


















How patients view optometry –and the clinicians working to make eye care more accessible


1 day

Health;comfort and great valuet 1 - all in one.
Health· - One-day lensesare the healthiest way to wear soft contact lenses.With siliconehydrogel materialfor high breathability and UV blocking··for added protection.
Comfort - Optimised Comfort Edge™and Wetloc'" Technologyfor all-day wearer comfort and hydration.
Valuet1 - Availableacrosssphere,toric and multifocal at a great price.t
Adam Sampson

AI is increasingly starting to drive eye care in the UK,

To a man of my age, Ernie will forever be the man who drove the fastest milk cart in the west. However, to my son, Ernie means something very different: the Chinese version of ChatGPT. Launched nine months ago, it has already amassed a sizeable Chinese following and appears to be refining its capability with amazing speed. In one test, Ernie 4.0 outperformed GPT-4 both on its knowledge and its understanding of the desires of the questioner. Yet the positive reviews of Ernie come with one important caveat. While it confidently discusses Western current affairs, when the topic turns to contemporary Chinese politics, Ernie’s previous certainty of tone pivots into marked diffidence, declaring itself unable to answer or, all too often, suggesting that “we talk about something else.” Sourcing its answers primarily from officially-sanctioned Chinese websites, Ernie has learned to avoid saying anything that is contrary to the acceptable local line.
The potential contribution of the new AI technology to improve healthcare cannot be overstated. But, as Ernie shows, its potential limitations are becoming increasingly clear too. AI has the capability of sifting the learning from huge data sets, but its functionality will be limited by the data it is analysing and the rules by which it operates. If the data it learns from is partial and the rules have biases, the results will be flawed.
As AI models increasingly start to drive eye care in the UK, this is a real issue we need to grapple with. Take, for example, the normative databases used with OCT, where the size and breadth are often small and lacking in diversity. Given the fact that glaucoma prevalence varies significantly within parts of the population, it is essential that the databases on which such machinery draws should be as wide as possible.

The potential for AI to massively transform our lives outside healthcare as well as in it cannot be overstated. At the AOP, we are currently exploring extended ways of using automated chatbot functions to supplement – not replace – the service our members get from us. But that is only scratching the surface of what AI will be able to provide in the future.


MILLION

Adam Sampson, AOP chief executive


lens fit success5-9*

*Basedon lens movement,centration and rotation at initial fitting. References:1. In a clinical trial to evaluateon-eye performance of TOTAL30°for Astigmatism lenseswhere n=69;Alcon data on file, 2021.2. In a clinical trial to assessoverall performance of DAILIES TOTAL1°for Astigmatismlenseswhere n=134patients;Alcon data on file, 2021.3. In a clinicaltrial to evaluatestability of axis orientation of DAILIESTOTAL1°for Astigmatismlenseswhere n=47;Alcon data on file, 2020.4. In a PRECISION1™ for Astigmatismstudy where n=78eyes:Alcondata on file, 2020.5. HinesB, et. al. Clinicalsubjectiveperformanceof two daily disposabletoric soft contact lenses.Poster presentedat: AmericanOptometric Association,Chicago.June15-18,2022.6. In a randomized,subject-masked,multi-site clinicalstudy with over 150patients;Alcon data on file, 2005.7. In a clinicaltrial to evaluatestability of axis orientation of PRECISION1™ for Astigmatismcontact lenseswhere n=78eyes;Alcon data on file, 2020.8. In a clinicaltrial to evaluatestability of axis orientation of DAILIESTOTAL1• for Astigmatismlenseswhere n=47;Alcondata on file, 2020.9. In a clinicaltrial to evaluateon-eyeperformanceofTOTAL30°for Astigmatismlenseswhere n=69;Alcon data on file, 2021.10. Perez-GomezI, ValenteR,VonbunH. Surveyof patient and ECPsatisfactionwith a new daily disposabletoric contact lens.OptomVisSci;2021;98:E-abstract215040. TOTAL30°are monthly contact lensesfor daily wear. See instructions for use, for wear, care, precautions, warnings, contraindications and adverse effects. Find at http://ifu.alcon.com
15605© 2024Alcon Inc. UKIE-DT1-2400038








OT features a range of expert contributors who share their optometry expertise and insight. Here are some of those who helped us put this edition together

100% Optical 2025 What’s in store?
OT takes its first look inside the 2025 show and finds out what readers can expect from the event’s next instalment

August/September 2024
Volume 64:04 Issn 0268-5485
ABC certificate of circulation 1 January 2023–31 December 2023
Editor: Emily McCormick emilymccormick@optometry.co.uk
Deputy editor: Lucy Miller lucymiller@optometry.co.uk
Features editor: Selina Powell selinapowell@optometry.co.uk
Senior reporter: Kimberley Young kimberleyyoung@optometry.co.uk
Web content and social media manager: Leah Boyle leahboyle@optometry.co.uk
Clinical editor: Dr Ian Beasley ianbeasley@optometry.co.uk
Clinical editor for multimedia: Ceri Smith-Jaynes cerismithjaynes@optometry.co.uk
Video production editor: Laurence Derbyshire laurencederbyshire@optometry.co.uk
CPD enquiries: 020 7549 2076 CPDhelp@optometry.co.uk
AOP membership and OT subscription team: subscriptions@aop.org.uk
How would you like the optometry profession to be seen by the public?

“Optometry as a profession must be seen as a necessity for health, but should also be a stylish, fun and enjoyable experience for all”
Camilla Anderson, brand and contact lens manager at Park Vision Opticians I could not live without, page 84

Sarah White, dispensing optician and AOP Councillor In focus, Five key topics, page 42PAGE 40 -
“I would like the optometry profession to be seen as respectable and respectful, caring and capable, forward thinking and reliable”


“I would like patient’s to view optometrists as being respected, informed and approachable friends”
Simon Berry, optometrist and practice owner Becoming a business owner, page 34
Advertising: Jamie Dawson 020 3771 7201 jamie.dawson@thinkpublishing.co.uk
Advertising production: aop@ccmediagroup.co.uk
Art director: Grant Pearce
Client engagement director: Kieran Paul Executive director: Jackie Scully
Published bimonthly for the Association of Optometrists by Think Media Group 20 Mortimer Street, London, W1T 3JW
Printed by Acorn Web, Normanton Ind Estate, Loscoe Close, Normanton, West Yorkshire, WF6 1TW
All rights in and relating to this publication are expressly reserved. No part of this publication may be reproduced in



At Newmedica. we choose to use the highest quality cataract replacement lenses for the best clinical outcomes. In fact. our monofocal lens for NHS patients has the lowest PCO rate of any lens on the market at 3 and 5 years. It's hydrophobic and is specially designed to reduce the need for YAG surgery*.
Which is great news for your patients and the NHS. and peace of mind for you.
*Source : The Royal College of Ophthalmologists, National Ophthalmology Database "Feasibility Study of Post-Cataract Posterior Capsule Opacification" May 2021
#EMILYMcCORMICK


OT’s Kimberley Young travelled to the Dolomite Mountains in Italy to visit eyewear brand Blackfin’s headquarters and took a tour of its Black Shelter Sustainable Factory

0
Read our latest content, updated daily online: www.optometry.co.uk
1
Terminology technicalities
Optometrist or optician?
OT explores the language underpinning the public’s perception of optometry

Next month OTwill release a CPD Survivial Pack in partnership with CooperVision. Designed to support practitioners during the final hurdle of the current CPD cycle, OTrecently filmed the pack’s bespoke CPD Video with CooperVision’s Nicky Latham




Keep up to date with all things optics by following OT’s social channels

OT’s Ceri Smith-Jaynes and Laurence Derbyshire met via Zoom with Yasmin Whayeb to discuss how to communicate myopia management for one of our latest Practice team training modules

OT’s Lucy Miller attended a Specsavers lived experience focus group in Bristol that explored the barriers to eye care for those experiencing homelessness as the multiple establishes out-of-hours eye care in 44 of its practices
2
The Imran Hakim episode
In the latest instalment of The OT Podcast, we sit down with the founder of Hakim Group, Imran Hakim
3
We have released four new video skills guides exploring contact lens fitting, which can be found in our Education library
4 Practice team guide
The latest instalment of our Practice team guide is available open access to everyone online


From cost concerns to the role of extended services, OT explores the factors shaping how the public view a visit to the optometrist

WORDS: SELINA POWELL PHOTOGRAPHY: ALEX LLOYD JENKINS, LOUISE HAYWOOD-SCHIEFER
First it was the television that faded out of focus, then her emails and her granddaughter’s homework.
Juanita Munroe attended Eyecare Express in Woodford Green for an eye examination, conscious that her uncle had lost his sight to glaucoma at the age of 21. However, after a period of financial difficulty, she could not afford to pick up the new glasses. “I was a little embarrassed to be honest,” she told OT
“Obviously, you don’t want to go to your opticians and say, ‘I can’t afford my glasses right now’,” she said.
With only £45 to last her to the end of the month after rent, electricity and gas were accounted for, Munroe ignored a series of reminders. Then, one day, she reluctantly followed optometrists Yassar and Adeil Yousaf into the Woodford Green independent after they spotted her walking past.

Ò When someone offers that kindness, and you’ve never had it before, it brings a lot of happiness to your heart
Juanita Munroe
“They sat me down and told me they wanted to offer me the glasses for free. I became all teary eyed, but in a joyful way. When someone offers that kindness, and you’ve never had it before, it brings a lot of happiness to your heart,” she said.
During Ramadan, the Yousafs began offering free sight tests and spectacles to those who might not otherwise be able to afford eye care – in doing so, playing their small part towards easing the cost of living crisis in their neighbourhood.
Yassar Yousaf explained to OT that the offer has been extended beyond Ramadan, with four hours currently allocated to the initiative each week.
“We have met numerous patients who are in these overwhelming, difficult situations,” he explained.
“If we can help one person see better, they can hopefully help themselves get into a better place,” Yousaf shared.



Yassar and his brother Adeil observed the financial struggles that their parents experienced growing up. “This has shaped who we are now. We remember something that our parents taught us and that is: the happiest person on this planet is not the one who gets more, but the one who gives more,” he said.


A survey of 2000 members of the public by the General Optical Council (GOC) in 2023 found that most (58%) respondents had never felt uncomfortable visiting an optometry practice. However, among those who had felt uncomfortable, the most common reason was the perceived pressure to buy contact lenses or glasses – with around one in five people reporting this as the reason for their unease.
Aaron Lewis, 23, shared with OT that it can take courage to go for a sight test.
“You worry about the eventual cost,” he said.
Lewis, who is currently looking for work, received his first pair of spectacles from Eyecare Express after experiencing headaches.
“It was definitely a stark difference in terms of the clarity I can see with the glasses and having peace of mind as well,” Lewis shared.
“I’m thankful I was able to go through this scheme without having to worry about how I am going to pay afterwards,” he said.
As part of its public perceptions research in 2023, the GOC uncovered racial differences in how comfortable different groups were within an optometry practice.
While 60% of white respondents said they had never felt uncomfortable in an optometry practice, only 44% of Asian or British Asian respondents and 40% of Black or Black British respondents reported the same experience.
Bhavini Makwana is chair of BAME Vision – a voluntary group that aims to tackle inequalities in how people from underserved communities access eye care.
Makwana shared that the cost attached to a sight test and



spectacles can prevent people from BAME backgrounds accessing eye care. This is supported by GOC research that found 15% of white respondents cited cost as a reason for being uncomfortable visiting an optician, compared to 29% of BAME respondents.
Makwana shared that among those who do access eye care, language can be a barrier. “Some of the issues we’ve encountered is that people are not offered interpreters. Even though they’ve turned up, the value of that appointment is not there because they can’t fully understand what they have been told,” she said.
“ I do get joy out of supporting others. I don’t want anyone else to feel the way I did Bhavini Makwana
Get involved
BAME Vision is looking for optometrists to volunteer in community engagement work. Contact info@bamevision.org
A stark example of this is a woman who spoke with Makwana after seeing a consultant ophthalmologist for her deteriorating vision. A communication breakdown meant she came away from the appointment unclear about her diagnosis.
“She was going about her daily life with a macular hole, really worried about what to do next,” Makwana shared.
Turning to the steps that can be taken to make eye care more accessible, Makwana encouraged optometrists to use language that is appropriate for the patient and to avoid jargon. If language barriers are an issue, Makwana recommended offering an interpreter, or asking if a patient would like a friend or relative at the appointment. “It will be different for different people, because patients are unique. Generally, I think it helps to ask, ‘How can we make the appointment more accessible?’.”
The Accessible Information Standard, which came into effect in 2016, aims to make health and social care information accessible to all

patients. Makwana would like to see explicit recognition of people who speak different languages within the Standard – for example, by ensuring the provision of interpreters and making information available in different languages from the beginning of the patient journey.
Makwana’s own experience of waiting almost 15 years between her diagnosis with retinitis pigmentosa (RP) and being signposted to appropriate support has fuelled her motivation to address inequality. “I do get joy out of supporting others. I don’t want anyone else to feel the way I did,” she said.
As a teenager, Makwana initially thought that her tendency to miss steps, walk into lamp posts, and not being able to see clearly in bright sunlight was down to exam stress. She realised that something was seriously wrong during a school trip to Disneyland Paris when she had to rely on a friend to guide her through a darkened tunnel for a ride.
After being diagnosed with RP at the age of 17, a consultant ophthalmologist told her that there was no cure, and her vision would deteriorate over time. For some people this can take years, while for others it can take months or even weeks.
“Those words really stuck with me. I was absolutely terrified that I would wake up one morning and be completely blind,” Makwana said.
For the next decade, Makwana kept her condition hidden from the people around her – afraid of how she would be perceived. The first person she told outside of her family was her future husband. But her secret created challenges for fitting in – she was the clumsy daughter-in-law,

who knocked over glasses, could not drive and struggled to make round chapatis. It was not until 2012 – 15 years after her initial diagnosis –that Makwana’s husband spotted a poster for the charity RP Fighting Blindness (now Retina UK) during a check-up appointment at Moorfields Eye Hospital. When she attended a support meeting with her husband, it was the first time she had met people with her condition.
“I cried, because I realised ‘This isn’t just me.’ I felt like a weight had been lifted off me,” she said.
She recognised the adaptations she had made in isolation whilst others she met also did the same. “For so long, I had thought I was struggling, but then I realised that it was ok to do things differently. We started showing each other the things we do to make life easier,” Makwana shared.
It is Makwana’s own experience that causes her to bristle when terms like ‘hard to reach’ are used to describe groups that face challenges accessing care. “I wasn’t hard to reach. I attended my appointments every year,” she said. “There were 15 years’ worth of opportunities for professionals to tell me about mental health, practical and emotional support, and signpost me to services,” Makwana emphasised.

She believes that the solution lies in involving the community groups that a service is trying to reach.
“Attitudes need to change from the design stage to delivery,” she said. “If you’re going to do the same thing over and over again, then guess what, you’re not going to reach new audiences,” Makwana shared.
She is determined that other people will have a different experience to the one she went through as a 17-year-old. “There is a huge world out there, even with sight loss,” Makwana shared.
Aside from the need to support patients with conditions that affect their vision, Makwana highlighted the importance of offering inclusive services to ensure early diagnosis
“ I want to see patients naturally thinking of us as the first port of call
Hannah Thomas


and treatment. “We know that half of sight loss is preventable, but it is only preventable if you have the information and eye care in an accessible format,” she said.
The role of independent prescribing
In 2023, for the first time since the GOC began its annual public perception survey, more UK residents selected an optometry practice (36%) as their first port of call for an eye problem than a GP practice (33%).
This is a substantial shift since the first survey in 2015 – when 54% of patients selected a GP practice and only 19% selected an optometry practice. However, disparities exist between the four nations of the UK.
People are more likely to present to an optometry practice if they woke up with an eye problem in Northern Ireland (49%), Scotland (46%) and Wales (39%) than in England – where less than a third of patients (30%) state that an optometry practice would be their first port of call.
Hannah Thomas is an independent prescribing (IP) optometrist and the
director of Parish and Green EyeCare, which has practices in Talbot Green and Pencoed. The majority of patients who attend the practice receive NHS-funded eye care.
Thomas has observed a shift in how people perceive optometrists since she qualified in 2011. “During the pandemic, you could see that patients were starting to understand that you should go to your optometrist for an eye problem,” she said.
Alongside changes to care during COVID-19, Thomas believes that the growth of IP and extended care schemes in the community also contributed to changing attitudes.
Being able to provide care that was traditionally offered within hospital has seen patients appreciate the clinical nature of Thomas’ role.
“Before they may have thought we were just there to get their glasses, but now I know my patients perceive me as a clinician,” she said.
Patients will recommend to their friends and family members that they visit an optometrist if they have an eye problem, while local primary care providers are also referring


“ It is quite a scary position to be in when there is something wrong with your sight
Dean Porter
patients to Thomas’ practice. “The GP practices and pharmacists in my local area will say to patients ‘If you’ve got an eye problem, go to your optometrist’,” she said.
The roll out of a new national contract for optometry in Wales has helped to remove inconsistencies in where patients could access services.
However, Thomas highlighted that a remaining hurdle is getting a better geographical spread of IP-qualified optometrists so patients do not have to travel long distances for care.
“At the moment, patients don’t necessarily see every practice as a clinical environment. But as we develop more IP optometrists, virtually every practice will have an IP or one next door,” she said.
Thomas would like to reach the point where attending an optometry practice for eye problems is engrained in “public consciousness.”
“I want to see patients naturally thinking of us as the first port of call,” Thomas emphasised.
Dean Porter, a Pontypridd IT delivery executive, first attended Parish and Green EyeCare in 2019 for the treatment of anterior uveitis.
After a stressful period at work involving 60-hour weeks, Porter began experiencing headaches and one eye became bloodshot, with a very sensitive eyelid and light intolerance.
Porter told OT that his symptoms culminated in an unplanned return from a work trip to Brighton in order to receive treatment.
“On the train trip back, I had no option but to cover my eyes because the light sensitivity was so bad,” he shared. After initially receiving treatment through the hospital, Porter visited Thomas’ practice and was impressed with the level of personalised care. “It is quite a scary position to be in when there is something wrong with your sight. Going in to see Hannah provides me with that reassurance,” he told OT.
In contrast to his experience in hospital, Porter said that Thomas has the time to talk through options for managing the condition and discuss any concerns he might have.
“The optometrist seems to be in tune with the patient’s needs. You’re not just a number,” he shared.
Porter appreciated the convenience of being able to receive a prescription for the medication he needs from a High Street practice.
In 2023 the AOP launched a public-facing Costoflivingcampaign highlighting the importance of community-led eye care, with research indicating that millions of people across the UK are struggling with poor vision due to the cost of living crisis. The campaign ensures that those who are struggling have access to the support they require and are entitled to. Get involved: www.aop.org.uk/cost-of-living
“ That
effort to
provide eye care during the pandemic has been recognised by patients
Grant Robinson
He shared that the experience has shifted his perception of the services that optometrists can offer. “It has opened up my appreciation and respect for what they can do,” Porter said.
The common good
Cardiff University lecturer, Dr Grant Robinson, was inspired to undertake IP training after seeing firsthand the benefits of this specialist care during the pandemic. “I was away from home and my mother called me, distressed, saying that she had this painful, red eye that had been getting worse,” Robinson said.
After his mother was diagnosed with viral keratitis through the hospital, she received follow up care from an IP optometrist.
“That was game changing for her. It was so much more convenient than
going to hospital and there was less stress,” Robinson said. “Seeing the tangible difference an IP optometrist can make gave me the push to enrol in the IP programme,” he highlighted.
Robinson believes that the pandemic accelerated a change in the public perception of optometrists in Wales. He highlighted that staff at optometry practices across Wales communicated with each other in order to share best practice and offer support, as well as forming connections with other healthcare providers.
“Commercial considerations were put aside. It was about ensuring that we used our expertise in order to help people,” Robinson observed.
“I think that collegiate effort to continue to provide eye care during the pandemic has been recognised by patients,” he said.
Reflecting on differences in public perception between England and Wales, Robinson highlighted the advantages of rolling out change as a smaller nation. “I think in England, it’s slightly more fragmented,” he emphasised.
“We benefit from the fact that we have more uniformity across the profession. For patients, that means that it doesn’t matter where they are in the country – the message will be the same,” he said.

OT features editor. Get in touch by email: selinapowell@optometry.co.uk

Purchase the ldra diagnostic device plus the Tearstim IPRLdevice and receive the Activa heat mask and one additional Tearstim consumables kit free of charge worth .£7,515
OT captured contributors at a park in London and an optometry practice in Talbot Green
A shared sporting passion put patient Dean Porter at ease during his photoshoot with Alex Lloyd Jenkins at Parish and Green EyeCare in Talbot Green, Wales.
“It turned out that the photographer had a shared interest with Dean, who is an Ironman. This made everything more relaxed,” optometrist, Hannah Thomas, explained. Tinted spectacles –which help with the symptoms of uveitis and are Porter’s go-to eyewear when training – featured in the photoshoot.
Thomas observed that the novelty of a photoshoot captured attention within the practice. “There were quite a few patients still in the practice when we started and they all found it very entertaining,” she said. “Our optical assistants kept me laughing and clearly enjoyed the whole process,” Thomas added.
Bhavini Makwana, chair of BAME Vision, was photographed at a park in central London and in the offices of the Thomas Pocklington Trust. Her guide dog, Colin, made cameo appearances within the photoshoot.
Makwana, who has retinitis pigmentosa, shared that as someone with sight loss, it is helpful for photographers to give clear directions – for example, regarding positioning and where to look. “Louise did this really well. I certainly enjoyed the experience. Louise was really lovely to work with and made me feel at ease,” she said.
Contributors Bhavini Makwana, Dean Porter, Hannah Thomas Photographers Alex Lloyd Jenkins, Louise Haywood-Schiefer


You can watch our online exclusive video with IP optometrist and academic, Dr Grant Robinson by following the QR code here



optometrist and
















Food Supplement with Lutein, Meso-zeaxanthin, Zeaxanthin + Vitamin B2 & 250mg DHA
Career paths and personal development
EDITED BY: LUCY MILLER

38 A CONVERSATION ABOUT…
Establishing an out-of-hours homeless service in Bristol


“No two days
are
ever the same”
Owner of Eye Clinic at Home, Harjinder Sunda, shares a glimpse into life as a domiciliary optometrist
What I enjoy about domiciliary optometry is… that no two days are ever the same. I meet incredible patients who are always happy and grateful to have accessed my service.
The one thing I would change about domiciliary optometry is… I would abolish the requirement for pre-visit notifications in all nations. I feel these notifications reduce patient access and increase health inequalities.
The most common misconception I hear about domiciliary optometry is… you cannot carry out a full eye examination in a patient’s home.
My most memorable moment was… delivering and fitting patient CP’s spectacles. CP had moderate learning disabilities and had never experienced an eye exam. He had a high refractive error. The look on his face when he tried on his spectacles was magical.
My most challenging moment was… during the COVID-19 pandemic. The uncertainty of not knowing when restrictions would be lifted was very concerning.
My must-have piece of kit is… my portable slit lamp because it allows a more thorough ocular examination.
HOW I GOT HERE With CooperVision’s Christina Olner
A DAY IN THE LIFE
Simon Berry walks OT through his day
IP AND ME
A second opinion on herpes simplex keratitis 26

I have been able to detect several retinal detachments and many cases of uveitis, thereby avoiding loss of sight.
The one piece of advice for those considering domiciliary optometry is… to expect the unexpected. The environments you find yourself testing in will vary tremendously and you need be able to adapt accordingly.

Read about Harjinder’s experiences as a domiciliary optometrist in full on our website. Scan the QR code.

“THERE’S SOMETHING ABOUT THE CAMARADERIE”
Christina Olner, head of professional affairs at CooperVision, tells OT about how her passion for customer experience led her from practice to industry
My sister was diagnosed myopic during her first sight test. I remember sitting outside the room, and the optometrist filling out the prescription. I was probably five years old. That was the first time that I thought, ‘I think I’d quite like to do this.’ I liked the numbers, and the structure.
I studied at Aston University, then moved back to Nottingham for my pre-reg with Dollond & Aitchison. My supervisor was an examiner for the College of Optometrists. I had a lovely experience as a pre-reg.
Moving into practice from academic studies was a positive experience. During my pre-reg, I really fell in love with the profession. There’s something about the camaraderie and that whole team experience. Having the patient at the heart of everything really made me passionate about optics. The highlight was recognising that my quite technical degree led to this career that was really different, and wonderful.
After qualifying, I took a job in Shrewsbury for Dollond & Aitchison. I worked alongside an experienced optometrist, with lots of support. It’s really important, when newly-qualified, that you spend time learning how you operate as a clinician and seeing your own patients when they have problems, so you understand where you’re making mistakes. When I’ve had pre-regs, I’ve often told them, ‘your pre-reg is like learning to drive – it’s not until you’ve passed that you really learn how to do it.’
I was at Dollond & Aitchison for a couple of years, before moving to independent practice. For five years, I worked in an independent and locumed part-time. In the independent practice, I was the sole decision maker and was accountable for the performance of a family-run business. It was an important part of my career. It supports me now, because I have insight into what’s important to an independent practice.
After five years as a locum and working in an independent, I had twins. When I went back to work, I joined Boots Opticians. After 12 months, I moved into management. I wanted to prioritise patients – not just clinically, but from a patient journey perspective.
The patient journey was the thing I was most interested in. That was everything from making the right clinical decision to making sure the team had the right skillset to get things right the first time. It was about making every patient feel like they were part of the family. I ran some
successful practices with some very happy patients. I was at Boots for nearly 10 years.
When lockdown happened, I was part of Project Gold at Boots, which was COVID-19 testing. Boots head office was the first car park COVID-19 testing site in the UK. I was happy in my role, but a previous colleague then approached me about joining the CooperVision team.
I“Some of these lenses literally give people their functional sight back”
I moved to CooperVision at the height of COVID-19, in July 2020. I went from COVID-19 testing in a car park to professional affairs consultant, sitting at my desk with a laptop, having never had a desk job in my life. I spent a year as professional affairs consultant, before moving to head of professional affairs. We’ve done lots of things since then: we’ve seen out the COVID-19 pandemic, and moved back to the new world of business as usual.
NAME: Christina Olner ROLE: Head of professional affairs at CooperVision
LOCATION: Nottingham
Less than 12 months ago, I took on responsibility for the professional and commercial interests of CooperVision Specialty Eye Care in the UK. I look after the core professional and the specialty professional teams. We’ve moved my focus from soft lens products to some of the less commonly prescribed products – products for irregular corneas, for example. Some of these lenses literally give people their functional sight back. Over the next couple of years, I’d like to encourage more eye care professionals into fitting specialty contact lenses for a broad range of eye conditions. That’s my next hill to climb.
Read more career insights online: www.optometry.co.uk/how-i-got-here
The variety of a professional affairs team
You don’t have to come through the clinical route to get a role in industry – passion for managing practices and looking after customers is equally valuable. We are aligned to marketing, but also have the joy of working with academics. I’m working with Aston University at the moment, and we will be co-supervising a PhD to support our customer journey work. I get the pleasure of linking marketing initiatives with my academic colleagues and building a 360-degree solution for clinicians. Getting the opportunity to go out and create evidence where we see a gap is valuable.
Locum optometrist in south west London, Janki Vadgama, tells OT how locuming provided the flexibility she needed as a new mum
Before I became a locum, I was working... As an optometrist-manager in an independent practice. Then I had my daughter – she’s almost five – and started locuming when she was one and a half.
When I started as a locum, I wish I had known… The importance of being more mindful and responsible for everything that you do, in terms of patients and referrals.
When you’re in practice, you take it for granted, because you’re always there. It’s about taking more accountability: wrapping up and finishing all the work that you need to do. I’ve learned that you’ve got to be more organised if you’re working in different places.
I made the decision to become a locum...
To have more flexibility to work the days, hours and months that I want to work, to suit my daughter’s lifestyle and childcare. Also, to have a different day each day.
On my first day of locuming... I was nervous, because it was a different computer system. So, I had to obviously learn how to use that. The nerves were there, but I was excited as well, just to meet new people and be in a different location. I remember my first day very well.
My biggest locum challenge is… Being cancelled at the last minute. Last minute cancellations can be difficult, because it’s quite hard to then fill those days. You’re not getting a regular income; you’re only getting work paid for the days that you work.
As a locum, I’ve adapted my days by… Once you have a relationship with the practice
manager or the team, you can work the hours that you can do, rather than being in practice from 9am until 6pm and that’s it. You can work out your own routine, your own schedule, and your own timetable.
So yes, I definitely have adapted my days. I do end up finishing earlier everywhere that I work, which is agreed in advance, and is much easier for me.
Practices can make life easier for locums by… It would be really nice, if a locum was coming in for the first time, to compile a little bullet-point sheet on where the nearest hospitals are, where you would refer to, and if there are any specific pathways in that area, just in case. It’s just more information around referrals, where to refer, who to, and how.
One change I’ve seen whilst working as a locum is… I feel like it has become more fast-paced. With the introduction of optical coherence tomography and the different machines, things are done for you pretty quickly. I come from a very independent, slow paced, 45-minute testing environment, so you’ve got to learn to keep up and be prepared for that.
My favourite thing about being a locum is… The flexibility of working when you want to, and not working when you don’t want to, without having to request holiday.
NAME: Janki Vadgama
ROLE: Locum optometrist LOCATION: South west London
My advice for new locums is... Make sure you’ve been qualified for some time before you go into locuming. It can be quite daunting for a newly-qualified optometrist.
My solid advice would be to make sure you’ve worked in a practice for at least two or three years before you start thinking about locuming. You need to be a little bit more well-rounded as an optometrist before going into the locuming world, because you’ll come across everything and anything.

My last word on locuming is... Do it if you want ease and flexibility in your life.
0
Read more locum insights online: www.optometry.co.uk

Specialist optometrist at Moorfields Eye Hospital, Rupa Patel, tells OT how a contact lens clinic appointment led to the diagnosis of a pituitary tumour in a young patient
How long have you worked as a hospital optometrist?
Since I qualified, in 2016. I did my pre-reg training in a supportive multiple practice. As soon as I qualified, I wanted to try a hospital job, to give me more clinical work.
I took a one-year fixed term contract, thinking it would be a year of me trying out what a hospital was like, and then probably going back to the community. I haven’t left hospital optometry since. It’s been eight years now.
Do you do any other work or volunteering alongside hospital optometry?
I’ve just been accepted as a council associate with the General Optical Council (GOC). It’s a two-year post, and I will hopefully get some experience of the inner workings of the GOC. I’m excited to get into something different.
You also work as a locum in practice. How does your hospital role support you in your High Street optometry work?
Immensely. Since I’ve worked in hospital, I’ve seen all the complex and unexpected cases that come through. When I see somebody with pathology in the community, I feel more confident in explaining it to the patient, managing them, and knowing how urgently they need to be referred. That comes from having known what happens on the other side.
How does working on the High Street benefit you in the hospital setting?
They go hand-in-hand. On the High Street, you can refine your routine and know what a patient wants in terms of screening for eye examinations, but also information about glasses and contact lenses. When I see patients in the hospital in a contact lens or a refraction clinic, I have that understanding of what it’s like when they go back to the High Street. It’s about giving the patient as much information as possible about their options.
What is the biggest challenge facing hospital optometry currently?
Opportunities outside of the hospital, which are perhaps more financially rewarding. Working within NHS hospitals is incredibly



rewarding. But increasingly, with the cost-of-living crisis, people are starting to look elsewhere.
What is your biggest success in the past three years?
I’m currently working towards a Master’s degree in advanced clinical practice in optometry and ophthalmology. I’ve also completed my independent prescribing qualification. I think my personal success is in trying to collate as much experience, education and qualifications as I can.
NAME: Rupa Patel
ROLE: Specialist optometrist, Moorfields Eye Hospital
LOCATION: London
What would you say to optometrists on the High Street about working in the hospital?
It’s incredible. If you want more interesting, varied cases, and a way to challenge yourself, hospital optometry is great.
Read more hospital insights online: www.optometry.co.uk/you-had-me-at-hospital
One valuable moment
I had a keratoconic patient in a contact lens clinic, whose vision was deteriorating. He was only reading down one side of the chart, which was unusual. I did more examinations, and sent him for a visual field test. He had bitemporal hemianopia – a potential sign of a compressing lesion. I urgently referred him to A&E and neurology, who found he had a pituitary tumour. He was very grateful that I took the time to do those extra tests. It made me realise that, if something doesn’t feel right in a contact lens clinic, it doesn’t mean you just focus on the contact lenses. You have to look at the whole picture.

“PRE-REG HAS GIVEN ME A GREATER
THE
As OT’s 2023–2024 pre-reg contributors approached their OSCEs, they shared what they have learnt in their first year of optometry practice
What was the standout moment of your pre-reg placement?
Hayley Smith (HS): Getting my Stage two results. My overarching and direct observation assessments were two weeks apart, which made the wait unbearable.
Lizzie Shaw (LS): Taking the first low vision appointment for a patient with age-related macular degeneration. Supplying magnifiers and leaflets, and knowing that someone could help with the patient’s visual problems, was extremely gratifying. She expressed to me what a difference it would make to her life.
What has been your scariest or most intimidating moment?
HS: When I had to do my first emergency referral, whilst also having a full diary. Trying to juggle the diary whilst also trying to get through to the triage nurses and write a referral letter was intense.
LS: During my community placement, when I saw a patient with bilateral extremely swollen discs, alongside significant sub-retinal and intra-retinal fluid. We sent the patient to A&E immediately. This was my first ocular emergency, and although I was glad we’d seen the patient, I was also very concerned for him. His vision was still 6/6 in both eyes.
Oran O’Connor (OO): At the start of pre-reg, when I was beginning to see real patients for refractions and contact lens appointments. This was the first time I had done this since university, and I had little confidence in my own ability. This was a feeling that lasted for some time – gaining confidence in dealing with patients was a gradual process.
Have you thought about your plans for after qualification?
HS: I am lucky to be able to stay at Peter Ivins Eye Care when I am qualified. I am very grateful and excited, after building a great rapport with the patients and staff as well as having the opportunity to take part in specialised clinics.
LS: I’ve started to look at PhDs for after I qualify. I have been interested in research since my second year at university, and would love to pursue a research-based career. I would hope to be able to take some bank shifts in hospital though, to keep my hand in.
OO: After pre-reg I’d love to continue working in my current practice. I’ve formed a good relationship with my supervisors, and they can help me on my journey when newly-qualified. I would like to gain further qualifications, broadening my knowledge, to become the best optometrist possible.
Did you have any misconceptions about optometry before you started your pre-reg?
HS: I didn’t realise how much information you can get about the rest of the body and a patient’s general health just from the eyes. It’s amazing.
“Gaining confidence in dealing with patients was a gradual process”
Oran O’Connor, pre-reg optometrist





LS: I am sometimes surprised by how patients view optometry and our role as optometrists. I had an afternoon in urgent care recently, and every patient we saw could have been seen in a High Street practice, but had chosen to come to A&E. We have a long way to go in encouraging people to visit an optometrist for problems beyond needing an update in spectacles. More education on how extensive the role of an optometrist can be could help to cut hospital waiting times and improve patient experience.
OO: Pre-reg has given me a greater appreciation of the role that optometrists play in people’s lives. Patients are also increasingly understanding how their optometrist plays a vital role in allowing them to see clearly.
Where do you see yourself in five years’ time?
HS: I would love to continue broadening my skills and expertise by delving deeper into the specialist clinics at Peter Ivins Eye Care, including visual stress, scleral lenses and dry eye. I am also planning on doing independent prescribing to allow me to prescribe and manage a greater range of pathology.
OO: There are many career pathways with Specsavers, including support for gaining additional clinical qualifications. This would allow me to offer my patients the best possible care. Over the next five years, I would like to build up a good reputation as an optometrist and be somebody who patients want to see.
Any regrets from your pre-reg placement?
HS: Pre-reg is full on, so it’s easy to lose that work-life balance. Although you do have to make sacrifices to ensure you’re on track for every assessment, I wish I was able to find a better balance as I think this would have stopped me getting overwhelmed during the harder stages.
OO: I might have gone through the different case scenarios earlier, as I found them useful in terms of how to think about each patient individually –what questions I should ask, what tests I should do, and how I should manage them. This would have been useful early in the year.
LS: There are four pre-regs in my cohort at Moorfields. I would try not to compare myself to the others so much. Pre-reg is tough enough, and everyone will have a different approach and timescale. We all have the same goal, and however and whenever we complete it is ok. I am lucky to be surrounded by such intelligent, supportive, and high-achieving peers.
0
“I had an afternoon in urgent care recently, and every patient we saw could have been seen in a High Street practice, but had chosen to come to A&E”
Lizzie Shaw, pre-reg optometrist at Moorfields Eye Hospital

















The AOP offers a newly-qualifed grade for optometrists during their first year of qualfication. To upgrade your membership when you qualify to continue to access the benefits that come with being an AOP member, contact the AOP’s membership team on 020 7549 2010.

06:30
I try to wake up as late as possible, but it’s generally about half past six. The first thing I do is get a cup of coffee.
My son has a learning disability, so he has a very particular morning routine. He goes to a special needs school, and gets a taxi there. I sort out his packed lunch, then we’ll be waiting for the taxi, hoping it comes on time so I can get to work on time.
08:30
If the taxi is on time, I arrive at the practice at about half past eight. My first task of the day is turning on all the machines. I’ll turn the bubble walls on, and look at the clinic to see who is coming in. We specialise in people with learning disabilities, and there are often also a couple of Minor Eye Conditions Service (MECS) patients.
08:45
We have a huddle with all staff at quarter to nine, to discuss what is coming up that day. The idea is to talk through the pressure points, and see what we need to be aware of.
11:00
We have a very busy practice, with a lot of technology. My main tasks vary, depending on which patient is coming in. We always keep one emergency slot free in every clinic. If a MECS patient phones, even if they are not our patient, we’re responsible for that person, so we need to get them in somewhere else. If it is our patient, we will try and squeeze them in at the end of the clinic or at lunchtime.
Simon Berry, optometrist and owner of Simon Berry Optometrists, talks OT through his day – from mornings with his son to evenings with sci-fi novels, TV thrillers and piano music
NAME: Simon Berry
ROLE: Optometrist and practice owner at Simon Berry Optometrists
LOCATION: Durham
My fantasy practice...
12:30
I never used to have a lunchtime. Now, if I miss lunch, my head is not right by the end of the day. I’ll nip out of the practice for at least 10 minutes, to walk around and get a bit of fresh air. I live three miles away, so I might go home and let the dog out.
13:30
We have a good staff communication system, where the practice management software has a to-do list and records all messages. That’s always live. I look at it between patients to see what else I need to do. The end of lunchtime is a bit of a catch up with that.
17:30
On a good day, I leave the practice at half past five. It’s always busy. We have a recruitment problem in the north east. We have a long waiting list. I like playing the piano, so I use that as stress relief.

19:30
To unwind in the evening, I read... sci fi novels
I’ve always got a couple of books on the go. We like watching half hour comedies in the evening, too. My wife likes thrillers such as Luther. We don’t really have a go to mid-week dinner – as long as it’s relatively quick and easy to make, and to put away afterwards.
Read more business owner stories online: www.optometry.co.uk/a-day-in-the-life
We see lots of people with learning disabilities, and we’re doing a lot of good with that. But every time we do that, we lose money. With an unlimited budget, we could do as much research as we wanted, and see more people with learning disabilities. I truly believe that having a practice is not about making money. I don’t want to just make money and retire. I want it to be there to have done some good, and to have built something, and to be part of the community. That’s the wildest ambition – that it’s done some good, and it still exists.
Regenerates dry and irritated eyeli provides preventative care for sens
10ml (0, Dryness + Flaking + R

AVAILABLE TO ORDER NOW


OT presents a clinical scenario to three of its resident IP optometrists. Here, a man with a recent diagnosis of herpes simplex keratitis presents looking for a second opinion
The scenario:
A 47-year-old man explains that he has been diagnosed with herpes simplex keratitis at a local practice. He was prescribed an aciclovir gel, which he has been using for six days without improvement. He is not satisfied, and is seeking a second opinion. How would you manage?
OT’s panel says...
Ankur Trivedi: I would start by ascertaining as many of the facts as possible. How often per day was the patient asked to use the gel, and has he done so? Does he have any history of similar episodes? I would also be keen to ascertain which exact aspect he is reporting no improvement on – visual acuity, pain or discomfort, or some other parameter? It would be useful to know how the issue
was at presentation, so I would ask permission to contact the original independent prescriber (IP), to give me an idea of that.
Kevin Wallace: I would encourage the patient to go back to the practice and explain what he has told me. It is best to continue with the care provider, especially as I don’t know what his presenting symptoms were.
When treating any eye condition, I tell the patient that if it is not doing what I expect it to, particularly in a more serious eye condition, I want to see them again promptly.
I would be worried if he said his eye was still painful and photophobic. If he didn’t want to go back to the previous practice, he would need to be examined again to gain confirmation that the initial diagnosis was correct.
It is important to verify that he has been using the medication appropriately. Depending on the circumstances and the findings, we can then modify treatment.
We have to be careful in using steroids for herpetic eye disease, but with appropriate anti-viral cover they are sometimes necessary. It is important to consider if you should treat this patient or seek advice from the local eye department – particularly because a delay of a few days in receiving appropriate treatment can lead to a worse outcome.
Ceri Smith-Jaynes: If one of my patients wasn’t improving from my treatment plan, or they weren’t happy with the service, I’d wish to know. Feedback is a means to improvement. IPs need to work together. The fact the treatment isn’t working, after six days, is a way of forming a new diagnosis. I have treated a few simple, epithelial, herpes simplex keratitis cases and they’ve healed with ganciclovir gel. It is cheaper and more gel-like, so nicer to use than aciclovir ointment, with similar effectiveness. We need to consider some differential diagnoses:
• It is herpes simplex, but is it in the stroma or endothelium? College of Optometrists Clinical Management Guidelines list this as A1 referral to ophthalmology
• That the lesion the first optometrist saw got infected by bacteria
• Acanthamoeba keratitis: contact lens wearers with dendritic ulcers are another A1 referral to ophthalmology
• Is it another organism, for example, fungal keratitis?
• Medicamentosa: the lesion got better, but the patient has a sensitivity to the paraffin in the ointment
• Is it actually filamentary keratitis, which looked like dendrites on presentation?



Kevin Wallace
OCCUPATION: AOP clinical adviser IP QUALIFIED IN: 2012



Ceri Smith-Jaynes
OCCUPATION: Clinical multimedia editor IP QUALIFIED IN: 2018



Ankur Trivedi

OCCUPATION: IP optometrist IP QUALIFIED IN: 2014


Specsavers Bristol Merchant Street was the first practice to trial an out-of-hours homeless clinic that is now being piloted at 44 locations. OT spoke to contact lens partner, Sarah Mcgowan, and store supervisor Karin Ferrandi
Initial relationship building Sarah Mcgowan (SM): Our practice is close to the Compass Centre, where Vision Care for Homeless People (VCHP) clinics take place, so we were invited to an open day. It was an interesting opportunity to meet lots of different people. That’s where we met Stan Burridge, who is in charge of Expert Focus, and members of the focus group of people with lived experience of homelessness.
As a city centre practice, we see homelessness every single morning and every single afternoon, when we come to and from work. Bristol city centre is particularly affected, so we wanted to do something to help, and
it seemed to be perfect timing and a perfect opportunity.
We were the first practice to join Specsavers with Expert Focus. The group came in for sight tests and dispensing. We went through a normal customer journey with them, and then had a feedback session one evening after work where we put on some food. We had a really nice feedback session, discussing where the stumbling blocks would be.
Karin Ferrandi (KF): We discussed how we could be more inclusive for people coming into the practice. Stigma is the biggest barrier. Even if you are given the possibility of a free sight
test, it’s hard to walk into a practice. That could be a daunting experience. A person experiencing homelessness might have a number of worries and preoccupations, and they might not be able to keep up with appointments. They might not have a phone. They might not want to know if there’s something wrong, because that means that they have to reach out for further help. So, it adds an extra worry. Experiencing homelessness is not a label. This is not who you are. Yes, at the moment you might feel disconnected. Interpreting cost could be confusing, and you might end up having to admit that you don’t have the money to pay. That is a vulnerable thing.

KF: We had to learn to adjust our ways quite a lot: to be more inclusive, and to be more attentive to people with emotional needs – to offer that extra 10 minutes for a chat. Just asking that person how they feel or how it’s going can make a huge difference.
I don’t want to make a division between people experiencing homelessness and customers. If we get NHS customers they get everything for free; we’re not asking for a penny. A person experiencing homelessness is no different. Everybody needs a safe space, and that can be created by explaining what’s happening during a sight test. Be clear about what each step of their journey is. If they want to open up, don’t rush them. We can make a difference to vulnerable people’s lives when we take that extra care.
SM: It has given the team a lot of pride. Focusing on working within local communities and making a difference has been empowering. From a business point of view, we are making a difference that is tangible.
Challenges from year one
SM: Trying to get clinics booked and filled has been challenging. Working with the focus group has helped with those questions: how can we get people to come into our environment? How can we make it safe?
NAME: Karin Ferrandi ROLE: Store supervisor, Specsavers Merchant Street
KF: Our biggest challenge is trying to engage patients. The fact that they often live transient lives means it is challenging for them to reach out and for the clinic to set a stable routine.
We want to be more out there in terms of outreach. The more people who know about the service, the more people will come, and the more free clinics we will establish.
Clinics that offer free services do work. But it takes time. It has to be consistent, and clinic users need to hear via word of mouth. The more people we can see, the more people are going to spread the good news, and the more people are going to show up. It needs more one-to-one engagement. We have to provide a compass point, which is a physical person, not a portal. We need to prove that we are human.
SM: There’s a lot of work that we need to do around what is covered, and what is available. We need to clarify that message, to make it easier for people to understand.
KF: When people walk into a store, we need to provide them with all the tools to make an informed decision and to feel empowered and in control of their care. Big projects and big social changes don’t happen overnight.
Read more in this series online: www.optometry.co.uk/a-conversation-about






NAME: Sarah Mcgowan ROLE: Contact lens partner, Specsavers




LOCATION: Bristol







With registration for 100% Optical set to go live in September, OT heard from organisers about plans for the show
September sees the supermarket shelves stocked with a rainbow of fresh notebooks, neatly arranged stationery, and impractical pencil cases, marking the beginning of a new year in the academic calendar for learning and growth.
But the month also heralds another horizon for learning and development, as September brings the opening of registration for 100% Optical 2025.
Tuesday 3 September will see registration go live on the 100% Optical website for delegates to secure their spaces at the show, taking place at ExCeL London on 1–3 March.
Independent eyewear
Selin Pera, senior marketing executive at 100% Optical, told OT: “One of our core values is to open up the doors for the next optical generation.”
“Back in 2020, we introduced 100% Studio, a dedicated area for independent brands from around the world creating unique, sophisticated and trendy designs. Within this space, we ensured we had a mix of every price point, from affordable to high-end luxury,” Pera explained.
For the 2025 event, the 100% Studio will be moved from the corner of the eyewear section of the exhibition further into the show to ensure delegates do not miss the curated selection of independent eyewear.
In moving the space, organisers have also expanded the 100% Studio, with more brands joining the area.

Sponsored by Nikon Lenswear UK, the Nikon bar will have multiple happy hours across the three-day event to support a fun experience while networking.
Newmedica has also been confirmed as a sponsor for the 2025 show, with Rebecca Lythe, managing director, telling OT: “We’re looking forward to being part of 100% Optical in 2025 and talking to optometrists who do so much for eye health communities up and down the country.”
“Following the success in 2024, our own specialist consultant ophthalmologists will be on hand again running a range of new and engaging CPD sessions for our colleagues in primary care as well as being on our stand to answer your questions,” Lythe continued, adding: “Together we can deliver better patient care. We look forward to welcoming you.”
Organisers of 100% Optical explained that 200 exhibitors are already signed up for the show, including Zeiss, Rayner, Haag-Streit UK, Altris AI, Roger Eyewear, La Font, and Nine Eyewear.
SpaMedica is another confirmed sponsor for the 2025 show, with its marketing manager, Alex France. commenting: “We’re always thrilled to sponsor and exhibit at 100% Optical. It’s a fantastic opportunity to see and hear about all the latest developments in the sector, spread the word about SpaMedica’s expanding services, and deliver informative CPD sessions to a national audience.”
“We really enjoy catching up with optometrists from across the country and meeting other industry experts, and we can’t wait to see what the 2025 event has in store,” France added.
The AOP’s collaboration with 100% Optical continues in 2025 as education partner for the show, developing a programme of CPD.
Reflecting on last year’s show, Dr Ian Beasley, head of education at the AOP and OT clinical editor, commented: “2024 marked the 10th anniversary of the event and was the most successful yet, attracting nearly 12,000 visitors across the three days.”
He told OT: “The CPD programme development for 2025 is in full swing, with plans to increase capacity in education sessions to keep pace with the year-on-year growth we’ve experienced since the event’s inception.”
January 2025 marks the beginning of a new CPD cycle, with 100% Optical presenting an opportunity to kick-start registrant’s progression


towards their development goals. “As we enter the first year of the new CPD cycle, attendees will benefit from access to a range of peer review sessions, discussion workshops and lectures on topics aligned to contemporary practice,” Beasley said.
For more details, and to secure your space at 100% Optical 2025, visit the website: www.100percentoptical.com 0
The current CPD cycle ends this year, with registrants responsible for recording points earned by logging into their MyGOC, and navigating to MyCPD. Remember, OT produces regular CPD content online. Find it all at: www.optometry.co.uk/cpd
OT heard from four of the AOP’s new Councillors about the issues at the forefront of their minds when it comes to the profession – now, and in the future
WORDS: KIMBERLEY YOUNG

The AOP Council welcomed new Councillors in June, representing optometrists and dispensing opticians all over the UK and across career stages.
To learn some of the key issues affecting the profession today, and the challenges that might arise in the future, OT heard views from AOP Councillors: Bonnie Lam, representing undergraduate student optometrists, Johnathan Waugh in Scotland, Martin Sweeney in Wales, and Sarah White, representing dispensing opticians.
Advancing skills and scope
Optometrist and practice owner, Waugh, reflected: “I think, with the General Optical Council (GOC) changes to the undergraduate programme, and the potential de-regulation of refraction, we have faced some pretty big issues recently which we seem to have got through.”
“I think optometry is probably in a stronger position now than it was


a few years ago, however, there are always risks going forward,” he said.
There is a trend towards higher clinical skills amongst the profession, Waugh suggested, though a balance is still required with providing appropriate remuneration for this work.
“In Scotland, thankfully our General Ophthalmic Services (GOS) examinations are paid at a higher fee, which gives us a little bit more income,” he noted. “It’s also given us a bit more scope to undertake more advanced clinical work in managing conditions, which is more interesting for all of us,” he added.
One example has been the NHS Community Glaucoma Service, which is being rolled-out across Scotland to enable patients who have lower risk glaucoma or ocular hypertension to be discharged to receive care from accredited providers in the community. The providers are independent prescribing (IP) optometrists who have completed the NHS Education for Scotland Glaucoma Award Training (NESGAT) qualification.

Waugh shared: “Having worked in the glaucoma service, I’m looking forward to this.”
Optometry student, Lam, also identified changes in optometry education as a key issue affecting the profession currently.
The change in the GOC’s education and training requirements has seen optometry schools refreshing and relaunching their degree programmes, moving to a Master’s model.
The new education requirements will see placements embedded into courses, while the current Scheme for Registration will end.
Lam shared: “I think many students are worried about what will happen if graduates are going to be completing a course that is more advanced than those who are currently on the pre-reg pathway.”
Students also have questions about what the new approach to patient-facing clinical experience will look like, Lam suggested.
While undergraduate optometry is changing across the country, the programmes may look particularly different in Scotland – delivered over five years and with an ambition to include IP training.
The changes could be beneficial for pre-reg optometrists in Scotland, Waugh felt, explaining: “I think they will get a better experience from it. But it suddenly becomes a two-tier profession, which I think would be a shame.”
“I think the risk is not necessarily a bad one for Scotland, but it might be to the detriment of UK optometry, and I’ll do what I can to try and make sure that we don’t drift too far apart,” he added.
Considering the challenges facing the profession, Waugh suggested that there is a risk in the devolved nations “moving in slightly different directions.”
“I think it would be wrong for us all to separate and go our own ways, because we’ve got a lot to learn together,” he shared.
Optometrist, Sweeney, shared that the key priority for him currently is: “How to progress further with the latest Welsh GOS scheme.”
The new contract came into effect in autumn 2023, bringing with it a new framework for service delivery in community optometry.
With the new contract in place, designed to enable optometrists and dispensing opticians to work to the top of their clinical licence, there could be new opportunities for the optometry profession, including in helping to address pressures facing eye care.
Sweeney told OT that coping with the strained hospital eye service is a challenge for the optometry profession, in particular determining: “how to best help our patients with that.”
“Waiting lists are bad and are not getting better. The hospitals are desperate to get cases out of the hospital eye service and moved somewhere else,” he shared.
“We are pushing on an open door. Previously, there was a lot of in-house resistance and protection of home turf,” Sweeney explained.
He continued: “Those arguments don’t hold anymore. This gives us an opportunity to
branch out our skills, and we should grab that opportunity.”
The biggest opportunity going forward is “pushing to further advance our clinical skills within the remit of Welsh GOS,” he added.
The ageing population
Dispensing optician, White, told OT: “The issue burning in my mind at the moment is forward planning for the population ageing and making sure that we have the ability to deal with whatever comes to us.”
The practice owner and director also agreed that one of the biggest challenges facing the sector in the past year has been the backlog in ophthalmology. She said: “I think it is the waiting lists and the fact that people are waiting to a point where they are losing some of their sight.”
Continuous development as eye care professionals presents an opportunity to help address some of these growing challenges.
White suggested: “Upskilling is a way to try and get more into primary care so that it can be dealt with, and so we are not adding to the waiting lists that people are sitting on.”
For White, upskilling is a major opportunity for dispensing opticians in particular, especially in the areas of dry eye and myopia management.
“We can, whether in the short-term or longterm, reduce the burden and need for secondary care appointments and that has got to be a benefit,” she said.
“From a dispensing optician’s point of view, the more ability you have, the more independence you have in certain situations,” White shared, adding that this also improves job satisfaction.
At an AOP Council meeting on 5 June, White discussed the challenges facing dispensing opticians when it comes to continuing professional development. (Read the report at: bitly.cx/9LT8).
Lam agreed that the question of how optometry can advance services to meet the needs of the ageing population poses a key challenge for the profession going forwards.
“I think it is a good thing that we can encourage more optometrists to undertake further study in higher certifications,” she shared.
Giving the example of glaucoma, Lam suggested seeing more patients in the community could mean only sending those patients who really need the hospital service into secondary care.
The application of artificial intelligence (AI) presents some opportunities for the profession, Lam suggested, but this area

of technology also presents ethical and regulatory questions that need resolving.
“Of course you want to provide a better service to the patient and AI can help us a lot. But we still have to find the balance,” she said, adding: “I think it’s probably one of the most exciting areas in optometry.”
Waugh also sees the emergence of AI as an area of both opportunity and risk for the profession.
Considering the role that AI could play in the future, Waugh shared: “As a clinician, I’m still uncomfortable with machines taking over the investigative work I do. I’m happy for technology to be taking the images, which I then interpret. I don’t really want AI to be taking on my clinical work, so I think there is a risk.”
In the future, it is possible that practices will differ in their approach to technology, with some taking the automated route and others remaining on a more traditional path.
“Technology is there to support what we’re doing,” Waugh said. “I think for each individual, it’s about doing what you’re comfortable with, doing it well, and seeing where the future goes.”
AI is already used in the diabetic screening service that Waugh is a part of, helping to grade some images. He noted:

“This actually saves us time and effort, although the grading isn’t always accurate,” he noted.
Read more about new AOP Councillors, and their views on the public’s perception of optometry: www.optometry.co.uk/ professional-support/aop


OT meets the optometrists who are helping to ease the burden on overstretched GP practices
On an avenue lined with hanging baskets, there is a fried chicken shop, a bakery and bank.
While the streets of Barnoldswick, Lancashire may seem similar to many other English towns, the attitude of its 10,913 residents to eye care is gradually shifting.
If a patient turns up at the pharmacist with a painful red eye, they are directed next door to
the green frontage of James Bontoft’s optometry practice. Around the corner, at the town’s only GP practice, it is the same story.
“Once they hear the word ‘eye’ or ‘vision,’ they say ‘Go see the opticians’,” Bontoft shared with OT.
Bontoft qualified as an independent prescribing (IP) optometrist in 2013 in one of the first cohorts to go through the specialist training. Since then, every working day he has been treating conditions that
“
I didn’t want to sit in a room saying ‘One or two?’ all day”
Drew Thompson
patients would traditionally present to a GP practice or hospital with – from infections and allergic reactions, to dry eye and viral keratitis.
He has painstakingly removed flecks of metal and rust rings from the eyes of welders and metalworkers who manufacture fan blades for a nearby factory.
More than a decade after he started prescribing, Bontoft is still greeted by the occasional look of surprise when he explains what his practice can offer.
“It’s been a very slow process, but we are certainly fostering the idea that if you have an eye problem, you come to see me,” he said.
At a UK level, a significant proportion of patients continue to view their GP as the first port of call. An AOP online survey of 1016 members of the public in May found that 32% of respondents would approach their GP first for an eye condition.
These results come at a time when NHS Digital data shows that one in five GP appointments in April was scheduled two or more weeks from the date of booking.
Dr Stuart Bryan, a GP partner at Barnoldswick Medical Centre, shared that the service provided by Bontoft has eased pressure on his practice.
“Due to the current and ever-increasing pressures in primary care it does make a difference to our workload having this service,” he said.
Bryan shared that he felt confident referring patients to Bontoft knowing that they would be seen quickly and have a thorough assessment.
“Having James literally on the doorstep is a real bonus. It is really easy to get through on the phone to organise a same day appointment and if needed speak to the optometrist to pass on our concerns and differential diagnoses,” he said.
Burnley General Teaching Hospital is two bus rides away from Barnoldswick or a half hour drive.
An initial motivation for Bontoft to become IP-qualified was to provide convenient care to the local community.
However, as one of only three community-based IP optometrists who are actively prescribing in East Lancashire, he is now seeing patients from towns 45 minutes away by car.
“We are getting a lot of referrals from the hospital now. Our eye department is pretty much at capacity,” he said.
Bontoft’s area has had a minor eye conditions service (MECS) since 2001. There are funded services for low vision, glaucoma referral
refinement, as well as pre and post cataract services. Plans are currently underway to refer stable glaucoma patients from Burnley General Teaching Hospital to be monitored within optometry practices.
Although there are funded schemes in place, Bontoft must keep the financial sustainability of his independent practice in mind.
“Capacity sometimes becomes an issue because I’ve got to have enough normal sight testing patients to make the day fund itself,” he said.
At the moment, Bontoft allocates around 18 appointments each week for IP patients. To avoid turning people away, he will work through his lunch break, start early, or finish late.
He finds that offering IP services has helped to build loyalty and grow his patient base.
“I wanted to do it from a personal interest point of view – it works for me and it works for my practice,” Bontoft shared.
He would like to see more optometrists become IP qualified in his area to distribute the workload and ensure patients are seen closer to home.
“My message to other optometrists is: do it. Be part of the change,” Bontoft said.
The IP crowd
Drew Thompson is an IP optometrist and the owner of Thompson & Hardwick Optometrists in Lytham Saint Annes.
Each month, he sees an average of between 90 and 100 patients for conditions ranging from blepharitis and conjunctivitis, to the removal of foreign bodies. Thompson, who works half a day each week in a hospital cornea clinic, also offers contact lens fittings for patients with keratoconus and ocular trauma in practice.
He shared that becoming IP-qualified was part of his professional development. “I am always looking to further myself. I didn’t want to sit in a room saying ‘One or two?’ all day,” Thompson said.
“ My message to other optometrists is: do it. Be part of the change”
James Bontoft

Withinhishospitalwork,thequalificationalso meansthathenolongerhastotapadoctoronthe shouldereachtimeheneedstoissueaprescription.
Thompsonsharedthatwithinhisarea,most patientswillstillapproachaGPorpharmacistfirst withaneyeproblem.
“I’dlovetoseethatchange.I’vebeentalkingabout thatwithmypatientspersonally,butitdoestakea whiletochangeperceptions,”hesaid.
Thompsonaddedthatitisgenerallyeasierfor apatienttogetanappointmentatanoptometry practiceandthepatientisultimatelybetterserved.
“Ourprofessionhasmuchmoreknowledgeabout eyesthanageneralpractitioner.Thepatientoften getsaresolutionsoonerbecauseweareabletotarget thetreatment,”hesaid.
IPoptometristandOTmultimediaclinicaleditor, CeriSmith-Jaynes,treatspatientsthroughthe communityurgenteyecareservice(CUES)Lytham StAnnesbranchof BroadhurstOptometristsand throughMECSatthePrestonbranch.
“Currently,mostthingsaremanagedtoresolution intheoptometrypractice,”sheshared.
“Thepatientsaregratefulatnothavingtopresent tohospitalandtheyaremanagedatanappointment timetosuitthem,inaconvenientlocation,”SmithJaynesobserved.
Shewillsometimesseekadvicefromthehospital beforeprescribingmedicationandarranginga followupappointmentatthehospitalwithina coupleof days.
DatasharedbytheAOPaspartof itsOnemillion appointmentscampaignhashighlightedthat around1.35millionGPappointmentsaretakenup withhayfever-relatedeyeconditionseachyear.
Smith-Jaynessharedthatwhilehayfeverdoes notfallunderthecurrentCUESspecification,she willoftenprescribeprivatelyforthecondition.
“Patientsdon’twanttobothertheirGPand prescriptionmedicationcanbebetterthantheoverthe-countermedication,”shesaid.
ThroughherroleattheGatesheadcommunity lowvisionclinic,optometrist,StephanieCairns, isprovidingpeoplewithalevelof personalised
Low vision assessments
Gateshead optometrists (or optometrists who have patients with a Gateshead GP or address) can refer patients directly to Sense Ability Matters with the email: sightservice478.team@nhs.net. Local optometrists outside of Gateshead can refer patients for sight loss support by contacting eye clinic liaison officers: Newcastle upon Tyne Hospitals nuth.eclo@nhs.net
Sunderland Eye Infirmary stsft.sei.eclo@nhs.net
RNIB single point of access rnib.waitingwell@nhs.net
carethatcannotbeofferedina10-minuteGP appointmentorbusyhospitaleyeclinic.
SenseAbilityMattersprovidesholistic supporttopeoplewithsensorylossinGateshead andSouthTyneside.
Afterareferral,thepersonwillbecontacted within48hourstosetupaninitialappointment todeterminetheirneeds.Afterthis,theywillbe referredtoarangeof availablesupport,including lowvisionwhereappropriate.
“It’sverydifferentfromhowthehospitalsystem works,whereyoucanrefersomeoneandtheymay sitandwaitforfourtosixweeksfortheirfirst appointment,”Cairnsexplained.
Thecharityemploysavisualrehabilitationofficer, whowillmakehomevisitstoseeif anyadaptations arerequiredandassistwithmobilityandorientation.
Thereisalsoadigitaltechnologyspecialist,who canprovidepeoplewithfreesupporttoenableaccess todigitalmagnifiers,virtualassistants,mobile phonesandtablets.Includingtimeforpaperwork, Cairnshasaroundanhourandahalf foreach appointment–whichgiveshertimetobuildtrust withpatients.
“
Some people are quite guarded. For ages, they’ve been telling everyone that things are ok”
Stephanie Cairns
“Somepeoplearequiteguarded.Forages,they’ve beentellingeveryonethatthingsareok,”shesaid.
Cairnswilltailorthesupportandequipmenttothe personbeforeher–fromtalkingclocks,magnifiers andlightingsolutionstoanti-glarelenses.
“Whenyouexplainthatyouaregoingtobeable togivepeoplethisequipmentfreeof chargeyoucan visiblyseethemrelax,”shesaid.
Asidefromequipment,Cairnsaddedthat sometimesitistheintangiblesupportthatpeople appreciate.“Somepeoplebenefitmorefromhaving achatbecauseitmaybethefirsttimeanyonehas actuallyspentthetimelisteningtothemandwalking themthroughwhathasbeengoingonwiththeir vision,”shesaid.
ThesupportofferedbySenseAbilityMatters helpstoreducepressureonotherpartsof the healthservice–forexample,byreducingtheriskof falls,helpingpeopleinstileyedropsproperlyand

enablingthemtoreadtheirinsulindevices.“Wehave beenabletohelppeoplecontinuetomanagetheir medicationbythemselves,”CairnssharedwithOT
PeoplearereferredtoSenseAbilityMatters througharangeof avenues,includingeyeclinic liaisonofficers,thecommunitynursingteamand thehousingassociation.Cairnswouldliketosee moredirectreferralsfromoptometrypractices withpatientswhoareGatesheadresidents,asoften referralscomethroughafterapatienthasbeen certifiedasvisuallyimpaired.
“It’sreallyimportantthatpeoplegetaccessearlier. Oftenwhentheycometome,theyhavealreadygiven upandyouhavetoreignitethatmotivation,”she sharedwithOT.
Optometristsshouldnotassumethatapatienthas alreadybeenofferedsupport,Cairnsadded.
“If you’vegotsomebodywhoyouthinkcould benefitfromhelp,andtheyarehappytobereferred, thengetintouch,”shesaid.
BernieMcColl,whohasdiabeticretinopathyand bilateralmacularischemia,sharedwithOTthatshe appreciatesthewaythatCairnslistenstoherand givesexplanationsinawaysheunderstandswhen shecomesinforanappointment.
“Youseethesamepeopleeachtime.There’sthat familiarity–itfeelsmorelikeafriendshipthana clinic,”McCollshared.
Throughtheservice,the72-year-oldhasreceived magnifiersandadaptationsinherkitchentomake cookingeasier–suchashighlighterstripsandaone potboiler.Shesaidthatthereisnotthesametime pressurethattheremightbeinaGPappointmentor atthehospital.“If yougotoaGP,theyaretalkingto you,buttheyarelookingattheirscreen.You’renot sureif theyarelisteningtoyouproperly,”shesaid. Herdaughter,KerryDezayi,whoalsoattended McColl’smostrecentappointment,added:“The doctorstalktoyou.IthinkStephaniewastalking withyou.”
McCollbecameworriedrecentlyaftershebegan seeingstrangethings–suchasapersoninthecorner of theroomorabirdoutof thewindow.
ShesharedthatCairnsexplainedthatthese hallucinationswereasymptomof CharlesBonnet Syndrome.“Iwasrelaxedaftershetoldmethat.I thought,‘I’mnotgoingcuckoo.’Before,Iwouldpoint somethingouttothegrandchildrenandtheywould say‘Ohnana,notagain’,”sherecalled.
Dezayishared:“WhenshetoldmumitwasCharles Bonnet,itreassuredherthateverythingwasfineand normal.Sheexplainedinlayman’stermsthatitwas thewaythebraincompensatesforeyes,whichmakes perfectsense.”
McCollobservedthatsheappreciatesbeingable totalkwithpeoplewhounderstandthechallengesof


“ It can be a very lonely world when you cannot see properly”
Bernie McColl
livingwithsightloss.“Itcanbeaverylonelyworld whenyoucannotseeproperly,”shesaid.
GP campaign
Aspartof itsOnemillionappointmentscampaign, theAOPiscallingontheGovernmenttomake investmentinprimarycareapriority,aswellas supportingthedevelopmentof minorandurgenteye carepathways.
AOPchief executive,AdamSampson,sharedthat atpresentunnecessarydemandsarebeingplacedon GPpractices.
“Ourlatestdatashows1.35mGPappointments aloneeachyearareusedtotreatcommoneye conditionsrelatingtohayfever.Andthisisthetipof theiceberg.Millionsmoreappointmentsareusedto dealwithothereyehealthissuesthatoptometrists ontheHighStreetaretrainedtomanage,”hesaid.
AOPclinicaldirectorandoptometrist,DrPeter Hampson,sharedthatoptometristsarequalifiedto treatabroadrangeof eyeconditions,andhavethe capacitytodomore.
“OptometristsontheHighStreethavethe premises,theequipmentandmostcrucially,the clinicalexpertisetodeliverspecialisteyecarethat isaccessible,”hesaid.
0
To get involved with the AOP Onemillionappointments campaign, follow the QR code here


Sponsored by:








EXAMS CLOSE: 26 OCTOBER 2024
This article explores the opportunity of fitting astigmatic patients with toric contact lenses and the impact of the relationship between vision and comfort on retention.
Sarah Morgan BSc (Hons), MPhil, MCOptom
Today’s toric lenses provide access to spectacle-free vision for over 90% of potential wearers.1 We must ensure even the happiest of spectacle wearers know that contact lenses may provide a better vision correction option, at least occasionally. For part-time use, daily disposables are a highly convenient option. The widespread use of computers and digital devices makes the correction of astigmatism an increasingly important part of managing visual needs and the symptoms of ocular comfort.2-7
Ensuring a contact lens wearer achieves all-day comfort is an important goal –both suboptimal comfort and vision are key reasons for discontinuation.8 Asking existing wearers for their ‘marks out of 10’ for comfort is a good starting point to identify those wearers for whom trying a new lens could elevate their comfort scores. Wearers appreciate our care and interest in giving them the best available lenses.
As eye care professionals (ECPs), the management of refractive error is a major aspect of our role. In spite of the affordability, availability and success of disposable soft toric lenses,
there are wearers who continue with compromised vision by using spherical lenses. It is well-established that spherical soft lenses do not mask astigmatism in either hydrogel or silicone hydrogel materials.9-11 Furthermore, vision is clinically significantly reduced (especially in low contrast and wide-pupil scenarios), even for low amounts of astigmatism of around 0.75DC.12 Aspheric design lenses do not optically correct astigmatism.12-13
To deliver comfortable vision for the everyday life of astigmatic wearers, it is important to fit a toric lens when the astigmatism is ≥0.75D in one or both eyes;14 this also helps to reduce perceived discomfort and subjective symptoms of dryness from uncorrected astigmatism.3-4
Globally, one in two new wearers is fitted with a spherical lens, and about one in four is a toric lens (for one or both eyes) – a greater percentage of toric lenses are fitted in the UK at 38%, nearing the proportion expected based on refractive need (≥0.75DC).15
Lenses can be pre-ordered empirically from a known spectacle prescription and tried while visiting the practice for new spectacles, or for existing wearers where torics may need to be considered or a new toric lens evaluated.
Front-of-house staff derive great benefit from shadowing the ECP during the fitting process and being shown the view down the slit lamp to gain
0.5 CPD POINTS
insights into how toric lenses are fitted and what the cylinder and axis mean in relation to visual performance and lens specification; this helps with understanding why a minority of wearers may need a different axis for their contact lenses to their spectacle prescription.
While it is possible to have a limited stock of trial lenses in the practice, it should be appreciated by the practice team that a full selection to cover the requirements of sphere power, cylinder power and axis would need many hundreds of different lenses to be held in stock, which is not practical.
Innovations in manufacturing and design have progressed modern toric lenses to a level where they provide predictably good vision in terms of performance from the empirical lens selected as well as their rotational stability,16 and importantly, astigmatic wearers notice the beneficial impact of toric lenses over spherical lenses.7
Discussing why a toric lens will be beneficial must relate to a patient’s daily environment (for example, at school, home or work) and their leisure time; this will involve explaining the astigmatic requirements of their prescription (for example, low, moderate or high) in relation to both a spherical contact lens versus a toric contact lens. However, this could be the first time the word ‘astigmatism’ has ever been mentioned.
52 Torics today
55 Torics today in practice
58 The evalution and treatment of ocular surface disease prior to cataract and lens-based refractive surgery
It is easy to make astigmatism sound complicated – and optically it is challenging to explain. Beginning with the details of the primary refractive error – ‘short sight’ or ‘long sight’ – and using phrases like ‘you particularly need help with seeing clearly in the distance/seeing up close;’ ‘in addition to this, to give you super clear vision, you need another ‘ingredient’ – something called astigmatism.’ ‘It’s not a disease, it’s simply another part of your vision correction requirement. Most people have some amount of astigmatism, and yours is at a level where it must also feature in your contact lenses – just as it does in your spectacle lenses.’
Be sure to tell the patient that around one in two people benefit from a contact lens for astigmatism in one or both eyes. To help reassure the patient that astigmatism is not a disease, it is helpful to explain where it originates. ‘The coloured part of your eye has a clear layer in front of it called the cornea — and this is very important to the focusing of the eye. The cornea is like a microscopic hill, and differences in the shape of the slopes from north to south and from east to west are what creates astigmatism.’ Endeavour to place the level of astigmatism they have into context, for example, ‘the amount of astigmatism you have is low, and we have some great choices in contact lens availability as you’re so straightforward.’
Most people make their decision based on sound advice from an expert, not on cost. However, they can do this only when sufficient education and information has been provided. Having explained the prescription requirements in full (which may be further demonstrated by removing the cylinder from the phoropter/trial frame to show the impact on vision with and without the astigmatic correction), recommending a contact lens for astigmatism is a natural step.
63 Do we need awareness to ‘see’?
68 Cataract surgery – do you know the risk factors?
A contact lens for astigmatism is clearly a more technological design, and there is usually a natural expectation that it will cost more. While the price is a little more, the benefits (compared with a standard spherical lens) are many:
• Crisp, clear vision
• Better vision for night driving or on grey rainy days
• Reduced eye strain – not needing to squint to see things clearly
• Enhanced visual comfort using a computer.
Allowing prospective wearers the chance to handle the lens beyond the consulting room, and experience them for a few days, is a great way to engage them in the process of evaluating the optimum lens for their needs.
Are toric lenses worth the difference in cost? To be able to convince a prospective wearer of this, it is essential for the ECP to be convinced themselves –treat them like a member of your family. Patients have little experience of the pros and cons of different lens types, so may raise the question of price as it is possibly the only question they can ask in order to explore their options and gain more information. Always remember that a question about price is often a request for more information.
All too often, a recommendation for a toric lens is accompanied by an apology about the price, for example, ‘I’m sorry they’re more expensive...’. In many cases, the patient is unaware of the cost of standard spherical lenses and the cost difference often amounts to only a few pennies per pair. Having thoroughly detailed the patient’s vision correction needs during the examination, the recommendation for a toric lens comes as no surprise, and is therefore, more readily accepted.
It is so important to involve the wearer in the decision-making processes when considering their options, and
Optometrists and dispensing opticians will be able to outline the benefits of toric contact lenses to patients
Optometrists and dispensing opticians will identify why and when it is appropriate to prescribe toric contact lenses
Contact lens opticians will be able to outline the benefits of toric contact lenses to patients
Contact lens opticians will identify why and when it is appropriate to prescribe toric contact lenses.
it is equally important to give them a confident recommendation to optimise their contact lens-wearing experience.
The author of this article is a paid consultant for Alcon.
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd


Sarah Morgan is an optometrist and communication specialist. She is a vision sciences fellow at The University of Manchester.
Headline sponsor
BAUSCH LOMB Workshop sponsors
Exhibitor sponsors

positi/e-impact
NOR!HERN LEfSES
Sponsored by:








This article will consider the indications for toric contact lenses and the clinical steps that can be taken to achieve successful clinical outcomes.
Dr Byki Huntjens PhD, PGDipAP, MSc, BOptom, FBCLA, FIACLE
In 2023, soft contact lenses accounted for 90% of global contact lens fittings, with spherical lenses comprising 50% of those and toric lenses 28%.1 In the UK, practitioners fitted around one in three soft contact lenses as toric.1 Historically, toric soft contact lens fittings were significantly less common;2 this could be attributed to hesitance in prescribing toric lenses, with some practitioners considering minor astigmatism clinically insignificant, favouring spherical lenses for simplicity and cost-effectiveness. However, nowadays the widely accepted benefit of toric lenses is comfortable vision, improving detail perception, and reducing discomfort and dryness symptoms associated with uncorrected astigmatism;3,4 this is particularly valuable for visually active patients and their lifestyle requirements, including work environments as well as activities and interests outside of those. It has also been found that a high modulus soft contact lens material,5,6 a thicker lens,7 or an aspheric soft contact lens design,8 are neither able to mask nor correct all corneal astigmatism even if less than 1.00DC. Nevertheless, some challenges persist with toric lenses, including longer fitting processes, potential vision fluctuations due to lack of lens stability, higher costs compared to spherical lenses, and limited success in those patients with high astigmatism and/or corneal irregularities. The steps of the typical fitting process will now be described.
The first step is to perform a comprehensive eye examination to assess the patient’s vision, ocular health and suitability for contact lens wear including lid position; this includes measuring visual acuity (VA), assessing refractive error, evaluating corneal curvature or shape and checking for any ocular conditions that may affect lens fitting. Research has indicated that lid position, including the upward or downward slope of the eyelids, along with the size of the palpebral aperture, are key patient factors influencing the orientation and stability of contact lenses.9
Corneal curvature or shape is ideally performed to identify: the presence and degree of astigmatism; whether the astigmatism is corneal or refractive, and any irregularities that may impact lens fitting.
Refraction is conducted to determine the patient’s precise prescription, including the spherical power, degree of astigmatism and cylinder axis. The spectacle prescription must be converted to the ocular prescription, by considering the back vertex distance. Online conversion tables can be used or calculated using the formula in Figure 1 (see page 56)
Based on the ocular prescription and corneal characteristics, the eye care practitioner (ECP) can select the most suitable toric contact lens design, including the lens material, base curve, diameter, spherical power, cylinder power and axis.
0.5 CPD POINTS
Optometrists and dispensing opticians will recognise how visual symptoms can relate to contact lens discomfort
Optometrists will identify when and how to prescribe toric contact lenses
Dispensing opticians will recognise the indications for prescribing toric contact lenses
Contact lens opticians will recognise how visual symptoms can relate to contact lens discomfort
Contact lens opticians will identify when and how to prescribe toric contact lenses.
Trial toric lenses are then applied to assess the fit, including the corneal coverage and centration of the lens, its movement with blinks and gaze changes, and the degree of rotation to ensure proper alignment for optimal vision correction. Allow at
least 10 minutes for the contact lens to settle on the eye before evaluating the fit.
A spherical over-refraction will ensure the best possible VA with the toric lenses in place. If the overrefraction also indicates a change in astigmatic axis, check whether the lens axis rotates on blink. If so, consider changing the design to obtain more stable lid interaction with the contact lens.
Once the appropriate toric lenses are selected and fitted, the patient should receive thorough instruction on proper lens insertion, removal, cleaning, disinfection and maintenance; this includes education on hygiene practices, wearing schedules and potential complications to watch for. Typically, a follow-up appointment is scheduled within five to seven days to allow the patient to test the lenses in various real-life settings such as at home, during work and outdoors. The follow-up visit serves to monitor the
patient’s adaptation to the toric lenses, assess their comfort and vision and make any necessary modifications to the fit or prescription.
Regular follow-up care is key to ensure the ongoing health and success of contact lens wear, minimising drop out.
Here is a case study that illustrates these principles in clinical practice:
This patient, a 38-year-old female administrator, who recently moved to the UK, attends for a contact lens aftercare. She reports good health and family history is unremarkable.
She has worn spherical contact lenses, six day per week, typically nine hours per day, for eight years without any problems. More recently, she reports blurry vision at the computer with her contact lenses. She is comfortable with the vision in spectacles, which are three years old. Her end of day comfort score is 5/10.

The patient spends around six hours per day at her computer and is a driver.
Current spectacles:
R -5.25 / -0.75 x 10 VA 6/6
L -5.25 / -0.50 x 170 VA 6/6
VA binocularly 6/6+ N5 @40cm
Current contact lenses: daily disposable, silicone hydrogels.
R -5.50 DS VA 6/6L -5.25 DS VA 6/7.6
VA binocularly 6/6- N5 @40cm
Today’s refraction:
R -5.25 / -1.00 x 15 VA 6/4.8L -5.50 / -1.00 x 170 VA 6/4.8-
VA binocularly 6/4.8 N5 @40cm
Slit lamp examination of her current contact lenses reveals a good fit, slight movement on blink and good coverage in all directions of gaze. Cornea and conjunctiva are clear. Despite visiting the practice later in the afternoon after wearing her contact lenses for seven hours, the lens surface remains clean. Dry spots do emerge on the lens surface approximately six seconds postblink; however, this does not appear to warrant a comfort score of five out of 10 and may be a clue that her perceived lens comfort is influenced by the decreased visual performance.
The patient observes a notable difference in her vision when the cylinder is removed from the trial frame. The change in vision is particularly evident when she wore the trial frame in-store and looked at the scenery outside on the high street. Keratometry readings reveal that all of the astigmatism is corneal. The lid aperture measures 8mm, with the lower eyelid not covering the limbus at six o’clock. Upon elevation, the superior lid does not feel too tight. The optimal eye features a wide aperture, normal lid tension, complete lid closure during blink, a lower lid resting at the inferior limbus, and absence of elevated conjunctival tissue. When the lower
lid exceeds 2 mm above the limbus, it frequently leads to undesired axis misalignments. An incomplete blinking pattern negatively impacts toric lenses due to localised dehydration and accumulation of surface deposits in the inferior region of the lens.
While eye lid configuration is valuable in selecting the initial lens design, it becomes particularly important for troubleshooting if the lens behaves unexpectedly. For prism ballast lens designs, the thinner section of the lens settles beneath the upper eyelid, causing the thicker portion to be pushed towards the lower lid, a phenomenon known as the watermelon seed principle; this means that prismballast designs use primarily the upper lid for stabilisation purposes.6 In contrast to traditional prism ballast designs, which may compromise oxygen transmissibility in certain areas due to their thickness profile, modified prism/ peri-ballast designs are thinner. This thinner profile generally enhances comfort by minimising interaction with the lower lid even further. Apart from lid position, blinking and gravity also significantly influence lens orientation with this design. On the other hand, non-prism-ballast designs (including double slab-off, dual thin zone, and accelerated stabilisation designs), which rely on the interaction from both eyelids and rotation, are less influenced by the effects of gravity.10,11
Following initial assessment, the patient is refitted with toric contact lenses.
The spectacle refraction at 12mm is converted to ocular refraction, using the formula outlined in Figure 1, giving:
RE -4.94 / -0.87 x 15
LE -5.16 / -0.87 x 170
A daily disposable silicone hydrogel lens is chosen to keep in line with her current lens material, particularly as she did not report any other comfort issues. The lenses are available in -0.75D and -1.25D cylinders, in
“PROVIDING PATIENTS WITH THE CHANCE TO EXPERIENCE NEWER OPTIONS... ENHANCES THE LIKELIHOOD OF THEIR SATISFACTION”
10°-degree steps. As a 15°-degree cylinder axis for the right contact lens is unavailable, and a slight nasal rotation during blink may possibly be present, the initial astigmatic trial lenses are:
R -5.00 / -0.75 x 10
L -5.25 / -0.75 x 170
After 20 minutes, the following VAs are obtained:
R 6/5
L 6/5
Lens positions, which are stable on blink, are shown in Figure 2. When an aligned and stable rotation is observed, no further action needs to be undertaken and the lens can be dispensed. Order the same lens with an axis compensation using the LARS or CAAS rule when the vision is reduced and the lens axis is misaligned but stable after five minutes, that is to say, the axis misalignment is not fluctuating on blink. LARS stands for Left Add Right Subtract, while CAAS stands for Clockwise Add Anti-clockwise Subtract.
If the lens axis keeps fluctuating after five minutes, it is unlikely to improve and it is recommended a different design is trialled. In this case, the misalignment is present but stable, and the right eye shows 10° misalignment to the right, while the left eye shows a 10° misalignment to the left. VA is also affected, with loss of several letters in each eye compared to the trial frame results. In this case, new trial lenses were supplied as:
R -5.00 / -0.75 x 180
L -5.25 / -0.75 x 180
VA for each eye after 10 minutes showed 6/4.8- in each eye.
Some final clinical tips to effectively assist with astigmatic patients include focusing on aligning the power and axis with the ocular refraction values, bearing in mind that some lenses may experience slight nasal rotation during blinking. This is not generally a problem if it is only a few degrees, and the lens moves back to its original position after blink. Achieving optimal distance vision in the dominant eye promotes maximum comfort and VA, and is therefore a useful additional measurement to take into consideration. And when lenses are worn for specific tasks including driving, observe quick recovery in lens rotation during large head movements. Similarly, sensitivity to minor changes during the Jackson cross cylinder test may subsequently affect vision following adjustments made during the (re-)fitting process. Finally, as material technology advances, it is essential to offer patients the opportunity to try new technologies rather than waiting for them to discontinue wearing contact lenses due to discomfort. Providing patients with the chance to experience newer options allows for a relative comparison and enhances the likelihood of their satisfaction and continued use of contact lenses.
0
The author of this article is a paid consultant for Alcon.
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd

Dr Byki Huntjens is an education and research consultant in contact lenses and dry eye, and education lead for the AOP.
Sponsored by:








This article considers the importance and relevance of ocular surface assessment before planned cataract and refractive lens exchange surgery illustrated by cases from the authors’ clinics.
Purvi Thomson BSc (Hons), MCOptom, DipTP(IP), Prof Cert Glauc and Prashant Shah BSc (Hons), MCOptom, DipTP(IP), PGDipOphth, DipClinOptom
Introduction
With an ageing and growing population, leading increasingly active lifestyles and a desire to be spectacle and contact lens independent, the uptake of elective refractive lens-based surgery and cataract surgery is on the rise.
A thorough evaluation of the ocular surface plays an important role in the decision-making process for all ocular surgeries, and as such, this article will discuss the importance of such examination prior to cataract and refractive surgery.
Refractive elective surgery comes with a cohort of patients who choose to enter the surgical route for an improvement in their vision and quality of life. Outcomes are heavily measured on postoperative vision and freedom from visual aids. Cataract surgery has also now become more refractive based with premium options such as toric and multifocal intraocular lenses (IOLs). Patients have an increased expectation for more spectacle independence even if they have monofocal IOLs; this means that the ocular surface and the effect on surgical outcomes must be carefully assessed in all of these patients.
The Tear Film and Ocular Surface Society (TFOS) in their Dry Eye Workshop (DEWS) II report classified dry eye disease (DED) as: ‘Dry eye is a multifactorial disease of the ocular

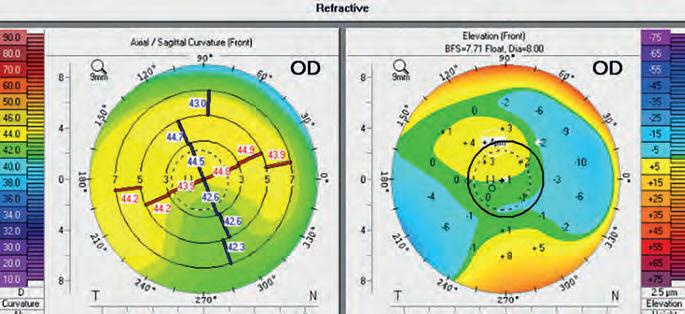

surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and
hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles.’1
This definition can be broken down into the elements that most influence refractive and cataract surgery decisions for the most successful outcomes in terms of quality of vision and ocular comfort levels.
Tear film instability can cause an increase in optical scatter and a degradation of quality of vision.2 Prior to surgery, this instability can result in inaccurate measurements for refraction and corneal topography – both very important factors when preparing a patient for refractive lens exchange (RLE) or cataract surgery. If the tear film becomes irregular in thickness, larger variations in tear film radius of curvature may appear in a localised fashion, leading to more variability in corneal dioptric power.3 For phakic IOL patients, this could result in an inaccurate refraction and lens power choice, and for cataract and RLE patients these would lead to incorrect biometry results therefore resulting in an incorrect IOL power being inserted.
Case one
Figure 1 shows preoperative measurements for a patient who presented with bilateral cataracts and an insistence on having complete spectacle independence post-surgery. Examination showed a low noninvasive tear breakup time (TBUT) of four seconds and fluctuating vision during refraction with evidence of corneal punctate epithelial erosions evidenced by fluorescein staining. She was prescribed hydrocortisone sodium phosphate drops to be used twice daily and preservative-free cross-linked artificial tears to be used four times a day in both eyes. She was brought back into clinic six weeks later for reevaluation. Figure 2 shows how the repeated preoperative measurements demonstrated an altered corneal power on both the topography and biometry. Her TBUT had also increased to seven seconds and showed greater stability. She was subsequently listed for surgery and a toric trifocal IOL was inserted into both eyes, allowing her to achieve
Optometrists will be able to explain to patients about treatment options for ocular surface disease prior to intraocular lens surgery
Optometrists will be able to outline to patients about the impact of ocular surface disease upon intraocular lens surgery options and outcomes
Optometrists will be able to evaluate the integrity of the ocular surface prior to intraocular lens surgery and prescribe treatments in line with their scope of practice
Specialty optometrists will be able to explain to patients about treatment options for ocular surface disease prior to intraocular lens surgery
Specialty optometrists will be able to outline to patients about the impact of ocular surface disease upon intraocular lens surgery options and outcomes
binocular visual acuity of 6/6 N5.
Extensive evaluation of the ocular surface can be a long process; however, in most cases, not all investigations need to be done before a treatment plan can be made. Often a dry eye questionnaire is sufficient to gauge whether the patient has significant symptoms that will affect outcomes of planned surgery. There are many useful questionnaires available such as the ocular surface disease index (OSDI) and the dry eye questionnaire (DEQ-5) and evidence shows that practitioners should use a relevant questionnaire
Specialty optometrists will be able to evaluate the integrity of the ocular surface prior to intraocular lens surgery and prescribe treatments in line with their scope of practice
Dispensing opticians will be able to outline to patients about the impact of ocular surface disease upon intraocular lens surgery options and outcomes
Dispensing opticians will recognise the importance of the integrity of the ocular surface with respect to intraocular lens surgery options and outcomes.
based on what they are looking for.4 The importance of asking the correct questions in patients undergoing surgery is to help predict outcomes and to prepare patients for postoperative recovery.
It has been estimated that the worldwide prevalence of DED ranges from 5% to 50%, depending on the geographic region.5 Many of these patients are unaware that they have DED when they present and often the implications of surgery can render them more symptomatic. Without thorough preoperative counselling
“THE UPTAKE OF ELECTIVE REFRACTIVE LENS-BASED SURGERY AND CATARACT SURGERY IS ON THE RISE”
R1(mm/DrJ 7.76/43.48@115
R2[mm/Dr) 7.64/44.16@25
R (mm/DJ 7.70/43.82
+AST [Dr) 0.67 @ 25 n 1.3375
WTW [mm] 11.93

LSPOO1B-See;2020• 1
(mm) 23.28
(µm] 513'
(mm) 2.71
(mm) 3.22
[mm] 4.08'
Warnings:
R1(mm/D/°) 7.83/ 43.11@ 75
R2[mm/D/°] 7.62/ 44.27@ 165 R (mm/DJ 7.73/43.68
+AST [DI°) 1.16@ 165 n 1.3375
WTW [mm] 11.76
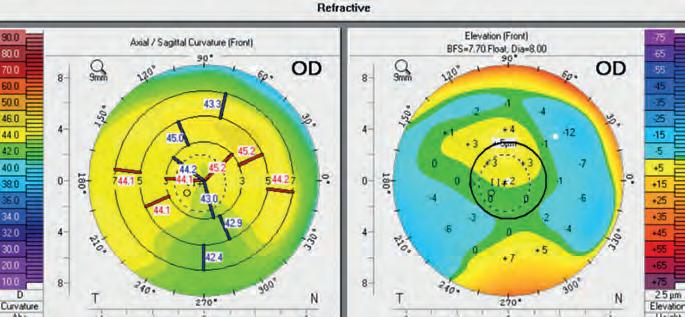

and optimisation of the ocular surface, these patients would end up with less than favourable results, either through quality of vision issues or highly symptomatic ocular surface disease. TBUT is a commonly used method of assessing the quality of the ocular surface. Figure 3 shows measurement of non-invasive TBUT (NITBUT) using specialist software. The latest TFOS DEWS II report suggests that a NITBUT is a more useful analysis than invasive measures as it keeps the tear layer in its most natural state
without any disruption.6 Measurement of tear osmolarity is an important consideration as evidence shows that tear hyperosmolarity stimulates death of the epithelial surface cells and results in a cascade of inflammatory events which exacerbates tear film instability and contributes to the cycle that perpetuates DED.7 Measuring osmolarity prior to surgery provides valuable baseline information on the tear layer and ocular surface and can determine where preoperative treatment for the ocular surface
is needed to limit postoperative complications and discomfort.
In patients who present for elective surgery, the assessment of the ocular surface plays a large factor in decision making. In the previous case, the patient who opted for multifocal IOLs was prescribed preservative-free hydrocortisone sodium phosphate drops and preservative-free artificial tears and brought back for review. Would the same have been done had she chosen monofocal IOLs? In patients electing for multifocal IOLs there is a lot of counselling necessary to educate them about the visual impact of diffractive optics. These IOLs work by splitting light to allow for multifocality, and therefore, the quality of the light entering the eye before it reaches the IOL should be optimal.8 As evidenced earlier, a poor tear film causes scatter, thus light has already been lost and split before it reaches the multifocal IOL where it further degrades. In patients with a poor ocular surface, it is strongly advised not to use a multifocal IOL, highlighting why it is important to evaluate the ocular surface before inserting premium IOLs. However, the question remains – should practitioners also be looking at the ocular surface in cataract patients who require monofocal IOLs?
The primary aim of cataract surgery is of course to improve vision and thus quality of life. As patients with cataract tend to present later in life, there is a greater potential for them to have DED.9 Studies have shown that patients previously diagnosed with DED report a worsening of symptoms after uncomplicated phacoemulsification.10 Often these patients will then find the treatment to improve the ocular surface post-surgery difficult to manage, that is to say, instilling eye drops and attending frequent visits back into the clinic. It is, therefore, important to consider the effect of surgery on these patients. There are many reasons why lens surgery results in an increase in DED
in patients: the anaesthetic drops and cleaning agents used during surgery can be toxic to the ocular surface; the speculum used to hold the eye open renders a large zone for tear evaporation; the incisions made during the surgery affect the corneal nerves, and therefore the postoperative tear production cycle. Phototoxicity from the light source, surgical time and trauma also leaves the patient with symptomatic ocular surface disease post-surgery. This is subsequently followed up with postoperative topical drops which are often preserved. So, while practitioners can confidently say to most patients that they will be able to see better following cataract surgery, it is important to remember to advise them that their DED could be exacerbated, and surgeons need to
“EVALUATION OF THE OCULAR SURFACE IS PARAMOUNT TO CONTRIBUTING TO SUCCESSFUL CATARACT OR RLE SURGERY”
take this into account during surgery. The central mechanism of DED is a vicious cycle where inflammation plays a key role. The resulting ocular surface damage is due to inflammation which is stimulated either by desiccating or hyperosmolar stress.11 Treating the inflammation and repairing the ocular surface is a key driver in improving tear film stability and reducing symptoms and signs of DED. Mild steroids, such

as fluorometholone or hydrocortisone sodium phosphate have been shown to be highly effective in the management of DED and are safer than other types of corticosteroids.12 The use of preservative-free steroids and artificial tears are used to protect the ocular surface from the chemicals found in preservatives.13 Crosslinked sodium hyaluronate drops have a higher viscoelasticity and have been shown to retain more water than noncrosslinked sodium hyaluronate. Therefore, crosslinked sodium hyaluronate results in longer lasting lubrication for patients.14 With the patient in this case, lowering the inflammatory markers and nourishing the eye helped regularise the ocular surface and the vision outcome was excellent. Furthermore, she was asked to continue the artificial tears following surgery and ensure her postoperative medications were preservative free where possible.
Case two is a paraplegic presbyopic patient just under 50 years of age who could not manage wearing glasses. His need for near vision correction and a non-tolerance to varifocals due to head posture made it very difficult for him to successfully manage in a single pair of glasses that gave him adequate vision at all distances. He presented in clinic to understand what his options for vision corrective surgery were. After a thorough consultation, it was found that RLE with multifocal IOLs was the best option for him. However, he presented with watery eyes, a low NITBUT, anterior (see Figure 4, page 62) and posterior blepharitis as well as facial rosacea and telangiectasia of the eyelid margins (see Figure 5, page 62). After examination, the ocular surface was deemed too poor to enable a successful postoperative outcome. He was advised that he would need to treat his ocular surface first. The presence of anterior blepharitis pre-surgery


causes an increased risk of post-surgical endophthalmitis and evidence shows that blepharitis increases following surgery.15 There are various eyelid exfoliation techniques which can be delivered in clinic and also at home. Due to the inflamed nature of his lid margin an okra-based gel eyelid treatment was carried out, which has been shown to reduce inflammatory levels, increase TBUT and reduce bacterial load on the eyelid margin.16 It is a less abrasive treatment than other techniques, and is effective where eyelid margins are inflamed and sore. The gel also lowers the inflammatory and bacterial load to have a more lasting effect on the ocular surface.
Eyelid margin telangiectasia and facial rosacea has been linked with ocular rosacea, an inflammatory disease, which leads to DED and renders patients very symptomatic.17 Intense pulsed light (IPL) has been shown to be effective in reducing inflammatory levels, increasing TBUT and expressibility of meibomian glands,

thereby improving tear film stability (see Figure 6).18 This patient underwent four sessions of IPL with gland expression and his TBUT increased from less than five seconds to around eight seconds. He noticed a decrease in his epiphora and a general improvement in his symptoms and proceeded with bilateral RLE with toric multifocal IOLs. An important consideration to evaluate was the lifestyle of this patient. He was unable to instil drops himself and needed a carer to manage these tasks for him. While he could have also been advised on home eyelid hygiene measures and artificial tears, the practicalities may have resulted in limited success with treatment.
In terms of postoperative care for this patient, he was advised that he may need subsequent treatment of IPL to help control his ocular rosacea. The use of tetracyclines such as doxycycline or lymecycline has also been established in the treatment of rosacea19 and this patient is likely to need further home or in-clinic therapies to ensure that his ocular surface remains healthy.
Evaluation of the ocular surface is paramount to contributing to successful cataract or RLE surgery. The integrity of the ocular surface can impact upon the type of IOLs available to a patient, and without diligently treating ocular surface disease, can affect postoperative outcomes. Without a stable tear film and optimised ocular surface, incorrect preoperative measurements
could result in incorrect amplitude of astigmatism measurements, incorrect IOL power calculations, further damage to the ocular surface, poor postoperative quality of vision issues or severe DED. Treatment can be given as part of a home care regime such as preservative-free artificial tears, warm compresses, eyelid hygiene, advice on diet and anti-inflammatory topical therapy. All these measures have shown to help optimise the ocular surface ahead of surgery. In-office treatments such as IPL, lid margin exfoliation and okra-based gel can also help improve the ocular surface, so the patient has a successful postoperative outcome.
Furthermore, patients should be counselled before surgery on postoperative dry eye symptoms due to the disruption of the homeostasis of the tear film. They should be suitably managed pre- and postoperatively to ensure that they achieve a good level of postoperative vision with minimal discomfort to their eyes. IOL choice discussion should be based not only on their needs, but the limitations of their eyes, including the ocular surface. Careful consideration needs to be given to the quality of vision that patients will achieve in all light levels following surgery, especially in the case of multifocal IOLs, and much of this should be based around the quality of their tear film and ocular surface.
0
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd

Purvi Thomson is a specialty optometrist and works at OCL Vision. Thomson also works in the contact lens department at Luton and Dunstable NHS hospital.


Prashant Shah has worked in a variety of settings including in a High Street multiple and primary care ophthalmology. He now works for OCL Vision.
Sponsored by:







BRILLIANTLY

This article will consider some of the factors contributing to visual perception, and the relative influence of visual stimuli of which we are not consciously aware of.
This includes attention, subliminal messaging, gist processing and the role of memory.
Dr Samantha Strong BSc (Hons), MEd, PhD and Grace Solola BSc (Hons), MCOptom
When a person visits their optometrist, they expect to have their sight measured in such a way that they feel the practitioner has understood what they themselves can see. However, it would be slightly truer to say that the optometrist is gaining valuable insight into how light refracts through the eye – which is not quite the same as understanding what they see.
To start with, we know that it is important for light (photon) energy to be focused correctly on the retina, as without this, our view of the world is blurry and/or distorted. However, it is also true that there are several more stages of processing which need to take place along the visual pathway and the brain before the individual becomes ‘aware’ of what the light energy represents. In this article, we will consider the afferent light energy as the ‘input’ and the individual’s perception as the ‘output,’ as this information is released to the person after the brain has performed a series of analyses to help us interpret and understand what we have seen.
Visual awareness can typically be defined as ‘having knowledge’ and ‘being alert and conscious of the visual scene,’1-2 and importantly, it serves to help us understand the world around us. For example, as you read this article, you are aware of the words on the page (or screen), and you understand what they mean; this serves as a nice example
of awareness of visual information helping to provide some wider context. Importantly, for our conscious awareness of the scene to be effective, we need to decide what visual information is relevant and what visual information is not; this requires a process of selectivity to take place, which can in most examples be driven by attention.3-4 Attention is the term attributed to our ability to focus on certain elements of a scene – for example, in reading this page it is likely that unless you are holding the page extremelyclose to you, your visual field will encompass many elements of the world around you – possibly your workspace, proximal colleagues or family members, and maybe even your mobile device. However, when focusing on the words on the page, your brain is deciding to selectively ignore those other elements (until we discussed them just now) and is demonstrating the link between attention and conscious awareness; as, when not attending to a stimulus, it is like it is considered invisible to you. This can be summarised as saying that when we attend to something, we tend to become aware of it,5 meaning that the inverse is also true: when we are not attending to something, we tend not to be aware of it – thereby indicating that our awareness of the visual world may only represent those elements that we consider worth our attention at the time.
Scientists have suggested that when we ‘see’ an object in the visual world, our brain activates an internal representation of the external visual scene,6 like having a television screen in our minds, showing us what we personally perceive to be real. However, we also know that attention
1 CPD POINTS
C-108600
LEARNING OUTCOMES
Optometrists and dispensing opticians will recognise the processes involved with interpreting the visual scene.
plays a role in determining what this representation will look like, and there are two opposing theories which discuss how this is achieved: the earlyselectiontheory;7-10 and the late selectiontheory.11-13
The early selection theory of attention puts forward that attentional selection of visual stimuli is at the forefront of processing, meaning that objects that are being attended to will be processed in detail while the unattended stimuli are processed in a very limited capacity.14 In contrast to this, the late selection theory suggests that all areas of the visual scene are fully processed initially, but that attentional selection is applied during later processing stages before releasing the relevant information to us as conscious visual perception.15 In both cases, it is assumed then that some stimuli will either fail to be encoded into our internal representation (early selection) or will fail to be
released to us as conscious awareness (late selection), but both theories suggest we may ultimately be ‘blind’ to some visual stimuli. Indeed, this has been shown to be the case in the now-famous ‘gorillas in our midst’ experiment16 in which experimenters showed a film of individuals passing a ball to one another and asked participants to count how many times the ball is passed between the group wearing white tops. As this was going on, a person dressed in a gorilla outfit walked through the people, beat their chest, and walked off (for a total duration of five seconds), and amazingly
46% of subjects failed to notice the person in the gorilla outfit even though they were looking directly at it. This is an example of inattentional blindness, whereby visual information is not perceived because the individuals’ spotlight of attention was focused on the ball, not the surprise gorilla. Figure 1 shows an example of how this might happen, highlighting the key distinction between selectively attended, and unattended stimuli.
Another key example of the role of attention in ‘seeing’ comes from the case of police officer Kenneth Conley, who, while chasing a suspect, ran past

four officers brutally attacking an undercover police officer. Interestingly, even though theoretically he would have been able to see and hear the commotion, Conley denied having seen the assault at all and was charged with perjury as a result. This led Chabris etal17 to replicate the scenario under controlled conditions to see whether it would be possible to miss something so salient in the scene. In their experiment, they got 16 participants to follow a colleague as he jogged a specific route through campus and count how many times he touched his head. Around 125m into the route, a staged fight appeared with two men supposedly beating a third man. At the end of the experiment participants were asked whether they saw anything unusual, and only 56% had noticed the scuffle. This may sound unusual but is in fact another very nice demonstration of inattentional blindness, whereby the individual may have the visual information reach their retinae but fail to become consciously aware of it due to attending to something else at the time. This effect can be surprisingly large at times (for example, opening a drawer to look for car keys and not seeing them sitting on the top) and demonstrates that vision is much more to do with how our brain choosesto release information to us, than it is about photons. In this way, we could argue that ‘seeing’ at a retinal level is not sufficient for sight to take place, as we also need awareness to process and understand the scene.
If you have ever heard of James Vicary (Snopes) and the controversy surrounding his fraudulent claim to have ‘brainwashed’ people with flashing images to buy more popcorn and Coca Cola in 1957,18 then you may be wondering where subliminal messaging or ‘covert manipulation’ comes into the consciousness question. Colloquially, we refer to subliminal messaging as any kind of hidden agenda, but in psychology, subliminal messaging is defined as: a message passed to the
human mind without the mind being consciously aware of its presence,19 which would apply to any sensory stimulus (for example, visual) and occurs so quickly that it falls below our threshold for recognising that we have seen it at all. This is different to inattentional bias because it is driven by the physiological limitations of our visual system, rather than an inability to attend to a stimulus. This means that it is of interest to us to understand the impact of imperceptible phenomena because if it is possible for a subliminal percept to infiltrate our mind, then it could be argued that we do not need to be consciously aware of stimuli in order to ‘see’ them on some level. Interestingly, research has shown that there are some physiological changes in response to subliminal stimuli20 as one study demonstrated increases in stressrelated electrodermal responses when participants were shown an anxietyinducing phrase (for example ‘NO ONE LOVES ME’) for 4ms (below perceptible levels). This was considered at the time to be evidence for the hypothesis that awareness of a stimulus inhibits responses to drive- and affect-related stimuli,21 and so emotion-inducing stimuli should have far greater effect on a person when presented below threshold for awareness. However, while this initially sounds like the potential for subliminal images to reach the unconscious mind, evidence of behavioural/performance effects is very minimal, if at all – for example, subliminal ‘cueing’ to a location does not improve performance in a visual search task.22 Overall, most researchers agree that hidden perceptual messages cannot alter behaviour (in that they cannot influence free will), and there is not a lot of convincing evidence to suggest that subliminal stimuli would have any impact on a person that would affect their conscious experience. Nevertheless, research shows that quickly-presented, perceptible images can be processed unconsciously – this is called gistprocessing because it involves very rapid extraction of global


Importantly, the reason that topdown processes (such as attention) have such control over our perceptual experience is because it allows rapid, mostly successful comprehension of the salient items in a scene. For example, if a car is driving towards you, you do not need to be able to recognise that it is a very cool Kia Picanto to know that you need to move out of the way; this essentially provides a shortcut to the information we need to know, which is driven by schema-led processing of new information relying on past experiences.26
structural and statistical information to access the idea of an image in ~10ms (that is to say, we get the ‘gist’).23 Interestingly, the ability to process the gist of a scene is relevant to healthcare professionals, as evidence shows that we can use these quick presentations to detect health concerns. One study found that when radiologists were presented with brief (2502000ms) flashes of medical images, they had above-chance performance (see Figure 2),24 which was best at the longest presented duration (2000ms). This suggests that we are able to consciously access more about an image than we may think, and links with a nice study25 which showed that participants performed better-thanchance at detecting whether an image was present or not in a sequence of six to 12 images presented at 13ms in succession. However, we note here that in both of these experiments, performance did not reach the ‘perfect’ level which means that while we are better at this than we might expect, there is still information that is not being processed in this rapid, unconscious way.
However, as JRR Tolkien27 put it ‘short cuts make long delays’, as when trying to find a shorter route, you may encounter unexpected consequences, and indeed, that is true of the visual system as well as hobbits. The reason, for example, that visual illusions persist at all is because they take advantage of the known schemata of our visual cortices. For instance, in the classic example shown in Figure 3 (see page 66), we can see two spheres on a grey background, and each of the spheres is coloured with a gradient from black to white.28 However, what is interesting about this is that the left sphere will likely appear concave (as if it dips down into the page), whereas the right sphere will likely appear convex (as if it lifts off the page). This is because our visual systems have learned about shadows over time, and we typically expect light sources to come from above (for example, the sun, room lights).
So, if we see a dark area on a sphere, logic says it must not be illuminated, and this can only be true if the surface is blocked from the light source, which must mean that the left sphere is concave, and the right sphere is convex. However, if you turn the image upside down, the illusion will persist, so now the left sphere (which was the right one) will look concave and the right sphere (which was the left) will look convex. This, in a way, shows that perception can be modified unconsciously to fit our
known assumptions, without the conscious decision to do this.
Up to this point, we have considered the link between input (stimulus) and top-down processing (attention, experience) but we have not yet explicitly considered what happens to that perceptual experience over time. In a few days’ time, when you are no doubt fondly remembering this article, you may recall the image of the cat, and you will likely remember the teeth because you were primed with the word ‘vampire’ in the figure caption (if you did not spot it, we recommend you go back and have a look), but you may have forgotten what it was she was doing. In this instance, it’s not that you can’t imagine the image, it’s just that you will most likely have to ‘fill in the blanks’ a little – so if asked ‘what was the cat doing?’ you may say something believable like ‘baring her teeth’ or ‘yawning’, and in that moment, it is likely that you will believe that is what you saw, even if incorrect. This highlights a fascinating feature of perception and awareness, wherein over time, our memories consolidate experiences in certain ways to highlight the salient points and effectively wash out the less salient points. This means that all perceptual memories are likely to be at least a little falsified. In a series of seminal experiments, Elizabeth Loftus and her collaborators demonstrated this and applied it to eyewitness testimonies of criminal proceedings. She found that when questioning witnesses to a crime, the wording of the question could actually alter their perception of the experience. In one study,29 participants watched footage of a car accident and were then asked if they saw something that didn’t exist in the footage, for example a broken headlight. These questions were posed either as indefinite articles ‘did you see abroken headlight?,’ or definite articles ‘did you see the broken headlight?’ Worryingly, when asked about the absent item with the
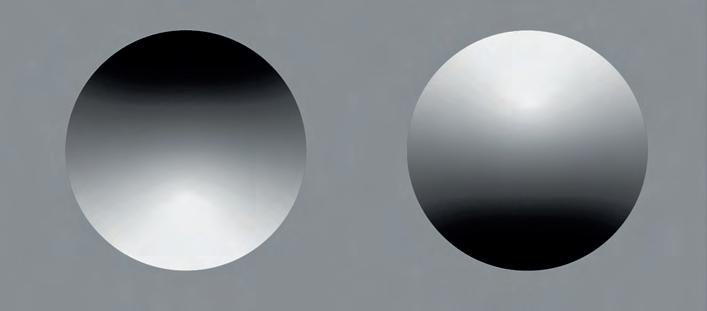
indefinite article, 7% of participants reported seeing it, but when asked with the definite article, 14% of participants reported seeing it. The trick here is that the indefinite article is subconsciously interpreted as ‘was there a broken headlight and did you see it?’ which leaves more room for uncertainty, whereas the definite article can be interpreted as ‘there was a broken headlight, did you see it?’ However, in both cases the clip was too short to answer either with any confidence so the 7–14% of incorrect testimonies is rather concerning. This highlights that even in the absence of a stimulus, our perceptual memory can be altered by semantics.
Similarly, it transpires that we as humans are also not very good at accurately choosing people in a police line-up. Several studies30-33 have found that when shown a line-up of potential suspects, we are most likely to choose the person who, in the mind of the witness, demonstrates most similar characteristics to the perpetrator because they resemble a ‘schema’ we have made. This means, that if you were in a line-up and the criminal happened to have similar hair to you, you may be identified as the culprit! Together this suggests that even once encoded and released to us as conscious awareness, the percept can become manipulated and altered by external stimuli and passing time.
To summarise, it is clear that visual processing is a very complex phenomenon. Evidence shows that conscious awareness of the visual word is facilitated and focused by attentional mechanisms, but that time and context (for example, phrasing of a question) can alter our memory of these experiences to such an extent that we believe we saw something we did not. Similarly, it is possible to achieve a reasonably reliable idea of a scene, with such a brief presentation that conscious processing mechanisms cannot possibly be involved. To answer the title of this article then, it seems we do not necessarily need conscious awareness of an image to ‘see’ it, but that this is only the very tip of the iceberg in terms of the factors that contribute to our idea of visual experience.
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd





At Newmedica. we choose to use the highest quality cataract replacement lenses for the best clinical outcomes. In fact. our monofocal lens for NHS patients has the lowest PCO rate of any lens on the market at 3 and 5 years. It's hydrophobic and is specially designed to reduce the need for YAG surgery*.
Which is great news for your patients and the NHS. and peace of mind for you.
*Source : The Royal College of Ophthalmologists, National Ophthalmology Database "Feasibility Study of Post-Cataract Posterior Capsule Opacification" May 2021
Sponsored by:








This article discusses risk factors for intraoperative complications during cataract surgery and highlights the importance of thorough examination and history taking during pre-operative consultations to improve outcomes.
Dr Kar Yen Phoong BSc, MBChB and Dr Deborah Armstrong PhD, MCOptom, DipTp(IP)
Cataract is defined as the opacification of the natural intraocular lens, leading to deterioration in visual acuity (VA) and may eventually lead to blindness if left untreated.1 It is a slow and painless process, but patients may experience blurring of vision, glare, poor night vision or loss of contrast sensitivity. The majority of cataracts develop with increasing age but secondary causes such as infection and inflammation, trauma or certain metabolic conditions enhance the risk of developing cataracts. Eye infections and inflammation such as uveitis, trichomoniasis or conjunctivitis can lead to the development of secondary cataract.1 Traumatic cataract can occur following blunt or penetrating eye injuries, and metabolic cataract develops in patients with uncontrolled diabetes, galactosemia or Wilson disease.1
Cataract is the leading cause of blindness worldwide, accounting for 94 million people with vision impairment.2 Sight can only be restored with cataract surgery which involves removing the opaque lens and implanting a new intraocular lens (IOL).1 It is the most prevalent surgery performed worldwide and also a highly standardised procedure with a success rate of 97% or higher depending on the setting and skills of surgeons.1
A complication rate of approximately 1.2% still occurs despite the advancement of cataract surgery.3 The most common complications include posterior capsular rupture (which increases the risk of vitreous loss and a dropped nucleus), postoperative cystoid macular oedema, retinal detachment and endophthalmitis.4 These surgical complications could be reduced by identifying risk factors prior to the surgery. This article will provide a concise summary of potential problems, enabling the optometrist to recognise high risk eyes at every step of the consultation.
Taking a good history is crucial in order to obtain information about a patient’s overall health, relevant medical history, previous eye operations, trauma or any
other ophthalmic conditions. Many systemic diseases such as diabetes, hypertension and other cardiovascular conditions have significant impact on eye health.5
For patients with diabetes, cataracts develop earlier and more rapidly.6 It is crucial to provide the necessary surgical intervention at an early stage to reduce complication rates that occur with dense cataracts. Studies have found that patients with no, or mild, preoperative retinopathy have a better visual outcome following cataract surgery compared to those with moderate or severe proliferative diabetic retinopathy;7 this is supported by the finding that patients with treated macular oedema prior to surgery had better visual outcomes than those with active macular oedema.8 It is recommended that cataract removal

should be performed at an early stage of retinopathy to achieve a good visual outcome.6 Moreover, diabetic patients have impaired wound healing due to hyperglycaemia, chronic inflammation and microvasculature changes.9
A retrospective study showed that patients with diabetes are at significantly higher risk of infection compared to non-diabetics, leading to intraoperative and postoperative complications.9 It is advised that patients should have strict glycaemic control both pre- and postoperatively.
Pre-existing hypertension is considered to be one of the most common chronic conditions within the population listed for cataract surgery.10 It is postulated that hypertension might increase the risk of cardiovascular adverse events and may lead to intraoperative suprachoroidal haemorrhage, which is a rare complication.10 It is also one of the common reasons for cancellation and postponement of elective cataract surgeries. However, the current evidence is insufficient to determine a direct correlation between hypertension and an increased risk of surgical complications.11 Despite that, pre-existing hypertension should be controlled before proceeding with cataract surgery to reduce any intra- or postoperative complications. Blood pressure control should be optimised many months before the surgery as it is also associated with other significant comorbidities such as diabetes mellitus, coronary artery disease, peripheral vascular disease and impaired renal function.12
According to the UK national cataract surgery survey, one in three people
have a pre-existing ocular condition that could significantly affect the outcome of their cataract surgery.13 The prevalence of ocular conditions increases with age, for example, agerelated maculopathy, glaucoma and diabetic retinopathy, which have been proven to be strong predictors of poorer surgical outcomes and higher risk of intraoperative complications.14 Cataract surgery may exacerbate many of these conditions and result in poorer vision than before surgery. It is well known that cataract surgery may accelerate the progression of diabetic retinopathy and development of macular oedema.15 Due to the possible consequences resulting from cataract procedures, it is preferable for more experienced clinicians to perform the surgery to reduce the complication rate. Patients with pre-existing ocular conditions require more frequent check-ups after cataract surgery to ensure stability of preexisting conditions.
Pre-operative BCVA is clinically important as it is needed to ascertain the visual success of cataract surgery.14 It can be affected by factors such as existing ocular conditions, systemic medical issues affecting vision or previous ocular trauma. An accurate BCVA helps to identify the severity of the cataract, determine the urgency of cataract surgery and provide a reliable prognosis post-surgery.
It is important to ensure that IOP is within the normal range before proceeding with surgery. If ocular hypertension or glaucoma are identified, then treatment is needed prior to surgery.
Optometrists will recognise the importance of taking a careful history for establishing factors that could influence cataract surgery outcomes
Optometrists will be able to identify factors that could influence cataract surgery outcomes during clinical examination and manage the patient accordingly
Specialty optometrists will be able to identify and treat ocular conditions that could influence cataract surgery outcomes, relative to their scope of practice
Dispensing opticians will recognise the importance of taking a careful history for establishing factors that could influence cataract surgery outcomes
Dispensing opticians will be able to identify factors that could influence cataract surgery outcomes during clinical examination.
During examination, general ocular health, depth of the anterior chamber, maturity of cataract and condition of the capsule should be assessed to determine the necessity of surgery. It is also important to rule out any subluxation of the lens which may lead to IOL dislocation and other intraoperative complications.
There are other areas that the optometrist needs to be aware of during the slit lamp examination. These are separated into five categories and include:
• Ocular infection
• Corneal abnormalities
• Iris and pupil abnormalities
• Anterior segment abnormalities
• Lens profile. These categories will be considered.
Ocular infection is one of the most common reasons for the cancellation of cataract surgery.16 Infective and inflammatory causes such as conjunctivitis, blepharitis, chalazion and uveitis should be treated before the operation. Eyelid and ocular surface infections leave the patient prone to the development of endophthalmitis, which is a potentially sight-threatening infection.17 Appropriate treatment with topical antibiotics and steroids should be provided to treat the condition prior to any intraocular surgery. Other conditions causing eyelid abnormality, such as entropion, ectropion and lagophthalmos increase corneal exposure leading to dryness and microtrauma from eyelashes rubbing on the cornea.17 These conditions remove the protective tear layer and
allow infection and inflammation of the corneal surface.17 Lid correction surgeries should be performed before the cataract is removed.
Corneal abnormalities can arise from congenital, traumatic, physical or chemical insult to the eye.18 Infection and inflammation such as trachoma, uveitis or recurrent dendritic ulcers can lead to corneal opacification. Raised IOP from uncontrolled glaucoma may cause epithelial oedema.19 In addition, previous ocular trauma or intraocular surgeries can also increase corneal haziness. Fuchs’ endothelial dystrophy is characterised by dystrophy of the endothelial layer of the cornea.20 The loss of endothelial cells, causes fluid from the anterior chamber to collect in the corneal stroma, leading to chronic oedema (see Figure 1). With more advanced disease, swelling increases in the epithelial layer of the cornea and fibrotic tissue forms in the subepithelial space, which further increases the corneal opacification.20 Medical treatment with hypertonic saline eye drops can be helpful to draw out excessive fluid from the cornea. However, as the disease progresses, surgical management such as penetrating keratoplasty may be necessary to restore vision.20
A small, rigid pupil is a wellknown risk factor associated with intraoperative complications as it restricts the visualisation of the operating field. Small pupils may be a result of inadequate preoperative mydriasis, previous ocular trauma
or surgery leading to iris damage, pseudoexfoliation, uveitis, glaucoma or diabetes mellitus.21 This issue can be overcome by using expansion devices such as iris hooks or pupil expansion rings. Ideally, pupil size needs to be increased to 4.5mm or more for specific surgical techniques, nucleus fragmentation and complete nucleus removal.21 Furthermore, intraoperative floppy iris syndrome (IFIS) is known to cause poor pupillary dilatation and intraoperative complications during cataract surgery.22 It is characterised by poor preoperative pupil dilatation, billowing of the flaccid iris stroma, iris prolapse into surgical incisions and progressive intraoperative pupil constriction (see Figure 2).22 The risk factors for developing IFIS are systemic medications (tamsulosin and doxazocin), increasing age, diabetes, and prolonged duration of phacoemulsification.23 Due to the laxity of the iris, there is a risk of this structure being aspirated and damaged by the ultrasound probe during the operation. Irrigation with epinephrine 1:10,000 may increase pupil diameter before the start of the surgery.22 Some studies suggest intracameral injection of epinephrine or phenylephrine may promote maximal pupil dilation and improve iris muscular tone. Appropriate surgical technique modification with the use of an ophthalmic viscosurgical device and vigilant hydrodissection are important to prevent iris prolapse during the procedure.22
A shallow anterior chamber can occur in hyperopic eyes which makes intraocular manipulation difficult;24

this poses a high risk of compromising other intraocular structures with surgical instruments, and can result in endothelial damage, iris injury and iridodialysis.24 Cataract surgery in patients with shallow anterior chambers should, therefore, be done by senior clinicians as they have more experience in dealing with these cases. Conversely, some studies have shown that high myopia is a significant risk factor for intraoperative complications during cataract surgery.25 The procedure can be challenging due to the high axial length, leading to a very deep anterior chamber, floppy and large capsular bag, and possible zonular weakness.26 Despite having more intraocular space for surgical manipulation, there is a high risk of overinflation of the anterior chamber leading to lens-iris diaphragm retropulsion syndrome,26 which is characterised by iridocapsular contact causing reverse pupillary block. In order to address this issue, fluid flow should be maintained under the iris to equalise the pressure between the anterior and posterior chambers.26
In general, it is recommended that cataract removal should be done when there is a significant deterioration of VA, which is affecting daily activities of life.27 Cataract surgery is usually safe, simple and straightforward as the majority present during an early stage of the condition. However, there are certain types of cataracts that may be more surgically challenging than others. These are commonly due to late presentation, such as white cataract, posterior polar cataract, milky cataract or dislocated lens.1
White cataract is a mature, totally opaque cataract at the end stage of cataract progression (see Figure 3).28 Due to epithelial impairment and fluid influx, the lens becomes hard, swollen and full of cortical material enveloping a hard nucleus.28 It has a characteristic milky white appearance and due to its opaque nature, it is very challenging to remove from the lens capsule. It is advised to use

trypan blue dye to stain the anterior capsule to help differentiate between the white cataract and the capsule.28
Posterior polar cataract is located in the subcapsular region of the lens, which is often adherent to a thin posterior capsule;29 this greatly increases the risk of posterior capsule rupture, leading to potential vitreous loss and the risk of the intraocular lens dropping into the vitreous chamber. In terms of prevention, adherence to the posterior capsule can be assessed preoperatively with several diagnostic techniques such as anterior segment optical coherence tomography, Scheimpflug imaging or ultrasound.29 The patient should be counselled about high-risk cataract surgery and support be provided for them to make an informed decision.
This happens when the cortex of the hypermature cataract becomes liquefied and the opaque nucleus is able to move freely within the capsular bag.30 Uncontrolled diabetes and chronic sunlight exposure are risk factors for this type of cataract. These cases have a high risk of intraocular complications as they may undergo spontaneous rupture into the anterior chamber causing an inflammatory reaction and secondary glaucoma from an increase in IOP.30 Detailed
pre-operative assessment should be performed to identify this high-risk cataract with arrangement for a more senior surgeon to undertake the procedure.
This can occur in many conditions such as very mature cataracts, pseudoexfoliation syndrome, chronic inflammation, trauma, Marfan’s syndrome and others.31 These conditions can weaken the zonular fibres and increase the risk of lens subluxation, capsular tears and other intraocular complications. However, these risks may be mitigated with capsular support devices such as capsular hooks or capsular tension rings.31
The recognition of risk factors and complications are vital in improving the quality and success rate of cataract surgery. Clinicians should be able to identify and manage appropriately to reduce the failure rate. Successful cataract surgery involves many different stages starting from preoperative assessment to post-operative care. Appropriate assignment of experienced clinicians is important as patients with a complex background require more detailed assessment and care. Meticulous preoperative risk assessment, new surgical techniques and technologies, and postoperative management are key to providing good patient outcomes.
To read this article online, access the references and take the exam, visit: www.optometry.co.uk/cpd


Dr Kar Yen Phoong is a foundation trainee in the East Lancashire NHS Hospitals Trust.
Dr Deborah Armstrong is a specialist optometrist in East Lancashire Teaching Hospitals and teaches at the University of Bradford.

*Driving (74%), reading (68%), travelling (62%), hobbies and social activities (43%), and the ability to work or volunteer (42%).
tFrom the global Geographic Atrophy Insights Survey (GAINS)(N=203) conducted by The Harris Poll and sponsored by Apellis Pharmaceuticals in 2021. Online/telephone survey in participants> 60 years old from the US, UK, France, Germany, Italy, Netherlands, Sweden, Canada, and Australia. Participants self-reported they had been diagnosed with age-related macular degeneration, with dry age-related macular degeneration in ;;:1of their eyes. They also had advanced atrophic age-related macular degeneration or advanced/late/late-stage dry age-related macular degeneration or advanced dry age-related macular degeneration or geographic atrophy in ;e1of their eyes and were experiencing ~3 geographic atrophy symptoms out of a list of -15 symptoms.
References:
1. Sivaprasad Set al. Ophthalmol Ther.2019;8(1 ):115-124
2.Jones D et al. Invest Ophth VisSci. 2022;4217-A0145.
Available from: https://ivors.arvojournals.org/articleid=2781790 Accessed November 2023
3. Apellis & The Harris Poll. Geographic Atrophy Insights Survey (GAINS). 2022.
Created and funded by Apellis. © Apellis UK Ltd. All rights reserved. UK-GA-2300063 I November 2023
Your need to know industry insights
EDITED BY KIMBERLEY YOUNG


Cyclist and ambassador for Red Bull SPECT eyewear, Gerald Rosenkranz, and his protective frames


DREAM TEAM
FIVE LAUNCHES
With Nicola Mari Alexander, co-founder of Peep Club 75S 83
Raising funds for wildlife, contact lens care, and more
BEHIND THE BRAND
To feature in OT’s What’s happening section, contact: kimberleyyoung@optometry.co.uk
Gill Smith, dispensing optician, contact lens optician, and regional manager for Valli Opticians in the North West
My role in the practice team is... dispensing optician, contact lens optician, and regional manager for Valli Opticians in the North West. I have worked at Valli Opticians for five years.
My first week in practice… I remember walking into Valli and thinking: ‘Wow, I can’t believe I’m working here.’ It’s a really nice practice. I was blown away by how much variety there was in the frames and lenses.
My role in the patient’s journey is... to guide them. As a dispensing optician, the patient puts their trust in you. They are choosing you to help them select
the right spectacles, so not only are they buying the product, but they are investing in you as well. I check the diary before the day starts and will greet patients by name when they arrive.
One thing I want my community to understand about eye care is... it is so important to get your eyes tested. It’s not just about vision, or glasses, it’s about health and wellbeing – so many issues can be picked up.

My favourite moment of the day is... when someone comes in for a collection. Say they are a first-time varifocal wearer, you’ve done the full dispense and they come back for collection, and you see how happy they are when they pick their glasses up.
I am excited about... developing further in my new role as regional manager to support the business and staff at Valli Opticians to help improve our patient experience and care.

For more from Gill on her practice team and lessons learnt from colleages, read the full profile on our website.

The NEW free-to-use CooperVision OptiStudent™ app is designed to put valuable, curated eye care content into the hands of optical studentsproviding a video library of high-quality content across key areas.
Through the app, students can also enter the CooperVision OptiStudent™ Awardsan annual competition that celebrates optical students from across Europe.
Raising funds for endangered species, children’s spectacles, contact lens care and more
1 On the wing SUNGLASSES
Bird Eyewear has launched new collaborations to raise funds for endangered bird species, including the ‘Swift’ frame, developed with the Royal Society for the Protection of Birds.The frame is inspired by the silhouette and speed of the bird, and has been made with plant-based patented material and Bird’s Activ-Adjust core technology. findyourbirds.com


2 Take care
CONTACT LENS CARE
PositiveImpacthas introducedCleadewcontact lenscareproductsfeaturing povidone-iodinefor disinfection.NickAtkins, managingdirectorof PositiveImpact,notedthe importanceoflenscarefor thesafetyandcomfortof contactlenspatients. positiveimpact.co.uk

3 Build your specs
SPECTACLES

Exeter Eyewear is making a splash in children’s eyewear with the SEEcreatures collection, distributed by Bondeye Optical.The collection fitting kits contain six fronts, six pairs of sides, and six combinations of trim colours. SEEcreatures-eyewear.com
4
Matte models
SPECTACLES
Silhouette highlighted its Pure Wave collection of lightweight full frame models with all-matte effects. Grooved glazing allows for an ultra-thin front and the planar trim zone transitions from the front to temple line in a minimalist style. silhouette.com


5 3D imaging EQUIPMENT
Haag-StreitUKhas launcheda3Dimaging optionfortheImaging Module910.Gemma Edwards,Haag-StreitUK productmanager,saidthe technologysupports clinicaleducation, includinginindependent prescribertraining. uk.haag-streit.com


Heidelberg Engineering highlighted its partnership with RetinSight, a provider of artificial intelligence-based solutions, through the Heidelberg Appway gateway. Used in conjunction with Heyex 2 and the Heidelberg AppWay, the Fluid Monitor produces a report to visualise and measure fluid. heidelbergengineering.co.uk
Sense Medical will host an educational webinar for eye care professionals focused on OCT and the diabetic eye screening pathway (DESP).The webinar, Getting ready for the OCTpathway in DESP, will take place on 4 September. shorturl.at/EKfVa


Zeiss will host a continuing professional development course, Optimising OCToutcomes: from acquisition to advanced analysis, on 3 December. It will feature a programme of interactive lectures and workshops. zeiss.ly/OCT-Course-24



After a successful launch in Australia, Cylite –which produces Hyperparallel OCT (HP-OCT) technology for whole eye imaging and measurements – told OT that it aims to make its technology available in the UK in the near future. cyliteoptics.com


Optopol Revo FC’s Biometry module has been enhanced for myopia management. Using reference data based on the NICER study, optometrists will be able to compare the spherical equivalent to refraction along with axial length of patients. bibonline.co.uk

Mountain biker and ambassador for Red Bull SPECT eyewear, on protective frames and taking style off-road

As a cyclist, or more specifically a mountain biker, I usually go for large screens because they offer me a lot of protection. They are sturdy when I have a crash. On the road bike, where I don’t have the danger of flying rocks or branches, I still go for the big ones because they protect me from the wind and weather. I also like the appearance.

The new ‘Kraft’ from Red Bull SPECT are my favourite frames. I love the shape and colours. It’s neutral because of the black and gold colouring, but still sharp-looking. What I really like is on the front it has vents which remind me of a sports car.The ‘Kraft’ also has a wing temple system.These are the last things I would lose if I crashed or rolled down a really bumpy section.

Number of frames: A drawer-full
What does vision and eye health mean to you?
For me, it means the world.The eyes are our portal to the world and to experiencing beautiful nature, friends; everything out there. It’s my highest priority to keep them safe. It is one of my biggest motivations to wear good protective sunglasses, especially in high-risk sports.
I even once went bungee jumping with them – they stay in place.The frame feels like it has the same level of protection and shield as a goggle but without the strange look of wearing a half-helmet and goggles. Even though sunglasses are a protective item, it’s a really cool possibility to express your style.That’s important to me.
There are two things I’m really proud of concerning this partnership. The first one is that Red Bull SPECTEyewear is my longest and oldest partner. I can’t even count, but it’s been a lot of years that I have been able to count on them.The second thing is that they’re from Graz, Austria, which is my hometown. It’s hard to find good partners near to you, even in your own country, but in your own hometown? It’s just so cool. It’s nearly too romantic.
0
Optical suppliers discuss the growing popularity of handheld tonometers and the potential direction of travel for glaucoma monitoring

Discussing the role of tonometry in informing a glaucoma diagnosis, Adrian Richards, sales director for Mainline Instruments, said: “It’s not the only thing that has to be considered when you’re diagnosing, but it’s an indicator and certainly important.”
Mainline Instruments distributes iCare tonometers in the UK, which utilise rebound tonometry to measure intraocular pressure (IOP) without the patient requiring anaesthetic drops.
Technological advancements have meant the iCare IC200 handheld tonometer can take measurements from a patient at any angle – sitting, standing, and lying down – making it beneficial for clinics where patients may struggle to sit up at a slit lamp.
Enhancements to the tonometers have included alignment functions which ensure the device is appropriately aligned to take measurements from the apex of the cornea.
The iCare Home2 tonometer allows patients to take pressure readings themselves, recording the date, time, intraocular pressure, and which eye the measurement is for. The results can be downloaded through an app or to clinic software.
Richards said: “Some hospitals now loan the devices out to patients with glaucoma so they can use it at home for a few days.”
This means that, instead of taking one pressure reading, multiple readings can be gathered at different times over the course
of several days, providing more data and opportunities to spot patterns.
This can be particularly helpful for patients with borderline readings who may find their pressures are higher in the mornings after waking, Richards shared, emphasising: “That could be doing damage to the eye if the pressure is too high. The increased pressure kills off cells within the eye and those aren’t repairable.”
Patients have shown an increasing interest in their own health over time, Richards said, adding: “They are very aware that taking a pressure reading can be critical.”
For example, at-home blood pressure monitors are allowing people to take regular readings. Richards suggested: “I think that’s the way technology will go. It will lead people into more self-monitoring and providing more information for better management of their problems.”
“There’s more to glaucoma diagnosis and management than just pressure, but it’s certainly a good indicator as to how your eye is performing,” he added.
Supplier, Grafton Optical, has partnered with AMETEK Reichert Technologies for more than 40 years.
David Thickens, CEO of Grafton Optical, explained: “The demand for reliable and user-friendly tonometry solutions has grown significantly, particularly within High Street optometry practices where efficiency and accuracy are paramount.”
Dave Taylor, director of marketing and business development at AMETEK Reichert Technologies, highlighted the need for tonometry to be easy-to-use and objective, so clinicians can be confident in the results.
Handheld tonometers are gaining popularity particularly due to space constraints in practice and the efficiency of the technology. Reichert solutions include the Ocular Response Analyser (ORA) G3 and the recently-introduced Tono-Vera Handheld Tonometer.
The ORA G3 offers benefits for risk stratification in glaucoma, incorporating corneal hysteresis to support predictions of glaucoma progression.
Taylor suggested that ORA is especially useful for clinicians who see a high number of patients with suspected and confirmed glaucoma, sharing: “It really helps refine
An AOP position statement, titled The role of optometry in revolutionising glaucoma care, details the association’s belief that a collaborative approach to glaucoma care, utilising the optometric workforce, could reduce the cost burden on the NHS.
The AOP has called for a new approach focusing on three core areas: a collaborative approach utilising the optometry workforce alongside secondary care, effective IT connectivity, and universal commissioning of glaucoma care for optometry to all patients, regardless of where they live.
Read more on the AOP’s economic modelling and key asks for glaucoma care on the website at: www.aop.org.uk/our-voice/policy/position-statements
who needs to be seen more frequently and possibly treated more aggressively.”
The Tono-Vera Handheld Tonometer features the ActiView alignment system to ensure measurements are taken at the corneal apex for objective and repeatable assessments.
Taylor suggested: “It takes the guesswork out of the measurement and provides IOP results that the clinician can trust.”
Advancing
Thickens told OT: “These advancements are crucial as optometry practices increasingly adopt a broader range of clinical services within the community.”
“By providing tools that enhance the accuracy and reliability of glaucoma management, we are supporting optometrists in delivering high-quality care to their patients,” he added.
Looking to the future of tonometry, Taylor shared that home measurement of IOP by patients is already here but quite rare, adding: “This will expand in the future once we better understand how the increased frequency of IOP data can help us better detect and manage glaucoma.”
He suggested: “Beyond that, implantable IOP devices are on the horizon that will provide 24-hour IOP data. One day we may manage glaucoma more like diabetes, where we have a feedback mechanism that can help us tailor the treatment to the individual eye more so than we are doing today.”

Advertorial brought to you by

Astheprevalenceofglaucomacontinues toriseglobally,1 sotoodoesasignificant andgrowingburdenonpatientcare.In additiontothe611,343peopleinEngland whoarewaitingforafirstappointment withanophthalmologist,2 theNHS backlogforfollow-upappointmentsis evenbigger.Thesedelaystocareare,in somecases,leadingtopermanentharm forpatientsintermsofavoidablevisual loss,whichisreportedtobeninetimes morelikelytohappeninfollow-up patientsthaninnewpatients.3 So,whatisaneffectivesolution? Domiciliarycareorvirtualclinicsthat areconvenientandefficientcould supportasolution.TheEyeoniconline perimetrytoolmakesremotecarefor glaucomaareality.Thevirtual applicationenablesvisualfieldtestingto beperformedinapatient’shomeonany computerortablet,withoutthe requirementfordedicatedmachinery. Thebenefitsincludelesstravel,more frequenttesting,earlierdetection,and reducedcostofcareinordertohelp alleviatetheglaucomamonitoring burdenandfacilitatescreening.
Eyeonic’scloud-based,AIpowered perimetryplatformisagamechangerfor optometristsandophthalmologists. Itprovides:
•Universalaccessibility:reachmore patientsonanycomputerortabletin yourclinicorbeyond
•Testprocess:similartoastandard perimetrytest,butwithoutthe limitationsofbulkymachinery.Users arepresentedwithflickeringtargetsof alternatinglightanddarkringsonthe screen.Theyfixateonaspinninggolden startandclickwhentheyseethetarget
•Webcammonitoring:detectchangesin headposition
•Verbalcuesandfeedbacksounds: guidetheuserthroughoutthetest
•High-security:architectureand databaseintegrity
Eyeonic discusses how its online visual field testing supports remote care glaucoma monitoring
•Testduration:aroundthreetofive minutespereye
•Assessmentoptions:24-degrees, 10-degrees,30-degrees,amonocular pilotvisiontest,andabinoculardriving visiontest.
Reliable test at home or in clinic
Eyeonicvisualfieldtestingdelivers:
•Accurate,sensitiveandrepeatable resultsthatarecriticallyvalidatedwith high-qualityscientificresearch. Accuracy,sensitivity,andrepeatability whichisonparwithconventional visualfieldmachines4,5
•Superiorpatientexperiencethan standardperimetrytests,6providinga comfortabletestingexperience
•Home-basedresultsthatareconsistent withthosegeneratedin-clinic.
Removing testing barriers
Eyeoniconlinevisualfieldtestingis patented.PoweredbyAIfacial recognition,itdetectschangesinuser headpositionthroughawebcam.The testonlycontinueswhenthehead positionisacceptable.Theapplication alsohasmulti-languagevoiceandtext instructionoptions.
Why Eyeonic online visual field test?
TheEyeonicplatformwasdevelopedbya distinguishedophthalmologist, glaucomaspecialist,andcomputer programmerinAustraliawiththevision toreshapeglaucomadetectionand monitoring.Theinnovativesolution helpspractitionersalleviatetheirpatient backlog,reducecostofownership, improveglaucomamonitoringefficiency bothat-homeandin-clinic,andimproves patientexperience.

Contact Eyeonic at support@eyeonic.com or visit the website www.eyeonic.com.au for more details and a one-month FREE trial for clinicians.
REFERENCES
1. Tham YC, etal. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and metaanalysis. Ophthalmology.2014
2. Statistical Press Notice – NHS referral to treatment (RTT) waiting times data, March 2024 (www.england.nhs.uk/statistics/wp-content/ uploads/sites/2/2024/05/Mar24-RTT-SPN-PrePublication-PDF-K.pdf)
3. www.rcophth.ac.uk/wp-content/ uploads/2022/11/RCOphth-response-to-PublicAccounts-Committee-inquiry-Managing-NHSbacklogs-and-waiting-times-Nov-2022.pdf
4. Simon Skalicky, etal.Online circular contrast perimetry via a web-application: optimising parameters and establishing a normative database, The Royal College of Ophthalmologists, 2022
5. Joshua Meyerov, etal.Online circular contract perimetry: a comparison to standard automated perimetry, Asia-Pacific Academy of Ophthalmology, February 2023
6. Joshua Meyerov, etal.Circular contrast perimetry via web application A patient appraisal and comparison to standard automated perimetry, American Academy of Ophthalmology, September 2022.

Co-founder, Nicola Mari Alexander, on designing dry eye treatments that patients look forward to

How did Peep Club come about?
I decided to change careers from working in tech and studied optometry at City, University of London. One of my practice patients was my lifelong friend, now partner in the business, Natasha. She was complaining of dry eyes and I suggested we try out different solutions. Natasha found that she had a graveyard-drawer of products that she had used for a few days or weeks, but ended up not continuing because she didn’t like keeping them out on the counter and forgot about them. As a brand strategist, she thought that if we could create a beautiful brand, we could have a whole new audience of people like her. I knew there was so much room for us to make a mark.
What can you tell us about the research behind the products?
Every month there’s new research, so we’re constantly looking at what’s out there and reformulating. I think one of the beautiful things about how we operate is that we are a



small batch manufacturer.That gives us a huge amount of agility. We have an amazing set of advisers, oculoplastic surgeons, ophthalmologists, and dermatologists, with a wealth of experience who constantly inform our development. Peep Club is sold by Positive Impact, which we love, to independent optometrists.The optometrists who have dry eye clinics know so much about the market – they go to the trade shows and have the top in-practice treatments – and ask us questions. Being able to take that all on board is one of our major assets.
What decisions went into the branding?
The principle behind our branding is: if you saw the product, would it make you feel good? If the product gives you that little endorphin hit and you look forward to it, then you are more likely to remember to use it. We also look at developing products that are easily incorporated into people’s routines without asking too much of them.
Peep Club in a few words: An award-winning provider of eye care products for dry or sensitive eyes
Three facts about Peep Club
Peep Club was formed by childhood friends, Nicola and Natasha
The brand’s ethos is to be ‘a treat, not just a treatment’ for dry eyes
Nicolaretrainedasan optometrist,inspiredby herfatherwhoshe describesas“thenicest maninoptometry.”








WI
LIVE WITHOUT…
Camilla Anderson, brand and contact lens manager at Park Vision Opticians, Nottingham, on how her practice keeps contact lens patients engaged
ehavehadourcontactlensbuddy systeminplaceforaboutayear.Oneof thereasonsforitsintroductionwasthe amountof clinictimethatwastaken upwithcontactlensteaches.Ihaveworncontact lensesfor20years,andI’verecentlystartedfitting orthokeratology(ortho-k)lensesaswell.Having thatpersonalexperienceallowsmetositdownwith patientsfromtheagesof sevento85(ouroldest patient)andgivethemthetimeandcarerequired.
Adapting the buddy system for ortho-k patients
When one of our three optometrists comes out of the testing room with a patient who wants to try contact lenses for the first time, they introduce them to me and say, ‘Camilla is going to be your buddy. Ask her questions now, before you come back and we fit your contact lenses. Is there anything that scares you? Is there anything you want to know beforehand?’
I always make sure that the parents and the children know that I’m at the end of the phone if they need to ask me anything before they come in. I am there as their point of contact for any questions. I say to them, ‘Go away and practise
holding your eye open.’ With children, I take the contact lens, put it in my own eye, take it out, and show them how easy it is and that it’s not scary or painful. We sit and work together, and find a specific way to make sure they’re comfortable.
I usually use the separate testing room, upstairs. It is just myself, the patient, and patient’s parent if needed. We put Alexa on, have a bit of a chat, and then get into it.
One patient, in his mid-50s, really wanted contact lenses to play squash. We had a weekly catch-up, for half an hour. I think he had four teaches with me, week after week. As soon as he got it, he was raving about it. He’s now telling everyone and suggesting contact lenses to people, whereas he was ready to walk away after the first go.
It’s about getting people into the swing of contact lenses, signing them up to the direct debits, and then discussing wear time with them, as well as subscriptions and how many lenses they need. Obviously, that includes care – keeping in contact with them about hygiene and eye health. It’s the continuity that’s important.
"This a great job for optometrists to provide that clinical excellence, to make sure your patients receive the best possible care. This is the job that you signed up for when filling out your UCAS form"
Tom Critchley, Principal Optometrist, SpaMedica

Do you have a passion for patient care and strive for clinical excellence? You could be the perfect fit for our growing team of talented optometrists.
• Great work life balance -Only 1 in 4 Saturdays
• Continuous training and development
• Biannual bonuses
As the soleoptometriston the island,you'llhavethe unique opportunityto work closelywith Dr. O'Neal,a respectedlocal ophthalmologist,and Mr. NicholasLeefrom WesternEyeHospitalin London.Our state-of-the-artpracticeis equipped with top-of-the-lineZeissCirrus 6000OCT and fundus cameras,ArgonLasersetc ensuringthe higheststandardof eye care for our patients.Join our team at TortolaVisionand make a meaningfulimpactto the localcommunity.
Job Description: Optometrist at Tortola Vision Centre, Road Town, Tortola, British Virgin Islands
Position : Qualified Optometrist
Contract: 2 years (with an option to renew)
Starting Salary: $72,000 per annum Locally taxes total of 14%
Working Hours:
- Monday to Friday: 9 am - 5 pm
- Every other Saturday: 9 am - 2 pm
- Potential work on holidays and community service
Start date 1st August 2024
Benefits:
- 15 days paid vacation (Not including Sat/Sun)
- 12 days paid sick leave (with doctor's certificate)
- Paid British Virgin Islands Public Holidays (14)
KeyResponsibilities:
- Conducting comprehensive eye exams using provided equipment (ophthalmoscope, retinoscope, slit lamp, phoropter, trial lenses, tonometer, autorefractor, lensometer, pupillometer, IOL measurement tools).
- Taking detailed medical histories.
- Performing routine and cydoplegic refractions.
- Conducting visual field tests, analysing results, and determining the best treatment plans.
- Writing prescriptions for glasses, contact lenses, and basic medical conditions.
- Referring complicated medical diagnoses to ophthalmologists.
- Educating and counselling patients on the proper use and care of glasses, contact lenses, and medications.
- Checking the prescription and alignment of glasses before dispensing.
- Performing patient follow-ups.

Requirements:
- Must be able to work independently without supervision.
- Proficient in all duties related to optometry.
- Honest, reliable, and able to take initiative.
- Boarding provided for the first month; thereafter, the applicant must find their own accommodation.
- Responsible for all immigration costs, living expenses, and expenses associated with family members.
- Responsible for transportation to and from work.
EmploymentDetails:
- Full details of employment will be provided upon application.
- Tortola Vision Center will pay a portion of your work permit fees up to a maximum of $2,000.
- Assistance with registering with the British Virgin Islands Medical and Dental council will be given
- Remuneration based on experience and evaluation.
- Salary is paid twice per month.
Indemnity Insurance
This is done via the practice but you will need to contribute $1000.00 per year.
Application Process:
Interested candidates should apply with their CV and cover letter. Full details of the employment contract and benefits will be provided upon application.
Mr Nicholas Lee works at the Western Eye Hospital in London and works four months of the year at Tortola Vision Centre. You are welcome to discuss the role with:
Jennifer O'Neal - calacrab45@yahoo.com, + I (284) 494-2020
Nick Lee - nicldeel@nhs.net, 07956 263804
Join our team at Tortola Vision Center and experience the beauty and serenity of the British Virgin Islands while advancing your career in optometry. We look forward to welcoming a dedicated and skilled professional to our team.

Paul Alexander, policy and governance manager for the AOP, on a message to the public about lifelong eye care and how optometrists support people through their lives

The AOP is launching a short animation to explain to the public how optometrists support people throughout their lives.
The 60-second animation, which will be publicised through social media, delivers quick and simple messages about the importance of getting a sight test, and the health benefits of regular eye examinations.
It will be supported by web pages for patients, explaining key facts about eye health and care, and encouraging them to use the full range of services that optometrists offer.
that dispensing plays in helping people get the most out of their sight, and their lives.
The messages illustrate the importance of detecting refractive error as early as possible in a child’s life. It also touches on looking after your sight throughout your life. The web pages supporting the animation provide advice on keeping your eyes healthy, such as UV protection, safe use of contact lenses, and giving up smoking.
These resources also refer to eye disease and problems that occur, particularly in older age. Our ageing population means that there will be more eye disease, more pressure on hospitals, and a greater role for optometrists in identifying disease, referring patients, and supporting them through disease and potentially sight loss.
NAME: Paul Alexander ROLE: Policy and governance manager
We know that many members of the public still do not understand the health role of optometrists. Many see their High Street practice as a retailer, not a health care provider. The animation emphasises the health aspect of optometrists’ work, while explaining the key role


The AOP’s patient leaflets are produced mainly for our members to hand out to their patients. But we have found that many members of the public access the leaflets from our website directly. This demonstrates the public demand for good quality information, and gives us an opportunity to amplify the role that optometrists play.
The animation touches on eye care issues from pregnancy and birth right through to older age, highlighting how optometrists enable people to live fully active lives, as well as how they identify eye disease and support people with eye issues.
We look at five key stages of life:
1. Pregnancy and childbirth: the eye issues that expectant mothers might experience, what they should expect after their baby is born, and how to spot eye problems early on
2. Early years and school age: emphasising the importance of checking children’s eyes early, and ensuring they get the right prescription as soon as possible
3. Young adulthood: underlining the point at which young people need to start looking after their own health, and the financial help still available to most young adults
4. Working age: covering the help available to get the right eyewear for work, and explaining the value of getting the right eyewear for hobbies and sports
5. Older age: showing how an active and rewarding older age can be facilitated by good eyewear, as well as talking about the eye diseases that might come at that time of life.
In addition to eye health-related information, the resources include advice on areas such as accessibility and financial support. Our research shows that many people put off attending their optometrist because they fear the expense that could result. Therefore, we are highlighting the financial support available in the four nations. This information was already available on the AOP website, and we wanted it to be easy to reach from the animation landing page.
The animation will be accessible on the AOP website. Although there is a voiceover, we designed it so that it can be understood if played silently and so would be ideal for showing on screens in practice waiting rooms.
As well as showing the video, we’d recommend that practices have copies of AOP patient leaflets available in case people who have seen the animation ask for copies.
Find the AOP’s new animation online at: www.aop.org.uk/lifelongeyecare
A review of AOP activity in the last two months

With a Labour government in place following the 4 July election, OThas been exploring the core priorities of the optometry profession for the new administration, and the next steps for ministers. Follow OT’s coverage on a dedicated General election 2024 page.
www.optometry.co.uk/general-election-2024

Dr Ian Beasley, AOP head of education and OT clinical editor, explored how adjustments to the three pillars of sleep, nutrition and exercise could deliver wellbeing benefits. Rewatch the webinar online.
www.aop.org.uk/webinars

GOC strategy discussed
The AOP Council met on 5 June, welcoming new Councillors and discussing key aspects of the General Optical Council’s draft strategy 2025–2030. Read the takeaways on the OT website.
www.optometry.co.uk/ aop-council-meeting
HSOC 21-22 September
The AOP, with headline sponsor Bausch + Lomb, will host the Hospital and Specialty Optometrists Conference. Find out more: www.aop.org.uk/events
OCT Day 6 October
A day of education dedicated to OCT will be delivered by OT Sponsors include Optos, Topcon, Specsavers and Apellis
CPD last year of cycle September
OTwill release a CPD survival pack, sponsored by CooperVision. It is designed to support practitioners in meeting their CPD requirements in the last year of the cycle
Ahmad, discusses the public perception of optometry in Scotland

I joined the profession when I was 16 years old, straight out of school, initially training as a dispensing optician, and later an optometrist.
Thinking back to what I recall about the public’s perception of optometry when I first qualified, practising in Scotland, it has always been relatively positive. These experiences have been post GOS changes in Scotland, when a sight test became free for everyone. Having a single message for the public that, regardless of where they live or what they earn, an eye test is free has allowed the public’s perception of optometry to change at a nation level.
I have observed positive change and evolution with the contract over the years as it hasn’t stood still. In the last couple of years, it’s evolved further to enhance the role of an optometrist. During the pandemic, it felt like more so than ever before, the profession was being looked at as the first port of call for everything related to eye care. Patients increasingly presented to their optometrist.
Nowadays, in most areas in Scotland, when a patient calls their GP with anything to do with their eyes, they are told to visit their optometrist by the receptionist. This has been drilled into GP practices over the last few years and, because of this, it has started to filter out to the rest of society. The efficiency at which we can see patients and treat them makes the patient ever wonder why they called their GP in the first place. The community has started to present themselves –they have learnt to come and see the optometrist first. However, these types of messages take time and effort to filter through to the general public. What worked in the past with posters and leaflets may not be as effective now when we are much more digital-focused.
“ The community has started to present themselves – they have learnt to come and see the optometrist first
The public’s perception of optometry in Scotland will continue to improve and is being fast tracked by the number of IP qualified optometrists. This gives patients an immediate response to their presenting eye problem, and quicker access to the treatment they require whilst being able to avoid long hospital wait times. In the future, I would like to see all optometrists IP registered and considered the first port of call for any eye-related issues. Shared care schemes are working well, but these require support and funding in order to roll out across nationally. Optometry is progressing in a positive direction as a profession, but it is up to each individual optometrist to make sure we continue to learn and develop our skills.
0
1 The cover feature
Read about the range of factors influencing the public’s perception of optometry PAGE 10
ADNAAN’S TOP READS
2 IP and me
Clinical scenarios are explored. This edition looks at herpes simplex keratitis PAGE 36
3 In focus
Three new AOP Councillors share their views on the profession, now and in the future PAGE 42
GPs are struggling to cope. And yet every year 1.35 million people visit their GP for medicines that optometrists are trained to provide. One simple solution can save one million appointments.
timising optometry ackle the GP crisis.

Association of Optometrists
The world'sonly myopiamanagementcontact lens supportedby a 7-year clinicaltrial2· 3 A

tUsing measuredandmodeleddata,pooledacrossages(8-17), MiSight®1 day slowedmyopiaprogressionby an averageof approximately50%. f12 monthspost-treatment,evidenceindicatesthat no accumulatedmyopiacontrolbenefitswere lost following3 or 6-years of MiSight®1 day wear (on average,for childrenaged8-15 at start of wear).Instead,eye growth revertedto expected,age-normalrates.
1.Arumugam8etal.ModellingAgeEffectsof MyopiaProgressionfortheMiSight1dayClinicalTrial.Invest.Ophtholmo/VisSd.2021 ;62(8): 2333. 2.ChamberlainPetal.
A 3-year RandomizedClinicalTrialof MiSightLensesfor MyopiaControl.Optom VisSci 2019; 96(8): 556-567. 3. ChamberlainPet al.Long-termEffectof Dual-focusContactLenseson MyopiaProgressionin Children:A 6-year MulticenterClinicalTrial.Optom VisSci 202 2; 99(3): 204-212. 4. Chamberlain Pet al. Myopiaprogressionon cessationof Dual-Focuscontact lenswear: MiSight 1 day 7-year findings.Optom VisSci.2021; 98(E-abstract): 210049. 5. ZadnikKet al. FactorsAssociatedwith RapidMyopia Progressionin School-agedChildren.Invest.Ophtholmo/.Vis Sci.2004; 45(13): 2306. 6. HammondD,ArumugamB,et al.MyopiaControlTreatmentGainsareRetainedafterTerminationof Dual-focusContact LensWearwtth no Evidenceof a ReboundEffect.Optom VisSci.2021; 98(E-abstract):215130.
© 2024 CooperVision.CooperVision®andMiSight®are registeredtrademarksof TheCooperCompanies,Inc.anditssubsidiaries.
CVGY122291-1