17 minute read
ENVIRONMENTAL QUALITY AND OCULAR SURFACE HEALTH
from OT April/May 2023
by TheAOP
Dr Katrina Schmid BAppScOptom (Hons), PhD, Grad Cert Higher Ed, Grad Cert Ocular Therapeutics,
IN BRIEF This in-depth article considers the outdoor and indoor environment, including air quality and climatic factors, and how this affects the tear film and ocular surface health.
Advertisement
Introduction
Poor outdoor and indoor environmental quality, including both air quality and climatic factors, can detrimentally affect the tear film leading to symptoms of ocular irritation. These effects can be acute or chronic depending on the duration and extent of the adverse environmental conditions. Air pollutants include those from natural (for example, wildfire smoke) and man-made sources (such as building materials, consumer products, and cooking) that emit strong sensory irritants, corrosive chemicals, and combustion-related pollutants (for instance, particulate matter and nitrogen dioxide). The quality of the outdoor environment can alter people’s daily habits, where often poor conditions lead people to spend greater time indoors; this increases the importance of indoor air quality (IAQ) and the indoor climatic conditions.
Knowledge in this area is important for eye care practitioners (ECPs) so they can understand the impact of environmental quality on ocular surface health, both for their own wellbeing and that of their patients. The goal is to protect the ocular surface from the adverse effects of air pollutants combined with the negative influence of thermal factors, such as dry air and high temperatures.
Assessment Of Outdoor And Indoor Air Quality
Outdoor air quality
People who live in countries with poor outdoor air quality (OAQ) are acutely
Cpd Points
aware of the detrimental health effects of polluted air1 and the ocular irritation this can produce.2 In Australia, reports show that measured particulate matter (PM) and ozone levels in Sydney can at times exceed the health standards.3 In the UK, the levels of roadside PM have reduced over the past 10 years as fuel efficiency has improved and emissions have reduced.4 In urban areas, residential combustion of wood in stoves and open fires contributes to elevated pollution levels during winter months.4
Poor OAQ affects the liveability of cities and people’s ability to enjoy the outdoor environment. The air quality index (AQI) provides information on daily air quality in cities around the world. The AQI is the average concentration of pollutants, but those included may vary (for example, carbon monoxide, lead, nitrogen dioxide (NO2), ozone, particulate matter, and sulfur dioxide (SO2)).
Air pollution band Value Accompanying health messages for at-risk individuals*
Low 1–3 Enjoy your usual outdoor activities
Accompanying health messages for the general population
Enjoy your usual outdoor activities
Moderate 4–6 Adults and children with lung problems, and adults with heart problems, who experience symptoms, should consider reducing strenuous physical activity, particularly outdoors
High 7–9 Adults and children with lung problems, and adults with heart problems, should reduce strenuous physical exertion, particularly outdoors, and particularly if they experience symptoms. People with asthma may find they need to use their reliever inhaler more often. Older people should also reduce physical exertion
Very high
10 Adults and children with lung problems, adults with heart problems, and older people, should avoid strenuous physical activity. People with asthma may find they need to use their reliever inhaler more often
It can be calculated in several ways. One method is to take the average of readings from air quality sensors of each pollutant over a stated time frame, the values are divided by the national quality standard, and multiplied by 100, with the highest value used as the AQI. The mathematical function used to convert from air pollutant concentration to AQI varies by pollutant.
The AQI is provided in real time, can be searched by location, and people can use this information to make judgements about the OAQ, and if they should alter their behaviour (for instance, not go outside). The lower the AQI, the better the air quality; a value of less than 50 is considered good, greater than 100 poor and greater than 150 hazardous to health. Countries with a very high AQI, and thus very poor air quality are numerous, and include Bangladesh, Chad, Pakistan, Tajikistan, and India.5
There are multiple websites that provide AQI information. Air quality data in the UK, including the AQI and PM level are available.5 AQI in the UK is
Enjoy your usual outdoor activities
Anyone experiencing discomfort such as sore eyes, cough or sore throat should consider reducing activity, particularly outdoors
Reduce physical exertion, particularly outdoors, especially if you experience symptoms such as cough or sore throat considered good, although the reported 2021 average PM concentration was 1.8 times the World Health Organization (WHO) annual air quality guidelines value. The UK Department for Environment Food & Rural Affairs UK-AIR converts the AQI to a daily score for use in public health messaging.6 The daily AQI (DAQI) is numbered one to 10 and divided into four bands, low (1–3) to very high (10), to provide simple information about air pollution levels (see Table 1). OAQ can be poor in countries relatively close to the UK such as Bosnia, Bulgaria, Italy, Poland, Serbia and Turkey.7 Depending on weather conditions, including the direction of the prevailing winds, the quality of UK air can be detrimentally affected from sources originating outside the UK. It is also known that during bushfire events, the AQI will be greatly increased.8 Extra care should be taken at this time. The UK is not immune to the effects of wildfires and the health hazard they create.9 For example, in August 2022,
Table
Increased to dry indoor air Greater exposure to dry air if heating (in cold climates) or air conditioning (in hot climate) systems required
Likely none for cleaners used in the home.
Issue with direct eye contact
Use of spray cleaners elevates exposure Uncertain effect of other
No evidence that standard indoor cleaners are detrimental to human health.
Uncertain as to whether harmful aerosols are produced. Poor evidence regarding whether ocular surface is affected, and if so, likely only with protracted use and/ or direct contact
Mask wear Localised change to air flow around the eye
Exacerbates dry eye, particularly when poorly fitting
Contact lens wear May exacerbate effect of detrimental air quality factors on ocular surface
Suggested to avoid spectacle fogging due to mask wear
Interacts with mask wear to decrease contact lens comfort the AQI in Greenock, Scotland was greater than 150 due to summer fires. Thus, the key is to reduce the likelihood of fires, and if they occur, ensure that the poor OAQ does not subsequently lead to poor indoor air quality (IAQ).
Indoor air quality
IAQ is the air quality within and around buildings and structures, that is to say, within the internal environment.10 As this varies locally, and must be individually monitored within each building, IAQ values are not reported. New air pollution sensing methods are being developed to measure IAQ,11 which could provide useful information in real-time.
As people spend most of their lives indoors (up to 90% of all time), the quality of the indoor environment has the potential to have a very large effect on human health. Poor IAQ has been linked to sick building syndrome, reduced productivity and impaired learning in schools.12 Along with the incursion of outside air pollutants, contaminants are also produced within the indoor environment. These can include emissions from building products and furnishings, and from activities like heating, cooling and cooking. Common indoor pollutants include second-hand tobacco smoke, air pollutants from indoor combustion, PM, moulds and other allergens, volatile organic compounds, carbon monoxide and carbon dioxide, and ozone.
Climate changes can translate into altered indoor environments; this is related to heat exposure, flooding, and chemical and biological contamination in buildings.13 It has been suggested that increased health burdens related to more extreme heat and cold, indoor exposure to air pollution derived from outdoor sources, and mould growth, will occur and that mechanical ventilation with heat recovery and air filtration will be required.13 Source control, filtration and the use of ventilation to dilute contaminants are the primary methods for improving indoor air quality in most buildings.
HOW DOES THE ENVIRONMENT AFFECT THE OCULAR SURFACE?
The potential adverse effects of air pollution on the eye have received much attention.14,2 Both poor OAQ and IAQ, can impact the ocular surface health, particularly if it is already compromised, leading to further exacerbation of ocular symptoms. Various degrees of inherent gland disease will contribute to the overall disturbance,15 and this may be worsened by a broad list of medications known to alter the tear film and cause dry eye.16
The tear film, which protects the ocular surface, is exposed directly to the air and hence affected by air quality.17,18 For instance, the tear film can be impacted by processes that increase tear evaporation and decrease its stability (for example, low humidity, high temperature, air current, that is to say, drafts). Inadequate ventilation can exacerbate the effects of dry air and high temperature, producing even drier air and further deterioration of the ocular surface. Tear film stability is further destabilised by a reduced blink frequency or increased portion of incomplete blinks during extended screen-based work involving digital devices or inadequate lighting conditions.19 For instance, during visually demanding work where the tear film is compromised, it becomes more vulnerable to external stimuli. People with unrecognised or mild to moderate dry eye disease may further experience exacerbation of dry eye symptoms during and after visually demanding screen-based work in an environment with poor IAQ and aggravated microclimatic conditions.20 Thus, the ocular surface becomes more vulnerable to the inadequate IAQ in the home environment, and even more so after extended screen-work.
Aggressive chemicals in combustion particles (environmental tobacco smoke, wildfire smoke, traffic emissions) are harmful to the ocular surface. For example, ambient levels of vehicle induced air pollution have been shown to alter conjunctival goblet cell density and increase MUC5AC mRNA levels; 21 these may be adaptive responses to long-term exposure to pollution. The exposure to high levels of PM may also increase the risk of meibomian gland dysfunction (MGD) and blepharitis. 22
Elevated concentrations of certain oxidative agents, mostly strong sensory irritants like formaldehyde or acrolein, can cause chemesthesis and sensory irritation. Pollution-induced irritation in the trigeminal distribution can cause sensory irritation to the eye, nose and throat. 23 Furthermore, chemicals in certain surfactants present in cleaning or disinfection products are potentially harmful.
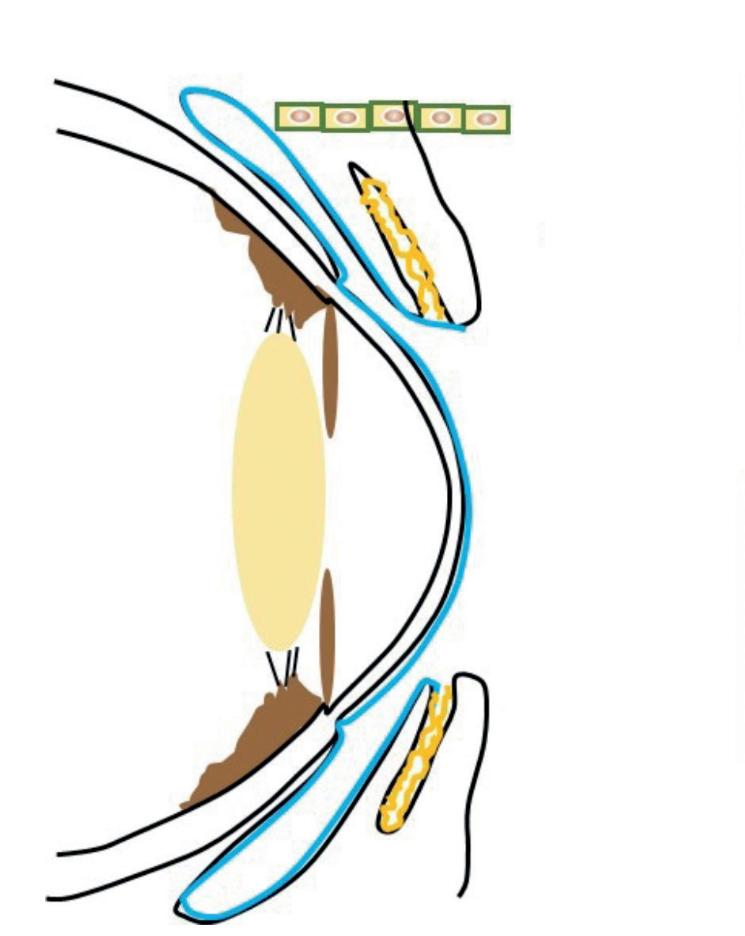
A key question from the perspective of managing the IAQ in residential environments, is how indoor air pollution, the microclimatic parameters (temperature, indoor air humidity, ventilation, and draft), and the workstation conditions (such as screen-based digital device work and position) may deteriorate the ocular surface health (that is to say, tear film stability). Figure 1 shows a pictorial representation of how environmental factors which affect air quality interact with human factors that affect ocular surface health, thus further exacerbating the reduction in tear film quality.
Influence Of Activities And Behaviours
Ocular surface diseases, in particular dry eye, are very common, often chronic, can be severe, cause ocular irritation and pain, and can reduce visual and work performance.17 The lockdown events as a result of COVID-19, and subsequent lifestyle changes,24 have exacerbated ocular surface issues and led to the proposed term ‘quarantine dry eye’.25 Domínguez-Amarillo etal describe a vicious cycle whereby increased time spent in the home deteriorates IAQ due to increased pollutant emission from activities (for example, cooking), increased cleaning, and steps undertaken to improve the home’s comfort (for instance, increased heating, reduced ventilation).26
People’s daily activities and behaviours can thus alter the environmental conditions they are exposed to. For example, when groups of people in cities commute less, there is a reduction in outdoor air pollution due to reduced vehicle emissions.27 At an individual level, the amount a person commutes to work, how much time is spent indoors, what tasks are carried out and whether air filters are used in the home will all vary environmental quality and duration of exposure to adverse conditions.
Table 2 provides a summary of how alterations to a person’s activities can potentially affect air quality, general health and the ocular surface. Some of these might have positive ocular effects, while others can exacerbate dry eye and other ocular surface problems.
Traffic related pollutants
Many studies have confirmed the important influence of traffic-related pollutants, for example, PM, NO2 (proxy of traffic and combustion), and SO2, on the development and exacerbation of dry eye disease and symptoms.15
Environmental exposure during commuting to and from the workplace might influence the ocular surface stability. It has been speculated that the reduction in dry-eyesymptom-scores measured during periods of lockdown could be due to reduced exposure to outdoor air pollution from not commuting to work.44
A positive outcome has been the many reports of reduced air pollution during periods of lockdown, with improvements in OAQ in many parts of the world.27 Analysis has shown that after accounting for meteorological variations, lockdown events reduced the population-weighted concentration of NO2 and PM levels by approximately 60% and 30%, respectively.27 Decreases in global transport emissions are largely responsible for the NO2 reductions. Improvements in OAQ during periods of lockdown have been reported both in Australia and the UK.45,46 The reported reductions in pollution levels in Australia were smaller than elsewhere and not always at significant levels.45 In the UK there was a large reduction in traffic, and this translated to a reduction in both NO2 and PM levels at urban traffic monitoring sites.46
Indoor air pollutants
A lifestyle of less time outdoors and more indoor time increases the risk from indoor environmental pollutant exposure.47 The assessment of IAQ factors impacting the ocular surface is the same whether the indoor environment is a home or office. These IAQ factors include thermal factors (temperature and indoor air humidity), a host of various kinds of pollutants, both volatile inorganic (NO2 and ozone), and volatile organic compounds (VOCs), and PM. While there are WHO global air quality guidelines48 and IAQ guidelines,49 most countries do not have IAQ standards.
The impact of indoor air pollutants, including VOCs and particles, has been reviewed.12,15,17 To summarise, only situations with high concentrations of strong sensory eye and airway irritants like formaldehyde and acrolein may result in acute sensory irritation by trigeminal nerve stimulation. These exposures are activity-dependent, for example, cleaning-related activities with fragrance-based consumer products in ozone enriched environments. However, the risk is low, and fortunately, VOCs have thresholds for sensory irritation orders of magnitude higher than those typically measured indoors in both office and home environments. Construction products, electronic devices and other polymer-based products found in the home can result in elevated concentrations of endocrine disrupting compounds (semi-VOCs), both in the indoor air and in dust particles, of which some may be associated with an elevated risk in dry eye.50
Indoor temperature and humidity
Other factors important for a stable ocular surface are the room temperature and the indoor air humidity. Elevated temperature and low indoor air humidity increase water evaporation, which can result in desiccation of the ocular surface. Furthermore, both high room temperature and/or low indoor air humidity compromise work performance.32 The lacrimal secretion is retarded during reduced stimulation of cold receptors by elevated ocular surface temperature and this will further alter the composition and basal flow of the tear film.51 Conditions of draft, that is to say, air flow across the ocular surface, may also increase the complaint rate of dry eye symptoms, possibly by elevated water evaporation from the ocular surface and consequently a sensation of cooling.
Exposure to environmental tobacco smoke
Indoor PM2 5 is the most reliable marker for the presence of tobacco smoke; the level of PM2.5 can be 10 times higher in houses of smokers versus those of non-smokers. Recent studies have demonstrated that PM2.5 levels are closely correlated with chronic lung diseases,52 highlighting the damage that can be caused by prolonged exposure to poor IAQ. Tobacco smoking can cause symptoms of itchiness and irritation, along with conjunctival redness. Changes to the ocular surface associated with smoking include a reduction in tear film break-up time, changes in the tear film lipid layer, reduction in tear secretion, corneal and conjunctival sensitivity, and tear lysozyme concentration.53 Exposure to secondary environmental tobacco smoke is associated with similar effects.54
Increased working and studying from home
Since an already compromised ocular surface may be more vulnerable to further insult from external stimuli, an important question is how occupational (office) working conditions, work habits and lifestyle may differ from conditions when working from home. It is important to consider that the potential ocular surface impact of IAQ can be exacerbated by many work-related factors, for example, duration of screen/reading work and other visually demanding tasks. Studies have found associations between the extended screen/reading hours after the lockdown and elevated prevalence of dry/irritated eye symptoms.24,55 Similarly, for students, online lectures have been associated with worsening of dry eye symptoms.56,57 It is well known that blinking frequency decreases during use of digital devices and this will further exacerbate the ocular surface dryness experienced in dry air.
Implications Of Health Advice For Air Quality
Infection control measures, including wearing face masks, physical distancing, regular cleaning of surfaces, hand hygiene (including alcohol-based sanitisers), and increased ventilation have been recommended.
Indoor ventilation
One possible major difference between the office (occupational) and home environments is the conditions of ventilation and the use of combustion-related activities at home like cooking and the use of (kerosene) heaters, fireplaces and infiltration of vehicle emissions from near-by traffic. The home activities might result in elevated PM concentrations relative to offices.27
Combustion particles are associated with an elevated acute risk of dry eye symptoms.17 Thus, adequate ventilation is essential to control the room temperature and the indoor air humidity within recommended limits of comfort and safety.32 However, ventilation may also impact the IAQ negatively during the cold dry air winter season because the incoming dry air becomes even drier in the heated indoor environment, thus, further exacerbating the desiccation of the ocular surface. Natural ventilation at the levels required to improve IAQ may be unachievable as the outdoor air is too hot, too cold or too polluted.
Cleaning of surfaces and hands
Indoor dust and moulds are potentially harmful to humans, can degrade furnishings and equipment, and need to be removed from surfaces. Dust can contain pollen, mould spores, fungus, bacteria, viruses, dust mites and dead skin cells. Other PM that may be present include degraded plastics, concrete dust, pesticides and fuel residues. Vacuuming and wiping surfaces with a damp cloth is the best way to remove dust PM. Infection control procedures also require the use of surface cleaners. There are reports that the intensity and frequency of the use of household cleaners has increased and newer cleaners containing hypochlorite and biocides utilised.26 Anecdotal reports state that ECPs alcohol wipe frequently touched items (PIN pads, keyboards, pens) and spray counters, chairs and doorhandles with surface cleaners proven effective against COVID-19 (for example, containing hydrogen peroxide, benzalkonium chloride (BAK)). These cleaners are stated to be safe with no harmful fumes, though safety instructions include use of gloves and eye protection. There is some indication of BAK in cleaning products inducing asthma,37 and of course, BAK is well known as an ocular surface irritant when used as a preservative in eye drops. 58 In terms of the ocular surface, the greatest risk is with direct contact, although there is little information on effects of aerosols on the ocular surface. For example, there are reported cases of ocular surface irritation caused using alcohol-based spray hand sanitisers, and as such, it is recommended to spray below eye level.35 Although it is well known that if alcohol comes in direct contact with the cornea, it will debride the epithelium, there is no current evidence of an ocular surface effect when in aerosol form.
Clausen etalreport that the evidence for respiratory effects after inhalation of quaternary ammonium compounds (QACs) found in cleaning spray products is
Environmental factors
Contribute to global sustainability and reduced emissions
Lobby for clean air and reduced pollution.
Increase outdoor time if OAQ is of good quality
Take steps to improve IAQ
Ensure adequate indoor air ventilation
Use air filters if IAQ is poor
If IAQ is too dry, humidify the air
Human factors
Take steps to avoid digital eye strain by taking micro-breaks when performing extended cognitive visual activities
Carefully consider which cleaning products are best, avoid using spray cleaners at eye level
If required, wear a correctly fitting face mask
Use ocular lubricants or contact lens rewetting agents as needed
Treat meibomian gland disease
Be aware that many medications can detrimentally affect the tear film quality ambiguous.34 They also report that solvents including glycols and glycol ethers as well as propellants are only very weak airway irritants and not expected to induce sensitisation in the airways (and thus not the ocular surface either); this does not preclude the fact that there may be people with a higher-than-normal sensitivity to these chemicals. Others suggest that only particular agents have asthma inducing potential (for example, chloramine, BAK) and there is much equivocal data.37 In any case, to reduce the risk, chemical free products should be used if possible, applied with a damp cloth rather than spraying a mist into the air. The aim is not to introduce additional aerosols into the air when cleaning.
Air filters (purifiers)
IAQ can often be improved by having good ventilation, that is to say, having outdoor air flow inside. However, when the OAQ is poor it may be better to lower the natural ventilation rate. IAQ can then be improved by using air filters which are designed to filter pollutants out of the air. Some filters (for example, MERV-13, HVAC systems, HEPA) can capture fine smoke particles and viruses. It is suggested that if the CO2 levels are above 800ppm, HEPA air filters should be installed. The benefits of air filters in improving IAQ have been reviewed.59 The key features are good air flow to ensure adequate ventilation, ability to filter out a range of small particle sizes, and easy-to-complete, cost-effective maintenance. There is currently a lack of good evidence for claims that household HEPA systems remove all small particles including airborne bacteria and viruses.60 While there are studies showing the positive effects of air filters/purifiers that reduce air pollution on cardiorespiratory health59 and ocular allergy,61 there are no comprehensive studies of effects on the ocular surface.
Mask-associated dry eye (MADE)
There are now many reports of mask use increasing dry eye symptoms;40 this includes increased corneal staining, representing increased epithelial cell desiccation and sloughing, in staff who wore masks all day.40 Although dry eye symptoms and ocular surface inflammation increase, changes in goblet cell density were not observed and corneal dendritic cell density only increased in participants that already had dry eye disease.42
It has been proposed that ocular surface dryness, and hence symptoms, occur because the exhaled air flows upwards towards the eyes’ surface when the mask is not fitted tightly across the bridge of the nose. This repeated warm air draft (36–37℃) causes tear film instability and dry spot formation and is thus termed mask-associated dry eye (MADE). 62 Relief of dry eye symptoms may occur by taping down the upper aspect of the mask. Primary management includes ensuring the mask fits well, particularly across the nose bridge, and secondly, rewetting eye drops are used as required.
Clinical Advice Relevant To Air Quality And Ocular Surface Health
Tips to consider for improving air quality with potential beneficial ocular surface health are summarised in Table 3. ECPs should consider how they can contribute to global sustainability and reduce their own emissions, and lobby for the importance of clean air and reduced air pollution. If the OAQ is of good quality, suggest patients increase their time outdoors. Take steps to improve IAQ; this might mean ensuring adequate indoor air ventilation, using air filters if the IAQ is poor and humidifying the air adequately. ECPs can advise patients to take frequent micro-breaks from screen use and consider their workstation design. Everyone should carefully avoid use of spray cleaning products at eye level. Wear a correctly fitting mask and use ocular lubricants, or contact lens rewetting agents in dry environments to reduce ocular surface desiccation. Be aware of medications that are known to alter the quality of the tear film.
ECPs should consider which of these recommendations might benefit individuals and thus what to focus on in the advice they provide to each patient. This advice is particularly important for patients that already have a compromised ocular surface.
Conclusion
This article highlights the critical importance of both OAQ and IAQ on the health of the ocular surface. ECPs should consider people’s environments and habits, the effect of these on the ocular surface and individualised advice provided.
Acknowledgement
This CPD article was developed from discussions with Professor Peder Wolkoff, Denmark, an expert on indoor air quality and its impact on the ocular surface.
Dr Katrina Schmid is associate professor in the School of Optometry and Vision Science, Queensland University of Technology. Her teaching expertise includes ocular pharmacology, and in particular, the mechanisms, uses and side effects of ocular therapeutic agents. Her research interests include assessment of the ocular surface, including meibomian gland dysfunction and dry eye, and its treatment.











