


Dear Readers,
If you're a researcher, the eye is the organ of choice. Transparent, structured and packed with elegant cell types—it lets you watch biology unfold in real-time.
I did my PhD in brain development, spending years slicing through formaldehyde-fixed mouse brains and chasing faint RNA signals. Madness. I should’ve worked on eyes; I might’ve actually seen something straight away.
Yes, retinal neurons are both excitable and exquisite. The outflow system? When it works, it's biological plumbing at its best. But lately, I keep coming back to the ocular surface and the tear film. A slick, shifting interface of mucins, salts and cytokines. When it works, it’s invisible. When it doesn’t, you start to have big problems all over the place.
It's a nifty system. It repairs itself on a molecular whisper. Growth factors—EGF, NGF, TGF-β, IGF-1—drift across the tear film and get to work. They nudge basal epithelium to divide, coax fibroblasts to behave and signal limbal stem cells to wake up. Scratch the cornea and the whole system reboots before you know it.
And when things fall apart—dry eye, limbal failure, denervation—it’s stem cells that try to restore order. Not by replacing tissue outright, but by issuing instructions. Their paracrine signals matter more than their presence. They don’t fill gaps; they re-establish protocol.
Some cells rebuild; others conduct. Limbal stem cells at the periphery. MSCs drifting in with anti-inflammatory scripts. iPSCs trying to be everything at once. They don’t need to succeed completely. They just need to remind the tissue what it was.
And underneath it all, a microbial murmur. Corynebacterium, Staph, and others clinging to lid margins, dodging lysozyme and blinking shear—like it’s normal. They’re not background; they’re part of the system. Strip them away, and immunity misfires. Leave them be, and they keep the rhythm. The smallest players, still setting the tempo.
So I have to wonder: Is the ocular surface the site of the next explosion of ophthalmic innovation? As one of this issue's themes is the ocular surface, read on to find out!

Mark Hillen, PhD Director of Communications
ELZA Institute, Zurich, Switzerland Editor-At-Large | CAKE

Conquering Compromised Corneas
When corneas are compromised, cataract surgery demands a meticulous, tailored approach for optimal visual outcomes
Illuminating Vision
Imaging Innovation Gets Personal
What works, what’s next—Insights from APAO 2025 16 13 19 22 06 10
The latest advances in Light Adjustable Lens™ Technology at the 2025 ASCRS Annual Meeting
Precision imaging paves the way for personalized care across subspecialties at APAO 2025
The Unseen War
Infectious keratitis poses a growing global threat to sight, forcing ophthalmologists to innovate beyond traditional treatments
Smart Tech in Refractive Surgery

Digital workflows are transforming refractive surgery by optimizing clinical performance
Presbyopia on the Table


28
Eye Care’s Triple Threat
Assoc. Prof. Yu-Chi Liu is redefining ophthalmology through groundbreaking research, compassionate care and global educational leadership
Amid a global donor shortage, the pioneering CALEC therapy is transforming corneal regeneration, offering new hope for sight restoration
Setting Cataract Surgery’s Stage
Before cataract surgery, optimizing the ocular surface, especially managing DED, is crucial for excellent vision outcomes
Tackling Tricky Corneas
Corneal experts offer pearls of wisdom for managing common corneal surface diseases
AI Beyond the Hype
Experts highlight AI’s practical progress in ophthalmology at ASCRS 2025


Dr. Harvey S. Uy
University of the Philippines; Peregrine Eye and Laser Institute, Manila, Philippines harveyuy@gmail.com

Dr. William B. Trattler
Center For Excellence In Eye Care Miami, Florida, USA
wtrattler@gmail.com

Prof. Burkhard Dick
University Eye Hospital Bochum Bochum, Germany
burkhard.Dick@kk-bochum.de

Dr. Francis Mah
Scripps Clinic Medical Group La Jolla, California, USA
Mah.Francis@scrippshealth.org

Dr. Cathleen McCabe
The Eye Associates Sarasota, Florida, USA
cmccabe13@hotmail.com

Prof. Dr. Sorcha Ní Dhubhghaill Brussels University Hospital (UZ Brussel) Brussels, Belgium
nidhubhs@gmail.com

Matt Young CEO & Publisher
Gloria D. Gamat Chief Editor
Mapet Poso Editor
Matt Herman Associate Editor
Maricel Salvador Graphic Designer Writers
Chow Ee-Tan
Diana Truon Elif Uslu
Hazlin Hassan
Kendra Bruning
Tan Sher Lynn
Contributors
Dr. Wei-Yi Yeh
Dr. Pi-Jung Lin
Hannah Nguyen COO
Travis Plage CFO
Ruchi Ranga Society Relations & Conference Manager
International Business Development
Brandon Winkeler
Robert Anderson
Sven Mehlitz




Screening within a few minutes, performed by your staff
Simple
Ensure the best results for your patients with the OCULUS Keratograph 5M
Ocular surface disease – such as dry eye – is a leading cause of refractive surprises and IOL exchanges. So, tear film analysis is essential prior to surgery. Use the OCULUS Keratograph 5M‘s comprehensive tool set to make the best possible decision for your patients.
Easy to understand results with traffic light colors oculus.de
Find
Safe
Make a reliable surgical decision
Meet us at SOE Booth: 17


When corneas are compromised, cataract surgery demands a meticulous, tailored approach for optimal visual outcomes
by Tan Sher Lynn
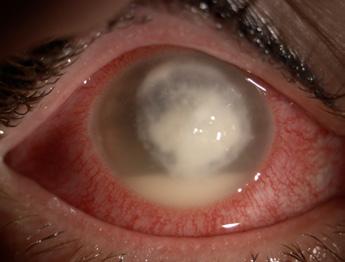
Successfully performing cataract surgery on compromised corneas requires a highly individualized approach, as highlighted by Dr. Johan A. Hutauruk. This involves meticulous preoperative evaluation, comprehensive ocular surface optimization, and careful timing when active corneal disease is present.
Cataract surgery is one of the most commonly performed and successful ophthalmic procedures. However, when the corneal surface is compromised— due to disease, scarring or structural irregularities—the surgical landscape becomes significantly more complex.
Cornea and cataract specialist Dr. Johan A. Hutauruk shared his insights
into the unique challenges of such cases and the meticulous strategies required for optimal outcomes.
A tailored pre-op and ocular surface optimization
In patients with compromised corneas, a one-size-fits-all approach is often inadequate.
“My approach to preoperative evaluation in cataract surgery patients is comprehensive and adapted based on the degree of corneal compromise,” Dr. Hutauruk explained. While standard biometry remains crucial, he adds several layers of diagnostic testing to account for the altered ocular surface. Specular microscopy is used to assess endothelial cell density, especially critical in eyes already at risk of decompensation. An optical coherence tomography (OCT) of the macula is employed to rule out underlying retinal pathology that might skew postoperative visual outcomes.
For more patients considering multifocal intraocular lenses (IOLs) or when irregular corneal surfaces are suspected, Dr. Hutauruk uses both the Pentacam (OCULUS Optikgeräte GmbH; Wetzlar, Germany) and iTrace (Tracey Technologies; Texas, USA) for topography and wavefront analysis, supplemented by noninvasive keratography tear breakup time (NIKBUT) to assess film stability. “This holistic approach ensures precise measurements and minimizes postoperative surprises,” he noted.
For patients with evidence of ocular surface disease, such as dry eye or blepharitis, Dr. Hutauruk implements a comprehensive ocular surface optimization protocol. This includes preservativefree lubricating eye drops and lipid-based tear supplements; topical anti-inflammatory agents, such as corticosteroids or cyclosporine A, for moderate to severe inflammation; and warm compresses and lid hygiene to manage meibomian gland dysfunction.
For patients with active or recurrent corneal disease, timing the cataract surgery requires caution. “In cases such as pterygium, I first perform surgical excision using conjunctival autograft and fibrin glue to promote healing and reduce recurrence. I would delay cataract surgery for at least three months post-pterygium excision to allow the healing process. This delay is essential to ensure corneal stability and more accurate astigmatic measurements. If significant corneal astigmatism is present (>0.75D), I would consider
toric intraocular lenses (IOLs). In cases of recurrent or active corneal disease (e.g. herpes simplex keratitis or ocular surface inflammation), I would postpone cataract surgery until the disease is under control,” he shared.
One of the biggest hurdles in compromised corneas is accurate IOL power calculation, as corneal irregularities and pathologies can distort keratometry readings and complicate wavefront-based assessments and toric axis alignment.
“The primary challenge is obtaining accurate keratometry (K) readings in eyes with irregular astigmatism or scarring,” said Dr. Hutauruk. To overcome this, he employed multiple multiple devices—including the Pentacam, IOLMaster (Carl Zeiss Meditec; Jena, Germany), and iTrace—to cross-validate measurements and identify outliers.
For patients with distorted or scarred corneas, advanced IOLs may not deliver the promised spectacle independence and may even exacerbate visual disturbances. “In eyes with significant corneal irregularity or scarring, I typically recommend monofocal IOLs to maximize visual potential and minimize photic phenomena,” he said.
On the other hand, in patients with stable and regular corneal
topography, Dr. Hutauruk noted that he may consider toric IOLs to correct astigmatism. He also emphasized thorough counseling to align patient expectations with realistic outcomes.
Surgical modifications for better outcomes
Even during surgery, adaptations are critical to protect the eye and improve outcomes.
“In cases with compromised visualization, I consider femtosecond laser-assisted cataract surgery (FLACS) to achieve precise capsulorhexis and lens fragmentation with minimal ultrasound energy,” he shared, adding that he would also reduce phaco power and adjusting fluidics setting to reduce endothelial trauma.
Poor visualization due to corneal opacities or edema can complicate every step of cataract surgery.
“When visualization is challenging, I rely on FLACS to create a precise capsulorhexis and segment the nucleus, thereby reducing the need for phaco energy. I also consider epithelial debridement to improve clarity,” he said.
In high-risk patients, I may consider topical cyclosporine A to modulate inflammation. Close follow-up is essential for detecting complications such as epithelial defects, persistent inflammation or infection,” he stressed.
Cataract surgery in eyes with compromised corneal surfaces demands more than technical skill—it requires comprehensive assessment, medical optimization, surgical precision and vigilant postoperative care.
As Dr. Hutauruk demonstrated, adapting each step to the individual patient's corneal status not only improves outcomes but also avoids complications, ensuring that visual rehabilitation is both safe and effective, even in the most challenging cases.

Postoperatively, Dr. Hutauruk applies a layered management strategy. “I prescribe preservativefree broad-spectrum antibiotics (e.g. fourth-generation fluoroquinolones) and corticosteroids to control inflammation,” he explained.
“Lubricating eye drops are continued to support ocular surface healing.
Dr. Hutauruk shared a challenging case involving a patient with advanced Fuchs endothelial dystrophy and significant corneal edema.
“The endothelial cell count was below 700. Visualization was significantly compromised due to epithelial and stromal edema,” he recalled. To enhance clarity, Dr. Hutauruk performed epithelial debridement followed by cataract extraction using FLACS. A monofocal IOL was implanted, targeting slight myopia (-1.00 D) to compensate for the expected hyperopic shift after posterior lamellar keratoplasty. He then proceeded with Descemet’s stripping automated endothelial keratoplasty (DSAEK) immediately following cataract surgery. “This allowed the patient to undergo both procedures in a single surgical session under general anesthesia,” he said.
Dr. Johan A. Hutauruk is a consultant ophthalmologist and director of the Jakarta Eye Centre in Central Jakarta, a private eye hospital in Indonesia with several locations in Jakarta and Indonesia. Dr. Hutauruk is the current president of the Indonesian Society of Cataract and Refractive Surgery (INASCRS) and is a member of the scientific committee of the Indonesian Ophthalmologist Annual Meeting. In recognition of having organized more than 10,000 free cataract surgeries per year since 2002, the Asia Pacific Academy of Ophthalmology awarded him the APAO Distinguished Service Award during the 2008 APAO and World Ophthalmology Congress in Hong Kong. Dr. Hutauruk has been a member of the advisory board for the Indonesian Ophthalmologist Association Annual Meeting for the last 10 years, mainly responsible for the scientific content, as well as a council member for the APACRS, and currently a member of the Editorial Board of EyeWorld Asia-Pacific.
johan.hutauruk@jec.co.id
What's going on behind the lens? A new report from the University of Houston College of Optometry adds a key piece to the myopia control puzzle, showing that high-add multifocal contact lenses not only slow the progression of nearsightedness in children but also trigger subtle anatomical changes that could explain why. 1
The study, published in Investigative Ophthalmology & Visual Science, is the latest analysis from the BLINK and BLINK2 studies, a multi-year clinical project funded by the National Eye Institute. Led by Dr. David Berntsen, Golden-Golden Professor of Optometry and chair of Clinical Sciences at the University of Houston and his collaborators at Ohio State University, the research tracks how different lens types affect eye growth in myopic children.
A closer look at the choroid
The star of this latest update isn’t the cornea or the retina, but the choroid, the vascular middle layer sandwiched between them that’s quietly nourishing the retina and playing an increasingly suspicious role in myopia progression. In the BLINK study, children wearing high-add (+2.50 D) multifocal contact lenses showed a measurable increase in subfoveal choroidal thickness and area just two weeks into treatment.1
And, according to co-author Dr. David Berntsen, that thickness difference “was maintained throughout the three-year study”.
Why does that matter? In myopia, the eye grows too long from front to back, causing light to focus in front of the retina instead of on it. A thicker choroid could be signaling a slowdown in that axial stretch, which is good news for long-term visual outcomes.
BLINK and you'll miss it? Not quite
The BLINK (Bifocal Lenses In Nearsighted Kids) study and its sequel, BLINK2, included 281 children between 7 and 11 years old. Participants were
randomly assigned to wear either single vision lenses or multifocal lenses with different add powers. The team then measured subfoveal choroidal thickness and area over time.1
From the start, the high-add multifocal lens group stood out. After just two weeks of wear, those kids showed an average increase in choroidal thickness of 8 microns and a 0.07 mm² increase in choroidal area, an effect that persisted across all three years of follow-up.1
Berntsen's team also found a meaningful link between early thickening and slower eye growth. Children who showed an increase in choroidal thickness at two weeks were more likely to have less axial elongation over the long haul. In fact, kids in the high-add group had 0.23 mm less axial elongation over three years than their peers in single-vision lenses.1
"While there were no changes in choroidal thickness or area in the single vision group, eyes in the high-add multifocal contact lens group that grew less maintained a slightly thicker choroid throughout the three years of multifocal lens wear," said Berntsen.
The initial choroidal thickening seen after just two weeks could explain roughly 20-29% of the reduced axial elongation in the +2.50 D group. While not the sole mechanism, this change is a measurable contributor to reduced axial elongation.1
Regional differences matter
The research revealed interesting patterns across different areas of the eye. The superior, inferior, and temporal quadrants of the choroid thickened with high-add lens wear, while the nasal side near the optic nerve stayed stable. These regional differences align with previous findings and anatomical expectations.1
Interestingly, the +1.50 D multifocal group didn't show the same benefits. Their choroids stayed about the same thickness, as did their rate of eye growth. When it comes to myopia control, it seems not all multifocals are created equal.1
Key takeaways from the BLINK studies
• Children wearing high-add power multifocal lenses had increased choroidal thickness and area
• This increase was apparent after two weeks and sustained for three years
• Eyes that thickened early were less likely to elongate significantly over time
• No such changes were seen in the single vision contact lens group
The bottom line for clinicians With childhood myopia rates rising globally (affecting 35% of children currently and projected to reach 40% by 2050), the need for effective, evidence-based interventions has never been clearer. These new findings give practitioners one more way to explain how multifocal lenses work, not just optically, but anatomically.
The BLINK study reinforces that early, measurable changes in the eye's structure can be linked to long-term benefits—a recurring theme in myopia control. For the choroid, it seems, thicker might just be better. And for clinicians battling the rising tide of childhood myopia, that's one more tool in the treatment toolkit.
Editorial Note:A version of this article was first published on cookiemagazine.org
1. Walker MK, Berntsen DA, Robich ML, et al. Three-year change in subfoveal choroidal thickness and area with multifocal contact lens wear in the Bifocal Lenses in Nearsighted Kids (BLINK) study. Invest Ophthalmol Vis Sci. 2025;66(5):5.
Join us for the latest clinical advancements and practical insights to help your practice thrive. Don’t miss:
• Subspecialty content from cornea to uveitis
• Cataract Spotlight, now on Sunday
• Courses for every level — residents to experts — and for the entire practice team
• AAO 2025’s must-attend social event, Illuminate, supporting ophthalmic education on Saturday
Plan your schedule with the Meeting Guide at aao.org/mtg-guide.
Register Early and Save
Secure your spot — and your Illuminate ticket — before they’re gone.

aao.org/registration
Where All of Ophthalmology Meets®

Sponsored by RxSight®
Experts highlight real-world applications of the Light Adjustable Lens™ (LAL®/LAL+®) for optimized cataract outcomes.

On Day 3 of the 2025 American Society of Cataract and Refractive Surgery Annual Meeting (ASCRS 2025) in Los Angeles, the RxSight (California, USA) booth drew a crowd with a lineup of expert-led talks focused on the Light Adjustable Lens. From clinical applications and patient selection tips to marketing and workflow strategies, attendees got a well-rounded look at how this gamechanging technology is being used in real-world practices.
LAL or LAL+?
Dr. Neda Nikpoor from Jenkins Eye Care (Hawaii, USA) shared practical guidance on selecting between the LAL and LAL+ for different patient types.
"The beauty of the Light Adjustable Lens is that it is the lens that gives us the ability to customize vision for our patients," she said, pointing out how the technology helps separate the
decision of surgery from the pressure of picking a final refractive target right away.
Drawing from post-marketing data (1,057 LAL and 407 LAL+ patients), 2 Dr. Nikpoor showed both versions delivered excellent uncorrected distance vision: better than 20/20 binocularly on average.
Another benefit? The LAL+ needed less anisometropia. “We pushed 0.91 diopters mean of anisometropia versus 1.1 diopters of anisometropia in the LAL patients," she explained.
For patient selection, Dr. Nikpoor offered practical guidance. "For somebody you would put a monofocal lens in, that's a great patient to do an LAL in,” she advised. “If there's somebody that you would feel comfortable putting an extendeddepth-of-focus lens in—normal anatomy, minimal ocular surface disease, no significant macular degeneration or glaucoma, not postrefractive—then that would be a good person for an LAL+."
The LAL+ is also ideal for patients new to vision optimized at different distances, since it delivers range without heavily inducing anisometropia.
"The beauty of the Light Adjustable Lens is that it is the lens that gives us the ability to customize vision for our patients."
- Dr. Neda Nikpoor
Dr. Nikpoor illustrated her approach with two cases: one, a high myope who did well with the LAL; the other, an optometrist who initially planned for near vision, but after experiencing the LAL+, chose distance in both

Dr.
eyes instead. The result? 20/10 vision and one very happy patient.
"Even somebody who really, really knows—just doesn't know," she concluded, emphasizing the value of post-operative adjustability.
Bring patients in…and keeping them
To round out the session, Christine Sykora, practice administrator at Advanced Eye Care (Illinois, USA), shared strategies for attracting and converting premium lens patients.
"We've heard a lot about how to optimize patient vision once the lens has been implanted. But we have to get the patients to the office and through that decision process first," she began. With acquisition costs ranging from $250 to $500 per patient, every touchpoint matters.
Today’s cataract patients are changing. They’re younger, more digital savvy and more informed. "Seventy percent of these patients are beginning their searches for healthcare providers online. And actually 92% believe that reviews are used as much as personal recommendation," she noted.
Ms. Sykora emphasized a strong online presence (especially Google Business Profiles), a modern, mobileresponsive website and consistent branding. But once they’re in the door, the in-office experience can make or break it.
"Why are patients not choosing us? It's not because of our competition. It's not because they didn't like what we had to offer. It's because of the behavior of one person in our practice driving them away," she stated bluntly.
To combat this, Ms. Sykora's practice focuses on a unified "premium patient experience," aligning language across all team members. "If the doctor is calling it a single distance lens, we call it a single distance lens. If the doctor calls it an adjustable lens, all of their materials need to say adjustable lens," she explained.
Patient education starts early, with printed materials sent ahead of appointments and one-on-one

sessions with a certified technician to handle the logistics, freeing up the surgeon to focus on outcomes.
Ms. Sykora also shared examples of their branded education folders, dry eye kits and post-op instruction packets. Regular audits, from tracking conversion rates to monitoring reviews, help keep the process sharp.
And it’s paying off. "Putting this process in place for our practice and the addition of RxSight lenses has moved our conversion of premium lenses from 20% to 33%, and it's growing," she reported.
Beyond the spotlight sessions, the RxSight booth also featured a diverse lineup of expert talks covering broader dimensions of Light Adjustable Lens integrations and outcomes.
Dr. Huck Holz of Kaiser Permanente (California, USA) shared insights on incorporating the Light Adjustable Lens into a large-scale integrated healthcare network, offering a systems-level look at making this technology work across multiple touchpoints.
Meanwhile, Dr. Alison Early, a cataract and refractive surgeon in Cincinnati (Ohio, USA) emphasized the importance of starting with the ocular surface, presenting tips on optimizing outcomes from the very first exam.
And for patients with complex visual demands, Dr. Christine Funke from Barnet Dulaney Perkins Eye Center (Arizona, USA) discussed how to fine-tune optical quality using
Light Adjustable Lens technology, highlighting its adaptability in challenging cases.
The sessions at the RxSight booth offered a clear picture of where Light Adjustable Lens technology is headed: more customization, better patient outcomes and stronger practice integration.
As Dr. Nikpoor aptly summarized, "This is really the beauty of the adjustable lens—the fact that patients can test drive their vision, and you can really customize their vision in both eyes after implantation."
With more than 1,044 practices and 1,850 surgeons now using Light Adjustable Lens technology in the United States—and over 225,000 lenses implanted to date—the shift toward adjustable vision is well underway.
References
1. Weikert MP. Spherical aberration and the Light Adjustable Lens. Presbyopia Physician. 2024;4:26-29.
2. PMCS-002 data on file at RxSight
Reporting for this story took place during the annual meeting of the American Society of Cataract and Refractive Surgery (ASCRS 2025) held from 25-28 April in Los Angeles, California, United States. A version of this article was first published on cakemagazine.org
INDICATIONS: The Light Adjustable Lens™ (LAL®) and Light Delivery Device™ (LDD™) system is indicated for the reduction of residual astigmatism to improve uncorrected visual acuity after removal of the cataractous natural lens by phacoemulsification and implantation of the intraocular lens in the capsular bag in adult patients with preexisting corneal astigmatism of ≥ 0.75 diopters and without preexisting macular disease. The system also reduces the likelihood of clinically significant residual spherical refractive errors.
CONTRAINDICATIONS: The Light Adjustable Lens is contraindicated in patients who are taking systemic medication that may increase sensitivity to ultraviolet (UV) light as the LDD treatment may lead to irreversible phototoxic damage to the eye; patients who are taking a systemic medication that is considered toxic to the retina (e.g., tamoxifen) as they may be at increased risk of retinal damage during LDD treatment; patients with a history of ocular herpes simplex virus due to the potential for reactivation from exposure to UV light; patients with nystagmus as they may not be able to maintain steady fixation during LDD treatment; and patients who are unwilling to comply with the postoperative regimen for adjustment and lock-in treatments and wearing of UV protective eyewear.
WARNINGS: Careful preoperative evaluation and sound clinical judgment should be used by the surgeon to decide the risk/benefit ratio before implanting an IOL in a patient with any of the conditions described in the Light Adjustable Lens and LDD Professional Use Information document. Caution should be used in patients with eyes unable to dilate to a pupil diameter of ≥ 7 mm to ensure that the edge of the Light Adjustable Lens can be visualized during LDD light treatments; patients who the doctor believes will be unable to maintain steady fixation that is necessary for centration of the LDD light treatment; patients with sufficiently dense cataracts that preclude examination of the macula as patients with preexisting macular disease may be at increased risk for macular disease progression; and patients at high risk for future vitreoretinal disease that may require silicone oil as part of therapy. The Light Adjustable Lens must be implanted in the correct orientation with the back layer facing posteriorly.
PRECAUTIONS: The long-term effect on vision due to exposure to UV light that causes erythropsia (after LDD treatment) has not been determined. The implanted Light Adjustable Lens MUST undergo a minimum of 2 LDD treatments (1 adjustment procedure plus 1 lock-in treatment) beginning at least 17-21 days post-implantation. All clinical study outcomes were obtained using LDD power adjustments targeted to emmetropia post LDD treatments. The safety and performance of targeting to myopic or hyperopic outcomes have not been evaluated. The safety and effectiveness of the Light Adjustable Lens and LDD have not been substantiated in patients with preexisting ocular conditions and intraoperative complications. Patients must be instructed to wear the RxSight-specified UV protective eyewear during all waking hours after Light Adjustable Lens implantation until 24 hours post final lock-in treatment. Unprotected exposure to UV light during this period can result in unpredictable changes to the Light Adjustable Lens, causing aberrated optics and blurred vision, which might necessitate explantation of the Light Adjustable Lens.
ADVERSE EVENTS: The most common adverse events (AEs) reported in the randomized pivotal trial included cystoid macular edema (3 eyes, 0.7%), hypopyon (1 eye, 0.2%), and endophthalmitis (1 eye, 0.2%). The rates of AEs did not exceed the rates in the ISO historical control except for the category of secondary surgical interventions (SSI); 1.7% of eyes (7/410) in the Light Adjustable Lens group had an SSI (p < .05). AEs related to the UV light from the LDD include phototoxic retinal damage causing temporary loss of best spectacle corrected visual acuity (1 eye, 0.2%), persistent induced tritan color vision anomaly (2 eyes, 0.5%), persistent induced erythropsia (1 eye, 0.3%), reactivation of ocular herpes simplex Infection (1 eye, 0.3%), and persistent unanticipated significant increase in manifest refraction error (≥ 1.0 D cylinder or MRSE) (5 eyes, 1.3%).
CAUTION: Federal law restricts this device to sale by or on the order of a physician. Please see the Professional Use Information document for a complete list of contraindications, warnings, precautions, and adverse events.
LIGHT ADJUSTABLE LENS+™ (LAL+®) INDICATIONS FOR USE AND IMPORTANT SAFETY INFORMATION
INDICATIONS: The Light Adjustable Lens+™ (LAL+®) and Light Delivery Device™ (LDD™) system is indicated for the reduction of residual astigmatism to improve uncorrected visual acuity after removal of the cataractous natural lens by phacoemulsification and primary implantation of the intraocular lens in the capsular bag in adult patients with preexisting corneal astigmatism of ≥ 0.75 diopters and without preexisting macular disease. The system also reduces the likelihood of clinically significant residual spherical refractive errors.
CONTRAINDICATIONS: The LAL+ is contraindicated in patients who are taking systemic medication that may increase sensitivity to ultraviolet (UV) light as the LDD treatment may lead to irreversible phototoxic damage to the eye; patients who are taking a systemic medication that is considered toxic to the retina (e.g., tamoxifen) as they may be at increased risk of retinal damage during LDD treatment; patients with a history of ocular herpes simplex virus due to the potential for reactivation from exposure to UV light; patients with nystagmus as they may not be able to maintain steady fixation during LDD treatment; and patients who are unwilling to comply with the postoperative regimen for adjustment and lock-in treatments and wearing of UV protective eyewear.
WARNINGS: Careful preoperative evaluation and sound clinical judgment should be used by the surgeon to decide the risk/benefit ratio before implanting an IOL in a patient with any of the conditions described in the LAL+ and LDD Professional Use Information document. Caution should be used in patients with eyes unable to dilate to a pupil diameter of ≥ 7 mm to ensure that the edge of the LAL+ can be visualized during LDD light treatments; patients who the doctor believes will be unable to maintain steady fixation that is necessary for centration of the LDD light treatment; patients with sufficiently dense cataracts that preclude examination of the macula as patients with preexisting macular disease may be at increased risk for macular disease progression; and patients at high risk for future vitreoretinal disease that may require silicone oil as part of therapy. The LAL+ must be implanted in the
correct orientation with the back layer facing posteriorly.
PRECAUTIONS: The safety and effectiveness of the LAL+ has not been substantiated in clinical trials. The effects of the LAL+ optical design on the quality of vision, contrast sensitivity, and subjective visual disturbances (glare, halo, etc.) have not been evaluated clinically. Surgeons must weigh the potential benefits of the modified optical design of the LAL+ against the potential for risks associated with degradation in vision quality and the lack of clinical data to characterize the impact of the LAL+ optical design on contrast sensitivity and subjective visual disturbance. These considerations may be especially relevant to patients with certain pre-existing ocular conditions (prior corneal refractive surgery, irregular corneal astigmatism, severe corneal dystrophy, macular disease, or optic nerve atrophy, etc.) or intraoperative conditions (posterior capsular rupture, complications in which the IOL stability could be compromised, inability to place IOL in capsular bag, etc.). The long-term effect on vision due to exposure to UV light that causes erythropsia (after LDD treatment) has not been determined. The implanted LAL+ MUST undergo a minimum of 2 LDD treatments (1 adjustment procedure plus 1 lock-in treatment) beginning at least 17-21 days post-implantation. All clinical study outcomes were obtained using LDD power adjustments targeted to emmetropia post-LDD treatments. The safety and performance of targeting to myopic or hyperopic outcomes have not been evaluated. The safety and effectiveness of the LAL+ and LDD have not been substantiated in patients with preexisting ocular conditions and intraoperative complications. Patients must be instructed to wear the RxSight-specified UV protective eyewear during all waking hours after LAL+ implantation until 24 hours post final lock-in treatment. Unprotected exposure to UV light during this period can result in unpredictable changes to the LAL+ , causing aberrated optics and blurred vision, which might necessitate explantation of the LAL+. When performing refraction in patients implanted with the LAL+, confirmation of refraction with maximum plus manifest refraction technique is recommended.
ADVERSE EVENTS: The most common adverse events (AEs) reported in the randomized pivotal trial of the parent LAL included cystoid macular edema (3 eyes, 0.7%), hypopyon (1 eye, 0.2%), and endophthalmitis (1 eye, 0.2%). The rates of AEs did not exceed the rates in the ISO historical control except for the category of secondary surgical interventions (SSI); 1.7% of eyes (7/410) in the LAL group had an SSI (p < .05). AEs related to the UV light from the LDD include phototoxic retinal damage causing temporary loss of best spectacle corrected visual acuity (1 eye, 0.2%), persistent induced tritan color vision anomaly (2 eyes, 0.5%), persistent induced erythropsia (1 eye, 0.3%), reactivation of ocular herpes simplex Infection (1 eye, 0.3%), and persistent unanticipated significant increase in manifest refraction error (≥ 1.0 D cylinder or MRSE) (5 eyes, 1.3%).
CAUTION: Federal law restricts this device to sale by or on the order of a physician. Please see the Professional Use Information document for a complete list of contraindications, warnings, precautions, and adverse events.
©2025 RxSight®. All Rights Reserved. COM1328 Rev. A

by Kendra Bruning
At APAO 2025, five top ophthalmic researchers revealed how new frontiers in imaging—from cellular-resolution OCT to CSF-flow MRI—are pushing the boundaries of personalized eye care.

Leading ophthalmologists converged at the 40th Congress of the Asia-Pacific Academy of Ophthalmology (APAO 2025) in New Delhi, India, to explore cutting-edge updates in ocular imaging, with applications stretching from limbal stem cells to high-res retinal scans.
The symposium, Exploring Visual Frontiers: Advances in Ocular Imaging Across Subspecialties, chaired by Dr. Kevin Chan (USA), featured speakers from India and the United States presenting five distinct approaches to seeing and understanding the eye in unprecedented detail.
Whether peering at Müller cell migration in macular holes or mapping cerebrospinal fluid (CSF) dynamics behind the optic nerve, one message came through loud and clear: imaging is no longer just about clarity, it’s about clinical consequence.
Corneal comebacks and the long road to normal
The session opened with Dr. Anahita Kate (India), whose longterm follow-up of simple limbal epithelial transplantation (SLET) patients provided the audience with a rare glimpse into the dynamics of epithelial recovery after corneal stem cell rescue.
Her team analyzed post-SLET outcomes over five to 12 years using a full suite of imaging tools, like slit-lamp photography, confocal microscopy, impression cytology and hyperreflective segment optical coherence tomography (OCT). The numbers were promising: “Around 70% of the patients between a period of 5 to 12 years had successful outcomes on each and every imaging modality,” Dr. Kate reported.
But normalization wasn’t absolute. Despite corneal thickness returning to near-normal in most cases, imaging still detected persistent irregularities in epithelial reflectivity and densitometry. “Although the thickness comes back to normal, there is still some room for improvement that can occur down the line,” she explained.
These findings weren’t just academic. Multivariate analysis confirmed that increased epithelial reflectivity and density correlated with lower final visual acuity, shifting the spotlight from thickness alone to more nuanced, function-linked biomarkers.
“Around 70% of the patients between a period of 5 to 12 years had successful outcomes on each and every imaging modality.”
-
Dr. Anahita Kate
As the field moves toward more personalized metrics of surgical success, her study highlights the value of multimodal imaging, not just for tracking structure, but also for predicting visual outcomes.
Shifting gears from surface diagnostics to deep neurofluidics, Dr. Muneeb Faiq (USA) took the audience on a journey down the brain-eye highway. Using contrastenhanced dynamic MRI in mice, his team visualized CSF flow patterns between the spine and the optic

nerve, charting a course through previously uncharted paravascular territory.
“The optic nerve may have a paravascular CSF circulation system similar to the glymphatic system,” he explained. The team’s data showed that flow was dependent on molecular size, with larger contrast agents experiencing delayed movement. Just like in the brain, aquaporin-4 channels appeared to regulate this flow, pointing to a shared mechanism between the central nervous system and ocular environments.
But things took a turn when intraocular pressure (IOP) entered the mix. “Chronic IOP elevation is associated with [a] significant decrease in CSF flow in the subarachnoid space and parenchyma,” said Dr. Faiq, suggesting that fluidic dysregulation may play a role in glaucomatous optic neuropathy.
Even the fellow eye wasn’t off the hook. “CSF dynamics in one eye can affect the CSF dynamics in the other eye,” he added, highlighting possible cross-talk or systemic compensation in bilateral disease.
Together, the findings offer a tantalizing glimpse into glaucoma’s fluidic undercurrents and hint at future therapeutic strategies aimed at restoring the brain-eye balance.
Taking the stage with a forwardlooking twist, Dr. Sujani Shroff (India) introduced a smartphonebased artificial intelligence (AI) model designed to detect referable glaucoma, bringing deep learning to the palm of the practitioner. Her system combines a segmentation model to evaluate the vertical cup-todisc ratio (VCDR) with a classification model powered by class activation maps, highlighting subtle structural changes in fundus images.
Trained on more than 5,000 images, the algorithm proved to be more than just a high-tech curiosity. “Specialists detected 60% of glaucoma cases versus 94% for the AI,” reported Dr. Shroff. While the specificity was lower, the increased sensitivity was nothing short of eye-opening.
“This could possibly mean that the AI is detecting very subtle structural changes that are not evident to the human eye,” she said, hinting at the system’s potential to catch glaucoma in its quietest stages.
But this tool isn’t just an automated screener. Its built-in visual overlays offer a second set of eyes for clinicians, showing exactly where the AI flagged abnormalities. That feature also makes it a powerful teaching platform for glaucoma fellows and general ophthalmologists alike.
Specialists detections of glaucoma cases AI detections of glaucoma cases 60% 94% vs.
“This could possibly mean that the AI is detecting very subtle structural changes that are not evident to the human eye.”
- Dr. Sujani Shroff
With its ease of use and smartphone compatibility, the model is being positioned for telemedicine outreach in underserved areas. Dr. Shroff’s team is now diving deeper into the algorithm’s decision-making logic, aiming to uncover the features it flags before human clinicians ever spot them.
When Dr. Srinivas Sadda (USA) took the stage, he didn’t just raise the resolution, he redefined it. His presentation showcased the power of high-resolution OCT, which tightens axial resolution from the standard 6-7 microns down to an astonishing 2-3 microns. The result was a nearhistological look at the retina without ever touching a slide.
“We may be able to use the highresolution techniques to provide a gold standard reference, which we can then use to train using AI faster, less expensive, but [lower] quality images.”
- Dr. Srinivas Sadda
“Each iteration of our technology brings us closer and closer to histology,” said Dr. Sadda, as he unveiled crystalline scans of retinal layers that captured individual capillaries, hyperreflective foci and early drusenoid deposits in exquisite detail. Features that once blurred together are now being teased apart, offering clearer differentiation between normal structures and biomarkers of disease progression, especially in age-related macular degeneration (AMD).
This subcellular sharpness isn’t just for show. These imaging improvements help clinicians pinpoint early signs of retinal atrophy, evaluate calcified drusen and distinguish between migrating retinal pigment epithelium (RPE) cells and

retinal vasculature. He emphasized that this matters when every micron counts in tailoring treatment and predicting disease courses.
But Dr. Sadda didn’t stop at diagnostics. He proposed a future where high-res OCT acts as the ‘gold standard’ for training AI models, bringing some of that precision to faster, more affordable systems. “We may be able to use the highresolution techniques to provide a gold standard reference, which we can then use to train using AI faster, less expensive, but [lower] quality images,” he explained.
With this level of detail, clinicians are now better equipped to identify subtle structural changes, assess disease progression earlier, and guide personalized treatment strategies—moving precision imaging into the realm of routine.
Immunofluorescence lights up macular hole healing
Closing the symposium, Dr. Thirumalesh M B (India) brought the microscope into focus, revealing the cellular mechanics that may explain why macular holes close. Through immunofluorescence studies of vitreoretinal interface membranes, his team uncovered glial fingerprints
across both the internal limiting membrane (ILM) and posterior hyaloid.
“The cells that we saw in the hyaloid were microglial cells,” he reported. “The Müller cell is actually a guide on which the migrating microglia can proliferate first, form the mass, then contract.” Together, these cells may form a [biological] scaffold that brings the retinal edges together and keeps them there.
His group stained membranes collected during macular hole surgery, revealing strong GFAP positivity, evidence of glial identity, in every sample. This challenged longheld assumptions about the passive role of the hyaloid, suggesting instead that it participates in repair.
One standout case drove the point home: after a failed ILM peel, Dr. Thirumalesh transplanted a segment of the anterior hyaloid, cut to fit the defect. Three months later, the hole was closed, and vision improved. His lab even cultured spindle-shaped cells from the same hyaloid tissue, confirming their glial nature.
These findings suggest that macular hole repair may be less about mechanical closure and more about creating the right conditions for glial recruitment and remodeling. Whether via inverted flaps or hyaloid grafts,
success may depend on biology as much as technique.
Across all five presentations, it was clear that advanced imaging is no longer just about better pictures, it’s about better strategy. The innovations on display weren’t isolated tools, but translational technologies designed to inform surgical choices, predict outcomes, and personalize care from the cellular level up.
From stem cell integration to AI diagnostics and glymphatic insight, today’s imaging guides tomorrow’s treatments, and often at the cellular or molecular level. But the future may be hybrid: training low-cost tools with high-res benchmarks, and pairing machine smarts with clinical nuance.
“The Müller cell is actually a guide on which the migrating microglia can proliferate first, form the mass, then contract.”
- Dr. Thirumalesh M B
As Dr. Sadda put it, “Being able to have this kind of cellular-level visualization… is going to be quite useful.” Especially when that clarity feeds into smarter algorithms, refined protocols, and ultimately, sharper outcomes for patients. These tools may differ in wavelength and resolution, but their destination is better vision, guided by better insight.
Reporting for this story took place during the 40th Congress of the Asia-Pacific Academy of Ophthalmology (APAO 2025), held in conjunction with the 83rd Annual Conference of the All India Ophthalmological Society (AIOC 2025) from 3-6 April in New Delhi, India.


Infectious keratitis poses a growing global threat to sight, forcing ophthalmologists to innovate beyond traditional treatments
by Hazlin Hassan
Infectious keratitis presents a quiet but challenging threat to sight as microbial culprits develop increased drug resistance. Ophthalmologists are witnessing a rise in stubborn bacterial strains and deep-seated fungal infections that no longer respond to first-line therapies—requiring a shift in conventional management strategies.
It might not grab headlines like a pandemic, but infectious keratitis is waging a quiet war against sight across the globe. Once dominated by easily treatable bacteria, today’s microbial culprits have upped their game. Cue the rise of drugresistant strains and deep-diving fungi that scoff at first-line drops. Ophthalmologists are being forced to match microbial creativity with innovation of their own.
Dr. Artemis Matsou, a consultant at Queen Victoria Hospital in the UK, knows the battlefield all too well.
“I increasingly see multi-drug resistant bacterial keratitis,” she said.
Patients arrive at her tertiary center after exhausting multiple courses of
antibiotics elsewhere, with some infections already entrenched. Even fungal keratitis, already notoriously difficult to manage, is becoming tougher.
“Clinically, I have observed more cases failing to respond to firstline agents like natamycin or voriconazole,” said Dr. Matsou, citing delays in diagnosis and prior corticosteroid use as aggravating factors.
She also noted that postcorneal transplant patients are particularly vulnerable to drug-resistant strains, not only because of reduced ocular surface immunity and steroid use, but also because the signs of infection can be subtle yet progress rapidly.
“Clinically, I have observed more cases failing to respond to first-line agents like natamycin or voriconazole.”
- Dr. Artemis Matsou
“But for me, the real red flag is how many cases now require fortified or combination therapy as first-line, and how often culture-negative infections behave clinically as if they’re resistant, perhaps due to biofilms, delayed presentation or altered host response,” she added.
In Malaysia, Assoc. Prof. Dato’ Dr. Khairidzan Mohd Kamal, director of Cornea, External Disease and Refractive Surgery at the International Islamic University Malaysia, echoed similar concerns.
“Over the past years, drug-resistant pathogens such as Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA) and fungal species, including Fusarium and Aspergillus, are becoming more common,” he said.1
Studies indicate that in parts of India and Malaysia, over 40% of bacterial isolates are fluoroquinolone-resistant
and antifungal-resistant, highlighting the urgency for new therapeutic strategies.
“Over the past years, drug-resistant pathogens such as Pseudomonas aeruginosa, methicillinresistant Staphylococcus aureus (MRSA) and fungal species, including Fusarium and Aspergillus, are becoming more common.”
What’s causing all this trouble?
Back at Queen Victoria Hospital, common culprits include Pseudomonas aeruginosa infections from contact lens-related microbial keratitis, as well as polymicrobial cases, made worse by delayed referrals. Post-surgical patients are also at risk, especially after corneal transplants, refractive procedures or ocular surface reconstruction.
Then there are patients with underlying ocular surface disease, such as severe dry eye, limbal stem cell deficiency or ocular surface inflammatory disorders.
“In those cases, you’re not just fighting the infection, you’re trying to preserve what’s left of a fragile ocular surface,” said Dr. Matsou.

Dr. Kamal noted that infectious keratitis is a major cause of vision loss in Southeast Asia due to the tropical climate, high prevalence of agriculture and increasing contact lens use.
To outmaneuver these pathogens, clinicians are turning to newer modalities. One of the most promising is a photoactivated chromophore for infectious keratitis (PACK-CXL).
Using riboflavin and UVA light, this technique simultaneously crosslinks collagen and zaps microbes. And it's not just anecdotal. Hashemi et al. found that PACK-CXL holds its own against antibiotic eye drops in bacterial ulcers, and is useful in fungal keratitis.2
Dr. Matsou uses the Hafezi protocol for non-responsive or progressive ulcers. For deeper or recalcitrant infections, she employs intrastromal injections. She also considers corneal biopsies to obtain deep tissue samples.
Early surgical intervention, such as therapeutic lamellar keratoplasty can salvage tissue and preserve vision in some cases, she added.
According to Dr. Kamal, studies have shown that using interstitial injections of antimicrobials has demonstrated efficacy for recalcitrant or deep ulcers.3
Another useful adjunct is amniotic membrane transplantation (AMT), he
added. “AMT has anti-inflammatory properties and stimulates epithelial healing, reducing scarring,” he said
Systematic reviews have demonstrated that AMT can shorten healing times and improve visual outcomes in moderate to severe infectious keratitis without associated complications.4
Nanotech, peptides and bacteria-attacking viruses If standard eye drops are blunt instruments, nanocarrier-based drugs promise scalpel-like precision.
According to Mahaling et al., nanostructured natamycin produced better results in experimental fungal keratitis.5
“Preclinical studies have shown that nanoparticle-based formulations, such as natamycin or amphotericin B-loaded liposomes, can significantly improve corneal penetration and drug retention time, especially in deep fungal keratitis,” said Dr. Matsou.
Meanwhile, antimicrobial peptides (AMPs) are demonstrating serious antimicrobial muscle in the lab. Roy et al. reported promising in-vitro activities in AMPs against keratitis pathogens, with clinical trials in progress.6
Phage therapy is another wildcard in the deck. In animal studies, specific bacteriophages or viruses that attack bacteria effectively cleared drugresistant P. aeruginosa keratitis.7 It remains experimental, but imagine prescribing viruses to cure bacterial


ulcers—the plot twist ophthalmology didn’t know it needed.
Empirical therapy might soon go the way of floppy disks. What excites Dr. Matsou most is the shift toward pathogen-specific treatment.
“This includes the development of rapid molecular diagnostics, such as PCR or next-generation sequencing platforms, which could help us tailor antimicrobial therapy within hours rather than days,” she said.
The future she envisions involves better diagnostics, smarter drug delivery and earlier, targeted intervention—all working together to preserve vision and reduce morbidity in what remains a sight-threatening ocular emergency.
1. Ting DSJ, Henein C, Said DG, et al. (2021). Amniotic membrane transplantation for infectious keratitis: A systematic review and meta-analysis. Sci Rep. 2021;11(1):13007.
2. Hafezi F, Hashemi H, Torres-Netto EA, et al. PACK-CXL vs. antimicrobial therapy for bacterial, fungal, and mixed infectious keratitis: a prospective randomized phase 3 trial. Eye Vis (Lond). 2022;9(1):2.
3. Sharma N, Agarwal P, Sinha R, et al. Evaluation of intrastromal voriconazole injection in recalcitrant deep fungal keratitis: case series. Br J Ophthalmol. 2011;95(12):1735-1737.
4. Ting DSJ, Henein C, Said DG, Dua HS. Amniotic membrane transplantation for infectious keratitis: A systematic review and meta-analysis. Sci Rep. 2021;11(1):13007.
5. Mahaling B, Baruah N, Dinabandhu A. Drug delivery systems for infectious eye diseases: Advancements and prospects. J Nanotheranostics. 2024;5(4)133-166.
6. Ting DSJ, Ho CS, DeshmukhR, et al. Infectious keratitis: An update on epidemiology, causative microorganisms, risk factors, and antimicrobial resistance. Eye (Lond). 202;35(4):1084-1101.
7. Fukuda K, Ishida W, Uchiyama J, et al. Pseudomonas aeruginosa keratitis in mice: Effects of topical bacteriophage KPP12 administration. PLoS One. 2012;7(10):e47742.

The power of combination therapies
In this shifting landscape, monotherapy may not be enough. Clinicians may need to employ a combination of advanced diagnostics, novel therapeutics and surgical interventions to preserve vision and combat this sightthreatening condition.
Combining PACK-CXL with intrastromal voriconazole or layering in amniotic membrane transplantation may mean the difference between scarring and sight. And while innovation is accelerating, equitable access and local resistance tracking remain critical. As Dr. Kamal put it: “The focus for Southeast Asia must be on early uptake of novel agents and equitable access.”
The war against infectious keratitis is far from over. But with smarter drugs, sharper diagnostics and a team of ophthalmic innovators on the front lines, the odds may finally be shifting.
Assoc. Prof. Dato’
Dr. Khairidzan Mohd Kamal currently serves as an associate professor at the Department of Ophthalmology, International Islamic University Malaysia (IIUM). He is also the director of Cornea, External Disease, and Refractive Surgery Services at IIUM Eye Specialist Clinic. Assoc. Prof. Dato’ Dr. Khairidzan received his MBBS from the University of Queensland and obtained his Master of Surgery (Ophthalmology) from the National University of Malaysia. He spent a year as an adjunct clinical instructor and international fellow in Cornea, External Disease, and Refractive Surgery at UCLA. Assoc. Prof. Dato’ Dr. Khairidzan has published several articles in scientific journals and made over 300 scientific presentations. He contributed his expertise to the Malaysia Dry Eye Advisory Board and directly supervised a number of PhD and Masters candidates in external disease and refractive surgery research. Additionally, he received the Asia-Pacific Association of Cataract and Refractive Surgeons Certified Educator Award in 2018, and was appointed a council member of the International Society of Refractive Surgery in 2021.
khairidzan@gmail.com

Dr. Artemis Matsou, MD, MRCP (UK), FEBOS-CR, FEBO, PgDip CRS, is a consultant ophthalmologist and cataract lead at the Queen Victoria Hospital, specializing in cornea, complex cataract and refractive surgery. Her clinical interests include ocular surface reconstruction and limbal stem cell transplantation. She has completed two prestigious Corneal Fellowships at Addenbrooke’s Hospital in Cambridge and Queen Victoria Hospital in East Grinstead. She holds advanced accreditation in cataract and refractive surgery from the European Board of Ophthalmology (FEBOS-CR), is a Fellow of the European Board of Ophthalmology (FEBO) and a Member of the Royal College of Physicians of London (MRCP). Dr. Matsou serves on the Education, Business & Leadership, and Diversity, Equity & Inclusion Committees of the European Society of Cataract and Refractive Surgeons (ESCRS). She also sits on the Councils of the Medical Contact Lens and Ocular Surface Association (MCLOSA) and the European School for Advanced Studies in Ophthalmology (ESASO).
Artemis.matsou1@nhs.net
by Dr. Wei-Yi Yeh and Dr. Pi-Jung Lin
Refractive surgery continually evolves, pushing boundaries in precision and patient outcomes—all thanks to digital workflow integration. This shift not only drastically reduces errors and boosts efficiency but also enhances staff coordination and standardizes clinical protocols for superior results.

The field of refractive surgery continues to be at the forefront of innovation in ophthalmology, driven by improvements in precision, efficiency and patient outcomes. Among these developments, digital workflow integration has significantly transformed surgical planning and surgical procedures.
Traditionally, refractive surgery depends on manual data entry, paper-based documentation and disjointed diagnostic and treatment planning systems. The adoption of digital workflow optimizes these processes by integrating diagnostic assessment, surgical planning

and treatment delivery, as well as optimizing clinical outcomes into one cohesive system. This not only reduces data entry and transcription errors but also helps improve efficiency, enhance staff coordination and convenience, and standardize clinical protocols.
Digital workflow is already established in cataract procedures.¹,2 Digital workflow solutions have streamlined preoperative planning, intraoperative execution and postoperative assessment, enhancing process efficiency, surgical accuracy and patient safety. These advancements have been widely implemented, leading to excellent visual outcomes and high patient satisfaction.2-4
On the other hand, digital workflow integration in refractive surgery remains relatively underexplored. This article examines the role of digital workflow in keratorefractive lenticule extraction (KLEx) surgery, in particular with small-incision lenticule extraction (SMILE), emphasizing its benefits, challenges and clinical implications.
In our clinic, patients considering KLEx undergo a thorough evaluation including manifest refraction, corneal topography and posterior segment assessments using optical coherence tomography (OCT) and fundus photography.
Integrating and documenting these examinations within a digital platform, such as ZEISS FORUM (Carl Zeiss Meditec; Jena, Germany), allows seamless management of patient data in a single system.5 The digital consolidation ensures that patient information remains updated, accessible, and, importantly, visible to both the clinic staff, the surgeon, as well as the patient during consultation.
Moreover, patient engagement is a crucial aspect of refractive surgery, influencing both satisfaction and clinical outcomes. Digital workflows, particularly platforms like ZEISS Refractive Workplace, incorporate powerful visualization tools that display diagnostic images and

treatment parameters in a clear, userfriendly format. These visual aids serve as effective educational tools, helping patients better understand their eye condition and the planned surgical procedure.
This improved understanding can increase confidence and reduce preoperative anxiety. Informed patients tend to be more comfortable and cooperative throughout treatment, enhancing their overall experience.
Furthermore, digital workflow allows for a structured and standardized consultation process. Patients can have their test results explained with the aid of visual tools and even access preoperative educational materials tailored to their specific case. This structured approach reduces miscommunication and ensures patients feel well-informed
and reassured throughout their journey.
Laser vision correction involves multiple procedural steps, each susceptible to human error. Potential errors can arise during data transcription, centration, cyclotorsion alignment and parameter settings. A digital refractive workflow significantly reduces these risks by eliminating manual transcription errors and ensuring secure data transfer from diagnostics to treatment planning.
Key digital features, such as automated ocular alignment (OcuLign) and computer-assisted centration (CentraLign), enhance accuracy in cylinder correction and centration, reducing variability
in treatment execution. Remote planning capabilities enable surgical planning outside the operating room, allowing for meticulous case preparation and reducing intraoperative stress for both the surgeon and supporting staff.
A well-structured digital refractive workflow provides a streamlined approach from initial consultation to postoperative assessment, enhancing workflow process efficiency and increasing convenience for clinical staff at every stage. It facilitates seamless patient interactions and customized treatment planning outside the operating room, allowing for greater flexibility and precision. Additionally, standardized data collection facilitates postoperative analysis and the development of personalized nomograms.
By integrating these functions into a single digital ecosystem, clinics can reduce redundancy, optimize scheduling and improve coordination among team members. The ability to plan procedures remotely not only allows clinical staff and surgeons to dedicate more time to patient consultations and complex case assessments, but it also provides greater flexibility in working hours— supporting a better work-life balance for the entire clinical team.
time savings pre- and intraoperatively to serve more
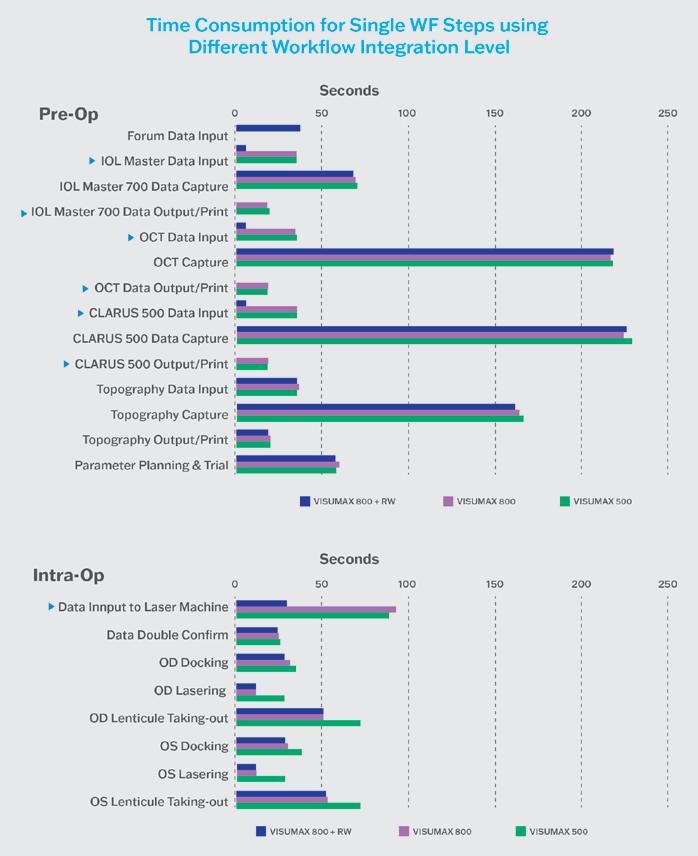
To evaluate how the integration of a digital workflow affects our clinic, we compared three separate groups undergoing KLEx:6
• VISUMAX 800 coupled with the Refractive Workplace: 20 patients treated using the ZEISS Corneal Refractive Workflow, which includes VISUMAX 800 and the Refractive Workplace
• VISUMAX 800: 20 patients treated using the VISUMAX 800 with conventional workflow (laser standalone, not connected to digital solutions like Refractive Workplace)
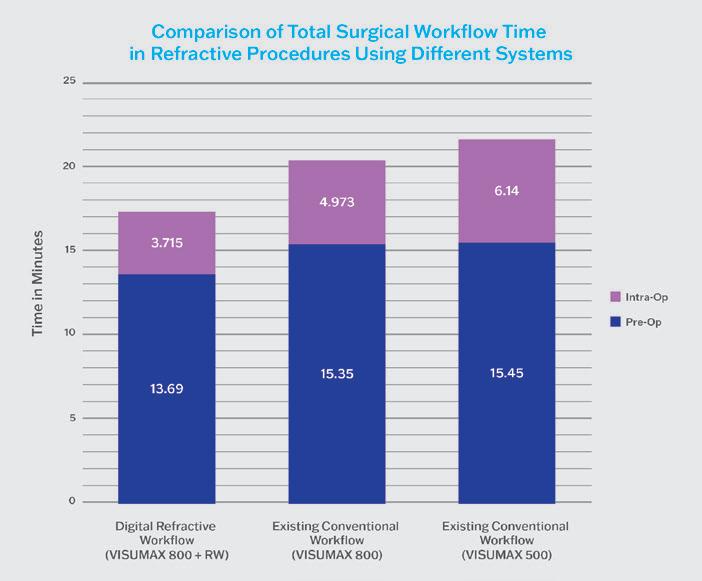
• VisuMax (500 kHz): 20 patients treated using the VisuMax (500 kHz) with conventional workflow
The digital workflow led to an average of 11% reduction in preoperative preparation time by eliminating redundant data entry; with a 10.82% reduction when comparing the VISUMAX 800 + Refractive Workplace group to the VISUMAX 800 group and an 11.37% reduction when comparing the VISUMAX 800 + Refractive Workplace group to the VisuMax (500 kHz) group (Figure 1)
Intraoperatively, the ZEISS Corneal Refractive Workflow with VISUMAX 800 + Refractive Workplace saved approximately 25.3% of the time (75.5 seconds) compared to the conventional VISUMAX 800 workflow, and 39.5% (145.5 seconds) compared to the conventional VisuMax (500 kHz) (Figure 2). Additionally, using the VISUMAX 800 + Refractive Workplace group also showed a significantly reduced overall surgical time of just 3.7 minutes per patient compared to 6 minutes per patient for the VisuMax (500 kHz) group.
This increase in efficiency allowed us to increase the number of procedures performed per hour from four patients to eight, without compromising surgical quality or patient satisfaction.
The integration of a digital workflow in refractive surgery represents a paradigm shift, offering notable improvements in precision, efficiency and patient experience. While its use in cataract surgery is already proven,

Dr. Pi-Jung Lin, MD, is the chief surgeon of Laser Refractive Surgery at Universal Eye Center and serves concurrently in Taiwan University Hospital as a visiting surgeon. Dr. Lin declares no financial interests or consulting relationships with any of the companies or technologies discussed in this study.
max.liu@eyecenter.com.tw
its application in refractive surgery is still evolving.
Current clinical experience suggests that a digital refractive workflow can enhance standardization, increase efficiency, reduce human errors, increase convenience and improve both surgical outcomes and patient satisfaction.
As digital integration in ophthalmology continues to advance, further research and longterm studies will help refine these workflows and maximize their clinical benefits to providers and patients.
1. Rombold F, Niederdellmann C, Pariti R, Khayat B. Time Savings Using a Digital Workflow versus a Conventional for Intraocular Lens Implantation in a Corporate Chain Hospital Setting. Clin Ophthalmol. 2024:18:113-119.
2. Brunner BS, Luft N, Priglinger SG, Shajari M, Mayer WJ, Kassumeh S. Saving of Time Using a Software-Based versus a Manual Workflow for Toric Intraocular Lens Calculation and Implantation. J Clin Med. 2022;11(10):2907.
3. Shetty N, Saxena A, Singh VM, Fernandes M, Garg P, Venkiteshwar M. Effect of digital cataract workflow on time and resource efficiencies in cataract surgery: time and motion study. J Cataract Refract Surg. 2024;50(12):1208-1214.
4. Russell MK, Hsing YI. Evaluation of the Efficiency of a Digital Workflow for Cataract Planning in Patients with Astigmatism. Clin Ophthalmol. 2024;18:1441-1446.
5. ZEISS Refractive Workplace: Optimize your workflow with integrated remote planning. Available at: https://www.zeiss.com/meditec/ en/products/data-management-software/ zeiss-refractive-workplace.html. Accessed on February 4, 2025.
6. Lin PJ. Achieve Excellent Patient Outcomes with Refractive Workplace and VISULYZE. In: ZEISS APAC Ophthalmology Symposium; 2024.

Dr. Wei-Yi Yeh, MD, is chair of Zhonche Universal Eye Center and has long been involved in clinical practice and research related to refractive surgery. Dr. Yeh declares no financial interests or consulting relationships with any of the companies or technologies discussed in this study.
beelzebub519@gmail.com

by Elif Uslu
The APAO 2025 Congress hosted a landmark session on presbyopia, exploring a new generation of personalized treatment options. Experts unveiled breakthroughs in IOL technology, including advanced EDOF and trifocal lenses, alongside innovative non-lens-based approaches like laser scleral restoration.
One of the most interesting sessions during the 40th Congress of the Asia-Pacific Academy of Ophthalmology (APAO 2025)—held in conjunction with the 83rd Annual Conference of the All India Ophthalmological Society (AIOS) in New Delhi, India—was a standout discussion on presbyopia.
Experts from around the world took the stage to spotlight breakthrough strategies, from true accommodation and extended depth of focus (EDOF) intraocular lenses (IOLs) to laserbased scleral restoration and a novel live simulation tool. They covered not only what’s working now, but what’s coming next.
Presbyopia correction with EDOF IOLs
Dr. Naren Shetty (India) shared why he prefers refractive EDOF IOLs for presbyopia correction. “We are in a generation where 20/20 or 6/6 vision is not enough—patients want more,” he said.
According to Dr. Shetty, monofocals still offer the best visual quality, “but you have very little presbyopic correction,” and multifocals, while effective at near vision, involve “a compromise in quality of vision.”
Refractive EDOFs, he argued, strike the right balance. “There is no splitting of light. That is how it's able to maintain quality of vision—and in the new generation of refractive EDOFs, the halo profile is almost similar to a monofocal level, including dysphotopsia,” he added.
On the other hand, Dr. Vaishali Vasavada (India) made a strong case for the use of refractive trifocal IOLs, emphasizing their ability to deliver both visual quality and independence.
“The number of patients whom I can implant a trifocal in is increasing,” she noted, echoing findings from recent meta-analyses showing that nine
out of 10 patients achieve spectacle independence, while only 3% to 5% report significant halos, glare or starbursts.
"I think the basic point we need to understand is that the newer generation trifocals have an excellent range of vision continuity, as well as [providing] best inline spectacle independence—and the whole discussion about dysphotopsia and the negative effects is really going down drastically," added Dr. Vasavada.
Her patient cases—ranging from surgeons and lawyers to those with nystagmus or in monocular situations—show that today’s trifocals work well beyond textbook candidates. “It’s no longer about who qualifies; it’s about identifying the few who don’t.” Her take-home message was clear: the main barriers are not the lenses, but “a hesitant surgeon or an uninformed patient.”
Dr. David Chang (USA) offered a fresh perspective with his mix-andmatch approach, pairing different IOL types to give patients exactly what they’re after: the best of both worlds. Recognizing that too many options can lead to confusion, he referenced The Paradox of Choice, explaining how excess information often fuels indecision and anxiety in patients.
To simplify the process, Dr. Chang blends technologies—typically pairing Alcon’s Vivity EDOF in the dominant eye with a PanOptix trifocal in the non-dominant. “I tell my patients this is like surf and turf. They’re getting the best of both worlds, so they don’t feel like they’re having to give up something by not choosing the other,” he explained.
With this strategy, patients gain strong binocular distance and intermediate vision, functional near and excellent night comfort.
Dr. Helena Prior Filipe (Portugal) addressed a key challenge in refractive surgery: helping patients choose the right IOL. Her solution? Live simulation.
“Live simulation replicates what the patient would experience if the IOL were already implanted. It uses adaptive optics, real-time post-op optical modeling, virtual reality and wavefront-guided imaging to create an immersive preview, so the patient can ‘test drive’ their vision before surgery,” she explained.
Patients can simulate near, intermediate and distance vision and explore options such as multifocal, EDOF or mix-and-match combinations. “Unmet expectations are usually about dysphotopsias, contrast sensitivity and vision in different lighting—things hard to explain but easy to simulate,” she noted.
In a live demonstration on stage, Dr. Ronald Krueger (USA) tested the simulation tool himself using a mix-and-match setup: an EDOF lens in one eye and a trifocal in the other. After comparing them in real time, he selected the EDOF as the better option for his visual needs.
Dr. Filipe emphasized that this approach “enhances shared decision-making, reduces regret and may soon become standard in clinical practice.”
The rise of accommodating
Prof. Dr. Jorge Alió (Spain) took the stage with 18 years of research behind him and a bold message: accommodating IOLs are ready for primetime. At the center of his talk was the Lumina lens (AkkoLens; North Brabant, Netherlands)—a next-generation, dual-optic, sulcusfixated IOL designed to mimic the natural eye.
The Lumina lens, designed around the Arradi principle, dynamically adjusts optical power in response to ciliary muscle activity without splitting light. In Phase III clinical trials, the results were promising: 81% of patients achieved uncorrected visual acuity (UCVA) of 0.7 or better, and 100% showed improved vision with correction. For distance vision, 91% maintained their UCVA at the one-year follow-up, and all patients
achieved a corrected distance visual acuity (CDVA) of 0.8 or better.
The takeaway? Accommodating IOLs like Lumina may finally deliver what previous generations could not: functional vision across distances without compromising optical quality.
Dr. Robert Ang (Philippines) presented a novel, non-lens-based approach to presbyopia correction: laser scleral microporation (LSM) using an erbium YAG laser. The concept is rooted in physiology, targeting age-related scleral stiffening caused by advanced glycation end products. By softening the sclera, LSM aims to restore the natural biomechanics of the ciliary body–zonule–lens system without touching the cornea or lens.
In a study of 50 emmetropic presbyopes (mean age: 52), laser micropores were applied in four scleral quadrants. The results showed significant improvement in intermediate vision and modest gains in near vision (J2–J3) over 12–24 months.
"Our study showed that we have a good intermediate and a modest amount of near vision. It reduced patients' dependence on reading glasses. The most important feature is that we reserve the cornea and the lens for future use, and it improves their quality of life,” Dr. Ang shared.
Dr. Krueger then shared promising early results on laser scleral therapy (LST), a non-invasive presbyopia treatment targeting the real root of the problem—“a stiffening sclera”— not just the lens.
The procedure targets the posterior sclera using a 1.55 µm pulsed diode laser, a wavelength chosen for its safety, precision and deeper tissue penetration without denaturation. “The goal is to shrink and soften tissues and increase compliance of the sclera,” Dr. Krueger explained.
This allows the ciliary body to move more freely, restoring natural accommodation.
In a pilot study of 11 emmetropic subjects aged 44 to 63, all retained their distance vision and gained one to five lines of near vision. One standout case improved from 20/60 to 20/20.
“It was a simple treatment that just took one minute,” he said. While still in early testing, LST shows promise as a repeatable, accessible option in the future.
If this APAO 2025 session made one thing clear, it's this: the era of one-size-fits-all presbyopia solutions is over. From refractive EDOFs and diffractive trifocals to accommodating IOLs and scleral-based laser procedures, the field is moving rapidly toward personalization and physiological restoration. As Dr. Chang put it, “patients want the best of both worlds,” and now, surgeons have more tools than ever to deliver that.
What unites these innovations is their shared goal: restoring function, preserving quality and putting the patient’s lifestyle at the center. Whether through simulation, lens design or scleral restoration, the focus is shifting from managing presbyopia to mastering it. As new technologies mature, the challenge won’t be finding options—it will be choosing the right one for each patient.
Reporting for this story took place during the 40th Congress of the Asia-Pacific Academy of Ophthalmology (APAO 2025), held in conjunction with the 83rd Annual Conference of the All India Ophthalmological Society (AIOC 2025) from 3-6 April in New Delhi, India. A version of this article was first published on cakemagazine.org

Amid a global donor shortage, the pioneering CALEC therapy is transforming corneal regeneration, offering new hope for sight restoration
by Diana Truong
A tiny biopsy, a big breakthrough. From lab-grown limbal cells to xenofree grafts with staying power, CALEC is turning heads—and healing eyes— in the race to restore sight after limbal stem cell loss. Here’s why the future of corneal regeneration might just be cultivated.
In the vast and varied garden of ophthalmology, some tissues bounce back like weeds, while others—once injured—wither away. Limbal stem cells fall into the former category…until they don’t. These tiny powerhouses, tucked into the outer edge of the cornea, usually excel at regenerating the eye’s surface. But when they’re lost to trauma burns or disease, the result—limbal stem cell deficiency (LSCD)—can leave the cornea vulnerable and vision in jeopardy.
Now, a pioneering therapy called CALEC (cultivated autologous limbal epithelial cells) transplantation is offering a glimmer of hope for patients once left with few options. Inside the cornea’s regeneration station
To understand why CALEC is such a breakthrough, it helps to zoom in on the cornea’s finely tuned ecosystem. "The wonderful thing about the cornea is that it has this regenerative ability to keep creating the epithelium,” said Prof. Dr. Sorcha Ni Dhubhghaill, head of ophthalmology at University Hospital Brussels. “The epithelium is a bit like the skin that protects the front of the eye. And every time you blink, you lose a few of those cells."
Enter limbal stem cells, the behindthe-scenes workers responsible for maintaining renewal. Nestled in the limbus, these cells steadily pump out fresh corneal epithelial cells to maintain the eye’s clarity and protection. “We can only reproduce these layers if we’ve got a cell population that keeps growing,” said Prof. Ni Dhubhghaill. “That’s what we call a stem cell population.”
"The wonderful thing about the cornea is that it has this regenerative ability to keep creating the epithelium.”
But these aren’t just any stem cells. Corneal epithelial cells are highly specialized: they must be transparent and protective. “They’re hard to make,” she added. “They need to stay transparent, and they need to protect all the underlying structures.”
The fallout can be dramatic if that stem cell source is damaged. "When you don't have these cells, you end up with an exposed corneal stroma,” Prof. Ni Dhubhghaill explained. “And the corneal stroma is like an Irishman. It's wonderfully
specialized, but it can't look after itself. It needs the epithelium to protect it so it can do the structural work."
From there, two things typically happen, and neither is ideal. First, the eye might try to self-repair by growing conjunctival tissue over the cornea. "But the conjunctiva is not transparent,” she noted. “It will eventually grow blood vessels, and it will have a vascularized appearance, so while it"s protective, it obliterates the functional ability of the cornea.”
The second, more alarming outcome? A total loss of protection that can lead to corneal perforation and, ultimately, loss of the eye.
The journey to treat LSCD has come a long way, from high-stakes risks to high-tech solutions. Back in the day, treatment meant removing a hefty chunk of limbal tissue from a patient’s good eye and transplanting it to the damaged one. It worked, but at a potentially steep cost.
“The problem here is, what if you risk the good eye?” asked Prof. Ni Dhubhghaill. “That's not acceptable to a patient who's already gone through literal trauma. It is very hard to justify risking a good eye in order to help the bad eye."
A major leap forward happened about 15 years ago when a team in Italy, led by Prof. Graziella Pellegrini, flipped the script. Instead of harvesting large amounts of tissue, they took a small biopsy and used cell culture to multiply the limbal stem cells in the lab.
"Rather than run the risk with a very small transplant, they expanded them in culture, grew them in a large number, put them on fibrin layers, and they used co-culture with 3T3 mouse feeder cells to really boost that population of stem cells," explained Prof. Ni Dhubhghaill. This led to the development of Holoclar (Holostem Advanced Therapies; Modena, Italy), one of the first therapies of its kind to be approved by the European Medical Association (EMA).
Holoclar was a big win, but not a perfect one. "You still need one good eye,” she explained. “So, in terms of restoring patients from total blindness, it didn't really do that.But it did improve their worst eye.” Plus, the process was complex and costly, making it a tough sell for many healthcare systems.
Now comes CALEC, the next-gen solution developed by Massachusetts Eye and Ear (USA). Like earlier therapies, CALEC uses a small biopsy from a healthy eye, but with critical upgrades to how the cells are cultivated and transplanted.
One of the standout features?
It’s xeno-free. "That means the elimination of all potential animal products,” explained Prof. Ni Dhubhghaill. “Ten years ago, I used to think, I'm not as worried about animal products as I am worried about human products,’ because, at that time, we weren't really thinking so much about the transition of diseases from animal to human.”
“We think about that a lot now because of what happened with COVID and how we know that it can jump from species,” she added. “So going xeno-free, I think, is a huge advantage of the approach from the [CALEC] group.”
CALEC also swaps out fibrin for amniotic membrane as the cell growth layer—a change that seems to be paying off. "Amniotic membrane is known to be a very beneficial wound healing addition,” Prof. Ni Dhubhghaill noted. “And what we are seeing from their published results is even better outcomes than what we had seen before. They're getting quite high rates of success.”
The CALEC procedure is a carefully choreographed bit of modern medicine. Here’s how it works, according to a detailed write-up in Nature Communications:
It all starts with a tiny limbal biopsy— just one clock hour’s worth—taken from the patient’s healthy eye using only topical anesthesia. This sliver


of tissue is then whisked away in an animal-free solution to the lab, where the real magic begins. 1
In the lab, a two-step manufacturing process takes over. Stage 1 involves growing the limbal cells in plastic until they reach confluency. In Stage 2, the cells are transferred to a deepithelialized amniotic membrane, where they continue to expand until they’re ready to go. 1
Throughout the entire process, these cells are subjected to a rigorous lineup of quality checks, including cell count, viability, phenotype, proliferation and sterility. And just in case, the team makes two CALEC constructs from every biopsy: one for transplant and one for backup. 1
Once the construct is ready, the patient heads into surgery. First, the surgeon removes the fibrovascular pannus from the damaged eye. Then the CALEC graft—carefully trimmed to 17 mm—is sutured to the limbus using fine 10-0 nylon stitches. A bandage contact lens is placed over the eye, and the patient starts a course of preservative-free antibiotics, steroids and serum tears to support healing. 1
The Phase I/II clinical trial of CALEC, conducted at Massachusetts Eye and Ear, delivered some eyecatching results. Between 2016 and 2021, 15 participants with unilateral LSCD were enrolled, and 14 of them received CALEC grafts. 1
The main focus was on feasibility and safety, and the big question
was: could a tiny biopsy reliably yield a viable graft? The answer was a resounding yes. Ninety-three percent (14 out of 15) of biopsies passed quality control and were deemed transplant ready. 1
As for safety, the news was equally reassuring. Only one major complication occurred in a recipient’s eye: a bacterial infection eight months post-op, linked to long-term contact lens wear, not the CALEC itself. No serious issues arose in any of the donor or recipient eyes. 1
On the efficacy front, results were encouraging. By the three-month mark, half of the participants had already achieved “complete success”—defined as a major improvement in the corneal surface. That figure rose to 79% at 12 months and held steady at 77% by 18 months. When including cases of “partial success” (reduced vascularization or symptom relief), overall success rates hit 86%, 93% and 92% at 3, 12 and 18 months, respectively. 1
As Prof. Ni Dhubhghaill put it, “This is very encouraging because these are some of the most notoriously difficult patients to treat. So any subsequent improvement on the previous knowledge is always welcome, and it is very encouraging that there is further evolution in the field.”
That said, even promising treatments come with their share of hurdles. One big unknown is durability. “The big question for us and for everybody in the field is how long will it last?” Prof. Ni Dhubhghaill noted. The 18-month

results are hopeful, but longer-term data will be key in determining how well these grafts hold up over time.
Then there’s the issue of the stem cell niche. In a healthy eye, limbal stem cells live in a protected threedimensional structure, like VIPs in a private suite. But the CALEC graft sits exposed on the cornea, which means these stem cells may take more wear and tear than nature intended, raising concerns about their long-term survival.
“The big question for us and for everybody in the field is how long will it last?”
CALEC also isn’t a one-size-fitsall solution. It’s currently limited to patients with one healthy eye to donate tissue, ruling it out for those with bilateral LSCD. Plus, the manufacturing process is no walk in the park. It requires specialized labs and skille personnel, which may limit widespread accessibility.
Cost is another consideration. While CALEC may be more affordable than Holoclar, it’s still a complex process. As Prof. Ni Dhubhghaill pointed out, the treatment must ultimately prove to be cost-effective to remain viable in the long run.
And let’s not forget the clock. Once the final CALEC product is ready, there’s a 24-hour window to get it surgically implanted. That tight turnaround can pose logistical challenges, especially in places where coordination between the lab and operating room isn’t exactly seamless.
With the Phase I/II trial of CALEC showing such encouraging results, the road ahead is looking wide open for researchers. A number of exciting possibilities are already on th table.
One of the biggest next steps is exploring allogeneic approaches, using donor cells instead of the patient’s own. This could be a game changer for people with bilateral LSCD. As Dr. Jerome Ritz, executive director of the Connell-O’Reilly Cell Manipulation Core Facility (CMCF), put it in a news release, “Our future hope is to set up an allogeneic manufacturing process starting with limbal stem cells from a normal cadaveric donor eye.” If successful, this approach could dramatically expand CALEC’s reach. 2
Another focus is extending the shelf life of CALEC grafts. Right now, the grafts must be transplanted within 24 hours of manufacture, which is not exactly ideal for shipping or scheduling. Developing preservation methods to keep these cells viable for longer would give surgeons more flexibility and patients more access.
Then there’s the need for larger, randomized trials. While the early data are promising, studies involving more patients across multiple centers will help fine-tune outcomes and uncover what factors predict success (or signal trouble).
“Our future hope is to set up an allogeneic manufacturing process starting with limbal stem cells from a normal cadaveric donor eye.”
Though CALEC isn’t quite ready for prime time, it’s already casting a long shadow of promise across the corneal surgery landscape.
For patients with unilateral LSCD who haven’t responded to traditional treatments, CALEC offers something that’s been in short supply: genuine hope. With its high success rates and stellar safety profile in clinical trials, CALEC could soon become a powerful new tool in the corneal surgeon’s kit.
But it’s not just about patching things up. By restoring a healthy ocular surface, CALEC may make previously ineligible patients viable candidates for corneal transplantation—essentially giving them a second shot at sight. That’s no small feat fo a condition as stubborn as LSCD.
Perhaps most significantly, CALEC signals a major shift in how we treat severe corneal damage. Instead of simply managing symptoms, we’re stepping into the realm of true regenerative therapy, where the goal isn’t just comfort, but actual healing.
edge experiment to mainstream solution. In the ever-growing garden of ophthalmologic innovation, CALEC is a bold new bloom—one that just might bear life-changing fruit.
1. Jurkunas UV, Kaufman AR, Yin J, et al. Cultivated autologous limbal epithelial cell (CALEC) transplantation for limbal stem cell deficiency: A Phase I/II clinical trial of the first xenobiotic-free, serum-free, antibiotic-free manufacturing protocol developed in the US. Nat Commun. 2025;16:1607.
2. Novel Stem Cell Therapy Repairs Irreversible Corneal Damage in Clinical Trial. Mass General Brigham. March 4, 2025. Available at:https:// www.massgeneralbrigham.org/en/about/ newsroom/press-releases/calec-stem-celltherapy-clinical-trial-repairs-corneal-damage . Accessed on June 6, 2025.

Think of CALEC as the ophthalmologist’s version of propagating a plant from a cutting. By taking just a sliver of limbal stem cells from a healthy eye and coaxing it to grow into transplantable tissue, the procedure is essentially gardening at the cellular level— and early results show it works beautifully.
Sure, there are still weeds to pull. Long-term durability remains an open question, the manufacturing process is complex, and it currently can’t help patients with bilateral LSCD. But even with those caveats, the success of CALEC marks a leap forward in the field of corneal regenerative medicine.
As Prof. Ni Dhubhghaill put it, “I think the approach and the success rates are very, very encouraging.” And she’s not alone. As research continues and larger trials unfold, CALEC may evolve from a cutting-
Prof. Sorcha Ní Dhubhghaill is an Irish-American ophthalmologist based in Antwerp and Brussels, fluent in English, Irish and Dutch. She earned her medical degrees (MB, BCh, BA with first-class honors in ophthalmology) from Trinity College Dublin in 2005 and completed a PhD in ophthalmology in 2012, focusing on genetic and environmental factors in agerelated macular degeneration. She received advanced surgical leadership training at Harvard Medical School in 2021–22. Since August 2023, she has served as Chair of Ophthalmology at UZ Brussels (VUB), following senior roles at Antwerp University Hospital (2015–2023) and a corneal surgeon position at NIIOS (2018–19). A prolific educator, she has taught numerous wet labs across Europe and held editorial roles in major ophthalmology journals. Her research spans clinical trials in corneal stem-cell therapy, endothelial keratoplasty and bag-in-the-lens cataract techniques. She’s also a recognized leader in European ophthalmology societies and recipient of awards like the ESCRS gold and Eithne Walls Memorial prize.
nidhubhs@gmail.com

Assoc. Prof. Yu-Chi Liu is redefining ophthalmology through groundbreaking research, compassionate care and global educational leadership
by Chow Ee-Tan
From pioneering corneal imaging to mentoring the next generation of ophthalmologists, clinician-scientist Assoc. Prof. Yu-Chi Liu’s work is redefining the calling of an ophthalmologist. She is transforming eye care through cutting-edge research, global collaboration and compassionate patient care.
In ophthalmology, few professionals embody the fusion of cutting-edge science, patientcentered care and educational leadership as effectively as Assoc. Prof. Yu-Chi Liu. A highly respected clinician-scientist, researcher and educator, Assoc. Prof. Liu has carved out a career defined by innovation, excellence and impact— not just in her homeland Singapore but internationally.
This year, she was named one of the Asia-Pacific’s Top 100 Ophthalmologists by the Asia-Pacific Academy of Ophthalmology—an honor that celebrates the most influential and inspiring figures in the field. For Assoc. Prof. Liu, this award is more than personal recognition.
“It’s a meaningful encouragement,” she shared. “This recognition highlights the contributions of the mentors, colleagues and team members who have supported me. It motivates me to keep striving for advancements that improve lives.”

A corneal specialist, Assoc. Prof. Liu holds multiple prominent positions. She serves as a clinicianscientist in the Cornea and External Eye Diseases Department at the Singapore National Eye Centre (SNEC), co-head of Regenerative Medicine and principal investigator at the Singapore Eye Research Institute (SERI), associate professor at DukeNUS Medical School, and adjunct associate professor at National Taiwan University.
Her work spans patient care, research and teaching—forming an interconnected ecosystem that keeps her constantly engaged in improving the standard of eye care.
Despite a demanding schedule, she believes each role strengthens the other. “Being a clinician helps me understand what patients truly need. That insight becomes the foundation for my research. And in turn, my research contributes directly back to patient care,” she explained.
From top of her class to top of the field
Raised in a medical household—her father is a physician—Assoc. Prof. Liu was immersed in healthcare from a young age. But it was the intricacies of ophthalmology that truly captivated her.
“Ophthalmology combines the precision of microsurgery with rapidly advancing technology,” she noted. “It offers the rare chance to make an immediate and lifechanging impact on a person’s vision and quality of life.”
Her journey in ophthalmology was paved with excellence and distinctions. She graduated among the top five in her class from Taipei Medical University, receiving the Excellent Scholarship. Her early promise blossomed into a career marked by awards, innovation and leadership.
Notably, she has been ranked among the World’s Top 2% Scientists (2022, 2023 and 2024) by Stanford University and Elsevier—a reflection of her research output, citations
and influence in the scientific community.
“Ophthalmology combines the precision of microsurgery with rapidly advancing technology. It offers the rare chance to make an immediate and life-changing impact on a person’s vision and quality of life.”
In 2021 and 2024, she received the Clinician Scientist Award from Singapore’s National Medical Research Council (NMRC). This prestigious grant supports highpotential clinician-scientists in conducting translational research that bridges lab discoveries and clinical applications.
“The path of a clinician-scientist is often challenging, requiring a balance between patient care, research, teaching and mentorship,” she said. “To have my research recognized on an international scale is both humbling and motivating. I see it as a shared success and a reminder of the impact we can work together to make the medical field better.
Receiving such accolades has indeed opened up doors and allowed her to scale her work globally, connecting with other leading researchers and helping position Singapore at the forefront of ophthalmic innovation.
Assoc. Prof. Liu’s research focuses on corneal neuropathy and neuropathic corneal pain—areas that are often underrecognized yet have a significant impact on quality of life. Her team at SERI is leading the way with novel diagnostic tools and therapeutic strategies.
Corneal diseases or ocular surface diseases are very common. In recent years, there have been several exciting developments in this field, such as regenerative therapy, cell
therapy, imaging modality and artificial intelligence (AI) technology in improving the diagnosis.
“My clinical expertise and research focus on corneal neuropathy and neuropathic corneal pain. We have breakthrough corneal imaging modality, i.e., wide-field corneal nerve imaging, which allows for more accurate disease monitoring for patients with corneal neuropathy. We also discovered a few drug candidates that can promote corneal nerve regeneration. Additionally, we built up several AI algorithms that utilize corneal nerve images and multi-modal data to predict patients’ diabetic complications such as


diabetic retinopathy and diabetic foot,” she elaborated.
Corneal and external eye diseases are among the most common ocular conditions—but many are highly treatable. “Whether through surgery, regenerative therapy or medication, restoring vision is one of the most rewarding aspects of my work,” she said.
Her excitement about the field is palpable. “We’re seeing rapid advances—cell therapy, imaging technologies, AI integration. It’s an incredibly dynamic and hopeful time to be working in this space.”
A passionate educator, Assoc. Prof. Liu views teaching and mentorship as essential pillars of academic medicine. She mentors numerous young clinicians and researchers, helping shape the future of ophthalmology in Asia and beyond.
“Mentorship is a privilege. Seeing junior doctors and scientists grow into confident, capable leaders gives me immense satisfaction,” she shared. “Education ensures the sustainability of progress in medicine.”
Her mentorship extends beyond the classroom—she serves on numerous committees, boards and professional associations across the Asia-Pacific region and globally. These roles allow her to influence the direction of ophthalmology, foster cross-border innovation and promote best practices in clinical care and research.
She views leadership not just as responsibility, but as service—to patients, science and the next generation.
As a clinician-scientist, it is often challenging to maintain excellence across clinical care, research, teaching and leadership—as each area demands time, focus and dedication, admitted Assoc. Prof. Liu.
“Early in my career, I struggled with prioritization and time management. I overcame this by learning to set clear boundaries, delegate when appropriate and plan strategically. I also sought advice from mentors and colleagues who had successfully navigated similar paths,” she shared.
Securing funding and maintaining research momentum amid growing competition is another constant hurdle. “I focus on building strong collaborative networks—both locally and internationally—and by staying persistent and adaptative,” she said.
What keeps her going is a deep sense of purpose in what she does. “This work allows me to make a real difference— whether by helping a patient see again or mentoring someone who will shape the future of ophthalmology.”
a legacy that improves lives,” she elaborated.
Despite her impressive list of accomplishments, she remains grounded. “I’ve learned that kindness is the greatest wisdom. At the end of the day, it’s human relationships— not awards or recognition—that truly matter,” she concluded.

So despite the pressures, she knows that “at the end of the day, it’s about making a difference—whether it’s in a lab, an operating room or a lecture hall.”
Looking back, Assoc. Prof. Liu attributes her accomplishments not just to hard work, but to the people around her. She’s deeply grateful for the support of mentors and collaborators. To her, everything she has achieved is part of a collective effort.
And looking ahead, she remains energized by the opportunities to grow, lead and contribute. “What brings me the most fulfillment is translating research into better care, and watching young clinicians evolve and succeed,” she enthused.
It is not surprising that for Assoc. Prof. Liu, success is not measured by titles or publication count, but by meaningful impact. “A truly successful ophthalmologist isn’t just clinically skilled or academically accomplished. They also care deeply about their patients, contribute to advancing medical science and mentor others. It’s about leaving
Assoc. Prof. Yu-Chi Liu is currently a clinician and clinician-scientist at the Department of Cornea and External Eye Disease, Singapore National Eye Centre. She is also the co-head of Regenerative Therapy Group, Singapore Eye Research Institute; an associate professor of Ophthalmology and Visual Sciences at Duke National University of Singapore (DukeNUS), Singapore; as well as an adjunct associate professor at National Taiwan University. Assoc. Prof. Liu has published 157 peer-reviewed papers, and she is the first or last author in more than half of these publications (69/143). She published two papers in prestigious journals: The Lancet and The Lancet Respiratory Medicine, as the first author. She has been successful in obtaining national research funding, with a total funding amount of 6.5 million Singapore dollars. She has won 19 awards both nationally and internationally, and her clinical and research work is internationally recognized. She is on the Advisory Board of American Academy of Ophthalmology, Global Ophthalmology. She is the editor of seven journals and contributed to seven book chapters. She is regularly invited to major international conferences to chair the scientific sessions or to present her clinical or research work.
liu.yu.chi@duke-nus.edu.sg

by Diana Truong
When it comes to cataract surgery, DED is the pesky villain that threatens precision and patient comfort. Savvy ophthalmologists are now giving the ocular surface a little backstage TLC before the grand performance. Here’s why a little pre-surgery prep can make all the difference.
In today’s precision-driven world of cataract surgery, the ocular surface plays the unsung hero— and dry eye disease (DED) is the villain waiting in the wings. Picture the eye as a camera lens on a highstakes film set: if it’s not crystal clear and perfectly calibrated, the final shot won’t be Oscar-worthy.
With patient expectations on the rise—especially when it comes to premium intraocular lenses (IOLs), ophthalmologists are stepping into the director’s chair, ensuring the ocular surface is prepped, polished and ready for its close-up.
The sneaky saboteur
Dry eye often flies under the radar, especially in cataract patients.
According to Dr. Bennie Jeng, chair of the Department of Ophthalmology and director of the Scheie Eye Institute at Penn Medicine, many cases are hiding in plain sight. “I would say half of my patients who ‘look’ fine on referral turn out to have some degree of dry eye,” he said.
“I would say half of my patients who ‘look’ fine on referral turn out to have some degree of dry eye.”
- Dr. Bennie Jeng
That’s no small number. Studies suggest that 50% to 70% of cataract patients show signs of DED, depending on the diagnostic method.1-2 What’s more, about 46% of these patients don’t even realize they have symptoms, yet clinical testing tells a different story.2
If dry eye goes untreated, it can create two major problems during cataract surgery: biometry and patient comfort. As Dr. Jeng pointed out, “If they are not optimized from a dry eye standpoint, they will be even more symptomatic after surgery.
Research backs this up. Studies have shown that patients with hyperosmolar tears (a marker of dry eye) show greater variability in keratometry readings—the measurements that determine IOL power.3-4 This variability can lead to errors in astigmatism calculation and IOL power selection, potentially resulting in less-than-perfect vision after surgery.
So what’s the best way to manage DED ahead of surgery? Dr. Jeng sticks to a standard dry eye treatment protocol and doesn’t schedule surgery until the eye is in top condition. “They can’t be cured, but

they need to be in their best possible shape,” he explained.
“Aside from routine history taking and dry eye tests, we perform wavefront aberrometry to evaluate the ocular surface.”
- Dr. Harvey Uy
For patients receiving premium IOLs, Dr. Harvey Uy from the University of the Philippines takes it a step further. “Aside from routine history taking and dry eye tests, we perform wavefront aberrometry to evaluate the ocular surface,” he noted. “If there is evidence of dry eyes such as higher order aberrations (HOAs), we initiate treatment with multi-targeted lubricants and cyclosporine drops.”
The toolbox for managing DED has expanded significantly in recent years, offering multiple solutions to address various aspects of the condition
First-line treatments include artificial tears and lubricants, which help replenish poor lacrimal gland secretion and stabilize the tear film. Punctal plugs, another nonprescription option, block the tear drainage system to keep tears on the eye’s surface longer.
Prescription treatments like cyclosporine help reduce inflammation and boost tear production, while Lifitegrast (Xiidra; Bausch + Lomb; Laval, Canada) works by blocking T-cell activation and inflammatory cytokine release associated with dry eye.
For more severe cases, thermal pulsation technologies like LipiFlow (Johnson & Johnson; Florida, USA), iLux (Alcon; Geneva, Switzerland), and TearCare (Sight Sciences; California, USA) apply controlled heat to the eyelids to improve meibomian gland function. Additionally, intense pulsed light (IPL) therapy is a newer option that reduces inflammation and
gland function.
The future of dry eye treatment looks promising. Miebo (perfluorohexyloctane; Bausch + Lomb) is the first FDA-approved medication specifically for dry eye associated with meibomian gland dysfunction (MGD). XDEMVY (lotilaner; Tarsus Pharmaceuticals; California, USA) targets Demodex mites, which can contribute to eyelid inflammation, while Tyrvaya (varenicline; Oyster Point Pharma; New Jersey, USA) is a nasal spray that stimulates natural tear production.
Reproxalap (Aldeyra Therapeutics; Massachusetts, USA), currently awaiting FDA approval, shows promise for treating both dry eye and allergic conjunctivitis with its antiinflammatory properties.
While DED is the most common ocular surface issue that affects cataract surgery outcomes, other conditions require attention as well. Epithelial basement membrane dystrophy (EBMD), a common corneal condition, can cause irregular astigmatism and visual disturbances, potentially affecting preoperative measurements.
Salzmann's nodular degeneration (SND), which leads to corneal opacities, can also introduce
irregularities that impact topography readings. Pterygia, fibrovascular growths on the conjunctiva, typically induce with-the-rule astigmatism, which can affect biometry as well.
These conditions often require surgical intervention and adequate healing time before cataract surgery can proceed.
Timing is everything
Patience is key when optimizing the ocular surface. "We ask that patients return for repeat evaluation of DED. Once symptoms, clinic exam and HOA normalize, we then perform biometry,” Dr. Uy explained.
For most ocular surface treatments, a waiting period of four to eight weeks is typically recommended before taking final measurements for cataract surgery.5 This allows the corneal surface to stabilize and ensures more accurate biometry readings.
Integrating ocular surface optimization into a busy surgical practice requires efficiency. "Have a protocol for the techs of what to do and what NOT to do,” Dr. Jeng advised. “I check sensation and staining myself, for example."
Practical strategies also include implementing a standardized screening protocol for all cataract surgery candidates and taking

multiple sets of measurements after treatment to verify consistency. Comparing measurements across different devices ensures accuracy, while noting discrepancies between eyes or marked changes in measurements before and after treatment can reveal ongoing surface issues.
Setting realistic timelines and explaining the possibility of staged procedures upfront can also help manage patient expectations.
Set expectations early
It’s vital to discuss the potential impact of dry eye on surgery with patients before the procedure. "You must discuss the above issues BEFORE surgery,” Dr. Jeng emphasized.
Clear communication around the chronic nature of DED, its effects on surgical

Contributors
accuracy, and the importance of ongoing treatment—especially postop—is essential. Patients should understand that even if their vision reaches 20/20, untreated dry eye can still affect how sharp and comfortable their vision feels.
In the end, preparing the ocular surface for cataract surgery is like setting the stage for a flawless performance. Tackling dry eye and other surface issues ahead of time ensures everything runs smoothly, leading to clearer, more comfortable vision after the procedure. It’s all about taking the time to get it right, so when the curtain rises, the results are nothing short of stellar.

Dr. Harvey S. Uy is a clinical associate professor of ophthalmology at the University of the Philippines, and medical director at the Peregrine Eye and Laser Institute in Makati, Philippines. He completed his fellowships at St. Luke’s Medical Center (Philippines) and the Massachusetts Eye and Ear Infirmary (USA). Dr. Uy is a pioneer in femtosecond cataract surgery, accommodation restoration by lens softening, modular intraocular lenses and intravitreal drugs. He has published over 30 peerreviewed articles and is on the editorial board of the American Journal of Ophthalmology Case Reports. He is a former president of the Philippine Academy of Ophthalmology (PAO) and current council member of the APVRS.
harveyuy@gmail.com
Dr. Bennie H. Jeng, MD, MS , is the William F. Norris and George E. de Schweinitz Professor and Chair of the Department of Ophthalmology, and director of the Scheie Eye Institute, of the University of Pennsylvania Perelman School of Medicine. He earned his bachelor’s degree summa cum laude from Washington University in St. Louis and his M.D. from the University of Pennsylvania School of Medicine. He then completed his ophthalmology residency and chief residency at the Cole Eye Institute of the Cleveland Clinic, which was followed by a fellowship in cornea and external diseases at the Francis I. Proctor Foundation/University of California San Francisco (UCSF) in 2003. He earned his Master’s degree in Clinical Investigation from Case Western Reserve University. He subsequently returned to Proctor/UCSF as an Associate Professor and then Full Professor, where he served as co-director of the UCSF cornea service, Director of the Proctor/ UCSF Cornea Fellowship program, and Chief of Ophthalmology at the San Francisco General Hospital. In 2013, Dr. Jeng began his tenure
1. Gupta PK, Drinkwater OJ, VanDusen KW, et al. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refract Surg. 2018;44:1090-1096.
2. Trattler WB, Majmudar PA, Donnenfeld ED, et al. The prospective health assessment of cataract patients' ocular surface (PHACO) study: The effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
3. Nilsen C, Gundersen M, Graae Jensen P, et al. The significance of dry eye signs on preoperative keratometry measurements in patients scheduled for cataract surgery. Clin Ophthalmol. 2024;18:151-161.
4. Epitropoulos AT, Matossian C, Berdy GJ, et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J. Cataract Refractive Surg. 2015;41:16721677.
5. Venkateswaran N, Luna RD, Gupta PK. Ocular surface optimization before cataract surgery. Saudi J Ophthalmol. 2022;36(2):142-148.
as Chair of the Department of Ophthalmology and Visual Sciences at the University of Maryland School of Medicine where he served for nearly nine years. He assumed his current position in 2022. Dr. Jeng is actively involved in the leadership of many of our ophthalmologic societies, including as a member of the Board of Trustees of the American Academy of Ophthalmology (as the Secretary for the Annual Meeting). He is also the Immediate Past-President of the Cornea Society, as well as a Past-President of the Eye and Contact Lens Association. Dr. Jeng has published over 140 peer-reviewed journal articles and 30 book chapters, and he has delivered nearly 500 invited lectures nationally and internationally. He currently serves as an associate editor for Ophthalmology, a senior editor for Cornea, and an editorial board member of several other journals. He is also the inaugural editor-inchief of Cornea Open, which is the official open access journal of the Cornea Society.
bennie.jeng@pennmedicine. upenn.edu


by Elif Uslu
From the gritty discomfort of dry eyes to the sightthreatening urgency of infectious keratitis, the corneal surface is a battleground that many ophthalmologists navigate daily. While these conditions may appear routine, they often hide complexity beneath the surface—and the key to managing them lies in understanding their nuances.
To shed light on what works in real-world practice, we spoke to four corneal disease experts: Dr. Artemis Matsou (United Kingdom), Dr. Ugur Tunc (Turkey), Prof. Dr. Farhad Hafezi (Switzerland) and Dr. Sneha Makhija (India). Together, they offered pearls of wisdom on tackling the most common corneal surface diseases: dry eye disease (DED), allergic keratoconjunctivitis, infectious keratitis, pterygium and contact lens–related complications.
Let’s take a closer look at their practical tips and go-to strategies— straight from the clinic’s front lines.
It may be one of the most frequent complaints in eye clinics, but DED is anything but simple. And when it comes to treatment, one size definitely doesn’t fit all.
"The most important lesson I’ve learned is that dry eye isn’t ‘just dry eye.’ It’s multifactorial and deeply individual," shared Dr. Matsou. "I always try to identify the dominant subtype—meibomian gland dysfunction (MGD), aqueousdeficient, inflammatory, neurotrophic, evaporative from poor blink—and match the treatment to that.”
Dr. Makhija keeps it simple yet sharp. “I check the lid margins, meibomian glands and lashes, and also assess for lid laxity. Issues like meibomian gland dysfunction or subtle blepharitis can easily go unnoticed unless you really look for them. I always ask about systemic symptoms—sometimes a bit of joint pain or fatigue can be the clue that leads you to an underlying autoimmune disease like Sjögren’s or Rheumatoid arthritis,” she explained.
According to Dr. Tunc, targeting inflammation is key. "I quiet the surface with a short, gentle pulse of topical steroid, then hand off to twicedaily cyclosporine A 0.05% for longterm immune modulation, all layered over preservative-free artificial tears for baseline lubrication,” he said.
Dr. Matsou layers therapy depending on the case: "In chronic cases, I usually layer therapy: preservativefree lubricants, anti-inflammatories (I use cyclosporine drops a lot), punctal plugs and lifestyle tweaks,” she noted.
Dr. Hafezi emphasizes surface safety. "I start with preservative-free artificial tears to avoid further damage to the ocular surface, as chronic preservative exposure is a known exacerbating factor,” he said.
They all agree on one thing: patient education and compliance make all the difference. “Overall, I feel patient education is the real game-changer;
once patients understand what dry eye is about, they become much more engaged in their care, and the results follow,” said Dr. Matsou.
Managing allergic eye disease is all about balance—relieving the acute misery while keeping long-term inflammation under control.
Dr. Tunc’s first-line approach is straightforward yet multifaceted. “Start with preservative-free artificial tears to rinse away pollen, add a potent dual-action antihistamine/ mast-cell stabilizer drop for fast relief, and use an oral antihistamine if the nose is acting up too,” he explained. “If symptoms still break through, I’ll calm the flare with a brief taper of low-dose loteprednol, then hand the baton to twice-daily topical cyclosporine.”
Dr. Matsou who often sees more advanced cases usually starts with a preservative-free dual-action antihistamine. “But I usually have to escalate to anti-inflammatory treatments with steroids or steroid-sparing agents like topical cyclosporine or tacrolimus ointment,” she shared.
For Dr. Makhija, tacrolimus is the ace up her sleeve. “In moderate to severe cases, I find that a combination of a topical steroid with tacrolimus ointment works best. I usually start with a mild steroid like loteprednol, dosing it four to six times a day
depending on how active the disease is, and then taper it weekly. At the same time, I introduce topical tacrolimus, especially in patients who have frequent flares or are steroiddependent,” she explained.
“Start with preservative-free artificial tears to rinse away pollen, add a potent dual-action antihistamine/ mast-cell stabilizer drop for fast relief, and use an oral antihistamine if the nose is acting up too.”
- Assoc. Prof. Ugur Tunc
Steroids can help—but they demand caution. “Topical dual-action antihistamine-mast cell stabilizers are first-line,” noted Dr. Hafezi. “In recalcitrant or chronic forms such as vernal keratoconjunctivitis, we escalate to topical corticosteroids with caution, and in some cases, cyclosporine or tacrolimus formulations.”
Counseling on allergen avoidance is just as critical. Dr. Tunc shared practical steps like showering before bed to wash away pollen, frequent

laundry, and using air purifiers. Dr. Hafezi emphasized minimizing exposure with wraparound glasses and HEPA filtration, while Dr. Makhija said she reminds patients to “never rub the eyes—no matter how bad the itch gets!”
Infectious keratitis is a race against time, where rapid diagnosis and targeted therapy can save vision—or let it slip away
"I start fortified dual therapy with vancomycin and gentamicin hourly, even before culture results are back," said Dr. Matsou. "It covers a broad range of gram-positive and gramnegative organisms and gives us the best shot at stabilizing the infection early.
Meanwhile, Dr. Tunc takes no chances. "No matter the organism, I pair aggressive topical therapy with oral doxycycline 100 mg BID (matrix-metalloproteinase blockade) and a cycloplegic for comfort. Daily photos at the slit lamp let me spot the first hint of melt or expansion so I can escalate—amniotic membrane, glue, or even a therapeutic graft— before the cornea is in real danger,” he explained.
But what about those tricky atypical infections? Dr. Hafezi shared a cutting-edge approach. “Our group has defined and validated highfluence PACK-CXL protocols that maximize bacterial killing,” he said. “Specifically, we demonstrated that increasing total fluence up to 15 J/ cm² using UV-A light (365 nm) in combination with 0.1% riboflavin can achieve bacterial killing ratios above 90% for Staphylococcus aureus and Pseudomonas.”
For atypical or treatment-resistant keratitis, Dr. Matsou said she frequently manages these infections in patients with corneal grafts, where the stakes are even higher. “My approach involves early and repeated corneal scraping or debridement to reduce microbial load and improve penetration,” she noted. “I also regularly use anterior segment OCT or confocal microscopy not only for diagnosis but to track depth of infiltration and evaluate treatment response.”

When it comes to reducing scarring, Dr. Makhija knows timing is everything. “In complex cases, especially those with deep stromal involvement or delayed presentation, I’ve found that judicious use of topical corticosteroids once the infection is under control can significantly help reduce scarring. The key is timing. I wait until the epithelium has healed and there’s no active infiltrate before introducing a mild steroid like loteprednol under close monitoring.”
Sun damage may be subtle at first, but over time, it can leave a permanent mark on the ocular surface. The real challenge? Preventing recurrence after removal.
“We educate patients that UV exposure is the primary risk factor for recurrence and recommend consistent UV-blocking eyewear with lateral shielding to avoid the Coroneo effect,”
- Prof. Farhad Hafezi
Dr. Matsou relies on a strong foundation. "My standard approach is conjunctival autografting with fibrin glue,” she shared. “In eyes
with high recurrence risk, I also apply low-dose intraoperative mitomycin C (typically 0.02%) for a short exposure time applied carefully to avoid scleral thinning. I sometimes combine the autograft with an amniotic membrane overlay or a more extensive conjunctival dissection to better restore the ocular surface architecture and reduce fibrovascular regrowth. I have also used intralesional 5-fluorouracil (5-FU) in select cases.
Dr. Tunc couldn’t agree more. "When I’m dealing with a regrowth, I add a two-minute soak of 0.02 % mitomycin C before the conjunctival autograft; that quick antimetabolite bath tames fibroblast rebound without appreciable toxicity. Finally, I prescribe a six-week loteprednol 0.5 % taper and insist on lifelong UV defense,” he said.
We avoid bare sclera techniques and favor conjunctival autografting.”
Above all else, prevention is key. “We educate patients that UV exposure is the primary risk factor for recurrence and recommend consistent UV-blocking eyewear with lateral shielding to avoid the Coroneo effect,” highlighted Dr. Hafezi.
Contact lenses are marvels of modern vision correction—but 5
Contact lens–related corneal complications

Dr. Makhija put something else in the spotlight. “I haven’t needed mitomycin C yet, but in recurrent cases, I always take a detailed history—was the first surgery a bare sclera technique? Did they have prior conjunctival autografting? Sometimes, it’s a pseudopterygium, especially in chemical injury patients,” she noted.
Meanwhile, Dr. Hafezi observed: "Recurrence is minimized by PTK smoothing of the corneal surface following surgical pterygium excision.

Prof. Farhad Hafezi, MD, PhD, FARVO, is a globally recognized ophthalmic surgeon and ocular cell biologist. He serves as medical and scientific director of the ELZA Institute in Dietikon and Zurich, Switzerland. He is also a professor of Ophthalmology at the University of Geneva; an adjunct clinical professor at the Keck School of Medicine, University of Southern California (Los Angeles, USA); a visiting professor at Wenzhou Medical University (China); and a research professor at NYU Grossman School of Medicine (New York, USA). Additionally, he leads the Ocular Cell Biology Group at the Center for Applied Biotechnology and Molecular Medicine (CABMM), University of Zurich. Prof. Hafezi has authored over 260 peerreviewed publications in journals including Nature Medicine, Nature Genetics, Investigative Ophthalmology & Visual Science and Ophthalmology. He is coinventor of the EMAGine C-eye device for slit-lamp-based CXL and has developed several advanced protocols for corneal cross-linking, including ELZA-PACE (personalized accelerated CXL), ELZA-sub400 for thin corneas, and PACK-CXL for treating infectious keratitis. He was also involved in developing Femto-/ ECO-CAIRS and AI tools for early keratoconus detection.
farhad.hafezi@elza-institute.com
they’re also a gateway to some of the most preventable corneal disasters.
Dr. Tunc shared his go-to approach. "Step one is ‘lenses out, cultures in.’ I remove the lens, scrape the leading edge of the infiltrate for Gram stain/PCR and send the lens case for culture. While the lab works, I launch hourly moxifloxacin 0.5 %; it hits most bacterial culprits linked to soft-lens wear, including Pseudomonas. If the ulcer is larger than 3 mm, central, or the patient has only one good eye, I escalate to alternating fortified vancomycin 25 mg/mL and cefazolin 50 mg/mL every 30 minutes for the first 48 hours,” he explained.

Dr. Artemis Matsou, MD, MRCP (UK), FEBOS-CR, FEBO, PgDip CRS, is a consultant ophthalmologist and cataract lead at the Queen Victoria Hospital, specializing in cornea, complex cataract and refractive surgery. Her clinical interests include ocular surface reconstruction and limbal stem cell transplantation. She has completed two prestigious Corneal Fellowships at Addenbrooke’s Hospital in Cambridge and Queen Victoria Hospital in East Grinstead. She holds advanced accreditation in cataract and refractive surgery from the European Board of Ophthalmology (FEBOS-CR), is a Fellow of the European Board of Ophthalmology (FEBO) and a Member of the Royal College of Physicians of London (MRCP). Dr. Matsou serves on the Education, Business & Leadership, and Diversity, Equity & Inclusion Committees of the European Society of Cataract and Refractive Surgeons (ESCRS). She also sits on the Councils of the Medical Contact Lens and Ocular Surface Association (MCLOSA) and the European School for Advanced Studies in Ophthalmology (ESASO).
Artemis.matsou1@nhs.net
For Dr. Matsou, she finds it most valuable to not hesitate to involve microbiology early, to re-scrape if things aren’t improving, and to use confocal microscopy when the picture doesn’t add up. “I keep a mental list of red flags— disproportionate pain, ring infiltrates, irregular epithelium, or radial perineuritis—that pushes me to treat more aggressively or broaden the antimicrobial cover,” she shared.
As for Dr. Makhija, it’s all about digging into lens habits. “I take a detailed lens history—hygiene practices, overnight wear, lens type, use of over-the-counter cosmetic lenses to identify contributing factors,” she said.

Assoc. Prof. Ugur Tunc, MD, is a young ophthalmologist devoted to unraveling the mysteries of the cornea and ocular surface. After completing his residency at Istanbul Beyoğlu Eye Hospital in 2021, he began investigating how ocular microbial communities influence ocular surface and corneal disorders, focusing on the connections among dysbiosis, ocular immunity and corneal disease. Between 2023 and 2024, he served as a research fellow at the Johns Hopkins Wilmer Eye Institute, where he expanded his expertise in advanced dry eye syndromes, Sjögren’s disease and ocular rosacea. Currently, he serves on the faculty at Istanbul Medipol University, leading ocular microbiome projects and collaborating with international teams exploring the eye’s microbial ecology. Clinically, he specializes in ocular surface disease as well as cataract and refractive surgery, while mentoring the next generation of physicians to think critically and embrace sciencedriven care.
ugur.tunc@medipol.com.tr
Dr. Tunc believes in showing, not just telling, by using digital reminders and educational videos. "Under the slit-lamp camera I zoom in on the ulcer or staining and let them see the damage," he shared. "Combining visceral visuals, bite-sized digital reminders, and a little friendly competition turns good lens care into a habit.”
For prevention, active counseling is essential. "I use every opportunity to reframe lenses as medical devices, not just lifestyle accessories,” said Dr. Matsou.
Dr. Hafezi echoed the importance of education. "We counsel on strict hygiene, daily lens replacement where possible, and avoiding overnight wear. Patient understanding of the consequences is crucial for adherence,” he noted.
In the end, it’s not just about treating the problem—it’s about preventing the next one in every eye disease.

Dr. Sneha Makhija Shah, MBBS, DO, DNB, FACS, FICO (UK), FOSD, MBA , is a board-certified ophthalmologist specializing in cornea and ocular surface diseases. She completed her Fellowship in Ocular Surface Diseases at Sankara Nethralaya, Chennai, and holds an MBA in Hospital and Healthcare Services. Based in Mumbai, India, she is attached to multiple hospitals as a consultant ophthalmologist and cornea specialist. In addition to her clinical work, Dr. Sneha serves as an innovation strategist and editor for Cloud 9 Development (USA), where she collaborates with the development team to design tools and calculators for the EyeHandbook app. Her work blends clinical excellence with a passion for technology, hospital administration and patient-centered care.
drsnehaeye@gmail.com

by Diana Truong
Artificial intelligence in eye care isn’t some far-off future—it’s already here, making waves in clinics, surgery centers and patient conversations. That much was clear at ASCRS 2025, where a jam-packed symposium explored how AI is already being woven into the fabric of ophthalmology practice.
From real-time scribing and smarter surgical planning to automated screening and patient outreach, a session at the annual meeting of the American Society of Cataract and Refractive Surgery (ASCRS 2025) showcased just how practical—and powerful— these tools have become.
“Artificial intelligence (AI) won't replace people, but the person who knows how to use AI will replace those who do not,” said Dr. John Kitchens (United States) during his talk on diabetic retinopathy screening, summing up the mood in the room with a dose of friendly provocation. This wasn’t a conversation about hype—it was about implementation.
To kick things off, Dr. Grayson Armstrong from Mass Eye and Ear (United States) broke down the often
intimidating lingo that surrounds AI. And let’s face it—terms like “machine learning” and “deep learning” can sound like something better suited to a computer science lab than a clinic.
“Artificial intelligence (AI) won't replace people, but the person who knows how to use AI will replace those who do not.”
- Dr. John Kitchens
“If we don't know the terminology, it's going to be harder for us to vet technology for our practices and interface with companies to know which solutions are best for us and our patients,” Dr. Armstrong noted.
To make it all a bit more digestible, he likened AI to different levels of medical training: AI as the attending physician—knowledgeable and versatile; machine learning as the resident, steadily improving with experience; and deep learning as the laser-focused fellow, mastering a very specific skill set. The message? You don’t need to be an engineer, but understanding the basics helps you steer the ship.
Next up, Dr. Robert Chang from Stanford University (United States) showed just how fast documentation can be transformed. Demonstrating real-time AI scribing that produces full clinical notes within 30 seconds, he shared a glimpse into the new rhythm of patient care.
“Stanford has already adopted this system-wide,” Dr. Chang said,
referring to Microsoft’s Dragon Copilot.
This isn’t just a fancy transcription tool. It’s multilingual, can summarize visits in patient-friendly language, and even generate follow-up instructions. Dr. Chang also spotlighted AI-driven phone systems that can field appointment calls with a surprising level of emotional intelligence, responding like an actual person (minus the hold music).
"The hope is we're going to get improved accuracy, especially in atypical eyes."
- Dr.
Ryan Smith
Dr. Ryan Smith (United States) took the conversation into the OR, focusing on how AI is reshaping intraocular lens (IOL) calculations. According to him, while traditional formulas typically reach 74% accuracy within ±0.5D, AI-driven platforms are pushing that number past 90%.
"The hope is we're going to get improved accuracy, especially in atypical eyes," Dr. Smith explained. Still, he urged caution, emphasizing the need for more head-to-head data before crowning a new gold standard.
One of the most compelling applications? AI-based diabetic retinopathy screening.
Dr. Kitchens highlighted a sobering stat: nearly half of patients with vision-threatening diabetic retinopathy aren’t getting screened. But three FDA-cleared AI platforms— LumineticsCore (formerly IDx-DR; Digital Diagnostics; Iowa, USA), EyeArt (Eyenuk, Inc.; California, USA) and AEYE-DS (AEYE Health; New
York, USA)—are stepping up to the plate, delivering high sensitivity and specificity…around 90% in some cases.
"AI gives us an opportunity to go to where these patients are and more seamlessly and easily screen these patients," he explained. Dr. Kitchens also touched on the potential of combining retinal images with demographics and health data to flag patients at high risk of progression.
To wrap up the session, several speakers gave the audience a closer look at AI solutions that are already up and running.
Dr. Greg Eippert (United States) introduced Alcon’s Adi, a platform designed to link clinics and surgery centers with real-time data sharing. One highlight: AI and radio frequency identification (RFID) tagging to automatically track IOL inventory and ensure the right lenses are on hand for the day’s cases.
Next, Dr. Mitchell Weikert (United States) shared ZEISS’s AI-enhanced formula—trained on a jaw-dropping 500,000 ray-tracing models and over 100,000 actual cases. His presentation showed how this tool is producing excellent outcomes even in trickier eyes, like post-refractive surgery cases.
Dr. Mark Packer (United States) rounded things out by showing how practices can turn their own data into opportunity using the Amaros EvidenceEngine platform. He pulled up a live demo revealing that his practice had 68,000 cataract patients with visual acuity of 20/40 or worse who hadn’t been seen recently.
“Who knew we've got 68,000 cataract patients with visual acuity of 20/40 or worse?" he said, echoing the surprise many in the audience seemed to share.
The big picture? AI in ophthalmology is no longer a niche experiment.
It’s real, it’s here, and it’s already delivering measurable results.
As Dr. John Hovanesian, chair of the ASCRS Digital Clinical Committee, said in his opening remarks, "There really are some wonderful technologies many of us have never heard about that work."
The key takeaway? Practices don’t need to wait. These tools are ready for prime time, but choosing the right ones requires thoughtful evaluation.
Dr. Armstrong left attendees with a practical litmus test. “Ask if it was validated in a patient population like yours, if the research shows high accuracy, and if it actually improves care, efficiency and outcomes,” he advised.
"There really are some wonderful technologies many of us have never heard about that work."
-
Dr. John Hovanesian
As AI solutions continue to evolve at a rapid pace, the question isn’t if you’ll use them. It’s which ones you’ll implement first, and how ready you are to get the most out of them.
Reporting for this story took place during the annual meeting of the American Society of Cataract and Refractive Surgery (ASCRS 2025) held from 25-28 April in Los Angeles, California, United States. A version of this article was first published on cakemagazine.org.