Seamless Care at Home: Integrating Home Health and

































Even the most rigorous reprocessing protocols can miss hidden debris or damage. Our advanced borescope goes where the eye can’t — deep into narrow lumens — using AI to ag anomalies in real time. Because when it comes to patient safety, nothing should go unnoticed.



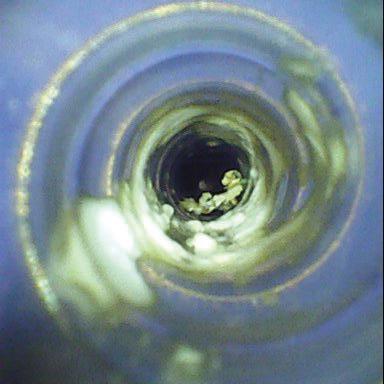




Use of the Flexible Inspection Scope helps to meet AAMI guidelines for borescope use and inspection of instruments with internal channels.
WatchDog AI will notify sta when an instrument has a condition hazardous to patient safety, thereby reducing instrument-associated infections.
WatchDog AI detects mechanical damage at an early stage which enables instruments to be removed from service while repair costs are relatively low. The Flexible Inspection Scope o ers enhanced vision and magni cation and is designed to inspect internal channels of potentially soiled or damaged items.





P.12 SPOTLIGHT
p.12 Department of the Month: Republic of Korea National Cancer Center Innovative Technology Department
p.14 Professional of the Month: Joe Deater, CBET
p.16 Next Gen: Riley Rossbach
p.18 Shifting Gears: Discipline, Resilience and Focus
INDUSTRY
p.20 News & Notes
p.24 Making it Work
p.26 TechNation Pulse
p.27 Welcome to the TechNation Community
p.28 AAMI Update
p.30 ECRI Update
p.32 Ribbon Cutting


P.34 THE BENCH
p.34 Biomed 101
p.37 Tools of the Trade: Fluke Biomedical
p.39 Webinar Wednesday
p.41 Shop Talk powered by MedWrench
P.42 FEATURE ARTICLES
p.42 Roundtable: Ultrasound
p.48 Cover Story: Seamless Care at Home: Integrating Home Health and HTM
P.52 EXPERT ADVICE
p.52 Careers Now
p.54 The Future
p.57 Right to Repair
p.60 Health-ISAC
PUBLISHER John M. Krieg
VICE PRESIDENT Kristin Leavoy
VICE PRESIDENT Jayme McKelvey BUSINESS DEVELOPMENT
EDITORIAL John Wallace
CONTRIBUTORS
K. Richard Douglas
Joie Marhefka
Steven J. Yelton
Garrett Seeley
Phil Englert
Nathan Proctor
Nadia ElKaissi
ACCOUNT Megan Cabot
EXECUTIVES Emily Hise
ART DEPARTMENT
Karlee Gower
Taylor Hayes
Alicia Brown
DIGITAL SERVICES Cindy Galindo
Kennedy Krieg
Haley Harris
EVENTS Kristin Leavoy
Kristen Register
Sydney Krieg
WEBINARS Linda Hasluem
HTMJOBS.COM
Kristen Register
Sydney Krieg
ACCOUNTING Diane Costea
CIRCULATION Joanna Manjarrez
Rob Bundick, Director HTM & Biomedical Engineering, ProHealth Care
Carol Davis-Smith, CCE, FACCE, AAMIF, Owner/ President of Carol Davis-Smith & Associates, LLC
Nadia ElKaissi, CHTM, Biomedical Engineer, HTM, VA Central Office (19HTM)
Bryant Hawkins Sr., Site Manager, Children’s Hospital of New Orleans
Earl Morris Jr., BMET, Director of Clinical Engineering, Harrison County Hospital
Leticia Reynolds, Clinical Engineering Operations Manager at UCHealth Parkview Medical Center

P.62 BREAKROOM
p.62 Biomed Brainbuster
p.64 Word Search
p.64 [Contest] What’s on Your Bench?
p.66 Preferred Vendors
p.70 Service Index
p.73 Alphabetical Index
p.76 Time Capsule







BY K. RICHARD DOUGLAS
In 1989, the Ministry of Health and Welfare in the Republic of Korea formulated a plan to establish a national cancer center. Ten years later, the hospital building was completed, and by 2005, the research building was finished and an information center was opened.
In 2014 came the inauguration of the Graduate School of Cancer Science and Policy. In 2015, the National Cancer Center (NCC) signed a memorandum of understanding with the University of Texas MD Anderson Cancer Center for the collaboration of cancer diagnosis, treatment, education and prevention.
Subsequent to accomplishing all of this development, the National Cancer Center opened a data center, central hospice center and national survivorship center.
The Republic of Korea National Cancer Center uses some of the most advanced cancer-fighting equipment to treat patients.
The team that manages that medical equipment is the Innovative Technology Department.
The department’s head manager is Dr. Hong Man Yoon. The team also includes Technical Team Leader Nak Bin Choi; Innovative Development Part Leader Dong Jun Kim; Technical Management Part Leader Yong Su Choi as well as eight engineers and an admininstrative support member.
“Our department’s name is the Innovative Technology Department and consists of eight technical engineers and one administrator,” Nak Bin Choi says.
He says that the department is divided into a technical team leader who acts as the overall medical and research equipment manager of the institution and two part-leaders who have jurisdiction over affiliated hospitals and lab equipment.
“A total of eight engineers are divided into special zones – OR, ICU, ER, CSR, proton therapy center – and general zones – ward, clinic, Center for Cancer Prevention and Detection – and an expert is in charge of imaging diagnostic equipment,” Choi says.
H e says that in the case of the research institute, it is divided into a research core center (animal laboratory, proteomics core, flow cytometry) and general department, and each person is in charge of their work.
“ The National Cancer Center is a government of the Republic of Korea-funded institution established to contribute to the improvement of public health by reducing the incidence and mortality of cancer patients and improving the quality of life of cancer patients,” Choi says.
H e says that among the world’s cancer center research institutes, affiliated hospitals, National Cancer business management headquarters, and the international cancer graduate university are the only NCC in one institution.
“ The affiliated hospital currently operates 500 beds, and our department belongs to the Healthcare Platform Center,” Choi says.
H e points out that there are only two sites that offer proton therapy centers in the entire country and NCC was the first to introduce the technology in Korea.
The team handles everything related to medical devices and service contracts.
“ We manage the whole cycle of mid- to long-term medical device introduction plan and strategy establishment, introduction deliberation, technical review, inspection, repair and service contracts and disuse,” Choi says.
The team reviews contract conditions such as the preventive maintenance cycle and the scope of parts provision and strives to maintain the best operation rate of medical devices by managing repair initiation, repair progress and a preventive inspection schedule in case of failure.
Choi says that by completing the technical training that manufacturer’s engineers get for initial diagnosis and preventive maintenance for MRI, it was possible for the team to reduce costs by about 10 percent for the initial response service by a biomedical engineer.


As a special project, the team of biomeds helped prepare cancer center counterparts in a West Africa country with an extensive overview and training.
“In preparation for the opening of the National Cancer Center in Ivory Coast, Africa, two local medical technician engineers and two technicians visited the National Cancer Center in Korea to conduct an educational training project,” Choi says.
He says that the training was conducted for six months from May to November 2023 with eight instructors from the Department of Medicine at the National Cancer Center.
“The main content was the general work of the Department of Medicine at the National Cancer Center, theoretical classes for medical equipment to be installed at the National Cancer Center in Ivory Coast, repair practice, field training, equipment manufacturer’s field visit and attendance at the conference,” Choi adds.
The team of engineers is also ready and able to address problem-solving.
“In relation to medical and research devices, devices or equipment are produced that increase convenience during treatment or research and parts of discontinued equipment are produced using 3D printers to contribute to the increase in equipment operation rates,” Choi says.
Another example of resourcefulness was the team’s ability to address the need for a cradle to allow clinicians a handy way to hold accessories for a patient monitoring device.
“The video monitoring system (VMS) in use in the ward is using a barcode scanner for Patient ID scanning and a thermometer for EMR interworking, but there was no cradle at the time of introduction, causing inconvenience to staff.
To solve this problem, a dedicated cradle was designed and manufactured, and a patent was applied for construction, and the results are waiting,” Choi says.
When team members are not on the job, they are involved in several national organizations.
Choi says that the cancer center regularly attends and presents seminars at the Korean Medical Association, which includes most hospital technicians in Korea, and the team leader is in charge of the association’s educational promotion and learning executive position.
He says that they also actively participate in training to acquire and complete the qualification as a medical device safety manager and strive to create a safe medical device use environment in the hospital.
The group also participates with the Korean Society of 3D Printing in Medicine.
“Attending 3D printing conferences every year, we are actively trying to utilize the latest 3D printing technologies and excellent use examples used in the medical field,” Choi says.
The department also is involved with the Korean Society for Quality in Health Care and the International Society for Quality in Health Care.
“We regularly attend [the] society for quality to identify excellent cases of quality improvement in other hospitals and try to apply them to our hospital,” Choi says.
As an HTM professional, when you represent your government’s official center of excellence in cancer care and treatment, you have to be at the top of your game. The Innovative Technology Department members’ resourcefulness and innovation along with the willingness to train other biomeds shows that they are up to the task.
BY K. RICHARD DOUGLAS
In the biomed world, you have to be pretty good to be recognized as the AAMI and GE HealthCare BMET of the Year. This year’s winner is Joe Deater, CBET, a BMET III with Munson Healthcare and a biomed engineering tech instructor at Northwestern Michigan College in Traverse City, Michigan.
Deater spends much of his time in Traverse City, Michigan, a place that is a popular tourist destination on the shore of Lake Michigan. It is known for its cherries and nearby Sleeping Bear Dunes National Lakeshore. It is an ideal location in which to work during the spring, summer and fall.
“I first heard about biomedical technologies from my brother that was in the Air Force. He knew that was my plan also; I was on an electronics track when I went in. He told me to try to get into biomed technologies. As any 17-year-old would do, I said what the heck is that? Well pretty much anyone not in a hospital would ask that too,” Deater says.
He gave it a try but did not land a slot.
“Instead, I got my electronics training background when I was assigned to work on F-16s avionics attack systems. Biomed tech always stayed in the back of my mind though. When I got out of the Air Force in 1993, after my four-year commitment, I moved back to [the] West Coast of Michigan. After a bit of time trying to figure out what I wanted to do with the rest of my life, I enrolled in Baker College of Muskegon and began gen ed classes,” Deater adds.
Baker College gave Deater credit for nearly all his Air Force courses which got him off to a good start.
“As I looked through the offerings at the college, I discovered they had a biomedical technologies degree program. The fates had aligned for me. I proceeded to declare my major in biomed and began taking the required pathway, which was much abbreviated since my Air Force credits took care of nearly all of the electronics and electrical theory classes,” he says.
By the time Deater graduated, he was already working in the field, getting a job at North Ottawa Community Hospital in
Grand Haven, Michigan.
“I have always been a biomed tech, BMET. I was at North Ottawa for 1.5 years working for Service Master. We lost the contract to the newly emerging Sodexo. I then found myself and my family in Traverse City, Michigan, at Munson Healthcare in northwestern Michigan, that has grown from two hospitals and a couple community centers, to now an eight-hospital system,” he says.
Deater progressed up through the ranks, starting as a BMET, moving toward becoming a senior biomed.
“That changed a few years ago to the standard BMET I, II, III structure. I have been all three of them. I am also currently a CBET. I am also the adjunct instructor at Northwestern Michigan College in Traverse City for the Biomedical Technologies Associate Degree Program, where I teach the biomedical technologies courses at the end of the degree for two semesters,” Deater says.
He has been in that position since 2018.
“I also have my own



Generally, they would have to send things out and we all know shipping can be costly. So, I do what I can for them,” Deater adds.
Since 2019, Deater has also been involved with AAMI and the world of standards.
“I have since been an active part of AAMI Standards Committees. I have sat on groups developing white papers such as the BMET Gray Areas, and an updated, as of 2022, listing of the recognized BMET programs across the country. We identified what schools had active programs for BMET associate degrees. Sadly, this was in the midst of the pandemic. Since then, we know we have lost about 10 programs due to cutbacks and lack of enrollment,” he says.
One of the challenges that Deater has faced as a biomed has been the lack of awareness of the biomed field in the rural community where he lives. He says that many people visit the area as tourists never considering that there are jobs there and they could live there as well.
“Munson for many years had open positions that would go unfilled. We had few applicants. So, my management finally approached our local community college about beginning a program,” Deater says.
At the time, he never imagined himself teaching a college course, but it just happened.
“I was meeting with my management and asked about the new program and how it was going. He laughed and said funny I should ask. The tech that was going to be teaching the biomed courses had to step out for some personal reasons leaving no biomed to teach the new biomed classes that had five students coming into it in January. This was all taking place in early November. My manager asked if I was interested in taking on the adjunct teacher position. If so, he would put me in touch with the director of the tech division for the school. I knew we couldn’t not have a biomed teaching the courses, so I reluctantly agreed,” Deater says.
He met with the director of the tech division that afternoon.
“I introduced myself, he shook my hand, handed me the book for the class and said, ‘Welcome aboard.’ I said wait, what? Should we discuss this first? I was officially a college educator now. I had 1.5 months to formulate a syllabus and put
together a course to educate five guys ready to begin their careers. That happened in 2017,” Deater says.
He began teaching in 2018 and all five new techs graduated and landed jobs in biomed technologies.
“My next cohort began fall of 2019; I had three in this class. I had decided to change our book for the class, so I retooled for the next class, rework number two. Fall went well and then there was a little hiccup in spring semester 2020,” Deater says.
The pandemic required regrouping and converting the program to completely online within a month.
“We made it through that and I was then asked to change rooms for a third time so I had to reset my labs and how we would work. I have had all my graduates land biomedical tech jobs that have decided to stay in the field. I now have graduates across the country,” Deater adds.
Away from work, Deater enjoys fishing small lakes in the area in his fishing kayak.
“Finding time to go is tricky most of the time though. I also Halloween. I have a different theme each year and decorate the yard for the big night. Oh, and my hobby garden, that I plant vegetables in. Great relaxation and is fun to see seeds transform into food,” he says.
He has been happily married to his wife, Tonya, for 30 years.
“We have two grown kids; my son, Jordan and my daughter, Logan. Both kids are college graduates. Logan is married, her husband Jarred is a sous chef in Ada, Michigan. Logan is working towards her Ph.D. at Western Michigan University in Kalamazoo, Michigan. Jordan works in IT in Grand Rapids, Michigan. We have three grand dogs. Both of us have both sets of parents still with us and doing relatively well,” Deater says.
Of the AAMI/GE HealthCare BMET of the Year Award, Deater is humble and reflects upon the focus of many in the field.
“I was in shock to hear that I had been awarded it. It isn’t a self-promoting award. Someone had to nominate me, then a review board had to look over the nomination amongst other stronger candidates from all of the world. As is the case for most BMETs, we are not looking for awards; we look to keep patients safe and equipment working. That’s our award; knowing we have a job well done,” he says.
Riley Rossbach is a clinical engineer for the Advanced Heart Failure Therapy Clinic at St. Luke’s Medical Center. She began her career by earning a Bachelor of Science in biomedical engineering and a minor in user experience from the Milwaukee School of Engineering.
TechNation found out more about this rising star in the HTM field via a Q&A.
Q: WHERE DID YOU GROW UP?
A: New Berlin, Wisconsin
Q: WHERE DID YOU RECEIVE YOUR HTM TRAINING/ EDUCATION?
A: Bachelor of Science in biomedical engineering from MSOE and most of the training happened on the job.
Q: HOW DID YOU FIRST DISCOVER HTM?
A: I searched engineering and healthcare on all of the job boards and eventually found a biomedical tech position at Aurora Healthcare. They offered me the job 5 minutes after my interview was completed.
Q: WHY DID YOU CHOOSE TO GET INTO THIS FIELD?
A: For the same reason I chose biomedical engineering as my degree. I love helping people in any way. I was always good at math and science, they just made sense to me, so I went into the industry where I could use my talents to help. Going into the medical field, I realized that technology is utilized in every little task and there are so many ways for someone in the biomedical education field to make healthcare better.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: In my current position I have a lot of patient interaction, and that is what makes getting up for work everyday easy. In past positions, it wasn’t always easy to see your direct impact on
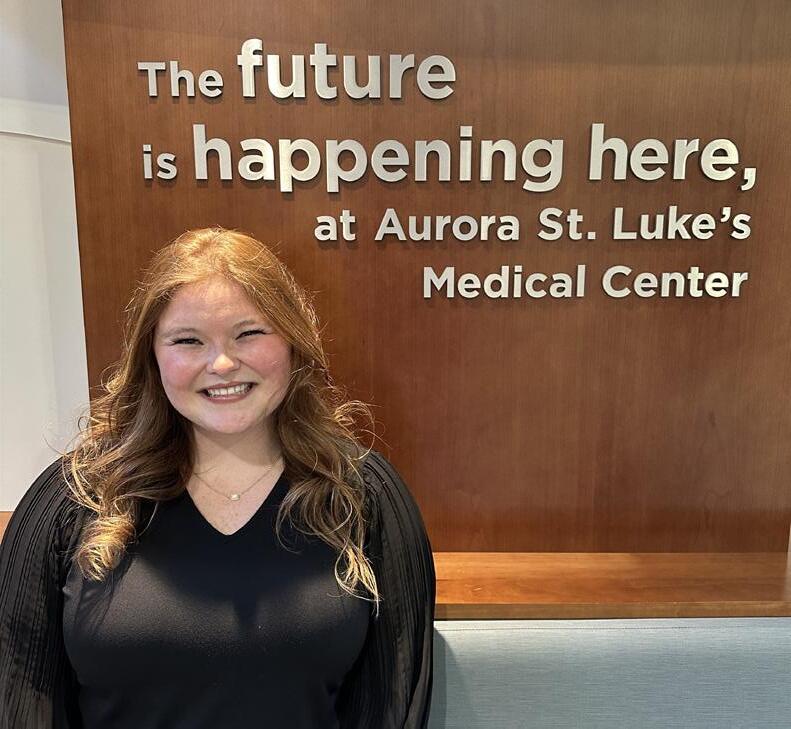
patient care or the community, but in this position, I feel accomplished seeing the smiles on my patient’s faces.
Q: WHAT INTERESTS YOU THE MOST ABOUT HTM?
A: My current position is working with left ventricular assist devices (LVADs) and there has been a lull in the industry for the past few years regarding innovations in the field. There is a new device that is currently in clinical trials and I am excited to see the improvements that this new device will make in our industry. There is always more to learn, improve and innovate in this field.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: I have completed my orientation for this position, which was a year of hard work and dedication to complete education, certifications, clinical experiences and teaching. I am also currently working on a project to make sure that we circle back with patients of our clinic who were not currently meeting criteria to need our advanced therapy options. These patients may need further education, re-evaluation or listing on the heart transplant list.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: I am hoping to continue improving the field of clinical engineering by continuing education of our patients but also our community such as our nurses, EMTs and students who want to get into the field. Stepping into this next era of a new device being in clinical trials will open up a lot of opportunities for innovation.
K. RICHARD DOUGLAS
Located between the Caribbean Sea and the North Atlantic Ocean, the Commonwealth of Puerto Rico is an island in the northeastern Caribbean. At only 100 miles long and 35 miles wide, it is the smallest island of the Greater Antilles.
Puerto Rico is a U.S. territory and has a tropical climate with a rainy season, dry season and hurricane season. In 2017, Hurricane Maria devasted the island and was catastrophic, causing widespread destruction.
Most of the time though, the island offers a culturally rich destination for tourists and an interesting history.
The island has 68 hospitals with most in major population centers. The manager of biomedical engineering at the Puerto Rico Medical Services Administration is Patricia García Pizarro.
The Puerto Rico Medical Services Administration (ASEM) is a government institution attached to the Department of Health of the Commonwealth of Puerto Rico.
While Pizarro’s focus during the workday is on managing a biomed team; her passion is fitness.
“At 15 years old, something in me changed. I had accompanied an athletic friend to the gym, and without knowing it, that day, a new chapter of my life began. The sweat, the effort, the sound of iron clashing and the atmosphere of determination awakened a passion that has never left me – the desire to change myself, to grow, to become the best version of who I am,” she says.
Pizarro says that by the time she was 20, she understood the pursuit of fitness wasn’t just about aesthetics.
“Weightlifting taught me discipline, resilience and focus. My body became an extension of my will; a tool not just to feel strong, but to be useful. The gym became my safe space; my therapy,” she says.
For years Pizarro trained in boot camps. In 2023, she found Jibaro CrossFit.
“What began as a physical challenge quickly turned into

a life-changing experience. CrossFit showed me that real strength isn’t just in the muscle; it’s in the mind. Every workout is a battle against doubt, fear and self-imposed limits. Here, I learned that I was far stronger than I thought,” she says.
Pizarro says that the significance of her story should not be limited to thinking about reps or barbells, but through the practical application of pursuing and maintaining fitness.
“After Hurricane Maria, while working at the medical center, I was haunted by one question: Was I truly prepared for a real emergency? Could I rescue someone from the rubble? Could I save a patient if all systems failed? That was the moment I knew I had to become a woman ready for anything. I didn’t just want to be fit; I wanted to be capable, empowered, and dependable in times of crisis; CrossFit became my answer,” she says.
She adds that she also takes gymnastics classes.
“I started with the goal of improving my performance in CrossFit, and it’s been an important part of my recent progress,” Pizarro says.
The dedication to both lifting weights and CrossFit have provided impressive results. Those who lift often cite their “personal best” in different lifts. For Pizarro, that includes a
225-pound deadlift, a 170-pound back squat and a 155-pound front squat.
“I’ve competed in the CrossFit Open in the women’s (45-49) scaled division, achieving in 2023; ranked 36th in the world and in 2025; ranked 20th worldwide in my division, and 7,635th among all athletes in my age group,” she says.
Pizarro’s interest in a biomed career was forged early in life. She is something of a rarity in the HTM field in Puerto Rico and her fitness drive is apparent in her career as well.
“My calling to serve others started early in life. My parents, through faith and church, taught me the power of blessing others through compassion and action. That same drive led me to pursue a career in biomedical engineering, a technical, demanding, and essential field within modern healthcare,” Pizarro says.
She says that she earned her associate degree in biomedical engineering from the Puerto Rico Institute of Technology in 1997.
“Since then, I’ve dedicated my professional life to service. I began as a technician at the San Juan Municipal Hospital, later became supervisor at Pavia Hospitals in Santurce and Hato Rey, and currently serve as the biomedical engineering manager at ASEM-Puerto Rico’s Medical Services Administration. I hold a professional license (No. 3148), and I am proud to be one of the few women in this field on the island,” Pizarro says.
She says that she works with life-saving technology and complex medical equipment. She has completed over 30 certifications-ranging from COVID-19 mechanical ventilation to emergency preparedness with FEMA and the U.S. Department of Homeland Security.
“My two worlds, biomedical and CrossFit, intersect with purpose. Both demand precision, endurance, quick thinking and action. Both prepare me to save lives,” Pizarro says.
She also finds that her personal life is a source of strength.
“I’m married to Joel Calderón, and we are proud parents of twins: Christian Joel Calderón and Joheilys Nicole Calderón,” Pizarro says. The family also has several pets.
The training and her work as an HTM manager all serve the same purpose for Pizarro.
“Today, I can proudly say I’m a woman of action. Whether in an operating room or CrossFit box, in a hospital hallway or under a loaded barbell, my mission is always the same: to give my best, to serve with purpose and to be ready always for whatever life may bring,” Pizarro adds.



The U.S. Food and Drug Administration (FDA) recently issued a new guidance in regard to the cybersecurity of medical devices. The new guidance “Cybersecurity in Medical Devices: Quality System Considerations and Content of Premarket Submissions; Guidance for Industry and Food and Drug Administration Staff; Availability”
This guidance updates the previous version of the guidance, of the same title, issued on September 27, 2023, and finalizes the draft guidance entitled “Select Updates for the Premarket Cybersecurity Guidance: Section 524B of the FD&C Act” issued on March 13, 2024. This guidance
The American Society for Health Care Engineering (ASHE) has announced that UNC Health Blue Ridge is the winner of the 2025 Excellence in Health Care Facility Management (FM Excellence) Award.
Each year, the FM Excellence Award recognizes individuals or facilities teams that implement new or innovative programs or processes to optimize the healthcare physical environment and improve patient care. Officials from UNC Health Blue Ridge were presented with the award in Columbus, Ohio, at the Health Care Facilities Innovation Conference.
For 120 years, UNC Health Blue Ridge has served as the nexus of health care in rural western North Carolina. The hospital’s new six-story pavilion on its central campus in Morganton, N.C., was planned to meet the needs of the growing patient population and modernize its infrastructure.
Completed in August 2024, the new facility expands the original hospital from 338,060 square feet to 557,181 square feet, encompassing 30 updated intensive care unit and emergency department rooms and dedicated behavioral health spaces. The expansion also enabled UNC Health Blue Ridge to centralize inpatient care across the system and increase capacity to 214 inpatient beds, as well as help the hospital secure Level III trauma center designation. The project team enacted an adaptive and highly
provides FDA’s recommendations to industry regarding cybersecurity device design, labeling, and the documentation that FDA recommends be included in premarket submissions for devices with cybersecurity risk.
Additionally, this guidance has been updated to identify the information FDA generally considers to be necessary for cyber devices to support obligations under the new amendments to the Federal Food, Drug, and Cosmetic Act (FD&C Act) for ensuring cybersecurity of devices.
The announcement of the guidance was published in the Federal Register on June 27, 2025.
collaborative design process, inviting perspectives from a range of clinical and operational teams, using value engineering and incorporating low-maintenance materials sourced locally. These strategies reinforced values of teamwork, resilience and innovation, helping the team deliver on its goals in the face of extraordinary obstacles including disruptions from the COVID-19 pandemic, labor shortages, supply chain issues and significant internal leadership changes.

The internal redesign deployed an evidence-based approach that has already improved clinician workflow and delivered improvements to patient care. The facility also incorporates modern technologies such as a digital communication system with electronic signage, as well as adaptations to facilitate reduced operational expenses, promote resiliency and meet energy reduction goals. These include high-efficiency HVAC systems, occupancy-based lighting and water-saving infrastructure, as well as stormwater management and streamlined mechanical systems to further reduce long-term maintenance expenses.

A new virtual training course designed to equip healthcare professionals with critical laser safety knowledge is launching this fall. The Medical Laser Safety Officer (MLSO) Course will be held online September 27-28, 2025, and is open for registration at medicallasersafety.com.
As laser technology continues to revolutionize surgical and clinical care, the risks associated with its use demand strict safety protocols. This comprehensive two-day course is approved by the Board of Laser Safety (BLS) and fulfills the training prerequisite to sit for the Certified Medical Laser Safety Officer Exam.
Led by nationally recognized experts Vangie Dennis, MSN, RN, CNOR, CMLSO, FAORN, and Patti Owens, BSN, MHA, RN, CNOR, CMLSO, the MLSO course delivers in-depth instruction on laser biophysics, tissue interaction, and safety management. Attendees will explore multiwavelength laser technologies and review standards from ANSI Z136.3-2024, the AORN Laser Safety Guidelines (2020), and CSA Z386-24.
Participants will gain the tools to:
• Understand laser-tissue interactions and classifications
• Assess and control laser-associated hazards
• Develop and evaluate laser safety programs
• Navigate compliance with regulatory bodies including TJC, CMS, OSHA, AAAHC, and QUAD A
• Address safety in surgical, dental, dermatological, and ophthalmological settings
The course is designed for perioperative nurses, surgical technologists, radiation safety officers, biomedical engineers, and laser safety officers (LSOs).
Having a certified Medical Laser Safety Officer is not optional – it’s essential. Without proper oversight, healthcare facilities risk regulatory violations, patient harm, and compromised staff safety. This course arms attendees with the knowledge and certification path necessary to manage these risks effectively.
For additional details about the course or to register, visit medicallasersafety.com. Learn more about the Certified MLSO exam at lasersafety.org.
EVOKMED has officially launched, marking the next chapter in a journey that began as Isikel Clinical Equipment Technology. The rebrand reflects a renewed focus on healthcare service excellence and a strategic shift to align more precisely with the evolving needs of healthcare partners nationwide.
The new name, EVOKMED, was chosen to represent the company’s mission to evoke precision, deliver superior support, and empower healing. While the branding has changed, the core team, values, and commitment to exceptional service remain the same.

“This evolution allows us to sharpen our focus on finding the right fit for every healthcare partner we serve,” said Michael Tripp, Partner, vice president of sales. “We’re building on a strong foundation while expanding our reach and capabilities under a brand that’s ready for the next challenge.”
The rebrand comes at a time of sustained growth for the company, reinforcing its dedication to delivering high-impact support to facilities across the country. With EVOKMED, the team aims to raise the bar for what dependable, highperformance healthcare service looks like.


TRIMEDX has been ranked 30th on the 2025 list of Top 100 Inspiring Workplaces in North America by the Inspiring Workplaces Group. In addition, TRIMEDX received Best in Class recognition for Leadership, one of only eight organizations to earn this distinction.
This recognition highlights TRIMEDX’s continued commitment to fostering a PeopleFirst culture – one that empowers associates through trust, purpose and belonging.
“Being named an Inspiring Workplace and recognized for Leadership is a powerful reflection of our culture and the incredible people who bring it to life every day,” says TRIMEDX Chief Human Resources Officer Dawn Griffin. “We are proud to lead with purpose and invest in our associates so they can thrive and make a meaningful impact on healthcare.”
The Inspiring Workplaces Awards evaluate organizations based on six key elements: Culture & Purpose, Leadership, Wellbeing, Inclusion, Employee Voice, and Employee Experience. TRIMEDX stood out among hundreds of entries across North America for its leadership development, associate engagement and commitment to innovation.
This year’s recognition builds on TRIMEDX’s momentum from 2024, when the organization was ranked #29 in North America and #30 globally.
“As we continue to grow and evolve, our focus remains on creating an environment where people feel seen, valued, and empowered,” says TRIMEDX CEO Neil de Crescenzo. “This recognition belongs to every associate who contributes to our mission and culture.”
The full list of winners and more information about the awards can be found at inspiring-workplaces.com.
PartsSource unveiled further development of Asset Uptime at the 2025 AAMI eXchange in New Orleans. Asset Uptime is described as a bold, evidence-based initiative to transform clinical asset management.
“PartsSource has a proven history of innovating to empower healthcare technology management (HTM) teams to solve critical challenges and deliver measurable cost, quality, and productivity outcomes, eliminating complexity and streamlining healthcare workflows,” according to a news release. “PartsSource is announcing the next step in the future of HTM, empowering professionals to proactively manage equipment health by assessing and visualizing true clinical and operational readiness.”
Asset Uptime is healthcare’s first data-driven technology solution to enable clinical operations and supply chain teams to manage the health and maintenance of equipment across federated multi-vendor, multi-modality, and multi-site care environments, the release states. Asset Uptime provides HTM teams the tools to proactively manage equipment health, automate service response, and improve clinical availability. This breakthrough technology aggregates asset telemetry from connected devices and systems, standardizes workflows by ingesting and normalizing disparate data signals, and introduces the first Asset Health Record, a centralized repository that stores and visualizes critical data across vendors and modalities.
By initiating and automating event-based workflows for parts and service, HTM teams can act faster and smarter. The result is higher equipment uptime and greater clinical capacity.
PartsSource has co-developed this innovative solution with its alpha partners, five healthcare systems, representing 87 hospitals.
Healthcare providers face increasing pressure to maintain asset availability amid growing operational strain. New research shows that most hospitals self-manage up to 30 internal and external software systems related to device maintenance, many of which are siloed and underutilized, resulting in significant inefficiencies. Inconsistent diagnostic procedures across proprietary vendor platforms can increase equipment downtime by 20 to 40 percent. The financial impact is substantial, as downtime costs the average health system between $20 million and $50 million annually. As health systems strive to protect revenue, optimize resources, and improve patient throughput, the industry demands a new approach to enterprise asset availability. Asset Uptime provides the healthcare industry with an unprecedented technology solution to improve missioncritical asset availability and clinical capacity for greater patient throughput, clinical satisfaction and improved profitability.
“Asset Uptime is an inflection point on our journey of radical transformation,” said Philip Settimi, MD, MSE, president and CEO of PartsSource. “We are building on the success of PartsSource PRO by co-developing a solution alongside our provider partners that allows health systems to make smarter, faster decisions that reduce costs, eliminate downtime, and expand clinical capacity. This is the future of healthcare.”

Asset Uptime delivers healthcare providers a new standard in enterprise visibility and control. The platform integrates real-time device monitoring, CMMS data and integration, and PartsSource supply chain intelligence to provide a centralized view of asset health and performance. It introduces purposebuilt digital workflows to eliminate manual processes, improve labor efficiency, and drive reliable cost savings.
“Asset Uptime gives us the power to move from reactive repairs to proactive readiness,” said Don Davenport, manager, clinical engineering at MultiCare Health System. “With real-time insights and a unified view of our inventory and operations, we can better prioritize resources, improve service response, and ultimately increase equipment availability. It’s a major leap forward in our ability to support clinicians and patients.”
PartsSource demonstrated Asset Uptime’s power through a live technical proof of concept in 2024, showcasing seamless integration between device monitoring tools, CMMS platforms, and the PartsSource ecosystem. At this time, the alpha development partners are the first healthcare providers in the U.S. utilizing Asset Uptime.
The announcement of Asset Uptime builds on a series of innovations that reinforce PartsSource leadership in healthcare technology management. PartsSource launched PRO Service during the 2023 AAMI eXchange in response to research that found hospitals have 50% of budgets allocated to underperforming legacy agreements. PRO Service is a scalable, evidence-based solution designed to replace fragmented service contracts with a unified, digital-first approach to service management. PartsSource is now responsible for overseeing more than 132,000 assets across its client base. The solution helps providers consolidate vendor contracts, standardize service quality, and gain transparency into labor performance.
“The flexibility that PartsSource PRO Service offered us was transformational,” said John Knapp, vice president of clinical engineering at LifeBridge Health. “By meeting us where we are, PartsSource helped remove the risk of taking equipment previously off-contract onto a new agreement, while their proactive recommendations for highly qualified vendors from their network are helping us manage and reduce our service spend.”
“I provide mission-ready equipment, used to service patient needs, by fixing what was inoperable when it was delivered to me,” Atkins said. “It can take weeks, sometimes months, to get new equipment. We have to get innovative so providers can continue caring for patients.”

BY TECH. SGT. ELORA MCCUTCHEON
While patients waited in crowded clinics and medical staff in crisp uniforms moved from room to room, a small maintenance shop tucked into the corner of Academic Hospital buzzed with a different kind of energy: less visible, but no less essential.
Senior Airman Adrese Atkins, a medical administration technician assigned to the 931st Aerospace Medical Squadron, spent most of his days not in scrubs but in a cluttered workspace no larger than 700 square feet. Surrounded by boxes of loose wires, aging
equipment, scattered tools and instruction manuals, he supported a critical component of AMISTAD 2025 few people ever saw.
Atkins is one of nearly 40 Total Force Airmen who deployed to Suriname in support of the medical readiness mission supported by Air Forces Southern and Air Force Reserve Command. The two-week Global Health Engagement, held from July 14-25, spanned three sites across the South American country: Wanica Hospital, Brownsweg Clinic, and Academic Hospital Paramaribo. It brought U.S. military physicians, technicians and support personnel together with Surinamese partners to provide dental, family and emergency care while exchanging vital medical knowledge.
“I provide mission-ready equipment, used to service patient needs, by fixing what was inoperable when it was delivered to me,” Atkins said. “It can take weeks, sometimes months, to get
new equipment. We have to get innovative so providers can continue caring for patients.”
But unlike the doctors and nurses whose work was center stage, Atkins’ contribution unfolded behind the curtains as he serviced patient beds, electrocardiograms, blood pressure pumps, respiratory devices and “anything that touches a patient,” as he explained. His civilian career as a biomedical equipment specialist enabled him to support the hospital’s four-person biomedical technical operations team, which was critical to maintaining the functionality and safety of the equipment that care teams relied on every day.
It was a job made even more complex by the tools he didn’t have.
“The Air Force provides us with a lot of resources,” he said. “Here, I’m fixing equipment while patients are actively being treated in the same room, or patching rusted gear with paint instead of being able to replace it outright. It’s been a valuable learning opportunity.”
Atkins wasn’t always in the medical world. He began his career on active duty as an aircraft metals technology specialist, where he learned to diagnose problems, think creatively and adapt to unpredictable maintenance challenges. That foundation, he said, shaped how he approaches his job now.
“What people may not know is how creative we have to be under pressure,” he said. “Panic can’t be the first button you press – it has to be critical thinking and creativity. Doctors and nurses use equipment they rely on every day, and we have to keep it in service no matter what. I call it ‘professional streetsmarts,’ because there are always unique problems outside of what textbooks teach you.”
His approach didn’t go unnoticed by the team he embedded with throughout the two-week mission. In a department where visitors typically observe rather than dive in, Atkins quickly earned a reputation for initiative and reliability.
“He is extremely helpful,” said Nico Djamikoen, one of the Academic Hospital Paramaribo biomedical technicians. “When the phone rings, he gets up and goes [to repairs] on his own, which we did not expect. He does not complain and he makes sure the job gets done. He’s been an amazing help, and he’s fun to have around.”
Another team member added with a laugh: “He can stay as

long as he wants – we’d love to keep him.”
AMISTAD 2025 was designed to improve access to care and strengthen regional health infrastructure in cooperation with the Suriname Ministry of Health. The mission also allowed U.S. and partner nation medics to share procedures, gain cultural insight and prepare for future humanitarian and disaster response operations.
“The [Surinamese] have been so welcoming and open to sharing how they do things,” Atkins said. “I’m glad to be here to help. I feel a great sense of importance, like what we’re doing here is genuinely mission essential.”
This was Atkins’ first AMISTAD mission, and one he volunteered for after previously deploying to Poland in a one-deep position.
“I like to push myself out of my comfort zone,” he said. “I wanted to see if I could help, or if I could make a positive difference. I really learned what I was capable of on that deployment, and it made me want to volunteer for this.”
Atkins’ experience underscores one of AMISTAD’s core objectives: preparing medics to operate in resource-constrained, expeditionary environments. Working with limited tools, unfamiliar systems, and cross-cultural teams mirrors the very conditions these Airmen may face in real-world contingencies.
Missions like AMISTAD test the agility and adaptability of medical teams while building trust and interoperability across the total force. By integrating active-duty, reserve and partner nation personnel, the mission strengthens the collective ability to respond effectively to future medical crises.
Despite the mission’s short duration, Atkins said he felt the urgency and necessity of his work from the first day.
“My impression of this mission is just how essential our help and resources are to these people,” he said. “It would be great to see this mission last even longer in the future, to really be able to get our feet under us and do good in the community.”
Though AMISTAD 2025 was centered on medical care, Atkins’ role is a reminder that successful missions aren’t just measured in patients seen – but in the infrastructure that enables their care.
“I hope to walk away with the knowledge that I was able to help someone who needed it,” he said. “That’s what inspired me [to enlist], and it’s what continues to bring me fulfillment.”

NOVEMBER 10-12, 2025
HTM professionals nationwide are invited to mark their calendars for the annual MD Expo Dallas, set for Nov. 10-12 at the Renaissance Dallas Addison Hotel in Addison, Texas. Hosted by MD Publishing and TechNation, this premier conference is one of the year’s must-attend events for HTM professionals.
The three-day agenda features industry-leading sessions on HTM best practices, cybersecurity, IT integration, compliance and equipment service – delivered by top experts in the field. An expanded exhibit hall will showcase the latest medical technologies and services, offering hands-on demos and direct access to vendors.
New features this fall include a Lunch & Learn session exclusive to attendees. Sponsorships are available for what promises to be a combination of learning, networking and comradery. The “Lunch & Learn” seminars offer complimentary meals paired with expert insights. MD Expo is also introducing its HTM Explorers Program where middle school and high school students will get an in-depth look at the HTM career field.
The MD Expo kicks off on Nov. 10 with H.O.T. (hands-on training) Workshops and the invitation only Leadership Summit, featuring a kickoff session, welcome reception and dinner.
Whether you’re a seasoned leader or new to the field, this year’s event is poised to deliver an unforgettable experience.
For full schedule details, speaker updates and registration information, visit MDExpoShow.com.
Enter the contest and help TechNation celebrate. Fill out the short form at 1technation. com/contest for a chance to win one of 12 prizes, each valued at $150 or more!
Additional entries to win can be acquired by sharing on LinkedIn or submitting a photo. Each month, a winner will be selected and featured in TechNation magazine!
July’s winner is Tony Mack.
Find out more information on Page 76.


TechNation is accepting nominations for its 2026 40 Under 40 program, spotlighting standout HTM professionals 40 years old or younger.
This increasingly popular honor highlights young leaders making meaningful contributions to the HTM industry.
“We are thrilled to continue this tradition of recognizing exceptional young professionals in the HTM community,” said Megan Cabot of MD Publishing. “The enthusiasm and talent of the next generation of HTM leaders is inspiring.” TechNation encourages HTM professionals to nominate colleagues or apply themselves. Those selected will be featured in a special edition of TechNation magazine next April.
For more information or to submit a nomination, visit 1technation.com/yp.
Q: WHAT PRODUCT, SERVICE OR SOLUTIONS DOES YOUR COMPANY PROVIDE TO THE INDUSTRY?
Admar Neuro keeps neurodiagnostic labs running at full speed. We:

Chad Stamper, Operations Manager
• Repair & refurbish EMG, EEG, VNG, TCD, and Ultrasound systems—OEM-grade parts and a 7-10 day average turnaround.
• Deliver preventative-maintenance programs that extend asset life and document compliance.
• Offer short-term rentals and Rent-to-Buy plans so clinics can bridge gaps, scale quickly, or “try before they buy.”
• Sell consumables and accessories to include needles, electrodes, cables with just-in-time fulfillment.
• Provide bilingual remote tech support & training for clinical staff across North and Latin America. .
Q: TELL US WHAT DIFFERENTIATES YOUR COMPANY FROM THE COMPETITION?
Over 40 years of neurodiagnostic repair and service experience
• Neuro-only focus: Our engineers are trained on the nuances of signal quality, patient safety and regulatory requirements unique to neurodiagnostics.
• Speed without shortcuts: A well-stocked parts inventory and standardized depot workflows let us return 98% of units within two weeks—backed by a 90-day warranty.
• Lifecycle mindset: We pair maintenance with asset-management dashboards,Trade In and Buy Back options paths so hospitals unlock residual value instead of scrapping older devices.
• Bilingual partnership: Our team supports customers in English and Spanish, giving Latin-American sites the attention they rarely receive from larger competitors.
Q: WHY DID YOU CHOOSE TECHNATION FOR ADVERTISING?
TechNation reaches the very professionals we serve—biomedical engineers, HTM leaders and clinical managers who make uptime and capital-spend decisions. Its engineer-centric content matches our no-nonsense approach, and its readership spans throughout North America, just like our customer base. Advertising with TechNation positions Admar Neuro alongside trusted voices in healthcare technology management and lets us share real maintenance insights with a community that values technical expertise.
For more information, visit admarneuro.com

As a veteran with 25 years’ experience, I started FDM Enterprises to support others in the industry with their MRI, CT, and Injector Service. I chose TechNation for advertising since their target audience are my people (imaging people). I am looking to expand contacts and relationships.
For more information, visit fdmenterprises.com

Omar Jarrah, Owner/ Contractor
Enterprises

At the 2025 AAMI eXchange, Dr. Binseng Wang of Sodexo and G. Wayne Moore of Acertera Acoustic Laboratories met for a rematch of their 2024 debate on medical device remanufacturing and servicing regulations.
The session was conducted in point-counterpoint format, with attendees voting on which questions the speakers debated.
AAMI Board member and COO of The InterMed Group Larry Hertzler graciously moderated this discussion on what he called “regulating the unregulated.”
As a neutral convener, AAMI does not take a stance on contested policy areas like remanufacturing and right to repair. But the Association gladly provides an open forum for debate among members. If you missed this session, be sure to look out for future events like it – the debate over remanufacturing is unlikely to go away soon.
IF ORIGINAL EQUIPMENT
(OEMS) SHOULD PROVIDE THE MATERIALS FOR SERVICE, THEN SHOULDN’T THE SERVICERS BE REGISTERED JUST AS THE OEMS ARE?
Moore answered with, “It depends on what type of servicing that we’re actually talking about.” He sees a fundamental difference among repair, parts replacement, and making a modification that may not be appropriate to add to a finished, cleared medical device in the field. That said, Moore believes manufacturers should make the necessary information to make on-site repairs available to independent service organizations (ISOs), provided they act on behalf of a hospital.
But Moore made his position clear. If an ISO asks for information beyond the scope of what an OEM feels is
appropriate or necessary to perform repairs in a hospital setting, then that activity has “crossed a line into potential remanufacturing.” If so, that ISO should be regulated in the same fashion as any OEM.
Wang responded by pointing out that FDA already has the legal authority to regulate ISOs in the same way as OEMs if the agency deems it necessary. “First of all, we are all regulated, like it or not.” He cited a 2018 FDA report that concluded there is no significant record of major issues related to ISO remanufacturing activities. To date, FDA has chosen not to regulate ISOs in this way. Based on this finding, Wang argued that there is no reason for FDA to invest its limited resources in regulating ISOs in same way as OEMs. Further, he posited that the remanufacturing issues discovered by FDA were likely the result of a lack of access to OEM information.
Wang then drew an analogy to the U.S. Constitution, stating, “If I am required to abide by the Constitution but I’m not allowed to read the Constitution, how am I going to be able to abide by it?” He also noted that the existing inspection and regulation regime for medical device manufacturers does not prevent all recalls or safety issues. Thus, he sees no reason why analogous regulations on ISOs would result in massively improved patient safety outcomes.
Moore offered a rejoinder, saying that “servicing can include component level change or a field replaceable unit modification,” but reiterating his point that there is no FDA definition for “bad servicing.” Instead, FDA differentiates servicing from remanufacturing, and defines servicing as an “activity that returns a finished medical device to original equipment specifications, substantially ... anything that doesn’t do that is classified as remanufacturing.” Moore indicated that he sees no issue with buying parts from the manufacturer, but it is vital to validate that those parts work as intended and align with the OEM’s intended purpose and function.
In Wang’s view, if ISOs do not have access to materials for
software and software codes, “how can we be sure” if an intervention is correct and safe? He nevertheless clarified that he is not advocating for “anyone under the sun” to have access to OEM service material but rather the purchasers or owners of medical devices who could then share as needed with their contracted third parties.
HERTZLER: WHY DON’T ALL HDOS REQUIRE MANUFACTURERS TO PROVIDE SERVICE DOCUMENTATION, SERVICE KEYS, ETC., AS A CONDITION OF PURCHASE?
In Hertzler’s words, “Why isn’t this a requirement of purchase?” After all, there is an inherent pressure created by the fact that “hospitals are going to buy equipment no matter what.”
Wang stated that if OEMs included this demand with their purchases, it would benefit HTM professionals. Ideally, this would be a “standard demand” made by healthcare delivery organizations. He also said that the U.S. Secretary of Defense recently issued a memo to secretaries of the various service branches demanding that equipment acquisitions by service branches include OEM information. However, “The issue is very simple. It’s called money.”
Healthcare delivery organizations like hospitals do not have the same resources as the U.S. Department of Defense. Further, Wang noted that some OEMs offer financing packages to HDOs that stipulate service contracts with the OEM. How many hospitals can say, “No, I don’t want the equipment?”
Moore countered, stating that while DOD has a great deal of taxpayer resources, they are “not infinite.” During his career, he did observe some HDOs successfully make demands of OEMs. “It can be done.”
Wang also expressed concern with OEMs discontinuing devices deemed legacy devices and then indicating that it is unsafe to allow third parties or in-house staff to work on their cyber capabilities or software. Without concrete action by Congress or FDA, he believes this trend could become “more and more aggressive.”
Moore responded by pointing out that “The FDA does not know everything.” While he acknowledged the agency’s efforts and expertise, FDA simply does not have subject matter experts for every issue that may arise in HTM. Given the pace of technological change, this can create a challenging environment.
HERTZLER: INSTEAD OF EACH STATE CREATING ITS OWN RIGHT-TO-REPAIR LAW, SHOULDN’T THE FEDERAL GOVERNMENT ESTABLISH A SINGLE, UNIFORM LAW FOR THE COUNTRY?
“Yes. Thank you.” But Moore elaborated, saying that he is skeptical that the U.S. Congress has the ability or willingness to act. If Congress does not settle the question of right-to-repair, a state-bystate approach may be a viable alternative.
Wang also favors a national right-to-repair law. Even if it is difficult to get Congress to act, “We still can come to some type of understanding even if we don’t have a nationwide law or regulation.” Given patients’ needs, ISOs “need a tool to provide prompt care.” His priority is ensuring that HTM professionals promote good patient outcomes by servicing medical devices.


ECRI, a global independent healthcare and patient safety nonprofit, named Prisma Health the winner of its 2025 Health Technology Excellence Award.
ECRI’s annual award honors a member facility for implementing an exceptional initiative to improve patient safety, reduce costs or otherwise facilitate better strategic management of health technology.
Prisma Health is the largest healthcare provider in South Carolina. The not-for-profit organization encompasses 19 hospitals on 12 campuses, including children’s, psychiatric, rehabilitation, and heart specialty facilities. As Prisma Health has expanded significantly in recent years –including merging two health systems, expanding urgent care and specialty service lines, and adding a community
hospital in Maryville, Tennessee – it faced the challenge of building a resilient technology infrastructure that could keep pace with growth.
Prisma Health won the award based on the success of its multi-layered, comprehensive approach to advancing its technology infrastructure and disaster preparedness while enhancing patient safety and care delivery.
ASPECTS OF THE PROJECT INCLUDED:
• Strengthening the network infrastructure: Prisma Health implemented a regional redundant network design with modular connectivity to ensure 100% uptime, even in the event of multiple fiber failures. A multi-carrier distributed antenna system was also deployed to ensure uninterrupted cellular coverage in hospitals.
• Improving workflow in the ED: Different login processes for different equipment pose a challenge in the fast-paced emergency department, so Prisma Health’s technology team collaborated with frontline staff to redesign
workflows and implement a secure “tap-in/tap-out” process. The result was more efficient, secure access to the electronic health record.
• Enhancing business continuity efforts: Prisma Health reassessed its disaster recovery capabilities and implemented new protocols and tools to provide uninterrupted care during catastrophic outages.
Most healthcare organizations are aware of what they need to do to maintain technical infrastructure and establish emergency backup plans, but not every organization invests in those initiatives and implements them well. Prisma Health did both, and their work was almost immediately tested.
In September 2024, Hurricane Helene swept through the region, ravaging the communities served by the health system. Although widespread outages impacted the region, the proactive infrastructure work led by Prisma Health ensured the hospitals could maintain EMR access, continue providing quality care, and restore full operations faster than most surrounding healthcare systems.
“We are incredibly proud of Prisma Health’s technology team for their unwavering commitment to reliable, round-theclock healthcare delivery,” said Daniel Leonard, vice president of technical services at Prisma Health. “Their innovation, imagination, and collaboration with clinical, facility, and management teams have strengthened our

infrastructure and workflows over the past five years. This recognition from ECRI reflects not only their technical excellence but also the strong partnerships that prioritize safety, continuity, and seamless transitions throughout our system.”
“Prisma Health has demonstrated a system-wide commitment to safe, innovative technology deployment,” said Dheerendra Kommala, MD, chief medical officer at ECRI.
“Their integration of reliable infrastructure, intelligent access solutions, and rigorous continuity planning have enabled uninterrupted care every day, even during natural disasters. Prisma Health not only protected their patients and clinicians – they established a blueprint for resilience that the entire healthcare community would do well to emulate.”
To read more about the Prisma Health initiative and past winners of the Health Technology Excellence Award, visit https://ly.ecri.org/HealthTechExcellenceAward.





rtisan Power was founded in the United States by established international battery manufacturers. Its replacement battery packs are widely used by in several industries and government agencies. All of our products are manufactured by ISO 9001 certified manufacturing plants and conform to NEMA’s American National Standard for Portable Rechargeable Cells and Batteries – Safety Standard, C18.2M, Part 2-1999. Artisan Power adheres to all of the same high standards and guidelines applicable to OEM battery packs.
Artisan Power is dedicated to excellence in battery manufacturing. It carefully tests raw materials and selects the finest quality Japanese cells, which are the best in the industry, in order to achieve consistent superior performance.
Co-Owner Samina (Gan) O’Hara recently shared more information about Artisan Power LLC.
Q: WHAT ARE SOME OF THE SERVICES AND PRODUCTS YOU OFFER?
O’HARA: We manufacture high-quality replacement battery packs for medical devices, with a focus on infusion pumps, patient monitors and ventilator support systems. One of our flagship products is the Baxter Sigma Spectrum battery pack, which delivers over 33% more capacity than standard alternatives and uses premium Japanese cells to ensure all-day performance and reliability. We also offer topperforming batteries for devices like the BD Alaris 8015,
Medfusion 3500 and 4000 syringe pumps, and Philips V60 monitors.
Q: HOW DOES YOUR COMPANY STAND OUT IN THE MEDICAL EQUIPMENT FIELD?
O’HARA: Batteries are our specialty: from cell procurement and PCB coding to in-house assembly and rigorous quality control. We design, manufacture, and ship directly, ensuring fresh stock, cost efficiency and a transparent supply chain. Our customers value our responsiveness, ease of collaboration and consistent, dependable delivery.
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY?
O’HARA: We’re excited to introduce this next generation of Artisan Power to the biomedical engineering community – the unsung heroes of healthcare. We’re expanding our catalog to include hard-to-source batteries and have extensive history partnering with customers on special requests or R&D for end-of-life products. Our direct model eliminates middlemen and MOQs. We aim for a seamless and joyful ordering experience – get what you need without hassle.
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE OUR READERS TO KNOW?
O’HARA: Our lines are always open. If you’re having trouble sourcing a battery or need a price match, we’d love to help. Feedback from the community helps us grow our catalog and improve our service. Don’t hesitate to reach out. Beyond medical devices, we support the healthcare ecosystem with our leading edge Vocera communications, two-way radio, scanner and clipper batteries.
For more information, visit artisanpower.com or email sales@artisanpower.com.






BY JOHN WALLACE
There is no shortage of professional conferences for HTM professionals. Whether you consider yourself to be a clinical engineer, a biomed or an HTM professional conferences have a lot to offer.
The AAMI eXchange is one of the largest conferences for the men and women who repair and maintain medical devices. However, it is far from the only conference for HTM professionals. MD Expo is held twice a year and provides many of the same benefits seen at the AAMI eXchange. HTM Mixers are another option offered by MD Publishing. Regional and/or state associations also have meetings and conferences worth attending.
Professionals from hospital in-house biomedical departments as well as those who work for third-party service companies and original equipment manufacturers can benefit greatly from attending conferences. There are
several reasons to attend, but I want to share the top four reasons. The first reason might be a surprise – fun!
REASON #1
It is difficult to list these in order of importance because people have different motivations and objectives. However, the #1 reason to attend a professional conference, in my opinion, is fun! There are some other more traditional reasons to attend, which I will mention soon, but having fun is important! Having fun and being entertained while at a professional conference can provide a reboot. A high energy level helps motivate everyone to hit the ground running when they return to work. Ideas will be shared during the fun times and those same ideas will be shared with a great deal of enthusiasm when each individual returns to work after the conference. Every MD Expo I have attended has been busy and lots of work, but it has also been fun! So, attend a conference for all the right reasons and don’t forget to have fun.
REASON #2
Continuing education is always a major reason to attend a
professional conference. Earning CE credits for certification, re-certification or to reach an individual goal are all important reasons to attend a conference. I suggest looking at the education schedule to determine which classes you plan to attend ahead of time. Look to see if the continuing education is accredited and how many credits you can earn for each session. When you attend the session, arrive early and introduce yourself to the presenter. Sit toward the front of the classroom and take notes. After the presentation, ask any questions you have about the topic. You may even want to set an appointment to discuss the information more in depth later in the day.
Expand your horizons by spending some time in the exhibit hall. It is easy to get comfortable with one company and stop researching what the market has to offer. The exhibit hall has the latest and greatest products and solutions from throughout the nation. Technology is ever evolving. New features and brand-new products could offer a perfect solution to your facility’s latest issue. Also, a new company or a merger of two companies can create opportunities for new expanded offerings.
Networking, networking and networking! A professional conference like MD Expo is the perfect place to connect with peers, re-connect with colleagues and add a few experienced mentors to your list of contacts. I have heard stories of people making lifetime friends with a person they meet in the hotel bar at a MD Expo. However, MD Expo doesn’t leave things to chance. It provides countless ways for attendees and vendors to interact via a keynote address, workshops, educational sessions, exhibit hall hours, a happy hour, final night party and more. Bring a big stack of business cards to hand out, but do more than just shake hands and hand off a card. Make connections. Have conversations. Interact. The rewards that come from a network of peers are amazing.
So, those are my top four reasons to attend a professional conference. The next MD Expo is set for November 10-12 in Dallas, Texas. Come experience all the fun, education, exhibit hall and networking! We even have a few “tools” to help convince your supervisor that you need to attend. You can find the Attendee Toolkit online at MDExpoShow.com/attendee-toolkit/ and you can find out more about the conference at MDExpoShow.com.






ESA700 Series Electrical Safety Analyzers
Our easiest-to-use electrical safety analyzers, ever. The ESA700 Series Electrical Safety Analyzers revolutionize electrical safety testing with precision, versatility and portability. They combine a safety analyzer and patient simulator, making them essential tools for producing comprehensive analysis on medical equipment.
· Small and Portable – Run procedures on the go
· Auxiliary Battery – Eliminate power on/off between testing equipment
· Touchscreen – Complete PMs quickly with the intuitive interface
· Run Procedures without a PC – OneQATM workflow automation software
Transform electrical safety testing with the ESA700 Series electrical safety analyzers today.
For more information, visit flukebiomedical.com/esa700-series
SEPT. 24 at 2PM ET
Registration on WebinarWednesday.live. Eligible for 1 CE credit from the ACI.











Watch these webinars on-demand

The recent Webinar Wednesday Tools of the Trade Live Demo “Maximizing Technician Efficiency Through Integrated Testing” presented by BC Group Director of Business Development Justin Barbour was sponsored by BC Group. The webinar is eligible for 1 CE credit from the ACI. A recording of the webinar is available for on-demand viewing at WebinarWednesday.live.
The Tools of the Trade LIVE Demo featured BC Group’s myBC Connect and myBC Mobile app.
The session introduced biomeds to myBC Connect and the myBC Mobile app, tools designed to optimize field service efficiency. Attendees saw how to eliminate manual documentation, automate test data capture, and access service history from any device. Barbour demonstrated how automated tests guide a technician through a test while reducing error rates and saving time.

“That it wasn’t another cybersecurity program, it was actually useful for biomeds and not IS,” said Casey Celver, Biomed, Legacy Emanuel.
Thank you to today’s sponsor BC Group International. BC Group International is a biomedical test equipment manufacturer and distributor for over 75 brands of products. BC Group’s flagship brand is BC Biomedical. BC Group sells direct and through distributors both domestically and internationally. BC Group provides equipment to medical device manufacturers, independent service companies and hospital biomedical and clinical engineering departments. For more information, please visit BCGroupStore.com
The webinar was popular among HTM professionals with 120 registrations recorded and 64 logged in for the live presentation. The session earned a 3.9 rating on a 5-point scale with 5 being the highest possible rating.
Attendees provided feedback via a survey that included the question, “What was your single biggest takeaway from today’s product demo?”
“The sharing of users’ test results,” said Joseph Cianciolo, BESS, VA Connecticut Healthcare System.
“It looks like biomed is changing again and the future is moving forward with technology innovation, and I need to keep up with it,” said Luis Manuel Ruiz, Biomed Tech I, Arrowhead Regional Medical Center.
“That integrated testing, software running alongside test equipment, could be a useful tool in conducting certain preventive maintenance tasks. Especially on the more complex items,” said Steve Dunn, Biomedical Engineer III, Kaiser Permanente Gaithersburg MOB.
The winner of a Swiss Force Meister Multi-Tool during the webinar was Preston Hueftle, a BMET with Community Hospital in McCook, Nebraska.
To view this presentation on-demand, visit WebinarWednesday.live.










POWERED BY

MedWrench is an online resource for medical equipment service professionals to engage with their peers about medical equipment repairs, source parts and to locate service companies. The following are examples of how the MedWrench community members help each other in the website’s forums.
Q: How do you change the battery
A: Hi Jmlee, Typically you need to remove the metal skirts from the base to gain access. Or loosen the bottom skirt from the base and lift them up using a bungee cord to keep them up.
Good Luck!
Q: I connect the device to the power and I get the error f5b, I need help please, I can’t charge the device.
A: F5b : Signal“CHBR2”is supplied and detected by hardware. Voltage of plus or minus side battery is more than 155V.
In rare cases, the charging-related errors F51, F52 to F5b occurred at the moment when the running brake was released due to a motor failure.There are cases where it happened. In this case, the power cables (CN14, C16) between the left and right motors and the MU DRIVER board can be disconnected one by one and tested, and
the cables connected in the reverse order can be tested to determine which motor is defective
Battery Charged Voltage Over 1. The “120+” and “120-” signals are checked for the error Charged Voltage Over by the operation amplifier A8. The threshold is 4.67V. It is equal to 156V (= 4.67×100/3) as the actual battery voltage (on both plus and minus sides). 2. The detection result is sent as the error signal CHBR2 to the XCONT PCB, then CHON signal turns off and battery charging stops. This signal CHBR2 causes the error message F5b. As shown above, F5b is detected by hardware. There is similar error messages F51 and F53, which are detected by software.
Q: The device sometimes has errors with F13, F14 and F32 when changing shooting positions (small focus => large focus). The device automatically shuts down. When re-on, the device works normally.
A: Hey — those F13, F14, and F32 errors during focus changes (small to large) are typically tied to tube voltage control faults, focus relay issues, or timing mismatches in the high-voltage generator.
If i look at the codes individually instead then F13 likely cause is that the two voltage is too low or unstable during exposure, F-14 the tube voltage control fault is the likely cause an F 32 is a focus switching fault.
To register for a FREE account on MedWrench, scan the QR code or visit medwrench.com

ltrasound systems have been described as the new thermometer because they are often used in the early stages of a patient diagnosis. These important medical devices can be amazing tools for healthcare providers. They can also be a headache when they don’t perform as expected. TechNation recently invited some leading ultrasound service experts to share tips and insights with readers.
Participating in this Roundtable article on ultrasound systems are:
• AllParts Medical Multi-Vendor Ultrasound Modality Manager Joni Charles;
• Solutech Vice President of Sales and Marketing Scott Gassel;
• MW Imaging Corp. Field Service Engineer Ryan Pratt; and
• Innovatus Imaging Vice President Sales and Marketing Matt Tomory.
Q: WHAT ARE THE MOST COMMON ISSUES YOU ENCOUNTER WITH ULTRASOUND SYSTEMS?
CHARLES: The most common issues involve power supplies, monitors, and control panels – components prone to wear over time. Regular preventive maintenance and timely replacement are essential to minimize downtime and ensure reliable system performance.
GASSEL: Ultrasound transducer issues typically fall into two categories – cosmetic and operational failures, both of which




can compromise image quality, patient safety, and diagnostic accuracy. Operational problems like image artifacts or static interference often result from cosmetic damage, such as a cracked acoustic lens, worn cord sheathing, or fluid intrusion. Severe cases of fluid ingress can damage internal electronics and render the transducer inoperable, posing serious risks to clinicians and patients. At Solutech, our advanced dehydration protocol has been proven to restore functionality in even severely compromised transducers, extending equipment life and supporting safe, high-quality patient care.
PRATT: Some of the common issues I see include faulty probe connectors, worn-out trackballs, touchscreens, power supply failures, and software crashes due to corrupted system files or failing hard drives. Overheating probes and image quality concerns are also frequent, especially on systems with aging transducers and without frequent system preventive maintenance.
TOMORY: Back when I started in the ultrasound industry in 1986, the systems were very hardware centric, and the probes were built like tanks, so the main problems were hardware failures of the system. Today, ultrasound systems have very little hardware and are very software driven so software issues are the most common. I strongly recommend backing up system hard drives so when, not if, the software gets corrupted, a backup may be restored. Speaking of backups, the system user files and presets MUST be backed up regularly so they may be restored when restoring the system software. Regarding the probes, they have become the highest frequency and cost associated with ultrasound support. Proper care and utilization of certified and reputable probe repair organization is vital to ensure safety, performance, and longevity.
Q: WHAT TOOLS OR SOFTWARE DO YOU RELY ON FOR CALIBRATION AND PERFORMANCE TESTING?
CHARLES: For calibration and performance assessments, we primarily utilize onboard diagnostics and system logs. These built-in tools allow for efficient troubleshooting and help ensure systems remain in compliance with performance standards without requiring extensive external equipment.
GASSEL: Unlike facilities that use only standard grayscale phantoms, we utilize advanced Doppler flow phantoms that simulate real fluid and blood flow, closely mimicking human physiology. This enables precise evaluation of Doppler and color imaging performance under realistic conditions. As a
result, clinicians can trust their equipment to deliver accurate, high-quality images that support confident diagnoses.
PRATT: I rely on a core set of tools to assess and maintain ultrasound systems. A digital multimeter and safety analyzer are essential for checking power supply integrity and ensuring patient safety. I use an ultrasound phantom to evaluate image quality parameters like resolution and depth accuracy. An antistatic vacuum is also part of routine preventive maintenance to safely clean internal parts of the system to improve airflow without risking ESD damage. On the software side, I make use of the system’s built-in self-test features, which often provide the first clues when something is wrong.
TOMORY: Calibration? I used to use an oscilloscope to calibrate the receivers on the old GE RT3200 systems which only the seasoned readers of this article will remember. Today, the systems are software driven and self-calibrate so service calibration is rare and uses the system diagnostic software. For performance testing, a tissue mimicking phantom should be utilized by trained personnel for preventive maintenance and accreditation purposes. There is a component missing from this question: safety. An electrical safety tester is critical to test not only the safety of the system (enclosure) but can be used to evaluate the electrical safety of the probes themselves. There are expensive and cumbersome devices on the market that can do this, but a basic safety tester is all that is required.
CHARLES: Yes, refurbished ultrasound systems can be a highly viable solution especially for facilities managing budget constraints. When sourced from reputable providers and maintained properly, refurbished units can deliver reliable performance and extend access to diagnostic imaging technologies.
GASSEL: Refurbished ultrasound systems can be a viable option for healthcare facilities when they are restored with the same rigor and attention to detail that Solutech provides. This approach not only extends the life of the equipment but also ensures that clinicians can trust these systems to build the road map for patient care with confidence and precision.
PRATT: Absolutely. When properly refurbished by experienced professionals and paired with a solid warranty,

refurbished systems can provide excellent value and reliability. For facilities with budget constraints, it’s a smart option that doesn’t compromise diagnostic quality.
TOMORY: Absolutely. Like automobiles, ultrasound systems depreciate fast once put into service. Technology has somewhat plateaued with ultrasound systems and there are many high-end systems available in the used market today. The buyer is advised to ensure the system is still supported by the OEM in the event of software updates, has all the features they plan on needing as adding features is very expensive or even cost prohibitive and can be serviced by inhouse teams if that is your service model. The probes should be from a source trusted to ensure and be able to supply data that verify they are OEM form, fit and function, are safe and effective and perform as the OEM intended.
Q: HOW DO NEW SOFTWARE FEATURES OR AI CAPABILITIES AFFECT MAINTENANCE OR TRAINING?
CHARLES: Advancements in software and the integration of AI capabilities have generally improved both maintenance and user training. These enhancements are typically embedded within the system architecture and do not add complexity to service routines. In fact, they often streamline processes and reduce the need for manual intervention.
GASSEL: Emerging AI capabilities and new software features are transforming ultrasound system maintenance and training by enabling predictive diagnostics and real-time performance insights. This evolution from reactive to preventive maintenance enhances system reliability and extends the lifespan of your equipment. At Solutech, we embrace these advancements through ongoing training programs that keep our teams and clients up to date, ensuring optimal
performance and exceptional patient care.
PRATT: New software features and AI capabilities are significantly improving both maintenance and training. Onboard software tools, such as system tests, now provide clear pass/fail indicators to quickly confirm whether a system is functioning properly. Additionally, systems offer more descriptive error messages that help us identify and resolve issues more efficiently. Many platforms also include built-in transducer tests that can detect faulty probes. AI is enhancing clinical training by introducing features designed to reduce variability between users, speed up exam times, and deliver more consistent results. These advancements ultimately lead to more reliable system performance, increased uptime, and greater consistency in clinical use.
TOMORY: Software features and AI continue to evolve and enhance the imaging quality, improve workflows, and assist in diagnoses in some cases but are typically part of the system software or the backups you should be performing. As software becomes more integrated into the systems, the criticality of system and user defined files become much higher.
Q: WHAT CHANGES WOULD YOU LIKE TO SEE FROM MANUFACTURERS IN TERMS OF DESIGN OR SERVICEABILITY?
CHARLES: One improvement that would greatly benefit service teams is the standardization of built-in Pass/Fail diagnostic tools for preventive maintenance. Having a consistent, accessible diagnostic module on every unit would reduce ambiguity during inspections and accelerate troubleshooting across varied equipment models.
GASSEL: Manufacturers are constantly improving their designs to improve patient health. These technological improvements are driving breakthroughs in ultrasound care. As technology continues to evolve, we expect to see serviceability and durability improved, meeting the demands of real-world clinical environments.
PRATT: I would like to see more modular designs that allow quicker replacement of major components, standardized connectors across models, and open access diagnostics that don’t require proprietary dongles and passwords to access. Remote diagnostic tools should be more widely supported to cut back on system downtime.
TOMORY: The pendulum of OEMs opening access to system diagnostics continues to oscillate. I would like to see a fair and equitable solution where the OEMs furnish diagnostics and other proprietary software including software needed when replacement parts are installed to ensure healthcare providers can repair their own systems or designate a qualified repair provider. There is a training component, licensing, etc. but we all have the same goal: ensure safety and access to patients which is affordable to the provider and patient.
Q: WHAT ELSE WOULD YOU LIKE TO SHARE WITH TECHNATION READERS?
CHARLES: Ultrasound systems are becoming more portable, software-driven, and integrated into hospital networks. As a result, service professionals must adapt by combining hardware skills with IT and cybersecurity knowledge. Staying










current and collaborating closely with clinical teams is key to ensuring optimal system performance and efficiency.
GASSEL: Solutech is your trusted partner in healthcare service, parts, and maintenance – delivering 360° solutions for your ultrasound equipment. We’re available 24/7/365, offering highly responsive, professional technical support to dramatically reduce downtime and maximize uptime –backed by an impressive repair yield and a 100% satisfaction rate. ISO 13485:2016 certified for quality and compliance, our systems ensure the highest standards in safety, reliability and performance.
PRATT: One of the most overlooked but critical aspects of ultrasound system care is maintaining an up-to-date backup of system settings. During preventive maintenance, I always ensure that a current backup is created or updated. This can save a lot of time and protect against data loss in the event of hardware failure or corruption. Beyond that, I’d like to emphasize the value of regular maintenance and good documentation to keep these high-demand systems running smoothly with minimal downtime.
TOMORY: When purchasing a system, it is critical to have access to diagnostics, service codes, etc. post warranty. You may or may not want to continue with the OEM after the warranty period but need to ensure you have options. Also, since probes are the most expensive aspect of ultrasound support, are the probes supported by a third party if you choose that option?



























BY K. RICHARD DOUGLAS

In the 1930s, about 40% of all doctor-patient interactions were house calls, compared to just 5% by 1970—but the trend is coming back with modern “hospitalat-home” programs that now operate in 39 states with over 380 approved programs.

In 1931, it was not uncommon for a doctor to pay a visit to their patient at home. The house call accounted for about 40 percent of all doctor interactions with patients during the 1930s. By 1970, that number had dwindled down to five percent.
The house call made sense for many reasons including the patient’s comfort level, enhanced by familiar surroundings, the ability for family members to be nearby, the avoidance of hospital or doctor office expenses and relieving the patient of the need for travel or arranging transportation.
The downside was that the medical equipment available was primarily what the physician could fit into their black bag, the lack of more robust diagnostic equipment, the absence of specialists who might be required for many conditions and a method for continuous monitoring.
The concept of bringing healthcare services to the home has seen a resurgence since those house calls of the 1930s with the resurgence of the “hospital-at-home” (H@H) approach to home healthcare. This new care model recognizes advances in technology alongside an aging population.
The baby-boom generation accounts for 73 million people. That population has been aging and most are in their 60s and 70s, so the need for healthcare has increased with this aging demographic. The home care model may provide patients some relief from the cost of a typical hospital stay.
The benefits offered by the traditional house call remain a constant, with familiar surroundings, the presence of family members and home-cooked food all contributing to the wellness of the patient. In addition, the risk of many pathogens found in hospitals, and contributing to hospital acquired infections (HAIs) may be reduced.
For hospitals and health systems that have been early adapters of the hospital-at-home model, many provide hospitallevel care in the patient’s home. The model can accommodate patients with a myriad of needs, including post-surgical care, wound care, urinary tract infections, dialysis, pneumonia, COPD and blood draws.
There are more than 380 approved hospital-at-home programs in 39 states. Patient outcomes are better than with a hospital stay with lower rates of complications and lower rates of readmissions as well as lower rates of mortality according to a CBS News report. The approach helps alleviate the overcrowding in hospitals seen during the pandemic.
Some of these programs, like the “Advanced Care at Home” program administered by the Mayo Clinic, include a tablet which allows the patient to access a clinician through a video chat. It also shows scheduled appointments.
Other medical equipment in the Mayo Clinic program can include a blood pressure cuff, a scale, a SpO2 measuring device, a personal emergency response bracelet or necklace, a
telephone that dials directly into the patient’s care team, a Wi-Fi extender and a backup power supply in the event of a power outage.
The hospital-at-home or home healthcare approach often requires that medical devices, often found in the clinical setting, are now present in a patient’s home. This brings an entire set of challenges and concerns that require oversight and maintenance workarounds.
Some medical devices that are found in home healthcare include dialysis, oxygen concentrator, blood pressure monitor, use of a CPAP or BiPaP machine, nebulizer and even a hospital bed.
ECRI, in its list of the “Top 10 Health Technology Hazards for 2025” posed the concern that supplemental oxygen can be a fire hazard, listing “Fire Risk in Areas Where Supplemental Oxygen is in Use,” as a potential hazard.
Also, the organization listed “Unmet Technology Support Needs for Home Care Patients” as a concern. ECRI pointed out that many modern medical devices are complex and in the home healthcare environment, this poses concerns when a lay person is responsible for operating a complex medical device.
The organization states: “Devices such as ventilators, dialysis machines, and infusion pumps traditionally have been used in acute care settings under clinical supervision but increasingly are being used in the home.”
Although the cost of home healthcare can be expensive, the cost of a stay in a nursing home can typically run $120,000 annually and a hospital stay of just a night or two can easily cost the patient and their insurance in excess of $10,000. Social Security only covers about 20 percent of nursing home expenses. Medicare will only cover nursing home expenses if the nursing home admission follows a qualifying hospital stay.
Telehealth existed before the COVID-19 pandemic, but it exploded during the pandemic out of necessity. The technology allows a clinician, either through a phone call or through a video chat, to converse with a patient, also often seeing vitals or engage in an assessment of the patient.
Consumer medical technology, including wearable technology, has increased in acceptance with fitness bands, smart watches, VR headsets, AI-powered hearing aids, smart rings and other devices gaining widespread use.
The hospital-at-home approach may put many biomeds outside their comfort zone. While many have experience as mobile techs visiting satellite clinics, the non-clinical environment of a patient’s home is another challenge. Those techs who were previously appliance or cable techs in a past life will find the routine more familiar.
Many hospitals have a home-health department responsible for providing home-based care and the devices sent home with patients. Major retailers, such as Best Buy Health and Amazon One Medical and Amazon Health, have entered the home healthcare market.

If it involves medical equipment, HTM has some involvement. Much of HTMs involvement with the hospital-at-home healthcare model may unfold in the future as the concept becomes a larger percentage of all care.
In a 2023 panel discussion at the Houston MD Expo titled “HTM-at-Home” the participants shared their personal experiences. The discussion, led by Carol Davis-Smith, president of Carol Davis-Smith & Associates, included Dave Scott, CBET, a senior biomedical equipment technician; Rafia Saqib, MSBE, LSSGB, a director of clinical engineering; and Rick Bowie, CBET, a director of clinical engineering.
The panel highlighted the different potential service models that may evolve to eventually become a standard. Davis-Smith posited; “What are the questions we should be asking?”
Davis-Smith pointed out in the discussion that the regulatory world for home health looks different than in the hospital. She asked the panel how they would now define the environment of care outside the hospital environment?
Bowie said that his first experience came at the end of the pandemic when his system was left with excess medical equipment and the question arose, “How do we warehouse this stuff?” That led to to the questions, “How could the stored equipment be used for a hospital-at-home program?” “Would equipment be shipped to the patient as replacements were needed or would there be a mobile van model?”
Saqib said the home health devices are easy to implement. She said that a lot of non-biomeds can implement the technology. She said that they would consider what type of person would be supporting the home health devices.
Davis-Smith asked what the panel thought of the regulator’s approach to home health. How does the environment of care extend to the patient’s home?
Scott said that most wearable devices are not covered under FDA regulations. With home dialysis, the tech must take contemporaneous notes: the water system in the home, an audit of the home environment, filters were changed, PMs were completed and this information is kept in a binder at the home health station.
This allows TJC or state inspectors to review this information.
One participant speculated that even an ICU patient could theoretically be brought home as the model expands. He asked how there can be controls on the home environment? There are water and power requirements to be considered.
Davis-Smith cited ANSI/AAMI HA60601-1-11 as evidence that regulation of the home environment, at least in terms of electrical, is already in existence.
Another session participant pointed out that almost anything is available out in the market, such as on eBay. He said that in some cases, it may get to the point where the hospital sends equipment home with the patient and has the patient sign a waiver, so they simply keep the device.
Davis-Smith said that HTM can influence the implementation of maintenance.
Bowie pointed out that if a patient brings their own CPAP into the hospital, the hospital can regulate its use in the hospital for purposes of infection control since some of those devices are clearly not sterile. In the same regard, if the patient purchases a consumer-grade device from a retailer for use during home care, the hospital needs to have a policy that requires use of their equipment for quality of care.
He asked, “How do you educate the user, the patient or family member in proper use of the equipment?”
HTM may have more of an arms-length involvement in many hospital-at-home settings. That is according to Perry Kirwan, executive, clinical engineering, eQuip-Center for Clinical Technology Management at Sutter Health.
“Most H@H tech works with 1-800 tech support number who will troubleshoot the device, and if it’s determined to be a hardware failure, will just overnight a device to the home. Some models rely on the travelling care navigators to do the exchange and they are provided perhaps a handful of exchange devices to do the swaps,” Kirwan says.
He adds that he hasn’t seen too many models where a biomed team is deployed to do that kind of work unless the
hospital has a model to supply the tech without or with minimal support from a technology provider.
“And frankly, that model isn’t very efficient unless you’re dealing with more substantial tech in the home, [like] home dialysis or patient beds,” Kirwan adds.
He says that most of the time, in cases of repair – the most efficient model for the patient is exchange – rarely will you see the service team attempt a repair in the patient home environment. It’s not zero but ideally you want to swap the device, ensuring it’s working properly, take the broken device and service it in a depot center away from the patient home. There are all kinds of reasons for that – safety, liability, infection prevention, etc.
“Because most H@H programs feature smaller, portable tech – these devices are much easier to swap in the field and in some cases the tech provider will just mail a replacement. Once the patient/family member receives the mailed replacement, they follow a fairly straight forward set of replacement instructions and then a 1-800 technical support line if assistance is needed,” Kirwan adds.
Kirwan says that the bigger challenge may be preventative maintenance. He says that otherwise, repair is relatively easy to conceive and deliver upon.
“Right now, a lot of tech manufacturers in the space have no recommended PM procedures/intervals with their tech. On solid state devices, you can kind of get away with that, however on things more mechanical, PM has to be considered and that’s not easy because it’s hard to schedule visits to the patient home on any kind of reliable basis,” he says.
He says that patients will call with a down device, however they are not a cooperative with a “working” device that just needs scheduled maintenance.
“Some models attempt to get the patient or patient’s family to bring the device into a service center and that service delivery model is moderately effective because the model assumes that the patient or family member has the level of urgency that matches the PM schedule,” Kirwan says.
He says that it is because of this that a lot of H@H models end up working like home health models where anything requiring preventative maintenance just waits until a patient has discharged from the program and then you do maintenance on the devices when they are checked back in to [the]
distribution site and before they are given out to the next program admission.
Wearable technology will play a bigger role in healthcare as the accuracy and capabilities continue to increase. The fitness bands/watches, rings and even clothing are all able to monitor certain vital signs, even measuring heart rhythm, and capture arrhythmias, oxygen levels and sleep quality.
How will wearable technology change healthcare? Scott presented “Wearable Medical Technology: What does it mean for BMETs?” at the Houston MD Expo.
“I think it will help identify problems earlier and will put healthcare more in the people’s hands to take care of their own wellness. Right now, all the data from wearables doesn’t go anywhere. There are starting to be subscription services that wearable owners can subscribe to that will monitor their vital statistics and notify the wearer of concerns as they show,” Scott says.
He says that he thinks AI will play a big part in wearable technology in the very near future.
“More healthcare will take place outside the hospital. I think acute care will still take place at the hospital. Wearable tech and AI will make doctors’ jobs easier. There seems to be more of a shortage of doctors now. The wait times for appointments has gotten worse in the last few years and this in-home tech may help the process in the near future,” Scott says.
Most of the wearables that consumers purchase are only consumer-grade and would not be up to the higher standards required of medical-grade.
“I think when a patient is in the hospital, the patient will most likely be put on hospital medical equipment, but I’ve seen patients bring home-use BiPaPs and CPAPs to the hospital now. I could see hospitals having to make rules regarding the use of wearable devices in the future if it becomes a problem. Or possibly, it is the same monitoring system? It could be but isn’t today,” Scott says.

While telehealth existed before COVID-19, its use exploded during the pandemic, enabling clinicians to assess patients through phone or video calls—often with access to vital signs and remote monitoring.
As the hospital-at-home care model increases in acceptance and use, the likelihood that an HTM professional will have some exposure to this delivery method will increase. There will be a role for the biomed, even if it doesn’t mean visiting the patient’s home. Like cybersecurity and wireless technology; it isn’t going away.

BY VICKI SALEMI
In a noisy world where multi-tasking is prevalent, how can you quiet your mind?
Whether you’re scrolling on social media or having a conversation with a colleague, chances are, you may feel impatient with a decreasing attention span. Take a moment to ask yourself how many windows you have open on your screen and how many profiles you just scrolled by on social media within 30 seconds.
In turn, constant streams of noise equate to continuous distractions and decreased focus. Suffice it to say, this doesn’t translate well into work when we need to focus on productivity and the quality of work without having constant interruptions. You may notice you’re drafting three emails simultaneously and your brain has just as many drafts in motion, yet nothing substantial is accomplished. It’s as if we’re on a large hamster wheel to nowhere. All of this multitasking doesn’t bode well. It’s a one-way road to being overwhelmed.
As we focus on attention spans, underneath it is the
intention for clarity, minimalism, doing less and achieving more.
Dr. Evita Singh, psychiatrist at Ohio State Department of Psychiatry and Behavioral Health, told The New York Post, “When people are multitasking, when they have so many things in their mind that they’re thinking about, they can get exhausted. And then it’s really hard to enjoy things, which can then lead to depression or anxiety.”
To help her patients boost their ability to focus, she coined the “take five” method. Think of it as an acronym with digestible actionable items: T — take breaks often, A — actively engage in just one task at hand, K — keep distractions to a minimum, E — eliminate multitasking and F — take five minutes to refocus by having a mini workout, doing mindfulness or a fun activity.
In our society that focuses more on doing rather than being, and in various workplaces that prioritize an unrealistic fast pace and output rather than preventing burnout, you’ll need to develop a muscle to push back. Start small. Schedule breaks on your calendar and force yourself to stick to them. Something as simple as a five-minute tech
break without your device combined with another activity such as walking outside your office to get a quick breath of fresh air and sunlight can put spring in your step! We’re allowed to take breaks at work. Our posture, our eyes, our everything needs to recharge.
The funny thing is, sometimes when we detach, new thoughts that are meaningful and important will emerge into our heads. For instance, by extending this beyond five minutes to let’s say, a 15-minute quick power walk mid-day, we’re prioritizing making space for ourselves and whatever else bubbles up – often, it’s work.
These small steps can move mountains. By being intentional to take a five- to 10-minute timeout every hour from tech, per Singh’s recommendations, you can attempt to reduce distractions. Start with five minutes and remember distractions and multitasking are not helpful; have a plan with your fun activity to refocus.

Vicki Salemi is a career expert for Monster, an author, a speaker and consultant, TV commentator and former corporate recruiter. Send your questions to hello@vickisalemi.com



Diagnostic Solutions is a customer service based parts provider that specializes in all imaging modalities and manufacturers. Created to offer hospitals and ISO’s a cost effective and time saving solution for ordering imaging replacement parts, equipment moves, ultrasound probe repair and on-site service. Contact us today, we are confident you will see us as THE Parts Solution!

BY JOIE N. MARHEFKA, PH.D.
As I write this column, the 4th of July holiday is approaching.
Summer definitely provides some much-needed downtime for me, as our students are doing internships, and I’m not teaching any other classes. I use some of this time to get caught up on administrative tasks and other work, but I also like to engage in other activities that can improve my technical skills, soft skills, work-life balance and overall health. In this column, I will share some ideas for combining summer fun with sharpening skills.
Summer is a great time to take a class to improve soft skills, learn something interesting or prepare for a job search.
Our local library offers a variety of courses on resume writing and job searching, which would benefit students as well as anyone looking for a career change. The local community colleges offer courses in writing and public speaking. Classes on computer programming languages and on artificial intelligence, as well as some other technical topics, are available through the community college and the library.
Summer is also a great time to catch up on some reading and podcasts. I like to create a book list during the year of things I hope to read over the summer. In addition to some fun reading, I try to include books on topics that will help me in my career, such as leadership and technology. A few books on my current list are “Teaching with AI,” “Leading in a Changing World,” “Remember Who You Are” and “Let the Story do the Work.” (I’d love to hear what’s on your list). I also enjoy listening to podcasts. Bearded Biomed is one of
my favorites, which is HTM focused. TechNation also has a great list of HTM related podcasts https://1technation.com/ category/podcasts/.
Summer is also a great time to attend a conference. I recently attended AAMI eXchange, where I learned about the latest trends and technologies in HTM and had the opportunity to network with other professionals in the field. HTM Mixers are also typically held over the summer. If you don’t have time or funding to attend a conference, many HTM-related webinars are available, and these great opportunities to hear about issues affecting HTM.
Volunteering is another great way to spend some free
volunteer opportunities are available through food banks, churches and other community organizations.
Finally, summer can be a good time to slow down a bit and focus on improving health and work-life balance. Taking a walk outside is a simple way to improve physical fitness that can benefit mental health. A yoga class or other fitness classes can be a great way to clear your mind while improving your health. Community colleges, gyms and yoga studios offer plenty of options.
I hope you all had a wonderful summer and perhaps consider some of these activities in summer’s last days (or next summer)!










Some one-third of Americans live in a state with a Right to Repair law that requires manufacturers to provide fair access to repair materials including spare parts and service manuals. U.S. PIRG Education Fund’s new report, Leaders and Laggards II, finds that, despite these requirements, many manufacturers do not provide the things people need to fix their stuff.
The new scorecard grades 25 products across five categories for how easily and thoroughly consumers can access repair documentation and spare parts. Of those products, 40% received a D or an F, 28% received Bs or Cs, and 32% received As. When the U.S. Pirg tried to get the repair materials the law requires manufacturers to provide, we could not access a repair manual for 48%, and 44% had no spare parts available.
“The premise of Right to Repair is simple: It’s our stuff, and we should be allowed to fix it – not just in theory, in the real world,” explained Nathan Proctor, senior director of U.S. PIRG Education Fund’s Right to Repair Campaign, and the report’s co-author. “It’s time for manufacturers to better
comply with the growing number of state repair laws, and for attorneys general in impacted states to step in when companies fail to.”
On July 1, 2024, the Right to Repair community celebrated “Repair Independence Day,” as Right to Repair laws took effect in California and Minnesota. Both of those laws improved upon New York’s pioneering consumer Right to Repair law, which took effect in December 2023.
Thanks to continued advocacy, new laws in Colorado, Oregon, Connecticut, Texas and Washington will begin to require access to repair options for similar products over the coming year and a half. Despite this progress, the new report found that manufacturers are not doing enough to support the repair of their products.
Even though consumer electronics companies are doing well with repair material availability for smartphones and laptops, tablet repair materials lag behind.
MSI, Atari, and Sony all fail to provide any repair materials for the game consoles reviewed.
“The report makes it clear that we need more enforcement to ensure that people can fix our electronics and appliances,” commented Gay Gordon-Byrne, Executive Director of Repair.org, the coalition working on Right to Repair.






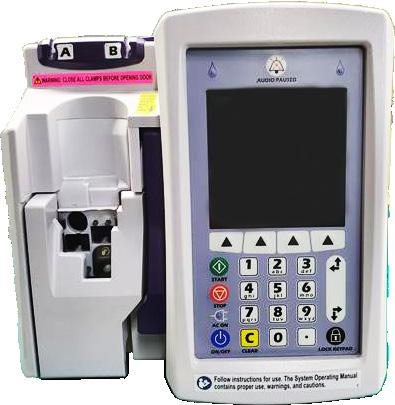
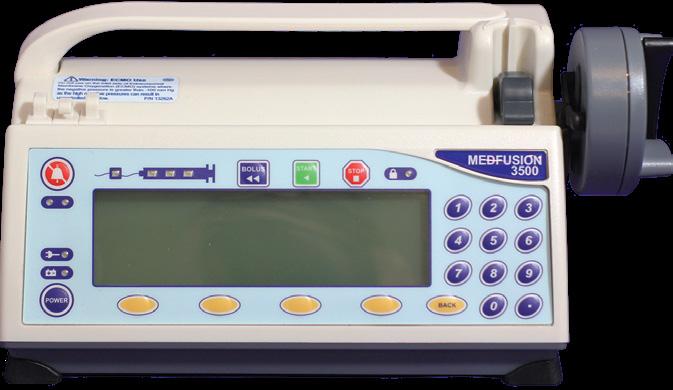











BY PHIL ENGLERT
As healthcare systems become increasingly digitized, the hyper-integration of innovative technologies into clinical environments demands a new approach to cybersecurity training. Social engineering remains a paramount threat to healthcare organizations, exploiting the human element, often the most vulnerable link in the security chain.
Generic training approaches prove insufficient against sophisticated attackers who leverage human psychology, the inherent helpfulness culture in healthcare, and the increasing use of artificial Intelligence to mimic human traits in text, email, audio, and video make it more challenging to detect phishing, smishing, and deep fake voice and image cloning. Personabased training customizes educational programs tailored to healthcare professionals’ specific roles, workflows, goals, and pain points, and has emerged as an effective strategy to improve educational effectiveness. This approach ensures that physicians, clinical staff, biomedical engineers and facility support staff can manage the clinical and operational risks associated with digitally connected medical devices, clinical applications, and essential infrastructure systems such as HVAC, medical gases and water.
Tailored training modifications are proposed for each persona, emphasizing relevant content, appropriate delivery methods (such as micro-learning for busy clinicians and advanced simulations for IT staff), and key behavioral nudges. The underpinning strategies for an effective program include fostering a strong security culture, ensuring continuous and evolving training, leveraging realistic simulations, establishing clear incident reporting protocols, integrating HIPAA compliance, measuring training effectiveness, and
utilizing established frameworks. Significant challenges include sustaining engagement in high-stress, high-turnover environments and demonstrating the return on investment (ROI) of such tailored training by moving beyond mere compliance to tangible risk reduction. Investing in robust, persona-based cybersecurity training is not just a regulatory necessity but a critical investment in patient safety, data integrity, and overall organizational resilience in the face of ever-evolving social engineering threats.
Traditional training models often adopt a one-size-fitsall approach, which fails to address the nuanced needs of different healthcare roles. Persona-based training, by contrast, recognizes that a nurse, a physician, and a facility engineer each interact with technology in distinct ways. By aligning training content with these unique perspectives, healthcare organizations can foster safer, more efficient and more responsive environments.
Awareness of how digital anomalies can impact patient care delivery is critical in the context of large language models (LLMs) and AI-driven systems, which are now embedded in everything from electronic health records (EHRs) to medical devices and predictive maintenance platforms. These systems can enhance care delivery and introduce new vulnerabilities, especially when they interface with critical clinical and facility systems.
Modern medical devices such as infusion pumps, ventilators, and patient monitors are increasingly networked and reliant on real-time data exchange for clinical workflows. Interruptions to these systems, whether due to software errors, cyberattacks, or AI misinterpretation, can have immediate and severe clinical consequences. For example, an AI-generated dosage recommendation that is not verified correctly could lead to medication errors.
Persona-based training prepares clinicians to recognize and respond to such risks. Nurses and physicians, for instance, can be trained to cross-check AI outputs against clinical guidelines. Biomedical engineers are trained to monitor

device logs for signs of malfunction or tampering. This layered approach ensures that each team member understands their role in maintaining device integrity and patient safety.
LLMs also transform clinical workflows by automating documentation, assisting in diagnostics, and supporting decision-making. While these tools can reduce administrative burden and improve care coordination, they are not infallible. LLMs like GPT-4 and Med-PaLM2 have demonstrated remarkable clinical reasoning, documentation and decision support capabilities. Misinterpretation of clinical language or context by an LLM can lead to flawed recommendations or incomplete records. LLMs can interface with electronic health records (EHRs), medical imaging systems, and even voice-controlled devices, raising the stakes for cybersecurity and operational continuity. Their integration into healthcare environments introduces new complexities in detecting and protecting against cybersecurity-induced errors.
Persona-based training helps clinicians understand these tools’ capabilities and limitations. Physicians, for example, can be trained to use LLMs as a second opinion rather than a primary decision-maker. Administrative staff can learn to validate AI-generated documentation before finalizing patient records. Human oversight remains central to clinical care.
Facility infrastructure is another critical area where AI and digital systems are making inroads. Smart HVAC systems regulate temperature and air quality in operating rooms and isolation units; medical gas systems deliver oxygen and anesthesia; and water systems support sterilization and hygiene. These systems are increasingly monitored and controlled by AI-driven platforms that can predict failures and optimize performance.
However, interruptions or malfunctions in these systems, whether due to AI errors or external threats, can compromise patient safety. For instance, a failure in the HVAC system could
disrupt surgical conditions, while contamination in the water supply could lead to infection outbreaks.
Persona-based training ensures that facility managers and support staff are equipped to interpret AI-generated alerts, perform manual overrides, and coordinate with clinical teams during emergencies. This cross-functional awareness is essential for maintaining operational continuity and patient safety.
The benefits of persona-based training include rolespecific protocols that reduce the likelihood and impact of successful cyberattacks. Staff are also prepared to respond to system interruptions, even if not cyber-induced. Personabased training improves retention and creates a shared understanding across clinical and facility teams. Finally, staff become better at critically evaluating and alerting on system anomalies and can adapt to evolving AI technologies and workflows.
Persona-based training can help safeguard clinical systems and infrastructure in the age of digital medicine. In an era where healthcare increasingly depends on digital systems and AI, persona-based training is not just a best practice but a necessity. By tailoring education to the specific roles within a healthcare organization, this approach enhances safety, improves system resilience, and ensures that technology is a tool for care, not a source of risk. Training must evolve as LLMs and intelligent systems continue to advance to ensure users can operate them safely, securely and effectively.

Phil Englert is vice president medical device security with Health-ISAC Inc.

We’d love to feature you, your colleague or the entire department in one of TechNation’s monthly features!
1
2 Professional of the Month, Shifting Gears and Department of the Month!
3
Think of a Biomed/CE Department deserving of recognition. Scan the QR code or email editor@mdpublishing.com. We will contact you for additional information if your nomination is accepted!
TheHoustonMethodistBiomedicalEngineeringDepartment uston,Texas oneofthebestknowncitiesinAmerica.Thecity andsurroundingcommunitiesforma metropolisthatextends theGalvestonBay.Withapopulationexceeding 2.3million, isthefourthlargest cityintheU.S.,covering637square miles.Houstonwasfounded 1836 andoffersattractionslikeSpace CenterHouston,thelargestfinearts museumintheSouthwestandthe downtownaquarium. cityofthissizedependsonhealthcaresystemswiththe capacitytoservesuch largepopulation.Thatcapabilityis embraced HoustonMethodistHospital,affiliatedhospitals andotherfacilitiesscatteredacrosstheHoustonmetroarea. Werecentlyprofiledasmalltwo-techniciandepartment,but takes biomeddepartmentattheotherend thespectrum managemedicaldevices such large-scalehealth network.Witheighthospitals,anacademicinstituteand2,509 operatingbeds,HoustonMethodistincludes27,947employees,withmanyworkinginbiomed.The85-memberbiomedicalengineeringdepartment ledbySystemDirector AnthonyMaroulis.Othermembersofleadershipinclude CampusDirectorofClinicalEngineeringMarcBateman, Managers ClinicalEngineeringTerresaEverhart,Javier Ruiz,MiguelMezaandCoreaunJacksonandProgram CoordinatorsBrandonHightandNathanStathos.Theteam’s clinicalengineersincludeZachSmith,CristianDelgado, BailynPiecewiczandHaniKhalil.Thedepartmentalso consistsoftwoadministrationassistants,fivebiomed equipmenttechleads, biomedequipmenttech 23 biomedequipmenttechIIIs,15biomedequipmenttechIs, biomedradiologyserviceengineersand1dataentry specialist.Batemansaysthatthebiomedteamservicesmorethan 91,000medicaldevicesin-housethankstotheexceptional trainingoptionsavailabletothedepartment’stechnicians. Inadditiontomanagingequipmentattheeighthospitals, thelargebiomedteamalsoservesmorethan20orthopedic andsportsmedicinelocationsofferingphysicalandoccupationaltherapyacrosstheGreaterHoustonarea. PhysicianTheyarealsoresponsibleforequipmentattheSpecialty Groupwith848physiciansat191locationsandthe PrimaryCareGroupwith169physiciansat42locations. ThehospitalisaffiliatedwithWeillCornellMedicine, NewYork-PresbyterianHospitalandtheTexasAnnual Conference UnitedMethodistChurch.TheHoustonMethodistAcademicInstitute,whichis researchand educationinstitute,has facultyof742,with2,110credentialedresearchers.BIGTEAM,BIGPROJECTS ThechallengestoaddressCOVID-19surgestaxedthe resourcesofhealthcarefacilitiesacrossthenation,butit requiredinnovationonagrandscaleforthebiomedteamat HoustonMethodist.“AttheonsetoftheCOVID-19pandemic,therewas glaringneedtoreduceexposuretopatientswithinthe hospitalforourRTdepartment.Thankfully,ourHamiltonG5 ventilatorshaveadetachableinteractionpanel.RTasked haveventsinsidetheCOVIDroomandplacetheinteraction paneloutsidetominimizeexposurefortheRTtherapist go insidetheroom.Theinteractionpanelwasattachedtoa tableoutsidethepatientroomandwehad dothisfor 90-100G5patientrooms,”Smithsays. Hesaysthattogetherwiththe medicaldeviceintegrationteam,theysuccessfullyopened virtualICU(vICU).“We had keyroletoplayinensuringthepatientphysiologicalmonitorswerecapable beingusedinthisnew,innovative setting,”Smithsays.Theteamtackledmanyotherprojectsrelated thevICU tomeettheneedsofpatientsandvisitorsduringthe pandemic.AnotherprojectwascenteredaroundAlarispump interoperabilityandtyingthemtopatientrecords. “Pharmacy,nursing,biomed,multipleITgroups,andthe
’90swhen highschoolfriend,JeffRedmon,was racing theMotorplexontheweekends. was helpinghimcrewand someseattimehereand there on some faster bikes and rode for some teams inDivision4,thenstartedracingsome bracketsandgrudgeracesinthelate’90s,”Barronsays. In2010,hewasintroduced theprostock motorcycleclassby mutualacquaintanceofUnderdahlRacingfamily. “When approachedthematthe Nationalsin Texas,andaskedwhat wouldtake transition prostockmotorcycle,GregUnderdahltoldmehe neededtoseeif couldhandleabike thatmagni-tudebyjustholdingthethrottlewideopenand 660releasingtheclutch;thenprogressedto330feet, feetandprogressinginto quarter-mile(1,320 feet)passinacoupleoftestsessions,”Barronsays. Underdahl Barron that felt comfortablesellinghimone hisbikesandhelpedBarrongetlicensedshortlyafter Suzukiheboughtin 2011. “Ialwayshad familymemberridinganything fromHondaCR125s,SuzukiRM250,YamahaYZ490 twostroke bikesgrowingup,butalwaysstayed uncles,interestedinthedragstripwhenwatchingmydad, grandpa,cousinsracemanylatenightsand playing ridingaround thepits,”Barronremembers. suburbsaysthatin1985,thefamilyrelocatedfrom ofFortWorthtoWaxahachie,Texas.Waxahachiejusthappenedto 10minutesfroma drivernationaldragstrip,builtbyformerNHRAfunnycar BillyMeyer,whichwascompletedin1986.“Itseemedlikeitwasmydestiny continue the goingtraditionofourfamily’sdragracinghistoryafter thefirstnationaleventheldthereandnever missed opportunitysince.All family,includingmykids,raceddownthatstripincompetition. am immenselyproud thefourgenerationsofdragracersthatstartedbefore wasbornwithmygrandpaHis1970,”Barronsays. coupesgrandpaanddadhadmatching1939Chevy Barron,”theyracedunderthemoniker“TheRed play theirlastnametakenfromthe famousWorldWar pilot. Snoopy“Irememberseeingthepaintedcoupeswith flyinghisdoghouseon sides. rememberas kidwatching CharlieBrownandPeanuts WorldserieswhereSnoopyoftendreamedoffightingthe War pilot,BaronManfredVonRichthofen,aka,TheRedBaron. stillhavemanyofmygrandinma’strophiesfromdragracingwhenshecompeted Ft.thePowderPuffWomen’sDragRacingSeriesin Worth thelate1960sandearly1970sbeforewasborn,”Barronsays. Barronsaysthat triestoattendeventsclose
1/6/23 9:08

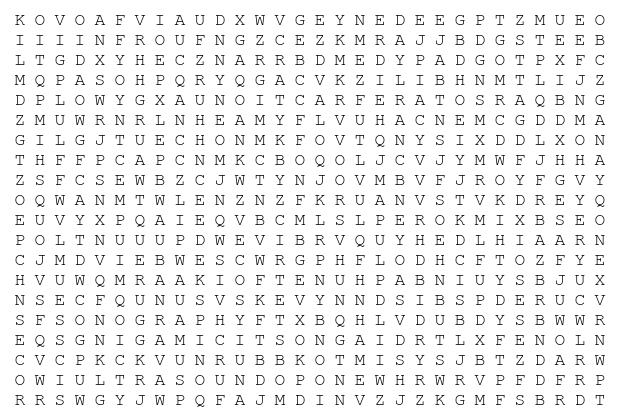
The words can appear horizontally, vertically, diagonally, and may be spelled forwards or backwards.
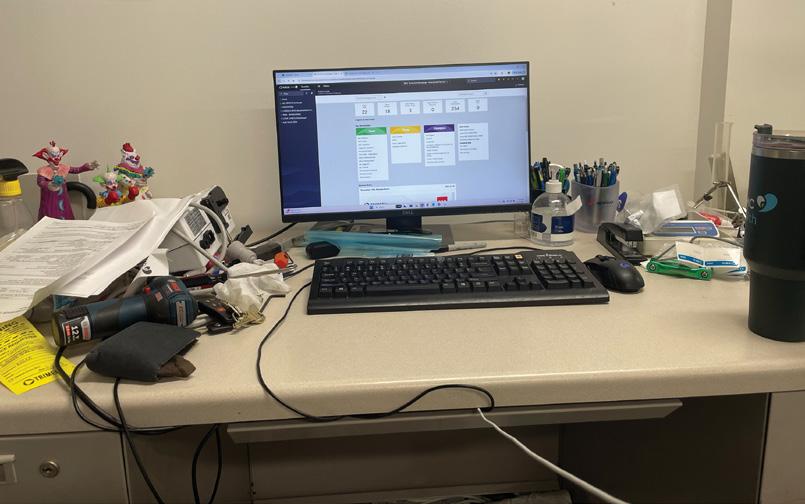
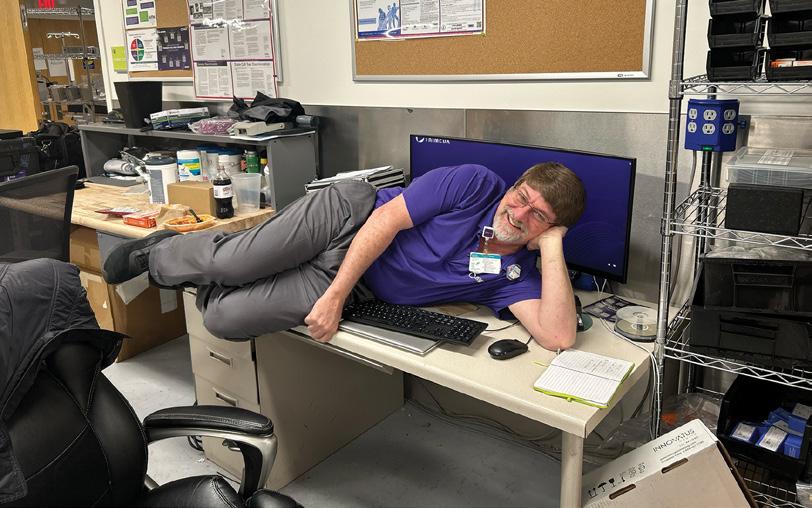
1. Ultrasound
2. Transducer
3. Diagnostic Imaging
4. Probe
5. Portable
6. Abdominal
7. Vascular
8. Obstetric
9. Refraction
10. Frequency
11. Echo
12. Sonography
Devin Fleming BMET II, Children’s Hospital New Orleans (Trimedx)
Five things I have at my desk are...
• Monitor
• Laptop
• Multimeter
• Dremel
• Soldering Iron and
• Imaging Engineer Billy Temple
Submit your bench to be featured in TechNation at 1technation.com/my-bench/. You could win a $25 Amazon gift card via the “What’s On Your Bench” Contest!





Admar Neuro admarneuro.com • 728-900-3969
AM Bickford ambickford.com • 800-795-3062
BC Group bcgroupstore.com.com • 314-638-3800
FiberTech Medical fibertechmedical.com • 866-628-6888
Interlight interlightus.com • 800-743-0005
Jet Medical jetmedical.com • 714-937-0809
Metropolis International metropolismedical.com • 718-371-6026
Ozark Biomedical ozarkbiomedical.com • 800-457-7576
PM Biomedical pmbiomedical.com • 800-777-6474
Pronk Technologies, Inc. pronktech.com • 800-609-9802
Secure Mount securemount.com • 517-784-9613
Tri-Imaging Solutions triimaging.com • 855-401-4888





















Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.


XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking


Tri-Imaging Solutions introduces a cutting-edge management, engineer performance, and system diagnostic tools and video tutorials, and streamlines Designed for efficiency, the platform minimizes setting a new standard for reliability in medical


XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.













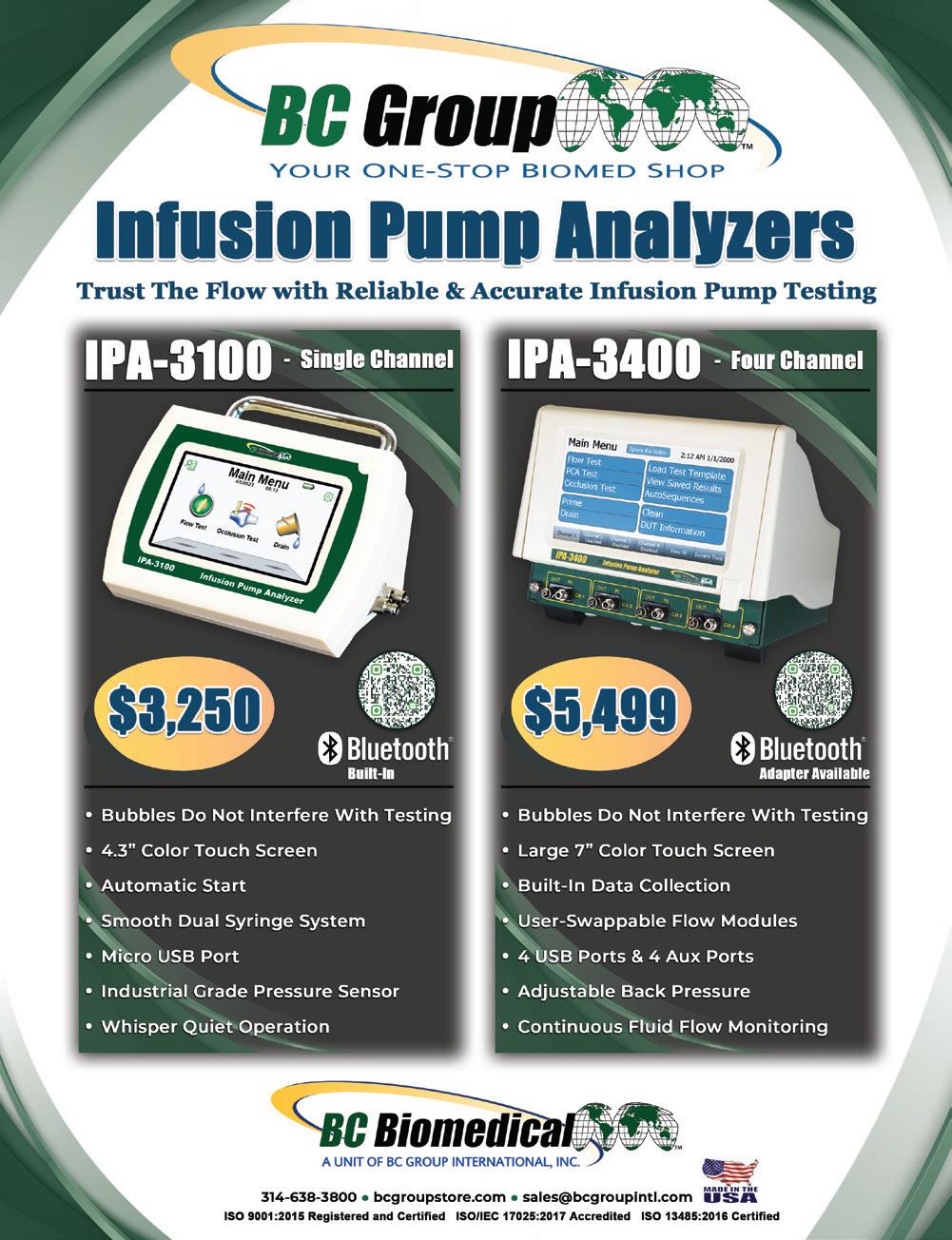
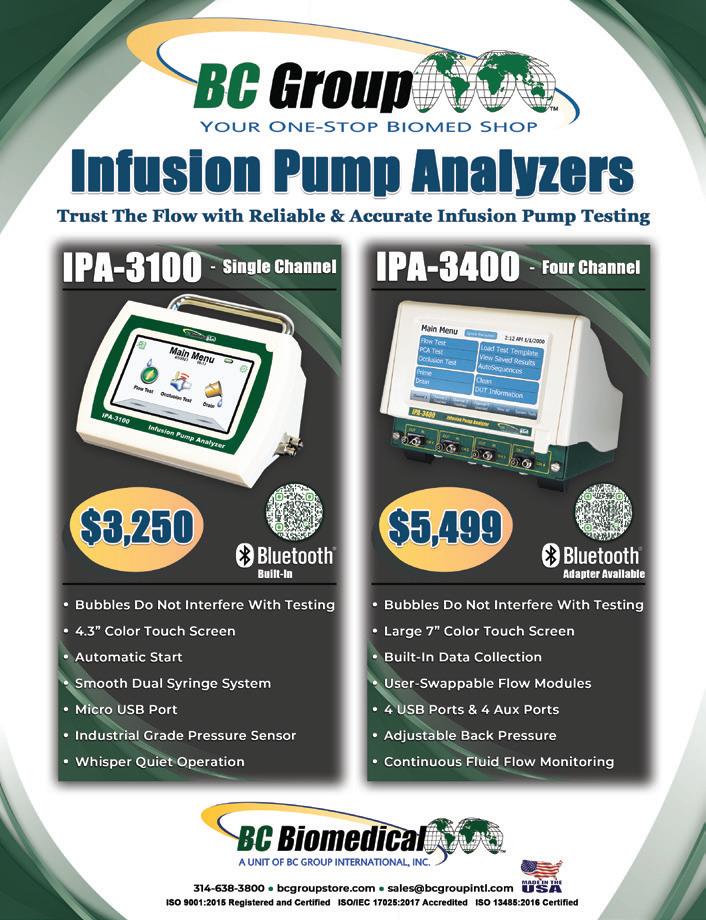
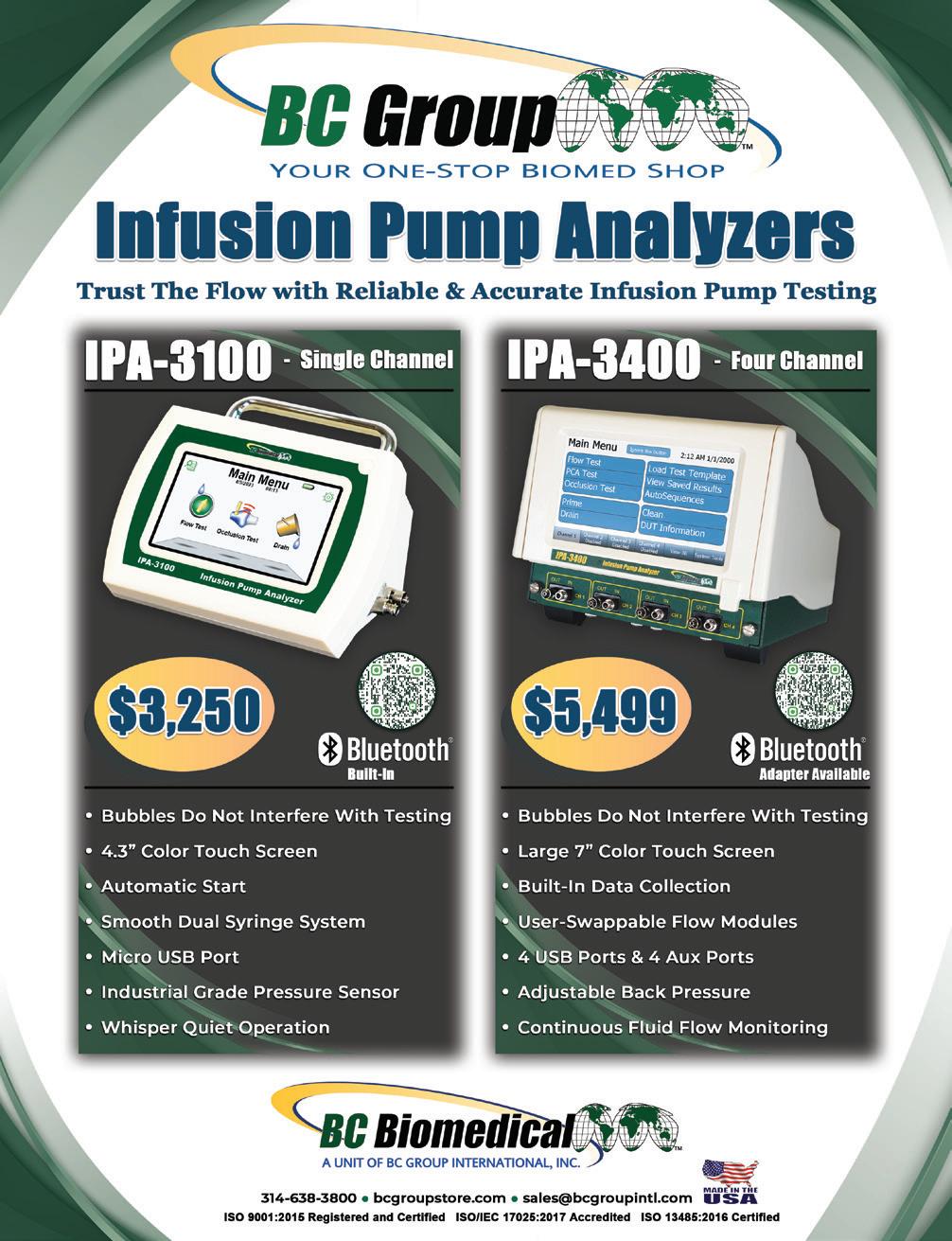


Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.



Tri-Imaging Solutions introduces a cutting-edge platform that management, engineer performance, and system monitoring. diagnostic tools and video tutorials, and streamlines parts Designed for efficiency, the platform minimizes downtime and setting a new standard for reliability in medical imaging.
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking
Solutions
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
10 Fant Industrial Dr Madison, Tennessee 855.401.4888
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
XperTIS proactively monit health, supports engineers in enhances the supply chain giving teams seamless acce ordering and order tracking
Struggling with staffing gaps in your biomedical or clinical engineering department? MultiMedical Systems provides expert short- and long-term staffing solutions to keep your operations seamless From preventative maintenance to equipment repair, our skilled technicians integrate quickly and efficiently with your team minimizing downtime and maximizing patient care

XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering. This helps maximize uptime and minimize repair costs.
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs

10 Fant Industrial Dr. Madison, Tennessee 855.401.4888

Anesthesia
Contrast Media Injectors
Cyber Security
Oxygen Blender






















The 2022 MD Expo held in Atlanta celebrating the 20th anniversary of the first ever MD Expo!
MD Expo returned to its roots in Atlanta—where it first began nearly two decades prior—in April 2022 to celebrate its 20th anniversary.




MD Expo SoCal continued the tradition of connecting HTM professionals in October 2022.
SEPTEMBER 17
SPONSORED BY

WEBINAR WEDNESDAY
Save the date for this live webinar. Participation is eligible for 1 CE credit from the ACI.
SEPTEMBER 24
SPONSORED BY

TOOLS OF THE TRADE
Save the date for this live webinar. Participation is eligible for 1 CE credit from the ACI.
SPONSORED BY Laser Safety in Healthcare Technology: Compliance, Maintenance and Risk Mitigation
SPONSORED BY Smart Tools for Smart Operations: AI and Technology in HTM/HFM
SPONSORED BY

TOOLS OF THE TRADE AAMI’s New CEU Journal and The Importance of ACI Certification

SPONSORED BY
Why Training is Key to a Strong Workforce
All webinars, podcast, and product demos are eligible for 1 CE credit from the ACI.








Choose the right capital equipment, supplies, and health IT for your facility with guidance from ECRI Instituteʼs team of biomedical and cybersecurity engineers, clinicians, and human factors experts.



ECRI is a trusted authority on healthcare technologies that improve the quality and cost-effectiveness of patient care.
Get test results and ratings, free of vendor bias


Stay on top of risks with hazard and recall notifications
Compare technology with overviews and specifications
Learn more at www.ecri.org/solutions/device-evaluations or contact us today at 610-825-6000, x5891.



