2 minute read
Conclusion
The growing use of EDs as diagnostic centers warrants further scrutiny to determine if this is the most clinically and economically efficient way to evaluate complex patients with worrisome symptoms. (Morganti, Bahuoff, Blanchard, Abir, Smith, Vesely, Okeke, Kellerman, Iyer, 2013).
Demand for emergency medicine continues to grow, and increased services are required to cater for a wide range of population groups, ages and specialisms. However the causes for increased presentations should be critically examined as part of the whole health system and future trends.
Advertisement
The Royal College of Physicians (RCP), NHS Confederation, Society for Acute Medicine and the College of Emergency Medicine in the U.K. outlined a vision in 2013 for the future of urgent and emergency care services. The challenges faced by EDs was reviewed and recommendations for action were outlined across the health network. Effective and simplified alternatives to hospital admission and emergency presentation were recommended. This includes 7-day services which provide hospital admission and discharge, consultation services and ambulatory care. This action plan highlights the need for the whole U.K. health system to support reductions in unscheduled care. Public health, preventative strategies and
improved access to information were highlighted as important aspects to ensure that patients have a clear understanding of services, as well as pathways to obtaining diagnosis and treatment. These recommendations identify current concerns that rising demand for emergency services cannot be met by simply increasing size, capacity and number of EDs within health networks.
EDs started off as treatment rooms for assessment and stabilisation of unplanned or unexpected cases. However, the unique challenge of emergency medicine has encouraged the evolution of new models of care and clinical specialisms. Over time, EDs have become the first point of entry for an extremely broad spectrum of care needs from ambulatory urgent care, to complex and chronic illness. The wide range of needs has driven demand for a wide range of diagnostic services, pharmacy, treatment and specialist care and nursing. Today, EDs demand collocation and proximity to nearly every aspect of acute care. In hospital planning and design, the centre of gravity almost always lies close to the ED along with the surgery and treatment spaces.
Collocation and adjacency of support services becomes difficult as physical space requirements increase. Travel distances also rise with the introduction of specialist streams for children, older people, behavioural health, medical/surgical assessment, and urgent care. What has traditionally
been a single department in a local hospital will evolve to become a large network of services in a major metropolitan context. A decentralised but networked approach has the potential to provide better customisation to support the range of patient needs. This should be reflected in building designs which provide connectivity and flexibility, as well as opportunities for future growth and adaptive spaces.
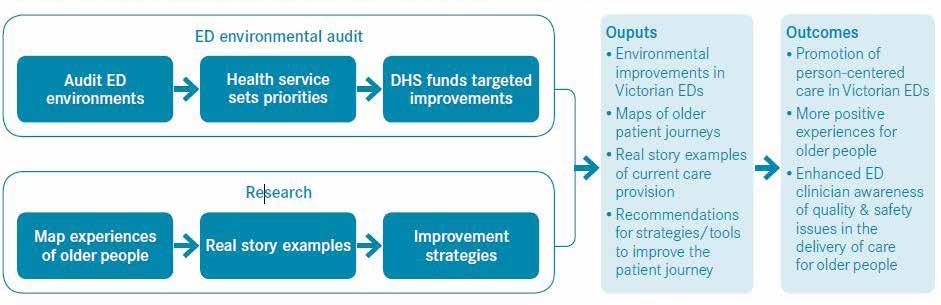
For patients, a timely response, with accurate assessment and diagnosis, and clear pathways for care are major concerns when accessing emergency care. The triage, registration and coordination of patients is critical to ensuring integrated care throughout the patient journey. The experience of people should remain at the centre of the design challenge for EDs. A humanistic and supportive environment should be the first priority, regardless of the situation or context.
To address the challenges faced by urgent and emergency care services, we must change the way we deliver and organise care across the whole system. (Royal College of Physicians, NHS Confederation, Society for Acute Medicine and The College of Emergency Medicine, 2013).