










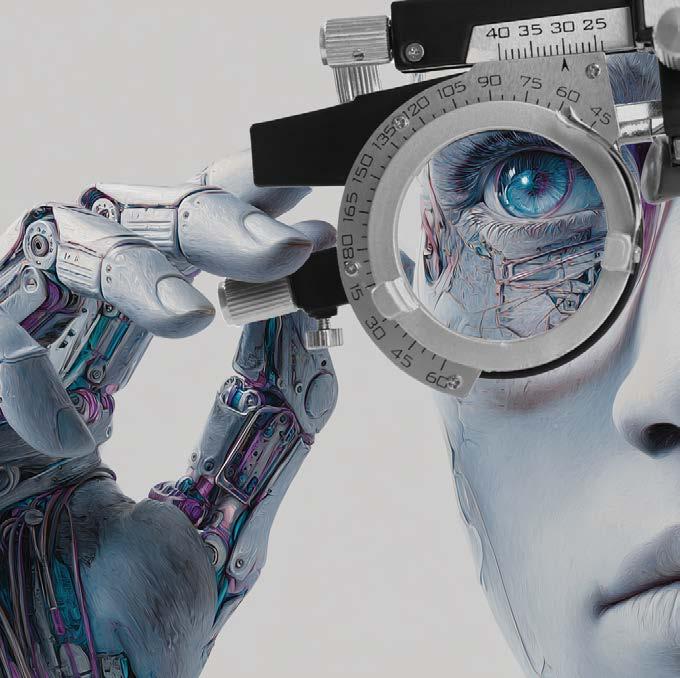
The Diagnostic technologies that will redefine the next decade p16
Amid shifting times, clarity often begins with courage… and the tools that help us look a little deeper.

Afew weeks ago, I found myself in the U.S. for a conference—the kind where your brain is buzzing from too many brilliant talks and your step count looks like you ran a marathon (thanks, exhibit hall).
After a long day of eye-opening sessions (pun intended), I grabbed an Uber back to my AirBNB, collapsing into the back seat with my badge still around my neck. My driver, a cheerful Venezuelan man, started chatting in that easy way strangers sometimes do when the traffic lights are long.
He’s been in the States for nine years, working hard, paying taxes and chasing that elusive thing called “stability.” But as we talked, it became clear that life hasn’t been easy lately.
Immigration policies have tightened, and ICE agents have been coming down hard. The prospects, he admitted, look grim. His next asylum hearing is coming up soon, and he doesn’t know what will happen. Still, he smiled. “You have to believe things will get better,” he said, one hand on the wheel, the other on his own fragile sense of faith.
That moment stayed with me. It reminded me that progress—whether in life or in eye care—often happens against a backdrop of uncertainty. We keep moving forward, hoping that the tools we have (and the ones yet to come) will help us see our way through.
Which brings me to this issue of COOKIE: all about diagnostic innovation. The new tech, smarter systems and fresh ideas that are reshaping how optometrists detect, diagnose and decide. From AI-powered imaging to VR platforms that catch what the naked eye can’t, these advances are lighting the path ahead.
So here’s to resilience—in our patients, our practices and the people who keep driving forward, even when the road is uncertain.

Diana Truong Associate Editor | PIE, CAKE and COOKIE









Dr. Carmen Abesamis-Dichoso Abesamis Eye Care & Contact Lens Center, Manila, Philippines carmen.dichoso@gmail.com

Dr. Kristie Nguyen
Dr. Feenstra and Associates; Dr. Kristie Nguyen PLLC, Florida, USA kristie817@gmail.com

Dr. Monica Chaudhry Learn Beyond Vision New Delhi, India monica.rchaudhry@gmail.com

Dr. Purvi Thomson OCL Vision London, United Kingdom Purvi@oclvision.com

Dr. Li Lian Foo
Singapore National Eye Centre (SNEC) Singapore foo.li.lian@singhealth.com.sg

Dr. Maria Sampalis Sampalis Eyecare Cranston, Rhode Island, USA msampalis@hotmail.com
Society Friends


We are looking for eye care professionals who can contribute articles to COOKIE. Interested? Let's talk! Send us an email at editor@mediamice.com.
To place an advertisement, advertorial, symposium highlight, video, email blast, or other promotion in COOKIE contact sales@mediamice.com
Matt Young CEO & Publisher
Gloria D. Gamat Chief Editor
Diana Truong Associate Editor
Maricel Salvador Graphic Designer Writers
Chow Ee-Tan
Elif Uslu
Hazlin Hassan
Kendra Bruning Tan Sher Lynn
Daniel Morgan-Williams Contributor
Matt Herman Head of Content Strategy
Hannah Nguyen COO
Travis Plage CFO
Ruchi Ranga Society Relations & Conference Manager
International Business Development
Brandon Winkeler
Robert Anderson
Sven Mehlitz


Streamline Clinical Decisions & Conversions with OCULUS Myopia Management Solutions
The OCULUS Myopia Master® and Pentacam® AXL WAVE support myopia detection, risk assessment, progression projection, and treatment efficacy analysis. Leverage exclusive growth curves and customized reports to support patient education, conversions, and compliance. Fit and evaluate ortho-k lenses while screening corneal health and stability on the Pentacam® AXL WAVE.
By Kendra Bruning
Artificial intelligence is already in the optometrist’s toolkit, improving everything from tear film analysis to retinal disease screening. Here’s how AI changes the day-to-day while clinicians keep the final say.
Apatient's retinal image pops on-screen. Before your coffee cools, an algorithm flags a subtle lesion hinting at early diabetic retinopathy (DR). This isn't sci-fi, it's Tuesday morning at the clinic.
Artificial intelligence (AI) has become the practitioner’s digital second set of eyes, supporting screening, monitoring and referrals while leaving the final word to clinicians. While
optometrists don't diagnose systemic disease, AI helps them flag risks and guide patients promptly to the right specialist's door.
AI has graduated from tomorrow's promise to today's practice. From dry eye analysis to DR screening, algorithms nest inside diagnostic devices clinicians already use daily.1-2
They don't replace judgment, they sharpen it, helping practitioners interpret complex data, reduce interobserver variability and smooth the handoff when referrals are needed.2
Across diagnostics, imaging and decision support, AI performance often matches or even surpasses human clinicians, particularly in electronic health records (EHRs) analysis, optical coherence tomography (OCT) and retinal fundus imaging. Portable, AI-enabled devices are expanding reach in underserved settings, proving intelligence doesn’t have to be tethered to a desktop.1-3
The FDA-cleared IDx-DR system (Healthvisors; Madrid, Spain) demonstrated sensitivity of approximately 87% and specificity of 90% in its pivotal trial, enabling autonomous DR detection in primary care settings without requiring an ophthalmologist onsite.5 The EyeArt (Eyenuk; California, USA) system reports even higher sensitivity—95.8% to 99.1% for referable DR—including capabilities for non-dilated imaging.2
DR has advanced quickly in AI in part because of clear lesion definitions and large, well-labeled datasets, building on foundational work in deep learning for fundus photographs.6
Today, non-mydriatic cameras paired with AI automate DR grading for population screening programs, making large-scale detection both economically viable and clinically reliable.2-4 What once demanded an army of specialists can now be efficiently triaged by tireless algorithms that can flag tiny microaneurysms at scale.
Devices like the Keratograph® 5M (OCULUS, Wetzlar, Germany) provide automated, software-based quantification of tear film stability and meibography, producing consistent outputs.2 These tools deliver objective, repeatable metrics that standardize a condition long
plagued by subjective assessment variability.
As Dr. Mark Eltis explains, "A more uniform analysis allows for better diagnosis and monitoring of progression. Just like interpreting an OCT, there's a lot of information and a computer can summarize it in greater detail faster than a human."
Corneal clarity, pixel by pixel
AI-enhanced corneal tomography is proving equally transformative, with models analyzing Scheimpflug imaging and biomechanics to achieve remarkable precision. These systems detect keratoconus with sensitivity exceeding 98% and accuracy up to 99.6%, even in subclinical cases where human observers might miss, at least in selected validation cohorts.2
"Once AI can integrate a full analysis of the nerve fiber layer, ganglion cells and visual field, that will be incredibly powerful for diagnosis and management, I see that coming in the near future."
- Dr. Mark Eltis
Glaucoma remains AI's most complex puzzle. Unlike DR's clear visual markers, glaucoma diagnosis requires integrating multiple data streams and lacks universal consensus. "If experts cannot agree on whether a case is glaucoma or not based on fundus images, we cannot expect AI to tell the difference," acknowledges Dr. Saif Aldeen Alryalat.
His research team's work with ChatGPT-4 (OpenAI; California, USA) demonstrated this challenge. While achieving 90% overall accuracy on fundus images, sensitivity remained at only 50%.7
Reviews point out that public glaucoma datasets remain smaller, less standardized and harder to validate than DR resources, complicating both model training and benchmarking.8-10
For Dr. Eltis, the solution lies in comprehensive integration. "Once AI can integrate a full analysis of the nerve fiber layer, ganglion cells and visual field, that will be incredibly powerful for diagnosis and management,” he predicts. “I see that coming in the near future".
Whose faces are in the dataset?
A critical challenge across all AI applications is dataset diversity. Many algorithms have been validated primarily in Caucasian populations, requiring region-specific adjustments to ensure equitable performance.2
Additionally, nearly a third of optometry-focused AI studies used fewer than 500 samples, with almost a fifth using fewer than 200.2
Without broad, diverse data, algorithms risk misreading shadows in underrepresented groups, meaning AI's vision can only be as inclusive as the faces it has studied.
Patient acceptance runs high when AI's role is clearly explained.1,11 "There is some research showing that ChatGPT can successfully answer many patient glaucoma questions," observes Dr. Eltis. "That may be true for dry eye as well. That is not to say that it should be used as a replacement for a doctor's visit."
A simple script helps: this tool helps us spot small changes early, but the clinician still makes the call.
Researchers are now racing to develop predictive models for myopia progression, age-related macular degeneration (AMD) risk and tailored treatment plans.1-3

Natural language processing tools mine EHRs to flag at-risk patients, while AI-enhanced OCT angiography (OCT-A) shows promise for earlier detection and monitoring in retinal disease.1-2
Meanwhile, optometry schools like Cardiff and Aston are weaving AI literacy into their curricula, preparing graduates to navigate this techenhanced landscape.12
The FDA's clearance of autonomous DR detection systems carved important pathways, though substantial regulatory obstacles still block wider adoption.5,13 "AI will have a big role in every aspect of medicine, including ophthalmology, but it will take a longer time for predictive AI to play a bigger role for two main reasons: limited data availability and regulatory hurdles," explains Dr. Alryalat.
Explainability is another key. "Having an AI model that does things without understanding the reason why would probably not be adopted in medicine,” he adds. “That's why we see researchers trying to implement explanatory models that explain the reason behind AI output.”
AI will have a big role in every aspect of medicine, including ophthalmology, but it will take a longer time for predictive AI to play a bigger role for two main reasons: limited data availability and regulatory hurdles."
- Dr. Saif Aldeen Alryalat
Keep the clinician in the loop
For practicing optometrists, AI integration brings both opportunities and responsibilities. "Doctors need to understand that regardless of
their use of AI, they are responsible for the final decision and outcome," emphasizes Dr. Eltis. "I think AI may be integrated into certain pieces of equipment, but it remains to be seen if doctors will rely on it for daily decision making".
The second set of eyes, but not the only one
AI is now routine across optometric devices, enabling earlier detection, consistent monitoring and greater access to care.
The technology's impact stretches beyond patient encounters. AI tools slash administrative burden through automated documentation while optimizing resource allocation.1-2 Industry reporting in 2025 notes that 78% of eye care specialists identify AI

Dr. Saif Aldeen Alryalat is an assistant professor in the Department of Ophthalmology and Visual Science at the University of Illinois, Chicago (USA), where he brings a rare dual expertise in glaucoma and neuro-ophthalmology. His passion? Harnessing the power of AI to tackle some of the most complex challenges in eye care.
as the most transformative trend in ophthalmology.4,11
Yet challenges still dot the landscape. Twenty percent of published AI studies in optometry report accuracy below 80%, while concerns about data quality and validation rigor shape adoption patterns.2
AI won't replace optometrists but it will equip them to deliver more precise, efficient care. The future belongs to systems that blend AI's analytical precision with human clinical judgment, ensuring technology amplifies rather than replaces the practitioner-patient relationship central to quality eye care.
Like a skilled scribe quietly taking notes during an exam, AI's second

By blending structural and functional data, Dr. Alryalat’s research is pushing the boundaries of how we diagnose diseases like glaucoma, making eye care smarter, faster and more precise. Beyond the lab, he’s a leading voice in global discussions about the ethical and equitable use of AI in medicine, ensuring technology serves patients everywhere.
A prolific writer, he has published two textbooks on ophthalmology and continues to contribute to the evolving dialogue at the crossroads of medicine and machine learning. saifryalat@yahoo.com
With over twenty years in practice and fifteen years part-time in academia, Dr. Mark Eltis has practiced in New York, California and Toronto. He is the current president of the College of Optometrists of Ontario and a director of the American Board of Optometry. Dr. Eltis has presented and published internationally and has been sought as an expert for national television and print. He is a graduate of the University of Waterloo School of Optometry and Vision Science and continues to lecture there.
Dr. Eltis has been honored as a member of the Optometric Glaucoma Society (OGS) having “demonstrated excellence in the care of patients with glaucoma through professional education and scientific investigation.” He has been a consultant for academic institutions overseas, law firms, and a subject matter expert for competency evaluations. Dr. Eltis has also been a previous examiner for US (NBEO) and the Canadian board examinations. He is the Canadian Ambassador for the American Board of Optometry and a team chair for US residency site evaluations (ACOE).
www.drmarkeltis.com
set of eyes catches details, reduces variation and frees the clinician to focus on what truly matters: the patient right in front of them.
1. Aldossary NA. Artificial intelligence in optometry: Potential benefits and key challenges: a narrative review. Int J Adv Comput Sci Appl. 2025;16(8).
2. Krishnan A, Dutta A, Srivastava A, Konda N, Prakasam RK. Artificial intelligence in optometry: Current and future perspectives. Clin Optom (Auckl). 2025;17:83-114.
3. Chen SY, Bai W. Artificial intelligence technology in ophthalmology public health: Current applications and future directions. Front Cell Dev Biol. 2025;13:1576465.
4. Znamenska M. Future of ophthalmology: 2025 top trends. Altris AI. 2025. Available at: https://www.altris.ai/article/future-ofophthalmology-2025-top-trends/. Accessed on September 13, 2025.
5. Abràmoff MD, Lavin PT, Birch M, Shah N, Folk JC. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. NPJ Digit Med. 2018;1:39.
6. Gulshan V, Peng L, Coram M, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316(22):2402-2410.
7. AlRyalat SA, Musleh AM, Kahook MY. Evaluating the strengths and limitations of multimodal ChatGPT-4 in detecting glaucoma using fundus images. Front Ophthalmol. 2024;4:1387190.
8. AlRyalat SA, Singh P, Kalpathy-Cramer J, Kahook MY. Artificial intelligence and glaucoma: Going back to basics. Clin Ophthalmol. 2023;17:1525-1530.
9. AlRyalat SA, Al Bdour M, Jammal HM. The diagnoses of glaucoma in the era of artificial intelligence. Front Ophthalmol. 2024;10:1496533.
10. AlShawabkeh M, AlRyalat SA, Al Bdour M, Alni'mat A, Al-Akhras M. The utilization of artificial intelligence in glaucoma: Diagnosis versus screening. Front Ophthalmol. 2024;4:1368081.
11. New report: Experts break down wide use of AI in optical industry. Rev Optom. April 30, 2025. Available at: https://reviewob.com/ai/. Accessed on September 13, 2025.
12. Artificial intelligence in optometry education. College of Optometrists. June 2025. Available at: https://www. college-optometrists.org/qualifying/sectorpartnership-optical-knowledge-education/ topic-of-the-month/june-2025-ai-in-optometryeducation. Accessed on September 13, 2025.
13. Desjardins P, Dennis C. AI-powered ophthalmic devices: Regulatory hurdles in the United States versus the European Union. CRS Today. February 2025. Available at: https://crstoday.com/articles/feb-2025/aipowered-ophthalmic-devices. Accessed on September 13, 2025.

Two treatments for nearly two years of relief. The Sahara trial puts TearCare on the map as a devicedriven therapy with staying power, and a serious contender to rethink how we manage MGD-related dry eye.
The Phase III findings from Sight Sciences’ (California, United States) Sahara randomized controlled trial are now in, and the results are telling.
Published in Optometry and Vision Science, the data shows that after just two TearCare treatments in the first five months, patients achieved clinically significant gains in tear stability, gland function and symptom relief that lasted nearly two years, with most requiring no additional retreatment.*
The Sahara trial at a glance
The Sahara randomized controlled trial is one of the largest and most rigorous evaluations to date of a device-based therapy for dry eye disease associated with meibomian gland dysfunction (MGD). Conducted across 19 U.S. sites, Phase III enrolled patients with moderate-to-severe disease and followed them for more than two years.
The study was structured in three stages. In Phase I, TearCare localized heat therapy with manual gland expression was compared with cyclosporine ophthalmic emulsion (AbbVie’s Restasis). TearCare achieved superior improvements in tear stability and demonstrated noninferior symptom relief.
In Phase II, patients originally assigned to cyclosporine crossed over to TearCare and experienced similar gains. Phase III extended follow-up for patients who had received two TearCare treatments, assessing the durability of benefits over the long term.
What is TearCare?
TearCare is a device-based therapy that delivers precisely controlled heat (45°C for 15 minutes) to the eyelids via SmartLids, followed by manual expression of the glands. This approach directly targets the obstructed meibomian glands that drive evaporative dry eye disease.
Unlike home remedies such as warm compresses, TearCare is designed to offer precise temperature control and professional clearance of the glands, ensuring both consistency and efficacy.
Sight Sciences introduces TearCare System
Key findings from the Phase III trial
• Improved tear film stability and gland function
At study entry, patients had unstable tears with an average TBUT of 4.4 seconds. After two TearCare
sessions, TBUT improved to around 7 seconds and remained significantly above baseline through 24 months. Meibomian gland secretion scores, which nearly tripled after initial treatment, also stayed elevated throughout Phase II.*
• Rapid symptom relief
On the Ocular Surface Disease Index (OSDI), patients improved by about 18 points after the second treatment and maintained a benefit of roughly 14 points above baseline at two years. This exceeds the threshold for clinically meaningful improvement and translates into noticeable relief in day-to-day life.*
• Durable outcomes with minimal retreatment
Two-thirds of patients never required another TearCare session during Phase III. Among those who did, the median time to retreatment was eight months. Even after retreatment, improvements remained significantly better than baseline.*
• Strong safety profile
Over 19 months, there were a small number of adverse events, none of which were linked to TearCare. No changes in visual acuity or eye pressure were observed, underscoring the safety of the procedure.*
Looking at the big picture
The Sahara Phase III trial offers some of the clearest evidence to date that an office-based, device-driven therapy can deliver sustained relief for patients with MGDrelated dry eye. For clinicians, the durability of TearCare’s effects reduces the burden of frequent retreatment and supports its use as a frontline intervention. For patients, the results translate into the possibility of nearly two years of meaningful comfort after only two treatment sessions.
Perhaps most importantly, these findings could reinforce a shift in how dry eye disease can be managed: from short-term palliative care to long-lasting restoration of gland function. TearCare’s performance in the Sahara trial positions it as a practical, repeatable and safe solution that could reshape dry eye management for both providers and patients alike.
* Hovanesian J, Ayres BD, Bloomenstein MR, et al. Durability ofthe TearCare treatment effect in subjects with dry eye disease: Stage 3 of the Sahara randomized controlled trial. Optom Vis Sci. 2025;102(8):495-504.
Editor’s Note:
This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore. A version of this article was first published on cookiemagazine.org.


By Tan Sher Lynn
Once trapped in high-tech labs and guarded by electrophysiology experts, ERG has broken free. Handheld devices are putting retinal diagnostics directly in the exam room, letting optometrists spot disease earlier, track intervention success and make treatment decisions with speed and precision.
Electroretinography (ERG) has long been hailed as a powerful diagnostic tool in eye care, but its role in day-to-day clinical practice has evolved dramatically over the last two decades. Once confined to high-tech labs, ERG is now becoming an accessible and essential tool for optometrists managing glaucoma, diabetic retinopathy and other retinal conditions.
From the lab to the exam room
Reflecting on his career as department chair at the State
University of New York, home to one of the most advanced electrophysiology labs in the U.S., Dr. Jim Thimons recalled a time when ERG equipment was largely confined to specialized centers.
About a decade ago, office-based systems began to emerge. They worked, but they were bulky and tricky to sustain. “They were quite large and very fixed—couldn’t be moved from office to office. Overall usefulness was limited by the complexity of the process,” Dr. Thimons explained.
Highly skilled operators were a must, and as trained staff moved on, practices often struggled to keep these systems functional. Utilization eventually “fell off notably because… it just became a very difficult system to support,” he said.
The true turning point arrived with the introduction of handheld ERG devices, such as those developed by LKC Technologies (Maryland, USA). “The newest generation—handheld systems like the RETeval—has effectively revolutionized in-office ERGs because of their simplicity of use and ease of transport,” he commented.
Dr. Thimons now uses the device across multiple offices daily, performing 10 to 15 tests a day. “It works exceptionally well, and the quality of the outcome is excellent,” he said.
Handheld systems also simplified reporting, especially in cases of diabetes management. “The company has put a fair amount of energy into developing the diabetic retinopathy score, which is an invaluable resource for myself as the family clinician, but equally so for the general medical diabetic specialty practice clinician,” Dr. Thimons explained.
Unlike older systems that generated pages of cryptic data, today’s ERG allows clinicians to share a single score to a patient’s physician, making communication far clearer and more actionable.
Dr. Thimons emphasized that modern ERG technology has become indispensable in managing chronic diseases. “I see a lot of patients every day. I receive referrals from countless medical practices for their diabetic patient care, and, as a result, this device has effectively revolutionized my decision making,” he said.
One case illustrates the impact. A patient believed their diabetes was well-controlled with an A1C around seven to eight percent, yet the ERG revealed a diabetic retinopathy score of 25.2, signaling a high risk
of vision loss within three years. “I communicated that to the doctor, and the doctor used that information to change or modify management,” Dr. Thimons said.
“The beauty of this approach is that when the patient returns in six months and I redo the tests, I may see a score of 21 or 20, indicating that they had initially been at high risk. However, thanks to vigilant management by the physician, we can demonstrate a notable reduction in both their risk and current disease progression, often resulting in a mild to low-moderate level of progression,” he explained. “This approach is useful not only as a diagnostic tool and a way to communicate effectively with the primary managing physician, but it’s also excellent for measuring the success of interventions.”
The handheld ERG device is equally valuable in glaucoma care. “It’s a terrific tool because physical examination shows anatomic reference, visual field shows functional status, but this test identifies physiologic stress much earlier,” Dr. Thimons noted.
By detecting stress in retinal ganglion cells before structural or functional changes become apparent, ERG adds a crucial layer to early intervention.
The device is also approved in the U.S. for evaluating glaucoma suspects to determine risk of progression into glaucoma and optic nerve damage. “I use it for patients with elevated intraocular pressure but no notable nerve damage. Even when nerve fiber layers, ganglion cells and visual fields appear largely normal, this test can detect physiologic stress at the ganglion cell and macular levels before OCT or visual field testing shows damage,” he explained. “You can think of it like corneal ischemia or early biochemical changes. The test identifies early stress before structural or functional loss occurs.”
Handheld ERG also scores high on simplicity. “It’s simple to use, provides
highly valuable information, and it’s a relatively low-impact test in terms of time and patient interaction,” Dr. Thimons explained.
Unlike some diagnostic tests that require dilation, ERG can be performed under natural conditions. With proper training, technicians and residents can administer the test in about 10 minutes, making it easy to integrate into routine practice.
Dr. Thimons often combines ERG with optical coherence tomography angiography (OCTA). “Those two together are really essential tools in diabetic management, and I find having both extremely valuable,” he said.
While OCTA shows the vascular patterns of the macula and posterior pole, ERG measures functional physiology. Together, they deliver a more complete picture of the patient’s condition.

and understand whether one predicts the behavior of the other in an accelerated fashion,” Dr. Thimons predicted. “That would make an amazingly powerful combination for the clinician and the patient.”
ERG has come a long way from its days as a niche test performed only in sophisticated labs. Thanks to handheld systems, it is now practical, efficient and indispensable in primary eye care. As technology continues to advance, ERG’s role in optometry is only set to grow, offering clinicians smarter ways to detect disease earlier, guide interventions and ultimately safeguard patients’ vision.
Looking ahead, Dr. Thimons sees room to refine ERG technology further. While devices are likely maxed out on portability, improvements in electrode contact could enhance reliability. “My hope would be that we can develop an even better system,” he said. “I would love to see it be 100% relative to the contact that’s placed on the cheek in order to read the stimulus.”
He also envisions studies linking OCTA with portable ERG. Much like how visual fields and OCT are interpreted together in glaucoma, combining OCTA with ERG could yield more powerful insights in diabetes care.
“Currently, we interpret them separately, but seeing these two data sets side by side could improve diagnostic potential for clinicians. While I don’t think the devices will be physically integrated, there is significant potential for a larger, longer study to analyze them together, grade levels of retinopathy
Dr. J. James Thimons is a powerhouse in modern optometry. He is the chief medical officer and board member of Medical Optometry America, as well as a celebrated clinician, educator and all-around champion of eye health innovation.
With more than 200 publications to his name on glaucoma, dry eye and corneal disease, Dr. Thimons has helped shape how the world sees (literally). His groundbreaking work has earned him countless professional honors, and he’s a sought-after speaker and mentor known for making complex science not just understandable, but exciting.
After earning his OD from The Ohio State University College of Optometry and completing his residency at the Chillicothe VA Medical Center, Dr. Thimons launched a remarkable career that blended research, leadership and clinical excellence. From founding The Glaucoma Institute at SUNY to co-founding Ophthalmic Consultants of Connecticut, he’s consistently stayed at the forefront of patient care and innovation.
Today, Dr. Thimons continues to inspire as a thought leader and educator, pushing the boundaries of what’s possible in clinical optometry.
jimthimons@gmail.com

Once upon a time, virtual reality (VR) and augmented reality (AR) were considered toys for gamers and sci-fi dreamers. Now, they’re stepping into the clinic with serious intent: reshaping optometric diagnostics and pushing eye care professionals to rethink how vision is tested, monitored and explained.
These immersive tools are delivering levels of precision, portability and
By Diana Truong
and patient education in ways we couldn't imagine before."
The arrival of VR and AR represents more than just gadgetry. It signals a paradigm shift.
patient engagement that traditional methods can’t always match.
"What excites me most is how VR and AR are moving eye care beyond the clinic, making assessments more immersive, personalized and even portable," explained Mayuri Deka, assistant professor at the School of Health Sciences, Kaziranga University (India). "They're opening up new possibilities for vision therapy, low-vision rehabilitation
"What excites me most is how VR and AR are moving eye care beyond the clinic, making assessments more immersive, personalized and even portable."
- Mayuri Deka
Traditional diagnostics, though effective, can feel rigid and confined to the clinical chair. In contrast, VR and AR bring the real world into testing, simulate dynamic environments and create mobilityfriendly solutions that bridge the gap between examination and daily life.

Among the most exciting applications is visual field (VF) testing for glaucoma patients. Standard automated perimetry (SAP), with stalwarts like the Humphrey Field Analyzer (HFA; ZEISS, Jena, Germany), has been the cornerstone of glaucoma care for decades. But these devices require significant investment, space and trained personnel.1
Enter VR-based visual field testing (VRVFT). Studies show that VRVFT offers reliability and efficacy comparable to SAP for detecting glaucomatous visual field loss, with the added perks of accessibility, patient comfort and cost savings.1
Dr. Babel and colleagues noted that "VRVFT's portability enables testing outside traditional clinical settings, enhancing access for patients with mobility issues, infection concerns or in remote areas. This can lead to earlier detection of disease progression and improved patient compliance."1
Still, VRVFT has its caveats. Many systems struggle with limited luminance ranges and lack advanced eye-tracking, which can affect fixation monitoring and test reliability.1
Strabismus evaluation is another frontier where VR shows potential. Mori and colleagues tested a VRbased simulated alternate cover test, leveraging eye-tracking to measure deviations against the gold standard sensorimotor exam.2
They reported moderate but significant correlations between VR and conventional measures, particularly for esotropia and constant deviations.2 Sensitivity, however, was underwhelming at 27.6%, though specificity impressed at 87.5%.2
"VR has the potential to expand our ability to detect, measure and monitor strabismus," the researchers concluded, though they cautioned
that "further improvements are needed before clinical deployment."2
AR is also making its mark, particularly in education and patient engagement. Velazquez and colleagues created KERATOCONUS AR, a mobile app that uses markerbased AR to generate 3D corneal models showing disease stages and treatment outcomes.3
Patients reported greater understanding of their condition, while clinicians and students praised its teaching utility. The tool proved especially useful during COVID-19 restrictions, when remote and interactive resources were at a premium.3
Notably, strong correlations were observed between the app’s visualization features and patients’ desire for similar tools, suggesting that effective visualization may be as valuable as explanation itself.3
Why clinicians (and patients) are paying attention
For professionals, VR and AR offer richer diagnostic data. And for patients, the experience feels less medical and more engaging.
Enhanced diagnostic capabilities. "VR and AR allow us to simulate real-world environments for testing and training," Ms. Deka noted. This capability enables clinicians to assess visual function in contexts that more closely resemble patients' everyday experiences, potentially uncovering functional deficits that might be missed in traditional clinical testing.
The technologies also facilitate more comprehensive and objective data collection. VR-based systems can precisely track eye movements, measure response times and quantify visual performance in ways that manual methods cannot.4
Improved patient experience and compliance. Patient comfort and engagement are significantly
enhanced with VR and AR technologies. "It makes therapy more immersive, engaging and personalized," Ms. Deka explained. "Patients feel empowered because the tools simulate real-world tasks, making the care experience less clinical and more relevant to daily living."
This improved experience can translate to better treatment adherence and outcomes. Ms. Deka recalled one amblyopia case where compliance improved dramatically with VR-based therapy. The child embraced the process because, to them, it felt like play rather than treatment.
"Patients feel empowered because the tools simulate realworld tasks, making the care experience less clinical and more relevant to daily living."
- Mayuri Deka
Resource optimization. In clinical settings with high patient volumes and limited resources, VR and AR technologies can optimize workflow and resource allocation. Cloud-based data storage in newer VRVFT systems facilitates seamless record-keeping and remote monitoring, enhancing efficiency and enabling telemedicine applications.1
Clinics can benefit from reduced space requirements and the ability to test multiple patients simultaneously, advantages that are particularly valuable in high-volume settings with limited resources.1
But the revolution is not without speed bumps. Current VR systems face limits which can affect test consistency…and that’s just the tip of the iceberg.
Technical limitations. Today’s VR systems have technical constraints
that may affect diagnostic accuracy. These include restricted luminance ranges, limited eye-tracking capabilities in some devices and challenges in ensuring consistent calibration across different environments.1
Velazquez and colleagues noted that their AR application for keratoconus was initially developed only for Android systems, limiting accessibility for iOS users.3 This highlights the importance of cross-platform compatibility in clinical applications.
Practical considerations. Patient familiarity with VR and AR technology varies significantly, potentially affecting test performance and requiring additional training time.1 Limited access to appropriate hardware can be a barrier, particularly for home-based testing in underserved populations.
"The main challenges are cost, clinician training and patient awareness," Ms. Deka acknowledged. "While the technology is promising, it needs to be affordable, easy to use and backed by strong clinical evidence to see widespread adoption."
Standardization needs. The lack of standardized protocols across different VR and AR systems complicates clinical adoption and comparison of results.1 Establishing standardized testing procedures and evaluation metrics will be essential for broader implementation and integration with existing clinical workflows.
Experts anticipate that VR and AR will soon move from novelty to necessity. "We'll see VR and AR becoming standard for visual field testing, vision therapy and low-vision rehab, with more portable, affordable devices that bring eye care directly into patients' homes," Ms. Deka predicted. "Beyond diagnostics and therapy, these tools will also support remote monitoring, enabling clinicians to track progress in real time."
"We'll see VR and AR becoming standard for visual field testing, vision therapy and lowvision rehab, with more portable, affordable devices that bring eye care directly into patients' homes."
- Mayuri Deka
"Ultimately, VR and AR will help shift optometry toward a more patientcentered, accessible and techenabled model of care."
The bottom line
VR and AR are poised to revolutionize optometric diagnostics, offering enhanced capabilities, improved patient experiences and optimized resource utilization. Despite technical and practical hurdles, the promise of sharper insights, better patient experiences and smarter workflows is too significant to ignore.
For eye care professionals willing to adapt, these tools offer not just a glimpse of the future, but a seat at its table. After all, why settle for two dimensions when you can practice in three?

The integration of artificial intelligence with VR and AR technologies holds particular promise. AI algorithms could analyze data collected through these platforms to identify patterns, predict disease progression and personalize treatment approaches.4
"I also expect integration with AI, which will personalize treatment plans and adapt exercises to each patient's needs," Ms. Deka added.
References
1. Babel AT, Soumakieh MM, Chen AY, Wong C, da Costa DR, Almeida DRP. Virtual reality visual field testing in glaucoma: Benefits and drawbacks. Clin Ophthalmol. 2025;19:933-937.
2. Mori DM, Kuchhangi A, Tame J, et al. Evaluation of a novel virtual reality simulated alternative cover test to assess strabismus: A prospective, masked study. Am J Ophthalmol. 2025;269:266272.
3. Velazquez JS, Panos E, Gonzalez-Cabrero J, del Barrio JA, Cavas F. New augmented reality application for improving clinical education and patient-doctor interaction in remotely-assisted ophthalmology consultations. Virtual Reality. 2025;29:96.
4. Deka M. Virtual and augmented reality in vision training: Transforming eye care. Vision Science Academy. April 1, 2025. Available at: https://visionscienceacademy.org/virtual-and-augmentedreality-in-vision-training-transforming-eye-care/. Accessed on September 10, 2025.
Mayuri Deka , M. Optom., is dedicated to advancing optometry education and eye care in Northeast India. With over a decade of teaching experience, she has shaped countless young professionals while championing community outreach in some of the region’s most remote areas.
For years, she served as assistant professor and academic in-charge at Ridley College of Optometry in Jorhat, Assam, where she helped build strong academic foundations for aspiring optometrists. Today, she continues that mission as assistant professor at the School of Health Sciences, Kaziranga University, inspiring students with both knowledge and passion for patient care.
Beyond the classroom, Mayuri is known for her tireless community work. She has organized numerous free eye screening and awareness camps across Assam and neighboring states, bringing critical services and education on blinding diseases to underserved populations.
mmona_deka@yahoo.in
Forget waiting weeks for results. Alcon’s newly launched TRYPTYR promises a first-of-its-kind, fastacting neuromodulator approach to dry eye, aiming to boost natural tear production from day one.
An intriguing novel mechanism of action is coming to the American dry eye landscape.
Alcon (Texas, United States) announced the U.S. commercial launch of TRYPTYR (acoltremon ophthalmic solution 0.003%). The news release comes just a few months after the drug’s FDA approval in May for the treatment of dry eye disease (DED).
The launch expands available treatment options for the estimated 38 million U.S. adults affected by dry eye disease.
“TRYPTYR is highly anticipated in the DED treatment space as the first neuromodulator eye drop to rapidly increase natural tear production,” said Lisa Praeger, vice president and general manager of U.S. Ocular Health Pharmaceuticals at Alcon.
“We’re committed to making this option available to eye care professionals and patients seeking new approaches to DED management.”
How does TRYPTYR work?
TRYPTYR’s new approach has intriguing potential.
As a first-in-class transient receptor potential melastatin 8 (TRPM8) receptor agonist, TRYPTYR stimulates corneal sensory nerves to enhance basal tear production. Alcon claims that this addresses potential underlying tear deficiencies, rather than solely managing symptoms.
The targeted TRPM8 receptors are cold-sensing thermoreceptors on the ocular surface which activate trigeminal nerve signaling to boost natural tear production. This neuromodulatory approach contrasts with existing treatments that aim to reduce ocular inflammation.
The evidence behind the approval
FDA approval was supported by two Phase III trials, COMET-2 and COMET-3, which enrolled more than 930 patients with DED.
Participants were randomized 1:1 to receive TRYPTYR or vehicle control, one drop per eye two times daily for 90 days. The primary endpoint, a ≥10 mm increase in unanesthetized Schirmer’s score by Day 14, was achieved by 42.6% of TRYPTYR patients in COMET-2 (vs. 8.2% for vehicle) and 53.2% in COMET-3 (vs. 14.4%), with p < 0.0001 in both studies.
While current therapies often require weeks to achieve clinical benefit, TRYPTYR demonstrated increases in tear production as early as Day 1 in the COMET-2 and COMET-3 clinical trials.
These tear production improvements were sustained through Day 90, with no serious ocular adverse events reported. The most common side effect was mild, transient instillation site pain, affecting approximately 50% of patients.
TRYPTYR is available in preservative-free, single-dose vials, with a recommended dosing of one drop per eye, two times daily. Alcon is offering initial patient support through a First Fill Free trial and copay assistance via BlinkRx, with home delivery for eligible patients.
Thought leaders in the space have since spoken on what this could mean for clinical practice in approved areas.
“TRYPTYR represents an important milestone in the treatment of dry eye disease,” said Dr. Preeya Gupta (United States). “Alcon is also supporting clinicians with educational resources to help integrate new treatments like TRYPTYR into practice.”
With only 13% of surveyed DED patients reporting adequate symptom control and the market projected to reach $9.85 billion by 2028, this rapid-onset, first-in-class therapy could help fill a major treatment gap.
For now, TRYPTYR offers a refreshing option. One that promises to leave both patients and prescribers with a little more sparkle in their eyes.
Editor’s Note:
This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore. A version of this article was first published on cookiemagazine.org.
By Elif Uslu
Tomorrow’s optometry is faster, smarter and more connected than ever. Here’s how AI, VR and a dash of science fiction are redefining reality.

Optometry is standing at the threshold of a technological renaissance as tools that once seemed confined to research labs enter everyday practice.
Over the next decade, the OD’s toolkit will feature instruments that sound straight out of a sci-fi script: artificial intelligence (AI) overlays on
optical coherence tomography (OCT) scans, virtual reality (VR) goggles replacing the dreaded perimetry bowl, remote monitoring platforms that live in patients’ pocket and smart contact lenses that double as microscopic labs.
For patients, the promise is clear: fewer surprises, faster answers and
exams that feel less like torture and more like teamwork. For ODs, it’s a call to evolve. Tomorrow’s optometrist won’t just diagnose. They’ll navigate data, integrate tech and guide patients through a future where machines can see what humans can’t.
So what’s coming down the pipeline? And how can ODs prepare today for a future that’s already knocking on the door? Let’s take a look at the tools that will shape the future of eye care.
For decades, OCT has been the gold standard for retinal imaging. But interpretation takes time, training and judgment. Even the most experienced clinicians can miss subtle signs of progression, especially in asymptomatic patients. AI is set to change that equation.
“AI-enhanced OCT will shift optometry from reactive care to proactive, data-driven disease interception,” says Dr. Carmen Abesamis-Dichoso (Philippines), an optometrist and member of the COOKIE advisory board.
Embedded AI, she explains, will not just detect what’s visible but highlight what’s likely to happen next. “Embedded AI will allow detection of sight-threatening findings like glaucoma, age-related macular degeneration (AMD), diabetic macular edema (DME), macular holes and central serous retinopathy (CSR) in real time through risk scores and heatmaps, avoiding misdiagnosis and reducing unnecessary referrals,” she notes.
That ability to peer into the future could be transformative. Rather than waiting for vision loss, ODs could catch what Dr. Dichoso calls “microprogression” months—or even years—before patients experience functional decline.
For Dr. Yangzhi Zhu (United States), assistant professor at Terasaki Institute for Biomedical Innovation, the real promise lies in both accuracy and efficiency. “AI-enhanced OCT will shift optometry from reactive image reading to proactive, risk-based care, catching glaucoma, diabetic retinopathy (DR) and AMD earlier,” he says. “In the near term, OCT/ OCTA will ship with autotriage and ‘second-reader’ risk scores that preread volumes and auto-draft referral notes.”
And the time savings aren’t theoretical. “AI-driven overlays can shave meaningful time off image review. Eye-tracking data suggests 40% faster time-to-first-fixation and 20% shorter total review time. At scale, that means more patients seen per session,” Dr. Zhu explains.1
Imagine interpreting twice as many scans without sacrificing accuracy. It’s a bold rethinking of workflow: OCT machines that capture, interpret, highlight risk, draft notes and even reconcile findings with visual field data will become decision-making partners.
And the technology won’t stop at interpretation. AI overlays will reconcile OCT results with visual field data, offering “true progression versus noise” and creating more objective glaucoma management. Algorithms will integrate images with demographics, genetics, IOP and lifestyle inputs to produce personalized forecasts. Follow-up intervals may soon be tailored to individuals rather than dictated by generic schedules.
And AI might not stay confined to specialty practices. “Primary care and even retail sites can run autonomous or semi-autonomous OCT screening referring to DR or DME specialists with proper recommendations instantly, reducing the backlogs in specialty clinics,” Dr. Dichoso envisions, elevating care and accessibility from high-volume clinics to local primary care settings.
Ask patients their least favorite part of the eye exam, and many will point to visual field testing. Long, tedious and uncomfortable, it has long been an ordeal. Enter VR and augmented reality (AR), which promise to make perimetry portable, immersive and— dare we say—tolerable.
“They’ll shift care from episodic, clinic-centered visits to continuous, risk-stratified management,” says Dr. Dichoso. Frequent VR/AR-based visual fields combined with IOP sensors could detect progression

weeks or months earlier than annual visits, freeing stable patients from unnecessary appointments.
Dr. Maria Sampalis, an optometrist and member of the COOKIE advisory board, already utilizes VR in her practice. “I use Virtual Field [New York, United States], it has been a great addition to the practice,“2 she enthuses. “I see more products switching to affordable small devices all in one. With small offices these fields will come up more and more.”
Dr. Zhu notes the numbers back it up. “VR/AR perimetry is getting close to ‘clinic-ready’ for many use cases: across multiple devices, global indices (MD/PSD) show good agreement with Humphrey (ICC ~0.8–0.95), tests often run about one to two minutes faster and fixation losses/false-positives can be lower.”3
Still, the technology isn’t perfect. Pointwise sensitivity agreement is weaker and progression analysis less reliable. But the trajectory is there. As Dr. Zhu predicts, “in 10 years, expect head-worn VF to be routine for screening and remote follow-up… with gold-standard HFA [Humphrey Field Analyzer] retained for baseline and progression until long-term data mature.”
For patients, the shift may feel revolutionary. “Portable, quieter, head-supported and less claustrophobic,” says Dr. Dichoso, meaning fewer sighs and less dread.
Could VR/AR eventually replace the gold standard entirely? Dr. Sampalis is optimistic. “I think as they become better with more data and patients tested, it can change the gold standard. AI will be incorporated to analyze VF,” she predicts.
Dr. Zhu is more cautious. “Not yet. Evidence shows head-worn VR/AR fields often agree with Humphrey on global indices and can be faster and better-tolerated, but progression analysis isn’t fully there,” he notes.
For now, though, the Humphrey bowl stays. But its days may be numbered.
The next big shift in eye care is unfolding outside the clinic. Remote monitoring, powered by AI and linked with telehealth, is turning the annual eye exam into continuous care.
Dr. Dichoso sees enormous potential for remote monitoring across high-prevalence eye diseases with measurable biomarkers. “For glaucoma, home-based VR/AR visual fields, IOP monitoring with smart tonometry or contact lens sensors, and even home OCT could make a big difference,” she says. “For diabetic retinopathy and DME, remote OCT to track macular thickness, or smartphone retinal cameras to spot hemorrhages and exudates, could transform care.”
She also envisions smartphone retinal cameras spotting hemorrhages in DR and DME, and home monitoring extending into dry AMD, high myopia, keratoconus and even dry eye.
For Dr. Zhu, the winners are clear: neovascular or at-risk AMD, glaucoma and diabetic disease. FDA-authorized OCT with onboard AI can already detect subclinical fluid between visits. For glaucoma, devices like iCare HOME2 (Vantaa, Finland) expose diurnal and nocturnal IOP spikes that may alter management dramatically.3
Dr. Sampalis sees it as both futuristic and practical. “It can be a device, images or even contacts that can monitor it or new meta glasses.”
Operationally, practices will need to adjust. Dr. Zhu envisions dashboards where technicians onboard devices, AI triages data and clinicians step in only when thresholds are crossed. “The net effect is earlier intervention, fewer urgent walk-ins and personalized recall intervals, while expanding access for patients who struggle with frequent visits,” he explains.
The implications are transformative. Instead of rigid appointment schedules, care becomes fluid and
personalized. And instead of waiting for vision to slip, ODs will intervene before patients even notice a change.
A decade from now, inserting a contact lens could feel less like vision correction and more like logging into a biometric dashboard.
“I am most excited with the following smart contact lens capabilities,” says Dr. Dichoso. “Continuous IOP monitoring, tear-film biomarkers, noninvasive glucose and lactate, drug-response telemetry, detection of micro-edema, alerts for infection or UV exposure and even tracking healing in abrasions and post-op.”
Dr. Zhu is particularly bullish on IOP profiling and tear biochemistry. He predicts IOP-sensing lenses in glaucoma clinics within two to four years and tear biomarker lenses debuting within a decade.
And it’s already in the works. Startups like XPANCEO (Dubai, UAE) are already pushing prototypes. Their AI-powered smart contact lens offers IOP tracking with 50% greater precision than today’s devices, plus tear-fluid biosensors capable of detecting glucose, cortisol, hormones and vitamins4 essentially a wearable diagnostic lab in lens form.
Of course, promise always comes with challenges. Dr. Dichoso points to practical concerns around safety and comfort. “If one will wear the lenses all day, oxygen permeability, edge comfort and minimal corneal swelling should be factored in,” she says.
Dr. Dichoso also flags compliance issues in elderly patients and the risk of signal interference from deposits or cosmetics.
Dr. Zhu, meanwhile, emphasizes the need for proof beyond novelty. “Clinical proof that changes outcomes, not just signals,” he warns. For IOP lenses, 24-hour profiles change therapy and preserve vision; for tear biomarkers, prove tight linkage to disease activity.”
He also highlights scalability, regulatory approval and reimbursement as barriers that must be overcome before smart lenses can move from hype to mainstream.
Of course, futuristic tools don’t come cheap or easy. Reimbursement, upfront costs, training, workflow redesign and patient education remain stubborn barriers.
“Reimbursement seems to be the biggest challenge,” says Dr. Dichoso, warning that burdensome requirements can make return on investment uncertain and leave many practitioners hesitant to jump in.
The financial strain doesn’t end there—upfront and ongoing costs include not only hardware but also subscriptions, integration fees, cybersecurity and the hidden time staff spend triaging alerts. “Cost, reimbursement and new adaptation will take time,” adds Dr. Sampalis.
And yet, money isn’t the only piece of the puzzle. Training and workflow redesign also loom large. Clear protocols, new staff roles and patient education—especially for elderly or novice users—are all part of the equation.
As Dr. Dichoso points out, even small details matter: oxygen permeability, lens comfort or how rubbing your eyes might interfere with smart lens sensors.
Meanwhile, Dr. Zhu frames the challenge in blunt terms, saying, “Reimbursement is the gate, cost is the drag, training is solvable.” In other words, the biggest hurdles are systemic, not clinical.
Still, none of the experts see these obstacles as deal-breakers. The consensus is to start small: pilot one high-yield use case like high-risk AMD or glaucoma, negotiate payer pilots early and embed templated documentation in the electronic health record (EHR) systems to make the workflow seamless.
Above all, invest in learning. As Dr. Sampalis reminds us, “Optometry is a lifelong education journey.”
So what does the “future-ready OD” look like a decade from now? Picture clinics buzzing with AI, VR and telehealth woven seamlessly into every patient interaction.
Dr. Sampalis sees a profession that is medically focused and tech-powered. Dr. Dichoso envisions expanded access and impact, reducing vision loss and elevating optometry’s role in primary care.
And then there’s Dr. Zhu, who paints the most vivid vision of all. “A decade

Dr. Carmen AbesamisDichoso is a passionate optometrist and educator based in the Philippines, whose influence extends far beyond the clinic. A fellow of the American Academy of Optometry, the British Contact Lens Association, the International Association of Contact Lens Educators and the Philippine College of Optometrists, she brings global expertise to every endeavor.
from now, a future-ready OD runs a hybrid clinic-virtual service where most ‘thinking’ happens before you enter the room,” he predicts. “Intake auto-pulls home data into a risk dashboard; AI pre-reads in-clinic OCT and proposes a plan. VR/AR perimetry replaces the dark room for most follow-ups, while remote diagnostics trigger same-day telechecks when thresholds are crossed.”
It’s a future where machines don’t replace optometrists—they’ll empower them. Where patients feel safer, seen and supported. Where practices thrive not by owning the fanciest gadget, but by mastering workflows that make technology invisible and care unmistakably human.

Dr. Yangzhi Zhu is an assistant professor and core faculty member at the Terasaki Institute for Biomedical Innovation (TIBI), where he’s shaping the future of smart materials and wearable bioelectronics.
Named Outstanding Optometrist by the Optometric Association of the Philippines in 2017, Dr. Dichoso has served in key leadership roles: on the World Council of Optometry’s Legislation, Regulations and Standards Committee, the Asia Pacific Council of Optometry, and the Technical Committee in Optometry under the Commission of Higher Education.
A tireless advocate for vision and education, she currently chairs the Education Committee of the Professional ODs Society of the Philippines and serves as Clinical Advisor for the Special Olympics Opening Eyes program in the Asia Pacific region. She is also a member of the Technical Working Group for Optometry at the University of the Philippines. carmen.dichoso@gmail.com

The next decade of diagnostics isn’t just about smarter tools. It’s about true transformation. The only question left is: will you be futureready?
1. Cioffi GM, Pinilla-Echeverri N, Sheth T, Sibbald MG. Does artificial intelligence enhance physician interpretation of optical coherence tomography: Insights from eye tracking. Front Cardiovasc Med. 2023;10:1283338.
2. An exceptional eye exam experience for all. Virtual Field. 2025. Available at: https:// www.virtualfield.io/. Accessed on September 24, 2025.
3. Takagi Y, Asano R, Yamashita K, et al. Comparison of IMO vifa24plus(1-2) and Humphrey Field Analyzer 24-2. Clin Ophthalmol. 2025;19:301-307.
4. iCare HOME2. iCare. 2025. Available at: https://www.icare-world.com/product/ home2/. Accessed on September 24, 2025.

Before joining TIBI, he honed his expertise as a postdoctoral researcher in Nanoengineering at UC San Diego, following a PhD in Chemical Engineering from UC Riverside.
Dr. Zhu’s groundbreaking work—spanning lab-on-a-contactlens technology to electronic skin—has appeared in some of science’s top journals, including Nature Biomedical Engineering, Nature Electronics, Nature Communications, Science Advances, Science Translational Medicine, and Advanced Materials.
A rising star in biomedical innovation, Dr. Zhu serves on the young editorial boards of Nano Research (Springer Nature), Exploration (Wiley), BMEMat (Wiley), and View (Wiley). His innovative research has also earned him the prestigious 2024 NARSAD Young Investigator Award.
yzhu@terasaki.org
Dr. Maria Sampalis is a powerhouse in optometry and the visionary founder of Corporate Optometry, a thriving Facebook community with over 33,000 members. Her social network now connects more than 70,000 eye care professionals worldwide—making her one of the most influential voices in the field.
A proud graduate of the New England College of Optometry, Dr. Sampalis brings passion, leadership and a serious dose of entrepreneurial energy to everything she does. Her work has earned her a string of accolades, including Young OD of the Year (Rhode Island, 2016), Vision Monday’s Influential Woman in Optometry (2019), World Council of Optometry Eye Care Hero (2020) and the Women in Optometry Theia Award (2024).
When she’s not mentoring the next generation of optometrists or shaping the conversation online, Dr. Sampalis is busy caring for patients in her Rhode Island practice.
msampalis@hotmail.com

By Chow Ee-Tan
From the exam room to the runway, Dr. Elise Brisco has redefined what it means to see clearly, blending optometry, holistic health, tech innovation and even pageantry into a career that proves midlife is anything but a slowdown.
or Dr. Elise Brisco (USA), vision care has always meant more than a crisp Snellen chart. “Vision affects almost every aspect of our lives: how you think, how you feel, how you move and how you perceive the world,” she explained. That belief shaped her pioneering career in optometry.
At her Hollywood Vision Center, and through co-founding the Rehabilitative Vision Clinic at Cedars-Sinai, Dr. Brisco built a truly multidisciplinary practice that was ahead of its time. From pediatric optometry and neuro-rehabilitation to a dry eye spa, sports vision, integrative care and even medical aesthetics, every department reflected her core philosophy: vision isn’t simply about 20/20 acuity but about helping people live fuller, healthier lives.
Blending medicine with mindfulness
Dr. Brisco’s training as a certified clinical homeopath gave her the tools to look beyond the eyes themselves. “Holistic health and homeopathy are a natural extension of vision care,” she said. “The eyes are sensitive to many health problems, so it is very beneficial for me to advise patients on whole-body health and lifestyle.”
She often saw how stress left its imprint on her patients in Los
Angeles, particularly those in the entertainment industry. “Stress compromises the immune system, which in turn makes you more likely to get an eye infection, inflammation or dry eyes,” Dr. Brisco explained. “Inevitably, when they were overwhelmed, they would come in with a chalazion or meibomian gland dysfunction.” She has even written about stress-induced dry eye, highlighting how intimately ocular health is tied to overall wellbeing.
For Dr. Brisco, counseling patients on nutrition, quality sleep and mindfulness was just as vital as prescribing lenses. “This helps keep not only their eyes healthy, but also their overall wellness.”
Dr. Brisco’s holistic outlook is anchored in her upbringing. She is the daughter of Vietnamese immigrants who arrived in the United States looking for greener pastures. “They had literally nothing when they came here,” she shared. “When I was born, they had to save a month’s wages just to buy a fan to keep me cool during the summer.”
Watching her parents work tirelessly instilled a similar grit. After graduating from optometry school, she took out four loans to buy her first practice. “I had to work seven days a week when I first bought my practice,” she
recalled. “Not only did I need to pay off my student debt, but also the loans I took out. I invested most of the profits into the practice, buying the latest technology and hiring the best-trained staff.”
That relentless dedication became the bedrock of her later success as a doctor, entrepreneur and public voice.
Since day one, Dr. Brisco’s career has been fueled by innovation. She is founder and CEO of NearSight, a wellness technology startup addressing vision problems linked to heavy screen use.
“All the time we spend on digital devices has taken a toll on our eyes,” she explained. NearSight’s first product—a smartphone case with a built-in reading lens—tackles presbyopia in the digital age. “It’s so much more convenient than having to look for your reading glasses when you need to see up close.”
As chief medical advisor of Natural Ophthalmics (Colorado, USA) and a key opinion leader in integrative health, she continues to influence the broader profession. Yet recognition has never been the goal. It has always been about helping people live better

lives through clearer vision and healthier habits.
In 2021, Dr. Brisco’s career took a surprise turn. At 59, she entered the pageant world and was crowned Ms. Woman California United States, becoming the oldest contestant to win a major title. “I started getting fan mail from around the world,” she recalled. “People told me they were eating healthy, working out, dancing and even dating again because of me.”
On Instagram she wrote, “I could motivate more people to live a healthy lifestyle in front of the camera and walking on the runway than I could in a year in the exam room.” What started as a crown became a calling. She sold her practice and pivoted to modeling and content creation full-time.
Pro-aging in a youthobsessed industry
Breaking into fashion in her late fifties was no small feat. “Fashion, entertainment and social media are youth-obsessed industries,” said Dr. Brisco. “Designers whose customers are middle-aged often use very young models to represent them. It’s like having a five-year-old drive a car in a commercial.”
Still, she persisted, carving her space as a “midlife influencer” and champion of “pro-aging.” For her, aging is not decline but liberation. “Life gets more rich and colorful as you age because of all the wisdom you’ve gained,” she enthused. “Being older also means freedom: less selfconsciousness, more self-confidence, more freedom of time and more financial freedom. I actually feel I am living my best life now.”
Her philosophy is simple: health creates beauty. “No amount of makeup, jewelry, plastic surgery or beautiful clothes can hide an unhealthy person,” she insisted. True self-care, in her view, is self-love, and beauty deepens with time.
It would be an understatement to call Dr. Brisco a pioneer. Long before her modeling career, she was already breaking barriers. One of the few women in optometry when she graduated, she often encountered skepticism.
“When I lectured at conferences, doctors would assume I was someone’s daughter,” she recalled. “When I was the team optometrist for the Anaheim Ducks, sometimes guards wouldn’t let me into the locker room because they thought I was a cheerleader instead of a doctor.”
She faced similar biases as the only female assistant coach for her son’s Little League team, where referees bluntly told her “no moms are allowed on the field.” Still, she persevered. Over two decades, she mentored interns from the University of Southern California and the University of California, Los Angeles—100% of whom went on to become ODs or MDs. Her legacy is not only in her clinics, but also in the next generation she inspired.
advice to women in midlife resonates well beyond fashion circles. “Be true to yourself. Use all the knowledge and wisdom you’ve gained to create the life you want. Take care of yourself so that you can take care of the people you love,” she recommended.
She will continue to grow NearSight while speaking about lifestyle and wellness. “My goal is to continue adding to the narrative that aging is a joy and a privilege, but that you have to take care of yourself by living a healthy lifestyle to enjoy your golden years,” she concluded.
And if her career is any indication, those golden years will be bold, bright and lived entirely in focus.

Dr. Brisco lives by the principle that anything worth having is worth working for. She prioritizes exercise, mindfulness and nutrition, but also safeguards family time. “I make sure I don’t let my workaholic nature interfere with time for my loved ones,” she said.
Her definition of success is refreshingly clear: “Happiness.” Accomplishments mean little without joy and balance. She embraces both challenges and opportunities with gratitude. “All of this has been a labor of love. Even though it’s been very difficult, I am grateful for both the blessings and the challenges.”
What’s next? Dr. Brisco plans to keep modeling, creating content and advocating for healthy aging. Her
Dr. Elise Brisco is an integrative optometrist, certified clinical homeopath and health tech entrepreneur who has made a career out of blending wellness, technology and media. She is the founder and CEO of NearSight, a vision wellness start-up, and clinical director at Hollywood Vision Center Optometry, now part of Total Vision, LLC. Her holistic approach focuses on vision rehab after brain injuries, sports vision, children’s and developmental vision and fresh treatments for dry eyes.
A true trailblazer, Dr. Brisco co-founded Rehabilitative Vision Clinic at Cedars-Sinai and has been team optometrist for the Anaheim Ducks, LA Galaxy and Long Beach Ice Dogs. She also serves as chief medical advisor for Natural Ophthalmics and is a soughtafter key opinion leader in both optometry and integrative health.
Outside the clinic, Dr. Brisco is no stranger to the spotlight. She’s been featured on The Doctors, ABC, CBS, Fox, NBC, MTV, Oprah, Vogue, Good Housekeeping, The New York Times and more. As a creator and influencer, she shares her expertise in beauty, fitness, nutrition, healthy aging and entrepreneurship, inspiring audiences to see—and live—better every day.
elisebrisco@hollywoodeyes.net
By Hazlin Hassan
Pilocarpine’s long reign in presbyopia is finally facing a challenger. With FDA approval in hand, aceclidine promises sharper near vision without the usual headaches, literally. But will it be a paradigm shift or a passing act?
For decades, optometrists seeking a non-surgical, nondevice solution for their presbyopic patients have had one pharmaceutical friend: pilocarpine. Known for its pupil-shrinking action, pilocarpine has been the sole FDAapproved drop for managing agerelated near vision decline.
But now, a new kid has arrived on the block: aceclidine, recently approved by the U.S. Food and Drug Administration (FDA) under the brand name Vizz (LENZ Therapeutics; California, USA). With promising data and a distinct mechanism of action, aceclidine could reshape the way eye care professionals approach presbyopia management.
Pharmacologic “readers-in-a-bottle” tackle presbyopia by increasing depth of focus through pupil constriction, sidestepping the problem of the stiffening crystalline lens.
Pilocarpine makes this happen by stimulating the iris’ sphincter muscle, but also acts on the ciliary body. That dual action can lead to baggage in the form of headaches, dim vision or a myopic shift.
“The goal of a miotic is to constrict the pupil and thus allow improvement in the depth of focus,” explained Dr. Marc Bloomenstein, director of optometric services at the Schwartz Laser Eye Center (USA). “While pilocarpine works by stimulating the sphincter muscle of the iris, it has an
affinity to stimulate the ciliary body, which induces a myopic shift and other side effects.”
Aceclidine, on the other hand, looks to be a smoother ride.
“Aceclidine, a smooth muscle agonist, has demonstrated that it has strong affiliation for the sphincter muscle with minimal effect on the ciliary muscle. Thus, inducing a sub-2 mm pupil without the negative impact of the ciliary body,” Dr. Bloomenstein noted. “The data clearly demonstrates that the efficacy of aceclidine to constrict the iris is consistent with the improvement in vision at near without sacrificing distance clarity.”
In short: aceclidine gives the near boost without the baggage.
FDA approval of Vizz was supported by the CLARITY program, a suite of Phase III trials designed to evaluate both short- and long-term outcomes.*
CLARITY-1 and CLARITY-2 enrolled 466 patients in randomized, double-masked, controlled studies.
Participants were dosed once daily for 42 days, and both primary and secondary endpoints for near vision improvements were met. Notably, benefits kicked in within 30 minutes of instillation and lasted for up to 10 hours.
CLARITY-3 involved 217 patients and extended dosing out to six months to assess long-term safety. Across more than 30,000 treatment days, no serious treatment-related adverse events were reported. Side effects were generally mild and included eye irritation, temporary dim or dark vision, headaches and redness.
“The FDA approval of Vizz now enables me to more broadly discuss a therapeutic option with my current presbyopic patients,” Dr. Bloomenstein said. “With approximately 70% of patients still maintaining functional binocular vision at near up to 10 hours after a single dosage, this is a game changer for my practice.”
Not all presbyopes are equal, and neither are their outcomes with aceclidine.
“According to the studies, this medication is ideal for adults who are struggling with age-related presbyopia or those who have sensitivity to previous pilocarpinebased treatments,” said Dr. Kristie Nguyen (USA), optometrist and member of the COOKIE advisory board.
“However, with only a two to three lines of visual improvement at near for the majority of the test subjects, I would have to say ideally 38 to 48 years of age and that’s being very generous on the age range. Anyone older would have a harder time achieving the desired near results they’re expecting with such a low margin of improvement.”
Dr. Bloomenstein added that inclusion criteria in the pivotal trials were encouragingly broad. “It is really significant that the clinical study included patients up to 75
years old, pseudophakes, as well as subjects that had undergone corneal refractive surgery,” he said.
pitfalls)
So how should ECPs think about aceclidine in daily practice?
“I anticipate optometrists embracing Vizz as an addition to their presbyopia toolkit,” Dr. Bloomenstein noted. “Vizz allows eyecare professionals to offer their patients a differentiated and transformative treatment option for presbyopia that can complement current offerings.”
Dr. Nguyen, however, struck a more cautious note: “Aceclidine would be an additional benefit to those who currently wear contact lenses—whether distance vision only or multifocal lenses—but need a little extra boost when they are out and about and don’t want to deal with their reading glasses, or youngish presbyopes in distance vision-only glasses. Definitely not a long-term option but more of a special occasion use.”
Nuts and bolts for the exam room
frustrated and struggling with the inevitable age-related loss of their near vision,” Dr. Bloomenstein said.
Dr. Nguyen was less convinced. “I would not consider this treatment option to shift my current standard of care or a game changer with the current stats,” she said. “The fact that the study was only conducted for the maximum of six months leaves me to wonder what long-term side effects can arise.”
LENZ Therapeutics is now focused on rolling out Vizz to U.S. adults with presbyopia. But experts agree more data would help.
“If a company can create a treatment with a better range of near vision

Dr. Marc Bloomenstein wears many hats and wears them well. As director of Optometric Services at Schwartz Laser Eye Center in Scottsdale (USA) and president of MRB Eye Consultants (USA), he’s at the forefront of patient care and innovation. He also chairs the Education Committee for Vision Expo, shaping how the profession learns and grows.
• Onset and duration. Aceclidine acts within 30 minutes, with effects lasting up to 10 hours, which is an attractive proposition for patients who want fast, reliable relief.
• Safety profile. Mild and transient side effects may be tolerable for patients more annoyed by reading glasses than by momentary dim vision.
Star of the show or just a cameo?
The million-dollar question is whether aceclidine will truly shift the standard of care.
“Vizz represents a disruptive paradigm shift in treatment options for millions of people who are
A born leader, Dr. Bloomenstein has served as chairman of the AOA Continuing Education Committee, sat on the board of the Ocular Surface Society of Optometry, and helped launch the Optometric Cornea, Cataract and Refractive Society. Closer to home, he’s been president of the Arizona Optometric Association, as well as legislation chair and president of the Arizona Optometric Charitable Foundation.
But Dr. Bloomenstein isn’t just about titles. He’s about impact. With more than 1,500 invited lectures delivered across the globe, 25+ clinical trials led as principal investigator and countless collaborations with top pharmaceutical, biomedical and tech companies, his fingerprints are everywhere in modern optometry.
mbloomenstein@gmail.com

improvement over a year of studying their candidates then this would be ideal,” Dr. Nguyen said. “Not only would more patients benefit but clinicians can better understand any potential long-term side effects of the treatment.”
For now, aceclidine has secured its place as the new kid on the presbyopia block. Whether it takes center stage or stays a supporting player depends on its performance in the real world.
* LENZ Therapeutics announces U.S. FDA approval of VIZZ for the treatment of presbyopia. LENZ Therapeutics. July 31, 2025. Available at: https://ir.lenz-tx.com/ news-events/press-releases/detail/39/lenztherapeutics-announces-us-fda-approval-of-vizzfor-the-treatment-of-presbyopia. Accessed on September 26, 2025.

Dr. Kristie Nguyen is a board-certified optometrist with a passion for helping people see life more clearly. She owns and runs her own practice, Dr. Kristie Nguyen PLLC, in sunny Winter Park, Florida (USA).
Her journey started in Texas, where she graduated in the top 10 of her high school class and went on to earn her Bachelor of Science at the University of Houston. While there, she rolled up her sleeves as a hospital volunteer and optometric assistant, sparking her lifelong dedication to eye care. In 2005, she completed her Doctorate of Optometry at Nova Southeastern University College of Optometry in Fort Lauderdale, followed by internships at the Chickasaw Nation Health Clinic in Oklahoma and Lake Mary Eye Care in Florida.
An active member of the American Optometric Association, Florida Optometric Association, Central Florida Optometric Society and several optometry networks, Dr. Nguyen is deeply connected to her profession. Beyond the clinic, she brings style to sight as a brand ambassador for eyewear lines like Kazoku Lunettes, KUWARE and RYAN ADDA.
kristie817@gmail.com

By Tan Sher Lynn
Optometrist Woon Pak Seong, founder of Vision Space
Optometrist in Malaysia, shared how technologies are shaping optometry practice.
Optometry, like the rest of healthcare, is riding a digital wave. What was once dismissed as a “luxury add-on” has become the backbone of modern practice. Whether it’s sharper diagnostics, smoother operations or savvier business management, technology is no longer the assistant. It’s the co-pilot. And like any good copilot, it can help avoid turbulence…if you know how to use it.
Few know this better than Malaysian optometrist Woon Pak Seong, founder of Vision Space Optometrist.
With more than two decades in private practice, he has seen the field shift from clipboards and manual charts to cloud-based dashboards and AI-ready imaging.
“Today’s patients expect fast, precise and transparent care, whether it’s in the exam room or at the dispensing counter. At the same time, practices face mounting demands in inventory, communication and compliance,” he said. “Without the right systems, running a clinic can feel like juggling fire.”
For Woon, technology is not a shiny distraction or a passing fad. “At Vision Space Optometrist, technology is not just a tool,” he explained. “It’s a strategic partner that enables us to raise the bar in both patient outcomes and operational efficiency.”
Step into Woon’s clinic and you’ll notice the quiet choreography of systems working in the background. Each piece of technology has been carefully selected not for novelty, but for impact. “We’ve selectively invested in technologies that align with our practice goals: clinical excellence, operational efficiency and exceptional patient experience,” he said
At the front end, the Frontwave point-of-sale (POS) and customer relationship management (CRM) system (Singapore) manages inventory, sales and patient records while automating recalls and reminders. What once required endless spreadsheets and phone calls is now streamlined into one system, allowing staff to spend more time with patients rather than paperwork. “This has created a leaner operation and improved patient retention,” Mr. Woon noted.
On the dispensing floor, EssilorLuxottica’s (Paris, France) Visioffice brings precision to lens measurements. Capturing parameters like pupillary distance, tilt and wrap angle, it minimizes errors and instills confidence. “The system has significantly reduced remakes and increased acceptance of premium lens solutions,” Mr. Woon said.
Diagnostics are equally powered by innovation. Topcon’s MYAH (Tokyo, Japan) platform has opened doors to myopia management and dry eye services, two growth areas in Malaysia. Meanwhile, the Topcon Maestro OCT provides high-resolution retinal imaging that seamlessly integrates with electronic health records (EHR), making early detection of glaucoma, age-related macular degeneration (AMD) and diabetic retinopathy (DR) more efficient.

The Medmont Corneal Topographer (Nunawading, Australia) has been transformative for specialty lens fitting, particularly ortho-K and keratoconus. “It has elevated our specialty services and positioned us as a referral point for complex cases,” Mr. Woon explained.
For intraocular pressure testing, the iCARE IC100 tonometer (Vantaa, Finland) offers a contactless option: fast, comfortable and ideal for children and anxious patients. Finally, the ZEISS Humphrey Field Analyzer (Oberkochen, Germany) provides robust visual field data essential for glaucoma and neuro-ophthalmic care
Each device, Woon stressed, isn’t just a “nice-to-have.” It plays a defined role in shaping better outcomes and smoother workflows.
The humans behind the hardware
Of course, even the smartest system can’t run itself. “We’ve learned that successful tech integration is as much about people as it is about the product,” Mr. Woon said.
At Vision Space, staff are part of the decision-making process from the start. When evaluating new systems, they are invited to test them, ask questions and give feedback. “If your team isn’t invested, adoption will be slow,” Mr. Woon cautioned.
Training is treated as an ongoing investment. Vendors provide structured sessions, but the clinic also appoints “champions”—staff members who become go-to resources for their peers. New technologies are introduced in phases, often starting with pilot testing in one department. “This approach has allowed us to implement change without disrupting our patient flow, which is a key concern in any busy clinic,” he noted.
Return on investment is carefully measured. For clinical tools, the team looks at diagnostic accuracy, treatment uptake and patient
satisfaction. For operational systems, they measure time saved, errors reduced and the impact on revenue. This dual lens ensures technology is evaluated not just in financial terms, but also in its contribution to care.
Looking ahead, Mr. Woon sees the horizon of optometry shaped by four major trends.
Artificial intelligence (AI) is at the forefront. “AI will become a trusted second opinion, particularly in OCT and fundus imaging,” he predicted. By providing real-time analysis, AI could boost early detection rates, reduce human error and speed up decisionmaking, particularly in busy practices where time is short.
Teleoptometry, though unevenly adopted, is another area poised to grow. For follow-ups, triage and remote consultations, it offers flexibility and accessibility. “Practices should invest in secure platforms and start training workflows now to be future-ready,” Woon advised.
Cloud-based practice management systems are evolving from simple scheduling tools into analytic powerhouses. “We’re moving toward all-in-one systems that provide live dashboards, KPI tracking and trend analysis. These insights are essential for growth, especially across multilocation practices,” he said.
applied with purpose. “Each system we’ve adopted was chosen not for novelty, but for how it aligned with our clinical values and operational goals,” he said.
His advice to colleagues is rooted in pragmatism. “Don’t chase every new gadget. Instead, identify your practice’s pain points and find technologies that solve them. Train your team well and measure success through outcomes, not features,” he recommended. “When implemented strategically, the right technologies don’t just make a good practice better. They future-proof it.”
And that, perhaps, is the true message of the tech-driven practice. The future of optometry won’t be decided by the flashiest machines on the showroom floor. It will be defined by practices that know how to integrate tools thoughtfully, empower their people and keep their focus firmly on patient care.
After all, even the best co-pilot is only useful if you’ve set the right destination.

And in optical retail, augmented reality is already knocking at the door. Virtual try-ons and lens simulations promise to elevate the shopping experience, particularly for younger, tech-savvy patients. “AR bridges the physical-digital divide,” Mr. Woon said. “It’s not just a gimmick. It’s becoming the expectation.”
For Mr. Woon, the lesson is simple: technology is powerful, but only when
Woon Pak Seong graduated as an optometrist in 1995 and founded Vision Space in 2004 with the mission of bringing world-class vision care to his customers. Driven by a commitment to continuous improvement and excellence, he finds joy in connecting with people and inspiring them to enjoy life to the fullest. A strong advocate of lifelong learning, Woon regularly delivers optical training and speaks at conferences and fairs. He is passionate about reading journals, magazines, and books to enhance his service and elevate the practice of optometry. His greatest passion lies in helping people see clearly and comfortably while preserving their eye health through early detection of potential eye diseases. enquiry@visionspace.com.my

By Hazlin Hassan
Forget hunches and half-clues. Point-of-care testing is giving dry eye diagnostics the hard evidence they’ve been missing, turning guesswork into a sharper science.
For decades, diagnosing dry eye disease (DED) has been a bit like detective work: lots of clues and not always a clear culprit.
Patients turned up with vague complaints like “my eyes feel gritty,” “I can’t stare at my screen too long,” or “my contacts burn after a while.”
For some time, clinicians leaned on questionnaires and slit-lamp exams, piecing together a diagnosis one symptom at a time.
Today, however, point-of-care (POC) testing is changing the game. By delivering objective in-office data, these tools move dry eye diagnostics beyond educated guesswork. Of course, they don’t replace patient histories or reported symptoms, but they do add the kind of quantifiable evidence modern medicine craves.
“I think both methods are helpful,” said Dr. Mark Eltis, Canadian Ambassador of the American Board
of Optometry and lecturer at the University of Waterloo, Canada. “In most medical tests you want both objective and subjective tests to understand what is physically present but also what the patient is feeling.”
The shift from “How do you feel?” to “Here’s the measurable data” could be transformative for both patients and providers.
DED can be notoriously inconsistent. Symptoms don’t always line up neatly with clinical signs. Some patients suffer significant discomfort with few visible changes, while others with advanced disease report only mild irritation.1
“Clinical signs and symptoms can vary widely in DED, so it’s important to have some objective testing and scientific data,” Dr. Eltis explained. “The POC tools allow us to have that clinical data that was limited in the past.”
Like fitting together pieces of a jigsaw puzzle, each test adds clarity. “We can never have all the pieces, but we want as many as possible to have a better understanding of the situation.”
Just as glaucoma management requires multiple diagnostic approaches, DED benefits from an arsenal of complementary tools.
Some of the most widely used POC tests include:
• Meibography. Imaging the meibomian glands for direct evidence of gland health.
• Tear osmolarity. Measuring tear film stability; compact and relatively affordable.
• MMP-9 testing. Identifying inflammatory markers; newer, but increasingly valuable.
“I think meibography is very common. Tear osmolarity is also more compact and potentially less expensive for a practice to purchase. MMP-9 is
helpful but is a newer addition to the dry eye armamentarium. Fewer doctors know about it,” said Dr. Eltis.
“I think all the above have their place,” he added. “We have a lot of tests because we don’t have one perfect test for dry eye. We need as much information as possible to guide our diagnosis and treatment.”
If these tools are so effective, why aren’t they everywhere? As with most new tools, cost and access are the main barriers.
“Any time there is something new, there is a cost involved. Either in terms of time or money,” Dr. Eltis said. “Some doctors are reluctant to invest, and some patients are hesitant to pay for advanced diagnostic services. There is also the time consideration for some busy clinics in terms of adding additional testing. While some doctors are early adopters, most will wait for a few close professional contacts to have positive results.”
The encouraging news is that most of these tools fit neatly into existing clinic workflows. “I don’t think these tests require much more training than any other type of pretesting,” Dr. Eltis noted.
“They are fairly straightforward and I haven’t had any issues. Upper lid meibography is probably the only part of these tests that can have a bit of discomfort, but when patients are properly counselled and the examiner is adequately trained, it should still be fine.”
So what’s next for POC testing? Dr. Eltis sees opportunity, but also some caveats.
“While at-home testing can have a role, I don’t think it is as critical as, say, at-home eye pressure monitors in glaucoma. Biomarkers could
be useful but, again, this would be more relevant to a disease like glaucoma in my view,” he reasoned. “Dry eye diagnostics are already impressive, I think effective longlasting treatments that address the source of the problem are a higher priority. If a diagnostic test can guide us to the most effective and efficient treatment, that would be revolutionary.”
Technology is advancing quickly. “High-tech dry eye solutions will continue to evolve from diagnostics to intense pulsed light to machines that improve the lid apposition. These options have changed the dry eye game, and I am sure we are just at the tip of the iceberg of what is possible,” said Dr. Eltis.
Artificial intelligence (AI) may also lend a hand. Machine learning algorithms and advanced imaging tools offer the promise of earlier detection, personalized treatment plans and more efficient decision-making. Still, hurdles such as data privacy, validation and workflow integration must be addressed before AI reaches its full potential in DED care.2

patient’s lived experience. It’s about adding depth and precision.
By blending subjective reports with objective data, clinicians can give patients a clearer picture and greater confidence in their care plan.
As DED cases rise worldwide, the marriage of advanced diagnostics with age-old holistic advice may be the perfect prescription.
1. Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: Clinical implications. Acta Ophthalmol. 2014;92(2):161-166.
2. Wu L, Huang Y, Lv T, Xiao C, Wang Y, Zhao S. Advances in AI-assisted quantification of dry eye indicators. Front Med (Lausanne). 2025;12:1628311.

That said, technology isn’t the whole story.
“When doctors generally think of technology, they think of something expensive or Star Trek-like and I have already mentioned those devices. However, I have also emphasized natural solutions and lifestyle changes that can have a significant impact in dry eye (and glaucoma) prevention and management,” he concluded. “Research, (sometimes) with the assistance of AI, is helping us to confirm what our ancestors knew: a healthy body and mind goes a long way. Exercise, healthy diet, sleep hygiene and mental health can help prevent or decrease the progression of dry eye disease and glaucoma.”
POC testing isn’t about replacing a doctor’s judgment or dismissing a
With over twenty years in practice and fifteen years part-time in academia, Dr. Mark Eltis has practiced in New York, California and Toronto. He is the current president of the College of Optometrists of Ontario and a director of the American Board of Optometry. Dr. Eltis has presented and published internationally and has been sought as an expert for national television and print. He is a graduate of the University of Waterloo School of Optometry and Vision Science and continues to lecture there.
Dr. Eltis has been honored as a member of the Optometric Glaucoma Society (OGS) having “demonstrated excellence in the care of patients with glaucoma through professional education and scientific investigation.” He has been a consultant for academic institutions overseas, law firms, and a subject matter expert for competency evaluations. Dr. Eltis has also been a previous examiner for US (NBEO) and the Canadian board examinations. He is the Canadian Ambassador for the American Board of Optometry and a team chair for US residency site evaluations (ACOE).
www.drmarkeltis.com

By Daniel Morgan-Williams
When sight fades, hope shouldn’t. Beyond the charts and clinical pathways, every word, gesture and bit of empathy can shape how patients live with vision loss. Learn how even the smallest acts can restore dignity, confidence and light.
One of the most damaging sentences a patient with sight loss can hear is, “There’s nothing more we can do.”
It slams the door on hope, shuts down conversation and leaves someone feeling abandoned just when they most need empathy and guidance. The truth is, there is always more that can be done: medically, socially, practically and emotionally.
From medical interventions to practical support, emotional guidance and social connection, optometrists and opticians are uniquely positioned to make a profound difference.
You might think, “I’m not a psychiatrist. My job is the eyes.” Yet every word spoken in the consulting room leaves an imprint. Delivering a diagnosis—or even hinting at one— places patients in a whirlwind of fear, grief and uncertainty about their future. Many leave feeling as if their life has been cleaved into ‘before’ and ‘after.’
Referrals to ophthalmologists can take months, leaving patients suspended in anxiety. During this time, mental health can feel like a ticking time bomb. Showing empathy and exercising emotional intelligence in that moment isn’t optional. It can make the difference between despair and resilience.
The time you take, the tone you adopt, and the reassurance you offer are far more than small gestures… they are lifelines.
Visual impairment doesn’t just affect eyesight. It ripples through every level of human need, as defined by Maslow’s hierarchy. At the base, physiological needs—like reading medication labels or cooking safely— can suddenly feel impossible. Safety is compromised when patients lose confidence crossing streets or navigating public transport.
Social connections and belonging suffer when activities feel inaccessible. Esteem falters as independence, work opportunities and identity shrink. Even selfactualization—the pursuit of passions, hobbies and dreams—can feel out of reach.
Each intervention, no matter how small, helps patients rebuild this hierarchy. A magnifier restores independence in cooking, a referral to a charity rekindles a sense of belonging, and thoughtful communication preserves dignity and self-esteem. Every action can either help a patient climb the pyramid or push them further down.

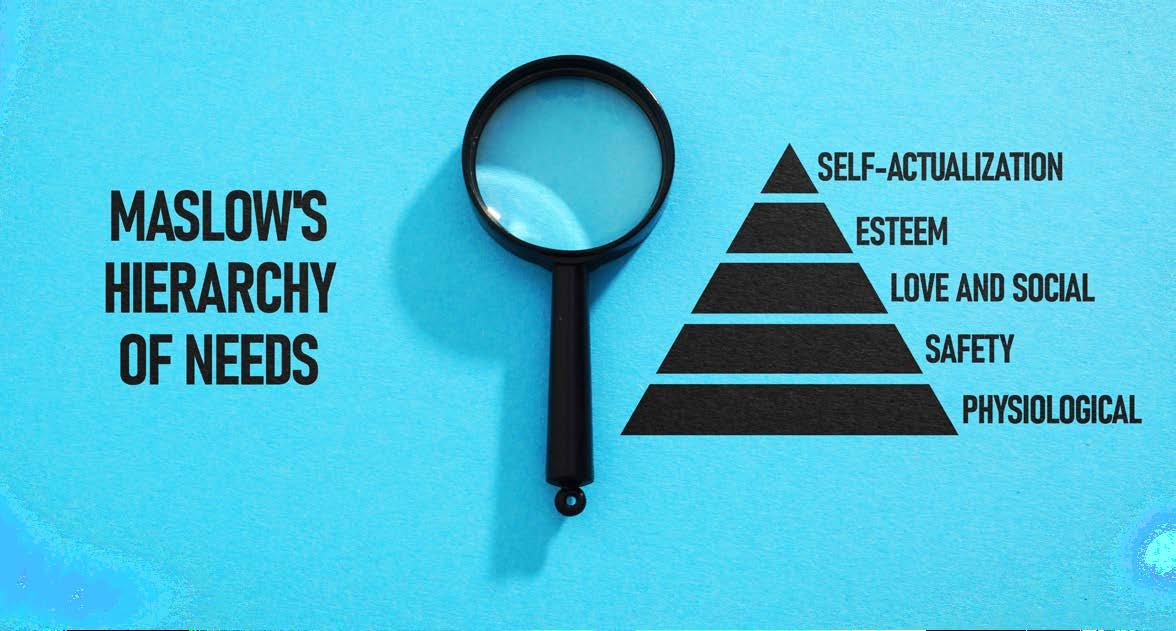
Mrs. Patel, 67, loved cooking for her family. When macular degeneration struck, she stopped, unable to read labels or recipes. Her optician didn’t just hand over a diagnosis. They demonstrated improved task lighting, suggested handheld magnifiers and connected her with a local sight-loss charity. Within weeks, Mrs. Patel was back in her kitchen, regaining control over her meals—and her sense of self. This story shows that practical tools, paired with emotional support, can rebuild confidence at every level of Maslow’s hierarchy.
John, 45, faced retinitis pigmentosa and was bluntly told nothing more could be done. He left the consultation feeling invisible, reduced to a pair of failing eyes. Over time, social withdrawal and anxiety set in. His story illustrates the damage when professionals fail to see beyond the clinical picture. A simple referral to a rehabilitation officer or support group could have reminded John he was still a full person, not just a diagnosis.
Sarah, 32, struggled with diabetic retinopathy. At first, she couldn’t read medication labels. Then commuting became unsafe, and finally, she withdrew socially. Her optometrist introduced smartphone
accessibility features, a video magnifier and peer support. Slowly, Sarah regained independence, rebuilt confidence and returned to work. Her journey demonstrates how small interventions can help patients climb back up Maslow’s pyramid, step by step, from physiological needs to self-actualization.
Polite responses like, “I’m fine, thanks,” can mask fear, sadness and uncertainty, especially after a difficult diagnosis. Emotional intelligence means reading between the lines, gently probing and reassuring patients that their feelings are valid.
Simple questions and thoughtful language can transform consultations.
Asking about a patient’s biggest concern, the impact on daily life, or offering connections to charities and support groups opens doors to honesty and reduces isolation.
services and support that can make life easier” demonstrates action and compassion simultaneously.
Optometrists and opticians shape how patients experience visual impairment. Every consultation is a chance to provide not just clinical care, but hope, dignity and direction. Empathy isn’t a soft skill. It’s a crucial part of care. And above all, never utter the words “there’s nothing more we can do.” There is always more—to support, to guide and to help patients reclaim control, in ways that extend far beyond the eyes.

Replacing phrases like “There’s nothing more we can do” with “There’s a lot we can do to support you while we wait for your hospital appointment” or “This may feel overwhelming, but there are tools,
Daniel Morgan-Williams founded Visualise Training and Consultancy in 2014 while gradually losing vision due to retinitis pigmentosa. Motivated by his own experiences of inaccessible workplaces and society, he developed programs to support people with sight loss, hearing loss, tinnitus and other hidden disabilities. What began as a focus on sight loss now encompasses all forms of sensory loss.
info@visualisetrainingandconsultancy.co.uk
