
6 minute read
MAKE HEALTH THE END GOAL OF CHRONIC PAIN MANAGEMENT
BY DR. ASARE B. CHRISTIAN, MD, MPH
Chronic pain affects a significant number of Americans and costs healthcare more than diabetes, heart disease and cancer combined. We have come to understand the many mechanisms underlying chronic pain development and factors keeping people in pain, Yet many continue to suffer in pain with huge implications on health, quality of life, healthspan, and economic strain on society. This is not because we don’t have effective treatment. This is because the goal of treatment of this complicated and complex issue is narrowly focused on solving the pain signal, instead of restoring health to the psychological and physiological derangement that has taken place with chronic pain. The lack of comprehensive treatment integration in the right order for the right patient, combined with an accountable support system that emphasizes pain education, nutrition, exercise, sleep, stress management, self-efficacy management, and habit changing strategies, keep many in the chains of chronic pain.
Our understanding of the cellular, biochemical, neuroanatomy, neurochemistry, functional, structural, and neuroaffective aspects of pain has improved. This understanding has led to a new classification of chronic pain as a complete disease entity of the brain. This knowledge has not changed outcomes for patients with chronic pain, who continue to suffer. Treatment often comes with many unwanted and serious side effects and fails to improve function and quality of life. National and international bodies concerned with the study of pain have proposed and recommended effective ways of managing pain, with emphasis on biopsychosocial treatment for those with chronic pain and validating the biomedical model for acute pain. Despite these well-meaning recommendations, there is a persistent gap in outcomes for the patient suffering in pain and the clinicians who treat pain. I believe this gap fails because we fail to set realistic end goals for pain management. The end goal of pain management should focus on getting patients healthy, not just solving pain signals.
Focusing on health starts with better assessment of pain and the health of the person with pain. This has to be done, especially with musculoskeletal issues through the lens of connective tissues & structures (orthopedics), functional limitation (physical rehab medicine), inflammatory (cellular medicine and rheumatology), and neuroaffective (pain neuroscience and psychology). Through these lenses, proposed by Dr. Helen Langevin, we are able to see continued on next page >
Make Health The End Goal Of Chronic Pain Management
continued from page 21 the broader picture of pain impact on the individual patient and prescribe the right integrative treatment (see figure 1). If we fail to address the neuroaffective aspect of chronic pain, for example, surgical outcomes are poor. It is also important to understand the secondary and tertiary complications that have developed due to chronicity of pain. Most patients develop compensatory mechanisms and impaired biomechanics that need to be addressed with appropriate therapy and strengthening programs with the goal to improve function. We also have to address neuroplastic or brain generated pain that has developed independent of tissue damage. This is done through Pain reprocessing therapy, Cognitive Behavioral Therapy, Acceptance Committed Therapy, and other neuro-framework techniques. These approaches improve psychological health which in turn improves biological health; an Integrative approach to musculoskeletal pain, bridging across neuroscience, physical therapy and rehabilitation, orthopedics, and rheumatology “silos.” Langevin, H. M. (2021). Reconnecting the brain with the rest of the body in musculoskeletal pain research. The journal of pain, 22(1), 1-8.
There are two important questions I ask each patient who comes to my clinic with complaints of chronic pain. First I ask, “What is your understanding of why you have pain?” And the second question is, “What does your pain prevent you from doing?”
The answers to these questions provide the opportunity to assess patient understanding of their pain and the functional imitations their pain has placed on their life. In my experience, most patients with chronic pain are not so concerned with pain sensation but the “painfulness” of the pain experience. They are most frustrated by the limitation that pain has placed on their life. They are angry, frustrated, anxious, and afraid. When I ask patients to tell me about their pain, they start talking about the fact they can’t go for a walk, they can’t hang out with their grandchildren, they can’t go to dinner with friends, they can’t go to the granddaughter’s wedding, all because of the pain. They can’t sleep in the same bed with their spouse, they are isolated from friends, and despite their best effort nothing gets better, or nothing works for them. They will often tell me, they have done physical therapy, chiropractic care, acupuncture, tried multiple pain medications including opioids, multiple epidural injections, joint injections, and sometimes surgery and still continue to have pain. The biggest revelation in the patient narrative and history is that they don’t understand what pain is. Their understanding of pain is often wrong or limited. This also unfortunately, is the case in many clinicians the patient encounters. This I see as one of the biggest obstacles to treatment. How do you manage something you don’t understand?
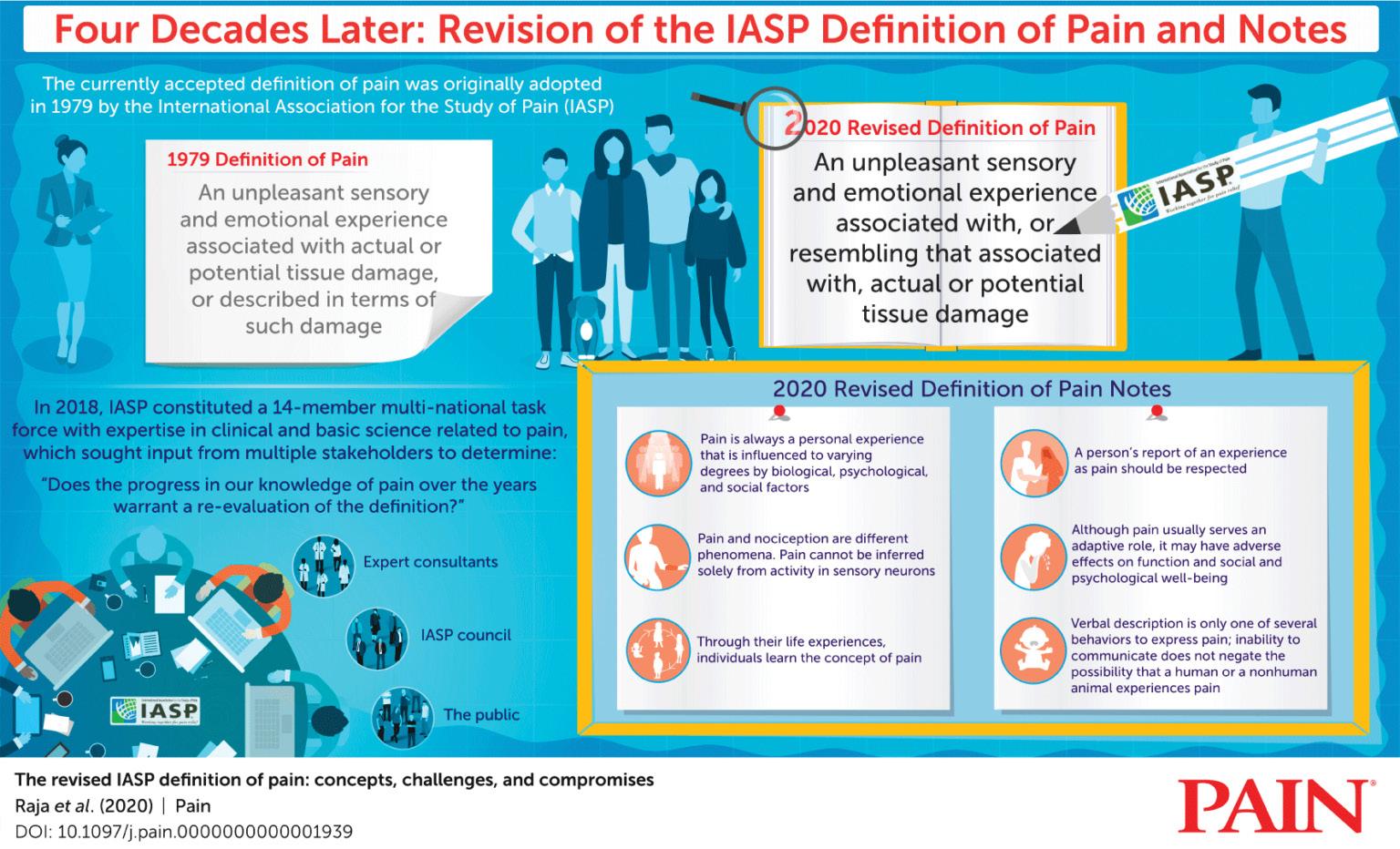
Pain, according to the International Association for the Study of Pain, is defined as a sensory and emotional experience associated with or may not be associated with tissue damage. We have had this definition since 1978 and the recent revision in 2020 maintains the same definition with 6 different qualifiers. These qualifiers were added based on our current understanding of pain in the last 40 yrs. Yet, how physicians and patients define pain are not in alignment of what pain is. First, treatment focuses only on the “Sensory” component of pain with limited attention to the “emotional component” of pain. We also tend to focus on treating “potential tissue damage” as real tissue damage, and don’t take into account the neuroplastic changes that have taken place and the resultant amplification of pain signals and more importantly brain generated pain signals.
It is important therefore to start with education before medications. It is important for patients to understand that their imaging findings alone don’t explain their pain. When I ask patients why they think they have pain, especially those with chronic pain will tell me “It is my L4/L5 herniation, their bone on bone knee, their car accident that happened 10 years ago, or the complications they got from a procedure or injections.” This does not invalidate patients’ narrative or complaints, but it is important for patients to understand that perhaps what started their pain is not the same process keeping them in pain. But what has “kept” them in pain may be something completely different. I break this education into Predisposing factors, Precipitating factors, and Perpetuating factors. There are certain predisposing factors to chronic pain including a small percentage relating to genetics, and many times psychological stressor (history of trauma, anxiety, depression, type A personality, unforgiveness, and metabolic disease). The precipitating factor is what patients remember most often. They are able to pinpoint the onset of the pain following a car accident, or a fall due to emotional crystallization.
It is important to explain to patients that what started their pain may not be what is keeping them in pain after 5-10 years. Disc herniations and most musculoskeletal injuries heal within 12 weeks, so why are they having pain after 5 years? We are still having pain because we have not focused on the health of the cells that generate, transmit, and interpret pain signals. We have not focused on healthy habits that allow the body to heal. How do we get the cells to become healthy whether it’s chondrocytes in the knee, microglia or astrocytes cells of the nervous system, or lymphocytes, neutrophils, macrophages, monocytes of the immune system? It becomes a function of addressing cellular efficiency and restoring homeostasis. This is not achieved with sodium channel blockade, epidural injections, anti-inflammatory meds, or opioid therapy. It becomes focusing on stress management, nutrition, exercise, and sleep. These interventions are well documented and validated in the literature, and consistently restore health to cells, tissues, organs, and organ systems. All these healthy approaches limit pro-inflammatory states and provide homeostasis. The evidence for these four pillars is overwhelming. Pain doesn’t get better when individuals are not getting restorative sleep, pain doesn’t get better if we continue to consume foods that perpetuate inflammation.
When this is paired with pain education, self-efficacy management, appropriate pain medications and interventions, pain improves and becomes manageable. The integration of complementary options and any other interventions should also focus on getting patients healthy. When patients are healthy, their outcomes from pharmacological interventions, surgical interventions, non-pharmacological interventions, and complimentary options are better.
Focusing on health as the end goal of pain management is an approach that rearranges the paradigm of chronic pain management to focus primarily on getting patients healthy. Of course, getting people healthy may seem like a daunting task but I will argue that it’s safer, cheaper, effective, and rewarding for both patients and physicians. It requires a new perspective from physician and patient. This starts with assessing patients’ psychology, physiology, and functional limitations relating to their pain.
The approach to getting patients out of pain should start with getting patients healthy. It is important for clinicians who are dealing with patients in chronic pain to focus on education before medications, self-efficacy management, optimizing sleep, nutrition, exercise and stress management. It is also important that our patients understand the importance of health focus as the way to get them out of chronic pain. When these are integrated not only do patients get pain relief, but get improvements in metabolic, cardiovascular, neurological, musculoskeletal and immune health.
Dr. Christian is founder of Aether Medicine, an Integrative & Regenerative Pain Management, and Rehabilitation Medicine Clinic in Wayne, PA. To learn more about Dr. Christian visit www.aethermedicine.com or call 484-806-1101.










