


















Fitting mandibular advancement devices to teeth is easy. Manufacturers have fine-tuned their process, many dentists use digital submissions, and the quality of materials has improved to provide confidence for every delivery appointment. Years ago, I maintained to learners in lectures that the devices are not the hard part. True then, truer now.
Dental Sleep Practice magazine was created in a time where dentists needed to hear that treatment was ‘easy’ and the rewards worthy of the work needed to achieve competence.
The treatment of sleep breathing disorders, which is only about 25 years older than this magazine, has evolved as science provides more insight into the impact on human health from physiologic disruption every night for years and decades. Medicine understands acute impact, which produces symptoms, very well. What is becoming more appreciated is chronic impact that results in degradation of allostatic capacity to the point where body systems cannot return to a stable, homeostatic state. It’s like a stone wall that can withstand a storm but is undermined by a slow steady stream eating away at the foundation.
A dentist encountering a patient diagnosed with SRBD has the opportunity to treat the acute impact – perhaps they should consider that their top priority. Some training programs and many dentists consider that their only obligation. Dentists who choose not to think about the chronic impact provide a limited service, leaving the bigger picture to the overburdened physicians on the patients’ health care team.
This is a legally defensible, staying-inyour-lane way of practicing medicine, but does little to engage every possible means of improving community health. Addressing the bigger picture means every member of the health care team must look beyond their comfort zone to see where else they can contribute. To improve our effect on
chronic impact, we must reduce fear of coloring outside our lines while maintaining good medical decision-making. That mandates dentists to learn more about what is in the ADA definition of our scope of practice, including ‘adjacent and associated structures and their impact on the rest of the human body.’ The American Dental Association hosts its second Wellness Conference in 2025; the Children’s Airway Initiative is in its 8th year of work to provide opportunities for dentists to learn about physiologic changes of chronic impact. Podcasts and webinars host guests from across the medical spectrum to showcase aspects of medicine that add to understanding of the interconnected and inseparable functions of the human organism.
Dentists reading this should ask themselves, or even better, write down so you can see it in front of you, how much time they have spent in the last month, quarter, or year learning about more than traditional dental skills or mandibular advancement devices. Have you studied how proper development of the craniofacial respiratory complex in early life impacts brain health? How breathing patterns can impact loop gain or arousal threshold? Why the FDA approved a blood sugar regulatory drug for treatment of comorbid sleep apnea? There is no limit on what’s out there to be learned, but don’t get stuck by not knowing where to start, or what’s next. Carry on, and go deep.
Dr. L.D. Pankey is famous for his wise statements. One I’ve recently embraced is ‘Take the next step now. The horizon will take care of itself’.

Steve Carstensen, DDS Diplomate, American Board of Dental Sleep Medicine

See Dr. Carstensen at the Northern Virginia Dental Society on June 6, 2025 in Arlington, Virginia... or at the ADA Children’s Airway Initiative from July 24-26 in Chicago, Illinois.

Cover Story
Lessons Learned and Lives Changed 3 Mistakes to Avoid When Launching a Dental Sleep Medicine Practice


Continuing Education Malocclusion and Sleep Related Breathing Disorders in Early Childhood, 1880-2025 by
Kevin Boyd, DDS, MSc
Life effects of poor early breathing are profound and preventable.


2 CE CREDITS
Special Section
Visit with these innovative companies at the AADSM.

Medical Insight Review of REM Sleep: Part Two – Pathophysiology by Amalia
A. Geller, MD
A review of the fascinating pathophysiology of REM Behavior Disorder.

Medical Insight Zepbound: The First FDA Approved Medication for Obstructive Sleep Apnea by Jyotsna Sahni, MD
Zepbound has shaken up the OSA community, read why.









6 Publisher’s Perspective Beating Burnout by Lisa Moler, Founder/CEO, MedMark Media
12 Communication Corner “OUT OF BREATH” by Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB
Sharing stories of real life impact in the first movie about sleep apnea.

14 Cardio-Sleep Corner Effects of Sleep Deprivation on Your Body by Lee A. Surkin, MD, FACC, FCCP, FASNC, FAASM
What happens when you lack sufficient sleep.
16 Product Spotlight Ease Your Mind with BioMatch: Advancing Sleep Apnea Treatment
Making DSM more predictable.
36 Product Spotlight VirtuOx Introduces Sleepifi DENTAL: Revolutionizing the Dental Sleep Medicine Workflow
Technology improves every sleep practice.

38 Product Spotlight The Future of Sleep Apnea Treatment: How the Advanced Titration Arm from DynaFlex is Revolutionizing Herbst Devices
Cutting edge manufacturing partner leads the way.

39 Communication Corner Why Your Consults Fail by Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB
Simple steps to improve office success.
40 Seek and Sleep DSP Codeword
Summer 2025
Publisher | Lisa Moler lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Jamila Battle, MD (Family/Sleep/Addiction)
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Saim Choudhry, DO (Internal Medicine, Sleep)
Alison Kole, MD, MPH, FCCP, FAASM (Sleep, Pulmonary, Critical Care)
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Bertrand de Silva, MD, FCCP, D.ABSM
Daniel Gartenberg, PhD (Behavioral Sleep)
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Steve Lamberg, DDS, D.ABDSM
Ian Lalich, MD (ENT, Sleep)
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD

National Account Manager
Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media
Felicia Vaughn | felicia@medmarkmedia.com
Website Support
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC
400 Crossing Blvd. Bridgewater, NJ 08807
Tel: (480) 621-8955
www.DentalSleepPractice.com
Subscription Rate: 1 year (4 issues) $149
• Advanced Education with Mini MBA Program and Other Advanced Certificates in Business Management and Leadership
• Retention Strategies
• Operational Support
• Technology Implementation
• Patient Trends & Analytics
• Efficiency Audit
• Competitive Fee Survey
• Production Analysis




Lisa Moler Founder/CEO, MedMark Media
The ADA cites that “more than 82% of dentists report feeling major stress about their careers.” In this very competitive and quickly changing world, the responsibilities can often feel like the walls of the office are closing in. Recognizing burnout symptoms and taking steps to calm your emotions can make a huge difference.
First, what does burnout feel like? Just a few signs are:
• Feeling tired, emotionally drained, or unenthusiastic
• Often feeling frustration toward work
• Negative outlook
• Problems concentrating
• Getting sick often
It is important to recognize and treat burnout to avoid issues such as heart disease and diabetes, sleep-related disorders, and in some cases, substance misuse.
Some Ways to Overcome Burnout
Get enough sleep: We’ve all had our nights of staring at the ceiling in bed while mulling over Plan A, Plan B, Plan C, and more, to solve the next day’s problems. Try to break your non-sleeping cycle. For example, ask your doctor about a possible supplement to lull your brain into the sleep cycle, or discover new relaxation techniques.
Detox from technology: Set specific technology-free windows where patient management systems and email notifications are completely turned off.
Eat and drink for health: Remembering to eat and keeping hydrated helps your brain function (improves memory, attention, and problem solving), raises your mood, and boosts your mental abilities.
Exercise: Exercising has been proven to help fight depression. It doesn’t have to take up much time – about 15-20 minutes per day should do it. A walk along a favorite path, around your neighborhood, on the beach, or even doing yoga or stretching can give your mind some time to reset.
There is nothing better than finding out that others can empathize with you and confirm that you are not “crazy.” Colleagues can tell you how they have navigated through similar times of burnout, or give some helpful tips, like reduced hours on Fridays or more intentional spacing of appointments. Look for summer dental retreats or workshops that combine professional development with wellness activities. Aside from work, friends or family can just listen, provide some good advice, or go along on that walk or for a quick cup of coffee and a shoulder to lean on. Finding a therapist can also be very helpful in working out your feelings and providing anti-anxiety techniques.
Give yourself a break: When you feel that burnout starting to eat away at your stomach lining, decide how you will take care of yourself at that moment. Take a few seconds. Grab your journal, and write a few lines. Go outside of the office and breathe some fresh air or look at the scenery. Research shows even 20 minutes of nature exposure significantly reduces cortisol levels. For more extreme situations, taking one day or a few days off, or a more extended vacation can bring you back with renewed spirits.
The ADA has some interesting resources just for dentists on its Wellness Resources page (https://www.ada.org/resources/practice/wellness) to help you start dealing with burnout. You can’t always control what happens in your office, but you can control the way you cope, put out those every day inner fires, and move forward to a fulfilling future with a positive outlook.















































































































For Dr. Anjoo Ely, dentistry has always been about more than the general practice, but rather, making a difference and changing peoples’ lives. Since graduating from the University of Michigan in 1997, she has dedicated herself to patient care, but it wasn’t until she discovered dental sleep medicine that she found her true calling.
Her journey into this field was both professional and personal. A 2013 continuing education course on sleep apnea, hosted by Nierman Practice Management, opened her eyes to the dangers of obstructive sleep apnea (OSA).
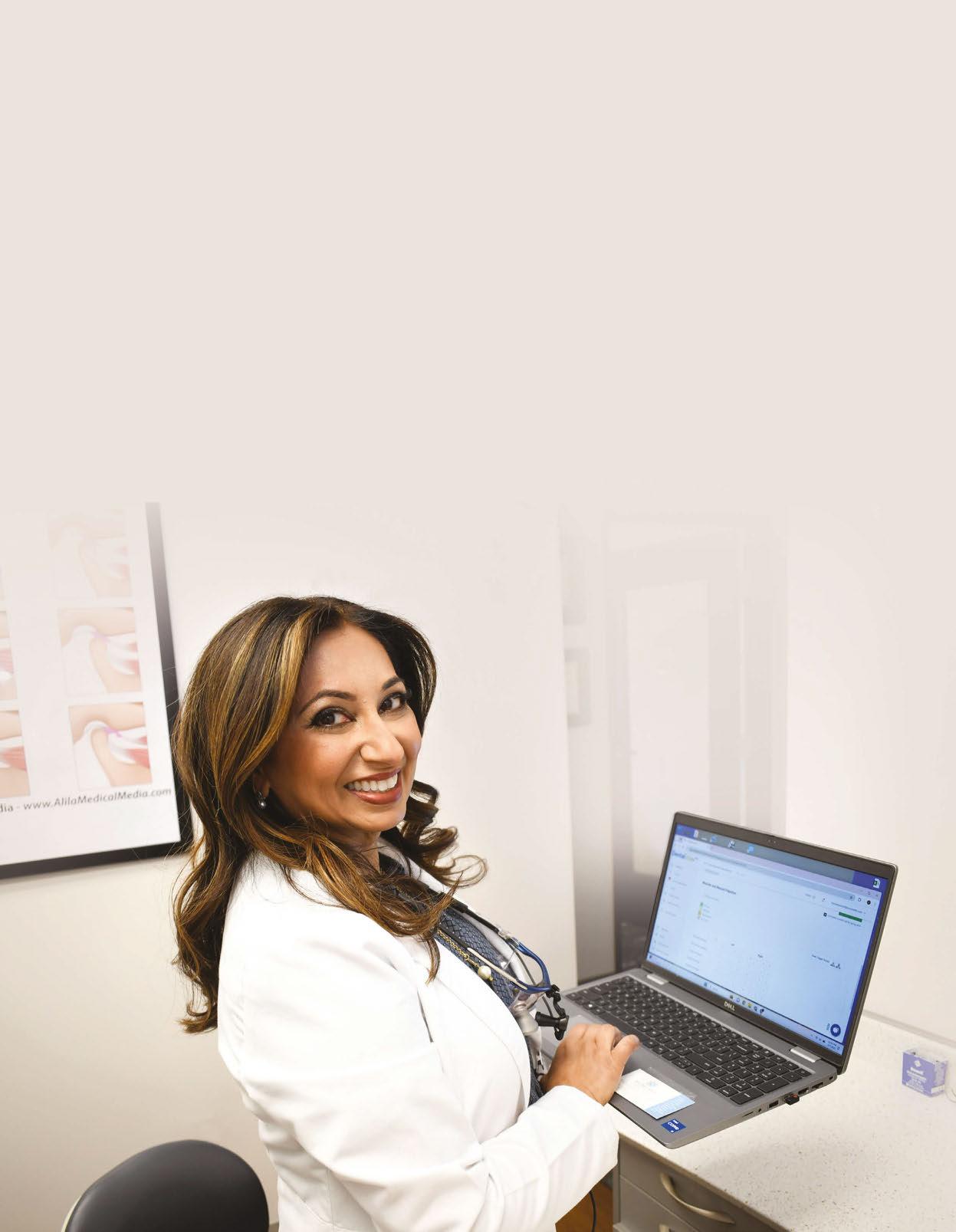
Through that course, she started to think about the symptoms her late father was exhibiting. Looking back, she now believes her father, who ending up passing away at the age of 54, was a victim of undiagnosed sleep apnea.
“He snored loudly, choked, and gasped in his sleep. But back then, sleep apnea wasn’t even a recognized disease,” Dr. Anjoo Ely recalls.
This realization fueled a new mission in her career: to help others identify and treat sleep disorders before it was too late.
Today, her practice is one of the most successful dental sleep practices in the country, with roughly 70% of her practice devoted to sleep patients, but the road to success wasn’t without its challenges. Here, Dr. Ely shares three mistakes dentists make when launching a dental sleep practice – and strategies you can implement to avoid hurdles.
Problem: Many dentists struggle to get their teams on board with dental sleep medicine. Without a team that understands and believes in the value of sleep apnea treatment, implementation can feel like an uphill battle.
Solution: Dr. Ely knew she needed her team to be just as passionate as she was. Instead of simply training them on protocols, she made it personal. She encouraged team members to think about their own family members who might have sleep apnea and got them evaluated. When they saw firsthand how treatment transformed the lives of their loved ones, it ignited their passion.
By aligning her team around a shared mission, Dr. Ely created an environment where the dental sleep medicine workflow became second nature.
“By the time I come into the room, my hygienists have already planted the seeds about airway issues,” she explains. “They are welleducated and can begin the conversation, which makes my job easier.”
Dr. Ely says without a team that understands and supports dental sleep medicine, dentists could be faced with struggles to get patients engaged in the discussion and willing to move forward with treatment. That’s why building a strong culture around dental sleep medicine is key.
“It’s not necessarily me asking all the questions – it’s about reassuring what my hygienist has already suggested. When patients feel that multiple team members are knowledgeable and concerned about their sleep health, they become much more receptive,” Dr. Ely said.
Investing in team education and ensuring that everyone understands their role in the process can significantly improve patient acceptance rates.
Problem: Unlike general dentistry, dental sleep medicine relies heavily on physician collaboration. Many dentists struggle to gain referrals from medical professionals, limiting their patient flow and discouraging them from staying in the sleep field.
Solution: Dr. Ely took a proactive approach. Instead of waiting for referrals, she built relationships with local physicians by positioning herself as an expert, sending narrative reports, and setting up in-person meetings.
Included in her recommendations is creating a dedicated sleep brand. Having a separate website just for sleep, distinct from your general dentistry site, helps establish credibility and makes it easier for patients and referring doctors to find you.
“You have to be willing to put yourself out there. You have to be willing to knock on doors





A. Dr. Ely with her team.
B. Dr. Ely showing an appliance to a patient.
C. Dr. Ely speaking at an event.
D. Dr. Ely teaching.
E. Dr. Ely with the Michigan Academy of Sleep Medicine.








and shake hands with physicians,” Dr. Ely said. “When I opened my general practice, the endodontist and oral surgeon who personally introduced themselves to me are still the ones I refer to today. That experience taught me that if I want to succeed in sleep medicine, I need to do the same.”
Dr. Ely explains she had success with dropping research packets off to local physicians to break the ice before setting up lunch-and-learns and other meetings.
“So, if I want to try and get to meet, say, a primary care physician, I might drop off a couple of articles about sleep apnea, blood pressure, something that’s in their wheelhouse to get their attention, and then try and get a meeting with that doctor.”
But beyond in-person meetings, Dr. Ely emphasizes the power of narrative reports as a marketing tool for staying in front of physicians and generating referrals. Dr. Ely says sending narrative SOAP reports to mutual providers has kept her name in front of them and has allowed her to maintain a steady flow of referrals.
“I get referrals every day from doctors that I say, well, who is this? And I realize, oh, yeah, there’s somebody that I sent a letter to because they’re in my database in DentalWriter. Now here they are sending me a patient. I didn’t do anything to woo them into referring them to me, but they’ve seen my name, and they know that I treated another one of their patients and now know what I do.”

Having a repeatable system, Dr. Ely says, is key in helping the overall process.
“If you have a trusted software like DentalWriter, you can have those letters easily created for you and ready to fax to all the healthcare providers that a patient sees. That’s probably the most valuable tool that contributed to my success,” Dr. Ely said.
Problem: Dr. Ely says many dentists when starting out in the dental sleep medicine field don’t realize the connection between TMD and sleep apnea. This frame of thinking unfortunately can impact treatment outcomes.
Solution: One unexpected discovery in Dr. Ely’s early days of dental sleep medicine
has been the connection between temporomandibular joint disorders (TMD) and sleep apnea. Over time, she says she saw a strong overlap – many sleep apnea patients also suffered from jaw pain, bruxism, or TMJ issues. Instead of viewing TMD as a roadblock to oral appliance therapy, she embraced it, integrating it into her sleep evaluations, leading to more comprehensive patient care.
“One of my mentors is Dr. Mayoor Patel, who I consider a dear friend. I used to think, gosh, why does he have to make it so difficult and go so deeply into the connection between TMD and sleep apnea, you know? But he was wiser than I was. And so, after doing this for many years, you start to realize that a lot of these patients are the same patients. About 52% of sleep apnea patients have some form of TMD,” said Dr. Ely.
Dr. Ely believes that the road to success in this field all comes down to keeping that passion alive. She says staying focused, and having a plan will make a world of a difference as you embark on this journey. Most importantly though, Dr. Ely says it’s important to remember that success doesn’t happen overnight. Consistent outreach, team training, and patient education are key.
“The secret ingredient really is passion. If you have that mindset to want to make this work and become an airway centric practice, you have to commit yourself to consistent and continuous learning.”
Looking back, Dr. Ely sees dental sleep medicine is more than just an addition to her practice – it’s a mission to save lives. What started as a personal realization about her father’s undiagnosed condition has grown into a thriving practice that helps countless patients breathe, sleep, and live better.
For those considering this path, she leaves one final thought for dentists to consider:
“Physicians need us. What are they going to do with their CPAP failures or their patients that don’t want to try CPAP? You’re giving them an option. You’re allowing them to practice cutting-edge sleep medicine. And that’s what I’ve been continuously told by the doctors I work with. They look at me and say, “You make me better.” We are an asset to these physicians, and we have to start realizing that.” Dr. Anjoo Ely said.


by Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB
The first film ever about obstructive sleep apnea (OSA) in modern history, OUT OF BREATH directed and produced by George T. Nierenberg, is available for screening. For the last 2 years I have used a trailer of the film as the intro to my lectures across the country. I will never forget the first time I saw it, being chilled by the empowerment it gave me clinically and followed by motivation for sharing with my team.
There are two reasons dentists need to know about this film:
1. It identifies the critical role dentists have for the treatment of obstructive sleep apnea.
2. Dentists need to be ready for the questions patients will ask them after they see it.
I have yet to see a more powerful documentary highlighting the suffering people endure when they have OSA. Watching someone gasp for air on film induces immediate stress for the viewer. I wondered if I should tell my patients to video record themselves at night. As common as this diagnosis & disease is, at the heart of it, patients have no idea what it means or how severe their problem is (unless something major has occurred). They struggle to believe us that they should
be screened, or that they have a total cessation of breathing. Watching young, seemingly healthy individuals on camera choking on their tongue at night, is an important reminder that our patients are not good witnesses of their sleep (and therefore you need to ask more questions).
Former Marine Billy Toto, one of the patients in the film, resonated with me hugely, having seen failed cases of UPPP many times in my practice. He talked about the toll the OSA took on his marriage and the pressure his wife put on him to have the UPPP, given the initial treatment of CPAP was unsuccessful. OSA affects both partners at night and his wife was on the verge of separation during sleep time. In an effort to save his marriage Billy underwent the UPPP surgery - which he described as “the most horrific surgery I’ve ever had in my life.” He mentions not being able to swallow food for weeks. Failed CPAP, failed UPPP… it is amazing he tried anything else after that, but he was successfully treated in the end with Inspire. Another very invasive surgery to add to his list.
Hard working devoted family man Victor Boyd details his struggles with CPAP. We all know the side effects and issues that come along with CPAP therapy, but what I noted here was he went years with a leaking mask on his eight-year-old machine. How often are we asking our dental patients on CPAP therapy if they are compliant or having issues with their machine? Reminding them that insurance may cover replacements after a certain number of years might help with compliance and not falling through the cracks. “Not our lane” some would say… I beg to differ.
The DISE procedure was highlighted which I felt was worthy of a comment. Many dentists are unaware of this procedure and it is a great way to collaborate with an ENT. We must figure out a better solution for physician-dentist collaboration, so understanding how the specialties can work together is key. Knowing where the level of collapse hap-
pens in the airway can change the treatment options that are appropriate for the patient. Given it requires sedation, it is not performed on every patient, but it is important to understand how it can be useful in your oral appliance therapy cases.
I cannot recommend strongly enough that you watch this movie and spread the word! As airway dentists, we need to be aware of the multitude of options that exist to treat OSA and be advocates for our patients who may be struggling with their current modality. Newly engaged Kalyn Mckenzie, 23, who was saved by oral appliance therapy in this film had suffered for many years before getting help. Identifying the signs/symptoms of OSA in your dental practice will be the difference in the health and longevity of your patients. We owe it to our patients and their families to screen appropriately during their dental visits. If you have not implemented that in your practice, it needs to be your next goal.
As the film concluded, I could not help but think how different these individuals’ lives would have been, had they been prop-
erly treated orthodontically as children. We have to start getting it right the first time, to save these kids from becoming adults who struggle to breathe at night.
The website is SleepApneaFilm.com. You can watch the trailer and learn about screening this remarkable film in your community.


Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB, is passionate about how our teeth affect our systemic health – the link between chronic jaw infections, periodontal disease, and subsequent heart problems. Her training in obstructive sleep apnea has transformed both her personal and professional career. Dr. Hale is a Clinical Advocate for VIVOS Therapeutics and works with dentists around the country to develop clinical protocols for the treatment of mild to moderate obstructive sleep apnea and sleep-disordered breathing. Her work in pediatric expansion and sleep-disordered breathing catapulted her speaking career and she lives by the slogan “we have to stop getting it wrong, for our kids.” She is faculty for the Dental Success Network, a key-opinion leader for Candid, and the Chief Dental Officer for Toothpillow. She travels monthly across the U.S. and abroad to teach dentists about Obstructive Sleep Apnea. Learn more about her sleep mentorship program at https://sleepwelljourney.com/.




by Lee A. Surkin, MD, FACC, FCCP, FASNC, FAASM
Baggy eyes and low energy levels aren’t the only consequences of sleep deprivation. Indeed, lack of sleep can negatively affect both physical and mental health. Therefore, it is key that you try to get the recommended amount of sleep each night, which is 7 to 9 hours for adults.
Now, let’s have a closer look at the seven most common consequences of insufficient sleep:
1.
Missing out on quality sleep can reduce your efficiency to function throughout the
entire day. Even after just one night of poor sleep, you can experience trouble focusing, concentrating, and decision-making. What’s more, a poor night’s sleep makes it a lot harder to acquire new knowledge and learn. Similarly, you won’t be efficient at work if you experience a lack of sleep.
According to one study, impaired memory is also one of the potential consequences of insufficient sleep (Vaseghi et al., 2021). This study was conducted on people who used to have a healthy sleep pattern and then fell to fewer than six hours of sleep per night
and found that those people were subjected to accelerated cognitive aging – a risk factor for Alzheimer’s disease and dementia.
As already noted, sleep is vital for maintaining optimal mental health. Indeed, research shows that sleep deprivation can put you at a higher risk for depression and anxiety. This is so because serotonin, known as the happy hormone, helps to regulate sleep and can be thrown out of sync in case of sleep deficiency. In other words, your mental health could suffer if you lack sleep.
Although it may sound surprising, your skin could also start to look bad if you aren’t getting enough sleep. Not only could you get those dark circles under the eyes, but your skin will also begin to show more symptoms of sleep deficiency over time. Common signs of sleep-related bad skin include more fine lines and wrinkles, a paler skin tone, and dehydrated skin.
5.
Unfortunately, sleep deprivation can have negative consequences on your heart health. That said, following a balanced diet and regular exercise aren’t enough for optimal heart health. Indeed, you should get a good night’s sleep, i.e. at least seven hours per night, regularly if you want to avoid the risk of heart attack, high blood pressure, and even stroke.
One study showed a remarkably strong connection between obesity and getting less

“Even after just one night of poor sleep, you can experience trouble focusing, concentrating, and decision-making.”
than six hours of sleep each night (Beccuti & Pannain, 2011). Namely, sleep plays an important role in restoring the body’s natural processes, as well as allowing the hunger hormones to function properly. Otherwise, in case of sleep deprivation, you’re likely to consume more calories, and thus gain weight.
Last but not least, just like hormone regulation, the immune system needs adequate sleep to function properly and fight off illnesses. Namely, getting insufficient sleep regularly has been closely linked with coming down with a cold. Therefore, you must get enough sleep every night if you want your body to be able to ward off illnesses.
The bottom line, the consequences of sleep deprivation on your health are remarkable. Thus, consider making sleep your number one priority if you want to avoid all the negative effects associated with lack of sleep.
1. Vaseghi et al. (2021, Jun 04). Inconsistent effects of sleep deprivation on memory function. EXCLI Journal. https://www.ncbi. nlm.nih.gov/pmc/articles/PMC8278215/
2. Beccuti, G., & Pannain, S. (2011, July). Sleep and Obesity. Current opinion in clinical nutrition and metabolic care. https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC3632337/
Lee A. Surkin, MD, is the Chief Medical Officer of Nexus Dental Systems. A private practitioner in cardiology, sleep medicine, and obesity medicine, he is one of a small group of physicians to be triple board certified in cardiology, sleep medicine, and nuclear cardiology. In 2009, he created Carolina Sleep – the only dedicated sleep medicine practice in eastern NC. Dr. Surkin has created a cardiovascular and sleep healthcare model that includes a multi-faceted diagnostic and treatment approach that is enhanced by a network of relationships with physicians, dentists, respiratory therapists, sleep technologists, and public officials who recognize the important role that sleep medicine has in our daily life. In 2012, Dr. Surkin founded the American Academy of Cardiovascular Sleep Medicine which is a not-for-profit academic organization dedicated to educating healthcare providers, supporting research, and increasing public awareness of the convergence between cardiovascular disease and sleep disorders. In 2014, Dr. Surkin created a new multi-specialty practice called Carolina Clinic for Health and Wellness which combines his specialties with primary care, gynecology, behavioral health and a medical spa. Dr. Surkin is married with three daughters and a golden retriever and resides in Greenville, NC.
In today’s fast-paced dental landscape, every moment counts. BioMatch is designed to ease your mind by simplifying the entire oral appliance therapy process – from ordering to manufacturing to delivery – so you can focus on providing exceptional care.
BioMatch continues to refine oral appliance therapy with its simplified single-step ordering, expert patientmatched design, rapid eight-day manufacturing process, and robust three-year warranty.
The journey begins with a streamlined single-step ordering system. Dental professionals can easily upload patient records directly from an intraoral scanner. This eliminates multiple steps and allows Panthera Dental’s expert design team and purpose-built software to take over immediately.
They design patient-matched, drop-in fit appliances tailored to each patient’s unique anatomy, reducing side effects, minimizing adjustment time and providing peace of mind for the clinician.
Once the design team has completed their work, Panthera Dental leverages an advanced eight-day smart manufacturing process. Utilizing a state-of-the-art purpose-built tech stack including automation, robotics, and M2M communication1 so that every appliance is produced with exceptional accuracy.
From your order to appliance completion, the entire process takes just 8 days. This rapid

turnaround means your dental office receives appliances quickly, enabling faster treatment with reduced patient wait times.
To ensure complete peace of mind, every appliance is backed by a comprehensive three-year, no questions asked replacement warranty. This warranty covers any issues related to breakage and fit problems.
With this warranty, dental professionals can trust in the quality and durability of their appliances, knowing that any concerns will be promptly addressed.
In summary, BioMatch continues to refine oral appliance therapy with its simplified single-step ordering, expert patient-matched design, rapid eight-day manufacturing process, and robust three-year warranty. This integrated approach not only enhances operational efficiency but also elevates patient care.
By integrating cutting-edge technology with a commitment to quality, BioMatch reduces delays and minimizes stress. This allows you to spend more time doing what truly matters – delivering outstanding dental care.
Trust in BioMatch as a groundbreaking advancement in the ordering and design process. With its streamlined single-step ordering, expert patient-matched design, and rapid eight-day manufacturing, BioMatch delivers a seamless, worry-free solution that propels your practice to the forefront of dental technology.
Experience the confidence of a system designed to simplify every step – from the initial scan to the final delivery – ensuring precision and efficiency that truly eases your mind.
1. Machine 2 Machine. Youssef Abdelmajied, F. (2022). Industry 4.0 and Its Implications: Concept, Opportunities, and Future Directions. IntechOpen. doi:10.5772/intechopen.10252





by Amalia A. Geller, MD
Part two of this article will review the fascinating pathophysiology of REM Behavior Disorder (RBD) and provide an update on treatment and management of RBD.
As mentioned in part one of this article, brain activity accelerates during REM sleep showing markedly different types of brain waves. The EEG will return to a relatively low-voltage, mixed-frequency pattern. No sleep spindles, K-complexes, or NREM findings will be seen. The chin EMG will also fall to its lowest level. The classic finding will be seen on electrooculography (EOG) channels showing rapid eye movements. Other sleep architecture we see during REM sleep include Sawtooth EEG waves (7-8 Hz in the posterior dominant region) as well as basic muscle twitches.
RBD is listed as a parasomnia. The hallmark of RBD is vigorous motor activity during REM sleep in the total absence of muscle atonia. Another name for REM behavior disorder is REM sleep without atonia (RSWA), which is defined as increased tone during REM sleep using EMG of the chin and/or limb leads (either sustained increased chin EMG during sleep or increased chin or limb twitching).
Home sleep testing cannot be used to evaluate RBD. In cases when abnormal behavior does not occur during the sleep study, RSWA is required for the diagnosis.
The scoring of RSWA requires at least one of the following features developed by the American Academy of Sleep Medicine:
1. Sustained muscle activity in the chin EMG during REM sleep stage.

2. Excessive transit muscle activity in the chin or limb EMG during REM sleep.
The International Classification of Sleep Disorders, third edition, states the diagnostic criteria for RBD must include the following:
1. Repeated episodes of sleep-related behaviors, including vocalization and/or complex motor behaviors.
2. Documenting behaviors by PSG during REM sleep or based on clinical history.
3. Recordings of PSG that demonstrate REM sleep without atonia on submental or limb leads.
4. Behaviors are not better explained by another sleep disorder, mental disorder, medication, substance use, or epilepsy.
Validated questionnaires include:
1. Mayo Sleep Questionnaire – 98% sensitivity and 74% specificity.
2. REM Sleep Behavior Disorder SingleQuestion Screen (RBD1Q) – 98% sensitivity and 87% specificity.
Other useful questionnaires include:
1. REM Sleep Behavior Disorder – Hong Kong Questionnaire (RBDQ-HK) – 82% sensitivity and 87% specificity
2. REM Behavior Disorder Screening Questionnaire (RBDSQ) – 96% sensitivity and 56% specificity
3. Innsbruck REM Sleep Behavior Disorder Inventory – 91% sensitivity and 86% specificity
A critical finding we see during REM sleep that would indicate evidence of behavior disorder is an increase above normal of chin EMG, and clinically, when the patient completely acts out or moves and has dream enactment.
1. Idiopathic RBD: RBD without an identifiable underlying cause; this form is uncommon.
2. Drug-induced RBD: Mainly caused by MAO-inhibitors, tri-cyclic anti-depressants, and serotonin reuptake inhibitors. Seroto-
nergic RBD can also be present in those with alpha-nuclear neuro degeneration. This would involve abnormalities like color vision, anomia, constipation, and motor impairments. It is thought that the serotonergic in a depressant may unmask RBD in individuals who are at increased risk for underlying Neuro degeneration.
3. Secondary RBD due to medical condition: Neurodegenerative synucleinopathies (dementia with Lewy bodies, Parkinson disease, olivopontocerebellar degeneration, multiple system atrophy, and Shy-Drager Syndrome), Traumatic Brain Injury (TBI), PTSD, Narcolepsy Type 1, and congenital and neurodevelopmental disorders are the main causes of this form of RBD. Less common causes include non-synucleinopathies: Progressive supranuclear palsy (PSP), familial amyotrophic lateral sclerosis (ALS), frontotemporal dementia, and myotonic dystrophy. Secondary RBD has also been seen with Wilson’s disease, cerebral degeneration, and autoimmune encephalitis. These are usually due to paraneoplastic cerebellar degeneration that is immune mediated; often, these conditions can improve after immunotherapy.
4. Autoimmune RBD: The autoimmune disorder known as anti-IgL0N5 disease is a rare neurodegenerative encephalitis involving bulbar symptoms, gait abnormalities, and cognitive dysfunction. In addition to sleep manifestations such as sleep apnea, non-rapid movement sleep parasomnia, and RBD, serotonergic agents can lead to dream enactment. Histopathology studies in these forms of autoimmune-mediated RBD show neuron loss and extensive deposits of tau in the tegmentum of the brainstem and hypothalamus.
Other classifications of behavior disorder include:
• Subclinical REM sleep behavior disorder.
• Clinically probable REM behavior disorder.
• Idiopathic, cryptogenic REM sleep behavior disorder.
• Secondary or symptomatic REM sleep behavior disorder.
The prevalence of REM behavior disorder in the general population overall is unknown, but it is estimated to be about 0.5%. RBD can occur in either gender or age group even during childhood or adolescence. Most often,
we find it occurring in middle-aged or older adult men.
Acute RBD can be related to medication side effects as listed above or underlying toxic-metabolic derangement. Also, benzodiazepine withdrawal and alcohol withdrawal can increase the risk for RBD.
RBD is thought to be a prodrome for degenerative diseases, in particular, diffuse Lewy body dementia, Parkinson disease, as well as multiple system atrophy. These are all listed as alpha-synuclein degeneration regulating nuclei in the brain – specifically in the pontine tegmentum area.
Studies have shown that up to 81% of men with RBD over the age of 50 had delayed emergence of Parkinson disease dementia over a decade after the initial REM behavior diagnosis. Other conditions that overlap with RBD are the disorder of arousal, rhythmic movement disorder, insomnia, or sleep-related eating disorders.
RBD can also occur with narcolepsy (30% of young individuals with narcolepsy type 1), brain tumors, brain trauma, psychiatric disorders, substance abuse, and muscular sclerosis. During dream acting, patients are acting out their dreams and have increased risk for injury to themselves and others. The dreams are usually associated with being chased or attacking themes, but they are not specific for behavior disorder.
Nightmares are frightening dreams that wake us up from REM sleep. In RBD, the pa-

Amalia A. Geller, MD, is a board-certified Adult and Pediatric Neurologist with a subspecialty board certification in Sleep Medicine and additional post graduate fellowship training in Epilepsy and neurophysiology. She had a pediatric internship at Arnold Palmer Hospital for women and children and post graduate training in Child Neurology at the University of California at San Diego. Dr. Geller’s Neurophysiology and Epilepsy fellowships were performed at University of California at Irvine and her Sleep Medicine fellowship at the University of Texas Southwestern in Dallas. Dr. Geller splits her practice time between pediatric sleep medicine with a focus on neurologically challenged children (Neuro Developmental Sleep, PLLC) in Boise, Idaho; along with being a Neurohospitalist for NuView Health covering in-patient adult acute stroke and acute neurology tele-medicine; and out-patient Traumatic brain injury (adult and pediatric) with Elevate Clinic in Dallas, Texas. Dr. Geller believes a comprehensive holistic integrative approach is what is imperative to treat children as a whole in order for them to achieve their maximum potential. Dr. Geller is the Nevada medical director for Nexus Dental Systems.

tients are acting out the dreams and usually do not awaken themselves out of sleep. If they do awaken, it is because they have harmed themselves such as falling out of the bed. In general, the patient will have a memory of nightmares; they are very detailed and vivid, and they occur with emotions of fear. This is usually not as strong in patients experiencing RBD.
• Substance abuse/withdrawal
• Benign childhood epilepsy
• Complex partial seizures
• Confusional arousals
• Delirium
• Epilepsia partialis continua
• Epileptic encephalopathy
• Juvenile myoclonic epilepsy
• Malingering
• Sleep apnea
• Parasomnia overlap syndrome
• Periodic limb Movement disorder
• PTSD
• Psychogenic non-epileptic seizure
• Sleep terror
• Sleep walking/Trauma-associated sleep disorder
Management of RBD should focus on injury prevention and treating the underlying disorder in addition to psychological treatment for severe cases. Recommended actions:
• To prevent fall risk, lower bed closer to the floor
• Safeguard firearms, knives, and other weapons
• Sleep in sleeping bag/restraining clothes
• Separate the partner from the patient to decrease risk of injury.
RBD
RAMELTEON (melatonin M1/M2 receptor agonist) dose 8mg at bedtime. A study on idiopathic RBD at this dose showed no impact on the RBD or RSWA, but subjective improvement was reported.
Videos Showing RBD
• https://bit.ly/4hPcFRl
• https://bit.ly/4iEDCIt
• https://bit.ly/4iEHo4H
MELATONIN typical dosing is 5-15mg. Sustained release preferred over immediate release since REM sleep events cluster at greater frequency in the second half of the sleep cycle.
CLONAZEPAM (long-acting with half-life of 30-40 hours) dose 0.25mg
30 minutes prior to bedtime. Dose can be increased to maximum 4mg. Side effects include: residual AM sleepiness, increased fall risk, memory dysfunction, impotence, and unstable gait. There can be an initial period of suppression in the RBD followed by re-emergence of more complex behavior.
Other agents: dopaminergic agents, paroxetine, acetylcholinesterase inhibitors and anti-convulsants: carbamazepine and levetiracetam, anti-HTN medications (prazosin AND clonidine).
Treatment for drug-induced RBD may require discontinuation, dose reduction, or earlier medication intake.
Treatment medications could include slow-release melatonin, clonazepam, or transdermal rivastigmine. Treating co-morbid OSA with CPAP can help reduce RBD. When RBD is due to Parkinson disease, managing the PD with dopaminergic agents, PPE, and deep brain stimulation are investigational.
Mount Sinai Medical Center has developed a model showing there is a neurodegenerative link with Tau protein and that the dual orexin receptor antagonist drugs that are used for insomnia can decrease REM behavior disorder. This was published in The Journal of Neuroscience. Their model shows an early biomarker which could guide prevention and treatment. The dual orexin receptor antagonist when given twice a day within a 24-hour period, decreased sleep latency, increased the quality and duration of sleep, and decreased REM behavior disorder.
1. Howell M, Avidan AY, Foldvary-Schaefer N, Malkani RG, During EH, Roland JP, McCarter SJ, Zak RS, Carandang G, Kazmi U, Ramar K. Management of REM sleep behavior disorder: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2023 Apr 1;19(4):759-768. doi: 10.5664/jcsm.10424.
2. Haba-Rubio J, Frauscher B, Marques-Vidal P, Toriel J, Tobback N, Andries D, Preisig M, Vollenweider P, Postuma R, Heinzer R. Prevalence and determinants of rapid eye movement sleep behavior disorder in the general population. Sleep. 2018 Feb 1;41(2):zsx197. doi: 10.1093/sleep/zsx197.
3. Fulda S. Idiopathic REM sleep behavior disorder as a longterm predictor of neurodegenerative disorders. EPMA J. 2011 Dec;2(4):451-8. doi: 10.1007/s13167-011-0096-8. Epub 2011 Jun 29.
4. Diaconu Ș, Falup-Pecurariu O, Țînț D, Falup-Pecurariu C. REM sleep behaviour disorder in Parkinson’s disease (Review). Exp Ther Med. 2021 Aug;22(2):812. doi: 10.3892/etm.2021.10244. Epub 2021 May 28.
• Whole-Team Training
• Ongoing Coaching
• Streamlined Protocols
• Precision Bite Technology
• Patient Education
• In-Network Medical Billing





by Jyotsna Sahni, MD
While CPAP is still the gold standard treatment for obstructive sleep apnea (OSA), it can be cumbersome, high maintenance, and difficult to tolerate for some patients. Oral appliance therapy, hypoglossal nerve stimulation surgery/UPPP, positional therapy, and weight loss may also be beneficial for some patients. The U.S. currently has a 42% obesity rate, and a recommendation of weight loss is often easier said than done. However, weight loss may be achievable with the introduction of a new pharmaceutical medication: “Zepbound,” Eli Lilly’s brand name for tirzepatide. Zepbound was approved for obesity or overweight with one weight-related comorbid condition in November 2023. It is also marketed as “Mounjaro” for type 2 diabetes. It is to be used in combination with a reduced calorie diet and increased physical activity. However, the obstructive sleep apnea community was shaken up when Zepbound was approved on December 20, 2024 by the FDA for moderate to severe obstructive sleep apnea in adults with obesity. (Moderate OSA is an AHI of 15-29.9/hour. Severe OSA is >= 30/hour.) This is the first drug treatment option for patients with obstructive sleep apnea.
What is its mechanism of action? Zepbound activates receptors of 2 hormones secreted in the intestine: GLP-1 (glucagon-like peptide -1) and GIP (glucose-dependent insulinotrophic polypeptide) to reduce appetite and food intake, thereby helping people lose weight. The dual receptor activation separates it from the other 5 GLP-1 agonists available on the market. Zepbound is a weekly subcutaneous (SQ) injection (single-dose prefilled pen), self-administered by the patient. Dosing starts at 2.5 mg and is increased by another 2.5 mg every 4 weeks to a maximum dose of 15 mg, if tolerated. While not all obstructive sleep apnea patients carry extra weight, many do. Obesity is a major risk factor for OSA which is seen in up to 70% of morbidly obese individuals. We know that weight loss improves OSA. Zepbound‘s approval for moderate to severe obstructive sleep apnea in adults with obesity is based on two randomized, double-blind, placebo controlled studies of 469 adults without type 2 diabetes (SURMOUNT-OSA). In both studies, participants were randomly selected to receive either 10
or 15 mg of Zepbound or placebo weekly for 52 weeks. In Study 1, participants were using PAP therapy, the standard of care treatment for moderate to severe sleep apnea. In Study 2, patients were without PAP therapy because they were either unwilling or unable to use it. The primary measure of efficacy was change in the AHI (apnea-hypopnea index) at week 52, the conclusion of the studies. The addition of Zepbound was about 5-6 times more effective than placebo alone. In patients on Zepbound and PAP, AHI decreased by 29 apnea-hypopnea episodes per hour verses 6 with placebo. In patients on Zepbound without PAP therapy, AHI decreased by 25 fewer breathing disruptions per hour verses 5 in the placebo group. It was clear that patients who received Zepbound either with PAP use or without PAP use experienced a statistically significant and clinically meaningful reduction in AHI compared with placebo.
In addition, 50% of participants treated with Zepbound and PAP therapy and 42% on Zepbound without PAP therapy achieved either remission of OSA or improvement in severity of OSA with resolution of symptoms compared to 14% and 16% of placebo, respectively. Obstructive sleep apnea is commonly associated with snoring, excessive daytime sleepiness, and disrupted restless sleep. In addition, it has strong correlations with dangerous medical conditions such as hypertension, cardiac arrhythmias, stroke, and motor vehicle accidents.
Moreover, the patients treated with Zepbound had a significant decrease in their body weights compared to placebo. After 1 year, participants on Zepbound lost an average of 45 lb (18% of initial body weight) and the participants on both Zepbound and PAP therapy lost an average of 50 lb (20% of initial body weight) compared to 4 lb and 6 lb on placebo, respectively.
Side effects of Zepbound can include nausea, diarrhea, vomiting, constipation, abdominal discomfort and pain, injection site reactions, fatigue, allergic reactions, burping, hair loss and gastro-esophageal reflux disease (GERD). In addition, Zepbound causes thyroid C-cell tumors in rats. Therefore, it is contraindicated in patients with a personal or family history of medullary thyroid cancer or in patients with multiple endocrine neoplasia syndrome, type 2 (MEN2). Its label also con-
“Zepbound
is the first drug treatment option for patients with obstructive sleep apnea. By having this additional tool in our toolbox to treat obstructive sleep apnea, likely numerous obese patients will seek screening for obstructive sleep apnea.”
tains warnings for pancreatitis, gallbladder problems, hypoglycemia, acute kidney injury, diabetic retinopathy in diabetic patients, suicidal behavior thinking, and pulmonary aspiration during general anesthesia or deep sedation.
It is currently estimated that there are 54 million people in the United States with sleep apnea. However, only approximately 8 million of those people have been diagnosed. By having this additional tool in our toolbox to treat obstructive sleep apnea, likely numerous obese patients will seek screening for obstructive sleep apnea, now knowing that there is a successful treatment for weight loss and sleep apnea. Additionally, many patients will return to their sleep doctors with their known diagnosis of OSA after having failed CPAP or other treatments. The approval of this medication provides a wonderful opportunity for treating obstructive sleep apnea effectively and screening and diagnosing many more patients.

Dr. Sahni has been in medical practice for 22 years. The first 11 years of her career she was an internist at Canyon Ranch Health resort. Since then, she has practiced sleep medicine exclusively. She opened her own practice, Swan Sleep Medicine, four years ago. When asked why she chose sleep medicine, she often jokes that she could not commit to a single organ. Fortunately, sleep medicine is a combination of pulmonology, cardiology, neurology, and psychiatry. Never boring, sleep medicine requires a multi-disciplinary approach to diagnosis and treatment. To that end, she has been certified in holistic medicine, nutrition, and Ayuvedic medicine as well as Sleep medicine. In general, sleep medicine is a happy field of medicine. When people are sleeping well, they feel more rested, of course, but also have better mood, sharper memories, lower heart risk, and stronger immunity. Dr. Sahni asks that you forgive the pun, but when sleep is improved, it’s like night and day! She evaluates patients in her office as well as administers home sleep tests to look for sleep apnea and insomnia studies to look at brain waves while sleeping. She treats a wide variety of adult sleep disorders. She is taking new patients.






























































We are more than just a magazine...
Information related to dental sleep medicine changes constantly, stay on top of the latest news and resources with Dental Sleep Practice. Your subscription gets you...
• Opportunities to Earn 8+ CE Credits Per Year
• Live & On-demand Webinars
• Bi-monthly Enewsletters
• Digital Editions
• Exclusive Online Content
• Special Event Invitations
• Podcasts, and More
Scan the QR code to take advantage of our





This self-instructional course for dentists suggests various ways to think about Sleep Related Breathing Disorders (SRBD) and pre-disease as it relates to children with malocclusion. The article describes how clinicians must give systematic attention to creating collaborative environments in which dentists, otolaryngologists, and sleep medicine practitioners can work in concert to screen, evaluate, and treat childhood SRBD within the parameters of evidence-based medicine.
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
1. Realize the historical context behind the diagnosis and treatment of SRDB-Malocclusion in the pre-WW II era, prior to the era of evidence-based medicine.
2. Realize the impact of the ADA House of Delegates 2017 policy statement on the role of dentists in screening and treating SRBD and referring affected patients to appropriate physicians.
3. Identify several SRBD screening tools currently being utilized for assessment of pediatric sleep hygiene status.
TMSc
o best help their patients, dentists and other allied health professionals like to consider their continuing education endeavors as being current, fresh, and challenging, with novel ideas. There should be strong evidence to back up a change in how they evaluate and plan both preventive and active therapy. Much of today’s norms of medical care were set decades before randomized control trials (RCT’s) became the standard after WW II. In the absence of robust data derived from RCT’s, dentists can seek out from peer-reviewed literature the best available evidence to identify children who might be deemed at-risk of disease. Further evaluation and treatment, when their present and future health might become compromised by waiting, is prevention in action. When suffering is obvious, children might need more complex and possibly critical care. This essay will show the wisdom of clinicians from decades ago and discuss screening tools. It suggests ideas to bring patients and collaborating colleagues into new and effective ways to think about disease and pre-disease.
At the1921 annual meeting of the American Academy of Dental Science, distinguished Boston orthodontist Dr. Leroy Johnson presented, ‘The Diagnosis of Malocclusion with Reference to Early Treatment’. Dr Johnson confidently concluded, ‘The face has evolved with the functions of mastication and respiration. The perversion of either or both
functions will result in some degree of modification of the structure of the jaws. This the law of biology….’.1 Similar observations had been expressed at a New York medical meeting in 1912 by physician-dentist EA Bogue: 2 “When the dental arch is narrow, the nasal openings are also narrow, and are accompanied with more or less nasal stenosis…..A large percent of these cases are caused by the lack of natural capacity, due largely to the contracted dental arch and nares…..The roof of the mouth is the floor of the nose…The proper lateral expansion of the upper dental arch especially in young patients, while in their developmental stage increases the narial openings and improves the breathing capacity….”
As these two particular early 20th-Century scientific meetings had preceded the era of evidence-based medicine (EBM) by several decades,3 Drs. Johnson and Bogues’ statements could not have been based upon conclusions gleaned from carefully constructed random control trial (RCT) designed studies. Dentists today should seek to be guided by the best available evidence.4 Consider, however, that neither Dr. John Snow’s conclusions about the casual relationship between consumption of water from a contaminated community well and the contagiousness of cholera,5 nor Dr. Ignaz Semmelweis’ conclusion about the importance of physicians washing their hands after necropsy dissection prior to delivering babies6 had been based upon RCT-derived data. Within the context of informing best clinical practices when/where RCT-derived data might be unavailable, not possible or impractical to obtain per IRB ethical constraints or financial resource restrictions, the usefulness of research data that are sometimes derived from observational study design is well established in the scientific literature.7
A commonly held position is that controlled trials of an observational vs. randomized trial design can be useful towards generating accurate and clinically useful data where and when RCT’s cannot or have failed to do so. In support of this idea, the editors of JAMA-Pediatrics recently published data from a well-designed observational trial regarding potential fetal neurotoxicity of maternal fluoride intake as measured from the mothers’ urinary excretion.8 To publish data from this non-RCT was an unusual policy decision ac-
cording to JAMA editors. In addition, the data were so compelling that JAMA issued a recommendation regarding excessive maternal fluoride intake.
Dx: SRDB-Malocclusion Co-morbidity: Pre-WW II Physician-Dentist Collaboration
There are numerous pre-WW II papers published within the corpus of medical and dental literature that support the practice of physicians and dentists collaboratively diagnosing and treating SDB and malocclusion co-morbidity, mostly skeletal-dental maxillary transverse deficiency and mandibular distal occlusion (retrusion/retrognathia) through the ‘spreading of the deciduous arches’ during the early childhood years (30 months-7 y.o./complete primary-early mixed dentitions).2,8 These interventions had been carried out for the primary purpose of improving nasal breathing and quality of life rather than solely for the purpose of correcting so-called ‘irregularities of the teeth’. As these historically important journal articles pre-dated the 1948 initial published report of an RCT by several decades, it is unreasonable to criticize their usefulness compared to current RCT standards. Developing malocclusions are nearly always first detectable in the primary dentition (ages 2.5-7 yrs),9,10 nearly always become more complex (i.e., get worse) with age without appropriate intervention,9 and are very frequently co-morbid with pediatric sleep related breathing disorders (SRBD). In the single-digit growth

Kevin Boyd, DDS, MSc, is a board-certified pediatric dentist practicing in Chicago, IL. He is also a dental consultant in Sleep Medicine at Lurie Children’s Hospital. He is a Visiting Scholar at the University of Pennsylvania doing research in orthodontics and evolutionary biology at the Penn Museum of Archaeology and Anthropology. Prior to completing his DDS degree from Loyola University’s Chicago College of Dental Surgery in 1986, he obtained an advanced degree (MSc) in Human Nutrition and Dietetics from Michigan State University. He completed his post-graduate residency training in Pediatric Dentistry at the University of Iowa due to its reputation for providing intensive clinical and didactic learning opportunities in the areas of early childhood orthodontics/dentofacial orthopedics, and also early childhood behavior guidance management and child psychological/emotional development. Treating and preventing pediatric disease through promotion of healthy breathing and eating is his primary clinical and research interest.
years they are non-surgically correctible with validated orthodontic/dentofacial orthopedic interventions. It seems reasonable to suggest that failure to diagnose and appropriately treat or refer afflicted young children is a medically-indefensible position.
In 2017, the ADA House of Delegates approved a policy statement on the role of dentists in treating SRBD.11 Key components include assessing a patient’s risk for SRBD as part of a comprehensive medical and dental history and referring affected patients to appropriate physicians. Specifically, the policy statement refers to the screening of children: In children, screening through history and clinical examination may identify signs and symptoms of deficient growth and development, or other risk factors that may lead to airway issues. If risk for SRBD is determined, intervention through medical/dental referral or evidenced based treatment may be appropriate to help treat the SRBD and/or develop an optimal physiologic airway and breathing pattern. It is widely believed that current dental education does not prepare dentists to recognize pediatric airway issues. Standardized methods of screening with recognized thresholds for referral are not currently available. Development of these metrics would displace the subjective criteria that are currently used and provide a common language for every provider on the child’s health care team. Contemporaneous educational materials on the screening methods and the significant signs of pediatric airway issues would benefit the dental community and public.
SRBD-PSQ Behavioral Scale
Several SRBD screening tools are currently being utilized for assessment of pediatric sleep hygiene status. Two commonly used tools are B.E.A.R.S.12 and Dr. Ron Chervin’s Pediatric Sleep Questionnaire (PSQ),13 a 22-question SRBD scale that has strong correlation with overnight polysomnography sleep test (PSG) metrics for determining a child’s sleep quality. The PSQ can be highly predictive of increased risk for SRBD neurobehavioral morbidity and risk of post-adenotonsillectomy OSA recurrence as well as or better than PSG.14
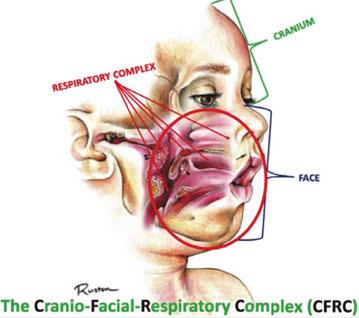
A pediatric-patient dedicated Sleep Medicine laboratory setting is difficult or impossible to find, setting aside what is considered the diagnostic gold standard, overnight PSG. Most screening questionnaires can be valuable as SRBD morbidity assessment tools and reliable for predicting increased risk. They are based solely upon identifying SRBD behavioral phenotypes known to be associated with suboptimal sleep hygiene (e.g., snoring, teeth grinding/bruxism, excessive bodily movements). The Sleep Clinical Record (SCR)15 is an exception because it relies on not only behavioral morbidity traits, but also some physical morbidity traits such as constrictive/retrusive and retrognathic jaw maldevelopments,16 which are known to be associated comorbidities with SRBD.17 Most of these physical traits can be classified as malocclusion phenotypes and generally are located within the interconnected craniofacial respiratory complex (CFRC)18 (Fig. 1) which was foreshadowed by Dr. LeRoy Johnson in the opening paragraph of
this review: ‘The face has evolved with the functions of mastication and respiration.’- L.J. 1921.
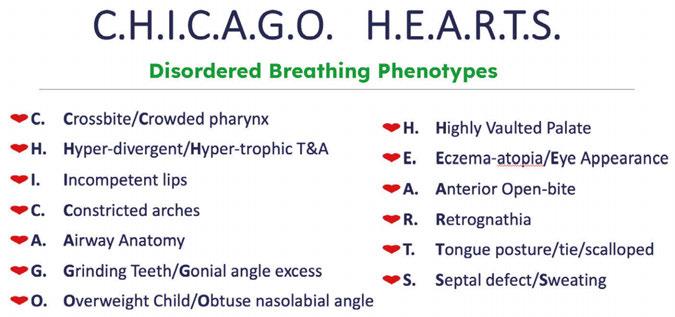
While the SCR goes further than most other screening assessment tools towards identification of some CFRC/SRBD co-morbidities, it is limited in its comprehensiveness. Ideally, in addition to screening for birth/perinatal history risk factors, such as pre-term birth,19,20 clinicians should have validated screening tools for identifying behavioral comorbidity traits, and for identification of physical risk phenotypes of the CFRC. The CHICAGO HEARTS screening tool combines these survey areas. (Fig. 2).
In a lecture held in 2018 at Boston University entitled ‘Sleep Disordered Breathing/Obstructive Sleep Apnea Symposium’,21 a new screening tool called C.H.I.C.A.G.O. H.E.A.R.T.S. (C.H.) had been introduced as potentially becoming the first validated screening device specifically designed to identify CFRC physical traits that can often be comorbid with SRBD. Several of these traits are listed within the C.H. acronym (Fig. 2). For instance, under the first letter ‘C’ are listed: Crossbite 22,23 Fig. 3 and Crowded Pharynx;24,25 ‘H’: Hyper-divergent growth (Fig. 4),16 Hypertrophic tonsils and/or adenoids;26,27 ‘I’: Incompetent lips;28 ‘C’: Constricted arches (Fig. 5);23,29,30 ‘A’: Airway anatomy (Fig. 6);22,31 ‘G’: Grinding teeth (bruxism)32 and Gonial angle excess;33 ‘O’: Overweight child34 and Obtuse nose-lip angle( NLA);35 ‘H’: Highly-vaulted palate;36 ‘E’: Ezcema-atopia37 and Eye appearance-venous pooling38 and scleral show;39 ‘A’: Anterior open-bite



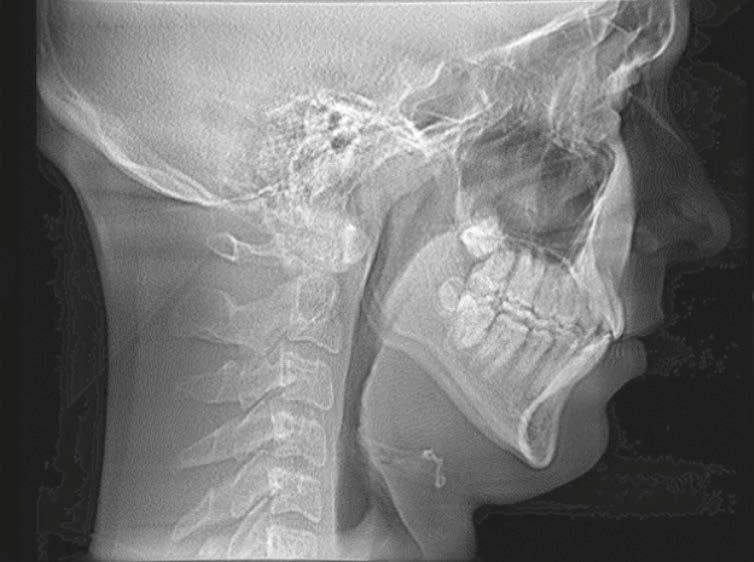

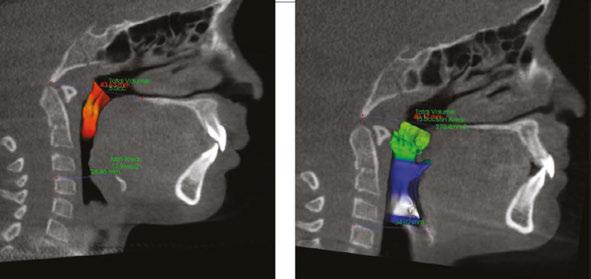



(Fig. 8):40 ‘R’: Retrognathia (Fig. 9) (mandible16 and/or maxilla);41 ‘T’: Tongue posture,42 tie (tether),43,44 scalloping;45 ‘S’: Septal deviation46 and night Sweats (diaphoresis).47
There is no single provider who can treat all aspects of a child’s developing airway, so it is necessary for every provider to communicate with other professionals. While dentists are used to working with specialist colleagues, merely filling out a referral form is inadequate. Multi-provider patient care requires sharing of critical information without the benefit of commonly-accessible health records or free clinical time to dig through dense reports in order to find the next step in the child’s health care plan. To achieve a balance between not-enough and too-much data in the report, agreements setting appropriate communication expectations are the way to go.
George Bernard Shaw famously said: “The single biggest problem in communication is the illusion that it has taken place.” This unfortunate truism exists in medicine today. The doctor who first identifies the child at risk has the primary duty to guide the patient (and their family) through the diagnostic and treatment option process. This is best done by contacting the child’s pediatrician (or family PCP) for medical status updates, share concerns, and work out the next steps to be taken. As the dentist opens the discussion, they must keep in mind that the physician likely had about 2 hours of instruction on all aspects of sleep-related topics during residency. The dentist is well-served to recall the paucity of
the topic in their own professional school and approach colleagues first with curiosity about their comfort with the evaluation and management of children with airway problems. Assuming other providers are well-aware of the subject might lead to defensiveness or other impediments to helpful exchange of information. The physician might appreciate the informed dentist helping them navigate unfamiliar territory; when done respectfully, the dentist-physician relationship improves.
A strategy that has worked well in several dental offices known to the author is for the dentist to reach out to providers important for diagnosing, treating, and managing SRBD in the community and initiate small-group meetings to establish common ground. Each provider (dentist, pediatrician, otolaryngologist, children’s sleep specialist, orthodontist, myofunctional therapist, school nurse – the list can include many health care professionals) is invited to share with the group their perspective and engage with others about how their expertise is valuable. Dentists, unlike physicians, are used to study clubs and other mutual-learning environments. Clarity of purpose and diplomacy in presenting the opportunity to providers who might question the need for such an effort is the first challenge. Once the group is assembled, before diving into the details, a ‘safe environment’ must be created so participants feel free to share their strengths and weaknesses. If the dentist is adept at convening and leading meetings, the first gathering should go well; another option would be to invite someone with facilitation skills to help with initial agreements. Like first impressions, the startup meeting sets the tone
for ongoing group dynamics, where questions arise, beliefs are challenged, and discussions lead to establishment of agreed-upon protocols that can be employed in many clinical situations. For those patients who fall outside the typical presentation, the relationships built in the small group enable more effective connections between providers to establish an optimum care path. Once established, the small group can be a source of much professional comradery, shared learning experiences, and great satisfaction in practice.
If a group cannot be assembled straightaway, it takes more work, but individual relationships must be fostered. The first may be for the dentist to find an airway-oriented orthodontist and like-minded otolaryngologist to talk over patient care. These doctors are the best-trained in all aspects of the craniofacial respiratory complex and this triad can form a nucleus of a preferred referral pattern. Once protocols are developed between the small group, they can be proffered to the other necessary professionals with credibility.
Growing awareness of the deleterious health impact of SRBD in adults has led to a sense of urgency in a variety of health fields to develop creative approaches to treatment, but that’s a subject for another essay. Another significant development over the past 10 years has been the realization that SRBD is common in children. We have learned that adenotonsillectomy, a treatment approach effective in improving sleep related respiration in many patients with SRBD, cannot be relied on as definitive treatment. Residual and recurrent SRBD after adenotonsillectomy have been demonstrated to be common,50 leading to curiosity among practitioners who care for children about why this occurs and what can be done about it. Once again, innovations emerged from collaborations between practitioners from different fields, united by their shared desire to improve the lives of children with SRBD. These innovations included the use of medications, drug induced sleep endoscopy, and non-retractive orthodontic/ dentofacial orthopedic (NRO/DO) approaches to treatment. While there are still very few examples, there is growing enthusiasm about what becomes possible when dentists, otolaryngologists, and Sleep Medicine physicians collaborate. Indeed, the imperative of hav-
ing practitioners from each of these fields involved in the care of any patient with SRBD is increasingly recognized in the field of sleep medicine. What is also emerging is a common recognition that beyond treating SRBD, practitioners caring for kids should set as their goal the establishment of unobstructed nasal breathing as early in life as possible. Our recognition of the complexity of SRBD, the impact a compromised airway can have on breathing during wakefulness, and evolving attitudes about what is required to make this diagnosis have led many of us who practice in this field to begin to look outside the current paradigm for potential ways to improve the lives of our patients. Naturally, the paradigm shift from surgical treatment of SRBD to multidisciplinary non-surgical or adjunctive-to-surgery efforts to optimize nasal breathing has met with some resistance. As a result, much of the research taking place in the field is focused upon measuring emerging treatment approaches against adenotonsillectomy based on polysomnography (PSG) results. The paucity of centers capable of performing PSG in children and effectively interpreting these recordings has limited our ability to learn about these questions at a large enough scale to generate a compelling basis of evidence for the need for collaboration between the medical, surgical, and dental fields. What the rediscovery of the publications reviewed in this article show is that in the late 19th-/early 20th-Century SRBD was a known entity in early childhood and was evaluated and treated by both surgical and dental collaborators.1,2,8, 47-55 Collaboration allowed patients with disordered breathing of sleep and wakefulness, primarily manifested as habitual and chronic mouth-breathing, to get the multidisciplinary care required to optimize their airways. This suggests that while research based upon PSG evidence of improved outcomes after NRO/ DO and other nonsurgical treatments of SRBD in children can and must continue, we must also give systematic attention to creating collaborative environments in which dentists, otolaryngologists, and Sleep Medicine practitioners can work in concert to screen for, evaluate, and treat disordered breathing in children. Our hope is that this review will demonstrate that these collaborations are essential and inspire a growing number of practitioners from diverse fields to begin conversations about how they can remove barriers to
this approach. Let’s get back to doing what was done before!
1. Johnson, L. The Diagnosis of Malocclusion with Reference to Early Treatment. 1921; J Dent. Res. 3(1):v-xx.
2. Bogue, E.A. New York Academy of Medicine-section of Laryngology and Rhinology. 1912;
3. Cochrane, A. Effectiveness and Efficiency: Random Reflections on Health Services. 1972; Nuffield Provincial Hospitals Trust
4. Buschang, P.H. An evidence-based stepwise approach to orthopedic treatment. 2023; Seminars in Orthodontics. 29(3):271-277
5. Paneth, N. Assessing the Contributions of John Snow to Epidemiology 150 Years After Removal of the Broad Street Pump Handle. 2004; Epidemiology. 15(5):514.
6. Bjerke, N. The Evolution Handwashing to Hand Hygiene Guidance. 2004; Crit Care Nurs Q. 27(3):295-307.
7. Faraoni D, Schaefer ST. Randomized controlled trials vs. observational studies: why not just live together? BMC Anesthesiol. 2016 Oct 21;16(1):102-.
8. Streptomycin treatment of pulmonary tuberculosis: a Medical Research Council investigation. BMJ 1948;2:769-82.
9. Green, R. et al. Association Between Maternal Fluoride Exposure During Pregnancy and IQ Scores in Offspring in Canada. JAMA-Pediatrics. 2019;173(10):940-948.
10. Cohen, S. Malocclusion and Its Far Reaching Effects. 1922; JAMA. 79(23):1895-1897.
11. Baccetti, T. et al. Early dentofacial features of Class II malocclusion: A longitudinal study from the deciduous through the mixed dentition. 1997; Am J Orthod Dentofac Orthop. 111;502-509.
12. Bishara, S. et al. Changes in the molar relationship between the deciduous and permanent dentitions: A longitudinal study. 1988; Am J Orthod/Dentofac. Orthoped. 93:19-28.
13. https://www.ada.org/en/member-center/leadership-governance/ councils-commissions-and-committees/dentistry-role-in-sleep-related-breathing-disorders# Accessed 01/16/2020
14. BEARS Owens, J. A., & Dalzell, V. (2005). Use of the “BEARS” sleep screening tool in a pediatric residents’ community clinic: a pilot study. Sleep Medicine, 6(1), 63–69.
15. Chervin, R.D. et al. Pediatric Sleep Questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. 2000; Sleep Medicine 1:2132.
16. Chervin, R. et al. Pediatric Sleep Questionnaire: Prediction of Sleep Apnea and Outcomes. 2007; Archives of Otolaryngology - Head and Neck Surgery. 133(3):216-22.
17. Pia-Villa, M. et al. Sleep clinical record: what differences in school and preschool children? 2016; ERJ Open Res. 2:1-8.
18. Flores-Mir, C. et al. Craniofacial morphological characteristics in children with obstructive sleep apnea syndrome: A systematic review and meta-analysis. 2013; JADA. 144(3):269-277.
19. Boyd KL, Sheldon SH. Sleep disorder breathing: a dental perspective. In: Principles and practice of pediatric sleep medicine. 2nd ed. Amsterdam: Elsevier Inc; 2012. p. 275–80.
20. Boyd, KL and Kelly, J. Prevention and Correction of Pediatric SB/ OSA and Post-T&A Relapse: A Non-Surgical Orthodontic/Dentofacial Orthopedic Approach. 2019; in: Friedman, M. and Jacobowitz, O.(eds) Sleep Apnea and Snoring 2nd ed. Elsevier Inc. p. 439-444.
21. Collaco, M. Respiratory Phenotypes for Preterm Infants, Children, and Adults: Bronchopulmonary Dysplasia and More. 2018; Annals ATS 15(5):530-538.
22. Ignacio, T. et al. Perinatal Risk Factors Associated with the Obstructive Sleep Apnea Syndrome in School-Aged Children Born Preterm. 2016; SLEEP. 39(4):737-742.
23. Boyd, K. Structure-Function/Function-Structure of Habitual Mouth-Breathing and Malocclusion in the Primary/Early Mixed Dentitions. Paper presented at : Sleep Disordered Breathing/Obstructive Sleep Apnea Symposium, Boston University, March 10, 2018
24. Fastuca, R. et al. Airway compartments volume and oxygen saturation changes after rapid maxillary expansion: A longitudinal correlation study. Angle Orthodont. 2015; 85(6):955-961.
25. Galiotti A. et al. Prevalence of malocclusion in children with obstructive sleep apnoea. Orthod Craniofac. Res. 2018; 21:242–247.
26. Tsuiki, S. et al. Oropharyngeal Crowding and Obesity as Predictors of Oral Appliance Treatment Response to Moderate Obstructive Sleep Apnea. CHEST. 2013; 144(2):558–563.
27. Ito, E. et al. Oropharyngeal Crowding Closely Relates to Aggravation of OSA. 2016; CHEST. 150(2):346-352.
28. Ballikaya E. et al. Oral health status of children with mouth breathing due to adenotonsillar hypertrophy. 2018; Int. J Ped.Otorhinol. 113:11–15.
29. Oliver, OA. The Evil Effect of Adenoids and Tonsils Upon the Dental Arches. 1918; The International Journal of Orthodontia. 4(8):391394..
30. Saitoh, I. et al. An exploratory study of the factors related to mouth breathing syndrome in primary school children. 2018; Archives of Oral Biology 92:57–61.
31. Pia-Villa, M. et al. Efficacy of rapid maxillary expansion in children with obstructive sleep apnea syndrome: 36 months of follow-up. 2011; Sleep Breath. 15:179–184.
32. Stellzig-Eisenhauer A. and Meyer-Marcotty, P. Interaction between otorhinolaryngology and orthodontics: correlation between the nasopharyngeal airway and the craniofacial complex. 2010; GMS Current Topics in Otorhinolaryngology - Head and Neck Surgery. 9:1-8.
33. Major, M et al. Agreement between cone-beam computed tomography and nasendoscopy evaluations of adenoid hypertrophy. 2014; Am J Orthod./Dentofac. Orthoped. 146:451-459.
34. Rouse, J. The Bruxism Triad Sleep bruxism, sleep disturbance, and sleep-related GERD. 2010; Inside Dentistry. May:32-44.
35. Anderson, S. et al. Correlation between gonial angle and dynamic tongue collapse in children with snoring/sleep disordered breathing – an exploratory pilot study. 2018; J Otolaryngology - Head and Neck Surgery 47:41-46.
36. Gozal, D. Obesity and Excessive Daytime Sleepiness in Prepubertal Children With Obstructive Sleep Apnea. 2009; Pediatrics. 12(1):13-18.
37. Conley, S.R. et al. Facial Soft Tissue Changes Following Maxillomandibular Advancement for Treatment of Obstructive Sleep Apnea. 2007; J Oral Maxillofac Surg. 65:1332-1340.
38. Guilleminault, C. et al. Death and the Naso-maxillary complex. 2012; European Journal of Pediatrics 171(9):1349-58
39. Ramirez, F. et al. Association of Atopic Dermatitis With Sleep Quality in Children. 2019; JAMA Pediatrics 173(5):1-9.
40. Sundelin, T Cues of Fatigue: Effects of Sleep Deprivation on Facial Appearance 2013; Sleep. 36(9):1355-1360.
41. Posnick, J. and Sami, A. Individuals With a Long Face Growth Pattern and Excess Inferior Scleral Exposure: Is There Improvement After Maxillary (Le Fort I) Advancement and Vertical Shortening? 2015; J Oral Maxillofac Surg 73:1809-1815.
42. Smithpeter, J. Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. 2010; Am J O Dentofac. Orthoped. 137:605-14.
43. Monteiro, P. et al. Dentofacial Morphology of Mouth Breathing Children. 2002; Braz Dent J. 13(2): 129-132
44. Guilleminault, C. et al. A frequent phenotype for paediatric sleep apnoea: short lingual frenulum. 2016; ERJ Open Res. 2:00043.
45. Yoon, A. et al. Ankyloglossia as a risk factor for maxillary hypoplasia and soft palate elongation: A functional – morphological study. 2017; Orthod Craniofac Res. 20:237–244.
46. Weiss, TM. The Association of Tongue Scalloping With Obstructive Sleep Apnea and Related Sleep Pathology. 2005; Otolaryngology–Head and Neck Surgery.133:966-971.
47. Guilleminault, CG et al. Adenotonsillectomy and obstructive sleep apnea in children: A prospective survey. 2007; Otolaryngology–Head and Neck Surgery. 136:169-175.
48. Hung, KS et al. Night sweats in children: prevalence and associated factors. 2012; Arch Dis Child. 97:470–473.
49. Whiting GF. Mouth-breathing and its Attendant Evils. 1883; Dental Cosmos.;5(6):295–306.
50. Pullen HA. Mouth-breathing. 1906; Dental Cosmos. 48(10):998–1014.
51. Haskin WH. The relief of nasal obstruction by orthodontia-A plea for early recognition and correction of faulty maxillary development. 1912; Laryngoscope. 2(11):1237–60.
52. Sobotky, I. Persistent Mouth Breathing Following Adenoidectomies. 1913; Boston Medical and Surgical. J 168(7):231-32.
53. Bogue EA. Enlargement of the nasal sinuses in young children by orthodontia. 1909; J Am Med Assoc. 53(6):441–4.
54. Bogue EA. The position of the deciduous teeth, an important diagnostic symptom. 1921; Int J Orthodon Oral Surg. 7(5):237–50.
55. Bogue EA. The Relations of the Dental Arches to Pathologic Affections of the Nasopharynx and Adjacent Parts. 1907; Jour.A.M.A. 49(2):102-105.
56. Weeks, MS. Relation Between Abnormal Breathing and Malocclusion. 1913; Archives Dis. Childhood. 30:46-51.
57. Brown, G. The Application of Orthodontia Principles to the Prevention of Nasal Disease. 1903; Dental Cosmos. 45(10):765.
AGD Code: 730
Date Published: April 15, 2025 Course Expires: April 15, 2028
Legal disclaimer: Course expires 3 years after publication date. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
n To receive credit: Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
by Kevin Boyd, DDS, MSc
1. A validated questionnaire for children’s breathing ____________.
a. Should only be used by pediatric sleep specialist physicians
b. Provides a definitive diagnosis of behavioral problems
c. Allows clinicians a means of assessment when PSG is not available
d. Involves subjective data assessed by a healthcare professional
2. Clinicians present clinical observations about growth, development, and breathing performance ________.
a. Following detailed published studies that link these characteristics
b. Based upon what they and others notice in their patients
c. Only with objective data gathered during normal night’s sleep
d. By studying tooth wear that indicates bruxing habits
3. C.F.R.C stands for _______________________.
a. Controlling Forces to Resist Consequences
b. Chicago Face Revision Communication
c. Checking Functional Remodeling Concerns
d. Cranio Facial Respiratory Complex
4. Most physicians’ limited training in sleep and sleep problems
_____________.
a. Provides the dentist an opening to build a mutually beneficial learning opportunity by working together
b. Provides sufficient expertise for their value to the patient’s family
c. Is rarely a barrier to families – they have little trouble sorting conflicting information
d. Means nothing – treatment in kids is controlled by dentists
5. The most common sign of poor breathing performance of the CFRC is __________.
a. Short chin
b. Long face
c. Habitual mouth-breathing
d. Crooked teeth
6. Dr. LeRoy Johnson posited that the “face has evolved with
____________.
a. Changing esthetic goals”
b. Mixed genetic influences due to population mixing”
c. Functional changes associated with mastication and respiration”
d. New ways of analysis through research”
7. Failure to recognize SRBD traits in children is ________.
a. Common
b. Medically indefensible
c. Creating lifelong health challenges
d. All of these and more
8. C.H.I.C.A.G.O. H.E.A.R.T.S. _____________.
a. Is a way to discover cardiovascular problems
b. Combines behavioral and physical assessments of risk
c. Provides a family a way to self-assess their child’s behavior
d. Focuses on breathing as the key to most things related to health
9. When assembling a group of health care providers for mutual patient care _________.
a. It’s important for the dentist to lead the group
b. Gathering everyone together for the first meeting is critical
c. The physician with the most specialized education drives the agenda
d. Creating excellent communication in a safe environment will foster mutual growth
10. A big benefit of non-retractive orthodontics / dentofacial orthopedics is ___________.
a. Lack of research linking it to lifelong risk of SRBD
b. Provides a therapy choice if adenotonsillectomy results in incomplete resolution of SRBD and there are growth deficiencies
c. General acceptance by the American Association of Orthodontics
d. Increased fees for fancy therapy that parents are told their children need
VirtuOx, the nation’s largest sleep diagnostics provider, is proud to introduce Sleepifi DENTAL, an innovative and comprehensive software platform designed to help dentists seamlessly manage every aspect of the dental sleep medicine workflow. From screening and diagnosis to treatment and documentation preparation for insurance billing, Sleepifi DENTAL simplifies and streamlines the process, allowing dental professionals to enhance patient care while improving operational efficiency.
From screening and diagnosis to treatment and documentation preparation for insurance billing, Sleepifi DENTAL simplifies and streamlines the process.

The Sleepifi DENTAL platform is designed with ease of use in mind, ensuring that dentists and their teams can effectively navigate the sleep apnea treatment process without unnecessary complications. Here’s how it works:
1. Screen for Sleep Apnea – The journey begins by identifying patients who may be at risk for obstructive sleep apnea (OSA). Dentists can use the electronic sleep screening questionnaire embedded in the Sleepifi software to assess patients efficiently. This tool helps pinpoint individuals who could benefit from further evaluation.
2. Home Sleep Testing – Once a potential sleep apnea patient is identified, they are sent home with a multi-use NightOwl testing device, provided at no cost to the dental office.
3. Telemedicine Consultation & Sleep Study – Using the Sleepifi platform, conveniently schedule a telemedicine consultation with a sleep physician. The physician evaluates the patient’s symptoms and orders the home sleep test. The software enables easy tracking of the patient’s appointment status, testing progress, and results – all in one place.
4. Diagnosis and Prescription – Once the home sleep test is completed, the
sleep physician interprets the results. If a diagnosis of obstructive sleep apnea is confirmed and medical necessity is established, the physician prescribes an oral appliance for treatment. All essential documents, including physician notes, prescriptions, and test reports, are automatically attached to the patient’s record within Sleepifi, ensuring a seamless and organized workflow.
5. Auto-Titration and Follow-Up Testing – To save staff time and enhance patient compliance, Sleepifi includes an auto-titration feature. The software automatically sends text and email reminders to patients, prompting them to repeat home sleep tests at designated intervals to titrate their oral appliance and measure its effectiveness. The dentist is notified when test results and patient subjective feedback questionnaires are available for review.
6. Simplified Insurance Billing – Submitting insurance claims is often a tedious and complex process. With Sleepifi, practices can generate all required supporting documentation with just one click, making the reimbursement process faster and easier. This ensures that practices receive timely payments while reducing administrative burdens on staff.
Sleepifi supports several of the latest HST device technologies, including NightOwl, SleepImage, and EnsoSleep PPG.
If you’re a dental professional looking to enhance your practice with cutting-edge sleep medicine technology, now is the perfect time to explore Sleepifi DENTAL. Contact us today at sales@sleepifi.com or (855) 472-8776 to learn more about how this innovative solution can benefit your practice and your patients.








In the evolving landscape of sleep apnea treatment, innovation continues to play a vital role in improving patient comfort and clinician ease of use. One such advancement is the AT (Advanced Titration) Arm, an upgrade from the traditional Herbst styled arms commonly used in sleep apnea devices. With a range of benefits for both patients and providers, this enhanced arm design sets a new standard in oral appliance therapy.
AT (Advanced Titration) Arm versus Traditional Herbst Styled Arms: A Clear Advantage
For years, the Herbst style sleep apnea devices have been a go-to option for health care providers, offering reliable treatment for patients with obstructive sleep apnea (OSA). However, the Advanced Titration Arm introduces several key improvements, making it the superior choice:
• Increased Durability & Strength – The AT Arm is constructed from high-quality materials designed to enhance longevity and reduce the risk of breakage, a common issue with traditional arms.
• Smoother Titration Adjustments –Unlike the traditional Herbst arm, which requires a more manual approach, the AT Arm allows for easier and more


precise adjustments (Figure 1), ensuring greater accuracy in mandibular positioning.
• Enhanced Patient Comfort – Its sleek, low-profile design minimizes irritation and bulkiness, leading to better patient compliance and improved long-term wear.
• Improved Retention & Stability – The AT Arm provides a more secure fit, ensuring the arm stays in place throughout the night, even for active sleepers.
The AT Arm is compatible with any DynaFlex or Respire Herbst devices (Figure 2). Whether patients are using a standard Herbst, a custom-fitted design, or a temporary mandibular advancement device, they can benefit from the precision and durability that the AT Arm offers.
This compatibility is a game-changer for clinicians, providing more flexibility in treatment options and allowing for retrofitting on existing devices. Patients no longer need to compromise on adjustability or reliability – the AT Arm delivers the best of both worlds.
As oral sleep devices continue to evolve, the DynaFlex Advanced Titration Arm sets a new benchmark in the industry. Its strength, adjustability, and comfort make it a clear upgrade from the traditional Herbst style arms, and its expanded compatibility ensures that more patients can benefit from its advanced design.
For dental professionals and sleep specialists looking to maximize patient outcomes, making the switch to the AT Arm is a step toward better compliance, fewer device failures, and ultimately, improved treatment success rates.
by Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB
Until you can take every ounce of responsibility for the consult failing, you will continue to tell yourself “My patients don’t want airway treatment.”
There are procedures dentists are excellent at explaining. For example, a filling. I would hope your restorative case acceptance rate is high. Discussing sleep related breathing disorders (SRBD’s) is wildly foreign to dentists and without serious additional education, you will lack the confidence to talk about it. Explaining to a mom that her 9-year-old son’s bedwetting can be ameliorated with a nighttime habit corrector appliance, takes true understanding of the physiology by which bedwetting occurs. But that’s just the beginning – you also must connect with that mom on a level that allows her to trust you to take care of her child with something “fringe”. I don’t know about you, but bedwetting wasn’t in my dental school curriculum.
Treatment planning interceptive orthodontic treatment for children, and traditional oral appliance therapy (OAT) for an adult, takes skills unlike what we were taught in dental school. Today, there is a tremendous amount of resources for education in dental sleep medicine. Most sleep dentists understand the etiology of bruxism; but if you cannot properly explain how it could be something worse, in a way that the patient can relate, they won’t let you help them. Tooth grinding has become so normalized in dentistry thanks to occlusal guards, most patients are surprised to hear it’s actually something serious. We must fill in the blanks so they can connect the dots that their symptoms are common, but not normal.
My consultations are held in a separate room from the operatory. I sit eye to eye with my patients to go over their sleep study, showing them the digital scan of their teeth and discussing exactly how their sleep symptoms relate to their bite. Using the verbiage “this doesn’t age well” or “this isn’t aging well” has helped patients to understand that continuing down the current path can have expensive consequences. I love helping patients realize that improving their sleep will improve the longevity of their health
and teeth. If you can get on their level and utilize the knowledge you have in a real-world way, you will succeed in treating more patients.
When you are analyzing your case acceptance rate and it’s below 60%, review what you said in that consultation. Were you paying attention to the patient’s body language? Did you ask them if they had questions about what you went over? If that patient does not schedule for treatment, ask your treatment coordinator (TC) what hesitation was expressed. Find out if they had to explain anything that you should have. Identify holes in your own understanding, then fix it. Cost is an excuse; don’t lie to yourself that all your patients are broke. I have maintained a 90% case acceptance rate over the years, in an entirely out of network practice. How you approach these patients, and the verbiage you use around their treatment options, is the difference in your success of increasing airway cases in your practice. As I mentor dentists all over the country, I realized we have one thing in common: the desire to serve our patients well. You are incredibly privileged to do what you do for a living, with a unique ability to transform the longevity of your patients’ lives.
To quote Einstein, “If you can’t explain it simply, you don’t understand it well enough.”

Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB, is passionate about how our teeth affect our systemic health – the link between chronic jaw infections, periodontal disease, and subsequent heart problems. Her training in obstructive sleep apnea has transformed both her personal and professional career. Dr. Hale is a Clinical Advocate for VIVOS Therapeutics and works with dentists around the country to develop clinical protocols for the treatment of mild to moderate obstructive sleep apnea and sleep-disordered breathing. Her work in pediatric expansion and sleep-disordered breathing catapulted her speaking career. She is faculty for the Dental Success Network, a key-opinion leader for Candid, and the Chief Dental Officer for Toothpillow. She travels monthly across the U.S. and abroad to teach dentists about Obstructive Sleep Apnea. Learn about her sleep mentorship program at https://sleepwelljourney.com/.

• In-Network options with major payors and plans
• Out-of-Network when appropriate
• Reliable, timely, predictable results with best rates
• Access to the Nexus Specialty Physician Network
• Nexus billing portal ensures error-free claim submission and tracking
• Personal billing representative
• Complete solution for:
º Sleep Medicine
º Airway Expansion
º TMJ/TMD
º Botox
º CBCT

Getting reimbursement from medical insurance can be a nightmare for dentists. With the Nexus Bill system, you can avoid the common pitfalls of inconsistent payments, endless delays, constantly fighting with insurance companies, and patients refusing care because you are not “In-Network” for medical.





