YOUR COMMUNITY RESOURCE FOR WHAT’S HAPPENING IN HEALTH CARE WINTER 2023 Published by Pennsylvania’s First Medical Society Nancy Fuhrman FTC Proposes Rule to Ban Noncompete Clauses Crisis of Healthcare Financing in America SHiNE: Lighting the Way to Excellence in Cancer Care, Close to Home p 6 p 9 p 12 p 16
OFFICERS 2023
President
David E. Bobman, MD
President Elect
Mahmoud K. Effat, MD Vice President
Richard O. Oyelewu, MD Treasurer
Winslow W. Murdoch, MD Secretary
Christina J. VandePol, MD
Editor & Immediate Past President
Bruce A. Colley, DO
Board Members
Norman M. Callahan, III, DO
Heidar K. Jahromi, MD
Mian A. Jan, MD
John P. Maher, MD
Manjula K. Naik, MD
Sean V. Ryan, MD
Francis X. Speidel, MD
Lynne A. Stilley, MBA Executive Director
Chester County Medical Society 1050 Airport Road PO Box 5344
West Chester, PA 19380-5344
Website – www.chestercms.org
Email – OurCCMS@gmail.com
Telephone – (610) 425-9190
Chester County Medicine is a publication of the Chester County Medical Society (CCMS). The Chester County Medical Society’s mission has evolved to represent and serve all physicians of Chester County and their patients in order to preserve the doctorpatient relationship, maintain safe and quality care, advance the practice of medicine and enhance the role of medicine and health care within the community, Chester County and Pennsylvania.
The opinions expressed in these pages are those of the individual authors and not necessarily those of the Chester County Medical Society. The ad material is for the information and consideration of the reader. It does not necessarily represent an endorsement or recommendation by the Chester County Medical Society.

PUBLISHER: Hoffmann Publishing Group, Inc. 2669 Shillington Rd, Box #438, Reading, PA 19608 For Advertising Information & Opportunities Contact: Tracy Hoffmann 610.685.0914 x201 tracy@hoffpubs.com www.Hoffpubs.com Contents WINTER 2023 Letters to the Editor: If you would like to respond to an item you read in Chester County Medicine, or suggest additional content, please submit a message to OurCCMS@gmail.com with “Letter to the Editor” as the subject. Your message will be read and considered by the editor, and may appear in a future issue of the magazine. Cover: Log House, 1920, Nancy Furhman Read more in The Art of Chester County on page 16. In Every Issue 3 President’s Message 16 The Art of Chester County 4 Letter to the Editor 6 FTC Proposes Rule to Ban Noncompete Clauses, Which Hurt Workers and Harm Competition 9 SHiNE: Lighting the Way to Excellence in Cancer Care, Close to Home 11 Did You Know? 12 Crisis of Healthcare Financing in America Features 20 Make Health the End Goal of Chronic Pain Management 24 Southeast PA Area Health Education Center Offering Community Health Worker Trainings 26 Wait a S.E.C.: Sympathy, Empathy and Compassion 28 Pursuit of Partisan Political Power 30 PAMPAC Provides a Unified Voice to Help 6
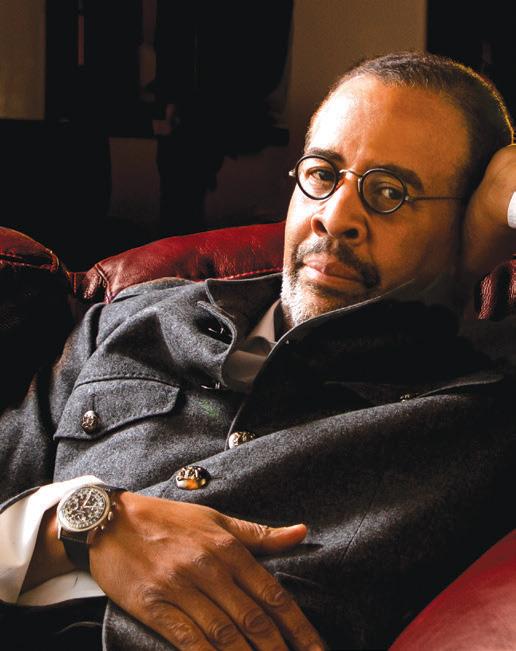
David E. Bobman, MD

PRESIDENT’S MESSAGE
BY DAVID E. BOBMAN, MD PRESIDENT OF CHESTER COUNTY MEDICAL SOCIETY

They say “time flies.” As I reflect on my career of over 30 years, several thoughts at once come to mind. First, it seems like the time has passed in “the blink of an eye.” In large part, this is because the practice of medicine is an unusually rewarding and fulfilling career. It is also a very dynamic one. Though there have been many changes in the practice of medicine, some things have stayed the same. For instance, we are again in a situation where it is a high priority to address medical malpractice venue reform. As the hard-fought reforms we were able to have enacted years ago, like sandcastles in the surf, have eroded away and again need to be addressed.
Access to medical care has in the past been an issue, and now has become an even greater issue. In part due to effects of the COVID crisis, hospital closures, and physician shortages, our patients are often waiting many months for doctors’ appointments or procedures. These represent only some of the issues which our medical society is working on.
Over these past many years, there has been a further diversification in medical practice. In the past, most physicians were in private practice; now many physicians have opted for hospital employment, pairing with private equity, or working in the pharmaceutical industry. This creates differing aims and practice needs for these physicians. For this reason, to better understand how we can be of assistance to the physician community, we would like to hear directly from member and non-member physicians as to their concerns, wants, and needs. Please email us at OurCCMS@gmail.com for this purpose.
At this time, I would also like to introduce Lynne Stilley, our new Executive Director. Lynne comes to us with a strong background in medical affairs and therefore knowledge of the medical system. I am impressed by her enthusiasm, tireless energy, and intriguing new ideas as we move forward. She has already been working on networking and revamping our website, as well as learning the workings of our society. I look forward to working together with her for many years to come.
At the same time, we will be saying goodbye to David McKeighan, our outgoing executive. Losing his guidance is bittersweet as we will sorely miss his participation but are happy for him in his retirement. David, along with our recent past presidents, has changed the Chester County Medical Society into a much more dynamic organization. David, thank you for all you’ve done!
Fond Regards, David
Winter 2023
What’s on your mind? Help us to learn more about emergent trends affecting your work! Write to us at: OurCCMS@gmail.com www. CHESTERCMS .org
WINTER 2023 | CHESTER COUNTY Medicine 3
Letter to the Editor
CENSORSHIP, MEDICINE AND DISPUTE
BY FRANK SPEIDEL, MD, MBA, FACEP
“Eppur si muove” (“And yet it moves”)
—Gallileo Gallilei, 1633
“Science is the organized skepticism in the reliability of expert opinion.”
“I would rather have questions that can’t be answered, than answers which can’t be questioned.”
—Richard Feynman
In the July 2022 Annals of Emergency Medicine (Volume 80, No. 1), the News and Perspective Section featured a special contribution: “The Other Pandemic: As Disinformation and Misinformation Go Viral, Attempts to Reign It In are Met With Confusion and Frustration” by Soo Youn. This opinion is timely and worth the read. It invites reflection and discussion and represents the concerns of many. Ms. Youn seems concerned with limiting circulation of misinformation that harms. She relates that no physician in California “…had their license revoked in connection with the spread of COVID-19 related misinformation …”. She then describes the challenge tech companies (Meta, Twitter, etc.) face in knowing who and what to censor, suppress or shadowban. Soo Youn seems to have leapt to the conclusion that speech outside the majority opinion must be curtailed for the good of all. I also sense an unstated assumption by the author that someone, somewhere knows with unchanging certitude, the truths of the pandemic.

The problem Ms. Youn considers is not new nor limited to medicine. It dates to the 4th century BC Greece and tracks through our shared culture. In 399 BC the citizens of Athens found Socrates guilty of corrupting the youth and disrespecting the acknowledged city gods. He asked questions. He challenged the state’s values.
The containment of misinformation progressed through the middle-ages. In Europe in the 17th century, we see Galileo Galilei and his helio-centric heresy contained, at least for a while, by the Roman Inquisition. I think both the Athenians and Inquisitors were acting for a cause they believed decent and vital. But how do we protect ourselves from those who recommend drinking bleach to cure COVID while avoiding becoming wellmeaning Inquisitors?
Beginning with John Milton’s Areopagitica in 1644, through John Stuart Mill’s On Liberty in 1859 to Andrew Doyle’s Free Speech in 2021, society has examined the benefits of unregulated, unlicensed speech and the harm of foolish, prattling delusions. Unless there is imminent harm, such as drinking bleach, our culture has adopted more speech not less speech as the antidote to bad ideas. And I think the solution to the Bleachers, is persistent, well thought and presented, evidence-based refutation of the efficacy and warning of the certain harms.
And we have adopted this value, that the concept of exchange of ideas, especially contested ideas, is the way we discover what the true and valid. A paper is published in a peer reviewed journal and then undergoes continuous review and validation by the larger community of the interested. Publication by a prominent respected journal is not validation. In 1998 Andrew Wakefield published in Lancet an article linking autism to the MMR vaccine. Lancet retracted the article 12 years later, but the damage was done. Out of this foolery, anti-vaxxers gained momentum. Events such as this remind us that rigorous, questioning skepticism is healthy, that recognized experts and institutions may err profoundly.
During the pandemic we have seen many ideas advanced with authoritarian certainty and mandated. One could be censored or de-platformed for questioning the origin of the virus, the value of school closures, the efficacy of “masking” or the benefits of shut-downs. These ideas may or may not be valid. But what benefit is there when we do not examine them vigorously?
Are we better off when experts declare we cannot question the “settled” science? Was science settled in 1905 before Einstein published? I think not. For as the polymath astrophysicist Carl Sagan remined us “… there are no sacred truths; all assumptions must be critically examined; arguments from authority are worthless.”
Thoughts?
Editor’s Note:
Dr. Speidel has a community television show “The Doctor is In” on Radnor Studio 21, Main Line Network, (public access tv). The shows include a wide range of interesting topics and guests and are available for viewing on You Tube at: https://tinyurl.com/48m4erzh.
4 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org



Meet Our Medical Banking Expert Anil Punjwani, Senior Relationship Manager (445) 231-3976 | CitadelBanking.com/Medical WELCOME TO BETTER Built for Your Practice BUSINESS BANKING We understand that starting, running, and expanding a practice is no small feat. Our team of Relationship Managers offers years of experience partnering with medical professionals to develop custom strategies that address their distinct healthcare business needs. Citadel is recognized as a Forbes 2022 Best-in-State Credit Union. Federally Insured by NCUA
FTC Proposes Rule to Ban Noncompete Clauses, Which Hurt Workers and Harm Competition
BY PETER KAPLAN, OFFICE OF PUBLIC AFFAIRS, FEDERAL TRADE COMMISSION
Agency estimates new rule could increase workers’ earnings by nearly $300 billion per year
The Federal Trade Commission proposed a new rule that would ban employers from imposing noncompetes on their workers, a widespread and often exploitative practice that suppresses wages, hampers innovation, and blocks entrepreneurs from starting new businesses. By stopping this practice, the agency estimates that the new proposed rule could increase wages by nearly $300 billion per year and expand career opportunities for about 30 million Americans.
The FTC is seeking public comment on the proposed rule, which is based on a preliminary finding that noncompetes constitute an unfair method of competition and therefore violate Section 5 of the Federal Trade Commission Act.
“The freedom to change jobs is core to economic liberty and to a competitive, thriving economy,” said Chair Lina M. Khan. “Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand. By ending this practice, the FTC’s proposed rule would promote greater dynamism, innovation, and healthy competition.”
Companies use noncompetes for workers across industries and job levels, from hairstylists and warehouse workers to doctors and business executives. In many cases, employers use their outsized bargaining power to coerce workers into signing these contracts. Noncompetes harm competition in U.S. labor markets by blocking workers from pursuing better opportunities and by preventing employers from hiring the best available talent.

“Research shows that employers’ use of noncompetes to restrict workers’ mobility significantly suppresses workers’ wages—even for those not subject to noncompetes, or subject to noncompetes that are unenforceable under state law,” said Elizabeth Wilkins, Director of the Office of Policy Planning. “The proposed rule would
ensure that employers can’t exploit their outsized bargaining power to limit workers’ opportunities and stifle competition.”
The evidence shows that noncompete clauses also hinder innovation and business dynamism in multiple ways— from preventing would-be entrepreneurs from forming competing businesses, to inhibiting workers from bringing innovative ideas to new companies. This ultimately harms consumers; in markets with fewer new entrants and greater concentration, consumers can face higher prices—as seen in the health care sector.
To address these problems, the FTC’s proposed rule would generally prohibit employers from using noncompete clauses. Specifically, the FTC’s new rule would make it illegal for an employer to:
• enter into or attempt to enter into a noncompete with a worker;
• maintain a noncompete with a worker; or
• represent to a worker, under certain circumstances, that the worker is subject to a noncompete.
The proposed rule would apply to independent contractors and anyone who works for an employer, whether paid or unpaid. It would also require employers to rescind existing noncompetes and actively inform workers that they are no longer in effect.
The proposed rule would generally not apply to other types of employment restrictions, like non-disclosure agreements. However, other types of employment restrictions could be subject to the rule if they are so broad in scope that they function as noncompetes.
This NPRM aligns with the FTC’s recent statement to reinvigorate Section 5 of the FTC Act, which bans unfair methods of competition. The FTC recently used its Section 5 authority to ban companies from imposing onerous noncompetes on their workers. In one complaint, the FTC took action against a Michigan-based security guard company and its key executives for using coercive noncompetes on low-wage employees. The Commission also ordered two of the largest U.S. glass container manufacturers to stop imposing noncompetes on their workers
6 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
CCMS Members – stay tuned for updates on this important matter with specifics on how it will affect physicians!
PentaHealth Colonial Family Practice

217 Reeceville Road, Suite A, Coatesville, PA 19320
610-269-9448
PentaHealth Primary Care Downingtown

142 Wallace Avenue, Suite 201, Downingtown, PA 19335
610-873-2700
PentaHealth Family Practice West Chester
1240 Wrights Lane, West Chester, PA 19380
610-431-1210
PentaHealth Endocrinology
795 East Marshall Street, Suite G2, West Chester, PA 19380
610-431-7929
PentaHealth Family Practice Newtown Square
4667 West Chester Pike, Newtown Square, PA 19073
610-356-7870
PentaHealth Village Family Medicine at Lionville
93 West Devon Drive, Suite 100, Exton, PA 19341
610-321-0200
because they obstruct competition and impede new companies from hiring the talent needed to enter the market. This NPRM and recent enforcement actions make progress on the agency’s broader initiative to use all of its tools and authorities to promote fair competition in labor markets.
The Commission voted 3-1 to publish the Notice of Proposed Rulemaking, which is the first step in the FTC’s rulemaking process. Chair Khan, Commissioner Rebecca Kelly Slaughter and Commissioner Alvaro Bedoya issued a statement. Commissioner Slaughter, joined by Commissioner Bedoya, issued an additional statement. Commissioner Christine S. Wilson voted no and also issued a statement.
The NPRM invites the public to submit comments on the proposed rule. The FTC will review the comments and may make changes, in a final rule, based on the comments and on the FTC’s further analysis of this issue. The comment period is open through Mar 10, 2023.
The Federal Trade Commission works to promote competition, and protect and educate consumers. You can learn more about how competition benefits consumers or file an antitrust complaint. For the latest news and resources, follow the FTC on social media, subscribe to press releases and read our blog.
Editor’s Note – for those reading this article in hard-print please go to the FTC website to view with hyperlinks: https://www.ftc.gov/.
PentaHealth Family Practice Exton
770 West Lincoln Highway, Exton, PA 19341
610 -269-1372
PentaHealth Internal Medicine West Chester
520 Maple Avenue, Suite 4, West Chester, PA 19380
610-430-8200
PentaHealth at Mt. Airy Family Practice
760 Carpenter Lane, Philadelphia, PA 19119
215-848-6880
WINTER 2023 | CHESTER COUNTY Medicine 7 www. CHESTERCMS .org
IT’S YOUR #1 DEFENSE AGAINST ONE OF THE MOST LETHAL CANCERS.
It’s fast. It’s painless. Most insurance will cover it for patients 45 or older. And it could save their lives.
Colon cancer can be deadly when it’s not caught early. But it can be completely eradicated through early detection by colonoscopy. Now, thanks to a GI Genius™-enabled colonoscopy, technology aided by artificial intelligence, doctors at Main Line Gastroenterology Associates can diagnose colon cancer with unprecedented accuracy.

DON’T PUT IT OFF. REFER YOUR PATIENTS FOR A COLONOSCOPY TODAY.
COLONOSCOPY CANCER
Main Line Gastroenterology Associates Main Line Gastroenterology Associates Call USDH at 610-644-6755 or schedule online at usdigestivehealth.com
It could be the choice of your patient’s life.
SHiNE: Lighting the Way to Excellence in Cancer Care, Close to Home
 BY MARY T. BOYLSTON, ED.D.
BY MARY T. BOYLSTON, ED.D.
There are words that fill us with joy…It’s a girl! It’s a boy! You won the lottery!
And then there are words that cause alarm:
“You have cancer.”
Shock and denial tangle hopelessness and depression around the recipients of these words as the battle against an invisible opponent begins. Innumerable emotions emerge, especially isolation while many shudder helplessly, alone in their fight.
Fortunately, the struggle toward wellness and longevity for a patient living with cancer at The Abramson Cancer Center at Penn Medicine Chester County Hospital has team support. In fact, the person has not been abandoned but has an entire community helping them as they focus on recovery and health with the assistance of SHiNE.
A unique prototype of community assistance, SHiNE is a volunteer-run organization that provides services and programs to assist patients living with cancer and their families. In 1997, community activist Maria McCool developed the Additions Program to provide cancer patients with a day of beauty which included a wig fitted and styled to make each person feel and look like themselves again. Through her efforts, SHiNE emerged as a community initiative.
The word shine can be associated with brilliance, brightness, sparkle, and radiate. Chester County’s SHiNE embraces the connotation while illuminating the darkness that patients may experience with their cancer diagnosis.
The Center for Disease Prevention and Control (CDC) (2023) maintains nationwide cancer statistics. In 2019, 1,752,735 new cancer cases were reported as 599,589 died from the disease. For every 100,000 people, 439 new cancer cases were reported with 146 deaths. This data indicate trends, demand for preventive efforts, elimination of disparities, and improved patient outcomes.
According to the American Cancer Association (ACA) and National Cancer Institute (NCI) (2022), the number of individuals living with a cancer diagnosis continues to rise
nationwide. The ACA disclosed more than 50% of the survivors were diagnosed in the past ten years, and 18% diagnosed more than 20 years ago as two out of three survivors are age 65 or older. These remarkable statistics testify to the success of early detection, treatment, and holistic person-centered care.
According to the Pennsylvania (PA) Department of Health (DOH), cancer is the number two cause of death behind heart disease. Based on data provided between 2016 and 2020, death rates have fallen in Chester County with a lifetime risk of one in five Pennsylvanians dying of cancer. The PA DOH Cancer Statistics Dashboard reveals the number of new cancer cases in 2019 was 79,004 with 27,703 deaths and 725,408 survivorship (between 1985 and 2018). PA rates for men and women for all cancers were lower in Chester County than the PA incidence rates between 2015 and 2019 (PA DOH, 2023). Yet, there are neighbors who have heard or will hear the dreaded words:
“You have cancer.”
SHiNE supports the person’s journey toward wellness. According to the mission, “Our goal is to provide support to the individual so that their strength, courage, and heart will continue to shine. Through the generosity of our neighbors, SHiNE aims to lessen the burdens of this disease by helping patients in Chester County to confront the challenges of cancer with dignity, determination, and hope.”
A cancer diagnosis can impact the entire person. The American Cancer Association (ACA, 2023) asserts patients living with cancer may need extra assistance to deal with the bodily and emotional changes that have been affected by the diagnosis and treatment. Emotions run the gamut between grief, hope, financial worries, and fear of death and dying. The ACA recommends counseling, support groups, education, and spiritual care. To enhance longevity, Life After Cancer Treatment (National Cancer Institute, 2022) suggests the patient develops a survivorship care plan which includes treatment summaries, follow up appointments, preventive measures that assist in wellness, description and abatement of cancer treatment side effects, and methods to manage physical and mental health.
continued on next page >
WINTER 2023 | CHESTER COUNTY Medicine 9 www. CHESTERCMS .org
Depicted in Figure 1, SHiNE’s services are part of an evidencebased program of care that aids the individual and family. With a holistic approach, defined as care of the mind, body, spirit, and emotions, SHiNE constructed a model of services and programs that can assist the patient to battle the disease. When a patient is treated holistically, patient-centered care can be actualized. Dr. Andrew Higgins (2022), a board-certified general surgeon, claims a holistic regimen can enhance patient outcomes and complement traditional treatments. For example, diet changes can improve and support overall health. Whereas massage stimulates blood flow and the feeling of wellbeing. Comparably, acupuncture can provide relief for certain ailments. Through donations, SHiNE provides these services free, based upon need, thereby helping to improve the patient’s quality of life.
SHiNE’s Services
Nurse Navigators
Transportation to and from therapies
Wig or headwear
Emotional support through participation in support groups
Treatment padfolios to track appointments, treatments, and documents through a custom organizer
Fitness membership at a participating gym
Therapeutic massage performed by an oncology-certified
masseuse
Acupuncture
As a volunteer organization, SHiNE’s fund-raising efforts offer patients an advantage in their battle as they maintain an administrative overhead of less than 2%. It is a grassroots and


community effort that assists the lives of people who may need it the most. Upon arrival at The Abramson Cancer Center at Chester County Hospital, the newly diagnosed patient living with cancer is given a padfolio to organize treatments and services. The nurse navigator helps patients schedule appointments and assists in obtaining other services, such as emotional support. Transportation to treatments is offered to patients who do not have any alternatives to stay on schedule without interruption.
The wig program, created by Maria McCool, offers patients the capability to look like their former self with a wig styled by one of the stylists at Calista Salon in West Chester.
SHiNE’s additional services include fitness memberships, acupuncture, and therapeutic massage. The goal is to promote determination, nurture dignity, and inspire hope.
As COVID-19 negatively impacted community organizations like SHiNE, Chester County businesses found unique ways to support one another. For example, Andiario Restaurant in West Chester sponsored An Evening to SHiNE and donated 100% of the proceeds to patients living with cancer. Similarly, Exton Place located in Exton, PA holds SHiNE Days with a donation of a percentage of sales.
Volunteers organize fundraising events annually, which include but are not limited to individual and corporate donations, SHiNE in the Vines events, West Chester’s Side Bar & Restaurant’s SHiNE golf outing and popular beard-growing contest Shave-Off for SHiNE, and The Eagles Home Association of West Chester golf outing. Annually, Ivan and Lisa Kaplan of Kaplan’s Fine Jewelers on Market Street in West Chester donate a stunning piece of jewelry to be raffled off with all proceeds earmarked to the care of patients who are battling cancer.
Neighbor helping neighbor is a paradigm associated with SHiNE as many individuals have been impacted by the generosity of the community. For example, Ann, an 85-year-old wife and mother of six, led an active life going to daily church, attending
10 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
SHiNE: Lighting the Way to Excellence in Cancer Care, Close to Home continued from page 9
family and community events, and enjoying life as a senior citizen. Ann was diagnosed with cancer during a routine procedure. She entered The Abramson Cancer Center at Chester County Hospital for chemotherapy. Anxious about the treatment, she relaxed when she met her chemotherapy nurse and was given a SHiNE padfolio presenting their programs and services.
Overwhelmed by the kindness of individuals and families she did not know; Ann was strengthened by their benevolence. Although donors of the services are anonymous, Ann knew that someone was generous enough to think about the unique needs of patients living with cancer. Her resolve to fight her diagnosis grew. With holistic, patient-centered treatment, Ann lived two more fulfilling years and spent time with family, friends, church, and her community. She took trips, headed ‘down the shore’, and enjoyed the simple joys of life. Although eventually succumbing to cancer, Ann finished her loving life uplifted by the encouragement of SHiNE supporters. She testified how SHiNE’s services and volunteers strengthened her during the darkest of times. In Ann’s memory, donations were sent to SHiNE to assist other patients in need.
Ann’s story is one of many as there are others who work diligently to fund SHiNE’s services and programs. Laurie Hissey, a West Chester resident, embraced the mission and annually hosts a paddle tournament at Radley Run, Kennett Square, and Concord Country Clubs to raise funds. Her efforts as a patient living with cancer have raised more than $60,000 for her community.
SHiNE’s profile asserts “our community, our patients, our responsibility.” With organizations like SHiNE and volunteers like Laurie, the words:
“You have cancer,” continue to be a call to step up and support the vulnerable.
As SHiNE celebrates its 25th anniversary, tenacious volunteers will continue to seek creative ways to actualize its mission. For more information about SHiNE and its services:

The Chester County Hospital Foundation ATTN: SHiNE
701 E. Market Street
West Chester, PA 19380
To access SHiNE Patient Services, please speak to a Chester County Hospital Social Worker, Nurse Navigator, or Health Care Provider.
Did You Know?
Number of Medical Liability Cases Filed in Philadelphia Dramatically Increases
The number of medical malpractice cases filed in the Philadelphia Court of Common Pleas in the first week of 2023 has already surpassed the number of cases filed during the entire month of January 2022. Recent data collections show that between January 1, 2023 and January 6, 2023 there were 19 medical malpractice cases filed in the Philadelphia Court of Common Pleas. In comparison, there were 16 medical malpractice cases filed in the same court in all of January 2022.
Following the Pennsylvania Supreme Court’s decision to rescind the venue rule for medical malpractice cases in the Commonwealth, PA Coalition for Civil Justice Reform warned lawmakers that there would likely be an increase in cases filed in high-verdict jurisdictions, of which Philadelphia is consistently rated one of the worst in the country. PCCJR will continue to closely monitor the filings and provide updates.
Follow this story and more on the PCCJR website:
https://paforciviljusticereform.org/
Get involved with the efforts to educate the community about the pending crisis in medical professional liability. Help put a stop to venue shopping which risks Pennsylvania’s medical care and jobs and puts patients in jeopardy. Become a member of the PCCJR & receive regular updates and advocacy information.

WINTER 2023 | CHESTER COUNTY Medicine 11 www. CHESTERCMS .org
Crisis of Healthcare Financing in America
 SEAN V. RYAN, MD, MBA
SEAN V. RYAN, MD, MBA
On a late Saturday night in Coatesville, PA, an altercation erupted between a group of young teenagers. As is too often the case in America today, gunfire left one young man with a bullet wound to the abdomen with injuries to the major vascular structures and intestines. Bleeding internally and dying in the street, the prognosis was grim. Police responded quickly and rather than wait for EMS to arrive, made the risky decision to transport the patient to the nearest hospital in their trooper car, known as a “scoop and run,” to quickly get him to care when every minute was critical to survival. On route, the emergency room was notified of their impending arrival. The ER staff then called general and vascular surgeons, Donelle Rhoads and Gerald Patton, seasoned veterans, who performed major abdominal surgery in a specially designed trauma bay in the ER designed and equipped for just such an emergency. In short order, Drs. Rhoads and Patton manage to control major bleeding and organ damage in what is known as “damage control surgery.” Once clinically stable, the patient was transferred via helicopter to the world-renowned Trauma Service at the University of Pennsylvania where cutting edge critical care and further lifesaving surgery was delivered for as long as it took for the patient to recover. All of this was done without any question of insurance coverage or ability to pay. This is the American medical system at its finest.
Dramatic stories such as the above are not all that rare in modern healthcare in America. Maybe it’s the much more routine emergencies, but no less stressful, like a heart attack or stroke where minutes count and a life is in the balance. In the modern American healthcare system and hospitals, life-saving care can be mobilized within a fraction of an hour, delivered by coordinated, highly trained and dedicated doctors and nurses utilizing the latest in modern medical technology, imaging, and critical care equipment. The modern American healthcare system is truly a wonder of the world, but often criticized for its massive expense and relatively poor outcomes when compared to other first world industrialized countries. In 2023, the US healthcare system is under serious financial threat. As our young patient will find
out, with or without insurance coverage, delivering care is not the issue, but how we choose to finance care is riddled with perverse incentives that will lead us to eventual collapse. It is unsustainable for all parties involved.
Patients, Doctors / Nurses and Hospitals, the key stakeholders delivering frontline care, are all under historic strain. The reasons for how we got here, and the many potential solutions, are beyond the scope of this article, but I hope to delve into these topics in future articles. My goal is to briefly outline the current economic realities facing three critical players in the modern MedicalIndustrial Complex: The Patient, the Hospital, and the Physician.
The Patient
In 2000, the average annual family employer-based health insurance premium was roughly $6,200. Fast forward to 2021, that figure is nearly $23,000.1 From 2011-2016 alone, single premium coverage saw a 63% increase while wages increased only 16%.2 As if this is not bad enough, workers are getting silently squeezed by paying more for their premium and paying a higher out-of-pocket deductible. In 2000, workers paid on average 25% or $1,600 out of their paycheck for the $6,200 premium, but by 2021, the number is $6,000 of the $23,000, or approximately 27%.3 In 2006, deductibles for employer-based family coverage averaged $584. By 2021, that number is over three times the cost at $1,700.4 Over the last two decades, families are finding healthcare costs to be the largest portion of the household budget. Like boiling a frog that doesn’t notice the heat until it’s too late, each year over the last two decades, families have incrementally shouldered more of the cost of their overall premium taken from their weekly paycheck and faced higher deductibles that need to be paid before insurance kicks in. Unfortunately, these expenses have seriously outpaced wage growth and overall inflation which clocked in around 7-9% in the last year. The hidden tax of inflation and increasing healthcare “insurance” expense
12 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
is insidiously stressing individual and family budgets. This is unsustainable and the cracks are evident. As of 2021, 58% of all debt collections in the US are for medical bills.5 A total of 41% of US adults, 100 million people, bear medical debts. One of every 8 individuals owes more than $10,000.6 Meanwhile, the Federal Reserve reports that 36% of Americans don’t have enough money on hand to cover a $400 emergency, 51% of Americans have $5,000 or less in savings, while 35% have $1,000 or less, and the median savings amount is $4,500.7 With more taken from wages to cover premiums, higher deductibles and little savings to handle a medical emergency, and inflation reducing the purchasing power at the pump and the grocery store, the unfortunate fact is that a vast majority of Americans are “functionally uninsured,” choosing foregoing basic medical care in order to cover the basic needs of food and shelter.

The Hospital
Philadelphians, and particularly Chester Countians, witnessed within just the past two years what was once unthinkable. Hahnemann Hospital, Delaware County Memorial Hospital, Brandywine Hospital and Jennersville Hospital all closed their doors to patient care due to financial losses! In the wake of the pandemic, the remaining regional hospitals that serve our communities reported severe operating losses stressing the ability to provide care and threatening more closures to come! For you MASH fans, in the words of “Radar” O’Reilly, what “H-E-double toothpick” (“hell”) happened? Is it all the pandemic, or is more going on? Obtaining a clear picture of the hospital financial landscape is difficult due to the opaque nature of hospital costs and reimbursements from private payers. Also, consolidation trends with major academic centers and community hospitals make it difficult to understand how much hospital finances are underpinned by “direct patient care” versus diversified market investments, IP investments and large endowments outside of
direct patient care that cross-subsidize hospital or service line losses. Nevertheless, some clear trends are notable. Hospitals traditionally operate at very low overall margins of around 3-5%.8 Hospitals have managed small positive net margins with higher reimbursement from a predominantly higher proportion of private payers that offset slight losses from a lower proportion of Medicare patients and major losses from a small minority of Medicaid patients. Hospitals without diversification strategies or a favorable payer mix are in serious jeopardy. Approximately 80% of hospitals in America are community hospitals, often serving the poorest populations that are on Medicaid (or Medicaid eligible / uninsured). The math just simply doesn’t work for these hospitals, and this may represent most small community hospitals in the US. Given these facts, it is not surprising that we’ve seen a record number of hospital and service line closures in the last few years. Nearly 180 rural hospitals have closed since 2005, with a sharp uptick in 2019-2021. Many experts predict this trend will continue.8 Unfortunately there are additional down-stream affects. When hospitals that serve poor communities fail, those patients naturally move to the next closest hospital, thereby straining the finances of their neighboring hospital. A vicious cycle ensues as less beds are available for patients with richer reimbursement insurance plans than Medicare and especially, Medicaid.
Another trend is the entirely predictable growth of Medicare. Medicare, as originally designed, was a principled idea rooted in a duty to care for the elderly. Before Medicare, many of our elderly patients, in need of hospital care, suffered and died indigent without even basic medical care. But the scope of Medicare today is a far cry from the original intent of the legislation. Since its passage in 1964, benefits expanded well beyond its original mandate along with the rising costs of the expansion. Like many government programs, the original estimates of the costs were wildly underestimated. Almost from the start, there was fierce ideological political debates on how to address the problem,
continued on next page >
WINTER 2023 | CHESTER COUNTY Medicine 13 www. CHESTERCMS .org
Crisis of Healthcare Financing in America
continued from page 13
numerous attempts at legislative fixes and political compromises intended to reign in expenses rising much faster than general inflation. None have worked. Let that sink in…none. Especially damaging was the transition to the prospective fee schedule adopted in 1983 that ushered in the DRG and CPT coding methodology that I believe is at the root of so many problems in healthcare financing problems. This system is underpinned by a simple question Yale Business School Professors in the 1970s asked when consulted by a physician hospital leadership group seeking to control hospital costs. What is the “product” of hospital care? Out of this simple academic exercise, the DRG system was born, and legislation passed in 1983 that changed reimbursement to pay for the “product” or the “output.” At the time, this was viewed as a revolutionary advance in healthcare financing. Unfortunately, incentives matter and you tend to get what you incentivize. We incentivized “product” and more product is what we got. * Since then, the reimbursement game rewards documenting for dollars, upcoding and the perverse incentives that rewards more tests, more surgeries, more medicines, and more diagnoses that appear to make our patients “appear sicker” to garner more reimbursement. The more the “product” the costs more it gets reimbursed.
Fast-forward to 2011-2012; the oldest of the baby boomers retired and signed up for Medicare. Medicare enrollment in 2010 was approximately 48 million Americans, by 2020 approximately 60 million and by 2035 projected to be 87 million all with much more expanded coverage than the original intent.9 This exponential rise in Medicare patients is stressing hospital finances because Medicare, similar but to a less extent than Medicaid, does not cover the typical cost of care, and a larger percentage of patients are on Medicare. Current forecasts suggest The Medicare Trust Fund will be bankrupt by 2026 without meaningful reform.9
The pandemic continues to wreak havoc on our health care system. Yes, we have the vaccines and better treatment, the virus becomes less virulent as it becomes endemic, admissions and deaths are waning. The havoc now is best described by the phenomenon dubbed in the popular press as “quiet quitting.” Empirically, health care workers seemed to have walked off the job. I suspect many close to retirement decided to exit early. Others may have found better opportunities with less personal risk and stress in other industries with better wages and lifestyle. The bottom line is that hospitals have found themselves short-staffed. The only solution is to resort to “travelers” or “agency workers” to staff necessary services. Temporary workers can command 2-3x the normal wage. This has massively blown a hole in hospital budgets and is the major contributor to negative margins. Short term, this is a necessary expense to care for patients. Long term, this is creating wage inflation for dedicated full-time workers. In the current environment, wages must and naturally will increase
until an equilibrium exists between “travelers” and long-term employees. The new wage must be accounted for in the long-term financial solvency of the hospital system.
The Physician
Some sobering statistics highlight the current crisis of Physician job satisfaction. “Physician burnout” was an emerging issue prior to the pandemic, but it seems to have worsened in the post-pandemic era.11 In a 2022 Medical Economics survey, 94% of physicians have experienced burn-out at some point in their career, nearly ¾ report burn-out at the time of publication. The top reasons for burn-out were too much paperwork / regulations, poor work/life balance, adoption of the EMR and lack of professional autonomy. Although physician reimbursement has declined in both real and nominal terms over the last two decades, only 10% cite this as a reason for burnout. This stat is refreshing and reinforces our professional belief that most of us don’t do this “for the money,” even if broader society might feel otherwise! Almost 80% expressed a desire to quit medicine.11 A 2022 report by Medscape mirrored the top three reasons as administrative burden, over-worked, and loss of professional autonomy. The highest levels of burnout were matched only by Nurses and Policemen!10 Sadly, nearly 1 in 5 physicians have contemplated suicide during their career. An estimated 300-400 do so each year.
Hospitals, now the largest employers of physicians, are starting to recognize the depth of the problem and are doing their best to implement programs to address the problem. Interesting solutions include Physician Wellness programs, better access to mental health professionals, free yoga, mindfulness training and lounges with message chairs. These are laudable and appreciated, but in my opinion are akin to rearranging the chairs on the deck of the Titanic. Why is this happening now? Physicians have always been gluttons for hard work. We love the challenges and rewards of patient care without regard to personal sacrifice. We love the discovery of the science. It’s never been a job, it’s a vocation. Why now, in the last few decades, are many of our colleagues finding ourselves disillusioned and seeking an exit? Maybe root cause is the way we finance and reimburse for healthcare? Maybe it’s the business model? The EMR, mandated upon us in the last decade, is first and foremost a cash register for managing the labyrinthine bureaucracy of insurance reimbursement. The EMR has taken a simmering problem of physician discontent to a full-blown boil. Physicians, the majority of whom are now employees of the hospital corporation, are routinely expected to document encounters to maximize reimbursement. If they don’t, they are barraged by “coding inquiries” informing them of the
14 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
*A reasonable criticism of this system is that the “retrospective cost basis system” in place prior to 1983 was also financially unsustainable.
opportunity to maximize reimbursement with better documenting strategies. After finishing routine patient care, hours at the end of the day are spent on documentation, responding to coding queries, and peer to peer reviews with insurance companies. I don’t know of any physician that doesn’t bring home 2-3 hours of “charting” each week, some 2-3 hours per day! With declining reimbursement every year, the natural incentive is to do more, go faster, and document / code better. Physician contracts are mostly based on productivity or “RVUs.” Again, sell more product! Additionally, commercial insurance companies and Medicare Advantage programs require prior authorizations for almost every medical recommendation that seeks to limit care. The entire reimbursement scheme is giant moral hazard that is inflicting “moral injury” on physicians and will only get worse as we see continued cuts in reimbursement. This is not what we thought we were getting into when we embarked on this journey. Most of us were idealistic teenagers when we chose this path! The noble profession of medicine, for many of us, just doesn’t seem so noble anymore.
I submit to you that the root of the problem is the reimbursement system. Without meaningful reform of the fundamental method of financing healthcare, patients, physicians, and hospitals will continue to face serious challenges.
In an interview for the Wall Street Journal, Wisconsin Representative Mike Gallagher commented on the state of the US military, but also aptly describes the healthcare predicament as well: “The military (healthcare) crisis is a microcosm of the broader societal crisis.” The U.S. is “increasingly becoming a healthcare and retirement organization that has guns.” The next president will have to “sail the ship of state through the Scylla of a confrontation with China and the Charybdis of an entitlement crisis.”
If you are unfamiliar with the Scylla and the Charybdis, Wikipedia provides an interesting read, but it’s best summarized as stuck between a rock and a hard place.13 The current system is financially unsustainable. The business model is failing. Hard choices will be thrust upon us. The patient is bleeding and dying on the street. It’s time for bold decisions. This is a challenge we can solve.
References:
1. Kaiser Family Foundation Employer Health Benefits Survey. October 2022.
2. Kaiser / HRET Survey of Employer Sponsored Health Benefits, 2011-2016. Bureau of Labor Statistics, Consumer Price Index, US City Average Annual Inflation (2011-2016). Bureau of Labor Statistics, seasonally adjusted Data from the Current Employment Survey (2011-2016)
3. Kaiser / HRET Survey of Employer Sponsored health Benefits, 1999-2017; KFF Employer Health Benefits Survey 2018-2021
4. Kaiser / HRET Survey of Employer Sponsored health Benefits, 1999-2017; KFF Employer Health Benefits Survey 2018-2021
5. Levey NN. 100 Million people in America are saddled with health care debt. Kaiser Health News. June 16, 2022. https://khn.org/news/article/diagnosis-debt-investigation100-million-americans-hidden-medical-debt/

6. Berwick DM. Salve Lucrum: The Existential Threat of Greed in US Health Care. JAMA. Published online January 30, 2023. doi:10.1001/jama.2023.0846
7. Economic Well-Being of U.S. Households in 2020 - May 2021. Board of Governors of the Federal Reserve System.
8. The Current State of Hospital Finances: Fall 2022 Update: Kauffman Hall
9. Intermediate Projections from 2005-2019 Annual Reports of the Board of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds.
10. Medical Economics: 2022 Physician Burnout Survey results
11. Medscape: Physician Burnout & Depression Report 2022: Stress, Anxiety, and Anger
12. America’s Military Faces a ‘Window of Maximum Danger’; Marine turned lawmaker Mike Gallagher warns that the U.S. is far more vulnerable to losing a war than the public recognizes. Wall Street Journal, Kate Bachelder Odell, Oct. 7, 2022
13. https://en.wikipedia.org/wiki/Between_Scylla_and_Charybdis
Sean V. Ryan, MD, MBA, is a practicing vascular surgeon providing care to patients at Bryn Mawr, Paoli, and Chester County Hospitals in the suburbs of Philadelphia, PA. He would welcome your input and opinion at sryan@ vascularss.com.
WINTER 2023 | CHESTER COUNTY Medicine 15 www. CHESTERCMS .org
Nancy Fuhrman
BY BRUCE A. COLLEY, DO
Iwas fortunate to spend some time with Nancy Fuhrman, our featured artist for the winter issue, at her home and studio recently. Although I knew Nancy was an artist, I never appreciated her breadth of art interest and her level of accomplishment. She was, when we first met about 20 years ago, the principal of my children’s elementary school. With her retirement from education some years ago she has been able to concentrate on her art full-time and thus I have been made aware of her emerging presence in the Chester County art community.
Nancy was born and raised on a Lancaster County farm. She earned her Bachelor’s and Master’s Degrees in Art Education. After teaching for many years Nancy received her PhD. in Education, eventually finding her way to Downingtown to be the Principal at East Ward Elementary School. As noted in her Artist Statement, her predilection for art was kindled by her elementary school art teacher who was, I suspect, also a model for Nancy’s career as an educator. “She freed my boundaries and affirmed my creative spirit.” A mistake, I believe, that is common to parents and in school settings is when we try to make our children into something, rather than shepherding them to make something of themselves. Buckminster Fuller, the 20th century polymath, famously wrote, “All children are born geniuses, then are quickly de-geniused. I was simply lucky to have escaped the typical indoctrination.” N.C. Wyeth and his wife Carolyn are widely known to have provided a learning environment that was akin to Mrs. Kauffman’s approach, to their clan. We see their results: three artists, a renowned musician and a scientist.
Nancy has also studied at, to name but a few, the Southwest School of the Arts, The Pennsylvania Academy of Fine Arts, West Chester University, Wayne Art Center, and the John Campbell Folk School. She is an accomplished artist in a variety of media including painting with watercolor, acrylic, and oil; clay, etching and fiber art. Nancy’s art has been featured in galleries and shows throughout the East Coast. Please take time to enjoy the small sampling of her art in this issue. Thank you, Nancy, what talent, what joy you share. The lucky children of Chester County to whom you were teacher, principal and advocate and who are so precious to you, they thank you! Forever.

www. CHESTERCMS .org 16 CHESTER COUNTY Medicine | WINTER 2023
Snow Scene Fiber Art





www. CHESTERCMS .org WINTER 2023 | CHESTER COUNTY Medicine 17 continued on next page >
My Hat
Art
Forgot
Frozen Lake Fiber
341 E Lanc Ave
Graystone Manor 1920
Terracina 1920
The Art of Chester County continued from page 17

Copper Beech

18 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
Rest Period
ARTIST STATEMENT
Nancy Furhman
I was fortunate to have a wonderful art teacher in elementary school. Mrs. Kauffman always supported my ideas and took away boundaries that tend to confine a creatives spirit. I remember making kites in 2nd grade out of a reed, tissue paper and string and glue. My classmates made diamond or round shapes … maybe a heart…but I wanted to make a bunny. As I shaped the body, head and ears, Mrs. Kauffman immediately knew what I was doing and said, “Oh you need more reed for the legs and tail!” as she proceeded to gather more. She never said no, can’t or shouldn’t. And thus, I have been creating whatever is on my mind, in whatever medium I choose. All my life I know she is the reason I became an elementary school art teacher. How lucky for me.
Most recently I have been working with fiber arts (wool most notably), needle felting with some wet felting. Felting allows me to combine my love of drawing and painting as I, “paint with wool.” My subject matter can be landscapes, florals, animals, and all things nature and living things. Images are selected that give a sense of calm and serenity – as a tall stoic tree that has existed a hundred years. Animals grazing in an open field, a sleeping kitten, a landscape that captures wonder. I want others to feel a sense of peacefulness, lightness, creating and capturing intimations that all is right with the world.


www. CHESTERCMS .org WINTER 2023 | CHESTER COUNTY Medicine 19
Tuscan Sunset Fiber Art
Fiber Art
MAKE HEALTH THE END GOAL OF CHRONIC PAIN MANAGEMENT
www. CHESTERCMS .org 20 CHESTER COUNTY Medicine | WINTER 2023
BY DR. ASARE B. CHRISTIAN, MD, MPH

Chronic pain affects a significant number of Americans and costs healthcare more than diabetes, heart disease and cancer combined. We have come to understand the many mechanisms underlying chronic pain development and factors keeping people in pain, Yet many continue to suffer in pain with huge implications on health, quality of life, healthspan, and economic strain on society. This is not because we don’t have effective treatment. This is because the goal of treatment of this complicated and complex issue is narrowly focused on solving the pain signal, instead of restoring health to the psychological and physiological derangement that has taken place with chronic pain. The lack of comprehensive treatment integration in the right order for the right patient, combined with an accountable support system that emphasizes pain education, nutrition, exercise, sleep, stress management, self-efficacy management, and habit changing strategies, keep many in the chains of chronic pain.
Our understanding of the cellular, biochemical, neuroanatomy, neurochemistry, functional, structural, and neuroaffective aspects of pain has improved. This understanding has led to a new classification of chronic pain as a complete disease entity

of the brain. This knowledge has not changed outcomes for patients with chronic pain, who continue to suffer. Treatment often comes with many unwanted and serious side effects and fails to improve function and quality of life. National and international bodies concerned with the study of pain have proposed and recommended effective ways of managing pain, with emphasis on biopsychosocial treatment for those with chronic pain and validating the biomedical model for acute pain. Despite these well-meaning recommendations, there is a persistent gap in outcomes for the patient suffering in pain and the clinicians who treat pain. I believe this gap fails because we fail to set realistic end goals for pain management. The end goal of pain management should focus on getting patients healthy, not just solving pain signals.
Focusing on health starts with better assessment of pain and the health of the person with pain. This has to be done, especially with musculoskeletal issues through the lens of connective tissues & structures (orthopedics), functional limitation (physical rehab medicine), inflammatory (cellular medicine and rheumatology), and neuroaffective (pain neuroscience and psychology). Through these lenses, proposed by Dr. Helen Langevin, we are able to see
continued on next page >
WINTER 2023 | CHESTER COUNTY Medicine 21 www. CHESTERCMS .org
Make Health The End Goal Of Chronic Pain Management
continued from page 21
the broader picture of pain impact on the individual patient and prescribe the right integrative treatment (see figure 1). If we fail to address the neuroaffective aspect of chronic pain, for example, surgical outcomes are poor. It is also important to understand the secondary and tertiary complications that have developed due to chronicity of pain. Most patients develop compensatory mechanisms and impaired biomechanics that need to be addressed with appropriate therapy and strengthening programs with the goal to improve function. We also have to address neuroplastic or brain generated pain that has developed independent of tissue damage. This is done through Pain reprocessing therapy, Cognitive Behavioral Therapy, Acceptance Committed Therapy, and other neuro-framework techniques. These approaches improve psychological health which in turn improves biological health; an Integrative approach to musculoskeletal pain, bridging across neuroscience, physical therapy and rehabilitation, orthopedics, and rheumatology “silos.” Langevin, H. M. (2021). Reconnecting the brain with the rest of the body in musculoskeletal pain research. The journal of pain, 22(1), 1-8.

There are two important questions I ask each patient who comes to my clinic with complaints of chronic pain. First I ask, “What is your understanding of why you have pain?” And the second question is, “What does your pain prevent you from doing?”
The answers to these questions provide the opportunity to assess patient understanding of their pain and the functional imitations their pain has placed on their life. In my experience, most patients with chronic pain are not so concerned with pain sensation but the “painfulness” of the pain experience. They are most frustrated by the limitation that pain has placed on their life. They are angry, frustrated, anxious, and afraid. When I ask patients to tell me about their pain, they start talking about the fact they can’t go for a walk, they can’t hang out with their grandchildren, they can’t go to dinner with friends, they can’t go to the granddaughter’s wedding, all because of the pain. They can’t sleep in the same bed with their spouse, they are isolated from friends, and despite their best effort nothing gets better, or nothing works for them. They will often tell me, they have done
22 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
Figure 1
physical therapy, chiropractic care, acupuncture, tried multiple pain medications including opioids, multiple epidural injections, joint injections, and sometimes surgery and still continue to have pain. The biggest revelation in the patient narrative and history is that they don’t understand what pain is. Their understanding of pain is often wrong or limited. This also unfortunately, is the case in many clinicians the patient encounters. This I see as one of the biggest obstacles to treatment. How do you manage something you don’t understand?
Pain, according to the International Association for the Study of Pain, is defined as a sensory and emotional experience associated with or may not be associated with tissue damage. We have had this definition since 1978 and the recent revision in 2020 maintains the same definition with 6 different qualifiers. These qualifiers were added based on our current understanding of pain in the last 40 yrs. Yet, how physicians and patients define pain are not in alignment of what pain is. First, treatment focuses only on the “Sensory” component of pain with limited attention to the “emotional component” of pain. We also tend to focus on treating “potential tissue damage” as real tissue damage, and don’t take into account the neuroplastic changes that have taken place and the resultant amplification of pain signals and more importantly brain generated pain signals.
It is important therefore to start with education before medications. It is important for patients to understand that their imaging findings alone don’t explain their pain. When I ask patients why they think they have pain, especially those with chronic pain will tell me “It is my L4/L5 herniation, their bone on bone knee, their car accident that happened 10 years ago, or the complications they got from a procedure or injections.” This does not invalidate patients’ narrative or complaints, but it is important for patients to understand that perhaps what started their pain is not the same process keeping them in pain. But what has “kept” them in pain may be something completely different. I break this education into Predisposing factors, Precipitating factors, and Perpetuating factors. There are certain predisposing factors to chronic pain including a small percentage relating to genetics, and many times psychological stressor (history of trauma, anxiety, depression, type A personality, unforgiveness, and metabolic disease). The precipitating factor is what patients remember most often. They are able to pinpoint the onset of the pain following a car accident, or a fall due to emotional crystallization.
It is important to explain to patients that what started their pain may not be what is keeping them in pain after 5-10 years. Disc herniations and most musculoskeletal injuries heal within 12 weeks, so why are they having pain after 5 years? We are still having pain because we have not focused on the health of the cells that generate, transmit, and interpret pain signals. We have not focused on healthy habits that allow the body to heal. How
do we get the cells to become healthy whether it’s chondrocytes in the knee, microglia or astrocytes cells of the nervous system, or lymphocytes, neutrophils, macrophages, monocytes of the immune system? It becomes a function of addressing cellular efficiency and restoring homeostasis. This is not achieved with sodium channel blockade, epidural injections, anti-inflammatory meds, or opioid therapy. It becomes focusing on stress management, nutrition, exercise, and sleep. These interventions are well documented and validated in the literature, and consistently restore health to cells, tissues, organs, and organ systems. All these healthy approaches limit pro-inflammatory states and provide homeostasis. The evidence for these four pillars is overwhelming. Pain doesn’t get better when individuals are not getting restorative sleep, pain doesn’t get better if we continue to consume foods that perpetuate inflammation.
When this is paired with pain education, self-efficacy management, appropriate pain medications and interventions, pain improves and becomes manageable. The integration of complementary options and any other interventions should also focus on getting patients healthy. When patients are healthy, their outcomes from pharmacological interventions, surgical interventions, non-pharmacological interventions, and complimentary options are better.
Focusing on health as the end goal of pain management is an approach that rearranges the paradigm of chronic pain management to focus primarily on getting patients healthy. Of course, getting people healthy may seem like a daunting task but I will argue that it’s safer, cheaper, effective, and rewarding for both patients and physicians. It requires a new perspective from physician and patient. This starts with assessing patients’ psychology, physiology, and functional limitations relating to their pain.
The approach to getting patients out of pain should start with getting patients healthy. It is important for clinicians who are dealing with patients in chronic pain to focus on education before medications, self-efficacy management, optimizing sleep, nutrition, exercise and stress management. It is also important that our patients understand the importance of health focus as the way to get them out of chronic pain. When these are integrated not only do patients get pain relief, but get improvements in metabolic, cardiovascular, neurological, musculoskeletal and immune health.
Dr. Christian is founder of Aether Medicine, an Integrative & Regenerative Pain Management, and Rehabilitation Medicine Clinic in Wayne, PA. To learn more about Dr. Christian visit www.aethermedicine.com or call 484-806-1101.
www. CHESTERCMS .org WINTER 2023 | CHESTER COUNTY Medicine 23


24 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
Southeast PA Area Health Education Center Offering Community Health Worker Trainings
Community Health Workers (CHWs) are frontline public health workers who assist in improving quality of care and breaking down barriers to treatment. CHWs bridge cultural, linguistic, knowledge and literacy differences among individuals, families, communities, and providers. As members of the community they serve, they help build trust and open lines of communication.
A CHW may go by many titles, such as: Community Health Representative, Community Health Advisor, Health Coach, Family Advocate, Health Educator, Liaison, Outreach Worker, Patient Navigator, Public Health Aide, Patient Care Coordinator, or Promotor(a) de Salud. Likewise, CHWs work in a wide variety of settings that may include hospital systems, non-profit and faith-based organizations, public and private clinics, educational systems, learning extension centers, or public agencies. CHWs may even provide services to patients through home visits.
CHWs are trusted members of their communities with a passion for helping others prevent or manage disease or other physical or behavioral health issues. Studies have shown that CHWs have a positive impact on patient health by decreasing missed appointments, increasing medication regimen adherence, improving access to primary care and preventative services, and helping individuals manage chronic conditions.”
While some CHWs may have minimal formal training in medicine or health, they tend to have an intimate knowledge of their communities and local resources.
CHWs provide a wide variety of services, such as health promotion, interpretation or translation services, health system navigation, advocacy on behalf of patients and their families, outreach before appointments, including appointment reminders, outreach to ensure adherence to treatments and medications, home visits, arranging transportation, making connections to community resources or social services, and providing care coordination and case management.
The Southeast Pennsylvania Area Health Education Center (SE PA AHEC), along with the other Pennsylvania Area Health Education Center (AHEC) regions, offers a 100-hour training program designed to provide the core competencies set by the Pennsylvania Certification Board needed for work in communitybased and inpatient settings. Core modules in this training program include, among others:
• Boundaries
• Building and Maintaining Relationships
• Communication, Networking & Conflict
• Documentation
• Chronic Disease
• Motivational Interviewing
• Accident Prevention
• Personal Safety
• Preventive Care
• Health Literacy
• HIPPA Privacy Rule
The curriculum utilizes various learning styles which include lecture, discussion, hands-on activities, guest speakers, specialized training, and student presentations. SE PA AHEC customizes each class according to the interests and roles of the trainees in each cohort by inviting guest speakers to present. Speakers from partner organizations have provided specified valuable trainings on topics such as interpersonal violence, Lupus, overdose awareness and reversal, and oral health, among others.
Grant funding and stipend support is available for select trainees. To learn more about the Southeast PA Area Health Education Center and their Community Health Worker Training Program, contact Christine Polit, Executive Director, at cpolit@sepaahec.org.
WINTER 2023 | CHESTER COUNTY Medicine 25 www. CHESTERCMS .org
Wait a S.E.C.: Sympathy, Empathy and Compassion
BY KATHLEEN E. WALLS, PSY.D., MS KRISTIN


Sympathy, empathy and compassion are the hallmarks of a solid patient-provider rapport. Although the need for sympathy, empathy and compassion is not race specific, its importance was highlighted during vaccine hesitancy work stemming from the COVID-19 pandemic. While conducting numerous COVID-19 focus groups, panel discussions, podcasts, and vaccine clinics, there were countless individuals, who identified themselves as part of the Black community, who stated they were hesitant to take the vaccine. Individuals reported that they did not trust the medical system. This stemmed from the history of systemic racism and inappropriate and unethical practices in their lives and the lives of their ancestors, disparate treatment within the healthcare system, and a lack of healthy, quality, and personal relationships with their Healthcare Providers.
The broken rapport between individuals and their Healthcare Providers became increasingly evident as individuals shared that they did not feel heard by their provider and that communication was experienced as “one-way” – from the Healthcare Provider to the patient. For instance, when some patients attempted to express their concerns and/or inquire about the vaccine, they received responses such as “I received my vaccine, and I didn’t grow an extra arm. You should get the vaccine too”; “Your kids received all their other vaccines. What’s the difference?”; and “The vaccines have gone through the clinical trial process. No safety issues have been found.” Unbeknownst to the Healthcare Providers,

these responses increased the divide within the patient-provider relationship, and left the patients feeling unheard. Consequently, many individuals left these encounters with unanswered questions and an uncertainty on who to trust, listen to, and how to proceed during a time of fear, anxiousness, and what was posed as a “life or death” decision for themselves and their loved ones.
In 2020, the COVID-19 pandemic, uncertainty about an impending vaccine, accompanying social and racial injustice and unrest and conflicting public health messages from the White House, increased the need for provider compassionate care during this unprecedented time. Patients needed providers who were emotionally intelligent and able to express sympathy, empathy and compassion. On the Pathway to Compassion Model (see Figure 1), by Dr. Kathleen E. Walls, sympathy is identified as the first

26 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
MOTLEY, PHARMD, MBA
step in the process. Sympathy focuses on the internal feelings that a person experiences in relation to someone else’s stimulating/ activating event. Once the personal feelings are experienced and identified, then the individual can empathetically connect to and with the feelings of another person. This empathetic connection has been found to be supportive and cathartic by itself. However, when the resulting empathetic connection motivates one to take action, compassion is the resulting outcome. It is this shift from sympathy to empathy to compassion that patients are desiring.
During one of the focus groups, a patient shared that they told their Healthcare Provider “I’m not getting vaccinated because I don’t know if it is safe.” The Healthcare Provider responded with “The vaccines have gone through the clinical trial process. No safety issues have been found.” This real scenario left the patient feeling unheard, uncared for, and not connected to the Healthcare Provider. This was a great opportunity for the Healthcare Provider to connect with the patient. The Healthcare Provider could have utilized the Pathway to Compassion Model to build and strengthen the patient-provider relationship in that moment. See possible Healthcare Provider responses below.
Healthcare Provider Responses
Sympathetic Response: I’m sorry that you feel this way. I feel bad and concerned about your safety. However, the vaccines have been proven to be safe.
Empathetic Response: It sounds like you’re hesitant. Am I hearing that correctly? I know there have been times when my doctor offered me medical advice, and I wasn’t sure what to do.
Compassionate Response: It sounds like you’re hesitant. Am I hearing that correctly? I know there have been times when my doctor offered me medical advice, and I wasn’t sure what to do. What helped me make a decision was getting a 2nd opinion as well as doing some additional research. What safety questions do you have? Also what resources can I provide that would be helpful for you to make an informed decision?
When Healthcare Providers offer compassionate care, they are actively listening, building a relationship with the patient, answering patient questions, participating in the solution finding, and invested in the patient’s overall well-being. Compassionate care stems from the first principle of the American Medical Association, which states, “A physician shall be dedicated to providing competent medical care, with compassion and respect for human dignity and rights.” In alignment with this principle, the Shane, S. et al 2016 article, Compassion in Health Care: An Empirical Model, recommended that “all health professionals be trained in compassion, that compassion be considered and evaluated as a core competency of health care providers, and that system wide
standards of compassionate care be adopted and implemented.” It has been found that the utilization and demonstration of sympathy, empathy, and compassion are essential for rapport building and patient retention.

Interestingly, although this first guiding principle lays the foundation for the importance of compassion, some providers have been taught and/or told not to care too much so that they could avoid burnout. However, contrary to this deliberate teaching, the research has shown the power and importance of compassion in healthcare. For instance, Baurers, S. (2022) noted that “Compassion can be a powerful beneficial therapy for the giver, too. Among health-care workers, more compassion was associated with more resilience and resistance to burnout” (The Philadelphia Inquirer, August 10, 2022). Dr. Stephen Trzeciak reported that “Scientific evidence shows that serving others, even showing simple kindness, is the best medicine for yourself. It is associated with tons of benefits for physical health, mental health, emotional health, and happiness, fulfillment, and well-being, as well as professional success” (Baurers, S. The Philadelphia Inquirer, August 10, 2022). This research has contradicted the earlier beliefs that engaging in less compassionate care would lead to less burnout. Instead, compassionate care has actually been found to create a win-win for both the providers and the patients.
Compassion was also found to be linked to other favorable personal qualities and characteristics. For instance, according to Shane, S. et al (2016) “Patients felt compassion stemmed from virtues of genuineness, love, honesty, openness, care, authenticity, understanding, tolerance, kindness, and acceptance (Journal of
www. CHESTERCMS .org
Pursuit of Partisan Political Power
 BY LARRY L. LIGHT RETIRED PAMED LOBBYIST
BY LARRY L. LIGHT RETIRED PAMED LOBBYIST

It’s easy to recap the 2022 general election in Pennsylvania. For the interested voter and the keen political observer alike, it simply exceeded all expectations! Keystone state voters elected two Democrats, sweeping the statewide races at the top of our ballots. John Fetterman defeated physician Mehmet Oz to help save the Democratic majority in the US Senate and Democrat Josh Shapiro won handily over mismatched Doug Mastriano to mark the first time in over 60 years that the office of Governor has been held by one party for 3 consecutive terms. Notably, Shapiro’s running mate, Representative Austin Davis, will become the first African American Lt. Governor. Those are significant achievements in a state considered to be “purple” and a swing state in national elections.
At the state level the State Senate elections were pro forma, incumbents won re-election and the Republicans retained their comfortable 28 – 21 majority (with one vacancy). In the 203-member Pennsylvania House of Representatives it was a different matter altogether. The solid GOP majority in the House before the election was transformed into a potentially razor thin Democratic win, a mostly unexpected outcome. And, for the first time in 56 years, a physician was elected to the Pennsylvania General Assembly.
So why does winning the majority matter so much? In each legislative chamber the salary and benefits for the majority and minority members are the same. Your party wins the majority, you get the same salary as your legislative colleagues in the minority. There is an equitable distribution of office space in the capitol building and the resources for staff and other administrative needs are adjusted to recognize shifts in power.
From one intriguing perspective it might even seem that being in the minority is “easier.” Legislators in the minority can concentrate on constituent services and embrace the numerous opportunities to simply vote against policy proposals advanced by the majority. In brief, they don’t have the responsibility to govern.
The functional advantage, and the primary underlying reasons to work so aggressively in the election cycle to win the majority, are control of the legislative chamber’s agenda and control of the committee structure. Committee chairs are named by
the leadership of the majority party and the committee chairs traditionally have absolute control of the flow of legislative bills from their committee to the floor. And once bills are approved at the committee level the same leadership takes over to manage which bills will be considered by the full chamber or perhaps sent to another committee or tabled for further “study.” When any of those procedural actions are challenged, it is almost guaranteed that the majority leadership will have the full support of their party members and win the vote.
A well-worn political saying notes that the “majority will have their way, while the minority will have their say.” In this era of highly charged political discourse, party line votes have become commonplace. While the minority will have procedural avenues to challenge the components and process of the majority’s agenda, they will likely not be successful in prying disgruntled members of the other party from being locked in loyalists. You win the majority so you can win when you play political hardball.
Two rarely acknowledged benefits of being in the majority are certainly real, but rarely acknowledged. A key element of every political campaign is fund raising. It’s much easier to raise the campaign contributions needed to fuel an incumbent’s reelection drive from a position in the majority. Another aspect is the unending strategy to get members of the opposing party to make a “bad” vote. The thinking being that the strategic vote will displease constituents and have a negative effect on a future election.
After the 2022 election cycle all of these factors contributed to an unprecedented level of partisanship, high levels of campaign spending and a chaotic environment in the legislative chambers at both the state and federal levels.
The PA House results were unusually surprising. The total of 48 new representatives is an uncommonly high number and that turnover foreshadowed the political upheaval that followed. Unexpectedly the House GOP lost enough seats to lose control over the lower chamber. Democrats predicted that they would capture the House majority early on election night. Then reality set in as it became clear that a winning Congressional candidate, Democrat Summer Lee, would have to resign her state House
28 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
Politics & Medicine
seat, as would the winning Democratic Lt. Governor candidate, Austin Davis. Also vacant was the seat of longtime Democratic Representative Tony DeLuca whose name legally remained on the ballot after he passed away just weeks before election day. Special elections were held to fill all three House seats, and all are in Allegheny County. Democratic candidates won all three of the special elections, giving them a 102-101 majority in the House. The majority “head count” will likely get even more complex if sitting House member Republican Lynda Schlegel Culver wins the special election for a vacant State Senate seat. Her replacement would likely also be a Republican, but the GOP caucus would only have 100 members until the House special election is held.
In the US Senate where elections are contested at the statewide level and more easily predicted, it became clear early that the Fetterman win in Pennsylvania would mean that Democrats would at least have a 50-50 split like they did the previous two years. The subsequent win by Democrat Ralph Warnock in the Georgia runoff election provided one more seat to their “working” majority.
Against the background of the epic 15 roll calls needed to elect the Speaker of the US House, the Republican party struggled to come together even while enjoying a 222-212 edge. Meanwhile the PA House endured its own controversy as Republicans with 101 members sought to hold off the takeover by Democrats who elected 102 members, but only had 99 sitting members sworn in on January 3rd. Controlling the dates of the special elections to fill the three vacancies and the public policy agenda that could be acted on in both the short and long term became the power struggle at the center of attention.
Elections are generally about two factors, the candidate with a focus on their qualifications to hold office and the policy agenda promoted by those candidates and their respective political parties. Post-election the primary concern is always controlling the partisan agenda. Consequently, political power struggles can get real ugly really fast. In the legislative arena the principal struggle for power is obviously winning enough races on election day to emerge as the majority party on swearing-in day.
In the US Senate the priorities will include confirming the more progressive judicial appointments being made by the Biden administration, back stopping (opposing) the partisan initiatives expected from the GOP controlled House and working closely with the Biden administration on addressing pending budget and debt ceiling issues. With so much at stake, the political power of the majority was the driving force in Senate elections across the county. In the House the debacle of partisan divide in the election of the GOP Speaker highlighted issues such as government funding, repeal of tax changes and even a constitutional change to term limits for Congressman and Senators.
At the state level there are clear differences between the parties’ agendas. Since the GOP holds a clear majority in the State Senate the priority policy agenda will be passed early and moved to the House, where the GOP majority may or may not exist. But regardless, the Senate will have done their work.

In this instance, three of the priorities are constitutional amendments that face a brief window to be passed and then advertised in newspapers across the Commonwealth before they can appear on the May 2023 primary ballot. They include a two-year statutory window for survivors of childhood sexual abuse, a reform of voter identification requirements and expanded legislative oversight of state regulations. Republicans will also push for mandatory post-election audits. The proposal to aid childhood sexual abuse survivors has bi-partisan support. While the others are unlikely to have support from Democrats in either the House or the Senate. For their part, Democrats will focus on protecting reproductive rights and curbing gun violence among other initiatives on education and property tax reform.
In each legislative chamber the current two-year session should be volatile and interesting.
For two terms, Republican John Cavender, MD, was elected to the Pennsylvania House of Representatives from Susquehanna County. His last year in office was 1966. Now, 56 years later, Arvind Venkat, MD, of Allegheny County has become the next physician elected to the PA General Assembly. Representative Venkat was elected to serve the 30th District in Allegheny County. He is an emergency physician.
New Chester County State Legislators
Replacing Dianne Herrin (D): Representative Chris Pielli (D)
Replacing Tim Hennessey (R): Representative Paul F. Friel, Jr. (D)
Replacing Craig Williams (R): Representative Catherine E. Spahr (D)
Key appointments by Gov Josh Shapiro: Valeri Arkoosh, MD, Secretary of Human Services
Debra L. Bogen, MD, Secretary of Health
(neither position was staffed by a physician in previous administration)
WINTER 2023 | CHESTER COUNTY Medicine 29 www. CHESTERCMS .org
Larry Light is a retired PA Medical Society lobbyist and senior staff executive.
PAMPAC PROVIDES A UNIFIED VOICE TO HELP ADVOCATE FOR MEDICINE, PHYSICIANS & PATIENTS


Established in 1964, the Pennsylvania Medical Political Action Committee (PAMPAC) is the political branch of the Pennsylvania Medical Society, and one of the largest bipartisan political action committees in the state.
It is comprised of PAMED members who are interested in making a positive contribution to the medical profession during the political process. Through the use of member contributions, PAMPAC supports the election and retention of pro-medicine candidates, as well as campaigning against incumbent legislators who consistently vote against the interests of patients and physicians.
“The primary focus of PAMPAC is raising money to help candidates get in office and stay in office,” says former Chair Tim Welby, MD. “We look to support folks who are interested in medicine, who are invested in the things that are important to physician practice in Pennsylvania, the things that are important to our patients. The things that make health care better in our state.”
PAMPAC also provides interested members with advice and information on organizing local fundraising events for legislative candidates, along with advising members who are interested in potentially seeking public office themselves.
“In addition to raising and distributing money, we also work with physicians to try and get them more involved in the political process,” continues Dr. Welby. “We advise them on how to approach local legislators, how to get meetings to sit down and discuss medical issues with them, and help educate the legislators on medical issues, on the things that are important to us and our patients.”
When Marilyn Heine, MD, began her tenure as Chair of PAMPAC in 2007, she saw an opportunity to develop a stronger PAC boosted with broader and deeper involvement by PAMED members. Through strategic planning, Dr. Heine helped develop a rebrand of the group that included cohesive mission and vision statements, annual assessments, a new logo, an online newsletter, and a tagline of, “the physicians’ voice in politics.”
In addition, Dr. Heine led efforts to inform county medical societies about the benefits of joining both PAMED and PAMPAC, utilizing peer-to-peer recruitment, and publicly recognizing groups when they achieved high levels of participation. “These initiatives were fruitful,” shares Dr. Heine. “PAMPAC saw a significant increase in our hard dollar revenues critical to our operations, as these are the only funds we can turn into direct contributions to candidates. PAMPAC actively engaged in judicial, legislative, and attorney general races and achieved a high success rate electing prophysician candidates.”
Unlike legislators, physicians understand what is best for their patients, which means they are also in the unique position of having the knowledge to advise on political issues that affect the medical community. PAMPAC provides a voice for these physicians, presenting a united front when it comes to the bills and legislation that will protect patients.
“You want the best possible care for Pennsylvanians and the way you do that is by electing the best people who understand all the issues well and can make good decisions,” says Dr. Welby. “As a PAC that’s our mission: put people in office who are going to help and educate folks so that they do the right thing for Pennsylvania patients. PAMPAC provides the opportunity to have some influence on that. Asking our members to consider supporting certain candidates, and then seeing them get elected… It’s one of those things where you feel like you’re actually making a difference in people’s lives.”
30 CHESTER COUNTY Medicine | WINTER 2023 www. CHESTERCMS .org
Physicians’ Voice in Politics
The
Through PAMPAC, members can have a highly visible impact on the election process and help shape the future of reforms such as medical liability, patients’ rights legislation, and insurance contract reform. Former PAMED President Lawrence John, MD, points to the recent signing of Senate Bill 225, which reforms the prior authorization process to expedite approval of patient care and reduce administrative burdens for hospitals, physicians, and other health care providers.
“PAMPAC is instrumental in allowing our voice to be heard in the legislature,” says Dr. John. “You have to be heard as a unit to get things done, and PAMPAC helps us get our word out to the legislature. We support them in their campaigns, we have dialogues with them as to what we think might help our patients and help medicine, we initiate conversations with them to try and get bills initiated and passed. Senate Bill 225 will allow things to be expedited much faster, which will benefit patient diagnosis and treatment. It’s a win-win when the legislators can understand the importance of something like that.”
And while PAMPAC continues to realize its goals, challenges in recent years including an increase in employed physicians, a decrease in society memberships, and many contentious races, means that the group sometimes struggles with engaging physicians in the political arena. “Lawmakers, appellate judges, and other elected officials increasingly impact the practice of medicine,” says Dr. Heine. “Many physicians are not aware that it is imperative to be involved in the political process. They may not recognize that a strong PAMPAC is instrumental to enhance PAMED’s advocacy efforts. Physicians must have a seat at the table to influence the legislative process. PAMPAC helps ensure our access.”


PAMED members, along with their families, are encouraged to join PAMPAC, and medical society staff are also eligible. There are several membership levels available, and lower rates are offered for medical students and residents. Becoming part of the group means your dollars help support the legislative lobbying that seeks to elect candidates who understand the needs of medicine and patients.
Dr. Heine concludes, “PAMPAC helps elect pro-physician candidates for the General Assembly and other positions within the Commonwealth. These elected officials impact the practice of medicine. PAMPAC is the “political muscle,” key to PAMED’s accomplishments in the advocacy arena. PAMPAC must be financially strong to be impactful and effectively serve as the ‘the physicians’ voice in politics.’”
Pennsylvania Medical Society 400 Winding Creek Blvd. Mechanicsburg, PA 17050



Reach Your Audience... Reach 35,000+ Engaged Consumers Plus, 3,500+ Physicians, Dentists & Practice Managers Throughout Chester County www.Hoffpubs.com Advertise in YOUR COMMUNITY RESOURCE FOR WHAT’S HAPPENING IN HEALTH CARE CHESTER COUNTY FALL2021 Published by Pennsylvania’s First Medical Society PAGE PAGE YouthPhilanthropy SowGoodNow Developments in Physician Peer Review The Art of Chester County PresentsLELE Galer Reach out to us today! Tracy Hoffmann 610-685-0914 x201 www. CHESTERCMS .org WINTER 2023 | CHESTER COUNTY Medicine 31







PROUD SPONSOR OF BOSCOV’S BERKS JAZZ FEST MARCH 24APRIL 2, 2023 Reading, PA Tickets on sale NOW at www.berksjazzfest.com 32ND ANNUAL THE MANHATTAN TRANSFER 50TH ANNIVERSARY & FINAL WORLD TOUR with special guest THE DIVA JAZZ ORCHESTRA CHRIS BOTTI RNR: RICK BRAUN & RICHARD ELLIOT with special guest PETER WHITE BRIAN CULBERTSON CELEBRATING WOMEN IN JAZZ II featuring REGINA BELLE, AVERY SUNSHINE, MAYSA, LORI WILLIAMS and more STANLEY CLARKE GERALD ALBRIGHT LARRY CARLTON & PAUL BROWN ACOUSTIC ALCHEMY with special guest JEFF KASHIWA VICTOR WOOTEN & THE WOOTEN BROTHERS WEST COAST GROOVE featuring ADAM HAWLEY, MARCUS ANDERSON, REBECCA JADE and more PRESENTED BY













 BY MARY T. BOYLSTON, ED.D.
BY MARY T. BOYLSTON, ED.D.




 SEAN V. RYAN, MD, MBA
SEAN V. RYAN, MD, MBA





















 BY LARRY L. LIGHT RETIRED PAMED LOBBYIST
BY LARRY L. LIGHT RETIRED PAMED LOBBYIST