
4 minute read
Wait a S.E.C.: Sympathy, Empathy and Compassion
BY KATHLEEN E. WALLS, PSY.D., MS KRISTIN

Sympathy, empathy and compassion are the hallmarks of a solid patient-provider rapport. Although the need for sympathy, empathy and compassion is not race specific, its importance was highlighted during vaccine hesitancy work stemming from the COVID-19 pandemic. While conducting numerous COVID-19 focus groups, panel discussions, podcasts, and vaccine clinics, there were countless individuals, who identified themselves as part of the Black community, who stated they were hesitant to take the vaccine. Individuals reported that they did not trust the medical system. This stemmed from the history of systemic racism and inappropriate and unethical practices in their lives and the lives of their ancestors, disparate treatment within the healthcare system, and a lack of healthy, quality, and personal relationships with their Healthcare Providers.
The broken rapport between individuals and their Healthcare Providers became increasingly evident as individuals shared that they did not feel heard by their provider and that communication was experienced as “one-way” – from the Healthcare Provider to the patient. For instance, when some patients attempted to express their concerns and/or inquire about the vaccine, they received responses such as “I received my vaccine, and I didn’t grow an extra arm. You should get the vaccine too”; “Your kids received all their other vaccines. What’s the difference?”; and “The vaccines have gone through the clinical trial process. No safety issues have been found.” Unbeknownst to the Healthcare Providers, these responses increased the divide within the patient-provider relationship, and left the patients feeling unheard. Consequently, many individuals left these encounters with unanswered questions and an uncertainty on who to trust, listen to, and how to proceed during a time of fear, anxiousness, and what was posed as a “life or death” decision for themselves and their loved ones.
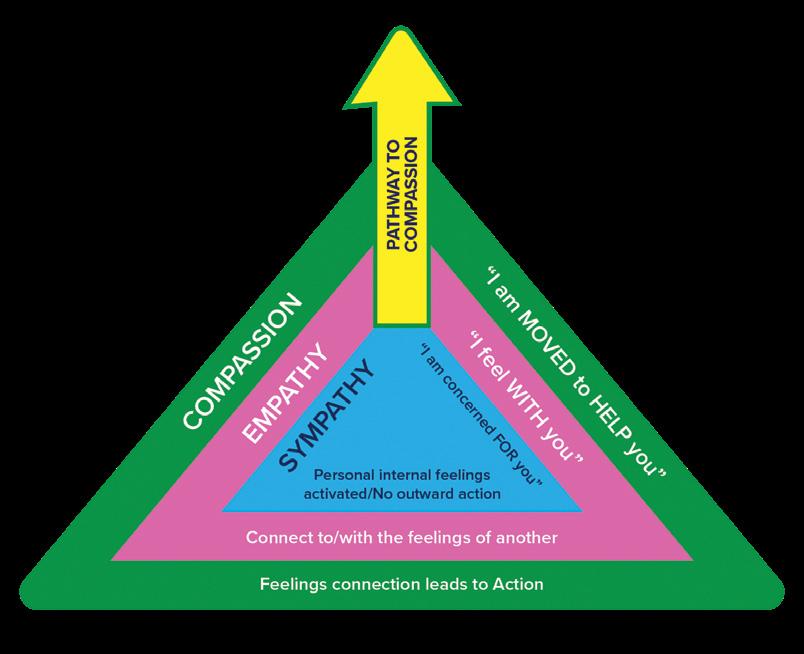
In 2020, the COVID-19 pandemic, uncertainty about an impending vaccine, accompanying social and racial injustice and unrest and conflicting public health messages from the White House, increased the need for provider compassionate care during this unprecedented time. Patients needed providers who were emotionally intelligent and able to express sympathy, empathy and compassion. On the Pathway to Compassion Model (see Figure 1), by Dr. Kathleen E. Walls, sympathy is identified as the first step in the process. Sympathy focuses on the internal feelings that a person experiences in relation to someone else’s stimulating/ activating event. Once the personal feelings are experienced and identified, then the individual can empathetically connect to and with the feelings of another person. This empathetic connection has been found to be supportive and cathartic by itself. However, when the resulting empathetic connection motivates one to take action, compassion is the resulting outcome. It is this shift from sympathy to empathy to compassion that patients are desiring.
During one of the focus groups, a patient shared that they told their Healthcare Provider “I’m not getting vaccinated because I don’t know if it is safe.” The Healthcare Provider responded with “The vaccines have gone through the clinical trial process. No safety issues have been found.” This real scenario left the patient feeling unheard, uncared for, and not connected to the Healthcare Provider. This was a great opportunity for the Healthcare Provider to connect with the patient. The Healthcare Provider could have utilized the Pathway to Compassion Model to build and strengthen the patient-provider relationship in that moment. See possible Healthcare Provider responses below.
Healthcare Provider Responses
Sympathetic Response: I’m sorry that you feel this way. I feel bad and concerned about your safety. However, the vaccines have been proven to be safe.
Empathetic Response: It sounds like you’re hesitant. Am I hearing that correctly? I know there have been times when my doctor offered me medical advice, and I wasn’t sure what to do.
Compassionate Response: It sounds like you’re hesitant. Am I hearing that correctly? I know there have been times when my doctor offered me medical advice, and I wasn’t sure what to do. What helped me make a decision was getting a 2nd opinion as well as doing some additional research. What safety questions do you have? Also what resources can I provide that would be helpful for you to make an informed decision?
When Healthcare Providers offer compassionate care, they are actively listening, building a relationship with the patient, answering patient questions, participating in the solution finding, and invested in the patient’s overall well-being. Compassionate care stems from the first principle of the American Medical Association, which states, “A physician shall be dedicated to providing competent medical care, with compassion and respect for human dignity and rights.” In alignment with this principle, the Shane, S. et al 2016 article, Compassion in Health Care: An Empirical Model, recommended that “all health professionals be trained in compassion, that compassion be considered and evaluated as a core competency of health care providers, and that system wide standards of compassionate care be adopted and implemented.” It has been found that the utilization and demonstration of sympathy, empathy, and compassion are essential for rapport building and patient retention.

Interestingly, although this first guiding principle lays the foundation for the importance of compassion, some providers have been taught and/or told not to care too much so that they could avoid burnout. However, contrary to this deliberate teaching, the research has shown the power and importance of compassion in healthcare. For instance, Baurers, S. (2022) noted that “Compassion can be a powerful beneficial therapy for the giver, too. Among health-care workers, more compassion was associated with more resilience and resistance to burnout” (The Philadelphia Inquirer, August 10, 2022). Dr. Stephen Trzeciak reported that “Scientific evidence shows that serving others, even showing simple kindness, is the best medicine for yourself. It is associated with tons of benefits for physical health, mental health, emotional health, and happiness, fulfillment, and well-being, as well as professional success” (Baurers, S. The Philadelphia Inquirer, August 10, 2022). This research has contradicted the earlier beliefs that engaging in less compassionate care would lead to less burnout. Instead, compassionate care has actually been found to create a win-win for both the providers and the patients.
Compassion was also found to be linked to other favorable personal qualities and characteristics. For instance, according to Shane, S. et al (2016) “Patients felt compassion stemmed from virtues of genuineness, love, honesty, openness, care, authenticity, understanding, tolerance, kindness, and acceptance (Journal of









