

INSIDE:
The Art and Science of Forensic Medicine
Berks County Medical Society Alliance Celebrates 100 Years
Legalization of Recreational Marijuana: Pros and Cons
Community Anchors: Reading Public Museum Celebrates 100th Anniversary




That’s why Healthgrades ranks Reading Hospital among America’s 50 Best Hospitals . . . and why Newsweek recognizes us as one of the World’s Best Hospitals.
Behind this honor is a team of exceptional doctors, nurses, clinicians, and support staff— each one committed to delivering outstanding care to every patient, every day.
Because for us, it’s not just about recognition. It’s about making a difference in the lives we touch.
Learn more at TowerHealth.org/Newsweek.
To provide news and opinion to support professional growth and personal connections within the Berks County Medical Society community.
D. Michael Baxter, MD, Editor
Editorial Board
D. Michael Baxter, MD
Lucy J. Cairns, MD
Daniel Forman, DO
Shannon Foster, MD
William Santoro, MD, FASAM, DABAM
Raymond Truex, MD, FACS, FAANS
Beth E. Gerber, IOM

Ankit Shah, MD, FACEP, FAAEM, FAMIA President
Olapeju Simoan, MD, MPH President Elect
Daniel Edwards, DO Treasurer
William Santoro, MD, FASAM, DABAM Immediate Past President
Beth E. Gerber, IOM Executive Director
Berks County Medical Society
2669 Shillington Rd,, Suite 501 Sinking Spring, PA 19608 (610) 375-6555 (610) 375-6535 (FAX) Email: info@berkscms.org www.berkscms.org
The opinions expressed in these pages are those of the individual authors and not necessarily those of the Berks County Medical Society. The ad material is for the information and consideration of the reader. It does not necessarily represent an endorsement or recommendation by the Berks County Medical Society.
Manuscripts offered for publication and other correspondence should be sent to 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501. The editorial board reserves the right to reject and/or alter submitted material before publication.
The Berks County Medical Record (ISSN #0736-7333) is published four times a year by the Berks County Medical Society, 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501. Subscription $50.00 per year. Periodicals postage paid at Reading, PA, and at additional mailing offices.
POSTMASTER: Please send address changes to the Berks County Medical Record, 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501.

Content Submission: Medical Record magazine welcomes recommendations for editorial content focusing on medical practice and management issues, and health and wellness topics that impact our community. However, we only accept articles from members of the Berks County Medical Society. Submissions can be photo(s), opinion piece or article. Typed manuscripts should be submitted as Word documents (8.5 x 11) and photos should be high resolution (300dpi at 100% size used in publication). Email your submission to info@berkscms.org for review by the Editorial Board. Thank YOU!

Ankit Shah, MD, FACEP, FAAEM, FAMIA President
As physicians, we are all familiar with the never-ending stream of requests to do “just one more thing.” Over time, these extra tasks add up – often without directly improving patient care or easing our administrative load. That is why this article focuses on a different question: What can BCMS do for you?

Let’s be honest: how many of us truly enjoy giving up a Saturday morning with family just to earn CME credits?
Finding time for CME is increasingly difficult. Budgets are tight, and when travel, meals, and registration aren’t covered, attending even one conference a year can be a stretch – let alone multiple ones. Recognizing this burden, BCMS spearheaded a state-level effort to make CME more accessible for physicians who are members of both BCMS and the Pennsylvania Medical Society.
As you know, Pennsylvania mandates CME on opioid prescribing and child abuse every two years, regardless of specialty – unless you’re in Addiction Medicine or don’t prescribe controlled substances. And yes, everyone still needs to complete the child abuse CME.
In the past, these requirements often meant giving up weekends or carving out time during already-packed workdays. Thanks to BCMS and PA Med, you can now complete these essential courses from the comfort of your home, on your schedule.
With CME budgets shrinking, joining professional societies is a tougher decision than ever. That’s why we’re proud to share some good news: starting in 2026, BCMS will be lowering annual membership dues for all renewing members (new members already receive a low introductory rate).

This is our way of saying thank you – and recognizing the challenge of deciding where to invest your time and resources. We hope this makes it easier for new and returning members to join or remain part of a society that has served physicians in our region for over 200 years.
The pandemic significantly disrupted our ability to foster professional connection and camaraderie among local physicians. In 2025, we’re committed to rebuilding that sense of community with increased networking and recruitment events.
These events are an opportunity to connect with colleagues you may not encounter during daily clinical routines – across different specialties and healthcare settings. We’re planning exclusive gatherings for members, as well as events that welcome your loved ones, to help deepen personal and professional ties throughout our society.
Quick poll – how many of you have heard of PA Med’s House of Delegates (HoD)?
BCMS has long had a seat at the table, but in recent years, our voice has grown stronger – thanks in part to the growing involvement of our resident and medical student members. The HoD brings together medical societies from across the state to shape the legislative agenda and advocate for policies that directly impact our profession and our patients.
Now more than ever, local representation in state-level decisionmaking is critical – and BCMS continues to lead on that front. If you have a passion for healthcare policy or simply want to learn more, we encourage you to reach out. Your voice can help shape the future of medicine in Pennsylvania.
We know you’re busy – and that “just one more thing” often feels like too much. But when it comes to BCMS, we hope you’ll see that our “one more thing” is doing more for you: making CME easier, reducing costs, reconnecting our physician community, and amplifying your voice at the state level.
Let us help lighten the load.


Adam J. Altman, MD
Angela Au Barbera, MD
Helga S. Barrett, OD
Jennifer H. Cho, OD, FAAO
Christine Gieringer, OD
David S. Goldberg, MD, FAAP
Marion J. Haligowski III, OD
Dawn Hornberger, OD, MS
Y. Katherine Hu, MD, MS
Lucinda A. Kauffman, OD, FAAO
Christina M. Lippe, MD
Tianyu (Tom) Lui, MD
Michael A. Malstrom, MD
Mehul H. Nagarsheth, MD
Abhishek K. Nemani, MD
Amy M. Olex, OD
Tapan P. Patel, MD, PhD
Jonathan D. Primack, MD
Kevin J. Shah, MD
Michael Smith, MD
Anastasia Traband, MD
Monica Wang, OD
Denis Wenders, OD
Linda A. Whitaker, OD, MS
Eye Consultants of Pennsylvania is the leading eye care practice in the region. And with good reason. Providing the best possible patient care begins with our board-certified professionals, clinical excellence and evidenced based practice. In fact, when it comes to comprehensive eye care, our ophthalmologists and eye care specialists are some of the best that you’ll find anywhere. But more than that, our entire practice is committed to cooperative management of your patient. It means that we communicate and consult 360°. We share information, and we provide direct cell numbers to our partner physicians. It means that we listen carefully to patients and their physicians and provide a wealth of patient and physician education materials. And ultimately, it means better outcomes for your patients.
For consultations and referrals, call 610-378-1344.

by D. Michael Baxter, MD, FAAFP


The Oxford Dictionary defines “inflection point” as “a time of significant change in a situation, a turning point.” Throughout history there have been many inflection points, some occurring abruptly and others over many years but all having the same effect – changing the course of human history, for better or worse. Such events have usually been viewed through the retrospective of time, long after change has occurred or at least has been irrevocably set in motion. Just a few examples include the early development of agriculture followed by the rise of the first urban societies, the fall of the Roman Empire, the Birth of the Renaissance and Enlightenment periods, the onset of the Industrial Revolution and our own Technological Age which has unfolded within our lifetime. We are now almost certainly once again at such an inflection point in human history and perhaps the one which is most consequential. However, unique to other such key historical times, we are aware of this inflection point and may have the ability to affect the outcome.
In recent issues of the Medical Record, we have focused on some of these issues: Artificial Intelligence (AI) in health care, the technological impact of Social Media on mental health (especially of adolescents), new powerful therapeutics for treating (and

Our long-term perspective and counseled insight provide the confidence investors need in today’s challenging environment. As a registered investment advisor, our fiduciary responsibility is only to you and the best interests of your investments.
Count on our qualified professionals for the trust, tenure and talent you can take confidence in—for the long term.
preventing) disease, e.g. immunotherapy (and gene-editing) and in this issue, the impact of Climate Change (CC) on Health. Indeed, historians may very likely identify our current generation as one which had the ability if not the moral imperative to make difficult but wise and ethical choices which could define our world for generations to come. In particular, while Artificial Intelligence offers tremendous opportunities to transform our lives for the better, there are also potential risks that could challenge the very definition of what it means to be human and how we live, work and manage our world and our relationships. Likewise, Climate Change, the subject of the cover feature in this edition, according to many scientists, poses an existential risk to society as we know it and perhaps to life on our planet. And these two interface where the immense demand for energy to power AI intensifies the very use of the fossil fuels which are driving the negative impact of Climate Change.
Recognizing that one is at an inflection point offers both an opportunity and a responsibility to ourselves and most importantly to those who follow us. Of course, that choice is complicated by a degree of scientific uncertainty, economic conflict, political unease
Integrity, Service, Performance. 610-376-7418 • connorsinvestor.com
and personal self-interest. However, hopefully we can agree that our choices moving forward on such critical issues must be based on the best scientific evidence available, truthful discourse and moral imperatives. Let us “choose wisely” as our decisions now will likely have a profound effect on the future of humankind.





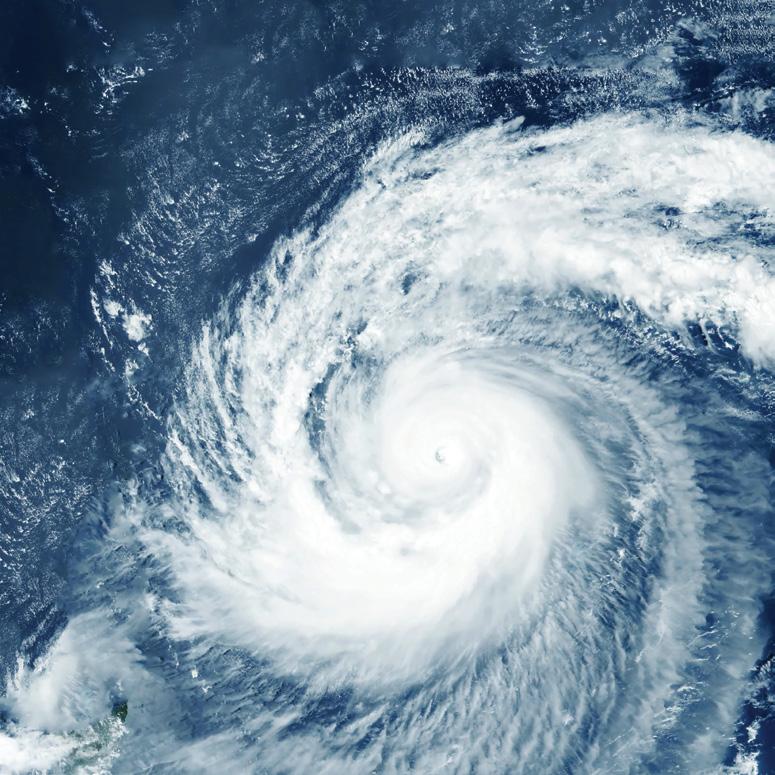

by Jasmine Slusser, BS, MPH
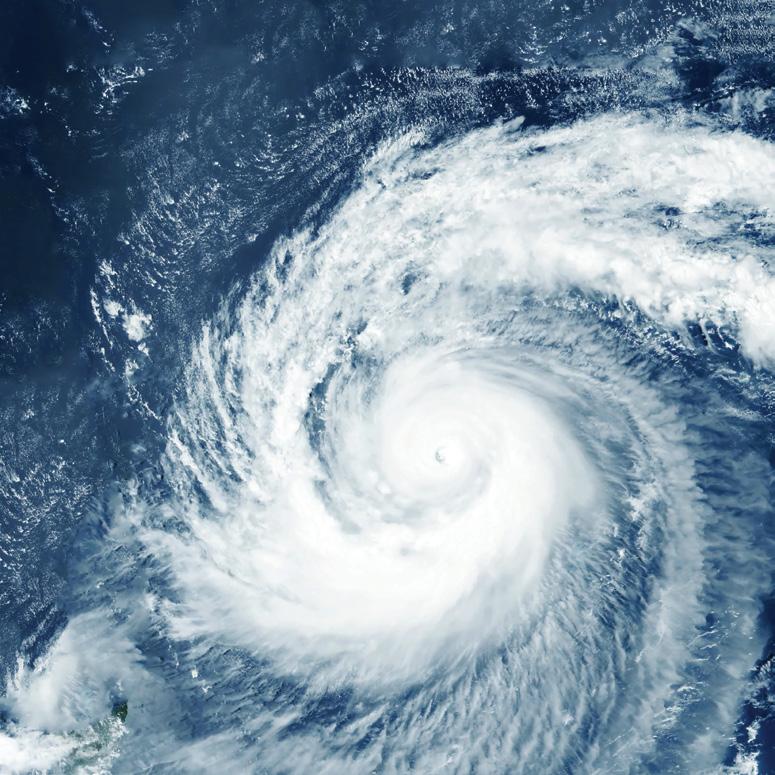
Visions of polar bears on melting ice caps, extreme forest fires, and devastating hurricanes might come to mind when first thinking of climate change, but the reality of climate change and its impacts is far more complex. According to the Intergovernmental Panel on Climate Change (IPCC), a United Nations intergovernmental panel which assesses climate science, climate change is defined as “a change in the mean and/or the variability of [a climate’s] properties…that persists for an extended period, typically decades or longer.”1 Historically, climate change has been a naturally occurring process initiated by volcanic eruptions covering the globe with ash, releasing greenhouse gases, blocking sunlight, and dramatically changing the planet’s temperature and, consequently, climate.2 The current global warming trend, which began in the mid-1800s, has been verified by institutions like the IPCC and National Aeronautics and Space Administration (NASA) to be the result of humans extracting, repurposing, and burning fossil fuels for energy production during the industrial revolution.1,3,4 On average, the Earth’s temperature has risen by 2° F each decade since 1850, and according to studies in 2023, “the 10 warmest years in historical record have all occurred in the past decade.”5 These findings are supported by the current level of atmospheric carbon dioxide (CO2) which is 50% higher than prior to the industrial revolution and “the annual rate of atmospheric CO2 accumulation over the past 60 years is about 100 times faster than previous natural increases, such as those at the end of the last ice age 11,000-17,000 years ago.”6

TIME SERIES: 2002-2022
Data source: Atmospheric Infrared Sounder (AIRS).
Credit: NASA
1: Atmospheric Carbon Dioxide levels throughout the history of the world
Greenhouse gas concentrations throughout the history of the planet can be estimated using ice cores, often harvested in Antarctica and Greenland. As samples of a core are slowly melted under laboratory conditions, gases are released from frozen bubbles which provide snapshots of atmospheric conditions.
National Oceanic and Atmospheric Administration. 1. Carbon dioxide concentration. climate.nasa.gov. August 15, 2023. Accessed May 30, 2025. https://climate.nasa.gov/vital-signs/carbondioxide/?intent=121
Fossil fuels such as coal, petroleum, and natural gas have undoubtedly paved the way for myriads of medical, technological, artistic, and social advances alike.7 Despite such advances, greenhouse gases, such as carbon dioxide, ozone, and methane, released in the process of generating electricity, creating single use plastics, and industrializing agricultural systems are driving climate change.1,3,4 Greenhouse gases naturally protect Earth’s biodiversity by trapping the sun’s infrared radiation, which presents as thermal heat, creating an inhabitable planet for life.8 The excess of greenhouse gases which have been re-released into the atmosphere by human activity is now raising the planet’s average temperature and generating climate changes.8
Unlike the term global warming may suggest, an increase in the planet’s temperature does not manifest in the same manner across all regions of the world.1,3,4,8 With approximately 71% of Earth’s surface covered by water, the planet’s climate is dictated by the nuanced physics of temperature and pressure.9 Just as the North and South poles of the Earth receive less sunlight with little precipitation, while the Earth’s equator is known for its lush rainforests and diverse
continued on next page >

Specializing in the diagnosis and treatment of ALL neck and back disorders.
ALL SURGERY PERFORMED IN BERKS COUNTY
• Pain Management
• Physical Therapy
• Epidural Injections
• Spinal Surgery
2607 Keiser Blvd, Suite 200, Wyomissing, PA 19610 484-509-0840

continued from page 9
ecosystems, a region’s climate is determined by its sunlight exposure and proximity to large bodies of water which influence precipitation and temperature.10 Thus, this increase in global thermal energy commonly manifests as the intensification of existing regional climate patterns.1,3,4,8 Subsequently, extreme weather and the blurring of biome boundaries better describe climate change today as the public experiences an influx in the severity and frequency of heat waves, cold fronts, snowfalls, landslides, forest fires, tornadoes, hailstorms, floods, and hurricanes.1,3,4,8
The practice of medicine has found itself as both perpetrator and victim of climate change. Reliable energy access has birthed state-ofthe-art robotics, technology, and facilities while plastic production aided infectious disease control with single use syringes, IV bags, gloves, packaging, and PPE (Personal Protective Equipment) – but at a steep cost. Healthcare has become one of the “most carbonintensive service sectors in the industrialized world,” accounting for approximately 4.4-4.6 percent of greenhouse gas emissions worldwide.11,12 Additionally, adverse outcomes associated with climate change are now affecting the field of medicine by limiting access to vital tools, presenting new barriers to care, and increasing disease burden.
Ozone, technically a greenhouse gas, is needed in the stratosphere to absorb harmful radiation, however, when it is released by vehicles and power plants, and trapped within the troposphere by humans, it adversely affects individuals with asthma.13 The U.S. Environmental Protection Agency has found increased tropospheric ozone associated with increases in medication usage, frequency of asthma attacks, and use of health care services.13 There is also research that suggests a positive association between Chronic Obstructive Pulmonary Disease (COPD) prevalence and “long-term exposure to trafficrelated air pollution.”14 Motor vehicle-centric infrastructure has also given rise to sedentary lifestyles increasing risk and exacerbation of chronic diseases.15 Elevated levels of particulate matter from wildfire smoke have been found to cause asthma attacks, headaches, fast heartbeats, wheezing, and breathing difficulties. In addition, such pollution places individuals with pre-existing chronic conditions such as COPD, asthma, diabetes, chronic kidney disease and heart disease at greater risk for adverse health outcomes.16 Lastly, studies on microplastic pollution which occurs as plastic products gradually break down in the environment indicate that human exposure to
microplastics may result in “oxidative stress, DNA damage, organ dysfunction, metabolic disorder, disrupted immune response, and neurotoxicity, as well as reproductive and developmental toxicity.”17
While extreme weather events, such as hurricanes and tornadoes, can result in direct mortality, intensification of weather patterns are also increasing morbidity incidence and prevalence. One study from the New England Journal of Medicine noted a “53.7% increase in heat-related mortality among individuals older than 65 years of age in the past 20 years.”18 Another concern is the lengthening of the ragweed pollen season since hay fever annually accounts “for more than 13 million visits to physicians’ offices and other medical facilities.”19 It is also crucial to note how individuals with a lower socioeconomic status are often more susceptible to long-term effects of extreme weather events due to living in areas more susceptible to extreme weather and possessing fewer resources to rebuild in the aftermath.1
Climate change, especially in the context of extreme weather events, poses many threats to the control and treatment of infectious diseases.20 Following extreme weather events, limited access to clean water, electricity, and sanitation methods fosters cross-contamination and infection.20,21 Climate change is also altering the landscape of infectious disease by expanding the territory of different disease vectors, as seen with Lyme disease and the spread of ticks.22 A study conducted by the National Institutes of Health (NIH) found that while the typical climate-driven incidence increase of dengue fever was 18%, increased temperature from manmade climate change could result in an incidence increase of 49%-76%.23 An additional NIH systematic review found increased temperatures will result in higher infection, dissemination and transmission of chikungunya as the virus’s incidence intensifies in tropical regions and encroaches into neighboring temperate areas.24 Increased incidence of coccidioidomycosis, a respiratory fungal infection also known as Valley Fever, has been observed during wildfires when regions of the Western U.S. experience transitions from extreme dry to extreme wet conditions.25 With extreme conditions becoming more common due to climate change, it is predicted that the incidence of diseases like coccidioidomycosis will continue to increase.25
In a streamlined and sterile medical world, it is easy to forget that many of the medications purchased over the counter and prescribed are non-synthetic, plant or animal derived. Thus, climate change poses threats to the global supply of many different drugs as crops are threatened by increased heat, reduced growing areas, and enhanced vulnerability to pests and disease.26,27 The current industrialized field of agriculture, which in 2021 accounted for 10.6% of greenhouse gases in the United States, has also contributed to antibiotic resistance.28,29 Combined with poor prescription and disposal practices, agriculture’s dependence on antibiotics for large-scale production of livestock has contributed to the rise of antibiotic-resistant bacteria strains.29,30 With few or no processes in place for capturing antibiotics or preventing antibiotic resistance within wastewater treatment plants, and no oversight of agricultural wastewater, antibiotics continue to be introduced into our environment and foster antibiotic-resistant bacteria strains.29,30,31
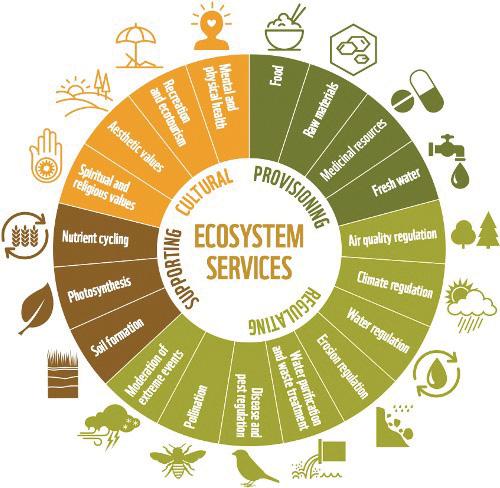
Human interaction with our environment is often viewed within the limiting confines of provisioning services, such as obtaining food, shelter and water. Among sustainability professionals, there is a movement to reimagine this relationship by acknowledging the intangible ecosystem services provided by the environment, such as pollination, erosion regulation, water filtration, spiritual and religious values, and aesthetic benefits. World Wildlife Fund. Living Plant Report 2016. awsassets.panda.org. 2016. Accessed May 30, 2025. https://awsassets.panda.org/downloads/lpr_living_planet_report_2016.pdf

Outpatient counseling for drug and alcohol addiction, mental health wellness and youth behavioral issues
• Has been serving the Berks County community for more than 45 years.
• Provides high quality, comprehensive and coordinated care utilizing evidence-based practices with same day access to services.
• Has a Child and Family Center designed specifically for families and children experiencing behavioral issues.
• Is a Certified Community Behavioral Health Clinic and an Integrated Community Wellness Center (IWIC).

continued on next page >




continued from page 11
In addition to the current stressors on our climate and our current food system’s promotion of antibiotic-resistant strains of bacteria, other environmental factors in our current dietary practices as a society threaten both our health and our planet. Palm oil and beef have been known to have large environmental footprints due to the copious amounts of land needed in their productions which are often obtained by deforestation via burning of land.32,33,34,35,36,37,38 The production of beef also requires large amounts of water and feed and results in the release of methane, a potent greenhouse gas.32,33,37,38 In addition to being contributors to climate change, consumption of red meat can increase risk of all-cause mortality by contributing to increased risk of cardiovascular disease, type 2 diabetes, and several forms of adenocarcinomas while consumption of palm oil has been linked to “higher mortality from ischemic heart disease.”39,40,41
Increased consumption of ultra-processed foods, a common source of single-use plastics which are a major source of environmental pollutants, are also associated with “adverse health outcomes, especially cardiometabolic and common mental disorders.”42,43,44
Climate change is no longer a conversation for the future; it is with us now and having a deleterious effect on health across the world. The question is no longer if, but how much damage climate change will inflict. The need for the voices and influence of physicians and other health leaders is essential and immediate in the current conversation about climate change.
Physicians, indeed all health care providers, as advocates for the health and well-being of their patients, can play a major role in local, national and even international policies that will impact the trajectory of climate change and its impact on health. From joining a local government environmental or medical advisory board to make healthy policy changes in our community, groups such as the City of Reading’s Environmental Advisory Council, to volunteering with an array of local or national environmental organizations, there is an active part to play. As medical professionals, physicians and their teams can educate patients on how decreasing their meat and processed foot consumption will not only improve their health but also protect our environment. Discuss the use of Seasonal Produce Guides that support local farmers’ markets for more affordable and sustainable consumption of fresh fruits and vegetables.45 Prompt patients to freeze produce before it decays to extend shelflife, prevent food waste, and avoid food-borne illness. Promote green spaces for environmental and health benefits of conserving ecosystems, spending time outside, and exercising outdoors. Educate patients on the importance of properly disposing of their medications, including their unused antibiotics. Provide brochures in office waiting rooms focused on climate concerns and environmental stewardship. Adopt a One Health perspective by engaging with local
colleagues in environmental science, veterinary medicine, and public health fields to craft more efficient and sustainable community health practices and policies.46 Lastly, physicians and all health care providers must stay informed. By exploring and supporting the tenets of sustainability in medicine and beyond, medical providers and professionals possess the power to create healthier lives for patients today while ensuring a promising future for generations to come.

Jasmine Slusser is a graduate of George Washington University with a BS and most recently an MPH degree. She is a native of Berks County and an alumnus of Berks Catholic High School. She is currently applying to medical school.
References
1. United Nations Framework Convention on Climate Change. unfccc. int. February 2011. Accessed May 30, 2025. https://unfccc.int/files/press/ backgrounders/application/pdf/press_factsh_science.pdf.
2. Volcanoes can affect climate. USGS. Accessed May 30, 2025. https://www. usgs.gov/programs/VHP/volcanoes-can-affect-climate.
3. Arias PA, Bellouin N, Coppola E, Jones RG, Krinner G, Marotzke J, et al. Technical summary. Climate Change 2021 – The Physical Science Basis. Published online July 6, 2023:35-144. doi:10.1017/9781009157896.002
4. Evidence - NASA science. NASA. October 23, 2024. Accessed May 30, 2025. https://science.nasa.gov/climate- change/evidence/#:~:text=The%20current%20 warming%20trend%20is%20different%20 because,rate%20not%20 seen%20over%20many%20recent%20millennia.&text=The%20 planet’s%20 average%20surface%20temperature%20has%20risen,into%20the%20atmos here%20and%20other%20human%20activities.
5. NCEI.Monitoring.Info@noaa.gov. Monthly climate reports. Monthly Climate Reports | National Centers for Environmental Information (NCEI). Accessed May 30, 2025. https://www.ncei.noaa.gov/access/monitoring/monthly-report/ global/202113.
6. Lindsey R. Climate change: Atmospheric carbon dioxide. NOAA Climate.gov. May 21, 2025. Accessed May 30, 2025. https://www.climate.gov/news-features/ understanding climate/climate-change-atmospheric-carbon-dioxide.
7. U.S. Department of Energy. Fossil. Energy.gov. Accessed May 30, 2025. https://www.energy.gov/fossil#:~:text=Fossil%20energy%20sources%2C%20 including 20oil,buried%20by%20layers%20of%20rock.
8. Calvin K, Dasgupta D, Krinner G, et al. IPCC, 2023: Climate change 2023: Synthesis report, summary for policymakers. Contribution of Working Groups I, II and III to the Sixth Assessment Report of the intergovernmental panel on climate change [core writing team, H. Lee and J. Romero (eds.)]. IPCC, Geneva, Switzerland. IPCC, 2023: Climate Change 2023: Synthesis Report Contribution of Working Groups I, II and III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [Core Writing Team, H Lee and J Romero (eds)] IPCC, Geneva, Switzerland. Published online July 25, 2023:1-34. doi:10.59327/ipcc/ar6-9789291691647.001
9. U.S. Geological Survey. How much water is there on earth? USGS. Accessed May 30, 2025. https://www.usgs.gov/special-topics/water-science-school/science/ how-much- water-there earth#:~:text=About%2071%20percent%20of%20 the,in%20you%20and%20your%20d g.
10. National Oceanic and Atmospheric Administration. Global Atmospheric Circulations. noaa.gov. Accessed May 30, 2025. https://www.noaa.gov/jetstream/ global/global atmospheric-circulations.
11. Eckelman MJ, Huang K, Lagasse R, Senay E, Dubrow R, Sherman
JD. Health Care Pollution and public health damage in the United States: An update. Health Affairs. 2020;39(12):2071-2079. doi:10.1377/ hlthaff.2020.01247
12. Pichler PP, Jaccard IS, Weisz U, Weisz H. International comparison of health care carbon footprints. Environ. Res. Lett. 2019;14. doi: 10.1088/17489326/ab19e1
13. Environmental Protection Agency. Health Effects of Ozone in Patients with Asthma and Other Chronic Respiratory Disease. epa.gov. Accessed May 30, 2025. https://www.epa.gov/ozone-pollution-and-your-patients-health/healtheffects-ozone- patients-asthma-and-other-chronic.
14. Hsu HT, Wu CD, Chung MC, et al. The effects of traffic-related air pollutants on chronic obstructive pulmonary disease in the community-based general population. Respir Res. 2021;22(1):217. Published 2021 Aug 3. doi:10.1186/s12931-021-01812-x
15. Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med. 2004;27(2):87-96. doi:10.1016/j.amepre.2004.04.011
16. Centers for Disease Control and Prevention. How wildfire smoke affects your body. cdc.gov. Accessed May 30, 2025. https://www.cdc.gov/wildfires/risk-factors/ index.html.
17. Li Y, Tao L, Wang Q, Wang F, Li G, Song, M. Potential health impacts of microplastics: A review of environmental distribution, human exposure, and toxic effects. Environment & Health. 2023;1(4):249-257. doi: 10.1021/ envhealth.3c00052
18. Patel L, Conlon KC, Sorensen C, McEachin S, Nadeau K, Kakkad K. Climate change and extreme heat events: How health systems should prepare. NEJM Catal Innov Care Deliv 2022;3(7). doi: 10.1056/CAT.21.0454
19. Environmental Protection Agency. Climate Change Indicators: Ragweed Pollen Season. epa.gov. Accessed May 30, 2025. https://www. epa.gov/climate-indicators/climate- change-indicators-ragweed-pollenseason#:~:text=Warmer%20spring%20temperatures%20cause%20some%20 plants%20to.
20. McMichael AJ. Extreme weather events and infectious disease outbreaks. Virulence. 2015;6(6):543-547. doi:10.4161/21505594.2014.975022
21. Hyde-Smith L, Zhan Z, Roelich K, Mdee A, Evans B. Climate Change Impacts on Urban Sanitation: A Systematic Review and Failure Mode Analysis. Environ Sci Technol. 2022;56(9):5306-5321. doi:10.1021/acs.est.1c07424
22. Centers for Disease Control and Prevention. Vector-borne diseases. cdc.gov. Accessed May 30, 2025. https://www.cdc.gov/climate- health/php/effects/vectors. html#:~:text=Climate%20changes%20can%20lead%20to,host %20immunity%2C%20and%20pathogen%20evolution.
23. Childs ML, Lyberger K, Harris M, Burke M, Mordecai EA. Climate warming is expanding dengue burden in the Americas and Asia. Preprint. medRxiv. 2025;2024.01.08.24301015. Published 2025 Feb 7. doi:10.1101/2024.01.08.24301015
24. Delrieu M, Martinet JP, O’Connor O, et al. Temperature and transmission of chikungunya, dengue, and Zika viruses: A systematic review of experimental studies on Aedes aegypti and Aedes albopictus. Curr Res Parasitol Vector Borne Dis. 2023;4:100139. Published 2023 Aug 24. doi:10.1016/j. crpvbd.2023.100139
25. Environmental Protection Agency. Climate Change, Wildfire & the Spread of Valley Fever. epa.gov. Accessed May 30, 2025. https://assessments.epa.gov/risk/ document/&deid%3D363179.
26. Climate Change Program Office, Walsh M, Buja L, et al. United States Department of Agriculture, Climate Change Program Office; 2020.
27. Reidmiller DR, Avery CW, Easterling DR, et al., eds. Fourth National Climate Assessment. Volume II, Impacts, Risks, and Adaptation in the United States. Summary Findings. Vol II. U.S. Global Change Research Program; 2018. 28. Sands R. Agriculture accounted for an estimated 10.6 percent of U.S. greenhouse gas emissions in 2021. ers.usda.gov. February 27, 2024. Accessed May 30, 2025. https://www.ers.usda.gov/data-products/charts-of-note/chartdetail?chartId=108623.
29. Manyi-Loh C, Mamphweli S, Meyer E, Okoh A. Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications. Molecules. 2018;23(4):795. Published 2018 Mar 30. doi:10.3390/molecules23040795
30. Nabidda S, Ssennyonjo R, Atwaru J, et al. Antimicrobial resistance and rational prescription practices: knowledge, perceptions and confidence of health profession interns in Uganda. JAC Antimicrob Resist. 2023;5(5):dlad105. Published 2023 Oct 3. doi:10.1093/jacamr/dlad105
31. La Rosa MC, Maugeri A, Favara G, et al. The Impact of Wastewater on Antimicrobial Resistance: A Scoping Review of Transmission Pathways and Contributing Factors. Antibiotics (Basel). 2025;14(2):131. Published 2025 Jan 26. doi:10.3390/antibiotics14020131
32. Cusack DF, Kazanski CE, Hedgpeth A, et al. Reducing climate impacts of beef production: A synthesis of life cycle assessments across management systems and global regions. Glob Chang Biol. 2021;27(9):1721-1736. doi:10.1111/ gcb.15509
33. Fitzherbert EB, Struebig MJ, Morel A, et al. How will oil palm expansion affect biodiversity? Trends in Ecology & Evolution. 2008;23(10):538-545. doi: https://doi.org/10.1016/j.tree.2008.06.012
34. Pirker J, Mosnier A, Kraxner F, et al. What are the limits to oil palm expansion? Global Environmental Change. 2016;40:73-81. doi: https://doi. org/10.1016/j.gloenvcha.2016.06.007
35. Fleiss S. Potential impacts of climate change on oil palm cultivation. University of York; 2017. Accessed May 30, 2025. http://www.sensorproject.net/ wp- content/uploads/2018/01/Climate-change-report-FINAL.pdf
36. Qaim M, Sibhatu KT, Siregar H, et al. Environmental, economic, and social consequences of the oil palm boom. Annual Review of Resources Economics. 2020;12(1):321-344. doi: https://doi.org/10.1146/annurevresource-110119-024922
37. Poore J, Nemecek T. Reducing food’s environmental impacts through producers and consumers. Science.2018;360:987-992.DOI:10.1126/science. aaq0216
38. Mekonnen MM, Hoekstra AY. A global assessment of the water footprint of farm animal products. Ecosystems. 2012;15(3):401-415.https://doi. org/10.1007/s10021-011-9517-8
39. UC Davis CLEAR Center. Why methane from cattle warms the climate differently than CO2 from fossil fuels. clear.ucdavis.edu. November 16, 2021. Accessed May 30, 2025. https://clear.ucdavis.edu/explainers/why-methane-cattlewarms-climate-differently-co2- fossil-fuels.
40. Alisson-Silva F, Kawanishi K, Varki A. Human risk of diseases associated with red meat intake: Analysis of current theories and proposed role for metabolic incorporation of a non-human sialic acid. Mol Aspects Med. 2016;51:16-30. doi:10.1016/j.mam.2016.07.002
41. Kadandale S, Marten R, Smith R. The palm oil industry and noncommunicable diseases. Bull World Health Organ. 2019;97(2):118-128. doi:10.2471/BLT.18.220434
42. Lane MM, Gamage E, Du S, et al. Ultra-processed food exposure and adverse health outcomes: umbrella review of epidemiological meta-analyses. BMJ. 2024; 384. doi: https://doi.org/10.1136/bmj-2023-077310
43. UN Environment Programme. Everything you need to know about plastic pollution. unep.org. April 25, 2023. Accessed May 30, 2025. https://www.unep. org/news-and- stories/story/everything-you-need-know-about-plastic-pollution.
44. United Nations Environment Programme. Plastic pollution science. wedocs.unep.org. 2022. Accessed May 30, 2025. https://wedocs.unep.org/ bitstream/handle/20.500.11822/40831/K2221533%20-%20%20UNEP-PPINC.1-7%20-%20AMENDED%20ADVANCE%20-%2014.10.2022.pdf
45. SNAP Education Connection. Seasonal produce guide. snaped.fns.usda. gov. Accessed May 30, 2025. https://snaped.fns.usda.gov/resources/nutritioneducation- materials/seasonal-produce-guide.
46. U.S. Centers for Disease Control and Prevention. One Health. cdc.gov. Accessed May 30, 2025. https://www.cdc.gov/one-health/about/index.html.










Nathaneal Hoskins, DO, a 4th year Obstetrics and Gynecology Resident at Reading Hospital/Tower Health, has been selected as a Top Physician Under 40 by the Pennsylvania Medical Society.
Dr. Hoskins is a graduate of the Edward Via College of Osteopathic Medicine in Blacksburg, Virginia. He is recognized for his commitment to the highest standards of obstetrical care, his contributions to clinical research, and his leadership and mentoring skills among his colleagues.
His career goals are to pursue a Maternal Fetal Medicine fellowship and to provide care for patients with high-risk pregnancies.
The Berks County Medical Society is certainly very proud of this recognition for Dr. Hoskins and for the work performed by all our Berks County residents.

by Mansi Vasconcellos, MD, President, BCMS Alliance


The Berks County Medical Society Alliance is celebrating 100 years! For the past century, the Alliance has partnered closely with the Berks County Medical Society to provide philanthropic contributions to our communities. We have many exciting events planned during this special year to bring our physicians and families together. Stay tuned!
We are celebrating another milestone: fifty years of funding scholarships to health care professionals who live in and attend school in Berks County. In previous years, we have supported the education of many health care students, and we know they have contributed to a stronger Berks County. This year we are distributing even more than our usual amount in scholarships to honor our 50year achievement.
It is our privilege to partner with several community agencies. Our past cycle of charitable donations has supported BCTV in programming specific to breast cancer education; Berks Free Medical Clinic for providing services to the uninsured; Lighthouse Women & Children’s Center to build a disability-inclusive playground; and North Star Initiative for providing medical care to its residents.
Our incoming Board is hard at work planning an impactful and meaningful year ahead as we open a new CENTURY of improving the health of Berks County. Thank you to the Medical Society and its members for your support over the years!


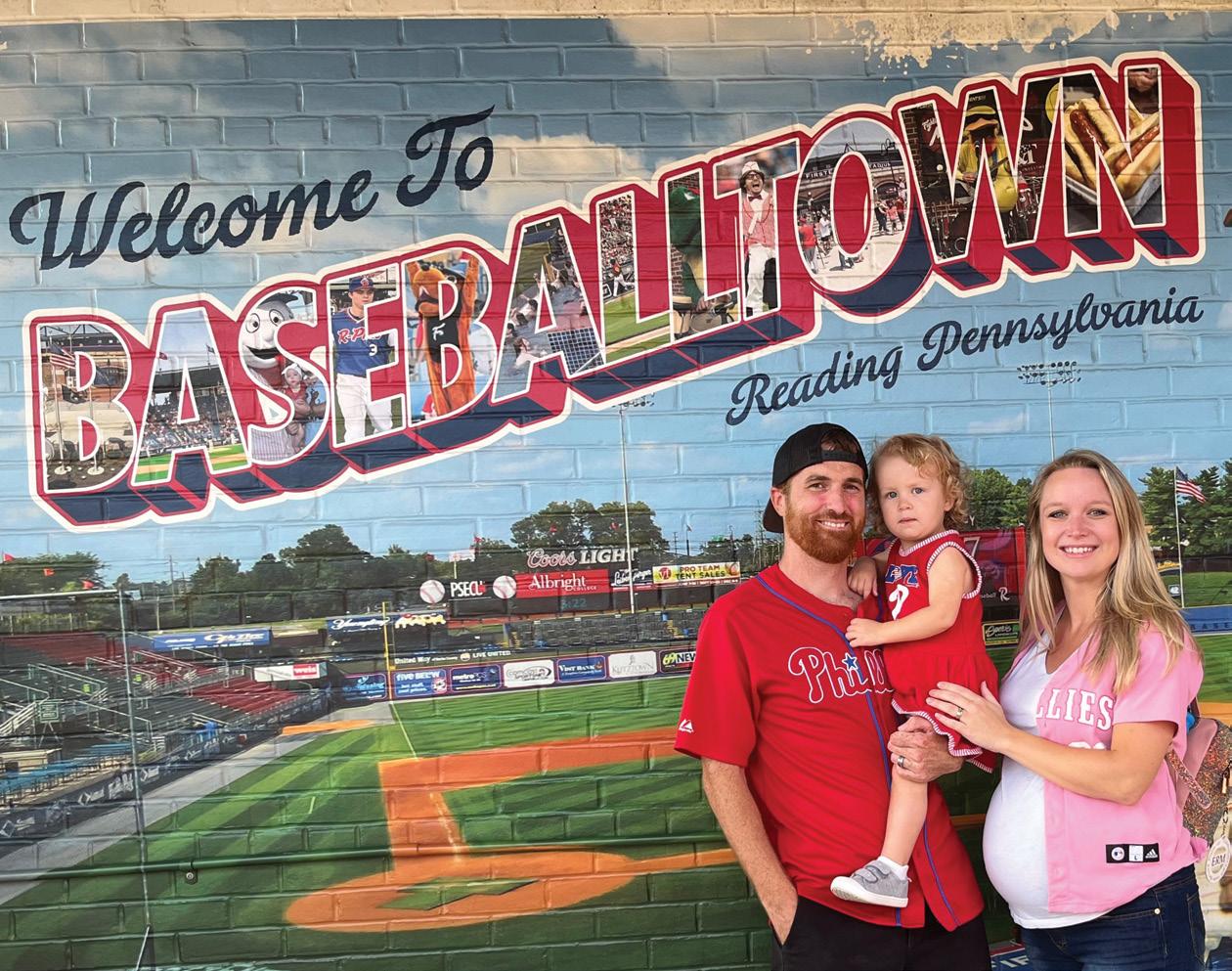
On Saturday, May 3rd, the Berks County Medical Society once again partnered with the Berks County District Attorney’s Office, the Council on Chemical Abuse (COCA), SOS Berks and the Reading Fightin Phils to sponsor the annual “Drug Take Back” event at First Energy Stadium. At this event, members of the community drive up that morning and drop off unused medications, including controlled substances, which otherwise might be inappropriately discarded or misused. These medications are then turned over to the Drug Enforcement Administration (DEA) who incinerates them.
Statistics for the event included:
32 pounds of controlled substances
353 pounds of non-controlled medications
385 pounds total, a 50% increase over what was collected in 2024.
A very big thank you to District Attorney John Adams and his officers, Marcia Goodman-Hinnershitz representing SOS Berks, Cindy and Jenna Martorana from COCA and Anthony Pignetti of the Fightins as well as our own BCMS members and staff. Also a special note of appreciation to the Drexel University College of Medicine, West Reading Campus students who played an indispensable role in sorting medications and learning a bit of pharmacology in the process.





As the premier Realtor in Berks County, Lisa Tiger uses her marketing, and extensive network to more quickly match buyers and sellers.
Lisa’s passion and tenacity combined with her sales and marketing skills have made her the most successful agent in Berks County. She would love to have the opportunity to share that success with you.
When you are ready to buy or sell, Team up with the Tiger!

•
•
•
•
•
•




Few landmarks are as central to the cultural life of Berks County as the Reading Public Museum (RPM) in its pictorial setting, embracing the Wyomissing Creek as it winds through Wyomissing Park. The setting itself appears as majestic as one of the works of art enclosed within its galleries. This year celebrates the 100th Anniversary of the laying of the cornerstone for a grand building in what was a rather remote section at the time. However, a generous gift of land by Irvin Impink and Ferdinand Thun resulted in the beautiful campus which we enjoy today. This event was commemorated on May 1st with the dedication of a time capsule encompassing contemporary artifacts and the planting of an Artemus 1 Moon Tree which grew from a seed that had traveled on a NASA mission to the moon.


The original museum was founded in 1904 by Levi Mengel, a legendary educator in the Reading School District, as his personal collection of life science exhibits for the purpose of teaching his students. It was initially located in the school Administration Building; however, as the collection grew, Dr. Mengel realized the value of making it available to the broader community. How prophetic he was, as the RPM, now including the Arboretum and the Neag Planetarium, has become an educational and cultural resource for the people of Berks County and beyond. With its many engaging programs for children as well as eclectic artistic exhibits and events for adults, the museum staff have created an institution that engages the interests of everyone in Berks County.
“The Museum is delighted to celebrate 100 years in its iconic building in the 18th Ward of Reading. The continuing existence of our building and grounds exemplify the timeless need for communities to have unyielding places to gather, learn and be inspired,” said Geoffrey K. Fleming, Executive Director and CEO.
Berks County Medical Society member and RPM Board member Seth Rosenzweig, MD, added, “Art has been my refuge from the
continued on next page >

continued from page 21

chaos of work for a long time, and my family and I have been going to the Reading Public Museum since shortly after we moved here in 1987. It has never ceased to amaze me how extensive the collection is for a medium-size museum like ours, and how the Museum is able to cater to so many interests with the galleries, Arboretum and Planetarium. This is a truly unique place. Having been involved with the Collections Committee and the Board of Directors for a long time, I have also had a privileged window into the staff at the

Museum. Their dedication to educating everyone in our community is inspirational.”
Our community is fortunate to have such a cultural landmark reminding us of the value of art, education and science in our lives. The Berks County Medical Society congratulates the Board and staff of the RPM for their many achievements, and we celebrate with all of Berks County the 100th Anniversary of this cultural gem.



Caitlyn Moss, MD
Academic Hospitalist Director, Continuing Medical Education, Department of Medicine Director, Curricular Development, Internal Medicine Residency Reading Hospital/Tower Health Associate Professor of Medicine, Drexel University College of Medicine
Tell us a little bit about yourself.

I am an Academic Hospitalist and core faculty member for the Internal Medicine Residency Program at Reading Hospital/Tower Health. I have been here for five years now and love it! I am originally from Lancaster County. I went to medical school at Penn State Hershey and then completed my residency training in internal medicine at the Beth Israel Deaconess Medical Center/Harvard Medical School in Boston. After I completed residency, my husband and I wanted to move back home to be near family, and I found a wonderful job at the Reading Hospital where I am able to do two of my favorite things – take care of patients and teach our trainees. My husband and I have two little girls, ages one and three, who are the light of our lives. We are active in our church and love to get on the golf course anytime we can.
Tell us about your role in the Berks County Medical Society and why membership is important for Early Career Physicians.
I serve as the Early Career Physician Chair on the Board of Directors of the Berks County Medical Society. Our Board wants all physicians in Berks County to be involved in this important organization; however, my role is specifically to target those early in their career. I found that joining BCMS early on was a terrific way to connect with my surroundings and get to know my colleagues working in Berks County. As opposed to where I trained in Boston which has >20 hospitals, Berks County is unique with only two hospitals and a lot of successful privately owned physician practices. It feels much more tightly connected here, which I love. Through BCMS, I have enjoyed getting to know physicians in different departments, hospitals, and practices. It makes it much easier to consult someone when you already have met them and know something of their interests or personality. I have also found the Berks County Medical Society to be a great way to connect with physicians who have been practicing for longer than I have, and who are full of sage advice and wisdom on how to have a successful and fulfilling career. For anyone who is considering membership in BCMS, I would love to talk more with you! You can reach me at caitlyn.moss@towerhealth,org.
We hope you (and your families!) can join us for our upcoming event at the Reading Fightin’ Phils game on August 14th.



orensic Medicine is perhaps one of the least understood of the various disciplines of medicine. For those of a certain age, the topic may suggest the extremely popular television series “Quincy, M.E.” (1976-83) starring Jack Klugman as a county medical examiner who investigated what appeared to be natural deaths for the clues that ultimately led to criminal charges and a sense of justice for the deceased. While the stories on “Quincy” were sensationalized for a television audience, they did emphasize the combination of intuitive “art” and scientific skill that made Dr. Quincy’s efforts highly successful. While intuition, instinctive understanding seemingly without conscious reasoning, seems to have little relationship to scientific knowledge, the combination of the two can increase the skills of any physician, but none more than that of the Forensic Medicine specialist.
The term Forensic Medicine encompasses a group of medical specialties, including Forensic Pathology and Forensic Psychiatry. Forensic Pathology is the branch of medicine which deals with the examination and diagnosis of individuals who have been injured by or who are presumed or suspected to have died because of external or unnatural causes, e.g. poisoning, assault, suicide, neglect and other forms of violence. These findings are applied to legal issues but also bring closure to the families of the deceased as well as to those who provided medical care. The primary clinical tool of the forensic pathologist is the autopsy, supplemented by an array of additional laboratory tests and other studies. Forensic Psychiatry is the sub-specialty of Psychiatry that deals with issues arising in the
interface of psychiatry and the law, particularly where mental illness and the criminal justice system interface. The forensic psychiatrist often works in specialized settings, e.g. correctional facilities and forensic hospitals. They perform independent psychiatric evaluations for criminal responsibility, competency and risk assessments and often serve as expert witnesses.
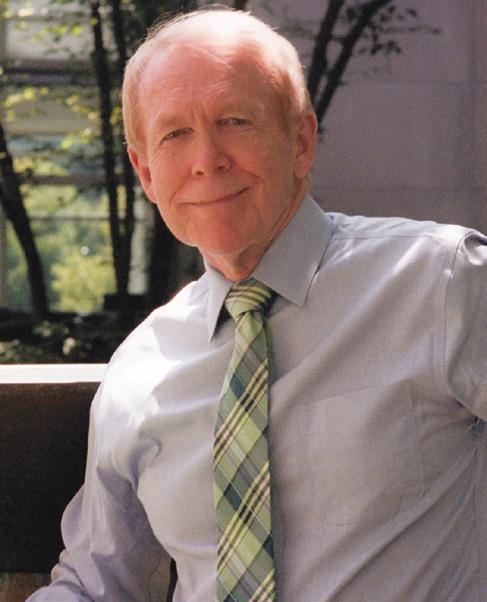
Berks County is fortunate to have two recognized experts in the field of Forensic Medicine, Neil Hoffman, MD (NH), a distinguished Forensic Pathologist, and Larry Rotenberg, MD (LR), a renowned Psychiatrist with extensive experience in forensic psychiatry. The following dialogue highlights their extensive knowledge and many years of experience in the fascinating field of Forensic Medicine.
The forensic pathologist is first and foremost a physician. Like clinical medicine, we rely on a history, often from medical records or the law enforcement or coroner’s investigators; we perform a physical examination, a physical examination in the form of an autopsy and microscopical studies. We order and interpret various laboratory tests and imaging and other ancillary studies to formulate opinions or diagnoses. We are trained like other pathologists, but are given additional training, usually through Fellowships with additional experience in toxicology, basics of criminalistics, and biomechanics of various forms of injuries. We apply these skills in the investigation of sudden, unexpected, and violent deaths and may be called upon
to testify in various legal proceedings. The word “forensic” itself is rooted in the Latin forensis, of or relating to the forum where public discussions and debates took place.
What unique role does the Forensic Psychiatrist have? (LR): Forensic psychiatry is the specialty of Psychiatry which deals with the interface of psychiatry and the law, either civil or criminal. If I am called as a witness, I always confirm my testimony; I never swear. I introduce myself to the judge, the opposing attorneys and the jury as a physician and lay the groundwork for my further testimony. In civil cases, my testimony often constitutes the study of various capacities or lack there of for an individual, often focused on questions of aging. An older person may show some degree of cognitive decline, and the question is whether they are competent to manage their own affairs, e.g. writing checks, paying bills and keeping track of their assets. If the Court determines that the individual is not competent, then a guardian is appointed to manage their affairs. This can become particularly challenging regarding the ability to create a will, in what is known as testamentary capacity.
The criminal portion of Forensic Psychiatry consists of the following: Competence to stand trial, Criminal responsibility and Competence to wave Miranda rights. In American and British law, a crime consists of two basic elements: the ACTUS RHEUS or the bad act and the MENS RHEA, the bad mind. In our system of law, the bad mind or the guilty mind is much more important than the bad act. For instance, if you accidentally run over someone with your car and the person dies, they are every bit as dead as if you pumped several bullets into them; however, you will not be judged guilty of the same crime to the same degree for both acts. Because the state of mind is a central issue, psychiatrists and psychologists are often called to testify to this question.
are presented with a “reasonable degree of medical certainty,” i.e. the expert witness feels that their opinion represents a 51% degree of certainty or “clear and compelling evidence” in which it is felt that there is at least a 75% degree of certainty. The latter, for instance, would be required to terminate parental rights in a custody case. What do you particularly find most enjoyable about your Forensics work? (NH): I like dealing with things that I can see, touch and yes, smell. I like facing a problem, bringing my faculties and techniques to bear on it and coming up with a solution. I like explaining my findings in a case to professionals, e.g. other physicians, judges and attorneys as well as lay people, the main constituency of a jury. When I became a pathologist, I felt pathology was one of the last bastions of true general practice medicine and that the pathologist played a major role in the diagnosis and treatment of patients in the hospital; that the pathologist is a true “doctor’s doctor.” The pathologist’s stock in trade is their opinion, which carries great significance.

What do you find most gratifying in your work in Forensic Psychiatry?
(LR): The most gratifying aspect of this work is educating the Court, the attorneys and, as necessary, the jury. While pathologists deal with concrete issues, mental health professionals have the much more difficult task of dealing with abstract issues involving the brain and the mind. In addition, there is a good deal of neurophysiology and psychopharmacology to convey to these lay people. So at the end of the day, if I have managed to convey a clear message and have helped to arrive at the truth, then in a particular case, I feel that I have done a good job.
Whose agent are you when you perform your duties? (NH): The majority of my autopsies are performed at the request of the Coroner of Berks County. If I am required to go to court to testify about any of these cases, I am paid for my time preparing and presenting my testimony. I am not paid for my opinion as that would be unethical. I may be called to testify by the prosecution, the defense or the plaintiff (civil case). At times I may be called to review the findings of another pathologist. Again, I bill for the time involved, not for my opinion; thus I am no one’s “agent” or perhaps my own agent or an agent of the court.
What does it mean for you to be a “witness” in court? (LR): In forensics one may be called as a “fact witness” or an “expert witness.” The former presents only the facts of the case as they see it. The latter gives their expert, professional opinion. Such opinions
How do you arrive at the “Cause of Death” as opposed to the “Manner of Death”? (NH): These concepts are quite technical and poorly taught in medical school and clinical residencies. “Cause of Death” is usually a pathogenetically related sequence of causes; the “Underlying Cause” which is to be entered on the bottom line of Part 1 of the death certificate. There might also be “Contributory Causes,” not pathogenetically related to the underlying cause but nevertheless important in understanding how the death occurred. The “Manner of Death” is essentially how the cause of death came about. Manners are categorized into two groups: natural diseases and violent deaths, the latter including homicide, suicide, accident and violence of undetermined origin. To differentiate among them we use historical data, physical findings including those at the scene of death, laboratory data and findings at autopsy. From these, I might also derive opinions regarding the time or place of death or injury, the identity of the decedent and possibly the type of instrument or weapon (modality) involved in the death.
continued on next page >
continued from page 25
Both of you have consulted and testified in hundreds of forensic cases. What particular case or circumstances stand out in your mind as especially challenging or noteworthy? (NH): In 1995 I was contacted by Robert Kirschner, MD, an excellent forensic pathologist at the University of Chicago, requesting my participation in a multidisciplinary multinational investigative team under the leadership of Physicians for Human Rights with ties to the United Nations and the International Courts. We were to investigate findings from a mass burial site outside Vukovar, Croatia, following the Croatia-Serbian War. Two hundred patients and personnel had been evacuated from the Vukovar Hospital four years previously by the invading Serbians who had promised that they would be safer in the location where the grave sites were eventually found. They were systematically murdered and buried in shallow graves. Our job was to identify the victims, if possible, and to establish the cause and manner of death. All the bodies were in an advanced state of decomposition, but because they were at least partially buried, the decomposition process was almost entirely chemical and without the help of insects or other postmortem predators. I well remember one of the 25 cases I examined in the two-week stint I was assigned in Zagreb. The body was that of an elderly man who had been shot multiple times. He had advanced degenerative joint disease. Also present was an aortofemoral bypass graft. On that basis, he was identified as the father of the head physician of the hospital, who herself was among those slaughtered.
Four years later, in 1999, the UN International Criminal Tribunal for the former Yugoslavia (ICTY) organized similar multinational multidisciplinary teams to examine remains being recovered from multiple primary and secondary graves near Srebrenica Bosnia. It had been determined that over a three-day period in July 1995 more than 8000 Bosnia Muslim men and boys had been systematically murdered and buried by the Bosnian Serb Army. This was the largest example of crimes against humanity and genocide (with perhaps the exception of the Rwandan murders) since the Nazi era. It was a much larger operation than had been carried on in Croatia. Even so, I was the sole American pathologist involved. Of the 22 cases I examined in my two-week stint in Visoko, Bosnia, one stands out in my memory: One of the remains appeared to be shorter than most of the others. There were three projectiles recovered from his torso. A bandana was wrapped several times around his head. As I examined his arms I saw that the humeral heads were separated from the shafts by defects that did not look like fractures. X-rays and direct examination showed that these were the humeral capital epiphyses, and the anthropologists determined that the victim’s age was 11. Both of these stints were very influential on me. The smells and sights we had to deal with were extraordinary, even for me. Each night I would have to go to my room and try to wash off the stench of the main decomposition
chemical, adipocere. But they gave me a sense that I had participated in history. Convictions of the military and political leaders for both the Bosnian and Croatian tragedies were handed down by the courts. One of those convicted committed suicide.
These brief encounters also were the closest I would come to the Holocaust in both setting and horror. I went to the Jewish section of the Miragoj Cemetery in Zagreb and observed memorials for families which lost many members in the genocide of the Holocaust.
For my work and subsequent presentations in Berks County, I was given the William Alexander Community Service Award by the Berks County Medical Society in 1995 and the Award for International Voluntary Service by the Pennsylvania Medical Society in 2001.
What particular cases or circumstances stand out in your mind as especially noteworthy? (LR): I have been involved in more than ten cases where the death penalty has been an issue. About ten years ago, the United States Supreme Court issued a decision that the death penalty for juveniles, children under eighteen, was unconstitutional. Shortly thereafter, the same court issued a decision that life without parole was cruel and unusual punishment for this same group. I evaluated at least ten individuals to help determine whether they should have a new trial. I found that nine out of the ten did indeed warrant a new trial. They were different people from the ones who had killed someone as a teenager. They were now in their 50s and 60s, totally different from their earlier selves, and had made new lives for themselves in prison. One of them, for example, had created a hospice service for elderly prisoners so that these individuals could die “at home” in their familiar prison surroundings rather than be shipped off to another facility with no one familiar around them at the end of life.
Another was anxious to return to his state prison from the county jail where I had examined him, because he feared losing his role training therapy dogs, part of a new life which he had created for himself. These were some of my most satisfying cases as they combined the best in Justice with the best in Psychiatric Medicine.

Neil Hoffman, MD, is an eminent Pathologist at Reading Hospital/ Tower Health with hundreds of Forensic Medicine cases in Berks County and beyond.
Larry Rotenberg, MD, is the retired Chair of Psychiatry at Reading Hospital/Tower Health and remains very active in clinical psychiatry, including his distinguished work in Forensic Psychiatry.

by Deba Osaghae, MD, PGY 3, Internal Medicine Residency Program, Reading Hospital/Tower Health
“I heard she’s from the county jail.”
Yes. That’s me. Are they talking about me?
“Really? Do you know why?”
“Yes, I heard she murdered her child.”
Wait. They are talking about me! That’s not the real story. Why can’t I speak? And wh-where am I?
“That’s sick! What?! How did she get here with such bad head trauma, though?”
Well, I was trying to break up a fight between two women, and I got hit in the head.
“She got into a fight with an inmate.”
Well, would you look at that? Another lie. Who are these people anyway? Where am I?! Why can’t I move?
“Hey, anesthesia’s kicked in, can we time out now?”
Time out? What’s that?
“Alright…we have Ms. De-Souza*, a 35-year-old inmate from the county prison, here with a traumatic brain injury complicated by a left epidural hematoma; we are performing a craniotomy and hematoma evacuation…”
“So, killed her child and tried to kill someone else, huh?”
Why is everyone saying that? My child was murdered by her father, and he framed me. I had no money. No support. No one to fight for me.
“What a loser. Some people do not deserve to live. How do you even know all of this?”
“I read it in her chart, also got the scoop from Dr. A.” Is this what is written about me? Is this who I am painted to be? I. Need. To. Move… why can’t I move my body?

“Yeah, Dr. A. always has the best scoop.”
“She should have died instead of that poor baby.”
I tell myself that every day.
“I agree; also read in her chart that she’s a difficult patient. Doesn’t take meds or adhere to medical advice.”
Does everyone here just lie? That happened only once, and I was in the middle of a divorce. I had no will to live or take medications. I was also homeless. How could I have made my appointments?
“Sheesh, she’s one of them.”
“Yeah, unfortunately.”
But I’m still here. Trapped in this body, screaming where no one can hear me. They see a chart, a rumor, a sentence served – but not the mother I was, the woman I am. I don’t know if I’ll wake up from this. But if I do… maybe then, someone will finally listen.
While medical documentation is essential for continuity of care, it also serves as the patient’s introduction to the healthcare system, often without their input. In this way, our notes become a form of advocacy.
Whether you are writing in a chart or reading one, remember: every patient has a story that extends beyond the lines of a progress note. Let us make room for that story, with accuracy, empathy, and humility.
*The patient name used in this narrative is fictional. Any similarity to real individuals, living or dead, is purely coincidental and unintentional.


by William Santoro, MD, FASAM, DABAM
Associate Medical Director of Addiction Medicine
St. Luke’s University Hospital Network
by William Santoro, MD, FASAM, DABAM
s cannabis policies evolve across Pennsylvania, the United States, and beyond, healthcare professionals are increasingly involved in discussions surrounding legalization. Understanding the nuanced differences between recreational and medical cannabis legalization is essential for clinicians tasked with patient guidance, public health advocacy, and policy input. What is needed is an objective, evidence-based discussion – free from emotion, stigma, and judgment – about the benefits and drawbacks of each approach. What follows, I hope, is a comparative analysis to inform medical professionals about the potential implications of each approach.
There are substantial benefits to the legalization of recreational cannabis, particularly in addressing long-standing inequities in the criminal justice system. One of the most impactful is the significant reduction in arrests for simple cannabis possession, which historically have disproportionately affected communities of color and those of lower socioeconomic status. According to the American Civil Liberties Union (ACLU), between 2010 and 2018, Black individuals were 3.64 times more likely than white individuals to be arrested for marijuana possession, despite similar usage rates across racial groups (ACLU, 2020). In some states, the disparity was even greater – up to 9 or 10 times higher.
Moreover, these enforcement patterns reflect broader systemic issues. In lower-income neighborhoods, heightened police presence, fewer legal resources, and implicit bias compound the effects of these laws. Arrests can have cascading consequences: loss of employment, housing instability, barriers to education, and family disruption. Legalization reduces the footprint of law enforcement in low-level cannabis offenses, thereby helping to address institutional disparities and promote equity. Several studies from states like Colorado and California have shown sharp declines in possession-related arrests following legalization, particularly among young Black and Hispanic men, suggesting that reform has tangible equity benefits (Sheehan et al., 2021).
States that have legalized recreational cannabis have seen substantial financial returns. For example, in 2022, legal cannabis sales generated over $3.7 billion in tax revenue across the U.S., with a significant portion allocated to public goods. In Colorado, more than $500 million has been directed toward education funding since legalization (MPP, 2023).
Legalization also allows for the implementation of standards to ensure product quality and consumer safety. Cannabis products sold in licensed dispensaries are routinely tested for THC and CBD potency, as well as for contaminants. Regulated testing significantly reduces the risks posed by illicit cannabis, which often lacks standardized dosing and may contain harmful adulterants (Paul, 2022). Legalization also enables data collection, which is critical for evidence-based policymaking and clinical guidance (CDC, 2025).
Despite regulation and the aforementioned benefits, recreational cannabis legalization carries significant drawbacks. Research indicates that even with age restrictions in place, states with legalized recreational use have experienced increased cannabis exposure among adolescents. While states have implemented age restrictions and public health campaigns, the effectiveness of these measures remains mixed, highlighting the need for continuous evaluation and improvement. This trend is concerning, given that early cannabis exposure has been linked to disruptions in brain maturation, particularly in regions related to memory, attention, and executive function. Long-term neurocognitive consequences—especially when use begins during adolescence—remain an area of active study, but current evidence suggests a potential for lasting cognitive impairment (NIDA, 2020).
Cannabis use disorder (CUD), now a recognized diagnosis, affects approximately 9-10% of users, with higher rates among daily or high-potency users (Hasin et al., 2015). Moreover, frequent cannabis use has been linked to the onset or worsening of psychiatric conditions, including anxiety, depression, and psychosis – especially in individuals with underlying vulnerabilities or genetic

predispositions. Clinicians should be aware of these associations when assessing mood and thought disorders in patients who report regular cannabis use (Hasin et al., 2015).
Tetrahydrocannabinol (THC), the primary psychoactive component of cannabis, has well-documented effects on reaction time, short-term memory, and motor coordination, all of which can compromise driving and occupational safety. However, THC can remain detectable in a person’s system for days to weeks depending on frequency of use, and unlike blood alcohol concentration (BAC), there is no accepted quantitative level that equates to impairment. This presents ongoing challenges for both law enforcement and workplace drug policies, as current testing methods cannot reliably differentiate between acute impairment and residual THC levels from prior use (Arkell et al., 2021).
Both recreational and medical cannabis legalization carry complex implications for individual and public health. As legalization efforts expand, physicians must play a proactive role in educating patients, shaping policy, and advocating for rigorous research and evidence-based regulation. The distinction between recreational and medical use is not always clear-cut, but the medical profession has a duty to support safe, informed, and compassionate use of cannabis when clinically appropriate. This needs to be done rationally, scientifically, and without emotion.
Evidence supports the use of medicinal cannabis for specific conditions, including chronic neuropathic pain, chemotherapyinduced nausea and vomiting, and spasticity associated with multiple sclerosis. In these cases, cannabis may offer symptom relief where conventional treatments fall short. There is little doubt that patients would benefit from physician involvement in guidance on product selection, dosing, route of administration, and monitoring for adverse effects or misuse. However, high-quality clinical evidence remains limited. The current body of research includes few highquality, randomized controlled trials, leaving clinicians to rely heavily on anecdotal reports and observational data (Whiting et al., 2015). The above notwithstanding, some observational studies suggest
that medical cannabis access may correlate with reduced opioid prescribing and opioid-related harms, though causality remains unproven and contested. Nonetheless, it would be disingenuous to overlook the potential role of legal medical cannabis as a therapeutic option for patients who have exhausted conventional therapies or for whom limited alternatives exist.
Unfortunately, in some jurisdictions, medical cannabis programs have been exploited as a proxy for recreational use, particularly where eligibility criteria are loosely defined or poorly enforced. When Pennsylvania’s medical cannabis law – Act 16 – was passed in April 2016, the law initially listed 17 qualifying medical conditions for eligibility (PA Dept. of Health, 2025). These included:
1. Amyotrophic lateral sclerosis (ALS)
2. Autism
3. Cancer
4. Crohn’s disease
5. Damage to the nervous tissue of the spinal cord
6. Epilepsy
7. Glaucoma
8. HIV/AIDS
9. Huntington’s disease
10. Inflammatory bowel disease
11. Intractable seizures
12. Multiple sclerosis
13. Neuropathies
14. Parkinson’s disease
15. Post-traumatic stress disorder (PTSD)
16. Severe chronic or intractable pain
17. Sickle cell anemia

continued on next page >
continued from page 29

Since its inception, Pennsylvania’s list of qualifying medical conditions for cannabis use has steadily expanded – a trend mirrored in other states. Notably, in 2019, the Pennsylvania Department of Health added Tourette’s syndrome to the list of qualifying conditions. Later, in 2022, chronic hepatitis was also included. Additional conditions – such as opioid use disorder and anxiety –were added in later years by the state’s Medical Marijuana Advisory Board and the Pennsylvania Department of Health (PA Dept. of Health, 2025). As of 2025, the state recognizes 24 serious medical conditions that make patients eligible for medical marijuana treatment.
These expansions are often driven by patient advocacy, political lobbying, and evolving public opinion. In some jurisdictions, eligibility criteria have become so broad that nearly anyone can qualify, raising legitimate questions about the purpose of maintaining a qualification system at all. Yet, cannabis remains classified as a Schedule I substance under federal law, a designation that restricts scientific research, complicates interstate commerce and prevents insurance coverage. As a result, patients are left to bear the full financial burden of treatment – further underscoring the need for policy reform grounded in evidence and equity. If medicinal cannabis is to be a viable process, this Schedule I classification must be reevaluated to enable broader clinical research and patient access.
As legalization efforts evolve, physicians are uniquely positioned to bridge the gap between public policy and patient care. We must champion rigorous research, advocate for sensible regulation, and ensure that patients receive accurate, compassionate, and clinically appropriate guidance. While the boundaries between medical and recreational use continue to blur, our responsibility is to promote better health and minimize harm through informed, evidence-based practice. History offers a useful reminder: alcohol is legal despite its well-documented harms, and the failure of Prohibition teaches us that blanket bans can yield unintended consequences. Even today, science continues to uncover the adverse health effects of alcohol – proof that legality does not equate to safety, and that ongoing scrutiny is essential.
In shaping policy and public understanding, we would do well to remember Aristotle’s enduring insight: “The law is reason, free from passion.” Let our contributions be guided not by ideology or emotion, but by clarity, integrity, and the unwavering pursuit of scientific truth.

References:
Marijuana Policy Project. (2023, May 1). States surpass $15 billion in tax revenue from legal, adult use cannabis sales. Retrieved from https://www.mpp. org/news/press/states-surpass-%2415-billion-in-tax-revenue-from-legal-adultuse-cannabis-sales/
Paul, S. (2022). A clinical framework for evaluating cannabis product quality and safety. PMCID PMC10249738. https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC10249738/
National Institute on Drug Abuse. (2020). Marijuana research report: What are marijuana’s long-term effects on the brain? National Institutes of Health. https:// nida.nih.gov/publications/research-reports/marijuana/what-are-marijuanaslong-term-effects-brain
Whiting, P. F., Wolff, R. F., Deshpande, S., Di Nisio, M., Duffy, S., Hernandez, A. V., … Westwood, M. (2015). Cannabinoids for medical use: A systematic review and meta-analysis. JAMA, 313(24), 2456–2473. https://doi. org/10.1001/jama.2015.6358
Arkell, T. R., Spindle, T. R., Kevin, R. C., Vandrey, R., & McGregor, I. S. (2021). The failings of per se limits to detect cannabis induced driving impairment: Results from a simulated driving study. Traffic Injury Prevention, 22(2), 102–107. https://doi.org/10.1080/15389588.2020.1851685
Association of Racial Disparity of Cannabis Possession Arrests Among Adults and Youths With Statewide Cannabis Decriminalization and Legalization. Brynn E. Sheehan, PhD; Richard A. Grucza, PhD; Andrew D. Plunk, PhD. JAMA Health Forum. 2021;2(10):e213435. https://doi:10.1001/ jamahealthforum.2021.3435
Centers for Disease Control and Prevention. (Accessed March 6, 2025). Cannabis: Facts and stats. https://www.cdc.gov/cannabis/facts-stats/index.html
American Civil Liberties Union. A tale of two countries: Racially targeted arrests in the era of marijuana reform. Published April 2020. Accessed [today’s date]. https://www.aclu.org/report/tale-two-countries-racially-targeted-arrests-eramarijuana-reform
Pennsylvania Department of Health. (2025). Medical Marijuana Program. Retrieved May 1, 2025, from https://www.pa.gov/agencies/health/programs/ medical-marijuana.html
Hasin, D. S., Saha, T. D., Kerridge, B. T., Goldstein, R. B., Chou, S. P., Zhang, H., ... & Grant, B. F. (2015). Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry, 72(12), 1235–1242. https://doi.org/10.1001/jamapsychiatry.2015.1858

by Amogh Nagol, MS lll, Drexel University College of Medicine
West
Reading Campus
still remember the first time I stepped into the operating room at Reading Hospital – the lights were bright, the air was cold, and my pulse felt louder than it should have. I was clumsy with my mask and even clumsier with putting on my gloves. But by the end of that case, something clicked. As I held the laparoscope in my hands, I wasn’t just observing, I was participating.
The third year of medical school has been a whirlwind, but nothing has challenged or transformed me like the surgery rotation. At Reading, the pace is fast, the expectations are high, and the learning is nonstop. I’ve scrubbed into laparoscopic cholecystectomies, assisted in hernia repairs, and helped close incisions after breast surgery. The anatomy I memorized in my first year of medical school was suddenly in front of me – pulsing, bleeding, and real.
But more than the procedures, what struck me most was this: these are REAL patients. Not standardized patients with scripts, checklists, and built-in teaching points. These are people with families, fears, and complications that don’t follow algorithms. The first time I stood at a bedside post-op and explained what happened in the OR – not as a simulation, but as part of the care team – it
felt like a milestone. I still remember the look on the patient’s face – the gratitude and relief that her surgery went well. I realized how different it is to earn a patient’s trust when the stakes are real.
That rotation also taught me lessons that go far beyond clinical knowledge. I learned to communicate with clarity under pressure, to anticipate the needs of the residents and attendings and to respect the quiet intensity that fills an OR. I saw firsthand how surgeons balance precision with compassion, and how much a patient’s recovery can depend on that balance.
This third year has tested my adaptability. Each rotation brings new teams, new workflows, and new expectations. But surgery has grounded me in a sense of purpose – reminding me why I chose this path in the first place. Even on the toughest days, there’s something deeply fulfilling about contributing, however small, to a patient’s healing.
As I move forward in medical training, I carry with me the lessons surgery etched into my hands and heart: presence matters, preparation saves lives, and real patients don’t come with checklists. They come with stories – and I’m grateful to be part of them.


As the 2025-2026 legislative session begins to come to an end, the legislative calendar has remained relatively light compared to previous years. This has been caused, in part, by the passing of a legislator in January, which resulted in a 101-101 tie in the House. Like last session, we have seen a strong partisan divide on votes, regardless of the bill under consideration. Now, as the Pennsylvania Legislature actively works on the 2025 State Budget, a surge of legislative activity is underway.

The Pennsylvania House passed House Bill 433, which would require health insurance policies to cover all costs associated with diagnostic breast imaging. The bill, introduced by Rep. Gina Curry (D-Delaware County), defines diagnostic imaging to include diagnostic mammography, breast MRI (standard or abbreviated), and breast ultrasound. Current Pennsylvania law already mandates insurance coverage for screening mammograms. House Bill 433 aims to expand this to follow-up imaging needed when abnormalities are detected. The bill awaits further consideration from the Senate.

House Bill 1200, a proposal to legalize cannabis for adult use in Pennsylvania, passed the House in a 102–101 vote. The bill allows adults age 21 and older to purchase cannabis through a stateregulated system. It includes provisions for personal cultivation, expungement of certain low-level marijuana convictions, and allocation of tax revenue to community programs. The bill was referred to the Senate Law and Justice Committee, where it did not advance out of committee following a vote on May 13.
PAMED has long been, and remains, opposed to broad-based use of cannabis as medicine. We support clinical research and trials evaluating the therapeutic use of cannabis and cannabis products, but do not believe the currently existing scientific evidence meets the standards for a prescription drug product. Regarding adult recreational use, PAMED supports the decriminalization of personal use but not full legalization. We believe continued research and monitoring of the public health effects of such use is necessary before making such a significant change.
As it relates to House Bill 1200, PAMED does not support legalization of adult use. However, we believe if legalization is pursued it must be accompanied by a robust regulatory framework that mitigates harm and promotes informed decision-making, such as the one outlined in HB 1200. Any state legalization should include requirements to regulate the products effectively to protect public health and safety. PAMED will continue to monitor the bill and its movement.
Introduced by Representative Lisa Borowski (D-Delaware), House Bill 1460 aims to strengthen oversight of major health care transactions involving private equity and large health systems. The bill requires advance approval from the Department of Health and the Attorney General, increases transparency, and limits saleleaseback arrangements.
PAMED supports HB 1460, aligning with its commitment to ensuring transparency and accountability in health care operations.
As of June 3, 2025, HB 1460 was reported as amended and received its first consideration in the House. It has since been recommitted to the House Rules Committee for further deliberation. PAMED will continue to monitor the status of HB 1460 as it advances through the legislative process.

Introduced by Representative Kristin Marcell (R-Bucks), House Bill 425 proposes creating a grant program to support J-1 visa physicians practicing in underserved areas. The program would allow for employers of physicians with a Conrad 30 waiver to apply for funding that would be intended to help cover physician salaries.
PAMED supports HB 425 as a strategic initiative to enhance access to primary care in underserved communities across Pennsylvania.
As of June 3, 2025, HB 425 was reported as amended and received its first consideration in the House. It has since been recommitted to the House Rules Committee for further deliberation. PAMED will continue to monitor the progression of HB 425 through the legislative process.
As we enter the end of this legislative session, PAMED continues to advocate for you and your patients.

JAN 1 - APRIL 1

Arjola Agoll, MD
Nagol Amogh
Muhammad Zain Ali, MD
Darius Argentinis
Megan Christine Barrett, DO
Brett Bentkowski, MD
Meha Bilkhu, MD
Raesham Bukhari, MD
Vincent Edmund DeVito, MD
Rohan Dhamsania, DO
Justice Dove, DO
Laurel Finson, MD
Sam Jedd, MD
Madhavi Devi Kakarlapudi, MD
Jade Kerr, DO
Fatima Khalid, MD
Alexander Abraham Kuruvilla, MD
Jason William Leonardo, DO
Zachary Louis Nobile, DO
Osadebamwen Winifred Osaghae, MD
Prakash Patel, DO
Thayjas Patil, MD

Berks County Medical Society:
Bailey Arias Pechner, DO
Udit Roy, MD
Pallab Sarker, MD
Alexander Keith Smaniotto, DO
Anastasia Smirnoff
Jesly Solaman, DO
Emily Tran, DO
Jami Truong Van Landingham, MD
Divya Venkat, DO
Kevin Scott Viera, MD


BCMS Night at the Reading Fightin’ Phils
Picnic for New Physicians/Residents/Students
Game tickets available for all BCMS members and families
Thursday, August 14th 6:00 PM
FirstEnergy Stadium
1824 Journal Club Fall 2025 (Topics)
1-“COVID-19 Review: Lessons Learned”
2-“2024-25 Specialty Literature Review”
Wednesday, October 15th 6:00-8:00 PM
The Highlands, 2000 Cambridge Ave., Wyomissing












At MADJ, we specialize in helping medical practices and health systems of all sizes thrive in competitive landscapes. From small beginnings to significant success, our tailored strategies have transformed healthcare providers into community cornerstones.
Glaucoma
Diabetic Eye Exams
Macular Degeneration
Yes, we can see your patients same day for emergencies and often same week for consults.
At BERKS EYE PHYSICIANS AND SURGEONS, we are happy to offer state-of-the-art and efficient care. Our doctors provide appropriate diagnosis and treatment, and fast feedback to you. Whether your patient has a sudden change in vision, cataracts, diabetes impacting vision, or even has a family history of glaucoma or macular degeneration, we would be honored to monitor and react to issues related to your patient’s eye health.