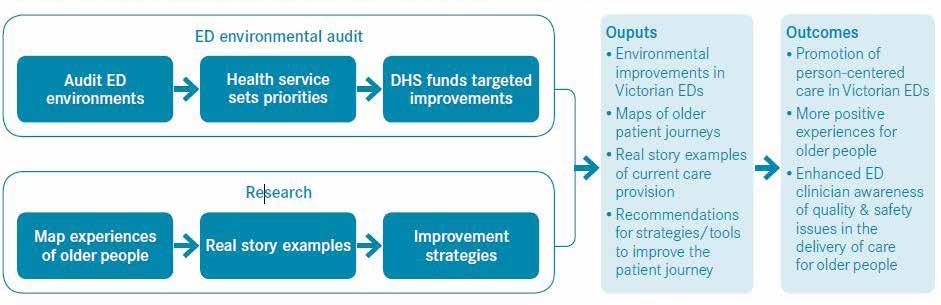
CASE STUDY 02: OLDER PEOPLE Australia’s aging population is a significant challenge across the health system and is recognised as having a disproportionate effect on EDs. Older people require emergency care more often than other populations, as well as experiencing longer lengths of stay and higher admission/readmission rates. The rapid triage and care process of EDs is often inadequate to manage the needs of older people with multiple medical conditions, a long list of medicines, communication challenges, and slowly evolving problems that impair effective understanding of the patient’s current need (Adams, 2003). The appropriate care for older people needs to be integrated into the design of EDs. Functional decline reduces the ability for some older people to navigate the physical environment, communicate effectively, and maintain a level of independence in EDs (Fisk, A, Rogers, W, Charness, N, Czaja, S & Sharit, J, 2004, as cited in State Government of Victoria, 2009). A 2008 initiative by Victoria Health focused on improving the experiences of older people in ED as part of a broader Patient Experience Program. An environmental audit of 21 major hospitals was used to identify and fund high priority items necessary to create more ‘older person friendly’ hospital environments (State Government of Victoria, 2009, p6). This audit revealed that there was a range of simple physical changes that could make considerable difference to older
10
ENVISION WELLNESS Acute Health Design
patients. Supporting sensory and physical impairment with mobility aids; volume-adjustable phones; improved lighting, signage and visual contrast supported better patient experiences. The opportunity for clinicians to be involved in the audit also increased their awareness and understanding of the issues experienced by older people. In 2013, the Aged Care Emergency (ACE) model of care was developed by the Emergency Care Institute NSW. The ACE Service model aims to support RACF staff to better manage residents experiencing acute onset symptoms within their facilities and avoid unnecessary transfer to ED. This includes providing telephone triage, and educational support for RACF. A collaborative working relationship between GPs, the community, RACFs and hospital care providers is required to ensure strong care continuity and case management. Medical Assessment Units (MAU) have been established as an ED model of care in NSW since 2008. They are intended as inpatient short stay units co-located with emergency to provide care for the elderly, as well as those with chronic conditions, and as an alternative to treatment in ED. These services can deliver reductions in length-of-stay and waiting times for transfers to medical beds. Direct referral to MAU can improve a hospital’s ability to manage patient flow and reduce the number of complex non-critical medical patients presenting to ED (ACI, 2014). These services
provide specialist care to adults, and especially older people, who have a chronic and/or complex condition, or issues that may take time to assess and require a range of clinical expertise to diagnoses and treat. Westmead Hospital in Western Sydney has developed a comprehensive model for aged care within hospital settings which has expanded over more than 10 years. A particular focus on ED streaming has led to innovations in the models of care. In 2005, the Older Persons Review and Assessment (OPERA) Unit was established as a patient-centred short stay unit. In 2008, Health Care for Older Persons Earlier (HOPE) strategy was established to better manage the increasing numbers of older people presenting at hospitals and reduce access block in emergency. A small rapid assessment unit known as HOPE_ED is located within the emergency apartment, providing initial assessment and treatment within 4-8 hours. Patients are then transferred to the HOPE/OPERA unit which provides a ward-based medical unit and allied health unit along with cardiac monitoring. Specialist assessment and management plan development occurs over 24-72 hours. The design of these units is focused around the specific needs of older patients including; delirium management, wandering patients, frailty and risk of falls, and the ‘trauma of admission’ (Loh, 2017). The HOPE/OPERA strategy is able to provide better specialist care within comprehensive aged care service;