent of modernising the practice.
“There was certainly an initial reluctance to these young guys, as we were then, coming in and making all these changes, but it wouldn’t have survived otherwise,” Smalridge shared.
After working the practice for more than three decades, Smalridge and Rodger have seen third and fourth generations of the same family. The greatgranddaughter of Thomas J Walls,
who is now in her 90s, would regularly come into the practice to have her eyes tested.
“She would tell us stories of her childhood sitting in the practice,” Rodger said.
While the practice has invested in new equipment, they have maintained the traditional ethos of a focus on a quality service.
When Rodger and Smalridge moved to their current Goldenacre Terrace premises, around 80% of their patient base followed.
“We’ve never advertised. We’ve never done sales or ‘buy one, get one free’,” Rodger highlighted.
“We don’t over-emphasise the commercial side of things,” he said.
This personal service sees them trust their patients to take two or three frames away without paying a deposit if they want to show their family members different options.
When it comes to the secrets of a successful, long-running business partnership, Smalridge reflected that because they had been friends at university, this formed a solid foundation for their business relationship. “Over the years, we’ve been through all the various things

in our personal lives – marriages, children being born, deaths. We’ve been through that together, so it is more than simply a working relationship,” he said.
“You have an appreciation for the person, not simply as a colleague,” Smalridge shared.
Rodger and Smalridge have overseen more than 12 pre-registration students during their tenure – some of whom have now retired.
While their own retirement is on the horizon, they want to ensure that people with the same values will write the next chapter of the practice’s history.
“Part of the reason that we’re still here in 2024 is that we have been trying to find the right people to carry it on,” Smalridge said.
“You’ve built the place up over 40 years, and you want to know that it is going into good hands,” he said.
Rodger observed that fresh ideas and leadership have helped to keep the optometry practice relevant throughout its history.
Thomas J Walls Jnr convinced his father to expand and modernise into the Forrest Road premises in 1934.
Then Ronnie Anderson invested in frame and lens manufacture in the “post-NHS boom years.”
Contact lens pioneer, Stuart Macfarlane, who became a specialist in artificial eyes, went on to receive an OBE for services to optics.
“Now it is time for new blood with the enthusiasm of youth to carry on the legacy of all these decades,” Rodger shared.
Thoughts on the future
Optometrist and practice owner, Ian Cameron, is the son of Donald Cameron – a university peer of Rodger and Smalridge.
He is also the director of nonagenarian practice, Cameron Optometry – which is a Hakim Group independent. When asked for his thoughts on how the High Street will continue to evolve over the next decade, Cameron shared that a trend defining retail currently is towards better experiences – both in person, and online.
“People don’t just want a product or service, they want to enjoy the process of acquiring it. To some extent that suits optometry as ultimately people come in for a face-to-face visit,” Cameron said.
In light of this trend, Cameron believes that it is key to ensure that patients and customers enjoy the time they spend within a practice –rather than simply treating it as a transaction.
“Why shouldn’t visiting our practices be the best hour of their day, and something they look forward to, not just a job on their to-do list? I think we’re well-placed to achieve stellar experiences compared to many other retail and healthcare businesses,” he emphasised.
He shared that patient behaviour has changed as digital technology has enabled people to access more products and services online.
“People love to shop for stuff in their jammies without leaving the house if they can. That’s fed into the way people want to access healthcare.
They want it quickly, easily and remotely where possible,” Cameron observed.
During the pandemic, Cameron and his team invested in video conferencing software, cameras and headsets to enable patients to be triaged remotely. His practice developed a set of written instructions for patients to follow when taking photographs or videos of anterior segment issues.
“We found when you do triage carefully – a thorough history combined with good quality smartphone images – you can actually manage a lot more than you think remotely,” Cameron shared. However, he still believes that the dawn of a solely remote eye examinations is some way off.
Ò
When it comes to healthcare, the personal, face-to-face element is crucialIan Cameron
“Although smartphones can do a lot, the sort of tech you need to examine an eye properly cannot be easily condensed into a smartphone or certainly not for many years,” he said. “More than that, when it comes to healthcare, the personal, face-toface element is crucial,” he added.
Reflecting on the role of technology, Specsavers clinical services director, Giles Edmonds, shared that how optometrists serve patients and support the NHS has evolved since Specsavers was founded 40 years ago.
“Technology is playing a central part in this evolution, with Specsavers committed to supporting the profession through innovation,” he said.
One of the key technological developments within Specsavers has been the roll out of more than 1000 optical coherence tomography (OCT) devices in High Street practices since 2017. “In the last year alone, we have captured more than 7.5 million OCT scans,” he said.
Specsavers was the first multiple to adopt autorefractors in the 1980s and the first to use motorised phoropters in the early 1990s.
Specsavers clinical efficiency lead, Phil Gray, told OT that the company carefully monitors how care is being delivered in developed countries across the world.
“In the US, for example, telehealth and more recently, teleoptometry, have been evolving for many years. If done in the right way, we believe remote care delivery will provide patients with better access to care in remote and rural locations,” he said.

Gray added that the General Optical Council (GOC) has recently proposed a new standard relating to how to utilise data in decisionmaking that has been generated by digital technology.
“This all points to the recognition that none of us can stop technology –rather we need to focus our work on finding how to use the appropriate
technologies in a way that is most effective and beneficial for our patients,” he said.
Research published by UK scientists in March examined how compliant websites advertising cosmetic contact lenses are with the requirements of the Opticians Act.
The study involved analysing the top website results that appear when the phrases ‘cosmetic contact lens,’ ‘colour contact lens’ and ‘novelty contact lens’ are entered into a search engine. The researchers found that only six out of the 47 websites met the requirements for cosmetic contact lens sales under the Opticians Act.
Of the 49 different cosmetic contact lens brands sold across the websites, 13 did not have CE marking.
Study senior author and ophthalmologist, Yu Jeat Chong, shared that treating a patient who had to be admitted to hospital as a result of complications related to cosmetic contact lenses formed the impetus for writing the article.
“Many of these websites selling cosmetic contact lenses were not following the required safety rules, and they often provide poor information about their products,” he said.
Chong added that two thirds of the websites examined through the research were run by companies operating outside of the UK.
He emphasised that the requirements under the Opticians Act – such as contact lenses being sold under the supervision of a registered eye care professional – are there for a reason. “Contact lenses are not riskfree. There is a risk of infection if we don’t use contact lenses properly, and if these contact lenses are of poor quality, it might pose a more significant risk,” he said.
Chong shared that on many of the websites, coloured contact lenses are advertised alongside cosmetic products – which may lead to the

misapprehension that the lenses are not a medical device. “Given the popularity of changing the colour of your eyes, I think people need to be aware that these are not just aesthetic products,” he said.
The shift in consumer behaviour to conduct more transactions online has led to calls for the GOC to play a greater role in digital spaces.
Director of regulatory strategy at the GOC, Steve Brooker, shared that the Opticians Act – which was implemented in 1989 before the internet was widely available – does not create a specific role for the GOC in relation to the online sale of contact lenses and spectacles.
“It creates criminal offences in respect of unlawfully supplying spectacles, and unlawfully supplying prescription and zero powered contact lenses that apply regardless of whether the sale is online or in person,” Brooker explained.
In terms of challenges implementing this requirement, the Opticians Act only applies in the UK.
“It is difficult to use UK law to prosecute an overseas company even where the purchaser is in the UK. There would be practical problems in presenting a hearing without the power to compel the
defendant to attend a UK court,” Brooker said.
Additionally, he highlighted that the criminal offence arises at the point of sale rather than distribution, so there is no legislative basis for the optical regulator to act against distribution centres.
“We consider that to do so would be beyond our statutory remit,” Brooker shared.
In terms of the work that the optical regulator is doing to address online sales, the GOC has published an updated illegal practice protocol (tinyurl.com/bdfn5hrn), which provides guidance on when the regulator will open an investigation and consider private prosecution.
“We are also proposing to expand the scope of regulation, which will mean all businesses within the scope of the legislation will be subject to our standards whether they operate physically or online.”

OT features editor. Get in touch by email: selinapowell@optometry.co.uk


From Belfast to the South Wales Valleys, OT captured longstanding optometry practices
A Keeler pantoscope dating back to the end of the 19th century was among an array of historical gems that were captured during OT’s June/July NotjustontheHighStreetedition photoshoots.
Alex Lloyd Jenkins photographed a collection of hand painted false eyes (below, right) at the Blackwood branch of Phillips Opticians. Dispensing optician and director, Lee Price, shared with OT: “The detail is fantastic. One of my first tasks as a newly employed dispensing optician in 1996 was to colour match a box of ‘browns’ to a patient’s eye.”
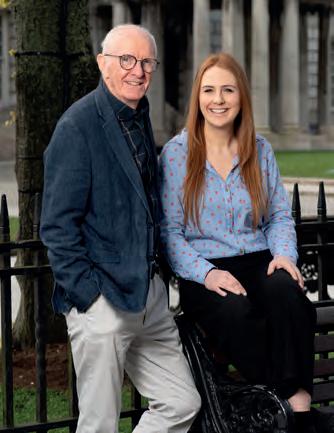
In Belfast, father and daughter optometry duo, Alan and Lucy Rundle, were photographed at Harris Rundle Optometrists and outside the Belfast City Hall.



Beginning in 1905, Lucy’s great-grandfather, Harris Rundle, established a network of practices. Boxes of Rundle family heirlooms also chart the course of the optometry practice’s history. Alan shared with OT that photographer David Cordner did an “excellent” job. “We have used him previously so we already knew that he is lovely to work with and very professional, with great ideas. We particularly liked the touch where he photographed us in the sunshine outside Belfast City Hall,” he said.


Contributors Alan and Lucy Rundle, Lee Price, Caroline Jenkins, Lois Griffiths Photographers David Cordner, Alex Lloyd Jenkins.
You can watch our online exclusive video with the owners of A J Rawling Opticians by following the QR code here


Real-time
Accessible Anytime, Anywhere
User-friendly
Career paths and personal development
EDITED BY: LUCY MILLER
36 A CONVERSATION ABOUT…
The pros, cons and opportunities of home monitoring
22 HOW I GOT HERE
Anglia Ruskin University’s
Shahina Pardhan on her diabetes awareness work
Read more about what’s happening on the ground at www.optometry.co.uk/life-in-practice This issue’s must reads...
32 A DAY IN THE LIFE
Wessex Optical’s Zabir Ali on starting the day with alpacas on his farmstead
34 IP AND ME
A 13-year-old with itchy eyes and an anxious mother presents in practice

THE SPECIAL SCHOOLS EYE CARE SERVICE: “A GENERATION OF CHILDREN HAVE MISSED OUT”
Uncertainty over fees and service specification is causing concern
Read online: www.optometry.co.uk/specialschools

“ACCESS TO EYE HEALTH IN THE COMMUNITY IS VITAL”
Professor Shahina Pardhan, the UK’s first female professor of optometry, on her beginnings in Tanzania and her long career in research
I was born in a small town in Tanzania. Eyes had always been something I’d wanted to know more about. I came across a lady who could have retained her vision, had her condition been diagnosed earlier. That was my first introduction to optometry.
I had a place to do medicine, but I didn’t want to become a doctor. Optometry, early screening, and finding people who had treatable eye diseases, was something I wanted to do.
My first sight of snow was in Bradford. I’d never seen snow, ever. It looked beautiful in pictures, but when I arrived in the UK, it was the coldest winter for a long time. I didn’t understand a word of Yorkshire dialect. English was my third language, so things were difficult. I had a good undergraduate project, and a brilliant supervisor, called Dr Jim Gilchrist. It was his passion for research that drove me to want to do a PhD. I loved my time in Bradford so much that I didn’t want to leave.
I graduated in 1984, completed my pre-reg placement, and worked for three months in practice before starting my PhD in 1986. My PhD was around how two eyes do or do not work together. If you had a cataract in one eye, would that influence your binocular vision?
I found that, if there was a significant difference between the eyes, the bad eye would influence the good eye and vision would be reduced.
When I became a research fellow at the University of Bradford, after I had finished my PhD, I went into the senior common room. A chairman said to me, ‘Secretaries are not allowed in here. You need to leave.’ I left, because I was so embarrassed. All I had wanted to do was make a cup of tea. I spoke to my PhD supervisor, who spoke to somebody else, who spoke to the chairman, who apologised.
It was unconscious bias. This man had decided this little Asian girl could not have been a member of staff. That was the start of my crusade to improve gender equity.
I was later invited to give a talk in America about gender equity in academia. I also joined Women in Vision UK, where I run the leadership portfolio. That incident in the common room was the start of it.
I stayed at Bradford for 10 more years, eventually becoming a senior lecturer. I realised there is a real problem with diabetes and diabetic retinopathy in South Asians. We looked to see what the barriers were, and
if there was a difference between Caucasians and Asians in terms of the risk of diabetic retinopathy.
In 2001, I was appointed as the first female professor at Anglia Polytechnic University. There was very little research at the university at that point. But I thought, ‘I’ve got a blank sheet that I can draw upon to develop the research.’ It was a challenge that I thought would be really good to take on.
“I don’t think anybody should have a higher risk of blindness just because they don’t have understanding or support”
We submitted the research profile to the Research Excellence Framework in 2008, where we got world class scores. Because of that, the university decided to invest in us. I then set up the Vision and Eye Research Unit, which has now become the Vision and Eye Research Institute within the School of Medicine.
I’ve been researching within India for over 15 years, because of its very high prevalence of diabetes. This is a real passion for me. I don’t think anybody should have a higher risk of blindness just because they don’t have understanding or support.
NAME:Professor Shahina Pardhan ROLE: Director of the Vision and Eye Research Unit at Anglia Ruskin
University LOCATION: Cambridge
I’m currently director of the Centre for Inclusive Community Eye Health at Anglia Ruskin. Access to eye health in the community is vital. Unless we can improve access to people who are underserved, we will not be able to make progress. We need to find innovative ways to improve access – from trying to prevent eye diseases, through to ensuring that those who have lost their vision get the best care.
Shahina’s global work on diabetes awareness
Asian people with diabetes have a higher risk of sight-threatening retinopathy. Our research showed that the literacy levels of those most at risk was low. They didn’t know that if they didn’t go for a walk, it would make the diabetes worse. We needed to improve the health literacy and make it culturally appropriate. We used research around barriers for these groups to develop videos in various Asian languages. We started with Hindi and Urdu, but now have them in nine languages. We’re also developing programmes in black and Caribbean, Chinese, and traveller communities.

At Newmedica, we choose to use the highest quality cataract replacement lenses for the best clinical outcomes. In fact, our monofocal lens for NHS patients has the lowest PCO rate of any lens on the market at 3 and 5 years. It's hydrophobic and is specially designed to reduce the need for YAGsurgery*.
Which is great news for your patients and the NHS,and peace of mind for you.
*source : The Royal College of Ophthalmologists, National Ophthalmology Database "Feasibility Study of Post-Cataract Posterior Capsule Opacification" May 2021
Independent prescribing optometrist, Kamal Sandhu, explains how locuming has given her the career progression and support she needed
Before I became a locum... I was working as a resident for a multiple. I started there aged 19 as an optical assistant whilst I was studying at university, and worked my way up to pre-reg and then to qualified optometrist.
When I started as a locum, I wish I had known... How essential it is to register with a good locum agency. They get to know your skills and what you’re comfortable with. Importantly, they know your worth. A good agency will always contact you with opportunities, rather than you having to chase them.
I made the decision to become a locum because... As a resident, I had had enough. As a newly-qualified optometrist, I moved to a large practice within the group where I had completed my pre-reg placement. I had promises of support, but I unfortunately did not receive this. I transferred to a different practice, which was better, but I still found little room for career or financial progression. I handed in my notice and left shortly after.
On my first day of locuming... I was nervous. I had never worked for another organisation, and I didn’t know what to expect. But I went in early to learn about the practice, and from then my day just flowed. I had such a fun time with the manager and the team, who were helpful and accommodating. That’s when I realised I had made the right decision.
My biggest locum challenge is… Not being able to follow up on patients, especially now that I’ve qualified as an independent prescriber (IP). It’s good for patients to follow up with their original clinician, but most of the time this isn’t possible if the patient has seen a locum. You have to trust other clinicians to continue with your follow-ups.
Practices can make life easier for locums by… Taking time out at the beginning of the clinic to go through how the store runs, and where everything is.
NAME: Kamal Sandhu
LOCATION: Surrey and Berkshire
LOCUM FOR: Seven years
6
It would be good if they could familiarise us with the staff, so we know who to hand over to after the eye examination. Show us where the trial banks are, and provide information on referral pathways and hospitals that we should refer to if needed. Lack of information makes it difficult to ensure the clinic runs smoothly.
One change I’ve seen whilst working as a locum is … The improvement of equipment in stores. When I first started locuming, the latest equipment was a fundus camera. Since then, most practices have acquired optical coherence tomography and Optomap machines, which has almost forced optometrists to educate ourselves on interpreting them. This has made it easier to assess patients, allowing for more detailed referrals.
My favourite thing about being a locum is… Without a doubt, meeting new people. I get to network with resident and locum optometrists, dispensing opticians, and optical assistants. I’ve made some great friends through locuming. It’s always nice meeting people from different walks of life, and it is refreshing to change your environment. Working as a locum has also enabled me to travel to different places in England that I wouldn’t have thought about exploring.
My advice for new locums is... Take the jump. It seems daunting chucking yourself into the unknown world of locuming, but you won’t know what is out there until you try it. Expose yourself to different scenarios, whether it’s a new location, different practices, or even block bookings. You’ll either love it or hate it, but either way you’ll know what is right for you.

My last word on locuming is... Never forget to upskill. Optics is changing, and it’s always important to keep up with continuing education. Having further education is worth its weight in gold when you work in unfamiliar areas. Being able to prescribe as an IP optometrist, when some patients have poor access to healthcare, can make a world of difference.
0
Read more locum insights online: www.optometry.co.uk/life-as-a-locum

* Compared to ACUVUE® OASYS 1-Day. t Filtering of HEV light by contact lenses has not been demonstrated to confer any systemic and/or ocular health benefit to the user. The Eye Care Professional should be consulted for more information. :j:Versus publicly available information for standard daily use contact lenses as of June 2023.
1. JJV Data on File 2022. TearStable™ Technology Definition. 2. JJV Data on File 2022. Effect on Tear Film and Evaluation of Visual Artifacts of ACUVUE® OASYS MAX 1-Day Family with TearStable™ Technology. 3. JJV Data on File 2022. Material Properties: 1-DAY ACUVUE® MOIST, 1-DAY ACUVUE® TruEye®,ACUVUE® OASYS 1-Day with HydraLuxe® Technology and ACUVUE® OASYS MAX 1-Day with TearStable™ Technology Brand Contact Lenses and other daily disposable contact lens brands. 4. JJV Data on File, 2022. CSM Subjective Responses ACUVUE® OASYS MAX 1-Day Contact Lenses-Retrospective Meta-analysis.

YOU HAD ME AT HOSPITAL
Principal optometrist at SpaMedica, Tom Critchley, on his close relationship with ophthalmology and why dialogue between primary and secondary care providers is so important

How long have you worked as a hospital optometrist?
I’ve just celebrated my 10th year working in a hospital. I am immensely proud of what I’ve learned in that time. I now also teach.
Could you describe working as a hospital optometrist in one sentence?
Helping patients in hospital is exciting, challenging and extremely rewarding.
When and why did you decide to become a hospital optometrist?
I worked in primary care for a number of years, followed by a spell in the refractive field, all of which I enjoyed, but I was always hoping for clinical advancement in the profession. I took a gamble with a small independent ophthalmology provider called SpaMedica. The cataract clinic was starting, and that’s when I was brought on board, to use my previous experience to build that service. The rest is history.
Do you do any other work or volunteering alongside your optometry job?
I carry the same passion I’ve got for my work into grassroots football. I run a local football team, spending the evenings and weekends coaching local children.
Can you describe the relationship you have with ophthalmology as an optometrist working in a hospital?
Historically, there has been a barrier between ophthalmology and optometry. But at SpaMedica we work very closely together, in a respectful way, and learn from each other. I think we’re pushing the professions forward with our mutual skills and ideas. It’s a great working relationship. We’ve got a wonderful team of surgeons.
What is the biggest challenge facing hospital optometry?
Speaking on a national level, the accessibility to NHS services does vary tremendously around the UK.


How can the optometry profession help to alleviate that?
There needs to be increased dialogue between the profession and commissioners of NHS services across the UK, to make sure the rollout of extended optometry services happens and is the same for all, regardless of where that patient might live.
Would you add anything else on the subject of working as a hospital optometrist?
NAME: Tom Critchley
ROLE: Principal optometrist at SpaMedica
LOCATION: Bolton
It’s a great job. I tell my new starters that it’s the job that you were going to do when you filled in that UCAS form. It’s never too late to make that brave leap into the world of hospital optometry.
Read more hospital insights online: www.optometry.co.uk/you-had-me-at-hospital
One valuable moment
My first YAG treatment. It was something I never believed optometrists would do. Doing something that has historically been the work of an ophthalmologist was really cool. Now, the optometrists love it. It’s their favourite clinic. Patients come in and they can’t see, and minutes later they have their vision restored. A lot of hospitals now are employing optometrists to do these advanced services, which brings down waiting times and is another string to the optometrist’s bow. I love watching our new optometrists do their first one, knowing exactly how they’re feeling.


Lizzie Shaw, pre-reg optometrist at Moorfields Eye Hospital, tells OT about gaining confidence in contact lenses as she completes Stage 1
When I encounter something interesting in clinic, I try to learn around it. For example, I had a patient with pigment dispersion syndrome in for a sight test. This was not something I had seen since university and at the time I was unsure what other signs I should be looking out for, as it isn’t commonly encountered.
I had an observation session in the glaucoma clinic later that day and saw another patient, who had pigment dispersion glaucoma, which helped me to solidify signs associated with the condition, such as Krukenberg’s spindle.
At the time of writing, I am about to start my Visit 4. I am focusing on bettering my skills and getting more comfortable being directly observed before the hard revision starts. I am picking up more things by myself that my supervisors could query, for example rechecking cylinder changes and calculating possible anisometropia in a new prescription. I feel I am able to view things more holistically.
NAME: Lizzie ShawROLE: Pre-registration optometrist at Moorfields Eye Hospital
LOCATION: London
The last few months have been intense, which I have particularly noticed in my logbook numbers as I move towards the end of Stage 1. I am able to do more and see more patients, which has been instrumental in growing my confidence. Initally, I found contact lens fits intimidating, as we mainly fit rigid gas permeable lenses for keratoconic patients. In pushing for numbers recently for my logbook, I have done a lot more in a short space of time. Now I feel confident with choosing specialist lenses depending on the position and steepness of the cone, and even look forward to fittings. I have seen the correct contact lens improve visual acuity enormously. It can be a very satisfying part of the day.
I know I have a long way to go, but I am now seeing patients where I think I will be capable of testing them unsupervised. I often feel stressed when I think about practising by myself without supervision, so these moments are nice, because I can see a light at the end of the pre-reg tunnel. I have decided to extend my contract at Moorfields, so I know that when I am qualified, I will be in an environment where I am comfortable asking for help.
Clinic leads are now starting to rely on us more, which is gratifying. Our pre-reg placement at Moorfields is always a little slower to start with, as we observe clinics first and get used to the environment and ways of working. Initially it can feel daunting to imagine yourself practising in the same way, so now feeling that I am a valued and useful part of the department is really fulfilling. I look forward to this continuing and developing.
This is a special year, and will probably be the fastest and most intense period of learning and development I will ever have, so I am trying my best to make the most of it and take in every opportunity I can.
I am preparing for the next assessments by... looking into mock objective structured clinical examinations (OSCE) courses. I have booked onto the July exam and am hoping to do some mock OSCEs.
At the beginning of my pre-reg, I wish I had known... that confidence really does come with time. I am feeling more confident every day and I feel I have come a long way.
The most important thing I have learned over the past few months is... that repetition is key. Knowledge and skills that I struggled with come naturally now. I feel confident managing pathology after seeing cases in practice.
Hayley Smith is a pre-registration optometrist at Peter Ivins Eye Care, Bearsden



05:45
The first thing I do in the morning is check my phone, to make sure everything has been ok over night.
I was always a city boy. When I moved to the south coast it was so different, and I fell in love with it. Three years ago moved to Dorset, 10 minutes from my main practice.
I’ve got a small farmstead, with peacocks and alpacas. I make sure they are fed and that they’ve had a run around and are ready for the day.
07:00
I have a quick breakfast, then go to the gym. I’ll do weights, functional training, and spend 10 minutes in the sauna. Then, I’ll get ready and go to one of my practices.
08:50
Zabir Ali, optometrist and owner of Wessex Optical, talks OT through his day –from feeding the free-range peacocks on his Dorset farmstead, to evening dinners with colleagues
I’ll arrive just before 9am. I’ve got an operations team, but it’s always nice to see the owner. I check in on how their weekends have been, and how yesterday ended.
Before my first patient, I set up my team for the day. I’ve got a financial director and an operations director, and if I’ve started testing at 9am, I’m back-to-back with patients and my day is gone. I learned that the hard way.
09:30
If I’m in clinic, which I am twice a week, I will start with my first patient by 9.30am. From then until lunchtime, I’ll be with patients, maybe supervising a pre-reg at the same time.
I never turn a patient away. If they come in late, I see them; if they have a problem, I’ll see them. That’s what I expect from my teams too.
NAME: Zabir Ali
ROLE: Optometrist and practice owner at Wessex Optical
LOCATION: Dorset
11:00
I don’t like to check emails between patients. I want to make sure patients feel like they are the most important person at that time. We are doing an important job, looking after people’s eyes and livelihoods. I feel like I’d do them a disservice if I was focused on anything else. I’ve got lots of business interests and lots going on in my world, but when I’m testing, the patient is my work. I always tell them that a clinic day is my favourite day of the week.
13:00
I love healthy eating. Chicken, fish, veg, and rice is my go-to lunch. If there’s an independent cafe, I’ll go there. Sometimes I feel like a plantbased day – Lymington has one of my favourite vegan places. It’s also supporting the High Street, which is important. By the time I’ve checked emails, and had a pace up the High Street, I get to sit down for 10 minutes and then I’m back with patients.
14:00
The first task of the afternoon is checking in with the team again, and then it’s setting up for the rest of the afternoon. I will see my last patient at 4.45pm, and finish by 5.30pm.
18:00
A few nights a week, I’ll meet people for dinner. It might be a business meeting, or with one of my team. I love a Wagamama.
The thing I most enjoy watching to unwind is...
21:30

The Apprentice and Dragon’s Den
At the moment I am loving The Apprentice and Dragon’s Den. When people are starting their careers, they make some funny mistakes. I do enjoy watching that. I like to read about holistic health, too.
22:30
I’m in bed by 10.30pm, and hopefully asleep by 11pm, so I can do it all over again the next day.

My fantasy practice...
Read more business owner stories online: www.optometry.co.uk/a-day-in-the-life
If I could make one change to the optometry profession, I would allow optometrists to take on more secondary care from hospitals. I think that would really open up healthcare for optometrists. I think optometrists could do a lot more for the general healthcare sector. My wildest ambition for my practices is for them to be the best practices in the world, leading the way for premium eye care and eye health.


OT presents a clinical scenario to three of its resident IP optometrists. Here, a teenager with itchy and blurred vision and an anxious mother
The scenario:
A 13-year-old girl attends your practice with her mother and explains that she has had blurred vision and bilateral itchy and watery eyes for the past week. She is in general good health, and is not taking any medication. Her mother is extremely anxious and pressures you for a fast resolution. How would you manage?
OT’s panel says...
Ceri Smith-Jaynes: There are three differential diagnoses on my mind: allergic conjunctivitis, blepharitis (and the consequential dry eyes), and infective conjunctivitis. All of these

can present with itch as the primary complaint. However, the blurred vision is troubling. Some additional questions will help:
• Do you have a cold or a runny nose? If yes, it could be viral conjunctivitis or allergy
• Is there yellow gunge coming out of your eyes? If yes, I’ll think bacterial conjunctivitis
• Does anyone close to you have it? If yes, it’s more likely to be infection, although it could still be allergy
• Do you have any allergies, such as hayfever, asthma or eczema? If yes, it’s a great clue – but she could still have an infection
• Is the itch mostly around your eyelashes? If yes, I’ll suspect blepharitis
• Did it start in both eyes at exactly the same time? If yes, it’s more likely to be allergy
• Any photophobia? Patients with dangerous photophobia usually have sunglasses on in the waiting area
• Do you wear contact lenses?
First things first: I would check acuity, and I might even have to do a refraction. Is this just blur from mucus, which clears with a good blink, or a 13-year-old becoming myopic? Or are there corneal lesions degrading the image? Adenovirus sometimes causes small white lesions in the cornea. Then, I would perform a slit lamp exam. Molluscum contagiosum on the lids can cause viral conjunctivitis. Blepharitis should be obvious.



Ankur Trivedi
OCCUPATION:
Papillae and follicles are harder to differentiate. Tiny petechial haemorrhages on the conjunctiva suggest viral infection. Check the cornea for lesions or oedema and instil fluorescein. Long strings of mucus suggest allergy.
There is a small lateral flow test called AdenoPlus, for detecting Adenoviral antigens in tears, but it’s around £15 per test and the sensitivity is <50%.
This is tricky. Without looking, I just can’t tell. If it’s viral conjunctivitis we can only offer cool compresses and lubricant drops for comfort. It’s June, so seasonal allergic conjunctivitis is common; my usual treatment is olopatadine 0.1% eye drops twice a day. This is a combined mast cell stabiliser and antihistamine that works quicker than the over-thecounter eye drops such as sodium cromoglicate 2%, dosed at four times a day. College of Optometrists guidance does include topical antihistamines for severe itch in viral conjunctivitis. And on the other hand, cool compresses and lubricant drops will help with allergy symptoms.
Kevin Wallace: As usual, Ceri has given us a very thorough answer. My thoughts are similar – particularly this time of year, I regularly see patients with seasonal allergic conjunctivitis. You would expect that the main symptoms of that would be the itching and watering, not blurred vision, so it is important, as always, to consider other reasons for the blurred vision.
If it doesn’t improve with the other symptoms, I would want to see her again to investigate – particularly if it had been a while since her last examination. I probably wouldn’t refract if there is an obvious conjunctivitis, but a pinhole would be useful to see if the vision improves.
A significant factor in my decision making is the patient’s recent history. If they’ve had an upper respiratory infection, I would suspect a viral cause (usually it would have started in one eye, and as Ceri said you may see signs such as petechial haemorrhages).
Without that, I would lean more towards allergy. If I decide that it is an allergy, I would use olopatadine drops,
which are very effective in a short time. The main issue with them is that they can only be used for, at most, four months. Fortunately, most just need a few weeks or a month of treatment.
Ankur Trivedi: There has been a recent upsurge in measles cases in certain hot spots around the country, including in the West Midlands and London, so this is where the questioning around general health is pertinent.
It would be unusual, in my limited knowledge of measles, if the ocular symptoms were the sole manifestation, sign or symptom. It does remind me of some anecdotal cases reported in the early pandemic, of COVID-19 presenting with conjunctivitis. I am not sure this ever made it to one of the primary symptoms of concern, however. If a viral aetiology is suspected, palpating the preauricular lymph nodes to check for tenderness is useful, but this is not present in all cases of viral conjunctivitis.
“It is important not to let the pressure you may feel from an anxious parent or carer sway your management plan”
Ankur Trivedi, AOP Councillor for IP optometrists
In this scenario, it is important not to let the pressure you may feel from an anxious parent or carer sway your management plan. I know this can easily happen, especially when children are involved.
In terms of differentiation between papilae versus follicles, I have always tried to look at the vascular appearance – papillae have a central redness with surrounding pallor, while follicles have central pallor with surrounding redness. I do appreciate, though, that it is never that clear cut outside of a textbook.







OT asked Moorfields Eye Hospital optometrist, Indy Ghuman, and specialist optometrist and director at Edgbaston Eye Clinic, Don Williams, for their views on home and remote monitoring
Challenges and opportunities
Indy Ghuman (IG): Whilst on paper, home monitoring looks like a very good idea, there is a significant initial outlay and investment that needs to happen, and I don’t think any largescale research has shown that it is sufficient. Before you spend money on something, you need to know there is an evidence base for it to work.
Aside from that, for a patient to do it, they need to know how to use it. They need to be able to obtain the equipment, they need to use it properly and accurately, and there needs to be a method for that data then to be taken from that home and analysed. We don’t even have digital referral systems that are the same
throughout the UK, so how are we going to do that?
I think we need to take a few steps back, and do the basics first in terms of electronic referrals, and improve digital connectivity before we start looking at home monitoring. But I definitely think there is scope for it in the future.
Don Williams (DW): Funding is always an issue with these things. Where do we get the money to set these things up? That’s why I think a lot of these schemes, although we talk about them, tend not to happen. Particularly with glaucoma, most patients are elderly, and they like to be seen in a clinic.
IG: For patients, sometimes it’s the highlight of their day to come out and see an optometrist. Also, those patients are often elderly, so they are a bit more frail, and they don’t have that dexterity. If you’re providing them with equipment to monitor their IOP, or for them to do their fields at home on a regular basis to pick up subtle changes, under certain circumstances, I don’t think it’d be practical. I think you need to look at the practicalities.
DW: Domiciliary companies are already kitted out to test patients at home. Could that be blended into what they do, with funding provided for the service?
IG: That’s a really good point, because they’ve got the infrastructure already set up. If there was a scheme commissioned, that would increase the variety of their work. Often patients in care homes also have the family support network, to help integrate that.
These patients often want to stay in their homes, or maybe don’t have the capacity to leave their homes, because they’re less mobile – that’s why they’re having a domiciliary appointment. This would be perfect for them, because maybe they have something that is referable, but they don’t want to be referred, and that’s within their rights. They might be in their 90s, and they don’t want to have x, y, z treatment. But if they can keep monitoring, whether that be their intermediate age-related macular degeneration (AMD) that is progressing to wet AMD, or their cataract, or their glaucoma, that gives them more power over their health. I think it’s more empowering for them.
DW: The main benefit is for those patients who can’t really come out of care homes. Other patients just don’t like going out, so they like someone to come and see them. To integrate that within the domiciliary service would be good, because they’ve already got the infrastructure there.
Future potential
IG: In the US, there is a lot of FDAapproved technology that is ready for home monitoring. I’m not saying it
NAME: Indy Ghuman ROLE:
Optometrist, Moorfields Eye Hospital LOCATION: London
should be adopted and implemented in the UK straightaway. There was a particular one called Foresee, which was really good at monitoring progression of macular degeneration into wet AMD, without using an Amsler. There was a study that showed that about 69% of patients who were referred for AMD treatment picked it up from home monitoring. It detected any distortions they saw in their visual field, and it was able to compare that to a baseline and pick up small changes.
That means patients get referred more quickly. They get seen more quickly, they receive the treatment more quickly, and it improves health outcomes. I think that’s brilliant, and if it was used effectively, it could have a lot of scope. It comes back to the same things: having scope, but also the funding.
DW: As a private provider, I’ve just ordered an iCare Home 2 for a patient. These patients travel a lot, and they want to monitor their eye pressures. They pay me, I order a machine, then they come in and I show them how to use it. They send me their IOP readings. There isn’t a scheme for this. Because patients pay for their care themselves, it’s a lot easier to set up these things. But I do see both NHS and private, and it’s a lot easier to set it up in the private setting.
Read the full conversation between Indy and Don on the OT website: www.optometry.co.uk/a-conversation-about







NAME: Don Williams ROLE: Optometrist and director of Edgbaston Eye Clinic LOCATION: Birmingham






OT gathered the key stats for readers to review the highlights of the 10th anniversary show
Though the start of 2024 already feels like a world away for many, for OT the fun of 100% Optical continues as the team works through interviews, product demonstrations, and lecture notes from the event.
The 2024 show, which marked 10 years of 100% Optical, was also the biggest yet, with 11,725 visitors – a 10% increase on figures in 2023.
Organisers shared that 96% of respondents to the post-show survey were either ‘very satisfied,’ ‘fairly satisfied,’ or ‘somewhat satisfied,’ with 74% of visitors confirming they plan to return in 2025.
Most visitors were from independent optometry practices – those with less than five practices –the organisers found.
Survey data revealed the most common reasons for attending the show included: searching for eyewear, gaining continuing professional development points, networking opportunities, and discovering new innovations.
Selin Pera, senior marketing executive at Media 10, the organisation behind 100% Optical, commented: “We are incredibly proud to find that 96% of our visitors were satisfied with the exhibition this year. Being the UK’s only optical show bringing together the optical community and wider practice teams, it’s massively important to us to provide an event that really does bring the whole industry under one roof and represent every aspect.”
“100% Optical has now expanded to be the fastest growing optical event in Europe, bringing British and international brands to a global audience and so to start off a new decade of 100% Optical knowing that we’ve experienced our largest number of international visitors, travelling from over 50 countries, is a real coup,” she continued.
THE BREAKDOWN: 100% Optical visitors in 202439% were first-time attendees 82% said attending was important to their business 62% have sole responsibility or direct influence over purchasing decisions 50 countries represented in visitors to the show
As media partner for 100% Optical, OT took to the show with a packed agenda full of interviews to record, lectures to report on, and products to demonstrate. OT’s output from 100% Optical 2024 included:
46
INTERVIEWS RECORDED
18 hours OF FOOTAGE CAPTURED
336
GIGABYTES OF DATA
See the full suite of articles from the show at: www.optometry.co.uk/100optical
The show achieved a Net Promoter Score (NPS) of 53.22, an increase from 49.95 in 2023 and well above the industry benchmark of 17.06.
Commenting on the metric, which measures customer experience and loyalty and a benchmark for performance, Pera said: “Achieving an NPS of 53.22 fills us with so much joy and allows us to take 100% Optical to the next level.”
Pera added that, with positive feedback from the 2024 show, organisers plan to grow the event with larger stands and new additions. Plans are underway to enhance the newly co-located 100% Ophthalmology for 2025.
“No optical event has previously brought together the optical and ophthalmic community under one roof, to this scale and all for free, so for us 2024 will always be a significant milestone reached,” she concluded.
Reflecting on the show, OT gathered key stats, stand-out reports, and must-watch video interviews for readers to re-experience the highlights of one of the biggest events of the optical calendar – available on the OTwebsite.
100% Optical 2025 will take place from 1–3 March at ExCeL London. Find out more: www.100percentoptical.com
Laurence Derbyshire, video production editor for OT, picked out five unmissable video interviews from 100% Optical 2024.
1

100% Optical 2024 show review
Trying to capture the vibe of a show is always tricky, especially with so many disparate parts. Here we try to show a slice of the totality that encompasses 100% Optical.
2 Tech from Thomson Software Solutions
Eye tracking binocular vision tests, improved near vision tests, and virtual synoptophore: exploring new avenues of diagnostics are just cool. Here we see something coming from research towards practice.
3 Eyesi Slit Lamp from Haag-Streit
How many frogs do you need to kiss before a posterior vitreous detachment comes along?


With this tech, students can get to see a lot more pathology with no patient needed.
4
Paediatric designs: the Star Fit collection
Lots of data drives the design of a new collection, engineered to ensure the best fit for kids’ frames. Learn the details from this interview.
5 EssilorLuxottica’s edging suite


Edging may not be the most exciting part of optics, but efficiency is efficiency, and EssilorLuxottica takes aim at ensuring you will have frames out as soon as possible. OT received a demo.

From eyewear to tech, clinical topics to top trends: catch up on all the interviews from 100% Optical on OTby scanning the QR code.

In partnership with Alcon, OT hosted a roundtable discussion that explored the needs of presbyopes, and how Alcon’s TOTAL® Multifocal contact lenses are meeting the needs of this growing patient group
Addressing the needs of presbyopic patients can present an opportunity for eye care practitioners, as well as a clinical and a communication challenge. How to address a change in need, potentially for an individual who has never needed vision correction previously, and how to do this via contact lenses?
In partnership with Alcon, OT spoke with four practitioners about the needs of this patient group, the concerns that can arise, and how Alcon’s TOTAL® Multifocal contact lenses can assist the presbyope who presents in High Street practice.
OT is interested in how the panel would define the presbyopic patient group, and what effect or opportunity an ageing population might be having on their practices.
Ian Chalmers, senior contact lens optician and owner at Chalmers Opticians, identifies presbyopes as an exciting and growing area for his practice, offering a different optical challenge for his team.
Along with daily disposables, “it is multifocals where we’re now doing more new fits,” he shared.
Kieran Minshull, contact lens optician and director at LK Leon Opticians, agrees that this
 Ian Chalmers senior contact lens optician and owner at Chalmers Opticians, Cardiff
Ian Chalmers senior contact lens optician and owner at Chalmers Opticians, Cardiff
 Kieran Minshull contact lens optician and director at LK Leon Opticians, London
Kieran Minshull contact lens optician and director at LK Leon Opticians, London
demographic presents an opportunity for his practice. “The presbyopic demographic is really important,” he said.
“If we have successful contact lens wearers, over the years, they’re going to start struggling. If we don’t give them alternatives, if we don’t find solutions for them, they’re going to look elsewhere. We need to educate them on what’s available, what’s on the market, and what solutions we have for their presbyopic situation.”
Minshull added: “Most contact lens wearers won’t just wear contact lenses – they will also wear varifocal spectacles. So, there will be an additional profitability aspect for the practice.”
It is not only about problem solving, Minshull believes: “It’s alerting them and educating them to what’s happening with their eyes, and that there are solutions.”
A growing market might present a clinical challenge and a commercial opportunity, but that is likely to come with its own challenges – something that David Gould, contact lens optician and director at David Gould Opticians, is quick to identify.
“The biggest challenge with presbyopes is managing expectations,” he said. “Most want the vision they had when they were 25. We need to find a way of explaining that that’s not always possible.” Being presbyopic himself allows for a high level of

David
Gould contact lens optician and director at David Gould Opticians
Michelle Beach optometrist director at Park Vision Opticians, Nottingham




“TO BE ABLE TO GO OUT WITHOUT TRYING TO FIT YOUR READING GLASSES IN YOUR CLUTCH BAG OR IN YOUR POCKET, AND TO BE ABLE TO READ A MENU, MAKES YOU FEEL YOUNG”
Michelle Beach, optometrist director at Park Vision Opticians, Nottingham
understanding, Gould explained. He added: “I think empathy is really important. We need to find a way of toning those expectations down and making things realistic.”
Minshull advised explaining to the patient that their vision, even with correction, will never be as good as it was 10 or 15 years ago.
“If you’re managing expectations, and if you over deliver on the lens, patients are happy,” he added. “Before they put the lens on, they’re already primed to know that this isn’t going to be the silver bullet. That’s the key, I think, to multifocal lens fitting.”
Michelle Beach, optometrist director at Park Vision Opticians, noted that, if the patient is a long-term contact lens or varifocal wearer, they are likely to believe that their vision will be the same with a multifocal lens. “They think it’s going to be a varifocal lens they are putting on their eye, but it doesn’t work the same. So, the conversations must be about explaining how that lens works,” she said.
Explaining her own situation – that she can ski, do yoga and walk the dog in the rain in her one-day multifocal contact lenses, but that she cannot work in them – is helpful, Beach said.
The wow factor
Minshull explained that almost all of his patients wear daily disposable contact lenses.
He has been fitting the Total1 for years, and recently fitted his first patient with Total30.
The majority of presbyopic patients will have some level of dry eye, Minshull has found.
Comfort is an important factor, he said, because patients want to wear their lenses all day, “but they are potentially marginal dry eye patients.”
“When we started fitting the Total1 Multifocal, the wow factor with patients was how long they could wear them for. These guys could put them in in the morning and take them out late in the afternoon,” he said.
He highlighted, however, that some patients have trouble with lens removal, so communication around this is vital.
It’s about “guiding them in the right direction,” and providing them with what he believes is the best material on the market, Minshull said.
He added: “It’s super comfortable. Most patients are unaware that they’re actually wearing it, once it is in – they don’t feel the lens.
“It ticks all the boxes there, and that’s why we go predominantly to Total1 multifocal as our first choice of multifocal lens.”
Gould also identified comfort and vision quality as key positives that have stood out in his patients’ experiences of these lenses.
He noted that, when using the slit lamp, practitioners can often see if an eye is very dry –and that this is never the case with the Total1.
“They retain the vision comfort as well as the physical comfort,” he said, adding: “People who have worn other lenses before, who try this product, are always more comfortable with it. It works brilliantly.”
Gould explained that he has not come across a better material in the 11 years that he has been using the Total1 single vision lens, and that the release of the Total30 will increase the choice that he is able to offer his patients.
The improved tear film over the surface of the single vision lens led some patients to believe that their prescription had been changed, Minshull revealed.
“It wasn’t breaking down as quickly as it was with so many other lenses, so the vision was more stable, giving the patient the impression that they had HD vision. It was so much clearer, even though the prescription hadn’t changed,” he said.
Beach, whose practice is 95% daily contact lens-led, agrees that the technology has been well received by patients, but acknowledges that the lens is “slippery.”
“I find the fit is excellent. It’s usually very stable, and it has a wow factor because they really can’t feel it,” she said.
Patients worrying that they might not be able to remove the lens is alleviated by a supportive teach and a buddy system, Beach revealed.
“Once you decide you’re going to wear lenses, you have your contact lens buddy who is your go-to teacher,” she said.
Beach noted that, “when people are wearing the lens, they want to wear it for long periods of time. I do think this is a comfortable lens to wear.”
Chalmers emphasised that adequate chair time and his own confidence in the lens contribute towards a successful fit.
“I feel confident, from the very first time I select the lens for them, in what I’m going to have to offer,” he said.
Minshull revealed that he has a patient who has been waiting for 18 months for the Total30 to come onto the market, and that she is booked in to pick it up the day after our conversation.
“IT’S SUPER COMFORTABLE. MOST PATIENTS ARE UNAWARE THAT THEY’RE ACTUALLY WEARING IT, ONCE IT IS IN – THEY DON’T FEEL THE LENS”
Kieran Minshull, director at LK Leon Opticians, London
“Tomorrow, I’m hoping she leaves the practice singing and dancing. This is the lens she has been waiting for for a long time,” he said.
Chalmers added that “that wow factor is so much the case, all the way through, right from the very start.”
Utilising the practice team for patient education
Gould is currently spending time at the front of his practice, “going back to my roots as a dispensing optician.” It is a position that allows him to have the contact lens conversations that he wants to be having from the beginning of the patient interaction.
Speaking about the practice team, Beach said: “I think it’s really important. Everybody has to talk the same language.”
“PEOPLE WHO HAVE WORN OTHER LENSES BEFORE, WHO TRY THIS PRODUCT, ARE ALWAYS MORE COMFORTABLE WITH IT. IT WORKS BRILLIANTLY”
David Gould, contact lens optician and director at David Gould Opticians, Lancashire
Beach revealed that her presbyopic female patients often struggle to put on their make-up –with some carrying a magnifying mirror with them for this reason.
“I can’t tell you how many patients, with the daily Total1 multifocal, say, ‘Goodness, I can put my makeup on now, and actually know what I look like.’ That is quite life changing for a patient,” she said.
Beach added: “There is a frustration to presbyopia, that you realise hits you as you get older. Not being able to see your face close-up in a mirror is quite big. That’s one thing that they love. It’s freedom.
“To be able to go out without trying to fit your reading glasses in your clutch bag or in your pocket, and to be able to read a menu, makes you feel young, and it makes you feel happy.”
It is about changing the conversation and the communication to being positive around the possibilities than a lens could offer, Beach said.
“There is opportunity for contact lenses with every patient,” she believes.
When it comes to the role of the practice team on the patient contact lens journey, Chalmers highlights the importance of having a point of contact should any issues arise.
That the whole practice team is enthusiastic about lenses from the first point a patient walks into the practice, right to their follow-up appointments, is key, he believes.
“You need to get everybody enthusiastic and on board,” Chalmers said.

TheparticipantsarepaidconsultantsofAlcon,and theiropinionsaretheirown. 0
Watch OT’s video discussion with Kieran, David, Ian and Michelle online, via the QR code. Find out more about Total1 and Total30 online at: www.myalcon.com/uk/professional

The only IPL that treats all Fitzpatrick skin types I-VI
Safety -The only IPL with built-in safety features featuring an adaptive cooling handpiece
Safety -The only IPL providing automatic energy calibration
Patient comfort -No stinging effect and no need for anaesthesia in gel
The Lowest running costs -30,000 light pulses with no on costsproviding 1000 treatments
The smallest most compact footprint of any IPL device. Fit easily into any consulting room
Indications: Thermaeye Plus not only treats Dry Eye Syndrome, but also delivers therapeutic treatments for Rosacea, Telangiectasia, Brown Spots, Wrinkles and Acne.
Differentiate and expand your clinical offering whilst enjoying the biggest clinical return on investment! Contact BiB today to find out more:

Since the pandemic, the pre-visit notification requirement for practitioners providing domiciliary eye care has become increasingly different across the four nations. OT reports
WORDS: EMILY McCORMICK
Statistics in the 2011 UK census reported that there were more than 15.5 million people aged 60 and over living in the UK, accounting for 23% of the population.
As the ageing population of the UK continues to grow, so too does the number of people who may require access to eye care remotely, either in their own home or in a care home. This can be evidenced by the increase in reported domiciliary eye tests, which has risen by more than 80,000 over the last nine years –379,867 domiciliary eye tests were recorded in 2010–11, compared to the most recently available 2019–20 data, which recorded 462,250. Annually,
when compared to all General Ophthalmic Services (GOS) sight tests performed, in 2019–20 domiciliary tests accounted for 3.5%, up from 3.18% in 2010–11.
Despite data suggesting that domiciliary sight tests will continue to rise, up until recently domiciliary eye care providers across all of the UK’s four nations had to provide pre-visit notification (PVN) before they were able to see a patient. These requirements meant that housebound patients could be required to wait between 48 hours and one month for their eye care.
Initially introduced nearly two decades ago, optometrists practising across different nations expressed to OTthey believe the requirements
were introduced to tackle over-testing, during a period where patients were receiving sight tests when they were not eligible.
By providing the required bodies with PVN, it is understood a patient’s eligibility can be checked, and an onsite “surprise” visit on the optometrist could be performed.
Over the years, domiciliary optometrists have navigated slight variations in PVN requirements across the four nations as a result of different bodies governing the verification process. However, when OTspoke to domiciliary optometrists practising across different nations, a common thread was clear: the requirements are (and were) ‘pointless,’ ‘unnecessary,’ ‘restrictive’ and ‘discriminatory.’
“I have spent much of my career fighting this,” domiciliary optometrist, AOP Councillor and co-chair of the Domiciliary Eyecare Committee (DEC), Paul Chapman-Hatchett, told OT.
Nineteen years on, domiciliary optometrists in two of the UK’s four nations are still bound by these requirements.
This is England
Despite requirements falling away formally in Wales and Scotland, in October 2023 and April this year respectively, the requirement for PVN is still in place, and most restrictive said Chapman-Hatchett, in England.
Chapman-Hatchett has spent his career practising as a domiciliary optometrist in England, during which he owned his own domiciliary eye care company, Care Opticians, for 27 years.
Since PVN’s introduction in England in 2005, he has been bound by the requirements, which sees contractors provide Primary Care Support England (PCSE) with a minimum of 48 hours notice (and eight weeks maximum) before performing a sight test on one or two patients at the same address, and a minimum of three weeks notice (and eight weeks maximum) before performing a sight test on more than two people at the same address.
When submitting PVN, contractors in England must provide the patient’s name, address, the approximate time of the appointment, and, if they have it, the date of their last eye exam, chair of the Optical Fees Negotiating Committee (OFNC), Paul Carroll, explained to OT.
They do not receive formal approval after submission; instead, “if they do not hear to the contrary, they can assume it is acceptable for them to make the visit,” Carroll shared.
With a spot check visit being one reason identified as to why PVN was introduced, the OFNC informed OTthat, in England, it has not been able to identify an optometric advisor who has ever conducted such a check. “Anecdotally, including feedback from optometric advisors themselves, we are not aware of any contractors who have ever experienced such spot checks across almost two decades,” Carroll said.
The OFNC believes PVN is unnecessary and has been negotiating with NHS England regarding its removal for some years now. Carroll highlighted: “This is an unnecessary, bureaucratic process which is discriminatory and adds no value.”
He explained: “The simple fact is that an ablebodied person could go to the High Street and


The whole system is completely pointless and serves no purpose, and definitely does not benefit the patient… What we are observing is our most vulnerable patients being penalised for being housebound
Paul Chapman-Hatchett, co-chair of DEC


“
Anecdotally, including feedback from optometric advisors themselves, we are not aware of any contractors who have ever experienced such spot checks across almost two decades
Paul Carroll, OFNC chair
have a sight test today if they have a relevant eye or vision problem. The same service has to be delayed by at least 48 hours if the person cannot leave home unaided because of illness or disability. Although it clearly contravenes the EqualitiesAct, even that does not appear to be sufficient reason to change the requirement for PVNs.”
Chapman-Hatchett agreed, asserting: “The whole system is completely pointless and serves no purpose, and definitely does not benefit the patient. What we are observing is our most vulnerable patients being penalised for being housebound. It is discriminatory to the patient and, as an optometrist wanting to provide eye care, it is devastating.”
“It should be removed altogether,” Specsavers domiciliary clinical director, Dawn Roberts, told OT, highlighting the administrative burden it also places on providers and the NHS.
An important barrier of concern for PVN in England is that it does not allow contractors to see someone urgently, shared
Carroll. From a patient perspective, “a delay of 48 hours, or if you happen to live in a care home and there are two other individuals who also need to be seen quickly, a delay of three weeks, can result in a sight threatening condition going undetected and untreated,” Carroll highlighted.
Chapman-Hatchett pointed out that while optometrists must provide PVN before seeing a patient with, for example sudden change in vision in a care home, there is no such requirement for GPs. “The message it sends to care home managers is that if you can present on the High Street you can get your sight tested immediately because that is a very trustworthy person, but if you need an optometrist to test the vulnerable person that you are caring for, you have to give 48 hours notice as we are not as trustworthy,” he said.
It is also confusing for the patient. “Patients don’t understand why they have to wait. I would explain that it is legislation, but when questioned as to why, I have never been able to explain it,”
Chapman-Hatchett said.
It is not only the patient being penalised by PVN, explained the OFNC. From the practitioner’s perspective, “they are prevented from maintaining efficiency,” Carroll stated.
The OFNC continues to express to NHS England its position that “the requirement for PVNs should be removed.”
Carroll revealed that “a few years back” the OFNC believed it was being heard, only for NHS England to change direction without explanation.
“The OFNC got close to agreeing with NHS England and the Department of Health and Social Care that the requirement should be abolished in England, and we had been promised draft regulations to this effect,” Carroll told OT, explaining it suddenly changed without explanation – “although there was mention of NHS England wishing to reconsider whether there would be any risks in making these changes on safeguarding grounds.”
Unfortunately, progress has subsequently halted. Carroll stressed that the issue remains a priority on the OFNC’s list of issues needing urgent attention “and is not going away.”

“Patient care and equality of treatment are too important for that, especially with an ageing and less mobile population with increasingly complex healthcare needs,” he added.
On 1 April this year, PVN requirements were formally dropped in Scotland. They had been suspended since the

pandemic and were never re-introduced. Talking to OTabout the removal of PVN, domiciliary care representative for Optometry Scotland and optometrist director of Specsavers Fife Home Visits, Mark Gillooly, emphasised that it has put eye care accessibility for care home and day centre residents “on the same level as everyone else.”
“Patients can be seen promptly which, as clinicians, we know can be critical to maintaining ocular health and quality of life for our patients,” he explained, adding: “It removes any distractions from our clinicians so every decision being made is purely in the best interests of the patient.”
Welcoming the end of PVN in Scotland, lead optometrist at Visioncare at Home in Scotland, Gavin Sommerville, is also pleased that patients now experience fewer barriers to accessing domiciliary eye care, while the administrative burden on optometrists is reduced too.
“This might seem like a small technical change, but it really does free up resource and allow us to be adaptable,” he said.
Prior to its removal, PVN in Scotland required domiciliary optometrists to provide their health board with one month’s notice when seeing three or more patients at the same address.
“Each health board had its own procedure for submitting notifications. Some used the NHS standard form, others had their own versions,” shared Sommerville.
“The system was admin heavy and a significant burden,” he added. Gillooly recalls times when due to PVN he had to explain to patients and family members that they had to wait one month to access eye care. “It was often met with confusion and created a sense of uneasiness because there were barriers being imposed which were entirely different to regular practice,” he said.
“ It was often met with confusion and created a sense of uneasiness because there were barriers being imposed which were entirely different to regular practice
Mark Gillooly, representative for Optometry Scotland and optometrist director of Specsavers Fife Home Visits

The first nation to formally remove PVN was Wales, with the introduction of new Wales optometry contract reform on 20 October 2023. Prior to reform, domiciliary providers in Wales were required to provide notice at least 48 hours before a domiciliary visit to one or two patients at a single dwelling, and three weeks’ notice to see three or more patients, optometrist and clinical adviser for Optometry Wales, Sharon Beatty told OT. They could visit sooner in “exceptional circumstances,” with practitioners required to phone NHS Wales Shared Services Partnership to request authorisation.
When consulting with the Welsh Government on the removal of the restrictions as part of reforms, Beatty highlighted that the importance of this change was noted in its consultation response, which highlighted the need to “ensure an equitable level of access and treatment for citizens of Wales who are unable to access services in fixed optometric premises.”
Today, to provide eye care as a mobile service, practitioners are required to have a mobile service agreement with the Health Board aligned to the location/s in which they wish to deliver the service. For Beatty, the introduction of the new rules ensures that “the domiciliary patient enjoys the same flexibility as the person visiting the High Street as to when they can access an eye examination or urgent care.”
On the removal of PVN in Wales, Beatty said: “It has been a positive step forward for both patients and practitioners, supporting equality in access for people who depend on care at home.”

Asked to share her advice for nations seeking change in PVN requirements, Beatty said: “[In Wales] we can’t stress enough how positive this change has been for our patients and our practices. If there is that desire to enact change, we are completely in support.”
FOR OPTOMETRISTS, SPECIALTY
DISPENSING OPTICIANS AND CONTACT LENS OPTICIANS
EXAMS CLOSE: 17 AUGUST 2024
Sponsored by:

This article explores the option of multifocal contact lenses for presbyopic patients, how they work and how to successfully fit them for optimum patient experience.
Dr Fabrizio Zeri PhDIntroduction
At the dawn of this decade, the global population affected by presbyopia (as predicted by Holden et al, 2008) reached a staggering 1.4 billion individuals 1 Presbyopia is an unpleasant condition because one loses some ability to manage the many everyday visual tasks at a near distance that characterise modern societies. Struggling to read a book or a text on their mobile device makes people aware of how precious the automatic and silent mechanism of accommodation is.
Do contact lenses represent an option for presbyopia correction?
Looking at contact lens (CL) market figures, it seems possible that they do represent an option for presbyopic correction, with soft multifocal contact lenses (MFCLs) in a leading position. According to the ContactLensandSolutions SummaryReportpublished annually by Contact Lens Spectrum, in the decade between 2009 and 2019, the number of different MFCLs available in the US market rose by 95% (from 22 to 43) – with increases of 14% and 36% for spherical clear and toric

0.5 CPD POINTS
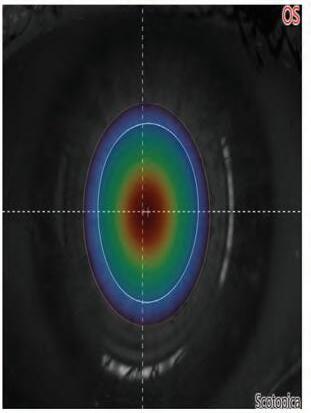
FIGURE 1 Example of the relationship between an entrance pupil of 4.8 mm (scotopic) acquired by a pupillography (A) and the power profile of the optic zone of a centre-near multifocal contact lens (AIR OPTIX Multifocal; high add) (B). Figure 1C shows the overlapping of the optic zone power profile on the entrance pupil (white circle).
Figure 1A is provided courtesy of Dr Fabrizio Zeri. Figures 1B and 1C provided courtesy of Alcon Vision, LLC
50 Multifocal contact lenses in presbyopia correction: what’s on the stage?
53 Enhancing visual clarity for presbyopia with spherical aberration
CLs, respectively;2,3 this reflects the big effort by CL manufacturers to release advances in optical designs and materials to improve performance.
How do multifocal contact lenses work?
MFCLs utilise the simultaneousimage principle: different areas of the optical zone provide simultaneous powers for distance and near correction in the entrance pupil.4 (see Figure 1) MFCLs present a rotationally symmetric change in power from the centre to the edge of the optical zone, modifying the spherical aberration (SA) of the ocular system. There are two main designs to achieve simultaneousimage in CLs (which differ in the way power is distributed): concentric or annular (as in bifocals); and aspheric (with a gradual change of curvature along the surface).5 Furthermore, there are two ways to distribute the distance and near power with respect to the lens centre: centredistance design MFCLs that induce
“ONE LOSES THE ABILITY TO MANAGE THE MANY EVERYDAY VISUAL TASKS AT A NEAR DISTANCE”
positive SA; and centre-near design MFCLs that induce negative SA.5 The induced SA increases the depth of focus (DoF) of the eyes’ system irrespective of the sign (positive or negative) of this change;6 however, the centre-near design is adopted in the majority of MFCLs available on the market.7 Therefore, MFCLs do not restore accommodation but offer a ‘passive’ approach to correcting the accommodation
55 What is vision rehabilitation and what are the priority needs of our patients with sight loss?
60 Freeform single vision lenses: do all patients deserve the best vision?
66 Everyone has a story to tell – implementing expert questioning and listening skills
impairment due to presbyopia, called pseudo-accommodation.8 Pseudoaccommodation (the increase of DoF through SA) also reduces the optical quality of the retinal image at the best focus.6 However, this drawback – which might cause contrast sensitivity loss and fitting failure9 –depends on several factors including: the amount of SA prescribed; the relationship between the different designs of MFCLs; CL centration; and finally, the neuroadaptation of the visual system.
Are there general rules or tips for a successful fitting of multifocal contact lenses?
Looking at the amount of SA prescribed, a simple clinical rule of thumb that can enhance overall MFCL performance is ‘the lower addition, the better’; prescribe the smallest add, which can provide a good DoF, then good reading performance, without sacrificing distance and intermediate vision. Regarding the design, keep in mind that centre-near design MFCLs are more effective when there is a shrinking of pupil size because this cuts the more peripheral areas of the lens – which provide the entrance pupil with the distance power – reducing the superimposition of images.10-12 Therefore, MFCLs work better for higher light levels available during reading and in synergy with the natural pupillary function because during near vision there is a reduction in pupil size in presbyopic people who are not able to accommodate as well as they used to.10-11 Figure 2 describes an example of this mechanism in a young person (see Figure 2A) where the accommodative demand recalls both accommodation and miosis, with the latter also being recalled in a presbyopic person unable to
Optometrists:
Optometrists will be able to outline contact lens options for presbyopia correction to patients
Optometrists will recognise how multifocal lenses work and identify rules and tips to enable successful fitting.
Dispensing opticians:
Dispensing opticians will be able to outline contact lens options for presbyopia correction to patients
Dispensing opticians will recognise how multifocal lenses work and rules and tips that can be used to enable successful fitting.
Contact lens opticians:
0 0 0 0 0 0
Contact lens opticians will be able to outline contact lens options for presbyopia correction to patients
Contact lens opticians will recognise how multifocal lenses work and identify rules and tips to enable successful fitting.

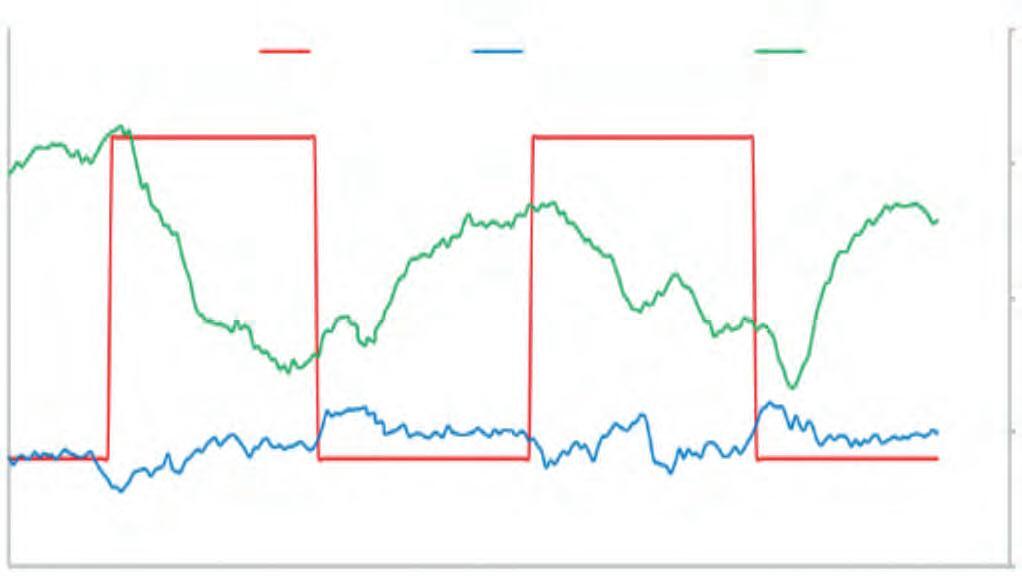
FIGURE 2 Example of accommodative (blue line) and pupillary response (green line) in a 25-year-old female (A) and a 54-year-old male (B) elicited by a stimulus with two cycles of 0-3D accommodation demand (red line), measured by aberrometer (Osiris Aberrometer; CSO, Florence Italy). In the young subject (A) with the onset of accommodative demand it is possible to observe a quick accommodative response of about 2.00 (D) (lag of about 1.00D) and a pupil constriction and the reverse at the accommodative stimulus offset. In the older subject, at the onset of the accommodative demand a negligible accommodation response occurs. However, a pupillary constriction elicited by accommodative demand is still present. Figures2Aand2Bareprovidedcourtesyof DrFabrizioZeri
accommodate (see Figure 2B). In a clinical setting, pupillography can help in understanding the role of the change of pupil size in MFCL functioning (see Figure 1).13 Finally, it has been suggested that overcoming visual disturbances due to multifocal correction may be dependent on neural adaptation;14 this powerful
process, linked to top-down brain mechanisms, can last several weeks. Eye care practitioners (ECPs) should communicate effectively with the patient to explain that they might need time to adapt effectively to MFCLs. Never give up after a few days of wear, and/ or adjusting the prescription too
“ECPs HAVE TO SELECT THE RIGHT DESIGN, PROVIDE THE RIGHT PRESCRIPTION, AND MINIMUM ADDITION ABLE TO GIVE GOOD VISION FOR THE INDIVIDUAL”
soon. ECPs should wait some days before changing the prescription of MFCLs, exactly as they do for spectacles with progressive addition lenses. Furthermore, in the assessment of MFCLs, one should not stop at the results achieved in the consulting room based on visual acuity and contrast sensitivity charts, but always have a look at the performance of MFCLs in everyday life because the needs of individuals may be very different.
On the stage of presbyopia correction, MFCLs represent an important option. ECPs have to select the right design, provide the right prescription, and minimum addition able to give good vision for the individual patient’s needs – and communicate effectively to manage adaptation or cope with possible mistargeting of goals.
The author of this article is a paid consultant for Alcon.
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd


Dr Fabrizio Zeri is a lecturer at the University of Milano-Bicocca and visiting research fellow at Aston University. He has worked in clinical practice for 30 years.
Sponsored by:

This article explores spherical aberrations in aspheric multifocal contact lens design and the positive influence this has on depth of focus for improved visual clarity in presbyopia.
Dr Damien Gatinel MD, PhDIntroduction
Inducing spherical aberration (SA) offers a solution for presbyopia’s effect on hampering the eye’s adaptability to shift its focus, particularly for closeup activities.1 Deliberately expanding the depth of focus (DoF) using SA can achieve clarity for both proximate and distant objects, even when the eye’s natural focusing mechanism is impaired.1
To understand how SA can influence the DoF, it is essential to understand the relationship between aberrations, the point spread function (PSF) and DoF. Let’s delve deeper into the mechanisms involved.
In an ideal optical system, a point source of light would be imaged as a point.
However, imperfections in real optical systems, including the human eye, cause this point source to spread, resulting in a distribution of light, termed the PSF.2 The ocular SA can be modulated by using surfaces of increased asphericity, such as contact lenses,3 intraocular implants,4 or the anterior surface of the cornea after excimer laser remodelling during refractive surgery (see Figure 1).5 The marked variation in the curvature of the highly aspheric surface induces a variation in the local power and a difference in focus between the rays refracted in the centre and the periphery.1 SA specifically changes the shape and characteristics of the PSF. Instead of having a sharp peak, SA causes the PSF to have a more spread-out profile, which plays a role in influencing the DoF.
DoF is the range over which an object can move in depth (closer or further
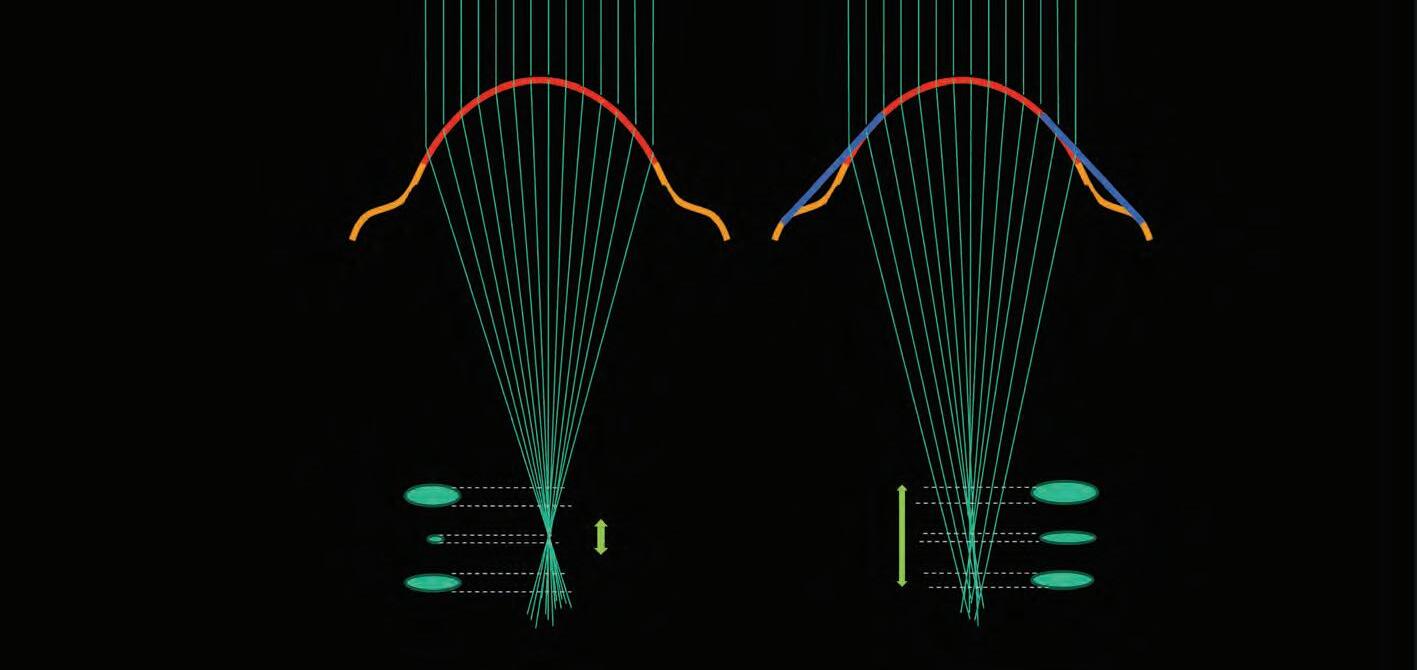
Optometrists and dispensing opticians:
0.5 CPD POINTS
Optometrists and dispensing opticians will recognise how spherical aberrations can be used to influence multifocal contact lens performance.
Contact lens opticians: Contact lens opticians will recognise how spherical aberrations can be used to influence multifocal contact lens performance.
from the optical system) and still produce an image that is acceptably sharp or in focus.6 The relationship between PSF and DoF is critical. When the PSF is sharp and narrow (like in a perfect system), the DoF is generally smaller because any change in the object’s position leads to a noticeable defocus. Conversely,
Vergence map (dioptres)

FIGURE 2 Example of successful surgical correction of presbyopia by increasing negative spherical aberration. The corneal profile is highly prolate (Q=-0.76), inducing negative corneal SA. The vergence map shows the variations of the ocular power (refraction) across the pupil area. Image courtesy of Dr Damien Gatinel
if the PSF is broader, the system has a greater tolerance for object movement without perceived defocus – hence, a larger DoF.
Ocular SA relates to the difference between the refractive power of the centre compared to the edge of the functional pupil;7 the larger this difference, the larger the SA value, regardless of the mathematical function that is used to quantify this aberration. When the refractive power (vergence) is higher at the pupil centre than its periphery, the SA is said to be negative. Conversely, when the refractive power is lower at the pupil centre than its periphery, the SA is said to be positive.1 Regarding refractive power, SA characterises the progressive variation of the refractive power from the centre to the edge of the pupil, independently of these power values.8
There are different methods to modulate the SA rate depending on the clinical context. Multifocal contact lenses (MFCLs) have an aspherical profile that increases the positive SA rate (profile with peripheral addition for near vision) or induces a negative SA rate (profile with central addition for near vision).8 Laser in situ keratomileusis (LASIK) can be used in presbyopes to correct distance vision and increase the DoF, at least for the non-dominant eye.9 Most commonly, negative asphericity is increased to
induce negative SA. Some extended DoF and multifocal refractive intraocular lenses (IOLs) also use these principles to increase the DoF10 and reduce postoperative spectacle dependence.11
Understanding the relationship between SA and the refractive variation throughout the pupil area is crucial in the context of presbyopia compensation using SA. If negative SA increases, the central pupil area should be myopic in local refraction (see Figure 2). Conversely, with positive SA, the pupil centre should have emmetropic refraction surrounded by myopic refraction; this ensures that the extended DoF range via the elongation of the best focus area is clinically useful.
As mentioned, SA modifies the PSF by broadening it. When the human eye is subjected to positive or negative SA (either naturally or induced), it creates a more extended PSF profile.1 This elongation can be advantageous – increasing the DoF.12,13 The broader PSF means the retina can accept a more extensive range of light distributions as ‘in focus.’ As highlighted, this lateral expansion of the PSF stems from the elongation of the useful focal point generated by the refractive system. By adding SA, the focus gets
blurred a bit. While this might sound counterintuitive, this controlled blurring means that small shifts in object position do not lead to noticeable defocus, granting a larger DoF.1
By artificially increasing the DoF through SA, it is possible to make both near and far objects appear in focus even when the eye’s accommodative ability is compromised.1 However, it is a delicate balance. Too much SA (that is to say, difference in refractive power across the pupil) can deteriorate image quality, especially in low light conditions, leading to haloes or reduced contrast sensitivity.12,14 The challenge for clinicians and researchers is to find the right amount of SA that provides enhanced DoF without significantly compromising vision quality.
Medical devices15 and surgical procedures16,17 that use SA modulation to compensate for presbyopia are designed to induce optimal tradeoffs through the use of sophisticated optical models combined with clinical feedback.
The mechanism by which SA increases the DoF hinges on its ability to modify the PSF. By increasing the range of focus and broadening the PSF, SA grants optical systems (like the human eye) a greater tolerance for positional shifts of objects without them going out of focus. This principle is being leveraged in various clinical settings to compensate for presbyopia, aiming to restore a range of clear vision without the constant need for reading glasses.
The author of this article is a paid consultant for Alcon.
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd

Dr Damien Gatinel is head of refractive and anterior segment surgery at the Rothschild Foundation.
Sponsored by:

This article will outline the approach to vision rehabilitation by identifying tasks that are important to patients and help enable independent living.
Dr Jane Macnaughton PhD, FCOptom, Prof Cert LV and Professor Keziah Latham PhD, FCOptom, Prof Cert LVA previous article by the authors (Optometry Today, June/July 2023) described the importance of assessing patients to determine the need for a functional or emotional needs assessment following sight loss.1
The article described the roles and responsibilities of health and social care colleagues working within the sight loss sector and discussed pathways of referral for support, so that practitioners can appropriately advise and signpost patients who have demonstrated a need for further intervention.
With an ageing population, the number of older individuals with vision impairment is set to rise, increasing the pressure on service providers to deliver timely and effective low vision and vision rehabilitation services. To try to reduce the long-term burden on health and social care systems, it is a statutory requirement under the current 2014 Care Act that all local authority or council providers support both the emotional wellbeing and personal independence of people
in need of assistance.2 This article will describe those tasks of daily living considered by patients to be the most important for independent living, together with additional factors that may influence the timeliness of referral for rehabilitation interventions.
Vision rehabilitation is an adaptive process and aims to maintain independence and quality of life by reducing the impact of sight loss while patients come to terms with the associated bereavement or emotional impact; this may involve, for example, learning new skills, or perhaps using previously used skills in a different way, to accomplish day-to-day living activities. Rehabilitation may also involve the optimisation of residual vision with the use of optical and nonoptical devices, appliances, a change in viewing techniques or modifications to the home or work environment. Outlined below are some examples and common approaches to vision rehabilitation.
and mobility techniques
Working with service users (SUs) to increase their confidence in moving
Optometrists and dispensing opticians:
Optometrists and dispensing opticians will be able to identify the priority needs of patients with sight loss relative to their scope of practice
Optometrists and dispensing opticians will recognise when patients with vision impairment require additional support from vision rehabilitation specialists.
around safely both indoors and outdoors in unfamiliar places is a key role for vision rehabilitation specialists; this may include, for example, cane selection and training (see Figure 1, page 56). Mobility canes may be used by SUs to scan their immediate surroundings for obstacles or to find orientation clues. Cane length is measured for each



individual to ensure safety of use. Mobility canes also come with a wide variety of tips depending on the user’s preference. A symbol cane is shorter than other types of cane and is used to make others aware of the user’s vision impairment. A white support stick is designed primarily to offer physical support and stability to someone who has a vision impairment.
The colour of most canes is white to indicate that the user has sight loss. Those who have dual sensory loss may also have the addition of red stripes to signify that the user has an additional hearing impairment. More recently, brightly coloured canes have become available for children to encourage use. However, it is important to be aware that recommended cane choice and training should be provided by vision rehabilitation specialists to ensure correct use of methods and thus improve safety when travelling. Other aspects of mobility training may also include reviewing routes to
work, school or to the shops, learning orientation skills, interpretation of the surrounding environment and the correct use of a distance aid such as a monocular telescope. Trailing techniques or the inclusion of additional lighting and guide rails within the home may also be provided. For those with visual field defects such as hemianopia, mobility and orientation training may also cover more specific scanning techniques.
A significant part of vision rehabilitation is to provide new skills and training to assist in maintaining independence at home; this may
include, for example, alternative approaches to meal preparation or household tasks such as laundry or cleaning. It may also include adopting a change in approach to personal care such as dressing, shaving, or taking medications safely. The rehabilitation team may organise for the instalment of guide rails to help with mobility, or better lighting in the kitchen to help the SU prepare meals safely. For all age groups, vision rehabilitation specialists also provide training on communication and information skills. This support may involve courses on the use of accessibility features available for smartphones, tablets or computers, or the use of tactile systems such as Braille. Communication-skill
“FOR ALL AGES, VISION REHABILITATION SPECIALISTS ALSO PROVIDE TRAINING ON COMMUNICATION AND INFORMATION SKILLS”
development is of particular importance when working with someone who has dual-sensory loss. Examples of assistance to promote independent living are shown in Figure 2
When considering whether or not a patient should be signposted for rehabilitation, there are a number of factors to consider which may impact upon both the need for rehabilitation and the timeliness of referral.
Distance visual acuity (VA) is the strongest measure of clinical visual function affecting the ability to perform tasks of daily living and a reduction in contrast sensitivity is known to impact mobility, face recognition and reading tasks.3,4 A reduction in near visual function, including a loss of central visual field not only impacts patients’ capacity to read but also affects their ability to accomplish many other close work activities such as setting the cooker temperature or checking use-by dates of food products. Loss of central visual field also impacts visual performance using a low vision device.5 Peripheral visual field loss is also associated with orientation and mobility difficulties and a higher risk of falls.6
While clinical measures are important to establish pathological change, it is worth remembering that they are not directly related to how a person responds to that sight loss, and the impact that impairment may have upon their quality of life or emotional health.7 Further discussion with the patient is, therefore, important to establish the need for intervention based upon how they manage functionally, as even those with mild or early vision loss may benefit from referral for support.8 Although older age is a highly significant risk factor for vision loss,9 a higher need for
rehabilitation has been found to be associated with younger age groups.8 The inevitable lifestyle changes and gradual reduction in patterns of daily activity with older age groups may explain the lower rehabilitation need with advancing age.10 It is, therefore, especially important to consider referring younger people for rehabilitation at an early stage in their sight loss.



FIGURE 2 Examples of tactile, colour contrast and auditory stimuli in the home. Brightly coloured raised, tactile markers (‘bump-ons’) assist with dial setting and switches on household appliances (top); brightly coloured rubber bands assist with product identification in the kitchen or bathroom (centre); a liquid level indicator makes an audible noise when pouring liquids (bottom)
Depression or depressive symptoms are a leading cause of disability in the adult population, affecting over 350 million people worldwide.11 Depression is significantly higher in older adults who are living with a chronic health problem or a disability such as irreversible vision loss. The challenges of simple daily living tasks, the inability to recognise familiar faces or the loss of independent mobility from the inevitable loss of driving privileges may lead to social isolation, which in turn may also generate symptoms of depression. Depression may also be associated with symptoms of anxiety12 and there is a general consensus that adult patients may experience both anxiety and depression at the same time.13 Anxiety may be described as a series of emotions characterised by a wide variety of feelings such as tension, nervousness, apprehension and worry, and may be associated with physical symptoms such as increased blood pressure and fatigue. Although symptoms of anxiety are more equivocal and may appear less prevalent than symptoms of depression, both certainly appear to show higher prevalence rates in older adults with a vision impairment.14 Specific symptoms of agoraphobia and social phobia are also prevalent in vision impairment and are likely linked to specific mobility or social situations such as using public transport or dining out.15
Given that there is no significant association between the level of vision loss and depression,16 practitioners are reminded to consider referring patients with symptoms of depression or anxiety for early intervention. However, of course, eye care practitioners are not psychologists. That said, practitioners are well placed to actively ask about the symptoms of depression in relation to the sight loss and functional impairment and thus act accordingly.17 The
National Institute for Health and Care Excellence (NICE) developed recommendations for practitioners working in primary healthcare and general hospital settings.18 When patients present with a past history of depression or a chronic physical health problem with associated functional impairment, practitioners are guided to ask the following two questions:
1 During the past month, have you often been bothered by feeling down, depressed, or hopeless?
2 During the past month, have you often been bothered by having little interest or pleasure in doing things?
If a patient answers ‘yes’ to either of the depression identification questions but the practitioner is not suitably qualified to perform a mental health assessment, they should refer the patient to an appropriate professional. If this professional is not the patient’s general practitioner (GP), then the GP should be informed of the referral. In the case of patients with sight loss, it is not unusual to refer on to the vision rehabilitation specialist, eye clinic liaison officer (ECLO), or patient support service, depending upon the area and local guidance. They may be able to advise on locally placed counselling services to assist those specifically with sight loss.
The development of new skills to compensate for the functional impact of vision loss is also dependent upon the individual’s acceptance of that loss.19 Like depression and anxiety, an individual’s level of acceptance or adjustment to vision loss is not related to any clinical measure such as distance VA, or even to the use of a low vision device;20 however, it is an important factor when considering their need for rehabilitation. The reaction to vision loss is often described as a form of bereavement and acceptance of loss may follow a phase of mourning.21 Adjusting to vision loss may, therefore, be
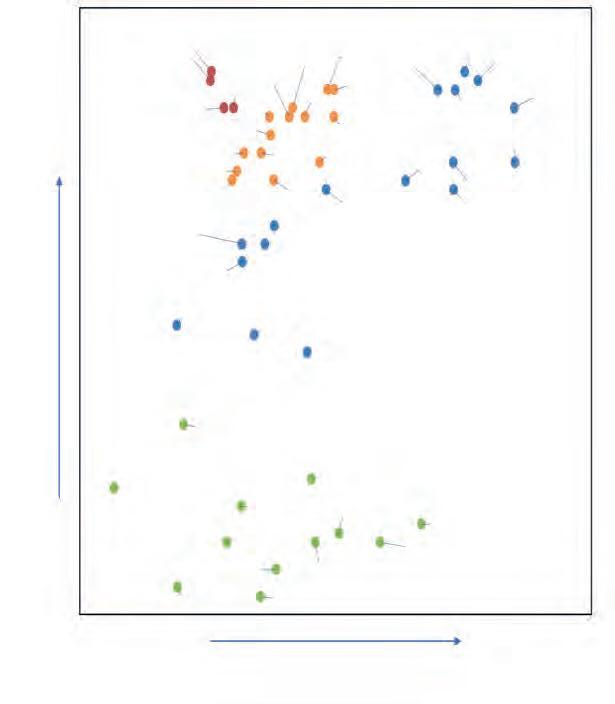
Reading
Mobility out of doors
Mobility indoors, unfamiliar location
Phone Watching TV
Writing Cooking
Post
Cash and card
Bills, admin
Dining out
General shopping
Researching information
Using public transport
Eating and drinking
Personal hygiene
Communication
Cleaning
Keeping a diary
Grocery shopping
Social events
Managing finances
Laundry
Mobility in the home
Emotional life acceptance of visual loss
Fatigue and energy levels
Day trips and holidays
Hobbies and crafts
Using computer or tablet
Interacting with strangers
Driving a car Looking for work
FIGURE 3 Self-reported difficulties with activities of daily living established at the point of entry to rehabilitation services in England. Those on the left are most difficult and those at the top are more relevant to a higher number of people. Those of highest priority are coded red, with orange, blue then green becoming less of a priority for the study sample. ReproducedwithpermissionfromMacnaughtonetal,20198 Relevance to the individual –% of people reporting the importance of each goal
Personal healthcare
Getting dressed
Having visitors
Following the news
Family relationships
Interacting with colleagues
Caring for another adult
Participating in education
independent of the natural challenges of adapting to older age and is a continuous process with potential negative effects upon quality of life and emotional wellbeing that may remain over time.22 In the UK, falls are the most common cause of hospitalisation for people over the age of 65 and the leading cause of death from injury among those over 75, with fractures resulting from falls costing the NHS over £2 bn per year.23 Falls may be defined as ‘an unexpected event in which the participant comes to rest on the ground, floor or lower level.’24 Falls in older people are often multifactorial.
A wide variety of factors such as increased age, impaired mobility, taking multiple medications, a history of falls and vision impairment have all been associated with an increase in falls in older people.25 Vision impairment is estimated to be directly attributable to 10% of the overall cost of all falls in the UK.26 The risk of falls also increases with the level of vision impairment and is high in patients with central vision loss due to age-related macular degeneration (AMD).27 Impaired depth perception and contrast sensitivity are also significant visual risk factors for falls, and a fear of falling may restrict daily living activities in older adults with established sight loss leading to higher levels of depression and anxiety.28
The College of Optometrists has published extensive guidelines for practitioners when examining older patients who may be at risk of falls.24,29 Where a risk of falls appears to be directly related to a vision
impairment, then a referral to the local ECLO or vision rehabilitation specialist is indicated. If the risk of falls appears more related to other factors such as impaired physical mobility, and where an assessment for home modifications or additional walking equipment is required, then referral to the local NHS trust’s falls prevention service is appropriate.
A recent study looked at the rehabilitation needs of adults with vision impairment at the point of referral for vision rehabilitation services in England, and whether these changed at all over the course of a year.8,30 Study participants had vision impairment due to a variety of causes, approximately half of which was AMD. At the point of referral for vision rehabilitation, priority activities were established as reading, mobility and writing (see Figure 3), supporting the need for timely interventions from both vision rehabilitation and low vision services. Addressing activities such as reading and writing are well within the remit of both optometrists and dispensing opticians, and so, a proactive approach to introducing magnification options within primary care is recommended.8 Mobility needs are best addressed by referral to vision rehabilitation specialists. Writing skills have perhaps been less well recognised as a priority need, being frequently coupled together with reading difficulties. While handwriting is a near vision task, the ability to use a pen includes the need for additional strategies including the use of alternative devices or technology to accomplish this task successfully.
The study also found at entry into rehabilitation, activities found to be the most difficult were sewing, undertaking hobbies and DIY. Although reported as difficult, they were not as
“PRACTITIONERS ARE IN A STRONG POSITION TO INITIATE DISCUSSIONS ON THE NEED FOR LOW VISION AND REHABILITATION SERVICES”
important to a large number of people; this may reflect that they are either not common activities or, as they are the most difficult to perform, that they had already been relinquished. Loss of high-valued activities may cause frustration or distress and may be associated with difficulty adjusting to vision loss.19 Therefore, for the practitioner, establishing the impact vision loss has had upon the patient’s high-valued activities and hobbies at an early stage in vision loss is important in managing expectations. It also encourages earlier assistance with compensatory strategies, thus assisting in the adjustment process and may well impact upon quality of life.
In younger age groups, priority rehabilitation needs were found to be in areas relating to independent domestic life, education, employment, and independent travel, which are, understandably, major themes in the transition to adult life.
Over the period of a year, and despite intervention from support services, there remained a perceived need for continued support from both vision rehabilitation and low vision services, particularly for the key goals of reading, writing and mobility;30 therefore, practitioners within all practice environments should establish whether any clinical or functional change has occurred that may indicate a need for review.
Referral pathways were discussed in the authors’ previous article.1 In summary, access to services is variable across the four nations. Practitioners are encouraged to contact the locally placed sight loss advisors through their local eye department for information on the preferred local referral pathway. If a
patient presents in primary care who would benefit from a review of their vision rehabilitation needs, the sight loss advisor may be able to initiate the process. The RNIB’s Sightline Directory provides a comprehensive list of ECLOs across the UK.31 In Scotland, a similar directory of locally based patient support workers can be accessed through Visibility Scotland.32
Eye care practitioners are in a strong position to initiate discussions on the need for low vision and vision rehabilitation services, and also whether there is a need for review. Often, practitioners in the community are the only eye care professionals who may remain in regular contact with our patients; this strongly supports the need to be aware of local service provision, the priority rehabilitation needs of patients and the pathways available to be able to bring them to the attention of colleagues working within the sight loss sector.
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd


Dr Jane Macnaughton is currently a specialist optometrist at University Hospitals of Leicester NHS Trust and a senior lecturer at Anglia Ruskin University.
Professor Keziah Latham is professor of optometry at Anglia Ruskin University, where she leads the Vision & Hearing Sciences Research Centre.
Sponsored by:

This article will consider the clinical advantages of using freeform lenses for single vision wearers.
Eluned Creighton-Sims FBDOMuch attention has been paid to the improvements made in progressive lenses due to the emergence of freeform manufacturing methods and advances in lens design. Considerably less attention appears to be paid to single vision lenses; this is surprising considering that in 2020 around 72% of all lenses sold each year in the UK were in this category.1
Often, single vision freeform lenses are only considered for high prescriptions, or for specific lifestyle needs, rather than being considered as the best solution for all wearers. How many have you recommended this week?
There is nothing more satisfying (yet equally horrifying) to hear a patient say ‘no one has ever told me that before’ when recommending a solution. It could be a 25-year-old who has just been told there is a lens which will make their bingewatching sessions on Netflix more comfortable, or perhaps a 30-year-old mobile hairdresser who has just been told (for the first time in 10 years of spectacle wear) that there is a lens that would enhance their driving experience.
This article will outline why single vision wearers should be given the option to wear a freeform lens design and will give an insight into some of the specialty solutions available for patients.
The primary function of an ophthalmic lens is of course to correct refractive error, thereby enabling people to see clearly. Both conventional and freeform lenses will do this, but a freeform lens can provide, among other benefits, an optimised or enhanced level of clarity; this is easily appreciated in higher powered lenses where the problems of blur in the periphery are a daily inconvenience for the wearer. However, talking to a patient with a relatively low refractive error (for instance, <±2.00DS / <1.50DC) about peripheral blur will likely not resonate and this is not the primary advantage of freeform lenses for them.
The benefits of decreasing peripheral blur for patients are numerous and offering a lens that delivers this is an excellent way to differentiate the practice and enhance the practitioner’s reputation for clinical excellence.
Consider the following prescription:
R 6/7.5 -0.50/-0.25 x 125 6/5
L 6/12 -0.50/-0.75 x 57.5 6/6-1
How many practitioners would you consider recommending a freeform single vision lens in this case? Probably most would not.
This real patient had been experiencing problems since becoming myopic at the age of 34 years. With conventional single vision lenses she reported visual fatigue by late afternoon accompanied by headaches, general ocular discomfort, and dry eye symptoms, which led to her not wearing the correction.
Her lifestyle involves heavy digital device use, often using multiple screens simultaneously and she also drives frequently. A conventionally surfaced anti-fatigue solution gave worse results. How did a freeform lens solve all these issues? We’ll revisit this case later.
If you add up all the input that the human brain receives from each sensory system (eyes, skin, ears, smell and taste), around 11 million bits of information are received every second.2 This is far more information than the brain is capable of processing, with the conscious
mind only able to process around 50 bits per second. The transmission rates of each of the senses (see Table 1) highlights how important the visual system is when gathering information, even if all of the received data is not consciously processed.
While awake, our eyes accumulate data about our surroundings. There are many ways in which our eyes move during this process.3,4 In brief, saccades provide rapid glimpses of the world around us, whether reading a sentence or scanning a room, they allow us to move our line of sight from one point of interest to another in the blink of an eye. Microsaccades, which help keep the visual system active and sensitive to changes in the environment are beyond the scope of this article. Unlike saccades, which are jerky in nature, smooth pursuit movements enable us to track objects effectively using fluid movements. The visual system will employ predictive mechanisms to anticipate the path of motion and
“SACCADES PROVIDE RAPID GLIMPSES OF THE WORLD AROUND US”

guide the eyes accordingly so that the object remains in our field of view. Optokinetic movements are a combination of smooth pursuit and saccadic eye movements. These are used while looking at a moving stimulus that covers a large portion of the visual field, for example, when looking out of a moving vehicle or watching a scrolling display. This smooth tracking of a moving object, with periodical saccades to reposition the eyes should it move too quickly, is how people maintain a stable perception of the world.
Vergence movements are synchronised adjustments which bring objects into focus as they approach or recede. These movements facilitate binocular vision allowing us to perceive depth and distance accurately.
Vestibular movements occur as a result of the brain integrating information from multiple sensory systems at once. It is due to these movements that we can maintain stable vision during head movements by counteracting the motion of the eyes with the motion of the head.
Finally, fixations are those moments when the eyes linger on a point of interest, allowing the brain to process the finer details before the next type of movement is initiated. However, the eyes are never truly stationary due to the
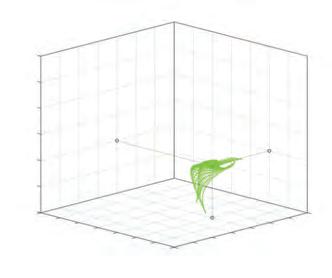
Optometrists and dispensing opticians:
Optometrists and dispensing opticians will be able to explain the benefits of freeform single vision lenses to patients
Optometrists and dispensing opticians will recognise the benefits of freeform single vision lenses.
continual nature of physiological nystagmus resulting in a constant movement of images on the retina.
It is clear that with the variety of eye movements employed by the visual system and the visual demands created by our modern lifestyles that patients use a




large area of their spectacle lenses throughout the day. Therefore, having uninterrupted clear vision is extremely important in ensuring efficient and effective information gathering and processing. The first attempt to provide uninterrupted clear vision came in the early 20th century when Zeiss launched its Punktal (point focus) lens design.5 With frame styles evolving and opticians beginning to deviate from the recommended base curves to provide thinner, more cosmetically appealing lenses, these aberrations were inevitably becoming more noticeable, hence the demand for a solution like Punktal. Using individually calculated curves
to reduce aberrations, this lens design provided an extended field of view. Unfortunately, the cost was substantial in comparison to standard lenses. Table 2 shows the effect of changing the base curve from the manufacturer recommendations. If you currently specify ‘low base, minimum substance’ for any orders, now is the time to stop and either use a more appropriateframe or switch to a freeform design which will allow for deviations from the ideal base curve with minimum negative consequences.
A cloud power plot is used in ophthalmic lens design to give a
graphical representation of perceived powers at different gaze directions (see Figure 1); this enables designers to evaluate how a lens will perform when the wearer views through the periphery. It consists of three axes which represent the spherical power and the cylindrical component, with the target power shown as a black dot. The desired power given as an example in Figure 1 is +3.00/+1.00 x 45. Each green dot represents the power at over 3000 different gaze directions. In this example, the calculations have been performed for this prescription in different designs, made in 1.5 index material with a base curve of 6.00D. Figure 1(a) shows the calculations for a conventionally surfaced lens with power deviations
TABLE 2 Off-axis performance with base curve changes6 (NB recommended curves for +4.00D is 8.50; for -4.00D it is 4.50)
spread over a wide area. In this example, only 11% of gaze directions have powers offering good acuity (less than 5% loss). Around 39% of gaze directions induce blur of greater than 1.00D. In Figure 1(b), the freeform calculated design yields far better results with a maximum blur of 0.89D in the periphery, and overall, around 40% of gaze directions give rise to good acuity – almost four times more than the conventional lens. By comparison, the advanced freeform design in Figure 1(c) provides good acuity in 99.5% of gaze directions.7 Figure 2 shows a visual simulation of the expected performance based on the cloud power plots and theoretical maps for these different lens designs.
While lower prescriptions are subject to lower levels of aberrations, the fact remains that they are still present, which means a significant percentage of gaze directions will induce blur when a conventional lens is worn. Uncorrected refractive errors are known to increase the ocular symptoms associated with digital
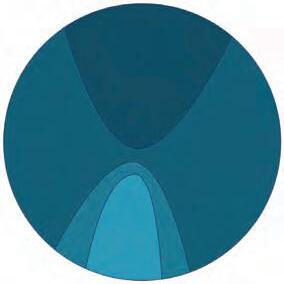

eye strain.8 By inducing even small levels of blur (aberrations) the lens is adding additional stress to the visual system, forcing the wearer to try to compensate for them. Returning to our ‘problem patient’ we can now understand why an advanced freeform solution resolved her complaints. Reducing the aberrations to a negligible level reduced the amount of stress on her eyes, increasing the comfort, not just when using digital devices, but throughout the day. For higher prescriptions, wearers moving from conventional to freeform designs can expect a ‘wow’ factor due to increased clarity throughout the lens. For lower powers, a different ‘wow’ factor occurs, as was the case with this patient – the benefits to her were increased comfort and a marked reduction in symptoms of visual fatigue. It is important to ensure that the right benefits are communicated during the recommendation to correctly manage expectations.
As well as single vision freeform, there are also specialty designs in
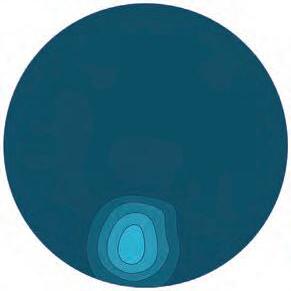

“ANTI-FATIGUE LENSES ARE SUITABLE FOR MANY DIFFERENT TYPES OF PATIENTS – STUDENTS, GAMERS, AS WELL AS THOSE APPROACHING PRESBYOPIA”
this category which are useful for various lifestyle needs. Here we look at some other options for single vision wearers.
Anti-fatigue lenses are suitable for many different types of patients –students, gamers, as well as those approaching presbyopia, depending on the outcome of the lifestyle conversation. Be alert to those patients who watch video content on a television as they are also likely to be using a second screen, typically a mobile phone9 and probably under suboptimal lighting. These people can be good candidates for antifatigue lenses.
Freeform anti-fatigue lenses provide a small increase in power in the lower portion of the lens to give accommodative support. Early generations were based on occupational designs rather than being developed specifically for pre-presbyopes (see Figure 3). This meant that postural comfort and binocular performance could be problematic for some wearers. Modern designs provide a more controlled zone for near which improves binocular vision. Power increases for anti-fatigue lenses vary by manufacturer; it is common to see 0.50D, 0.75D and 1.00D. In fact, some suppliers can adjust this on demand to create bespoke ‘boosts’ in steps of 0.12D. These lenses are particularly beneficial for those who report symptoms of digital eye strain.10 It
“FREEFROM SINGLE VISION DESIGNS HAVE BENEFITS FOR ALL SPECTACLE LENS WEARERS... DOESN’T EVERYONE DESERVE THE OPPORTUNITY TO HAVE THE CLEAREST AND MOST COMFORTABLE VISION?”
should be noted that the study which concluded this used a blue light filter in conjunction with an anti-fatigue design. A systematic review of blue light filters published in 202311 has since questioned the validity of claims that blue-light filters reduce symptoms of visual fatigue from computer screen use.
Myopes can sometimes find antifatigue lenses difficult to tolerate; however, some designs have been developed with their needs in mind, so it is worth clarifying with the supplier if this is the case. Those with poorly compensated exophoria may not tolerate anti-fatigue lenses and instead may prefer a different freeform design.12
It is possible to order a tailored intermediate prescription to use anti-fatigue designs as an occupational lens for presbyopes with the justification that there is reduced unwanted astigmatism and therefore wider fields with this approach. The power distribution of these two designs are poles apart, each being developed with knowledge of wearer behaviour to deliver better vision and more comfortable posture. With this in mind, using anti-fatigue designs as an occupational lens is not advisable for maximum performance.
Driving is one of the most complex tasks we perform on a day-today basis and visual information plays a key role in ensuring that drivers perform well behind the wheel. While there is a weak link between reduced visual acuity and accidents,13,14 research indicates that it can lead to reduced road sign
recognition and hazard avoidance,15 which can impact upon driver performance. While driving, we use our vision to control the vehicle and perform risk assessments.3 Arguably, the most important visual information comes from moving objects located in the driver’s field of view. Perception of these objects and fast decision making on their relevance and whether they warrant more attention, is critical in collision avoidance.3
Eye tracking devices are becoming increasingly popular to assess driver behaviour, and although they have limitations, the research is useful for practitioners and lens designers. One study found that the first saccades when identifying objects of interest while driving had a mean angular distance of 12.6° with a strong skew into the 30° region indicating the importance of peripheral vision in detecting potential hazards.16 Ensuring that patients who drive have optimal correction in this zone is therefore important.
A driving design for prepresbyopes will offer the same benefits as a single vision freeform lens enhancing peripheral performance but some designs go further by including features such as a night myopia zone and coatings specifically developed for driving. These coatings have wavelength cut offs which are more appropriate to the lights encountered while driving under low illumination with some reporting benefits such as reduced ghost images, faster recovery time from dazzle and enhanced contrast under low light.17
Although sports vision is worthy of its own article, it is worth briefly
touching on here as freeform solutions for sport offer additional benefits over their conventional counterparts. Providing excellent peripheral vision for more dynamic sports such as football, shooting and skiing, sports designs also work well for activities that have sustained visual demands such as mountaineering, where troublesome aberrations will increase visual effort. Where a high wrap frame is required, many sports designs will include an additional calculation such as lenticularisation or lenticular blending, which can create a lens with a marked reduction in aberrations even where the base curve significantly departs from the optimum.
Freeform single vision designs have benefits for all spectacle lens wearers. The primary benefit for higher powers is offering the widest possible field of clear vision with fewer head movements required to maintain uninterrupted clear vision. For lower powers, the improved comfort and reduced symptoms of visual fatigue will be the main noticeable improvement. Doesn’t everyone deserve the opportunity to have the clearest and most comfortable vision possible?
0
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd

Eluned ‘Lil’ Creighton-Sims is a dispensing optician and UK manager for IOT Lenses, supporting freeform laboratories in developing their own lens designs.

Sponsored by:

This article outlines the importance of honing questioning and listening skills, as an essential part of the communication process to identify and respond to patient needs.
Peter Greedy BSc (Hons), MCOptom, MACDuring history and symptoms, eye care practitioners (ECPs) have the privilege of listening to a selection of remarkable and sometimes very moving stories –stories of achievement, loss, heartbreak, suffering and pain. Being able to share their story may have been the most helpful aspect of the patient’s time that day. The patient’s story is also a window into their life and provides the practitioner with a wealth of information about their needs, eye health, general health, lifestyle and overall wellbeing. Rushing through a formulaic, check box history and symptoms list can potentially miss important, occasionally lifesaving, information. Engaging with the patient’s story makes all the difference and can create a lifelong connection to the practitioner and their practice.
Listening and questioning: the enablers of storytelling ECPs perform a key healthcare role within the NHS. This role is expanding with schemes for screening, diagnostic and treatment services being delivered in a primary care setting.
People attending for eye care services can be vulnerable, anxious, frightened, hopeful, expectant, impatient, demanding and more. Many have a story of one kind or another. Some want to tell it, others do not, but it may be the key to understanding the origin of vision, eye
health and general health issues; this can start in the reception area, during prescreening, and in the consulting room where the patient has a captive audience in a confidential, safe, space.
Some people start telling the whole practice about all their problems and issues from the moment they walk in. This type of person requires a set of skills and care to ensure they do not dominate the whole environment, occupy the time of too many staff and adversely affect the experience of other patients. At the opposite end of the
spectrum, there are the stoics who say that everything is fine, they have no problems and yet there is an issue that the practitioner can help with.
How people are welcomed and treated has huge consequences for the verbal, behavioural, advisory and fiscal transactions that follow.
The key is listening attentively, asking brave questions, and having the courage and compassion to direct the conversation in the most appropriate way to make an effective connection with the individual.
Listening: neither a soft nor passive skill
Communication is firmly embedded with the General Optical Council (GOC) standards of practice:1
1 Listen to patients and ensure they are at the heart of the decisions made about their care
1.1 Give patients your full attention and allow sufficient time to deal properly with their needs
1.2 Listen to patients and take account of their views, preferences, and concerns, responding honestly and appropriately to their questions.1
Listening is a hard skill to develop that requires active attention, through eye contact, facial expression, body language, vocal (not necessarily verbal) responses and silent pauses. It takes effort.
Stephen Burt, in his 2019 book: The art of listening in coaching and mentoring, 2 suggests there are four modes of listening, each requiring a level of expertise. These modes are attention, inquiry, observation and resonance. While not using the same terminology, all four of these modes are considered in this article.
Mehrabian’s 7–38–55 rule (see Figure 1) asserts that when we are communicating face to face, 55% of our emotions and attitudes are conveyed by body language, with just 7% of the communication coming from the words we speak and the remaining 38% from the tone of our voice.3
How do you ensure your body language is saying: ‘I’m listening’? What are the key areas of body language that need to be considered when communicating face to face in the consulting room, at a dispensing desk or at reception?
Eyes can say all sorts of different things, especially when combined with the rest of the face and can convey kindness, warmth and acceptance, but can also make someone appear disinterested, judgemental, or
suspicious. Eye contact needs to be balanced – insufficient eye contact can suggest lack of attention, but too much can feel intimidating and uncomfortable. Brief eye contact for a few seconds every few seconds is considered ideal, so that it is maintained about 50% of the time. Naturally, taking notes during a consultation means that it is necessary to look at a screen. However, practitioners should ensure they look back and make eye contact, and if necessary, ask the patient to pause while making notes to demonstrate that careful attention is being given by capturing valuable information.
Smile! A warm, welcoming, open, kind, non-judgemental smile is important. Even a simple emoji can say a lot, so how much more does the human face convey?
Gesticulation is expressive. Although these actions are often associated with speaking, they can also express openness and receptivity while listening. Once notes have been captured, hands should be taken away from the keyboard to adopt an open position, taking care to avoid folded arms.
The ergonomics of the consulting room can mean that the computer screen is in a position where the practitioner is sat at right angles to the patient, and therefore, facing away from them. Where possible, the workstation should be set up so that notes can be taken while still being attentive to the patient. Of course, there is other equipment that must be close by, so it is important to bear all these factors in mind when setting up the space. Facing the client as much as possible and minimising the time spent facing the screen is important for patient perception. What is more important, the patient or the screen?
Active listening is the art of listening to, and understanding what, a person is saying, both verbally and nonverbally by tuning in to the three Mehrabian modes by which we communicate:
• What do the words mean?
Optometrists and dispensing opticians:
Optometrists and dispensing opticians will recognise the importance of honing questioning and listening skills to identify and respond to patient needs.
• What does the tone of voice say about the feelings behind the words?
• How does body language support or contradict what the person is saying? This all takes work, and active listening is a way to communicate understanding back to the speaker. Simple things that can be done to reassure the person that is speaking is being listened to includes:
• Nodding
• Adding an occasional, gentle ‘ah, ok’
• At an appropriate moment summarise back to the speaker the understanding of what they just said. For example, ‘Ah, so what you’re saying is that you…’. For signs and symptoms, this can be crucial to aid differential diagnosis, so it is important to get it right.
What is the story behind the story?
Referring back to the General Optical Council (GOC) standards of practice, it is important for practitioners to: 2.3 Be alert to unspoken signals which could indicate a patient’s
lack of understanding, discomfort, or reluctance to consent.1
What is the patient thinking? There will be times when what is said is not what is meant. People may lack the vocabulary or ability to accurately describe what they have been experiencing. Clarifying questions is particularly important. For example, a follow-up question could be along the lines of:
‘You mentioned you have been getting headaches. It would help to know a bit more about them. How often you get them? When do they usually occur? Are they at the front around your eyes or elsewhere?’
What feelings and emotions are the patient portraying? Losing one’s sight can be very scary and emotional for a lot of people. Empathising with the emotional state of the patient is a real superpower for building trust and loyalty. If they become emotional, pause. Let them process the emotions. Offer a tissue and a glass of water.
What does your intuition tell you about what is being said? Is there something going on that they are not telling you? A potential follow-up question could be: ‘You mentioned the headaches are worse with the anxiety you are experiencing. Is there more you would like to say about that?’
The familiar quote from the Greek philosopher Epictetus ‘We have two ears and one mouth so that we can listen twice as much as we speak’ is particularly good to keep at the forefront of the mind when trying to understand what patients are saying. Like listening, what is asked can be less important than how it is asked.
Consider when it is appropriate to ask closed or open questions. A closed
“TAKING GREAT HISTORY AND SYMPTOMS IS THE OPPORTUNITY FOR PRACTITIONERS TO GET TO KNOW THEIR PATIENTS”
question is one that has a brief, usually binary, answer – most often yes or no. Do you have headaches? Is your vision blurred? Do you take any medication? Do you drive? These types of questions have their place, and often will be followed up with clarifying questions: Do you take any medications? Yes. What do you take them for? How long have you been on them? Do you know the names of the tablets? Closed questions are effective for information gathering but they do little for relationship building and overall understanding of the patient. An open question is one that encourages longer answers and can start a dialogue. They are great for building rapport with the person and understanding their story, including their vision, health concerns and requirements. Useful phrases to start open questions: Can you describe…? How would you describe…? Can you tell me a bit more about…? As the rapport builds the patient will often start to open up, especially when they feel they are being listened to.
Silent pauses can be awkward for some people. However, a considered response to a great question may need time to be formulated. Do not rush to repeat the question or ask another question as this will interrupt the person’s train of thought, potentially losing the chance to capture a vital piece of information. Be patient.
By actively listening to the answers the patient gives, the head, heart or gut may indicate that a true or full answer was not given and could be because the original question was framed inadequately. For example, asking the question ‘How is your general health?’ might elicit the common response of
‘Fine,’ which may be neither true nor complete. They may be on multiple medications for hypertension, type 2 diabetes, hypercholesterolaemia, anxiety and more. In the patient’s mind, they may consider that because they are on medication for these conditions, that they are ‘Fine.’ To avoid this, consider phrasing the question differently. For instance, ‘Can you tell me about your general health and any conditions you are taking medication for?’ This can lead to a lengthy list of conditions being reported leading to a more detailed conversation about health.
It takes practice to develop the skill to ask great questions. Take time to write out a few well-crafted questions and practice them in other conversations. It can be surprising how friends and family will notice this more caring and interested approach.
Taking great history and symptoms is the opportunity for practitioners to get to know their patients. It provides a safe place for patients to tell their story and give the fullest understanding of their vision, health and lifestyle needs and wants; this allows the practitioner to provide the best care, services and products, grow a loyal base of patients and establish a reputation as a goldstandard healthcare provider.
0
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd

Peter Greedy is an optometrist and coach with over 35 years experience of professional and leadership roles in primary healthcare.
 EDITED BY KIMBERLEY YOUNG
EDITED BY KIMBERLEY YOUNG
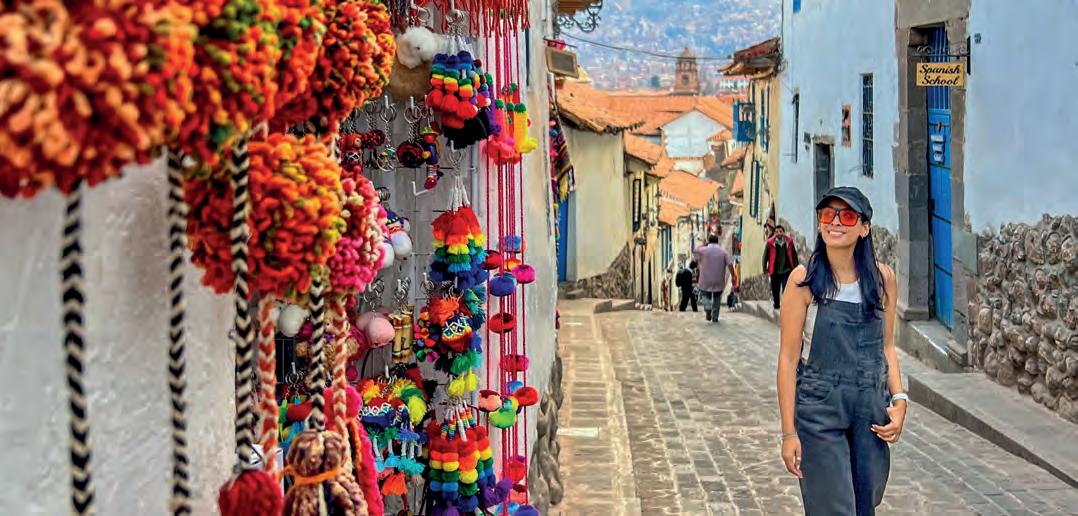


OT rounds up the latest in lenses and coatings
To feature in OT’s What’s happening pages, contact: kimberleyyoung@optometry.co.uk

TheNEWfree-to-use CooperVisionOptiStudenf· app is designedto put valuable,curatedeye care contentinto the handsof opticalstudentsprovidinga videolibraryof high-qualitycontent acrosskeyareas.
Throughthe app,studentscanalsoenter the CooperVisionOptiStudent™Awardsan annualcompetitionthat celebrates opticalstudentsfrom acrossEurope.
Eyewear for athletes, cartoon campaigns, formulas for dry eye, and practice support


1 Ace designs SUNGLASSES
Oliver Peoples and Roger Federer have released the first eyewear collection in their partnership, which includes six styles.The lightweight frames feature rubber grip nose pads and end tips to support fit for performance wear. Special features include references to Federer’s number of Wimbledon titles, and patterns mimicking details of tennis rackets. essilorluxottica.com


2
Dry eye support DROPS
TheBodyDoctorhas launchedTheEyeDoctor AdvancedTripleActionEye Drops,featuringan advancedmicroemulsion lipid-basedformulafor treatingandpreventing symptomsofmoderateto severedryeye. the-body-doctor.com


3
Cartoon fun CHILDREN
Entia Barcelona’s Kids Spring/Summer 2024
Cartoon Collection sees frames in fun shapes and bright colours. Models are named after the expressive language of comics including: ‘BOOOOM!,’ and ‘KA-POOOW!’ etniabarcelona.com
4
Eyewear for athletes SPORTS
Red Bull SPECTEyewear highlighted its Wing system to support better grip. A slider on the arms enables a second, curved metal element to be extended, which can be shaped around the ear for a secure fit.The technology was tested by Red Bull athletes.
mpg-eyewear.com

5 In the cloud PRACTICE MANAGEMENT
Optinethaslaunchedits newcloud-basedpractice managementsoftware: Nova.Cloudintegration enablesuserstoaccessthe platformfromanylocation ordevice.

optinetuk.com

OT gathers launches from photochromic designs, to myopia management in the sunshine

Transitions Optical has launched theTransitions Gen S photochromic lens in the UK.The lens reaches category three levels of darkness in 25 seconds and fades back in less than two minutes.
transitionsPRO.com





ColorMatic X, its fastest and clearest photochromic lens. Featuring ColorMatic CompoundTechnology, the lens fades 54% faster than the previous generation of lenses. rodenstock.com
Nikon Lenswear UK has launched the SeeCoat Next Reveal, SeeCoat Next Drive, and SeeCoat Next Blue lens coatings.The new coatings bring together Nikon’s technologies for clarity and durability, “no matter the wearer’s lifestyle.”The SeeCoat Next Reveal lens features Light Purification and Contrast Boost technologies for enhanced protection and colour perception. nikonlenswear.com/uk
Essilor has launched its Stellest lenses with sun tints, encouraging children and teenagers to continue wearing the spectacle lenses outdoors, while offering protection from sunlight.The lenses will be available in a range of colours and will also feature Crizal Sun XProtect coating. ecp.essilor-pro.com/gb
Caledonian Optical has showcased the Neochromes lenses that darken “within seconds” and fade back within minutes at standard room temperature.The lenses, available in brown and grey, also protect against UVA and UVB. caledonianoptical.com


References:
The creator of the Curious Pixie travel blog, told OT about her collection of sunglasses



I can never have enough sunglasses: I have eight pairs and a pair of spectacles. Even though I love my bright coloured sunglasses, my favourite is a pair of beige Chanel ones. A classic square shape, they go with everything and are so timeless and chic. That’s probably why I’ve had them for so long.
With a long face I find that square frames suit me better. The sharp corners help balance out the length of my face. In terms of colours – anything goes. One of my go-to pairs at the moment is a large black square frame with orange lenses. When I wear them it’s like seeing the world with a permanent ‘happy’ filter.

Pairs of glasses: eight
Eyewear icon: Audrey Hepburn
Having good eye health is crucial. My eyes have deteriorated with age and now I always keep up with regular eye check-ups as any changes to your eyes can signal so many other underlying health problems. It’s essential to stay on top of it.
I didn’t start wearing spectacles until recently. The ageing process comes for us all. My prescription isn’t actually that strong, but I started suffering from a lot of headaches so now have a pair of varifocals, which have really helped when I’m pouring over my laptop or mobile for work.They also help me to see the flight board at airports so I don’t miss my connections.
Sima was recognised in the bCreator influencer and creator awards for her travel content in 2023
Anything I wear is a reflection of my personality and my individual style. My eyewear absolutely has to suit my mood on the day. Being a full-time travel content creator, I feature in a lot of content on my website and across my social media platforms – so sunglasses when I’m on my travels are always the finishing touch to any outfit.

Celebrating its 10th anniversary, Dick Moby has introduced a limited collection crafted from its surplus stock – repurposing materials into never-to-be-repeated colour schemes.
dick-moby.com






Ultra-thin, elegant, compact and lightweight, yet just as avant-garde as the main collection, styles in Gigi Studios’ new XS line are specially designed for narrow faces. gigistudios.com



New for summer 2024, Blumarine’s ‘SBM216’ has a sensuously wide wraparound design in gold-tone. Additional style details include the brand’s signature ‘B’ monogram. blumarine.com



Optometrist and lifestyle blogger, Lizzy Yeowart, on the styles inspired by Japanese design. See more from Lizzy on her Instagram page at @WHATLIZZYLOVES
‘Pakobra’ Vasuma
Emphasising craftsmanship, Stockholm-based brand, Vasuma, offers a Japanese collection, manufactured with a small family business in Fukui. tradersandmakers.com

‘M3023-V2,’ Matsuda

Lizzy's top frame picks this edition
When it comes to optical manufacturing, Japan is one of the world’s top manufacturing hotbeds for eyewear, with only Italy and China ahead. These eyewear brands have their finger firmly on the fashion pulse and are keeping things interesting with inspiring, stylish products.

The ‘M3023-V2’ is a reimagined aviator fashioned from a harmonious fusion of Japanese acetate and high-grade titanium with semi-flat sun lenses. matsuda.com

‘Pleats,’ Face a Face
A new palette inspired by Japanese craftsmanship permeates and enhances the curves of the models in the latest collection by Face a Face. Think turquoise to indigo blue, via yuzu green and magenta. faceaface-paris.com






How would you describe Optopol’s growth in the UK?
Optical CoherenceTomography (OCT) has become a must-have device in every practice, but what is especially important for the UK market is that the unit has to be equipped with a fundus camera. Since 2019, when we launched Revo FC, which combines the OCTwith a fundus camera, our average growth of sales in the UK is 60% per year. The UK is the fastest growing European market for Optopol. Such a great success would not be possible without our UK partner BIB Ophthalmic Instruments.
How does the UK market differ from Europe?
The UK market is undoubtedly a rapid growth opportunity sector for OCT manufacturers who can provide OCT producing very high-quality tomograms combined with speed and ease of use.The Optopol Revo series meets these criteria nicely, hence our rapid growth. Plus, we offer additional software modules such as OCT-A,


OCT-B and topography, some of which are unique when combined with the OCT. It’s important to note that the way in which the UK market is structured is quite unique, whereby both optometrists in primary care, as well as hospital eye departments and private ophthalmology clinics, can all use and benefit from OCT.The rest of Europe is very different, where in the main, it is only the ophthalmology sector that can perform clinical diagnostic tests such as OCT.
How do you see technologies such as artificial intelligence (AI) affecting OCT? We take the AI revolution very seriously. A few years ago we created the AI Software Division headed by Professor Krzysztof Krawiec from Poznan University of Technology. Our current OCTsoftware is already using AI support. We will shortly be releasing a module that enables retina segmentation using AI algorithms. I’m sure in the future AI will be widely used in OCTsoftware.
Three facts about Optopol Technology
OptopolTechnology was founded by Adam Bogdani, and is now run by his son, Marcin Bogdani
The company commercialised the first spectral domain OCTin 2006
Optopol is based in Zawiercie, a town in the Silesia region of Poland.
Manufacturers in lenses and contact lenses share key elements to cover in myopia management consultations

Nicky Latham, professional affairs lead for myopia management at CooperVision, emphasised the need for clear communication: “Parents, including those without myopia, must grasp the condition’s implications and how it can worsen over time.”
The value of early intervention and prompt action is an important conversation to have in the consulting room. She said: “It’s essential to realise that while interventions can slow down the worsening of myopia, they cannot reverse it.”
Latham pointed out that evidence demonstrates some myopia management interventions, such as the MiSight 1 day, work for as long as the eyes are growing.
“Parents should therefore be counselled to anticipate keeping their child in myopia management for as long as the eyes are changing,” she said.
In discussing this, Latham recommended educating patients and parents that, even during a myopia management treatment, a change in prescription can occur, adding: “Myopia management slows the worsening of myopia, rather than stopping it or reversing it.”
Abiding by the recommended wear times is a necessary conversation.
“Treatment is dose-dependant, so adherence with the recommended wear times for the selected product is highly correlated with increased myopia control
efficacy,” Latham said, adding: “Eye care professionals and families need to consider the required minimum wear time for myopia management spectacles or contact lenses, and how achievable this will be with the child’s weekly routine of activities.”
CooperVision has created a myopia management tear pad which can be a useful way to plot the patient’s prescription.
Latham explained: “This indicates whether the child is at risk of myopia and its associated ocular health problems later in life. Other resources and online tools also exist to support with conversations about healthy eye growth, such as the Predicting Myopia Onset and Progression Risk Indicator tool, which is open access.”
Risk levels of myopia
Fabio Carta, global professional services manager for the myopia management business division at Menicon, suggested explaining the factors influencing a child’s risk of developing myopia.
This could include explaining how the level of refractive error deemed as normal for a patient would be influenced by ethnicity, or parental levels of myopia.
“The presence of myopia in one parent increases the risk of myopia in the child. That risk further increases if both parents are myopic. Even if both parents are nonmyopic, their child may still develop myopia,” Carta said.
When it comes to discussing the healthy growth of the eye within myopia management, Carta suggested a number of different steps for children of different ages and at different stages of myopia.
This begins with encouraging pre-school age children to attend an eye exam, and emphasising the importance of follow-ups, particularly for children at an increased risk.
Advice for parents and families should include lifestyle factors, such as explaining the 20–20 principle or spending time outdoors, with Carta suggesting: “A minimum of two hours per day of outdoor activity at any point during the day, including school time.”
Andy Sanders, professional services director at Hoya Lens UK, commented: “When you talk about myopia, some people know what it is, whereas others don’t know what short
Myopia management: resources from OTand the AOP
Dr Ian Beasley, head of education at the AOP and OTclinical editor, commented: “The AOP’s myopia management resources are designed to support practitioners in making evidence-based clinical decisions on a case-by-case basis, while also guiding patients through an informed consent process.”
Find the AOP’s myopia management resources online: www.aop.org.uk/advice-and-support
On 12 May, OT in partnership with the AOP and headline sponsor, CooperVision, hosted a day of myopia-focused education. Watch the MAYopia webinar recordings at: www.optometry.co.uk/webinars
sightedness is. So, it is important to use both terms and ensure understanding.”
Providing a demonstration of what a child’s prescription is like can be helpful to show the impact of myopia on vision, along with utilising visual tools to illustrate how the child’s vision is predicted to change with and without an intervention.
Discussing myopia management in terms of ocular health can be a helpful approach, particularly for younger children who might be high myopes.
“Long-term, we need to start talking to them about the potential pathology,” Sanders suggested, adding: “You might say to the parents, ‘Your child’s vision is healthy now and we want to keep it that way. By slowing the worsening or progression of myopia, we want to reduce the end point prescription which, in turn, can improve quality of life and reduce the risk of eye health problems. In a nutshell, we want them to have the best possible future life and keep their vision healthy.’”
“When we talk about myopia management, we are supporting natural eye growth,” he said.
Consent is a crucial component of the myopia management conversation.
Sanders emphasised the role of compliance, suggesting: “You need to have the discussion with both the child and the parent, putting the child at the heart of the decision of what they would really like. This may be different to what the parent thinks the child wants or needs, but there is no point giving the child an intervention if they are not going to wear it. Compliance is key to any of these interventions, and that’s why I think we sometimes get more progression than we would expect.”
“Compliance is key to any of these interventions”
Andy Sanders, professional services director, Hoya Lens UK

At Newmedica, we choose to use the highest quality cataract replacement lenses for the best clinical outcomes. In fact, our monofocal lens for NHS patients has the lowest PCO rate of any lens on the market at 3 and 5 years. It's hydrophobic and is specially designed to reduce the need for YAGsurgery*.
Which is great news for your patients and the NHS,and peace of mind for you.
*source : The Royal College of Ophthalmologists, National Ophthalmology Database "Feasibility Study of Post-Cataract Posterior Capsule Opacification" May 2021


CI COULDN’T LIVE WITHOUT…
Karen Gennard, optometrist at Norville Independent Eyecare, on an ICB-commissioned software that is revolutionising digital image sharing
ommunityOphthalmicLinkisadirect linkintotheophthalmologyrecordsof the hospitalswithinGloucestershireHospitals NHSFoundationTrust.Itallowscommunity optometriststoseeanyimagingapatienthashad done–topography,opticalcoherencetomography scans,orvisualfields.WealsohaveaccesstoGP letters,andanythingelsethatiselectronically stored.Itbringstheimagingtogetherinoneplace, meaningyoucansearchbyrighteyeorlefteye,by equipment,orbybringingupalltheHeidelberg images,forexample.Youcanalsosearchbydate,so youcanfindwhatyou’relookingforeasily.
InGloucestershire,wehavehadCommunity OphthalmicLinkforaround18months.The integratedcareboard(ICB)piloteditinafew practices,thenrolleditoutquitequickly.Now,most optometrypracticesinGloucestershireandmost practitionershaveaccesstoit.
Thesoftwarehadanimpactonourpractice straightaway.Everythingisononeplatform,and youcanseeitinreal-time.Youdon’thavetosearch separatelyfortheHeidelbergimaging,thenthe keratometerimaging,thentheHumphreyimaging. Youcanpullupallthefieldresults,oralltheGP letters,foraparticularpatient.
ThefirstpersonIcheckedwasmydad,whohas diabeticretinopathy.Icouldbringupallhisimages, andallhisletters,straightaway.
Itgivesyourealconfidence,butalso,it’saneasy interfacetousewiththepatient.Youcanbesitting withthepatient,askif theyarehappyforyouto lookattheirhospitalophthalmologyrecords,and thenbringthemupimmediately.It’sgreatfroma patientperspective,becauseyoucanshowthem thatyou’vegotthatlinkedconnectivityandthatthe communicationisthere.
Also,theycanseethingsinreal-time.If you’ve donesomeimaginginthepractice,andyouwant toshowthemthatsomethingisthesameasitwas whentheywenttothehospitaltwoyearsago,itis easytodothat.
BeforeCommunityOphthalmicLink,we’dstruggled foralotof years.Optometristsaregenerallythe primaryreferrerintothehospitaleyeservice,but becauseof howthehospitalsystemwassetup, ophthalmologyletterswentstraightbacktotheGP. Unlesssomebodyintheophthalmologydepartment askedthepatientwhotheiroptometristwasand putthosedetailsin,theydidn’tcomebacktous.So, havingaccesstothoseGPletters,goingbackyears, isfantastic.
Wearea10-minutewalkfromthehospital.We havehadpatientswhohavebeeninclinicandhave cometoseeusafterwards,andwithinthetime they’vewalkedtothepracticetheinformationis there.Fromapatient’sperspective,Ithinkitmakes ahugedifference.
Getty/Orbon"This a great job for optometrists to provide that clinical excellence, to make sure your patients receive the best possible care. This is the job that you signed up for when filling out your UCAS form"
Tom Critchley,PrincipalOptometrist,SpaMedica
Do you have a passionfor patient care and strive for clinical excellence?You could be the perfect fit for our growingteam of talented optometrists.
• Great work life balance - Only 1 in 4 Saturdays
• Continuoustraining and development
• Biannualbonuses

HSOC returns for 2024, and with double the capacity of last year’s event, Dr Ian Beasley, head of education at the AOP and OTclinical editor, shares what attendees can expect

After a three-year hiatus, 2023 saw the welcome return of the Hospital and Specialty Optometrists Conference (HSOC) to a face-toface setting. As the AOP team set about planning for last year’s event, it was challenging to predict the willingness of practitioners to leave the comfort of ‘learning by Zoom’ and venturing back to a ‘real’ conference. We need not have worried – the event sold out in record time, and it was clear from post-event feedback that delegates relished the opportunity to come together to learn, network (and party a little) with their friends and colleagues.
Bookings for the event open in June
Event takes place Saturday 21–Sunday 22 September, at Emirates Old Trafford, Manchester Delegates can earn over 18 interactive CPD points including peer reviews for general and specialty (AS/SP/IP) optometrists.
decision to extend the invitation for specialty optometrists working in the community to attend the conference, providing a platform for primary and secondary care colleagues to foster collaboration and share key learnings.
The 2024 event will take place on 21–22 September in Manchester, offering an accessible location to delegates from all four nations. The extensive two-day programme of education will provide a mix of lectures, short paper sessions, discussion workshops and numerous peer review sessions.
NAME: Dr Ian Beasley ROLE: Head of education at the AOP and OT clinical editorSo, with the success of 2023 in the back pocket, the team has been able to plan for a much bigger event in 2024, increasing capacity by over 50%. Another triumph to carry forward to 2024, is the
The main lecture programme will explore a diverse range of topics such as eye disease
The main lecture programme will a such as eye disease



“I am delighted that the Committee and the AOP are working together again to deliver this year’s conference. In 2024 we have a larger conference, building on the success of last year. We will be showcasing lectures, workshops, peer discussions, and hands-on practical stations, covering all areas of specialist practice including glaucoma, medical retina, and medical contact lenses, in a format directed at those undertaking advanced practice within these subspecialities, as well as those who are just starting out within these fields. I look forward to welcoming you all back to this year’s conference, so spread the word to colleagues.”
and visual hallucinations, and entrustable professional activities, while retaining the longheld tradition of hosting a memorial lecture. In response to demand seen in 2023, capacity for short paper sessions will be doubled, enabling practitioners to share empirical research findings with their peers.
In addition to the main lectures, delegates will be able to build their own programme by selecting their preferred sessions from five distinct content streams including anterior eye, contact lenses, glaucoma, medical retina and general optometry. Within the streams, some content will be pitched at an advanced level for practitioners with subspecialties, whereas others will deliver at a more accessible level for those without extensive experience in the clinical area.
Practitioners attending across the weekend have the opportunity to accrue over 18 interactive CPD points, covering core and specialty domains.
Alongside education, delegates will also have ample opportunity to meet a range of exhibitors who will be showcasing their latest products and innovations. And of course, the conference would not be complete without the gala dinner on the Saturday night, where dancing is not mandatory, but certainly encouraged.
-
For more details on the conference, and booking details, visit www.aop.org.uk/events
A review of AOP activity in the last two months

The AOP’s campaign featured in a news broadcast across seven ITV regional networks with AOP Councillor and Board member, Nizz Sabir, and AOP member, Dermot Keogh, interviewed about the role community optometry can play in reducing the waiting lists.
http://bit.ly/3UQqXYp

Education highlights
OT, in partnership with the AOP, delivered two days of themed education with Paediatrics Day and MAYopia Day 2024, the latter delivered with support from headline sponsor, CooperVision.
www.optometry.co.uk/cpd/ education-library


Locum wellbeing a focus
The latest in OT’slocum guides, delivered in partnership with Johnson & Johnson, is focused on maintaining wellbeing as a locum optometrist. Read the series in full online.
www.optometry.co.uk/locumoptometrist-guide
Onemillionappointments Summer
The latest AOP campaign highlights the mounting pressure on GPs, and how optometry patient pathways can help. Find out more at: www.aop.org.uk/our-voice/campaigns
AOP student reps Summer
The AOP’s latest cohort of student representatives from optometry schools across the country will be announced.
New AOP Councillors welcomed June
With the results of the AOP Council elections announced, look out for interviews with new AOP Councillors in the August/September edition of OT
Pixabay/200 Degrees Pixabay/LukasTrivedi,

“ The pandemic forced our hand and we had to explore and start to deliver care remotely as there was simply no other way of surviving, delivering eye care and keeping in touch with our patients
As an IP optometrist, I first encountered remote care during the pandemic. For me, remote care is a clinical care episode that’s delivered to a patient and/or client by way of something other than a traditional face-to-face in-practice consultation. It could be delivered partly or entirely remotely. It can also be delivered through a multitude of methods, such as online, or via the telephone. It’s about finding the right method of delivery for eye care that is most appropriate for that interaction at that time. Remote care really came to the fore during the pandemic. In the constraints of early COVID-19, we had to look at other methods of delivering care. We had to also make sure that we took steps to mitigate the risks with triage, and that we were prioritising patients appropriately when, in those early days, we were only seeing the emergency and the urgent patients. Initially it was really difficult, but as a profession the pandemic forced our hand and we had to explore and start to deliver care remotely as there was simply no other way of surviving, delivering eye care and keeping in touch with our patients. It’s horrible to think that anything good came out of COVID-19, but there have been some positives. One learning is that it’s shown the profession that we can deliver care to patients in different ways, and that it is possible to deliver some elements of care, when and where appropriate, on a remote basis. For me, remote care is a positive as it can remove a barrier that some patients might face when trying to access healthcare. The pandemic improved our comfort levels as clinicians in providing remote care. It also improved the level of comfort of our patients in this space. When it comes to remote care in the future, overall, I would like to see it being used appropriately for those cases where it’s safe to do so. I don’t think it’s ever going to be a case of one-size-fits-all. But I do think there will always be a case and a category of patient where, depending on what they’re there for, it will be suitable. However, we should remember that when using remote care, we do need to make sure that we’re managing and mitigating the risks appropriately – that we’re giving good advice around escalation and red flags, and recording conversations appropriately.
0
1 You had me at hospital
Learn what it is like to practise in a hospital optometry setting PAGE 28
ANKUR’S TOP READS
2 IP and me
Clinical scenarios explored by three IP optometrists, including me PAGE 34
3
Supplier insight
Advice on managing expectations around myopia interventions in practice PAGE 82
Sight Test Minimum Intervals

Patient is at risk of frequent changes of prescription for reasons not requiring medical referral or for reasons already known to a medical practitioner.
Patient has pathology likely to worsen, for example age-related macular degeneration, cataract, corneal dystrophy or congenital anomalies.
Patient has presented with symptoms or concerns requiring ophthalmic Investigation resulting in referral to a medical practitioner
Patient has presented with symptoms or concerns requiring ophthalmic Investigation resulting in issue of a changed prescription
Patient has presented with symptoms or concerns requiring ophthalmic Investigation resulting in either no change or no referral (the patient's record should indicate any symptoms shown to support this category of claim if necessary).
Patient needing complex lenses
with corrected vision of less than 6/60 in one eye.
has presented for a sight test at the request of a medical practitioner
Patient has is being managed by an optometrist under the GOC referral rules, for example suspect visual fields on one occasion which is not confirmed on repeat, or abnormal IOP with no other significant signs of glaucoma
Patient has been identified in protocols as needing to be seen more frequently because of risk factors.
Other unusual circumstances requiring clinical investigation.
1 day
The world'sonly myopiamanagementcontact lens supportedby a 7 -year clinicaltrial2· 3 A
tUsing measuredandmodeleddata,pooledacrossages(8-17), MiSight®1 day slowedmyopiaprogressionby an averageof approximately50%. t12 monthspost-treatment,evidenceindicatesthat no accumulatedmyopiacontrolbenefitswerelost following3 or 6-yearsof MiSight®1 day wear (on average,for childrenaged8-15 at start of wear).Instead,eye growth revertedto expected,age-normalrates.
1.Arumugam8etal.ModellingAgeEffectsofMyopiaProgressionfortheMiSight1dayClinicalTrial.Invest.Ophthalmo/VisSci.2021; 62(8): 2333. 2. ChamberlainPetal. A 3-year RandomizedClinicalTrialof MiSightLensesfor MyopiaControl.OptomVisSci 2019; 96(8): 556-567. 3. ChamberlainPet al.Long-termEffectof Dual-focusContactLenseson MyopiaProgressionin Children:A 6-year MulticenterClinicalTrial.OptomVisSci.2022; 99(3): 204-212. 4. Chamberlain Pet al. Myopiaprogressionon cessationof Dual-Focuscontact lenswear: MiSight 1 day 7-year findings.OptomVisSci.2021; 98(E-abstract): 210049. 5. ZadnikKet al. FactorsAssociatedwith RapidMyopia Progressionin School-agedChildren.Invest.Ophthalmol.Vis.Sci.2004; 45(13): 2306. 6. HammondD,ArumugamB,et al.MyopiaControlTreatmentGainsare Retainedafter Terminationof Dual-focusContact LensWearwith no Evidenceof a ReboundEffect.OptomVisSci.2021; 98(E-abstract):215130.
© 2024 CooperVision.CooperVision®andMiSight®areregisteredtrademarksof TheCooperCompanies,Inc.anditssubsidiaries.
CVGY122291-1