When the Doctor Became Critically Ill
Harvey Serota, MD
Can You Exercise Your A-fib Away?
Shingles Increases Odds of Stroke and Heart Attack
Two Healthy Diets May Reduce Alzheimer’s Risk
Had a Kidney
Stone?
This Diet May Help Prevent Another Emergency Room Vs. Urgent Care: Knowing Which You Need
Parkinson’s Disease
May Be More Common than We Thought Organ Donation
Debunking the Myths
Hot Flashes
Everything You Ever Wanted to Ask
SPRING/SUMMER 2023 | ST. LOUIS METRO
NEW!Fora FreeSubscription Seepage4
Publisher Editor
Todd Abrams
Design Art Direction
Production
Michael Kilfoy
Studio X
Account Executive
Carol Kindinger
Printing
Walsworth Fulton Advisory Board
Dr. Donald Bassman
Dr. Joshua Cohen
Dr. Shaun Donegan
Katy Dowd
Robert Fruend
Joel Iskiwitch
Dr. James Jenkins
Dr. Steve Lauter
Humor Credits:
Robert Mankoff
Welcome to HEALTH&CARE Journal.
To our Readers:
Welcome to the Spring/Summer 2023 Issue of HEALTH&CARE® Journal.
Our mission with this publication is to save people from preventable suffering and premature death caused by the leading chronic diseases. The way we seek to do that is to provide helpful, easy-to-understand information from experts that our readers can put to use for improved health outcomes.
Examples in this issue:
n Learning how to perform CPR can help you save lives of heart attack victims, and where you can be trained to perform it.
n When to use an urgent care clinic and when you really need to go to a hospital emergency room.
n The shingles vaccine not only is very effective at preventing that painful and potentially dangerous condition, but may also help prevent heart attacks and stroke.
n Diet and sleep prescriptions that may help prevent Alzheimer’s disease.
n Why cancer screenings are so important to prevent more advanced and harderto-treat spread of the disease.
n How organ donation is saving lives while protecting live donors.
n And much more . . .
So, please take time to page through this issue and help yourself to information that can help you achieve better health outcomes for yourself and your loved ones.
We continue to be very interested in hearing from readers about HEALTH& CARE Journal – content in the magazine, topics you would like to see covered and other information that would be helpful. You can contact us on our website.
Todd Abrams Publisher
toddabrams1@gmail.com

4 H&C
For a free subscription to HEALTH&CARE Journal, or to unsubscribe, visit healthandcarestl.com
Don (pictured right)
Diagnosed with lung cancer – Early detection
Lung cancer screening
You’re more important than you know.
You touch lives. You give smiles. You are someone’s favorite person. Your health matters.
A retired Navy petty officer, Don smoked a pack a day for more than 40 years. After receiving a flyer in the mail explaining the risk factors for those with a smoking history, he decided to schedule a lung screening. He was shocked to discover that he had early-stage lung cancer. As a husband, father, and active grandparent, he is now cancer-free and living a happy life surrounded by his loving family.
Four out of 10 adults will develop cancer in their lifetime, but screening tests can catch cancer early and help save lives. Give yourself and those who love you peace of mind, schedule a routine cancer screening and take control of your health today.
To see Don’s story and to learn which cancer screenings might be right for you and to schedule an appointment, visit getscreenednow.com or call 314-310-7574

For the lives you touch.

#10 in the country. #1 in Missouri.
Spring/Summer 2022-23
ARTICLES IN THIS ISSUE
10 Health Briefs
12 The Patient’s Advocate Heart & Vascular Health
14 Can You Exercise Your A-fib Away?
16 Shingles Increases Odds of Stroke and Heart Attack
17 Leg Cramps and Pain? It Could Be PAD
18 Heart Attack Deaths Fell Over
20 Years
19 If Someone Collapsed, Could You Perform CPR?
20 Marijuana, Meth, Cocaine & A-fib
21 Exercise OK for Inherited Enlarged Heart
22 Deadly Form of High Cholesterol Can Catch Blacks by Surprise Cover Story
24 When the Doctor Became Critically Ill
Neurology & Stroke
26 Depression Ups Odds for a Stroke, and vice-versa
28 Severe Seizures Are Rising, Especially Among Minorities
29 Hints That a Sleeping Pill Might Help Prevent Alzheimer’s
30 Two Diets May Reduce Brain Plaques, Alzheimer’s Risk
31 Americans’ Odds for Parkinson’s May Be Higher Than Thought
32 Essential Tremor and Parkinson’s Disease: How They Differ
33 Is It Parkinson’s? These 10 Signs Could Tell
Cancer Prevention & Treatment
34 Only 1 in 7 Cancers Are Caught Through Cancer Screenings
36 Just Half of Those with a Positive Stool Test for Colon Cancer Get Follow-Up Colonoscopy
38 U.S. Cancer Deaths Decline
Overall, But Prostate Cancers Make Rebound
Diabetes Care & Prevention
40 Spinal Cord Stimulation May Ease Diabetic Neuropathy
42 40-Year Study Finds Weight-Loss Surgery Extending Life Spans
43 Certain Class of Diabetes Meds Could Cut Dementia Risk
Kidney Disease
44 Had a Kidney Stone? This Diet May Help Prevent Another
45 Debunking Myths About Organ Donation
Better Breathing
46 Advent of Electric Cars Is Already Improving Health
47 Global Review Finds Vaccination Cuts Odds of Long COVID in Half
48 The Most Common Sleep Disorders
51 New Screening Questionnaire Might Spot More Cases of Hidden COPD
6 H&C
Aches & Pains
52 Many Turn to Marijuana to Ease Chronic Pain in Place of Opioids
54 Emergency Care Vs. Urgent Care: Knowing Which Is Needed
56 What Exercise Regimen Works Best to Ease Lower Back Pain?
57 Natural Ways to Manage Arthritis Pain
Mental Health
58 For Adults with ADHD: Let’s Make Now Better So Later Is Easier
60 Could Bacteria in Your Gut Help Spur Depression?
61 Americans Are Getting More Comfortable Talking Over Mental Health with Their Doctors
62 Acts of Kindness Could Be Natural Antidepressants
Women’s Health
64 Everything You Ever Wanted to Ask about Hot Flashes
66 MRI Might Boost Cancer Detection for Women with Dense Breasts
Aging & Caregiving
67 Good Sleep Could Keep Illness at Bay as You Age
68 Drug and Alcohol Fatalities Among U.S. Seniors Have Tripled Since 2000
70 Brisk Walk Daily Can Prevent Early Death
HEALTH&CARE JOURNAL is published twice a year by HealthCom Network LLC and distributed to Missouri and Illinois homes in the St. Louis Metro area. Article topics are chosen to provide helpful information about health and care topics of interest.

Opinions expressed in articles and editorials are those of the authors, and do not necessarily reflect the views of HealthCom Network. While every effort is made to assure accuracy, we are not responsible for how information found in HEALTH&CARE Journal is used. Readers are encouraged to consult with their healthcare providers for advice about their own care.
We are very interested in hearing from readers about content in this magazine, and about topics they would like covered. Correspondence should be sent to the address below or to editor@healthandcarestl.com
Reproduction of content of this magazine without permission is prohibited. All submitted materials, including images, logos and text for advertising, articles and editorials are assumed to be the property of the contributor, and HealthCom Network does not take responsibility for unintentional copyright infringement. HealthCom Network has the right to refuse advertising and content not deemed appropriate for this publication.
For information regarding advertising, call, write or email: HealthCom Network
P.O. Box 411036 St. Louis, MO 63141
Todd Abrams, Publisher toddabrams1@gmail.com
314-443-3024
Carol Kindinger, Account Executive carolkindinger@gmail.com
314-452-3576
HEALTH&CARE is a registered trademark with the US Patent and Trademark Office
71 Quiz: Seniors, How Much Do You Know About Exercise?
72 Quiz Answers
74 Book Review & Healthy Humor
7 H&C
Association of Health Care Journalists
Features in this Issue
12 The Patient’s Advocate
24 Cover Story: When the Doctor Became Critically Ill
48 The Most Common Sleep Disorders

58 Emergency Room vs. Urgent Care – Knowing Which You Need

68 Drug and Alcohol Fatalities Among U.S. Seniors Have Tripled Since 2000


8 H&C

Health Briefs
Big U.S. genetics study is already helping participants.

Called “All of Us,” the study aims to eventually include at least 1 million people, in an effort to accelerate medical breakthroughs.
U.S. National Institutes of Health
Artificial intelligence is coming to a medical practice near you.

Experts who reviewed advice from ChatGPT gave it high marks for accuracy and empathy. But human doctors aren’t an endangered species; AI will help them respond to a growing wave of patients who are seeking help online.

Exercise could be an antidote to addiction.



Investigators who analyzed 43 studies from around the world found a link between physical activity and reduced substance use among people in treatment for alcohol and drug abuse.

Young guys are
People whose work is piecemeal and sometimes depends on tips and commissions tend to be in poorer health than workers with more stable incomes, new research confirms.

Journal of Applied Psychology


The FDA sent out yet another warning, noting that no selective androgen receptor modulators (SARMs) have been approved by the agency, and the substances are dangerous drugs, not dietary supplements.
Journal of the American Medical Association
A new report estimates that dozens of different types of everyday consumer products contain chemicals that emit airborne toxins called volatile organic compounds (VOCs).

Silent Spring Institute


10 H&C
JAMA Internal Medicine
PLOS ONE
using banned ’SARM’ supplements to bulk up, with harmful results.
Thousands of tons of noxious chemicals are released into U.S. homes each year.
Gig economy could be harming workers’ health.
Years after COVID, some struggle with lung conditions.
One Houston police officer is still fighting an interstitial lung disease (ILD) known as pulmonary fibrosis (PF), and he’s not the only COVID survivor to do so.
Pulmonary Fibrosis Foundation
Deep sleep could be a buffer against Alzheimer’slinked memory loss.

In a study, getting good amounts of that high quality sleep helped those with beta amyloid plaques in their brain perform better on memory tests.
BMC Medicine
One in 7 U.S. veterans with a firearm at home has considered suicide.

Suicide by firearm is the No. 1 cause of suicide death among vets. Researchers say there is an urgent need for mental health and substance abuse services for veterans as well as programs to encourage secure gun storage.
UCLA Center for Health Policy Research
Dog-walking downside: Fractures and head injuries.
Over 20 years, more than 422,000 U.S. adults went to the ER because of leashed dog-walking injuries, with fractured fingers topping the list.
Medicine & Science in Sports & Exercise
Your hospital room affects outcomes after surgery.
A new study finds that a private room, close to the nursing station with a clear line of sight from it improves survival rate following surgery.
Experts suggest parents start conversations about social media with their children and set safe boundaries for them.
The American Psychological Association
University of Michigan School of Medicine
11 H&C
In survey, half of parents said they believe that social media is harming their kids.
The Patient’s Advocate
By Jane Tucker
Being a patient is not for sissies.
I’ve been a cancer patient for 24 years and, quite frankly, started out as a sissy…. But not anymore.
I will give you some tips in this column about what to do and what not to do when you become a patient.


Let’s start with the “to-do” list. Many of us have been brought up with “don’t bother the doctor”. I’m here to say bother the doctor if you want control over your condition. Now don’t be silly about it but be your own advocate. That’s my first and most important message.
Second is to get a positive vision in your head. Maybe your college graduation, your daughter’s wedding or even some-
thing simple like how your garden will look in the spring. If you are unsure about your own illness, find yourself a hero to visualize. A swimmer without a leg, a single parent who somehow made it. You get the idea.
Number three: your emotions might be all over the place. It’s part of the process. It’s OK to be scared, go ahead…then get un-scared. Maybe cry ... then stop crying. Finally, find something to get happy about. It could be your healing or something else. Then…get strong! Everyone feels vulnerable when they become a patient. You can get over it quickly.
Point four….as I mentioned, be an advocate, but no one should go this alone. Get a friend or make a new one, a family member, a neighbor, someone you trust. You can take someone to every appointment. That is your right, and we all need help and support.
Five…pay attention to your body. You know it well. If something doesn’t seem

right and it’s been over two weeks… tell your doctor. If you have something new and it doesn’t go away…. speak up. If it’s in a personal area don’t let that stop, you. All of us, including your doctor, has probably had something in a personal area. Again, don’t be afraid.

Next…if you can’t get an appointment in a reasonable time, get tough. See a nurse practitioner or another doctor. Get on a wait list but don’t wait if you need help. You can challenge decisions. You can get second opinions. A good doctor will encourage you. Appeal insurance decisions about procedures or drugs if they seem unfair.
So finally, a few extra tips.
You’re the boss over your body, your injury, your disease, and yes, even your doctors and your family. Pay attention, be kind to people who help you and speak up when they are not. Finally, and most importantly, visualize your body free of your issues or at least in control of them. Don’t be hard on yourself…just do the best you can.
And really, finally…. I wish you well.
LEARN MORE AT ArchWellHealth.com/LiveWell or call (314) 449-9727
Senior primary care with same-day appointments for members.
This is what retirement looks like
by Charles Brennan
Retired KMOX host Charles Brennan talks about his new life of leisure.
Retirement has changed me. I’ll give you some examples.
Before I turned off my microphone at KMOX radio, I got up every morning at 5:45. Now, I regularly sleep in till 6:15.
I used to spend the early morning poring over the newspaper to stay abreast of the local issues we’d discuss on my morning radio show and then again Thursday evening on Channel 9’s Donnybrook.
Ok, I still consume a lot of news. But now, it’s because I like to stay informed. And, retired or not, I’m still Donnybrook’s resident provocateur.
As a retired person, I also sit still less than I used to. Since May, my wife Beth and I have traveled more than 20,000 miles. I’ve taken golf lessons and studied French. But retirement is not all fun and games. I rake leaves and take out the garbage more, too.
Since retiring, I’ve also led efforts to plant 10,000 daffodil bulbs in Forest Park and along the River Des Peres and to enhance a Hanley Road underpass with chalk art. Even us old guys want to make St. Louis a prettier place.
I also hike more. I log 25,000 steps several days a week. On Sunday mornings, I sometimes run up and down the steps at Cahokia Mounds 20 times or more. Why do I do it? Because I can. Also, I’m 63. Who’s going to stop me?
That reminds me of one thing that has NOT changed since my retirement: my weekly appointment at 20 Minutes to Fitness in Clayton, where I have worked out since 2006.
The half hour I spend there on Wednesday afternoons helps me build the strength and maintain the energy I need to live this glamorous retirement lifestyle.
At my side is my personal trainer Darrell Connor. He guides me through a series of exercises designed to work every major muscle group on specialized MedX equipment.

There’s no cheating with Darrell. There’s also no worry about injuring myself by performing an exercise incorrectly.
Over the years, Darrell has also become a friend. Remember those Sunday mornings at Cahokia Mounds I mentioned? Darrell runs those steps with me.
The truth is the staff at 20 Minutes to Fitness are all firstrate. Many have backgrounds in physical therapy or exercise physiology. A physical therapy assistant named Robb recently worked wonders on my sore shoulder. Others have helped me train safely while recovering from a hip replacement and a hernia.
If you’re busy, or if your strength and balance aren’t what they used to be, or you’re tired of being out of shape, I suggest you give 20 Minutes to Fitness a call. First-timers get a complimentary in-person consultation and workout. You can’t beat free.
If you’re like me, you’ll feel better and have a more positive outlook afterwards. Retired or not.
For more information on 20 Minutes to Fitness, call its local studios in Clayton (314-863-7836), Chesterfield (636-536-1504), Sarasota or Tampa, or visit 20MinutesToFitness.com.
Just 20 minutes. Just once a week.
Can You Exercise Your A-fib Away?
Millions of Americans live with a common abnormal heart rhythm known as atrial fibrillation (A-fib), but new research suggests that exercise might ease the severity of the condition.
A-fib occurs when the upper chambers of the heart quiver chaotically, causing a fast and irregular heartbeat. Symptoms may include heart palpitations, breathlessness, dizziness and/or extreme fatigue. When left untreated, A-fib dramatically increases risk for stroke and heart failure.
Benefits of exercise
When folks with A-fib participated in a six-month exercise program, they were better able to maintain a normal heart rhythm and had less severe symptoms than those who only received information about the benefits of exercise. The benefits lasted for at least one year.
“Participating in a structured exercise program for up to three and a half hours per week can reduce the likelihood of ongoing episodes of arrhythmia and decrease the severity of A-fib-related symptoms, such as palpitations and shortness of breath,” said study author Adrian Elliott, a physiologist and research scientist at the University of Adelaide in Australia.
For the study, 60 people with A-fib participated in a six-month exercise regimen that included supervised exercise each week for three months and then every two weeks for the remaining three months. They also received an individualized weekly plan to follow at home. The goal was to work up to 3.5 hours of aerobic exercise each week. Another 60 people received exercise advice and were asked to engage in 150 minutes of physical activity every week.
Treatments for A-fib
Everyone in the study continued their usual A-fib medications. A-fib is typically treated with medication to lower the risk for stroke and/or drugs that control heart rate or rhythm. Sometimes a procedure known as ablation is needed. During
ablation, your doctor creates small scars in the area of your heart that is causing the irregular heartbeat using radiofrequency energy.
Results of the study
After one year, the A-fib recurrence rate was 60% in the exercise group, compared to 80% in the advice-only group. In the study, recurrence was defined as having an A-fib episode that lasted longer than 30 seconds, undergoing an ablation procedure, or requiring ongoing anti-arrhythmic drug therapy.
People in the exercise group also had fewer heart palpations and less shortness of breath and fatigue at one year compared to those folks in the advice-only group.
“Our findings do suggest that patients who participate in regular aerobic exercise may be able to reduce the need for rhythm control therapy,” Elliott said. Exactly how exercise helps control heart rhythm is not fully understood yet, he said.

The findings were presented at the European Society of Cardiology’s annual meeting online. Research presented at meetings is typically considered preliminary until published in a peer-reviewed journal.
Outside experts agreed that exercise is an important part of A-fib treatment.
“This is a very interesting and important study for patients with a history of
atrial fibrillation, the most common heart arrhythmia,” said Dr. Deepak Bhatt, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital Heart and Vascular Center in Boston.
“Physical activity and exercise appear to decrease atrial fibrillation, including the severity of symptoms,” Bhatt said. “So, like for most things in cardiovascular medicine, exercise is good for you.”
Dr. Laurence Epstein agreed. He is the system director of electrophysiology at Northwell Health’s Sandra Atlas Bass Heart Hospital in Manhasset, N.Y.
Epstein said many factors are effective in managing A-fib, including “weight loss [if needed], smoking cessation, treatment of sleep apnea and exercise, often along with medication or ablation.” Sleep apnea – or pauses in breathing during sleep – can trigger A-fib episodes, he noted. When a person does all of these things, the odds that A-fib treatment is successful go way up, Epstein said.
Still, he cautioned that exercise is helpful – until it’s not. Too much intense exercise can increase the risk for A-fib, he added. Epstein’s advice? “Moderation is always the key.” Aim for 3.5 hours a week of cardiovascular and strength training exercise. And “if you have any underlying condition, it’s important to check in with your doctor first.”
More information
Learn more about how to treat and prevent A-fib at the American Heart Association.
14 H&C HEART & VASCULAR HEALTH
Our specialty is superior heart care.

Our specialty is you.
At St. Luke’s Heart and Vascular Institute, you’ll find a full range of state-of-the-art procedures, treatments and services to keep your heart strong and healthy. Whether you’re dealing with a history of heart disease, need follow-up care, or are simply seeking a second opinion, our diagnostic tools and surgical expertise are second to none.
Compassionate care
Strong relationships that help you navigate every step of your health and wellness journey.
Nationally recognized America’s 50 Best Hospitals for Cardiac Surgery™ by Healthgrades® 5 years in a row.
Best technology
In alliance with Cleveland Clinic’s Heart, Vascular & Thoracic Institute.
Easy access
Convenient locations plus same-day second opinions.
appointment at StLukesCare.com/Heart
Schedule your
Shingles Increases Odds of Stroke and Heart Attack
People who’ve had a bout of shingles may face a heightened risk of heart attack or stroke in later years, a new, large study suggests. Anyone who ever had chickenpox can develop shingles — a painful rash that is caused by a reactivation of the virus that causes chickenpox. About one-third of Americans will develop shingles in their lifetime, according to the U.S. Centers for Disease Control and Prevention.
The new study, of over 200,000 U.S. adults, found that those who’d suffered a bout of shingles were up to 38% more likely to suffer a stroke in the next 12 years, versus those who’d remained shingles-free. Meanwhile, their risk of heart disease, which includes heart attack, was up to 25% higher.
Long-term risk
The findings, published recently in the Journal of the American Heart Association, do not prove that shingles directly raises the risk of cardiovascular trouble. But it is biologically plausible, according to the researchers: The reactivated virus can get into the blood vessels, causing inflammation, and that could contribute to cardiovascular “events” like heart attack and stroke.
Some past studies have found that cardiovascular risks can rise after shingles, but they have looked at the short term. It hasn’t been clear how long that risk persists, said Dr. Sharon Curhan, the lead researcher on the new study.
“Our findings demonstrate that shingles is associated with a significantly higher long-term risk of a major cardiovascular event, and the elevated risk may persist for 12 years or more after having shingles,” said Curhan, of Brigham and Women’s Hospital, in Boston.
That’s an important finding, said Dr. Elisabeth Cohen, an ophthalmologist and professor at NYU Grossman School of Medicine, in New York City. “What they’re showing is the short-term risk doesn’t just go away,” said Cohen, who studies shingles-related eye disease.
Risks with shingles
While shingles is very common, it is not taken as seriously as it should be, according to Cohen. It all starts with the chickenpox virus, called varicella zoster. Once a person contracts that virus — as

neuralgia (PHN), nerve pain that can last for months to years after the skin rash recedes.
Shingles vaccine reduces risks
Through much of the study period, there was no shingles vaccine. The good news is there is now a highly effective one available, both doctors said. “Shingles vaccination could provide a valuable opportunity to reduce the burden of shingles, and also possibly reduce the risk of cardiovascular complications,” Curhan said.
The CDC recommends that adults age 50 and older get two doses of the shingles vaccine, called Shingrix. It’s also recommended for people age 19 and up who have weakened immune systems due to disease or medical treatments.
The vaccine is over 90% effective at preventing shingles and PHN in healthy adults, with immunity remaining strong for at least seven years, the CDC says. It’s somewhat less effective for people with weakened immunity.
nearly every American born before 1980 has — it remains dormant in the body, hiding out in the nerves.
Generally, the immune system keeps the virus in check. But when a person’s immune function weakens — due to age, illness or medications, for instance — the varicella zoster virus can reactivate, causing shingles. Typically, shingles causes a painful skin rash consisting of fluid-filled blisters, and usually clears up in a few weeks, according to the CDC.
In some cases, shingles affects the area around the eye — a condition called herpes zoster ophthalmicus — which can lead to serious problems like ulcers on the cornea and lasting vision loss. Meanwhile, between 10% and 18% of people with shingles develop postherpetic
The latest findings are based on over 200,000 U.S. health professionals who were followed for up to 16 years. During that time, just over 3,600 had a stroke, while 8,620 developed heart disease. Overall, people with a history of shingles were up to 38% more likely to suffer a stroke, with the risk being greatest five to eight years post-shingles. Similarly, their risk of heart disease was up to 25% higher, peaking at nine to 12 years after their shingles episode.
Those were the risks after the researchers took many other factors into account — including age, chronic health conditions, weight, exercise habits and smoking.
Anyone unlucky enough to have had shingles can, unfortunately, get it again, Cohen pointed out. So those people should be vaccinated when eligible, too.
“Most of us who’ve had shingles — and I’m one of them — never want to get it again,” Cohen said.
More information
The U.S. Centers for Disease Control and Prevention has more on shingles.
16 H&C
Difficult Care Choices: Helping Families Navigate
If you or someone you know are choosing care options for a loved one, you know how bewildering and time-consuming these decisions can be: Do you need help navigating the healthcare system? Are you in family conflict over a loved one’s health care? Need an advocate to review options for in-home care, benefits, independent, assisted or nursing home care? What are costs and how to pay for it?
Care Choice Care Management offers a holistic, client-centered approach to caring for older adults, those with disabilities or

mental/behavioral health needs. We put safety and security first while improving quality of life and reducing family stress. We provide planning, problem-solving, education, advocacy and family caregiver coaching. Care Choice is one of the leading practices of its kind in the Midwest.
Our Care Managers assist in actively considering, evaluating and monitoring care and living options, assisting with medical needs, both complex and routine. Our wide network of specialists in aging, special needs and health care help

coordinate the best care for individuals and loved ones.
A Care Plan is prepared through a comprehensive assessment with the individual and family. Local, cost-effective resources and solutions are identified and engaged as needed. The plan is modified as circumstances and needs change, to continue to meet the goals of the individual and family.
Let us help you or a loved one navigate the healthcare system.
Leg Cramps and Pain? It Could Be PAD
Pain or cramping in your legs during physical activity may be an early sign of a condition called peripheral artery disease (PAD) – and you should get checked out by your doctor, an expert says. PAD occurs when plaque develops in the arteries of the extremities and restricts blood flow to the legs, and sometimes the arms. The condition is more common in older people and affects up to 10% of those in their 60s and 70s.

PAD causes no symptoms in its earliest stages. The first and most common symptom people notice is repeated pain, cramping or heaviness in one or both legs during walking or exercise. These symptoms occur because muscles can’t get enough oxygen and nutrients.
As PAD advances, symptoms typically become more severe, and can include wounds or ulcers on the feet that won’t
heal, or continuous pain or numbness. In the most severe cases, PAD can lead to amputation, according to Dr. Matthew Cindric, a vascular surgeon with Penn State Health.
“Vascular problems tend to escalate rapidly without prompt diagnosis and intervention, particularly in patients who have wounds on the feet that won’t heal,” Cindric said in a Penn State Health news release. “The earlier you notice the signs and get evaluated, the sooner we can get you on a path toward healing.”
If you notice any signs of PAD, talk with your doctor, Cindric said. Treatments can include diet changes, exercise, medications or procedures to open blocked arteries.
Genetics play a role in PAD, but the other 4 of the 5 top risk factors are controllable: smoking, high blood pressure, high blood cholesterol, and high blood sugar or diabetes. “Smoking is far and away the
For a confidential, no obligation discussion about needs for you or a loved one, call or email today.
636-288-1764
info@carechoicestl.com
leader,” Cindric said. “PAD is far more prevalent in smokers than nonsmokers.” He offered the following advice for people with PAD.
“Start with smoking cessation, get into a structured exercise habit, and work with your [doctor] to manage these risk factors,” Cindric said. “Even if you ultimately require a surgical intervention, long-term results are strongly dependent on how well these other factors are managed.”
There’s more on peripheral artery disease (PAD) at the American Heart Association.
17 H&C
FEATURED SERVICE
Maria Miskovic MSW, LCSW, C-ASWCM
Heart Attack Deaths Fell for Americans Over the Past 20 Years
The United States saw a significant decline in the overall rate of heart attack-related deaths over the past 20 years, and the gap in the rate of heart attack deaths between white people and Black people narrowed by nearly half.
Significant improvement
“It’s good news,” said study lead author Dr. Muchi Ditah Chobufo, a cardiology fellow at West Virginia University’s School of Medicine.
“People should know that even if we’re not there yet, we’re making progress in the right direction. I think the reasons are multifactorial, spanning all the way from health-promoting and prevention activities through treatment during and after a heart attack,” he said in a news release from the American College of Cardiology. For the study, researchers analyzed data from the U.S. Centers for Disease Control and Prevention from 1999 to 2020. Age-adjusted rates of heart attack fell by an average of over 4% per year across all racial groups over the two decades.
In 1999, there were about 87 deaths from heart attack per 100,000 people. By 2020, there were fewer than half that - 38 deaths per 100,000 people.
Reasons for the decline
It’s difficult to determine whether the decline is due to fewer heart attacks or better survival rates because of new diagnostic strategies and treatment options, according to the study authors.
One example of this is that hospitals now frequently test for troponin in the blood when a heart attack is suspected. This can help clinicians diagnose a heart attack sooner, leading to earlier and more sensitive heart attack detection.
The authors also noted that Americans have become more aware of the need to reduce heart risk factors, including quitting smoking and managing cholesterol.
And doctors better understand the signs of a heart attack. Hospitals are equipped with mechanical support devices to assist with heart attack treatment. New medications, such as potent antiplatelets, have become available. These may have improved survival rates and reduced the likelihood of a second heart attack.
Racial disparities
Black Americans still had the highest death rates from heart attack, with 46 deaths per 100,000 in 2020, but that was down dramatically from 104 deaths per 100,000 people in 1999. Death rates from heart attack were lowest among Asians and Pacific Islanders.
The authors also noted the racial disparity differences in these past two decades. The difference in rates of heart attack were about 17 deaths per 100,000 between Black people and white people in 1999. That dropped to eight per 100,000 by 2020.
“That’s a big closure of the gap,” Chobufo said. “I didn’t think the disparities were going to drop this far this fast.”
Researchers noted a slight uptick in 2020, an exception to an overall steady decline in heart attack-related deaths. This is likely related to the COVID-19 pandemic but will require more study.

The study findings were presented at a meeting of the American College of Cardiology and the World Heart Federation, in New Orleans. Findings presented at medical meetings are considered preliminary until published in a peer-reviewed journal.
What This Means for You
Gains in prevention, detection and treatment mean you’re less likely to die of a heart attack today than you were in 1999. About 80% of premature heart attacks and strokes could be prevented with a heart-healthy lifestyle. That means eating a healthy diet, exercising and avoiding tobacco.
More than 800,000 people have a heart attack in the United States each year, according to the CDC. Common signs include shortness of breath and pain or discomfort in the chest, jaw, neck, back, arm or shoulder. Some people may feel weak, lightheaded or faint. Anyone experiencing this should call 911 and get to an emergency room.
More information
The U.S. Centers for Disease Control and Prevention has more on heart attacks.
18 H&C
If Someone Collapsed in Front of You, Could You Perform CPR?

If you answered no, you’re hardly alone. Just over half of Americans know how to perform the emergency procedure. And even fewer know the recommended hands-only technique for bystanders, a Cleveland Clinic survey revealed. Cardiac arrest occurs when the heart suddenly stops beating normally, due to a problem in its electrical system. Usually, the person collapses into unconsciousness and stops breathing normally. It is quickly fatal without emergency medical treatment.
If a bystander immediately starts CPR chest compressions, that can keep blood and oxygen flowing in the victim’s body until paramedics arrive.
“When someone is suffering from cardiac arrest, time is not on their side,” Dr. Steve Nissen, chairman of cardiovascular medicine, said in a clinic news release. “Immediate CPR can be the difference between life and death, doubling or even tripling a person’s chance of survival. It’s a skill that can be easily learned, and we encourage everyone to equip themselves with
this knowledge and not be afraid to use it during an emergency,” Nissen said.
The online poll queried more than 1,000 U.S. adults. Fifty-four percent of respondents said they know how to perform cardiopulmonary resuscitation. However, only one in six knew that hands-only (just chest compressions, no breaths) is the recommended CPR method for bystanders. And only 11 percent knew the correct rate (100 to 120 a minute) for chest compressions.
Confusing heart attack and stroke symptoms
The survey also found that heart attack and stroke symptoms were frequently confused, which could lead to delays in patients receiving proper treatment. Fifty-nine percent falsely believed that sudden numbness or weakness of the face, arm or leg is a symptom of a heart attack. And 39 percent incorrectly thought that slurred speech is a heart attack symptom. These actually are common stroke symptoms.
Most respondents knew that pressure/ squeezing in the chest, shortness of breath, and pain in one or both arms were typical symptoms of a heart attack, but less than half knew that back or jaw pain and nausea/vomiting can also indicate a heart attack.
“Every year about 735,000 Americans experience a heart attack. It’s vital to know the correct signs and symptoms, so people can take the best first steps to help themselves during an emergency. Knowing how to properly respond to a heart attack could save your life or the life of a loved one,” Nissen explained.
Most respondents knew that calling 911 was the first thing to do when someone suffers a heart attack. But only 36 percent knew that the patients should chew an aspirin right away, the survey revealed.
Racial and ethnic disparities
A recent separate study found that when someone collapses in front of witnesses, the chances of receiving potentially lifesaving CPR may partly depend on the color of their skin, a new study suggests. Researchers found that when Black and Hispanic Americans suffer cardiac arrest, they are up to 37% less likely than white people to receive bystander CPR in public places and at home.
The reasons for the disparity are not certain, but there are potential explanations, said senior researcher Dr. Paul Chan, of Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
CPR trainings, he said, are less available in Black and Hispanic communities, and there are other barriers like cost, which may help account for the disparities in responses to at-home cardiac arrests.
But going into the study, the researchers expected that disparities would be lessened when cardiac arrests happened in public. With more people around, the chances that a bystander would be trained in CPR are greater.
Instead, the disparities were greater: Among cardiac arrests that happened at home, Black and Hispanic individuals were 26% less likely than white people to receive CPR. In public settings, that gap grew to 37%.
For CPR training or certification, visit www.redcross.org.
19 H&C
Marijuana, Meth, Cocaine Use Can Help Trigger Dangerous A-fib U
sing marijuana increases the risk of developing the heart rhythm disorder atrial fibrillation (a-fib), a new study suggests. Users are at greater risk
It’s been known that drugs such as methamphetamine, cocaine and opiates can directly affect the heart and cause abnormal rhythms like a-fib, but weed can increase the risk by 35%, researchers found.
“There is a common perception that cannabis may be healthy because it’s ’natural,’” said lead researcher Dr. Gregory Marcus, a professor of medicine at the University of California, San Francisco. “But as laws become more lenient in allowing use of these substances, it’s important to recognize adverse consequences that may substantially impact the lives of users.”
This study doesn’t prove drug use causes a-fib, only that users seem to be at greater risk. “These data are sufficiently compelling to suggest that cannabis users suffering from atrial fibrillation should at least experiment with cessation to see if it indeed has a meaningful effect on their particular arrhythmia,” Marcus said. “Once one has had an episode of atrial fibrillation, I find that patients are often especially eager to identify anything they can do to avoid subsequent episodes.”

Dangers of A-fib
A-fib reduces quality of life and increases the risk of stroke, heart failure, kidney disease, heart attack and dementia, he said.
“We used to think that a diagnosis of atrial fibrillation was just bad luck, but we now recognize this common and sometimes devastating disease can actually be prevented, largely with lifestyle interventions such as reducing alcohol consump-
tion or enhancing physical fitness,” Marcus said. “Although various treatments are available, avoiding the disease in the first place is always better.”
Methamphetamine, cocaine, opioids and cannabis use were each associated with a heightened risk for a-fib in the study, even after adjusting for multiple established risk factors for the disease.
Methamphetamine increased a-fib risk by 86%, researchers found. For cocaine, the risk rose 61%, and for opiates, 74%. For the study, Marcus and his colleagues collected data on more than 23 million people treated in California emergency rooms from 2005 through 2015.
Of 1 million patients who had no preexisting a-fib but developed it later, nearly 133,000 had used marijuana. Nearly 99,000 had used methamphetamines; nearly 49,000 had used cocaine, and 10,000 had used opiates.
How marijuana increases a-fib risk is unknown, Marcus said. Inhalation of combustible products is known to trigger an inflammatory response, and acute inflammation heightens a-fib risk, Marcus said. In addition, blood from the lungs flows directly to where a-fib begins – the pulmonary veins and left atrium of the heart. As such, lung irritants such as pot smoke could aggravate areas of the
heart that are particularly vulnerable to arrhythmia.
Links between nervous system and heart
All of the drugs studied can have dramatic effects on the link between the nervous system and the heart, Marcus noted. “Rapid fluctuations occur with the use of these substances and can also trigger atrial fibrillation,” he said.
A-fib is an abnormal pumping rhythm caused by electrical disturbances in the heart’s upper chambers, the atria. In severe cases, clots can form in the atria and then break off into the bloodstream, causing strokes. Strokes related to a-fib claim more than 150,000 Americans a year. In addition, cocaine and meth can lead to sudden cardiac death from disruptions in the electrical signaling and pumping in the ventricles, the heart’s lower chambers. Researchers said there is no way, however, that pot causes these life-threatening arrhythmias.
Know thyself
Dr. Laurence Epstein, system director of electrophysiology at Sandra Atlas Bass Heart Hospital in Manhasset, N.Y., said many factors can trigger a-fib. Therefore, it’s not easy to predict which will trigger an episode.
“I don’t think it’s like, oh my God, nobody should ever smoke weed because they’re going to develop a-fib,” said Epstein, who wasn’t part of the study. “Everybody’s different. I have patients I treat for atrial fibrillation, and we talk about triggers, and everybody’s different.”
“My recommendation to patients is know thyself,” Epstein said. “Moderation is the key. If you find every time you get high, you start having palpitations, maybe that’s not for you. If you’re not having issues with it, then I’m not sure that puts you at increased risk.”
With the other drugs discussed in the study, the risk is known, Epstein said. “It’s not only the risk of a-fib, but the risk of other bad things, which can give you an acute heart attack or cardiac arrest,” he concluded.
The findings were published in the European Heart Journal.
20 H&C
Exercise Is No Threat to People with Inherited Form of Enlarged Heart
People with the rare heart disorder hypertrophic cardiomyopathy (HCM) can safely engage in vigorous exercise, according to new research.
HCM is an inherited disorder that affects about one in 500 people worldwide. HCM makes it harder for the heart to pump blood because the thickened lower chambers of the heart are too stiff. Some patients may experience shortness of breath, chest pain, fatigue and a life-threatening irregular heartbeat, known as arrhythmia. Rarely, this causes sudden death.
Yet the U.S. National Institutes of Health-funded study found that those who exercised vigorously are no more
likely to die or experience severe cardiac events than those who exercised moderately or not at all.
“Based on these data, we’re learning that we don’t need to universally restrict HCM patients from participating in vigorous exercise,” said study co-author Dr. Rachel Lampert, a professor of medicine at Yale School of Medicine, in New Haven, Conn.
The researchers recruited 1,660 people from ages 8 to 60 with HCM or who carried the gene for it from the United States, United Kingdom, Canada, Australia and New Zealand. About 15% reported they were sedentary, another 43% did moderate exercise, and about 42% said they exercised vigorously.
The study followed the groups for about three years, looking for sudden deaths, resuscitated sudden cardiac arrests, appro-

priate implantable cardioverter-defibrillator (ICD) shocks, and something called arrhythmic syncope, which can include fainting or passing out.
The researchers found that about 1.5% of participants a year who reported exercising vigorously died or had severe cardiac events. This was the same percentage as those who exercised moderately or described themselves as sedentary.
“This finding is significant and provides a measure of reassurance that exercise may be safe for persons with HCM,” said Dr. Patrice Desvigne-Nickens, a medical officer in the U.S. National Heart, Lung and Blood Institute’s division of cardiovascular sciences.
“However, individuals with the condition should not be exercising until they’ve first had an evaluation by a provider with expertise in HCM about their overall risk of sudden cardiac death. It is important to know that all patients with HCM could potentially be at risk for sudden death,” she added.

The study findings were published online in JAMA Cardiology.
Regardless of your health, you can save your monthly premium expense and still have protection for your savings with a Medicare Advantage plan. And you probably won’t have to change any doctors. Plus, the plan will include valuable benefits you don’t get with your Medicare Supplement and Part D Prescription plan.
I am licensed and certified to present all major Medicare health plan options available in our area. Let me cut through the clutter of commercial messages to find your best solution.
I can help you:
n Save money on your health plan premium and benefits
n Find a plan that includes your doctors and covers your prescriptions
n Find a plan that protects your retirement assets
n Spouse needs a plan? I offer Affordable Care Act and Short Term Medical options too.

am a career health insurance executive. For over 10 years as an independent broker, I have been helping my clients save on insurance and health care costs. My services to you are completely free. I am compensated by the insurance carrier based on your plan enrollment. My impartial no obligation consultation will be at a time and place convenient to you. Call me directly at 314-866-8667 Contact me by email at TA@Thor-Anderson.com Please visit: Thor-Anderson.com
Thor Anderson I
Are you paying too much for your Medicare Supplement Insurance? It could be time to save with Medicare Advantage We do not offer every plan available in your area. Any information we provide is limited to plans we do offer in your area. Please contact Medicare. Gov or 1-800-MEDICARE to get information on all of your options.
Deadly Form of High Cholesterol Can Catch Black Americans by Surprise
Chad Gradney underwent quadruple bypass openheart surgery at age 27, and afterward spent eight fruitless years battling extremely high cholesterol levels.
Then in 2012 he found himself back in an emergency room, again suffering from chest pain. “That’s when I found out three of the four bypasses basically had failed again,” recalls Gradney, now 44 and living in Baton Rouge, La.
Gradney suffers from familial hypercholesterolemia (FH), a common genetic condition that impairs the way the body recycles “bad” LDL cholesterol. People with FH essentially are born with high cholesterol levels that only increase as they grow older. About one in every 250 people inherits the condition, according to
the U.S. Centers for Disease Control and Prevention.
But Gradney also is Black, and FH tends to be dramatically underdiagnosed and untreated in Black Americans compared to whites, experts say. Black people are diagnosed with FH at an older age than any other racial or ethnic group in America, according to the nonprofit Family Heart Foundation.
Research also has shown that Black Americans with FH are less likely to have been prescribed cholesterol-lowering medications, even though normal lifestyle modifications aren’t enough to prevent heart disease in someone with the genetic disorder.

“It’s most important to recognize that people with FH are at risk not just because they have an unhealthy lifestyle
or diet,” said Dr. Keith Ferdinand, chair of preventive cardiology at Tulane University School of Medicine in New Orleans. “Many of these patients will need not only statins but three to five medications to lower cholesterol.”
No one checked for FH
Gradney says no one bothered to check him for FH after his first heart emergency, even though nothing he did afterward seemed to lower his abnormally high cholesterol.
“The doctor wouldn’t blame it on me directly, but it was always something I wasn’t doing,” Gradney said. “My wife was a registered dietitian, so I felt like I had the eating-healthy aspect down pat. I was taking my medications. I was being active and exercising. But it was never enough.”
People with FH have 20 times the risk of developing heart disease if they are not treated, the American Heart Association says.
Men with FH develop heart disease 10 to 20 years earlier than expected, and women 20 to 30 years sooner, according to the AHA. Half of men with untreated FH will have a heart attack or angina before they turn 50.
“Unlike patients who develop high cholesterol later in life, these patients have extremely high cholesterol levels from birth and during childhood,” said Dr. Anandita Kulkarni, a preventive cardiologist in Plano, Texas. “It’s not only how high the cholesterol is, but the duration of time for which the cholesterol is elevated that impacts their risk for heart disease.”
Gradney lost his father to a sudden heart attack one morning in 2004. Five months later, he suffered chest pains that made him fear he was having a heart attack himself. “I woke up one morning and I just felt like my heart was going to explode, you know?” said Gradney, who underwent open heart surgery in 2005.
Eight years later, after learning he was in serious danger again, Gradney decided to take matters into his own hands. Through an uncle, Gradney contacted a cardiol-
22 H&C
ogist at Johns Hopkins who agreed to see him. After three days of testing, the doctor diagnosed him with FH.
“Once that was diagnosed, just like that all the dominoes fell into place,” Gradney said. “Everybody knew what to do, how to treat it. I was put on aggressive prescription medications. Six months later, my levels basically were normal, probably for the first time in my life.”
Research has shown that Gradney’s struggle is not unusual. Black people are slightly more likely than whites to have FH, with a prevalence of 0.47% compared to 0.4%, according to a 2016 study in the medical journal Circulation.
Fewer Black patients get standard treatment
But only 61% of Black people with FH treated at special cholesterol clinics in the United States are prescribed cholesterol-lowering drugs, compared with 73% of whites, according to a 2021 study published in the Journal of the American Heart Association.
Black patients also tend to have other problems left untreated that add to their
heart risk, compared to white people, the study found. These include high blood pressure (82% versus 50%), diabetes (39% vs. 15%) and smoking (16% vs. 8%).
Structural racism and racial discrimination are the most likely causes of these disparities, Kulkarni said. Black Americans have more limited access to cholesterol screenings and medications, Kulkarni and Ferdinand said. They also are less aware of the risk posed by FH.
“Furthermore, and understandably so, [structural racism] has eroded trust towards the health care system among Black individuals and communities,” Kulkarni said. “Taken together, this has led to disparities that impact not only the treatment of hypercholesterolemia, but moreover, the delivery and adoption of high-quality medical care.”
The experts recommend that Black people take proactive steps to protect their heart health, just as Gradney ultimately did.
“Every adult should have his or her cholesterol checked. Know your cholesterol,” Ferdinand said. “And if you have a family history of people having heart attacks, strokes, especially early on in their 50s
and early 60s, then it’s not enough to just say that heart disease runs in your family. You should receive a specific diagnosis.”
This worked for Gradney. He hasn’t visited an ER or spent another night in a hospital since receiving his diagnosis in 2012.
“My numbers are amazing. My last blood work, my total cholesterol was under 71, so that was astounding,” Gradney said.
“Be mindful. Check into it. Take advantage of the resources that are available out there,” Gradney said. “Don’t just accept that high cholesterol runs in the family. Advocate for yourself.”
More information
The Family Heart Foundation has more about Black Americans and heart risk.
SOURCES: Keith Ferdinand, MD, chair, preventive cardiology, Tulane University School of Medicine in New Orleans; Anandita Kulkarni, MD, preventive cardiologist, Baylor Scott & White The Heart Hospital–Plano, Texas; Chad Gradney, Baton Rouge, La.
A Painless, Lasting Treatment for Hemorrhoids: Infrared
Almost everyone suffers from hemorrhoids at some time in their lives. Hemorrhoids are normal “cushions” of tissue filled with blood vessels at the end of the rectum. If enlarged, they can cause unpleasant symptoms. If left untreated, surgery may be required, which can be painful and require days to weeks of recovery.
Topical medications can relieve itching and shrink mild hemorrhoids. But for enlarged or bleeding hemorrhoids, options for longer-term relief have been limited to sclerotherapy, involving injections
similar to those for varicose veins, rubber band ligation, stapling and surgery. Each can have varying results, days of discomfort and possibly complications, some of which are severe.
Our practice, Midwest Hemorrhoid Treatment Center, offers another option, an outpatient procedure called infrared coagulation (IRC). It is a minimally invasive, non-surgical procedure that many studies have shown to be the optimal non-operative treatment of choice. It is fast, effective, well tolerated and has fewer complications than other

options. Dr. Betsy Clemens, MD has performed almost 60,000 IRC procedures with very high levels of patient satisfaction.
The IRC treatment focuses infrared light on hemorrhoidal tissues. This coagulates blood vessels, causing the hemorrhoid to shrink and retract. The IRC procedure does not require anesthesia or special preparation. Patients may feel a slight warm sensation, but it usually is painless, and most patients return to work the same day. IRC received FDA clearance in 1984 and is covered by most insurance plans.

FEATURED PRACTICE
Coagulation 2821 N. Ballas Rd. Suite 205 Town & Country MO 63131 For a consultation, call 314-991-9888 To learn more about IRC and our clinic: www.mwhtc-stl.com
MD
Betsy Clemens,
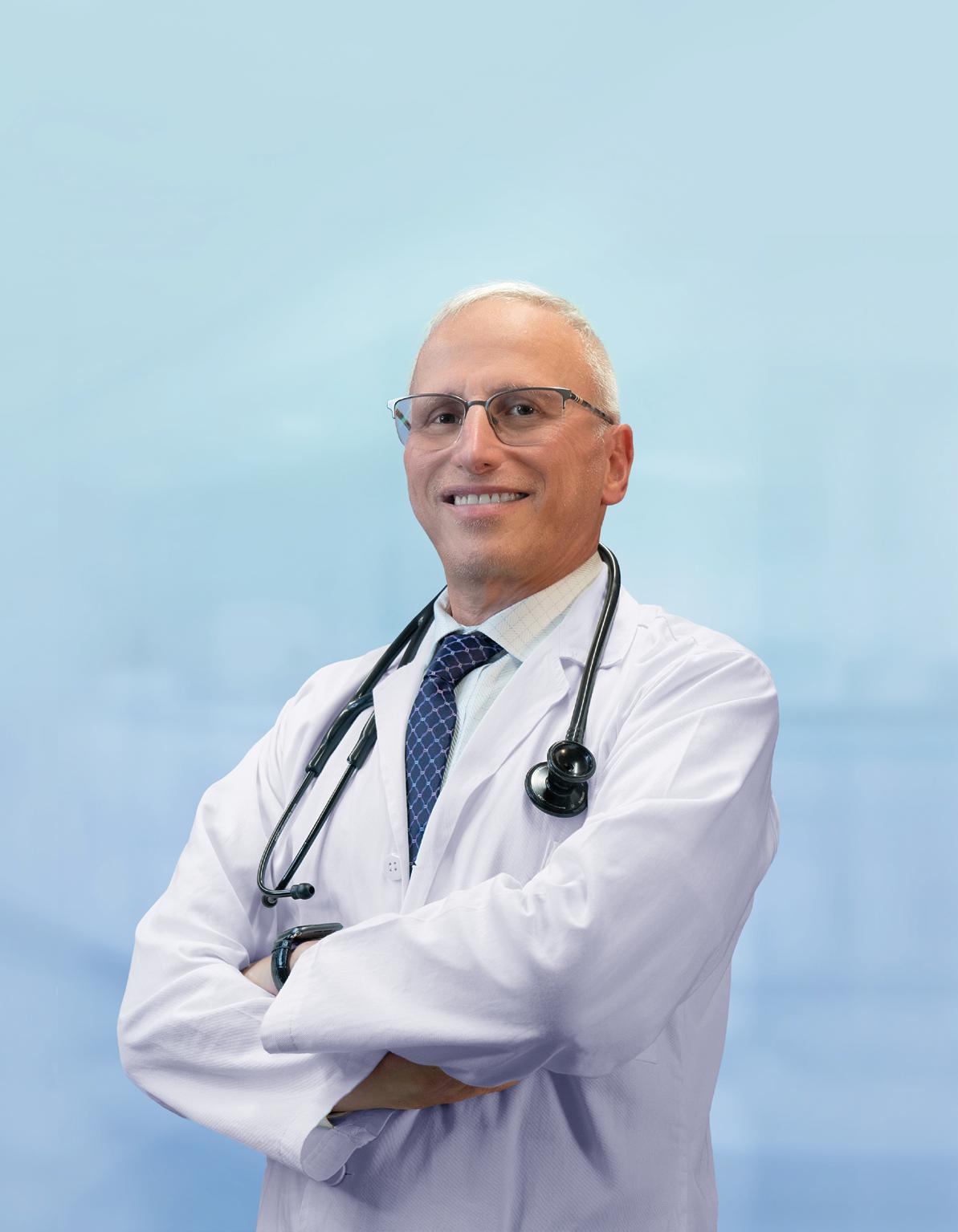
When the Doctor Became Critically Ill
By Todd Abrams
In October 1999, Dr. Harvey Serota was 42 years old, in a successful four doctor practice in interventional cardiology. It was his turn on call that weekend, and his wife Pearl was away visiting friends in New York. On Friday he started feeling achy and had a fever. On Saturday he went to work at Christian Hospital as usual, did an emergency surgery on a heart attack patient, then started feeling sweaty, still had a fever and now chest pains. He took Vioxx to knock the fever down.
Early Sunday morning he did hospital rounds but started feeling sicker and was having trouble breathing. He was in the basement of the hospital when he knew he had to immediately make a decision – to get an X ray or go to the Emergency Room. He walked into the ER through the doctors’ entrance, where all the doctors knew him, and they quickly determined that he was too sick for triage and was sent immediately to the Trauma Room. With his chest pains they knew he had pneumonia even before the X-rays came back.
Acute respiratory distress syndrome
Dr. Serota called his partner to finish his rounds for him, was put in a private room on oxygen and antibiotics and expected to go home in a few days. But it was soon determined that what had started out as pneumonia in one lobe of his lung had become acute respiratory distress syndrome, a serious lung condition in which blood vessels in the lungs become leaky and have trouble oxygenating. He was given more oxygen, but his blood oxygen level kept dropping.
Dr. Josh Glaser, a general surgeon friend, visited him in his room, told him that he didn’t look good and put him in the Intensive Care Unit. When attendants in the ICU asked for the name of Dr. Serota’s patient, Dr. Glaser said, “It’s Dr. Serota himself.”

Two or three days of oxygen by mask was not working; his blood oxygen levels were still too low. Dr. Serota asked to see his X-rays, which showed his lungs as solid white, meaning that the infection and fluid had spread everywhere. He called his family and agreed to be put on a ventilator.
When oxygen levels are that low, oxygen through a mask and sedation are not enough. On a ventilator you’re knocked out and totally immobile so that muscles don’t consume oxygen that is needed by major organs to keep the patient alive. His wife, Pearl, a psychiatrist, quickly came back from New York and stayed with him in his room for the next three weeks. Another friend from the hospital, Ahmed Jafri MD, a neurologist, gave instructions for keeping his limbs moving and turning him frequently to keep his joints from freezing up, so that when he recovered, he would have normal movement.
Prayer and prone ventilation
During Dr. Serota’s 35 days on the ventilator, the hospital chaplain arranged for an interdenominational prayer service
in a conference room. Some close friends showed up with an Orthodox rabbi, who held a service in which Dr. Serota’s Hebrew name was changed, a tradition based on the ancient belief that a person’s name is the spiritual conduit through which blessings are received. If death had been decreed for one individual, by changing the name, he or she becomes someone else, not the one decreed for death. His name was changed to Raphael, which means “God has healed.”
During this time, Steven Hadzima MD, Vice President of Medical Affairs at the hospital, brought in Dr. George Matuschak, an expert in acute respiratory distress syndrome, who also was a professor at St. Louis University School of Medicine. He agreed that everything was being done correctly by Dr. Myron Jacobs’s team but wanted to try something that was new at the time called prone ventilation, in which the patient is placed face down to improve oxygenation.
After 35 days on the ventilator, Dr. Serota’s condition began to improve, he was put on his back and sedation was reduced. While sedated he managed to chew through the ventilator tube, separating the cap that keeps it securely directing oxygen into the lungs. He had to have an
24 H&C COVER STORY
emergency extubation to take the tube out. His doctors didn’t know if he would be able to breathe on his own or if the next step would be a tracheotomy, a surgical procedure in which an incision is made in the front of the neck and a breathing tube is placed into the trachea, or windpipe. He was able to breathe on his own and didn’t require the normal weaning process from the ventilator, although he was having hallucinations and seeing double. After having been essentially paralyzed for that long on the ventilator, Dr. Serota’s muscles were very weak – he couldn’t roll over, brush his teeth or even lift a towel. His resting heart rate was 110 beats per minute, about twice normal. He couldn’t do even the simplest things; his handwriting went back to grade school level. But he started long-haul physical therapy with a passion: instead of the recommended three hours a week, he worked at it eight hours a day.
His doctors had told him that his recovery would take six months, but he said he had a family and patients to take care of. His recovery took six weeks of painfully working with a trainer every day.
How the experience affected him
On reflection, Dr. Serota believes that the entire ordeal made him much more sensitive to what patients go through. Many doctors have no idea how painful, both physically and mentally, treatments are. For instance, he learned how much shots of the blood thinner Heparin really hurt. Instead of giving the customary three shots of Heparin he now gives one shot of Lovenox or one pill of Xarelto.
The experience reinforced for him the importance of a doctor who practices with deep experience in the basics of his or her specialty, but who is also up to date with new techniques like the prone ventilation that was used for him, and which became a very important procedure during the Covid epidemic.
Dr. Serota has even changed how he talks to patients. Once during his recovery, he was ambling about on a walker in the hospital when his doctor came up to him and said, “Harvey, you will probably be OK.” He said he collapsed when he heard the word “probably” – it made him fall to his knees. Patients need to go into surgery and recovery with a positive attitude, so he now errs on the optimistic side. He would rather give patients a positive statement
and be wrong than deny them the hope that can help in their healing. And having been through so much himself, he is inspired by some people with terrible diseases who still manage to stay positive.
He even has a different perspective on hospital food. Patients always say hospital food tastes bad, but he realized that it is because they are sick, or the bad taste can be a side effect of medications. Pearl brought him dinner from Tony’s one night while he was in the hospital, and he says even that didn’t taste good.
Dr. Serota also gained a much greater appreciation for the need to exercise regularly, to be in good physical shape in case something happens to you. Patients who have good muscle strength do much better in recovery than those who don’t. During the Covid epidemic it became readily apparent which patients were more likely to survive – those in better physical shape when they became ill. And he understands much better now how important physical therapists are – he says they are among the most important people working in the hospital. Walking every day and other forms of rehab are critical.
From a personal relationship standpoint, the experience also gave him a richer sense of enjoying relationships of those who are important to him, and he accelerated the timetable for doctor employees in his practice to become partners. He also became much closer to family and friends, balancing work with the rest of life. He learned that you have to find time for yourself and for doing those things you enjoy.
When I asked Dr. Serota if he had any idea how he became vulnerable to the virus that caused his critical illness, he said that back in those days he did not take care of himself; he didn’t exercise regularly, and would rush around outside even in chilly weather, sometimes exhausted and dressed just in scrubs. He reflected that he hadn’t listened to his mother, who always told him to dress warmly.
Just for the record, on the day I interviewed him we were indoors in late April, and he showed me the skier’s long underwear he now wears under his clothes.
Dr. Harvey Serota, MD, FACC, FSCAI, is a board-certified cardiologist in internal medicine, interventional cardiology, and cardiovascular disease at St. Louis Heart & Vascular.
Above: Dr. Serota with his daughter Danielle.

Middle: Dr. Serota with his father Ely Serota and daughter Danielle.

Below: Dr. Serota with his daughter Danielle and son Joshua

Depression Ups Odds for a Stroke, and a Stroke Ups Odds for Depression
In yet another example of the mindbody connection, people with depression symptoms may face an increased risk of having a stroke, as well as a worse recovery afterwards.
Depression before a stroke
A new international study found that about 18% of those who had a stroke had symptoms of depression, compared to 14% of those who did not have a stroke.
After adjusting for other contributing factors, researchers determined that people with symptoms of depression before stroke had an overall 46% increased risk of stroke compared to those with no symptoms of depression. As the symptoms increased, so did the higher risk of stroke.
“Depression affects people around the world and can have a wide range of impacts across a person’s life,” said study author Dr. Robert Murphy, of the University of Galway in Ireland.
“Our study provides a broad picture of depression and its link to risk of stroke by looking at a number of factors including participants’ symptoms, life choices and antidepressant use,” Murphy said in a journal news release. “Our results show depressive symptoms were linked to increased stroke risk and the risk was similar across different age groups and around the world.”
The researchers used data from more than 26,000 adults in the INTERSTROKE study, which included 32 countries across Europe, Asia, North and South America, the Middle East and Africa. More than 13,000 of the participants had a stroke. They were matched with more than 13,000 people who had not had a
stroke but were similar in their age, sex, racial or ethnic identity.
Information was collected about depression symptoms in the year prior to the study, including whether participants had felt sad, blue or depressed for two or more consecutive weeks in the previous 12 months.
results show that symptoms of depression can have an impact on mental health, but also increase the risk of stroke. Physicians should be looking for these symptoms of depression and can use this information to help guide health initiatives focused on stroke prevention.”
Depression after a stroke
Depression is also common after a stroke, and most stroke patients who need mental health care for it aren’t getting the help they need, separate new research reveals.
Roughly one in three stroke victims have post-stroke depression. But about twothirds of those received no mental health treatment. Patients who were older, male, Black or Hispanic were even less likely to get help, the study found.

“This study shows a very significant number of survivors are not getting the help and support they need after a stroke,” said study author Dr. Linda Williams, a research scientist at the Regenstrief Institute in Indianapolis. “This rate has remained low over more than a decade, despite societal changes in attitudes toward mental health treatment.”
Participants also answered questions at the beginning of the study about cardiovascular risk factors, including high blood pressure and diabetes.
Researchers found that people who reported five or more symptoms of depression had a 54% higher risk of stroke than those with no symptoms. Those who reported three to four symptoms of depression had 58% higher risk and those who reported one or two symptoms of depression had a 35% higher risk.
The people who had depression symptoms weren’t more likely to have severe strokes. They were, however, more likely to have worse outcomes a month after the stroke.
A study limitation is that depression symptoms were assessed only at the start of the study and not over time.
“In this study, we gained deeper insights into how depressive symptoms can contribute to stroke,” Murphy said. “Our
For the study, researchers at Regenstrief, the Indiana University School of Medicine and the University of Michigan analyzed mental health services received by a nationally representative sample of stroke patients and others between 2004 and 2017.
During that time, depression treatment rose among the non-stroke population but held steady among stroke patients.
“Unmet needs for depression after stroke remain significant and are important because they impact stroke survivors’ quality of life and their recovery,” Williams said in an institute news release. She said it’s important to determine barriers to mental health care for stroke survivors, with an emphasis on closing gaps.
The findings from both studies were recently published in the journal Neurology. More information
The American Stroke Association has more on depression and stroke.
26 H&C NEUROLOGY & STROKE

Severe Seizures Are Rising, Especially Among Minorities
Growing numbers of Americans are suffering prolonged, life-threatening seizures known as status epilepticus, and Black people are nearly twice as likely to experience these seizures as white people.
These are the main findings from new research looking at hospitalizations for status epilepticus from 2010 to 2019 across the United States. Status epilepticus refers to a seizure that lasts for more than 5 minutes. Some people may experience convulsions during this state, while others may appear confused or seem like they’re daydreaming. Status epilepticus is an emergency and requires treatment in the hospital.
professor of neurology at Baylor College of Medicine in Houston.
For the study, the researchers reviewed nearly 490,000 hospitalizations for status epilepticus. These rates increased significantly over the study period, especially among minorities.
Disparities in incidence and treatment
What’s more, minorities who experienced status epilepticus were more likely to need advanced treatments, including a breathing tube or feeding tube.
“I was surprised to see that disparities in the incidence of status epilepticus for minorities have unfortunately persisted and even widened from 2010-2019 despite a greater awareness of status epilepticus and seizures, and changes in insurance with increasing coverage over time,” Tantillo said.

Older adults were up to six times more likely to die during hospitalization with status epilepticus and were more likely to require breathing tubes or feeding tubes, compared to younger folks with these seizures, the study found.
Causes and Prevention
Status epilepticus can be a result of uncontrolled epilepsy, a brain bleed, a brain tumor, or a severe underlying illness such as meningitis, she explained.
“For cases of status epilepticus that are potentially preventable, such as in people with epilepsy, improving health literacy and reducing the stigma associated with seizures in the community would help get more patients the treatment they need,” Tantillo said.
Minorities in the studies were less likely to die from status epilepticus. This may be because people with status epilepticus due to low antiseizure medication levels fare better than their counterparts who have other causes for the condition, such as a brain bleed or lack of oxygen to the brain. Expanding access to outpatient care can also help bridge some of these gaps, Tantillo said. In addition, working to diversify the medical workforce in neurology may also improve patient-physician trust and communication, and reduce implicit biases and health inequity over time, Tantillo suggested.
The study wasn’t designed to say why these severe seizures are on the rise, but researchers have their theories. “It may be related to several causes including changing definitions for status epilepticus over time,” said study author Dr. Gabriela Tantillo. (At one time, only seizures lasting longer than 20 minutes were considered status epilepticus.)
Also, there’s “greater recognition of seizure, including non-convulsive seizures, by the medical community and the general public,” said Tantillo, an assistant
The researchers also noted that electroencephalogram (EEG) monitors, which record electrical activity in the brain, were more widely available for people with higher incomes or those treated at urban teaching hospitals.
There are things that will help make care for people with status epilepticus more equitable, Tantillo said. “We need to understand the underlying causes of these seizures as they differ by sociodemographic factors, which requires greater research and investment from government, community groups and philanthropy,” she noted.
“The findings are terrible but not surprising,” said Dr. Daniel Lowenstein. He is a professor and vice chair of neurology at the University of California, San Francisco. “The big picture is that it reveals yet again disparities that exist within the health care system based on race and socioeconomic class.” Such disparities are seen in the diagnosis and treatment of many diseases and conditions, he noted. Treating status epilepticus involves intervening as early as possible with a benzodiazepine and/or other antiseizure medication, said Lowenstein, who was not involved with the new study. How well someone fares is based on the underlying cause since some causes are more treatable than others.
The findings were presented at the American Epilepsy Society annual meeting in Nashville in December of 2022. Findings presented at medical meetings should be considered preliminary until published in a peer-reviewed journal.
What This Means for You
Status epilepticus can be caused by uncontrolled epilepsy, a brain tumor or a severe underlying illness.
28 H&C
Study Hints That a Sleeping Pill Might Help Prevent Alzheimer’s
Taking a particular sleep medication may help stave off Alzheimer’s disease, but it’s too soon to say for sure after a preliminary study.
Researchers at Washington University School of Medicine in St. Louis found that participants who took a sleeping pill called suvorexant before bed had a drop in levels of key Alzheimer’s disease proteins. “This is a small, proof-of-concept study. It would be premature for people who are worried about developing Alzheimer’s to interpret it as a reason to start taking suvorexant every night,” said senior study author Dr. Brendan Lucey, an associate professor of neurology and director of Washington University’s Sleep Medicine Center.
Proteins that cause Alzheimer’s
“We don’t yet know whether long-term use is effective in staving off cognitive decline, and if it is, at what dose and for whom,” he added in a university news release. “Still, these results are very encouraging. This drug is already available and proven safe, and now we have evidence that it affects the levels of proteins that are critical for driving Alzheimer’s disease.”
Suvorexant (Belsomra), a dual orexin receptor antagonist, is one of three in this class of drugs that are already approved by the U.S. Food and Drug Administration for insomnia. Orexin is a natural biomolecule that promotes wakefulness. When it is blocked, people fall asleep, according to the study.
In Alzheimer’s disease, plaques of the protein amyloid beta build up in the brain. Years after amyloid begins accumulating, another brain protein called tau, starts forming tangles that are toxic to neurons. As those tangles become detectable, people with Alzheimer’s disease start
experiencing memory loss.
In past research, Lucey and his colleagues have linked poor sleep to higher levels of both amyloid and tau in the brain. What they don’t know is whether good sleep would reduce those levels, and with that halt or reverse progress of Alzheimer’s disease. Mouse studies with orexin inhibitors have been promising. The study
For this study, researchers recruited 38 people between the ages of 45 and 65 who had no mental impairments. Researchers gave 13 of them a lower dose – 10 milligrams (mg) – of suvorexant. Twelve others received a 20 mg dose, while 13 participants received a placebo.
The doses were each given at 9 p.m. Researchers withdrew a small amount of cerebrospinal fluid from participants via spinal tap every two hours for 36 hours. This began an hour before the sleeping aid or placebo was administered. The purpose was to measure how amyloid and tau levels changed over the next day and a half.
Amyloid levels dropped 10% to 20% in the cerebrospinal fluid of people who had received the high dose of suvorexant compared to those who received a placebo. Levels of a key form of tau known as hyperphosphorylated tau dropped 10% to 15%, researchers found. These differences are considered statistically significant. No significant difference was found between the people who received a low dose of suvorexant and those who received the placebo.
Investigators administered another dose of suvorexant on the second night. Levels of both proteins again dropped in the high-dose group. “If we can lower amyloid every day, we think the accumulation of amyloid plaques in the brain will decrease over time,” Lucey said. “And hyperphosphorylated tau is very important in the development of Alzheimer’s disease, because it’s associated with forming tau tangles that kill neurons. If you can reduce tau phosphorylation, potentially there would be less tangle formation and less neuronal death.”
The findings were published in Annals of Neurology.
Lucey cautioned that the study is preliminary. Ongoing studies aim to assess the longer-term effects of orexin inhibitors in people who are at higher risk of dementia. “Future studies need to have people taking these drugs for months, at least, and measuring the effect on amyloid and tau over time,” Lucey said. “We’re also going to be studying participants who are older and may still be cognitively healthy, but who already have some amyloid plaques in their brains.”
He noted that this study involved healthy middle-aged participants. Results may be different in older participants.
“I’m hopeful that we will eventually develop drugs that take advantage of the link between sleep and Alzheimer’s to prevent cognitive decline,” Lacey said.
“We’re not quite there yet. At this point, the best advice I can give is to get a good night’s sleep if you can, and if you can’t, to see a sleep specialist and get your sleep problems treated.”

29 H&C
Two Healthy Diets May Reduce Brain Plaques Tied to Alzheimer’s Risk
Elderly adults who eat plenty of leafy green vegetables, fish and other healthy fare may take years off their “brain age,” a new study suggests.
Researchers found that seniors with either of two healthy eating patterns – the Mediterranean and MIND diets –showed fewer brain “plaques,” abnormal protein clumps that are a hallmark of Alzheimer’s disease. In fact, people with the highest Mediterranean or MIND scores had brains that were up to 18 years younger than their counterparts with more of a burger-and-fries diet.
Experts said the findings do not prove that spinach and fish will ward off dementia. But they do add to a growing body of evidence linking healthy eating to slower brain aging. Lead researcher Puja Agarwal called the results “exciting,” because they suggest that even a simple dietary change could make a substantial difference.
Based on the findings, older people who eat, say, a cup of leafy greens a day could have a brain that’s four years younger, versus their peers who shun the likes of kale and spinach. The study, published in the journal Neurology, builds on past research into diet and dementia.
Connection of diet with plaques
Both the Mediterranean and MIND diets have already been linked to slower mental decline and a lower risk of Alzheimer’s disease, the researchers said in background notes. Now the new findings connect the diets to fewer objective signs of Alzheimer’s – the plaques that begin to form in the brain years before dementia symptoms appear.
That strengthens the case that the eating patterns are truly associated with lower Alzheimer’s risk, according to Agarwal, an assistant professor at Rush University Medical College in Chicago. “It also gives us a first view into the mechanisms,” she said. That is, less accumulation of brain plaques may be one way the diets protect against Alzheimer’s – though, Agarwal said, it’s not yet clear how they might accomplish that.
The traditional Mediterranean diet –famously linked to lower risks of heart disease and stroke – is generally high in fish, olive oil, vegetables, beans, nuts and fiber-rich grains. The MIND diet is very similar but emphasizes leafy green vegetables and berries over other vegetables and fruit. That’s based on research tying those foods to better brain health.

Both diets, according to the Rush University researchers, are high in plant foods that have various nutrients and chemicals that can ease inflammation in the body and protect cells from damage. Both diets are also notable for what they leave out: red meat, sugar and heavily processed foods.
Learning from brains after death
The new findings are based on autopsied brain tissue from 581 participants in a long-running Rush study on memory and aging. When they entered the study, typically in their early 80s, they gave consent
30 H&C
to donate their brains after death.
Each year, study participants complete detailed dietary questionnaires. Agarwal’s team used that information to give each of the 581 deceased participants a Mediterranean and a MIND diet “score.” The more their eating habits looked like those diets, the higher the scores.
Overall, the researchers found, participants who’d scored highest in Mediterranean-style eating had brains that, based on plaque buildup, were 18 years younger than those of participants with the lowest Mediterranean scores. The differences were similar, though somewhat smaller, when it came to MIND diet scores.
Certain foods stood out, too, Agarwal said. People who ate the leafiest greens – at least seven servings a week – spared themselves about 19 years of brain aging, versus their peers who ate no more than one serving a week.
Of course, people who eat healthfully may have advantages, like a higher income or more education. They may also have fewer chronic medical conditions, or do other things to support their health, like exercising and refraining from smoking. Agarwal’s team accounted for as many of those factors as they could, and healthy eating was still strongly linked to a younger-looking brain.
The findings are “intriguing,” said Heather Snyder, vice president of medical and scientific relations at the Alzheimer’s Association. “This study takes what we know about the link between nutrition and risk for cognitive decline a step further by looking at the specific brain changes that occur in Alzheimer’s disease,” said Snyder, who had no role in the study.
She noted that the Alzheimer’s Association is leading a two-year clinical trial that is testing whether a combination of lifestyle changes can slow cognitive decline in older adults. The MIND diet is part of that combo.
It’s not yet clear what the best lifestyle “recipe” is, according to Snyder. What is clear, she said, is that people should strive for a “heart-healthy diet that incorporates nutrients that our bodies and brains need to be at their best.”
Role of vitamin D
In a separate study, a team of British and Canadian investigators report that vitamin D can lower dementia risk. They spent roughly a decade tracking more than 12,000 older people. None had dementia at the start of the study period. In the end, the team determined that those who had been taking vitamin D supplements during that time appeared to face a 40% lower risk for dementia, compared with those who had never taken the supplements. Even so, Claire Sexton, senior director of scientific programs and outreach at the Alzheimer’s Association, cautioned that much more research is needed to better understand a possible link between vitamin D and dementia risk.
The participants in the Rush study were asked about their eating habits in the past year. It’s not known, Agarwal said, if they’d eaten that way their whole lives, or made changes at some point. Still, she said, “it’s never too late” to revamp your diet for the better.
More information
The Alzheimer’s Association has advice on healthy brain aging.
Americans’ Odds for Parkinson’s May Be Higher Than Thought P
arkinson’s disease is a much bigger problem than previously thought, particularly for aging Americans, a new study finds.
There are about 50% more new cases of the degenerative disorder diagnosed each year in North America than currently estimated, researchers concluded after an extensive data review.
“We used to say 60,000 people a year were getting diagnosed, but really it’s 90,000 people a year are getting diagnosed with Parkinson’s disease,” said co-researcher James Beck, chief scientific officer at the Parkinson’s Foundation.
The results highlight that increasing age is a primary risk factor for Parkinson’s, Beck said. With an aging population, more cases of Parkinson’s are being diagnosed.
The numbers showed that the risk of Parkinson’s dramatically increases with age, with men more likely to develop the disease than women. The data also revealed specific regions of the US in which more cases are diagnosed, which jibes with research linking Parkinson’s to pollution, pesticides and other environmental factors.
Parkinson’s rates are higher in the “Rust Belt” states of the northeastern and Midwestern United States, as well as in the central valley of Southern California, southeastern Texas, central Pennsylvania and Florida, the study showed.
It’s hard to pinpoint one single environmental factor, but there has been research looking into the impact of pesticides and byproducts of industrialization and different chemicals on Parkinson’s risk. There needs to be more research looking into why there are certain geographic areas where there is higher incidence. More than anything, the study provides a new understanding of Parkinson’s toll on American society.
About a million people in the United States have Parkinson’s, compared to 5 million people living with Alzheimer’s disease. “There’s a fivefold difference between the diseases, but it’s closer to a 10-fold difference in how much is being invested in Alzheimer’s versus Parkinson’s. We’re trying to make the case that Parkinson’s should be on a proportional footing as Alzheimer’s,” Beck said. “If we could at least get to parity on a proportional basis for Parkinson’s funding, that would be tremendous.”
The new study was published in the journal npj Parkinson’s Disease.
More information:
Find out more about Parkinson’s at the Parkinson’s Foundation or the American Parkinson Disease Association.
31 H&C
FROM ABBOTT
Essential Tremor and Parkinson’s Disease: How They Differ W
hen someone has trembling hands or involuntary movements in their arms, legs or head, people tend to conclude the shaking is a sign of Parkinson’s disease.
However, the symptoms may be the result of a more common, less severe condition called essential tremor. Essential tremor can be confused with typical Parkinson’s disease symptoms, but the two movement disorders are separate conditions.
Because these diagnoses can get tangled up, it’s helpful to understand their differences.
First, let’s explore the basics of each condition.
Essential Tremor
Essential tremor is the most common type of tremor. It’s a neurological disorder that causes involuntary shaking, most often of the hands and arms. The condition is not life-threatening, though in severe cases it can cause disability.
Tremors start in the hands and arms and can affect the head and voice as well. Usually, it starts as a low-amplitude
tremor, meaning the shaking is mild. The low-amplitude tremors may have a higher frequency, meaning there are many repetitions per second. As the condition progresses, which it may do with age, the tremors themselves may become more severe but with lowered frequency.
Doctors and researchers aren’t sure what causes essential tremor, but it may be inherited. This thought rises from findings that people with a parent who has a genetic mutation for essential tremor are 50 percent more likely to have it as well, according to Mayo Clinic.
Even though essential tremor can happen at any age, it’s most common in people older than 40 years and affects men and women equally.
Parkinson’s Disease
Parkinson’s disease is a neurological disorder that happens when nerve cells in the brain don’t produce enough dopamine. The disease progresses over time, leading to more and more disability. The disease occurs more often in men than women and usually develops in people over 60.
Tremors are one of the most well-known Parkinson’s disease symptoms and one
that sends many people to their doctor for evaluation. Parkinson’s tremors usually start on one side of the body, commonly in the hands, and progress to the other side. The movements tend to be more forceful (high amplitude) with lower frequency. The disease carries many other symptoms that help distinguish it from essential tremor, as well. Tremors may not always be the most prominent symptom, with other symptoms including stiffness in the body, slow movements and trouble with balance.
Recognizing the Difference
Parkinson’s disease is much less common than essential tremor, and it presents itself in markedly different ways. While treatments overlap in some areas, getting the best care requires the right diagnosis. The two conditions have key differences to look for:
n Essential tremor doesn’t cause associated health problems, while Parkinson’s carries other symptoms, such as stooped posture and balance problems.
n Essential tremor may affect the voice box, but Parkinson’s does not.
n Essential tremors are usually felt more when in motion, but Parkinson’s tremors are felt more when at rest.
n Essential tremor symptoms can progressively get worse, but won’t necessarily shorten the patient’s life span. Parkinson’s tends to progress over time and may shorten the patient’s life span as the brain produces less and less levodopa over time. For many people, essential tremor may be mild and may not interfere with daily life. However, any tremor that worsens should be evaluated by a doctor.
Medications, physical therapy, deep brain stimulation and other techniques may be used to manage tremors, depending on how severe they are. Your doctor can also offer tips to cope and ways to avoid triggers like caffeine and stress, so don’t hesitate to seek professional advice if tremors are a part of your life.
For more content like this, visit the newsroom at abbott.com

32 H&C
Is It Parkinson’s? These 10 Signs Could Tell P
arkinson’s disease can be hard for the average person to identify, but 10 warning signs may offer an early clue that you or a loved one may be developing the disease.
The Parkinson’s Foundation suggests being aware of the signs, while knowing that having any one of them doesn’t mean the disease is present.
1. Tremor, such as in a finger, thumb, hand or chin, can suggest Parkinson’s, though it can also be a side effect of stress, injury, medication or a lot of exercise.
2. Parkinson’s can also cause a change in handwriting known as micrographia, where letter sizes become smaller and words more crowded.
3. People with Parkinson’s can also thrash around during sleep, something a spouse may notice.

4. Sense of smell may diminish with foods like bananas, dill pickles or licorice. Of course, viruses, including cold, flu and COVID-19 can also affect sense of smell.
5. Another possible sign of Parkinson’s is stiffness in the body, arms and legs. A person’s arms may no longer swing in a typical fashion or feet may feel like they’re “stuck to the floor.” Some other health conditions, such as arthritis, can also cause stiffness.
6. A change in voice may signal Parkinson’s. It may become softer, breathy or hoarse.
7. Another sign is “facial masking,” in which a person’s face looks serious, depressed or mad but doesn’t match their mood. But some medicines can also cause a person to have a serious look or stare.
8. Constipation or trouble with digestion.
9. Dizziness or fainting.
10. Stooping or hunching when a person is standing are two additional signs of Parkinson’s disease.
If you have more than one of these symptoms, you may want to talk with a doctor about the possibility of Parkinson’s disease. More information
The U.S. National Institute on Aging has more on Parkinson’s disease. The American Parkinson Disease Association Missouri Chapter, located in Chesterfield, offers education programs, a newsletter, exercise classes and support groups for those impacted by Parkinson’s Disease, both in person and virtual. See their ad on this page.
The APDA Missouri Chapter works tirelessly every day to support and empower those in our community who are impacted by Parkinson’s disease (PD). We promote hope and optimism through innovative services, programs, education, and support, while also funding vital research. We are here to help you and your loved ones every step of the way.

33 H&C
16100 Chesterfield Parkway W., Suite 125 | Chesterfield, MO 63017 Email: apdamo@apdaparkinson.org 636.778.3377 Tuesday through Friday – 9:00 am to 4:00 pm EDUCATION PROGRAMS in-person and virtual 29 SUPPORT GROUPS MONTHLY BI-MONTHLY NEWSLETTER + hundreds more on YouTube Channel 192 EXERCISE CLASSES PER MONTH SCAN NOW to visit our website and download our Newly Diagnosed Kit C M Y CM MY CY CMY K
Strength in optimism. Hope in progress.
Only 1 in 7 Cancers Are Caught Through Cancer Screenings
Just 14% of all cancers diagnosed in the United States are detected through routine screening, a new analysis finds – pointing to many missed opportunities to catch cancer early.
“It’s surprising, but true,” said Caroline Pearson, senior vice president of the research institution NORC at the University of Chicago, which conducted the review.
Cancer screening, by definition, refers to tests that can detect tumors before they cause symptoms – giving people the best chance of early treatment and beating the disease. Right now, there are routine screening tests recommended for breast, cervical and colon cancers. Lung cancer screening, meanwhile, is recommended for some smokers and former smokers.
Why cancers are missed in screening
One major reason for the findings is that for most cancers, there are no routine screening tests available. But there are also missed opportunities with the existing ones, according to Pearson.
“For one, screening isn’t perfect,” she said, so there will always be some early cancers that are missed.
In addition, Pearson said, some cancers will develop in the intervals between screening tests. Mammography screening, for example, is typically done every one or two years, while colonoscopy – one of the screening tests for colon cancer – is recommended every 10 years for people at average risk.
But there’s also a third reason, Pearson said: Many Americans do not get the recommended cancer screenings.
“Look at something like colorectal cancer, where we have lots of screening options,” Pearson said.
Besides a traditional colonoscopy, there is “virtual” CT colonoscopy, as well as various stool-based tests. A recent report from the U.S. Centers for Disease Control and Prevention found that 69% of Americans ages 50 to 79 said they were up-to-date with colon cancer screening in 2020.
But that percentage varied widely state to state – going as low as 58% in California –and 22% of Americans in the age range for colon cancer screening said they’d never been screened.
Other screen-detectable cancers have similar room for improvement. The CDC says that in 2019, 69% of U.S. women age 40 and older had a mammogram in the past two years, for example.

Getting those rates up, Pearson said, is the most straightforward way to boost the number of cancers detected by screening.
Better screening tests needed
But there’s also a need for better screening tests, including methods that are more accessible and less burdensome, according to Pearson.
Researchers are, in fact, working on that.
A major goal is to develop a single blood test that can detect multiple cancers, according to Dr. Ned Sharpless, former director of the U.S. National Cancer Institute.
“While not market-ready, this concept is currently in development,” Sharpless said.
“These simple tests could detect evidence of cancer in blood or other bodily fluids so that the disease can be treated very early, before it spreads,” he said.
If such a blood test pans out, Sharpless said, “it could have a tremendous impact on cancer mortality rates.”
The NORC analysis, which is not published in a peer-reviewed journal, used various data sources to estimate the percent of cancers detected by screening in 2017.
Overall, that figure was 14%. In part, that was because so many cancers lack a screening test: 57% of all cancers diagnosed in 2017 were types that have no routine screening method. However, 15% of all cancers diagnosed that year were screenable, but were not detected that way. In those cases, the disease is typically caught because symptoms have developed – which may also mean the cancer is more advanced and tougher to treat.
Cancers detected by type
The percent of cancers detected by screening does vary according to type, the analysis found. Of all breast cancers diagnosed in 2017, 61% were caught by screening. That figure was 52% for cervical cancer, 45% for colon cancer, and just 3% for lung cancer.
That low number, Pearson noted, could be because lung cancer screening is recommended only for certain high-risk people. It’s also newer than screening tests for other cancers, and studies show that few eligible Americans are receiving it at this point.
For the general public, Pearson said, the most important thing is to get the cancer screenings that do exist.
“Talk to your primary care provider and know which screenings are recommended for you,” she said. “Awareness and education can go a long way.”
Not enough cancers are being spotted by screening tests in the United States, but a single blood test that could spot multiple cancers could be a game changer down the road.
More information
Visit the U.S. National Cancer Institute website for more on cancer screening.
34 H&C CANCER PREVENTION & TREATMENT

Just Half of Those with a Positive Stool Test for Colon Cancer Get Follow-Up Colonoscopy
Many people undergo a stool test to screen for colon cancer, but a new study finds too few follow up with a colonoscopy when that test warns of a possible cancer.
Not following up undermines the point of screening, said study-co-author Jeff Mohl, director of research and analytics for the American Medical Group Association, a trade organization.
In this study of almost 33,000 people at average risk for colon cancer, just 56% who had a positive result from a stool test had followed up with a colonoscopy within a year. Poorer people and the COVID-19 pandemic were associated with lower follow-up rates.
“Obviously, that’s a huge problem,” said Mohl. “If you’re trying to estimate how many lives are saved, you’re assuming that everyone gets follow-ups if they have a positive result, and if half of them don’t do that, obviously you’ll only save half as many people.”
The findings were published Jan. 18 in JAMA Network Open and were based on screenings between 2017 and 2020.
“Colorectal cancer is definitely a significant health problem and increasing, particularly in younger patients,” said Dr. William Dahut, chief scientific officer with the American Cancer Society. Rates have been increasing by 1% to 2% a year since the mid-1990s in Americans younger than 50, the cancer society says.
The U.S. Preventive Services Task Force recommends that everyone age 45 to 75 undergo colon cancer screening. This can be a stool test, flexible sigmoidoscopy, colonoscopy or CT colonography.
People with higher risk factors, such as inflammatory bowel disease, family history of colon cancer or polyps, or certain genetic syndromes may need to be screened earlier, according to the U.S. Centers for Disease Control and Prevention.
Noninvasive stool-based screening, which is usually done at home, tests your feces for signs of cancer. You can receive either a negative or positive result. A positive finding doesn’t guarantee cancer. It might also be that someone has a precancerous colon polyp that should be removed or maybe ate something that triggered the test. False positives are also possible, Mohl said.
py,” Mohl said. “The reasons about why people might do a stool-based test are also reasons why they might not follow up. It’s inconvenient. They are weirded out by it or they don’t have transportation.”
It’s also possible some individuals don’t understand the significance of a positive stool-based test result. “If you have a positive stool-based test, you’re at roughly 10 times higher risk of having colon cancer, so that it makes it very urgent that you would go in,” Mohl said.
At-home tests like this are very important to democratize health care, said Dahut.“I think it’s concerning,” Dahut said of the study’s results. “Not shocking, sadly, but concerning.”
The importance of follow-up colon cancer screening may not be resonating with people in the same way other screenings do, Dahut said, using an abnormal mammogram as an example of screening that might have higher response.
Someone who gets an abnormal mammogram may also have more persistent follow-up from their doctor’s office, Dahut said.
“There needs to be an immediate link between a positive test and your colonoscopy,” Dahut said. “If you get a positive test, in a perfect world you would then be put into a system where you would be given options for colonoscopy, as opposed to having to just take care of it yourself.”

“They’re not diagnostic. They can’t diagnose the condition you have. They just tell you that maybe you’re at particularly high risk,” Mohl said. In that case, patients should schedule a colonoscopy.
Reasons people might opt for stool screening as a first step over colonoscopy are that a colonoscopy involves sedation and is more time consuming. Generally, someone getting a colonoscopy needs to take the day off work and arrange transportation home after the procedure. Sometimes it’s hard to get an appointment because there may not be enough providers.
“One of the big factors is just patients being uncomfortable with colonosco-
A patient navigator or nurse practitioner might fill that role, Dahut said. “It needs to be done in a way to close that loop up,” he added. Another solution may be more provider education, the researchers suggested. Researchers were also from the cancer detection business Exact Sciences Corporation in Madison, Wis., and the Allegheny Health Network in Pennsylvania.
More information
The U.S. Centers for Disease Control and Prevention has more on colon cancer.
36 H&C
Few Americans Understand Alcohol’s Impact on Cancer Risk
Alcohol increases the risk of cancer, but some Americans think it does the opposite, a new study shows.
Researchers set out to understand people’s awareness of the links between alcohol and cancer, finding that many would benefit from further education on the issue.
“All types of alcoholic beverages, including wine, increase cancer risk,” said senior study author William Klein, associate director of the U.S. National Cancer Institute’s Behavioral Research Program. “This study’s findings underscore the need to develop interventions for educating the public about the cancer risks of alcohol use, particularly in the prevailing context of national dialogue about the purported heart health benefits of wine.”
Using data from a government survey that included responses from more than 3,800 adults, the researchers analyzed answers to questions that included “In your opinion, how much does drinking the following types of alcohol affect the risk of getting cancer?” The investigators also asked the participants about their own alcohol intake. About 31% of participants were aware of the cancer risk for liquor, followed by nearly 25% for beer and just over 20% for wine. Some actually thought that alcohol reduced cancer risk, including 10% of participants who said wine reduced risk, 2.2% who thought beer lowered risk and 1.7% who said that liquor did, the findings showed. More than 50% of people reported not knowing the impact of these beverages on cancer risk.
Awareness about alcohol and cancer risk was not associated with drinking status. Nondrinkers, drinkers and heavier drinkers all had similar awareness rates.
Alcohol contributed to an average of more than 75,000 cancer cases and almost 19,000 cancer deaths each year between 2013 and 2016, according to the American Association for Cancer Research (AACR).
“Alcohol is a leading modifiable risk factor for cancer in the United States and previous research has shown that most Americans don’t know this,” Seidenberg said in an AACR news release.
Any beverages that contain ethanol increase cancer risk, including wine, beer and liquor. Alcohol consumption has been linked to cancers of the breast, mouth and colon.
“Educating the public about how alcohol increases cancer risk will not only empower consumers to make more informed decisions, but may also prevent and reduce excessive alcohol use, as well as cancer morbidity and mortality,” Klein said.
The findings were published in Cancer Epidemiology, Biomarkers & Prevention.
More information
The American Cancer Society has more on the causes of cancer.

You are cordially invited to the
MC:
The
For
Every
Cost: $395 per person
Dress Code: jacket and tie

314-786-5950
Invitations
2023 Annual Men’s Dinner
November 9
5:45 Dinner 6:45 The Ritz-Carlton St. Louis
Speaker: Former Mizzou Football Coach Gary Pinkel
Thursday,
Cocktails
Featured
Guy Phillips
Annual Men’s Dinner raises funds for cancer research, care and prevention for men and women, pediatric to geriatric.
man will enjoy a gourmet dinner and receive a $150 gift certificate that can be used at one of several stores.
www.mensgroupagainstcancer.org
more information about the St. Louis Men’s Group Against Cancer, visit or call
will be mailed the first week in October and will be available online.
U.S. Cancer Deaths Decline Overall, But Prostate Cancers Make Rebound
Cancer deaths continue to decline, dropping 33% since 1991 and saving an estimated 3.8 million lives, according to the American Cancer Society’s Cancer Statistics 2023 annual report.
But individual trends within that overall success story highlight the struggle to find the best ways to prevent, detect and treat cancer for all Americans, the society said.
On the positive side, the United States saw an “astounding” 65% reduction in cervical cancer rates among 20- to 24-yearold women between 2012 and 2019, a direct result of human papillomavirus (HPV) vaccination, said Dr. William Dahut, chief scientific officer at the American Cancer Society (ACS).
“The effort that our children went through over the last 20 years or so to get vaccinations have actually saved lives,” Dahut said, noting that the plummeting case level “totally follows the time when HPV vaccines were produced.”
Chief executive officer Karen Knudsen added that “this is some of the first real-world evidence that HPV vaccination is likely to be effective in reducing cancer incidence and [death rates].”
Prostate cancer on the rise
Unfortunately, rates of advanced prostate cancers are on the rise, likely driven by confusion and conflict over screening guidelines, ACS officials said. The second-leading cause of cancer death for U.S. men, prostate cancer cases rose 3% a year from 2014 through 2019 after two decades of decline, the report found.
There’s also been a 5% year-over-year increase in diagnosis of men with advanced prostate cancer, “so we are not catching these cancers early, when we have an opportunity to cure men,” Knudsen said.
Black men, in particular, are being affected by the rise in prostate cancer, according to the report. “Black men, unfortunately, have a 70% increase in incidence of prostate cancer compared to white men
and a two- to fourfold increase in prostate cancer [death rates] as related to any other ethnic group in the United States,” Knudsen said.
More screening is needed
The nation’s leading authority on health screening, the U.S. Preventive Services Task Force, recommends that men between 55 and 69 years of age discuss the potential benefits and harms of prostate cancer screening with their doctor and then decide for themselves.
American Cancer Society guidelines recommend that doctors discuss screening with men at an earlier age — 40 for those with a close relative who has had prostate cancer, 45 for men at high risk, and 50 for nearly all others.
The concern is that the screening tool — the blood-based PSA (prostate-specific antigen) test — can be influenced by factors other than prostate cancer, Knudsen said. For example, inflammation of the prostate can cause a rise in PSA.

38 H&C
Men who undergo prostate cancer surgery or radiation therapy can wind up with lifelong side effects like impotence or incontinence. Because of this, screening guidelines have tended to be conservative. But the science around prostate cancer detection has advanced in recent years, Dahut said. Doctors can now put together a genetic profile that will reveal increased risk in some men. For instance, the BRCA2 gene normally associated with breast cancer “puts people at higher risk for having more aggressive prostate cancer,” Dahut said.
“MRI imaging of the prostate has really dramatically changed the way we think of actually determining if prostate cancer is likely to be there and how to go ahead and biopsy it,” Dahut said. “And there may be ways to do relatively rapid MRIs. They’re doing that actually in the U.K. right now.”
Combining family history, genetic risk factors and MRI results can help doctors weed out potential prostate cancers from cases where PSA levels have increased for other reasons, Dahut said. Knudsen agreed. “This is not the 1990s, where a rising PSA would trigger potentially premature strategies for prostate removal,”
she said. “We have moved so far beyond that as a field.”
The IMPACT initiative
To address these prostate cancer trends, the ACS is launching the IMPACT initiative — Improving Mortality from Prostate Cancer Together. It’s aimed at reversing the disparities in prostate cancer for Black men and reducing death rates overall by 2035, Knudsen said. IMPACT will include new research programs, improved education efforts and a reconsideration of prostate cancer screening guidelines, she explained.
The Cancer Statistics 2023 report contained other pieces of good news, including an all-time high 12% five-year survival rate for pancreatic cancer, up 1 percentage point from the previous year. This is the first time since 2017 that the survival rate for pancreatic cancer has increased two consecutive years, the Pancreatic Cancer Action Network noted in a statement. There’s no standard early detection method for pancreatic cancer, which often only has vague symptoms. The disease is typically diagnosed late, once it has already spread.
“For a disease as difficult as pancreatic cancer, an annual increase of 1 percentage point is an important and encouraging milestone that shows we’re headed in the right direction and our comprehensive approach is working,” said Julie Fleshman, president and CEO of the network. “But 12% is still the lowest five-year survival rate of all major cancers so we need to build on this momentum by continuing to fund research to find an early detection strategy and better treatment options for pancreatic cancer patients.”
The findings were published online in CA: A Cancer Journal for Clinicians.
More information
The American Cancer Society has more about cancer facts and statistics.
Our specialty is you.
As an accredited Commission on Cancer (CoC) program, St. Luke’s understands that a cancer diagnosis can be overwhelming. At the St. Luke’s Center for Cancer Care, we offer comprehensive inpatient and outpatient services to support patients and their families throughout their cancer journey. From world-class medical expertise and state-of-the-art technology to convenient and accelerated access to care, the St. Luke’s team is ready to help you fight cancer with a renewed hope for tomorrow. Schedule your appointment at StLukesCare.com/Oncology
Compassionate care
Strong relationships that help you navigate every step of your health and wellness journey.
Nationally recognized
Consistently honored as America’s best for excellence in patient care and more.

Best technology
The innovation and tools to ensure you get the best results for your health.
Easy access
Convenient locations plus same-day appointments at some offices.
Our specialty is innovative cancer care.
Spinal Cord Stimulation May Ease Diabetic

Neuropathy
Electrical stimulation from a spinal cord implant can provide long-lasting relief for people with diabetic neuropathy, updated clinical trial results show.
“Two years after starting with using that stimulator device, they’re still having the same quality of improvement as what we first saw,” said lead researcher Dr. Erika Petersen. She is director of functional and restorative neurosurgery at UAMS (University of Arkansas for Medical Sciences) in Little Rock, Ark.
Approximately 37 million Americans have diabetes, and about one-quarter develop painful diabetic neuropathy, researchers explained in background notes. Their diabetes does damage to small nerves, typically in their hands and feet, Petersen said. This causes a variety of painful sensations — burning, pins and needles tingling, and itching among them.
“I’ve had someone describe it to me as if they feel like they’re walking on crushed glass when they put their feet on the floor. Even just having a sheet over their feet when they sleep at night is uncomfortable,” Petersen said. “I have one patient who had to build a custom little tent frame for his blankets at the bottom of his bed with PVC pipes to prevent the sheets from brushing on his feet.”
Spinal cord stimulators
Spinal cord stimulators have been around for decades, used to treat various forms of pain. In 2021, the U.S. Food and Drug Administration approved the use of a spinal cord stimulator device specifically
to treat diabetic neuropathy in the legs and feet, Petersen said.
Electrical leads are placed into the spinal canal, and run back to a battery pack that is placed under the skin. “You can think of it like a pacemaker for pain,” Petersen said. “The device delivers small impulses that change how the nerves within the spinal cord process the pain messages that are coming from the feet through the spinal cord up towards the brain and helps them decrease how those pain messages are conducted.”
For their clinical trial, Petersen and her colleagues recruited 216 people with painful diabetic neuropathy symptoms for at least a year who were no longer responding to medications. Initially, half of the people received spinal cord stimulation for six months, while the other half received regular medical treatment (the “control” group).
At six months, people with the implant reported a 76% decrease in their pain and a 62% improvement in their motor function and reflexes, the results showed. By comparison, the control group had a 2% increase in pain and a 3% improvement in function.
After six months, those in the control group were given the option to receive an implant. More than 90% opted to get the stimulator, while no one with an implant asked to be switched to medication, the study authors reported.
The researchers continued to follow the patients, and now report that two years out 80% still have less nerve pain and 66% report continued improvement in motor function.
There also were no nerve damage issues associated with the stimulator, and the surgical risks were comparable to what are found in patients without diabetes who receive spinal stimulator implants for other conditions, Petersen said. Eight people had surgical infections related to the device, and five had to have their devices removed due to infection.
Use after medications no longer help
The results showed that spinal cord stimulation is a solid option to pursue if medications stop helping a patient with diabetic neuropathy, Petersen said. “Over time, these medicines stop working
40 H&C DIABETES CARE
as effectively, or people develop side effects. Some of the medicines are really expensive, and people just don’t pay for them because it isn’t worth it,” Petersen said. “Up to about 70% of people taking Pregabalin, for example, will stop taking it within a year because of various problems with the medication.”
The findings were scheduled for presentation at the American Academy of Neurology annual meeting, to be held April 22 to 27 in Boston. Findings presented at medical meetings should be considered preliminary until published in a peer-reviewed journal.
Dr. Michael Polydefkis, a professor of neurology with Johns Hopkins Medicine in Baltimore, agreed that the results are “exciting.”
However, Polydefkis noted that the clinical trial results could have been influenced by a placebo effect, given that the people who received the implant knew that they were receiving special care.
“The placebo effect is notorious in pain studies,” Polydefkis said.
Cleveland Clinic pain management expert
Dr. Shrif Costandi found the clinical trial results persuasive as well.
“The findings are very promising, and it’s providing an important tool to help those patients who are suffering and whose quality of life is being compromised by this chronic pain,” Costandi said.
Still, Petersen and Costandi said medications should remain the front-line therapy for diabetic neuropathy. Patients should be offered the implant after drugs fail to diminish their pain.
“I think it makes sense to try medicines first, but I don’t think that people should be on medicines for years and years and years if they’re not helping,” Petersen said. “I think that if you try medicines for a reasonable amount of time, that moving on to the stimulator is a good option.”
Spinal cord stimulator implants can be pricey, costing tens of thousands of dollars, but following the FDA approval more insurers are moving to cover their cost, Petersen noted.
“So about 60% or more, last time I checked, of insurance companies are covering the device in the U.S., and that
includes Medicare as well as commercial insurances,” Petersen said. “Access is definitely improving, as far as that goes.”
Try before you buy
One nice thing is that patients can “test drive” spinal stimulation before receiving a permanent implant, Petersen said.
“The person gets the wires placed in through needle in an office procedure, and they wear an external device home for about a week so they can test drive and see what kind of response they have over that week and decide whether that benefit is enough for them to go forward with the permanent procedure,” Petersen said.
“It’s one of the few operations where my patients can actually test out what their results will be like before they actually have their operation, and it gives a really good idea as to whether it meets their expectations,” she continued.
The clinical trial was funded by Nevro Corp., the maker of the spinal cord stimulation system.
More information
Johns Hopkins Medicine has more about diabetic neuropathy.

41 H&C
40-Year Study Finds Weight-Loss Surgery Extending Life Spans
It’s well known that obesity fuels an increase in a person’s risk for other chronic health conditions. Now, a new study shows that weight-loss surgery could set that person’s health, and longevity, on a different path.
Utah researchers who followed patients for up to 40 years after they had one of four types of weight-loss (bariatric) surgery found they had significant reductions in death rates from all causes compared to obese patients who did not have surgery. All-cause death for both men and women was 16% lower. For heart disease, it was 29% lower. For cancer, deaths dropped by 43%, and it was down a full 72% for diabetes. “The take-home message is that people are generally long-term going to have improved health in those areas,” said lead study author Ted Adams. He’s an adjunct professor in internal medicine and an adjunct associate professor in nutrition and integrative physiology at the University of Utah School of Medicine.
Potential negative outcomes
Unfortunately, his team also unearthed some important negative outcomes. Death rates from chronic liver disease in patients who had bariatric surgery were 83% higher, when compared to patients who didn’t have the surgery. Patients who had the surgery also had a 2.4 times higher risk for suicide, though that effect was seen primarily in younger people, ages 18 to 34.
Although the researchers in this study didn’t look at data on pre-surgical behavior or substance use, these issues have been reported in other studies, Adams noted. For liver disease, it is possible this happens because weight-loss surgery changes how alcohol is absorbed by the body, Adams noted.
In terms of increased suicide risk, the study noted that younger patients may need more aggressive pre-surgery screening for psychological issues and follow-up after surgery.
Four bariatric procedures
The four procedures included in the study were Roux-en-Y gastric bypass, adjustable gastric banding, sleeve gastrectomy and biliopancreatic diversion with duodenal switch. Researchers used data from the Utah Population database that included nearly 22,000 patients, matching those with bariatric surgery and those without it.

Patients who had bariatric surgery had done so between 1982 and 2018 and were identified through three large bariatric surgery practices in Salt Lake City, as well as at the University of Utah and Intermountain Healthcare.
Researchers said the results may increase interest in weight-loss surgery. The findings were published in the journal Obesity.
Most important is weight loss
Dr. Angela Fitch, president of the Obesity Medicine Association, said though the research is focused on bariatric surgery, what it may really be showing is the impact of reducing overall weight by more than 20%.
“What surgery has provided us for many years is the ability for patients to maintain and sustain a greater than 20% weight reduction,” said Fitch, who was not involved in the study. “The outcome data for a long time have shown some of these things, but this is just much more definitively putting it in a nicer sort of box, so to speak, and looking at it much longer-term.”
That is a goal that can’t be reached by most patients through other methods. Only about 5% of obese people can sustain a 20% weight loss with lifestyle interventions such as exercising more, eating better and getting good sleeping, Fitch said.
“I think what’s most exciting too is certainly not only the cardiovascular risk reduction, but the cancer risk reduction,” she said.
“Yet there’s this huge stigma in the world [that] if you have [weight-loss] surgery, you’re taking the easy road and you’re cheating the system,” Fitch said.
The findings on suicide suggest that some patients need more support and there should be a discussion on whether surgery is right for that person based on his or her mental health history, she added. In terms of liver damage, it’s possible some patients are turning to alcohol for comfort, rather than food, Fitch said.
For some patients, surgery is the only viable treatment for obesity because insurance may not cover weight-loss medications, Fitch noted.
“I think it confirms that surgery for obesity treatment is the most effective tool we have today to cause a risk reduction of mortality from these other diseases, that in the long run, having surgery is beneficial and we should probably have it sooner rather than later to prevent some of these other complications,” she said.
More information:
The U.S. Centers for Disease Control and Prevention has more on obesity.
42 H&C
Certain Class of Diabetes Meds Could Cut Dementia Risk
An older class of type 2 diabetes drugs known as thiazolidinediones, or TZDs, may protect you from dementia down the road, according to new research. Thiazolidinediones cut dementia risk by 22% among folks at high risk who also had mild or moderate type 2 diabetes when they took these medications for at least one year.
Exactly how these diabetes drugs lower risk for dementia is not fully understood, and the study wasn’t designed to answer that question.
Diabetes and Dementia
Diabetes is a known risk factor for dementia, and glucose or blood sugar is the brain’s main fuel for important functions, including thinking, understanding, and problem-solving, said study author Roberta Diaz Brinton. She directs the Center for Innovation in Brain Science at the University of Arizona Health Sciences. “With type 2 diabetes, the mechanism for driving glucose out of the blood and into the cells is less functional and this can affect cognition, which is one of the most energy-demanding functions,” Brinton said.
Specific Drugs Tested
For the study, researchers compared risk for dementia in older veterans with type 2 diabetes who were treated with either a sulfonylurea or a thiazolidinedione drug for diabetes to those treated with metformin alone between 2000 and 2019 in the U.S. Veterans Affairs Healthcare System.
These diabetes drugs all work differently. Thiazolidinediones help your body better use insulin to allow blood sugar to enter your body’s cells where it can be used for energy. Sulfonylureas boost insulin production and help your body use this
hormone. Metformin makes your body more sensitive to insulin and decreases the amount of glucose secreted by your liver.
Results
People aged 60 and older who were given a first prescription of metformin, a sulfonylurea or a thiazolidinedione between January 2001 and December 2017 were followed for about eight years. Those who took thiazolidinedione had an 11% lower risk of Alzheimer’s disease and a 57% lower risk of vascular dementia, the study showed. Vascular dementia is typically caused by multiple strokes.
The risk of dementia from any cause was 12% higher among folks who used a sulfonylurea drug alone for their diabetes, the study showed.
Folks under age 75 saw more benefits from a thiazolidinedione than older people, and these drugs seemed to be more protective in people who were overweight or obese. “Thiazolidinediones were the most effective in reducing the chances of developing Alzheimer’s disease later in life,” Brinton said.
Like all drugs, thiazolidinediones can have side effects, including weight gain, liver problems and vision problems. One drug in this class, rosiglitazone, has been removed from the market in several countries due to serious heart risks.
“Starting early and sustaining glucose metabolism without moving into taking insulin has long-lasting benefit,” Brinton said.
Lifestyle counts, too. “There is pharmacotherapy and the things we are in charge of, like what we eat and how much we move,” Brinton said. “Sitting is the new smoking.”
The study was recently published in BMJ Open Diabetes Research & Care.
Dr. Howard Fillit, co-founder and chief
science officer of the Alzheimer’s Drug Discovery Foundation in New York City, noted that diabetes is a risk factor for dementia, so effective treatment of diabetes is important.
“It remains unknown which class of anti-diabetic agents would be most beneficial in reducing dementia risk in diabetics,” Fillit said. It’s also too early to recommend these drugs if you are at high risk for dementia but don’t have diabetes, he added. “These observational studies, when combined with other epidemiological data, as well as preclinical data, might indicate benefit,” Fillit said. “However, at this time, it is certainly premature to promote or recommend widespread use of anti-diabetic agents of any class for the prevention of dementia, particularly Alzheimer’s disease.”
More Information
The Alzheimer’s Drug Discovery Foundation offers seven steps to prevent or delay dementia:
1. Specific diets — including the Mediterranean, DASH, and MIND diets— may promote brain health.
2. Good sleep - To protect your brain, establish a bedtime routine, maintain a regular sleep schedule, and treat sleep-disordered breathing such as apnea.
3. Exercise - Avoid long periods of physical inactivity and engage in moderate-intensity aerobic exercise for at least 30 minutes, 3 to 5 days per week.
4. Avoid stress - Prolonged stress can harm your brain, leading to fatigue, disturbed sleep, poor concentration, and memory lapses. Make changes to your lifestyle and learn ways to cope.
5. Be social - Loneliness and depression can impair cognitive health, causing memory loss and attention deficits. Maintain and build your social connections.
6. Keep learning - Stimulate your brain throughout life by engaging intellectually. Education at any age may protect against cognitive decline.
7. Manage chronic illness - Some chronic diseases can raise the risk of dementia and some medications can impair your brain’s function. Periodically review your medications and supplements with your physician and work with them to manage your brain health.
43 H&C
Had a Kidney Stone? This Diet May Help Prevent Another A
nyone who has ever had a kidney stone never wants a repeat of the blinding pain that comes when it passes. Now, a new study maps out a diet that can help guard against that.
Importance of potassium and calcium
The cornerstones of that diet include eating plenty of foods that contain potassium, as well as a few servings of low-fat dairy daily, to get enough calcium. High-potassium fruits and veggies that could help include bananas, oranges, grapefruits, apricots, mushrooms, peas, cucumbers, zucchini, and melons such as cantaloupe and honeydew.
To arrive at those recommendations, researchers from the Mayo Clinic used data from questionnaires completed by kidney stone patients between 2009 and 2018. The team compared the diets of 411 people who had already had their first kidney stone and a control group of 384 individuals.
“We had this information and then we, number one, could look at things that … differed between controls and kidney stone formers, but then we’ve also been following these people forward in time,” said study author Dr. John Lieske, director of the O’Brien Urology Research Center at the Mayo Clinic in Rochester, Minn.
During a median of just over four years of follow-up, 73 patients in the study had recurrent kidney stones.
Lower levels of calcium and potassium predicted that recurrence. After adjustments for non-dietary factors, lower calcium continued to be a predictor. So did lower potassium, but only among those who weren’t already taking certain types of diuretics and calcium supplements.
So, how much calcium and potassium should be consumed each day to keep kidney stones at bay?
Two to three servings of low-fat dairy daily would be the ideal way to consume the needed calcium, Lieske said, or an amount equal to 1,200 milligrams. That number matches the U.S. Department of Agriculture’s (USDA) daily recommended amount for most adults.
Pinpointing a number for potassium was less precise, because the USDA doesn’t offer a recommended level for potassium intake.
always be helpful,” Lieske said.
Importance of the study
Unfortunately, people who’ve had one kidney stone have a good chance of a repeat one, about 30% within five years.
Having a kidney stone isn’t only an excruciating experience, but it’s also associated with other health issues, including chronic kidney disease, osteoporosis and heart disease.
The findings were published online in Mayo Clinic Proceedings.
Dr. Gary Curhan, a member at the Channing Laboratory and Renal Division at Brigham and Women’s Hospital in Boston, has researched kidney stones for decades. Curhan was not involved in this study.
“One of the things that’s novel about this now is that they look for stone recurrence, which actually is really important,” Curhan said. “Up to now, we’ve extrapolated our findings on incident formation to recurrent, but we didn’t have that.”
One challenge, however, is knowing whether a new symptomatic kidney stone was truly recurrent or whether it was formed around the time the first one formed, but didn’t pass until later, Curhan said.
Drink lots of water
The good news? While patients may not be willing to adjust their diet before a first kidney stone, they are far more likely to do so to prevent a recurrence, the authors noted. A key piece of advice on avoiding recurrent kidney stones includes drinking water, lots of it — about nine 12-ounce glasses of water per day.
Though this new study didn’t note the benefit from water, that may be because it was following people who already were drinking high quantities of water after their first kidney stone, Lieske noted. “I would still say that’s always one of the mainstays when we see people, that they should definitely drink more fluid if they’ve had a kidney stone. That just will
He noted that there is more than one type of kidney stone, with the most common being a calcium oxalate stone. In addition to adding plenty of fluids and more of certain foods to a diet, it may also be necessary to limit other foods. That can best be determined by working with a specialist who can evaluate the type of kidney stone a patient has, Curhan said.
“I think the takeaway is that diet does matter for stone formation. Lots of people think that diet doesn’t matter, but it absolutely does,” Curhan said. “We now have decades of evidence that that’s the case.”
More information
The U.S. National Institute of Diabetes and Digestive and Kidney Diseases has more on kidney stones.

44 H&C KIDNEY DISEASE
Debunking Myths About Organ Donation
Far more people need an organ transplant than there are organs available, but it doesn’t have to be that way. Dr. Johnny Hong, chief of transplantation at Penn State Health’s Milton S. Hershey Medical Center in Hershey, explored some of the myths about organ donation.
Shortage of donated organs
“We have an organ shortage crisis,” he said in a center news release.
Seventeen people on the waiting list for an organ will die today, and misinformation is a big part of that.
While more than 100,000 people in the United States wait for organ transplants, less than half that received them last year. Nearly 43,000 people received an organ, up 3.7% from 2021.
One reason: Many potential donors fail to check the organ donation box on driver’s license applications or choose not to register. Yet, Hong said, a single deceased organ donor can save as many as eight lives.
Organ donation is highly regulated
The first myth Hong wants to correct is that doctors won’t revive you if you’re near death and have signed up to be an organ donor because they want to harvest your organs. “There is absolutely no truth to that,” Hong said.
The words “organ donation” aren’t even mentioned in an emergency until the patient meets very specific legal criteria for being past the point of no return – when the heart has stopped or the brain has died, he emphasized. Health care workers are entirely concerned with saving the person’s life, Hong said.
“Organ donation is highly regulated,” he said. “There are multiple layers of
regulatory requirement.” The Organ Procurement and Transplantation Network website (https://optn.transplant.hrsa.gov) has the specifics.
The heart can be transplanted four hours after death, according to donatelife.org. A liver can last 24 hours. Corneas can be donated 14 days after someone dies. Some donations can be made years after a donor’s death. Bones and skin, for exam-
State Health. Likewise, when part of the liver is donated, the remaining part of the organ will grow and supply full function.
Safeguards and recovery
Doctors also put living donors through a vigorous battery of testing. Penn State Health noted that the medical team is worried about protecting two lives – the living donor and the transplant recipient.
Living donors do have to recover from the surgery, but surgery is becoming easier as medical science progresses, Hong said.

While donating a kidney once meant a five- to seven-day hospital stay, today’s laparoscopic procedures mean donors typically go home within three days.
ple, are viable for five years. Heart valves can be used 10 years after they’ve been removed from living tissue, according to Penn State Health. “A huge focus in our medical research today is geared toward developing new therapies to allow donated organs to remain viable for an extended period,” Hong added.
More donors are needed, and there is no lifespan risk
Another myth is that there’s a fee for donating organs. Hospitals and doctors can’t charge people making a donation and donors can’t be paid for their donation. That’s the law.
Nor is it true that there are already enough donors, Hong said. Transplantation experts use nationwide lists to search for matches in blood type and immunology. Organ size must also match.
Another myth is that if a person donates an organ such as a kidney or part of a liver, their life span will shrink. It’s not true. If you have two healthy kidneys, one kidney will take up the job of its missing counterpart with no ill effects, according to Penn
Liver donation typically results in a longer hospital stay – a week or more. That’s because the remaining portion of the liver must be nurtured to regenerate what was lost. Home recovery can take two to three months. Doctors are now moving toward less invasive methods for liver donation, Penn State Health noted.
Finally, Hong said it’s not true that someone can’t donate if they’ve had an illness or they’re older. “The No. 1 priority for a living donor program is the safety and well-being of the living donor,” he said. “So, if there’s anything that would subject the donor to an additional risk, like a chronic illness, then most likely the person will not be able to donate. But again, we have to define that illness clearly.”
Physiological age is more important than chronological age when donating, according to Hong. There is no age cutoff and deceased donors are sometimes 70 to 80 years old. Organ function and overall health are what matter. Living donors must be healthy enough to undergo the operation safely and be well after donation.
45 H&C
Advent of Electric Cars Is Already Improving Health E
lectric cars are still in the minority on America’s roads, yet researchers are already seeing health benefits from reduced tailpipe pollution.
Decline in asthma-related ER visits
In a new California study, neighborhoods with the most all-electric cars – called zero-emission vehicles – saw a decline in asthma-related emergency room visits. Researchers believe this was a result of lower levels of nitrogen dioxide (NO2) in the air.
“Results from this study provide some of the first real-world evidence suggesting that switching to zero-emissions vehicles could be a win-win, both reducing emissions of greenhouse gases and potentially improving local air quality and health,” said study co-author Sandrah Eckel, an associate professor of population and public health sciences at the University of Southern California’s Keck School of Medicine in Los Angeles.
Income and education factors
The adoption of electric cars, however, was seen in areas with higher incomes and educational levels, she said. This might be due to their higher cost and the lack of charging facilities in rental properties.
“We are concerned about environmental justice because the communities that stand to benefit the most from reductions in air pollution and asthma ER visits are the communities at risk of being left behind in the transition to electric,” Eckel said.
“We need to overcome some of these barriers and make sure that the policies that are made can target the populations that stand to benefit the most from these environmental and health care benefits,” she added.
Eckel and her colleagues used data from the California Department of Motor Vehicles to look at electric automobile
purchases by zip code and data from the U.S. Environmental Protection Agency to analyze NO2 levels. They also tracked emergency room visits for asthma between 2013 and 2019. Asthma, a respiratory disorder, has long been associated with air pollutants such as NO2. At the zip code level, for every additional 20 electric or zero-emissions vehicles per 1,000 people, researchers saw a 3.2% drop in the rate of asthma-related ER visits.
Community health benefits to come
As more electric cars and trucks inhabit the nation’s roads, Eckel believes the health benefits will continue to grow. She noted that all cars and light trucks sold by 2035 must be zero-emission vehicles in California.
“It was remarkable that we are already seeing health and possibly air quality improvements related to increasing numbers of zero-emission vehicles, even though zero-emission adoption levels are still low,” Eckel said.
As of last fall, nearly 18% of new cars sold in California were all-electric, according to California’s Office of the Governor. That compares with about 6% throughout the nation.

Will Barrett, senior director for clean air advocacy at the American Lung Association, was impressed by the study findings. “That study really underscores that we will continue to see that by eliminating transportation pollution at the tailpipe you could have a real benefit in community health,” said Barrett, who wasn’t involved with the study.
“By transitioning to zero-emission technologies, we could be looking at over a trillion dollars in public health benefits across the United States over the coming decades,” he added.
The potential health benefits are considerable, Barrett said. “We’re talking about reductions in asthma attacks, reductions in heart attacks and strokes, reductions in premature deaths and lung cancer,” he noted. “And also millions of lost workdays could be avoided by making the transition away from combustion to zero-emission.”
Barrett agreed that zero-emission vehicles need to be within the reach of all Americans. “Those in all communities, whether they’re rural or low-income – making sure that this distribution of health benefits is equitable across communities,” he said. Zero-emission trucks and buses
As the nation moves toward zero-emission heavy-duty trucks and buses, you can expect to see even more air and health improvements, Barrett said.
“The benefits of that transition are going to be even leaps and bounds greater in some ways than the passenger vehicle fleet benefits, because, for example, about
5% to 10% of all the vehicles on the road in the United States are medium and heavy-duty trucks, but they produce the most pollution of anything else on the road,” he explained.
“The transition to zero-emission trucking is going to be one of the most important public health interventions that we could see,” Barrett said.
The report was published in the journal Science of the Total Environment.
More information
For more on car pollution, head to the Union of Concerned Scientists.
46 H&C BETTER BREATHING
Global Review Finds Vaccination Cuts Odds of Long COVID in Half
Areview of studies from around the world finds that getting vaccinated halves the risk of long COVID-19. For the review, a team led by researchers from the University of East Anglia in the United Kingdom looked at data from 41 studies involving more than 860,000 patients to gauge risk factors for the array of symptoms that can linger after a COVID infection.
Several groups were more likely to experience long COVID, including women, people who are overweight or over 40, smokers, and those with anxiety, depression and preexisting conditions such as asthma, COPD, type 2 diabetes, coronary heart disease or suppressed immune systems. Patients hospitalized with COVID
were also more likely to experience long COVID.
“Conversely, it was reassuring to see that people who had been vaccinated had significantly less risk – almost half the risk – of developing long COVID compared to unvaccinated participants,” said researcher Dr. Vassilios Vassiliou, a clinical professor of cardiac medicine at the university’s Norwich Medical School.
“These findings are important because they enable us to better understand who may develop long COVID and also advocate for the benefit of vaccination,” he said in a university news release. Long COVID affects about 2 million people in the United Kingdom. The U.S. Government Accountability Office estimates that up to 23 million Americans have been affected
by long COVID.
Symptoms, which persist for more than 12 weeks after infection, include shortness of breath, coughing, heart palpitations, headaches, severe fatigue, chest pain or tightness, brain fog, insomnia, dizziness, joint pain, depression and anxiety, tinnitus, loss of appetite, headaches, and changes to sense of smell or taste.
“Our findings help define the full demographic characteristics and the risk factors for developing long COVID,” said co-author Dr. Eleana Ntatsaki of University College London and Ipswich Hospital in the U.K. She said doctors can now better understand, plan for and serve this population.
“Furthermore, we can have a better strategy for optimizing any modifiable risk factors, with public health promotion campaigns, encouraging smoking cessation, vaccination and healthy weight management in the target population,” Ntatsaki said in the release.
For
Better Breathing Purify the Air
Your Home with Whole-House HEPA Air Filtration
Poor indoor air quality is a leading health risk. Pollutants, germs, mold spores, bacteria, and viruses recycle through air systems.
HEPA (High Efficiency Particulate Air) filtration scrubs 99.7% of all bacteria, germs, dust, dander and pollen and 95% of virus particles. It also removes odors, smoke and chemicals present in older homes.

BEAM offers an exclusive HEPA system that connects to your ventilation system and runs 24/7, circulating clean air throughout your house.


in
Call or email for a FREE phone estimate 314-567-1515 sales@beamstl.com
The Most Common Sleep Disorders
By Beth Orenstein
Almost everyone has trouble sleeping occasionally, but when you toss and turn often enough that it affects your health, moods and safety, your bad nights of sleeping may be elevated to the level of a sleep disorder.
Sleep disorders are among the most common medical problems that health care providers see in their practices, according to the book Sleep Disorder published on the National Center for Biotechnology Information government site. Many people with sleep disorders find they have trouble staying awake during the day because they haven’t gotten quality sleep at night.
There are more than 80 sleep disorders, according to the U.S. National Library of Medicine. Some common ones include:
n Insomnia
n Narcolepsy
n Sleep apnea
n Restless leg syndrome (RLS)
n REM sleep behavior disorder
n Shift work sleep disorder (SWSD) Here, learn about the most common sleep disorders, their signs and symptoms, and what treatments may be available.
Insomnia
Insomnia, the most common sleep disorder, is defined as having difficulty falling asleep, staying asleep or being able to get quality sleep, according to the National Heart, Lung, and Blood Institute (NHLBI).
Insomnia may be: Short term (lasting a few days or weeks). This type may develop from stress or schedule or environment changes. Long term or chronic (lasting 3 months or more and for 3-plus nights per week). Chronic insomnia may increase your risk of high blood pressure, diabetes, heart disease and cancer. Often, the cause of chronic insomnia is difficult to determine.
Having another health issue may also contribute to insomnia.

Some things to try when sleep eludes you include:
Establishing a routine and sticking to it. Go to bed close to the same time every night, and wake up at the same time each morning (yes, even on weekends and holidays).
Getting regular exercise. Exercis-
ing at least 30 minutes most days of the week may help you sleep better. Be sure to finish at least 2 or 3 hours before bedtime though to keep your workout from affecting your sleep.
Nixing caffeine and nicotine before bed. Both are stimulants, and their effects may last up to 8 hours. Plus, if you smoke, you may wake up because you feel a craving to smoke.
Relaxing before you go to bed. Unwinding by reading, taking a bath or listening to calming music may make you feel sleepy.
If you can’t sleep, don’t toss and turn — it’ll only make you more anxious. Instead, get out of bed and do quiet activities until you feel sleepy again (such as reading), and then return to bed.
Narcolepsy
When you have narcolepsy, your brain is unable to regulate sleep-wake cycles properly, so even if you sleep well at night, you’re still severely sleepy during the day, and the sleep you get isn’t restful. Excessive daytime sleepiness may cause you to fall asleep in the middle of doing something else, such as driving, eating or talking. Narcolepsy can be very dangerous.
People with narcolepsy may also lose muscle tone, especially when they laugh, feel angry or feel excited. The effect can range from drooping eyes to looking like you’re having a seizure. While scary, episodes tend to be brief and over quickly.
Other symptoms include sleep paralysis, which is the inability to move or speak while you’re falling asleep or waking up, and hallucinations.
Narcolepsy is a chronic condition that doesn’t go away or get worse as you age. It affects men and women equally, and though it may start in childhood, it may occur at any time over the course of your lifetime.
While there’s no cure, narcolepsy may be treated with medications and certain lifestyle changes. According to the National Institute of Neurological Disorders and Stroke (NINDS), medications may include stimulants, antidepressants or an H3 receptor antagonist/inverse agonist. Talk to your health care provider if you think you may need medication to treat narcolepsy.
48 H&C
Lifestyle changes for those with narcolepsy include:
n Taking short naps
n Sticking to a regular sleep schedule
n Avoiding caffeine or alcohol, especially later in the day
n Exercising, making sure to finish at least 4 to 5 hours before bedtime
n Avoiding large, heavy meals before sleeping
n Making time to relax before bed
n Keeping your bedroom cool and comfortable, which is optimal for sleep
Sleep Apnea
Sleep apnea is a sleep condition that causes you to stop breathing over and over again as you sleep, which prevents you from getting adequate oxygen. This lack of oxygen interferes with your ability to get a restful night’s sleep.
Sleep apnea can be one of two types: Obstructive sleep apnea, the most common type, is when your upper airway is blocked, reducing or stopping airflow. It may be caused by obesity, large tonsils or hormone level changes.
Central sleep apnea is when your brain doesn’t send your body the signals required to tell you to keep breathing. If you have a health condition that affects how your brain controls your airway and chest muscles, you’re more susceptible to central sleep apnea.
A sleep study is often used to determine whether you have sleep apnea.
According to NHLBI, the most common treatment for sleep apnea is a breathing device known as a continuous positive air pressure (CPAP) machine. The machine keeps your airway open as you sleep by providing constant air pressure on your throat.
Other treatment options NHLBI notes include:
Oral appliances. You may be fit with a customized oral device to wear in your mouth when sleeping to help prevent your upper airway from becoming blocked. There are two types:
n A mandibular repositioning mouthpiece to hold your jaw in a way to keep it from obstructing the upper airway
n A tongue retaining device to keep your
tongue forward to keep it from obstructing the upper airway
Surgery. Possible procedures include:
n Removing your tonsils and adenoids (called an adenotonsillectomy)
n Implanting a device that monitors breathing and helps control muscles that open your airways
n Removing soft tissue from your mouth and throat to help make your upper airway bigger
n Moving your upper jaw (maxilla) and lower jaw (mandible) forward, which also helps your upper airway become bigger Orofacial therapy. You may be given exercises to help position your tongue and strengthen certain muscles, such as muscles in the lips, tongue, upper airway and face.
Restless Leg Syndrome (RLS)
Restless leg syndrome (RLS) is a sleep disorder and a movement disorder that may start at any time over the course of your life. Women are more likely to have RLS than men, but it affects both sexes. RLS causes uncomfortable sensations in your legs, most often and most intensely at night while you’re asleep. According to NINDS, the sensations cause you to move your legs and disrupt your sleep, and may feel like:
n Aching
n Throbbing
n Pulling
n Itching
n Crawling
n Creeping
Most often, the sensations affect both legs, but they may affect just one. Sensations in your arms, chest or head may occur, too, but are less common. Symptoms may vary from day to day in frequency and severity, and they may become more frequent as you age.
According to NINDS, more than 80% of those with RLS also have periodic limb movement of sleep (PLMS), where your legs twitch and jerk usually every 15 to 40 seconds throughout the night.
While there’s no cure, RLS symptoms may be treated. Treatments may include:
n Iron supplements
n Anti-seizure medications
n Dopaminergic agents, which increase dopamine in the brain
n Certain opioids, such as methadone, codeine, hydrocodone and oxycodone
n Benzodiazepines, which may be used to treat anxiety, insomnia and muscle spasms
Lifestyle changes may also help, such as:
n Drinking little or no alcohol or caffeinated beverages
n Stopping smoking
n Maintaining a regular sleep schedule
n Getting moderate exercise on a regular basis, especially aerobic and leg-focused exercises
n Giving yourself a leg massage
n Taking a warm bath
n Applying heating pads or ice packs to legs
REM Sleep Behavior Disorder
Most people spend about 20% of their sleep time in rapid eye movement (REM) sleep, which is the sleep stage where you dream. Typically, REM sleep is in the later part of the night.
People with REM sleep behavior disorder have unpleasant dreams and act them out with sudden, sometimes violent arm and leg movements.
REM sleep behavior disorder may come on gradually, and the condition may worsen over time.
The disorder may be associated with other neurological conditions, such as Parkinson’s disease, Lewy body dementia and multiple system atrophy (MSA).
According to the Mayo Clinic, symptoms may include:
n Punching, kicking, flailing limbs
n Jumping out of bed in reaction to dreams that are violent or action-filled
n Making noises, such as talking, laughing, shouting, cursing and crying out while dreaming
49 H&C
You may recall your dream if you wake up while having an episode.
REM sleep disorder is treated with medications. According to the Mayo Clinic, medication options may include: Melatonin. Most people are able to take this dietary supplement with little or no side effects.
Clonazepam (Klonopin). This is a prescription medication used to treat anxiety. It may cause you to be sleepy during the day, and it may worsen sleep apnea if you have that condition as well.
If you have REM sleep behavior disorder, it’s imperative you make your sleeping environment safe for you and your bed partner. You may want to:
n Pad the floor near your bed
n Place rails on the side of the bed where you sleep
n Rid the room of dangers, such as weapons and sharp objects
n Remove furniture and clutter from the bedroom
n Fortify windows
Shift Work Sleep Disorder (SWSD)
People who work different shifts and who work at night may have shift work disorder (SWSD). According to the Cleveland Clinic, up to 40% of people who work different shifts might have this disorder. Symptoms may include:
n Trouble sleeping
n Sleepiness
n Difficulty concentrating when awake
n Headaches
n Lack of energy
According to the Cleveland Clinic, people with SWSD are also prone to:
n Accidents and making errors at work
n Dependency on drugs and alcohol
n Irritability or mood issues
n Gastrointestinal, cardiovascular and metabolic health conditions
Treatments may include:
n Aiming for 7 to 9 hours of sleep a day
n Making sleep a priority
n Limiting the number of night shifts in a row to 5 or fewer
n Having days off in between shifts
n Avoiding long commutes if possible
n Practicing good sleep hygiene, which includes sticking to a sleep schedule and avoiding stimulants such as caffeine, alcohol and nicotine
n Napping before starting a night shift
n Getting exposure to light during the early part of your shift
n Keeping a sleep diary to identify your problem and monitor your progress
If you live with others, ask them to respect your sleep time by keeping their voices down, not running noisy appliances such as the vacuum or dishwasher while you’re trying to sleep, and wearing headphones when they’re watching television or listening to music when you’re sleeping.
As a last resort for SWSD, you may want to talk to your health care provider about the use of prescription sleep aids.
FIND YOUR BEST NEW PATIENTS HERE
HEALTH&CARE Journal/St. Louis Metro provides a unique new opportunity for medical practices and health care providers to reach thousands of prospective patients in their homes. These are adults ages 45+ living throughout the St. Louis Metro area.
Each issue features informative articles about prevention, diagnosis, treatment and care for leading chronic health conditions, quoting local and national experts.

Please email or call to set an appointment to discuss this opportunity.
Todd Abrams Publisher toddabrams1@gmail.com 314-443-3024
Carol Kindinger Account Executive carolkindinger@gmail.com 314-452-3576
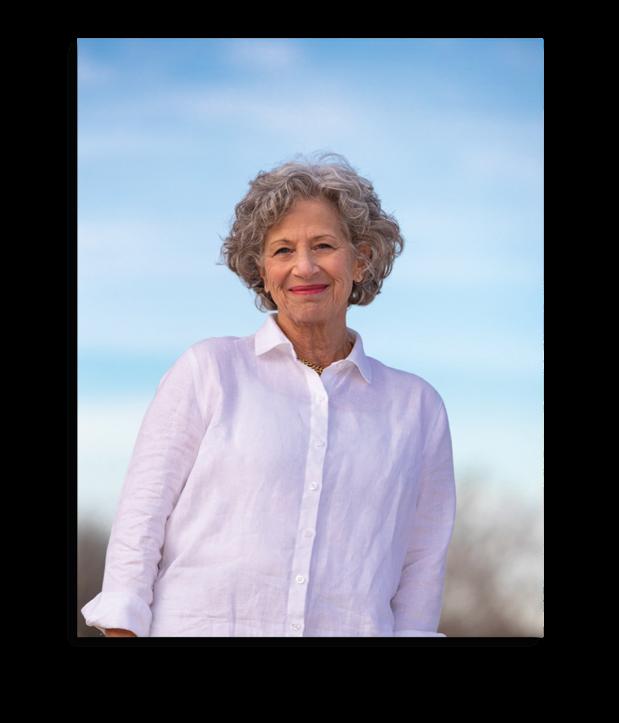
New Screening Questionnaire Might Spot More Cases of Hidden COPD
Chronic obstructive pulmonary disease (COPD) is a leading cause of death in the United States, and with an aging population COPD will continue to become an even greater problem.
Dangers of COPD
COPD is a group of diseases that include emphysema and chronic bronchitis. They can cause airflow blockage and breathing problems. Common COPD symptoms include coughing, shortness of breath, wheezing or whistling, tightness or heaviness in the chest.
Patients with COPD are more likely to also have coronary heart disease. In elective surgery they have lower survival rates and increased costs in the year following surgery.
More than 16 million Americans have COPD, according to the U.S. Centers for Disease Control and Prevention, and experts think millions more have it but don’t know it. But doctors could soon have a new tool to help diagnose COPD. A questionnaire called CAPTURE successfully identified almost half of clinical trial participants who had moderate to severe forms of previously undiagnosed COPD, researchers report.
“The goal with trying to find COPD is to treat it earlier, which will help make patients feel better and hopefully prevent their disease from progressing,” said principal investigator Dr. Fernando Martinez, chief of the pulmonary and critical care medicine division at Weill Cornell Medicine in New York City.
The CAPTURE tool
The CAPTURE tool asks patients five questions that assess their breathing, health symptoms and exposure to chemicals or air pollution. Those with medium scores take an in-office breathing test called spirometry to gauge the force of their exhalation, a measure of lung function.


CAPTURE screening gives doctors additional information to assess patients with respiratory symptoms. “CAPTURE was designed to be easy for physicians to use. The screening is simple, takes less than a minute, and helps identify adults with trouble breathing who should be evaluated further,” Dr. Antonello Punturieri, program director of the U.S. National Heart, Lung, and Blood Institute’s Chronic Obstructive Pulmonary Disease/Environment Program, said in an institute news release. CAPTURE’s clinical trial involved more than 4,300 adults aged 45 to 80 and ran from October 2018 to April 2022. By the end, about 2.5% of the study sample had been diagnosed with moderate to severe forms of COPD. Of those cases, CAPTURE accurately identified about 48% as having COPD. The researchers estimated that 1 in 81 CAPTURE screenings would identify an adult with treatable but previously undiagnosed COPD, based on these results.
However, CAPTURE also gave a false positive result for 479 participants who did not have COPD. The researchers said they are studying ways to improve the tool’s accuracy through minor changes like altering questions or adding others.
Using CAPTURE
“The study shows that there is a high degree of respiratory burden in primary care, and physicians need to ask about it and do the appropriate testing to determine if symptoms are driven by COPD or another process so that patients can get the right treatment,” said principal investigator Dr. MeiLan Han, a professor of medicine in the division of pulmonary and critical care at the University of Michigan, in Ann Arbor.
The findings were published in the Journal of the American Medical Association.
www.medresources.com 15464 Olive Blvd., Ste. 200 (across from Schnucks Hilltown Village) Chesterfield, MO 63017 636-306-1218 Med Resources is your one-stop for all of your respiratory and sleep needs • Clinical assessment in your home • Comprehensive CPAP set-up and re-supply program • Work directly with your physician and caregiver for personalized respiratory and sleep care
eat h
Eas
Br
e
i e r
Many Turn to Medical Marijuana to Ease Chronic Pain in Place of Opioids
People who use medical marijuana to treat their chronic pain tend to cut their use of opioids and other painkillers, but the trend may also have a downside, a new survey shows.
Folks treating chronic pain with cannabis reduced by more than 50%, on average, their use of prescription opioids, other prescription painkillers and even overthe-counter pain medications like aspirin, acetaminophen (Tylenol) or naproxen (Aleve), the researchers reported.
“Most people who use cannabis to manage their chronic pain have said that in doing so, it resulted in lower use of their prescription medicines and specifically prescription opioids,” said lead researcher Dr. Mark Bicket. He is an assistant professor of anesthesiology with the University of Michigan’s School of Public Health, in Ann Arbor.
Less use of prescription opioids would seem like a good thing, given the ongoing U.S. opioid crisis.
The number of U.S. drug overdose deaths has quintupled since 1999, and nearly three out of four overdose deaths in 2020 involved an opioid, according to the U.S. Centers for Disease Control and Prevention.
But some chronic pain patients who use medical marijuana may also tend to stop trying non-drug therapies proven to help, including physical therapy, meditation and cognitive behavioral therapy, the researchers found.
What’s more, people ditching their prescription drugs for marijuana are relying on a medication that still doesn’t have a lot of evidence behind it, Bicket added. The survey results “really underscore the need for research on the benefits and risks of using cannabis for chronic pain,” Bicket
said. “Cannabis is accessible as a treatment for chronic pain for most adults in the United States, but we don’t know how safe and effective cannabis is for chronic pain.”
For this study, Bicket and his colleagues surveyed more than 1,600 people suffering from chronic pain that wasn’t related to cancer.
Three out of 10 people said they had tried cannabis to treat their pain, and most of those patients reported that they wound up substituting weed in place of other painkillers.
The findings were published online Jan. 6 in JAMA Network Open.
Marijuana has a small effect on a person’s perception of pain, but its real benefit appears to come from easing the fear and anxiety that accompanies and exacerbates chronic pain, said Dr. Steven Cohen, director of the Blaustein Pain Treatment Center at Johns Hopkins Medicine, in Baltimore.
“It definitely doesn’t work better than other things, like anti-inflammatory drugs or opioids, at least acutely. But I think it works a lot on the affective component of pain,” Cohen said.
Unfortunately, cannabis also led some people to eschew pain management techniques that don’t rely on a pill or injection.
About 39% said their marijuana use had
led to decreased use of physical therapy, 19% said they meditated less and 26% said they didn’t use cognitive behavioral therapy to manage their pain as often.
“Typically the treatments that aren’t drugs, the non-pharmacological therapies, have been thought of to be first-line therapies, because their benefits typically far outweigh the risks,” Bicket said. “For many types of chronic pain, physical therapy is part of the first step. So things that would take the place of that, you would really want to seriously question if that were the right move or not.”
There aren’t any U.S. Food and Drug Administration-approved uses for medical marijuana in terms of chronic pain, Bicket noted.

Further, weed purchased from dispensaries can vary widely in terms of the levels of different chemicals like cannabidiol (CBD) and THC — the component that causes intoxication, Bicket and Cohen said.
“If I write a prescription for gabapentin or I write a prescription for oxycodone, I give a specific amount of medication, I tell people how to take it, and I monitor them,” Cohen said. “The issue with medical marijuana is that we’re not actually prescribing it. We’re certifying that people have a condition that might be amenable to treatment.”
Medical marijuana needs to be better regulated and understood if it’s to become a legitimate substitute for other pain therapies, the experts concluded.
“Right now with cannabis, it’s a big question mark whether the risks are larger than the benefits,” Bicket said. “We need additional information to give to patients about how it would work for them.”
More information
The U.S. Centers for Disease Control and Prevention has more about marijuana use for chronic pain.
52 H&C
ACHES & PAINS
Trust the national award-winning Joint Replacement Center at SSM Health DePaul Hospital.
St. Louis’ first program with advanced certification in knee and hip replacement.
If serious joint pain is limiting your activities, it’s time to consult the experts at SSM Health Orthopedics’ Joint Replacement Center. Our team utilizes the most advanced techniques, including minimally invasive options, to provide a personalized, compassionate approach to knee, hip, and shoulder replacement.

Plus, the Joint Replacement Center is the first program in St. Louis to be awarded advanced certification in knee and hip replacement and core certification in shoulder replacement by The Joint Commission.
Learn more at ssmhealth.com/JRC.
©2023 SSM Health. All rights reserved. ORT-STL-23-1703354 5/23
What Exercise Regimen Works Best to Ease Lower Back Pain?
Chronic lower back pain can make the most routine tasks difficult. But a recent study suggests patients can learn new, practical and less painful ways to move through individualized “motor skills training,” or MST.
MST vs. SFE
A two-year study of nearly 150 patients found that MST appears to better relieve disability from lower back pain than a more common but less-tailored exercise regimen broadly focused on improving strength and flexibility (SFE).
“Our findings suggest that motor skill training in functional activities is an effective and efficient treatment that results in important short-term and long-term improvement in function in people with chronic low back pain,” said study lead author Linda Van Dillen. She’s a professor of physical therapy at Washington University in St. Louis School of Medicine.
Lower back pain is incredibly common, and the No. 1 cause of disability, according to Van Dillen. It is the most frequent cause of chronic pain among American adults.
Van Dillen notes that at least 60% to 80% of adults will experience lower back pain, and “almost half of them will have had a major episode by age 30.”
Yet there is no accepted standard of care
for chronic lower back pain patients, nor a clear sense of what type of exercise intervention might work best, researchers said.
To get a better handle on the issue, Van Dillen’s team focused on a pool of patients diagnosed with what is known as “non-specific” lower back pain. That means they have tension, stiffness and/or soreness in the lower back area for which there is no clear cause.
The Study
Before the study began in, all participants had struggled with lower back pain for at least a year.
Participants, who ranged in age from 18 to 60, were randomly divided into two groups. One group received “strength and flexibility treatment for the trunk and lower limbs” – a common exercise intervention, according to Van Dillen. The other group took part in MST, which teaches patients new ways to carry out everyday tasks rendered difficult by back pain. MST aims to zero in on each patient’s personal posture and movements throughout an entire day, and then to tailor pain-free movement strategies to their specific routines.
Emphasis was on changing movements and alignments relevant to the person-specific activities to reduce lower back pain. The primary treatment principles were to teach the participant to (1) move the lum-
bar spine later and reduce the amount of lumbar spine movements related to their specific lower back pain classification, (2) increase use of other joints (eg, hips), and (3) avoid positioning of the lumbar spine in specific directions related to their specific lower back pain. Treatment was provided at a university-based outpatient physical therapy clinic.
Both groups received six weeks of training for one hour per week. Half of each group also received three “booster” treatment sessions six months later. Disability questionnaires were completed at the outset, and at six months and one year out. While both groups’ ability to perform daily functions without pain improved, the MST group achieved “significantly” better gains (meaning lower disability scores) over the study period.
MST patients were more satisfied with their care and less likely to use drugs for back pain. They were also less fearful of addressing work-related needs, and less likely to avoid normal daily activities, the study found.
Six months out, MST patients had fewer acute back pain flare-ups and were more likely to keep up with their exercises. And after a year, when their back pain flared up, it was less severe, researchers said.

Conclusions
People with chronic lower back pain who received person-specific motor skills training to change functional activity performance displayed greater short-term and long-term improvements in function than those who received more generalized strength and training exercises. Pain, physical function, and psychological outcomes also improved to a greater degree in the MST group compared with the SFE group.
These findings suggest that a priority of treatment for people with chronic lower back pain is to provide person-specific, challenging practice that promotes learning new strategies of movement and alignment during lower back pain-limited functional activities.
The findings were published online in JAMA Neurology.
More information
Learn more about lower back pain at the U.S. National Institute of Neurological Disorders and Stroke.
54 H&C
Natural Ways to Manage Arthritis Pain
There are more than 100 types of arthritis and related conditions, and they affect at least 54 million adults and 300,000 children in the United States, according to the Arthritis Foundation.
“We’ve really come a long way in the past decade in terms of helping our patients live relatively symptom-free lives,” Scripps Clinic rheumatologist Dr. Kavitta Allem explained in an interview for San Diego Health.
There are many medication and surgery options available to help manage arthritis pain and other symptoms. But there are also natural lifestyle changes and therapies that can be very effective.
The Arthritis Foundation states that eating a healthy diet, exercising regularly, applying heat and cold to your joints, and taking short 15-minute breaks to rest throughout the day can help improve your symptoms.
Research published recently in the Annals of Internal Medicine showed that even light exercise can help ease the pain of arthritic knees and give you wider range of motion.
Natural therapies for arthritis include massage, acupuncture, biofeedback and cognitive behavioral therapy. The foundation also recommends working with a physical therapist to improve your posture and range of motion.
American Physical Therapy Association (APTA) spokesperson Maura Iversen, who is also dean of the College of Health Professions at Sacred Heart University in
We Tailor a Fitness Program for You to Achieve Your Goals –Whatever Shape You’re In
I have been working with men and women of all ages for almost 20 years, and what I’m finding is that now there is more interest in improving overall health. Yes, losing weight is still a big motivator, but clients are more conscious of the need to reduce health risks - control blood pressure, prevent diabetes, reduce medications where possible, as well as address specific mechanical issues like knees, back or posture that may have prevented them from exercising.
Our personal training studio is focused on the indi -

vidual needs of our clients. Working collaboratively, we provide knowledge, support and accountability in a workable program that keeps them focused on achieving their goals. My education and training across the healthcare continuum enables me to consider not just exercise, but diet, rest and lifestyle for an overall balanced benefit program.
We offer a warm, friendly exercise studio with equipment to achieve resistance, cardio, flexibility/mobility and recovery fitness. We focus on results – both
Fairfield, Conn., pointed out that when physical therapists create an exercise plan, they consider the type of arthritis you’re diagnosed with, where in the body it manifests, its severity and whether you’re in remission or are experiencing a flare-up.
“All of that is taken into account, into the individual exercise programs that a physical therapist would prescribe,” she explained.
Iversen suggested several physical activity programs that are supported by APTA to help improve arthritis pain and other symptoms, including those offered through the Arthritis Foundation.
“The YMCA has a long, long history, at least in my 30-year career, of partnering with the Arthritis Foundation to offer aerobic programs for patients with arthritis,” she noted. “There’s also a walking program [and] we are fortunate nowadays with mobile phones where you can download a health app for arthritis.”
For more information on arthritis treatments, you can check out Arthritis Foundation’s Treatment Guides for additional therapies and surgeries to help improve your arthritis pain.
measurable and, importantly, how you feel. We meet clients where they are and help them get to where they want to be, with a do-able program that becomes self-motivating.
If you have been frustrated by past attempts to achieve your goals on your own, then I would recommend that you not waste another day. I have helped dozens of clients achieve their goals and I can help you, too. I will be happy to set up a no-obligation, no-pressure consultation to discuss your goals and what we offer.
bret@stronghumanfitness.com

FEATURED SERVICE Call or email me today 314-691-9040
www.stronghumanfitness.com
Bret Kliethermes
Emergency Room Vs. Urgent Care: Knowing Which Is Needed


If you’re sick or have been injured, you might wonder whether a hospital emergency department or urgent care clinic is the right place to be treated.
The American College of Emergency Physicians (ACEP) offers some general advice, to help take the “guesswork” out of deciding where to go when prompt medical attention is needed.
The Emergency Department
Go to the nearest emergency department if a medical emergency is suspected.
“The emergency department is the best option for concerning symptoms, severe illness or injury, and we’re open 24/7, 365,” said ACEP President Dr. Christopher Kang. “Emergency physicians are ready to help anyone who needs them — we are trained to treat every kind of medical emergency.”
“Knowing when and where to go in a health emergency can save a life,” Kang said. “If you need care for a severe illness or injury, or if you’re unsure about what’s wrong and your regular physician is not available, an emergency physician will always be there for you.”
Emergency departments have the advantages of having advanced medical
equipment and rapid access to hospitals’ operating rooms and intensive care units, if such care is needed. Emergency departments are staffed to handle more complex care for severe health issues, the ACEP said in a news release.
Some of the most common reasons to seek emergency care include trouble breathing, chest pain, uncontrolled bleeding, seizures, severe abdominal pain, head injuries, sudden severe headache or dizziness, and sudden weakness, confusion or disorientation.
Dr. Gary Gaddis is an experienced emergency department physician, served as Professor of Emergency Medicine at the Washington University School of Medicine, and is currently a Teaching Professor of Biomedical and Health Informatics at the University of Missouri-Kansas City School of Medicine. He points out, “Many people are unaware that emergency medicine has been an officially recognized medical specialty since 1979. All emergency physicians board-certified by the American Board of Emergency Medicine have completed an emergency medicine residency which has specifically trained them how to evaluate and manage a very broad range of mystery injuries or ailments.”
Dr. Gaddis adds, “Emergency departments are required by a law known as ’EMTALA’ to evaluate all patients who arrive for a medical evaluation, to determine whether an ’emergency medical condition’ exists in those persons, and then to treat or attempt to stabilize the condition of anyone who manifests evidence of a possible medical or surgical emergency, regardless of their ability to pay or their insurance status.
“This guarantee does not require emergency departments to provide medical care at no cost to the patient. Uninsured patients will eventually receive a bill for services rendered. However, the guarantee does assure that a patient’s medical well-being takes precedence over the financial issues that can be worked out later. For patients of limited financial means, hospitals and emergency physicians will often agree to a discounted payment plan, adjusted to a patient’s income level, as documented by recent year tax returns.”
Urgent Care
Urgent care is a vital part of the health care system, the ACEP president noted, and is a good option for minor medical issues, especially after-hours or on weekends when you can’t see your primary care doctor. However, most urgent care centers are not equipped to substitute for emergency care.
Urgent care tends to be the right choice for symptoms such as a modest cough, runny nose, sore throat, rashes, minor cuts, an upset stomach, pink eye and other seemingly mild symptoms, as well as for minor injuries such as suspected joint sprains and lacerations. Dr. Gaddis notes, “Some bony fractures can be handled by urgent care centers, but many cannot. It is difficult to expect most lay people to know
56 H&C
at the time of an injury whether fracture care beyond simple splinting will be necessary, so it is difficult to give airtight advice regarding how to address such an injury.”
Urgent care centers often require proof of health insurance or the presentation of a charge card before initiating an evaluation of a patient. Importantly, urgent care centers often decline to accept Medicaid as a form of payment, because Medicaid, a federally funded and state-operated form of payment for health care goods and services, technically is not a form of health insurance.
The understandable belief that Medicaid is health insurance is pervasive among those covered by the Medicaid program. However, Medicaid is a federal entitlement program that reimburses physicians and hospitals at rates markedly lower than is paid by Medicare or health insurers. In any case, urgent care centers require payment when services are delivered, and many can accurately estimate a patient’s insurance “deductible”, and thus expect payment for the patient’s share of expenses as part of the discharge process.
When to call 911
In an emergency that requires on the spot attention, dial 911 from your phone immediately. This includes any situation that requires immediate assistance from an ambulance and/or paramedics.
When you call 911, be prepared to answer the call-taker’s questions, which may include:
n The location of the emergency, including the street address. (Some patients may know that many municipalities adopted “Enhanced 911” (E911) in earlier decades, but this form of 911 activation requires the presence of a land line phone to function effectively. “E911” cannot be expected to accurately accommodate for the location of a caller using a mobile phone.)
n The phone number you are calling from
n The nature of the emergency
n Details about the emergency, such as a physical description of injuries or symptoms being experienced by a person having a medical emergency.

Remember, the call-taker’s questions are important to enable dispatch of the right kind of help to you quickly. Be prepared to follow any instructions the call-taker
gives you. Many 911 centers can tell you exactly what to do until help arrives, such as providing step-by-step instructions to aid someone who is choking or needs first aid or CPR. Do not hang up until the call-taker instructs you to do so.
What This Means for You
Consider the severity of symptoms when deciding whether to visit urgent care or the emergency room and when to call 911. Dr. Gaddis adds, “When in doubt, err on the side of caution and access care in an emergency department. Symptoms such as severe bleeding, trouble breathing, chest pain and seizures require emergency care, but so do many other symptoms. It is difficult for most lay persons to predict how serious their condition is with 100% accuracy. Heavens, even doctors or nurses can’t do that! It is only after they deploy their knowledge and training, obtain a patient history, perform a physical examination, and order lab tests and/or X-rays that such a determination can be accurately reached.”
SOURCES: American College of Emergency Physicians and 911.gov
Our specialty is you.
At St. Luke’s, we offer a full range of orthopedic solutions for joint, bone and muscle pain. Whether you’re dealing with an injury or a chronic condition like arthritis or osteoporosis, our renowned doctors and specialists will design an approach specific to your exact needs — providing you with relief from pain, and a quick return to your daily life and all the things you love. Schedule your appointment at StLukesCare.com/Orthopedics
Compassionate care
Strong relationships that help you navigate every step of your health and wellness journey.
Nationally recognized
Consistently honored as America’s best for excellence in patient care and more.
Best technology
The innovation and tools to ensure you get the best results for your health.
Easy access
Convenient locations plus same-day appointments at some offices.
Our specialty is comprehensive joint care.
For Adults with ADHD: Let’s Make Now Better So Later Is Easier
By Tom Scott, M.S. L.P.C.
Have you ever wondered what happens to the millions of children who’ve been diagnosed with ADHD? Well, they grow up to be the millions of adults with ADHD. But being diagnosed as an adult can feel different. It can be disconcerting, or perhaps a relief because the diagnosis explains a lot of frustrations adult ADHDers continually encounter.
Understanding the diagnosis
However, diagnosing ADHD in adulthood can be difficult because certain ADHD symptoms are comparable to those caused by other conditions, such as anxiety or mood disorders. And many adult ADHDers, whether diagnosed in childhood or adulthood, have at least one other mental health frustration like depression or anxiety. But who hasn’t been depressed, or experienced anxiety in some form or another? With adult ADHDers depression can come and go, but anxiety and apprehension seem to lurk in their minds’ stairwells.

Anxiety is permeated with “what if” questions, stoking worry and ruin about their future. Unfortunately, we believe that if we worry enough things won’t get worse. But note: We are the only species who bring the future into the present. My cat isn’t thinking about next Tuesday.
Getting our minds on our side
We can’t believe everything our minds tell us because the mind is capable of automatically turning on us. We’re all influenced by our past, subconsciously reliving it, and acting it out. Present-day difficulties snag memories stored in our subterranean implicit memory system.
Traumatic memories get seared into our brain then embodied cellularly. These memories unknowingly activate our physiology, directly affecting our ability to cope in any particular moment. Corrosive tones of disapproval, or a displeasured glance, can flood the mind and body with angst and trepidation. But the adult ADHDer does not consciously connect the present feelings to the past.
Rather than pause and reflect, they react.
ADHD adults build their defenses around their weaknesses, not their strengths. Such defensive postures make it difficult to express themselves in ways where they “feel felt.”
A painful hyperconsciousness of injustice, futility, rage, or shamed silence make adult ADHDers feel forever the victim, while their partner may feel forever victimized. With my patients I find it very productive to help them discover these ingrained responses so they can begin to dislodge them.
Hope management
Good news abounds. Even as adults we can learn to develop, renovate, and install new beliefs and generate new behaviors. For most ADHDers, young or old, it’s very painful knowing you’ve “been a disappointment” to yourself or others. The adult ADHDers I see in my office are not there because they’re running in the hallways, spinning in their chairs, or creating uproarious sounds with hand-toarm pit. They’re seeking help because of relationship and career issues, along with a distorted sense of self. Distractibility, impulsivity, and bumbling emotional moments provoke an already overactive central nervous system. But here’s more good news: self-regulation can be learned. What a relief that is for everyone involved. But to notice it takes self-awareness to “still” one’s mind and body. ADHD adults are forever rushing around, often tardy, and disorganized, torpedoing healthy relationships, and fomenting poor job performance. These aren’t just fleeting states that have been acquired after the diagnosis, but rather ancient, calcified traits, that with the right help can be therapeutically resolved.
As adults, we can outgrow many of these early challenges by first acknowledging them, then celebrating the numerous pluses adult ADHDers possess: drive, resilience, generosity, empathy, spontaneity, great sense of humor (up for debate), romantic, tenacious, and creative. But these attributes can be systematically whittled away when one’s not loved for the very person they are. Being shamed into
58 H&C
MENTAL HEALTH
compliance, repressing our true selves, being over-medicated, which can suppress our instinctual data and unique proclivities, does not produce cheerful, insightful adults.
When looking for help
Never go to a therapist who never goes to a therapist is something I believe. I can’t take people places I’ve never been. My therapist helped me learn from my mistakes. He wouldn’t just let me accept my dog Tucker’s approval as irrefutable evidence of my wonderfulness. He helped me understand that it’s better to change before you have to. This I learned, but often after the third or fourth lesson. What can
I say?
If there is no struggle there is no progress. What consumes your mind, controls your life. My therapist helped me imagine things actually getting better. When looking for help, ADHDers possess great sensory acuity, sensing whether or not their therapist is safe, sincere, and competent. A therapist must be willing to understand the ADHDer by meeting them on their
map of development. As a therapist, I would never expect patients to contort themselves to be as I need them to be. The therapist should never be wedded to one approach. The truth of who we are is found at the intersection of many diverse beliefs. Avoid “paragons of virtue” who are appalled by your perceptions, proclivities and indiscretions. I always accept the wild with the mild. Don’t tolerate a know-it-all. I recommend that medication be the last option. The best way to cushion apprehension and self-doubt is to help the individual feel better about themself. Moment-to-moment
gentle inner corrections
Since “right now” is truly all we have, learning to be aware of our awareness, and doing moment-to-moment gentle inner corrections will make now better, so later is easier.
We can learn to nurture a committed curiosity, noticing our habitual thoughts, reactions, and behaviors that don’t serve us or others well. If it’s not rewarding, then why perpetuate it? When we view
TMS: An FDA-Approved, Non-Drug Therapy for Chronic, Treatment-Resistant Depression


For Veterans and Civilians struggling with depression, anxiety, and PTSD, research has identified a specific region of the brain that is involved in depression and mood control called the dorso-lateral prefrontal cortex (DLPFC), which is located near the temple. Patients who suffer from depression show decreased blood flow in this region, as shown in fMRI and PET scans. Transcranial Magnetic Stimulation (TMS) is an FDA-Approved, non-invasive treatment that is an alternative or augmentation for antidepressant medications and psychotherapy, when those have not been effective. TMS also has open-label applications for treating anxiety and PTSD.
In TMS treatment, the patient is awake and seated in a comfortable chair. A module is placed near the
patient’s temple to painlessly deliver a magnetic field that stimulates specific regions of the brain to increase neuronal activity that can alleviate depression. Leading neurology and psychiatric hospitals in the US, including the Mayo Clinic, Massachusetts General Hospital, Stanford, and Johns Hopkins incorporate TMS in their treatment of depression.
Precision TMS is a clinic in Creve Coeur founded by a former DOD traumatic brain injury (TBI) and PTSD researcher who integrates TMS with traditional psychiatric treatment. Our state-of-the-art facilities and dedicated staff are recognized as the leading TMS clinic in the St. Louis area with the best outcomes.

TMS is FDA approved and covered by most health insurance and VA benefit plans.
our curiosity as a superpower, we then begin to see what’s really transpiring inside. It’s not always about breaking bad habits, but rather learning to develop new ones.
We all can learn to take better care of our inner world by grounding our emotions, continually resuscitating our spirits, focusing on positive behaviors, and keeping our minds flexible and accepting. I daily embrace a mantra that keeps this adult ADHDer going, and that is, “Much good still lies ahead.”
TOM SCOTT, M.S. L.P.C., a licensed psychotherapist and educational consultant for 35 years, has presented on ADHD, addiction, anxiety, depression, trauma and parenting nationally and internationally. His new book, When Living & Learning Hurt: Making Now Better So Later Is Easier, is an authentic, informative, and hopeful read from the author, who is ADHD himself.

FEATURED SERVICE
by Research. Driven by Results. Call or email us today to find out more. 314-673-2670 info@precisiontms.org
Dr. Vadim Baram, MD Distinguished Fellow, American Psychiatric Association Thomas Malone, MBA CEO | Former DOD Traumatic Brain Injury and PTSD Researcher | Certified TMS
Powered
Could Bacteria in Your Gut Help Spur Depression?
Depression may be a disorder of the brain, but new research adds to evidence that it also involves the gut. While depression is complex, recent research has been pointing to a role for bacteria that dwell in the gut – suggesting that certain bacterial strains might feed depression symptoms, while others might be protective.
In a pair of new studies, researchers identified 13 groups of bacteria that were related to the odds of adults having depression symptoms. In some cases, the gut bacteria were depleted in people with depression, while in others they were present at relatively high levels. However, experts stressed that the findings do not prove that any of the gut bugs cause or protect against depression. So, it’s far too soon to recommend probiotics as a depression treatment.
In fact, gut bacteria seem to change in their diversity and abundance when any chronic disease is present, said Dr. Emeran Mayer, director of the Oppenheimer Center for Neurobiology of Stress at the University of California, Los Angeles David Geffen School of Medicine.
Mayer, who was not involved in the research, is also the author of the book The Mind-Gut Connection. He said the findings may reflect a “general disease effect,” rather than gut bacteria patterns that are specific to depression.
The research, published in the journal Nature Communications, is the latest to dig into the question of whether the gut microbiome is somehow involved in depression.
The gut microbiome refers to the trillions of bacteria and other microorganisms that live in the digestive system. Those
microbes are believed to do much more than aid in digestion, however. Studies show they are involved in everything from immune system defenses to producing vitamins, anti-inflammatory compounds and even chemicals that influence the brain.
Some research has linked certain gut bacteria to higher or lower odds of depression. The new findings confirm that those microbes are tied to depression – and identify some new ones, said study co-author Najaf Amin.
And whether gut bacteria actually help cause depression or not, it’s still important to know whether they correlate with the disorder, according to the researchers. That could help in diagnosis, they say.
“What we are looking for is to identify the bacteria that associate with major depression,” Amin said. “This will help us in identifying a biomarker for depression that can be used as an objective measurement in identifying cases – which is lacking at the moment for depression.”
The findings come from two studies. One involved nearly 2,600 Dutch adults who were screened for depression and gave stool samples to be analyzed for their bacterial makeup. The other included just over 3,000 Dutch adults living in the same urban area; many were of Ghanaian, Moroccan, Surinamese or Turkish descent. In all, the researchers found 13 bacterial groups that correlated with participants’ depression scores. In most cases, the gut microbes were decreased in people with depression. But some bacterial groups, like Sellimonas and Eggerthella, were present in greater abundance when people were depressed.
If future research proves that any bacterial imbalances actually help cause depression, that could form the basis for new treatments, Amin said – such as probiotics or prebiotics.
Beyond that, the study included people of diverse ethnic backgrounds. And it appeared the microbiome-depression links were consistent across those groups, said Amin, of Oxford University in England. She, too, said the findings do not prove cause and effect.
Depression can, for instance, cause people to eat poorly – and diet is a primary factor in the makeup of a person’s gut bacteria. So, that could be one explanation for the results, Amin said.
At the same time, the notion that gut bacteria could affect depression risk is not far-fetched. According to Amin’s team, some bacteria in the groups they identified help synthesize certain chemicals that affect the brain – such as butyrate, glutamate and serotonin.
Mayer, however, doubted the findings are “clinically relevant.” For one, he said, the study implicates large groups of gut bacteria, each of which contain multiple strains – which in many cases have opposite functions.
He also said that “microbiome science” is moving away from focusing on the relative abundance of different gut bacteria, and toward more nuanced measures of how the gut microbiome is functioning.
More information
The Harvard School of Public Health has more on the gut microbiome.

60 H&C
Americans More Comfortable Discussing Mental Health with Primary Care Doctors

Primary care doctors are no longer just in the physical health business: Americans are increasingly turning to them for mental health care, too, a new study finds.
Looking at Americans’ primary care visits between 2006 and 2018, researchers found a 50% increase in the proportion of visits that addressed mental health concerns. That figure rose from just under 11% of visits, to 16% by the end of the study period.
One reason is that mental health conditions are becoming more common: During the same period, other studies show, the national rate of mental health disorders rose by about 18%. In addition, it seems primary care doctors are shouldering more responsibility for diagnosing and in some cases treating, mental health conditions.
“I think this study really underscores the importance of primary care in our country,” said lead researcher Dr. Lisa Rotenstein, medical director of population health at Brigham and Women’s Hospital in Boston. That also means primary care doctors need the resources to make sure patients diagnosed with mental health conditions get the best treatment, she said.
The findings – published in the journal Health Affairs – are based on an ongoing government survey that collects information on Americans’ office-based medical care. Rotenstein’s team analyzed records from nearly 110,000 primary care visits, representing roughly 3.9 million appointments nationwide. A visit was considered to have “addressed a mental health concern” if the record listed that as the reason for the appointment, or the doctor diagnosed a mental health condition at that time.
Overall, the proportion of visits falling into that category rose by nearly 50% between 2006 and 2018. The study cannot pinpoint the reasons – whether it’s doctors doing more mental health screenings, or patients more often bringing up mental health symptoms, for example. But it’s probably a combination of those and other factors, Rotenstein said.
Dr. Robert Trestman, chair of the American Psychiatric Association’s Council on Healthcare Systems and Financing, agreed. He noted that the Affordable Care Act – better known as “Obamacare” – was passed during the study period, which reduced the ranks of the uninsured nationwide.
At the same time, the stigma around mental health loosened. “People are more
comfortable talking about mental health and addiction,” said Trestman, who was not involved in the study. “It’s a very big deal that the stigma is being reduced.”
But, both experts said, systems need to be in place to support primary care doctors in addressing mental health – and getting patients the treatment they need. That includes adequate insurance reimbursement. It also means primary care providers need to be able to refer patients to a mental health specialist when necessary, to make sure they get the best care.
Routine depression screening, for example, is recommended for adults and teenagers. “But we need the capacity to treat them,” Trestman said, “and right now we don’t have it.” He said it’s important for primary care doctors to “proactively build relationships” with mental health professionals in their community, to make it easier to refer patients when needed. But, Trestman and Rotenstein both said, that’s also a big challenge in the many areas of the country with a dearth of mental health care providers. “Telehealth” services that connect patients and providers over distances can help to an extent, Trestman said. But that does not address the shortage of mental health specialists. And then there are the racial and ethnic disparities. Rotenstein’s team found that, in comparison to their white counterparts, Black and Hispanic Americans were 40% less likely to have a mental health concern addressed during a primary care visit. Rotenstein said future studies need to dig into the reasons – including whether doctors are less likely to screen patients of color, or whether differences in insurance coverage are a barrier.
As for the message for patients, Rotenstein pointed to another study finding: Mental health concerns were more likely to be addressed when patients visited their established primary care doctor – someone who knows them, in other words. At a time when many Americans are using walk-in clinics for as-needed health care, that’s important, according to Rotenstein. It points to one of the benefits of having a regular provider you know, she said.
More information
The National Alliance on Mental Illness has an overview of common mental health conditions.
61 H&C
Acts of Kindness Could Be Natural Antidepressants
People suffering from depression or anxiety may be able to help themselves by helping others – even in small ways, researchers report.
In a recent study of 122 people with depression or anxiety symptoms, those who started fitting small acts of kindness into their day showed an improvement in their symptoms.
And when it came to boosting feelings of social connectedness, those kind gestures worked even better than two techniques used in standard “talk therapy,” the study found.
Focusing on others helps
Experts said the findings point to the power of simply being kind – possibly be-
cause it helps people with mental health symptoms get out of their own heads, even temporarily.
“When you have these symptoms, you can become preoccupied with your own suffering – understandably,” said David Cregg, one of the researchers on the study. So intentionally focusing on others’ well-being, and choosing to support them in some small way, can free people from that mindset for a while, according to Cregg.
He conducted the study as part of his PhD dissertation at Ohio State University, and is now a clinical psychologist with the South Texas Veterans Health Care System.
How to Relieve a HUGE Stress Point for You and Your Family
We all live with so much stress these days. One very important way you can reduce stress is by putting a plan in place to help prepare yourself and your family for any unexpected life crisis. Planning is especially important for the elderly and families with members who have special needs.

Our boutique law firm focuses on estate planning and elder law. We take pride in giving personal care for our clients, so that you can complete your legal steps to protect you and your family. Estate planning is not just filling out forms. We give clients an interactive process, working on what is most important to you. You


receive a tailored comprehensive package for wills and trusts that include a financial power of attorney, medical power of attorney, living will, and other options such as special or supplemental needs trusts addressing specific needs you may have. You are offered an Estate Client and Maintenance Plan (ECAMP).

At your direction, we can set up a team approach to work with family members, financial advisor and/or accountant on steps they need to take to put your comprehensive plan in place. Our entire personal care approach is designed to give you confidence and to keep you from becoming overwhelmed by a lot of details.
Past research has shown that acts of kindness – writing a supportive note to a friend or buying someone a cup of coffee – can not only make the recipient feel good, but also be a boon to the givers’ well-being. But few studies have focused on people with depression or anxiety, Cregg said.
The study
For the latest study, he and Ohio State colleague Jennifer Cheavens, a professor of psychology, recruited 122 adults who had elevated scores on a standard measure of depression and anxiety. They then
62 H&C
FEATURED SERVICE Call us, visit our website or follow the QR code to book your appointment. 400 Chesterfield Parkway, Ste. 400 Chesterfield, MO 63017 Sheri Tucker, Esq.. 314-332-0011 TuckerLegal-llc.com
randomly assigned each participant to one of three groups.
One group was told to plan social activities for two days out of each week, and a second was instructed to complete “thought records” at the same frequency – with the goal of helping them identify their negative thought patterns and try to redirect them. Both techniques are used in cognitive behavioral therapy (CBT), a standard “talk therapy” for depression and anxiety.
People in the third group were told to perform acts of kindness, three times per day on two days out of each week. The specifics, Cregg said, were left up to the participants. Based on what they later reported, many reached out to people in their lives in small ways – offering a ride, baking cookies for them or writing a thoughtful note.
After five weeks, the study found, all three groups were showing an improvement in their mental health symptoms, on average. The impact also had some staying power, based on evaluations done at week 10 (five weeks after the interventions ended).
But the kindness group was the only one with substantial gains in “social connectedness” – which gets at a person’s feeling of belonging. “There really does seem to be something special about acts of kindness,” Cregg said.

The study also turned up hints of what that is: People in the kindness group showed a change in a standard scale measuring “self-absorption” – or a habitual preoccupation with one’s own thoughts and feelings.
The finding makes sense, according to James Maddux, a senior scholar with the Center for the Advancement of Well-Being at George Mason University.
Breaking the cycle of rumination
“In the moments they’re interacting with other people, they’ve stepped outside of their own heads,” said Maddux, who was not involved in the research. “That could help them break the cycle of rumination.”
And while social activities also involve being with other people, Maddux said the intention behind acts of kindness is different: When people are socializing,
they are typically focused on enjoying themselves. Kindness shifts the focus to someone else’s feelings. Maddux said the message from the study is simple: “Be nice to people. It feels better to be nice to people.”
Of course, both he and Cregg said, that can be tough for people who are dealing with depression or anxiety. In the study, researchers simply told people to perform acts of kindness, and were careful not to suggest the goal was to make the participants feel better.
So, both experts said, be kind for the sake of others, and there may be bonus benefits for your own well-being.
The findings were recently published online in The Journal of Positive Psychology.
More information
The Mayo Clinic has more on the art of kindness.

We Accept Insurance • elliementalhealth.com Our Services Include: • Individual Therapy • Couples Counseling • Family Therapy • In-Person and Virtual Sessions • Medication management at select locations NOW OPE N IN ST. CHARLES AND ST. LOUIS COUNTIES
Everything You Ever Wanted to Ask about Hot Flashes
What are hot flashes?
Ahot flash (also known as a hot flush) is a sudden feeling of heat, usually on your face, neck, shoulders, and chest. You may begin sweating profusely, and your heart might start pounding. These symptoms can last for only a few seconds or minutes, or they can go on for as long as half an hour. The overheated sensation is sometimes
pause. In fact, hot flashes are the most common sign that menopause is on the way. About 75 percent of women have them, often beginning two or three years before they stop menstruating and, in some cases, even earlier. Some women are bothered for only a few months, but more commonly, hot flashes continue for three to five years.
Can medications help?
If your hot flashes are frequent and interfere with sleep or daily life, your doctor may suggest hormone replacement therapy to supplement your declining estrogen. Because some evidence links hormone replacement therapy used for as little as five years or less with increased risk of strokes, blood clots, heart disease, and invasive breast cancer, you’ll want to review your medical history thoroughly with your doctor to decide whether HRT is a good option for you.
What about alternative treatments?
followed by a slight chill, and hot flashes that occur during the night are called night sweats.

For some women, hot flashes are little more than a nuisance, an occasional passing sensation of warmth. Others experience intense waves of heat that come on out of the blue, leaving them drenched in sweat several times a day and disturbing their sleep at night.
What causes them?
Researchers don’t know exactly what causes hot flashes, but they’re thought to be linked to a decrease in the body’s production of estrogen – something that usually happens as you approach meno-
You can also get hot flashes after giving birth (when your estrogen levels fall back to normal), after having your ovaries removed (since that’s where your estrogen comes from), or during a time when you’re on medications such as GnRH inhibitors or tamoxifen (because they’re designed to reduce your estrogen levels). Finally, you may experience similar symptoms if your levels of thyroid hormone are out of whack.
What can I do?
Try to keep cool, both physically and emotionally. Dress in loose layers so you can quickly peel off some clothing if a hot flash should hit. Choose absorbent cotton clothes when you can; synthetic fabrics trap heat. Keep your home cool, a fan handy, and an ice-cold drink by your side. And cut down on stress; meditation, yoga, or massage can help. Avoid spicy foods and hot drinks if you find that they bring on hot flashes. It’s also a good idea to cut back on caffeine, alcohol, and smoking and to get plenty of aerobic exercise, such as walking or swimming.
Some women find that taking a vitamin E supplement brings relief (try 400 international units daily) but talk to your doctor first if you’re on any blood-thinning medication. Others have discovered that acupuncture helps them keep their cool. Most so-called natural remedies come from plants and herbs containing phytoestrogens, compounds that are chemically similar to human estrogens.
Take soybeans, for example: It’s long been known that Japanese women, who eat large quantities of soy foods, have fewer hot flashes than women in the West, though studies of the effect of soy on hot flashes have had mixed results. Since soy can benefit your body in other ways –some studies show it may help keep your heart healthy, for instance – adding soybean-based foods like tofu, tempeh, miso, soy milk, and roasted soy nuts to your diet is still a good idea.
Then there’s black cohosh root, which has been approved for the treatment of hot flashes by Germany’s Ministry of Health. In one study, 80 women who’d been averaging about five episodes per day were down to one a day after taking the herb for three months.
Dong quai is often promoted as a remedy for hot flashes and other menopausal symptoms, but a recent study found that it’s no more effective than a dummy pill. (Chinese herbalists recommend that it be taken in combination with other herbs, as prescribed by a qualified practitioner.)
64 H&C WOMEN’S HEALTH
Women Need to Move More to Help Keep Mental Decline at Bay
Alot of people wear watches that count their every step as they try to move more. Now, a new study finds that getting more of those steps each day, along with moderate-to-vigorous physical exercise, could cut the risk of dementia and thinking impairments for women.
Dementia affects more than 5 million people in the United States, according to the U.S. Department of Health and Human Services, and that number could double by 2050. Women have a higher risk than men of developing memory and thinking issues, the study authors noted.
Benefits of more activity
For women aged 65 or older, each additional 31 minutes per day of moderate-to-vigorous physical activity was associated with a 21% lower risk of developing mild cognitive (thinking) impairment or dementia, according to the study led by researchers at the University of California, San Diego (UCSD). The risk was 33% lower with each additional 1,865 daily steps.
“Given that the onset of dementia begins 20 years or more before symptoms show, early intervention for delaying or preventing cognitive decline and dementia among older adults is essential,” said senior study author Andrea LaCroix, a professor at UCSD’s Herbert Wertheim School of Public Health and Human Longevity Science.
The study
Much of past research on movement and sitting in relation to mild cognitive impairment and dementia has used self-reported measures rather than devices, noted first study author Steve Nguyen, a postdoctoral scholar at the School of Public Health. For this study, the researchers included data from 1,277 women who were in Women’s Health Initiative ancillary studies that looked at memory, physical activity and heart health. Study participants wore research-grade accelerometers (a device that measures motion). They were asked to go about their daily activities for up to seven days.
The women averaged 3,216 steps and 276 minutes in light physical activities, such as housework, gardening and walking, each day. They also averaged 45.5 minutes of moderate-to-vigorous physical activity, such as brisk walking, and 10.5 hours of sitting per day.
The findings were published online in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
Conclusion
“Older adults can be encouraged to increase movement of at least moderate intensity and take more steps each day for a lower risk of mild cognitive impairment and dementia,” Nguyen said in a university news release.
Know your breast cancer risk. Create a plan.
St. Luke’s High-Risk Breast Services
Knowing your personal breast cancer risk can help you take steps to reduce your chances of developing it or catch it early, when it is most treatable.
St. Luke’s Women’s Center offers a comprehensive high-risk program to help you learn your risk and work with our specialists to develop a personalized plan and seamlessly coordinate your care. It begins with a breast risk assessment at your annual mammogram.

Learn more about St. Luke’s High-Risk Breast Services at stlukes-stl.com/BreastHealth, or call 636-530-5512.

9-0096
MRI Might Boost Cancer Detection for Women with Dense Breasts
Nearly half of women have dense breast tissue, which can be a double whammy on their odds for breast cancer. Not only are dense breasts a risk factor for cancer, but this glandular and fibrous connective tissue make it harder to detect cancers on a mammogram, the usual method for breast cancer screening.
and should be performed,” Freitas said. “This is my first message to [patients who have dense breasts].”
Even though the studies found MRI superior in terms of cancer detection, Freitas urged patients to discuss the pros and cons of each method with their health care providers.
Among the concerns about breast MRI is its availability and its price. “The costs are actually the biggest barrier for our widespread implementation of MRI,” Freitas said.
Screening mammograms are highly effective for women with fatty breasts, detecting about 98% of cancers. For those with dense breasts, they can give false reassurance, however. Both dense tissue and breast cancer show up as white on the image, making it harder to detect cancer in dense breasts, Freitas said.
Breast cancer risk
tomosynthesis. More than 132,000 of the women had dense breasts and a negative mammogram. Researchers found 541 undetected cancers in that group. Breast MRI detected even tiny cancers.
Still, more research is needed, researchers said. It’s important to investigate the cost effectiveness of breast MRI and any impact each method may have on death rates.
Susan Brown, a managing director at the Susan G. Komen breast cancer organization in Dallas, reviewed the findings. She noted that MRI technology is much more sensitive but also not very specific, which can lead to false positives. Brown said she would like to see the additional research that the authors also said was needed on the impact of other screening methods on cancer survival. Komen’s policy focus has been on removing barriers to breast imaging, she said.
Cost is a factor
Although the Affordable Care Act enabled widespread access to free screening mammograms, patients who need additional screening because of an inconclusive or abnormal mammogram may still incur high out-of-pocket costs.
Alternative imaging options
New research looked at other kinds of imaging to see which might be more effective for the 47% of women who have dense breasts with low levels of fatty tissue. One emerged as an effective alternative: Breast MRI was superior to other methods, using that detection criteria.
Researchers also looked at hand-held breast ultrasound, automated breast ultrasound and digital breast tomosynthesis. All showed about the same level of effectiveness, said study co-author Dr. Vivianne Freitas, an assistant professor at the University of Toronto and a staff radiologist at the Joint Department of Medical Imaging, also in Toronto. “I would say supplementary image modalities in those with dense breasts and negative mammogram are recommended
On average, women have a lifetime risk of 12% to 13% for developing breast cancer. A history of treated breast cancer or previous breast biopsies with high-risk lesions boosts that to an intermediate risk. High-risk patients, with a lifetime risk of 20% or higher, were not included in this study because MRI benefits for them have already been established.
The study
To investigate the effectiveness of screening methods, the researchers did a meta-analysis of 22 studies that included more than 261,000 patients who had been screened for breast cancer.
The studies included 10 that covered hand-held breast ultrasound; four on automated breast ultrasound; three on breast MRI; and eight on digital breast
“Our position is that mammography is one step, the initial step, in early detection and is alone not able to diagnose breast cancer in every woman, and women with breast density is an example,” Brown said. People who face high costs for diagnostic and supplemental imaging are less likely to have those tests, she said, citing past research. “As a result, if they have breast cancer, that delay in diagnosis can be associated with a much poorer outcome,” Brown said.
Nine U.S. states have eliminated cost sharing for these follow-up tests, Brown said. Several others have introduced legislation this year to address this issue. Federal legislation may also be reintroduced later this year.
“To have that screening test but then not to be able to follow up if there’s an abnormality can have really very negative consequences, of course, to those individuals that do have cancer,” Brown said. The findings were published in the journal Radiology.
More information
The U.S. National Cancer Institute has more about dense breasts.

66 H&C
Good Sleep Could Keep Illness at Bay as You Age
As men and women enter their golden years, those who regularly fail to get a good night’s sleep face a higher risk for developing not one but two serious chronic illnesses at the same time, new research shows.
Researchers from France, Finland and United Kingdom tracked the self-reported sleep routines and health status of nearly 8,000 Britons from ages 50 to 70.
While the new analysis can’t prove cause and effect, “the breadth of observational and interventional studies are strongly suggestive of inadequate sleep compromising good health,” concluded Dr. Virend Somers, who reviewed the findings. He’s a professor of cardiovascular medicine at the Mayo Clinic College of Medicine in Rochester, Minn.
For the study, researchers first looked at how much sleep study participants were getting back in 1985, when they were 50 years old and disease-free.
At the time about 4 in 10 reported regularly getting fewer than seven hours sleep
a night, with nearly a third getting five hours or less.
For most people, seven hours is the minimum needed for a healthy night of sleep, said lead author Séverine Sabia, a research associate with the National Institute of Health and Medical Research (Inserm) at the University of Paris. Her team then looked at which participants were routinely sleeping no more than five hours a night as they entered their 60s and 70s.
And at each milestone, regularly sleeping those fewer hours was linked to a 30% to 40% higher risk of developing multiple illnesses, compared to regularly clocking seven hours a night.
Included among the list of possible illnesses were diabetes, cancer, coronary heart disease, stroke, heart failure, chronic obstructive pulmonary disease, chronic kidney disease, liver disease, depression, dementia and a variety of other mental disorders, Parkinson’s disease, and arthritis/rheumatoid arthritis.
Notably, those who slept five hours or fewer at age 50 faced a 30% higher risk – compared with good sleepers – for simultaneously developing two of those illnesses. At age 60, poor sleepers saw their relative risk rise by 32%. By 70, the increased risk hit 40%.
Those who failed to get enough shut-eye at age 50 also faced a 25% spike in their risk of early death, largely because of an increased risk for getting sick, researchers found.
Sabia acknowledged that it’s possible that poor sleep could be a function of disease, rather than the cause. But she expressed confidence that her team “used a comprehensive approach to reduce the risk that the findings reflect the impact of the disease on sleep duration.”
Adam Krause, doctoral candidate in cognitive neuroscience at the Center for Human Sleep Science at the University of California, Berkeley, said the study makes sense.
“These findings are not too surprising, in showing that short sleep can predict higher incidence of chronic disease later in life,” Krause said. “Sleep processes touch every system of the body, so a lack of sleep, especially when experienced long-term, will impact multiple systems whose chronic dysregulation can lead to the development of these common chronic diseases.”
As for limiting one’s risk of disease, Sabia emphasized the importance of trying to maintain “good sleep hygiene.”
That, she said, generally “includes a comfortable bedroom, being physically active and exposed to light during the day, having a sleep routine, avoid screen time and reduce light in the 30 minutes before sleep.”
Somers offered one more important tip. “If there is any likelihood of a sleep disorder – such as disruptive snoring, sleep apnea or insomnia – it would be helpful to be evaluated and treated by a sleep physician,” he said.

The findings were published in the journal PLOS Medicine.
More information
Learn more about good sleep at the American Academy of Sleep Medicine.
67 H&C
AGING & CAREGIVING
Drug and Alcohol Fatalities Among U.S. Seniors Have Tripled Since 2000
Growing numbers of older Americans are dying from drug overdoses and alcohol abuse. That’s the tragic takeaway from two new reports by the U.S. Centers for Disease Control and Prevention.
More than 5,000 people aged 65 and older in the United States died of a drug overdose in 2020, and this number has tripled since 2000, according to one of the reports.
The other report revealed that more than 11,600 U.S. seniors died from alcohol-induced causes in 2020. Alcohol-induced death rates in this age group have been on the rise since 2011 and jumped more than 18% from 2019 to 2020.

The new research wasn’t designed to look at why more older Americans are dying from drug overdoses or alcohol abuse, but the findings mirror what has been seen in younger age groups.
Abuse of fentanyl and other synthetic opioids has had a big impact on the older population as well as younger folks, said study author Ellen Kramarow. She is a demographer at the CDC’s National Center for Health Statistics, which published the data last November in an NCHS Data Brief. Death rates from these drugs increased by 53% from 2019 to 2020 among people aged 65 and older, Kramarow said.
The increase in deaths from drug overdoses and alcohol use has been rising faster in men, she added.
The study also highlighted a racial gap in deaths from drug overdoses among older adults. Drug overdose death rates among 65-year-olds are highest among Black people with one exception: white women aged 75 and older have the highest death rates from drug overdose.
The risk of dying from alcohol-induced causes among people aged 65 and older
was highest among American Indian and Alaskan Native people, the investigators found.
Experts who reviewed the new study were distressed but not surprised by the statistics. The findings sadly reflect what Anne Fernandez is seeing in her practice. She is an associate professor in Michigan Medicine’s department of psychiatry, in Ann Arbor.
“I am struck by the increase in fatality from alcohol and drug use among both older adults and among younger adults, as well,” Fernandez said. “The two things that stand out to me are deaths from alcohol-associated liver disease and deaths from a drug overdose.”
What’s behind this?
Many factors play a role in this uptick, she said. “The baby boomer generation is now reaching older adulthood, and baby boomers historically have higher rates of substance use than the generation before,” Fernandez explained.
It’s also been a perfect storm for drug and alcohol abuse. “Alcohol and drug use also
tend to increase when there are economic challenges, when drugs and alcohol are accessible and affordable, and when major stressful events take place, like the COVID-19 pandemic,” she said.
In addition, the drugs people take now are also more lethal than they were even a decade ago. “Early on, the opioid overdose crisis was driven by prescription opioid use but now it is driven by highly lethal synthetic opioids like fentanyl in the drug supply,” Fernandez noted.
Alcohol often gets pushed aside in discussions about substance abuse and addiction. “We often talk about the opioid epidemic, but we are also living in an alcohol epidemic and have been for some time,” she said. “Americans are simply drinking more in recent years and this is driving increases in deaths from liver disease, motor vehicle accidents and poisoning/overdose.”
Alcohol use and drug overdose also intersect, she added. “Alcohol is an often overlooked but major contributor to overdose deaths,” Fernandez said. “Combining alcohol and other drugs, particularly other depressants, greatly increases overdose risk.”
Decreasing deaths from drugs and alcohol is a national priority, and many groups are working on prevention and intervention. “More stringent alcohol policies could be used to reduce the accessibility and affordability of alcohol,” Fernandez suggested. “As a culture, I also think we need to change the conversation around alcohol to focus more on alcohol’s impact on health like we did for smoking decades ago.”
68 H&C
Prioritizing addiction treatment
Addiction treatment should be accessible, affordable and high quality. “We need to make addiction care as well-funded and prioritized as any other type of health care, and that is not the case currently despite these alarming national trends,” she said.
In addition, destigmatizing these conditions is also hugely important so that people can talk about these issues openly, and seek help early and often, Fernandez advised.
Substance use disorder — whether it be alcohol or drugs — has grown significantly since the start of the COVID-19 pandemic, agreed Dr. Tucker Woods. He is the chair of the emergency department and associate medical director of Lenox Health Greenwich Village, in New York City.
“In some ways, the COVID-19 pandemic has
masked the opioid public health crisis by taking it out of the forefront of the news,” he said, “On the flip side, the COVID-19 pandemic has truly exacerbated the opioid epidemic because it has resulted in unprecedented levels of anxiety, depression and isolation.”
What’s more, the COVID-19 pandemic also made it difficult for many individuals to seek help, Woods said. Treating addiction saves lives, he added.
“We need more physicians who have specialized in addiction medicine as, currently, there is a national shortage of board-certified addiction medicine physi-

We Help Families with Important Life Transitions
Our streamlined support system provides a stress-free process
Regardless of the situation, planned or unexpect ed, the loss of a loved one or the need to relocate someone can be challenging. The physical challenges and emotional strains can be overwhelming enough, without the added stress of life’s unexpected events.
Caring Transitions serves all of the St. Louis Metro area with a streamlined support system for a less stressful transition, taking care of the details so you can take care of yourself or a loved one.


From sorting through years of memories, working with estate planners, coordinating movers and real estate agents to designing a functional and comfort able floor plan, our compassionate and experienced professionals can be involved as much or as little as you like. We’ll serve as your family’s advocate, ensur ing your best interests are kept in mind throughout the process.






cians in the United States,” Woods said. Calling the data “tragic,” Dr. Catherine Sarkisian pointed out that current seniors came of age during the Vietnam War and/ or were baby boomers and had a much higher rate of drug use than people who came of age during World War II. She is a geriatrician and professor at the University of California, Los Angeles.
“It is terrible but not completely surprising that drug overdose would also be higher in this cohort than in previous cohorts of seniors,” Sarkisian said.
Going forward, it would be interesting to try to learn to what extent the overdoses are accidental versus intentional, as this information can help design appropriate and effective prevention strategies, she added. More information
The U.S. National Institute on Drug Abuse has more on substance abuse in older adults.
FEATURED SERVICE
us assist your family with an important lifetime transition.
the details to us. Call today!
Let
Leave
314-804-7575
Short Brisk Walk Each Day Could Cut Your Odds of Early Death
Abrisk 11-minute daily walk can help you live longer, a new University of Cambridge study reports. Researchers found that 75 minutes a week — 11 minutes daily — of moderate-intensity physical activity is enough to lower a person’s risk of heart disease, stroke and cancer.
The investigators estimated that 1 in 10 early deaths could be prevented if everyone got that amount of exercise, which is half the level recommended by U.S. and British guidelines.
The good news
“If you are someone who finds the idea of 150 minutes of moderate-intensity physical activity a week a bit daunting, then our findings should be good news,” co-researcher Dr. Soren Brage, of the Medical Research Council at the University of Cambridge in the United Kingdom, said in a university news release.
“Doing some physical activity is better than doing none,” he added. “This is also a good starting position — if you find that 75 minutes a week is manageable, then you could try stepping it up gradually to the full recommended amount.”
Cardiovascular diseases (heart disease
and stroke) were the leading causes of death worldwide, responsible for nearly 18 million deaths in 2019. Cancers were responsible for 9.6 million deaths in 2017. To examine how much exercise could make a dent in those numbers, the researchers pooled and analyzed data from 94 large studies involving more than 30 million people.
Most people don’t exercise enough
The findings showed that 2 out of 3 people don’t get their recommended 150 minutes per week of moderate-intensity exercise, and fewer than 1 in 10 managed more than 300 minutes of activity per week.
Broadly speaking, the researchers concluded that getting more than 150 minutes a week of exercise produces marginal benefits in terms of reduced risk of disease or death.
But even half that amount came with significant benefits, the team reported. For example, 75 minutes per week of moderate-intensity exercise reduced risk of early death by 23%. It was also enough to reduce the risk of heart disease and stroke by 17% and cancer by 7%.
For some specific cancers, the reduction in risk was even greater. Getting that
amount of exercise reduced the risk of head and neck, myeloid leukemia, myeloma and gastric cardia cancers between 14% and 26%.
The researchers calculated that if people get their recommended 150 minutes of exercise a week, around 16% of early deaths would be prevented. In addition, 11% of cardiovascular disease cases and 5% of cancer cases would be prevented. But if folks manage at least 75 minutes per week of moderate-intensity physical activity, around 10% of early deaths would be prevented. And 5% of cardiovascular disease cases and 3% of cancer cases would be prevented.
Exercise doesn’t need to be intense
Further, moderate-intensity exercise doesn’t require you to run yourself ragged, the researchers noted. It raises your heart rate and makes you breathe faster, but you’d still be able to speak during the activity.
Other examples include dancing, riding a bike, playing tennis and hiking. Moderate activity doesn’t have to involve what we normally think of exercise, such as sports or running,” co-researcher Dr. Leandro Garcia from Queens University Belfast explained.
“Sometimes, replacing some habits is all that is needed,” Garcia added. “For example, try to walk or cycle to your work or study place instead of using a car, or engage in active play with your kids or grand kids. Doing activities that you enjoy and that are easy to include in your weekly routine is an excellent way to become more active.”
The findings were published in the British Journal of Sports Medicine.
What This Means for You
If you get 11 minutes daily of moderate-intensity physical activity, you will greatly reduce your risk of an early death. More information
The U.S. National Institutes of Health has more about moderate-intensity physical activity.

70 H&C
Quiz: Seniors, How Much Do You Know About Exercise?
 By Chris Woolston
By Chris Woolston
There’s a world of difference between being old and feeling old. Your birthdays may be piling up, but that doesn’t mean you have to slow down, grow weak, or lose energy. All it takes to keep your body and spirits strong is a little exercise — and an understanding of what it does. Take this quiz to see how much you know about exercise for seniors.
1. Aerobic exercise is the fastest way for seniors to lose weight.
3. Which of the following exercises will NOT help build bone and prevent fractures?
a. Swimming
b. Weight lifting
2. Weight lifting isn’t safe or effective for people in their 80s and 90s.
c. Tennis
d. Walking
e. Bicycling
“Cedarhurst. ”
How can I make more friends? What’s the solution to boredom? How do I prepare for the unknown ahead? How can I stick to a healthier diet? How do I offload my household chores and free up my time? What should my plan be?
When you’ve got questions, call (314) 200-4302 and find your answers.
Assisted Living, Memory Care & Independent Living
Locations in St. Charles, Tesson Heights, Granite City, Centralia and Breese. Find a community near you at CedarhurstLiving.com
4. Which of these activities can cut your risk of heart disease roughly in half?
a. Regular walks
b. Jogging
c. Aerobics classes
d. All of the above
e. None of the above
5. Aerobic exercise can be just as effective as medications for treating severe depression in seniors. True False
6. Which disease usually makes it impossible to engage in vigorous exercise?
a. Arthritis
b. Diabetes
c. High blood pressure
d. All of the above
e. None of the above
Answers on the next page
True False
True False
THE
LIVING STRONG, CLEAR AND FOCUSED HOW YOU LIKE TO FACE EACH DAY
ANSWER IS
Exercise for Seniors Quiz Answers
1. Aerobic exercise is the fastest way for seniors to lose weight. True or false?

The correct answer is: False
Most seniors can lose weight faster through strength training than through aerobic exercise, according to a report in Medicine and Science in Sports and Exercise. Lifting weights helps replace fat with muscle and speeds up the metabolism. After a few weeks of strength training, the study found, most of the subjects need to increase calories by 15 percent just to maintain body weight. However, since muscle is denser than fat, your weight can also stay the same or increase slightly as you gain muscle mass and burn fat.
Alzheimer’s Association Greater Missouri LOCAL PROGRAMS AND SERVICES

The Alzheimer’s Association Greater Missouri Chapter offers assistance to keep individuals living with dementia, their caregivers and family members supported, connected and engaged.

The following programs and services are free and available for all:
• 24/7 Helpline—Our free Helpline connects you with specialists who offer confidential help and decision-making support, crisis assistance and education on issues families face every day.
• Support Groups—We offer groups for caregivers, individuals living with dementia and others dealing with the disease. All support groups are facilitated by trained individuals.
• Education Programs—Our free education classes teach participants about the signs, symptoms, causes, risk factors, diagnosis, treatment, care strategies and resources for individuals impacted by dementia.
• Care Consultations—This free service with our social workers helps individuals and families navigate through the difficult decisions and uncertainties that is the journey of dementia.
To learn more visit alz.org/greatermissouri or call our 24/7 Helpline at 800.272.3900. Connect with our social media @alzgreatermo
2. Weight lifting isn’t safe or effective for people in their 80s and 90s. True or false?
The correct answer is: False
A group of nursing home residents ranging in age from 87 to 96 improved their muscle strength by almost 180 percent after just eight weeks of resistance training. In general, frail elderly people find that their balance improves, their pace quickens, and stairs become less of a challenge after they begin age-appropriate strength training. Just be sure that any exercise program for seniors takes into account that they are more prone to bone fractures, tendinitis, and muscle strains.
3. Which of the following exercises will NOT help build bone and prevent fractures?
The correct answers are: a. Swimming and e. Bicycling
Swimming or biking are excellent for a workout, but they don’t build bone. To ward off osteoporosis
and prevent fractures, you need exercises in which you stay on your feet and support your own weight. Walking, jogging, dancing, tennis, and weight lifting are all good choices for maintaining healthy bones.
4. Which of these activities can cut your risk of heart disease roughly in half?
The correct answer is: d. All of the above
You don’t need to push yourself to the limit to improve your odds against heart ailments. Researchers at Harvard found that women who walked just three hours a week cut their risk of heart disease by 40 percent, equivalent to the benefits of much more vigorous exercise.
5. Aerobic exercise may be just as effective as medications for treating severe depression in seniors. True or false?
The correct answer is: True
Your loved one deserves a higher standard of care.
When your loved one needs extra care at home, choosing the right caregiver agency can be tough. Let BrightStar Care® make it easier.
• We offer companion and personal care, including bathing, meal prep, medication reminders, mobility assistance and more.

• We also offer Alzheimer’s and dementia care.
• Our services include skilled nursing care such as medication administration, infusion therapies, catheter and wound care, and more.

In a study of 156 severely depressed men and women over 50, Duke University researchers found that 16 weeks of aerobic exercise eased symptoms as thoroughly as a 16-week regimen of antidepressant drugs. People who are depressed should consult with their doctor to determine the best course of treatment and what part exercise can play.
6. Which disease usually makes it impossible to engage in vigorous exercise?
The correct answer is: e. None of the above
In fact, regular exercise can be excellent therapy for all of these diseases - and many others. Just remember, always check with your doctor before starting any high-intensity exercise program.
©BrightStar Care Independently Owned and Operated Call for your free in-home assessment. BrightStar Care of West, Central and South St. Louis and St. Charles 314-819-6000 brightstarcare.com/central-st-louis-county 636-866-0722 brightstarcare.com/st-charles
Young Forever: The Secrets to Living Your Longest, Healthiest Life
By Dr. Mark Hyman


Mark Hyman, MD, is the senior advisor for the Cleveland Clinic’s Center for Functional Medicine, board president for clinical affairs for the Institute for Functional Medicine, founder and director of The Ultra Wellness Center and host of one of the leading health podcasts, The Doctor’s Farmacy. He is the author of numerous best-selling books.
In his book published this year, Young Forever, Dr. Hyman starts with the proposition that disease, frailty and gradual decline are thought of as inevitable parts of life, but they don’t have to be. Science today sees aging as a treatable disease. By addressing its root causes we can not only increase our health span and live longer, but prevent and reverse the maladies of
aging – including heart disease, cancer, diabetes and dementia. He presents a comprehensive plan for reversing disease, easing pain, and living younger longer.
The book is divided into three parts.
The first part, “How and Why We Age,” explores the latest research on aging, its causes and consequences, and how it can be slowed down or reversed.
The second part, “Optimizing Your Health Span and Life Span,” outlines the foundations of
Healthy Humor
longevity, including eating, moving and other ways to optimize lifestyle beyond diet and exercise. The third part, “The Young Forever Program,” brings it all together, with guidance on biometric testing, the Young Forever Longevity Diet and managing key lifestyle components including sleep, exercise and stress.
Young Forever is a well-written and informative book that provides a comprehensive plan for living a longer, healthier life. Dr. Hyman’s plan is based on the latest research on aging and is backed by decades of clinical experience. Some of the diet and exercise recommendations may not be easy or convenient for all readers to follow to the letter, but if you are looking for a way to slow down or reverse the aging process, this book provides a great start.

74 H&C
BOOK REVIEW

Our
Our specialty is you.
As the only independent health system in the St. Louis area, one thing truly sets us apart: We believe everyone deserves compassionate, expert care. Our highly accomplished doctors practice in more than 60 specialties in our two hospitals and nearly 30 outpatient locations. When you choose St. Luke’s, our entire care team cherishes the opportunity to help you and your family achieve your very best health. Learn more or schedule your appointment at stlukescare.com.
Compassionate care
Strong relationships that help you navigate every step of your health and wellness journey.
Nationally recognized
Consistently honored as America’s best for excellence in patient care and more.
Leading technology
The innovation and tools to ensure you get the best results for your health.
Easy access
Convenient locations plus same-day appointments at some offices.
specialty is compassionate care.
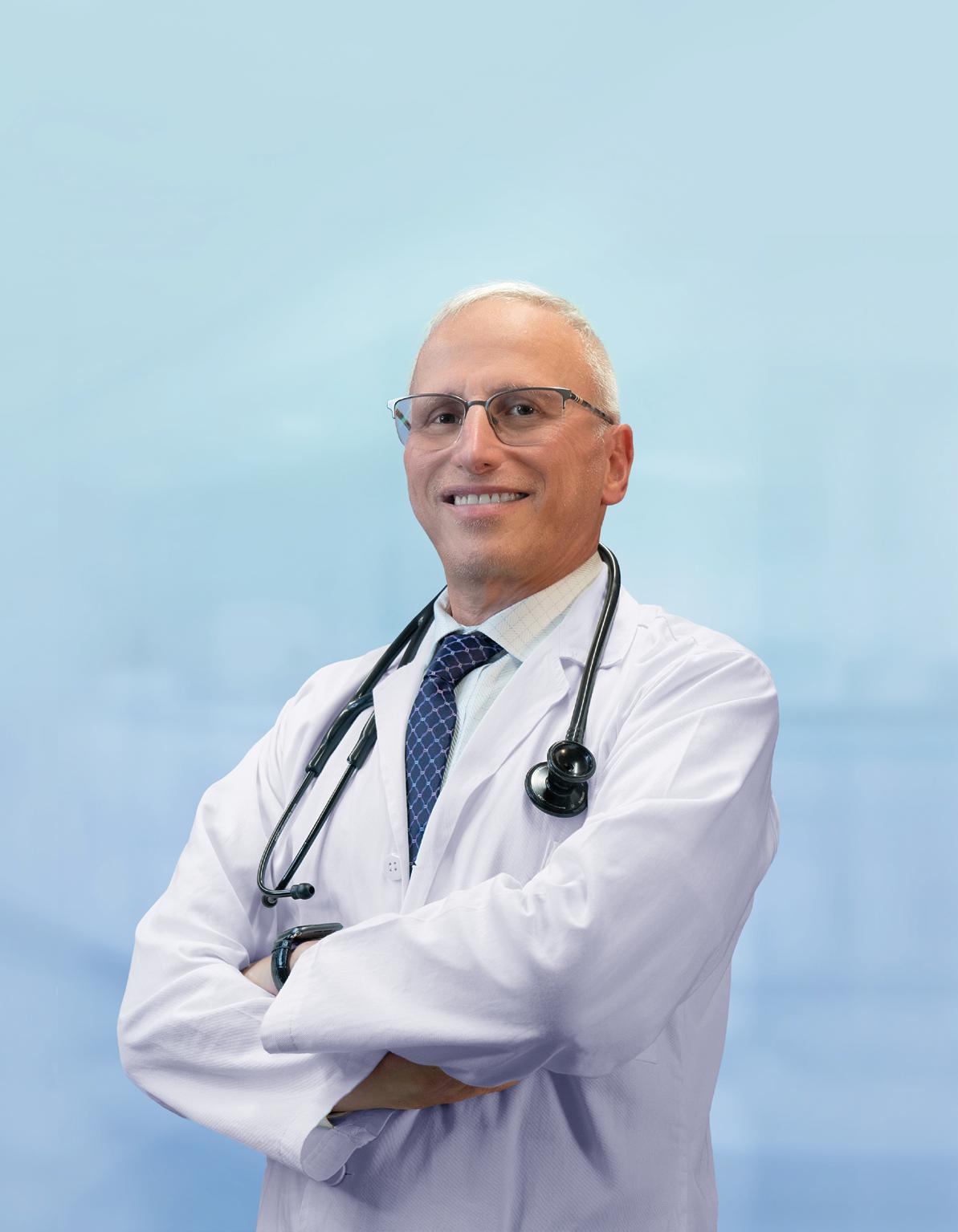











































































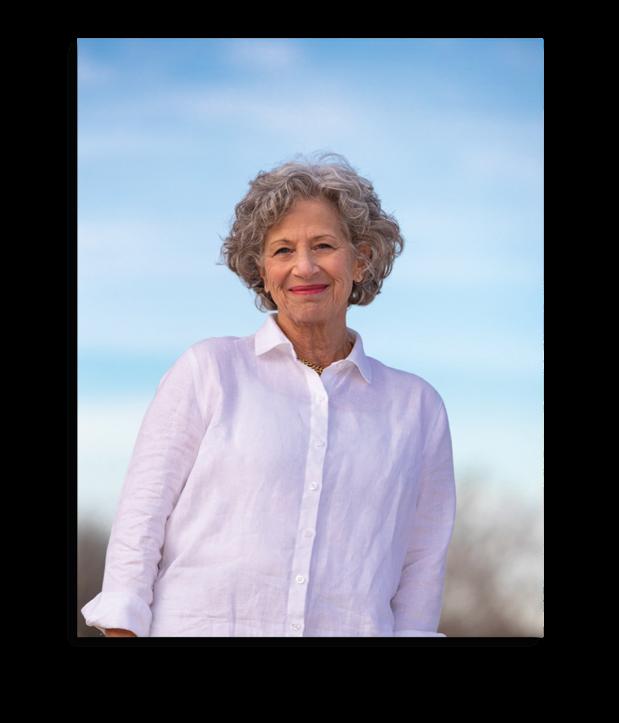


































 By Chris Woolston
By Chris Woolston