ORTHO connection
Increasing airway volume with a removable orthodontic dental appliance: a multi-case report by Theodore R. Belfor, DDS, Michael Philcock, and Scott Simonetti, DDS Introduction
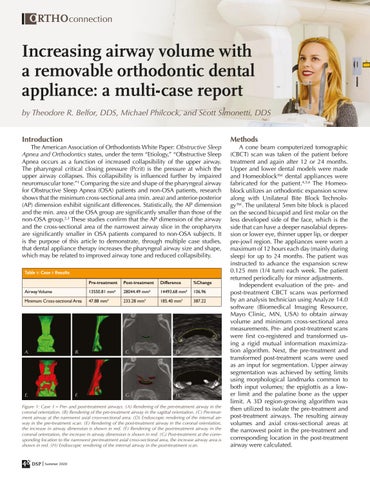
The American Association of Orthodontists White Paper: Obstructive Sleep Apnea and Orthodontics states, under the term “Etiology,” “Obstructive Sleep Apnea occurs as a function of increased collapsibility of the upper airway. The pharyngeal critical closing pressure (Pcrit) is the pressure at which the upper airway collapses. This collapsibility is influenced further by impaired neuromuscular tone.”1 Comparing the size and shape of the pharyngeal airway for Obstructive Sleep Apnea (OSA) patients and non-OSA patients, research shows that the minimum cross-sectional area (min. area) and anterior-posterior (AP) dimension exhibit significant differences. Statistically, the AP dimension and the min. area of the OSA group are significantly smaller than those of the non-OSA group.2,3 These studies confirm that the AP dimension of the airway and the cross-sectional area of the narrowest airway slice in the oropharynx are significantly smaller in OSA patients compared to non-OSA subjects. It is the purpose of this article to demonstrate, through multiple case studies, that dental appliance therapy increases the pharyngeal airway size and shape, which may be related to improved airway tone and reduced collapsibility. Table 1: Case 1 Results Pre-treatment
Post-treatment
Difference
%Change
Airway Volume
13550.81 mm3
28044.49 mm3
14493.68 mm3
106.96
Minimum Cross-sectional Area
47.88 mm2
233.28 mm2
185.40 mm2
387.22
A.
B.
C.
D.
E.
F.
G.
H.
Figure 1: Case 1 – Pre- and post-treatment airways. (A) Rendering of the pre-treatment airway in the coronal orientation. (B) Rendering of the pre-treatment airway in the sagittal orientation. (C) Pre-treatment airway at the narrowest axial cross-sectional area. (D) Endoscopic rendering of the internal airway in the pre-treatment scan. (E) Rendering of the post-treatment airway in the coronal orientation, the increase in airway dimension is shown in red. (F) Rendering of the post-treatment airway in the coronal orientation, the increase in airway dimension is shown in red. (G) Post-treatment at the corresponding location to the narrowest pre-treatment axial cross-sectional area, the increase airway area is shown in red. (H) Endoscopic rendering of the internal airway in the post-treatment scan.
48 DSP | Summer 2020
Methods
A cone beam computerized tomographic (CBCT) scan was taken of the patient before treatment and again after 12 or 24 months. Upper and lower dental models were made and Homeoblock™ dental appliances were fabricated for the patient.4,5,6 The Homeoblock utilizes an orthodontic expansion screw along with Unilateral Bite Block Technology™. The unilateral 5mm bite block is placed on the second bicuspid and first molar on the less developed side of the face, which is the side that can have a deeper nasolabial depression or lower eye, thinner upper lip, or deeper pre-jowl region. The appliances were worn a maximum of 12 hours each day (mainly during sleep) for up to 24 months. The patient was instructed to advance the expansion screw 0.125 mm (1/4 turn) each week. The patient returned periodically for minor adjustments. Independent evaluation of the pre- and post-treatment CBCT scans was performed by an analysis technician using Analyze 14.0 software (Biomedical Imaging Resource, Mayo Clinic, MN, USA) to obtain airway volume and minimum cross-sectional area measurements. Pre- and post-treatment scans were first co-registered and transformed using a rigid mutual information maximization algorithm. Next, the pre-treatment and transformed post-treatment scans were used as an input for segmentation. Upper airway segmentation was achieved by setting limits using morphological landmarks common to both input volumes; the epiglottis as a lower limit and the palatine bone as the upper limit. A 3D region-growing algorithm was then utilized to isolate the pre-treatment and post-treatment airways. The resulting airway volumes and axial cross-sectional areas at the narrowest point in the pre-treatment and corresponding location in the post-treatment airway were calculated.