7 minute read
Case Study 04: Patient Stress & Wayfinding
Understanding the patient perspective and designing patient flows to accommodate for the wide range of presentations is vital in providing the right care, at the right time, and in the right place. Following a near fatal shooting of a police officer and security guard at Nepean Hospital Emergency Department in January 2016, a review of ED security was commissioned by NSW Health. This review led to a 12 point action plan established by auditors along with recommendations to NSW Health. The report includes a focus on the safety and security of workplaces, funding for security upgrades and ongoing auditing of facilities (NSW Minister for Health, 2016).
Wayfinding, guidance and training can be used to reduce incidents of violence and aggression in EDs. “A Better A&E” is a design solution developed by PearsonLloyd for The Design Council UK and 3 partner NHS Trusts to provide a cost-effective method of reducing violence in emergency. The design solution successfully reduced hostility, as well as providing social and economic return, with monetised benefits outweighing costs 3 to 1. (Frontier Economics, 2013, p6).
Advertisement
Negative patient experiences often cause operational problems and workplace stress in EDs. Studies have shown that there are common psychological principles that apply to the ‘waiting experience’. Understanding and managing these waiting patients appropriately can help to reduce anxiety and frustration of patients
and carers (NSW Health, 2011, p7). For example, an ED model of care which incorporates a Clinical Initiatives Nurse is recommended by NSW Health (2012 (1) , p15) to maintain a nurse presence in the waiting room, as well as supporting and streamlining the triage process. This approach supports nurse-initiated interventions such as ordering diagnostics and administering pain-relief.
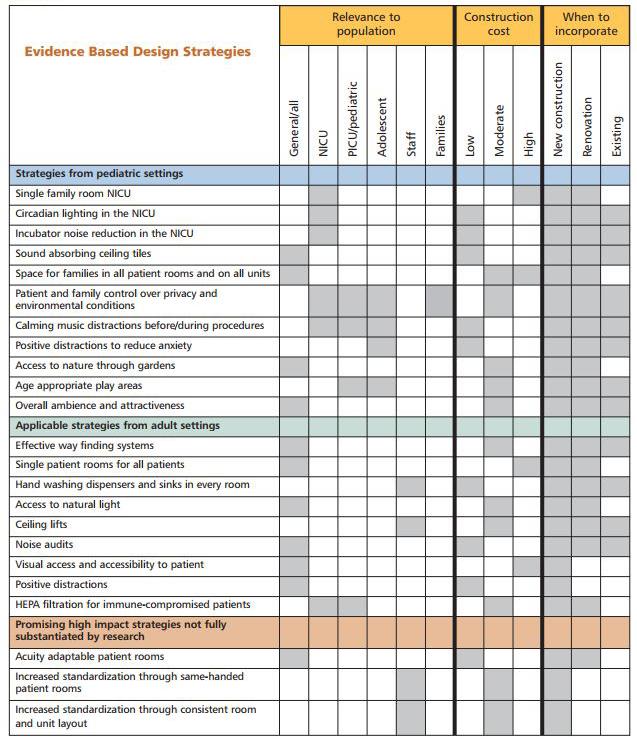
The physical design of healthcare spaces has transformed in many ways to become more welcoming and inviting, with a renewed focus on light and sound attenuation, positive distraction and access to useful information (Suchomel, 2016). In new Kaiser Permanente health hubs, reception areas are designed as public ‘mall’ with indoor, outdoor spaces, health monitoring stations, and a staffed ‘Thrive Bar’ where patients can access advice on nutrition, exercise and other wellness issues while they wait (Bluestein, 2016). This approach supports Ulrich’s (1991) theory of supportive design for healthcare facilities, which focuses on patient wellbeing and alleviation of stress to provide a sense of control, positive distraction and social support.
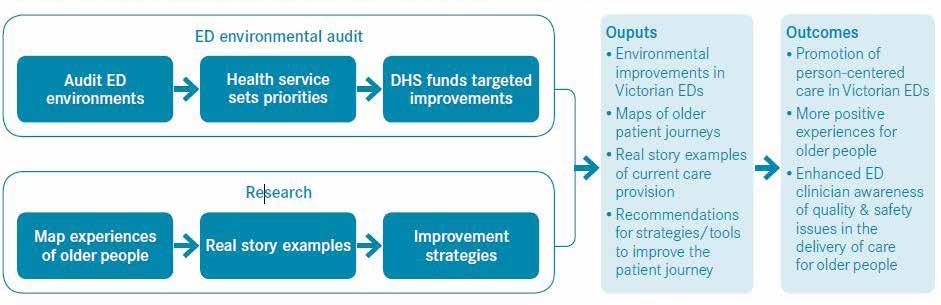
In 2011 the UK Design Council in collaboration with the UK Department of Health sought to deal with the ever increasing numbers of attendances at Accident and Emergency (A&E) departments in England and the negative experiences of staff and patients. The intention was to use design to alleviate tensions, and ultimately to reduce
violence and aggression. A multi-dis ciplinary design team led by Pearson Lloyd worked with the Design Council and 3 partner NHS Trusts to develop a set of design solutions and an online design kit to provide recommenda tions to NHS Trusts. An evaluation and findings report was conducted by Frontier Economics to review the outcome of the project.
Frontier Economics (2013, p16) and ESRO research agency conducted pre liminary research to identify triggers of violence and aggression such as:
Clash of people: Many areas in ED departments are crowded with a range of different people, forced together by difficult circumstances – each under going their own stresses and dealing with their own complex mix of clinical and non-clinical needs. Lack of progression: While all Trusts aim to treat 95% of patients within 4 hours, waiting for any length of time can be a difficult experience. There are few situations in our lives when we are forced to wait for such lengths of time without any sense of progression.
Inhospitable environments: Many people describe a dislike of hospitals, not least because they are full of sick people. Beyond the patients, hospitals can be uncomfortable places which are not pleasant to spend time in.
Dehumanising environments: When arriving at ED people can feel ‘out of sorts’ or in a negative mood. Sometimes the way patients are managed can further lead to a loss of perspective.
“Patient stress has a variety of negative psychological, physiological, and often behavioural manifestations that work against wellness.” (Ulrich, R. 1991, p98).
Fig. 2 Fig. 1
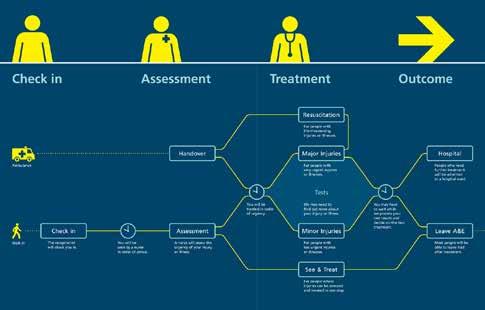
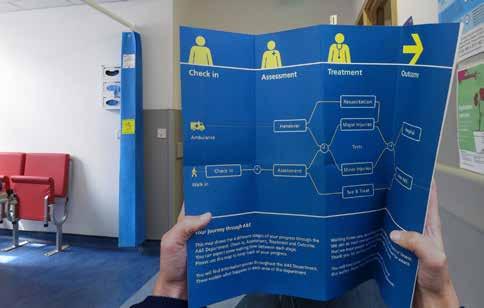
Fig. 3
16. Patient Flow Diagram indicating models of care. “A Better A&E”, 2017. 17. Bed-side signage aligning with Patient Flow Diagram . Ibid. 18. Printed Material available to patients and visitors. Ibid.
Intense emotions: ED is a place where people may be experiencing extreme life events, suffering with pain or stress, or having to witness how other people are coping (or not) with their own stressful experiences.
Unsafe environments: ED is typically a very busy environment, with considerable amounts of equipment and large numbers of people using the space. Sometimes these factors can help to trigger or worsen violence and aggression. Perceived inefficiency: From a patient’s perspective it can sometimes feel as if staff in ED environments are disorganised and lacking focus. Patients observe themselves and others seemingly waiting for hours, while staff ‘busy themselves’ with perceived non-essential tasks.
Inconsistent response: Hospital environments are often tightly controlled by policies, guidance, rules and regulations, much of which is difficult to decipher, inconsistently applied, and can be contrary to what happens in practice.
Staff fatigue: Working in an ED department is highly demanding on staff, many of whom work 12-hour shifts. Over time, staff can become both physically and emotionally tired, struggling to find the energy to deal with the constant flow of patients. A model for the ideal patient journey was developed comprising of 4 stages of the user experience: Arrival, Wait, Treatment and Outcome. In each phase, the design team explored impact of positive interaction and clarity, with an emphasis on keeping patients informed and up-to-date throughout their visit to emergency.
The ‘Guidance Project’ was implemented to provide information to patients and visitors including a process map, wayfinding signage, patient leaflets and live digital information. The process map is the central tool used to inform patients and help them understand what their patient journey might look like. Signage throughout the department was linked back to the process map to help patients understand where they were in their journey. Screens installed in waiting areas provided live digital information such as the number of patients in each area of the department, expected wait time and department operational status. This offered patients a better understanding of the reasons they were being asked to wait.
Human contact and compassion was also identified as an effective way to support patient experiences, however ED staff are often working under intense stress and time pressure. This can lead to fatigue, low morale and poorer care outcomes. The ‘People Project’ was developed to improve emergency staff skills in working under pressure and managing potentially aggressive patients whilst maintaining empathy. The primary aim was to promote staff engagement, boost morale, and support staff who
may deal with potentially aggressive and violent patients. Staff facilitators were appointed and trained in trial sites and a department engagement programme was developed. Staff discussed personal experiences, identified trends in the nature of incidents and when incidents were likely to happen. Data was collected to improve understanding of when, how and why violent and aggressive incidents occurred, and how these could be better managed. The Project opened a dialogue around key operational issues affecting staff and emphasised the need for design solutions to be sufficiently flexible to support the specific needs of individual departments.
The results of the ‘Guidance’ and ‘People’ projects were collated and published in the form of a design toolkit to support implementation in other hospitals. The research and knowledge collected in this report represents a valuable tool for EDs around the world. The design solution provided a cost-effective retro-fit approach which delivered improvements in patient experience and reduction in aggressive incidents. This approach could be utilised in other health districts around Australia. The NSW Health ED streaming approach to models of care in ED could form the basis of a patient flow diagram for NSW EDs tailored to individual services.
Waiting in ignorance creates a feeling of powerlessness, which frequently results in visible irritation and rudeness. (Maister, 2005, p6).
Fig. 4


Fig. 6

19. Ideal Patient Journey with streaming to models of care. NSW Health, 2012. 20. Waiting Room Digital Information. “A Better A&E”, 2017. 21. Installing Ceiling signage above beds. Ibid.