





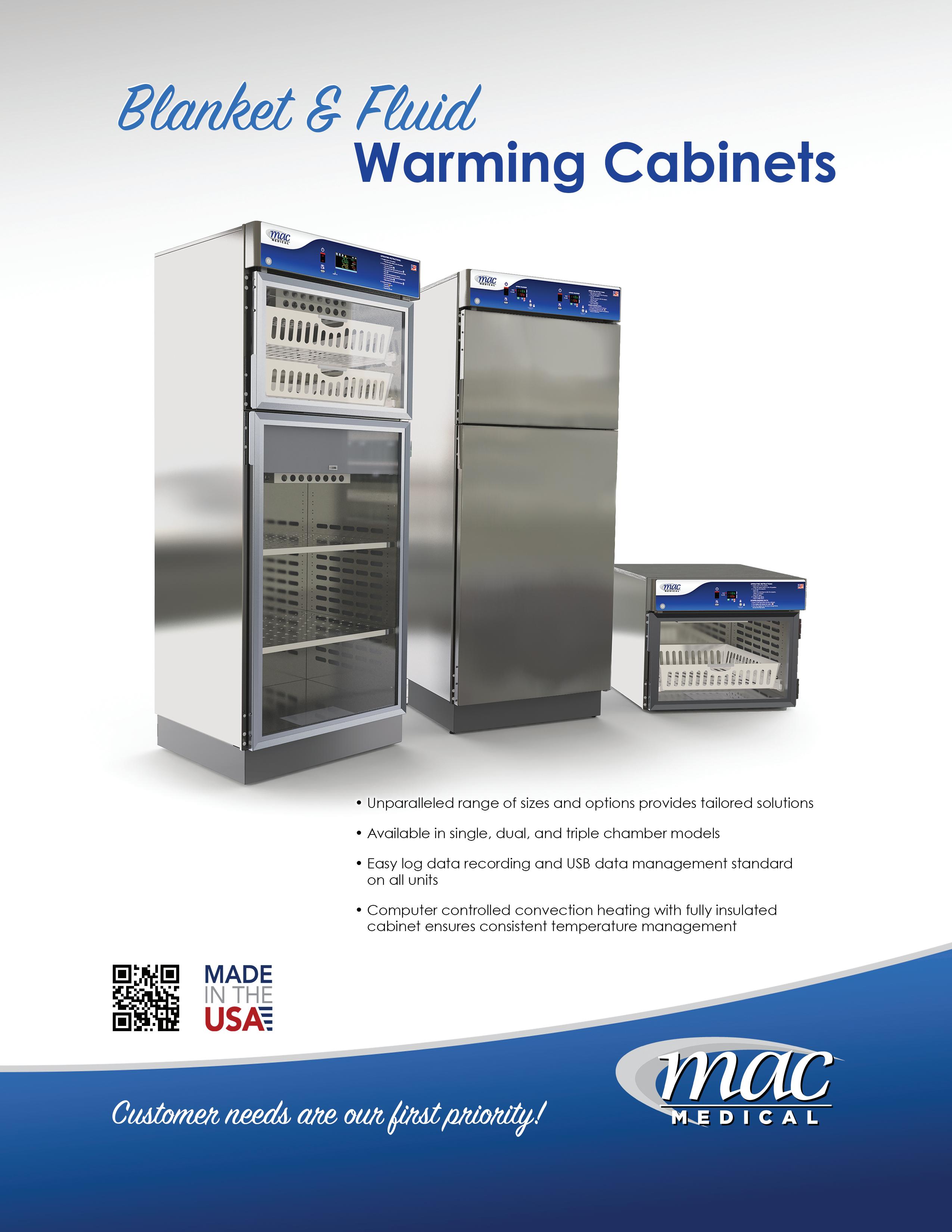
for use with Ruhof’s Prepzyme® Forever Wet Enzymatic Pre-Cleaner
The cleaning process begins at the point of use. When soils dry, they become harder to remove and increase the risk of corrosion, biofilm formation, and HAI’s. The Forever Wet Auto Sprayer delivers a consistent application of Prepzyme® Forever Wet in less than half the time—keeping instruments moist for up to 72 hours.











Enclosed and vented dispensing chamber for complete operator and specimen safety
Built-in scale for automatic specimen weighing

Programmed maximum and minimum formalin levels for correct ratio

Printed labels with customizable fields for complete documentation

One-way valve lids for automatic filling and formalin fume protection

Easy to use touchscreen with on-board tutorial videos for training









30 MARKET ANALYSIS
The Rise of Single-Use: Medical Disposables Market Set for Explosive Growth

44 FITNESS
Stabilization-Focused Movements Deliver Benefits
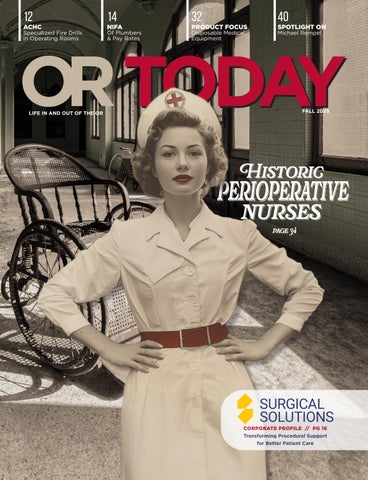
Discover the evolution of perioperative nursing from its roots with Florence Nightingale to its emergence as the first recognized nursing specialty. This feature highlights pioneering figures, key innovations, and the development of professional organizations that shaped perioperative practice into the highly specialized, patient-focused field it is today.

48 EQ FACTOR
Beyond the Box: Behaviors Demystified
OR Today (Vol. 25, Issue #4) Fall 2025 is published quarterly by MD Publishing, 1155 Senoia Road, Ste. 200 Tyrone, GA 30290. POSTMASTER: See address changes to OR Today at 1155 Senoia Road, Ste. 200 Tyrone, GA 30290. For subscription information visit www.ortoday.com. The information and opinions expressed in the articles and advertisements herein are those of the writer and/or advertiser, and not necessarily those of the publisher. Reproduction in whole or in part without written permission is prohibited. © 2025


PUBLISHER
John M. Krieg
john@mdpublishing.com
VICE PRESIDENT
Kristin Leavoy kristin@mdpublishing.com
VICE
Jayme McKelvey jayme@mdpublishing.com
EDITOR
John Wallace editor@mdpublishing.com
ART DEPARTMENT
Karlee Gower
Taylor Hayes
Alicia Brown
ACCOUNT EXECUTIVES
Megan Cabot
Emily Hise
DIGITAL SERVICES
Cindy Galindo
Kennedy Krieg
EVENTS
Kristin Leavoy
ACCOUNTING
Diane Costea WEBINARS
Linda Hasluem
EDITORIAL BOARD
Vangie Dennis, MSN, RN, CNOR, CMLSO Assistant Vice President, Perioperative Services, AnMed
Justin Fontenot, DNP, RN, NEA-BC, FAADN Associate Professor, Tulane University School of Medicine, New Orleans, LA
Natalie Lind, Education Director for the Healthcare Sterile Processing Association, HSPA
Pat Thornton, MSM, RN, CNOR Perioperative Consultant, RNFA Dermatology Institute
Dawn Whiteside, DNP, MSN, RN, CNOR, NPD-BC, RNFA, Director of Education, CCI
Julie Williamson, BA Director of Communications,

Preoperative skin antisepsis is a critical part of reducing the bacteria on the skin that may cause infection prior to surgery.1 There are many factors to consider in the determination of which antiseptic to use for a particular patient.
ChloraPrep™ Skin Prep for:
Proven efficacy
Backed by over 60 clinical studies, ChloraPrep stands out with scientifically proven results.
Persistent protection
Enjoy peace of mind of persistence for at least 7-days.2,3
Orange tint
Our hi-lite orange tint helps mark the prep area and reduces the risk of clinical misdiagnosis based on skin coloring during post op care.4,5,6,7
Fully sterile
BD® sterile applicators and solutions help prevent the risk of intrinsic and extrinsic contamination.8,9

ChloraPrep™ Skin Prep demonstrates at least PERSISTENCE1,2



Follow the QR Code to discover the difference of unmatched experience on proven performance.
1. Association of preoperative Registered Nurses (AORN). Guidelines: Key Takeaways for Patient Skin Antisepsis. https://www.aorn.org/article/guidelines-key-takeaways-for-patient-skinantisepsis 2. Beausoleil C, Comstock SL, Werner D, Li L, Eby JM, Zook EC. Antimicrobial persistence of two alcoholic preoperative skin preparation solutions. J Hosp Infect. 2022 Nov;129:816. 3. Degala, et al. United States Patent 9,078,934. July 14, 2015. BD, the BD Logo and ChloraPrep are trademarks of Becton, Dickinson and Company or its affiliates. ©2025 BD. All rights reserved. BD-143543 (2/25) 4. Adeyinka A, Kondamudi NP. Cyanosis. In: StatPearls [Internet]. Treasure Island (FL):StatPearls Publishing; 2022 Jan. Available from: https://www.ncbi.nlm. nih.gov/books/NBK482247/ 5. Fletcher J. Bruise colors: Causes,timescale, and when to see a doctor. Medical News Today. 2020 Jan 4. Available from: https://www.medicalnewstoday.com/ articles/322742 6. Mount Sinai. Jaundice Information. Available from: https://www.mountsinai.org/health-library/diseases-conditions/jaundice 7. 2021 AORN Guidelines for Perioperative Practice: Patient Skin Antisepsis. 8. Food and Drug Administration. https://www.fda.gov/drugs/drugsafety/ucm374711.htm 9. Weber DJ, Rutala WA, Sickbert-Bennett EE. Outbreaks associated with contaminated antiseptics and disinfectants. Antimicrob Agents Chemother. 2007 Dec;51(12):4217-24.
BD, the BD Logo and ChloraPrep are trademarks of Becton, Dickinson and Company or its affiliates. © 2025 BD. All rights reserved. BD-143543 (3/25)
By Megan Clancy
Gerry O’Dell is a past co-chair of AAMI’s Industrial Ethylene Oxide (EO) and Moist Heat (MH) Sterilization Working Groups, and she was named an AAMI Fellow in 2019. O’Dell is a Certified Industrial Sterilization Specialist (CISS) for ethylene oxide, moist heat, and radiation (RAD), and holds a master’s degree in microbiology from the University of South Florida. She is also the co-owner of O’Dell & Hodge Consulting, where she advises medical device, pharmaceutical, and biologics companies on sterilization, environmental monitoring, laboratory operations, and compliance. Additionally, she co-authored a chapter in the January 11, 2023 issue of AAMI Array, and has authored chapters in several publications on sterilization.
From Microbiology to Medical Devices: O’Dell’s Career Development
O’Dell landed her first job out of college as a lab technician for a medical device company owned by Johnson & Johnson. There, she was promoted
to the sterilization services group and then to a role as laboratory supervisor, where she oversaw everything from microbiological processes to sterilization. “I enjoyed the lab piece of it, but it wasn't as interesting as the sterilization aspect,” she said.
The company was involved in sterilization standards development, which introduced her to AAMI’s working groups early on. “I had a very good mentor in the area of sterilization,” she shared. That mentor, Jim Gibson, allowed her to participate in AAMI’s first EO sterilization standard meetings, though she wasn’t a member at the time.
And when Gibson retired and moved into consulting, O’Dell took on his role as the company representative for the group, for which she was eventually elected co-chair. This new position opened up opportunities to join several other working groups, and also introduced her to the ISO standards she participates in to this day.
Following a break from Johnson and Johnson, she continued along the path of her mentor and founded her own consulting firm. And after 10 years on the EO committee, she traded in that role to become the new co-chair for
AAMI’s working group on moist heat sterilization. Though she no longer serves as co-chair for either group, she continues to be active in AAMI and ISO standards work, while serving as an instructor for many of AAMI’s sterilization courses – including three upcoming courses on ethylene oxide, industrial sterilization, and radiation.
Building Bonds – and Business – through AAMI
O’Dell has participated in AAMI’s standards work since 1985. From the beginning, that involvement was rooted in O’Dell’s business-forward thinking. “[When I started], if you participated in the working group, you got the standards and any Technical Information Reports for free,” she said. “But it's not just the knowledge that you gain… and influencing the direction of the standards, but also meeting people that you can network with,” she said.
The tight-knit nature of the standards work has proven to be an asset. “Some of the people that I've worked with, we've worked together on standards for 30-plus years,” she explained. “You really get to know people pretty well … and to have a better understanding of where they're coming from on different
things. So, it does make a difference [in your career].”
Though O’Dell began working with AAMI on standards development early on, she didn’t start teaching for the association until 2009, when AAMI was developing their first ethylene oxide-specific sterilization course. “I was involved in initially writing that course and putting it together,” she said.
Noticing that many courses focused on theoretical knowledge, she strove to make the course applicable to the work of sterilization specialists. As a result, witnessing the real-life impact of her courses has turned out to be one of the greatest rewards of teaching.
One of O'Dell's first students is now an instructor for AAMI whose career saw tremendous benefits from her hands-on teaching strategy. “He took a lot of the principles that we talked about when it comes to optimizing EO sterilization cycles, and he took them back to his company and implemented them,” she said. That successful optimization led to around a million dollars in savings for his company, along with a promotion.
Teaching Sterilization: Interactive Learning in a Changing Industry
According to O’Dell, hands-on learning has become even more important in recent years. Changes in the industry have led to fewer in-house sterilization processes at medical device companies, forcing many professionals to imagine the processes they are developing without ever seeing the equipment that performs them.
“There's usually a good 25 to 30 percent of the class that has never been to the sterilizer,” she said. “That means there’s often a gap. Because we like to think that the product or the process is going to drive things, but sometimes we're also limited by what the equipment capabilities are.”
For that reason, O’Dell works to ensure that her students understand those potential restrictions, not just in theory, but in practice.
From August 25 to 28, O’Dell will teach a course on Ethylene Oxide Sterilization, which will help experienced professionals optimize sterilization processes, identify problems in the cycle, and determine whether validation is needed. “I’ve been in the industry now for 42 years. And even at this point, I see new things. Stuff crops up that I didn’t expect, particularly with lower gas concentrations – so that gets transmitted in the course,” she said.
The Future of Sterilization and Standards – And How to Prepare AAMI News asked O’Dell where she sees sterilization heading. “What I see in the future is more variability with how products will be sterilized,” O’Dell shared. “Ethylene oxide makes up about 50% of all of the sterilization that occurs worldwide, with radiation taking up a bulk of the other part of it … Eventually, that other piece is going to get bigger as people figure out other methodologies for sterilization that are not only niche-oriented.”
To stay on top of these changes, O’Dell advises professionals to get involved in the standards process now. “Because that’s where a lot of this information starts coming out,” she said.
But like technology, standards work is not immune to change. In the wake of the COVID pandemic, most standards meetings that were once held in-person are now virtual, making active participation more important than ever. “So, making sure that companies are picking the right people for being involved in the standards process – people that are willing to speak out and convey their opinions – that's something that people need to push for within their organizations,” she said.

“What I see in the future is more variability with how products will be sterilized— new methods are emerging beyond the traditional standards.” “

By Richard Parker, MBA, CHFM, CLSS-HC, FASHE, FACHE
W hen it comes to ensuring fire safety in surgical environments, most healthcare professionals think about quarterly fire drills, fire barriers, and proper storage of flammable materials. Yet, hidden within the text of NFPA 99–2012 is a lesser-known but equally critical requirement: the annual fire exit drill for anesthetizing locations. This drill, distinct from general fire drills conducted hospital-wide or within ambulatory surgery centers (ASCs), addresses the unique risks present in surgical suites.
The Code Behind the Drill
Section 15.13.3.10.3 of NFPA 99 (2012 edition) states:
Fire exit drills shall be conducted annually or more frequently as determined by the applicable building code, NFPA 101, Life Safety Code, or fire code.
This simple sentence carries important implications. Unlike the more familiar quarterly fire drill requirements from NFPA 101, which apply broadly to healthcare occupancies, this section focuses specifically on anesthetizing locations such as ORs and procedure rooms.
It is also important to note what
this section does not say. There is no requirement for these fire exit drills to be unannounced, nor do they need to incorporate varying conditions. They are not part of the routine fire drill schedule and are best understood as a unique and targeted training opportunity for OR teams.
Why Are Fire Exit Drills in the OR Different?
ORs present fire hazards that are fundamentally different from those in patient rooms or administrative areas. In addition to the presence of ignition sources (e.g., electrosurgical units, lasers, and fiber-optic light cables), these areas often involve:
• Flammable surgical drapes and prepping agents
• High-flow oxygen and nitrous oxide sources
• A team intensely focused on sterile procedures Because of these factors, a fire in the OR can spread quickly and create a chaotic and life-threatening environment. The annual fire exit drill provides a dedicated opportunity for surgical staff to practice response actions that can save lives and minimize harm.
Key Elements of an Effective Fire Exit Drill
To be meaningful and compliant, fire exit
drills should go beyond checking a box.
1. Involve the whole surgical team: Fire emergencies don’t happen in silos. The drill should engage anesthesiologists, surgeons, nurses, scrub techs, and any support staff who might be present during a procedure.
2. Simulate OR-specific fire scenarios: While it may not be necessary to use theatrical smoke or alarms, the drill scenario should reflect real threats such as:
• A surgical drape catches fire.
• Equipment malfunctions and ignites.
• An oxygen-enriched atmosphere accelerates ignition.
3. Define clear roles and communication protocols: During a drill, assign and practice specific responsibilities:
• Who announces the fire?
• Who turns off the oxygen?
• Who retrieves the extinguisher?
• Who coordinates evacuation or continued patient care?
Incorporate the RACE (Rescue, Alarm, Confine, Extinguish) protocol or your facility’s equivalent.
4. Document and Debrief: Post-drill evaluation is essential for improving performance and documentation is required. Your debriefing session should record:
• Date, time, and participants.
• Scenario overview.
• Actions taken and observed.
• Lessons learned and improvement plans.
Documentation also supports compliance with ACHC hospital and ASC standards, particularly those for acute care and critical access hospitals covering fire drill critique, and staff training in fire response.
Fire On or In a Patient NFPA 99 does not describe fire response protocols for situations where the fire involves the patient, but this risk is very real in surgical settings. Importantly, because this type of event occurs within an anesthetizing location, it reinforces the rationale behind having a dedicated fire exit drill for these settings. A fire on a patient, particularly involving surgical gases or drapes, is not easily addressed through general facility-wide fire response training.
Guidelines from AORN and the ASA offer best practices for these events. Consider integrating these protocols into your fire exit drills or developing parallel training sessions.
Immediate steps
• Verbally announce: "Fire on the patient!"
• Douse flames using sterile saline (not alcohol-based solutions).
• Turn off all flammable gas sources.
• Remove burning materials and drapes.
• If airway fire: disconnect circuit, remove endotracheal tube.
Post-fire management
• Assessing the patient and providing immediate care
• Documenting the event and the staff response
• Reporting to internal safety and quality committees
Some facilities treat this as a separate fire response plan. Others include it in a comprehensive plan that outlines all fire risks, including evacuation and in-place defense strategies.
Clarifying Terminology: Defend-in-Place vs. Evacuation
The phrase "defend in place" often arises in discussions about OR fire safety, but it can be confusing. In Life Safety Code terminology, "defend in place" refers to protecting patients within a smoke compartment rather than evacuating them immediately – a strategy supported by the presence of fire-rated barriers and automatic suppression systems.
In the operating room, additional clinical realities complicate the idea of evacuation. Patients are often anesthetized and supported by complex life-sustaining equipment. More critically, the surgical procedure may have already begun, meaning the patient is open and exposed. For these reasons, staff must be trained to control the fire as quickly as possible and immediately assess and continue care for the patient. Evacuation may still be necessary for larger or uncontained fires, but only after ensuring the patient’s condition allows for safe transport.
Clarifying this distinction is important during drills and documentation. Surveyors may ask about your defend-inplace strategy, and staff should understand that in the OR, defending in place reflects both the physical constraints of the environment and the clinical imperative to prioritize patient safety and continuity of care.
A well-executed fire exit drill can identify critical safety gaps and reinforce staff confidence. Consider these tips:
• Don't skip the pre-drill briefing. Let staff know the purpose of the drill. A short huddle can improve engagement.
• Practice turning off medical gases. Staff often know this in theory, but rarely practice it.
• Rotate roles. Let different staff members take the lead in various drills to broaden familiarity.
• Avoid token participation. All members of the OR team should be fully involved – not just observers. Common mistakes include:
• Treating the drill like a paperwork exercise.
• Only involving environmental services or facilities staff.
• Failing to debrief and capture lessons learned.
Accreditation surveyors will likely ask about the frequency, documentation, and content of fire exit drills. Be prepared to demonstrate:
• The distinction between quarterly drills and the annual OR-specific drill.
• Evidence of active participation by OR personnel.
• Integration of training into broader emergency preparedness efforts. Facilities accredited by ACHC should ensure their drills align with fire response and emergency management standards. Having a clear, practiced plan supports compliance and helps build a culture of safety.
Another form of excellence in surgical care
Fire exit drills for anesthetizing locations are more than a regulatory checkbox. They are a chance to prepare for a highrisk, high-impact event that demands immediate and coordinated action. By tailoring these drills to the unique environment of the OR, and integrating guidance from organizations like AORN and ASA, healthcare facilities can elevate their fire response readiness.
Most importantly, these drills offer a practical way to protect patients and staff – and reinforce the values of safety and teamwork that define high-quality surgical care.

– Richard L. Parker is associate director, physical environment and life safety at Accreditation Commission for Health Care Inc. where he provides guidance to customers and surveyors in the ASC and hospital programs.
By James X Stobinski, Ph.D., RN, CNOR, CSSM(E), CNAMB(E)
I would like to comment on a recent social media post which generated considerable discussion among nurses. The post featured a list of the range of salaries for tradesmen such as plumbers and electricians and made a comparison to nursing compensation. The consensus from many of the nurses that responded was that nurses were undervalued in comparison to these workers. Full disclosure here – my father and many of my relatives were/ are skilled tradesmen so my view is a little different than some nurses. I would like to offer another perspective on comparisons between nurses and other workers.
First, let’s narrow the field and speak to just one trade – plumbing. Much like nurses, plumbers have a long period of education and training. The Salary.com website informs us that the median salary of a journeyman plumber with roughly 5 years of experience is $67,020.¹ On the Salary Solver website, we are told that MidLevel RNs (5-10 years of experience) earn $70,000 to $85,000 per year.² This gives us a rough comparison
of salary levels of registered nurses who are not APRNs and journeyman plumbers who are not licensed as master plumbers.
We can argue about the relative value of nursing work versus plumbers. We can also speak to nurses making lifesaving decisions and that the work of nurses is more consequential than that of a skilled tradesman. From my perspective as someone well familiar with the work of skilled tradesman I maintain we should not begrudge these workers their hard-earned wages. We should instead consider a larger question –Why do the nurses who responded to that Facebook post feels undervalued? For that we should look a little deeper.
In many healthcare facilities nursing is seen as a necessary but substantial labor expense. Keeping nursing staffing lean is a priority for leadership and nursing-related education and training is often an early casualty when budgets are tight. The visceral responses of nurses to that Facebook post on the compensation of skilled tradesmen then logically follows.
What could benefit nursing over the long term is a change in how American healthcare views the labor

costs of nursing care. The work of Dr. Olga Yakusheva from the University of Michigan with the Nursing Human Capital Value Model can inform a change in perspective. The authors state that, “ … we propose a new conceptual model and definition of nursing's economic value.”(3) They maintain that the economic value of nursing should be redefined as an outlay which can yield a real, concrete return on investment (ROI) in terms of, “ … the improvement of consumer, nurse, and organizational outcomes.”³ In this view, improving staffing ratios and nursing professional development is as an investment in human capital versus just an expense. These authors contend that nursing-related expenditures are, “ … investments in growing, developing and sustaining an organization's nursing human capital.” which initiates a cycle of value creation.³ In this cycle the delivery of nursing care is a “ … a foundational ingredient to the production of healthcare services and consumer outcomes. Improved outcomes, subsequently, drive organizational revenue growth.”³ To justify this cycle, we must find ways to substantiate the value driven by nurses. But first, we must start talking the language of ROI and think in

“To elevate our profession, we must stop framing nursing as an expense and start speaking the language of ROI - nursing is human capital that drives measurable outcomes and revenue growth.”
human capital terms.
This article, although a challenging read, is well worth your time. Consider it a worthwhile investment and an alternative to social media posts. We know the value we can bring but we need to better articulate that and the Nursing Human Capital Value Model provides a framework for discussion and future research. The ROI for our profession could be substantial.

References
– James X. Stobinski, Ph.D., RN, CNOR, CSSM(E), CNAMB(E), Ph.D., RN, CNOR, CSSM(E), CNAMB(E), is on the faculty at Central Michigan University and director of hospital and ASC surgical education relationships with National Institute of First Assisting (NIFA).
1. Salary.com (2025). Plumber, Journeyman Salary in the United States. https://www.salary.com/ research/salary/alternate/plumber-journeyman-salary
2. Salary Solver (2025). NP vs RN Salary in 2025. https://salarysolver.com/np-vs-rn-salary/
3. Yakusheva, O., Lee, K.A., & Weiss, M. (2024). The Nursing Human Capital Value Model, International Journal of Nursing Studies, 160:104890. doi: 10.1016/j.ijnurstu.2024.104890. Epub 2024 Aug 31. PMID: 39316994.
KEEP YOUR OR STAFF COOL
The lightweight CoolOR® Circulating Water System is a proven solution for keeping surgeons and staff cool and comfortable.
CONVENIENT, EASY-TO-USE AND PORTABLE DESIGN
VEST STYLE CHOICES
Adjustable and fitted cooling vests cool by circulating cold water through a series of tubes sewn into the vest.
WATER-TIGHT COOLING RESERVOIR
Neoprene gasket seal with secure stainless steel compression latches.
NO ELECTRICAL CORDS

Optional lithium-ion battery offers increased mobility with more than six hours per charge.
MULTI-PERSON SYSTEMS! Cool two, four or six people at the same time with a single cooling reservoir!



Based in the Kansas City metropolitan area, Surgical Solutions is a trusted leader in on-site surgical support services. Surgical Solutions is dedicated to making surgeries safer and more efficient. Since its foundation in 2007, the company has focused on delivering tailored services in procedural support, sterile processing leadership and staff, and endoscopy support.
Today, Surgical Solutions serves hospitals across the U.S., providing customized support to ensure surgeons focus on patients and ORs run smoothly. Surgical Solutions was recently recognized as a Top Sterile Processing Services Provider of 2025 and is also ISO 9001 certified. This recognition reflects their commitment to quality,
innovation, and operational excellence.
At the helm is CEO Kirk Leonardelli, whose two decades of experience in hospital systems, healthcare operations, and strategic partnerships have propelled the company into its next phase of growth. Under Kirk’s leadership, Surgical Solutions continues to innovate, expanding services that enhance efficiency and patient outcomes.
“We ensure every detail is handled with precision, from setup to sterilization,” Kirk states.
OR Today Editor John Wallace recently interviewed Kirk and was blown away by his infectious energy and commitment to excellence. Another striking takeaway from the interview is the process Surgical Solutions uses to create a partnership. It might technically be “outsourcing” but in reality, the
Surgical Solutions team becomes one with the hospital or ASC staff, much like third-party biomedical equipment service providers blend into a facility’s team creating a champion for quality healthcare.
“More broadly, our goal is to reshape how hospitals view outsourcing,” Kirk explains. “It’s not a loss of control, but more of a collaborative way forward. Hospitals are often told to do more with less, and we help them overcome those obstacles through efficiency and partnership. Unlike traditional outsourcing, our teams live in the communities we serve, plus the bonus of bringing access to our deep national knowledge base. That includes clinical specialists who have worked in multiple SPDs across the country, and clinical educators that many hospitals could not hire on their own due to budget
Client: Major IDN (11 hospitals, $5.5B annual revenue)
Challenge: Surgical inefficiencies, rising costs, and the need to modernize operations.
Phase 1: At the first hospital, we modernized equipment, deployed skilled technicians, and improved turnover times to achieve 100% OR readiness.
Phase 2: Expanded to two more hospitals, driving:
• 70% increase in laparoscopic procedures
• 31% increase in endoscopic volumes
• 20–32% reduction in hospital costs
Phase 3: Network-wide expansion to five additional hospitals, delivering measurable value and reducing Joint Commission deficiencies to 0.
constraints. Our people are truly our greatest resource and expanding that talent base is a major focus for our future growth.”
Q: Can you explain your company’s core competencies and unique selling points?
KIRK: Our strength lies in SPD, endoscopy, and OR support, particularly with complex instrumentation such as endoscopes, robotics, and surgical devices. What sets us apart is our ability to provide personalized support instead of generic outsourcing.
Q: How is your leadership shaping the company’s direction?
KIRK: Stepping into the role of CEO has been an incredible opportunity to help shape Surgical Solutions for its next chapter. My background is in hospital systems and healthcare operations, so I’ve seen firsthand the challenges hospitals face and the kind of partnerships that make a real difference. Over the past year, we’ve sharpened our focus on innovation and strengthened our partnerships across the industry to ensure our solutions truly align with the evolving needs of hospitals nationwide. For me, leadership starts with listening. I spend a lot of time with our teams and with our hospital partners, understanding where the pain points are and how we can help. From there, it’s about tailoring strategies that drive efficiency, compliance and ultimately

better patient outcomes. I’m proud of the growth we’re seeing, but even more proud of how we’re redefining what an effective collaboration in surgical services looks like.
Q: How have you been able to help with recent challenges faced by your customers?
KIRK: Hospitals today are under constant pressure such as staffing shortages, rising costs, compliance demands, and the need to improve patient outcomes. One of our biggest strengths is rapid response. When challenges arise, we can deploy specialized teams, something most hospitals can’t do with a limited staff. We’ve stepped in to stabilize sterile processing departments, ensure Joint Commission readiness, and modernize processes that were holding teams back. Our OpsGUARD platform has also been a powerful tool, giving hospitals real-time visibility into performance so issues can be identified and addressed before they disrupt care. In short, we help hospitals adapt quickly, save resources, and stay focused on safe, high-quality care.
Q: What are some advantages that your company has over the competition?
KIRK: At Surgical Solutions, we combine clinical and business expertise in a way that’s unique to our industry. We’re nimble enough to adapt quickly to customer needs and focus on creating
tailored solutions, not a “one-size-fits-all” model. Our goal isn’t to sell more of something, but to work side by side with clients, embedded in their teams, to help them succeed.
Q: What service that your company offers are you most excited about right now?
KIRK: We’re incredibly excited about the recent release of OpsGUARD, our new proprietary hospital performance improvement platform. This gives hospitals real-time visibility into their operational metrics through interactive dashboards, compliance tools, and analytics. In practice, issues are identified and fixed before they disrupt workflows. We built this into our service model which has proven to be a game-changer for driving efficiency, compliance, and patient safety.
We’re also deeply proud of our sterile processing services, which remain at the very core of our business. Surgical success begins in the SPD, where scopes and instrumentation must be meticulously processed in a timely way to meet the growing demand. To elevate this critical function, every Surgical Solutions technician is CRCST certified, even though only five states require it. We also incentivize advanced certifications and continuing education, ensuring our clients have access to top-tier expertise. This commitment earned us recognition as a Top Sterile Processing Services Provider of 2025.
Q: Can you share some company success stories with our readers?
KIRK: We had the privilege of bringing measurable and lasting impact on hospitals. One example is through a recent case study with a large IDN. We started with one hospital, where we modernized equipment, deployed skilled technicians and achieved immediate efficiency gains, including faster turnover times and 100% OR readiness. The results here led to expansion across their entire network. Across the IDN, procedural volumes grew by up to 70% in laparoscopic cases and 31% in endoscopic volumes, while costs dropped by 20-32%. This is just one powerful example of how Surgical Solutions can create real transformation.
That said, our success isn’t limited to large health systems. Our clients vary in size and scope, and each has unique needs. For example, one hospital saved $150,000 after we identified underutilized robotic services, while another reduced medical waste and saved over 600,000 gallons of water by transitioning from wet to dry cleaning. The variety of outcomes show measurable results tailored to each hospital’s unique needs.
Q: How does Surgical Solutions support customers?
KIRK: We streamline surgical operations
by providing end to end support from sterile processing and equipment management to onsite surgical support and intraoperative support. For us, it’s all about reducing OR downtime and improving outcomes to free up clinical staff to focus on what they do best: delivering top quality patient care.
We support hospitals at every stage of the surgical workflow. From the OR suite to sterile processing, we focus on improving efficiency and helping teams operate more smoothly. Most importantly, we work alongside hospital staff, sharing expertise, addressing challenges, and providing resources that make a tangible difference in operations and patient care.
Q: What is your company’s vision statement?
KIRK: We are guided by our vision: to improve the lives of all those we serve. It’s simple, but it drives every decision we make. At Surgical Solutions, we build lasting relationships with our clients, and we measure our success by theirs.
Q: How are you using data to drive OR efficiency?
KIRK: In many ways, hospitals are data organizations as much as they are care providers. Every decision in the OR depends on information about time, cost and utilization. The challenge is that this

data is often scattered across systems and is difficult to use. That’s where our OpsGUARD™ platform makes a difference. It unites auditing, asset management, and analytics in a secure, cloud-based system. Leaders gain realtime visibility, while our team works to anticipate issues and resolve them before they disrupt care. The service delivers measurable results that keep the OR running smoothly and patients at the center of care.
Q: What’s next for Surgical Solutions?
KIRK: We just announced a new partnership with Belimed, a leading global provider of infection control and sterile processing solutions. We are working together to bring comprehensive sterile processing and instrument management solutions to hospitals. Looking ahead, we’re focused on expanding these kinds of collaborations that strengthen our ability to deliver efficiency, compliance, and patient safety.
We’re continuing to invest in data-driven solutions, expand our partnerships, and innovate around sustainability and efficiency. With hospitals under increasing pressure, our role as a trusted resource is more important than ever, and we’re excited to help shape the future of surgical support.


Hospitals don’t have time to wait for results. That’s why Surgical Solutions guarantees measurable OR improvements within 90 days. We’re not just advising from the sidelines. We’re in your OR, making it happen.










Initiates pretreatment at the point of use in the OR or ED, giving SPD teams a head start.
Broad-spectrum formula emulsifies and lifts all soil types, making bioburden easier to remove.

hmark.com
800.521.6224

Helps prevent biofilm and corrosion, protecting instruments from the start. Now is the perfect time to try XEN Xcelerate. For a limited time, purchase one case and get one free—making it easier than ever to stock up and clean without compromise. Don’t miss this opportunity to enhance your pretreatment process while doubling your value.
Scan here to see how XEN aligns with your department’s pre-cleaning protocol




Designed for electrically testing electrosurgical instruments, the low-frequency high-voltage Insulation Tester is used to detect and locate defects such as pinholes, cracks and bare spots in the jacket or coating of laparoscopic and bi-polar electrosurgical instruments. The Insulation Tester is a handheld, portable unit that tests the insulation integrity of electrosurgical equipment for flaws in protective coatings applied over conductive instrument surfaces in order to prevent inadvertent tissue burns, which may occur during electrosurgical instrument procedures.












The recent OR Today webinar
"Truth or Dare: Is an LSO Required?" was presented by Vangie Dennis, MSN, RN, CNOR, CMLSO, FAORN, Perioperative Consulting LLC, and Patti Owens, MHA, BSN, RN, CMLSO, CNOR, AestheticMed Consulting International LLC.
"Truth or Dare: Is an LSO Required?" discussed the need for a Laser Safety Officer (LSO). The webinar covered guidelines, standards, and procedures for safe laser use in medical settings, as well as defined the roles and responsibilities of an LSO.
The webinar clarified whether an LSO is required based on specific guidelines and standards for laser use. The presenters, with expertise in laser safety, addressed the crucial aspects of laser safety, including biophysics, tissue interaction and safety protocols. A question-and-answer session delivered additional insights as the presenters answered questions from attendees.
This webinar is eligible for 1 CE
credit. OR Today is approved and licensed to be a Continuing Education Provider with the California Board of Registered Nurses, License #16623.
More than 100 healthcare professionals registered for the informative webinar with 58 logged in for the live webinar. A recording of the session is available for on-demand viewing under the “Webinars” tab on the ORToday.com website.
Sandra Curatola, a PAT/Charge Nurse with Rochelle Community Hospital in Illinois won an OR Today lunch bag during the webinar.
Attendees shared positive feedback regarding the webinar via a survey that included the question, “What do OR Today webinars provide the industry?”
“Educational opportunities,” said Sharon Ford, who works in clinical informatics at Wellstar Health System.
“OR Today webinars provide updated information in relation to guidelines, new advancements and also provide educational CMEs for credentialing,” said Curatola.
“Current information on important
topics,” said Dorothy Connell, medical information manager with Baxter Healthcare.
“Latest clinical practice applications in the perioperative environment,” said Hung-Fu Lin, a nurse practitioner at Stanford Medicine Children's.
“A general understanding of regulatory information as well as other stories,” shared Mary von Ohlen, a procedure line educator with Doctors Hospital at Renaissance.
“Education to improve safety measures and/or quality care provided for surgical staff and patients,” said Kelli Atchinson, a nurse manager operating room with Doctors Hospital of Augusta.
Healthcare providers are invited to join a virtual training course on medical laser safety set for September 27-28. Gain valuable insights into laser biophysics, tissue interaction and crucial safety protocols tailored for medical settings. Visit medicallasersafety.com to learn more.
For more information about OR Today webinars, visit ORToday.com.
The Illinois AORN Chapter 1411 will present its 4CNE Seminar & Vendor Fair on November 8. It will bring together perioperative professionals, industry vendors, and nursing students for a day of education, networking and fundraising.
The event will take place at Ascension Alexian BrothersKennedy Conference Room in Elk Grove Village. Doors open at 7 a.m. with registration, breakfast, and vendor visits. Attendees will enjoy a full day of continuing nursing education, dynamic presentations and interactive opportunities with industry partners.
The seminar offers 4 Continuing Nursing Education
(CNE) credits and 1 Continuing Education Unit (CEU), featuring renowned speakers and timely topics.
Between sessions, attendees can browse the vendor fair, participate in the split-the-pot raffle and bid on themed auction baskets. Lunch will be provided, along with ample time to network with peers and connect with suppliers showcasing innovative perioperative products and solutions.
Register by October 30 at http://forms.gle/ Wcg4d9HZSNMCNWQA7
Regristration is $20 for members, $25 for non-members and $5 for undergraduate nursing students. Add $5 after the deadline or at the door.
Advanced Sterilization Products (ASP) recently launched the BIOTRACE Instant Read Steam System, the fastest FDA-cleared steam biological indicator system available in the U.S. Designed with sterile processing departments (SPDs) in mind, the new system delivers a readout in just seven seconds, drastically reducing wait time, minimizing errors and enhancing clinical workflow efficiency.
“The launch of BIOTRACE Instant Read Steam System represents a significant advancement in our ability to deliver fast, actionable sterility data to frontline staff,” said Dr. Ivan Salgo, vice president and chief medical and scientific officer at ASP. “By reducing the readout time to just seconds, we’re addressing a long-standing bottleneck that often impacts both productivity and peace of mind. This system supports SPDs not only in meeting compliance standards, but in exceeding them, with confidence.”
Developed with advanced fluorescence detection, BIOTRACE Instant Read Steam System streamlines routine monitoring of steam sterilization cycles without compromising accuracy. The compact reader accommodates
two simultaneous test positions, records the last 50 results, and connects seamlessly to digital infrastructure via USB, Wi-Fi, or Bluetooth. Integration with the BIOTRACE Assist App and SM Cloud Web Application enables secure cloud storage, enhanced traceability, and automated reporting for hospital instrument tracking systems including CensiTrac and other major ITS software solutions.
A recent usability study confirmed that throughput and staffing remain top concerns in SPDs nationwide. Respondents cited a strong willingness to invest in time-saving technology, recognizing the value of immediate sterilization verification in high-pressure clinical environments.

Hospitals and health systems can request demos and evaluation kits by contacting their ASP representative.
EvoEndo Inc. has announced that the EvoEndo Model LE Gastroscope is now FDA-cleared for patients of all ages – from neonates to adults. Since 2022, the EvoEndo System has been the only option available for sedationfree transnasal endoscopy for pediatric patients five and older. Now, the expanded indication makes safe, transoral endoscopy available to infants and young children, a previously underserved population.
CEO Jonathan Hartmann remarked, “EvoEndo was the first to achieve FDA clearance for an ultra-slim endoscope for pediatric patients, age five and older. We continue to innovate and are pleased to announce that we have expanded our indication to include all patients. The EvoEndo endoscopy system is now FDA-cleared for use with no age restrictions, elevating care for newborns and infants who will benefit from our ultra-slim technology.”
The new indication establishes EvoEndo as the leading choice for all endoscopies, from sedated transoral procedures in babies to sedation-free transnasal procedures preferred by older pediatric and adult patients.
“This expanded clearance is a major step forward,” stated pediatric gastroenterologist Dr. Michael Manfredi. He
added, “Being able to use the EvoEndo system in children under five allows us to safely support diagnosis and care in even the youngest patients. It also opens the door to broader applications beyond transnasal endoscopy, giving pediatric specialists more flexibility to deliver safer, more effective care for this vulnerable population.”
According to co-founder and CMO Dr. Joel Friedlander, the new indication “enables gastroenterologists and pediatric surgeons to provide care for patients across the entire age spectrum.” ChannelMax technology accommodates most standard pediatric accessories, and with scopes available in both 85 and 110 cm lengths, they are suitable for small or challenging anatomy and a broad range of indications.
The EvoEndo System is lightweight, portable, and easily scalable to multiple settings, allowing for care at the site of service. This makes diagnostic and therapeutic endoscopy more accessible, timely, and convenient for both patients and physicians. EvoEndo remains committed to expanding access and elevating the standard of care for every patient and is already available in over 40 facilities nationwide, with additional locations coming soon.






University of Georgia researchers have developed a new type of hand sanitizer that eliminates more than 97% of bacteria and fungi, including antibiotic-resistant strains. The new gel provides an alternative to traditional, drying alcohol-based sanitizers.
The nitric oxide gel formula, called NORel, significantly outperformed an alcohol-based sanitizer by maintaining effective antimicrobial activity as long as two hours after application. The alcohol-based gels the researchers tested had long evaporated and taken their antimicrobial agents with them by that time. Typical hand sanitizers evaporate shortly after application and lose much of their microbe-killing power within 30 to 60 minutes. NORel’s potential as a long-lasting, powerful hand
hygiene solution is particularly promising for high-risk environments such as hospitals, clinics and long-term care facilities.
“Regular hand sanitizers with alcohol in them do a pretty good job at killing bacteria when you apply them initially,” said Elizabeth Brisbois, lead author of the study and an associate professor in the UGA College of Engineering. “We showed that the nitric oxide persists on the skin for a longer period of time, so it’s kind of an extended protective effect. That was the most exciting result.”
The gel’s antimicrobial activity is on par with commercial, alcohol-based sanitizers containing 62% ethyl alcohol.

Quality In Flow (QinFlow) has released the Warrior AC Station – its newest blood and fluid warming solution engineered to meet the demanding needs of operating rooms (ORs) and intensive care units (ICUs). Part of the Warrior technology platform, the next-generation AC Station expands QinFlow’s mission to deliver simple, highperformance and versatile warming solutions across the entire continuum of care.
Purpose-built for hospital-based resuscitation and infusion needs, the Warrior AC Station delivers warm blood and IV fluids in seconds – supporting rapid bolus resuscitation and a wide range of infusion methods. Its compact footprint, one-button operation, and compatibility
with QinFlow’s Compact Disposable Unit (CDU) make it ideal for any patient population in high-acuity environments.
Unlike traditional warmers that are bulky and slow, the Warrior AC Station streamlines care delivery with unmatched speed, simplicity and performance. Its shared consumable design supports seamless warming transitions across the care continuum – from prehospital to the OR and ICU – boosting efficiency and systemwide standardization.
More than a warming device, the Warrior AC Station is a strategic solution that supports the Quadruple Aim of Healthcare: improving provider experience with intuitive operation; enhancing patient outcomes with immediate and precise warming; increasing operational efficiency through standardization and shared components; and lowering the cost of care by minimizing waste and simplifying logistics.
“The Warrior AC Station reflects what clinicians value most in our platform – simple setup, immediate performance, and seamless integration into their workflows,” said Ariel Katz, CEO of QinFlow. “We’re equipping hospitals with a tool that simplifies delivery, elevates patient safety, and reduces waste and cost across every point of patient care.”
The Accreditation Association for Ambulatory Health Care (AAAHC) has released its v44 Standards, the latest update to its accreditation and certification handbooks. Developed through a collaborative process with surveyors, expert committees, and accredited organizations, the Standards reflect current best practices and reinforce AAAHC’s commitment to patientcentered care and continuous quality improvement.
Effective December 16, 2025, the v44 Standards provide greater clarity for ambulatory health care organizations. Key updates emphasize enhanced education for informed decisionmaking, stronger guidance for data collection and outcomes measurement, and increased sensitivity to patient preferences, cultural needs, and expectations. The revisions also improve alignment with state scope-of-practice requirements, helping providers comply with regulatory frameworks while operating safely. Updates to structure and language further reduce administrative burden and support everyday implementation of quality practices.
“These Standards renew our promise to keep patients at the center of every decision,” said Noel Adachi, MBA, president and
CEO of AAAHC. “The v44 Standards also enable organizations to focus on what’s most relevant to their health care facilities through curation.”
The updates apply across all AAAHC Accreditation and Certification programs, including Ambulatory, Medicare Deemed Status, Advanced Orthopaedic Certification, Health Plans, and Health Plans FEHB.
According to AAAHC, the release underscores its 1095 Strong, quality every day philosophy by helping organizations sustain excellence between surveys. Paired with the 1095 Engage platform, the Standards are positioned as a springboard for daily quality improvement. Resources such as the Help Curtain, learning modules, and historical access empower professionals to integrate QI practices into daily operations.
“Patient-centered care remains a guiding force in how we shape our Standards,” said Joy Himmel, Psy.D., LPC, NCC, RN, FACHA, EMDR-C, Board Chair. “This update supports diverse patient needs through communication, culture, and education, while refining structure and language to reduce complexity.”
For more information, visit https://store.aaahc.org/handbooks.






Eliminate staff exposure
Reduce turnaround time


Pays for itself in one year!
Save canister & solidifier costs
Check cost saving on our website
Use the DM6000 for your project!
• Surgery, endoscopy, SPD
• Requires vacuum, electrical & drain





•
•
•






G
lobal Market Insights (GMI) reports that the medical disposables market is set to grow significantly from 2024 to 2032 driven by the ongoing transition from the use of reusable medical equipment to disposable medical supplies in an effort to reduce the risk of cross-contamination and surgical-site infections. In addition, the growing use of bioplastics to reduce the environmental impact of the healthcare sector will boost the usage of biodegradable medical
supplies and disposables by 2032, the report added.
Medical disposables are systems intended to be used once or temporarily to render quality patient care. These single-use products include gloves, blood bags, needles, and face masks, which can replace conventional equipment that involves a costly and time-consuming sterilization procedure.
According to the NCBI data, nearly 21% of the elderly population in India have at least one chronic disease. The high incidence rate of chronic
conditions and the subsequent increase in the rate of hospitalizations leading to risk of HAIs are some of the factors bolstering overall industry performance through 2032.
“There is a shift towards eco-friendly and sustainable disposable products in the medical sector,” GMI reports.
“The growing adoption of telemedicine leading to increased demand for remote patient monitoring devices, and a focus on infection prevention among and across patients and doctors are bolstering the demand for medical disposables. Additionally, innovations in materials and manufacturing
“Healthcare facilities are rapidly transitioning from reusable tools to disposable alternatives to streamline operations, reduce risks, and ensure compliance with evolving healthcare standards.”
processes are enhancing product quality and performance, while regulatory changes and standards are building trust among the users and patients. All these trends will combinedly shape the market outlook.”
A PR Newswire report citing Valuates Reports states that the global disposable minimally invasive surgical instruments market was valued at $2.8 billion in 2024 and is projected to reach a revised size of $4.8 billion by 2031, growing at a CAGR of 7.8% during the forecast period.
“The disposable minimally invasive surgical instruments market is experiencing robust growth due to rising surgical procedure volumes, increasing preference for outpatient surgeries, and heightened focus on infection prevention,” the PR Newswire release states. “Healthcare facilities are rapidly transitioning from reusable tools to disposable alternatives to streamline operations, reduce risks, and ensure compliance with evolving healthcare standards. The market is also witnessing significant innovation, with manufacturers offering specialized tools catering to various disciplines. As demand for cost-effective, efficient, and patientsafe solutions continues to grow globally, the market for disposable minimally invasive surgical instruments is expected to expand steadily in the coming years.”
MarketsandMarkets forecasts growth in a report focused on single-use surgical instruments and states that the "single-use surgical instruments market is projected to reach $7.80 billion by 2030 from $5.92 billion in 2025, at a CAGR of 5.7% during the forecast period.”
The growing aging population is a
significant factor driving the singleuse surgical instruments market. Older individuals typically require more medical interventions, including orthopedic, cardiovascular, and general surgeries. Age-related health conditions often lead to complex procedures, increasing the demand for reliable and sterile surgical tools. Single-use instruments provide an infection-free, convenient solution that meets the heightened safety needs of elderly patients. As the global senior population continues to rise, so does the need for safe and efficient surgical solutions, further fueling market growth.
The reports added that the handheld surgical instruments segment held the largest share of the single-use surgical instruments market, by product type, in 2024.
The market report for single-use surgical instruments is segmented by product type into various categories, including handheld, electrosurgical, endoscopic, and other single-use surgical instruments. In 2024, the segment for single-use handheld surgical instruments is projected to capture the largest portion of the global SUSI market. This prominence is primarily driven by the operational dynamics of ambulatory surgical centers (ASCs) and outpatient clinics, which frequently lack comprehensive sterilization facilities. As a result, they rely significantly on disposable handheld instruments to ensure patient safety and procedural efficiency. The increasing preference for these disposable tools not only enhances convenience and reduces the risk of cross-contamination but also supports the growing demand for single-use options within the surgical landscape.
The general surgery segment held the largest share of the single-use surgical instruments market, by application, in 2024, according to MarketsandMarkets.
“The single-use surgical instruments market is categorized based on various applications into general surgery, orthopedic surgery, cardiovascular surgery, gynecology & obstetrics surgery, ophthalmic surgery, ENT surgery, and other applications,” MarketsandMarkets states. “In 2024, general surgery emerged as the leading segment in terms of market share within the SUSI market.”
“The high turnover rates often seen in general surgery departments present significant challenges in the timely sterilization and reprocessing of reusable surgical instruments. This situation can create bottlenecks that delay surgical procedures and impact patient care. Single-use instruments provide a practical solution to these issues, as they eliminate the need for cleaning and reprocessing, thereby streamlining surgical workflows. As a result, the increased adoption of singleuse options is expected to significantly contribute to the growth of the SUSI market, enhancing operational efficiency and improving overall healthcare delivery,” the report adds.
Grand View Research states that the global disposable surgical devices market size was estimated at $6.7 billion in 2024 and is projected to reach $11.26 billion by 2030, growing at a CAGR of 9.3% from 2025 to 2030. This can be attributed to the rising prevalence of chronic diseases, the increasing number of surgical procedures, the growing geriatric population, and technological advancements.
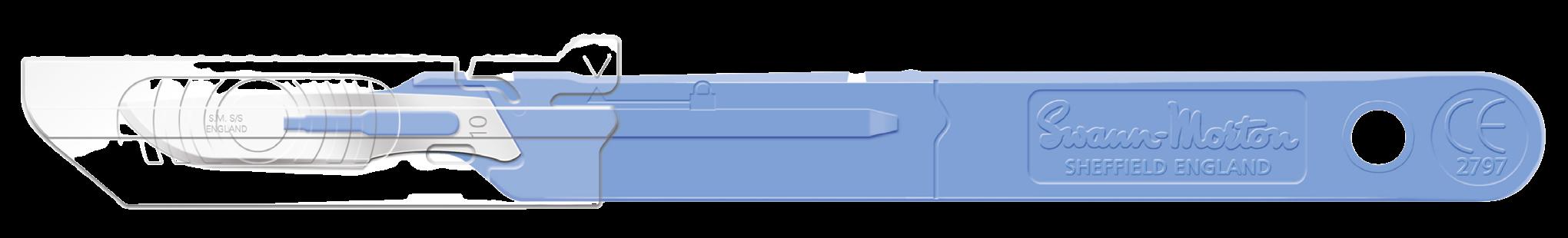
The Swann Morton retracting sheath safety scalpel combines retracting sheath technology with the trusted quality of the world leading surgical blade manufacturer. Engineered with the trademark Swann Morton blue handle and ring pattern, this scalpel is intended to improve sharps safety in every surgical setting. The safety scalpel is available in a variety of blade sizes, so there is an option for most surgical procedures. Swann Morton blades and scalpels are manufactured to ISO 13485, ISO 14001 and ISO 50001 standards with an open edge grinding technology for a better tactile feel. All blades go through 200 percent visual inspection, meaning there are no defects in the finished product. Swann Morton blades and scalpels are recognized for their consistency, reliability and durability.

From the operating room to behavioral health settings, single-use, nonwoven garments are redefining protection and efficiency across the continuum of care. In the OR, disposable surgical apparel delivers optimal performance in highstakes environments – supporting infection control, ensuring staff and patient comfort, and streamlining linen management. Beyond the surgical suite, purpose-built solutions for behavioral health offer safety, durability, and dignity, empowering caregivers while enhancing the patient experience. Together, Encompass offers a comprehensive, vendor-ready portfolio designed to meet diverse clinical needs with confidence. For more Information, visit encompassgroup.com

Anterior hip procedures involve an incision at the front of the hip, offering patients a quicker recovery. Historically, these procedures have required the use of more than four surgical drapes for the sterile field, which can complicate and extend prep time for clinical staff. Now clinicians can utilize the Cardinal Health Hip-O Anterior Hip Drape designed specifically for anterior hip replacements. Developed with clinicians in mind, the Hip-O drape offers a single product that can help eliminate the need for multiple drapes, saving surgical prep time and reducing waste1. It also features a rotatable design that can be used on either the right or left hip, helping to enhance versatility. Clear head and foot

panels offer visibility of both the table controls and anesthesia during surgery. Additionally, the drape helps provide AAMI Level 4 barrier protection, the highest level of fluid protection for surgical drapes.
1: Cardinal Health Data on File: Physicians Direct Conference, physicians survey N=15, December 2024.
November 1-2, 2025
Join perioperative professionals throughout the Southeast for CE-accredited education, exhibits with leading vendors, and great networking events.

By Don Sadler
It can be fun to look back at the history of various professions, especially perioperative nursing. A look back reveals how perioperative nursing emerged as the first recognized nursing specialization in the late 1800s and grew to become the highly specialized field that it is today.
This month, we examine the history of perioperative nursing and focus

on some of the most instrumental nurses in the advancement of this specialization.
The history of perioperative nursing begins with Florence Nightingale Though she wasn’t technically an OR nurse, her groundbreaking work with the British military during the Crimean War in the mid-19th century laid the groundwork for modern nursing.


Nightingale was an upper-class British woman who led a group of volunteer female nurses to the Crimea in 1854 to help care for British soldiers who were wounded during the fighting. The conditions were brutal as medicines were in short supply and hygiene was being neglected, resulting in mass infections and death.
In fact, many more soldiers were dying from battlefield illnesses than from wounds themselves. Nightingale




believed that implementing basic sanitary principles like hygiene, ventilation and hand washing were the key to preventing infections. It’s estimated that her work was instrumental in reducing the death rate among wounded British soldiers in the Crimea from 42% to just 2%.
When she returned to England after the war, Nightingale established nurse education programs in British hospitals based on what she learned out in the field. The programs were
organized around Nightingale’s beliefs and ideas about how nurses should be educated, which came to be known as “Nightingale Principles.”
The Nightingale Training School was established in 1860 and the first Nightingale-trained nurses started work five years later at the Liverpool Workhouse Infirmary, which is now called the Florence Nightingale Faculty of Nursing, Midwifery & Palliative Care. In 1859, Nightingale wrote “Notes on Nursing,” which is
still considered a classic introduction to the nursing profession.
The late 1800s saw several scientific advancements and discoveries in healthcare, including the advent of anesthesia, that resulted in a growing number of hospitals and surgical cases. Before this, surgeries were usually performed in patients’ homes.
This led to the need for specialized
surgical nurse training. The use of a surgical assistant first appears in the literature in the late 1800s and student nurses were first assigned to assist in surgeries in 1891. These early OR nurses were mainly given responsibility for cleaning and sterilizing instruments, preparing patients for surgery, bandaging and hemostasis.
The term “operating room nurse” first came into general use around the turn of the century. One of the first nurses to specialize in the OR was Caroline Hampton Halstead. She was appointed the chief nurse of the OR at the Johns Hopkins Hospital in Baltimore in 1889 by world famous surgeon Dr. William Halsted, whom she would later marry.
While working as Dr. Halsted’s scrub nurse, Caroline Halsted developed a severe contact dermatitis due to contact with disinfectants mercuric chloride and carbolic acid.
Dr. Halsted asked the Goodyear Rubber Company to manufacture two pair of thin rubber gloves with gauntlets for her to wear during surgeries. Thus, Caroline Halsted was the first nurse to wear surgical gloves in the OR.
Another influential early perioperative nurse was Edith Dee Hall, who was born in Nebraska in 1897. At the outbreak of World War I, Hall answered the call to serve along with thousands of other women by applying to the Army School of Nursing in 1918. Between her acceptance in 1919 and her graduation in 1921, Hall received training at military hospitals in Fort Des Moines, Iowa; Fort Hill, N.Y.; St. Lukes Hospital, N.Y.; Camp Dix, N.J.; and Walter Reed Hospital in Washington, D.C.
After the war, Hall became the OR supervisor at the New York Polyclinic Medical School and Hospital. She
strongly believed it was important for OR nurses to organize to increase their ability to provide better patient care.
Hall’s education, Army experience and work with surgeons and nurses all over the country uniquely positioned her to help create the Association of Operating Room Nurses. This later became the Association of periOperative Registered Nurses (AORN), the nation’s largest organization devoted to uniting and empowering perioperative nurses and healthcare organizations to support safe surgery for every patient.
After founding AORN, Hall served as the first AORN Executive Secretary from 1957-1962. Before her death in 1971, Hall worked as a consultant and writer for “Hospital Management” magazine.
Amy Armour Smith is an early 20th century nurse who made her mark as an author. Though she wasn’t technically an OR nurse, Smith wrote “The Operating Room: A Primer for Pupil Nurses,” which discussed concepts and ideas that were revolutionary at the time. For example, she stressed the
importance of personal follow-up visits so nurses knew how patients were progressing post-operatively and to learn the results of product use first-hand.
Smith advocated for refinements in aseptic techniques and recommended OR practices that soon became common, such as caps and masks going on first instead of last, boiling instruments after every operation, using white canvas laundry bags in metal wheeled frames, and avoiding leaning over a sterile field.
In addition, Smith championed the continuing development and education of OR nurses, recommending recertification every three years through theoretical and practical examinations. She promoted standardization of perioperative practices and more frequent conference attendance by OR nurse supervisors, as well as visits to other hospitals to discuss common problems and compare methods.
Edythe Louise Alexander is another pioneering OR nurse who made her mark as an author. In 1943, Alexander published the first edition of “Operating Room Technique,” which remains a staple for new nurses entering the perioperative arena. The third and fourth editions of this landmark book, retitled “Care of the Patient in Surgery, Including Techniques,” were published in 1958 and 1967, while later editions of the book bore her name: “Alexander’s Care of the Patient in Surgery.”

One of the most influential perioperative nurses during the later part of the 20th century was Jane , who served as the president of AORN in 1994-1995. Upon assuming the presidency, she made a number of promises to the perioperative community which were fulfilled during her tenure.

The first was to be a “back to basics” president who would form partnerships with AORN members. This was accomplished through outreach and collaboration with chapter presidents, national committee members and committee liaisons to establish strategic alliances with other professional organizations.
Rothrock also pledged to focus on substantive issues related to the perioperative workplace. During her tenure, AORN devoted time and energy to investigating workplace redesign and promoting reimbursement for RN first assistants. Instead of being drawn into debates that focus on function or who completes tasks, she remained adamant that the performance and evaluation of patient care requisites cannot be separated.
She demonstrated her commitment to accessibility by making 100 phone calls each month in response to AORN members who had reached out to her and visiting 50 different chapters over the year. In addition, AORN undertook a number of activities to influence public policy, provide professional development opportunities and support the vital work of AORN’s specialty assemblies during her tenure.
Rothrock received numerous awards throughout her career, including the AORN Jerry G. Peers Distinguished Service Award, a Recognition Award for Excellence in Nursing Practice from the Nightingale Awards, and the Christian R. and Mary F. Lindback Distinguished Teaching Award. In addition, she was a longtime editor of “Alexander’s Care of the Patient in Surgery.”
In 2004, Bill Duffy became just the second man to serve as the president of AORN after serving in various leadership roles since joining AORN in 1983. He has made numerous contributions to perioperative nursing throughout his long and distinguished career, especially in the area of nurse education.
Duffy has published numerous journal articles and made dozens of national and regional presentations covering virtually every aspect of perioperative nursing. In addition, he has written three books: “Care Coordination and Transition Management



Core Curriculum” “Perioperative Services: Administration; Resource Management and Patient Care;” and “Leadership in Action: A Manager’s Guide to Success.”
Perhaps his most influential work were his efforts to make the surgical Time Out a standard OR practice. The surgical Time Out is a groundbreaking perioperative practice that some have compared with wearing gloves and following sterile procedures as among the most important changes in perioperative history.
In the early 2000s, The Joint Commission published a list of “never events” that should never occur in the operating room. Also referred to as sentinel events, these include wrong site, wrong patient and wrong procedure surgeries.
Duffy observed that in their efforts to avoid making these errors, some surgeons were marking the surgical site while others were marking the site not to be operated on. He believed it was important to establish a standardized process for all surgeons to follow to avoid sentinel events.
Working together with the AORN Board of Directors, they created a taskforce to develop a standardized process for the surgical Time Out. A surgical Time Out toolkit was mailed to every AORN member and hospital in the country and AORN soon received requests for toolkits from hospitals in Canada, Europe and Asia as well.
The final step was making the public aware of the surgical Time Out and getting their buy-in. AORN hired a PR firm which helped create the National Time Out Day, which occurs annually on the second Wednesday of June. Duffy conducted interviews with major media outlets such as the CBS Early Show, Fox News, NPR, the Associated Press, USA Today and The Wall Street Journal.
More than 150 AORN members from 14 states even marched in Chicago’s St. Patrick’s Day parade in 2009 carrying a banner that read, “Time Out: Every Patient, Every
Time.” Over the past two decades, the surgical Time Out has become a worldwide practice that’s performed in the vast majority of surgical procedures.
Patricia Seifert was an influential perioperative nurse who specialized in cardiac surgery and helped pioneer the RN First Assistant (RNFA) role. In an interview with OR Manager before her passing in 2022, she described how soon after starting work in cardiac service, a surgeon asked her to move up to the chest to assist him.
At that time, the RNFA role was just beginning and only two states interpreted their nurse practice acts to include first assisting. After this surgery, Seifert began first assisting and promoting the opportunity to first assist to other members of the cardiac perioperative team. She also started an RNFA class that included surgeons, anesthesia personnel and expert staff members as teachers.
Over the next 40 years, Seifert personally assisted in more than 3,000 cardiac procedures. She told OR Manager that this experience
gave her numerous insights into patients, colleagues and administrators, as well as anatomy, techniques, rules and other aspects of cardiac surgery. Her work resulted in the first comprehensive textbook on the perioperative nursing care of cardiac surgery patients, which was published in 1994.
Seifert, who served as AORN president in 1999-2000, was a big believer in “sharing” instead of “hoarding” knowledge. As a leader, she had a clear vision, respect for team members at all levels (both RN and non-RN) and wanted to help each team member succeed, stated OR Manager. While her expectations for other team members were high, she worked to be fair and encouraging and to provide “tough love” when it was needed.
Seifert was beloved by the many perioperative professionals she worked with throughout her long career. She shared these parting words of wisdom to live by with OR Manager:
“Make it your primary, personal and professional goal to help others succeed in an environment that focuses on patient safety. One of



You might not have ever thought about the parallels between a perioperative team and a hockey team, but Michael Rempel sees similarities. Michael grew up playing hockey in Brooklyn, N.Y., and when he got his first exposure to the OR while in nursing school, he observed the similarities right away.
“For me, the dynamics of a hockey team resonated with the dynamics between OR team members,” he says. “Every member of the perioperative team has an important position to play, just like every member of a hockey team. I knew right away that I wanted to be an OR nurse, so I pursued this as soon as I graduated nursing school.”
After earning a bachelor’s degree in nursing from Pace University in 2009, Michael went to work as a staff nurse, perioperative services at Weill Cornell Medical Center in New York City. In this position he specialized in cardiac, thoracic, vascular, urology, colorectal and robotic surgery.
In 2013, Michael obtained a master’s degree in nursing education from Pace University. He followed that with a doctor of nurse practice

degree from Chamberlain University in 2020. These degrees opened the door for roles as a clinical nurse manager; director of surgical services; registered nurse CNIII, operating room; educational specialist, perioperative services; education specialist; and his current role as the pediatric trauma program manager at University Hospital in Newark, N.J., in which he has served since 2023.
“This role involves a lot of quality analysis, performance improvement, policy integration and policy creation specific to our pediatric trauma patient population,” Michael explains.
One of his biggest accomplishments has been the development of a customized educational plan through the analysis of stakeholder needs and clinical insights. Michael is also responsible for maintaining and renewing program accreditation and certification, such as the trauma center designation by the American College of Surgeons, and ensuring ongoing compliance with standards and requirements.
In addition, Michael is a part-time lecturer at the Rutgers University School of Nursing.
“I recently taught my first didactic course, intro to perioperative nursing,
which went really well,” he says. And he presented at the AORN 2025 Surgical Expo on periop DEU and the perioperative student experience.
One of Michael’s professional passions is helping bridge the gap between nursing academia and realworld practice for nursing students and new perioperative nurses.
“There’s often a disconnect between academic prep and the highly specialized skills that are required in the OR,” he says. “I’ve dedicated much of my career to building partnerships with nursing schools and developing DEU programs that create pathways for students to gain early exposure to the perioperative environment.”
Michael believes it’s more important now than ever to prepare the next generation of OR nurses as the surgical environment becomes more demanding and experienced OR nurses retire.
“Early exposure to the OR helps spark real interest, builds confidence and shows students what working in this specialty truly involves,” he says.
Mentoring and guiding the next generation of OR nurses is one of the most rewarding parts of his job, says Michael.
“Seeing their confidence grow
“Watching a nursing student walk into the OR unsure and walk out confident is one of the most fulfilling parts of my job.”

professional associations such as the Association of periOperative Registered Nurses (AORN).
“AORN has been instrumental in helping me connect with likeminded professionals and giving me a platform to advocate for perioperative education and professional development,” he says.
Michael previously led AORN’s perioperative academic mentoring partnership program that pairs experienced nurse mentors with new nurses to help them transition from the classroom to practical training.

structure for mentorship and helps
theoretical concepts to real-world
Michael and other mentors discuss has been deeply fulfilling and reinforces how mentorship helps both new OR nurses and mentor nurses grow,” he says.
When mentoring young nurses, Michael urges experienced OR nurses to share personal experiences that highlight the unique aspects of perioperative nursing and what makes this specialty so rewarding.
“Recognize young nurses’ accomplishments and provide encouragement and constructive feedback while also acknowledging the challenges they face and reflecting on what they need to continue building on,” he says.

An injury derailed Michael’s nascent hockey career but he remains actively involved in the sport by coaching youth hockey.
“This is the most fulfilling thing that I do outside of work,” he says.
“I love working with these kids and sharing my knowledge and passion for the game with them.”

A clinical evidence assessment by ECRI, a global patient safety organization, found that cranial electrical stimulation relieves anxiety symptoms. The treatment was found to be more effective at relieving symptoms than fake stimulation – with or without medication – for some patients.
Cranial electrical stimulation (CES) is a noninvasive neuromodulation technique intended to treat some psychiatric disorders, including anxiety disorders, by delivering diffuse electrical stimulation through
electrodes placed on the patient's scalp or earlobes. This type of electrical stimulation is thought to normalize electrical activity in parts of the brain that contribute to excessive fear and anxiety.
Evidence suggests some effects of CES persist for at least one month after treatment stops, and in some cases, may continue for up to six months. It is unclear if patients continue to respond to the treatment over longer periods of time.
CES is not to be confused with electroconvulsive therapy, a different, more invasive treatment that is considered a last resort therapy for treatment-resistant depression and
other psychiatric pathologies.
Treatment for anxiety disorders usually involves medication, psychotherapy, or both. However, these treatments do not work for all patients. Psychotherapy may be expensive, and it may be difficult to find a suitable psychotherapist. Some patients experience negative side effects from medication or do not want to take daily medication. Two cost studies suggested that cranial electrical stimulation may provide a cheaper alternative for patients seeking treatment.
"Cranial electrical stimulation is not widely used to treat anxiety," said Marcus Schabacker, MD,
Ph.D., president and CEO at ECRI.
"Most patients bear the full cost of treatment since it's not covered by Medicare, Medicaid, or most private payer insurance companies. Usually, patients who have had this treatment have done it in a research setting, or they've exhausted all other options for treatment with no success. Because this treatment can be given by a nurse in a clinic, or by the patient at home, it could be more convenient than psychotherapy, and it's scalable. It can be given with little-to-no psychiatry time."
ECRI assessed peer-reviewed clinical literature published through mid-April of 2024 that addressed the treatment's safety and effectiveness for anxiety, including five studies of more than 630 patients.
"This therapy has been studied since the ’60s, but until now there hasn't been sufficient evidence showing that it's a successful treatment option," added Schabacker. "But new research in the last several years sheds light on this treatment option as a way to relieve anxiety symptoms – not necessarily to replace the traditional treatment pathways of psychotherapy and medication. It's exciting to see we now have a body of work that presents evidence of its effectiveness.
Anxiety disorders are among the most common psychiatric illnesses. Anxiety disorders include generalized anxiety disorder, panic disorder, phobias, social anxiety disorder, separation anxiety disorder, and selective mutism (i.e., the inability to



speak in certain situations).
ECRI also assessed cranial electrical stimulation's safety and effectiveness for treating depression and insomnia. However, the published evidence is insufficient to determine whether it improves symptoms for patients with depression or insomnia.
The ECRI team that generated this clinical evidence assessment helps healthcare providers, thirdparty payers, and industry leaders make objective, evidence-based decisions on new, emerging, and existing healthcare products and interventions. These doctoral-level researchers identify, synthesize, and rate the strength and quality of the available evidence to help to drive positive outcomes, improve care quality, and lower costs.


soma@somatechnology.com (800) 438-7662 somatechnology.com @Somatechintl

By Miguel J. Ortiz
W hen it comes to stabilization training, we tend to naturally think of balance exercises. Taking it to the next level is tricky because most of these exercises aren’t regularly practiced and are sometimes used for “fun” challenges. This has caused the majority of people to only perform these exercises at certain times instead of adding them to their regular routine.
So, I want you to keep it simple and start small. To do so, we must understand the benefits of this type of
training. We must understand when to add it into a program and why one should implement stabilizationfocused movements.
Balance exercises require a more attentive mindset and that can improve three important areas of the body. Your brain is among them, according to author John Ratey. He wrote the book “Spark, The Revolutionary New Science of Exercise and the Brain.” I was fortunate enough to be a part of a workout program that he was involved in and there was a great deal of balance.
Here is what Ratey had to say,
“While aerobic exercise elevates neurotransmitters, creates new blood vessels that pipe in growth factors, and spawns’ new cells, complex activities put all the material to use by strengthening and expanding (neural) networks.”
Short exercises like these increase your Brain Derived Neurotrophic Factor (BDNF) which is like “miracle grow” for the brain. It allows people to remember information better and an improved attention span.
The next area it can improve is your heart. By activating more muscle groups, your heart must work slightly harder, depending on the exercise, to
get oxygen and blood to the area. The third area of improvement are your joints. Stabilization movements require you to be exactly that, stable. So, don’t think that jumping around on one foot will strengthen your ankle as much as standing on one foot (stability) for a certain amount of time will. The reason for that is because joint muscles work like cables on a bridge. When you look at them you can see that they are strong and holding the bridge, but they don’t move. You can add movement, but that goes into advanced levels of deceleration, acceleration and control throughout the movement.
Let’s get back to keeping it simple. When should someone add this into a fitness program? I recommend adding it in the beginning because it can be a great warm up to whatever other training you may be doing. Balance training increases heart rate. It helps brain activity and
stabilizes the joints. It’s a fantastic way to warm up specific muscle groups before training them. Even something as simple as push-ups on a BOSU ball can help increase shoulder stabilization, depending on how much you prevent the BOSU from moving. Doing a glute raise on a stability ball before squatting can help glute/hip activation and can help ankle stability for future strength movements. Plank holds on a stability ball can increase core muscle activation. The list of potential exercises is endless. Simply put, you’re working more muscles and burning more calories while improving brain and heart activity.
Finally, the most important reason for stabilization training is injury prevention. The number one reason athletes do balance training is for this exact reason. Adding some simple and very effective stability training to your routine will not
we’re on instagram!



OUT OF THE OR fitness
- Miguel J. Ortiz
Miguel J. Ortiz is a personal trainer in Atlanta, Georgia. He is a member of the National Personal Trainer Institute and a Certified Nutritional Consultant with more than a decade of professional experience. He can be found on Instagram at @migueljortiz.




By Grace O
A s fall settles in, we crave recipes that warm us from the inside out. It's the perfect time to add seasonal fruits, vegetables and soups to our cooking lineup.
Many of the vegetables I’ve highlighted are available year-round, thanks to partnerships with growers in Mexico and the Southern Hemisphere. But during fall, local harvests are at their peak, making it the ideal moment to explore vibrant, healthful additions to your fall recipe repertoire.
FoodTrients is a wellness philosophy and resource focused on using nutrient-rich foods to combat aging and support longevity. Each recipe blends the latest scientific research with medicinal herbs and ingredients
from diverse global traditions, creating dishes that are packed with flavor and superfoods. These recipes are designed to boost wellness, enhance energy and vitality, improve skin health, and help people look and feel younger.
Here are some of my favorite fall vegetables that make healthy eating as delicious as it is nourishing:
Artichokes enjoy a second crop in the fall (the first is in the spring). Fall produces small to medium artichokes, so everyone can have their own. Artichokes are packed with vitamins, minerals and antioxidants; they are also a source of probiotics, which support gut health by feeding the good bacteria that live there. The classic way to enjoy artichokes is steamed, and
then dip the leaves and heart in melted butter. But for a healthier alternative, make the ‘dip’ from extra virgin olive oil, balsamic vinegar, a drop of Dijon or spicy mustard, and a dash of salt. See my recipe for Herbed SpinachArtichoke Dip below.
About five-to-seven inches long and one-and-a-half to three inches in diameter, Delicata squash have a scalloped shape and beautiful green and orange stripes. The deep yellow to orange flesh tastes somewhere between a sweet potato and butternut squash. When roasted or steamed, even the skin is edible. To bring out their natural sweetness, cut into rings or chunks (discard the seeds or clean and roast those separately to munch

on later like pumpkin seeds), toss with olive oil, a little salt, and roast for about 20-25 minutes at 400 degrees F. Delicata are also delicious stuffed with breadcrumbs, chestnuts, and herbs or cut into small chunks to be added to rice or cous-cous. Nutritionally they’re a good source of potassium, iron, and vitamins A and C.
Honeynut squash has dark tan to orange skin and orange fleshy pulp. It has two-to-three times more betacarotene than butternut squash. Honeynut squash can be roasted,
sautéed, puréed, added to soups, stews, and braises, and is even sweet enough for desserts.
Leeks are in the allium family, so they’re related to garlic, chives, shallots and onions. They have a sweet, oniony flavor that adds depth to soups, stews and pasta dishes. Grilled or roasted, they make a delicious side dish. They’re at their best in the fall and spring. Nutritionally, leeks are rich in flavonoids. Flavonoids are antioxidants and studies suggest that they provide anti-inflammatory, antidiabetic, and anticancer properties.
First grown in Greece and eventually China, persimmons come into season in fall through winter. There are two main types of persimmons, the round, tomato-shaped Fuyu and the more elongated Hachiya.
The winter months are full of rich foods and parties. This time of year is for celebrating with friends and family, but does it have to lead to yearly weight gain? Support the health of the ones you love with a lighter, healthier holiday classic dip that retains all of its flavor. This simple high-fiber dip can be made in minutes with one simple step: blend until smooth! Serve this savory dip alongside fresh veggie sticks or whole wheat crostini for added nutrition your guests will love.
Ingredients
• 2 (14-oz.) cans of artichoke hearts, drained (unmarinated, canned in water)
• ½ cup mayonnaise (vegan or regular)
• ½ fresh lime, juiced with seeds removed
The Fuyu can be eaten when firm and have a sweet, honey-like taste, while the Hachiya are not edible until they are soft to the touch, when they exchange their astringent flavor for a sweet one. Both varieties are high in vitamin A, fiber and some vitamin C. They’re great in baked goods, puddings and salads.
– Grace O is the creator of FoodTrients, a unique program for optimizing wellness and longevity. She is the author of three award-winning cookbooks. Her latest cookbook is Anti-Aging Dishes from Around the World. You can find more age-defying recipes at Foodtrients.com/recipes. Recipes and photos reprinted with permission of FoodTrients.com and Anti-Aging Dishes from Around the World by Grace O.

• 1 cup fresh spinach, roughly chopped
• 1 tsp. dried thyme
• 1 tsp. dried basil
• ½ tsp. chili powder
• 2 Tbs. olive oil
• ½ tsp. garlic salt
• ½ tsp. freshly ground pepper
INSTRUCTIONS
1. Place all ingredients in the bowl of a food processor and process until relatively smooth, leaving some texture if desired. An immersion blender will also blend appropriately if it is more convenient.
2. Transfer dip to a small bowl and refrigerate for 1 hour or until set.

By Daniel Bobinski, Th.D.
T
he starting point of learning emotional intelligence (EQ) can be summed up in two words: know thyself. EQ is the skill of being able to perceive and assess one's own and other's emotions, desires, and tendencies, and then act in a way that's best for everyone. To do this well, one should learn about different behavioral, motivational, and cognitive styles, as well as the strengths and blind spots for each.
Since no single tool measures all of "personality," I always advocate using tools that focus on specifics. For example, DISC assessments help
us learn about behavioral styles.
Despite the growing use of DISC assessments worldwide, people still have questions and concerns about them. Well, since two-thirds of the difference between average and top performers is EQ, it's worthwhile addressing those concerns.
One of the most common misconceptions about a DISC assessment is that it's a personality test. It's not. The word "test" implies right and wrong answers, and your style isn't right or wrong. Yes, it may be more effective or less effective in given situations, but “right and wrong” does not apply. Your DISC profile simply tells us your preferred behavioral style in given situations.
You should also know that DISC assessments measure four specific
dimensions of behavior: how you tend to act when handling problems, people, pace, and procedures.
You should also know DISC assessments measure only a slice of your personality. Other tools assess other aspects, such as motivational and cognitive preferences. As a concept, "personality" is a complex, multidimensional picture of who you are. Think of it this way: your personality is like your entire house and your DISC profile is like the foyer. It’s the first thing we see and it tells us something about the house, but it's not the whole house.
Let me address several misconceptions about DISC.
Misconception 1: "DISC puts people in boxes." Not true. DISC
assessments describe tendencies. And not just your natural preferences, but also how you tend to adapt to succeed. And even that's just a tendency. People adapt their behaviors in many different ways when the situation requires it. One main purpose of DISC is understanding your starting point so you can predict your tendencies and know how to adapt.
Misconception 2: "Some DISC styles are better than others." Not true! Every style has strengths and challenges. The most effective teams include a diversity of styles that complement each other. Success comes from knowing your natural strengths and blind spots so you can leverage your strengths
and adapt when your natural style doesn't fit the situation.
Misconception 3: "DISC assessments are all a team needs to get better." Not true. DISC assessments play a key role, but motivators and cognitive preferences are also important for determining how we approach our work.
Bottom line, the basic purpose of any assessment tool is to give you greater self-awareness so you can make conscious choices about how to approach different situations. Your greatest competitive advantage isn't what you know, it's how well you know yourself and how you can adapt to bring out the best in others.

Single-use, nonwoven garments and bedding are redefining protection, comfort, and efficiency across the continuum of care.
One Solution. Every Setting. Total Confidence.
• Superior infection control & comfort for high-stakes surgical environments

Daniel Bobinski, is the author of the best-selling book “Creating Passion-Driven Teams” and the owner of Workplace Excellence. Also a certified behavioral analyst, Daniel consults and conducts training on workplace effectiveness and leadership development. He can be reached at danielbobinski@protonmail.com or eqfactor.net.


• Comprehensive protection for staff, patients, and bedding





INGREDIENTS:
8 lasagna noodles
1 pound hamburger meat
1 tablespoon garlic powder
1 tablespoon onion powder
15 ounces ricotta cheese
1 teaspoon rosemary (optional)
1 jar marinara sauce
2 cups mozzarella cheese, divided
In pot, boil noodles according to package instructions. Drain under cold water and set aside.
In same pot, brown hamburger meat then add garlic powder and onion powder. Mix in ricotta cheese; rosemary, if desired; marinara sauce; and 1 cup mozzarella cheese.
Heat oven to 350 F.
Line baking dish with layer of hamburger sauce. Line cooled noodles on cutting board or parchment paper. Add hamburger sauce to each noodle and roll. Place lasagna rollups, seam sides down, in dish. Cover with remaining hamburger sauce and sprinkle with remaining mozzarella cheese.
Bake 20 minutes.
By family features
R escue your loved ones from a dinner rut with a simple solution that answers “what’s for dinner?” with an exciting, flavorful meal. These Lasagna Rollups require just one pan, making both cooking and cleanup a breeze on busy weeknights.

To mix it up even further, try adding spinach or mushrooms, swapping out ricotta for cottage cheese or any number of personal preferences.

Did you know? BD ChloraPrep™ Skin Prep is the only 2% CHG/70% IPA fully sterile surgical skin antiseptic in the US with demonstrated persistence of at least 7 days.1,2 Choose BD ChloraPrep™ Skin Prep and have peace of mind knowing that you are covered with persistent protection.
Why is persistence important?
Limits bacteria on the skin and helps minimize entry into a surgical incision after application
Healing takes time Re-epithelialization can take up to two weeks3
Dressing Changes can occur between 2–7 days
Recommended by numerous clinical guidelines4–10

Follow the QR Code to discover the difference of unmatched experience on proven performance.
BD ChloraPrep™ Skin Prep demonstrates at least PERSISTENCE1,2

1. Beausoleil C, Comstock SL, Werner D, Li L, Eby JM, Zook EC. Antimicrobial persistence of two alcoholic preoperative skin preparation solutions. Degala, et al. United States Patent 9,078,934. July 14, 2015. 3. desJardins-Park HE, Mascharak S, Chinta MS, Wan DC, Longaker MT. The Spectrum of Scarring in Craniofacial Wound Repair. Front Physiol. 2019 Mar 29;10:322 4. CDC, Berríos-Torres SI, Umscheid CA, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017;152(8):784-791. 5. WHO. Global Guidelines for the Prevention of Surgical Site Infection, second edition. WHO Guidelines Approved by the Guidelines Review Committee. 2018. 6. Lok CE, Huber TS, Lee T, et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. American Journal of Kidney Diseases. 2020;75(4):S1-S164. 7. Ling ML, Apisarnthanarak A, Abbas A, et al. APSIC guidelines for the prevention of surgical site infections. Antimicrob Resist Infect Control. 2019;8(1):174. 8. Ling ML, Apisarnthanarak A, Jaggi N, et al. APSIC guide for prevention of Central Line Associated Bloodstream Infections (CLABSI). Antimicrob Resist Infect Control. 2016;5(1):16. 9. NICE. Healthcare-associated infections: prevention and control in primary and community care. In: National Institute for Health and Care Excellence (UK) 10. O'Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-193.
Everyone likes FREE stuff and we want to hear from our readers! It is a win-win! Please take a moment to tell us what you like about OR Today magazine. HOW DO YOU ENTER?
Simply go to ORToday.com/Contest and fill out the short form for your chance to win!




“Articles are short easy reads that you can easily complete on a break while as work or waiting in carpool! The topics are always great for 'boots on the ground' but also leadership.”
- Crystal Hawk








