
















Dr. Seuss got it right, many times. In this classic, he points out how life brings us opportunities in unexpected ways. When we recognize those open doors and step through them, we create experiences that allow us to achieve our dreams. You’ve probably gotten Oh, the Places You’ll Go as a birthday or graduation gift.
Improv is like that. Conversations with patients and colleagues are like that, too. Friend to breathing Emma Cooksey talked to me about improv classes helping her communicate on her podcast. She used it when seeing her sleep doc about her own treatment. We all benefit from expanded thinking and avoiding ‘one size fits all.’
Yes, and…. Is more than a construct used on stage. I’ve been reading a lot of books about communication using principles based on good listening, building on what the ‘scene partner’ says, and staying focused on how decisions are best made together. Most readers of this magazine likely eschew doctor-determined, patient-accepting unilateral treatment decisions. That’s not to say the old model doesn’t still exist. Your patients may tell you stories about how their medical encounters were wonderful exchanges of data, points of view, and thoughts about what treatment will be most successful. Other patients may be challenging to develop into relationship because an open invitation to participate in their care has not been their experience. They come to you closed, not expecting to be consulted for their wishes.
Take any opportunity you can to change their perspective on what it means to make decisions together, to take what they know and add to it with a ‘move forward together’ attitude. Listen to their history and ask good questions about something they just said. You will learn what is true for them. Responding
with a positive acknowledgment is not agreeing or condoning what might be related as a negative experience. It simply says you are with them in their current condition. You can look them in the eye and with integrity tell them you heard them.

Moving forward is blocked if a ‘no’ is the next step. The way to lead people to make their best decisions is through ‘yes,’ followed by what you can add to their understanding, their list of options, and, most significantly, making clear the power they have to participate. If you expect people to make great health decisions, you must accept responsibility to be an open communicator, not just about what you know but how you feel towards that human connection.
Dr. Samuel Shem writes about making good connections in his book Man’s 4th Best Ho$pital. He describes mutual empathy as when two parties see each other, feel seen by the other, and senses the other feeling seen. Achieving this level of relationship is intentional, beneficial, and can set any person, patient, or clinician on a different path towards a healthier future.
Take your practice to another place. If you’ve not begun that journey, find your old copy of Oh, the Places You’ll Go and read it with new eyes. Try out ‘Yes, and…’ with your next new patient. You just might feel your heart grow three sizes that day.
Do you like what you are reading in DSP? Do you have ideas you want to share about what works in your practice? As Chief Dental Editor, I am happy to consider essays from any reader! Contact me at stevec@medmarkmedia.com.
Steve Carstensen, DDS Diplomate, American Board of Dental Sleep Medicine8

Cover Story
The Panthera Pioneering Spirit: Unveiling Innovations in Dental Sleep Health Through Collaboration
Gain treatment confidence with excellent partners.


Medical Insight
16
Impact of CBT-I Based Sleep Coaching Program Delivered via Mobile on Sleep Duration and Sleep Quality by Dr. Michael A. Grandner
Sleep coaching interventions can bridge the gap by providing support.

Medical Insight

22
Continuing Education Overview of Abnormal Movements During Sleep by Amalia A. Geller, MD
A discussion of the categories of disorders associated with abnormal movements during sleep.
Nightmares Versus Night Terrors by Jyotsna Sahni, MD
Discussing these two conditions and how they can relate to OSA.
Practice Management Applying Improv Tactics to Sleep Apnea Treatment by Emma Cooksey Combination therapy is no laughing matter.
42


• Offer FDA-cleared therapeutic procedures that provide pain relief and rehabilitate force imbalances for new and existing patients
• Provide medically necessary dentistry using tested technologies including ultrasound, photobiomodulation, microcurrent, and muscle manipulation.
• Precisely diagnose and deliver state-of-the-art treatment for chronic migraines and headaches, tinnitus, and other neck/jaw/face pain
• Address an individual patient’s symptoms with a drug-free, needle-free treatment plan that has a 95%-100% clinical success rate
• Receive clinical training along with ongoing implementation assistance
• Add a revenue stream to your practice, increasing your non-doctor revenue
• See nearly 389% ROI and only 30 minutes of doctor chair time per case.


6 Publisher’s Perspective 2024 – Appreci-8 Your Potential
by Lisa Moler, Founder/CEO,MedMark Media
12 Expert View Overcoming Challenges: Educating and Preparing Sedation Dentists for Treating OSA Patients
by Michael Silverman, DMD
Patients who have OSA and want sedation in a dental office need special care.
28 Cardio-Sleep Corner
The Link Between Insomnia and Heart Failure
by Lee A. Surkin, MD,FACC, FCCP, FASNC, FAASM
A look at the impact of insomnia on cardiovascular health.
30 Communication Corner
“The First Thing I Changed”
by Kalli Hale,DDS, MPH, D.ABDSM, D.ABSB
Think you can’t change? The first step is the key.
32 Pediatric Pediatric Sleep Research Update for ‘Sleep Wrecked Kids’ 2023
by Sharon Moore
Global leaders are paying attention to how children sleep.
34 Clinical Focus
Boning Up on Nitric Oxide: Just the Hard Facts!
byDr. Steve Lamberg
Even more to learn about this important little molecule.
40 Choosing Appliances Which Design is the ‘Best?’
by Sonnie BocalaSeveral common designs with pros and cons.
44 Product Spotlight SomnoSeal: Enhancing Nasal Breathing and Sleep Therapy Comfort
by Kimberly Hutchison, MD, FAASM Stop mouth breathing for PAP and OAT patients.
46 The Bigger Picture
The Breathing-Smile Connection: The Intersection of Airway Health in Orthodontics
by WilliamE. Harrell, Jr, DMD, ABO, C.DEM
Form and function are established early; no time to waste!
51 Clinician Spotlight

Guiding Our Way for 40 Years!
an interview with Laura Sheppard, CDT, TE
How our profession took shape, from an insider.
54 Product Spotlight
Tongue Positioning and Sleep Quality
A simple idea to boost therapy success.
56 Sleep Humor
The Lighter Side of Sleep Apnea
Spring 2024
Publisher | Lisa Moler lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Jamila Battle, MD (Family/Sleep/Addiction)
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Alison Kole, MD, MPH, FCCP, FAASM (Sleep, Pulmonary, Critical Care)
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Bertrand de Silva, MD, FCCP, D.ABSM
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Steve Lamberg, DDS, D.ABDSM
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD

National Account Manager
Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media
Felicia Vaughn | felicia@medmarkmedia.com
Website Support
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9
Scottsdale, AZ 85260
Tel: (480) 621-8955 | Toll-free: (866) 579-9496
www.DentalSleepPractice.com
Subscription Rate: 1 year (4 issues) $149
©MedMark, LLC 2024. All rights reserved. The publisher’s





 Lisa Moler Founder/CEO, MedMark Media
Lisa Moler Founder/CEO, MedMark Media
Numerology is the study of numbers that deal with their mystical meaning and effect on our lives. When you think of all of the numbers that surround us every day – our dates of birth, other special dates, births, anniversaries, and deaths of those near and dear to us, even your home address can have a deeper meaning. No better time to think about the power of numbers than this year. Add up the numbers in our new year, 2024, and the result is the number 8. Turn the number 8 on its side, and you get the infinity symbol – this year, you can harness the power of 8 – when opportunities to reach goals in our personal and private lives can be limitless.
A little numerology research on the number 8 shows that it represents the achiever and goal-reacher. The number symbolizes good sense, a powerful presence, and strong success drive. Balance is also a hallmark of the number 8, as reflected in its symmetrical shape that promotes stability, potential, and productivity.
The number 8 is ruled by the planet Saturn (as is the zodiac sign, Capricorn). Traits of this planet are perseverance and ambition, so during 2024, our “8” year, we should strive to find our places as strong leaders ready to transform our plans and words into actions.
For this Spring 2024 issue, we want to help turn your plans into prosperity with our clinical articles and marketing expertise. In our Cover Story, dental sleep health meets collaboration, as Dr. Ashley Spooner incorporates Panthera Dental appliances, processes, and workflows into her DSM options at her initiative, Dynamic Dental Sleep, LLC. Our Continuing Education article, by Dr. Amalia A.
Geller, explores disorders that cause abnormal movements during sleep, and how collaboration can lead to effective solutions. In her Practice Management column, Emma Cooksey suggests that combining therapies, like her CPAP and an oral appliance, or collaborating with other specialists may provide better outcomes for patients.
What can you do to make the most of your “8” year? Keep achieving, be strategic, and fiercely tenacious. Be a leader, but listen to your team and let them know that the most fulfilling achievements are the ones that you reach together. Give back when you can because the karma of the number 8 is connected to the infinite balance between success and gratitude. And remember like the balanced number 8, to make time for personal life, even while you pursue professional success. 2024 is the year to turn your potential into prosperity.
With appreci-8-tion for success in 2024,
Lisa MolerDental Sleep Practice subscribers are able to earn 2 hours of AGD PACE CE in this issue by completing the quiz online at https://dentalsleeppractice.com/continuingeducation/ after reading the article “Overview of Abnormal Movements During Sleep” by Dr. Amalia A. Geller, which starts on page 22.

Creative thinking and a collaborative mindset can have a transformative effect in the world of dental sleep medicine. The story shows how a dentist visionary has tenaciously worked to establish a training and support model for other dentists seeking dental sleep medicine expertise.
Ashley Spooner, DDS, D.ABDSM, is a passionate advocate for her patients regarding screening and treatment of obstructive sleep apnea (OSA). She became involved with dental sleep medicine (DSM) in 2015 and achieved diplomate status in 2020 from the American Academy of Dental Sleep Medicine (AADSM).
Dr. Spooner has partnered with dental support organization Pacific Dental Services® (PDS) for business support services since 2013. PDS is a prominent proponent of dental-medical integration, seeking to improve health outcomes through closer collaboration between the dental and medical fields.
Leveraging the support and vision of the PDS platform, Dr. Spooner was motivated to
The Promise of Panthera Dental: Excellence, Commitment, and Collaboration Panthera Dental manufactures the D-SAD Panthera Classic and Panthera X3 oral appliances (OA) for treating obstructive sleep apnea (OSA). Panthera’s expertise and investment in “Industry 4.0“ enables the company to use the latest technology in the evolution of robotics, automation, analytics, and 3D printing of oral appliances. Panthera’s proprietary purpose-built sleep appliance CAD/CAM software is at the heart of this process, which allows for the broadest range of OA customization options available, including avoiding appliance contact with the weaker anterior teeth and circumventing excess interproximal material. Panthera uses versatile medical-grade nylon material, which is easily adaptable to the uniqueness of each individual, from basic to the most complex cases. The choice of nylon material is essential as it can be printed either very thin for flexibility, without snapping

or breaking (very useful for bands), or thick for rigidity (useful for plateaus) while always maintaining its durability and dimensional stability. The combination of software and material allows for an OA design to perfectly match the patient’s complex oral anatomy.
Investing in such technology ensures faster delivery time, improved first-time fit, enhanced patient experience, and the practitioner has reduced chair time. You can learn more about this process at https://bit.ly/3RUL73b or by scanning the QR code below. These features combined allow for improved workflow and profitability, aligning well with a DSM and DSO operations.
Panthera prides itself on partnering with the DSM provider and seeing ourselves as partners in the patient journey. The above processes allow us to provide a patient-matched device, which not only streamlines the initial fitting, reducing chair time and re-fitting but can lessen the therapeutic burden on the patient. Therapeutic burden is one aspect of care that may lead to reduced initial acceptance and long-term adherence to therapy, which is vital to the health and well-being of the patient.
Our “Panthera Patient Partnership Philosophy (4Ps)” is in alignment with the P4s of medicine, “predict, prevent, personalize and participate”.1,2 Although Panthera cannot be integral to all of the parts of the P4s, our goal is that by providing better patient-aligned, effective products, listening to providers’ needs, and acting on that knowledge, we can ensure our D-SAD products fit into new models of care.
The surrounding story highlights this partnership between Panthera, a dental sleep provider, and the patient. The story exemplifies how working creatively together can achieve optimal outcomes for all involved. We promise to continue striving to meet the needs of patients and providers alike.

1. Postal, K. The P4 Approach: What is it and how is it being used in dental sleep medicine. Sleep Lab Magazine, November/December 2023 https://www.calameo.com/ sleeplabmagazine/read/00637204605197a75765a
2. Lim DC, Sutherland K, Cistulli PA, Pack AI. P4 medicine approach to obstructive sleep apnoea. Respirology. 2017;22(5):849-860. doi:10.1111/resp.13063
cultivate expertise in DSM while fostering a clinical culture in her practice that prioritizes proactive screening and treatment of chronic inflammation and OSA. The PDS platform has provided her with opportunities to approach patient care with an interdisciplinary mindset, enabling greater collaboration with the patient’s broader healthcare team. Throughout the years, significant changes have occurred in the field of DSM, from new appliances to a heightened understanding of OSA’s significance. While these changes have increased awareness within dental practices concerning the necessity of screening and treatment, the under-treatment of OSA persists, significantly impacting patients’ quality of life, health, and mortality
Driven by the increasing potential for dentists and their teams to address OSA, Dr. Spooner founded Dynamic Dental Sleep, LLC (DDS) as an initiative separate from her affiliation with PDS. DDS provides comprehensive educational elements, complemented by ongoing mentorship beyond the course duration. Through DDS, Dr. Spooner provides dentists high-quality, affordable training encompassing both the clinical and business aspects of DSM. The DDS PACE-accredited program brings together education, team training, billing, and industry relationships so dentists can focus on their patients and be confident in the streamlined workflows that drive efficiencies and result in effective patient care, provider satisfaction, and increased revenue.







Establishing workflows that provide a positive experience for the patient and the clinician can be challenging. “Many times, dentists will take courses and get excited about implementing something new into their practices, but the day-to-day of a busy practice engulfs them, and that new ‘thing’ gets put on the shelf for when the time is right,” reflected Dr. Spooner. “My question is: Is the time ever just perfect for something new? There will always be a reason to wait or to not do it at all. Understanding that this may be the case for many, it became my mission to establish workflows for the general dentist who would like to add more purpose to what they do while not distracting from their core business.”
Dentists who train with DDS gain a deep understanding of the importance of sleep, learning to provide the dental aspects of OSA screening and treatment with oral appliances following AADSM guidelines. They receive comprehensive documentation templates and a step-by-step guide, enabling the establishment of a consistent, reliable, and scalable framework to seamlessly integrate DSM into any dental practice.
After completing the DDS course, dentists have the option to work with DDS vendors or their own network of healthcare providers. The goal is to provide dentists with the know-how to develop a truly turn-key workflow that can be seamlessly implemented into practice.
In 2021, Dr. Spooner was introduced to Panthera Dental. Panthera is renowned for its expertise in designing and manufacturing dental sleep appliances, manufacturing the D-SAD Panthera Classic and Panthera X3 oral appliances for treating OSA. Leveraging Industry 4.0 principles, their expertise in robotics, connectivity, artificial intelligence (AI) and advanced 3D printing techniques enable the manufacturing of state-of-the-art oral appliances. This
Ashley Spooner, DDS, D.ABDSM, is the owner of Falcon Park Dental Group in Highlands Ranch, Colorado, a practice supported by Pacific Dental Services. She is also the Founder/CEO of Dynamic Dental Sleep, LLC*. She graduated from University of Colorado School of Dental Medicine and is a Diplomate of the American Board of Dental Sleep Medicine. Dr. Spooner can be reached at aspooner@dynamicdentalsleep.com.
process includes proprietary purpose-built sleep appliance CAD/CAM software. Panthera uses a versatile medical-grade nylon material that readily conforms to the distinct anatomical requirements of each individual, accommodating a wide range of cases from basic to the most complex. (See side bar on previous pages.)
As Dr. Spooner began delivering more Panthera devices to her patients, a relationship was born. She states that “while continuous positive airway pressure devices, or CPAP, continue to be prescribed, patients are looking for other options. Shared decision-making regarding treatment has demonstrated that patients often opt for an oral appliance versus a CPAP. I’ve found Panthera’s devices to be durable and lightweight, which leads to a smoother and more comfortable fit for the patient.”
“There are many steps in a DSM workflow, but when executed well, it is efficient,” continued Dr. Spooner. “Panthera’s processes for streamlining the ordering and delivery process allows patients to receive their oral appliance within two weeks. In combination with DDS screening workflows, a patient can be screened and treated within four to six weeks.”
Dr. Spooner commends Panthera’s dedicated support in case design and swift issue resolution, emphasizing their comprehensive understanding of sleep medicine. Additionally, she praises Panthera’s diverse team and their commitment to education, emphasizing their valuable role in DDS’ continuing education programs, further ensuring successful DSM implementation in dental practices.
“While there are many choices for oral appliances, Panthera is my preferred device when appropriate for the patient,” says Dr. Spooner. “Their additional support, customized care, and educational acumen truly sets them apart.”
The ongoing support of Panthera Dental for Dr. Spooner and DDS’ dental sleep program, aimed at educating and training dentists interested in incorporating DSM, presents an exceptional opportunity. This initiative holds the promise of extending diagnostic and treatment services to millions more individuals affected by OSA. In the end, Dr. Spooner’s aspiration is for this collaboration to significantly enhance patients’ overall health and well-being.


Approximately 39 million Americans suffer from obstructive sleep apnea (OSA), of which 80% are undiagnosed and untreated.
During sedation, monitoring technology is similar to that used in sleep studies. Consequently, patients undergoing dental sedation may exhibit apneic events, temporarily cease breathing, and trigger the End Tidal CO2 alarm or a drop in the oximeter measurement below 90, signaling potential undiagnosed sleep apnea.
This is a significant concern for sedation dentists. Under dental sedation, sleep apnea, particularly in overlooked instances, can pose a serious health threat when the patient falls asleep. Therefore, sedation dentists should be vigilant regarding sleep apnea, understand the safest monitoring procedures, and take steps to ensure the most effective care possible.
During sedation dental procedures, patients are administered sedatives to help them relax and they often fall asleep. However, patients with sleep apnea are at an increased risk of health complications during sedation due to the collapsible nature of their airway soft tissues.
Sleep apnea can lead to airway obstruction and decreased oxygen levels, which can have severe implications for dental sedation. Proper oxygenation levels are crucial during dental sedation and require a clear, unobstructed airway.
As such, using the STOP-Bang method, every dental sedation patient should be screened for sleep apnea during the health history pre-screening process.
It’s then advised that dental patients with known sleep apnea only be sedated if a physician is successfully treating their condition.



Pediatric MiniResidency
$6,500/person
June 2024 (Virtual and In-person)


Dental Sleep Medicine
$12,000/person
October 2024April 2025 (Virtual and In-person)


Craniofacial Pain and Sleep Maxi Res.
$9,975/person
September 2024December 2024 (Virtual and In-person)

TMD and Orofacial Pain
$12,000/person
September 9, 2023 -
February 24, 2024 (Virtual and In-person)

“As simple as it sounds, monitoring a patient’s heart rate is elemental in administering and monitoring sedative drugs.”
This precaution ensures their airway remains unobstructed and adequate oxygenation levels are maintained throughout the procedure.
Dental professionals should be aware of the potential risks associated with sedating patients with unknown or untreated sleep apnea. By pre-screening patients for the condition and ensuring that those with OSA are being medically treated, dental professionals can help minimize the risk of complications and ensure the safety of their sedation patients.
Sedation dentists must take extra precautions when treating patients with sleep apnea, as they may be more sensitive to sedative and muscle relaxant agents.
Five steps to consider in treating apneic dental sedation patients:
1. During the appointment, use 100% supplemental oxygen and consider using triazolam or midazolam for IV sedation. Longer-acting agents like lorazepam should be avoided, and diazepam should not be used the night before. Short-acting sedatives are preferred to minimize the risk of the patient being sedated at home without medical supervision. It’s also best to minimize or avoid the use of analgesics with hypnotic action.
2. Increased attention should be given to the position of the patient’s airway.
3. Because of the compromised airway, it’s recommended to sedate the patient to a lighter level and avoid letting them fall asleep. If they do fall asleep, it’s crucial to arouse them. Reversing them is acceptable if sleep apnea episodes are noticed.
4. Patients requiring a full BiPAP are not candidates for sedation dentistry. Ask
Michael Silverman, DMD, is a globally recognized lecturer, educator, author, and patient rights advocate and the founder and president of DOCS Education. He has appeared in front of 28 dental boards to advocate for the right of dentists to provide sedation in an environment of safe and reasonable regulations. A graduate of the University of Pennsylvania School of Dental Medicine and believer in lifelong continuing education, Dr. Silverman continues to champion for safe and effective minimal and moderate dental sedation. He can be reached at dr.silverman@docseducation.com or docseducation.com.
Disclosure: Dr. Silverman is the President of DOCS Education, but received no compensation for writing this article.
this question during the health history pre-screening process.
5. It’s imperative to avoid alcohol, muscle relaxants, and opioids. Opioids should not be prescribed for pain in these patients.
When administering sedation to patients with sleep apnea, it is crucial to monitor their vital signs using reliable and trusted industry-standard equipment.
Intravenous (IV) sedation, and enteral (oral) sedation should only be performed using a monitoring device that measures heart rate, oxygenation percentage, blood pressure, and end-tidal CO2.
The End Tidal CO2 measurement is essential for monitoring a patient’s airway during sedation and is the earliest indication of any potential breathing issues.
levels is one of the latest care standards in sedation practice, while oxygenation is arguably the most important due to a need to maintain a high percentage of oxygenated hemoglobin. Monitoring ETCO2 has the advantage of alerting the practitioner of a cessation of breathing before the SpO2 measurement drops. Therefore, dental practices should invest in a high-quality monitoring device, such as the Edan X-10 or X-12, when practicing sedation.
These hospital-grade devices can print and digitally record heart rate, three-lead heart rhythm, end-tidal CO2, and pulse oximetry every 5 minutes. It is worth noting that monitoring a patient’s heart rate is essential in administering and monitoring sedative drugs throughout the appointment. Therefore, ensuring the monitoring technology is high quality and can provide accurate readings is crucial for sedation dentistry.
Prevention is essential. However, in an emergency, the entire dental team must be prepared to assist immediately and effectively when necessary.
To determine if assistance is needed, you must first know the patient’s tissue oxygenation and ventilation status.
If the pulse oximeter alarm sounds, indicating an undesirable level of oxygenation, the dental team should take the following steps in a logical series to correct the desaturation:
1. Establish Consciousness by asking the patient questions like “Are you okay?” If the patient responds verbally, they are determined to be conscious.
2. Open the airway by raising the chin.
3. Check the equipment to ensure the finger clip is adequately positioned.
4. Have the Patient Take a Few Deep Breaths.
5. Administer 100% Supplemental Oxygen.
6. Reversal with Flumazenil – 0.2-0.3mg or 2-3cc.
7. Call for Help by dialing 911.
The acronym for the steps to take when the O2 Saturation Alarm sounds is CAEBOR, which stands for Consciousness, Airway, Equipment, Breaths, Oxygen, and Reversal.
If the patient does not respond to verbal stimulation when the O2 Saturation Alarm sounds, then the above algorithm is modified to:
1. Establish Consciousness (patient is unconscious).
2. Open the Airway.
3. Administer 100% Supplemental Oxygen.
4. Reversal with Flumazenil.
It’s important to note that patients with sleep apnea may present some challenges for sedation dentistry. However, with proper education and preparation, dental professionals can provide these patients safe and effective sedation.
It’s crucial for the team first to be aware of the patient’s medical history and any potential risks associated with OSA. Sedation dentists can ensure a successful and safe procedure for apneic patients by taking the necessary precautions and using high-quality monitoring technology.
Regular dental sedation education also reassures patients they’re being looked after by a dental team that meets or exceeds dental sedation safety standards and regulations.




Poor sleep health affects a significant portion of the American population, with prevalent sleep-related issues impacting overall quality of life. A tiered approach to sleep health services is necessary, ranging from intensive interventions for severe issues to more widely accessible options for milder problems. Sleep coaching programs have emerged as a potential solution for addressing minor sleep concerns, offering education, support, and motivation to promote beneficial sleep habits.
Week 1 Initial assessment, personalized sleep evaluation, introduction to the program, introduction to key techniques and concepts, setting an initial schedule
Week 2 Begin stimulus control and some sleep compression, journaling, worry lists, relaxation exercises
Week 3 Daytime support activities including managing bright light exposure, exercises, caffeine intake, napping, motivation and self-talk
Week 4 Addressing bedtime issues, snacking at night, environmental factors, sleep supplements, relaxation exercises
Week 5 Bedroom-related factors, sleeping positions, mattresses, sleep technologies, reflection and behavior change
Week 6Physical activity, nutrition, sleep as part of overall health, rest and recovery
Week 7 Embracing setbacks, cultivating self-compassion, cognitive and emotion-focused techniques
Week 8 Managing anxiety, reducing stress, dreaming, muscle relaxation and self-reflection
Week 9 Reflection and maintenance of healthy habits, reinforcing stimulus control and schedules
Week 10 Reflection and maintenance of healthy habits, reinforcing daytime and evening routines that support sleep health
Week 11Wapping up, relapse prevention, revisiting helpful behavioral exercises and ideas
Week 12 Wrapping up, relapse prevention, revisiting helpful cognitive and emotional exercises and ideas
While clinical interventions like Cognitive Behavioral Therapy for Insomnia are wellestablished for severe sleep problems, lessintensive interventions for subclinical issues are still limited. Sleep coaching interventions aim to bridge this gap by providing support for improving sleep behaviors. Some recent pilot studies have demonstrated the efficacy of sleep coaching in enhancing sleep health for various populations, including shift workers, military personnel, and adolescents with chronic illnesses.
A recent study published in the journal Frontiers in Sleep evaluated the impact of a 12-week app-based sleep coaching program, called “Sleep Reset,” in a real-world setting. The program combines personalized coaching, education, and tracking components to promote healthier sleep habits. A total of 564 participants who completed the program were included in the study. They were initially screened for medical and psychological conditions that might contraindicate participation. Those individuals who likely needed more intensive care were referred toward clinical resources.
Table 1The Sleep Reset program spans 12 weeks and includes three main aspects: tracking and assessment, education on sleep and circadian habits, and interactive coaching with a live coach. The coaches communicate with participants through the app, offering personalized recommendations and feedback. The curriculum covers a range of sleep-related topics, from sleep compression to managing stress and anxiety (Table 1).
The study’s primary goal was to assess whether participants completing the Sleep Reset program would show improvements in sleep continuity (parameters like sleep latency, wake after sleep onset, number of awakenings, sleep efficiency), sleep duration, and use of sleep aids. It was hypothesized that participants would experience reduced sleep latency, wake after sleep onset, and awakenings, along with increased sleep duration and efficiency.
The results of the study demonstrated significant improvements in sleep parameters among participants who completed the program. Notably, there were reductions in sleep latency and wake after sleep onset, as well as improvements in sleep efficiency, number of awakenings, and total sleep time. Moreover, individuals with lower initial sleep efficiency and shorter sleep duration experienced more pronounced improvements. These findings suggest that the Sleep Reset program had a positive impact on sleep continuity and duration.
Among those who completed the program, they reduced their sleep latency by 41%, reduced their wake time after sleep onset by 35%, reduced their number of awakenings by 17%, increased sleep efficiency by a relative 8%, and increased sleep duration by about 45 minutes, or 11% (Table 2).
Like any sleep intervention, those who stand the most to benefit are more likely to

“Those who completed the Sleep Reset program on average saw notable, significant improvements in several dimensions of their sleep health.”

Dr. Michael Grandner is a licensed clinical psychologist, board-certified in Behavioral Sleep Medicine and Lead Scientific advisor to Sleep Reset. He is the Director of the Sleep and Health Research Program at the University of Arizona and Director of the Behavioral Sleep Medicine Program at the Banner-University Medical Center in Tucson. Dr. Grandner is Associate Professor of Psychiatry, Psychology, Medicine, Nutritional Sciences, and Clinical Translational Science at the University of Arizona. He is an internationally-recognized expert in sleep health, has over 250 academic publications, and frequently consults with health, technology, athletics, and nutritional companies and organizations regarding sleep, health, and performance. Read more about him at michaelgrandner.com.


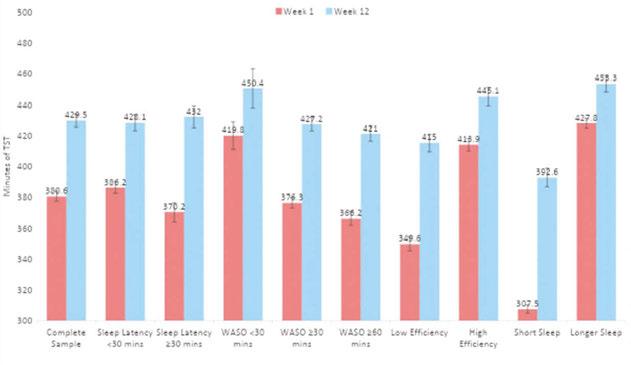
see greater improvements. When those who started out with a lower sleep efficiency (<85%) were compared to those with a higher sleep efficiency at the outset, those whose sleep started out worse experienced greater improvements (Table 3).
And those who started out sleeping less gained more sleep and improved their sleep to a greater degree than those who were already sleeping more hours (Table 4).
Taken together, those who completed the Sleep Reset program on average saw notable, significant improvements in several dimensions of their sleep health. They were falling asleep faster, staying asleep longer, waking fewer times, and sleeping more hours. These effects were especially pronounced for those who started out with worse sleep health, since they had more room for improvement.
The study has some important limitations, including the absence of a control group and the focus on program completers, which might introduce biases. The reliance on self-reported sleep data through diaries could lack objectivity. Rigorous methodologies, such as control groups and intent-totreat analyses, are needed for a more accurate assessment of the program’s effects.
This study highlights the potential of an app-based sleep coaching program, Sleep Reset, in improving sleep parameters and sleep continuity for individuals without diagnosed sleep disorders. The multifaceted approach of coaching, education, and tracking appears effective in promoting healthier sleep habits. However, further research involving control groups and broader samples is required to confirm the program’s efficacy. As sleep-related issues continue to affect public health, interventions like Sleep Reset offer promise for enhancing sleep health in various populations.
Editor’s note: This article was adapted from Gorovoy SB, Campbell RL, Fox RS and Grandner MA (2023) App-supported sleep coaching: implications for sleep duration and sleep quality. Front. Sleep 2:1156844. doi: 10.3389/frsle.2023.1156844 and the complete article can be accessed here: https://www.frontiersin.org/articles/10.3389/ frsle.2023.1156844/full



Everybody has a bad dream from time to time, and everybody has had the experience of a nightmare. They are a universal phenomenon commonly experienced during childhood and may persist throughout adulthood. Frightening dreams that awaken us out of REM sleep, nightmares, are often related to anxiety, stress, and trauma. The peak age for nightmares is between 6–10 years old with boys and girls being equally affected. Over the age of 12 years, girls have more nightmares. While the predominant emotions in nightmares are fear and anxiety, anger, embarrassment, and sadness may also be present.
Nightmare disorder is a clinical diagnosis based on history taking and requires that ICSD-3 criteria be met. Frequency of nightmares should be 3 times a week for at least three months. They can be precipitated by various factors. These could include generalized stress or a specific emotional trauma e.g. a car accident, war, or sexual assault. They are common in the diagnosis of post-traumatic stress disorder (PTSD). They can also be seen in the very common diagnoses of depression and anxiety. Their etiology could be based in a physiological route, however.
For example, certain medications can promote vivid dreams or nightmares. These can include over-the-counter drugs, like melatonin or antihistamines, or commonly prescribed medications, such as beta-blockers for hypertension, dopamine agonists for Restless Leg Syndrome or Parkinson disease, or mirtazapine, which is often used for depression, or off label as a sleeping pill. The relatively new class of sleeping pills, dual orexin agonists (DORA) such as Belsomra, Dayvigo, and Quviviq, are also associated with vivid dreams and nightmares. Sometimes a nightmare could be triggered by cessation of a medication and can be part of its withdrawal phenomenon. For example, nightmares can be seen associated with the withdrawal of benzodiazepines, SSRIs, or alcohol. Untreated sleep apnea, which is more prevalent during the REM cycle of sleep, can be an easily treatable cause of nightmares, and a clue to its presence. A diagnostic polysomnogram or home sleep apnea study is generally not required for the diagnosis of nightmares unless a secondary medical disorder is suspected, such as sleep apnea. Treatment will depend on causation, but may include
prazosin, a well-tolerated alpha1-blocker, which can reduce trauma related nightmares.
Night terrors, also called sleep terrors, or pavor nocturnus, is a type of non-REM-related parasomnia which is an arousal from stage three sleep (N3). It is most common in children younger than five years of age when there is a higher prevalence of slowwave sleep. They occur in 5% of children and 1-2% of adults. There may be a genetic component. They tend to be benign, especially in children. They typically occur in the first third to the first half of sleep, when stage three is most prevalent. There are strong signs of autonomic activation, including sweating, fast heart rate, rapid breathing, flushing of the skin, and large pupils. The patient may scream, cry and appear panicked. Some patients sit up in their beds with their eyes open and seem to be awake, but are actually in deep slow wave sleep. They could flail or thrash in bed or get up from bed and sleep walk. They could grow combative and be a danger to themselves or others. Patients may be unresponsive during these episodes and can become more agitated when others try to console them. Unlike nightmares, where there usually is detailed recall of at least part of the scary dream, patients with night terrors typically have partial or complete amnesia for these episodes, which could last 1 to 10 minutes. While dramatic and often very disturbing (especially to the parents), night terrors usually only require reassurance from parents as treatment alone until the child grows out of it.
Night terrors in adults may be brought on by stressors such as psychological pressure

“Night terrors are most common in children younger than five years of age. The patient may scream, cry and appear panicked. Some patients sit up in their beds with their eyes open and seem to be awake, but are actually in deep slow wave sleep.”

or trauma, sleep deprivation, alcohol use, and shift work. Depression, anxiety, PTSD, phobias, obsessive compulsive disorder, and other psychiatric comorbidities should be evaluated in adults. If another sleep disorder or medical problem is suspected, a further work up may be needed. An in-lab polysomnogram with an extended EEG montage may be required to rule out nocturnal seizures. A polysomnogram will also rule out sleep apnea and periodic limb movement disorder which may lead to arousals from sleep into wake. Practicing good sleep hygiene such as a consistent bedtime and wake time may help prevent night terrors along with avoiding alcohol use close to bedtime. Although there are no FDA-approved drugs for nonREM parasomnias like night terrors, benzodiazepines or tricyclic agents are sometimes prescribed off-label. Medications are usually reserved for frequent episodes or those which may pose safety issues.
Dr. Sahni has been in medical practice for 22 years. The first 11 years of her career she was an internist at Canyon Ranch Health resort. Since then, she has practiced sleep medicine exclusively. She opened her own practice, Swan Sleep Medicine, four years ago. When asked why she chose sleep medicine, she often jokes that she could not commit to a single organ. Fortunately, sleep medicine is a combination of pulmonology, cardiology, neurology, and psychiatry. Never boring, sleep medicine requires a multi-disciplinary approach to diagnosis and treatment. To that end, she has been certified in holistic medicine, nutrition, and Ayuvedic medicine as well as Sleep medicine. In general, sleep medicine is a happy field of
medicine.
When people are sleeping well, they feel more rested, of course, but also have better mood, sharper memories, lower heart risk, and stronger immunity. Dr. Sahni asks that you forgive the pun, but when sleep is improved, it’s like night and day! She evaluates patients in her office as well as administers home sleep tests to look for sleep apnea and insomnia studies to look at brain waves while sleeping. She treats a wide variety of adult sleep disorders. She is taking new patients.

Abnormal movements during sleep are common in early life — with between 15% to 20% of children experiencing this condition, and 4% continuing to have abnormal movements during sleep into adulthood.
This self-instructional course for dentists aims to define disorders associated with abnormal movements during sleep; offer a comprehensive view of the impacts, symptoms, and treatment of these disorders; and provide common language that dentists can use with other medical providers.
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
1. Understand how abnormal-movement sleep disorders are categorized
2. Understand how to take an appropriate patient history
3. Realize which diagnostic studies are required
4. Recognize the value in referring patients with symptoms of these movement disorders to the appropriate specialist
Abnormal movements during sleep can be divided into two categories:
A. Simple behaviors (single movements, repetitive, and periodic): These occur during the transition from wake to sleep or from sleep to wake and occur during stages N1 and/or N2 (NREM) sleep.
B. Complex behaviors (sleep talking, sleepwalking, night terrors, and dreaming enactment): Complex movements are disruptive and interfere with the control mechanisms within stages N1, N2, N3, and REM sleep.
We will focus on understanding how these disorders are categorized as well as understanding how to take an appropriate history, which diagnostic studies are required, and ultimately a summary of management tactics.
It is important to note that both simple abnormal movements and complex movements

can be seen during seizures, dissociative states, psychiatric episodes, or during periods of metabolic derangement (hypoglycemia).
Simple movements can be normal during childhood such as disorders of arousal, nightmares, and benign myoclonic jerks during infancy.
1. Hypnic Jerks
These are brief jerks of a whole body or can involve segments of the body. They primarily occur when falling asleep. They can occur at any age and are, for the most part, considered benign. They can be related to sleep deprivation, excessive caffeine intake, and can be associated with visual as well as auditory and tactile behaviors. They are sometimes known as “sensory starts” which are associated with hallucinations without motor involvement.
2. Exploding Head Syndrome
This is a benign sensory parasomnia. It is the sensation of hearing a loud sound during sleep-wake/wake-sleep transitions. It is multi-sensory and painless. In ICD3 coding, it is termed as “other parasomnias.” Often, it is misdiagnosed as a sub-arachnoid hemorrhage but usually not associated with any other signs or symptoms. Rarely, it can be associated with muscle jerks and twitching. More than 80% of those diagnosed have a feeling of impending doom and often will have tachycardia.
3. Propriospinal Myoclonus
This is associated with flexion or extension of the abdomen, trunk, or neck. This can occur during wakeful drowsiness (stage one sleep). It can occur throughout the day, and if so, is associated with spinal cord pathology. There is no evidence that it is only associated with sleep onset or structural nerve damage. MRIs are usually normal, but one in five people with this condition may have a focal lesion found in the spinal cord.
4. Epileptic Myoclonus
This is associated with sudden jerks of the limbs associated with waking or soon after waking. It is often seen in children and teenagers. It is very important to rule out juvenile myoclonic epilepsy (Primary Generalized Epilepsy).
5. Benign Myoclonus of Infancy (a.k.a. Benign Neonatal Sleep Myoclonus)
This condition includes brief bilateral, symmetric jerks of the limbs during NREM sleep in young infants. It occurs within the first few weeks of life, and it usually resolves by 2 to 3 months of age. It is often misdiagnosed as seizures. It only occurs during sleep, unlike myoclonic epilepsy that can occur during wakefulness. Infants go on to have normal development.
6. Sleep Related Bruxism (SRB)
SRB involves rhythmic and non-rhythmic clenching, jerking, and grinding of the muscles of mastication. It primarily occurs at sleep onset, with or without arousals, multiple times throughout the night. The outcome is usually dental wear, TMJ disorder, and headache. The anxiety trigger associated with bruxism is localized to the limbic part of the basal ganglia. Bruxism is thought to be a “protective” reflex attempt to open the airway and increase masseter tone. The brain goes into “survival mode” which activates the sympathetic nervous system to the open airway. The jaw pushes forward, and grinding bottom teeth press against the top to increase the volume of the airway.
In Upper Airway Resistance, narrowing between the retro-palatal and retroglossal areas lead to being unable to enter REM sleep. A similar condition that can occur with bruxism is Oral Mandibular Dys-

Bruxism is thought to be a “protective” reflex attempt to open the airway and increase masseter tone.
Amalia A. Geller, MD, is a board-certified Adult and Pediatric Neurologist with a subspecialty board certification in Sleep Medicine and additional post graduate fellowship training in Epilepsy and neurophysiology. She had a pediatric internship at Arnold Palmer Hospital for women and children and post graduate training in Child Neurology at the University of California at San Diego. Dr. Geller’s Neurophysiology and Epilepsy fellowships were performed at University of California at Irvine and her Sleep Medicine fellowship at the University of Texas Southwestern in Dallas. She is a full-time sleep medicine physician at Saint Alphonsus Sleep Medicine Center in Boise, Idaho. Her areas of interest include developing collaboration with sleep medicine dentists, orthodontists, oral myofunctional therapists, as well as ENT specialists for an integrative approach to pediatric sleep, focusing on airway management in malocclusion. Dr. Geller believes a comprehensive holistic integrative approach is what is imperative to treat children as a whole in order for them to achieve their maximum potential. Dr. Geller is the Nevada medical director for Nexus Dental Systems.
tonia (OMD). OMD is different because it is a sustained or intermittent muscle contraction and occurs later during the day, but not upon awakening like bruxism. The age of onset in OMD is in the fourth or fifth decades of life, whereas bruxism is childhood onset. Consider the patient with daily frontal headaches for bruxism. Patients with blepharospasm or cervical dystonia are at increased risk for bruxism.
7. Nocturnal Leg Cramps
This condition is defined by painful, sustained muscle contractions involving the calf, foot, and thighs. It can occur any time during the night during any sleep stage. The duration of action can be seconds to minutes. The primary differentiating feature versus other sleep-related leg movements is the sustained muscle contraction.

The primary differentiating feature for nocturnal leg cramps versus other sleep-related leg movements is the sustained muscle contraction.
1. Sleep-Related Rhythmic Movement Disorder
This involves large groups of muscles such as rolling and body rocking. It occurs in early childhood with sleep onset and is associated with normal development. When it involves interference with function, then it becomes known as Sleep Related Rhythmic Movement Disorder. It rarely affects adolescents and adults. Examples of factors involved would be obstructive sleep apnea and restless leg syndrome.
2. Hypnagogic Foot Tremor
This condition involves rapid, rhythmic movements occurring in only one foot at sleep onset and into light N2 sleep. It is not pathologic.
3. Alternating Leg Muscle Activation (ALMA)
This is activation of the anterior tibialis muscle in one leg with alternating in the other leg during sleep. It is associated with
arousals and not associated with any awareness. It can be associated with breathing-disordered sleep and periodic limb movements during sleep. It can be a side effect of taking serotonin reuptake inhibitors.
This condition is associated with clinically significant cortical arousals. Its repetitive movements occur every 5 to 90 seconds. It can only be diagnosed by polysomnography; it is not a clinical diagnosis. It occurs primarily during the first half of the night in stage 2 sleep. An increase of this condition is noted in the elderly with or without neurological problems.
Disorders of Arousal
This is a mixture of both NREM and wake where the two states combine. This could be due to the inability to fully allow or inhibit arousal from sleep, and it is primarily characterized by minimal cognitive function, amnesia, and features of appearing awake. This can be very common in children and adolescents. Triggers involve:
• Acute sleep deprivation
• Stress
• Breathing-disordered sleep
Examples of disorders of arousal include sleepwalking, confusional arousals, sleep terrors, and sleep-related eating disorders. Sleep-related eating disorder is a mixture of being awake and in NREM. It includes recurrent, involuntary amnestic eating of peculiar foods. There could be partial or no memory of the event. It can be associated with sedative hypnotics. For example, women on 5mg or greater of zolpidem have experienced sleep talking, sleep driving, confusional arousals, and sleep eating. It can also be associated with Restless Leg Syndrome. However, a differentiation exists between the Sleep-Related Eating Disorder and Night Eating Syndrome (NES). NES is recurrent episodes of hyperphagia during wakefulness, occurring in the middle of the night. It can lead to a delay in the circadian pattern of eating.
1. Recurrent Isolated Sleep Paralysis
Partial or complete inability to move; the intrusion and persistence of REM sleep-related atonia into wake. Events can be remembered for years later. Leads to a sense of impending doom and can occur as an isolated symptom. Triggers include:
• Sleep deprivation
• Childhood PTSD
• Chronic pain
• Depression
2. Nightmare Disorder
Complex visual imagery experienced during REM sleep carries over into wakefulness. It is usually associated with recall. It can involve motor components such as screaming, abrupt awakening, and sudden jerking. Violent dream enactment though is not nightmares. Nightmares are not night terrors (NREM/slow wave sleep). There is recall with nightmares, but usually no recall with night terrors.
3. REM Behavior Disorder
A pathologic loss of muscle paralysis (atonia) associated with vocalizations and complex movements. It is primarily seen in older men who have the beginnings of neurodegenerative diseases such as Parkinson’s Disease, multiple system atrophy, and dementia with Lewy body disease. It can be the harbinger of Alpha synuclein neurodegeneration. Young people who exhibit REM Behavior Disorder can have comorbidities with narcolepsy or exposure to serotonin reuptake inhibitors. It has also been associated with PTSD with or without traumatic brain injury.
4. Vocalizations
Vocalizations are common. They can be simple vocalizations or complex vocalizations and can be associated with sleep-related behaviors. They can occur with disorders of arousal. The primary difference between “physiological sleep talking” and Disorders of Arousal with REM sleep is when it involves the inclusion of motor behaviors. An example is expiratory groaning (carathrenia); this is a prolonged expiratory vocalization occurring during REM sleep. Carathrenia is often associated with obstructive sleep apnea.
5. Nocturnal Epilepsy
This can involve focal seizures and can be associated with stereotypical complex
behaviors. The primary feature of seizures versus parasomnias is seizures are stereotyped. Sleep-related Hypermotor Epilepsy is also known as Nocturnal Frontal Lobe Epilepsy. It can occur in late childhood to adulthood. A patient’s EEG is usually normal during wakefulness.
6. Panic/Dissociative Events
Most dissociative events are diurnal and associated with a history of post-traumatic stress disorder or major mood disorder.
The first goal is to obtain a clear patient history to rule out if there is any chance for selfharm and to determine the trigger(s). There are two questionnaires that can be helpful.
The Mayo Sleep Behavior Questionnaire contains 16 questions and can help distinguish between REM Behavior Disorder and Restless Leg symptoms. The FLEP Scale helps differentiate between frontal lobe epilepsy and parasomnias.
A complete history of the patient’s experience(s) should include the following categories:
• Predisposing factors
• Event description
°Eyewitness
°Time of the night
° Are they simple movements or complex movements?
° Are they nocturnal seizures or psychiatric?
• Duration of the event
°REM versus NREM
° REM Behavior Disorder: brief, lasting only seconds, rarely more than a minute.
° Disorders of Arousal: seconds to minutes.
° Frontal Lobe Epilepsy: behavioral and variable. Can last 30 seconds to 60 seconds.
° Psychiatric: can last 30 minutes up to an hour
• Variable versus stereotype behaviors
° Stereotype: seizures (with the exception of Rhythmic Movement Disorder and Periodically Movement Disorder during sleep)
The first step in the physical examination should be to detect if there are any signs of trauma, such as tooth wear, bruises on the body, or tongue biting.
°Polymorphic: less-likely seizure
• Eyes open versus eyes closed
°Disorders of Arousal: Eyes open
° Complex Movement Disorder/REM Behavior Disorder: Eyes closed
• Memory recall
°REM Behavior Disorder: Recall
°Disorders of Arousal: No recall
° Seizures: may have a recall if the seizure is brief and does not involve both temporal lobes. When both temporal lobes are involved, patients will have decreased memory recall.
• Age of onset
° NREM Parasomnia: Early childhood onset; resolved by adolescence
° REM Behavior Disorder: Older adult onset. In younger age groups, it could be related with narcolepsy.
• Family history of nocturnal events
The following triggers should be evaluated for each patient:
1. Poor sleep hygiene
2. Sleep deprivation
3. Circadian disturbance
4. Fever infection
5. Emotional stress
6. Medication used
7. Alcohol/sedatives/herbal supplements
• Non-benzodiazepine receptor agonists: zolpidem, zaleplon, and eszopiclone. These drugs are known to cause complex sleep-related behaviors such as sleep eating, sleep driving, and sleepwalking.
8. Medical problems
• COPD
• hypoglycemia
• gastroesophageal reflux disease (GERD)
• congestive heart failure
• renal disease
• neurological disease
9. Family history: genetic issues are often associated with arousals from NREM sleep
10. Other Sleep Disorders
• Obstructive Sleep Apnea will aggravate Disorders of Arousal such as with bruxism, epilepsy, and Rhythmic Movement Disorder.
• Narcolepsy
• Periodic Movement Disorder during sleep often causes a sleep disruption followed by daytime fatigue and daytime sleepiness.
The first step in the examination should be to detect if there are any signs of trauma, such as tooth wear, bruises on the body, or tongue biting. Then, check for signs of sleep fragmentation disorder, such as obstructive sleep apnea (hypertension increased, increased BMI, crowded nasopharynx, and posterior nasopharynx). Finally, if REM Behavior Disorder is indicated, look for signs of Parkinson’s disease such as cognitive impairment — lack of arm swing, mask-like faces, orthostatic hypotension, and hypokinesis.
Although the management of abnormal movements during sleep is usually overseen by a neurologist or sleep neurologist, the basics involve the following:
1. Identifying the triggers.
2. For Periodic Movement Disorders, implementing treatment options such as a foot wrap (Restiffic) and pharmacological agents with dopamine agonists and gabapentin.
3. For Parasomnias of unclear ideology, the most important aspect is to keep the patient safe. Patients should maintain an event diary and be referred to neurology for a video EEG.
1. Vaughan B, Avidan AY, Eichler AF. Approach to abnormal movements and behaviors during sleep. UpToDate. https://www.uptodate.com/contents/approach-to-abnormal-movements-andbehaviors-during-sleep (Accessed January 4, 2024).
2. Frisardi G, Iani C, Sau G, Frisardi F, Leornadis C, Lumbau A, Enrico P, Sirca D, Staderini EM, Chessa G. A relationship between bruxism and oral facial dystonia? A trigeminal electrophysiological approach in a case report of pineal cavernoma. Behav Brain Funct. 2013,9(41).
3. Yoshida K. Bruxism or Dystonia: That Is the Question. J Oral Maxillofac Surg. 2023 Aug;81(8):935-937.
4. Taylor M. Bruxism in the neurology clinic. Practical Neurology. September 2015;38-40.
5. Pocket Dentistry. Four Oral Motor Disorders: Bruxism, Dystonia, Dyskinesia and Drug-Induced Dystonic Extrapyramidal Reactions. 2016. https://pocketdentistry.com/four-oral-motor-disorders-bruxism-dystonia-dyskinesia-and-drug-induced-dystonic-extrapyramidal-reactions/. (Accessed January 4, 2024).
6. Heboyan A, Karobari MI, Alwadani AH, Marya A, Zafar MS. Bruxism as a consequence of stress and movement disorder: brief review. Eur J Gen Dent. 2002;11(2):81-83.
7. James L. Bruxism: the grind of the matter. [Course 485] Crest+OralB DentalCare.com. https://www.dentalcare.com/enus/ce-courses/ce485 (Accessed January 4, 2024).
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
n To receive credit:
AGD Code: 730
Date Published: February 15, 2024 Course Expires: February 15 2027 Legal
Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
1. Examples of simple movement disorders during sleep include _____________.
A. Hypnic Jerks
B. Exploding Head Syndrome
C. Propriospinal Myoclonus
D. Epileptic Myoclonus
E. All of the above
2. Benign sleep myoclonus of infancy occurs with brief jerks during REM sleep, is asymmetric, and resolves at 2 to 3 years of age
A. True
B False
3. does involve rapid movement of the foot and activation of the anterior tibialis muscles during NREM sleep.
A. Periodically Movement Disorder during sleep
B. Hypnagogic Foot Tremor
C. Alternating Leg Muscle Activation (ALMA)
D. Restless Leg Syndrome
4. Periodic Limb Movement disorder is a clinical diagnosis.
A. True
B. False
5. A condition that involves a mixture of NREM and wake with these two states combining, believed to be due to the inability to fully allow or suppress arousal, includes the following, except _________.
A. REM Behavior Disorder
B Disorders of Arousal
C. Associated with acute sleep deprivation, stress, or breathing disordered sleep
D. Associated with amnesia, patients can appear awake.
6. The symptoms of Oral Myofascial Dystonia are worse in the morning upon awakening compared to bruxism which worsens as the day progresses.
A. True
B. False
7. The anxiety that involves bruxism is localized to which neuroanatomical structure?
A. Parietal cortex/motor integration
B. Frontal Cortex: executive function
C. Premotor cortex
D. Occipital Lobe: visual motor cortex
E. None of the above.
8. Which anatomical areas are involved with sleep-related bruxism that involves narrowing which stops the person from entering REM sleep?
A. Frontal and maxillary sinuses
B. Upper and lower dental arches
C. Large broad-based tongue with fissuring
D. Retro-palatal and retro-glossal area
E. None of the above
9. __________ is the best position for a person to sleep in with bruxism.
A. Supine position
B. Side position
C. Prone position
D. Sleeping in a recliner
10. NES (Nighttime Eating Syndrome) is a disorder that occurs at the beginning of the night with recurrent episodes of hyperphagia and can cause delays in the circadian pattern of eating.
A. True
B. False
Did you know that insomnia can lead to heart health complications? Unfortunately, the truth is that this sleep disorder can increase the risk of heart disease, stroke, and heart failure, although it remains unclear whether insomnia causes these cardiovascular health issues or is merely linked with them. To learn more, continue reading below.

lized. As a result, blood vessels get damaged.
• Obesity – Weight gain is closely connected to lack of total and quality sleep since it affects the part of the brain responsible for controlling hunger and satiety.
of heart failure patients suffer from obstructive sleep apnea...
Insomnia is the most common sleep disorder affecting 10% to 15% of people worldwide characterized by difficulty falling, difficulty staying asleep, and/or waking up too early. A published study revealed that 44% of people with heart conditions experience insomnia frequently, also making it a common heart failure symptom (Bhaskar et al., 2016).
In addition, those who have all three insomnia symptoms, are at significantly higher risk, by more than three-fold, of heart failure. And, when it comes to the insomnia and heart failure connection, researchers came up with two theories: an underlying biological cause and the stress insomnia puts on the body takes a toll on heart health.
Insomnia increases the risk of heart disease and stroke in people who suffer from these conditions (all considered precursors to heart failure):
• Hypertension (high blood pressure) – Blood pressure typically decreases approximately 10-20% during sleep (nocturnal dipping). So, if you cannot sleep, your blood pressure remains higher for longer than usual.
• Diabetes (Type 2) – This chronic disease impacts how glucose (sugar) is metabo-
There are several sleep disorders common in heart patients that negatively affect sleep and can aggravate existing insomnia and sleep deprivation. These include:
Up to 50% of heart failure patients suffer from obstructive sleep apnea, a sleep disorder characterized by breathing interruptions during sleep (Khattak et al., 2018). This condition can result in many sudden arousals per night, leading to chronic sleep deprivation. Sleep apnea typically worsens heart failure and worsened heart failure worsens sleep apnea. Therefore, it’s a vicious cycle. Treating sleep apnea has proven to improve sleep, quality of life, mood, blood pressure, cardiac ejection fraction, irregular heartbeats, and vascular parameters.
When compared to the general population, heart failure patients are at a higher risk of developing two types of nocturnal movement disorders that negatively affect sleep. These include:
• Restless Legs Syndrome (RLS) – This sleep disorder is characterized by an urge to move the legs that usually occurs in the evenings typically described as a burning, twitching, and/or “creepy crawling” sensation which can

be relieved by moving the legs. As a consequence, these movements make falling asleep difficult.
• Periodic Limb Movements of Sleep (PLMS) – Similar to RLS, this disorder is also characterized by involuntary leg movements. However, it is different from RLS because these movements occur during sleep so the person may not even know they have the disorder. Still, it can disrupt sleep and lead to sleep deprivation. Statistically, 80% of individuals with RLS also have PLMS.
The bottom line, although not clear enough, there’s a strong link between insomnia and heart health. Hence, you need to improve your sleep to reduce your risk of heart failure, heart disease, and stroke. To do so, you have to take your sleep routine seriously and improve your sleep hygiene, but eventually, you will enjoy all the benefits that come with getting enough quality sleep.
1. Bhaskar, S., Hemavathy, D., & Prasad, S. (2016). Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. Journal of family medicine and primary care. https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC5353813/
2. Khattak, H. K., Hayat, F., Pamboukian, S. V., Hahn, H. S., Schwartz, B. P., & Stein, P. K. (2018, June 1). Obstructive sleep apnea in heart failure: Review of prevalence, treatment with continuous positive airway pressure, and prognosis. Texas Heart Institute journal. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6059510/#:~:text=The%20results%20of%20several%20studies,conditions)%2C%20AHI%20cutoff%2C%20and

Lee A. Surkin, MD, is the Chief Medical Officer of Nexus Dental Systems. A private practitioner in cardiology, sleep medicine, and obesity medicine, he is triple board certified in cardiology, sleep medicine, and nuclear cardiology. In 2009, he created Carolina Sleep – a dedicated sleep medicine practice in eastern NC. Dr. Surkin has created a cardiovascular and sleep healthcare model that includes a multi-faceted diagnostic and treatment approach that is enhanced by a network of relationships with physicians, dentists, respiratory therapists, sleep technologists, and public officials. In 2012, Dr. Surkin founded the American Academy of Cardiovascular Sleep Medicine which is a not-for-profit academic organization dedicated to educating healthcare providers, supporting research, and increasing public awareness of the convergence between cardiovascular disease and sleep disorders. In 2014, Dr. Surkin created a new multi-specialty practice called Carolina Clinic for Health and Wellness which combines his specialties with primary care, gynecology, behavioral health and a medical spa.


Dental sleep medicine changed my life and practice in immeasurable ways. I have made it my mission to screen every patient for signs of sleep disordered breathing, both children and adults. When caught early enough, we can spare our children from a lifetime of systemic health issues that arise from underdeveloped jaws. We HAVE to stop getting it wrong, for our kids, right now.
I am often asked what we did to grow our dental sleep practices so quickly. We average over 300 cases per year in one of our locations, due to a focus on saving lives. After an extensive education in obstructive sleep apnea (OSA) and sleep related breathing disorders (SRBD’s) in 2019, the first thing I changed was implementing a sleep questionnaire. We have since grown to 5 locations across the greater Houston area, with 3 offices focused entirely on pediatric growth/ development and adult oral appliance therapy/orthodontics.
Every patient, new or old, was asked to fill out a sleep questionnaire, so we could start having the right conversation (more to come

Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB, is passionate about how our teeth affect our systemic health – the link between chronic jaw infections, periodontal disease, and subsequent heart problems. Her training in obstructive sleep apnea has transformed both her personal and professional career. Dr. Hale is a Clinical Advocate for VIVOS Therapeutics and works with dentists around the country to develop clinical protocols for the treatment of mild to moderate obstructive sleep apnea and sleep-disordered breathing. Her work in pediatric expansion and sleep-disordered breathing catapulted her speaking career and she lives by the slogan “we have to stop getting it wrong, for our kids.” She is faculty for the Dental Success Network, a key-opinion leader for Candid, and the Chief Dental Officer for Toothpillow. She travels monthly across the U.S. and abroad to teach dentists about Obstructive Sleep Apnea. Learn more abour her sleep mentorship program at https://sleepwelljourney.com/.

Mentorship with a purpose
on this later). If you are new to this space and looking to add sleep to your arsenal of treatment options, take this elephant one bite at a time. What you will find is >80% of your patients are suffering from at least one symptom of poor sleep; and when you dig deeper into the specifics of pediatric growth/development you will find that nearly all children need early intervention orthodontics.
Gone are the days that we can ignore the symptoms of SRBD’s in our adult patients and “band-aid” them with poor solutions, such as occlusal guards. We must stop letting our patients damage their teeth and start identifying the root cause of their bruxism, mouth breathing, fatigue, etc. In addition, it is vital that we stop telling these parents their child’s snoring is normal and they will grow out of it! The ‘watch and wait method’ is no method at all and is dangerous to developing brains. In children, obstructive sleep apnea (OSA) can have significant effects on behavior, neurodevelopment, metabolism, and general health.1
There are many ways to treat this epidemic of sleep disordered breathing in dentistry. But to treat it, you must be able to identify it. Without the systems in place to properly screen your patients, you will fall short. Do not get overwhelmed by the multitude of oral appliance therapy options; start by educating yourself on the oral signs of sleep disordered breathing and then ask more questions. Find your tribe and band with the dentists in the trenches tackling this every day. You can save the lives of your patients and reduce the economic burden of obstructive sleep apnea our country is facing. You are not “just a dentist”, you are the most qualified person that exists to identify the glaring signs in someone’s mouth that they are struggling to breathe at night.
Watch for Dr. Hale’s next article: The First Thing I Got Wrong.
1. Kansagra S, Vaughn B. Pediatric sleep apnea: Five things you might not know. Neurol Clin Pract. 2013;3(4):321-325.








Iwill start by saying ‘there is literally nothing good about bad sleep.’ We all suffer from poor sleep from time to time and the inevitable brain fog the next day. However, when insufficient quantity or quality of sleep is a consistent feature, there are consequences, irrespective of age. It is not a good sign.

“All sleep problems benefit from early identification and treatment.”
Since Sleep-Wrecked Kids was first published in 2018, the subsequent research makes it sound like children’s sleep problems are getting worse, not better. I will share some of this new research. However, I see the increase in studies as a reason to be hopeful. More research means increasing awareness of both the prevalence and gravity of sleep problems in children. As the academic and medical world take poor sleep seriously, my hope is that this thinking will extend to parents and families, who are in the perfect position to be the lifeguards of their children’s sleep and transform their long-term outcomes. All sleep problems irrespective of cause or severity, benefit from early identification and treatment.
When I first published Sleep Wrecked Kids in 2018, I wrote about the many possible causes of sleep problems, some easy to fix with tweaks in the home, others requiring professional expertise. I wrote that up to twenty-four per cent of all children, and thirty-five per cent of children under two years of age, have frequent problems sleeping.1 Six years later, multiple studies show that we continue to face a global sleep-health crisis.
The ‘real’ figures are thought to be much higher. Further, over eighty per cent of sleep problems are going undetected in children.
The 2019 Parliamentary Enquiry into Sleep Health of Australians found that thirty-five percent of children snore, a figure
somewhat higher than the oft-quoted median statistic of habitual snoring of ten to twelve per cent and up to twenty-seven percent of children affected.2
Regardless of whether sleep problems are due to poor sleep health practices or diagnosable sleep disorders, they impact every domain of a child’s development: physical, mental, social and emotional. Kids with insufficient sleep showed smaller grey matter volume that lasted for two years.3 We cannot train kids to need less sleep. We simply need to ensure they get good sleep.
If we look at breathing issues that affect sleep and how they affect behaviour, a study in 2021 by the University of Maryland School of Medicine on 10,000 pre-adolescent kids showed that ‘children who regularly snore (three or more times per week), have structural changes in their brain that may explain the associated behavioural problems including lack of focus, hyperactivity, and learning difficulties at school.’4
When kids snore, even in the absence of hypoxic events, it disrupts sleep cycles resulting in behaviour, thinking and learning deficits the next day and further into the future.5 In fact, snoring is common among children who have ADHD, and up to twenty-five per cent of these children may have obstructive sleep apnoea (OSA).6
After insomnia, SDB is the second-most prevalent sleep disorder, with clear links to development of chronic inflammation.
Recent studies also indicate that cerebrovascular diseases and processes of atherosclerosis originate in childhood and are largely influenced by chronic inflammation.7,8
From a mental perspective, multiple studies show alterations in brain function, growth and development, related to untreated SDB that have short and long-term consequences; neuro-behavioural and neuro-cognitive.9-12 Perhaps the most illuminating studies are those that show a reduction of brain matter with SDB that may account for the known behavioural and cognitive challenges.13,14
A 2022 paper outlines the relationship of SDB and poor craniofacial growth, stressing the important role of general and paediatric dentists as part of a multidisciplinary team consisting of a pediatrician, ENT specialist, orthodontist, allied health professional, myofunctional therapist, and sleep medicine physician to manage all the downstream effects of abnormal anatomy and function that can lead to SDB.15-18
Dentists may identify the anatomical and other possible factors related to sleep disruption that may be correlated to increased airway collapsibility. Dentists can provide ongoing monitoring of craniofacial development in young children as part of regular dental care. Dentists can recognise and help prevent abnormal anatomy and function that are risk factors for SDB.
The ramifications of early sleep problems can follow children later in life with a 20-year follow up study showing that adults with a history of severe childhood OSA have a high risk of snoring, elevated body mass index, and lower academic achievement in adulthood along with increased risk of chronic diseases later in life.19 Further, in addition to learning and behaviour problems, speech and language difficulties are common in children with SDB which have significant effect on education and social outcomes.20
It is an exciting time to be involved in the world of sleep medicine.
Whilst the fundamental messages conveyed from the research, foresee much doom and gloom, they are in fact messages of great hope, because there is much that can be done to ensure every child gets the sleep they need every night to be healthy and happy. Our kids can’t afford to wait.
Editor’s note: This was first published as the preface for her book Sleep Wrecked Kids Japanese translation. Used with permission.
1. Olivero Bruni, ‘Insomnia: Clinical and Diagnostic Aspects’, World Sleep Society Conference (Prague, 2017).
2. Parliament of the Commonwealth of Australia: House of Representatives Standing Committee on Health, Aged Care and Sport. Inquiry into sleep health awareness in Australia, Hansard Hearing Melbourne, Hansard transcript. February 6, 2019.
3. Children Who Lack Sleep May Experience Detrimental Impact on Brain and Cognitive Development That Persists Over Time Neuroscience, July 31, 2022
4. Isaiah, A., Ernst, T., Cloak, C.C. et al. Associations between frontal lobe structure, parent-reported obstructive sleep disordered breathing and childhood behavior in the ABCD dataset. Nat Commun 12, 2205 (2021). https:// doi.org/10.1038/s41467-021-22534-0
5. Csábi, E., Gaál, V., Hallgató, E. et al. Increased behavioral problems in children with sleep-disordered breathing. Ital J Pediatr 48, 173 (2022). https://doi.org/10.1186/s13052-022-01364-w
6. Yoo Hyun Um, Seung-Chul Hong and Jong-Hyun Jeong, ‘Sleep Problems as Predictors in Attention-Deficit Hyperactivity Disorder: Causal Mechanisms, Consequences and Treatment’, Clinical Psychopharmacology and Neuroscience 15, no. 1 (2017): 9–18, https://doi.org/10.9758/cpn.2017.15.1.9.
7. Hertiš Petek T, Petek T, Močnik M, Marčun Varda N. Systemic Inflammation, Oxidative Stress and Cardiovascular Health in Children and Adolescents: A Systematic Review. Antioxidants (Basel). 2022 Apr 30;11(5):894. doi: 10.3390/antiox11050894. PMID: 35624760; PMCID: PMC9137597.
8. Kheirandish-Gozal L, Gozal D. Obstructive Sleep Apnea and Inflammation: Proof of Concept Based on Two Illustrative Cytokines. Int J Mol Sci. 2019 Jan 22;20(3):459. doi: 10.3390/ijms20030459. PMID: 30678164; PMCID: PMC6387387.
9. Brockmann PE, Gozal D. Neurocognitive Consequences in Children with Sleep Disordered Breathing: Who Is at Risk? Children (Basel). 2022 Aug25;9(9):1278. doi: 10.3390/children9091278. PMID: 36138586; PMCID: PMC9497121.
10. Isaiah, A., Ernst, T., Cloak, C.C. et al. Associations between frontal lobe structure, parent-reported obstructive sleep disordered breathing and childhood behavior in the ABCD dataset. Nat Commun 12, 2205 (2021). https:// doi.org/10.1038/s41467-021-22534-0
11. Harding R, Schaughency E, Haszard JJ, Gill AI, Luo R, Lobb C, Dawes P, Galland B. Sleep-Related Breathing Problem Trajectories Across Early Childhood and Academic Achievement-Related Performance at Age Eight. Front Psychol. 2021 Jun 29;12:661156. doi: 10.3389/fpsyg.2021.661156. PMID: 34267700; PMCID: PMC8276242.
12. Menzies B, Teng A, Burns M, Lah S. Neurocognitive outcomes of children with sleep disordered breathing: A systematic review with meta- analysis. Sleep Med Rev. 2022 Jun;63:101629. doi: 10.1016/j.smrv.2022.101629. Epub 2022 Mar 31. PMID: 35439720.
13. Moon C, Melah KE, Johnson SC, Bratzke LC. Sleep-disordered breathing, brain volume, and cognition in older individuals with heart failure. Brain Behav. 2018 Jul;8(7):e01029. doi: 10.1002/brb3.1029. Epub 2018 Jun 19. PMID: 29920994; PMCID: PMC6043704.
14. Philby MF, Macey PM, Ma RA, Kumar R, Gozal D, Kheirandish-Gozal L. Reduced Regional Grey Matter Volumes in Pediatric Obstructive Sleep
15. Tiina Ikävalko, Matti Närhi, Aino-Maija Eloranta, Niina Lintu, Riitta Myllykangas, Anu Vierola, Henri Tuomilehto, Timo Lakka, Riitta Pahkala, Predictors of sleep disordered breathing in children: the PANIC study, European Journal of Orthodontics, Volume 40, Issue 3, June 2018, Pages 268– 272, https://doi.org/10.1093/ejo/cjx056
16. Heit T, Tablizo BJ, Salud M, Mo F, Kang M, Tablizo MA, Witmans M. Craniofacial Sleep Medicine: The Important Role of Dental Providers in Detecting and Treating Sleep Disordered Breathing in Children. Children (Basel). 2022 Jul 15;9(7):1057. doi: 10.3390/children9071057. PMID: 35884041; PMCID: PMC9323037.
17. Saint-Fleur A.L., Christophides A., Gummalla P., Kier C. Much Ado about Sleep: Current Concepts on Mechanisms and Predisposition to Pediatric Obstructive Sleep Apnea. Children. 2021;8:1032. doi: 10.3390/ children8111032.
18. Hansen C., Markstrom A., Sonnesen L. Specific dento-craniofacial characteristics in non-syndromic children can predispose to sleep-disordered breathing. Acta Paediatr. 2022;111:473–477. doi: 10.1111/apa.16202.
19. Nosetti L, Zaffanello M, Katz ES, Vitali M, Agosti M, Ferrante G, Cilluffo G, Piacentini G, La Grutta S. Twenty-year follow-up of children with obstructive sleep apnea. J Clin Sleep Med. 2022 Jun 1;18(6):1. PMID: https:// pubmed.ncbi.nlm.nih.gov/35164899/
20. Mohammed D, Park V, Bogaardt H, Docking K. The impact of childhood obstructive sleep apnea on speech and oral language development: a systematic review. Sleep Med. 2021 May;81:144-153. doi: 10.1016/j. sleep.2021.02.015. Epub 2021 Feb 16. PMID: 33677253.

Sharon Moore is an author, speech pathologist and myofunctional practitioner with 40 years of clinical experience across a range of communication and swallowing disorders. Sharon has a special interest in early identification of craniofacial growth anomalies in children, concomitant orofacial dysfunctions, and airway obstruction in sleep disorders.

If you’re not already jazzed up by nitric oxide “NO”, buckle up for a deep dive into this multifarious messenger molecule that impacts vascular and metabolic functions. Learn how NO, SRBD and dentistry are inseparable. Gain an understanding of intrinsic and extrinsic factors influencing pathways of both NO production and inhibition, along with issues of bioavailability and health consequences. NO is at the crossroads of dentistry, airway, and total health, and this is where our journey begins.
There are two distinct pathways that produce NO in eukaryotic cells. One is an oxidative pathway which uses L-arginine as a substrate and produces NO and citrulline while the other is a reductive pathway to produce NO from nitrate and nitrite as substrates, all of which exhibit enhanced vasoactive signaling in hypoxia and stress.

The oxidative pathway, also referred to as the endogenous pathway, uses nitric oxide synthase “NOS” to convert L-arginine to NO and citrulline. NOS has three isoforms which have been identified as follows: neuronal NOS (nNOS or NOS 1), inducible NOS (iNOS or NOS 2), and endothelial NOS (eNOS or NOS3). See Figure 1.
eNOS is primarily involved in the regulation of vascular tone, inhibition of platelet aggregation, and atherosclerosis prevention and is produced by vascular endothelial cells. iNOS is rapidly upregulated in inflammatory and infectious conditions and is thought to be involved in septic shock and immune defense against: bacteria, viruses and other microbes. iNOS also helps in synaptic transmission including getting information from peripheral nerves to the brain. nNOS is most noted for production in neuronal tissue where its functions include synaptic plasticity, blood pressure regulation and pain perception.
The reductive pathway involves oral microbial communities which supplements endogenous NO production by reducing dietary nitrate to nitrite. This exogenous “enterosalivary” pathway starts in the mouth where oral bacterial reductases convert dietary nitrate to nitrite as a substrate.2 Some nitrite is further reduced to NO in the acid environment of the stomach and intestines. Nitrate and ni-
trite are absorbed in the intestines and into the blood. Excess nitrate (about 75%) is excreted by the kidneys. While Nitrite “NO2” in the blood is reduced to NO or oxidized to nitrate “NO3”, NO is oxidized to nitrite and nitrate. Finally, active uptake of nitrate from the blood then occurs in the salivary glands. See Figure 2.
Cardiovascular disease “CVD” is arguably the most significant consequence that connects NO and SRBD. NO protects against the onset and progression of CVD.2,3,4 Not only does hypoxia from SRBD decrease the oxygen necessary to make NO, but SRBD could also be described as the intermittent failure to transport the full complement of nasal NO to the lung with each breath. The nasal NO is mainly produced in the paranasal sinuses using iNOS.5,6 Interruption of NO supply to the tissues as well as lack of oxygen eventually leads to hypertension, myocardial infarction and stroke. Arguably the most important NO role is in vasodilation which is initiated by the stimulation of soluble guanylate cyclase, leading to increased production of cyclic guanosine monophosphate (GMP) from GTP that is dephosphorylated, which in turn activates GMP-dependent kinases to decrease intracellular calcium concentrations. This leads to relaxation of the smooth muscle cells in the media of the endothelium. Other roles of NO include the following: anti-thrombotic, anti-smooth muscle proliferation, anti-inflammatory, reduces release of and scavenges superoxide radicals, reduces oxidation of LDL cholesterol, reduces monocyte stickiness and adhesion which helps prevents plaque formation reducing risk of heart attack and stroke. And of course, it activates relaxation of corporal cavernosal smooth muscle tissue increasing blood flow in the penis resulting in an erection. See Figure 3.



Dr. Steve Lamberg has been practicing comprehensive restorative dentistry in Northport, NY for 40 years. Always passionate about sleep and wellness, he became a Diplomate of the American Board of Dental Sleep Medicine in 2011 and has served on their board review faculty. He holds several patents, and is the inventor of the Lamberg SleepWell Appliance, which is FDA-cleared for the treatment of OSA. Dr. Lamberg also launched and serves as the director of the Pediatric and Adult Airway Network of New York (PAANNY), to provide a local platform where dentists, physicians, orofacial myologists, and other related professionals learn and collaborate on treatment patients of all ages. Additionally, Dr. Lamberg serves as a Scientific Advisor at the Kois Center in Seattle. His recently published book for the general public, “Treat the Cause…Treat the Airway” correlates many common medical conditions to airway and sleep and is available on Amazon.
“NO is more relevant to the health span than you’ve ever imagined.”
Another prisoner of SRBD that relates to NO is dementia. It can be caused when SWS is decreased leading to decreased glymphatics which results in buildup of plaque in the glial cells. Dementia can also be caused by blood flow problems which is called vascular dementia “VaD”.7 VaD is the second most common dementia which occurs when eNOS is inactivated and leads to cerebral vascular endothelial dysfunction, while nNOS is overactive and can produce excessive NO resulting in neurotoxicity.
NO also plays a role in pulmonary arterial hypertension “PAH”. PAH with subsequent right ventricular failure can lead to death. Administration of nitric oxide by inhalation acutely improves hypoxemia associated with pulmonary hypertension in humans and animals. This is due to its ability to increase levels of cyclic GMP and induce pulmonary vasodilation. Drugs for treatment include phosphodiesterase-5 (PD-5) inhibitors which have been approved to control pulmonary vascular tone.
The exogenous enterosalivary pathway of reducing dietary nitrates, found in leafy green vegetables, to nitrite in the mouth has

some interesting connections with dentistry. The final reduction of nitrite to NO happens in the acidic environment of the stomach and intestines. This “enterosalivary” pathway is dependent on oral bacteria to produce the requisite reductase enzymes.2 The oral microbiome consists of commensal and pathogenic bacteria, both of which can produce reductases. Mouthwashes prescribed to reduce pathogenic bacteria may inhibit all bacteria which would decrease the production of reductases and greatly reduce this pathway for NO production. As it turns out, the pathogenic bacteria are more sensitive to higher pH rinses whereas the commensal bacteria are less affected by the higher pH mouthwashes. Due to this differential in pH impact on the oral biome it is recommended to use a high pH mouthwash to maintain the enterosalivary pathway for NO production while still being able to control the levels of pathogenic oral bacteria. This becomes even more important over the age of 50 when eNOS is decreased due to aging changes in the endothelium (Figure 4). Recent evidence shows that tongue cleaning does not have a negative affect on NO production.8
Can you have too much of a good thing? Although NO has an anti-inflammatory effect under normal physiological conditions, it is a pro-inflammatory mediator that induces inflammation due to over production in abnormal situations. As NO plays a role in inflammation, recent studies indicate that exhaled oral nitric oxide measurement in OSA may be used as a marker of upper airway obstructive episodes due to mechanical trauma and of hypoxemia causing local oropharyngeal inflammation. As well as being a possible risk factor of OSA, exhaled oral NO, through its ability to amplify oxidative and nitrosative stress may also have a pathogenetic role in OSA.9
NO is more relevant to the health span (the length of your lifetime that you’re healthy) than you’ve ever imagined. In addition to regulating vascular smooth muscle tone, NO directly affects mitochondrial respiration which can wreck havoc with carbohydrate metabolism. Studies show that NO plays important roles in the development of metabolic syndrome components such as: endothelial dysfunction, insulin resistance,

12 modules cover both the medical and dental science of sleep medicine. Dentists who complete the coursework and pass the exam are qualified to submit cases for board review to achieve Diplomate status.
The certificate is a prerequisite for ACSDD Fellow and Diplomate


“The saddest aspect of life right now is that science gathers knowledge faster than society gathers wisdom.” – Isaac Asimov

hypertriglyceridemia and chronic adipose tissue inflammation. Decreased eNOS-derived NO bioavailability as well as iNOS-induced overproduction of NO is involved in the development of type 2 diabetes mellitus (T2DM). NO donors may improve insulin signaling and glucose homeostasis in T2DM and insulin resistance (IR), suggesting the potential clinical importance of NO-based interventions.10
Inhibitors of NO include many factors such as: aging, oxidative stress, lack of exercise, poor nutrition, diet high in saturated fats11, diabetes, smoking, salt, non-basic pH mouthwash, high levels of ADMA12, SRBD, medications that reduce acid production in the stomach such as PPIs. Research shows being on PPIs for 3 years increased the rate of heart attack and stroke by 35%.
Upregulators of NO include the following: nasal breathing, eating vegetables high in nitrates (celery, garlic, cress, chervil, lettuce beetroot, spinach, arugula), and other
foods that support NOS bioavailability (meat and seafood that contain CoQ10, dark chocolate, citrus fruits, pomegranate, nuts and seeds, watermelon, and don’t forget the red wine!), antioxidants (Vit C, Vit E, Polyphenols, Glutathione, Melatonin), NO boosting supplements (L-Argenine, L-Citrulline), highest pH mouthwash, 30 mins per day exercise to keep endothelial cells healthy, and having good quality sleep. If all else fails, try listening to Barry White.
The next time you hear about NO you’ll not only appreciate its role in relaxation of blood vessels but also how it correlates with SRBD and so many dental conditions. This article can help you optimize your health and the health of your patients. Hopefully learning about the roles and misbehavior of NOS enzymes and their connection to mitochondrial health will pique your curiosity to learn more about the miracle molecule NO. How we build on this science and incorporate it into a workflow in our day to day dental practice is a topic for another article but spending more time on reviewing and discussing the medical history is a good place to start.
“The saddest aspect of life right now is that science gathers knowledge faster than society gathers wisdom.” – Isaac Asimov
1. Kawasumi, Takeno, Ishikawa, Takahara, Taruya, Takemoto, Hamamoto, Ishino, Ueda. The Functional Diversity of Nitric Oxide Synthase Isoforms in Human Nose and Paranasal Sinuses: Contrasting Pathophysiological Aspects in Nasal Allergy and Chronic Rhinosinusitis. Int. J. Mol. Sci. 2021, 22,7561.
2. Charlene E. Goh , BDS, DrPH; Bruno Bohn , MPH; Clarisse Marotz , PhD; Rebecca Molinsky , MPH; Sumith Roy , MBBS, MPH; Bruce J. Paster, PhD; Ching-Yuan Chen, PhD; Michael Rosenbaum, MD; Melana Yuzefpolskaya , Nitrite Generating and Depleting Capacity of the Oral Microbiome and Cardiometabolic Risk: Results from ORIGINS , J Am Heart Assoc. 2022
3. Jinqiang Zhu, Wanshan Song, Lin Li and Xiang Fan, Abstract Endothelial nitric oxide synthase: A potential therapeutic target for cerebrovascular diseases, Molecular Brain (2016) 9:30
4. He M, Wang D, Xu Y, Jiang F, Zheng J, Feng Y, Cao J, Zhou X. Nitric Oxide-Releasing Platforms for Treating Cardiovascular Disease. Pharmaceutics. 2022 Jun 25;14(7):1345.
5. JON O. LUNDBERG, Nitric Oxide and the Paranasal Sinuses, THE ANATOMICAL RECORD 291:1479–1484 (2008)
6. Remon Bazak, Samy Elwany, Amir Mina and Mostafa Donia, Nitric oxide unravels the enigmatic function of the paranasal sinuses: a review of literature, The Egyptian Journal of Otolaryngology (2020) 36:8
7. Zhu, Hong, Yang, The Roles of Nitric Oxide Synthase/Nitric Oxide Pathway in the Pathology of Vascular Dementia and Related Therapeutic Approaches. Int. J. Mol. Sci. 2021, 22, 4540.
8. Tribble GD, Angelov N, Weltman R, Wang B-Y, Eswaran SV, Gay IC, Parthasarathy K, Dao D-HV, Richardson KN, Ismail NM, Sharina IG, Hyde ER, Ajami NJ, Petrosino JF and Bryan NS (2019) Frequency of Tongue Cleaning Impacts the Human Tongue Microbiome Composition and Enterosalivary Circulation of Nitrate. Front. Cell. Infect. Microbiol. 9:39. doi: 10.3389/fcimb.2019
9. Feng X, Guo X, Lin J, Zhao Z, Tong Z. Risk factors and fraction of exhaled nitric oxide in obstructive sleep apnea in adults. J Int Med Research. 2020 Jul;48(7)
10. Bahadoran, Mirmiran, Ghasemi,Role of Nitric Oxide in Insulin Secretion and Glucose Metabolism,Trends in Endocrinology an dmetabolism, REVIEW VOLUME 31, ISSUE 2, P118-130, FEBRUARY 2020
11. Yvette C. Luiking, PhD, Mariëlle P.K.J. Engelen, PhD, and Nicolaas E.P. Deutz, MD, PhD, REGULATION OF NITRIC OXIDE PRODUCTION IN HEALTH AND DISEASE, Curr Opin Clin Nutr Metab Care. 2010 January ; 13(1): 97–104.
12. Mohammad Badran, Saeid Golbidi, Najib Ayas, and Ismail LaherNitric Oxide Bioavailability in Obstructive Sleep Apnea: Interplay of Asymmetric Dimethylarginine and Free Radicals Review Article, Sleep Disorders, Volume 2015, Article ID 387801





As a lab that is licensed to manufacture over a dozen of the top sleep devices, we spend most of our day coaching our clients to align their clinical findings, diagnosis, treatment plan, and insurance constraints with one of the 4 (A,B,C,D) mechanisms of mandibular advancements. Once we understand what the mouse needs, we can then select “the best” mouse trap. The following are “pearls of wisdom” that we have gathered from over 20 years of helping our clients to select “The Best” sleep device for their patient. I’ve also asked some of our clients for remarks about their clinical experiences.
The TAP Sleep Care (Airway Management, Inc.) device has been the leader in this category. Medicare approved. Thin overall profile with various material options for fit and comfort. Uses the anterior teeth to “engage/lock” the mandibular in position without a cumbersome buccal profile often seen in sleep devices.

I find the TAP design very helpful for patients with ‘supine dependent’ OSA – the interlock won’t let the jaw fall back in any position. It has very low buccal profile, so no metal to interfere with the cheeks – great for wide upper arches. Unique to TAP is a lip shield (I call it a nasal breathing trainer) that can be attached to the front to help seal the lips. I don’t use it with weak or heavily restored upper anterior teeth or when the patient has a large maxillary incisal angle. –
Steve Carstensen, DDS, DABDSMCommonly referred to as “herbst/hinge” and available through most brands (Apex Dental Sleep Lab, Inc., Oasys, Kava, SomnoMed North America, OravanOSA, ProSomnus® Sleep Technologies, Panthera Dental etc.) Often prescribed for compliance with Medicare guidelines/reimbursements. Available in many materials for comfort and durability with various technologies being utilized for manufacturing. Uses herbst hardware on the buccal to mechanically hinge and advance the mandible. The Oasys hinge is the most preferred mechanism in this category because of its simple adjustability, low profile, and least lateral restriction.
During the titration process, TMJ issues may occur. The fact that the appliance allows for lateral play and can be adjusted on both sides, gives it an advantage in redirecting the mandible to reduce or eliminate TMJ symptoms. –
J. Todd Gray, DDS, D.ASBADesign C – “Bilateral
Commonly known as “Dorsal” and available through most brands (SomnoMed North America, ProSomnus Sleep Technologies, Panthera Dental, Apex Dental Sleep Lab, Inc.) Originally made famous in North America by SomnoMed Team, the dorsal design has evolved significantly and is now available in milled PMMA and SLS Nylon.
The bilateral dorsal wings allow for simple and easy mandibular advancement while maintaining tongue space. The efficacy of this MAD has been well researched by industry leading companies such as SomnoMed Team, Panthera Dental, and ProSomnus Sleep Technologies.
The Dorsal Fin design for the oral appliance has served many patients who have a limited vestibular space between their cheeks and teeth. The key feature for me is to have a 90-degree angle of the maxillary block when it contacts the mandibular fin. This helps prevent the fin from disengaging while the patient is sleeping in a supine position and assures the mandible will not “fall back”. Two additional design features I favor are to place the Dorsal Fin mechanism in the first molar area, where the molar teeth are the most stabilizing to limit tooth movements and bite changes. The second feature is to be mindful of those patients who have nighttime Bruxism. If Bruxism is moderate to severe, perhaps another mechanism would be indicated. However, it is standard for me to request a vertical reinforcing metal support implanted within the Dorsal Fin to resist lateral forces and Fin Breakage. – Barry N. Chase, DDS, D.ABDSM
Originally introduced and patented by Dr. Don Frantz as the EMA (Elastic Mandibular Advancement), using a simple vacuform base design. This design has since been adapted to various forms such as the Medicare approved SLS Nylon D-SAD by Panthera Dental and the Avant by SomnoMed North America. This design category is the fastest growing because of its sleek and TMJ-friendly design. It appears that EMA will continue

to be the top contender as it evolves to add milling technology with a proprietary puck as well as the SLS nylon by Serena.
As it was stated in the opening of this article, there are many different dental sleep appliances on the market and they all will work to treat OSA. The key to success with treatment is a good examination of the patient to see the oral anatomy and what the needs of the patient are and then you can pick the appropriate appliance for that patient. Too many times we tend to buy into the newest, latest, and greatest appliance (as advertised by that company) and forget that all of them work and then put some of the best on the shelf while we try others. I have done this myself. Most of the time, I have gone back to one of the first appliances that I was introduced to, the EMA. With the different base materials available (milled and printed), one of the tried-and-true appliances is exceptional with minimal problems. This appliance is very easy for anyone to titrate themselves (even seniors), has a very low profile in the buccal area, has a very good lateral movement possible (for bruxers) and will withstand the forces exerted. I have used this appliance on hundreds of patients over the years and had very few failures with the treatment or problems with the appliance. One of the main drawbacks of the older versions, breakage of the plastic bases, is not an issue now. – Terry R. Bennett, DMD, DABCP,
Undoubtedly, these 4 mechanical designs categories are here to stay and fortunately, Apex Dental Sleep Lab, Inc. has long-standing manufacturing licenses with the top brands in each category. Thanks to our licensing partners for pushing the envelope of bioengineering.
Sonnie Bocola was born into a family with five generations of 16 Dentists, so it wasn’t a surprise when he decided to pursue the same career path. He graduated from San Diego State University in 2004 with a Bachelors in Cellular Molecular Micro-Biology. While awaiting acceptance to dental school, he began working for a private practice as a dental assistant. Very quickly Sonnie found his passion in the dental lab side of the industry and assumed the position as Director of International Lab Certification for TMJ and Sleep Research International from 2004-2016. He opened T & S Dental Lab, which he owned and operated from 2006-2016. This is where he began his journey that has led him to where he is today; having lectured internationally on TMJ, Sleep Therapy and oral appliance designs, and trained and certified international dental labs on the fabrication of TMJ orthotics. Currently, Sonnie is the President and owner of Apex Dental Sleep Lab, President of Sketchpad Innovations, Developer and Patent holder of Kava Mandibular Advancement device and a manufacturing consultant to EMA-Sleep.

About ten years ago I spent a few years at home with small kids and felt like I needed to break out of my predictable routine. I read an article about the growth of improv comedy classes and how adults were signing up for classes to try something new, meet new friends and face their fears. I was all in!
What is there to fear about improv comedy? How about standing in front of an audience without a script or any idea of what your fellow improv-ers are about to roll out? Fortunately, it doesn’t start there. I began with weekly classes trying out lots of exercises with one underlying principle: The unifying mantra running through all improv is the simple phrase “Yes, and”. This phrase encapsulates the idea that you must first accept whatever your scene partner throws out and then build upon it. You aren’t competing with your fellow improv partners; you’re working together to build the best possible scene.
What does any of this have to do with sleep apnea and dental sleep medicine? I see a lot of either/or treatments offered to patients, and I would love that to move to a more “Yes, and” approach. Marketing to patients pointing out benefits of oral appliance therapy versus CPAP is great but what about those patients for whom an oral appliance alone doesn’t entirely treat their sleep apnea? I’d love to see us incorporate messaging about combining therapies available to patients. The “Yes, and” principle applied to sleep apnea treatments.
I have been a CPAP user for more than 15 years. Like most sleep apnea patients, there was no discussion of additional treatment options that could be used together with CPAP. Last year, as I entered perimenopause, I experienced a sudden weight gain. My CPAP therapy needed to be adjusted. I had a sleep study, and my sleep specialist increased my
CPAP pressure. That’s when I started struggling with mask leaks, frequent awakenings at night and general discomfort at this new, higher pressure. As a veteran CPAP user, I knew all the tips and tricks to try but I started looking for ways to improve my comfort.
On my “Sleep Apnea Stories” podcast, I interviewed a patient who had added an oral appliance to her CPAP therapy. She explained that her pressure could be lowered because she was using the mandibular advancement device AND the CPAP together. This isn’t the case for every patient with severe sleep apnea, but I thought it was worth trying in my case.
So, I found an excellent dentist who specializes in dental sleep medicine here in Jacksonville, Florida by searching the AADSM website. When I met with Dr. Alan Krantz of ‘Dental Sleep Medicine of Jacksonville’ he seemed knowledgeable and did a thorough intake to check that an oral appliance was a good choice for me. We decided together on a ProSomnus EVO oral appliance and took the required digital measurements to have it made.
It took a few days to get used to wearing the appliance along with my CPAP and about a week to try different advancement settings. About a month later, I had an in-lab titrating study to adjust my CPAP pressure with me wearing my oral appliance. This allowed the pressure to be significantly lowered, and I found all the issues I was having with mask leaks and frequent awakenings resolved at this lower pressure.
I would love more patients to know about combining therapies. Right now, it can be difficult to get insurance to cover multiple treatment options, but we should work toward this being the norm if it helps patient outcomes. If you are a dentist building a dental sleep medicine practice, familiarizing yourself with other treatment options that can work well alongside an oral appliance is vital to ensure your patients are getting the best possible result. That could be adding CPAP therapy in collaboration with a sleep specialist for a patient with severe sleep apnea, like me. It might mean consulting with an ENT surgeon to improve nasal patency for a patient struggling to breathe through their nose.
Not every patient will be served best by an oral appliance on its own and in that case, a “Yes, and” approach is what’s needed. I’m not asking you to take improv classes and stand in front of an audience without a script. I am asking that you push yourself out of your
comfort zone and connect with other healthcare providers treating sleep apnea patients to come up with the very best treatment option, or combination of treatment options, for each patient.

Emma Cooksey is a podcast host and writer. She was diagnosed with obstructive sleep apnea at the age of 30, after more than a decade of unexplained health problems. By sharing her journey and encouraging others to tell their stories, Emma has been breaking down stereotypes of sleep apnea while also raising awareness of symptoms and treatment options. Emma hosts the weekly podcast, “Sleep Apnea Stories” and writes articles for Health Union’s patient support website. In January 2022, Emma was appointed to the board of directors of Project Sleep, a 501(c)(3) non-profit organization raising awareness about sleep health and sleep conditions.
Learn more about her podcast by visiting www.sleepapneastories.com or www.instagram.com/sleepapneastories.



In the realm of sleep dentistry, the management of obstructive sleep apnea (OSA) is a critical focus. Continuous Positive Airway Pressure (CPAP) therapy and oral appliance therapy (OAT) are common interventions, but they often come with challenges, particularly for patients who breathe through their mouths. The innovative SomnoSeal device offers a groundbreaking solution to these challenges, enhancing therapy efficacy and patient comfort.
The inception of SomnoSeal stemmed from a pressing need to address the discomfort and ineffectiveness caused by mouth leaks during CPAP therapy. Traditional solutions, such as chin straps, mouth tape, and full-face masks, were not well-tolerated due to discomfort. Thus, the development of SomnoSeal was propelled by a sleep medicine physician on the quest for a more patient-friendly solution. Designed to comfortably seal the lips from the inside, SomnoSeal creates a closed system, ensuring that the pressurized air from the CPAP machine is directed solely through the nasal and posterior pharyngeal passages.
Oral appliance therapy, another common treatment for OSA, can also benefit from the integration of SomnoSeal. While oral appliances are effective in maintaining an open airway by repositioning the jaw, they do not address the issue of mouth breathing. SomnoSeal complements oral appliance therapy by encouraging patients to breathe through their noses, thereby increasing the therapy’s overall effectiveness. It offers a comfortable alternative to mouth tape, which some patients find intolerable or inconvenient.
SomnoSeal enables mouth breathers to comfortably utilize smaller, nasal or nasal

pillow style CPAP masks, which are generally better tolerated than full-face masks, enhancing both comfort and compliance in therapy. Mouth leaks in CPAP therapy can significantly reduce the treatment’s effectiveness. Air escaping through the mouth leads to a decrease in the necessary airway pressure, resulting in suboptimal treatment outcomes. SomnoSeal addresses this issue by promoting nasal breathing and preventing mouth leaks. SomnoSeal not only enhances the efficacy of CPAP therapy but also alleviates the discomfort associated with dry mouth and sore throat, common side effects of mouth breathing during CPAP use.
Nasal breathing plays a crucial role in effective sleep apnea therapy. It not only helps in maintaining optimal oxygen levels but also contributes to better sleep quality. Nasal breathing warms and filters the air, making it more conducive to healthy respiration. By promoting nasal breathing, SomnoSeal helps ensure that patients receive the full therapeutic benefits of their treatment, whether through CPAP or oral appliance therapy.
In the landscape of sleep apnea treatment, the introduction of SomnoSeal marks a significant improvement over existing mouth closure methods such as chinstraps and mouth tape. These traditional modalities, while effective to an extent, come with their own set of drawbacks that can affect the overall treatment experience and efficacy.
Chinstraps, often used to prevent mouth
breathing during sleep, have a critical downside. By design, they can inadvertently pull the lower jaw backward. This backward movement of the jaw can exacerbate obstructive breathing, especially in patients with sleep apnea where airway patency is already a concern. The resultant effect can be a reduced effectiveness of CPAP. Patients with a history of TMJ disorders are more at risk with chinstraps also.
Mouth tape, another common solution for mouth leaks, presents its own set of challenges. Firstly, removing mouth tape can be difficult, especially in an emergency or groggy state upon waking. Secondly, it can cause skin irritation, making it uncomfortable for users with sensitive skin. Furthermore, mouth tape often fails to adhere properly in the presence of facial hair, limiting its applicability and effectiveness for a significant portion of patients.
SomnoSeal is designed to circumvent these issues effectively. Its key benefits include:
• Comfort: SomnoSeal is engineered to be comfortable for all-night wear, avoiding the discomfort associated with chinstraps and skin irritation common with mouth tape.
• Discretion: The in-mouth design of SomnoSeal is discreet, making it less obtrusive and more aesthetically acceptable to users compared to bulkier chinstraps or visible mouth tape.
• Reusability and Affordability: With a lifespan similar to CPAP masks, SomnoSeal is reusable and needs replacement only about every 90 days, making it an affordable and sustainable option.
• Compatibility: Unlike mouth tape, SomnoSeal is compatible with facial hair, ensuring effective use across a diverse patient population.
• No Compromise on Breathing: Importantly, SomnoSeal does not compromise the natural position of the jaw, ensuring that there is no additional risk of exacerbating obstructive breathing patterns during sleep. It ensures that
the mouth remains closed enhancing comfort and oral health.
By addressing the limitations of chinstraps and mouth tape, SomnoSeal stands out as a more patient-friendly, effective, and practical solution. Its ability to enhance comfort, ensure therapy compliance, and maintain airway patency without the drawbacks of traditional modalities positions it as a superior choice in mouth closure solutions.
The SomnoSeal device represents a significant advancement in the management of obstructive sleep apnea by addressing the challenges of mouth leaks in CPAP and oral appliance therapies. Its emphasis on promoting nasal breathing and eliminating dry mouth makes it a valuable tool for sleep dentists and their patients.
As sleep dentistry evolves, devices like SomnoSeal play a pivotal role in refining treatment strategies and improving the quality of life for those suffering from sleep apnea. Its development is not just a leap forward in sleep medicine technology; it also represents a significant stride forward in the collaboration between sleep medicine and sleep dentistry.
The SomnoSeal is now available for online purchase. For detailed information, including professional bulk discounts, visit www. SomnoSeal.com. Additionally, explore www. KimberlyMD.com for an extensive range of educational and patient empowerment tools, including the interactive CPAP101 online course, a library of informative videos, and our weekly ‘Sleep Bytes’ video series.

“SomnoSeal promotes nasal breathing and prevents mouth leaks.”
Kimberly Hutchison, MD, FAASM, serves as an associate professor of neurology and sleep medicine at Oregon Health and Science University in Portland, OR. Her diverse work spans clinical practices in neurology and sleep medicine and spearheading a remote sleep medicine program in Saipan for the underserved. Focused on improving sleep apnea care, Dr. Hutchison developed the SomnoSeal device to enhance treatment compliance. She also founded KimberlyMD.com, an educational hub offering resources like the CPAP101 course and weekly sleep-related videos. Discover more about her groundbreaking work at www.kimberlymd.com and learn about SomnoSeal at www.somnoseal.com.
There is a controversy looming in dentistry as it relates to the role of orthodontics in airway health.
• Should orthodontics only be concerned with smile esthetics, facial balance, periodontal health, occlusion, and stability?
• Should orthodontics including dento-facial orthopedics be concerned with airway / breathing disorders?
Orthodontic treatment has focused on smile esthetics, facial esthetics, and dental occlusion since its inception1 and ‘smile design’ has become an important aspect of esthetic dentistry and orthodontics.2 The human airway, especially as it relates to mouth breathing vs nasal breathing affecting health and craniofacial growth, has been an important topic in orthodontics for well over 100 years.3 Unfortunately, with the passage of time, this knowledge has been overlooked, misunderstood, criticized, and forgotten.
This article presents the connection of airway, breathing, smile esthetics, occlusion, and TMJ disorders and how these should be considered as integral parts of the education, training, and integration of a new orthodontic paradigm as research in medicine and dentistry are confirming that early screening for breathing disorders at age of 3 years old, and improving craniofacial growth early (before 6), improves not only dental and facial esthetics, periodontal health, and occlusion, but more importantly overall breathing and airway dynamics for improvement of long-term health.4 Furthermore, Welkoborsky et al. (2022)5 found that reproducible rhinomanometric measurements were possible in children aged 3 years and older prompting endorsements from academia healthcare system and providers known as “We Can See at 3”. This new finding prompts screening and rhinomanometry testing with patient cooperation as soon as 3. Sleep Disordered Breathing (SDB) in children and its long-term negative effects were first described by the late Christian Guilleminault, MD (‘CG’) one of the ‘fathers of sleep medicine’ at Stanford University in 1976.6,7 Early intervention and growth guidance were advocated by ‘CG’ and researchers presently at Stanford University6-10 and other experts at other prestigious universities and clinics around the world.6,11-13 This is now known as “fix before 6” by the Children’s Airway First Foundation www.childrensairwayfirst.org which was founded by Brad and Candy Sparks.
As stated by ‘CG’6,12,14 establishing proper nasal breathing is critical for improving health and decreasing the effects or possibly even eliminating potential co-morbidities later in life. These problems have been associated with obstructive breathing disorders, both during the day and asleep. Additional benefits include creating esthetic and functional results as part of the
complete orthodontic and dento-facial orthopedic treatment of our patients. Orthodontics / Dentistry / Dento-facial Orthopedics, which includes airway health, will bring medicine and dentistry closer together. An interdisciplinary team with other allied healthcare professionals and a coordinated approach with a common goal of airway and breathing health is the key to successful treatment of our mutual patients. Diverse opinions are shared and filtered with objective clinical and academic research, leading to diagnosis which then evolves into evidence-based and experience-based therapies. The success or failures of these therapies will vary from patient to patient and doctor to doctor for many reasons. These experiences circle back to confirm or refine the diagnosis and add to clinical knowledge when shared. Patients win when professionals, who may not totally agree with each other, openly share true experiences. Remember, at one time surgeons never washed their hands, put on gloves, or used masks.
Arthur Perry Gordy, DDS, an orthodontist from Columbus, GA, is quoted in his article of 192915 “In 1836 Charles Dickens, [in the “The Posthumous Papers of the Pickwick Club”16], pointed out the relationship between open mouth, backwardness, and delinquency, that would have saved millions of lives and would have averted millions of life failures had the civilized world realized the true importance of his [Dickens] words”. Dr. C.E. Kells of New Orleans (the father of dental radiography) sent this quote as part of his letter congratulating Dr. Gordy: “You have given the profession and the world something worthwhile, don’t be discouraged – remember Jenner, Pasteur, Roentgen and Wells”.15,17
Increased nasal resistance, from allergies, habits, or genetics, during growth years affects the craniofacial growth pattern by the
alteration of functional nasal airflow and an increased effort to nasal breathe.6,12 This increased effort and strain on the system affects the development of the heart, brain, and other organ systems of the body.18,19 Intraluminal pressure changes from respiratory effort cause structural effects such as narrowed naso-maxillary complex, enlarged turbinates, deviated septum, and altered posture of the mandible, tongue, and head. A conversion to mouth breathing leads to changes in brain function19, cardiovascular effects, a long facial growth pattern with an obtuse mandibular plane angle and TMJ degenerative changes, resulting in more clockwise rotation of the mandible and encroachment on the airway. This backward growth, along with a lower tongue posture and hyoid position, may lead to a more collapsed airway in the pharyngeal area and naso-maxillary complex in all 3 planes of space. This results in further increase in nasal resistance.20,21
Health professionals are concerned with long-term implications of this poor growth pattern. CG said, “Pediatric OSA in nonobese children is a disorder of oral-facial growth”.6 Because of the many signs, symptoms, and etiologies involved, evaluation and therapy by Allergist / Sleep Physician / Pediatrician / Dentist / Speech Pathologist / Myofunctional Therapists / ENT is critical for success. What is necessary is expertise in the growth of the craniofacial respiratory complex, more common in pediatric and orthodontic residencies than in many other parts of medical and dental training. Any or all of these disciplines may be required to meet the needs of the individual child at risk.
Static 2D imaging such as lateral cephalometric x-rays and advanced 3D volumes, like CBCT, are being used to evaluate the airway. No static imaging can provide dynamic functional information of airway resistance or air flow especially in the nasal region. Computational Fluid Dynamics (CFD), a computer modelling of airflow, and functional MRI (fMRI) of nasal vs. mouth breathing are promising new technologies that might be helpful but are just beginning to be researched. Changes to the pharyngeal airway between upright, supine, awake, and sleep states cannot be predicted by static imaging due to variable responses of airway dilator muscle activity and mucosal tissues.
When considering pressure changes and their effects on growth, principles of physics aid in the understanding of how an increase in nasal resistance creates an upstream problem for the craniofacial respiratory complex with a down-stream effect. A deviated septum (see Figures 1A and 1B) can cause a 38-55% increase in nasal resistance vs the open side and results in a pressure drop of 60 - 120%.22 In a growing child, this distorts the shape of airway structures, but is often not discovered until much later in life.
Deviated Septum (blue arrow) to the left and swollen right middle turbinate (red arrow) and swollen left inferior turbinate (yellow arrow). This is the same patient shown in Figures 3A-4C using 4-Phase Rhinomanometry and Acoustic Rhinometry.
The objective nasal resistance measurements correlate to the structural alterations. Also note the skeletal constriction of the naso-maxillary complex and the dentoalveolar maxillary constriction shown by the lingual inclinations of the maxillary first molars and the narrow maxillary intermolar width (orange arrow 28.2 mm, normal ranges from 36-49 mm4,12,23) contributing to the low tongue posture.
Smile esthetics has always been the main stay of traditional orthodontic therapy. The esthetic quality of the smile is improved with a wider smile, improved buccal corridors, and a consonant smile arc, etc. Expansion of the


William (Bill) Harrell, Jr., DMD, graduated from the University of Alabama School of Dentistry in Birmingham in 1975 and completed his orthodontic residency at the University of Pennsylvania School of Dental Medicine in 1977. He is a Board-Certified Orthodontist (ABO) in private practice in Alexander City, Alabama and Auburn/Opelika, Alabama. Dr. Harrell is also Certified in Dental Sleep Medicine. Dr. Harrell has served as VP and President of the Alabama Association of Orthodontists; as the Secretary-Treasurer, VP, and President of the 9th District Dental Society of Alabama; and served on The Board of Trustees and in the House of Delegates of the Alabama Dental Association. He has also served on various committees of the American Association of Orthodontists. Dr. Harrell is the first orthodontic private practice in Alabama to have ConeBeam CT (CBCT) and the first in the USA to combine both CBCT and 3D facial imaging (3dMD) in early 2005. Dr. Harrell’s practice focuses on airway centered orthodontic diagnosis and treatment and TMJ Disorders. Dr. Harrell is the Chairperson of the RadSite ConeBeam CT Standards Committee for setting standards for the Insurance industry of reimbursement.
maxillae and uprighting the teeth over basal bone while optimizing their AP location accomplishes these goals. Matching mandibular arch dimensions within the more limited boundary conditions available also improves tongue space and airway dimension in the naso-maxillary-mandibular complex. See Figures 2A-2C. Figures 2D and 2E shows after skeletal expansion either with surgery or skeletal/dentoalveolar enlargement using some form of palatal transverse expansion and/or uprighting and AP development when needed. This results in not only good smile and facial esthetics with broad arches and no dark buccal corridors, but also positively affecting airway dimensions with decreased resistance and increased airflow.
In an article by Eric Thuler, MD, PhD (Division of Sleep Surgery, Dept of Otorhinolaryngology, University of Pennsylvania – Perelman School of Medicine, Philadelphia, PA) entitled “Transverse Maxillary Deficiency Predicts Upper Airway Collapsibility during Drug-Induced Sleep Endoscopy”24,25 stated “Our results further the concept that skeletal restriction in the transverse dimension and hyoid descent are associated with elevations in pharyngeal collapsibility during sleep, suggesting a role of transverse deficiency in the pathogenesis of airway obstruction.”
Dynamic airflow through the nose should be objectively measured to aid evidence-based diagnosis and to monitor therapy. The technology is based on the pressure/flow relationship in the awake state in both sitting and supine positions. As a gold standard of care, each level of pressure change dictates the treatment option through interpretation as well as the monitoring of progress pre, mid and post treatment. The concept of the technology was founded on the physics of “Manometry”, the study of pressure measurements and function such as measuring air flow through Transnasal Pressure differences. See Figures 3A-3C. This data is obtained with 4-Phase Rhinomanometry, a technology invented and developed by Dr. Klaus Vogt, MD, DDS, PhD, an ENT, Dentist, and PhD since 1966.26
In 1983, The International Standardization Committee on the Objective Assessment of the Nasal Airway (ISCOANA) consisting of experts from Austria, Germany, Greece, Italy, Norway, Latvia and Ukraine, representing physics, mathematics, statistics, fluid dynamics, biotechnology and clinical rhinology was formed to write a consensus on the validity of objective measurements of the nasal airway. The committee, chaired and created by Dr. Vogt, last met in Riga, Latvia 2nd Nov. 2016 to address the existing nasal airway function tests and to take into account physical, mathematical and technical correctness as a base of international standardization as well as the requirements of the Council Directive 93/42/EEC of 14 June 1993 concerning medical devices. This was necessary because some of the diagnostic procedures currently in use in rhinology, and now dentistry, no longer fulfil the requirements of quality manage-
ment for medical devices. In addition, recent studies critically evaluating techniques for nasal airway assessment have not addressed technical progress in this field in recent years and the resulting experimental work, which has a great impact on daily practice.
Figure 3A shows the 4 Phase Rhinomanometer unit.
Figure 3B shows the Nasal Resistance graph of the right side. The “Tall Lazy S” represents a normal result. The Mean Resistance of the Right Inspiration is 0.262 and Right Expiration is 0.315, which are close to the normal range less than 0.33 Pa/cm3/sec. Normative values differ based on age, gender, race and other factors. Women have higher levels of nasal resistance than men, and children even higher, especially neonates. By age five, resistance decreases by 50%. There is continual reduction due to growth of the airway bounding structures until adult resistance is reached. Disease can disrupt this progression at any stage.
Figure 3C the left side, shows the graph as almost a flat line which shows severely limited nasal flow. Mean Resistance on Inspiration of 3.995 Pa/cm3/sec and on expiration of 12.391 Pa/cm3/sec. See CBCT in Figures 1A-B.
To enhance communication of outcomes, an algorithm has been developed by Karen Davidson, RN, PhD,27 called the DAFNE SCORE (www.DAFNESCORE.com), to help clarify the results and give suggestions of common therapies and interprofessional collaboration. The clinician enters data from rhinomanometry; the software provides medically sound guidance.
It is important to understand the differences between Rhinomanometry, a measurement of airflow, and Rhinometry, a structural assessment.
Rhinomanometry measures transnasal pressure differences in the nose – Resistance, Function, Flow. See Figures 3A-C




Acoustic Rhinometry measures structure/ geometry of the nasal cavity using sound waves like sonar. See Figures 4A-C.
Figure 4A shows the Acoustic Rhinometer being used. The tube sends sound waves (like Sonar) through the nose to determine structural integrity.
Figure 4B the nasal structure graphs are more closely aligned with the normal curve (Green Curved Line).

Figure 4C, the measurements of nasal structure in the nasal cavity show that the bottom graphs (Red/Blue Curved Lines) are well below the top graph (Green Curved Line) which represents the normal of nasal structure from the nares to the naso-pharynx). These graphs (Red/Blue Curved Lines) below the normal curve – Green Curved Line) represents significant structural abnormality which can be from hard tissues and/or soft tissue being responsible for the obstruction.
When decongested and repeated if the acoustic waves become closer to the “normal curve” that suggests a soft tissue issue. If there is little to no change, that represents a hard tissue problem. This is extremely important for




Figures 4A-4C: 4A. Patient being tested with Acoustic Rhinometer. 4B. Nasal structure graphs for right side. 4C. Nasal structure graphs for left side.


proper diagnosis of soft tissue issues vs hard tissue issues leading to proper therapy from a MD, ENT, Orthodontist, Dentist, etc.
A new comprehensive textbook to be published by Springer in mid-tolate 2024 entitled “Growing into Breathing Problems: The Quest for Collaborative Lifetime Solutions”11, will discuss the progression from pediatric sleep disorders to adult OSA. It will discuss pediatric and adult screening and diagnosis, medical and dental therapies, early vs late treatment options, myofunctional therapy, objective measurements of nasal resistance, surgical solutions, and much more.
The editors are: William E. Harrell, Jr, DMD, ABO, C.DSM (Private Orthodontic Practice Alexander City and Auburn/Opelika, Alabama, USA and Assistant Associate Professor in Orthodontics at the University of Alabama Birmingham School of Dentistry); David Gozal, MD, MBA, PhD (Pediatric Pulmonologist, Dean Joan Edwards Medical School Marshall University. the most prolific writer/author in the world on Sleep Disordered Breathing especially on Obstructive Sleep Apnea); and David McIntosh, MBBS, FRACS, PhD (Pediatric ENT, Queensland, Australia, author of several books).
The additional 25+ co-authors that are all well-known experts in their respective diversified fields of Sleep Medicine, ENT, Pediatrics, Neurology, Surgery, Dental Sleep Medicine, Dentistry, Pediatric Dentistry, Orthodontics, Speech Language Pathology, Myofunctional Therapy, Nursing, Legal, Standards, etc.
Mini, Micro, and Macro smile esthetics, smile projection, smile arc, consonant smile, buccal corridors, etc. are all considered esthetic qualities of a successful and esthetic orthodontic outcome.2 These qualities should be expanded (no pun intended) to the area of improving craniofacial growth, airway, breathing, and TMJ function. Our forefathers in orthodontics were very aware of how obstructed breathing alters craniofacial growth and its effect on the physiology of the body, the occlusion, and dental/facial esthetics.3 Sometimes, we must go Back into history ... in order to proceed to the Future.
1. Asbell MB. A brief history of orthodontics. Am J Orthod Dentofacial Orthop. 1990;98(3):206-13
2. Sarver D. Smile projection – A new concept in Smile Design, J Esthet Restor Dent 2021;33:237-252.
3. Ki Beom Kim, How has our interest in the airway changed over 100 years? Am J Orthod Dentofacial Orthop 2015 Nov;148(5):740-7.
4. Thuler E, Fabio A.W. Rabelo FAW, Yui M, Tominaga Q, dos Santos Jr V, Arap SS, Correlation between the transverse dimension of the maxilla, upper airway obstructive site, and OSA severity, Journal of Clinical Sleep Medicine, Vol. 17, No. 7, July 2021.
5. Welkoborsky, H.J., Rose-Diekmann, C., vor der Holte, A.P. et al. Clinical parameters influencing the results of anterior rhinomanometry in children. Eur Arch Otorhinolaryngol 279, 3963–3972 (2022).
https://doi.org/10.1007/s00405-02107218-1
6. Huang YS, Guilleminault C, Pediatric obstructive sleep apnea and the critical role of oral-facial growth: evidences, Front Neurol. 2013 Jan 22;3:184
7. Guilleminault C, Eldridge FL, Simmons FB, Dement WC. Sleep apnea in eight children, Pediatrics, 1976 Jul;58(1):23-3
8. Yoon A, Abdelwahab M, Bockow R, Vakili A, Lovel K, Chang I, Ganguly R, Liu SY, Kushida C, Hong C. Impact of rapid
palatal expansion on the size of adenoids and tonsils in children, Sleep medicine 2022 Apr;92:96-102.
9. Guilleminault C, Sullivan SS. Towards restoration of continuous nasal breathing as the ultimate goal in pediatric OSA. Enliven: Pediatr Neonatol Biol 2014;1(1)
10. Iwasaki T, Yoon A, Guilleminault C, Yamasaki Y, Liu SY. How does distraction osteogenesis maxillary expansion (DOME) reduce severity of obstructive sleep apnea? Sleep and Breathing December 2019
11. Harrell W, Gozal D, McIntosh D. Growing into breathing problems: the quest for collaborative lifetime solutions, Springer Publishing in Press 2024.
12. McNamara JA. Maxillary transverse deficiency. Am J Orthod Dentofacial Orthop. 2000;117:567-70.
13. Krishnaaswamy NR. Expansion in the absence of crossbite – rationale and protocol. APOS Trends Orthod 2019;9(3):126-37.
14. Marin-Oto M, Vicente EE, Marin JM. Long term management of obstructive sleep apnea and its comorbidities. Multidiscip Respir Med. 2019 Jul 4;14:21.
15. Gordy AP. Mouth breathing and a few facts seldom discussed. The cause, effect & treatment of malocclusion with specific reference to pernicious habits as affecting the physiognomy. Published and presented before the GA State Dental society, 1929.
16. Dickens C. The Posthumous Papers of the Pickwick Club. Chapman & Hall publishers 1836.
17. Gordy AP. Nose & throat conditions and allied habits in relation to irregularities of the teeth and development of the jaws. National Health Asso, 4th District Dental Society of GA, 1929.
18. Zelano C, Jiang H, Zhou G, Arora N, Schuele S, Rosenow J, Gottfried JA. Nasal Respiration Entrains Human Limbic Oscillations and Modulates Cognitive Function. J Neurosci. 2016;36(49):12448-12467.
19. Jung Ju-Yeon, and Kang Chang-Ki. Investigation on the Effect of Oral Breathing on Cognitive Activity Using Functional Brain Imaging, Healthcare (Basel) 2021 Jun; 9(6): 645
20. Harvold EP, Tomer BS, Vargervik K, Chierici G. Primate experiments on oral respiration. Am J Orthod, 1981, Apr;79(4):359-72.
21. Linder-Aronson S, Backstrom A. A comparison between mouth and nose breathers with respect to occlusion and facial dimensions. 1960, Orthod Revy 11:343
22. Corda JV, Shenoy BS, Lewis L, Prakashini K, Khader A, Ahmad KA, Zuber M. Nasal airflow patterns in a patient with septal deviation and comparison with a healthy nasal cavity using computational fluid dynamics. Front. Mech. Eng., Sec. Biomechanical Engineering Vol 8 - 25 November 2022.
23. Azlan A, Mardiati E, Evangelina IA, A gender-based comparison of intermolar width conducted at Padjajaran University Dental Hospital, Bandung, Indonesia, Dental Journal, Majalah Kedokteran Gigi, 2019, dec;52(4):168-171.
24. Thuler E, Seay EG, Woo J, Lee J, Jafari N, Keenan BT, Dedhia RC, Schwartz AR, Transverse Maxillary Deficiency Predicts Increased Upper Airway Collapsibility during Drug-Induced Sleep Endoscopy, Otolaryngology - Head and Neck Surgery, 2023, vol 169(2):412-421
25. Hutz MJ, Thuler E, Cheong C, Phung C, Evans M, Woo J; Keenan BT, Dedhia RC, The Association Between Transverse Maxillary Deficiency and Septal Deviation in Adults with Obstructive Sleep Apnea, Laryngoscope The American Laryngological, Rhinological and Otological Society, 2023
26. Vogt K, et. al. 4-Phase Rhinomanometry (4PR) – Basics and practice, Rhinol Suppl. 2010;21:1-50
27. Davidson K., Harrell W. Validation of a Novel User Interface and Calculation Method for Determining Nasal Resistance and Patency, in press 2024.
Continuing in our occasional series of talking to the founders of dental sleep medicine, this time I sat down with Laura Sheppard, one of the lab artists responsible ‘behind the scenes’ for DSM success. Here’s part of her story. A future issue will bring some critical tips from the laboratory professional.


Oral appliances to treat sleep or breathing disorders first appeared on my radar in the 1980’s. At the time, I was a lab technician specializing in TMJ & orthodontic appliances and working for Dental Services Group laboratories. This is when we first began to receive inquiries for palatal lifter appliances. This device resembled a maxillary orthodontic retainer with a small adjustable paddle-like extension. The paddle was designed to extend past the palatine bones, and its purpose was to hold up the soft tissue and keep the airway open for patients with muscular issues such as palatopharyngeal incompetence. These were worn full time, not just during sleep. Then, we started getting requests for tongue retaining devices. In 1982, there had been a compelling study conducted by Drs. R.D. Cartwright and C.F. Samelson regarding the importance of getting the relaxed tongue out of the airway during sleep. But for most people experiencing sleep and snoring problems, the standard non-surgical solutions were relegated to body positioning devices, chin straps, nose plugs, earplugs or sleeping alone.
Toward the end of the 80s with more awareness came more appliances being introduced to open the airway during sleep. Great Lakes Orthodontic Lab introduced the Tepper Oral Proprioceptive Stimulator (TOPS), invented by Dr. Harry Tepper. This device was worn on the upper arch and had a spring-activated flipper to stimulate the tongue during sleep. Then came the Snore Guard. Such a great name. To this day, many patients and practitioners still call a sleep appliance a ‘Snore Guard’. The actual Snore

Guard was invented by Dr. Thomas Meade. It was a single piece (fused monoblock) boiln-bite. It was an upper and lower mouthpiece that covered the anterior teeth. It was designed to keep the jaws end-to-end and mouth closed during sleep. Dr. Meade developed this concept by building from Dr. Wolfgang Schmidt-Nowara’s findings concerning the therapeutic airway benefit of mandibular repositioning and corresponding tongue positioning. This appliance would theoretically replace surgery by moving the mandible forward, thus advance the tongue out of the airway. Dr. Meade laid one of the first critical steppingstones for our appliance journey. For me, together with my early growth and development training, this ‘airway thread’ just kept growing in length and width. While the Snore Guard was a great concept, the design was fraught with side effects. The ‘end-to-end’ positioning did not work for all patients. And patients’ anterior teeth became sensitive. We noticed that anterior bites were opening due to hyper-eruption of uncovered posteriors. The boil-n-bite process and material itself were not ideal. Around this time, I received a call from John Tregillis, a dear technician friend from our partner laboratory in MN. He wanted me to get in touch with Dr. Jonathon Parker. Dr. Parker would become my mentor and dear friend. He would also become one of the finest educators in dental sleep medicine, teaching and mentoring countless successful practitioners in the field today. Dr. Parker was a TMJ specialist looking for technical support in developing a ‘Snore Guard-type’ device that was ‘custom-fit’ and full coverage. This became the PM Positioner. It solved several of the identified issues, but still was not an ideal design. Concurrently, Dr. Peter George, an orthodon-
Lighthouses Laura and Christina LaJoie with their mentors, Dr. Jonathon Parker and Dr. Alan Lowe
tist, introduced a similar custom made, fused mandibular repositioner called the Nocturnal Airway Patency Appliance (NAPA).
By this time, dentists started realizing a dual challenge. Every patient was different, possessing their own optimum therapeutic position. ‘How to measure and capture the bite?’ And, ‘How to adjust an appliance to test it – to the point of optimum?’ Dr. George went to work on the bite registration issue right away, inventing the George Gauge, the first bite registration tool to measure and capture protrusive positioning. Since these fused appliances could not be adjusted to the patient’s best position, the concept of the ‘trial’ appliance was developed. Trial appliances became a standard preliminary step to finding the optimal mandibular position, before manufacturing a final fused appliance.
The 1990’s ushered in adjustable appliances. Everything changed when Great Lakes Orthodontic Lab introduced the Klearway appliance invented by Dr. Alan Lowe, Professor and Chair of Orthodontics at the University of British Columbia, Vancouver,

Laura Sheppard BS, CDT, TE, is a practicing 40 year board-certified dental laboratory technician with her AAS in Dental Technology and BS in Education for Allied Health. Named to the ‘Top 25 Women in Dentistry’ roster by Dental Products Report, Laura has been nationally recognized and published as an expert and educator in the development and implementation of Dental Sleep Medicine and Quality Systems since 1993. As the design collaborator for DSG APM Positioner™ and DSG Remed-eze™, inventor for DSG Relaxer™, and co-inventor of MicrO2™ aka ProSomnus® AI, Laura’s expertise and contributions in dental sleep device invention, design, manufacturing, and regulatory compliance has been widely utilized to the success of many of today’s advanced sleep devices.
Canada. His design was the first custom-fit, upper and lower appliance that was not fused together. And it offered incremental adjustability for mandibular titration! I was thrilled, a valid treatment appliance made with orthodontic parts and mechanisms. This device was speaking my language.
Dr. Parker had prescribed many Klearway devices, and while treatment results were vastly improved, the appliance had some design related issues. The advancement screw was a Hyrax RPE screw turned laterally, which was rather large in the palatal space, and its long extended arms to the mandibular portion would adversely bend with patients’ functional forces. This resulted in a weak, fracture-prone area. So, together we came up with various design options to remedy these faults and created Dr. Parker’s Adjustable PM Positioner (APM). The APM utilized buccal advancement screws to avoid encroaching on the tongue space or the palate, but its fault was its limited lateral freedom.
Great Lakes Orthodontic Lab began to re-purpose the Herbst appliance as a sleep appliance. The Herbst had a long history of orthodontic mandibular repositioning for Class II patients to encourage condylar growth in adolescents. The Herbst arms were also buccally placed, but offered more lateral freedom. The Herbst flaws were related to wire framework fractures. In 1994, Dr. Keith Thornton, a TMJ and restorative dentist in TX, developed the Thornton Adjustable Positioner (TAP). The TAP appliance had a threaded adjustable hook placed on the upper midline positioned to engage a lower anterior bar. These main 4 adjustable appliances were demonstrating great results by being able to titrate to the optimal position for each patient.
Meanwhile, as we were each exploring our way into dental sleep therapy, a powerful nucleus of momentum was forming. A small motivated group of esteemed practitioners from across North America, equally passionate about the untreated sleep-deprived patient, started a study club which led to the formation of the Sleep Disorders Dental Society (SDDS) in 1992. Arthur Strauss, DDS; Peter George, DDS; Alan Lowe, DMD, PhD; Michael Alvarez, DDS; Gary Johnson, DDS; Jeffery Hall, DDS; and Don Rosenbloom, DDS were all committed to learning and experiencing as much about sleep and breath-
Honoring the OGs! Founders of the SDDS (from left) Arthur Strauss, DDS; Mary Beth Rogers, Robert Rogers, DMD; Michael lvarez, DDS; and Alan Lowe, DMD, PhD. Paying it forward. The lecture team at the Pankey Institute with (from left) Drs. Gy Yatros, Ed Zebovitz, and Steve Carstensen, and supporting team Glennine Varga, Christina and Laura.ing as possible. The SDDS would become the AADSM in 2006.
Attending my first SDDS meeting blew my mind! It was a pivotal point in my life. It was such a privilege to meet and engage with the founding doctors and the attendees. Mind you, it was a very small group at the time, no more than 50 people. But from the first, and until now, the AADSM doctors have always been the most receptive, open, curious, and caring group of physicians I have ever had the pleasure to work with. This is also where I first met my dear friend Christina LaJoie from Great Lakes Orthodontics Lab. I had met my tribe and gained a purpose.
The SDDS knew that it would be a long uphill battle to gain knowledge and credibility, and to provide awareness, resources, and education to interested treatment professionals everywhere. In the process, their challenges would come from all sides: the dental status quo, the medical community, public media, insurance companies, and the FDA. And dental laboratories and inventors would be challenged with continually improving appliance design. Every year the SDDS would come together, and we would share new research, developments, successes and realizations that would continue to raise the standard of care.
For example, by the mid-90s, there was no doubt that mandibular repositioning was working well. But in the process of conducting follow-up with their successful patients, Dr. Parker and his colleagues became aware of an irreversible side effect happening. Bites were changing. I remember the CEO of my laboratory company wore an APM Positioner for 3 years and we noticed he had a Class III bite that we had not seen before. When I voiced my concern that this may be from wearing the sleep appliance, he defensively stated “I’m not worried about my bite change, just don’t take away my appliance!” He felt his appliance helped him so much that it was worth sacrificing his normal occlusion. And he had been a dental lab guy all his life! As much as we were enjoying the success of mandibular repositioning, it was becoming more and more evident that these appliances were changing bites and occlusions. That’s when the concept of the morning aligner was developed. With a good morning exercise routine, the bite changes could be minimized. Going forward, the morning alignment routine became a standard of care recommendation.
Filling the need for improved treatment has always been my goal. For me, I am always looking for a better treatment design and improved materials. Thankfully, our 40 year evolution in device design has not disappointed. I have had the opportunity to work with many labs, inventors and designers to improve appliance design and manufacture. I’ve assisted in the development of successful patented devices and have provided guidance in understanding and implementing the requirements involved in FDA compliance and regulatory standards.
As for Christina and myself, it was as if we were two lighthouses, lighting and guiding our doctors’ journeys. And we reveled in their success. Through the years, many doctors would come to rely on us. Our labs promoted and sponsored many courses, presented at universities, and provided support materials, training assistance and demo appliances. Together, Christina and I have made this our mission for 40+ years. As was the nature of this group, personal competition was not in our purview. United and committed, we both knew the importance of this emerging field and respected each other’s different skill sets. Christina and I had the pleasure of working with, and coaching hundreds of doctors to start and succeed in practicing DSM. We even started the Lady Sleep Docs group, where most of our ladies became full-time practitioners and mentors, and many were elected to the highest leadership positions within the AADSM. And, we truly loved entertaining our doctors! We had so many good times and made a lot of great memories!
So much for my trip down memory lane. Next issue, I’m going to pass along some clinical/lab tips from these four decades I’ve enjoyed working with all of you.


 Our Annual AADSM Lady Sleep Doc dinners Celebrating Women Who Rock!
Our Annual AADSM Lady Sleep Doc dinners Celebrating Women Who Rock!
Did you know that the way you position your tongue can have an impact on the quality of your sleep? Tongue posture plays a crucial role in maintaining proper airway alignment during sleep. Adequate tongue posture affects breathing patterns and overall sleep quality. Improper, low resting position of the tongue during sleep can lead to the narrowing of the airway, which can then result in sleep-disordered breathing. By adopting correct tongue posture techniques, such as resting the tongue within the confines of the hard palate (roof of your mouth), you can promote better airflow, reduce the risk of snoring, and possibly even reduce certain sleep disorders.
“By facilitating natural arch expansion, promoting nasal breathing, and enhancing the overall quality of life, SPOT PAL contributes to the comprehensive well-being of our patients, especially children.”
– Lauren Argentina, DDS, PC,
Without the proper evaluation from a certified clinician, it’s often overlooked that an individual’s tongue is the root of the problem. However, with the world’s first custom-fit tongue training appliance, SPOT PAL™, your airway can open more easily than ever before.
SPOT PAL™ is designed to teach the proper resting posture of the tongue, thereby eliminating tongue thrusting and sucking habits. By encouraging the tongue to rest against the palate instead of the teeth, this unique appliance not only supports optimal oral health but also plays a vital role in an individual’s overall well-being. SPOT PAL™ increases the space in the airway by keeping the tongue in the correct resting posture and reduces the risk of the tongue infringing on the airway space. The “Spot Dot” feature provides a tactile cue for where the tongue tip should rest while the “tongue pokes” feature deters the tongue from resting on the teeth.


Janine Stiene, a highly regarded Speech Language Pathologist, Myofunctional Therapist, and the visionary creator behind SPOT PAL, emphasizes the importance of proper tongue resting posture: “SPOT PAL is the first-ever tongue training appliance designed to train

the tongue to rest up in the palate, and not against the teeth. Correct tongue resting posture is crucial for nasal breathing, proper development of orofacial musculature and structures, articulation and maximizing airway space. As a speech-language pathologist and myofunctional therapist, Spot Pal has proven to be an invaluable tool in our patients’ treatment and is seen as a revolutionary addition to dentistry.”
Recognizing the profound impact of SPOT PAL, Lauren Argentina, DDS, PC, an independent dental professional, shares her perspective: “Dentistry encompasses a complex system that goes far beyond teeth. SPOT PAL addresses some of the most challenging issues in dentistry, such as breaking non-nutritive sucking habits, correcting tongue thrusts, and teaching proper tongue posture on the palate. By facilitating natural arch expansion, promoting nasal breathing, and enhancing the overall quality of life, SPOT PAL contributes to the comprehensive well-being of our patients, especially children.”
SPOT PAL is for all ages and is customized to each individual and their needs. A 3D scan or dental impression is required to ensure a proper fit. SPOT PAL can be purchased at thespotpal.com. Embark on a journey towards revitalizing nights of deep and peaceful sleep by seeking guidance from a healthcare professional who can guide you to those restful nights you have always dreamed about!
TONGUE POKES

A custom-fit tongue training appliance designed to teach proper tongue resting posture resulting in: Reduced symptoms related to sleep disordered breathing
Improved articulation of lingual alveolar and palatal sounds.
Minimized symptoms associated with TMJ/D
Proper oral rest posture to eliminate lingual pressure against the dentition
To support the long term success of your patients!
Increases lingual strength, range of motion and tongue-jaw dissociation to maximize airway space, and proper oral posture and function for speech, breathing, and chewing/swallowing.
Promotes the habituation of proper lingual and labial resting posture which maximizes long-term retention.
Eliminates extraneous force on the dentition and/or palate to support natural growth and development of facial structure.
THE SPOT DOT WHERE TO REST YOUR TONGUE

DETER THE TONGUE FROM PUSHING ON THE TEETH














