Sydney Opera House launch, and hearing aids with Auracast
NEW NAL-NL3 HEARING AID FITTING FORMULA
We reveal the groundbreaking prescriptions and how they'll influence fitting for the better.

Sydney Opera House launch, and hearing aids with Auracast
NEW NAL-NL3 HEARING AID FITTING FORMULA
We reveal the groundbreaking prescriptions and how they'll influence fitting for the better.
THE BOOM OF CUSTOM EARPLUGS
There’s an explosion of earplugs on the market. Take a look at the trends, tips and innovations.

Tips to innovate and thrive from the record-breaking 2025 event in Melbourne. 40
HEARING BUSINESS ALLIANCE SEMINAR WRAP


The National Acoustic Laboratories’ long-awaited NAL-NL3 hearing aid fitting prescription formula has been revealed at the American Academy of Audiology (AAA) conference with major new features to have big implications for audiology prescribing worldwide.
The new formula features a suite of prescriptions, rather than the existing one-size-fits-all solution, and will help practitioners solve one of the biggest problems in audiology worldwide –how to fit hearing aids to people with audiometrically normal hearing tests (minimal or no audiometric hearing loss) who have trouble hearing in noise. Estimates suggest half of new clients walking into audiology clinics are in this category.
Another key change advises how to fit hearing aids to help other clients hear better in noise.
The version to follow NAL-NL2, which launched 14 years ago, is set to become the most widely used fitting prescription for hearing aids in the world when it launches on the market later in 2025 and is embedded in hearing aid fitting and verification software used daily to fit hearing aids.
A NAL team travelled to the AAA conference in New Orleans and on 28 March 2025, Dr Padraig Kitterick, NAL’s head of audiological science who has overall responsibility for delivery of the NAL-NL3 project, and NAL director, Dr Brent Edwards, revealed details and the evidence behind it to a packed auditorium of hearing health leaders.
Dr Edwards said: “I’m probably most excited about delivering the next generation of fitting prescription that will help hearing health companies and hearing care practitioners provide

the best hearing aid fittings possible.”
Dr Kitterick told Hearing Practitioner Australia: “We’re excited to provide not just the next generation of what has been a long line of evidence-based hearing aid fitting prescriptions, but for the first time introduce brand new ways of fitting hearing aids.
“These new prescriptions will help clinicians address needs that they’re seeing in clients where they don’t have a really good evidence-based solution for fitting, particularly those
The Hearing Health Sector Alliance (HHSA) has named four priority actions for the 2025 Australian federal election including extending the Hearing Services Program (HSP) to those on low incomes, mandating hearing screening on admission to aged care and creating a new HSP Schedule item for aged care screening.
Other priorities focus on addressing regional and remote workforce shortages and improving Aboriginal and Torres Strait Islander hearing health.
The HHSA, which represents 15 of the nation’s peak organisations involved in hearing health, has presented its election priorities
statement to the Federal Labor Government and the Opposition Liberal Party.
The statement says: “The HHSA urges all levels of government to commit to improving access to hearing health care for Australia’s most vulnerable populations through four priority actions: prioritising Aboriginal and Torres Strait Islander hearing health, enhancing care for aged care residents, addressing regional workforce shortages, and supporting low-income and unemployed individuals.”
Its recommendation to extend the HSP is to support low-income and unemployed individuals with hearing loss greater than 26 dB in
the better ear. “This initiative would increase employment opportunities, estimated to yield $311 million in productivity gains, while improving the budget position by $33,135 for each individual who gains employment, ultimately generating a net fiscal benefit of over $268 million,” the statement says.
“Many Australians with hearing loss, especially those on low incomes or who are unemployed, are left unsupported due to restrictive eligibility requirements. With approximately 15,000 individuals excluded from the National Disability Insurance Scheme (NDIS) due to strict hearing loss eligibility thresholds, this group faces
continued page 8
with minimal hearing loss and those with difficulties in noise. It’s a whole new ball game.”
Dr Kitterick said a key new feature was the shift from one prescription for everybody in NAL-NL2 to a modular system that will expand over time which contains a suite of different prescriptions to achieve different things.
The new formula aims to help audiologists fit hearing aids to someone with an audiometrically normal hearing test but who experiences difficulties when listening in noise and who is motivated to use hearing aids.
“NAL-NL3’s minimum hearing loss module solves how to fit hearing aids to people who we would traditionally class as not having hearing loss.
“Depending on the audiology
continued page 8

brain stimulation in suppressing tinnitus or altering its perception has resulted in a Flinders University-led group receiving a large NHMRC grant to progress trials of the treatment. Professor Raj Shekhawat found the technique was having great success in stroke rehabilitation and adapted it for tinnitus. page 44
COMING SOON!

Discover a new world of opportunities with our most intelligent portfolio yet Lead the way
Let clients enjoy life to the fullest with our new intelligent portfolio that will let you illuminate life and bring speech clarity and connectivity for all.
With Beltone Envision, get ready to discover how GN is taking a human approach to AI. Intelligent solutions for you and your clients, without compromise.
Beltone Commence combines our proven technologies to bring greater clarity and ease to everyday connections. Small, sleek and connected solutions for mild to profound hearing loss.


18

A lifetime of care
Queensland audiometrist Mike Carter is retiring after devoting nearly five decades to changing lives through hearing care.

3D ear scan offer
Sydney business owner Peter Ling’s unique proposition is bringing scans for custom earplugs to clinics.

Nutrition and ears
Audiologist Dr Celene McNeill and dietitian Dr Diana Tang discuss the potential impact of diet on hearing and tinnitus.

Balloon dilation for OM
ENT surgeon Dr Martin Nue Møeller says Eustachian tube balloon dilation is a promising new treatment for chronic otitis media.
It’s hard to believe it’s been a year since Practitioner Australia hearing health sector.
From the outset we wanted to be a platform for the entire industry, helping it grow by championing the individuals and organisations within it. We hope you have enjoyed our wide-ranging coverage, documenting the professional lives of many who work within this thriving industry.

We’ve been here a short time, but it’s impressive to watch this sector at work. We’re only one-quarter through 2025, and we’ve got so much to tell you about.
First up, we reveal the groundbreaking new NAL-NL3 formula and how this will influence hearing aid fitting for the better.
We were there for the Auracast launch at Sydney Opera House, hosted by GN, NAL and Hearing Australia, which made global headlines as the first major cultural institution to introduce the revolutionary broadcast technology.
The Hearing Business Alliance also invited us to cover its most successful business seminar so far, including great tips on how independent practices can innovate to be more profitable.
Readers may be interested in Queensland audiometrist Mike Carter, 73, who’s reluctantly retiring after nearly five decades. What did he learn in his time, including as a business owner?
There are more excellent reports from wearers of Starkey’s new Edge AI hearing aids, with Sydney audiometrist Krystal Allen, who has hearing loss, among those “blown away” by their performance.
There’s an in-depth feature on the explosion in earplugs. Audiometrists John Lucchese and Partho Pal, who are experts in this field, give us a glimpse of their custom earplug practises along with tips and predictions.
On the same theme, we reveal a new proposal from Sydney’s Mr Peter Ling to bring 3D ear scanners into hearing clinics, underpinned by an innovative business model that many independents will be interested in.
The impact of diet on ear and hearing health, plus non-invasive brain stimulation as a tinnitus treatment, round out this eventful edition.


HELEN CARTER Editor



Just as HPA went to print, AUDIOLOGY AUSTRALIA expressed disappointment that audiology and hearing health were overlooked in the 2025 Australian Federal Budget. CEO Ms Leanne Emerson said barriers such as limited Medicare funding and inadequate recognition of audiologists’ scope of practice continued to limit access to vital services, despite audiologists’ key roles in primary care. She said targeted investment in funding models, direct referral pathways from audiologists to ENTs, title protection for
Weird
Sound plays a significant and often poignant part of a skateboarders’ relationship with their sport, a University of Exeter study shows. Skateboarders develop the skill to tune into the noise of urban surfaces and hear and feel noise which means images and videos alone are a poor insight into the sport. They use sound to verify the success of their manoeuvres and judge the veracity and capacity of surfaces for use and as a social cue, the researchers said.
Wonderful
Japanese researchers have developed a propagation phenomenon of acoustic waves, paving the way for developing advanced communication technologies using acoustic devices. Surface acoustic waves (SAWs) play a crucial role in modern communication technologies. They used nanofabrication techniques to create a periodic array of nanoscale magnetic materials, a grating that waves go through. Instead of a typical symmetric diffraction pattern, they saw an asymmetrical diffraction phenomenon of SAWs called nonreciprocal diffraction. This may enable precise control of SAW propagation paths using magnetic fields, leading to development of acoustic devices that advance classical and quantum communication technologies, they said.
Wacky
Deaf male mosquitoes don’t mate, US researchers have found. The sound of a female mosquito’s wingbeats normally attracts males to brief mid-air mating. When researchers investigated the insect’s auditory neurons, they focused on a sensory channel called TRPVa and the corresponding gene, trpVa, the mosquito analogue of a channel required for hearing in fruit flies. Removing the gene that codes for TRPVa in Aedes aegypti mosquitoes prevented mating.
audiologists, and expanded workforce programs would improve equitable access to hearing care, particularly for vulnerable and underserved populations. There was also no commitment to addressing workforce shortages. IN OTHER NEWS, The Cass Foundation has awarded $60,000 to support Bionics Institute researcher Dr Demi Gao improve cochlear implant programming for infants to ensure their implants are set up correctly at the earliest stages. The research uses a hearing test developed by the institute which employs non-invasive functional near-infrared spectroscopy to measure brain
responses to different sound levels while infants sleep. It will also establish a new standard for care for babies with cochlear implants. FINALLY, a sign bank to express mental health-related words has launched to support deaf people in Bangladesh, developed by Monash University researchers, Bangladeshi sign language interpreters, people from the deaf community and healthcare professionals. The Digital Tools for Deaf Mental Health Project has online resources to support mental wellbeing of people with deafness. Nearly 10% of the Bangladeshi population is deaf or has hearing difficulties.

in noise is a new feature in NAL-NL3, says Dr Padraig Kitterick. Page 20.
THIS MONTH
CI2025 BOSTON
30 APRIL – 3 MAY
The American Cochlear Implant Alliance’s CI2025 Boston Conference on Cochlear Implants in Children and Adults will be in Massachusetts, US. acialliance.org
Complete calendar page 51.
NEXT MONTH
VCCA 2025 ONLINE
26-27 JUNE 2025
The Virtual Conference on Computational Audiology is free to attend. It aims to unite hearing scientists, clinicians and audiologists to stimulate innovations for hearing loss. computationalaudiology.com
Published by:
379 Docklands Drive, Docklands VIC 3008 T: 03 9690 8766
www.primecreative.com.au
Chief Operating Officer
Christine Clancy christine.clancy@primecreative.com.au
Publisher
Sarah Baker sarah.baker@primecreative.com.au
Managing Editor Myles Hume myles.hume@primecreative.com.au
Editor
Helen Carter helen.carter@primecreative.com.au
Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Isabella Fulford isabella.fulford@primecreative.com.au
Head of Design Blake Storey
Art Director Bea Barthelson
Subscriptions T: 03 9690 8766 subscriptions@primecreative.com.au
Cover – Image: GN.

The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright –No part of this publication can be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.
continued from page 3
provider, we have heard estimates of anywhere between 40% and up to 60% of new clients walking through the door of clinics can have minimal or no audiometric hearing loss but are reporting problems listening in noisy environments.
“It’s a huge portion of the population seeking help for their hearing problems and for many of them being told they have normal hearing is not helpful; but it is really challenging clinically to know how to best help this kind of client.”
The prescription formula, the first upgrade in 14 years, will be integrated into clinicians’ fitting software, is compatible with Windows and will later be compatible with mobile apps.
The engineer responsible for the project, Mr Justin Zakis, did a similar reveal at the Audiology Australia 2025 Conference in Adelaide in early April 2025.
Dr Kitterick said: “The point is making hearing aids acceptable and beneficial even if you’ve got little or no audiometric hearing
loss, to help you hear better in noise.”
He said NAL surveyed clinicians worldwide asking for use cases where NL2 was not providing the best solution for their clients.
“We got a lot of feedback and consistency across clinicians from around the world,” he said. “They said it worked really well for most clients, but they identified pain points.
“They told us that sometimes NL2 prescribes too much compression and can prescribe too much gain for specific kinds of hearing losses like mixed losses and reverse sloping losses.
“Data from hundreds of thousands of hearing aid fittings also suggested that often for many users, particularly new hearing aid users, NL2 prescribed too much high frequency gain that did not really improve intelligibility in a meaningful way.”
Dr Kitterick said NL2 has remained the gold standard of fitting and the best option for patients who want to listen and understand well in quiet environments. “It is well validated and well understood.

PORTION OF THE POPULATION SEEKING HELP FOR THEIR HEARING PROBLEMS AND FOR MANY OF THEM BEING TOLD THEY HAVE NORMAL HEARING IS NOT HELPFUL.”
DR PADRAIG KITTERICK, NAL
"We’re keeping that same philosophy for quiet and are fixing pain points with it, making it even more effective by bringing the latest machine learning approaches and over a decade of experience with fitting NL2.”
Another feature is a comfort-in -noise module.
“We don’t believe NL2 is the best we can do to fit a hearing aid when the use case is listening in noise,” he said. "Our NL3 noise module maximises comfort-in-noise without sacrificing speech intelligibility.
"It gives a much more comfortable experience but maintains the focus on maximising speech understanding that has been at the core of NAL hearing aid prescriptions for decades.”
NAL will release the final version of the software to manufacturers in September 2025 for them to integrate into fitting and verification software and equipment.
continued from page 3
significant barriers to wellbeing, social inclusion, and employment.”
The HHSA believes two key initiatives the government could implement would make a huge difference to older Australians in aged care settings. The first is mandating a uniform protocol to conduct hearing screening for all new residents of aged care facilities within one month of residency and include this as a quality metric in aged care reporting.
The second is creating a new schedule item in the HSP Schedule for aged care facility hearing screenings at the same price as a hearing assessment ($157.40), reflecting the true cost for hearing health care professionals to conduct remote visits and diagnostic services.
Hearing loss is estimated to affect more than five in six older people. Despite this, the HHSA says there is no standardised approach to managing hearing loss in aged care, leaving many residents unsupported and creating communication challenges between residents and staff, which can lead to misdiagnoses of cognitive decline, increased risks of isolation and mental illness.
To address regional and remote workforce shortages, the HHSA recommends
reducing HECS debts for domestically trained hearing health professionals by 10% for each year they live and work in designated regional or remote areas.
“With only around 250 new domestic graduates each year, this measure would attract more professionals to areas where they are most needed,” it said.
It urges improving the Skilled Employer Sponsored Regional (provisional) visa for hearing health professionals, including lowering application fees, adjusting residency requirements, and increasing the age limit to attract skilled international professionals to regional areas.

“People experience hearing loss at higher rates in rural and remote areas yet hearing health professionals are concentrated in urban centres,” it states.
Recommendations to enact meaningful improvements in Aboriginal and Torres Strait Islander hearing include reassessing Hearing Australia’s outreach targets for Aboriginal and Torres Strait Islander children and holding contracted service providers to account regarding resource allocation relative to achievement of agreed targets. A second priority is refining funding mechanisms in the Community Service Obligations program to make it focussed on and responsive to local
qualified providers to deliver services. A third is mandating ear and hearing health professionals to move away from a standard approach of service delivery and embed cultural safety at an individual and system level to enable culturally responsive services accountable to and aligned with Aboriginal and Torres Strait Islander people and communities.
Ms Jane MacDonald, HHSA chair, said the alliance was a collaborative resource for governments and policymakers, offering unified expertise on hearing health matters across sectors. It brings together key national voices in the hearing health ecosystem to improve equitable access to essential hearing health support for all Australians.
Global optical giant EssilorLuxottica has announced that its “hearing glasses” –spectacles that include hearing aids – have received approval from the FDA and EU certifications enabling them to be sold in America and Europe. The company is marketing its Nuance Audio Glasses, which it states audiology practices can access, as a “breakthrough in hearing technology” and an “over-the-counter (OTC) hearing aid integrated into smart glasses for perceived mild to moderate hearing loss in adults aged 18 and over”. The audio component is invisible as it is embedded within the spectacle frames. Optional lens upgrades, which are not required for use, include customising the glasses with the client’s preferred optical lenses, whether they need a prescription, Transitions lenses or blue light filtering.
The Department of Health and Aged Care has updated forms for Hearing Services Program (HSP) providers, upgrading to digital format and improving accessibility, usability, clarity and readability. All HSP forms can now be completed digitally, and providers must use the updated forms from 1 July 2025. The department said the changes were the final piece of the program’s web transition which involved a new website at health. gov.au/hear and an update of content and resources. “Improvements have been made to accessibility and usability, and you can complete all forms digitally. The forms have been updated to improve readability and give greater clarity for clients completing the forms. There is space at the top for providers to add branding. Providers can adapt the design of the forms for their purposes however they cannot alter the text.”
Australia’s Therapeutic Goods Administration (TGA) is evaluating Norgine Pharmaceutical’s PEDMARQSI for the prevention of hearing loss induced by cisplatin chemotherapy in children. The proposed new indication is “for the prevention of damage to parts of the ear that is sometimes caused by cisplatin chemotherapy”. Trials show the treatment halves the incidence of ototoxicity, or permanent hearing loss, in those who receive it while undergoing cisplatin chemotherapy compared with those who just receive the chemotherapy. “PEDMARQSI is to be used in children aged one month to under 18 years with localised solid tumours that have not spread to other parts of the body,” the TGA said. The treatment is already in use in the US, Germany and the UK.
A small Scottish study has suggested headphones may be detrimentally changing the way young people hear, causing trouble localising sounds. The findings made global headlines along with a BBC investigation that found more young people were reporting to audiology departments struggling to process sound.
The British Academy of Audiology then called for research into “how noise cancellation and earphones affect young peoples' developing hearing”. The BBC said other audiologists stated more research was needed into the potential effects of prolonged use of noise-cancelling headphones.
A researcher from the Scottish study, Dr Claudia Freigang said: “Our findings raise big questions about how modern listening habits are shaping auditory development.
“This isn’t just about hearing loss or noise exposure — it’s about the way we process sound in space. If young adults are struggling with spatial hearing now, what might this mean in the long run?”
Dr Freigang, a former auditory neuroscientist, CEO and co-founder of Edinburgh company Hearing Diagnostics Limited, was commenting on her study’s incidental finding on the company’s website.
While testing its new hearing screener Audimetroid, the study found 40% of the 30 adults under age 30 with normal hearing could not localise sounds. But only 5% of 56 adults over age 50 with normal hearing had trouble localising sounds.
About 40% under age 30 with normal hearing could not localise sounds compared with 5% of adults over age 50. Image: NOPPHINAN/ stock.adobe.com.
“We set out to validate our hearing screener, which uses a spatial-hearing paradigm to detect hearing loss,” Dr Freigang said on the Hearing Diagnostics website. “We didn’t expect young adults to have any trouble with the test.”
The BBC said five NHS audiology

departments said there had been an increase in the number of young people referred to them from GPs with hearing issues. Their hearing tests were normal, but they struggled to process sound.
The BBC said auditory processing disorder (APD) was more common in neurodivergent people, those who had suffered a brain injury or had a middle-ear infection as a child. But more patients with APD were presenting outside those categories, leaving audiologists to question if external factors, such as noise-cancelling headphones, were contributing.
Dr Freigang said most research suggested young people should perform well – if not better than older adults – on tasks involving binaural processing. Binaural processing is the ability to use sound cues from both ears to determine where a sound is coming from.
In her study, participants listened to simulated spatial sounds through headphones and turned towards them to localise them, relying on their binaural processing.
Dr Freigang said results were unexpected; 95% of adults over 50 with normal hearing localised the sounds without any issues while only 60% of adults under 30 with normal hearing could localise the sounds.
“At first, I was convinced something had gone wrong,” she said. “I’ve spent years researching central auditory processing and spatial hearing, and this went against everything I’d seen before. But as we continued testing, the trend remained.
“It wasn’t until we started chatting with the younger participants that a possible explanation emerged. Many told us they struggled to hear in noisy environments.
“When we asked about their listening habits, a pattern became clear: most were using headphones for hours every day – for university, gaming, socialising, you name it. Some had been wearing them all day, every day, since high school – years of near-constant headphone use.” She did not think noise-cancelling headphones were the issue, but rather the nature of headphone listening as they strip away spatial cues.
Auditory Processing Institute founder Dr Angela Alexander said they could be a potential factor in why some people had more auditory processing issues now than years ago when they weren't used.
Audiology Australia (AudA) is calling for Federal Government policy changes to improve access to hearing care services for more Australians.
On 19 March 2025 it joined a call for political parties and independent politicians to make “common-sense changes” to their policies in the lead-up to the 2025 federal election.
The nation’s peak audiology body is also supporting a recommendation from the Hearing Health Sector Alliance (HHSA) to expand the Hearing Services Program (HSP) to low-income and unemployed Australians.

AudA is urging audiologists, hearing care professionals, clients and the public to show their support and get behind the campaign by emailing their local MP.
It said it supported the Allied Health Professions Australia (AHPA) election campaign for five priorities aiming to further embed allied health services in care systems and rural locations, and increase cooperation between allied health and other health professionals.
It also joined ear and hearing care leaders in the HHSA to lobby for four additional priorities specific to hearing health.
“Greater action is urgently needed to help the one in six Australians affected by hearing
loss and address the financial impacts of hearing loss, estimated to cost Australia $20 billion annually,” said Ms Leanne Emerson, AudA’s CEO.
“We urge candidates to act on the recommendations put forward by AHPA and the HHSA.
“These are common-sense recommendations. Acting on them will ensure Australians can be more easily supported by an allied health professional, resulting in earlier intervention, easier treatment processes, and a reduced financial burden on taxpayers.”
One recommendation put forward by AHPA is to further integrate allied health services such as audiology within the primary care system, helping to improve Australians’
AudA also supports expanding the HSP to low-income and unemployed Australians. Image: TEERAPONG/stock. adobe.com.
access to multidisciplinary care. Audiologists play a vital role in primary care, providing essential services for hearing health that directly support better health outcomes. But Emerson said barriers such as limited Medicare funding, workforce shortages, and inadequate recognition of audiologists’ scope of practice continued to restrict access to these services. “Addressing these challenges through targeted government investment in funding models, direct referral pathways from audiologists to ENTs, ensuring audiologists achieve greater recognition through protection of title, and expanding workforce programs will improve equitable access to hearing care, particularly for vulnerable and underserved populations,” she said.
The HSP was an important measure already servicing pension concession card holders, veterans and referrals from the Disability Employment Service, Emerson said.
The recommendation put forward by the HHSA to expand the HSP to low-income and unemployed Australians would help make hearing services and devices more affordable for even more Australians, she said.
“The voucher program is essential to helping more Australians manage their hearing loss and other conditions,” she said.
Apple’s AirPods Pro 2 can now be used as hearing aids in Australia for adults with mild to moderate hearing loss after Apple updated software enabling use of the device’s Hearing Aid feature and Hearing Test in the region.
Apple announced on 26 March 2025 that Australia had joined more than 100 countries worldwide that are already using the features. “This experience includes a scientifically validated Hearing Test, a clinical-grade Hearing Aid feature, and Loud Sound Reduction,” Apple said in a statement.
It said the over-the-counter Hearing Aid capability supported people with mild to moderate hearing loss by “seamlessly transforming AirPods Pro 2 into a clinical-grade hearing aid.” This is based on a personalised hearing profile from the Hearing Test.
“The Hearing Test is intended for use by people aged 18 years or older, and the Hearing Aid is intended to amplify sound for
individuals 18 years or older with perceived mild to moderate hearing impairment,” Apple said.
Dr Nicky Chong-White, principal engineer at National Acoustic Laboratories said: “The new hearing features in AirPods Pro 2 are an exciting advancement — they give people a way to check their hearing and set up hearing assistance at home using familiar devices.”
The five-minute Hearing Test is based on pure-tone audiometry. Users can take the test themselves with their AirPods Pro 2 and a compatible iPhone or iPad that leverages acoustic science.
“When a user completes the Hearing Test, they will see an easy-to-understand summary of their results, including a number representing their hearing level in each ear, a classification, and recommendations,” Apple said.
“The results, which also include an audiogram, are stored privately and securely in the Health app on an iPhone or iPad, and

The AirPods Pro 2 transform into a hearing aid after doing the Hearing Test on an iPhone or iPad. Image: Apple.
can be shared with a healthcare provider to have more informed conversations.”
After setup, the Hearing Aid feature enables personalised adjustments so users have the sounds around them filled in and boosted in real time, Apple said. “This helps them better engage in conversations and keeps them connected to the people and environment around them,” it said.
Their personalised hearing profile was automatically applied to music, movies, games, and phone calls across their devices, without needing to adjust any settings.
Users could also set up the Hearing Aid feature with an audiogram from a hearing health professional. Apple said the Hearing Test feature was not a substitute for seeking medical advice from a healthcare practitioner if people had concerns about their hearing health.
A Loud Sound Reduction feature also minimises exposure to loud environmental noise.

Virtual Attendee Registration Now Open!
Register as a virtual attendee and gain access to a curated selection of recorded conference presentations from industry experts, available for online viewing from 11 April – 30 June 2025.
VIRTUAL ATTENDEE REGISTRATION RATES
Audiology Australia Member
Non-Member
What’s Included?
$515
$665
•Access to a selection of recorded presentations from the AudA 2025 Conference and additional content from conference partners.
•The to watch at your own pace.
•The opportunity to earn CPD points upon successful completion of quizzes or
Please note: Virtual attendee registration is not a live stream and does not include access to Keynote Speaker, Abstract, Learning Lab, or Masterclass presentations.
Enjoy a range of insightful presentations covering cutting-edge topics, including:
• Revolutionising audiological care with AI –Brent Edwards
• Person-centered care from the patient’s perspective –Shari Eberts
• Dementia and hearing loss: The critical role of audiologists – Christine Dunbar
• Evaluating the evidence on hearing loss and cognitive health – Prof Julia Sarant
• Closing the gap: Providing better healthcare access for people with intellectual disabilities – Dani Fox
• Help, there’s a musician in my clinic! – Dr Ian O’Brien
• Denis Byrne Memorial Lecture: The evolving landscape of audiology education – A/Prof Helen Goulios …and many more!

Register Now and Elevate Your Learning!
Secure your virtual seat and stay at the forefront of audiology innovation! For more information and to register, visit https://www.audaconference.com.au/virtual-attendee
Hearing Australia, with the support of the Australian Government, has announced the launch of a landmark program to help people at risk of isolation access vital hearing services including free hearing aids.
Ms Katy Gallagher, Minister for Government Services, welcomed the establishment of the nationwide initiative while visiting The Shepherd Centre in Canberra, a not-for-profit organisation providing support to families of children with hearing loss across Australia.
Launching on 1 July 2025, the initiative will be funded by Hearing Australia’s commercial operations. The program will provide free hearing assessments, hearing aids and support to at risk individuals who are ineligible for Australian Government funded hearing services.
The Profit for Purpose initiative will focus on people who are unemployed, people experiencing homelessness, and Aboriginal and Torres Strait Islander people aged 26 to 49.
“The Australian Government provides support to over one million children

and adults with hearing loss each year,” Gallagher said. “This announcement will allow Hearing Australia to help more Australians get the support they need, when they need it.
“This new program will open doors for vulnerable people not currently supported through the Australian Government’s Hearing Services Program and will build on Hearing Australia’s 78-year legacy of changing the lives of millions of children and adults with hearing loss.”
Those ineligible for Australian Government-funded services through the HSP will be supported. Image: Engima/stock.adobe. com.
Mr Kim Terrell, Hearing Australia’s managing director, said the organisation was committed to improving the lives of people with hearing loss, regardless of their age, location or background.
“Our mission is to provide world leading research and hearing services for the wellbeing of all Australians,” he said.
“Hearing loss can be devastating and it’s not something people ‘just have to live with’. Hearing loss can make it difficult for people to engage and communicate, impacting a person’s ability to learn or find work. It can lead to social isolation, impacting wellbeing and mental health.
“I know from my own personal experience that getting help and using hearing aids can improve your life – at home, in the workplace, and in social settings.
Hearing Australia will also work with its partners, including The Shepherd Centre and Cochlear, to invest in small community hearing health pilots and support research to advance treatment and prevention strategies.
New Australian research suggests cochlear implants may improve cognitive function and slow dementia symptoms in older adults.
Lead author, audiologist Professor Julia Sarant, who leads the Hearing Loss & Cognition Program in the Department of Audiology and Speech Pathology at The University of Melbourne, said she was excited to share the latest results of the COCHLEA (Cochlear Implant Outcomes & Cognitive Health – Longitudinal Evaluation of Adults) study.
“The results suggest cochlear implant use may actually improve cognitive performance and/or delay cognitive decline in older adults with severe-profound hearing loss for several years, promoting wellbeing and healthy ageing,” she said on the university’s Pursuit platform.
They suggested cochlear implantation may increase cognitive resilience/function, providing proof-of-concept evidence of the effects of hearing intervention with CIs on cognitive function, the researchers said when reporting findings in Brain Sciences
The prospective longitudinal observational study followed the cognitive performance of 101 adults aged 60 and over with severe to profound hearing loss and cochlear implants (CI) (mean age 74) over four and a half years. Their outcomes were compared with outcomes for 100 participants aged 60 and over with untreated hearing loss or normal hearing without hearing aids or cochlear implants. Computerised card games were used to assess cognitive performance before cochlear implantation and in both groups at each follow-up interval of 18-months.
“Cochlear implant users demonstrated significantly improved performance in executive function and working memory, as well as stability in attention, psychomotor function, and visual learning at 4.5-year follow-up,” the researchers said.
Untreated participants showed significantly greater worsening performance per year in attention and psychomotor function, and stability in working memory and visual learning at three-year follow-up.

Prof Julia Sarant, University of Melbourne, and a cochlear implant wearer. Image: Julia Sarant and Sarah/ stock.adobe.com.
“Our research found that both executive function and working memory performance improved and other cognitive functions remained stable for the cochlear implant group,” Prof Sarant said. The other participants declined significantly on two of four cognitive functions assessed, despite having much better hearing.
“It’s highly unusual to see cognitive performance improving significantly in ageing adults, and for this to be sustained over several years,” she said. “Even older adults with normal hearing are expected to decline cognitively over time as part of the natural process of ageing.”

Google’s updates mean people can change their hearing aid presets directly from their Android device settings. Image: trik/stock.adobe.com.

Google is rolling out updates to make Android’s hearing aid and screenreader experiences more accessible on phones.
The changes mean people can change their hearing aid presets directly from their Android device settings.
Starting with the Samsung Galaxy S25, the company said it was bringing the benefits of the next generation of Bluetooth to GN Hearing and Oticon Intent hearing aids, using new LE Audio technology.
“For people who are d/Deaf or hard of hearing, we’ve brought LE audio features, the next generation of Bluetooth, to Galaxy S25 devices,” Google said.
“This update enables easy hearing aid management, hands-free calling, easy-to-use personalised audio adjustments and a low-latency connection to GN Hearing and Oticon Intent hearing aids when paired with a Galaxy S25 device using Android 15.
“This new integration will be available on the Pixel 9 with Android 16 beta and come to Galaxy S25 with Android 15 in coming weeks.”
A Google Australia spokesperson said the update would work in Australia on Google Pixel 9 and Samsung S25 devices. Google revealed Auracast broadcast audio is coming to Android, meaning people can tune into Auracast broadcasts from TV streamers or public venues. “This also means hearing aid presets, available within your phone settings, can be conveniently applied to broadcasts to personalise streams to your hearing,” it said. “We’re bringing to Pixel 9 devices the ability to connect to broadcasts through QR codes . " "To use Auracast, pair LE Audio compatible hearing aids from GN Hearing and Starkey with Samsung Galaxy devices with One UI 7 and Android 15 or Pixel 9 devices running the Android 16 beta and tune into Auracast. broadcasts from compatible TV streamers or public venues."
Leading Ménière’s disease researcher, Prof Jose Antonio Lopez Escamez. Image: Kolling Institute.
The inherited or genetic form of Ménière’s disease may be more common than first realised, according to Kolling Institute researchers who have discovered a new gene mutation for the disease.
In a crucial step towards a better understanding of Ménière’s disease, researchers at the Kolling Institute and the University of Sydney discovered the mutation which they believe could greatly inform future treatment of the condition.
Meniere’s can be an inherited condition with about 10% of patients having one or more relatives affected by it. The new research, led by world leading Ménière’s disease researcher Professor Jose Antonio Lopez-Escamez, indicates the inherited or genetic form of the disease may be more common than first realised.
His team discovered a rare mutation of the GJD3 gene in both patients with and without a genetic history of the disease. They reported their findings in Genome Medicine on 15 January 2025.
It is the first time this gene has been
linked to any disease.
More than 400 people with Ménière’s disease were involved in the study, with 18 people or 4.4% of the group found to have the genetic mutation, a statistically significant percentage.
“Many people will say that they don’t have the genetic form of the disease, but this research indicates there are many more people whose disease is directly linked to their genetic make-up,” Prof Lopez-Escamez said.
“This is important as it will inform how we treat the disease going forward, particularly given the different forms of the disease and the exciting advances with gene therapy.”
The research also identified a connexin (connecting protein) linked to the GJD3 gene in the tectorial membrane of the organ of Corti (the hearing organ).
“This is the first time that a connexin has been found in this part of the ear, and it may support the view that connexins regulate the microenvironment in the ear and influence hearing,” he said.
Children who play video games are more likely to develop hearing loss than non-gamers, the World Health Organization (WHO) and International Telecommunication Union (ITU) have warned after launching the first global standard for safe listening in video game play and esports.
Nearly 50% of people aged 12 to 35 years are at risk. Image: The World Health Organization.
The organisations said children who actively participate in video gameplay activities are twice as likely to have high-frequency hearing loss

compared to non-players. They risk permanent hearing loss from prolonged exposure to loud sounds while gaming or listening to music. Children are particularly vulnerable due to their lower sound tolerance.
The evidence-based WHO-ITU global standard on safe listening for video gameplay and esports was launched for World Hearing Day (WHD), 3 March 2025. It aims to reduce the risk of and prevent hearing loss among the world’s three billion gamers. Previously no safe listening guidelines or standards existed for video gameplay devices or software.
The WHO also warned that more than one billion young people face the risk of permanent hearing loss due to unsafe listening practices such as prolonged exposure to video games and loud music. It said nearly 50% of people aged 12 to 35 years are at risk of impaired hearing due to excessive exposure to loud sounds including music they listen to through personal audio devices, smartphones, or at music gigs or clubs.

Ten of 12 children with profound genetic hearing loss who received Regeneron Pharmaceutical’s gene therapy showed “clinically meaningful, notable improvements in hearing” the 48th ARO conference has heard.
Latest results of the phase 1/2 CHORD clinical trial were presented at the Association for Research in Otolaryngology’s annual midwinter meeting in Florida, America on 24 February 2025.
The children, ranging from infants to teenagers, were from countries including the US and the UK. All had received at least one post-treatment assessment.
In the first child treated, speech and development progress followed dramatic improvements in hearing.
One of the children, British baby Opal Sandy made global headlines in May 2024 when it was revealed that
Biotech company Regeneron announced updated data from 12 children in the trial of the investigational gene therapy DB-OTO. They all had profound genetic hearing loss due to variants of the otoferlin (OTOF) gene. These included 72-week results showing speech and development progress in the first child dosed at 10 months of age, and initial results in 11 children (aged 10 months to 16 years old) including three who received DB-OTO in both ears.
Trial investigator, Dr Jay Rubinstein, Virginia Merrill Bloedel Professor of Otolaryngology and Bioengineering, and Director, Bloedel Hearing Research Center, University of Washington School of Medicine, reported findings at the ARO conference.
“A year after treatment in one ear

Otolaryngology professor Dr Jay Rubinstein reported findings. Image: Jay Rubinstein.
bedtime reading when the cochlear implant on their other ear was removed,” he said.
“These seemingly small interactions are life-changing for these children as well as their families and these results continue to underscore the revolutionary promise of DB-OTO as a potential treatment for otoferlin-related hearing loss.”
Nine of the 12 participants received the therapy via an intracochlear injection in one ear and three received it bilaterally.
Regeneron said DB-OTO was an investigational cell-selective, dual adeno-associated virus (AAV) vector gene therapy which aims to deliver a working copy to replace the faulty OTOF gene using a modified, non-pathogen virus.
The virus is delivered via an injection into the cochlea under general




Share Products that deliver new experiences for your patients
Looking to diversify your practice and provide higher levels of hearing care?
Are your clients after the latest in hearing protection technology? Contact Auricle Digital and Challenge what’s possible.
"As soon as it started, I was in tears. It was the most incredible experience,"

The dawn of a new era of
Sydney Opera House is the first major cultural institution globally to introduce revolutionary Auracast broadcast technology, setting a benchmark for accessibility in the arts and removing barriers for people with hearing loss.
In a world first, hearing aid manufacturer GN, Hearing Australia, National Acoustic Laboratories and the Sydney Opera House have collaborated to bring Auracast broadcast audio technology to the iconic venue. The ‘hear the future’ event on 18 March 2025 was an overwhelming success, indicating live performances are about to get a whole better for people with hearing loss.
A highlight was the emotional reactions of people in the audience with hearing loss who, for the first time in years, could hear music and vocals the way they are meant to be experienced.
Auracast is a Bluetooth Low Energy (LE) Audio technology, and streams high-quality audio to unlimited listeners, making it ideal for large venues and public spaces. Sound quality is described as excellent with

GN, the first manufacturer to pioneer hearing aids that connect with Bluetooth LE Audio and Auracast, had been working with technology companies for years to ensure hearing aid users have early access to the breakthrough technology in venues globally.
The Opera House became the first global cultural institution to fit Auracast transmitters into its Drama Theatre, Playhouse and studio venues for hearing aid users. The advanced assistive listening technology provides access to high-quality broadcasts from a nearby transmitter through hearing devices to Auracast-compatible audio devices.
It’s a major step forward in removing barriers and achieving greater inclusion for the one in five people globally who live with hearing loss.
MC Mr Osher Günsberg, TV presenter, former roadie/DJ and hearing aid user, welcomed representatives from the audiology sector, the deaf and hearing loss community, industry and media to experience the technology. They heard a live performance broadcast directly to hearing aids and earbuds featuring the powerhouse vocals of singer Dannielle Cartisano enhanced by the magic of Celeste Strings ensemble.
GN has integrated Auracast across its entire new Beltone and ReSound hearing aid portfolios and introduced an app-based Auracast Assistant. (See p34). Event attendees who did not wear hearing aids experienced Auracast using Samsung Galaxy Buds3 Pro.
Next level emotional response
“As soon as the music started, I had tears in my eyes; it was an emotional reaction,” said hearing aid wearer Ms Marian Jones. “I haven’t heard like that for so long, the whole breadth, how natural it sounded and the distinction between the instruments.
“People without hearing loss listening to it today might think it was good, but for someone with hearing loss, it was next level.”
Jones said music had always been a compromise. “I go to events knowing I will not have the same level of engagement as everyone else and miss some things. Live music is one of life’s great joys but like many people with hearing loss, I’ve found my enjoyment has been dulled by poor sound quality or being restricted to certain seats. I’ll go more now because I know it’s going to be great.”
Jones, principal research audiologist at Cochlear, added: “Hearing the beautiful music via Auracast was the crispest and clearest experience I’ve had in years. It was quite emotional to see the reactions from others with hearing loss at the performance. This is so important to drive forward accessibility.”
Günsberg, who spent years avoiding social situations due to hearing loss before receiving hearing aids, said he also found it very emotional to feel that again. He said the venue was now a beacon of accessibility. “With telecoil I struggled to hear, but this is game-changing technology for millions of people worldwide and will make the world more inclusive and accessible,” he said.
Representatives from Samsung Electronics, Google and the Bluetooth Special Interest Group (SIG) underscored the support for Auracast and its potential to enhance accessibility across a range of devices and platforms. They showcased Auracast-enabled products that demonstrated how it enhances listening experiences in public spaces and venues.
Hearing aid users can face barriers at live performances, with current assistive listening systems such as induction hearing loops optimised for speech while music can sound distorted. Available seating in theatres and other arenas is often limited for loop wearers to areas with coverage.
Mr Peter Karlstromer, GN CEO, travelled from Denmark and said Auracast would make the world of sound inclusive for everyone. “We are at the forefront of bringing Auracast to hearing aid wearers so they can easily connect to and enjoy great sound no matter where they are.
“We are very proud to collaborate with the Sydney Opera House, National Acoustic Laboratories and Hearing Australia to enable Auracast and inclusive performances at this iconic venue. We hope it will encourage more to follow suit and enter the next era of connectivity; it’s time to get Auracast out to the world and make it standard across all industries.”
While telecoil did not provide the full experience or frequency range and was difficult to connect, Auracast provided hearing aid users the richest possible experience, he said.
Ms Janelle Ryan, Sydney Opera House senior manager impact access and operations, said the technology helped remove barriers to the arts and engage audiences more meaningfully.
“It literally took minutes to install compared to hearing loops that can take half a day, and didn’t interrupt the fabric of the building. It was extraordinary – almost plug and play,” she said.
“The community will come and drive a groundswell of support for more venues to have this technology.”
Opening the event, Ms Ingrid Dahl-Madsen, Danish Ambassador to Australia and New Zealand, said she was excited to celebrate the new era which represented a significant leap in accessible listening globally and in Australia. She highlighted the connection between Denmark, a global leader in hearing technology innovation, and Australia, home to the Sydney Opera House, designed by Danish architect Jørn Utzon.
During a panel discussion, Ms Emma Scanlan, Hearing Australia principal audiologist for adults, said Auracast was so important because it normalised hearing assistance for everyone and would enable people with hearing loss to access many more environments.
“It’s not all about speech, music has been one of the most difficult areas


for people with hearing loss to engage with,” she said.
Dr Padraig Kitterick, NAL’s head of audiological science, said barriers to hearing affected every aspect of life but technology enabled people with hearing loss by giving them tools and teaching them to connect. Auracast was brilliant because it was universal and for everyone.
He said loops and telecoils were important to support speech and Auracast was not a replacement for telecoil, but it had a bigger range of benefits including music and high-quality low latency stereo stream.
Ms Noelle Chun, Google’s senior product marketing manager from the US, said it was committed to accessibility and some Android phones were now supporting Auracast. “The Auracast promise is huge for us and Android, and Google, hopes to introduce it to more phones,” she said.
Günsberg concluded: “It’s the dawn of a new era of accessibility.”

Queensland audiometrist MIKE CARTER, 73, is reluctantly retiring after devoting nearly five decades to changing lives through hearing care. His story provides a fascinating glimpse of the industry in Australia and New Zealand throughout his time.
Mr Mike Carter’s 48–year career in hearing care has at times been a rollercoaster. He has ridden the highs and lows, including being a victim of a crime that saw him lose everything, only to start again and rebuild in another country.
Through it all Mike’s commitment to provide the best hearing care possible, to thousands of patients, has never wavered.
Mike’s Dad, Rex Carter joined the industry in New Zealand in its pioneering stages.
“He invented a couple of the big old body hearing aids – pocket talkers –which I still have,” Mike recalls. “He designed them for British Hearing Aids but didn’t get any money out of it – that wasn’t a thing in those days.
“A lot of people didn’t know that because Dad was a quiet achiever, working in the background. He had his own clinic and helped set up some of the hospital clinics in New Zealand in the early days “
As a young man, Mike moved to Sydney and worked as a troubleshooter for a Japanese company Koyo, earning about $50,000 annually – a lot of money in those days, he says.
“Dad called me 48 years ago when I was 25 and asked me to come home to work with him for about $300 a week,” he says. “I did because I thought it would be more fulfilling and less stressful.
“We started Gemini Hearing and exclusively did home visits around Auckland doing hearing aid fittings. We would test the clients and come back and make the hearing aids in our own factory; they were all custom made back then.”
Changes in technology have been nothing short of amazing, he adds.
“We used to walk around with a screwdriver to adjust hearing aids but
now you need a laptop and (internet/phone) connections,” he says.
“Dad made a hearing aid that was skin colour to blend in with the ear and it had two little gold pins on it. To adjust the volume, wearers would remove the pins, wet their finger and touch it.
“Nowadays, you’re wearing computers. I have high frequency hearing loss from noise exposure at work, since we had no hearing protection in those days, and I wear hearing aids. Manufacturers I deal with allow me to ‘trial’ the latest hearing technology so I can give feedback to them.”
After working with his father for a few years, Mike ventured out on his own and set up his own audiology business. Over many years of hard work, one clinic expanded to 26 across New Zealand in Auckland, other parts of the North Island, and Christchurch.
“We were one of the first chains of hearing aid clinics in New Zealand,” he says. “We employed audiologists and set up clinics in shopping centres and doctors' rooms. Some in the industry knocked us because they said we were treating it as retail but now everybody does or at least has a major retail component.”
Mike has travelled the world with the industry. “The manufacturers we were dealing with in the early days regularly flew me to the US and Singapore. I gained a wealth of knowledge from these trips,” he adds.
Business was good but a significant setback occurred when Mike contracted hepatitis in Mexico and was off work for 12 months.
Unfortunately, the company's finances were left to his accountant.
“The accountant he had employed ripped him off, leading to the loss of
the business,” his second wife Trish adds. “The accountant was eventually jailed but Mike lost everything.”
Mike and his family – first wife Becky and two children – migrated to Australia to start again.
He opened one store, Carter Hearing, in Wynnum, Queensland. Unfortunately, Becky died soon afterwards, and he faced another challenge – raising his children as a single father while trying to rebuild his business.
Again, he triumphed over adversity and Carter Hearing grew to include six permanent clinics. One opened in a shopping centre in Broadbeach and is still operating.
“We were the first to have a retail outlet in a shopping centre in Queensland and were trailblazers,” Mike says.
He later married Trish, who had a nursing background, and she joined him in the business. Carter Hearing later incorporated partners to grow the business to 13 clinics in both New South Wales and Queensland under the names Carter Hearing and Allied Hearing.
In 2014 Mike, Trish and partners sold Carter Hearing and Allied Hearing to Hearing Life after being approached with a good offer.
Mike and Trish later formed Total Hearing which has three permanent sites in Brisbane and near Sydney. The hearing industry connection has continued through three generations as the couple’s daughters, Ms Amy Green, who works in one of the Brisbane clinics, and Ms Kate Robertson, who now works for another independent audiology practice outside Melbourne, are both audiometrists. They have worked in the industry for more than 18 years.
One day a patient in his mid-60s who was also from New Zealand came into Total Hearing in Brisbnane and for some reason Mike decided to show him a photo of his father. “The patient said, ‘I know him’ and it turns out Dad fitted his hearing aids when he was a child,” Mike recalls. “He was fitted quite young and still remembered him.
“The amazing thing was this man happened to randomly come into our clinic and had a consultation with my daughter Amy, the grand-daughter of Rex, his original practitioner.”
Apart from helping thousands of patients over decades and teaching them much about hearing care, Mike reflects on the importance of listening to patients and learning from their experiences. Over the years he has followed the advice of several clients including one who advised to dress casually to make patients feel more comfortable.
“In those days we wore suits, and I was called to a shop for a hearing aid fitting in New Zealand for a client called Lady Wattie,” he recalls. “I went in and one woman was wearing gumboots and the other was dressed like the Queen. I approached the one dressed like the Queen and inquired, ‘Lady Wattie?’
“She said ‘no’, so I went to the one in gumboots who told me later as I got to know her, ‘Don’t wear a suit to work because if you wear smart casual

clothes instead people will feel you're on the same level,’ and I’ve never worn a suit to work in the 40 years since.”
Another lesson, learnt in America , was to never put a desk between patient and practitioner.
“Don’t put the desk in front of you, put the desk against a wall and the person beside you so you haven’t got a barrier on the journey. You do the hearing aid journey together,” Mike explains.
Trish says her husband is incredibly service orientated. “We've always run our businesses with that in mind from the front desk right through. Leading from Mike, there’s no one person more important than the next.”
Mike also emphasises the importance of client relationships and business acumen. “I say to clients, when I’m selling hearing aids, I have to be a good salesman because I’m selling you something you don't want. I also put one hand up in the air and the other down below and say we meet in the middle.”
His father was still selling hearing aids while aged in his 80s, highlighting his dedication to the profession. Before he died at 85, he was even trying to sell hearing aids to a man in hospital in the opposite bed, Trish recalls.

While Trish, Total Hearing’s operations manager, and Mike are in the process of selling their last business so they can retire, his retirement plans are different from his father’s. He plans to spend more time volunteering with the RSPCA and driving its local wildlife ambulance.
Some voluntary hearing care work may also be on the cards as many years ago he flew fortnightly to Fiji from New Zealand to work with an ENT surgeon in a medical centre.
Mentoring is another possibility. “There’s many new startups now and Mike and I were saying the other day it’s almost a tragedy that there's so much knowledge between the two of us that’s not being shared; we could help people,” Trish says. “Mike knows how to win and lose, and that's invaluable."

Those behind NAL-NL3 discuss everything audiologists need to know about the updated hearing aid fitting formula, now featuring a suite of prescriptions rather than a one-size-fits-all solution.
Modern day audiology clinics face all kinds of complex problems, but there’s one patient cohort that creates a high degree of uncertainty and indecision.
Those with audiometrically normal hearing tests (minimal or no audiometric hearing loss) – who have trouble hearing in noise – are a particularly challenging set of patients who can be disillusioned after being told their hearing is 'normal'.
The practitioner can be left wondering how they can optimally manage such patients.
It’s a problem the new NAL-NL3 hearing aid fitting formula hopes to address, along with a raft of other updates unveiled by the National Acoustic Laboratories (NAL), which has developed hearing aid fitting formulae used by clinicians globally.
Estimates suggest half of new clients walking into audiology clinics fit in this category (no audiometric hearing loss), Dr Padraig Kitterick, NAL head of audiological science who has overall responsibility for delivery of the project, tells HPA
Another key change advises how to fit hearing aids to help other clients hear better in noise. "The point is making hearing aids acceptable and beneficial even if you've got little or no audiometric hearing loss, to help you hear better in noise,” Dr Kitterick said.
With NAL director Dr Brent Edwards, he revealed details and evidence behind the new program at the American Academy of Audiology conference in New Orleans on 28 March 2025.
Dr Kitterick says NAL has been at the forefront of hearing aid fitting prescriptions for decades. Its NAL rule was launched in 1976, a revised rule in 1986 and in 1999 the NAL-NL1 algorithm was released.
“It was the first non-linear formula from NAL and was revolutionary because it started what is still used today, a process of using computer models to find the best way to program hearing aids to maximise speech understanding,” he says.
“That was superseded about 12 years later with NAL-NL2, which became the most popular and widely recognised fitting algorithms available globally, compatible with Windows or mobile apps.”
NAL-NL2 is the second generation of prescription procedures for fitting wide dynamic range compression instruments. Like its predecessor NAL-NL1, NAL-NL2 aims at making speech intelligible but without making sounds too loud. NAL-NL2 is the world’s most widely used fitting prescription for hearing aids to date.
“When NAL launched NL2 it was a huge step forward and kept with the same type of approach, using computer models and evidence to find the best

targets,” Dr Kitterick says.
“It included a lot of information we had learned about fitting hearing aids, such as how we should adjust hearing aids based on somebody's experience of using them, whether users are male or female, or they primarily listen to tonal languages versus non tonal languages like English.”
These empirical adjustments were learnt from decades of using NL1.
Dr Kitterick says NAL surveyed clinicians worldwide asking for use cases where NL2 was not providing the best solution for their clients.
“We got a lot of feedback and consistency across clinicians from around the world,” he says. “They said it worked really well for most clients, but they identified pain points.
“They told us that sometimes NL2 prescribes too much compression and can prescribe too much gain for specific kinds of hearing losses like mixed losses and reverse sloping losses. Data from hundreds of thousands of hearing aid fittings also suggested that often for many users, particularly new hearing aid wearers, NL2 prescribed too much high frequency gain that did not really improve intelligibility in a meaningful way."
Apart from clinical pain points, there were a lot of hearing needs and use cases that NL2 didn't address. “One is how to fit hearing aids to people with minimal or no audiometric hearing loss, and the other is how do we help our clients with hearing loss who use hearing aids listen more comfortably in noisy situations? These are two important needs we're addressing for the first release of NL3 later this year,” Dr Kitterick says.
“A key new feature of NAL-NL3 is the shift from one prescription for everybody to a modular system that we will expand over time that contains a suite of different prescriptions to achieve different things.

Same approach as NL2 for quiet environments
Dr Kitterick says there are different philosophies and ways of solving the problem of how best to fit hearing aids. When fitting the best option for patients who want to listen and understand well in quiet environments, NL2 has remained the gold standard since its release 15 years ago.
“It is well validated and well understood. We’re keeping that same philosophy for quiet and are fixing pain points with it, making it even more effective by bringing the latest machine learning approaches and over a decade of experience with fitting NL2.”
"The minimum hearing loss module has a very different philosophy from NL2. All our prescriptions to date are based on the idea that you’re amplifying sounds to make them audible (compensate for hearing loss) and therefore make speech understandable,” Dr Kitterick explains.

“That's the primary thing we're trying to do when we fit hearing aids. But for people with minimal or no (audiometric) hearing loss, our existing solution in NL2 would provide no amplification because it was based on the assumption that the person using the hearing aid would have a hearing loss.
“Hearing aids are amazing devices that can remove noise and make it easier to listen. The minimum hearing loss module we're introducing with NAL-NL3 adopts a completely different philosophy from NAL-NL2 on how sounds should be amplified by the hearing aid.”
The goal of the new module is to make hearing aids both acceptable to new hearing aid users with minimal or no audiometric hearing loss while also ensuring they help them to hear better in noise.
Dr Kitterick says practitioners often thought that telling these patients they have normal hearing was reassuring, but if they're having problems in noise, what they often want is a recommendation for which solution could help address their listening difficulties. “We get lots of queries from around the world from practitioners who saw our research on the benefits of hearing aids for these individuals,” he says.
“Practitioners keep asking – but how do I fit them? And that's what we're going to solve with NAL-NL3’s minimum hearing loss module.”
Another feature of NAL-NL3 is a comfort in noise module. Dr Kitterick says every audiologist knows most people coming to their practice who are motivated to take up hearing aids are not sitting in quiet rooms all day. They want to use their hearing aids in the real world – and that world is a noisy place.
“We don’t believe NL2 is the best we can do to fit a hearing aid when the

use case is listening in noise. Our NL3 noise module maximises comfort in noise without sacrificing speech intelligibility. It gives a much more comfortable experience but maintains the focus on maximising speech understanding that has been at the core of NAL hearing aid prescriptions for decades.
“NL3 is both an evolution and a revolution. The evolution is that it provides a replacement for NL2 that builds on a solution which is widely validated and trusted, but we're addressing pain points and making a better version. The revolution is the new modules that address specific unmet needs where existing prescription formulae do not provide a suitable solution."
“We will grow and improve modules over time and have started to reach out and talk to practitioners, manufacturers and providers about what are other key use cases that are most important to address for future modules such as non-speech focused modules like listening to music.”
The changes were introduced due to practitioner demand and to address needs that were not being met. They were also driven by technology improvements. NL2 was based on computer models that maximised speech intelligibility and was a very early use of machine learning to maximise outcomes with hearing aids.
“With our noise module we want to make speech much more comfortable when listening in noisy environments without sacrificing intelligibility. Intelligibility is core of the key new parts of NL3 but importantly in two out of three cases, it's intelligibility in noise to reflect how most people are using hearing aids today.”
NL3 is a team effort and one of the most important projects NAL has done. It involved every NAL employee including audiologists, signal processing engineers, and engineers with expertise in hearing aid design and manufacture, machine learning and artificial intelligence.
Promising results
Dr Kitterick has been involved in running in-house studies and in clinic studies for a while – and they’re seeing “exciting and important findings” that verify these new philosophies do deliver the benefits they’re seeking with the new modules. “We have evidence from our trials to demonstrate the new minimum hearing loss module significantly improves speech understanding in noise, while not impairing speech clarity, naturalness and comfort of listening, making hearing aids acceptable to people with minimal hearing loss or normal (audiometric) hearing while delivering significant speech benefits,” he says.
” Our trials also show that our new noise module can significantly improve people's comfort in noise. The way we have shown that is to send hearing aid users out into the real world and get them to report back which option they prefer – hearing aids fitted on our noise module or the existing quiet module from NL2 but improved in NL3.
"Our listeners showed significant preference for the noise module when listening in noise and our lab-based studies showed they received no detriment in their speech intelligibility from using the noise module. Trials are occurring using NL3 as a drop-in replacement for NL2’s general fitting formula. About 30 clinicians across more than 25 clinics have done almost 600 REM sessions with their clients using NL3.
"We're getting feedback and learning a lot so when this new solution is released, it will be a tried, well tested and verified solution. It's exciting to have the first patients being fit so we can get feedback from the clinical coalface that this is working as we would like it to.” Hearing Australia clinics including its Innovation Centre, and Hearing Savers clinics, a member of the Hearing Business Alliance, have taken part in the trials.

Earplugs are more popular than ever, with sales of customised versions from hearing practitioners thriving along with online and in-store varieties. Able to be used in many situations, they’re making work and leisure safer while better design is improving comfort.

t seems there’s an earplug for just about everything these days. No longer do they only help prevent hearing loss in noisy workplaces; they also improve musicians’ lives, block snoring and aid sleeping, prevent infections from swimmers’ and surfers’ ear, and assist people with autism and other noise-sensitive conditions by reducing overwhelming sounds.
They’ve even become trendy among young people who – with increased awareness of the potential for loud music to damage their hearing – are sporting earplugs at concerts and music festivals, particularly opting for high-fidelity devices. Studies show prolonged exposure to noise levels above 85 decibels (dB) can lead to hearing damage, and typical festival sound levels can soar up to 100 dB or more.
High fidelity earplugs can also help tinnitus patients, and motorcycle enthusiasts are another group increasingly adopting earplugs for hearing protection.
This surge in popularity is something an increasing number of independent audiology clinics in Australia are leaning into, with custom-made earplugs adding a small point -of-difference and cementing the reputation of hearing practitioners as established professionals.
The Earplugs Global Market Report January 2025 from market research company, the Business Research Company, provides evidence that the market has grown strongly in recent years. The report estimates it will grow at a compound annual growth rate of 6.1% from $1.09 billion in 2024 to $1.16 billion in 2025 and $1.45 billion by 2029.
This is due to increased use of 3D modelling and printing earplugs for military application, growth in construction and manufacturing industries, and rising popularity of music festivals and concerts, it says. A rise in noise pollution, increase in awareness of the benefits of hearing protection, and increased use among singers and musicians are also driving this.
Major trends in the forecast period include technological advancements in comfort and design, advancements in noise-cancellation technology, materials, integrations with health monitoring sensors, and adoption of personalised fit through 3D printing.
Age-related hearing loss is another trigger for growth in the market as people with hearing loss may be more susceptible to noise-induced damage and tinnitus.


The report categorises earplugs as electronic and non-electronic. Electronic earplugs include active noise-cancelling earplugs, communication earplugs and Bluetooth earplugs while non-electronic versions provide passive noise cancellation and are made of foam or silicone. They can be custom molded or flanged.
Users include construction workers, miners, consumers and those working in forestry, military, mining and manufacturing industries. Healthcare is another industry where workers can be exposed to noise and increasingly dentists and their assistants, operating room nurses and orthopaedic surgeons who are frequently exposed to loud noise, are wearing earplugs.
Lions Hearing Clinic at the Ear Science Institute Australia provides custom-made earplugs and says some companies make certain types of earplugs, such as sleep plugs, to minimise noise distractions at night and block out snoring.
It says sometimes people need hearing protection but also need to communicate with others through a phone or radio such as workers on noisy construction sites. “Communication plugs start with a custom noise plug, then your audiologist will add an earpiece,” it says. “The combination of the plug and earpiece protect your ears from noise, whilst maintaining your ability to communicate at the same time.”

and became the first JHAudio supplier in Australia.”
Jerry Harvey (JH) Audio are pioneers of custom in-ear monitors used by engineers and top performing and touring artists.
Custom earplugs protect hearing better for people who work in noisy workplaces than one-size-fits-all solutions as they are designed to fit ears perfectly, the clinic advises.
Musicians’ earplugs contain a special filter that controls the type of noises being reduced and keeps the sound people want to hear from sounding muffled.
Sydney audiometrist Mr John Lucchese is ideally placed to help musicians with their custom ear protection. The former sound engineer and opera singer is co-owner and co-founder, with his wife Kylie, of NS Audiology independent audiology clinics based in St Leonards and at Five Dock.
“When we started in audiology, we immediately started servicing the arts,” he recalls. “We learnt all we could about the special needs of the music industry
“This led to us taking very specialised ear impressions for various custom audio products, including ear protection,” Lucchese says. “We have been in practice for many years and have built a reputation for outstanding ear impressions.
“With our connections in the music industry we have serviced clients from A list performers, engineers and audiophiles to TV broadcasters and entire casts for shows such as musicals and circus.”
While the earplug depends on the needs of the specific client, he uses 64 Audio, GN Musician HearSavers and Etymotic products the most. “We are also finding it more common that clients are purchasing custom ear protection online and coming to us for the ear impressions. There are so many products out there now.”
Lucchese believes their experience in taking specialised ear impressions is what sets them apart.

“We have done hundreds of ear impressions for a range of industries and for many custom ear products,” he says. “Having this experience means that when it comes to custom products, we get it right first time, every time.
“We also provide our clients with a 3D scan of their impressions, so if they would like a different kind of custom product made, they already have their impressions on hand.”
There are many new products in this space, Lucchese says. “As little as 10 years ago, there were only a few generic plugs available and customs were just emerging,” he says.
“The attenuators used in custom hearing protection plugs have improved greatly, offering much flatter responses which are able to attenuate very specific sound sources, such as gun shots for shooters and hunters.”
Emerging trends include manufacturing earplugs with AI algorithms and 3D printing techniques, he says. Also, the younger generation are more aware of protecting their hearing and there is not as much stigma around wearing ear protection.
“We have many younger clients who want custom products to wear at music festivals and out clubbing,” he says.
While 3D scans of the ear are already happening and have been used in the hearing industry for hearing aid manufacture for many years, Lucchese says there are now new scanners which can be used for custom hearing protection and in-ear monitors.
“One drawback is that the scanners are still quite expensive but over time this will reduce and the transition to no physical impressions will be industry wide,” he predicts.
Superior outcomes start with a good impression, he adds. “It all starts with a
really good ear impression. Manufacturers of custom ear products have their own preferences, so it’s important to check this before doing an impression as this impacts the manufacturing process.
“Some manufacturers want open-mouthed impressions with the use of a bite block, but some don’t require that. Also, for in-ear monitors, the second bend in the external auditory canal is vitally important in the impression, so they can direct the drivers towards the tympanic membrane.”
Information and understanding is paramount. “Informing clients on how hearing protection can be part of the solution and giving them some understanding about loudness and how long they can be exposed to loud sounds without the possibility of suffering hearing loss, will also ensure that your clients are able to look after their ears in loud environments,” he says.
Gold Coast hearing specialist Mr Partho Pal believes shifting attitudes toward earplugs and hearing protection have contributed significantly to their rising popularity. “With more people using AirPods, earbuds, and headphones, the idea of wearing something in your ears has become normalised,” he explains.
He says while active noise cancellation features in consumer devices can help reduce general environmental noise, they are not effective against industrial noise.
Pal achieved his Bachelor's in Audiology and Speech Pathology and a Masters in Hospital and Healthcare Administration in India and has worked as an audiologist in several parts of the world but practises as an audiometrist in Australia.
He founded Australian Audiology Hearing Specialists, a Queensland-based company, 15 years ago as a contractor service provider. Early in his career, he performed industrial hearing tests for airline staff and other workers.
Pal held contracts with Lifestyle Hearing and Bay Audio before opening his own clinic in Tweed Heads. Today, the business has grown to five clinics, offering a wide range of hearing aids, primarily in the low to mid-price range. The practice serves adults and children and offers Hearing Services Program services as well as custom earplugs.
His extensive experience includes working with Aboriginal communities in remote Western Australia, where he helped implement newborn hearing screening protocols.
During his time in hospitals across Derby, Broome, Kalgoorlie, and the Kimberley, he regularly treated mine workers. “If someone was exposed to a blast or needed urgent care, they were referred to the hospital,” he recalls.
He has witnessed significant advancements in hearing protection over the years. “We started with basic soft-moulded plugs, then moved to 3M cushion-style plugs,” he says. “Now, we can check attenuation levels. Brands like ReSound, Starkey, and Pacific Ears offer filters allowing us to choose attenuation levels – 10, 14, or up to 25–26 decibels.”
Modern noise filters are more comfortable and versatile, allowing users to maintain some level of communication, he adds.
Pal says active electronic earplugs widely used by the US Defence Forces



Swimmers’ earplugs help prevent otitis externa, while surfers’ earplugs prevent exostosis.
have been revolutionary but are unsuitable for mining environments, where any electrical discharge could pose a risk due to underground gases. In such cases, passive noise filters remain the standard.
Growing demand: Snoring partners drive sales
Since he began working in the field, the hearing protection segment has gained significant momentum, helping independents like his add another string to their bow.
Demand for earplugs has grown steadily, particularly for sleep-related issues.
“It’s still a small part of our business, but we’re seeing more people come forward – mostly one partner snoring while the other can't sleep,” he explains.
He often refers clients for medical evaluation to rule out sleep apnoea, while offering both custom-fitted and standard soft foam plugs. “The soft sponge ones, like the 3M squishy plugs, are very effective – offering up to 40 dB attenuation, and they’re disposable and affordable.”
In industrial settings, trays of foam plugs are commonly made available, with staff encouraged to use them, he adds.
For custom options, Pal takes either physical or digital ear impressions, which are then sent to (GN) ReSound, Starkey or Pacific Ears for production. “These brands offer comparable levels of protection,” he says.
“For musicians' plugs, musicians don't want too much attenuation and prefer 18 dB attenuation because they want to listen and enjoy the music and feel the music, especially the drummers.
“We also have motorbike enthusiasts whose mufflers are very loud. They do recreational riding for maybe one, two or five hours, and even that can severely affect their hearing because they’re on top of that motorbike for so long.”
Apart from recommending earplugs for motorcyclists, Pal also suggests they wear padded gloves because “what most people forget is that vibration can also damage hearing”.
“Vibrations travel through bone conduction so often with miners or somebody using a jackhammer, they need to have protective gloves. It's not only the noise over the years, but they need protective gloves to stop the vibrations from traveling via the bones into the cochlea and damaging the cochlea,” he says. Being on the Gold Coast, Pal also fits a lot of ear plugs for swimmers and surfers. “They all need ear protection because they're aware that as they grow older, they can get ‘swimmer’s ear’,” he adds.
Swimmer’s ear, or otitis externa, is an infection or inflammation of the skin in the outer ear canal, often caused by water trapped in the ear after swimming, creating a moist environment for bacteria and fungi to grow.
It can be painful, itchy and muffle hearing but can be treated with eardrops prescribed by doctors containing antibiotics, steroids, or acidic solutions to treat the infection and reduce inflammation.
Exostosis is another condition that earplugs can help prevent. These benign bony growths that extend outwards from the surface of a bone often appear as a bump or spur. They can occur in the ear canal and can cause pain.
“Exostosis is common around the Gold Coast with surfers and to prevent them you need to have protection from the splash of the water,” Pal says. “It's not only the cold water, but the splash which can lead to exostosis. It’s basically the body's defence mechanism to protect the eardrum from any sort of harm or injury.”
Pal warns that at-home impression-taking kits to order online earplugs, rather than being seen for a proper fit, provide “a high chance of people not being able to take the impression correctly”.
"The biggest challenge is you have to go up to the second bend in the ear canal and that is quite deep,” he says. “In addition, without performing an otoscopy before impressions you may end up pushing the wax down further in your ear canal which may result in perforation or subsequent ear infections.
“Even when the ear canal is clean and clear, people often either place the otoblock incorrectly or forget to use it altogether."
He agrees digital ear scanners to take impressions are a great advance and believes there will be more uptake in future. This involves scanning to provide a digital impression and sending this digitally to the manufacturer.
“Digital ear scanners are quite expensive, but they are cost saving, save time, and postage costs. We have one in our Tweed Heads clinic but in our Brisbane clinic they prefer to take a physical impression mold and send it in an overnight courier,” Pal says.
He recommends updating soft, silicon mold-based ear plugs every two years. “We know the ear shape and canal shape change over time so it's recommended that any ear molds should be replaced after two years,” he says.
“This is because soft silicon gets discoloured, and we advise changing noise filters after six months especially if they are used regularly.
“Some people come back after using them for five or six years though and they’re still going so there's no hard and fast measurement yardstick to say they should be changed after two years.
“However, as people age, and especially for seniors, the ear canal shape changes because the ears become bigger as their collagen reduces.”
Another reason for increased earplug use is that the noise level is rising across the world, he says. “NASA has done measurements from outer space and seen how much noise has changed from Earth by determining how much noise it can pick up,” he says.
“There have been studies done showing the noise level has grown exponentially compared with what it was in the 1940s for example. We will see a deterioration in noise levels as more modern cars, electric cars and more silent things come into play.”
While earplugs are not a hugely profitable part of Lucchese’s business, he says it is something they have been steadily doing for a long time.
“It is an important service to provide to clients who rely on their ears for their profession or enjoy listening to music as part of their daily lives,” he says. “As a hearing care clinician, our industry is best placed to look after people’s ears and protect their hearing so they can always hear, listen and live.”
Pal also encourages hearing practitioners to provide customised ear plugs.
“It’s an area of need and some people are not aware of where to go. It’s rapport building and establishment of yourself, your products, and faith in you as an established professional,” he says.
“They will take your advice more seriously than just buying something off the shelf or online. You know exactly what they need and it’s a more professional approach.
“Starting from humble beginnings of providing just a noise plug can build trust and relationships. A motorbike enthusiast aged 50 might come in for earplugs but then see your service, and might say, ‘Ok, let’s do a hearing test. I've never had a hearing test’.” And that could lead to a loyal client for life.

PETER LING wants to partner with audiology clinics nationwide to provide innovative 3D ear scanners for custom earplugs, delivering an alternative to invasive and time-consuming physical impressions.
Sydney business founder Mr Peter Ling has a sound proposition for Australia’s independent audiology clinics to help them add value and attract clients. He will sponsor 3D ear scanner investment upfront, place them in clinics and, with the practitioner, jointly charge clients for scans that provide specifications for custom earplugs.
Ling started doing the scans for local musicians seeking customised earphones (often called “custom in-ear monitors”/CIEMs) in 2022 as a side hustle in a Sydney audio store. The service became so popular that people began flying to Sydney to access it which “speaks to the desirability of the method and outcomes”. Manufacturers of earplugs and CIEMs still regularly refer their customers to him.
As demand grew, he started working full-time in his business, Auricle Digital, and in 2023 began flying to Melbourne and Brisbane every second month to do scans in rented premises once there were enough website bookings.
“I can't be on a plane all the time so I'm really excited to work with audiologists to offer them this new opportunity,” he says. “We’ll work in a partnership model; I can sponsor the purchase of a Natus 3D Otoscan so clinics aren’t put under a large financial load to start providing direct ear 3D scanning services.
“We will work out a clinic–specific pricing structure together for the process. I’d love to see places all over Australia where people can be scanned.”
It’s a win-win for everyone, Ling adds, as the innovative technology and new custom ear products will drive clients to clinics for a more comfortable, more accurate, less invasive and less risky non-contact scan. Practitioners will save time as the scan takes about three minutes per ear and is quicker than a
physical impression. It also reduces the need for repeat impressions due to
“Our success rate over the past year was 92.7%, meaning 92.7% of people were extremely happy that their customised ear products based on the digital scan were comfortable, fitted and worked well,” he says. “This compares with the 70% to 75% industry standard of people being satisfied after an impression fit, where a-quarter were returned or adjusted.”
The scanned custom fit solution enhances function, comfort and performance but the strongest benefit of a 3D scanned earplug is comfort, Ling says. “We estimate at least a 10% to 15% difference in the actual size and shape of a person’s ear in a 3D scan versus what an impression tries
“This is because the impression material creates pressure in the ear and pushes on crevices, soft tissue and cartilage, oversizing the ear shape. When we use the scanner, we're only measuring using light so there is no deformation of your ear; products produced off the back of that are fundamentally different and significantly more likely to be comfortable and
Ling says the American Navy funded development of the technology to eliminate risks of injuries during impression taking. While rare, these include eardrum perforations from a sealed pressure chamber, distorting the ear’s shape and attachment of impression material to the eardrum.
However, risk is further minimised with direct 3D ear scans, he adds. A probe goes past the ear’s second bend, so people must be careful and trained, but a camera is attached providing visual feedback to guide the process ensuring there is little to no contact. Light rays create the image by scanning the canal
The scanning process never fully seals the ear and does not introduce pressure into the ear. “The process is much less invasive with minimal contact. We do not place any objects or materials near the eardrum,” Ling adds. He likes to talk the customer through what's happening and why, and make observations and decisions including around the jaw position.
“I’m wanting to address the person, context and need; for example, some shooters will be in fast–paced tournaments with complex courses,” he says. “Understanding where their jaw is helps us to better support them; do we need to cater for this person's heavy breathing if they’re moving quickly through a tournament course and have an open mouth to get air in while yelling instructions to others? This is different from someone using earplugs for work focus in an open plan office or to listen to music at home.”
Famous musicians and actors
Ling has provided scans for more than 250 people including many in the music industry such as Tones and I, some of her touring musicians and crew,


ABOVE: A traditional physical impression (beige) versus a 3D scan (blue) of the same ear. It shows there is a 10-15% difference in accuracy with the scan providing a better fit.
and Angus and Julia Stone. Actor Chris Hemsworth wore custom in-ear monitors in Limitless series 2 which were based on Ling’s scans. They were used in a viral performance with singer Ed Sheeran surprising a packed arena with a stealth drum performance from Hemsworth.
Ling has spent 25 years doing audio for a large house of worship. “Supporting musicians and artists is something I find rewarding so it’s great being able to grow that from part time into something more meaningful,” he says.
“I’ve also worked for more than 20 years in the IT industry including health projects and I always wanted to have my own business. The logistics and lessons I learned empowered me and helped me grow to a place where I thought I could take a good crack at my own business.”
He thought of the business model in 2016 when direct ear 3D scanning came to market but was not in a position to act.
“MiniDisc, a leading personal audio technology store near me has reseller agreements with several in-ear monitor companies, so I approached them, said I wanted to sell ear scans, and they said they’d support it,” he says. “We said ‘let’s see how it goes’ but demand quickly grew and it’s gone really well.”
The first thing he tested for his business model was consumer support and the answer from the market was a resounding yes, locally and internationally. While most website visitation is from Australia, much is also from the US, Europe and South America.
Ling has also fitted pilots, recreational shooters, motor enthusiasts, motorcyclists and construction workers as well as event and communications workers, and fitted for sleep, swimming, sports and travel. “We’ve had very positive feedback with clients saying comfort and performance is great.”
As of April 2025, a single scan is $249 (incl GST) to use with hearing aids, earplugs or CIEMs. Auricle Digital Alpha earplugs are also $249 including GST and a second pair of earplugs, $180. A case, neck rope and clothes clip help prevent loss or damage from dropping earplugs.
The scans can be used with Ling’s in-house earplugs, or with any other manufacturer. Ling sends the scans to manufacturers who make the customised ear products and mail them to customers. If there are issues related to the scan he will work with the manufacturer so the customer/patient doesn’t need to worry.
The 10 manufacturers he has partnered with are also impressed as scans reduce the amount of reworking they have to do due to increased accuracy.
3D ear scans taking over


From a customer viewpoint, it’s a no-brainer, Ling says, and there are also many benefits for practitioners.
“Enabling audiologists to access the scans will bring people to clinics sooner in their hearing journey,” he says. “We are working on some things that will benefit people in new ways that will be immediately useful to them every day and our audiology partners will have a front row seat. My desire is to create a good relationship with the audiologist so patients will move into their hearing journey with practitioners much earlier.”
Ling has seen the challenges audiologists have with commercialisation and accessing expensive technology. “I’ve been able to model something that's going to help them gain access to this technology even if they can’t invest in it upfront,” he says.
“In future, the number of situations where impression material is going to be more appropriate than a direct 3D scan will be rare but never zero,” he predicts. “Clinically the right tools must be used for the right clinical application and currently impression material is the more available/accessible clinical tool so the appropriate choice.
“As more scanners come online this will move the balance to where a
“These innovative products set up the conversation with consumers about how something fits perfectly in their ear and can be comfortable and functional. That's exciting, and I need to take a community of clinical people with me on that journey, because there will be different perspectives on the products and how they're used, and I want clients to receive the correct information from practitioners.”
For more information, see auricledigital.com or contact Peter Ling on 0435 544118 or info@auricle.digital.

Members of the Specsavers Audiology recruitment team for Australia and New Zealand discuss the most common questions they are asked by audiology professionals interested in joining the network.
they have to pay the full cost upfront. Specsavers will support them with
“They also receive all the usual entitlements plus five weeks annual leave
A percentage of turnover goes to the optical business to pay for store rent and utilities, along with the marketing team and finance team in supporting partners as required. The recruitment team also assists with hiring
When audiology partners move on from Specsavers , they sell their shares in the business they have built.
Another drawcard is the local business owner-driven nature of the opportunity along with Specsavers offering the best value due to our global buying power, La Ferla adds.
“There’s no other business that provides quality, affordable hearing aids at the prices we do which makes it easier for each business to grow,”

“Specsavers is not a business where we decide where the opportunities are; it’s driven by our partners’ needs.”
Amanda La Ferla Specsavers
Specsavers says it doesn't compromise on technology, price or quality.

She describes a scenario of a customer coming to have their eyes tested, and while they wait, the optical assistant offers a hearing screening. This simple step initiates the audiology customer journey.
“When explaining to an audiologist or audiometrist that they’re coming into a business within a business, it can be daunting,” Wijesinghe adds. “It helps to give a picture of what that means, the conversations, lay of the store, the fact their room is next to the optometrist’s.
“They're drawn to partnership because it’s a unique opportunity. Many are ready for a new career challenge but aren’t sure where to start, or they want to start their own business but lack the financial resources or expertise.
“All they need do is show us they're willing to learn and grow, and we can guide them through the rest. Our audiology relationship managers act as business coaches and mentors, supporting partners in developing their business management skills.”
Wijesinghe explains that Specsavers entered the hearing care industry due to the lack of education, stigma surrounding hearing aids, and the high prices that often deterred people from seeking help.
“Our customer journey allows audiology professionals to vet whether the customer is ready and committed to a hearing aid,” she says. “They advance from a hearing screen to a hearing check, and if needed, an assessment. They take away information about products, benefits and prices to discuss with their loved ones, and return for a fitting another day.”
A 90-day money back guarantee means customers can return devices within three months if not satisfied.
The Specsavers audiology recruitment team regularly engages in confidential discussions with audiology professionals through roadshows, conferences, and chapter events. “These conversations are all about building trust, and ensuring they feel comfortable reaching out when they’re interested in exploring new career opportunities," says La Ferla.
As part of this ongoing dialogue, the team also speaks with graduates looking to advance their careers.
“One graduate who started three years ago recently completed our partner assessment program and is on track to become a partner soon,” La Ferla says. “It shows the evolution and how quickly you can achieve your career goals at Specsavers.”

all new partners through their first 12 months, providing support in every aspect of business ownership,” La Ferla says.
Word of mouth from Specsavers partners and employees is what gets most candidates over the line, she adds. “It's important to speak with someone who has experienced it. If they don’t know anyone, we can put them in touch with someone.
“Don't shy away from an initial conversation. Reach out to the recruitment team, even if it's just out of curiosity, if you'd like to know more as there’s no obligation.”

Sydney audiometrist KRYSTAL ALLEN, who has moderate hearing loss, has upgraded to Starkey’s Edge AI hearing aids and fitted the revolutionary new device to many happy patients who are similarly astounded by its features.
As someone who works in the Australian hearing care industry, Mrs Krystal Allen had been watching with interest from afar the impacts of Starkey’s new Edge AI hearing aids after they were launched in the US and Europe.
She was eagerly awaiting their arrival here so she could try them for herself and fit her patients with them. Now this has happened, and she’s been blown away by how they’re performing.
The devices hit the Australian and New Zealand markets in February 2025, launched months sooner than expected, due to the company not wanting to delay benefits to Australasian customers.
Allen, who has moderate hearing loss, had trialled a few other brands from other companies but found the buffer (to ensure consistent audio flow) was running out by the day’s end.
She had originally been wearing Starkey’s Genesis AI, which she says were great – but was then handed Edge AI to try.
“I thought, ‘How different can they be? It's only been a year since the last version,” she recalls. “But when I put Edge AI on, I was really surprised, I was quite blown away.
“The difference is huge. When I put them on, I couldn't honestly believe it.
It was so different from Genesis AI. It's just made everything easier. I'm not fiddling with the hearing aids, I put them on, leave them on all day and I'm not thinking about my hearing anymore.
“Compared to other manufacturers’ (brands) I've tried, it's just so natural. It's like a transparent sound, so I can hear clearly and there's no robotic or obvious notification; it just sounds normal.”
As for everyday use and speech in noise, Edge AI is “brilliant” and doesn’t need adjusting, she adds.
“I can control and change the listening intent and features with the Edge+ Mode on my phone using the My Starkey app which has great user controls,” she says.
“But I’m not having to activate Edge Mode+. I honestly feel like I don't need to do anything to them – and that's what I love about them. I just leave them. They know exactly what to do and I can hear well; I have a busy, noisy life, and I love them.”
Allen describes the sound as “clear and natural”. “I can stay focused and I'm not getting that fatigue anymore,” she adds.
Shire Hearing in Sydney, where Allen works, offers hearing aid trials for clients with different brands and levels so they can make informed decisions.
“Time and again, we are seeing more people selecting Starkey based on their experience, and feedback is that it’s natural and easy," she says. “Clients say, 'I'm not having to fiddle with them and they’re not beeping at me all the time for different alerts'.”
So far, the practice has fitted Edge AI to many happy clients.
Previously in restaurants Allen tried to sit in certain areas to assist hearing, but “it doesn’t matter where I sit now; Edge AI figures it out”.
Battery life is another big bonus.
“It's never come up saying ‘battery low’. The RIC RT model has got up to 51 hours of battery life and the mRIC R model which I wear has up to 41 hours. I charge them each night, I don’t let them run out, but it’s reassuring to know that if I have a big day at work and then I had a social night out, I wouldn’t have to hurry home like Cinderella to charge them.”
Balance Assessment Tool feature
Allen also finds Edge AI’s industry-first self-guided Balance Assessment Tool feature interesting and helpful not just for older people. It uses motion



“I THOUGHT, ‘HOW DIFFERENT CAN THEY BE? IT'S ONLY BEEN A YEAR SINCE THE LAST VERSION.’ BUT WHEN I PUT EDGE AI ON, I WAS REALLY SURPRISED, I WAS QUITE BLOWN AWAY. THE DIFFERENCE IS HUGE.”
sensors and AI to assess balance and potentially identify people at higher risk of falls, encouraging them to seek further balance testing if needed.
“I’m on a bit of a health and fitness journey so I thought it would be good to do the balance assessment and keep track of it as my fitness progresses to see if I can do it quicker and better,” Allen says.

The Balance Assessment Tool feature measures a person’s balance as they do certain exercises, including sitting on a chair and how many ‘sit and stands’ they can do within a certain period. It then tells the user how they rank compared to peers of the same age and gender.
“I've also used it in clinic with clients. A lot of people don't realise how much their balance is impacted by the hearing loss,” Allen adds.
“We do the exercises with them, some of my elderly clients, and if it comes back saying it recommends seeing a doctor as they have a risk of falling, that’s good for opening up those conversations.”
Allen says while Edge AI is discreet, this is not something she worries about as she dresses her hearing aids up with DeafMetal hearing aid earring jewellery including safety chains.
Another bonus is they are waterproof to up to one metre (rechargeable styles only), which is helpful for when she accidentally forgets they are in and pops in the shower, which has happened, or is kayaking with her son.
It was ironically her son’s mild hearing loss that directed Allen to a career in audiometry. She began working in banking and finance, and spent a decade in a high-level career but didn’t feel she was making a difference to people’s lives.
“I started my career in the UK then relocated to Australia 14 years ago and I was making good money, but I didn't feel like I was making any difference to the world,” she says.
“My son was in intensive care when he was born in Australia. I was watching the nurses who were literally keeping him alive and I had this overwhelming guilt that I was earning more than them but nothing I was doing really mattered.”
When she returned to the bank after maternity leave, her job was made redundant. “At first I was devastated but I met this amazing professional business coach, Yvonne Cohen, and together we worked on what I could do
and we came up with audiometry,” she says.
Allen was unaware she had hearing loss but as her son was born with mild hearing loss she had been taking him to audiologists. “Watching them conduct VROA (Visually Reinforced Orientation Audiometry) was fascinating and one audiologist invited me to the 2018 Audiology Australia conference in Sydney to get some information,” she recalls.
“I hadn't signed up for study but I listened to the presentations and networking and I was hooked.”
She studied audiometry at TAFE while working for I Hear and moved to Shire Hearing, which has clinics in Cronulla and Engadine, in June 2024.
“I love working for an independent and being able to really choose what's right for each client rather than being tied to one manufacturer,” she says.
During her studies, Allen discovered she had a conductive hearing loss while doing hearing tests.
“Looking back, I was probably straining, getting tired easily, and on TAFE education days I had to really focus and was having to ask the person next to me, ‘What was that?” she says.
“One day we were testing each other's hearing and mine came back with a conductive loss, so I was sent off with a GP report for an MRI to confirm there was no tumour. It was interesting, being a student but also going on the patient journey as well,” she says.
Allen’s hearing loss started around the time of her pregnancy and the ENT diagnosed otosclerosis, which her mother also had. Her mother recently wore Starkey’s Evolv AI hearing aids and apart from helping her hearing, they also stopped her vertigo and tinnitus symptoms.
“As my hearing loss progressed into the moderate range, I realised I needed to do something about it, as I was asking people to repeat themselves. It was my son who triggered me to do something. He was getting frustrated,” she says.
Allen started with a Starkey device and has stuck with the brand. “I was very happy with the connectivity; it made things a lot easier. I’m so lucky to be working in the hearing industry with a hearing loss because since I’ve joined Rachel Dorman at Shire Hearing I can access any hearing trial and select the ones I really want to wear,” she says.
“And so far, Edge AI has been the best.”
For more information on Edge AI hearing aids, visit starkeypro.com.au
Audiologists DOMINIC POWER and DR BROOKE HANBY discuss the importance of using the right device to achieve excellent visualisation and depth perception for intricate procedures in the ear canal.
Mr Dominic Power and Dr Brooke Hanby spend considerable time training students and practitioners in cerumen removal and other procedures deep in the ear canal.
Power is a lecturer at The University of Melbourne and lead audiologist at its Melbourne Hearing Care Clinic, while Dr Hanby is project manager for Phonak’s Lyric hearing aids in Australia and an Ear Health Courses consultant.
Due to the demands of their roles they need to rely on equipment that won’t throw further complications into the equation. The VorOtek O Scope, invented in Australia specifically for ENT and audiological work, is their preferred teaching and in-practice tool for wax removal and deep canal procedures.
There are two versions: a head-band model and a spectacle frame model. They both combine LED illumination with a unique optical pathway for looking in ear, nose and throat cavities.
Its biggest benefits are its exceptional depth perception and stereoscopic vision due to both eyes reaching the bottom of the ear canal. This unique converged optical pathway of laser-aligned mirrors and precision magnifiers converges both eyes from 65 millimetres apart at the top to just a few millimetres apart at the bottom.
In conventional loupes and phone otoscopes, sight from only one eye reaches the bottom of the ear canal, providing poorer depth perception and monocular vision, VorOtek says. This indirect pathway can’t achieve the same level of depth perception as the VorOtek O Scope or provide binocular vision in narrow ENT cavities, making it more difficult to accurately judge small distances.

the ear, removing bits that have fallen off hearing aids, doing wax removal, or manipulating or placing small objects in the ear, such as a probe or microphone tubes,” he says.
“For trickier cases, having good illumination and magnification makes difficult tasks much easier.”
For practitioners, including Power and Dr Hanby, proper depth perception dramatically enhances their ability to judge very small distances. This minimises patient discomfort, reduces the risk of accidental contact with sensitive ear structures, and helps avoid complications such as pushing earwax deeper into the canal or accidental eardrum damage including perforation. It also enables hearing care professionals to work more efficiently and effectively.
The design enables viewing to the bottom of the ear canal into a very narrow cavity. Natural, bright light and illumination is directed into the space. Light, optics and field of vision in some competitors’ products are broader however and use a narrow prism lens to converge, Power says. This loses some of your peripheral vision which gives cues such as if the patient is uncomfortable.
Peripheral vision also helps when introducing instruments from the periphery.
“If you can do your job with greater precision, it will be more comfortable for the patient,” Power says. “If using light that's colouring the skin, you can't see where some of those subtle bruises or irritation scratches are so it helps to keep the anatomy neutral.”
He says the VorOtek O Scope is mainly used for wax removal, but an equally important application is for more thorough otoscopy. “It gives us greater accuracy and precision over finer, more detailed techniques we need to apply when identifying whether anything suspicious is going on in
The O Scope also helps place probe microphones for certain hearing aids close to the eardrum.
“Being able to visualise and gauge the depth perception and distance from the eardrum at the end of a probe microphone gives greater confidence that we’ve placed it in the right spot,” he says. “It also allows for more accurate adjustment of hearing aids when fitted deep in the canal.”
Removal of foreign bodies is another procedure where the device proves its worth. “You can’t do foreign body removal without having good depth of perception, light and magnification for removing hearing aid domes or wax filters that have dislodged in ear canals,” Power says.
“If removing beads, Lego, styrofoam balls, dead bugs – which I have – we must remove these objects safely without causing bleeding, scratching or other trauma to the ear canal.”
A perforated eardrum was the main risk of not being able to see deep into the ear canal to perform procedures or place hearing aids, Power explains.
“I've seen many ears unfortunately that have been syringed out by GPs or practice nurses, where they have not visualised the ear canal properly,” he says, noting some GPs ask patients to sign a waiver, indicating risks.
“With the VorOtek O Scope you can be much more precise where you are removing the wax from and have better judgement on whether the wax should be left alone or the best way of removing a foreign body. It allows for safer, more precise, more effective and gentle care of the ear.”
He says other otoscopes, including pen and phone versions, have much


lower resolution, less light and lower quality of optics and illumination which can provide inaccuracies in colour and representation. This can make it harder to detect differences between where the eardrum starts and the canal is. People might be left guessing if it’s wax or a shadow.
“Using both eyes is what gives depth of perception. You can work in that visual field and if using a curette or suction cannula, depth of perception guides precisely where you need to place your instrument.”
The university has several VorOtek O Scopes in its prac room and Power and others train audiology students in their correct use for otoscopy and cerumen removal.
While an operating microscope is the gold standard, it’s more expensive and less portable, making the VorOtek O Scope the best option for audiologists, he adds.
Power says cerumen removal workshops are popular because audiologists recognise it as a knowledge gap. “It’s something we are hoping that audiologists as a profession can be the gatekeepers to,” Power says. Demand is increasing for cerumen removal as is community awareness that audiologists have the skills and techniques to perform it, he adds. It also needs to be done for hearing aid maintenance.
“People who wear hearing aids all day, every day, have to ensure that when wax blocks their ears, practitioners can remove it quickly and easily so it doesn't get in the way of their hearing aid use,” he says.
The VorOtek O scope has been equally invaluable for Dr Hanby who trained in audiology in America before arriving in Australia 14 years ago to launch Lyric. Apart from being the Lyric project manager for Phonak, she also teaches cerumen removal to hearing care providers, GPs and nurses. Dr Hanby sometimes also teaches with Dominic Power.
Additionally, she teaches people across Asia-Pacific how to use the VorOtek O Scope to place Lyric invisible hearing aids deep inside the ear canal.
“I’m passionate about VorOtek. When teaching I make it clear that it’s not complicated when you’re using the right tool,” she says. “You can’t be


confident with a procedure if you can’t see what you're doing and if you're going to do it the right way, you can't fly blind.”
Dr Hanby has used the device for 14 years since its launch. “When we launched Lyric people had to use a certain operating microscope from Germany. After a few years, it became clear that some clinics didn't have the footprint or space to house it so we investigated a solution for smaller visiting sites.”
She started looking into other options and met Melbourne ENT surgeon, Dr John Vorrath AM, who invented and manufactured the VorOtek O Scope which is now used by nearly all Australian ENTs.
“He just wanted the best optics for what he needed to do and that was working in the ear canal but he couldn’t find anything so he designed it himself,” she says. “As soon as I used it I knew this was going to change the Lyric market which it did by opening the door to the number of providers, who became confident in Lyric fitting. Many prefer it for wax management, since it is easier to bend in certain positions that you cannot with the microscope.” This also makes it ideal for practitioners dealing mostly with elderly people who find it hard to bend their stiff neck, she says.
Dr Hanby says when looking at that tiny space, people often can’t see around it because there’s a block to the canal. “With the VorOtek O Scope I love the visual because your two eyes converge like laser beams coming together. There’s a 12-millimetre space at the start but by the time it hits the ear canal with your working distance, it's about three millimetres.” She refuses to sign-off on those undertaking the cerumen removal course if they use other illumination, as she believes other devices are a liability. Typical head loupes don’t focus on the ear canal, she adds, as one eye looks through the lens but the other looks elsewhere.
“I tell my students to be careful because in our field there's a lot of equipment that’s designed for other health professions; for example, equipment to remove dental plaque and flush water was used in ear irrigation and that’s why there’s perforations,” says Dr Hanby, adding that patients traumatised by wax removal by irrigation are transferring to safe microsuction.
“The O Scope is specific to ears. We should be so proud of VorOtek in Australia.
“Working distance is important because equipment's often designed for other professions who are at arms’ length from a surgical patient. When working up close with little tools in ears, we must ensure people don’t move so the instrument won’t perforate the eardrum.
“We need to be close, so our arms aren't stretched out and we have a good base, which you won't see in a lot of head loupes.”
Convergence goes to that spot; the inferior posterior is important when performing wax removal and especially in such a tiny space. “It’s important because it’s where foreign objects sit or the thickest part of the wax to be removed is, the most crucial part. I think that’s why Dr Vorrath felt so passionate; he couldn’t find anything to do the job properly, so he invented his own form of illumination and it's the safest way.” See vorotek.com.

Hearing aid manufacturer GN is continuing its history of innovation by launching its “most intelligent hearing portfolio yet”. It features best hearing in noise technology for Beltone Envision – the industry’s smallest AI-powered hearing aid – plus a new Auracast-enabled essentials range, Beltone Commence.
It’s welcome news for independent audiology practice owners around Australia who will have access to a raft of new technologies in GN hearing aids.
For example, a new True Focus feature in Beltone Envision responds to the direction a person is looking, allowing AI to prioritise sound based on where the user looks.
The company has also introduced a groundbreaking, world-first Auracast Assistant to connect from its hearing aid apps to Auracast broadcast audio. The new ranges feature connectivity to Bluetooth LE Audio and Auracast across all Beltone Envision and Beltone Commence technology levels (2/3 to 17).
Plus, GN says the new Deep Neural Network (DNN) chip in Beltone Envision is up to 17 times more efficient than other leading hearing solutions with directionality and DNN noise reduction, resulting in significant improvement to speech understanding.
The new product features are spread across GN’s entire portfolio of brands, including ReSound (Vivia and Savi launching in May), and key accounts such as Hearing Australia. The Beltone range was launched at the Audiology Australia 2025 Conference in Adelaide in April 2025.
In Beltone Envision, GN says it has pioneered a unique approach to AI that mimics the brain’s natural sound processing via the True Focus feature to create a superior hearing experience in noise.
“This breakthrough technology is packed in the industry’s smallest AI-powered RIE (receiver in ear) offering all-day battery power and comfort without compromise,” it says.
The Beltone Envision microRIE style offers 30 hours wear on one battery charge and 20 hours of use for a typical day using a combination of True Focus and streaming.
“Powered by a dedicated DNN chip trained on 13.5 million spoken sentences

In its biggest launch, GN has released a new portfolio featuring innovative hearing aid families in Australia and New Zealand, including an Auracast Assistant to enable direct connection from hearing aids to Auracast broadcast.
in various languages that spotlights speech and eliminates distracting noise, it offers the best solution for hearing in noise without cutting people off from the world around them,” GN says.
The chip trains the AI to recognise and suppress thousands of unwanted noises while highlighting sounds and voices that users want to hear, ensuring a clearer and more focused listening experience.
“Beltone Envision delivers unparalleled sound quality in noisy environments and all-day comfort without compromising size or battery life. Central to this innovation is GN's unique human approach to AI, which models the brain's natural sound processing capability to create voice clarity in complex listening environments.”
Direction response
True Focus responds to the direction the wearer is looking, ensuring the AI enhances sounds based on the user's natural response to their environment. The proprietary technology provides a more natural and effortless listening experience, even in challenging situations like noisy restaurants or crowded venues, GN says.
“Studies show Beltone Envision offers the industry’s best hearing in noise experience, with 64% of users experiencing improved hearing in noisy environments compared to other AI hearing solutions, so they can enjoy conversations with greater ease and understanding,” GN says.
And Beltone Envision was preferred 89% of the time using the True Focus feature for hearing in noise compared to GN legacy devices.
Mr Scott Davis, hearing division president at GN, says the new Beltone families represent a significant leap forward and mean GN can continue offering the most advanced hearing aids that cater to all lifestyles, budgets, and types of hearing loss.
Mr Brian Dam Pedersen, GN’s chief technology officer, head of research and technology, adds: “With Beltone Envision, we've fundamentally reimagined how AI can enhance the hearing experience.
“Our unique True Focus feature mimics natural human behavior, allowing the AI to prioritise sounds based on where the user is looking, not just how loud they are. This creates a far more intuitive and natural listening experience,




seamlessly integrating with the user's own perception of their environment and ensuring the user is in control and is the decision maker.
“It's not just about amplifying sound; it's about intelligently enhancing sounds that matter most.”
Beltone Envision is available in a microRIE rechargeable and two non-rechargeable RIE models, including a CROS model in the microRIE style, in a variety of colors including new navy blue. Beltone Commence is available in a new miniRIE rechargeable and two non-rechargeable RIE models in five colors.
Key features of Beltone Envision include:
• Advanced noise management and voice clarity: Cutting-edge AI excels at managing and reducing background noise, allowing wearers to clearly hear and engage.
• New, comfortable designs: The microRIE smallest option offers a discreet fit with a gently curved shape, while updated RIE styles are also ergonomically designed for all-day comfort. A variety of colours include new navy blue.
• Effortless streaming: Users easily stream TV audio, music, and more directly to hearing aids for crystal-clear sound and take phone or video calls hands-free by tapping their ear or device.
• Compatibility with Auracast: This enables people to stay connected to news, entertainment and public broadcasts through hearing aids.
All-over IP68 coatings make Beltone Envision and Beltone Commence weatherproof and sweatproof. They’re available in rechargeable and replaceable battery styles, with the rechargeable option providing all-day power on a single charge.
Beltone Commence essentials range is suitable for people with mild to profound hearing loss and combines innovative technology and updated designs.
The first-of-its-kind Auracast Assistant feature enables users to connect to Auracast. Beltone Envision and Beltone Commence wearers access



Auracast via a single tap in the Beltone HearMax app.
The process simplifies selecting Auracast streams, even with smartphones and devices that don’t yet have an Auracast assistant built in.
At a pre-launch event in Sydney in March, Mr Christopher Brew, training manager with GN ANZ, explained that hearing aid manufacturers had gone to Bluetooth requesting an upgrade which became Auracast.
Classic Bluetooth allows for a one-to-one connection between one person and one device, while Auracast enables many people to connect to one stream, he said. Auracast allows electronic devices to broadcast simultaneously to an unlimited number of nearby audio devices with Bluetooth LE Audio.
“You don’t need to pair to an Auracast streamer because it’s broadcast audio across the Bluetooth spectrum,” he said. For example, Auracast can connect thousands of people at an airport to its public broadcast system to hear flight announcements, and connect users in other public places such as theatres, restaurants and arenas.
Ms Rebecca McAneaney, GN country manager New Zealand, told the same event that GN’s organic hearing philosophy kept the user at the centre to create a hearing experience which sounded and felt natural. In keeping with this, the new devices were based around ‘intelligence augmented’.
McAneaney said GN was making changes to better support independent practitioners. It is introducing improvements to fitting software, alignment of domes and receivers for optimal comfort and acoustic performance across the new portfolio, and exchangeable mic filters for easy care to improve hygiene and device longevity. These enhancements aim to streamline clinic workflow, improve fitting accuracy, and enhance user experience.
Ms Megan Quilter, lead audiologist, global audiology, global medical affairs, GN Hearing, said sound was the undercurrent of life all around us, so we sometimes forgot it was there. GN’s hearing aids made the sounds that matter rise above, she said, and its new hearing aids were based on intelligence augmented.
“Intelligence augmented puts the human front and centre, with help from the machines to empower the human,” she said. “We are not replacing human intelligence.”
Intelligence augmented included machine learning, deep learning and deep neural networks (DNNs). DNNs were a gamechanger in AI and the “muscle” behind deep learning, she said. A DNN is a type of artificial neural network to mimic the human brain and includes an input layer, two hidden layers where learning happens, and an output layer.
Quilter said the DNN was trained on enormous datasets of real-world sound. GN trained the dual chip on 13.5 million speech sentences or 3.5 years of continuous sentences, across 3.9 million tuned sound parameters. The dual chip can do 4.9 trillion operations a day to spotlight speech and reduce background noise.
“That’s a powerhouse we are putting into the smallest AI hearing aid in the world,” she said.

Ms Lisa McBride, product and audiology manager, GN Hearing Australia, said: “This is the biggest launch we’ve ever done. It’s not just one new product but a whole new portfolio and our most intelligent portfolio yet.
“Beltone Envision with DualChip is the highest form of intelligence augmented, including a 360-chip co-processor with warp, environmental classification and beamforming, and the noise reduction DNN chip co-processor which filters out noise and replicates clean speech signal.
“The third part is the human brain which makes the decision. Together, this is the highest form of intelligence augmented."
ReSound Vivia and ReSound Savi with the same features launch in May 2025.
NOTE: Visit gn.com.

Audiologist DR CELENE MCNEILL and Macquarie University Hearing postdoctoral Research Fellow and dietitian DR DIANA TANG discuss the potential role of diet and nutrition in hearing loss, ear health and ear disorders.
Food is increasingly being found to have a significant role in preventing, managing and helping to treat various conditions. Studies are also growing looking at what role nutrition may have in hearing and ear disorders.
Sydney audiologist Dr Celene McNeill says evidence indicates the relevance of diet and nutrition in preventing and treating ear disorders. She says lifestyle modifications including nutritionist referrals are relevant clinical tools in audiology, and suggests audiologists consider patients’ lifestyle and nutrition in the prevention and management of hearing and balance function.
Dietitian and Research Fellow Dr Diana Tang says Macquarie University Hearing research shows there may be an association between poor diet and increased risks of age-related hearing loss and tinnitus, with fish, zinc and iron being possible protectors. But she says overall data isn’t strong or consistent enough yet for audiologists to advise that good nutrition prevents or protects against hearing loss.
By Dr Celene McNeill PhD Healthy Hearing & Balance Care, Bondi Junction, NSW
My interest in nutrition and health goes back a long way. I have always been intrigued by why we give so much faith to medication to treat illnesses while ignoring the effects of food in the body. I wonder if we would have more scientific evidence on the effects of food on our health if farmers funded medical research as much as pharmaceutical companies do.
The potential effect of poor diets as the root cause of some ear disorders is
vastly neglected. We tend to accept that most diseases are caused by intrinsic and extrinsic factors while overlooking food consumption, or the lack of, as a contributor.
Western diets are mostly based on processed and ultra-processed foods that our bodies do not even recognise as nutrients. According to Watanabe et al (2024), Australia comes second to the US for the highest consumption of ultra-processed foods in the world.
A study from 2019 (Jung et al) showed that high levels of carbohydrates, cholesterol and fats in the diet affect hearing health. The researchers showed that a lack of vitamins A, B, C, D and/or E as well as minerals like zinc, magnesium, selenium, iron and iodine, increase the risk of hearing loss. An appropriate diet seems the best prevention as the body draws these nutrients from the foods we eat and not from the medicines we take.
A recent literature review on the effects of diet and lifestyle on audio-vestibular dysfunction (Chen et al 2022) found 24 relevant publications on the topic. These studies showed compelling evidence on the effects of diet and nutrition in hearing, although there were not many references about the vestibular system. Research is still lacking in this field. Nevertheless, available evidence indicates the relevance of diet and nutrition to prevent and treat ear disorders as well as health conditions in general.
I had a personal experience after modifying my diet, following research on nutrition, with incredible results. I had ongoing issues with one knee and shoulder which I could barely move. The prescribed treatment was cortisone injections to reduce inflammation but I did not want to proceed as I knew it was


the elderly seek our services as we are qualified to perform diagnostic tests to investigate the integrity of the auditory and vestibular pathway to help identify any lesion causing loss of function. ENTs and other specialists rely on our test results to diagnose and treat ear pathologies with medication and/surgeries, when available.
At present, however, most ear disorders causing hearing loss and balance disturbances have no available medical cure, so patients rely on non-medical methods and techniques to improve their symptoms and quality of life. Audiologists play an important role, providing counselling, technology
and methods to manage hearing and balance disorders after any life-threatening pathologies have been properly investigated and treated by medical specialists.
The focus of audiological rehabilitation in Australia lies mostly on the provision of hearing aids and implants. Our university master’s degree training qualifies us to provide more than that. The Australian health funding model may be to blame for this situation, leaving patients with hearing and balance conditions without any further management or rehabilitation if hearing devices are not the solution for them.
Lifestyle modifications including nutrition, in my view, are relevant clinical tools in audiology. Nutrition is an integral part of health and that includes the ear. The foods in our diets potentially affect the prevention, causation and management of hearing and balance disorders.
Patients’ lifestyle and diets should be considered in their case history and part of the audiological assessment and management plan. Referrals to a doctor who practises integrative medicine or to a functional nutritionist might be as valuable as to an ENT and other specialists.
There is compelling evidence that diets high in sugar, fat, dairy, gluten, corn, soy, preservatives and heavy metals can cause insult to the ear causing symptoms of hearing loss, tinnitus and dizziness. It is important to refer patients for appropriate investigations using more integrative medical approaches.
Consideration of nutrition in the audiology clinic is not a new concept. In 2003, at a conference organised by the Australian Association of Audiologists in Private Practice (now Independent Audiologists Australia), late audiologist Dr William Tonisson suggested audiologists should offer nutrition advice to patients such as those with a high frequency hearing loss like in presbyacusis, stating it could be an early sign of heart disease.
Dr Tonisson suggested audiologists should discuss the benefits of low sugar and fat diets to prevent high frequency hearing losses and vascular diseases. His suggestion was not well received by peer audiologists on this occasion.
Years later, at an ACAud (Australian College of Audiology) congress, South Australian audiologist Ms Kelly Korcec presented a case study of a patient with Ménière’s disease who had symptoms reversed by following a gluten-free diet. Again, the topic was not embraced by the audiology community.
A recent literature review (Chen et al, 2022) found evidence that diet significantly impacts ear health and when the effects are negative, it causes symptoms like hearing loss, tinnitus and vestibular disturbances such as dizziness and vertigo. The effects of nutrition on ear health seem much stronger than accounted for.

Of course, audiologists are specialised in hearing and balance function, not nutrition, but some knowledge on the topic should be a welcome addition to our toolkit. We already consider many probable causes of hearing and balance conditions in our assessments such as hereditary, medications, noise and toxic exposures. Diet and nutrition should also be part of the history taken. Children referred to us for assessment of middle ear diseases, for example, may be identified with possible allergies and food intolerances as the root cause of their problems, with dairy usually being the main culprit. This should be reported to the referring source for further investigation.
It is also common for children diagnosed with auditory processing disorders to have associated food intolerances and allergies. We can provide all the training and rehabilitation required to improve their processing skills, but the results may not be sustainable if we are not addressing the root cause. Reporting all identified potential causes of an audio-vestibular disorder and making appropriate referrals is part of our scope of practice and can only benefit our patients.
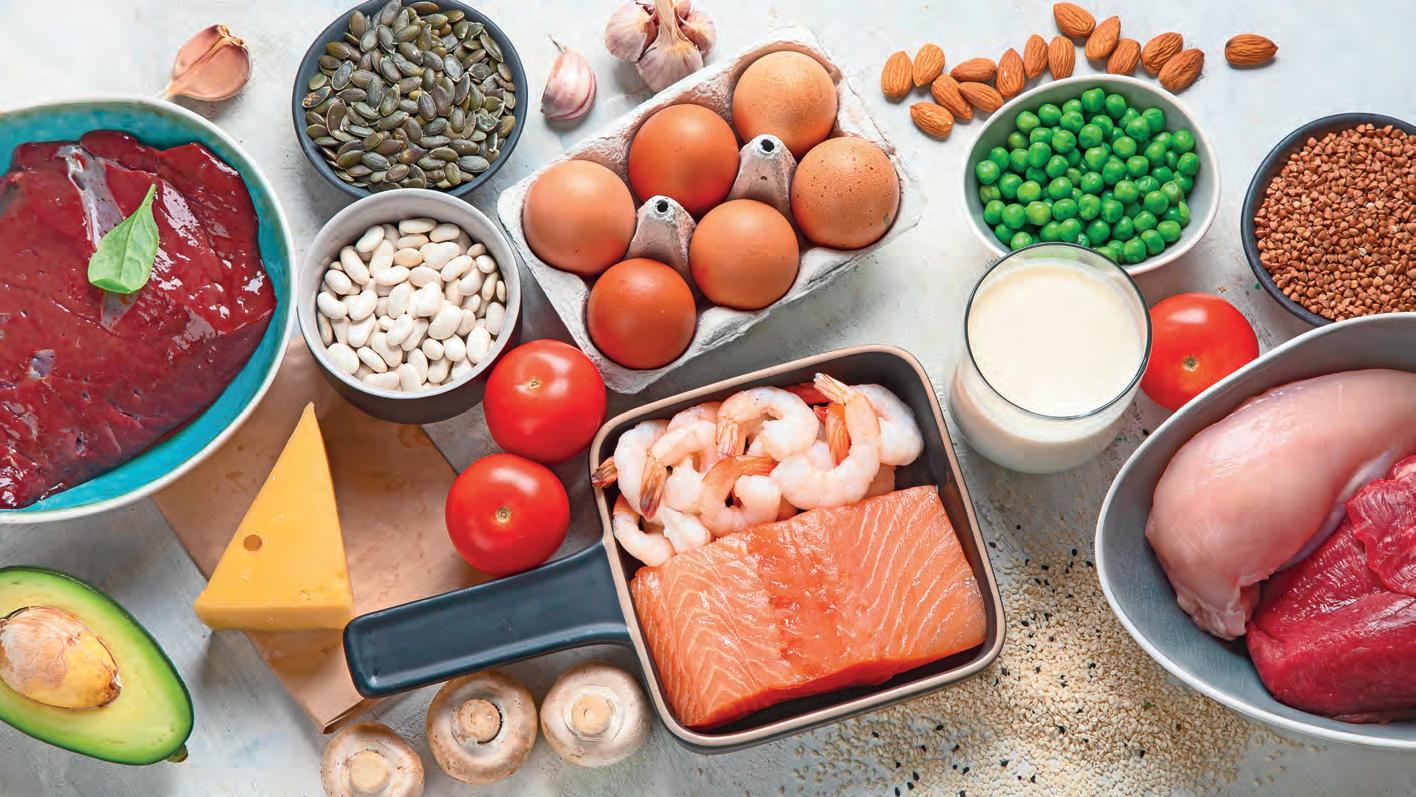

In Ménière’s disease, my main topic of interest, there is increased evidence that some patients control their symptoms by changing their diet and lifestyle. There is no current cure for Ménière’s and the aim of medical treatment is to manage symptoms, especially vertigo. There is an arsenal of medications prescribed for this population attempting to reduce vertigo attacks, nausea and vomiting. But not many practitioners check patients’ diet and lifestyle. There is only emphasis on salt restriction for these patients even though there is no strong evidence that it works for most. Diuretics are also widely prescribed for Ménière’s patients despite studies showing that increasing water intake has the same result with no negative
side-effects. (Naganuma et al, 2006).
Recent research by ENT surgeon and neuroscientist, Professor Jose Antonio Lopez-Escamez and his team at the Kolling Institute, Sydney University and Granada University, Spain, confirms that Ménière’s symptoms are caused by inflammation in the inner ear (Frejo et al, 2024).
These findings endorse a case study published in 2013 of a patient who had all symptoms resolved after following a gluten-free diet. The inflammatory properties of gluten, researchers concluded, were responsible for inner ear inflammation leading to symptoms of fluctuating ear fullness, tinnitus, hearing loss and vertigo (Di Berardino et al). In my clinical practice I have come across similar results.
Unfortunately, the current approach to address inflammation in ear diseases is to use anti-inflammatory drugs without considering the possible effects of patients’ diets that could be increasing inflammation in the first place. I am not disregarding the utility of pharmaceutical drugs to alleviate acute symptoms but appropriate diet and nutrition should also be part of any treatment.
In September 2024 I attended a conference in Brazil organised by the Fundacao Otorrinolaringologia (FORL) or Brazilian Otolaryngology Foundation. Endocrinologist Dr Delane Goldbach delivered a session on culinary medicine, describing the positive outcomes of reducing high levels of glycaemic and lipid index in a group of sick patients after teaching them “cooking skills” instead of prescribing medication.
Many in the study group also experienced tinnitus and dizziness due to their metabolic disorder and had these symptoms resolved by her approach. Dr Goldbach’s treatment methods included educating patients on healthy food habits such as how to read and interpret food labels as well as preparing and cooking meals.
The genetic profile of individuals is also an important consideration when it comes to the effects of food and nutrition; what affects one person may not affect the other and it is not one size fits all. Current developments in genetic research mean we will be able to provide individualised treatments for each patient’s genomic profile. The influences of epigenetics such as the food we eat and the environment we live in will also play an important role.
It seems unlikely that conventional western medicine in Australia will embrace such approach any time soon, for various reasons. In the meantime, audiologists could start looking outside the box to include patient’s lifestyle and nutrition for the prevention and management of hearing and balance function for the benefit of their patients. A good starting point would be a search of literature on the topic of nutrition and its impact on human health.
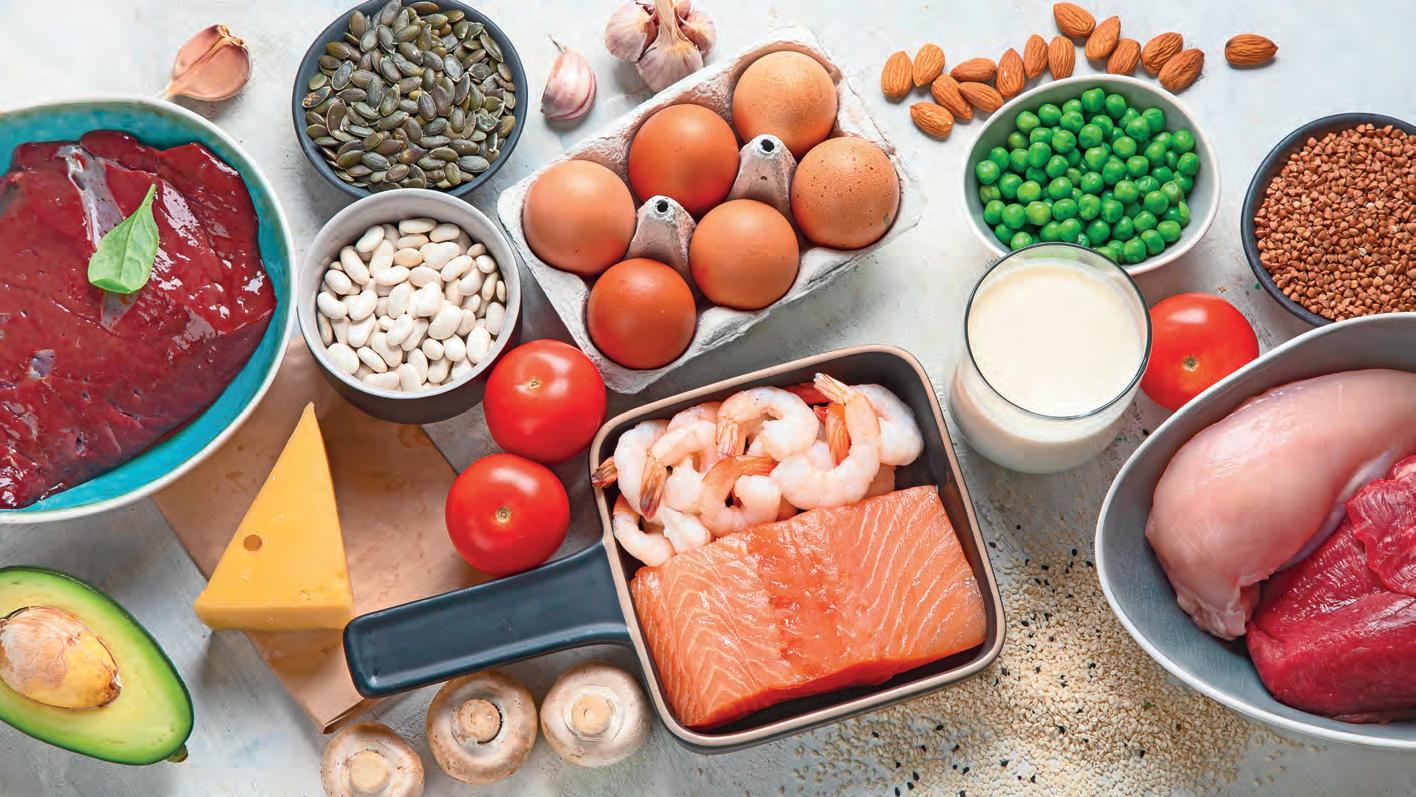
By Dr Diana Tang, PhD, MNutriDiet, Research Fellow, Macquarie University Hearing, NSW
The Macquarie University Hearing team looked at longitudinal data from a cohort of Australians aged 50 and over and found there may be an association between hearing health and specific dietary factors. It was the first longitudinal study to explore associative links between dietary intakes of iron and zinc and prevalence and incidence of tinnitus in an older adult population.
The evidence indicated higher intakes of zinc and iron were associated with significantly lower risk of developing tinnitus over 10 years. As there are no other studies like this in Australia, more research is needed to confirm the accuracy of our findings especially because the amounts of iron and zinc found to be protective against tinnitus exceed current dietary recommendations.
We need to be sure about these benefits before providing recommendations to consume higher nutrient intakes to patients. We also need to keep in mind that our findings are based on data collected in the 1990s to 2000s among a mostly Caucasian cohort of adults who were consuming a more western-style diet. This may not reflect current Australian demographic or eating patterns.
We also found those with lower diet quality had twice the likelihood of having concurrent hearing and vision loss (dual sensory impairment). Poor nutrition could have a role in concurrent, age-related hearing and vision impairment due to the importance of diet in healthy ageing. For vision impairment, there is evidence from high quality research to support the link between nutrition and age-related macular degeneration (AMD). This includes a large clinical trial evaluating effectiveness of nutritional supplements in preventing or slowing progression of AMD. Further investigation found only participants with lower intakes of lutein and zeaxanthin from their diet significantly benefited from these supplements. Those with higher dietary intakes of lutein and zeaxanthin did not gain further benefit, suggesting supplements and food have the same impact.
Fish intake reduced risk of hearing loss
A third study from our group showed higher intakes of omega-3 fatty acids and regular intake of fish reduced the risk of age-related hearing loss. The benefits of fish intake and omega 3 fatty acids for hearing health were significant.
A key finding was participants who had two or more servings of fish per week compared with participants who had less than one serving weekly significantly reduced their risk of developing hearing loss by 42% after five years. Our study is the only study globally to report on this link and more research is encouraged to confirm our findings.
The research we have conducted suggests more food-focused research is needed. As nutrients obtained through the diet are more potent than supplements and the influence of the food matrix unknown, single-nutrient solutions like supplements may not be the answer as they are more typically linked to relative deficiencies such as those arising from restrictions of certain foods or food groups or due to physiological changes in the body.
Although the pathophysiology of hearing loss and tinnitus are unknown, it’s hypothesised that good vascular health and adequate blood flow to the cochlea supports good hearing health.
Iron is known to play an important role in oxygen circulation with poor circulation to the inner ear increasing susceptibility to ischaemic damage resulting in impaired inner ear functioning.
In a similar way, omega 3 fatty acids and fish intake have been shown to prevent heart disease through various biological actions such as hypolipidaemic properties, triglyceride lowering, and anti-inflammatory and anti-atherothrombotic properties.
Higher intakes compared to lower intakes may contribute to better heart health and thus hearing health.

It is hypothesised that zinc is involved in cochlear pathology and the synapses of the auditory system. Zinc plays a key role in various cellular processes and pathways and has antioxidant and anti-inflammatory properties. Lower intakes of zinc may therefore increase the s usceptibility of the auditory system to the effects of inflammation, leading to tinnitus.
The data we analysed was collected in the 1990s to the early 2000s from older Australians living in the Blue Mountains area of Sydney. It has given us insights into a potential association between hearing health and some dietary factors, but we need more large Australian studies to back up these findings.
Our team, in collaboration with the Westmead Institute for Medical Research, UNSW Sydney, The Brien Holden Foundation and The George Institute for Global Health, is wrapping up the Australian Eye and Ear Health Survey.
Hearing health and nutrition data has been collected along with other information in Aboriginal and Torres Strait Islander people aged 40 years and over, and non-Indigenous Australians aged 50 years and over. With analyses underway, it will be interesting to see what current data will tell us about links between hearing health and nutrition and how it compares to what we know so far.
Based on the limited data we have, research evidence isn’t strong or consistent enough for audiologists to provide specific nutrition advice or recommendations that are guaranteed to prevent or protect against hearing loss.
A scoping review published in 2021 identified 22 studies related to hearing health and nutrition. However, when they broke down the evidence by individual dietary components or nutrients, most only had evidence from one or two studies or from data coming from cross-sectional studies which are lower quality.
Until there is more concrete evidence about the role of specific nutrients in hearing health, it is important to acknowledge what we do know; that is, a healthy diet is an important contributor to healthy ageing.
As much hearing loss is age-related, a healthy and balanced diet would be beneficial for the overall health of most of the population. Anyone who has other health conditions or concerns should speak to their GP or dietitian for more specific advice relevant to their needs and circumstances.

Hearing Business Alliance’s 2025 Seminar in Melbourne achieved record attendance, reflecting continued growth of the organisation in membership, strength and as an increasingly influential industry voice.
‘Innovate or die’ and ‘innovate to fly’ in hearing healthcare were the key threads in Hearing Business Alliance’s 2025 Seminar, and a crucial take home message for 184 delegates from 121 independent businesses who attended.
It was a record turnout, and a vital chance for practice owners to take a breather from working in their business, so they can work on their business instead.
At the Pullman Melbourne on the Park from 28 February to 2 March, attendees learnt new skills and insights from inspiring presentations by practitioners, industry, researchers and government representatives.
HBA represents small to medium independent audiology practices and the seminar theme – the importance of innovation in transforming small business models – aimed to help them remain competitive, be profitable and achieve better clinical outcomes.
Delegates caught up on latest technology innovations at a trade show, pre-conference workshops, and socialised at a GN-sponsored dinner.
Mr Stephen Logan, HBA’s business manager, said the event was twice the size of the organisation’s inaugural event in 2019, also in Melbourne, attended by 92 people.
“It was a great turnout and outcome, with a 20% increase in seminar registrations from last year,” he said.
“The market’s faced constant change over the past decade and there’s still uncertainty with economic challenges and inflation which affect consumer spending and behaviour.
“It’s hard to get and keep staff in metropolitan areas, and in regional areas it’s a nightmare but on the positive side, the market is growing and there’s a 12% increase in aged clients expected by 2030.”
Audiologist Ms Jane MacDonald, HBA’s CEO, said its 165 member businesses represented 490 audiologists and audiometrists in 700 sites nationwide, representing half of the nation’s independent audiology businesses.
“HBA is deeply honoured that as we grow, we are becoming a louder and more influential voice in the industry,” she said.
MacDonald detailed advocacy the alliance has undertaken in the past year including opposing cuts by NSW’s State Insurance Regulatory Authority to hearing aid fitting and rehabilitation for those sustaining workplace-related hearing loss; involvement in prioritising Hearing Roadmap recommendations from 140 to five; consultation on changes being made to the Hearing Services Program (HSP) changes.

intelligence,” he said. “It’s going to be an amazing opportunity for all of you. At some point, AI will be integrated into your practice, management, how you consult and develop treatment strategies.”
He said AI could be viewed as no different from having another ‘partner’ in the practice, a tool to do mundane work so practitioners could focus on skills. AI would help train practitioners, screen and triage patients, diagnose conditions, advise on treatment and assist with administrative work.
“Sensors can monitor a patient’s condition and advise on treatment strategy when they leave hospital or a health facility – this is happening in healthcare already and it will happen in hearing healthcare,” Dr Edwards said.
Every hearing aid manufacturer was using AI in some capacity to optimise devices including accessing big data from device use and neural networks learning from users’ devices, he said.Dr Edwards said suppliers had access to millions of data points from diagnostic and treatment fitting software to improve devices, and in future this would help tailor treatment by determining the best hearing aid for each patient.
“We have a looming practitioner crisis, but AI can help fill the shortage,” he

said, adding that AI scribes could offload creation of case notes and goal summaries, freeing practitioners to see more clients.
The event’s keynote speaker was American audiologist Dr Cliff Olson, founder of YouTube channel Doctor Cliff AuD and audiology clinic, Applied Hearing Solutions. He treated delegates to four inspiring presentations entitled ‘innovate or die’; explaining the value of your testing; consulting like a boss; and implementing innovation.
Dr Cliff said his HearingUp network, which HBA members have discounted access to, focuses on clinical evidenced-based best practice to achieve optimal outcomes and the highest level of hearing. He advised adjusting the delivery of hearing care to be better than competitors with conversion to hearing aids often coming down to the way practitioners deliver care.
“Recommend the highest level of technology each patient can reasonably afford but say that ‘by the end of it you’ll be hearing your absolute best because we have followed best audiological practice’,” he said. “I don’t treat patients unless they commit to four visits within 45-days as this ensures best practice and outcomes.
“Innovate in your clinic and disrupt yourself before someone else disrupts you.
“Most people are not doing anything new in their practice from a year ago. If you’re still doing the same thing year in year out and you’re lagging, you’ll be left behind because you chose not to innovate, and it will be hard to catch up.”
Only refer to doctors you know are excellent and who will refer back to you, and focus on your brand and how your patients perceive you, he added.
Website investment and Google reviews
“Your website is the number one driver of people to your clinic," Dr Cliff continued. "Spend significant time and money disrupting it, look at what others are doing and do it better.
“Does it convey the quality you’re delivering? Is its SEO targeting the people you want? Is it first on Google? Is there a video? If your website and video are poor quality, people are less likely to schedule an appointment.”
Google reviews were another driver and the more good reviews, the better.
“If you are doing an excellent job, then market the crap out of what you’re

“Recommend the highest level of technology each patient can reasonably afford but say that ‘by the end of it you’ll be hearing your absolute best because we have followed best audiological practice’.”
Dr Cliff Olson HearingUp


doing,” advised Sydney audiometrist and audiology clinic owner Mr Daniel Fechner in his presentation. “The only reason patients won’t come to you is if you don’t tell them about your practice.”
Fechner showed delegates that following Dr Cliff’s advice from last year’s HBA seminar had transformed his business from debt to profit. This was due to fully adopting comprehensive best practice principles and changing the way he presented the hearing aid discussion to clients, clearly explaining why it is recommended to “go for the highest level of hearing aid technology as they can reasonably afford”. The result was significantly increased client outcomes and a better bottom line.
He shows patients a document explaining that he follows best practice to achieve best hearing outcomes for each client. Dr Cliff explained this works because “it’s a psychological concept that people fear the loss of something; they don’t want to give up anything.”
Fechner also incorporates automated booking systems and embraces technical applications which enable him to review his business data.
“Take time out of your business to set goals. You may be set in your ways but look at workflow and efficiencies with systems and processes. Cancel a day of appointments and with your team, work through every single corner and refresh it, assess technical capabilities. Is there double handling of data, missed opportunities and leads?” he said.
On the topic of double handling of data, Fechner surveyed delegates in the conference room and found 65% of clinics had done this through four to five different systems or processes. Only 20% had a CRM (customer relationships management system) which was set up in the most efficient way – working as the heart of audiology practice.
“Lots of people don’t have online scheduling which only takes half a day to set up,” he said.
In a panel session, HBA secretary, Melbourne audiologist Ms Emma Batrouney said she had a good online booking system and half of her

without having your finger on the pulse of your business financials,” she said. “Profit and loss must be set up correctly with direct costs sitting in expenses. Look at profit and loss weekly, if not monthly, but not just at the end of the financial year because that’s too late.”
Dr Cliff emails patients when new hearing aids come out resulting in significant uptake as they expect to be told and want to try them. Investing in new technology and promoting it with videos on the website also drove patients to the clinic and increased search results.
His conversion rate to hearing aid adoption, focusing on clinical best practice to achieve optimal outcomes and the highest level of hearing, is 82%. “If your conversion rate is under 70%, track and measure, look at your data. Track each provider to client, set goals and train them to improve using processes to help them consult better,” he said.
“Consulting is about understanding behavioural psychology. Don’t start with, ‘You have hearing loss, we need to treat it’ because that is logical, and people don’t make decisions based on logic. Instead connect on an emotional level.”


appointments were made online between 9pm and 2am.
Queensland audiologist Mr Wesley Ong said his marketing tool automatically sent reminders before warranties expired and patients were grateful to come in and test their devices and receive a replacement if required.
Fechner introduced a deposit before attendance that reduced his five to six no-shows a day to zero.
“Dr Cliff says ‘innovate or die’, but I prefer to say, ‘innovate to fly’ because what happens is your choice,” Fechner said. Put an hour a week aside in the practice diary to ‘innovate’ and take baby steps testing one small change at a time such as adjustments in pricing structure, to systems or processes, he said.
Accountant Ms Katie Bryan from Propeller Advisory agreed that putting an hour aside weekly to work ‘on’ your business, not ‘in’ your business enabled innovation to start. “It’s impossible to make a decision which drives growth
Dr Cliff’s tips for a better conversion rate include:
• In the first five minutes of a consultation, talk for 15 seconds then let the patient talk the rest of the time. “It’s not our time to talk. When they come in, it’s their time to talk. Interject if you must but listen.”
• Read their patient form before so you have all the details and say, “I want to hear from you what’s going on with your hearing.” After the first question we feel we need to start talking but that’s a cardinal sin; listen.
• Don’t give too many hearing aid options which risks them going away to think about it and not returning. Make the choice easy with only a few options.
• The hardest part is getting the patient through the door so take a deposit before attendance to reduce no shows.
• Consult for at least an hour, giving time to articulate the value of your offering and do tests. Data shows consulting for this time significantly increases conversion rate.
• Have them bring a companion. The receptionist can say, "We find it very valuable to get the perspective of your partner and the full understanding". If they cannot come in person, phone them during the consult and arrange follow-up calls.
• Frame the importance of tests. If they say they have trouble hearing in restaurants, say, “The good news is we have a speech-in-noise test so I can measure your hearing in this situation”. They then understand the value of the test and bespoke diagnosis and treatment.
• When they ask, "Why these hearing aids?", never say, “Because they’re the best;” say “Because the tests show they’re the best custom fit for you.”
• Ensure your body language matches and mirrors the patient; if they sit back in the chair, you do; if they lean forward, you do also.
• Repeat their words back to them. If they say they are frustrated because they cannot hear, say “I understand you are frustrated,” but don’t say “that must be embarrassing” because then they feel you aren’t listening, it implants the idea of stigma and that’s one way to blow a consult.
• Have the patient say ‘yes’ throughout the consult so at the end it’s easier to say yes to hearing aids. To close, ask, “Is that what you want to do?”
• Train staff. Consultants can train on greeting, and script what they say on the phone, including providing scripts for new providers.
• Recommend the highest level of technology each patient can reasonably afford but say that “by the end of it you’ll be hearing your absolute best because we have followed best audiological practice".
• If patients say they’ve had hearing loss for five years so what’s the hurry in getting a hearing aid now, create a sense of urgency and react – “What, five years! I’ll clear my schedule, that’s how important it is we get this treated now".
• Self-reflect after consultations; what could you have done better? Have monthly consultation reviews. Don’t waste a single opportunity because you haven’t communicated properly; they’ll only see there’s no value if you didn’t sufficiently articulate it.
Initial success of non-invasive brain stimulation in suppressing tinnitus or altering perception of the condition has resulted in a Flinders University-led group receiving a large NHMRC grant to progress the treatment.
When audiologist Professor Raj Shekhawat started researching tinnitus 14 years ago, he looked for something that could disrupt the disorder and its perception. He found that a technique called direct current stimulation was having great success in stroke rehabilitation and began adapting it to tinnitus.
“After a couple of sessions of magnetic stimulation, stroke patients did physical training and those who had stimulation sessions early had much better improvement of their paralytic arm,” he says. “It was almost like a priming training protocol to stimulate or prime the brain which made it more ready and susceptible to respond better to the intervention which followed.”
Over the next decade and a half, trials he led in New Zealand, England and Australia found that (transcranial) direct current stimulation (tDCS) disrupted tinnitus perception immediately, reducing symptoms. But the effect was transient, lasting only a few hours.
Prof Shekhawat’s Flinders University team is now progressing this research with two upcoming trials he hopes will lead to sustained relief. The aim is for audiologists to enhance and personalise tinnitus management using brain stimulation, hearing aids, and genetic testing.
The project, which is being branded as TINNOVATE: Tinnitus Innovation and Advanced Therapeutics Enterprise, will also draw on research expertise from colleagues at The University of South Australia, the Bionics Institute in Melbourne, and The University of Sydney.
More than 200 tinnitus patients will be enrolled in the South Australian studies in 2025 and 2026. They aim to pinpoint areas of the brain that need to be targeted for optimum and sustained disruption.
“The project aims to disrupt tinnitus perception using tDCS and optimise the settings for maximum impact,” Prof Shekhawat says. “It’s simple, non-invasive – we don’t do surgery or shave people’s heads – and uses a small device with two electrodes placed on the person’s head to stimulate specific areas of the brain.
“The device generates electric current, and we place the electrodes – called anode and cathode – around the area of the brain we want stimulated. The current flows between those two electrodes across the cranium, transcranially.
“This changes polarisation of neurons in the brain which can either result in suppression of tinnitus or altered perception of tinnitus.”
The trials will investigate a form of tDCS called High-Definition tDCS which allows researchers to stimulate certain brain regions more specifically. They aim to determine whether stimulating these regions can suppress tinnitus more effectively, reducing loudness and annoyance, and for longer.


The first study will test the effect on tinnitus of stimulating two regions – the auditory cortex which processes sound, and the pre-frontal cortex which is involved in emotional perception of sound – either separately or together.
This will be tested in people with tinnitus and be compared to results from people who receive ‘sham’ stimulation, to see which treatment is the most effective and lasts the longest.
The second study will investigate changes in the brain when High Definition tDCS is used. It will use the most effective treatment strategy, identified from the first study, to do this again in people with tinnitus and do brain imaging to assess changes in detail.
The need for personalised treatment
Prof Shekhawat, Dean of Research in the College of Education, Psychology and Social Work at Flinders University, has received $2.23 million from the National Health and Medical Research Council for the novel tinnitus management project.
It combines brain stimulation with hearing aids personalised to dampen tinnitus and genetic testing to help determine which patients may be more likely to respond to this therapy.
“Tinnitus doesn’t have a cure yet and one reason is it’s a very heterogeneous condition requiring a personalised approach due to its unique impact on each individual,” he explains. “Every person who has tinnitus is unique and the way they perceive their tinnitus is unique.
“Their hearing profile is unique, as are the difficulties they encounter so we can’t have a one size fits all solution. It requires a personalised management approach.”
Tinnitus is common, with one in six Australians affected, and invisible, he adds. “Nobody can tell if someone has tinnitus by looking at them,” he says.
Prof Shekhawat is chief investigator of the project, and Dr Boaz Mui, who has a PhD in Audiology from Flinders University and is in a postdoctoral fellow role, will manage the project. Its success is about bringing in exceptionally talented people such as Mui, an outstanding student, Prof Shekhawat adds.
The project also draws on the expertise of colleagues from The University of South Australia, the Bionics Institute, and The University of Sydney.
The previous pilot and feasibility studies of tDCS in tinnitus investigated


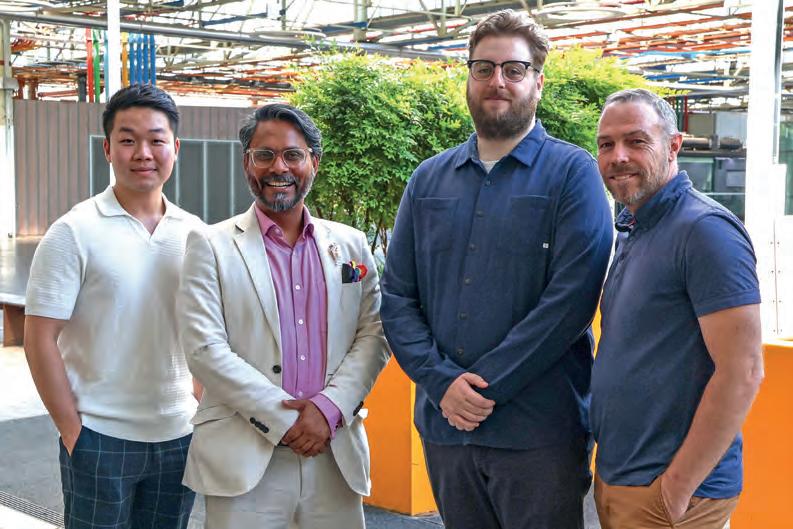
Flinders PhD student Mr Lynton Graetz, an expert in fMRI, will lead the fMRI and EEG part of the trials in collaboration with the South Australian Medical Research Institute. Mr Simon-Peter Telford, who recently passed his PhD defence with University of South Australia, will run research and media communications for the project across a steering committee of industry leading advisors and a large Investigator team.
intensity, duration, the ideal number of sessions, the best gap between sessions, and which areas should be stimulated.
The researchers found the optimum intensity and duration, and that the impact of cumulative sessions was non-linear – with an increasing number of sessions, the overall impact also increased, but reached a saturation point at six sessions.
The new trials will use those parameters and include six sessions of High Definition tDCS at 2mA (milliamp) for 20 minutes. This will be followed by hearing aid treatment with GN’s ReSound hearing aids uniquely programmed by researchers rather than just set to a standard tinnitus setting.
“We’ve partnered with GN who has generously given us their advanced hearing aids to use in the trials,” Prof Shekhawat says. “We want to replicate what happened with stroke patients in tinnitus patients. They’ll have brain stimulation to prime the brain for training but instead of physical training like stroke patients, they’ll receive hearing aids.
“They won’t be set on the tinnitus feature but programmed by us in a unique way based on our previous research. It will re-look at how we program hearing aids for people with tinnitus because conventionally, when a person with tinnitus goes to an audiologist, they look at their hearing loss and program the aid based on hearing loss, not tinnitus.”
Professor Jose Antonio Lopez-Escamez and his team from The University of Sydney’s Kolling Institute will lead genetic studies in patients with tinnitus. Their goal is to identify common and rare variants and to use them as response biomarkers to determine who are the best candidates for High-Definition tDCS therapy.
Every participant will undergo brain stimulation, receive hearing aids and undergo objective and subjective assessments including a diagnostic measure of tinnitus, fMRI (functional MRI) brain scans and electroencephalograms (EEGs) to measure brain electrical activity.
“It’s very rich data we’ll be collecting. We will correlate audiological data, fMRI data, hearing aid data and blood data to bring it all together,” Prof Shekhawat says. “We hope this will help us identify who is more likely to respond to this intervention versus others based on their hearing profile, tinnitus profile, hearing aid profile, tinnitus features or genes.”
Patients don’t feel anything from the brain stimulation and it doesn’t generate noise which is an advantage as people with tinnitus can be sensitive to sound including loud noises that can alter tinnitus perception.
The double-blind studies will ensure objective results, as the lead investigator can change settings to ensure participants and researchers are unaware who is receiving real or sham stimulation.
As any treatment can have a placebo effect, a world-first brain imaging technique to objectively measure the presence and severity of tinnitus will be used. Bionics Institute biomedical engineer Associate Professor Mehrnaz Shoushtarian developed the technique which uses near-infrared light and AI. It will generate meaningful data and hopefully provide strong evidence of how the stimulation works.
“We can then hopefully take that to market and out into the world,” Prof Shekhawat says. “In a blue-sky situation, fast forward several years, if the technology helps and things move in the right direction, we hope clinical audiologists can objectively measure tinnitus using the Bionics Institute technique and offer brain stimulation as an option for patients in their clinics.
“We could run training programs for audiologists wanting to use these techniques and options so patients can access this everywhere in Australia.”
Prof Shekhawat says South Australian audiologists with tinnitus patients wanting to be part of this “exceptionally innovative world class research” can contact the team at tinnovate@flinders.edu.au “because they will be getting access to a management option not available anywhere in the world”. Tinnitus patients interested in taking part can email tinnovatevolunteer@flinders.edu.au to participate in clinical trials.
Danish ENT surgeon DR MARTIN NUE MØLLER discusses use of the procedure as a treatment for chronic otitis media in children.

BALLOON
DILATION SEEKS TO TREAT THE CAUSE OF THE DISEASE AND, IF PROVEN EFFECTIVE IN THE FIRST LINE STUDY, IT MAY PREVENT THE NEED FOR A SECOND GROMMET FOR 50% OF PATIENTS.
Eustachian tube balloon dilation can be a first line tool in the treatment of chronic otitis media in children. We are undertaking a multi-national clinically controlled, randomised, patient blinded, prospective trial of this therapy.
The cumulative incidence of otitis media with effusion in Denmark for children younger than seven years is 61%, making the disease one of the most common in Danish children.
Denmark also has one of the world’s highest prevalence’s of ventilation tube (grommet) treatment, which is as high as 26% of chronic otitis media (COME) patients. Almost 16% of all Danish children under seven are treated with ventilation tubes at least once and some materials suggest this is as high as 25%.
Up to half of children treated with ventilation tubes fail to recover from COME and are treated with a second ventilation tube within the first two years of treatment. In Denmark with a population of only 5.9 million people, more than 18,000 children are treated with ventilation tubes every year.
pharyngeal muscles.
Also, an enlarged tuba-tonsil (local inflammatory burden of the posterior lip of the Eustachian tube orifice) contributes to dysfunction. The latter is a very common phenomenon in children under seven and has the same characteristics as adenoids, both functional and histological.
The principal result of balloon dilation of the Eustachian tube appears to be a reduction of inflammatory epithelial changes and submucosal inflammatory infiltrate of the tuba tonsil. The effect is much like that seen after adenoid removal. However, Eustachian tube dilation is not included in any part of the treatment of COME in Denmark. It is used in first and second line treatment in countries such as Germany and the USA.
Several studies have shown that balloon dilation of the Eustachian tube in children may be effective in treating COME and perhaps be better than grommets.
recurrent acute otitis media, delayed speech development and failure to thrive.
Dr Martin Nue
It is commonly accepted that the main reason for the disease is Eustachian tube dysfunction. Children under seven have different anatomy of the Eustachian tube, with a more horizontal angle of the tube which causes slightly impaired ability to open due to the less efficient pull from the
PRIMARY AND SECONDARY ENDPOINTS
If included in our study, patients with verified COME will have bilateral grommets and only balloon dilation of one ear. Patients will be their own control. We will evaluate the effectiveness of Eustachian tube dilation in those older than two and younger than seven through the need of a second grommet later when the first is extruded (failure to treatment).
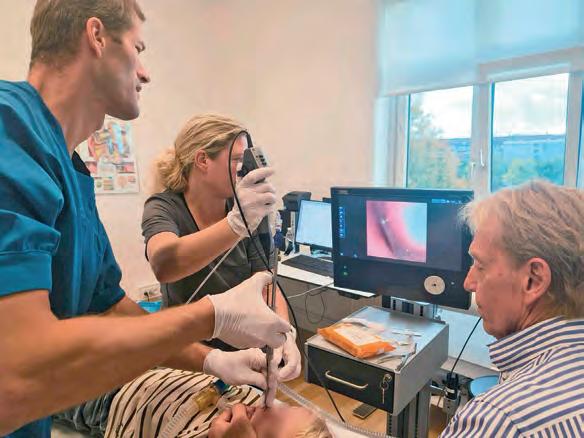
The secondary endpoint will be assessment of the prevalence of adenoids higher than Cassano grade 2 in children with COME aged two to seven years. These patients will be excluded from the study after verification by nasal endoscopy under full anesthesia.
The socioeconomic burden from COME in children is huge. Patients and parents often have multiple assessments and consultations with ENT practitioners, as well as high sick-leave, loss of sleep at night,
There is no relevant medication for patients under four, but betamethasone may be used for children aged four to seven with questionable effect and compliance. Grommets is a symptomatic treatment and introduces risks such as 3% tympanic membrane perforation, risk of infections, clogging, hearing deterioration and some literature even suggests secondary cholesteatoma. Further, 50% will need a second grommet and full anesthesia. Balloon dilation seeks to treat the cause of the disease and, if proven effective in the first line study, it may prevent the need for a second grommet for 50% of patients. If we succeed in showing benefit from this study, a second study is warranted and should be planned as a direct comparison between grommets and balloon dilation in a randomised, clinical study. A Queensland Children’s Hospital Department of Otolaryngology systematic review and meta-analysis of outcomes after balloon dilation of the Eustachian tube in children was published in the Australian Journal of Otolaryngology on 15 March 2024. Reviewers said there was hesitancy in performing it in children due to their shorter and more horizontal Eustachian tube.
The review concluded balloon dilation of the Eustachian tube was ”a safe and potentially effective procedure for the treatment of obstructive Eustachian tube dysfunction” but prospective cohort studies and randomised controlled trials were needed before it could be recommended as evidence-based management. The potential impact from our study is massive and could affect millions of children world-wide, from a socioeconomic perspective and a paediatric healthcare perspective.
*References will be in the online version.
ABOUT THE AUTHOR: Dr Martin Nue MØller is a Danish ENT surgeon and founder of Venteus surgical devices for otorhinolaryngology, head and neck surgery.
Audiologist JANETTE BRAZEL discusses a pilot program to build capacity and confidence in audiometry skills for Aboriginal Health Workers in Indigenous Communities and train them in their Certificate IV in Audiometry.

STUDENTS HAVE HAD THE OPPORTUNITY TO VISIT SCHOOLS FOR HEARING SCREENING DAYS AS WELL AS TESTING ADULT CLIENTS IN CLINIC AND COMMUNITY SETTINGS.
JANETTE BRAZEL
Middle ear disease is a chronic condition in First Nations people and there is often a lack of access to services, particularly in regional and remote areas. Otitis media occurs much earlier in infancy for Indigenous children (often the first occasion being in the first 12 months of life), than in non-Indigenous children. When left untreated, chronic otitis media can affect every aspect of the child’s life including hearing loss, education and future employment outcomes. These ongoing problems can affect quality of life, over the person’s lifespan.
In 2023 a consensus statement evolving from the Routine ear health and hearing checks for Aboriginal and Torres Strait Islander children aged under 6 years attending primary care: a national consensus statement, an extension to the existing guidelines, was recommended to include the following: “Undertake checks at least six-monthly, commencing at six months until four years of age, then at five years. Undertake checks more frequently in high risk settings for children under two years, when acceptable to families, or in response to parent/carer concerns”.

Last December in the Australian Government web report Ear and hearing health of Aboriginal and Torres Strait Islander people 2024, the following statistics were reported:
• The prevalence of hearing loss among First Nations people is high, with 43% of those aged seven and over having measured hearing loss in one ear (20%) or both ears (23%) in 2018–2019.
• A mong First Nations people assessed as having moderate to profound hearing loss, fewer than half (47%) reported having long-term hearing loss.
One possible way to address these statistics of high, and often untreated occasions of hearing loss, is to train more hearing health clinicians, particularly from Community. With that thought in mind, two teachers from the Australasian College of Audiometry (AuCA) developed a pilot program to train a
group of Aboriginal Health Workers in gaining their Certificate IV in Audiometry. Several prospective students from regional NSW coastal areas, working in Aboriginal Medical Services and Community Health organisations, were approached to take part in this program. Eight students signed up for the course with most having had some experience in ear health and with working and/or training with the teachers, audiologists Janette and Eliza Brazel, in other programs.
The students’ work environment as Aboriginal Health Workers includes assisting children, families and Elders from their communities. The Certificate IV in Audiometry includes assessing adults and screening the hearing of children aged four years and older (as outlined in the government training package HLT47415). Early identification of hearing loss in children is critical to learning language, speech and stories from their community.
The more regional and remote hearing assessors we have on the ground able to test children’s hearing (and adults’) is vital in identifying hearing health issues.
The training program is highly interactive, with two online tutorials per week, regular face-to-face workshops and clinical practicum settings, as well as yarning opportunities with other students and
their trainers. This experiential teaching model is one I have used before in my long history of teaching audiometry students. I believe early opportunities with hands-on equipment and placing students in real-life clinical settings, from the start of their training, is important to gaining confidence in using audiometric skills. Building trust is also important when building confidence in students, to ensure they excel in their studies. The program began in February 2025 and so far students have had the opportunity to visit schools for hearing screening days, as well as testing adult clients in clinic and community settings. The aim is to have the students complete the program over 12 months and then use their hearing assessment skills in their roles as Aboriginal Health Workers, to build capacity for ongoing hearing services in much needed areas.
ABOUT THE AUTHOR: Janette Brazel is a NSW audiologist on the Australasian College of Audiometry (AuCA) teaching panel. She has had a varied audiological career working across public and private institutions for almost four decades. For much of it she has worked as a teacher/trainer/ supervisor for students of audiometry, audiology and occupational health. Her main passion has been working with Indigenous communities to improve access to hearing services and build capacity for health workers in audiometric skills. She is a board member of ACAud Inc. HAASA and works for a local community health service.
The healthcare sector is a lucrative target for cyber-attacks, which means cyber security should be a top priority for hearing practice owners, writes Australian digital health expert DANIELLE PENTONY.

CYBER CRIMINALS CAN EXPLOIT WEAKNESSES WITHIN HEARING PRACTITIONER AND AUDIOLOGY ORGANISATIONS BY TARGETING THEIR SYSTEM VULNERABILITIES.
Digital transformation is central to ushering in a new era of patient care and improved operations, but implementing this is a complex process.
Healthcare providers, health technology partners and consumers have all come to trust in and rely on digital platforms to store and access health information.
As we pioneer the future of healthcare at an increasingly rapid pace, it is important to remember any digital tool, system or process is scalable, interoperable and user-friendly with a strong emphasis on data security and privacy.
Therefore, it’s critical that digital health infrastructure remains fit for purpose and cyber resilient, even as changes occur in the cyber threat environment, where both the pace of change and the levels of risk are elevated.
• S ignificant interruptions to healthcare service delivery
• R eputational damage
• D ecreased consumer confidence in the organisation’s ability to protect data.
The path forward for hearing practitioners and audiologists demands strategic thinking, concerted action, and a steadfast commitment to cyber resilience. Collective effort and innovation from leaders are important as we work collaboratively towards a more secure, resilient and trustworthy digital future.
that relate cyber security concepts to scenarios in healthcare organisations. Cyber Security Alerts – audiologists and hearing practitioners can register to receive Cyber Security Alerts and understand the cyber security risks that can impact their operation. The agency actively monitors potential cyber security risks through our dedicated Cyber Security Team. Should the team identify any potential threats, the agency sends out alerts regarding digital health software vulnerabilities and cyber-attack campaigns.
BELOW: Cyber-attacks can lead to significant interruptions to healthcare service delivery and even reputational damage.
Human factors and technologies can inadvertently create vulnerabilities or introduce security risks. These factors can include staff mistakes that may put their organisation’s data or systems at risk. Mistakes may be accidental, or come from a lack of required training, and at times it could be with malicious intent. Cyber criminals can exploit weaknesses within hearing practitioner and audiology organisations by targeting their system vulnerabilities. Attackers are often driven by the potential for financial gain, with the healthcare sector particularly lucrative due to the potentially sensitive nature of patient data.
The consequence of these cyber-attacks can lead to:
• D ata breaches through the loss or theft of sensitive information
At the Australian Digital Health Agency, we have embarked on a collaborative journey with the digital healthcare sector to build a unified vision for the future security of digital health. We have collaborated with states and territories, and peak bodies, to deliver the requirements of the Cyber Security Strategy 2022-2025.
In addition, there are three key strategies and initiatives specific to digital transformation and cyber security in the health sector: the Digital Health Blueprint, the National Digital Health Strategy, and the Agency Cyber Security Strategy. All three recognise the importance of cyber security and security by design in the healthcare sector.
A core part of this strategy is uplifting cyber security awareness across the entire healthcare ecosystem, including with allied health practitioners, to ensure we proactively adapt to changes in the threat environment and support the secure evolution of digital health. Security underpins the agency’s strategic priorities and achievements in digital healthcare to date. It will remain a critical enabler into the future.

Digital Health Security Awareness –the agency has developed free cyber security e-learning courses from a range of healthcare settings and disciplines, including allied health. The Digital Health Security Awareness e-learning course includes five modules and examples
Cyber Champions Network – join the agency’s new Cyber Champions Network. This program is fostering a proactive, engaged, and security-conscious healthcare ecosystem to significantly strengthen Australia’s defence and response against cyber threats.
Cyber skills can protect organisations through:
• Enhanced security awareness and intelligence sharing
• T hreat identification abilities
• Leading and driving cultural and behavioural change
• R educing the likelihood of cyber incidents and data breaches
• I mproved workplace cyber resilience
• I mproved and more up-to-date compliance and risk management.
It is only by working together that the agency and the Australian healthcare community will be able to continue strengthening our individual and collective cyber posture for a truly resilient healthcare ecosystem.
Visit the Australian Digital Health Agency’s website at www.digitalhealth. gov.au to learn more about how to manage cyber security effectively.
ABOUT THE AUTHOR: Danielle Pentony is the Australian Digital Health Agency’s chief information security officer. She is a champion of digital healthcare, and responsible for the development, deployment, and secure operation of critical national healthcare assets, including the sensitive healthcare information of Australians.

improving patient outcomes – has not always universally embraced this ethos of solidarity. In my experience, and in talking with many colleagues, it is not uncommon for audiologists to openly criticise one another, whether in professional settings or, unfortunately, in front of patients. While these critiques may stem from genuine differences in practice, they can also be motivated by financial interests, such as gaining a patient’s business.
I worry this behaviour, while potentially advantageous in the short term, can erode the credibility of audiology over time. When patients see practitioners undermining each other, they may perceive the profession as fragmented and unreliable. This can lead to broader scepticism about the value of audiology services, impacting not only individual practitioners but the profession.
The broader impact of public criticism

patient outcomes and foster innovation within the field.
• Educating patients: Emphasise the scientific and evidence-based nature of audiology to reinforce its legitimacy as a healthcare profession.
• Setting an example: Senior audiologists and leaders should model respectful and constructive behaviour, encouraging a culture of mutual respect.
ABOVE: By promoting collaboration, audiologists can enhance patient outcomes and foster innovation.
The medical profession:
Presenting a unified front
Medical practitioners everywhere have long recognised the importance of maintaining a unified front. It is uncommon to witness overt criticism among doctors, particularly in public or in front of patients. This is not due to a lack of disagreements; rather, it reflects a deep understanding of the potential damage such behaviour can cause to the public’s confidence in the medical field. When a doctor publicly criticises another, it risks undermining trust not just in the individuals involved but in the medical profession as a whole. Doctors are guided by a commitment to science-based, evidence-driven practices. A unified approach reassures patients that their care is consistent, credible, and rooted in shared expertise. Disagreements are typically addressed through private channels, ensuring the trust patients place in the healthcare system remains intact.
Audiology: A lesson in professional conduct
In contrast, audiology – a field equally grounded in science and dedicated to
The consequences of professional criticism extend far beyond the immediate context. In healthcare, trust is delicate, and actions that diminish it can have lasting repercussions. When patients perceive disunity or hostility within a profession, they may:
1. Lose trust in care: Patients may hesitate to follow recommendations, undermining their treatment outcomes.
2. Avoid necessary services: Distrust could lead to patients delaying or avoiding vital healthcare interventions, particularly in audiology, where early intervention is critical.
3. Harm the profession’s reputation: A fractured professional image can make it harder to attract new talent, secure funding, or gain the respect of other healthcare sectors.
Moving forward: Building trust through professional etiquette
To secure the future of audiology in Australia, practitioners must prioritise professionalism and the collective good over individual interests. This means:
• Avoiding public criticism: Differences in opinion should be addressed privately, ensuring that patients see a cohesive and supportive profession.
• Promoting collaboration: By working together, audiologists can enhance
Learning from medicine
Australian audiologists can draw inspiration from the medical profession’s approach to handling disagreements. By prioritising patient trust and focusing on the reputation of the profession, audiology can strengthen its standing within the healthcare landscape. Collaboration and mutual respect are not just aspirational values –they are practical strategies for ensuring the long-term credibility and success of the field.
How a profession manages internal conflicts speaks volumes about its maturity and commitment to the public it serves. In healthcare, where trust is everything, professionals must put the collective good above individual interests. Audiology has the opportunity to embrace a culture of collaboration and professionalism, ensuring it remains a respected and trusted field. By avoiding public criticism and working together, audiologists can build a stronger, more unified profession that benefits both practitioners and the patients they care for.
Name: Dr Yazdaneh Galt.
Affiliations: ACE Audiology, Bulleen and Ivanhoe.
Location: Melbourne, Victoria
“BY PRIORITISING PATIENT TRUST AND FOCUSING ON THE REPUTATION OF THE PROFESSION, AUDIOLOGY CAN STRENGTHEN ITS STANDING WITHIN THE HEALTHCARE LANDSCAPE.”


to raise awareness about the industry.
Audiology Centre as a clinical audiologist/clinical support from 2017 to 2024.


more than 35 years’ experience in public education leadership positions, she recently retired as deputy director-general of the ACT Government’s Education
jurisdictional and national boards and committees, including the Australian Curriculum and Assessment Authority Board, and is an Adjunct Professor at Macquarie University and the University of Canberra.
peak industry body for Australia’s medical colleges, organisation noted her proven track record in executive roles across healthcare, professional associations, and healthcare corporations, previously serving as CEO of the Australasian Sonographers Association for several years and, most recently, Speech Pathology Australia.

and promoting the work of Hearing Australia and its delivery of quality care to its clients. Managing director Mr Kim Terrell congratulated Ms Crouch on her reappointment and thanked her for her leadership and guidance, which will support Hearing Australia in continuing to provide world leading research and hearing services for the wellbeing of all Australians.

auditory sciences, has made Dr Bettina Cockroft its new chief medical officer. She has had senior roles in large pharmaceutical companies and biotech organisations, currently serving on the board for two US public biotech companies. Previously, Dr Cockroft was chief medical officer at Auris Medical, where she led clinical development programs focused on ear disorders, including tinnitus and sensorineural hearing loss.
To list an event in our calendar please email helen.carter@primecreative.com.au

IAA SUMMER SUNSET SESSION
Enhancing cochlear implant mapping through objective measurement Online 23 April independentaudiologists.net.au
CI2025 BOSTON
American Cochlear Implant Alliance conference Boston, US 30 April – 3 May acialliance.org
12TH INTERNATIONAL ADULT AURAL REHABILITATION CONFERENCE Massachusetts, US 5 May hearingrehab.org
NEXTSENSE
How music training can enhance auditory and psychosocial outcomes for DHoH adults and children
Online 28 May nextsense.org.au
CERUMEN MANAGEMENT 101 COURSES
In person training, theory and practicuum. Perth - 6 June. Macquarie University - 13 June. earhealthcourses.com.au

NEXTSENSE
Exploring the intersection between identify, stigma and cochlear implants Online 17 June nextsense.org.au
HEARING LOSS ASSOCIATION OF AMERICA
HLAA 2025 Convention Idianapolis, US 11-14 June hearingloss.org
VCCA2025
Virtual conference on computational audiology Online 26-27 June computationalaudiology.com
ASOHNS Frontiers 2025 Hobart, Australia 13-15 November asohns.org.au

Thanks to the industry’s most advanced processor, G2 Neuro Processor, and Neuro Sound Technology 2.0 – our proprietary sound experience system that’s agile, precise and designed to mimic the way the human brain works – Edge AI gives every person who wears them the edge they’ve been looking for!
styles only)
