


Retinal conditions rarely exist in isolation, and their interplay with systemic comorbidities significantly complicates patient care and outcomes. In this 36th issue of PIE, we delve deep into some retinal comorbidities and the latest breakthroughs in treatments transforming patient care.
First stop is exploring the delicate balance of anticoagulation management in vitreoretinal surgery (Anticoagulation Management in Vitreoretinal Surgery, page 6) and tackling one of the field’s most persistent challenges: treatment adherence in retinal conditions— The Adherence Equation, page 8—examines, according to The Barometer Global Survey, how we’re finally making headway in reducing the treatment burden that has long frustrated both patients and practitioners.
Also, we’re particularly excited to share promising developments in drug delivery systems, with hydrogels emerging as a potential game-changer in anti-VEGF therapy. This innovation could revolutionize how treatment intervals and clinic workflow are managed, offering hope for both healthcare providers and patients alike. Read the full article—When Less is More— on page 12.
Proliferative vitreoretinopathy (PVR) is being reframed as a biological continuum rather than merely a surgical challenge—a paradigm shift that opens new avenues for treatment (Quieting the PVR Storm, page 16).
In the article, From Degeneration to Regeneration (page 18), the quest for vision restoration in dry AMD continues to evolve, and we highlight the latest regenerative approaches that could reshape the therapeutic landscape.
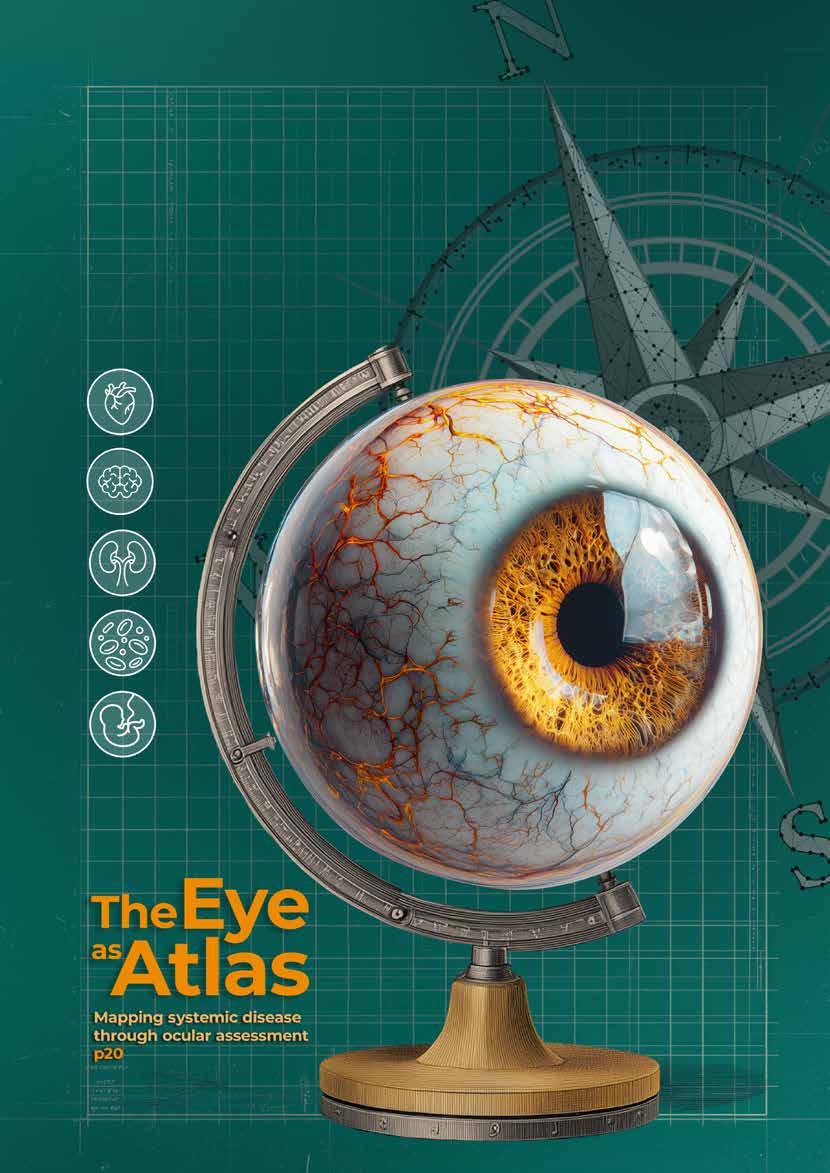
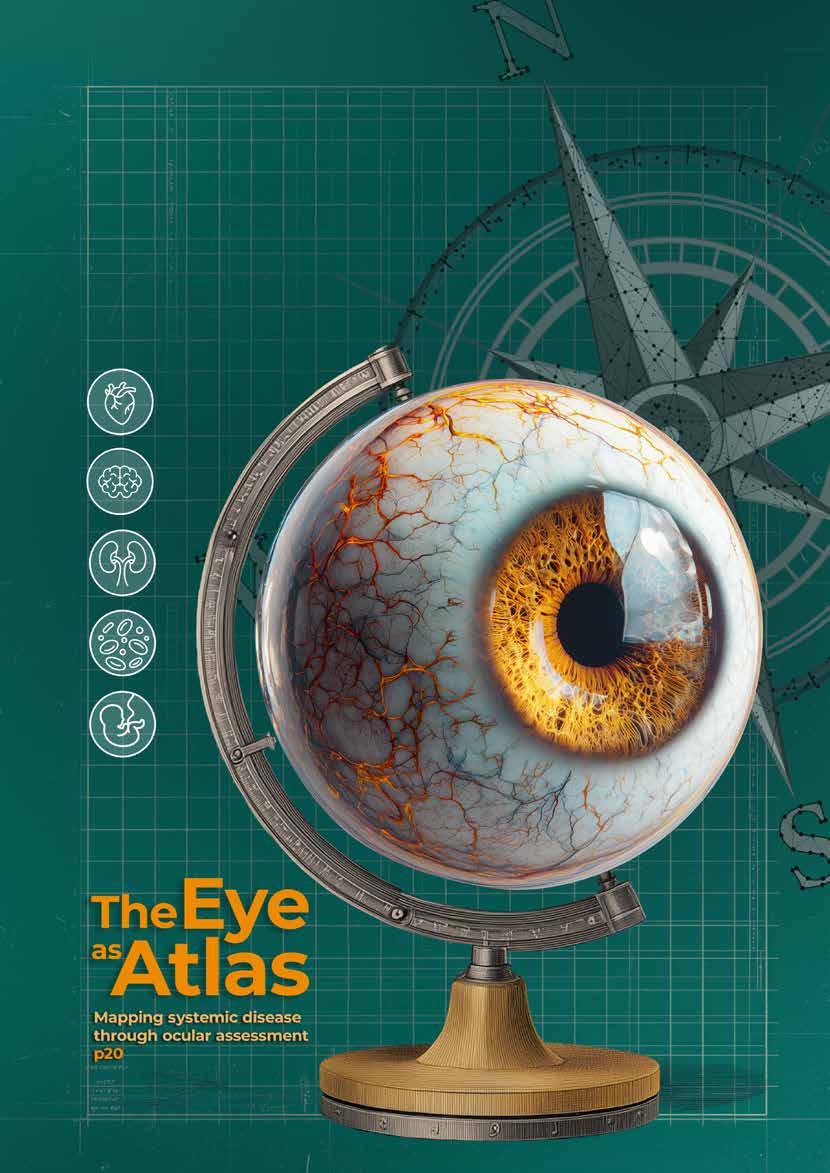
In this issue’s Cover Story—The Eye as Atlas (page 20) —we examine the eye’s role as a window to systemic health, exploring how ocular assessment can map and predict systemic diseases.
This issue’s Women in Ophthalmology section features Dr. Jesse Berry, director of Ocular Oncology and Retinoblastoma Programs at

Children’s Hospital Los Angeles (California, United States). This is the first time we are featuring a WIO in the challenging subspecialty of ocular oncology. In her field, Dr. Berry advances not only science, but also a vision of medicine where care, equity and humanity are inseparable.
Furthermore, in the Enlightenment section, we shine a light on two of the more complex discussions in retina today. On page 26, A Shot in the Dark? takes a closer look at the ongoing debate surrounding anti-VEGF therapy and systemic safety—an area where questions still linger despite years of widespread use. Then, on page 28, Uveitis Meets CSCR explores the delicate balance of managing inflammation and fluid, a clinical tightrope that challenges even the most experienced specialists. Both pieces underscore the importance of careful judgment, individualized care and the evolving science that continues to guide the ophthalmic field.
Last but not least, the Conference Highlights section features insights from ARVO 2025 and the recently held EURETINA 2025. At these meetings, innovative approaches to retinal repair that transcend traditional genetic therapies were showcased (Beyond the Genetic Code at ARVO 2025, page 34), while groundbreaking research on microglia, ischemia and vessel caliber offered new possibilities for early intervention in retinal disease (The Retina’s Early Warnings, page 32).
Finally, we extend our gratitude to our contributors, industry partners, collaborators and, most importantly, you—our readers—for your continued engagement with PIE magazine. Together, we are advancing the field of retinal care and working toward better solutions for both patients and practitioners.

Sincerely,
Gloria
D. Gamat
Chief Editor
| PIE, CAKE and COOKIE
Head, Editorial Department | Media MICE





Dr. Alay S. Banker
Banker’s Retina Clinic and Laser Centre Ahmedabad, India alay.banker@gmail.com

Dr. Arshad Khanani
Sierra Eye Associates; University of Nevada, Reno School of Medicine Nevada, USA arshad.khanani@gmail.com

Dr. Barbara Parolini
Eyecare Clinic Milan, Italy parolinibarbara@gmail.com

Prof. Gemmy Cheung
Singapore National Eye Centre (SNEC) Singapore gemmy.cheung.c.m@singhealth.com.sg

Dr. Hudson Nakamura
Bank of Goias Eye Foundation Goiânia, Brazil hudson.nakamura@gmail.com

Dr. Veeral Sheth
University Retina and Macula Associates; University of Illinois at Chicago, USA vsheth@gmail.com




For single-use on the ZEISS RESIGHT ®
• Perfect view in every case
Single-use means no scratches or opacities
• Always st erile
Minimizes risk of infection and cross-contamination
• Always available on the spot
Increase your O.R. capacity utilization


By Tan Sher Lynn
In vitreoretinal surgery, anticoagulants aren’t just pills, they’re pawns, bishops and knights on a high-stakes chessboard. Learn how one top surgeon weighs bleeding versus systemic risk to keep every patient (and every move) safely in play.
Managing anticoagulant and antiplatelet therapy in vitreoretinal surgery is less like following a playbook and more like a chess match. Every move must anticipate the next, balancing sightthreatening hemorrhage against lifethreatening thromboembolic events.
One false step, and the game could be lost on either side. Senior
consultant ophthalmologist and vitreoretinal surgeon Dr. Lee Shu Yen (Singapore) shared her perspective on how she keeps patients safely in play.
When determining whether to continue or withhold anticoagulation
therapy before surgery, Dr. Lee emphasized two primary considerations: the underlying medical reason for anticoagulation and the type of vitreoretinal procedure being performed.
“It would depend on the medical reason for requiring antiplatelet or anticoagulant therapy, for example, severe coronary artery disease,” she explained. “We have to work with the physicians to determine the feasibility and safety.”
The surgical indication itself also plays a pivotal role. “If it is a simple surgery such as for macula disorders, I will not stop the antiplatelet or anticoagulant,” Dr. Lee said. “But if it is a surgery where a lot of manipulation is required or if there is a high risk of bleeding such as for diabetic traction retinal detachment or proliferative vitreoretinopathy (PVR), I would work with the primary physician to stop the medications preoperatively.”
This patient-specific, case-by-case approach underscores the delicate balance between systemic and ocular risks. Even with the advent of newer oral anticoagulants and antiplatelet agents, Dr. Lee noted that her decision-making has not significantly changed compared to older therapies like warfarin or aspirin.
The key determinants remain the underlying indication for anticoagulation and the nature of the planned surgery, rather than the specific pharmacological agent.
A perennial question for surgeons is whether the benefits of continuing anticoagulation outweigh the risks of intraoperative or postoperative bleeding.
On one hand, continuation avoids exposing patients to life-threatening systemic complications such as stroke, myocardial infarction or pulmonary embolism, which can occur if therapy is interrupted. It also prevents the rebound hypercoagulability that may follow abrupt cessation. These systemic considerations often outweigh
the relatively small ocular risks in straightforward cases such as macular surgery.
On the other hand, anticoagulation can increase the likelihood of perioperative and postoperative hemorrhage, particularly in more complex surgeries requiring extensive membrane dissection or diathermy, such as proliferative diabetic retinopathy or proliferative vitreoretinopathy. In such high-risk situations, careful collaboration with physicians to temporarily stop therapy may be warranted.
Dr. Lee reiterated that her practice aligns with this risk–benefit reasoning, but she also pointed to advances in surgical technique that influence her decision-making, “With the smaller gauge surgery, I am less inclined to stop these preoperatively,” she explained.
Minimally invasive vitrectomy systems reduce tissue trauma and have lowered the incidence of hemorrhagic complications, shifting the balance toward continuation in certain cases and allowing surgeons to safeguard systemic health without unduly compromising ocular outcomes.
This perspective is echoed in a recent systematic review on antiplatelets and anticoagulants in vitreoretinal surgery, which concluded that, despite only one completed randomized controlled trial to date, the evidence is “nearly unanimous in recommending that patients continue taking antiplatelets and/or anticoagulants.”1
The review found no increased risk of hemorrhagic complications requiring secondary surgery in either pars plana vitrectomy or scleral buckle. On the contrary, continuation offers clear advantages: reducing delays between diagnosis and surgery while maintaining strong protection against cardioembolic events.1
For patients who must remain on anticoagulation, intraoperative and postoperative strategies become crucial. Dr. Lee outlined several
practical measures that she adopts to minimize bleeding risk.
“First, I press down a little longer after administering the periocular block,” she said, illustrating a simple step that can reduce the chance of periocular hemorrhage.
Intraoperatively, vigilance and preparedness are essential. “I would also be more alert and proactive with the endodiathermy usage intraoperatively to prevent uncontrolled hemorrhage,” she continued. “For example, diathermizing around the retinal break before trimming around to relieve the traction.”
She also noted her preference to avoid general anesthesia in such cases, further lowering the risk of bleeding-related complications.
Diabetic patients often pose particular challenges, as they are both more likely to require retinal surgery and more likely to be on systemic anticoagulation. For this group, Dr. Lee highlighted the importance of coordination and timing.
“I work with the physicians,” she said. “If stopping is necessary, then I would ensure adequate time preoperatively, and I would restart (the anticoagulation) postoperatively.”
This structured planning helps mitigate the competing risks of systemic events and surgical complications.
decisions are well-informed, balanced and aligned with both ocular and systemic health priorities.
For patients, transparent communication is equally vital. Helping them understand the risks of both bleeding and thrombosis fosters trust and shared decision-making, a cornerstone of modern surgical care.
Anticoagulation management in vitreoretinal surgery is not governed by rigid rules but by individualized assessment and multidisciplinary collaboration. Like a well-played chess-match, it’s about positioning, foresight and knowing which risks to trade. The ultimate goal? To safeguard vision without putting systemic health in check.
1. Confalonieri F, Ferraro V, Di Maria A, et al. Antiplatelets and anticoagulants in vitreoretinal surgery: A Systematic Review. Life. 2023;13(6):1362.

Perhaps one of the most important aspects of anticoagulation management is communication— both with patients and their cardiology or anesthesiology teams. Dr. Lee stressed the collaborative nature of these discussions.
“I would work with the physicians and the anesthetist,” she said. Such comanagement ensures that
Dr. Lee Shu Yen is a vitreoretinal surgeon at Advanced Eye Clinic & Surgery in Singapore, where she brings both precision and passion to the operating room. Trained at the Singapore National Eye Centre (SNEC) and the Lions Eye Institute in Perth, she has built her career around the delicate art of saving sight. Previously, Dr. Lee held leadership roles including head of Surgical Retina at SNEC, clinical director of the Retina Clinic at the Diabetes and Metabolism Centre, Singapore General Hospital, and director of the Operating Theatre and Inpatient Services at SNEC. She has also steered the profession forward as president of the Singapore Society of Ophthalmology and vice president of the College of Ophthalmologists, Academy of Medicine, Singapore. Her surgical interests include tackling the complex retinal complications of high myopia, such as myopic traction maculopathy—cases that demand both technical skill and creative problem-solving. A dedicated researcher and widely published author, Dr. Lee has advanced the field while mentoring countless residents and fellows in vitreoretinal surgery. Whether in the clinic, operating theatre or classroom, she’s committed to pushing boundaries in retina care and shaping the next generation of surgeons.
drlee@aecs.sg

By Kendra Bruning
From packed waiting rooms to shaky patient trust, the world’s biggest retina survey shows just how fragile adherence still is in 2025…and where clinics, tech and new therapies might finally lighten the load.

“E
very time I miss a shot, I see less. But I also might lose my job if I go. What would you choose?”
It’s a choice no one should have to make, yet in clinics around the world nearly two decades into the anti-vascular endothelial growth factor (anti-VEGF) era, patients with age-related macular degeneration (AMD) and diabetic macular edema
(DME) still face the impossible trade-off between sight and survival. The treatment burden, well-known for years, hasn’t disappeared, but in 2025, it has finally come into sharper focus with unprecedented global data to guide solutions.
The Barometer Global Survey, spanning 24 countries, over 10,000 voices and six continents, is the largest initiative of its kind.1,2
It captures the perspectives of patients, providers and clinic staff on the real-world friction of managing retinal disease.
While it confirms what many in the field already know—that treatment burden is high and adherence is fragile—it also offers something rare: clarity of direction and purpose. The data maps out where patients fall through the cracks and where clinics are struggling to catch them.
This feature goes beyond the headlines to ask: what does the data mean in the scheme of things? And how does the picture look different now that we’re seeing it clearly, all at once?
Seeing the big picture with the Barometer
The scope of the Barometer program is enough to make anyone sit up a little straighter in the exam chair. The initiative conducted parallel surveys drawing responses from:
• 4,558 nAMD patients, 659 providers and 1,208 clinic staff1
• 3,752 DME patients, 680 providers and 1,249 clinic staff2
• Across 77-78 ophthalmology clinics in 24 countries1,2
This isn’t a niche report. It’s a retina reality check, and the results paint a sobering picture of treatment adherence in 2025.
Almost half of all respondents said the frequency of treatment was overwhelming:
• 45.9% of nAMD and 51.7% of DME patients found treatment frequency too high1,2
• Nearly 50% cited long wait times as a major burden2
• A third of DME patients reported clinic visits lasting 2-4 hours1,2
Add to this the hidden costs like parking fees, transport struggles and unpaid leave, and it’s clear that injections are only one part of the story.
“Patients do not build trust in a perfectly efficient injection factory,” said Prof. Focke Ziemssen of
Eberhard Karls University. “What improves adherence is a balance of streamlined process and personal connection.”
Yet connection takes time, and time is in short supply. Over 60% of providers reported that clinic capacity limits patient outcomes. Nearly 80% flagged poor adherence in the first year of treatment as a major challenge.1,2 These findings point to broader challenges in how care is organized and delivered.
A clinical communication breakdown
The Barometer findings also uncovered a troubling trust gap between what patients believe and what doctors assume they understand:
“Patients do not build trust in a perfectly efficient injection factory. What improves adherence is a balance of streamlined process and personal connection.”
- Prof. Focke Ziemssen
• 22.5% of nAMD patients questioned whether treatment was necessary1
• 41.1% of DME patients weren’t sure how long treatment would last2
• 45.1% expected significant visual improvement, which isn’t always realistic1,2
“Even basic facts like ‘this is a chronic condition’ are not universally known,” said Prof. Ziemssen. “There can be no treatment adherence over many months if the patient doesn’t understand what’s meant by ‘chronic’.”
Assoc. Prof. Adrian Koh from Singapore agrees, explaining that “Thirty percent of patients were unsure if the treatment they were receiving was working or not. That tells me we are perhaps assuming too much about what patients understand.”
He’s introduced standardized counseling protocols in his clinic
to better align expectations, train support staff and deliver information at every phase, from diagnosis and loading to maintenance. “Without this clear understanding,” he said, “it’s not difficult to see why some patients default or give up.”
These insights help explain why adherence so often unravels, even when care is available. It’s not always the cost or the commute. Sometimes, it’s the context.
The good news is that the data doesn’t just highlight problems, it also points to real-world solutions that are gaining traction across different healthcare systems.
What patients are really asking for:
• Appointment reminders
• More time with their doctor
• Clarity about long-term expectations
• Consistency in care teams
• Tools to explain their condition to employers and caregivers1,2
Practical moves clinics are making:
• Nurse-led injection days to free up physician time
• Educational materials tailored to phase of care
• Visual OCT summaries to show progress
• Audits of no-shows and tailored follow-up
• Flexible communication methods for younger patients balancing work and treatment
“We’ve introduced a patient audit system,” said Dr. Koh, “to monitor and contact patients who don’t show up. And we use patient education tools developed by the Barometer program to support our staff and patients.”
Small shifts like these can ripple out into major improvements. But the system also needs to evolve.
Technology’s growing role in 2025
In 2025, technology is increasingly bridging the gap between clinic capacity and patient needs. Mobile apps now remind patients of
appointments, track symptoms and even provide virtual visual field tests between visits.3 Telehealth platforms offer remote monitoring for stable patients, reducing unnecessary travel while maintaining surveillance.4
These digital tools work best when tailored to patient demographics. While younger DME patients prefer app-based communications, older AMD patients often benefit from simplified phone reminders and family portal access.
Dr. Jane Barratt, Global Ageing and Health Systems Strategist, emphasizes the need to reframe vision care as public health infrastructure. “Adherence is not just a behavioral issue, it’s a system failure,” she said. “The pathway to treatment may be technically available but practically inaccessible.”
Her recommendation is to integrate eye health into primary and community care. That includes:
• Screening at the community level
• Transportation assistance
• Home visits where feasible
• Coverage for wraparound services under national health plans
And perhaps most importantly, a shift in mindset.
“Adherence is not just a behavioral issue, it’s a system failure. The pathway to treatment may be technically available but practically inaccessible.”
- Dr. Jane Barratt
“We need to move from seeing patients as passive recipients to people as partners in their health,” said Dr. Barratt. “That shift changes everything, from how we design care to how we define success.”
As care evolves, so does the therapy landscape. One of the

biggest regulatory shifts came earlier this year, when the European Commission approved Bayer’s Eylea 8mg (aflibercept) for use in nAMD and DME. The new formulation is now the only anti-VEGF therapy in the EU authorized for extended treatment intervals of up to five months, showing the growing demand for lower treatment burden and longerlasting control.5
China has also approved Eylea 8mg for nAMD, joining a growing list of more than 50 markets.6 The decision was backed by data from the PULSAR trial, which showed that the 8mg formulation matched standard Eylea in maintaining vision gains, while allowing for significantly longer intervals between injections.7
The therapy landscape continues to diversify beyond aflibercept. Port delivery systems, gene therapies and combination approaches are all advancing through clinical pipelines, promising to further reduce the injection burden in coming years.8
The hope is that longer intervals can lighten the load. But doctors are quick to note that this is not a silver bullet. “Longer intervals are welcome,” said Prof. Ziemssen, “but they can also lead to overconfidence. Patients assume they’re cured and drop off care.”
Even Bayer’s leadership team emphasized that long-duration therapies must be paired with systemic changes.
“The Global Survey produced valuable insights into the different struggles that patients with nAMD and DME face,” said Vice President, Global Ophthalmology Lead at Bayer, Anna Braeken. “It highlights the value of long duration therapies and allows us to uncover practical and meaningful interventions to help improve outcomes for patients.”
While treatment burden is universal, the Barometer data reveals the key regional nuances in adherence challenges.
In Asia-Pacific regions, family involvement is essential. Over 70% of patients rely on relatives for
transportation and support, and caregivers often attend appointments alongside patients. Yet logistical issues persist: 48.3% of nAMD patients in the region say they need help getting to clinics, and 45.7% struggle with scheduling.1
European clinics report better coverage, but capacity is a pressing issue. Patients cite long wait times, limited appointment availability and insufficient consultation time as major concerns. In Germany, for example, the emphasis is shifting toward communication-based interventions like tailored treatment plans and visual OCT summaries to mitigate misunderstanding and build trust.2
In North America, insurance constraints loom large. U.S. patients, in particular, expressed uncertainty around treatment costs, eligibility and long-term coverage.1 More than half of respondents flagged co-pays and out-of-pocket expenses as adherence barriers, even when clinics were geographically accessible.2
Each region faces a different flavor of the same problem. But across the board, a few constants remain: clear communication, continuous access and a coordinated care team.
“What works in Singapore may not work in Stockholm,” notes Prof. Koh. “But the fundamental need for clear communication, accessible care and realistic expectations is universal.”
It’s one thing to cite percentages and it’s quite another to hear what those percentages sound like in real patients’ lives.
“It’s like I’m alive again,” said Nicholas Berharovic, 81, who now receives quarterly rather than monthly injections. “Sticking to the monthly injection plan was a real pain… but now I can see my grandkids in Europe and still make it back for my next shot.”
Actress Juta Kamen, living with nAMD for 15 years, echoed that balance of resilience and realism.
“I go for long walks, write books and go on reading tours. I won’t let AMD
take that from me,” she said. “But I’m lucky to have support. That’s what makes this work.”
Not all patients are so fortunate. The data shows significant barriers remain:
• Over 50% of DME patients feel like a burden to family
• 40.8% struggle to find someone to accompany them
• 48.4% say transportation is a barrier1
Prof. Koh pointed to the mental health and occupational toll on younger patients. “Some struggle to explain their clinic visits to employers or teachers. Developing an information pack for supervisors to justify absences is one practical way we can better support them.”
Dr. Barratt believes the next step is reframing vision care as a public health issue.
“We need to embed vision screening, diagnosis, treatment and rehabilitation into primary care and community-based services,” she said. “This is about autonomy, participation and dignity.”
“The greatest opportunity lies in first understanding the landscape. When we clearly identify the barriers faced by patients, caregivers and clinic staff, we can tailor our strategies and build a more resilient, responsive system.”
- Assoc. Prof. Adrian Koh
Key recommendations include:
• Building vision care into universal health coverage
• Funding transportation, home care and culturally appropriate education
• Clinic audits to better understand drop-offs
• Simplified pathways with clear expectations
Prof. Ziemssen adds that Germany’s public coverage gives clinics room to innovate. “We can focus on how care is delivered, not just what’s delivered,” he said. “Long-acting agents used systematically can reduce the breaking points of a consistent therapy.”
“The greatest opportunity lies in first understanding the landscape,” said Prof. Koh. “When we clearly identify the barriers faced by patients, caregivers and clinic staff, we can tailor our strategies and build a more resilient, responsive system.”
So what does this mean in the scheme of things?
Treatment burden in 2025 is no longer a vague idea floating in the clinical ether. It has names, numbers and a paper trail. Adherence isn’t just a patient problem or a clinic problem. It’s both a system-wide challenge and an opportunity.
It means we know where the gaps are and who’s falling through them. It means we have data, tools and
References
1. Loewenstein A, Sylvanowicz M, Amoaku WM, et al. Global insights from patients, providers, and staff on challenges and solutions in managing neovascular age-related macular degeneration. Ophthalmol Ther. 2025;14:211-228.
stories that weren’t available a year ago. And most importantly, it means there’s no excuse for acting like adherence is still a mystery.

2025 may not be the year we solve the treatment burden, but it’s the year we ran out of reasons not to try. Looking ahead to 2026 and beyond, the field stands at an inflection point: with longer-acting therapies continuing to emerge and digital health solutions maturing, the focus must shift from identifying problems to scaling solutions.
The Barometer Survey brought the problem into focus. What comes next is keeping patients in the picture.
A version of this article was first published on piemagazine.org

2. Ziemssen F, Sylvanowicz M, Amoaku WM, et al. Improving clinical management of diabetic macular edema: Insights from a global survey of patients, healthcare providers, and clinic staff. Ophthalmol Ther. 2025;14:229-246.
3. Morjaria P, Massie J, Harvey A-A, et al. Application of mobile health (mHealth) in the field of eye care: a scoping review of interventions used by individuals and health services to communicate. Res Online LSHTM. 2025. Available at: https://researchonline. lshtm.ac.uk/id/eprint/4675888/ Accessed on June 10, 2025
4. Jacobs J, Sanborn G. A tele-ophthalmology model for remote monitoring of patients with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2023;64:1757.
5. Bayer. New Eylea 8 mg approved in EU for nAMD and DME. 2024. Available at: https://www.bayer. com/media/en-us/new-eylea-8-mg-approved-in-eu/ Accessed on June 10, 2025
6. Bayer. Eylea 8 mg approved in China for wet age-related macular degeneration. 2025. Available at: https://www.bayer.com/media/en-us/eylea-8mg-approved-in-china-for-wet-age-related-maculardegeneration/ Accessed on June 10, 2025
7. Lanzetta P, Korobelnik JF, Heier JS, et al. Intravitreal aflibercept 8 mg in neovascular age-related macular degeneration (PULSAR): 48-week results from a randomised, double-masked, non-inferiority, phase 3 trial. Lancet. 2024;403(10432):1141-1152.
8. Campochiaro PA, Avery R, Brown DM, et al. Gene therapy for neovascular age-related macular degeneration by subretinal delivery of RGX-314: A phase 1/2a dose-escalation study. Lancet. 2024;403(10438):1574-1584.
including
Prof. Focke Ziemssen is the newly appointed director of the Clinic and Polyclinic for Ophthalmology at University Hospital Leipzig in Germany. His academic path took him through Bochum, Bern and London, where his doctoral research uncovered new mutations in neuromuscular and metabolic diseases such as MODY. After completing his studies, he joined the University Eye Hospital in Tübingen in 2007, became adjunct professor the following year, and rose to vice director of the Centre for Ophthalmology in 2017 before taking up his current role in Leipzig in 2021.
Prof. Ziemssen’s research zeroes in on retinal disease mechanisms, pathological myopia and pharmacovigilance. With over 200 peer-reviewed publications and experience as principal investigator on numerous Phase II to IV clinical trials, he is deeply embedded in both scientific discovery and clinical practice. He also serves as a reviewer for more than 30 journals, including The Lancet, Ophthalmology, and IOVS.
Beyond research, Prof. Ziemssen plays a key role in shaping ophthalmic care in Germany and beyond. He is active in national and international societies, develops clinical guidelines and champions initiatives on diabetic eye disease and aging vision.
Focke.Ziemssen@medizin.uni-leipzig.de
Assoc. Prof. Adrian Koh is a founding partner and senior consultant at Eye & Retina Surgeons, Camden Medical, director of Retinal Centre International, and vice president of the International Retinal Foundation. He is also a visiting consultant at Singapore National Eye Centre and Tan Tock Seng Hospital, and serves on the Council of the College of Ophthalmologists, Academy of Medicine, Singapore. He is the immediate past president of the Singapore Society of Ophthalmology and has held leadership roles in APAO, Retina International and the Retinitis Pigmentosa Society of Singapore.
Dr. Koh trained at Moorfields Eye Hospital, London, and the Jules Stein Eye Institute, UCLA, under world-renowned retina specialists. He specializes in degenerative macular diseases, diabetic retinopathy, inherited retinal conditions, visual electrophysiology and retinal vascular disease. He has extensive experience in advanced therapies including antiVEGF, photodynamic therapy, laser treatments and intravitreal adjunctive therapies.
A prolific researcher and educator, Dr. Koh has authored numerous publications and helped establish the ISCEV-standard visual electrophysiology laboratory at SNEC. He receives referrals locally and regionally for complex retinal cases, combining cutting-edge diagnostics with tailored treatment plans.
Passionate about both patient care and advancing the field of ophthalmology, Dr. Koh bridges science, technology and clinical expertise to improve vision outcomes for patients across Asia.
ahckoh@yahoo.com

With over 30 years of global leadership in health and aging, Dr. Jane Barratt is a trusted voice at the intersection of policy, practice and purpose. As the former secretary general of the International Federation on Ageing, she has helped shape major international frameworks—from the WHO Immunization Agenda 2030 to the UN Decade of Healthy Ageing— always championing systems that respect and respond to the dignity of older people.
Today, Jane works at the leading edge of global health reform— advising institutions, convening bold conversations and speaking around the world on what aging truly demands of us.
Her work bridges silos. Her words move rooms. And her focus is unwavering: evidence, equity and action.
jbarratt@drbarratt.com
By Diana Truong
Anti-VEGFs may still be “the one,” but hydrogels promise to make treatment a whole lot easier with steadier drug levels, longer intervals and fewer frazzled clinics.
In retina care, patients and their anti-vascular endothelial growth factor (anti-VEGF) injections are locked in what you might call a “complicated” relationship. It’s effective, yes, but hardly effortless. Regular meetups (a.k.a. injections) are essential to keep things on track, and the maintenance can be exhausting.
What if there was a way to ease the demands of this partnership: fewer appointments, fewer needles and a lot less strain?
That’s where hydrogel-based sustained delivery systems enter the picture. They’re the “relationship counselors” aiming to turn a highmaintenance arrangement into something more sustainable for both patients and providers.
For wet age-related macular degeneration (AMD), the “standard of care is repeated intravitreal injections of anti-VEGF biologics,” explains Dr. Rehan Hussain, a vitreoretinal surgeon at Midwest Regina Consultants (United States). These therapies are highly effective at reducing vascular leakage and macular edema, stabilizing or improving vision, and preventing blindness…so long as patients stick with the regimen.
The catch? Effectiveness comes at a cost: financial burden, time in the clinic and plenty of patient fatigue.
“The major clinical challenges are: frequent injection and clinic visits (monthly to every 8-12 weeks
depending on drug and regimen), adherence and access issues, patient/caregiver burden, cumulative cost and real-world undertreatment that leads to worse outcomes than seen in trials,” Dr. Hussain notes.
It’s a paradox: medicine that can preserve sight, yet the sheer frequency of injections makes it hard for patients to keep up. The result is a strained, complicated partnership between treatment effectiveness and real-world adherence.
So what exactly are hydrogels, and why all the buzz?
“Hydrogels are 3-D, water-rich polymer networks that can be engineered to carry drugs (small molecules, proteins, nanoparticles or cells) and release them over time,” explains Dr. Hussain.
Think of them as tiny drug couriers with remarkable adaptability. Hydrogels can be classified by their cross-linking method (physical or chemical), their origin (natural, synthetic or hybrid) and their sensitivity to environmental triggers (pH, temperature, light or reactive oxygen species).1
Their biggest strengths for eye care? Versatility and biocompatibility.
In practice, “hydrogels are often delivered into the vitreous either as performed implants or as injectable, in-situ-gelling formulations that solidify after administration,” says Dr. Hussain.
“Hydrogels are 3-D, water-rich polymer networks that can be engineered to carry drugs (small molecules, proteins, nanoparticles or cells) and release them over time.”
- Dr. Rehan Hussain
And their release strategies are equally clever:2
1. Diffusion. Slow and steady release through the hydrogel mesh.
2. Hydrogel degradation. Enzymatic or hydrolytic breakdown that lets the drug payload loose.
3. Combination systems. Nanoparticles or microspheres tucked inside for a staged, multiphase release.
This flexibility allows scientists to fine-tune how drugs like anti-VEGF agents are delivered, potentially rewriting the rulebook on how we treat chronic retinal disease.
Hydrogels might just be the counseling partner this complicated relationship needs.
“Major potential advantages include sustained release that reduces injection frequency (fewer clinic visits, improved adherence), localized, high intraocular drug concentrations with reduced systemic exposure, and reduced peaks and troughs in drug vitreous concentration, which results in steadier control of neovascular activity,” says Dr. Hussain.
Translation: unlike the highs and lows of conventional
injections, hydrogel systems aim to provide steady, consistent drug levels over extended periods.
But the appeal doesn’t stop there. They’re also versatile carriers. “They can carry native proteins, modified proteins or drug-loaded particles, and can be engineered for refillable or biodegradable approaches,” Dr. Hussain notes.
And when stacked up against other long-term delivery methods, hydrogels may just be the “Goldilocks” option. Not too invasive, not too permanent, but just right.
As Dr. Hussain explains, “Hydrogels may sit between these approaches— less invasive than the Port Delivery System (most hydrogel designs are injectable and do not require surgery) and less permanent and complex than gene therapy—with a potentially favorable safety profile.”
Among the hydrogel-based delivery systems in development, an axitinib implant (Axpaxli, formerly OTX-TKI) from Ocular Therapeutix (Massachusetts, United States) is furthest along in clinical development.
“Axpaxli is a bioresorbable intravitreal hydrogel implant using Ocular Therapeutix’s ELUTYX formulation technology, loaded with axitinib, a potent tyrosine kinase inhibitor targeting VEGF receptors,” Dr. Hussain explains.
The Phase II trial of the axitinib implant showed a reduced treatment burden compared to aflibercept every eight weeks.3 Phase III trials are now underway.4
The ultimate goal? Extending dosing intervals to every six months.4 While not yet clinically validated, reaching that milestone could significantly reduce the treatment load for patients and physicians alike.
But the axitinib implant isn’t alone. Other hydrogel contenders are also showing promise:
• Hyaluronic acid-based hydrogels achieved six months of anti-VEGF release in studies.5
• Peptide amphiphile hydrogels, self-assembling systems for ranibizumab, released just 18.8% after 150 hours.6
• Tetra-armed polyethylene glycol (tetra-PEG) hydrogels, designed for bevacizumab, released only 43.3% of the drug by week two.7
• Microsphere-hydrogel systems sustained drug release lasting nearly 200 days in some cases.8
Even the best relationship counselors face hurdles, and hydrogels are no exception. Moving from the lab bench to clinical practice comes with obstacles both scientific and logistical.
“Protein stability is a key challenge,” notes Dr. Hussain. “Some antiVEGF proteins are large, sensitive biomolecules. Preserving activity over months in a matrix is a potential challenge.”
And that’s just the start. Other sticking points include:1
• Burst release and dose controlavoiding an initial drug dump while ensuring reproducibility.
• Safety concerns - inflammation, toxicity or unwanted changes to the vitreous.
• Manufacturing and sterilizationscaling up without damaging drugs or altering hydrogel structure.
• Regulatory pathway - providing non-inferiority to standard injections in rigorous trials.
• Clinical logistics - training providers and adjusting workflows.
• Long-term data - essential for therapies that chronic patients will use for years.
Of all these, sterilization stands out as particularly thorny. As one study points out, “Due to their polymeric nature and the presence of high amounts of water in their structure, hydrogels generally present high sensitivity to terminal sterilization.”9
“Protein stability is a key challenge. Some antiVEGF proteins are large, sensitive biomolecules. Preserving activity over months in a matrix is a potential challenge.”
- Dr. Rehan Hussain
In other words, traditional sterilization methods (head, radiation, gas) risk altering hydrogel properties. Meanwhile, newer techniques can end up denaturing the very proteins they’re supposed to protect.9
In the end, hydrogel-based delivery systems may be the bridge this complicated relationship needs. By stretching injection intervals from weeks to months, they could dramatically lighten the anti-
1. Truong D, Wu KY, Nguyen L, Tran SD. Advancements in hydrogel technology for ocular drug delivery. Explor BioMat-X. 2024;1:331-352.
VEGF treatment burden without compromising vision.
For patients, that could mean fewer needles and fewer appointments. For clinics, it could mean smoother workflows and expanded access for those who struggle with frequent visits.
The bond between patients and antiVEGF therapy may never be totally maintenance-free. But with hydrogels acting as relationship counselors, it could evolve from a clingy, highmaintenance affair into a healthier, quarterly or even biannual check-in.
In the world of chronic disease management, that’s the kind of relationship upgrade worth committing to.

Dr. Rehan Hussain is a vitreoretinal surgeon with a career built on both precision in the operating room and leadership in the retina community. He earned his medical degree from George Washington University before completing his ophthalmology residency at Indiana University, where his peers selected him as Chief Resident and he received the Merrill Grayson Leadership Award. His training continued at the world-renowned Bascom Palmer Eye Institute, where he completed dual fellowships in ophthalmic pathology and vitreoretinal surgery—experience that gave him a strong foundation in both the science and art of eye care.
2. Zhang C, Wang J, Wu H, et al. Hydrogel-based therapy for age-related macular degeneration: Current innovations, impediments, and future perspectives. Gels. 2024;10(3):158.
3. Clinical Trials. Ocular Therapeutix. 2025. Available at: https://www.ocutx.com/pipeline/clinical-trials/. Accessed on August 18, 2025.
4. We aim to redefine treatment for retinal disease. Ocular Therapeutix. 2025. Available at: https://www.ocutx.com/ pipeline/axpaxli/. Accessed on August 18, 2025.
5. Jung JH, Kim SS, Chung H, Hejri A, Prausnitz MR. Six-month sustained delivery of anti-VEGF from in-situ forming hydrogel in the suprachoroidal space. J Control Release. 2022;352:472-484.
6. Yaylaci S, Dinc E, Aydin B, Tekinay AB, Guler MO. Peptide nanofiber system for sustained delivery of anti-VEGF proteins to the eye vitreous. Pharmaceutics. 2023;15:1264.
7. Murakami T, Hoshi S, Okamoto F, et al. Analysis of the sustained release ability of bevacizumab-loaded tetra-PEG gel. Exp Eye Res. 2022;223:109206.
8. Osswald CR, Guthrie MJ, Avila A, Valio JA, Mieler WF, Kang-Mieler JJ. In vivo efficacy of an injectable microsphere-hydrogel ocular drug delivery system. Curr Eye Res. 2017;42:1293-1301.
9. Bento CSA, Gaspar MC, Coimbra P, de Sousa HC, Braga MEM. A review of conventional and emerging technologies for hydrogels sterilization. Int J Pharm. 2023;634:122671.
Dr. Hussain’s influence extends beyond the clinic. He chairs the scientific poster session for the American Society of Retina Specialists and serves as vice president of Digital Relations for the Vit-Buckle Society, bringing fresh energy to the field’s professional circles. A prolific contributor, he has presented surgical videos and retina research at major national meetings, authored over 80 publications in journals and textbooks, and advises pharmaceutical companies developing next-generation retinal therapies. Whether in the lab, lecture hall or the OR, Dr. Hussain is dedicated to advancing treatments and improving vision outcomes for patients worldwide.
rhussain27@gmail.com
This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
The road to U.S. approval for ONS-5010 has been anything but smooth.
Outlook Therapeutics (New Jersey, USA) is once again turning to the U.S. Food and Drug Administration (FDA) after facing another regulatory setback for its wet AMD candidate, ONS-5010 (Lytenava, bevacizumab-vikg).
Following a second complete response letter (CRL), the company has formally requested a Type A Meeting to clarify what confirmatory efficacy evidence regulators will require to advance its resubmitted biologics license application (BLA).
A road marked by challenges
The most recent CRL, issued on August 27, 2025, stemmed from the NORSE EIGHT trial, which did not meet its primary efficacy endpoint.1 While the FDA acknowledged the earlier Phase III NORSE TWO pivotal trial had demonstrated safety and efficacy, the agency concluded that additional confirmatory evidence is necessary to support approval.2
This marks the second CRL for ONS-5010. The FDA first rejected the therapy in August 2023, citing chemistry, manufacturing and controls (CMC) issues, unresolved findings from pre-approval inspections, and what it called a lack of substantial evidence. That rejection prompted Outlook’s first Type A Meeting in September 2023.3
Despite the challenges, Outlook leaders remain committed to the program.
“We believe this Type A meeting will provide us with additional clarity on the FDA’s requirements to remedy the deficiency identified in the CRL,” said Bob Jahr, CEO of Outlook Therapeutics, in a news release.
“Our mission has not changed: to deliver a safe and effective FDA-approved alternative to compounded bevacizumab, which U.S. patients and physicians have relied on off-label for years despite concerns over potency, sterility, consistency and regulatory oversight.”
If approved by the FDA, ONS-5010 would be the first and only on-label ophthalmic bevacizumab for thousands of patients needing anti-VEGF treatments for wet AMD.
How ONS-5010 works
ONS-5010 is a purpose-designed ophthalmic formulation of bevacizumab. Unlike compounded bevacizumab, which is adapted from oncology use, ONS-5010 is built specifically for intravitreal injection to treat retinal diseases.
Its active component, bevacizumab-vikg, is a recombinant humanized monoclonal antibody (mAb).
It binds with high affinity to all isoforms of vascular endothelial growth factor (VEGF) and neutralizes VEGF’s biological activity by blocking its interaction with the receptors Flt-1 (VEGFR-1) and KDR (VEGFR-2) on endothelial cells.
By cutting off VEGF signaling, ONS-5010 reduces endothelial cell proliferation, vascular leakage and abnormal new blood vessel formation—the key drivers of wet AMD.
While Outlook struggles with U.S. regulators, the therapy has made steady gains abroad. In March 2024, the European Medicines Agency (EMA) issued a positive CHMP opinion for ONS-5010.
By June 2025, the drug became commercially available in Germany and the UK for wet AMD, pending additional national reimbursement approvals across the EU.
The upcoming second Type A Meeting will be pivotal in determining ONS-5010’s U.S. future. If Outlook can reach alignment with the FDA on the confirmatory trial requirements, it may yet move the therapy back toward approval.
Until then, the company stands at a crossroads: with international momentum building but U.S. approval still uncertain, all eyes are on whether ONS-5010 can overcome its latest regulatory hurdle and finally deliver a long-awaited alternative to compounded bevacizumab for American patients.
1. Outlook Therapeutics Provides Regulatory Update on U.S. Food and Drug Administration Review of ONS-5010/LYTENAVA™ (bevacizumab-vikg) for the Treatment of Wet AMD. Outlook Therapeutics. August 28, 2025. Available at: https://ir.outlooktherapeutics.com/news-releases/news-release-details/ outlook-therapeutics-provides-regulatory-update-us-food-and-drug. Accessed on September 4, 2025.
2. Outlook Therapeutics Presents NORSE TWO Phase 3 Pivotal Safety and Efficacy Data for ONS-5010 / LYTENAVA™ (bevacizumab-vikg) at the Retina Subspecialty Day, American Academy of Ophthalmology (AAO) 2021 Annual Conference. Outlook Therapeutics. November 13, 2021. Available at: https:// ir.outlooktherapeutics.com/news-releases/news-release-details/outlooktherapeutics-presents-norse-two-phase-3-pivotal-safety. Accessed on September 4, 2025.
3. Outlook Therapeutics® Requests Type A Meeting With FDA. Outlook Therapeutics. September 29, 2023. Available at: https://ir.outlooktherapeutics. com/news-releases/news-release-details/outlook-therapeuticsr-requests-typemeeting-fda. Accessed on September 4, 2025.
A version of this article was first published on piemagazine.org.

By April Ingram
Once considered a stubborn surgical nuisance, PVR is now being reframed as a complex biological continuum, and that shift is rewriting the playbook. From methotrexate to molecular profiling, retina specialists are pushing past ‘magic bullets’ toward precision prevention and smarter therapies.
Proliferative vitreoretinopathy (PVR) is a term coined back in 1983 by the Retina Society Terminology Committee, with an aim to bring order to the chaos of membrane proliferation complicating rhegmatogenous retinal detachment surgery. Four decades later, imaging breakthroughs and a deeper grasp of PVR pathophysiology—plus the sometimes unpredictable behavior of rhegmatogenous detachments— have led to multiple re-classifications and refined management strategies.
Preclinical studies reveal PVR as a biological tug-of-war, involving retinal pigment epithelial (RPE) cells, macrophages, glial cells, inflammatory cells and various mediators. The outcome of this unruly gathering is fibrosis and epiretinal membrane (ERM) formation, which stiffens the retina and makes surgical repair both challenging and prone to failure.
Even today, PVR is the leading cause of complications in retinal detachment repair, affecting an estimated 5% to 10% of patients, with higher rates in trauma-related detachments and giant retinal tears.1
Historically, treatment meant surgical removal of membranes, which is a reactive rather than preventative approach. But as the mechanisms behind fibrocellular membrane formation are better understood, medical therapies are stepping in to block the process before visionthreatening sequelae occur.
To explore these new strategies we spoke with Dr. David Almeida, president and CEO of Erie-Retina Research. Reflecting on his changing views, Dr. Almeida says, “My perspective has evolved from viewing PVR as a simple, binary surgical complication to understanding it as a complex biological continuum,” adding, “In 2025, the narrative must shift away from the crude endpoint of anatomical re-detachment alone.”
The holy grail for vitreoretinal surgeons remains primary prevention of PVR. Methotrexate (MTX), long used to treat cancer and chronic
inflammatory diseases, has been under investigation for PVR for decades. Clinical trials testing various doses and injection frequencies suggest potential benefit. The GUARD trial, for example, found that 24% of patients treated with MTX required repeat surgery within six months compared with 39% in the historical group.2
“We now have evidence that adjunctive therapies like MTX may not significantly alter overall redetachment rates in severe PVR but can profoundly modulate the severity of the disease, significantly reducing the incidence of limited PVR recurrence or macula-off detachments,” Dr. Almeida explains. “This is a critical distinction others often miss; it reframes ‘success’ as a mitigation of the proliferative response rather than its complete prevention.”3,4
Another therapeutic duo—5fluorouracil combined with low molecular weight heparin—attracted attention as an intraoperative treatment to reduce PVR. While 5-FU theoretically curbs cell proliferation and heparin targets other stages of PVR development, larger trials failed to show meaningful improvements in vision or anatomical outcomes despite early promise.5
As in many corners of medicine, focusing only on the acute event risks missing the forest for the trees. Dr. Almeida highlights the importance of a holistic lens, “We must see PVR not as an isolated ocular event, but as a reflection of a patient’s entire inflammatory and healing profile.”
This view links systemic and local factors to prognosis. “Our work identifying systemic factors like cigarette smoking and local inflammatory surrogates like postoperative epiretinal membrane and cystoid macular edema underscores this,” Dr. Almedia adds. “These are not just risk factors; they are windows into the underlying biological turmoil that drives this aberrant wound healing process.”6,7
Precision over one-sizefits-all
Dr. Almeida believes molecular profiling will guide the next leap forward. “Most importantly, will be how to adequately molecularly characterize the PVR pathogenic drivers to stratify patients before a precision-led treatment paradigm. In my opinion, proteomics—and specifically ClinOmicsAI—will be the key that ultimately unlocks the PVR conundrum that has eluded us for over two decades.”
ClinOmicsAI, founded by Dr. Almeida and Dr. Vinit Mahajan, leverages liquid biopsy proteomics and artificial intelligence to track disease activity non-invasively and in real time. Dr. Mahajan, professor of Ophthalmology at Stanford University, notes, “To follow on Dr. Almeida’s comments, my lab published an analysis of liquid biopsies from PVR patients and found activity of the mTOR pathway, paving the way for precision medicine and rational therapeutic targeting.
References
1. Pastor JC, de la Rua ER, Martin F. Proliferative vitreoretinopathy: Risk factors and pathology. Prog Retin Eye Res. 2002;21(1):127-144.
2. Brodin A. PVR Pipeline Roundup. Retina Today. November/December 2023. Available at: https:// retinatoday.com/articles/2023-nov-dec/pvr-pipelineroundup. Accessed on September 1, 2025.
A recent big-data study confirmed the potential of this pathway.”8
He adds, “Another strong molecular target is RUNX1, identified and validated in preclinical PVR models by Dr. Leo Kim and colleagues.”9
For Dr. Almeida, the future lies in tailoring prophylaxis. “Looking forward to the next development cycle over the next 12 to 15 years, the era of seeking a single ‘magic bullet’ for PVR is over. The future lies in precision medicine and risk stratification. We will move beyond treating all high-risk retinal detachments similarly and instead use validated biomarkers and predictive models…tailor therapy to the individual.”
He envisions evolving delivery systems as well. “The therapies themselves will evolve from singleagent injections to sustained-release combination therapies delivered via intelligent platforms, such as pharmacologically active silicone oils

3. Babel A, Chin EK, Almeida DRP. Vitrectomy with silicone oil tamponade and single-dose intravitreal methotrexate for recurrent retinal detachment with proliferative vitreoretinopathy. Case Rep Ophthalmol. 2022;13(3):777-782.
4. Babel A, Almeida D. Methotrexate as an Adjunctive Therapy for Proliferative Vitreoretinopathy: A Critical Review of Evidence with Emphasis on Intra-Silicone Oil Administration Strategies. Med Res Arch. 2025;13(6).
5. Chen C, Chen P, Liu X, Li H. Combined 5-fluorouracil and low molecular weight heparin for the prevention of postoperative proliferative vitreoretinopathy in patients with retinal detachment: A meta-analysis. Front Med (Lausanne). 2021;8:790460.
6. Xu K, Chin EK, Parke DW 3rd, Almeida DRP. Epiretinal membrane and cystoid macular edema as predictive factors of recurrent proliferative vitreoretinopathy. Clin Ophthalmol. 2017;11:18191824.
7. Xu K, Chin EK, Bennett SR, et al., Almeida DRP. Predictive factors for proliferative vitreoretinopathy formation after uncomplicated primary retinal detachment repair. Retina. 2019;39(8):1488-1495.
8. Alsoudi AF, Loya A, Wai K, et al. Mammalian target rapamycin inhibition as a therapeutic target for prevention of proliferative vitreoretinopathy. JAMA Ophthalmol. 2025:e252497.
9. O’Hare M, Miller WP, Arevalo-Alquichire S, et al. An mRNA-encoded dominant-negative inhibitor of transcription factor RUNX1 suppresses vitreoretinal disease in experimental models. Sci Transl Med. 2024;16(775):eadh0994.
Dr. David Almeida wears many hats. He is president and CEO of Erie Retina Research in Pennsylvania, United States, as well as founder and CEO of The Centers for Advanced Surgical Exploration (CASEx). A vitreoretinal surgeon by training, Dr. Almeida has carved out a reputation as both a skilled clinician and a forward-thinking innovator.
His work bridges the operating room and the boardroom. He has led the development of successful ventures and built strategic partnerships with powerhouses like Stanford University and global corporations, proving he knows how to scale ideas into impact. On the academic front, he’s as prolific as they come—authoring more than 300 peer-reviewed papers and delivering over 125 conference presentations worldwide.
Internationally recognized as a thought leader in ophthalmology, Dr. Almeida’s accolades include the American Society of Retina Specialists (ASRS) Honor Award and a spot on The Ophthalmologist’s “Top 50 Rising Stars” Power List. Whether he’s advancing research, mentoring peers or steering new enterprises, he’s driven by one goal: pushing the boundaries of retina care.
drpa@pm.me
or gas-phase aerosols that provide uniform retinal coverage.”
Ultimately, Dr. Almeida emphasizes a shift in goals. “The ultimate goal will be to normalize the postoperative inflammatory milieu, not just inhibit proliferation. By ‘quieting the eye,’ we can reduce the host of secondary complications and create an environment where the retina can truly heal, maximizing not just anatomical success but, most importantly, the patient’s final visual function. Solving the pharmacokinetic puzzle of these depot delivery systems is the critical next step to unlocking this more sophisticated and effective future.”
PVR may no longer be just the surgical nuisance it was in 1983—it’s a biological riddle slowly giving up its secrets. And while no one’s holding a ‘magic bullet’ yet, the field is edging closer to a reality where prevention is personalized, precision-driven and— dare we say—quietly brilliant.

Dr. Vinit Mahajan is a professor and vitreoretinal surgeon at Stanford University, where he serves as vice chair for Research and leads the Molecular Surgery Program. He also directs the NIH-funded Omics Laboratory, which harnesses proteomics, genomics and phenomics to uncover the molecular roots of eye disease. His team goes beyond discovery—they use protein crystallography and structural modeling to design potential therapies, then test them in stem cell and transgenic models.
Innovation doesn’t stop at the bench. Dr. Mahajan’s group created TEMPO, a precision health platform that integrates human proteomics with single-cell gene expression to map out molecular pathways in real time. With this approach, they’re charting new territory in how we understand and treat blinding conditions. What sets his work apart is its translational focus. By connecting cutting-edge science with clinical practice—and even spinning out biomedical start-ups—Dr. Mahajan and his multidisciplinary team ensure discoveries don’t stay trapped in the lab. Instead, they move forward into trials, treatments and tangible impact for patients worldwide. mahajanlab@gmail.com
By Hazlin Hassan
From complement inhibitors that merely slow the clock to bold gene and cell therapies aiming to reset it entirely, GA research is shifting gears. The race is on. Not just to delay decline, but to flirt with the once-unthinkable prospect of restoring sight.
For decades, patients with advanced dry age-related macular degeneration (AMD) and its devastating late stage, geographic atrophy (GA), were told nothing could stop the inexorable march of vision loss.
But in 2023, a sliver of hope arrived. The U.S. Food and Drug Administration (FDA) approved two complement inhibitors for GA , the first therapies ever greenlit for the condition.1,2 By targeting components of the complement cascade implicated in retinal cell death, these drugs offered a way to slow lesion growth.
But slowing decline is not the same as restoring sight. For many researchers, complement inhibitors marks not the finish line but the starting gun for a more ambitious race: gene and cell therapies that might preserve, or even regenerate, vision.
“Complement inhibitors have indeed shifted the treatment paradigm by slowing GA progression, but their benefits remain modest and revolve around frequent dosing and risk of conversion to neovascular AMD,” said Dr. Veeral Seth, a partner at University Retina and Macula Associates (United States). “These agents provide an important bridge while more durable, regenerative therapies mature.”
Prof. Gemmy Cheung, head of the Medical Retina Department at Singapore National Eye Centre, echoed the sentiment. “The treatment effect of currently available complement inhibitors is limited,
so in that sense, we definitely need stronger treatments to be a real game-changer,” she noted.
Apellis has also reported increased incidence of eye inflammation during clinical trials, which has led to some concerns.3
The unmet need in GA is stark. Current drugs buy time, not vision. Gene and cell therapies, however, aim to change the trajectory entirely.
Gene therapies deliver genetic material to retinal cells, encouraging production of therapeutic proteins that can last for extended periods, with a one-time treatment rather than endless injections. Cell therapies go further, attempting to replace tissue lost in GA, particularly the retinal pigment epithelium (RPE), to rescue endangered photoreceptors and preserve vision.4
Prof. Cheung noted their promise. “Both gene and cell therapies have the potential advantage of longlasting treatment, which addresses the immense treatment burden associated with repeated intravitreal injections,” she said. “If we are able to replenish lost tissue, we also hope to be able to bring about functional improvement and not just slowing deterioration.”
Still, she cautioned, the path forward is riddled with obstacles like delivery techniques, long-term safety, scalability of cell therapies and the refinement of study endpoints among them.
Yet early glimpses are encouraging. “I am hopeful. There have been several Phase I studies which have reported improvement in vision. These may be possible with different strategies which rescue the function of dying cells,” she added.
India-based Eyestem Research (Bangalore, India) has emerged as a frontrunner with its EyecyteRPE program, which uses induced pluripotent stem cell (iPSC)-derived RPE in suspension form.
“Full vision recovery remains aspirational at this stage. However, early phase cell therapy trials, particularly Eyestem’s Eyecyte RPE, demonstrate the first concrete hints of ‘vision rescue,’ making true restoration increasingly plausible if administered before irreversible photoreceptor loss,” said Dr. Sheth.
Phase I results in six patients showed an average improvement of 14.9 letters on ETDRS vision testing over four to six months, with no serious adverse events.5 Imaging also suggested early signs of structural reversal in some patients.
“These are compelling early signals,” Dr. Sheth noted.
Prof. Cheung was cautiously optimistic, saying, “[The results] are encouraging. The study will help generate important information about which patients are most likely to benefit.”
Another contender, Luxa Biotechnology (New Jersey, United States), also shared first-in-human data on its candidate RPESC-RPE4W. Results from a Phase I/IIa trial showed that patients with the poorest baseline vision gained an average of +21.7 letters at 12 months, while those starting with better vision gained +3.3 letters at three months. No serious adverse events were reported.6
“Gains of this magnitude are rare in GA and can translate to realworld improvements, though larger, longer follow-up is needed,” said Dr. Sheth.
While cell therapies try to replace lost tissue, gene therapies aim to alter disease biology more durably than injections. One candidate drawing attention is KRIYA-825, an AAV-based therapy from Kriya Therapeutics (North Carolina, United States) designed to inhibit complement C3 and C5. Delivered via suprachoroidal injection, it is engineered to produce a complement inhibitor that could halt GA progression.
Preclinical data presented at ARVO 2025 showed dose-dependent preservation of retinal thickness in mice, suppression of harmful complement fragments and effective transgene biodistribution in non-human primates.7
Still, delivery remains a thorny issue. “Achieving sufficient transduction across large, irregular GA zones without under- or overdosing is a key technological hurdle the field is actively addressing,” said Dr. Sheth.
The next few years will determine if these regenerative approaches can transition from early phase trials into mainstream care. Patients with

1. FDA Approves SYFOVRE™ (pegcetacoplan injection) for Geographic Atrophy Secondary to Age-Related Macular Degeneration. Apellis Pharmaceuticals. Press release, February 2023. Available at: https:// investors.apellis.com/news-releases/news-releasedetails/fda-approves-syfovretm-pegcetacoplaninjection-first-and-only. Accessed on September 1, 2025.
2. FDA Approves IZERVAY™ (avacincaptad pegol intravitreal solution) for Geographic Atrophy. Iveric Bio (Astellas). Press release, August 2023. Available at: https://www.astellas.com/en/news/28281. Accessed on September 1, 2025.
3. Witkin AJ, Jaffe GJ, Srivastava SK, Davis JL, Kim JE. Retinal vasculitis after intravitreal pegcetacoplan: Report from the ASRS Research and Safety in Therapeutics (ReST) Committee. J Vitreoretin Dis. 2023;8(1):9-20.
4. Sharma R, Bose D, Maminishkis A, Bharti K. Retinal pigment epithelium replacement therapy for agerelated macular degeneration: Are we there yet? Annu Rev Pharmacol Toxicol. 2020;60:553-572.
5. Eyestem’s Eyecyte-RPE trial shows vision rescue for geographic atrophy patients. The Economic Times. News article, April 14, 2025. Available at: https://economictimes.indiatimes.com/small-biz/ sme-sector/eyestems-eyecyte-rpe-trial-showsvision-rescue-for-geographic-atrophy-patients/ articleshow/120271413.cms Accessed on September 1, 2025.
6. Luxa Biotechnology presents clinical data from first-in-human retinal pigment epithelium cell therapy trial for dry age-related macular degeneration at the 77th Annual Wills Eye Conference. Luxa Biotechnology. Press release, March 6, 2025. Available at: https://www. businesswire.com/news/home/20250306998366/ en/Luxa-Biotechnology-Presents-Clinical-Data-fromFirst-in-Human-Retinal-Pigment-Epithelium-CellTherapy-Trial-for-Dry-Age-Related-Macular-Degeneration-at-the-77th-Annual-Wills-Eye-Conference. Accessed on September 1, 2025.
7. KRIYA-825 Preclinical Data in Geographic Atrophy Presented at ARVO 2025. Kriya Therapeutics. Press release, May 2025. Available at: https:// kriyatherapeutics.com/news/kriya-presents-dataat-the-2025-association-for-research-in-vision-andophthalmology-arvo-annual-meeting/. Accessed on September 1, 2025.
Prof. Dr. Gemmy Cheung is currently the Arthur Lim Professor in Ophthalmology at the Duke-NUS Medical School, National University of Singapore. She is head of the Medical Retina Department at, Singapore National Eye Center, and head of the Retina Research Group at the Singapore Eye Research Institute (SERI). Her research interests focus on Asian retinal diseases, specifically agerelated macular degeneration (AMD), polypoidal choroidal vasculopathy (PCV), and myopic macular degeneration. She has published more than 300 peer-reviewed articles, including high-impact work advancing the understanding of AMD, especially in the context of an Asian population, and secured research funding of more than SGD $40 million. Internationally, Prof. Cheung has assumed leadership roles in the field of AMD and PCV. She has delivered more than 200 invited lectures and has trained numerous fellows and Ph.D. students. Prof. Cheung has represented the Asian-Pacific perspectives at highlevel international ophthalmology meetings, including the annual American Academy of Ophthalmology subspecialty day, the EURETINA Congress, and the Asia-Pacific Vitreoretina Society Annual Congress. She is a council member of the AsiaPacific vitreo-retina society, regional advisor to the American Academy of Ophthalmology, Exco member of the International Retinal Imaging Society and the Asia-Pacific Ocular Imaging Society, and credentialing committee member (past) of the prestigious Macula Society. She serves on the editorial boards of the American Journal of Ophthalmology, AsiaPacific Journal of Ophthalmology, Retina, Eye, and PLoS One. She has received several prestigious awards from the American Academy of Ophthalmology, the Asia-Pacific Academy of Ophthalmology, the AsiaPacific Vitreo-retinal Society, and the Macula Society.
gemmy.cheung.c.m@singhealth. com.sg
early or intermediate GA, where photoreceptors are still viable, stand to gain the most, according to Dr. Sheth. Those with bilateral progressed GA and residual vision may also benefit. “Early intervention remains the key shift needed to maximize potential,” he concluded.
For patients with GA, the hope of regaining vision has long felt out of reach. Now, early cell therapy trials showing letter gains suggest that hope is not misplaced. Whether those gains prove durable and reproducible remains to be seen.
The race from degeneration to regeneration is still in its early laps, but the course has been set. Gene and cell therapies may or may not fulfill their promise, but one thing is clear: the future of GA treatment will not be defined by merely slowing decline. It will be driven by the pursuit of something bolder…the chance for patients to truly see again.

“Dr. Veeral Sheth , a proud Chicago native, has built his career around advancing care for diseases of the retina and vitreous. He is a partner at University Retina and Macula Associates and serves as a clinical assistant professor at the University of Illinois in Chicago. Beyond the clinic, Dr. Sheth is the director of clinical trials at one of the nation’s busiest research sites, where he has led more than 60 trials exploring new treatments for macular degeneration, diabetic retinopathy, vein occlusion and surgical pathology.
An engaged leader in the field, he is active in major professional societies including the American Society of Retina Specialists, Retina Society, American Academy of Ophthalmology, ARVO and the European Society of Retina Specialists. His work has not only pushed forward innovation in eye care but also helped shape the next generation of therapies reaching patients.
Dr. Sheth also dedicates time to his community, having served as chairman emeritus of the Board of Directors for Meals on Wheels Chicago. Fluent in English, Spanish and Gujarati, he connects easily across cultures—whether mentoring colleagues, guiding patients or leading groundbreaking research. vsheth@gmail.com
By Kendra Bruning
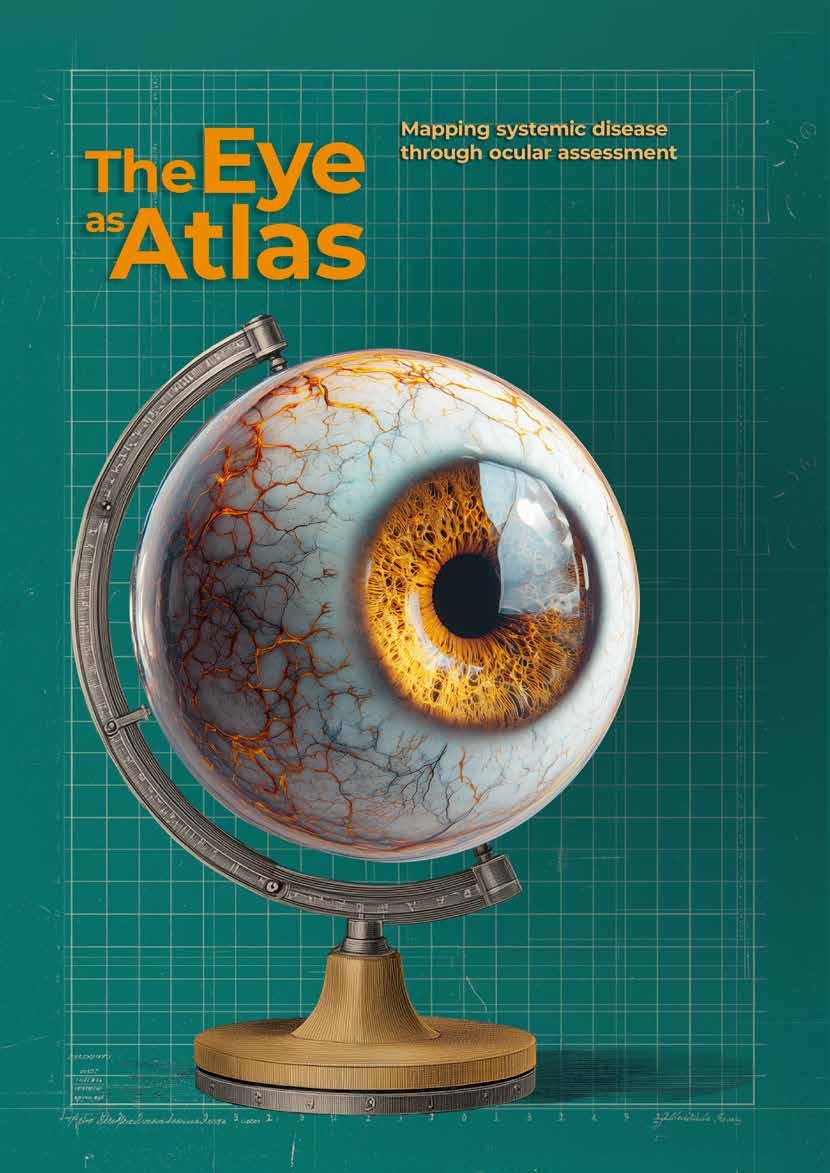
Medicine’s most revealing map is hiding in plain sight. With AI as its compass, the eye is charting systemic disease from the retina outwards, redrawing how clinicians navigate cardiovascular, metabolic and neurologic health long before symptoms appear.
The eye is no longer just the organ of sight, it’s shaping up to be a roadmap of the body itself. Enter oculomics, the science of decoding ocular biomarkers, where retinal landscapes and vascular pathways reveal systemic health long before symptoms surface. Like explorers tracing rivers, researchers are uncovering clues to cardiovascular, metabolic and neurological disease from the back of the eye.
What began with the humble ophthalmoscope in the 19th century has been supercharged by modern tools such as optical coherence tomography (OCT), hyperspectral imaging and AI-powered analytics. Massive datasets—from INSIGHT’s 35 million retinal images to Moorfields’ AlzEye project—now serve as atlases for systemic disease.1, 2
As Prof. Andrzej Grzybowski, a retina specialist at the University of Warmia and Mazury in Poland, explains, “The eye is uniquely suited to reveal systemic health because it allows direct, non-invasive visualization of microvasculature and neural tissue in real time.”3
At Moorfields Eye Hospital in London, Dr. Josef Huemer adds, “Through the imaging of the retinal vasculature and the neural structures…we understand more about systemic diseases.”

Meanwhile, Prof. Haotian Lin, of Zhongshan Ophthalmic Center, Sun Yat-sen University in China, frames it this way: “The eye has become a powerful window into systemic health. Advances in imaging have transformed ophthalmology from simply ‘seeing’ to actually ‘measuring,’ revealing changes linked to cardiovascular, metabolic, kidney and pregnancy-related conditions”.
Taken together, their perspectives frame the eye as far more than a gateway to vision. It’s an atlas clinicians can read to chart systemic disease.
“The eye is uniquely suited to reveal systemic health because it allows direct, non-invasive visualization of microvasculature and neural tissue in real time.”
- Prof. Andrzej Grzybowski
The idea that the eye reflects systemic health is hardly new. Ancient Egyptian papyri described ocular changes linked to systemic illness, and centuries later, Hippocratic texts noted the diagnostic value of the eye.4
By the 19th century, the ophthalmoscope gave physicians their first true ‘window’ into the body, linking diabetic and hypertensive changes to retinal signs.5 Fast forward to 2020, when researchers at Moorfields Eye Hospital and University Hospitals Birmingham coined the term oculomics—a deliberate nod to genomics and proteomics—to spotlight the eye as a field of systemic biomarkers.2
What makes the eye unique is its accessibility. Unlike most organs, it can be examined directly and noninvasively, offering a high-resolution look at both vessels and neural tissue
in real time.6 Few other diagnostic tools, whether ultrasound or ECG, can match this dual vantage point.
Embryology plays a role as well. The retina develops as an outgrowth of the central nervous system. That’s why retinal nerve fiber layer (RNFL) thinning and optic nerve head (ONH) changes often parallel processes in multiple sclerosis (MS) and neurodegenerative diseases such as Alzheimer’s and Parkinson’s.7-9
The retinal vasculature also functions like a living atlas of systemic circulation. Retinal vessel caliber and tortuosity strongly correlate with hypertension and systemic vascular risk.10,11 Hypertensive retinopathy has long been linked to stroke and coronary artery disease. And retinal artery occlusions, as Dr. Huemer notes, are the “stroke equivalent of the eye,” proof that when blood flow falters, the eye sketches a warning for the whole body.
Beyond cardiovascular risk, retinal vascular features can distinguish subtypes of chronic kidney and liver disease and even predict preeclampsia, expanding the eye’s reach into maternal and systemic medicine.
All these insights are only possible because advances in imaging now allow clinicians to chart the eye’s terrain with unprecedented precision.
If the eye is an atlas, modern imaging tools are its surveying instruments, adding fresh layers of topography to the map of systemic health. The retina offers some of the most reliable landmarks of disease: its rivers of vessels, shifting layers and patches of pigment encode signs of hypertension, diabetes, neurodegeneration and more.
Fundus photography and handheld cameras. Fundus photography remains the workhorse of population-level screening. In the UK, the national diabetic retinopathy (DR) program screens around 2.7 million patients annually.11
Handheld fundus cameras paired with AI are pushing reach even further.12 In Poland, Prof. Grzybowski’s Retinobus project has delivered AI-assisted DR screening to nearly 20,000 patients since 2019.13 Meanwhile, in China, Prof. Lin describes the Smart Eye Mobile Hospital, a 5G-enabled mobile clinic that has reached more than 220,000 people across 29 provinces, detecting disease in over 150,000 individuals.
These cameras don’t just capture images—they collect predictive data. Deep learning algorithms can now extract subtle features from fundus photographs to predict blood pressure, age, smoking status, body mass index (BMI) and other cardiovascular risk factors.14
According to Prof. Grzybowski, three AI-based DR screening devices are FDA-cleared, with more than 20 CE-marked in Europe. Handheld fundus cameras paired with AI achieve mean sensitivity of 77.5% and specificity of 80.6% for referable DR detection, though results vary across algorithms.13
Optical coherence tomography (OCT) and OCT-A. OCT has become the Swiss Army knife of retinal imaging, mapping retinal layers and microvasculature to reveal early signs of systemic disease. Conditions as varied as multiple sclerosis, Alzheimer’s, Parkinson’s and lupus leave detectable signatures, from RNFL thinning7-9 to vascular anomalies.15
In the UK, OCT is now available in high-street
optometry practices at modest cost,4 while Moorfields and UCL are piloting AI-assisted OCT analysis in community clinics.16 When systemic biomarkers appear, seamless referrals to neurology or cardiology can follow—turning everyday eye exams into a gateway to broader healthcare.
Ultra-widefield and hyperspectral imaging. Ultrawidefield imaging captures the peripheral vasculature, now recognized as an important marker of systemic vascular disease.10 Hyperspectral imaging has shown promise in tracking tissue oxygenation and detecting amyloid deposits in animal models,17 hinting at the eye’s role in neurodegenerative disease detection years before clinical symptoms emerge.2
With all these new tools, what does the future hold? According to Prof. Grzybowski, it lies in explainable AI and multimodal models that weave retinal imaging together with genomics and health records—tools that don’t just observe the eye, but connect it to the broader landscape of human health.
The future of oculomics depends on building bridges beyond ophthalmology, linking its maps with the disciplines that treat the body’s other frontiers.
“If we can identify the right patient through an eye scan and direct them to the right physician at the right time, that would be amazing.”
- Dr. Josef Heumer
Cross-specialty models already exist. INSIGHT, a database of retinal images, connects eye images with systemic health records across the UK,1 while AlzEye demonstrates how ophthalmology can merge with neurology and psychiatry research.2
Dr. Huemer sees this as triage with a compass. “If we can identify the right patient through an eye scan and direct them to the right physician at the right time, that would be amazing,” he said.
In dementia research, Moorfields’ collaboration with neurologists and psychiatrists has enabled AlzEye to probe retinal biomarkers linked with Alzheimer’s and schizophrenia.2 Cardiologists are increasingly interested in retinal microvasculature as a predictor of stroke and heart disease,11,14 while neurologists now rely on OCT to monitor progression in multiple sclerosis and Parkinson’s disease.15
Prof. Grzybowski adds that ophthalmologists must be central navigators. His diabetic retinopathy prevention program in Poland integrated AI-based screening directly into routine diabetes clinics, strengthening ties between ophthalmologists and endocrinologists and demonstrating how shared pathways can scale beyond specialty silos.13
Yet even with these advances, the map of oculomics is far from complete.
In cartography, every map begins with blank spaces, and oculomics still has its unknowns. Variability in imaging devices, data quality and analytic pipelines makes standardization a pressing concern.15,17
Many biomarkers remain correlative rather than causative. Prof. Grzybowski cautions that while diabetes, hypertension and DR are firmly validated, conditions such as kidney disease or anemia still need larger cohorts before they can be trusted as navigational markers.12
Dr. Huemer adds that true significance will only emerge from multimodal datasets linking retinal imaging with systemic diagnostics such as brain scans or genomics.
AI adds its own pitfalls. Algorithms trained on narrow datasets may
fail to generalize, risking bias and misclassification. Commercial DR systems, for instance, have shown uneven performance across ethnic groups, risking delayed care in underrepresented populations.13
A Nature Medicine study revealed systematic underdiagnosis in women, minority groups and those with lower socioeconomic status due to dataset imbalances. Findings like this show that faulty maps can deepen inequities, making fairness audits and explainable AI essential for safe navigation.18
Prof. Lin points out that challenges include the black box problem of AI interpretability, ensuring biomarker specificity and technical hurdles in multimodal integration. Beyond this, many systemic disease departments still lack ophthalmic imaging devices or trained personnel, and clinicians need both AI literacy and clear regulatory frameworks to use these tools with confidence.
Ethical and logistical barriers, from patient consent and data privacy to reimbursement and training, must also be addressed to bring AI in oculomics from research to routine clinical care.12 Addressing these challenges is essential before the field can chart its full potential and guide healthcare on a broader scale.
The atlas of oculomics remains unfinished, with many regions still blank. The next decade will determine whether those spaces are filled with validated biomarkers or left as speculative sketches.
Prof. Grzybowski predicts that large, multi-ethnic cohort studies will be essential to confirm ocular biomarkers for cardiovascular, metabolic and neurodegenerative disease, potentially elevating retinal imaging to the same level of risk stratification now given to blood pressure or cholesterol testing.12
Portable and home-based devices like smartphone fundus cameras
and community OCT could expand screening in primary care and underserved regions. Dr. Huemer imagines a future where a general practitioner visit includes an OCT scan, with AI triaging patients toward cardiology, neurology or endocrinology.
“First, multi-disease integration, where a single scan predicts risks across cardiovascular, neurological and metabolic conditions.”
- Prof. Haotian Lin


Prof. Lin sees the future of oculomics taking shape on three fronts. “First, multidisease integration, where a single scan predicts risks across cardiovascular, neurological and metabolic conditions,” he forecasts. “Second, moving from prediction to personalized care using multimodal data to tailor management to each patient. And third, access for all, where smart devices and cloud platforms bring early systemic disease detection into community clinics and resource-limited settings worldwide.”
If such efforts succeed, the eye may no longer be seen as an isolated organ, but as the mapmaker of medicine, helping clinicians truly see the whole patient more clearly.
Dr. Josef Huemer is a consultant ophthalmologist at Moorfields Eye Hospital in London, with a sharp focus on medical retina and cataract surgery. Originally from Austria, he studied medicine at Medical University in Innsbruck before making his way to the UK, where he completed both clinical and research fellowships at Moorfields. His day-to-day practice revolves around helping patients with retinal conditions, including AMD and DME. Alongside his clinical work, Dr. Heumer has built an impressive research portfolio, publishing widely on topics ranging from retinal vascular disease to the growing role of telemedicine. He’s also part of the exciting movement exploring how AI can be harnessed to transform the future of ophthalmology.
josef.huemer1@nhs.net

References
1. Oculomics. INSIGHT Health Data Research Hub. Available at: https://www.insight.hdrhub.org/oculomics. Accessed on September 1, 2025.
2. Wagner SK, Hughes F, Cortina-Borja M, et al. AlzEye: Longitudinal record-level linkage of ophthalmic imaging and hospital admissions of 353 157 patients in London, UK. BMJ Open. 2022;12(3):e058552.
3. Grzybowski A, Brona P. Approval and certification of ophthalmic AI devices in the European Union. Ophthalmol Ther. 2023;12(2):633-638.
4. Sim PY, Tripathy K, Leffler C. History of Ophthalmology. EyeWiki. Available at https://eyewiki.org/History_of_ Ophthalmology. Accessed on September 1, 2025.
5. Benson CE, Somisetty S, Martin HMI. History of diabetic eye related diseases. J Diabetes Mellit. 2021;11(5):371378.
6. Jin K, Zhang J, Grzybowski A. Predictive and diagnostic approaches for systemic disorders using ocular assessment. Front Med. 2024;11:1529861.
7. Parisi V, Manni G, Spadaro M, et al. Correlation between morphological and functional retinal impairment in multiple sclerosis patients. Invest Ophthalmol Vis Sci. 1999;40(11):2520-2527.
8. Wagner SK, Romero-Bascones D, Cortina-Borja M, et al. Retinal optical coherence tomography features associated with incident and prevalent Parkinson disease. Neurology. 2023;101(16):e1581-e1593.
9. Yu JG, Feng YF, Xiang Y, et al. Retinal nerve fibre layer thickness changes in Parkinson disease: A metaanalysis. PLoS One. 2014;9(1):e85718.
10. Arnould L, Meriaudeau F, Guenancia C, et al. Using artificial intelligence to analyse the retinal vascular network: The future of cardiovascular risk assessment based on oculomics? A narrative review. Ophthalmol Ther. 2023;12(2):657-674.
11. Wagner SK, Bountziouka V, Hysi P, et al. Associations between unilateral amblyopia in childhood and cardiometabolic disorders in adult life: A cross-sectional and longitudinal analysis of the UK Biobank. eClinicalMedicine. 2024;70:102493.
12. Miao H, Zou Z, Xu J, et al. Advancing systemic disease diagnosis through ophthalmic image-based artificial intelligence. MedComm Futur Med. 2024;3(1):e75.
Prof. Andrzej Grzybowski is a professor of Ophthalmology at the University of Warmia and Mazury in Poland and heads the Institute for Research in Ophthalmology in Poznań. A true force in the field, he has served as president of EVER, sits on boards including ESCRS and ISRS, and is both a lifelong member and treasurer of the European Academy of Ophthalmology.
His global reputation speaks for itself: ranked #1 in the world for cataract research by Expertscape, named among Stanford University’s Top 2% of scientists and featured on The Ophthalmologist’s prestigious “Power List.” Along the way, he has earned top honors such as ISRS Founders’ Award and Poland’s Officer’s Cross of the Order of Polonia Restituta, celebrating his impact on research, education and international collaboration.
ae.grzybowski@gmail.com

Prof. Haotian Lin is the director of Zhongshan Ophthalmic Center at Sun Yat-sen University, where he also wears the hats of professor, PhD mentor and chief scientist of China’s National Key R&D Program. His passion lies in harnessing medical big data and AI to transform how eye diseases are diagnosed and treated—an area where he’s made his mark with more than 150 publications in Nature, Science, The Lancet and other top journals.
13. Kubin AM, Huhtinen P, Ohtonen P, et al. Comparison of 21 artificial intelligence algorithms in automated diabetic retinopathy screening using handheld fundus camera. Ann Med. 2024;56(1):2352018.
14. Poplin R, Varadarajan AV, Blumer K, et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nat Biomed Eng. 2018;2:158-164.
15. Król-Grzymała A, Sienkiewicz-Szłapka E, Fiedorowicz E, et al. Tear biomarkers in Alzheimer’s and Parkinson’s diseases, and multiple sclerosis: Implications for diagnosis (systematic review). Int J Mol Sci. 2022;23(17):10123.
16. Moorfields launch AI model to boost global research into reducing blindness. Moorfields Eye Hospital NHS Foundation Trust. September 13, 2023. Available at https://www.moorfields.nhs.uk/about-us/news-and-blogs/ news/moorfields-launch-ai-model-to-boost-global-research-into-reducing-blindness. Accessed on September 1, 2025.
17. More SS, Vince R. Hyperspectral imaging signatures detect amyloidopathy in Alzheimer’s mouse retinas well before onset of cognitive decline. ACS Chem Neurosci. 2015;6(2):306-315.
18. Tan W, Wei Q, Xing Z, et al. Fairer AI in ophthalmology via implicit fairness learning for mitigating sexism and ageism. Nat Commun. 2024;15:4750.
Beyond the lab, Prof. Lin plays key roles in both national and international organizations, from the Asia Office of the Afro-Asian Council of Ophthalmology to the Chinese Association for Artificial Intelligence. His work has not gone unnoticed: he’s the recipient of the prestigious China Youth May Fourth Medal, the Wu Wenjun Science and Technology Award for AI, and holds over 30 patents for medical devices and software now used in clinical practice.
haot.lin@hotmail.com
This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.

By Chow Ee-Tan
An ocular oncologist, researcher, mentor and mother, Dr. Jesse Berry is shaping the future of eye cancer care while staying grounded in the values that matter most.
Some physicians build careers. Other build movements. Dr. Jesse Berry seems to be doing both. She is a clinician, researcher, mentor, advocate and mother. But beyond the titles, what defines her is the compassion woven into every role. In every patient encounter, every research breakthrough and even in her thoughtful blog posts, she advances not only science but a vision of medicine where care, equity and humanity are inseparable.
What makes Dr. Berry stand out, whether through her published work, her writing or her interview, is her ability to hold worlds together that most would consider impossible to balance.
She carries multiple portfolios with uncommon grace. At Children’s Hospital Los Angeles (CHLA), she directs the ocular oncology service, caring for children with retinoblastoma and adults with rare ocular cancers. She also leads an NIH-funded laboratory exploring aqueous humor “liquid biopsy,” a technique reshaping diagnosis and treatment. Add in her roles as mentor, social media voice and mother of two daughters, and
the picture is complete: professional excellence tied to deep compassion and a determination to ensure every child, wherever they live, has access to life-saving care.
At the core of every role is one constant: Dr. Berry’s determination to advance care while never losing sight of the humanity at medicine’s heart.
To call ocular oncology demanding would be an understatement. “One of the greatest challenges in ocular oncology is balancing the urgency of saving a child’s life and vision with the delicate realities of treatment,” Dr. Berry answered candidly when asked about the biggest challenge in her field.

2025.
She emphasized how rare eye cancers like retinoblastoma make advancing research and securing funding especially difficult, even as progress remains incredibly necessary.
“Globally, disparities in access to care remain a significant challenge. Children in low-and middleincome countries often present late with advanced disease,” she said. “We’ve seen this recently even in L.A. This drives me to keep pushing for innovation, collaboration and advocacy to ensure equitable care for all children.”
For many physicians, social media is an afterthought. For Dr. Berry, it’s a natural extension of her clinical and research work. Her blog, Hope, Vision and a Cure, along with social media presence amplify her work beyond the walls of CHLA.
Dr. Berry has found ways to use social media meaningfully, both as a professional and a layperson.
She blogs and shares on platforms like Twitter and Instagram, not out of obligation, but when she has something important to say.
“Social media and blogging allow me to bridge the gap between the clinic, the lab and the community,” she explained. “They provide a platform to educate families, share research breakthroughs and advocate for awareness of retinoblastoma worldwide.”
Dr. Berry also values the way these platforms connect her to the next generation of ophthalmologists. “I find it to be a powerful space to mentor young physicians and scientists, offering a glimpse of what an academic and clinical career can look like,” she said.
And it’s not just professional utility. “It humanizes the work,” she noted. “Families and friends see the person behind the white coat, and colleagues see the passion that drives the science and the care.”
Despite the intensity of her work, Dr. Berry makes space for joy at home. “At work, my focus is on my patients and my team. At home, it’s on my husband and my two young daughters,” she said.
“Taking on leadership roles, from mentoring fellows to directing a clinical program, challenged me to grow beyond myself when I learn to listen deeply, and to make decisions that put patients and people first.”
And the things that ground her are not grand but simple. “Family
dinners, pool time, trips to the beach, Disney adventures or exploring a new place together. Those moments anchor me,” she reflected. “They remind me why I do the work I do and they restore the joy and energy I need to return to my patients and research with full heart.”
This clarity of purpose allows her to approach medicine not as a job but as a calling. “Medicine is not a job for me, it’s a career and a passion,” she said, and that passion is fuelled and sustained by her life outside the hospital and lab.
Dr. Berry’s journey as a leader has been shaped by a tapestry of experiences: early mentors who modelled curiosity and humility, patients and families who taught her courage and trust, and leadership roles that demanded growth and deep listening.
“Taking on leadership roles, from mentoring fellows to directing a clinical program, challenged me to grow beyond myself when I learn to listen deeply, and to make decisions that put patients and people first,” she said.
is preserved, or when I can tell a parent that the cancer is cured, is profoundly rewarding.”
Yet her drive is not only rooted in the present. Research continues to open new doors, from liquid biopsy to global collaborations.
“Pushing the boundaries of research gives me hope that tomorrow’s treatments will be safer, less invasive,” she said. “And the use of aqueous liquid biopsy may help to do this in a personalized fashion, making [treatments] available to every child, no matter where they live.”
Between the patients’ resilience and the promise of discovery, Dr. Berry finds fresh fuel every day to keep pushing forward. After all, building the future of eye cancer care takes not only sharp science but also a full heart.

Motherhood has also been transformative. “It has profoundly influenced me. It has deepened my empathy and sharpened my priorities as a leader,” she shared. Beyond innate qualities, she views resilience itself as a skill to be learned and practiced, honed by both medicine and motherhood.
For all the complexity and challenge of ocular oncology, Dr. Berry finds her career very satisfying and rewarding.
“What inspires me most is the resilience of children and families facing retinoblastoma, uveal melanoma and other rare ocular cancer diagnoses,” Dr. Berry said. “The moment when a child’s vision
Dr. Jesse Berry wears a lot of hats, and she wears them well. She is chief of Ophthalmology, director of the Vision Center and director of Ocular Oncology and Retinoblastoma Programs at Children’s Hospital Los Angeles, while also serving as professor of Ophthalmology and director of Ocular Oncology at the USC Roski Eye Institute.
A Harvard-trained physician, Dr. Berry completed her ophthalmology residency and fellowship at CHLA and USC under the mentorship of Dr. Jonathan Kim and Dr. A. Linn Murphee, founder of the hospital’s Retinoblastoma Program.
Dr. Berry has made it her mission to push the field forward. She pioneered the use of aqueous humor as a liquid biopsy for retinoblastoma and other ocular tumors, groundbreaking work funded by the National Cancer Institute.
She also leads globally, as founder of Women in Ocular Oncology, current president of the International Society of Ocular Oncology (20242026) and treasurer of the American Association for Ophthalmic Oncology and Pathology.
Her clinical expertise spans retinoblastoma and uveal melanoma, and she holds two prestigious endowed chairs in cancer research.
jesse.berry@med.usc.edu


and other cardiovascular risk factors, while patients with DR often already face a higher likelihood of arterial thromboembolic events.
Clinical trials generally suggest minimal systemic risks from antiVEGF treatment, yet some factors appear to raise the stakes. Patients with pre-existing cardiovascular or kidney disease may be more vulnerable, and systemic absorption rates differ among agents. Dosing frequency, too, may affect cumulative exposure.
By April Ingram
Anti-VEGF is a vision lifesaver, but is the body along for the ride? Experts weigh in on systemic safety, risks and practical patient strategies.
No one doubts that intravitreal anti-vascular endothelial growth factor (anti-VEGF) injections have transformed the management and outcomes of retinal diseases such as wet agerelated macular degeneration (AMD), diabetic retinopathy (DR) and retinal vein occlusion (RVO).
VEGF, after all, is the troublemaker driving pathological angiogenesis and vascular permeability, leading to neovascularization and intraretinal fluid buildup when left unchecked. Anti-VEGF is the bouncer at the door, keeping things orderly.
Originally developed for systemic diseases and delivered intravenously,
anti-VEGF therapies were associated with systemic side effects, including hypertension and arterial thromboembolic events. While intravitreal injections largely confine the drug to the eye, small but detectable amounts still enter systemic circulation, prompting concerns about potential risks to the heart, brain and kidneys.
The visual benefits are undeniable, but it is worth remembering that many patients receiving anti-VEGF are elderly and may carry a host of systemic comorbidities. Some retinal conditions also come with systemic baggage of their own. Branch retinal vein occlusion (BRVO), for instance, is tightly linked with hypertension
To shed more light on this, two large analyses examined systemic safety in patients treated with intravitreal antiVEGF injections.
Dr. Rajeev Muni, staff vitreoretinal surgeon at St. Michael’s Hospital and the Kensington Eye Institute in Toronto, Canada, led a meta-analysis of 20 randomized controlled trials involving more than 12,000 eyes.
“We
found no significant difference in the risk of systemic thrombotic events between commonly used antiVEGF agents.”
-
“We found no significant difference in the risk of systemic thrombotic events between commonly used anti-VEGF agents,” he said. His group concluded that treatment decisions should be guided by factors like efficacy, durability and cost rather than fears of systemic risk.1
“Based on this evidence, it is not recommended to modify anti-VEGF treatment regimens solely out of concern for thrombotic events, as there is no indication that there is a significant risk of these events,” he emphasized. “Intravitreal anti-VEGF therapy is considered systemically safe in this regard.”
Dr. Roomasa Channa, associate professor in the Department of Ophthalmology and Visual Sciences
at the University of WisconsinMadison (United States), and her team took a different approach.
“Anti-VEGF injections were independently associated with a higher likelihood of developing any systemic adverse event after controlling for confounders.”
- Dr. Roomasa Channa
Analyzing data from more than 1.7 million U.S. veterans with type 2 diabetes, including about 14,000 who received anti-VEGF injections, her group reported a striking finding.2 “The five-year cumulative incidence of any systemic adverse event (i.e. coronary artery disease, cerebrovascular disease and/ or kidney disease) was 37.0% in the injection group versus 18.4% in the non-injection group,” she explained. “Anti-VEGF injections were independently associated with a higher likelihood of developing any systemic adverse event after controlling for confounders.”
Dr. Channa’s study further highlighted that risks climbed in certain subgroups, including current smokers, patients with proliferative DR, and those with higher DeyoCharlson Comorbidity Index (DCCI) scores.
So what does this mean in practice?
Dr. Channa advised balancing the benefits of anti-VEGF therapy with alternative strategies. “While antiVEGF injections are the mainstay of treatment for many retinal vascular diseases, alternative treatments such as laser or steroids, and strategies to reduce anti-VEGF injection burden should be considered when possible, particularly for patients with a high burden of systemic co-morbidities and in smokers,” she said.
Dr. Muni also underscored the importance of coordinated care. “For patients at higher systemic risk for thrombotic events, such as those with a history of cardiovascular disease, cerebrovascular disease or clotting disorders, it is essential to involve their primary care physician, cardiologist, neurologist, hematologist or other relevant specialists if these risks are not optimally managed,” he explained.
Patients today have more access to medical information than ever, so clear and balanced communication is key. While anti-VEGF injections have not been definitively linked to increased risk of major arteriovenous thrombotic events, clinicians should counsel patients that certain systemic risks exist, especially for those with diabetes, prior stroke or recent myocardial infarction.
1. Jhaveri A, Balas M, Muni RH, et al. Systemic arterial and venous thrombotic events associated with anti-vascular endothelial growth factor injections: A meta-analysis. Am J Ophthalmol. 2024;262:86-96.
2. Zafar S, Walder A, Channa R, et al. Systemic adverse events among patients with diabetes treated with intravitreal anti-vascular endothelial growth factor injections. JAMA Ophthalmol. 2023;141(7):658-666.

Dr. Muni advised, “When counseling patients, it is important to emphasize that the safety of intravitreal anti-VEGF agents has been extensively evaluated in large clinical trials, with no significant difference in the risk of thrombotic events among the various agents. The risk is considered to be no higher than with placebo injections, and the absolute likelihood of such events occurring as a result of treatment remains very low.”
He adds, “Patients can be reassured that the visual benefits of antiVEGF therapy for conditions such as neovascular age-related macular degeneration, diabetic macular edema and retinal vein occlusion far outweigh the potential systemic risks of thrombotic events, and this message may apply consistently across the different retinal diseases we treat.”
Dr. Rajeev Muni wears many hats in Toronto’s ophthalmology scene. A staff vitreoretinal surgeon at St. Michael’s Hospital, The Hospital for Sick Children and the Kensington Eye Institute, he brings precision and compassion to some of the most complex cases in eye care. Beyond the operating room, he helps steer the future of vision science as vice-chair of Clinical Research in the Department of Ophthalmology and Vision Science at the University of Toronto. rajeev.muni@utoronto.ca

Dr. Roomasa Channa is an associate professor in the Department of Ophthalmology and Visual Sciences at the University of Wisconsin-Madison in the United States, where she also co-directs the Artificial Intelligence unit. A skilled retina surgeon and innovative researcher, she focuses on unraveling the complex factors that drive vision loss in diabetic retinal disease. Her work doesn’t stop with understanding the problem, she’s also harnessing cutting-edge technology, including AI, to transform how these conditions are detected, managed and ultimately prevented.
Her research team has drawn support from a wide-range of prestigious institutions, including the National Eye Institute, NASA, the U.S. Department of Defense, Johns Hopkins Children’s Center, and the Veteran Affairs hospital. This breadth of funding highlights both the importance of her work and its potential impact on eye care worldwide.
And so, anti-VEGF therapy remains a cornerstone of retinal care, with systemic risks that are low but worth keeping an eye on. As always, the art lies in balancing sight-saving benefits with whole patient care, and that’s a calculus ophthalmologists are well accustomed to solving.
Beyond the data and technology, Dr. Channa is driven by a clear mission to improve access to care and close the gaps that leave too many patients behind. By combining surgical expertise, research leadership and an eye toward innovation, she is helping to shape a future where fewer people lose their sight to diabetic eye disease.
rchanna@wisc.edu

FIllustration: Leremy/Shutterstock.com
By Elif Uslu
ew scenarios in ophthalmology test a clinician’s nerves quite like the patient who presents with both uveitis and central serous chorioretinopathy (CSCR).
On one hand, corticosteroids are the time-honored weapon against inflammation. On the other, that very treatment can pour fuel on the CSCR fire, worsening subretinal fluid and sabotaging vision. It’s a therapeutic balancing act that feels less like medicine and more like tightrope walking…except the safety net is someone’s sight.
The danger is not just pharmacologic but diagnostic. CSCR often masquerades as active uveitis, tricking even the sharpest clinicians into escalating steroids when, in reality, they are quietly stoking the problem. The result is a vicious cycle of treatment and harm.
To break that cycle, modern practice is shifting. Steroid-sparing agents, biologics and advanced imaging now form the backbone of strategies designed to calm inflammation
without tipping patients into CSCR relapse.
Corticosteroids: Friend, foe or double-edged sword?
“Inappropriate or prolonged steroid use in patients with CSCR can lead to atypical clinical courses, including exudative retinal detachments.”
- Prof. Marion Munk
Prof. Marion Munk (Switzerland) frames the dilemma with clarity and caution. “My approach was always very conservative with corticosteroids in patients at risk of or with coexisting CSCR. Even short courses of steroids can exacerbate choroidal hyperpermeability and worsen subretinal fluid,” she says. “I try to avoid it completely, and, if
necessary, I now prioritize the lowest effective steroid dose, the shortest duration possible and often try not to bridge at all with steroids until the effect of steroid-sparing agents sets in.”
“Intravitreal steroids are completely avoided in this setting,” Dr. Munk adds.
Assoc. Prof. Hüseyin Baran Özdemir (Turkey) echoes this vigilance. “Inappropriate or prolonged steroid use in patients with CSCR can lead to atypical clinical courses, including exudative retinal detachments,” he warns. “These complications may cause more harm than the uveitis itself. If steroid use is absolutely unavoidable, I proceed with extreme caution and monitor the patient very closely for early signs of CSCR development or worsening.”
Imaging: The compass in complexity
In the delicate overlap of uveitis and CSCR, precision is everything. A study published in Journal of Ophthalmic and Vision Research analyzing 1,657 patients with posterior uveitis revealed that nearly 1% were actually CSCR misdiagnosed as inflammation.1 That small fraction carries big consequences, resulting in patients given high-dose corticosteroids that not only fail to help but actively worsen their disease.
“Multimodal imaging is critical for distinguishing active inflammatory fluid from CSCR-related subretinal fluid,” explains Dr. Jay Chhablani (United States). “OCT, fluorescein angiography and ICGA provide complementary insights, helping avoid misdiagnosis and ensuring that therapeutic adjustments target the underlying pathology rather than merely the fluid.”
Dr. Alay Banker (India) highlights the power of comprehensive imaging in this diagnostic minefield. “Dense structural OCT and enhanced-depth imaging of the choroid (EDI-OCT) are indispensable, but I rarely stop there,” he says. “ICG, fundus autofluorescence, fluorescein
angiography (FFA) and even widefield FFA and autofluorescence give us the broader picture. Together, these tools help us determine whether we’re dealing with true uveitis activity or CSCR masquerading as inflammation.”
Prof. Munk adds that for monitoring, SS-OCT or EDI-OCT are her mainstay, while FA and ICGA are essential in moments of diagnostic doubt or when planning photodynamic therapy. She also highlights the growing role of OCT angiography in ruling out secondary choroidal neovascularization, which is a complication that can arise in both conditions.
“ICG, fundus autofluorescence, fluorescein angiography (FFA) and even wide-field FFA and autofluorescence give us the broader picture. Together, these tools help us determine whether we’re dealing with true uveitis activity or CSCR masquerading as inflammation.”
- Dr. Alay Banker
Determining when—and how— to taper steroids in this patient population is an art in itself, requiring equal parts science and instinct.
Prof. Munk tapers when inflammation is quiet yet fluid persists or worsens in a pattern consistent with CSCR rather than uveitis, “particularly subfoveal fluid on OCT without evidence of active vitreous cells or angiographic leakage.”
In such cases, prolonging steroids risks fueling CSCR rather than controlling inflammation. But if inflammatory signs persist— vitreous haze, angiographic leakage or structural progression—
she pivots quickly to systemic immunosuppression.
That balance—knowing when to taper, when to escalate and when to abandon steroids altogether—was echoed by Assoc. Prof. Özdemir, who places phenotype and disease course at the center of his decision-making.
“If the patient has chronic uveitis without a severe flare, then my clear preference is to initiate systemic immunosuppression,” he notes. “Similarly, in patients with recurrent uveitis, I prefer starting steroidsparing immunosuppressives rather than repeating systemic corticosteroids with each new flare.”
Building on that theme of minimizing steroid burden, Dr. Chhablani adds, “When subretinal fluid is primarily CSCR-related and inflammation is controlled, tapering steroids and optimizing steroid-sparing therapy is preferred to prevent further CSCR exacerbation.”
The rise of immunosuppressives and biologics
As the limits and dangers of corticosteroids become clearer, the field is moving decisively toward steroid-sparing therapies. These treatments, once considered second-line, are now viewed as the cornerstone of management.
“Steroid-sparing immunosuppressants are central to management today. Agents such as methotrexate, mycophenolate mofetil, azathioprine, or biologics like adalimumab allow durable control of intraocular inflammation while minimizing corticosteroid exposure,” says Prof. Munk. “Their use not only prevents steroid-induced worsening of CSCR but also provides a longterm therapeutic backbone for patients with recurrent or chronic uveitis.”
Dr. Banker underscores how far the field has come, saying, “Immunosuppressives, JAK [Janus kinase] inhibitors and biologics are currently the mainstay as steroidsparing treatment and in some cases are being used even as primary therapy.”
Still, steroids cannot always be withdrawn. “If steroids cannot be stopped, treating CSCR with lowdose photodynamic therapy [PDT] or focal laser might be considered,” he added.
Assoc. Prof. Özdemir stresses that tailoring therapy to severity is essential. For patients with mild-to-moderate chronic uveitis and coexisting CSCR, he favors conventional immunosuppressives as his first-line steroid-sparing options. But in severe flares, he leans toward anti-TNF (tumor necrosis factor) agents, particularly infliximab, for its rapid onset. For long-term maintenance, he tends to switch to adalimumab.
Despite advances, managing uveitis with concurrent CSCR remains riddled with unanswered questions.
“Gaps remain in predicting which uveitis patients are at risk for CSCR and how best to combine steroid-sparing therapies,” says Dr. Chhablani. He calls for research into reliable biomarkers, individualized treatment protocols and imagingguided strategies that balance inflammation control with CSCR risk.
Even with today’s sophisticated tools, uncertainty persists. Assoc. Prof. Özdemir notes that despite careful use of OCT, ICGA and autofluorescence, some patients “fall into a diagnostic gray zone.” Biomarkers that flag vulnerability before steroids trigger complications would be invaluable, as would new immunosuppressives that control inflammation without worsening CSCR.
For Dr. Banker, the next frontier lies in innovation. “Local non-steroidal therapies targeting different pathways need to be researched,” he says, envisioning targeted inflammation control without CSCR collateral damage.
Prof. Munk highlights a broader gap: the absence of evidence-based guidelines. Current management relies heavily on extrapolation from

separate uveitis and CSCR studies. “We really need larger datasets to clarify which immunosuppressive agents are most effective in this dual pathology, and whether certain biologics might reduce both inflammation and choroidal hyperpermeability,” she says.

She also points to overlooked questions. “Often these patients have systemic lupus erythematosus and are on Plaquenil. Since this drug can cause maculopathy by itself, it would be good to understand whether its use should be considered a strict contraindication,” she concludes.
“We really need larger datasets to clarify which immunosuppressive agents are most effective in this dual pathology, and whether certain biologics might reduce both inflammation and choroidal hyperpermeability.”
- Prof. Marion Munk
Contributors
Prof. Marion Munk is a uveitis and medical retina specialist whose career blends clinical expertise with bold innovation. She serves as chief scientific officer and head of research at Augenarzt-Praxisgemeinschaft Gutblick AG, professor at Inselspital, University Hospital Bern and adjunct professor at Northwestern University in Chicago. On top of that, she is director of Eyegnos Consulting and chief medical officer at Isarna Therapeutics—roles that reflect her knack for bridging science, strategy and patient care. With more than 270 scientific articles to her name, Prof. Munk is a force in ophthalmic research. Her work spans image processing, artificial intelligence, macular diseases and uveitis, always with a focus on turning complex data into insights that matter. She currently chairs research at the International Retinal Imaging Society and lends her expertise as an editorial board member for journals including IOVS, Acta Ophthalmologica, Ocular Inflammation and Infection, BMC Ophthalmology and EyeNet. Whether pioneering AI applications or fine-tuning imaging techniques, Prof. Munk brings rigor, creativity and a touch of Swiss precision to everything she does.
marion_munk@hotmail.com

Managing uveitis with coexisting CSCR is less like following a protocol and more like playing chess. Every move demands foresight, strategy and a careful reading of the board. Steroids may still have a role, but the spotlight is shifting toward immunosuppressives, biologics and smarter imaging. Until biomarkers and guidelines catch up, clinicians remain both detectives and tightrope walkers, balancing inflammation and fluid one cautious step at a time.
1. Papadia M, Jeannin B, Herbort CP. Central serous chorioretinopathy misdiagnosed as posterior uveitis and the vicious circle of corticosteroid therapy. J Ophthalmic Vis Res. 2015;10(3):303-308.
This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
Dr. Alay Banker is the director of Banker’s Retina Clinic and Laser Centre in Ahmedabad, India, a practice he has led with dedication since 2007. His career began in the U.S. as a clinical instructor and fellow at the University of California, San Diego, in the Department of Diseases of Retina and Vitreous, Uvea and Inflammation of Eye—a formative chapter that set the tone for an ambitious career.
Dr. Banker quickly made history, becoming the first Indian to receive the AAO International Scholar Award (2010) and, earlier, the youngest India to receive the AAO Achievement Award (2006). His ongoing service to peers and society has earned further recognition, including AAO Senior Achievement Award (2013) and the Dr. Piyush Patel Award for Service to Society and Mankind from the Ahmedabad Medical Association (2013).
A senior founding editor of the Retina Image Bank , Dr. Banker is as prolific as he is passionate. He has presented at more than 250 international and national conferences, authored over 40 peerreviewed papers and contributed to five chapters to international books— always with an eye toward advancing retinal care and education worldwide. alay.banker@gmail.com

Hüseyin Baran Özdemir is an associate professor of Ophthalmology at Gazi University Faculty of Medicine in Ankara, Turkey. His expertise spans vitreoretinal surgery, medical retina and uveitis, and he has played a key role in multicenter studies on retinopathy of prematurity as well as pioneering adjuvant strategies for complex retinal detachment and uveitis.
After completing his residency at Gazi University, Dr. Özdemir sharpened his skills in the Uveitis Unit at Ulucanlar Eye Research and Training Hospital. He has also earned top international credentials, passing the European Board of Ophthalmology exam in 2019 and the ICO Advanced exam in 2021.
Beyond the clinic and OR, Dr. Özdemir is passionate about membership and leadership. He currently serves as president of the Turkish Ophthalmological Association, Young Ophthalmologists Group (2024 - present), helping shape the next generation of eye specialists. From advancing treatments to guiding young colleagues, Dr. Özdemir is committed to making a lasting mark in ophthalmology.
huseyinbaranozdemir@gazi.edu.tr

Dr. Jay Chhablani is a vitreo-retina surgeon at the University of Pittsburgh Eye Center in the United States, where he also leads the Choroid Analysis and Research Lab. His team dives deep into both computational and biological research, with the choroid as its central focus.
A globe-spanning career has shaped Dr. Chhablani’s expertise. After completing his vitreo-retina fellowship at Sankara Nethralaya in India, he became an ICO fellow at the Jules Gonin Eye Hospital in Switzerland. He then served as a clinical instructor at the Jacobs Retina Center, Shiley Eye Center, University of California, San Diego (USA), before returning to India to join the LV Prasad Eye Institute faculty. In 2019, he brought his experience and energy to Pittsburgh. With more than 500 peerreviewed articles to his name, Dr. Chhablani is one of the most published voices on the choroid. He has also edited three authoritative texts: Choroidal Disorders, Central Serous Chorioretinopathy, and Choroidal Neovascularization . Beyond publications, he is an active member of the Macula Society and contributes to committees of leading international ophthalmology societies, including the AAO.
jay.chhablani@gmail.com
The race to restore sight for patients living with retinal degeneration just gained serious momentum.
Nanoscope Therapeutics (Texas, United States) recently announced that its lead candidate MCO-010 (sonpiretigene isteparvovec) has earned five new Orphan designations from the European Medicines Agency (EMA), covering a wide range of retinal dystrophies. At the same time, the U.S. Food and Drug Administration (FDA) has granted Regenerative Medicine Advanced Therapy (RMAT) designation for Stargardt disease (SD)—a strong signal of regulatory confidence in the therapy’s potential.
The EMA designations span non-syndromic and syndromic rod-dominant dystrophies, cone-dominant dystrophies and macular dystrophies, paving a pathway that could impact dozens of currently untreatable conditions. The FDA’s RMAT status for SD builds on prior Orphan Drug and Fast Track designations in both SD and retinitis pigmentosa (RP).
These twin recognitions mark a critical step in positioning MCO-010 as a potential disease-agnostic therapy platform for patients living with progressive vision loss.
“Securing RMAT designation for Stargardt disease in addition to our prior FDA designations for SD and RP is a major validation for our therapies that warrant expedited development and review,” said Sulagna Bhattacharya, CEO of Nanoscope, in a news release. “Combined with five EMA Orphan designations, these achievements highlight the global momentum behind our MCO platform as a potential visionrestoring therapy for patients with few or no treatment options.”
A vision-restoring platform
At its core, MCO-010 (multi-characteristic opsin) optogenetic platform is designed to reimagine how degenerative retinal diseases are treated. Unlike gene-specific or surgical interventions, MCO-010 is a one-time, in-office intravitreal therapy.
It works by activating dense bipolar retinal cells to become light-sensitive, harnessing existing visual circuitry even after photoreceptor death. The approach requires no genetic testing, no surgery and
no repeat dosing, making it broadly compatible with standard retina clinic workflows.
Clinical progress has reinforced this promise. In the RESTORE Phase IIb/III trial for retinitis pigmentosa (RP)—a multicenter, randomized, double-masked, sham-controlled study—MCO-010 delivered positive results, prompting Nanoscope to initiate a rolling Biologics License Application (BLA) submission to the FDA. If approved, the therapy could become a new standard of care for RP patients.
Momentum extends beyond RP. The STARLIGHT Phase II trial in SD yielded encouraging data, and a Phase III registrational trial in SD is set to launch in 2025. In parallel, Nanoscope plans a Phase II trial in geographic atrophy (GA) later this year, further expanding the therapy’s potential reach.
Retinal degenerative diseases such as RP, SD, macular dystrophies and syndromic retinal disorders affect millions globally, with no effective therapies available today.
Regulatory recognition creates new opportunities. In Europe, EMA Orphan status offers protocol assistance and up to 10 years of market exclusivity following approval. In the U.S., Orphan, Fast Track and RMAT designations enable accelerated development, flexible trial design and seven years of exclusivity upon approval.
Together, these regulatory milestones combined with advancing clinical programs underscore the potential of MCO-010 to transform the treatment landscape for retinal degeneration and offer hope to patients facing irreversible vision loss.
Results from the RESTORE Phase 2b/3 for RP (NCT04945772) and STARLIGHT Phase 2 clinical trial for SD (NCT05417126) can be found at clinicaltrials.gov. A version of this article was first published on piemagazine.org.

By Kendra Bruning
At EURETINA 2025, five talks revealed how microglia, ischemia and vessel caliber signal risk long before vision fades.
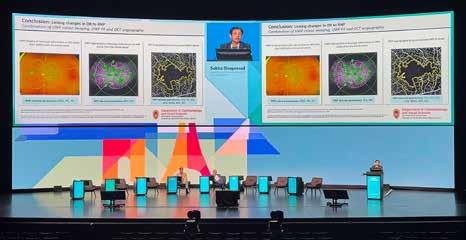
The Grand Amphitheater of Palais des Congrès in Paris was the arena for a session devoted to diabetic retinopathy (DR) on Day 2 of the 25th Congress of the European Society of Retina Specialists (EURETINA 2025).
Guided by Prof. Edoardo Midena (Italy) and Prof. Dr. Reinier Schlingemann (The Netherlands), five speakers tackled the condition from multiple vantage points spanning cellular inflammation, ischemic burden, structure-function correlation, AI-guided phenotyping and vascular signatures.
What emerged was a portrait of DR as a disease of early warning signs: quiet structural shifts that accumulate, interact and ultimately shape visual fate. It was science with urgency, casting light not just on where the retina stands today, but how the future of management might be rewritten.
Zooming in on microglia’s role
Kicking off Friday morning’s session, Dr. Andreas Pollreisz (Austria) took the Grand Amphitheater deep into the retinal microenvironment where
microglia, the immune sentinels of the retina, may be sounding early alarms in disease progression.
Using adaptive optics optical coherence tomography (AO-OCT), his team achieved volumetric, in vivo imaging of individual microglia with micrometer precision. The prototype system provided 10 times the resolution of conventional OCT, enabling real-time visualization of ramified (resting) versus activated microglia.
In diabetic eyes, there was a striking increase in activated microglia, particularly near the fovea, closely linked to other hallmarks such as microaneurysms, hard exudates and hyperreflective foci under 30 μm.
“Adaptive optics OCT allows the visualization of contrast structural details in diabetic eyes over time which are undetected with conventional OCT imaging,” Dr. Pollreisz explained.
“Through increased imaging resolution it allows in vivo retinal microglia sense, their retinal location, inter-retinal location and their activation states in humans.”
Dr. Pollreisz stressed that AOOCT not only sharpens disease characterization at the cellular level, but also opens doors for monitoring early progression and therapeutic response. While imaging deeper retinal layers remains challenging, refinements in dual-signal resolution may soon widen this window into DR’s earliest inflammatory footprint.
Prof. Sobha Sivaprasad (United Kingdom) delivered a sobering update on the challenge of retinal ischemia measurement in DR, reminding the audience that a true gold standard is still out of reach.
Drawing on insights from the INSPIRE study and trials such as the Rho-PDE inhibitor (PER-1) and CRIMSON, she outlined how current tools often fall short.
While Diabetic Retinopathy Severity Scale (DRSS) scores can align with nonperfusion at a population level, the variability between individual patients is striking. Moreover, anti-VEGF therapy can improve DRSS scores without necessarily improving perfusion, creating a dissociation between clinical grading and vascular reality.
“We actually do not have any accurate methods in quantifying retinal ischemia at present,” Prof. Sivaprasad noted, emphasizing the mismatch between scoring systems and perfusion status.
Conventional imaging like fundus photography, ischemic index mapping and even widefield angiography struggles with reproducibility, particularly at the periphery. Automated segmentation and AI-based analysis may improve matters, but variability is still apparent.
Prof. Sivaprasad pointed to emerging tools such as macular ischemic indices, OCT-A and flicker ERG, while stressing that central ischemia does not reliably predict peripheral involvement. For now, she argued, composite biomarkers will be essential for future trials, as demonstrated in early anti-SEMA3A studies. Until then, ischemia remains an elusive and fuzzy endpoint.
Prof. Noemi Lois (United Kingdom) presented findings from a rigorous two-year longitudinal study that probed the complex relationship between retinal ischemia and retinal sensitivity in DR.
Unlike earlier investigations limited to the macula or short follow-up, her team overlaid microperimetry data onto fluorescein angiograms across the full posterior pole, mapping point-by-point correlations between structure and function.
The results revealed a strong association that’s still far from perfect. Non-perfused regions generally displayed reduced sensitivity, yet many perfused zones still showed functional deficits, and some ischemic areas retained normal vision.
“We found a strong correlation between perfusion status and reference sensitivity, but we found sensitivity low in some perfused areas and normal sensitivity in some non-perfused areas,” Prof. Lois explained.
Approximately half of these anomalies could be attributed to factors such as overlapping vasculature or adjacency to ischemic zones. However, the remaining unexplained cases pointed to underlying mechanisms beyond visible perfusion status.
Importantly, Prof. Lois’s team found that retinal sensitivity declined gradually over time even in perfused regions, underscoring the subtle but significant functional impact of DR progression.
Her message was that vascular imaging and functional testing tell overlapping yet distinct stories. Both are essential for clinical management and for evaluating emerging therapies targeting neurodegeneration or reperfusion.
AI as the retinal refiner in DME
Diabetic macular edema (DME) is not one disease, but a spectrum
of phenotypes and treating it as a single entity is a recipe for suboptimal outcomes. That was the message from Prof. Edoardo Midena (Italy), who opened his talk with the stark statistic that around 40% of patients fail to respond to anti-VEGF therapy after one year. The reason, he argued, is an overreliance on central subfield thickness, a crude measure that fails to capture the nuances of disease biology.
To address this, Prof. Midena’s team has developed an AI algorithm capable of segmenting and quantifying key OCT biomarkers, including intraretinal and subretinal fluid, ellipsoid zone integrity and hyperreflective foci. “The concept that we need to go to precision medicine to decide which kind of DME [we have] for this particular patient, [and] which is the best treatment,” he explained, “I can monitor this one according to the use of modern science and the technology.”
By consistently quantifying these biomarkers, the AI system enables clinicians to phenotype patients and guide therapy accordingly. In a dataset of more than 2,000 eyes, outcomes varied significantly by biomarker profile, pointing the way toward tailored, profile-driven DME management that anticipates recurrence rather than reacting to it.
Dr. Jennifer Sun (United States) analyzed a post hoc dataset of the DRCR Retina Network’s Protocol S, asking a deceptively simple question: do panretinal photocoagulation (PRP) and antiVEGF therapy leave different longterm signatures on the retinal vasculature?
Her team applied Integrated Vessel Analysis Software (IVAN) to highquality fundus photographs from 107 eyes, measuring central retinal artery and vein equivalents (CRAE and CRVE). The results revealed early divergence. CRAE thinned faster in PRP-treated eyes during the first two years, while ranibizumabtreated eyes showed slower changes but gradually caught up by year
five. CRVE shifts emerged later but ultimately showed greater thinning in the PRP group.
Importantly, vessel caliber changes were not just cosmetic. Greater thinning correlated with increased visual field loss, hinting at a possible structure-function link. “These results suggest that the two treatments may result in different rates of change in vascular caliber over time,” Dr. Sun explained, “which may need to be taken into account in future analyses of vascular caliber and treatment.”
While exploratory and limited by image availability, the findings hinted at intriguing possibilities. Vessel caliber may emerge as a biomarker not only for tracking treatment effects, but also for predicting longterm visual outcomes in proliferative DR.
While no single biomarker or imaging modality can capture the full complexity of diabetic retinopathy, this session demonstrated how close the field is getting. From microglia and ischemia to structurefunction mismatches, vessel caliber and AI-enabled prediction, each study pointed toward earlier, more nuanced detection and raised critical questions about structural change versus functional outcomes.
As the focus shifts from late intervention to true preservation, the tools of tomorrow may be those that can interpret the retina’s subtle cues long before vision fades. As EURETINA 2025 showed, the retina whispers its warnings early. The task ahead, therefore, is learning how to listen.
The 25th EURETINA Congress was held from 4-7 September, in Paris, France. Reporting for this story took place during the event. A version of this article was first published on piemagazine.org.

By Matt Herman

Retinal researchers are ditching the one-gene-one-drug playbook. From reprogramming glial cells and harnessing inflammation to metabolic tweaks and stem cell transplants, these bold, gene-agnostic strategies are rewriting the rules of retinal repair.
Forget one gene, one therapy— the future of retinal disease treatment may be universal.
Vision scientists are increasingly straying from the path of one-gene, one-treatment approaches to retinal degeneration in favor of broader, gene-agnostic strategies. At the annual meeting of The Association for Research in Vision and Ophthalmology 2025 (ARVO 2025), five pioneering researchers revealed how such strategies as manipulating inflammation, reprogramming glial cells, tweaking metabolism cycles and transplanting engineered cells could revolutionize treatment for millions worldwide suffering from blinding conditions.
With over 100 different genes linked to retinitis pigmentosa alone, and countless more involved in other retinal diseases, the gene-specific approach faces overwhelming challenges, especially in orphan diseases, where commercialization and funding for targeted approaches are limited. The novel gene-agnostic approaches on display in Salt Lake City for ARVO 2025 aim to protect, rescue or replace retinal cells regardless of the underlying genetic defect, potentially offering more universally applicable treatments for retinal diseases.
Dr. Muriel Perron’s (France) opening talk upended conventional wisdom about inflammation’s role in retinal regeneration. She described her team’s discovery that certain species of Xenopus frogs can regenerate their retina after injury through Müller cell reprogramming—and inflammation appears to be a key driver rather than a hindrance.
“We discovered a few years ago that actually Xenopus laevis can indeed regenerate its retina upon injury, thanks to Müller cells,” Dr. Perron explained. The presence of microglia, the retina’s immune cells, strongly correlated with Müller cell proliferative capacity—and her research followed this key insight.
By manipulating inflammatory conditions, Dr. Perron’s team transformed previously nonresponsive cells into proliferative ones. They identified APOE (apolipoprotein E) as a crucial molecular player.
“APOE is one of these candidates because we found that its expression correlates with Müller cell proliferative capacity,” Dr. Perron
noted. “Our knockout experiment suggests that it is required for a Müller cell proliferative response to injury in Xenopus. And it seems to be sufficient to trigger a Müller cell proliferative response in the mouse.”
These findings suggest that inflammatory signals, particularly APOE, may be therapeutically harnessed to stimulate retinal regeneration across species. Dr. Perron’s work challenges previous assumptions about inflammation in neural repair and opens new avenues for promoting regeneration in mammals with typically limited regenerative capacity.
Dr. Thanh Hoang (United States) demonstrated significant progress in reprogramming mammalian Müller glia into functional neurons. While zebrafish can naturally regenerate retinal cells, mammals have lost this ability. Dr. Hoang’s team found that simultaneously knocking out multiple factors—specifically Notch signaling components and NFI transcription factors—could trigger mammalian Müller cells to become neurons with remarkable efficiency.
When knocking out all these inhibitory factors together, around 65% of Müller cells transformed into neurons after injury. His team also developed a more streamlined approach using Neurog2 overexpression, which converted approximately 25% of Müller cells into neurons even without injury.
The reprogrammed cells primarily differentiated into bipolar and amacrine cells, with occasional rod photoreceptors. Importantly, electrophysiological recordings confirmed these new neurons responded to light stimuli and formed connections with existing retinal circuits. Dr. Hoang has extended this work to human retinal explants and is optimizing protocols to generate specific neuron subtypes for targeted replacement therapies.
“I’m very glad to see the growth of reprogramming topics in this conference. I remember when I was a postdoc a few years ago, there were only a handful of posters and talks on this. And now, especially in this conference, this increased exponentially,” he said. “My hope is that we all work together to finally push regeneration therapy to be reality in the next few years.”
Preserving cones through metabolic intervention
Dr. Yunlu Xue (United States) demonstrated how manipulating metabolic pathways could preserve cone photoreceptors in retinitis pigmentosa (RP). His work targets TXNIP, a protein that regulates glucose transport and mitochondrial function.
“In RP, for some reason, glucose gets trapped in the RPE, so they are having trouble reaching the cone photoreceptors,” Dr. Xue explained. “This is causing some sort of starvation of the cones in RP condition.”
By overexpressing TXNIP in cones or a modified version in the retinal pigment epithelium, his team achieved substantial cone preservation and maintained visual function across multiple mouse models of retinitis pigmentosa. The approach helped cells switch from glucose to lactate metabolism when glucose availability was limited.
“TXNIP is a great therapy,” Dr. Xue said in conclusion. “The C terminus of TXNIP in RPE removes GLUT1 and rescued RP cones. Full TXNIP is thus still one of the most potent alleles when put into the cones.”
Dr. Stephen Tsang (United States) presented a variety of innovative CRISPR-based approaches targeting metabolic regulation in the retina. His research revealed the crucial metabolic coupling between photoreceptors and retinal pigment epithelium.
“Photoreceptors mix lactate, and then you need the RPE to consume the lactate,” Dr. Tsang explained. “You need a balance between production and consumption.”
Dr. Tsang’s clinical insights came from an unexpected source— patients with thalassemia taking iron chelators who developed retinal degeneration. This led to the discovery that hypoxia-inducible factors (HIFs) play a critical role in retinal metabolism.
Using CRISPR to ablate HIF pathway components in either photoreceptors or RPE cells, his team demonstrated improved photoreceptor survival and function across multiple retinal degeneration models, including phosphodiesterase and rhodopsin mutations.
“This may be a fruitful area for gene-agnostic treatment,” Dr. Tsang concluded, emphasizing the therapeutic potential of metabolic reprogramming without addressing the primary genetic defect.
With the last talk, Dr. Michiko Mandai (Japan) shared her team’s progress in stem cell-based retinal replacement therapy. Her team has successfully transplanted human pluripotent stem cell-derived retinal organoids into patients with advanced retinal degeneration, with some grafts surviving for nearly four years.
“These images really motivate me to find the key to consistently reproducing this type of integration,” Dr. Mandai said, showing striking images of transplanted cells integrating with host retinas.
Building on promising initial clinical experiences, Dr. Mandai’s team developed genome-edited organoids with fewer inner retinal cells to improve integration. “We’re moving on to the genome-edited type of brain grafts where we are trying to delete these inner graft bipolar cells which sometimes seem to impede the contact between the host bipolar cells and the graft photoreceptors,” she explained.
The modified organoids showed enhanced integration in both rodent models and non-human primates. Detailed electron microscopy analysis revealed host bipolar cells extending dendrites to form functional synaptic connections with transplanted photoreceptors—a crucial step for vision restoration.
“If we find a good timing, it’s quite likely that the host can be activated,” Dr. Mandai concluded. “The use of genome-edited retinal organoid sheets is a promising option for regenerative therapy in human retinal degeneration including macular degeneration.”
Collectively, these presentations highlighted complementary approaches that could work in tandem to address the complex challenges of retinal degeneration.
While each approach on display remains at different stages of development—from basic research to early clinical trials—the session demonstrated tantalizing progress toward treatments that could transform the landscape of retinal disease management in the coming years along with the lives of the patients who need such therapies most.
Reporting for this story took place during the annual meeting of The Association for Research in Vision and Ophthalmology (ARVO 2025) held from 4-8 May in Salt Lake City, Utah, United States. A version of this article was first published on piemagazine.org
