Class of 2025




























































P.14 | PRO OF THE MONTH CHRIS AVILA


P.40 | ROUNDTABLE BEDS & STRETCHERS

P.94 | PREFERRED VENDORS DID YOU KNOW, FUN FACTS






















Millions of products, thousands of suppliers, one marketplace. Experience an unmatched selection of biomedical products all in one place. The PartsSource biomedical parts and equipment marketplace has everything from bed parts and accessories to infusion pumps and patient monitoring systems, with thousands of products Ready-to-Ship. You can buy confidently knowing you’ll get what you need when you need it.
Visit www.partssource.com to browse our online marketplace.
Scan the QR code to start shopping







P.12 SPOTLIGHT
p.12 Department of the Month: Children’s Hospital Colorado Clinical Engineering Department
p.14 Professional of the Month: Chris Avila
p.16 Next Gen: Amanda Nyen
p.18 Association of the Month: Arizona Healthcare Technology Management Association (AZHTM)
P.21 INDUSTRY UPDATES
p.21 News & Notes
p.27 Ribbon Cutting: Paubox
p.28 AAMI Update
p.30 ECRI Update

P.32 THE BENCH
p.32 Biomed 101
p.35 Tools of the Trade: AAMI CEU Journal
p.36 Webinar Wednesday
p.38 Shop Talk powered by MedWrench
P.40 FEATURE ARTICLES
p.40 Roundtable: Beds & Stretchers
p.46 Cover Story: Make Succession Planning a Goal: Developing a Sustainable Team
p.50 40 Under 40
P.75 EXPERT ADVICE
p.75 Careers Now
p.76 Leadership
p.80 Health-ISAC
p.82 Networking Notes
p.84 Right to Repair
p.86 The Future
PUBLISHER John M. Krieg
VICE PRESIDENT Kristin Leavoy
VICE PRESIDENT Jayme McKelvey OF SALES
EDITORIAL John Wallace
CONTRIBUTORS Roger Bowles
K. Richard Douglas
Jim Fedele
Joie Marhefka
Manny Roman
Steven J. Yelton
ACCOUNT Megan Cabot
EXECUTIVES Emily Hise
ART DEPARTMENT Karlee Gower
Taylor Hayes Alicia Brown
DIGITAL SERVICES Cindy Galindo
Kennedy Krieg
Haley Harris
EVENTS Kristin Leavoy
WEBINARS Linda Hasluem
HTMJOBS.COM Sydney Krieg
ACCOUNTING Diane Costea
CIRCULATION Joanna Manjarrez


Rob Bundick, Director HTM & Biomedical Engineering, ProHealth Care
Carol Davis-Smith, CCE, FACCE, AAMIF, Owner/ President of Carol Davis-Smith & Associates, LLC
Nadia ElKaissi, CHTM, Biomedical Engineer, HTM, VA Central Office (19HTM)
Bryant Hawkins Sr., Site Manager, Children’s Hospital of New Orleans
Earl Morris Jr., BMET, Director of Clinical Engineering, Harrison County Hospital
Leticia Reynolds, Clinical Engineering Operations Manager at UCHealth Parkview Medical Center




Gain the foundational knowledge and technical skill s you need to thrive in the growing field of Healthcare Technology Management. CBET provides comprehensive online programs, including our newly launched Denta l Equipment Technician training, specifically designe d to advance the skills of industry professionals. Our f lexible, expert-led courses enable technicians to stay ahead in this rapidly evolving field.

Virtual Reality (VR) labs provide a flexible and immersive learning experience tailored to accommodate busy schedules. These labs enable users to practice and refine skills in a controlled, risk-free environment, fostering the development of essential competencies.




BY K. RICHARD DOUGLAS
Ranked by U.S. News and World Report as one of the top 10 children’s hospitals in the nation, Children’s Hospital Colorado has a history that finds its origins in the cowboy days of the late 1800s and a group of tents.
Originally founded in 1908 in Denver, and converting a former residence in 1909, the first patients were admitted in 1910. The current facility was opened in 2007. The hospital is affiliated with the University of Colorado School of Medicine. Each year the hospital is consistently ranked among the best pediatric hospitals.
The Children’s Hospital Colorado Clinical Engineering Department manages the large inventory of medical devices that can be found in the current facilities.
Under the leadership of Director James Grissom and Manager James Stebbins, the CE team includes 28 technicians working across four hospital campuses with associated clinics
and outreach program locations. Many of the techs are CBETcertified and some have B.S. degrees in biomedical engineering.
“We have 27,728 assets in active inventory. The team has approximately 250 years of combined experience,” Grissom says.
In addition to the four hospital facilities – with a combined 600-beds – the CE team manages medical equipment for a level 1 trauma center, two level 2 trauma centers, two urgent care locations, 50-plus anesthetizing locations and more than 30 clinic and outreach programs in multiple states.
The IT and CE teams are unique departments but often work jointly on projects.
“While we are still two separate departments, we maintain a strong working relationship, especially patient monitoring and EMR integration. We worked with IT to create CE user group and a folder with files, programs and service manuals to push to all technician’s accounts,” Grissom says.
The department plays a key role in equipment acquisition.
“The department sits on the capital procurement committee and has created a Biomedical Equipment Acquisition Review (BEAR) Committee to validate and standardize the purchases
“Our vast years of experience are used to review contracts and determine hardware, software and training needed.”
of all medical devices. We facilitate inter-departmental communication and support due to the vast institutional knowledge of the team members that have worked here for more than 15 years,” Grissom says.
He explains that service contracts go through multiple layers of approval and the team is working to bring these in through the BEAR program to provide a central repository for all equipmentrelated contract data.
“Our vast years of experience are used to review contracts and determine hardware, software and training needed. When contracts are proposed, the department workload, as well as quantity across the enterprise go into determining if the service line should be brought in-house. We are working toward integrating our contracts into our computerized maintenance management system (CMMS) to alert technicians of coverage status, as well provide customers with accurate ROI/renewal recommendations,” Grissom adds.
For data collection, Grissom says that new equipment is directed to the department at each facility to be checked and for inventory information entered in the CMMS.
“We align our information with accounting for install date, purchase price and depreciation tracking. We assign four-year inventory validation work orders on all equipment deemed to have no required maintenance per the manufacturer. Manual data validation is performed during preventative maintenance cycles, as well as when specific department requests come in,” he says.
For special projects the team members rely on their years of experience. Those projects run the gamut from upgrading feeding pumps to the challenges posed by the pandemic.
One of those challenges was the need for patient floor expansions.
“We participated in the opening of a new campus during COVID. We provided project and program management on specialized treatment floors to ensure that proper medical
devices are available for that patient population, as well as technical resources for equipment purchases and installation,” Grissom says.
Other projects included research inventory tracking and a feeding pump fleet upgrade.
“Children’s Colorado’s growing research program needed assistance tracking equipment coming in/going out for recall and regulatory compliance. We had a short turnaround time for a system-wide feeding pump upgrade due to nationwide supply chain feeding cassette shortage and successfully coordinated with clinical and non-clinical departments for training, deployment and supplies,” Grissom says.
The team’s abundance of experience serves them well when it comes to problem solving. Grissom says that one example was creating a Philips testing station in department to work with the IT EPIC integration team.
The CE team also worked with anesthesia physicians to accommodate all the ancillary equipment mounted to the anesthesia machines. Team members worked with clinical educators to be called when new feeding pumps fail on the floor, the team responds promptly to witness/troubleshoot.
On the soft skills side, the group created a department flyer to inform customers what they do, how to get a hold of CE, as well as miscellaneous asset tags used in the CMMS if requesting work that is not directly related to a piece of equipment.
They also brought their experience to an MRI upgrade.
Grissom explained that a “manufacturer-performed upgrade led to a quenched magnet” and CE “assisted in facilitating rental and placement of portable MRI while the unit was repaired and re-certified.”
Away from work, members are involved with the Colorado Association of Biomedical Equipment Technicians (CABMET), AAMI and ECRI.
For pediatric patients and their families in Colorado, there is the assurance that they are being treated by a national standout facility, backed by the clinicians and HTM professionals who are up to the same standard.
BY K. RICHARD DOUGLAS
hris Avila, a biomed intern, walks into the shop, sits down at a bench, and begins work on an Alaris pump. Just another day in the life of a biomed; right?
Well, not exactly, Avila should be an inspiration to every biomed. Heck, he should be an inspiration to any person … in any walk of life. Avila is blind.
The sense that most biomeds depend on the most to maintain and repair medical equipment; Avila is doing without. Yet, he sits in his shop working on an important piece of medical equipment.
Avila lost his sight at the age of five as the result of an accident.
“I was born with sight and only went blind due to a car accident. I was five-years-old and was hit by a drunk driver outside of my grandparent’s house while speaking with my stepfather. I lost my sight and am now totally blind; for an example, I could stare at the sun all day and never blink,” he says.
Avila says that he is a braille reader and learned braille over the course of three months.
“I attended Salk Elementary School in Merrillville, Indiana. When I entered fifth grade, after talking with my mother, we decided that I would attend the Indiana School for the Blind and Visionally Impaired (ISBVI). I had been going there for several years at this point, starting when I was in second grade, but only as a short-course student. Short-course was a program that offered students like myself the opportunity to go to ISBVI for one week out of every month while still attending public school,” Avila says.
He says that in fifth grade, he switched to going full-time, which meant he would have to travel back and forth from Indianapolis each week, and stay in the dorms on ISBVI’s campus.

“I continued to go there until my graduation in 2017; my graduating class was less than 15 students and I was the valedictorian. During my time at ISBVI, I was introduced to many assistive technologies, such as screen-readers and braille displays, which I use to this day. I also participated in sports from seventh grade to my senior year of high school; track, goalball, wrestling and swimming,” Avila says.
In his sophomore year, he began taking classes at North Central High School; world history, AP U.S. History (only for a semester), global marketing and business law.
“For college, I originally went to Indiana University-Purdue University Indianapolis (IUPUI), pursuing a business degree, but after a year, decided to give it up and switched majors; thus began my journey as a biomedical engineer. Now, after the divorce of IU and Purdue, I am a Purdue student,” Avila says.
FAVORITE BOOK:
The Wheel of Time series by Robert Jordan
FAVORITE FOOD:
Steak tacos with corn tortilla and a glass of horchata
HIDDEN TALENT:
I am rather good at playing darts, not getting the exact score needed to win a game but hitting the bull’s eye; the most I ever hit in one night was six.
FAVORITE PART OF BEING A BIOMED?
I have always found working with my hands to be quite satisfying; as a child I always loved taking things apart – my toys, radios, engines, etcetera. Being a biomed allows me to do the same with medical devices, and unlike then, I actually can put things back together again and have them work.
He says that over the summer of 2024; he participated in an internship program facilitated by the Gregory S. Fehribach Center at Eskenazi Health.
“I am a biomedical engineering student that was interested in medical devices; specifically, the process of maintaining and repairing them,” Avila says.
The challenges of working as an HTM professional as a blind person were precipitated by the challenges of training a blind person to be a biomed.
“Originally, I wanted to be a business major and work for a shipping company off the East Coast. However, after taking a year of classes I realized it just wasn’t for me, and because of a book I read, ‘23 Years on Fire,’ I chose to then try my hand at biomedical engineering. To [the best of] my knowledge, I am the first blind student in either the IU or Purdue schools to pursue this degree, and it has been quite the challenging experience,” Avila says
He says it wasn’t only a challenge for him, but also for everyone involved; professors, the university staff, and his auxiliary aids.
“We all had to figure out how to best present to me the information being taught, it was a learning curve that just kept going. With new challenges and difficulties seemingly arising every semester; how to present the information, how to navigate programs that were not designed for people without sight, getting course material in a timely manner, etcetera,” Avila says.
How did Avila actually transition to hands-on work?
“In the beginning, I was introduced to many different devices, and was given the task of disassembling and then reassembling said devices. The purpose of which was to familiarize myself with the components of each; when reassembled, everything was tested to ensure I had put things back together again correctly. From there I was shown how to do the PMs for several of the more common devices that came through the shop. I thoroughly enjoyed my time working in the biomed department, and returned for another internship in the spring of 2025,” he says.
The ability to go hands-on with medical equipment repair and maintenance still did not come without challenges. It took some ingenuity and trial and error to move toward a workable solution.
“During my first internship, I very much enjoyed working with the other technicians in the
department; there was an issue however. The programs and software used for the preventive maintenance were inaccessible to me; this made it so that one of the techs would always have to be present when I worked on a PM. Towards the end of that internship – and what I have mainly focused on during this current internship – my objective was to figure out a way to complete a PM independently,” Avila says.
He says that since the Alaris pump is the most common device that needs to be repaired, the Alaris program became the first to be tackled.
“The main challenge was determining how to navigate the Alaris program using a tool called JAWS; a text-to-speech screen-reader. JAWS would read certain things within the application window but not others, and not consistently.

Another challenge was that when mapping out the program, JAWS would not read the different tabs, windows, icons, or buttons in the order they would appear on the screen; if at all,” Avila says.
He says that after weeks of testing, the solution proved to be something called the touch cursor.
“The touch cursor is one of several possible cursors used to move about the screen; this process is slower than I would like, but works. The next steps would be to gain a better understanding of the JAWS script editor. Instead of using the arrow keys to navigate across the screen, I could just press a key on the keyboard and skip directly to the area I want,” Avila says.
Away from his biomed work, Avila has trained in Jiu-Jitsu for about three years and has competed in tournaments. He also spends time keeping his mind challenged.
“Instead of watching TV, I listen to audiobooks, favorite genre as of right now is litRGP. I enjoy studying and playing with numbers to see the different patterns that arise. If I’m feeling particularly adventurous, I experiment with cooking,” he says.
Avila’s family members include six siblings: two brothers and four sisters.

Can a blind person compete in Jiu-Jitsu or repair and test medical equipment? If that person doesn’t know the meaning of the word “obstacle,” they can. When Chris Avila is faced with a challenge; he just figures out a work-around. Obstacle has no meaning.
Amanda Nyen earned an associate of applied science degree in biomedical electronics before serving as a biomedical electronics technician IV/lead with St Luke’s Health System. TechNation recently found out more about this rising HTM star via a Q&A session.
Q: WHERE DID YOU GROW UP?
A: Blair, Wisconsin
Q: WHERE DID YOU RECEIVE YOUR HTM TRAINING/EDUCATION?
A: Western Technical College in LaCrosse, Wisconsin
Q: HOW DID YOU FIRST DISCOVER HTM?
A: Exploring the electronic programs offered at Western Technical College.
Q: WHY (OR HOW) DID YOU CHOOSE TO GET INTO THIS FIELD?
A: I have always been, and continue to be, fascinated by the realms of medicine and electronics. Upon reviewing the description of this program, I recognized it as my true calling.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: I take great satisfaction in resolving issues. When I am needed to address a situation involving malfunctioning equipment and I can provide a solution, it is an unparalleled experience.
Q: WHAT INTERESTS YOU THE MOST ABOUT HTM?
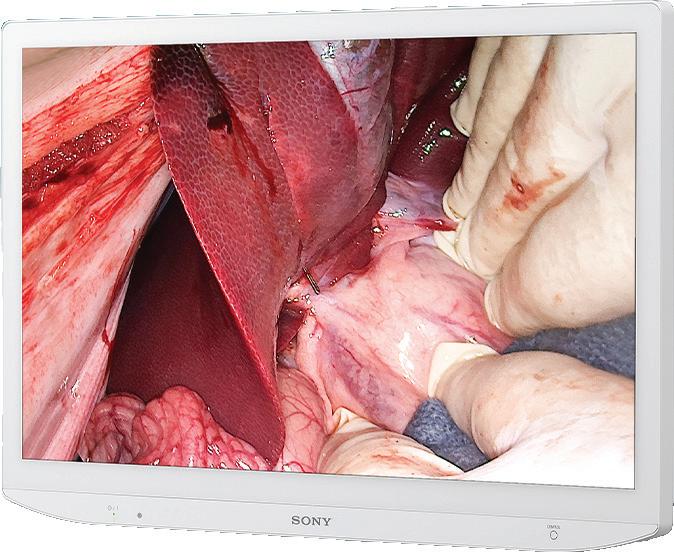
A: I take great pleasure in my role within the surgery department. The advanced life-support technology, which continually evolves, provides a rewarding experience. Each day presents new challenges due to the diverse range of surgical equipment I encounter.



Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: Working in a Children’s Hospital has long been a dream of mine, and St. Luke’s has provided me with that opportunity, being the sole Children’s Hospital in Idaho.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: My goal is to further develop my leadership capabilities within HTM and to mentor others, enabling them to excel in troubleshooting and repair skills.
FAVORITE HOBBY: I love softball; I have been playing softball for 25+ years.
FAVORITE SHOW OR MOVIE: “Pitch Perfect”
FAVORITE MEAL: Steak and potatoes
WHAT WOULD YOUR SUPERPOWER BE?
I consider myself modest as I continuously seek knowledge and am eager to assist others.
1 THING ON YOUR BUCKET LIST: One day I will swim with a dolphin.
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU:
I enjoy exploring literature and shows related to crime and murder, including the series “Dexter.”
BY K. RICHARD DOUGLAS
Arizona is a state of hot summers, winter tourists and snowbirds, the Grand Canyon and the Saguaro cactus. The state is best known for its Sonoran Desert region, although it offers several eco-systems, with pine forests in the north.
Maricopa County contains the largest population center, with the city of Phoenix within it, as well as being the central location for the state’s biomed association.
The Arizona Healthcare Technology Management Association (AZHTM) is the state’s biomed association. The association was founded in March of 2008. Desiree Nielsen is the president.
Prior attempts to gain traction with a statewide biomed association have run out of steam, partly because the state’s population center is in the Phoenix area and other population centers are more remote.
“The association originally founded in 2008 as AZMIA, but had a decline of presence around the time COVID happened. After COVID, the organization resurrected under the name Arizona Healthcare Technology Management Association in 2021 and has been going strong ever since,” Nielsen says.
Like many biomed associations, the pandemic proved to be a big interruption and halted many activities.
“It wasn’t until near the end of 2021 that the association was able to put together in-person meetings and ramp up
attendance,” Nielsen says.
Since 2021, the association has managed to host bi-monthly meetings, which include education sessions to enhance the knowledge of the technicians, engineers, leaders and vendors who attend.
“They are not casted online currently, but it is our goal to do so soon,” Nielsen says.
The group has also been active in promoting the HTM profession.
“Besides education, community outreach to spread the knowledge about this industry is another goal we are focusing on. For example, our Vice President Theresa Heitchler recently manned a booth at a youth spring carnival. The goal was to educate young students on what this field is and expose them to some of the equipment we work on. Our goal is to continue to do community outreach, as the industry will need new people to join the workforce, as the people who are currently in it start to retire,” Nielsen says.
There remains a need for more biomed training programs nationwide and there is some presence in Arizona. AZHTM had contact with one program in the Phoenix area last year.
“We have been in contact with a couple of people from the Maricopa Community Colleges. Representatives from the college system have come to some of the meetings to gain insight on what information is necessary to have in their programs and what type of programs they need to create to get students hired,” Nielsen says.
The reformed Arizona biomed association hosted its first convention this year. The first outing turned out to be a success.
“This year was our first year we were able to successfully host a conference. There were education sessions directed at biomedical and imaging technicians. Some of the topics included: AI in healthcare, lasers, soft skills, and X-ray basics, to name a few,” Nielsen says.
She says that there was also a vendor hall for attendees to peruse and interact with the vendors who participated.
“I think the main highlight from the conference this year is the fact that we were able to pull it off. We have never put on a conference before and we received a lot of positive feedback from the vendors and the attendees. We aim to make it bigger and better next year, now that we know what to expect,” Nielsen adds.
The one-day conference was on February 7 at Desert Willow Conference Center in Phoenix. The AZHTM board members and executive committee planned the conference, and Nielsen says they will likely be the planning committee for future conferences.
“Attendance was pretty decent, with about 100 people, including vendors and members,” she says.
Nielsen says that the turnout was mostly from Phoenix, though she believes that there were some attendees from other cities around the state.
“The goal in the future is definitely to expand the outreach to the northern and southern regions,” she adds.
The group is working to get news of their organization out to the biomed community and those entering the field.
“Our main source of recruiting has simply been through word of mouth and social media. Our association uses LinkedIn predominately to share the word about our association and try to bring in new members. We are currently strategizing a way to get the word out through higher education, as well as youth that are getting ready to leave high school,” Nielsen says.
She says that they have also reached out to those in affiliated professions.
“For example, our meeting in February was a combined meeting with the Central Arizona Society for Healthcare Engineering, which we leveraged to try and get new members from as well,” Nielsen adds.
The state known for cowboys, cacti and pleasant winters is also home to many HTM professionals. The AZHTM gives them an opportunity to network, gain education and unify.




Finally, the features you love most about your favorite ride share app, food delivery app, Angi, UpWork, or TaskRabbit are available for medical imaging equipment maintenance and repair.
Enter a Trace Ticket with one tap to broadcast your repair needs to a network of qualified technicians.
Review Bids to find the best service option for improved repair outcomes with less equipment down time, resulting in a lower overall cost.
Track progress, issue payments and rate services all in a single dashboard.


Speed
Instantly blast your service request to every qualified and vetted service provider

From response times to uptime, you no longer have to rely on service companies to track their own activities and performance


Like your favorite personal apps, get in-app alerts when a service technician is on their way, arrived, waiting for a part, completed a job, etc.
Competitive bidding among service technicians allows you to get the best price and only pay and track one entity


Compass One Healthcare has announced its signature healthcare technology management (HTM) brand: Intelas. Healthcare is evolving rapidly, and the need for integration, standardization, and scale is growing with it. Intelas exemplifies that and represents the next evolution of HTM at Compass One Healthcare, building upon an established foundation of trusted clinical engineering services.
“Healthcare now spans urgent care clinics, ambulatory surgery centers, imaging centers, and more and systems must manage the thousands of devices needed to connect and share data,” said Jim Cheek, president of Intelas. “Intelas captures what we stand for today: data-driven decisions, consistent performance, and a team that brings clarity and confidence to every stage of the equipment life cycle.”
Over the past decade the team has seen tremendous growth, and the new brand is in line with this and continued growth.
Cheek explained that the name itself combines intelligence and telas – Latin for web – which evokes interconnected systems. That’s intentional as it reflects the complexity of modern healthcare and Intelas’ role in bringing order and clarity to that complexity.
Intelas is now its own branded solution under the Compass One Healthcare umbrella with its own structure, specialized

tools, and a clear strategy. What hasn’t changed is the team behind it: experienced leadership, national reach, and the strong backing of resources.
HTM plays a critical role in shaping the healthcare experience for patients and care teams alike. Intelas reflects what the team has been delivering all along – a dedicated, site-based clinical engineering program with 24/7 support and deep expertise in the ongoing management of biomedical and imaging equipment. Now with a name that emphasizes the scale of its impact.
“We are just getting started. Customers will start to see new tools and solutions including forecasting system healthcare equipment maintenance,” Marley Pritchard, vice president of client experience and strategy at Intelas.
Intelas will continue to work alongside its sister sectors –Crothall Healthcare for EVS and support services, Morrison Healthcare for food and nutrition services, and TouchPoint for food and support services.
“Intelas reflects who we’ve become today, through our expanded capabilities and offerings, and use of data and analytics. We’re excited for the future of HTM and smarter asset management,” said Cheek.
The acquisition is complete, and Richardson Healthcare has officially rebranded as DirectMed Imaging.
In early 2025, DirectMed Imaging acquired Richardson Healthcare, investing deeply in expanding its Canon/ Toshiba capabilities, X-ray tube offerings, and training resources. Now, with the rebrand and integration complete, Richardson’s expertise in CT parts, tube repair, and engineer training is fully integrated into DirectMed’s operations.
“This acquisition supports DirectMed Imaging’s goal to deliver the most reliable, responsive, and comprehensive support for the diagnostic imaging community worldwide,” a news release stated.
DirectMed Imaging now offers:
• Canon/Toshiba aftermarket parts inventory
• Exclusive global distribution of ALTA750D and ALTA750G CT X-ray tubes
• Repaired Siemens Straton Z CT tube distribution
• Expanded training programs for Canon/Toshiba CT platforms
Additionally, the Toshiba representative you’ve worked with in the past will continue to be attached to your relationship with DirectMed Imaging moving forward, according to the release.
Fluke Biomedical, a Fortive company and leader in innovative healthcare solutions, recently unveiled the ESA715 and ESA712 Electrical Safety Analyzers. These groundbreaking tools revolutionize electrical safety testing, offering the same advanced capabilities as the recently launched ESA710 but with additional features, facilitating global standards testing and manual measurement mode respectively.
The ESA715 Electrical Safety Analyzer replicates the robust functionality and convenience of the ESA710, but it goes a step further by offering testing to global standards. Similarly, the ESA712 delivers the same advanced testing options but exclusively through Manual Measurement mode. These additional models continue the commitment to enhancing workflow automation, accuracy, and efficiency for healthcare technology management professionals.
The ESA715 and ESA712 maintain the compact design, 5-inch color LCD touchscreen, intuitive user interface as the ESA710, and OneQATM Workflow Automation Software onboard for the ESA715. These features standardize testing procedures, promote procedural adherence, and lead to time and cost savings for healthcare facilities. The onboard software supports automated documentation and integrates with several CMMS/EAM systems for end-toend workflow automation.
Key features of the ESA715 and ESA712 Electrical Safety Analyzers include:
• Global standards testing Manual Measurement mode

• Portable, ergonomic design with integrated handle
• OneQA-enabled workflow automation (ESA715)
• Wireless capability for field testing and automatic result synchronization
• Ten applied parts posts with LED lighting guidance
• Insulation resistance range from 50V, 100V, 250V, and 500V
• Automated test sequences for compliance to electrical safety standards (ESA715)
• ECG waveform tests and dual-lead measurements
• Easy data entry via barcode scanner, external keyboard, or on-screen keyboard (ESA715)
• Robust construction tested for rugged field applications
• Comprehensive service and coverage with the Protect+ Program
“The introduction of the ESA715 and ESA712 Electrical Safety Analyzers, in addition to the ESA710, underlines our dedication to innovation and excellence in healthcare technology management,” said Mike Nguyen, Senior Product Manager at Fluke Biomedical. “These models further our aim to set new standards for electrical safety testing in the healthcare industry.”
A proposed ASTM International standard will provide general principles for generating test report summaries from standards for medical and surgical materials and devices. The proposed standard (WK92947) will also recommend best practices regarding both content and form of these summaries.
ASTM’s medical and surgical materials and devices committee (F04) is developing the proposed standard.
“This proposed guide will help manufacturers and laboratories looking to generate clearly written and structured test reports,” said ASTM member Jove Graham, associate professor, Center for Pharmacy Innovation and Outcomes, Geisinger Health. “It will help those who are
writing new standards to make their report sections more consistent, and it will help the readers users of test report summaries.”
Graham notes that clarity of communication in test reports is important for vendors, purchasers, and regulators of medical and surgical materials and devices.
“A well-structured and well-formatted presentation of the results of premarket testing is necessary to demonstrate how those results support the claims regarding conformance of a test unit to a test method, or more broadly, claims of product conformance to medical device regulations in various jurisdictions,” said Graham.

AllParts Medical, a Philips company, announced two key leadership updates that will strengthen the organization’s growth trajectory and operational excellence. Kelly Feist has joined the company as vice president of sales, and James Akins has been promoted to vice president of operations.
The announcement was shared by Richard Gerler, newly appointed CEO of AllParts at Philips and former vice president of operations for AllParts Medical.
“We’re entering a pivotal time for AllParts Medical as we continue to scale our impact across the healthcare service ecosystem,” said Gerler. “I’m incredibly excited to welcome Kelly to the team and to celebrate James’s well-earned promotion. Both bring outstanding experience, leadership, and vision to our organization.”
Kelly Feist officially joined AllParts Medical on May 19, bringing with her over a decade of experience in healthcare technology and service leadership. She most recently served as managing director of Ascom Inc., where she led transformational initiatives in healthcare information and communications systems.
Feist holds an MBA from Vanderbilt University and a post-graduate certificate in Healthcare IT Leadership from the Harvard School of Public Health.
“Kelly’s ability to align strategy with customer value is unmatched,” added Gerler. “She’s not only a proven leader – she’s also someone who deeply understands the challenges and opportunities within our space.”
In her new role, Feist will oversee the national sales team, focusing on growth, innovation, and maintaining AllParts Medical’s industry-leading customer satisfaction.
AllParts Medical also announced the promotion of James Akins to vice president of operations. Since joining the company in 2014, Akins has served in key roles across sourcing, logistics, technical operations, and supply chain management.
Starting as a Sourcing Specialist III, Akins advanced into operational leadership roles including logistics manager and, most recently, senior manager of repair operations. Under his leadership, the company’s repair and refurbishment services have seen significant improvements in quality, efficiency, and scalability.
“James is a leader who leads with precision,” said Gerler. “He knows our business inside and out, and his steady hand has helped us continuously raise the bar on performance. This promotion is not only well-deserved –it’s critical to our ongoing success.”
In his new role, Akins will lead operations across AllParts Medical’s facilities, ensuring seamless execution, supply chain efficiency, and continued excellence in customer delivery.
The National Fire Protection Association (NFPA) Health Care Section has elected Chad Beebe, AIA, CHFM, CFPS, CBO, FASHE, deputy executive director of the American Society for Health Care Engineering (ASHE), as the group’s next chair. Beebe, who has been a section member since 2000, will start the new role on June 17.
NFPA’s Health Care Section is comprised of health care professionals from across the field – from fire safety officials and facilities engineers to long-term and acute care providers – who work together to minimize risk in health care environments. The section provides a forum to discuss and disseminate pressing issues facing health care in an effort to share ideas, solve problems and exchange information – as well as discuss and review the latest NFPA codes and standards and share opportunities for NFPA code/standard development. The section also reviews changes to the more than 80 NFPA codes and standards that apply to health care, collect section member feedback on the impact of those changes, and present the section’s recommendations to
Veteran and HTM leader Bruce Madden passed away on June 10, 2025. He was born July 27, 1950, in Lynn, Massachusetts where he attended school and graduated from Lynn Trade in 1969. He enlisted in the Air Force and served in weather equipment maintenance while stationed in Orlando; Guam; Washington, D.C.; Weisbaden AFB in Germany; and Pease AFB in New Hampshire.
After his discharge from the Air Force, Bruce went to work at Brigham and Women’s Hospital in the biomedical department and worked his way up to director the biomedical department and was in Boston for 10 years. He relocated with his wife to Fort Lauderdale, Florida, in 1989. He worked at Broward Health Hospital and then went to work at Miami Children’s Hospital where he worked in the biomedical department for 10 years. He then worked at MedEquip Biomedical until he retired in 2016.
Colleagues recall his dedication and hard work.
“Bruce and I worked together for many years, both in Boston and in Miami. In addition to being a pleasure to work with, he was knowledgeable and dedicated to his profession. I consider myself fortunate to have known and worked with him and will always treasure our years together,” Frank Magnarelli shared online.
“Bruce will always be in my heart. He was best man at my
NFPA’s technical committees developing the standards. Finally, the section identifies and delegates members to serve on the various NFPA codes and standards committees to represent health care’s interests.
“Chad’s election to chair of the NFPA Health Care Section gives health care facilities professionals an amplified voice in code and standard development and gives ASHE access to vital cross-field code and standard information that we can share with members,” says Lizzie Ortolano, ASHE’s executive director. “This also further solidifies ASHE’s role as a leader in the health care field and provides the opportunity to share how our work in the health care physical environment impacts patient care and supports better patient outcomes.”
Beebe will serve as chair of the section for a two-year term. In addition to his work at ASHE, Beebe serves on more than 20 NFPA technical committees, including as chair of the Health Care Section Codes and Standards Review Committee.
wedding with Linda, Bruce was (is) my friend. No nonsense leadership in clinical engineering at Brigham and Women’s Hospital, loved by his co-workers, dedicated and committed to healthcare,” Phil Levine wrote online.
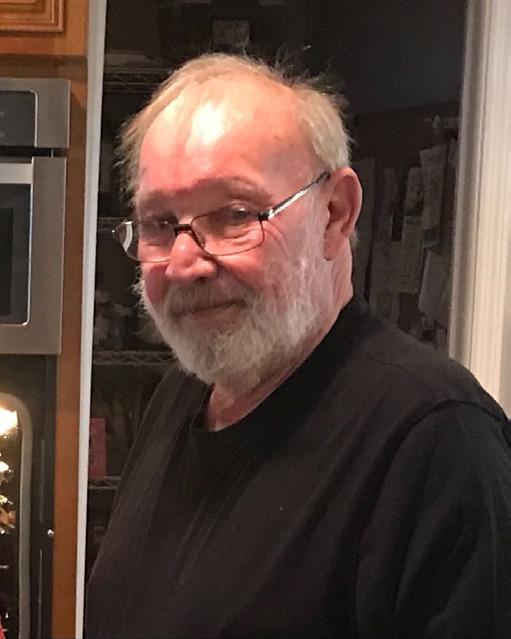
His greatest pleasure was traveling, and he enjoyed several cruise trips. Travels included a World Cruise, Alaska, Hawaii, Northern Europe, and Mediterranean cruises.
Bruce is survived by his wife Janice; sister Pamela J. Maden (Sanbornville, N.H.); sister-in-law Cathie Daugherty (Winter Springs, Fl); Sister-in-law Carol Kennedy ( Astatula, Fl); brother-in-law Thomas Clarke (Anderson, S.C.).
Nephews: John Paul Story (Swampscott, Ma). Jeffrey Rains (Anderson, S.C.); Donny (Shelly) Daugherty( Winter Springs); niece Brandi McAlister (Iva, S.C.), grandnephews Joseph Rains, Jeremy Rains, and Wyatt McAlister. grandnieces: Amber Daugherty, Madelynne Daugherty, Lauren Daugherty, Sophia McAlister.
TechNation magazine continues to promote and applaud the men and women of healthcare technology management (HTM) with the third annual Tech Choice Awards. The Tech Choice Awards (also known as the Wrenchies) shine a spotlight on the heroes of HTM.
Nominations are open through August 15, 2025. Visit 1technation.com/techchoiceawards to nominate yourself or someone else.
The newly updated award categories are:
• Professional of the Year
Sponsored by Innovative Radiology
• ISO Professional of the Year
• Young Professional of the Year
Sponsored by Prescott’s
• Military BMET of the Year
Sponsored by College of Biomedical
Equipment Technology
• Educator of the Year
Sponsored by Maull Biomedical
Enter the contest and help TechNation celebrate. Fill out the short form at 1technation.com/contest for a chance to win one of 12 prizes, each valued at $150 or more!
Additional entries to win can be acquired by sharing on LinkedIn or submitting a photo. Each month, a winner will be selected and featured in TechNation magazine!
June’s winner is Alexis Haley.

Find out more information on Page 104.

• Director/Manager of the Year
Sponsored by MW Imaging
• Women in Leadership Award
Sponsored by Avante Health Solutions
• Humanitarian of the Year
Sponsored by Pronk Technologies
• ICON Award
Sponsored by Renovo Solutions
• Industry Influencer of the Year
Sponsored by Soma Tech Intl
• Midsize Department of the Year
Sponsored by USOC
• Large Department of the Year
Sponsored by USOC
• Outstanding Vendor of the Year
• Association of the Year
Sponsored by MultiMedical Systems
The 2025 TechNation Tour rolls on this month after a stop at the HTM Mixer in Milwaukee. The tour features a long list of stops where TechNation representatives will give away swag and host some reader parties.
The next TechNation Tour stop is the 47th annual NCBA symposium being held at the Cherokee Casino Resort and Convention Center August 25-27. The annual Mike McCoy golf tournament will be held on Monday, August 25th followed by a welcome party with golf awards (all are welcome). Tuesday will be a day packed with educational opportunities, annual business luncheon, vendor show and The TechNation After Party where all are welcome. The third day includes more education and lunch with the vendors during exhibit hall hours.
The TechNation party will serve as a TechNation Tour Stop on Tuesday, August 26 at one of the restaurants inside Harrah’s Casino Cherokee from 8-10 p.m. Stop by the TechNation booth to pick up drink tickets during exhibit hall hours (4:30-7 p.m.) on August 26.
Upcoming TechNation Tour stops include:
• NESCE, Oct. 15
• MD Expo Dallas, Nov. 10
• FBS, Dec. 5





aubox is a leader in HIPAA compliant communication and marketing solutions for healthcare organizations. Trusted by over 7,000 customers, including DeVry University, Cost Plus Drugs, and Covenant Health, Paubox allows healthcare organizations to send secure, seamless messages without portals or passwords.
Its HITRUST certified platform includes outbound email encryption, inbound threat protection, and secure marketing capabilities that integrate with Google Workspace, Microsoft 365, and Microsoft Exchange. Every email is encrypted by default, reducing risk and ensuring HIPAA compliance without disrupting workflows.
Paubox Email Suite provides secure email encryption, advanced inbound threat protection, data loss prevention, and workflow automation. Paubox Marketing is the only HIPAA compliant marketing platform that lets recipients read personalized emails with PHI directly in their inbox. Paubox Email API makes it easy to integrate HIPAA compliant communication into applications and systems – no portals or logins required.
One of the newest features, Paubox ExecProtect+, blocks phishing and impersonation attempts before they reach the inbox – something traditional tools often miss. Paubox [Tags] brings instant clarity to inboxes by authenticating incoming emails that are sent by verified, safe senders, helping staff quickly identify legitimate communications. Paubox Transcription automatically converts voicemail messages into text and delivers them via encrypted email, enabling faster follow-up without compromising HIPAA compliance. Together, these tools enhance security, streamline workflows, and reduce friction for both staff and patients.
Paubox COO and Chief Compliance Officer Rick Kuwahara has over 15 years of strategic leadership in various industries from telecom to non-profits. He has established and developed Paubox’s information security and compliance program to
become the first known email encryption solution to receive HITRUST certification. He recently shared more information about Paubox.
Q: HOW DOES YOUR COMPANY STAND OUT IN THE MEDICAL EQUIPMENT FIELD?
KUWAHARA: Paubox plays a critical role in securing the communication infrastructure that supports the healthcare industry. Whether you’re a provider, vendor, or partner exchanging PHI, email remains the most common – and vulnerable – channel in healthcare. Paubox is HITRUST certified, rated #1 in HIPAA compliant messaging software by G2, and trusted by over 7,000 customers. Our platform encrypts every email by default and blocks inbound threats – without portals or passwords – helping healthcare organizations meet compliance standards and protect patient data with minimal IT overhead.
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY?
KUWAHARA: In keeping with our focus on using customer feedback as our roadmap for what to build and when, we continue to leverage AI to provide exceptional value in the following areas: email encryption, security, archiving, and data loss prevention (DLP). In the near future, we will ship enhanced email threat detection powered by large language models (LLMs).
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE OUR READERS TO KNOW?
KUWAHARA: Email security is often taken for granted – until something goes wrong. Last year, 60% of healthcare organizations experienced an email-related security incident, and many didn’t discover it until patient data had already been compromised. At Paubox, we’re on a mission to change that. Our tools work quietly in the background, helping healthcare teams protect sensitive information, reduce risk, and focus on what matters most: patient care.
For more information, visit paubox.com.

Coasting has never been Sheila O’Donnell’s style. Even in retirement, she remains deeply invested in the healthcare technology management (HTM) field, where she spent over three decades – including nearly 10 years at Crothall Healthcare.
Her path to HTM, however, was anything but routine. O’Donnell began her career focused on supply chain issues, rising steadily at the University of Virginia to become associate director of materials management. Along the way, she deepened her expertise with coursework in purchasing and material management – earning the coveted Certified Purchasing Manager credential. Never one to stand still, she later returned to her alma mater, James Madison University, to complete an MBA and strengthen her leadership acumen.
That same curiosity proved invaluable at Crothall, where she served as senior vice president of the technical resources group. Her reach was broad – touching everything from quality and informatics to cybersecurity and capital planning. Under her watch, the company earned ISO 13485:2016 recertification – a key benchmark for medical device organizations.
O’Donnell became known for her high standards and steady hand. But it was her guiding philosophy – evolve or fall behind – that truly defined her leadership style.
That mindset served her well as she navigated the evolution of HTM. “One of the coolest things in the last 10 years has been seeing the rapid evolution of IT needs in HTM,” she says.
During O’Donnell’s tenure at Crothall, many HTM departments moved away from block-and-tackle CMMS platforms and adopted smarter systems – tools that did more
than track work orders. These platforms supported real-time dashboards and deeper analytics into equipment performance, repair history, and service costs. Watching the transformation unfold, she says, was both exciting and rewarding.

“Clients’ demand for data transparency has pushed the industry to improve real-time data quality,” O’Donnell says. She likens it to a patient medical record: “We must enter data into the system on time, ready for instant consumption by our clients. Now, clients can have even greater confidence in their clinical engineering team, as real-time dashboards show exactly how their program is performing.”
Artificial intelligence, she believes, will push things even further – predicting system failures, fine-tuning labor needs, and driving smarter purchasing decisions.
“It’s an exciting new world,” she says.
Also exciting – and surprising, O’Donnell says – is the growing adoption of ISO 9001 and ISO 13485:2016 standards, which she views as a major force reshaping healthcare. These quality management systems have significantly reduced medical device risk and improved patient safety – cutting defective part rates for imaging equipment from double digits to under 2%. To O’Donnell, that shift stands out as the most unexpected innovation of her career.
While technology transformed HTM, O’Donnell’s leadership proved just as critical – especially early in her career, when she was tasked with rebuilding a team plagued by years of
instability. With morale low and an internal bet she wouldn’t last two years, she took a methodical approach. In her first 90 days, she focused on understanding the team’s challenges, then launched a three-pronged strategy built on client service, team building, and operational excellence.
“I started with planes, trains, and automobiles,” she says, “trying to learn everything that I could.”
At the heart of her plan: hiring “wow” candidates – the kind who made interviewers stop and say, “Wow, this person brings something special.” But mapping out a plan with her team made the biggest difference. “I’ve always found that the more you share and discuss with your teams, the better buy-in and support you’ll receive,” O’Donnell says. “The financial performance modeled the results of the improvements in the other areas.”
Two years later, the team had reclaimed its spot as a top performer.
O’Donnell’s advice to rising HTM leaders is simple but powerful: stay curious, stay informed, network widely, and never stop learning. “Think positive,” she adds. “That’s the No. 1 thing that opened doors for me. Have a ‘can do’ attitude!”
She emphasizes that while AI can synthesize information, human strengths – like communication, emotional intelligence,
and a relentless focus on quality – remain the bedrock of leadership.
One of the most important – yet often overlooked – skills, she says, is the ability to present ideas with clarity and conviction. “I actively sought out opportunities to present and sharpen my abilities, always welcoming feedback from my peers,” O’Donnell says. “And my peers encouraged me because they knew that improvement comes from practice.”
Throughout her career, she invested in sharpening those communication skills – training with Dale Carnegie, Toastmasters, and Ty Boyd. “The ability to tell a story that moves teams to action is critically important,” she says. Strong presentation skills, she believes, are one of the biggest differentiators in leadership – and something AI can’t replicate.”
“Seize the opportunity to develop this essential skill,” she encourages the next generation.
Grounded in curiosity, operational discipline, and powerful storytelling, Sheila O’Donnell continues to raise the bar in healthcare operations – bringing energy, insight, and innovation to every chapter. Even in retirement.
Editor’s note: O’Donnell continues to also serve on the AAMI Foundation Board of Directors. She shared more about this for the AAMI Foundation newsletter.



In today’s complex healthcare environment, the push toward becoming a high reliability organization (HRO) is not just aspirational – it is essential. HROs operate under the principle that even in high-risk, high-complexity industries, harm can be reduced or eliminated through systemic design, culture transformation, and relentless learning. For healthcare providers, this means zero preventable harm to patients and staff.
Yet, reaching high reliability is not a solo journey. It requires robust support, collaboration, and access to actionable insights. That’s where patient safety organizations (PSOs) step in – serving as critical accelerators for health systems striving toward high reliability.
High reliability organizations are those that achieve consistently safe operations over long periods despite high levels of complexity and inherent risk. In healthcare, this translates to systems and cultures that:
• Prioritize safety over hierarchy or production pressure
• Respond proactively to risk
• Learn continuously from errors and near misses
• Promote resilience and adaptability in crisis
• Empower staff at all levels to speak up and take action Moving from awareness to implementation, however, requires deep structural and cultural shifts – something many healthcare organizations struggle to sustain alone.
Becoming an HRO is a complex transformation. PSOs help healthcare providers navigate several common barriers:
• Fear of reporting – By offering federal confidentiality protections, PSOs reduce fear and encourage staff to report
safety issues early.
• Data silos – PSOs aggregate safety data across settings, breaking down silos and providing a more comprehensive picture of risk.
• Inconsistent learning – With standardized frameworks and shared insights, PSOs promote continuous, system-level learning.
• Cultural inertia – PSOs help organizations engage leadership and frontline staff alike in a shared commitment to safety and reliability.
The ultimate goal of high reliability is zero preventable harm – not only to patients but to the caregivers who support them. Partnering with a PSO can accelerate improvements in both domains:
• Improved Patient Outcomes – Safer systems lead to fewer medical errors, better clinical outcomes, and greater trust from patients and families.
• Enhanced Staff Safety and Morale – When staff feel safe to speak up and know that systems – not individuals – are held accountable, burnout decreases, and engagement increases.
• Resilience in Crisis – PSOs help organizations prepare for and adapt to emerging risks, whether it’s mitigating external factors like public health threats or an internal systems failure.
Patient safety organizations, designated under the Patient Safety and Quality Improvement Act of 2005, provide a legally protected environment for healthcare organizations to report, analyze, and learn from patient safety events without fear of litigation or public disclosure.
Here’s how ECRI’s PSO directly contributes to advancing high reliability:
1. Safe Learning Spaces: HROs thrive on learning – but true learning requires candor. PSOs offer a confidential environment where organizations can share errors, near misses, and system vulnerabilities without blame. This transparency is critical for identifying patterns and driving continuous improvement.
2. Systems Approach to Improvement: A preoccupation with failure begins with a deep, data-driven understanding of how and why things go wrong. PSOs support this by helping organizations systematically collect and analyze patient safety data to uncover patterns, identify root causes, and reveal latent system vulnerabilities. This holistic view enables proactive improvements that address failures across all levels of the organization – before harm occurs.
3. Aggregated, Actionable Intelligence: By collecting and analyzing safety event data across multiple organizations, PSOs identify systemic issues that may not be apparent within a single institution. These insights help providers anticipate risks and implement best practices grounded in collective experience – not just isolated cases.
4. Expert Guidance from Patient Safety Advisors: In HROs, frontline expertise is valued and elevated. ECRI’s Patient Safety Advisors embody this principle by providing hands-on guidance from seasoned professionals with deep clinical and operational knowledge. They work directly with
your teams to interpret data, navigate complex safety challenges, and implement best practices tailored to your environment. Their support ensures that decisions are informed by real-world experience – enhancing your organization’s capacity to learn, adapt, and lead with safety.
5. Culture Transformation Tools: ECRI’s PSO offers safety culture assessments, leadership engagement strategies, and just culture training – all of which align closely with HRO principles. These tools help organizations shift from reactive, punitive models to proactive, learning-focused environments.
6. Accelerated Implementation of Safety Practices: Through expert guidance and data comparison, PSOs help healthcare systems implement proven safety strategies more rapidly and effectively. This shortens the cycle from incident to improvement and helps spread innovations system-wide.
High reliability is not a destination – it is a disciplined, ongoing pursuit. In this journey, PSOs provide guidance, protection, and data-driven insights healthcare organizations need to succeed. By working with a PSO, health systems do not just aim for zero harm – they build the foundation to achieve it. Discover how ECRI’s PSO can help your organization achieve high reliability and put safety at the center of care.
• Over $3000 in free PM kits available with training
• Massive Troubleshooting Library
• 100s of Error Codes not found in OEM Lit
• Online and Onsite Training Available • Training BMETs since 2008


BY ROHAN PATEL
In the complex and ever-evolving world of healthcare, biomedical equipment technicians (BMETs) hold a vital yet often overlooked role. Charged with maintaining, calibrating, and repairing life-saving medical equipment, these professionals carry responsibilities that extend far beyond the technical. At the heart of their work lies a series of ethical decisions – some clear-cut, others mired in ambiguity. In the context of healthcare technology management (HTM), ethics can be defined as the principles and standards that guide responsible behavior in the development, use, and maintenance of medical technology, with an emphasis on patient safety, accuracy, transparency, and respect for human dignity. Defining and applying ethics in this field is no simple task; it requires navigating a landscape shaped by clinical needs, confidentiality, corporate pressures, and rapid technological advancement. Unlike written procedures or mechanical standards, ethical guidelines are not always concrete. They are influenced by personal values, organizational culture, and the ever-shifting expectations of society.
This essay explores the ethical challenges BMETs face, emphasizing the difficulty of outlining universal ethical standards in a field where the stakes are high and the margins for error are razor thin.
Consider a situation where a BMET is urgently called to troubleshoot a malfunctioning infusion pump in an intensive care unit. A patient is waiting on critical medication, and clinical staff are understandably anxious to get the device working again. The technician identifies the issue quickly and realizes that a temporary fix – bypassing a safety protocol – would bring the pump back online almost immediately. However, completing a proper, validated repair would take several hours and render the equipment unusable in the meantime.
Here, the technician is faced with a dilemma that many professionals in the field eventually encounter: solve the problem fast with some compromise, or take the time to ensure the equipment meets safety standards before being used again. It’s not a matter of right versus wrong in a
clear-cut way – it’s a balancing act between immediate clinical needs and the potential consequences of cutting corners.
In these moments, the core ethical principles that guide BMETs come into focus. Patient safety must always be the top priority. A quick fix that compromises the integrity of the device might help in the moment but introduces unknown risks. If something were to go wrong – if the machine malfunctions again or delivers the wrong dose – the consequences could be serious, even life-threatening. The ethical duty of a BMET is not just to get machines running, but to ensure they are reliable and safe for every patient who depends on them.
Navigating this kind of scenario requires more than just technical know-how. Communication plays a critical role. The technician should clearly explain the situation to the clinical staff: what the issue is, why a temporary repair isn’t safe, and how long a full repair will take. If there’s backup equipment available, it can be used to meet the patient’s needs while the repair is carried out properly. In some cases, consulting with a supervisor or referencing institutional policies can help support the technician’s judgment and relieve some of the pressure to rush.
Documentation is another key part of the process. Keeping accurate records of what was found, what was done, and why, not only provides accountability but also reinforces the technician’s commitment to transparency and professionalism.
Another common ethical challenge BMETs face involves the decision to repair or retire outdated medical equipment. Imagine a technician is asked to fix an aging defibrillator that has been reliable in the past but no longer meets updated manufacturer specifications or current safety standards. Replacement parts are increasingly difficult to find, and although the device could be repaired to function temporarily, it lacks the precision and performance of newer models. The hospital, however, is working under a tight budget and cannot immediately afford a replacement. In this situation, the BMET must carefully weigh technical feasibility against ethical responsibility.
From an ethical standpoint, the main concern is patient safety. Even if obsolete equipment appears functional, its
reliability may be compromised. Devices past their expected life cycle may fail unpredictably, lack modern safety features, or not meet current clinical requirements – all of which could impact patient outcomes. Continuing to use them may create a false sense of security for healthcare providers and expose patients to unnecessary risk (ECRI Institute).
At the same time, healthcare institutions operate within real-world constraints. Limited funding, especially in smaller or underserved facilities, often means extending the life of older equipment as long as possible. BMETs are thus caught in a difficult position – tasked with maintaining equipment that they know may be less safe or effective while also trying to support patient care with limited resources.
To navigate this ethical dilemma, technicians and clinical engineers can adopt a strategic, evidence-based approach:
1. Conduct a Risk Assessment: Evaluate the equipment’s history of performance, current condition, and known failure risks. This can help determine if continued use is justifiable or presents an unacceptable level of danger to patients.
2. Assess Clinical Need: Consult with healthcare staff to understand how critical the device is to patient care. If alternative equipment or procedures exist, retiring the device might not have a significant impact.
3. Review Regulatory Guidelines: Refer to manufacturer end-of-life recommendations and compliance standards to ensure continued use does not violate safety codes or facility policies (AAMI).
4. Consider Total Cost of Ownership: Sometimes the cost of frequent repairs, downtime, and lost productivity outweighs the investment in a replacement. Highlighting this to decision-makers can strengthen the case for new equipment.
5. Document and Report: If a BMET believes that using obsolete equipment poses a serious risk, it’s important to document those concerns clearly and escalate them to clinical or administrative leadership.
The long-term ethical implications of using outdated technology can’t be ignored. Beyond immediate patient care, continued reliance on aging devices may slow the adoption of better, safer technology and contribute to systemic inequality in care quality. BMETs have a duty not only to fix what is broken, but also to advocate for progress and safety within their institutions.
By grounding their decisions in risk analysis, open communication, and professional integrity, BMETs can play a vital role in balancing resource constraints with ethical obligations to patients. The choice to repair or retire isn’t just a technical one – it’s a reflection of the values that guide modern healthcare.

Rohan Patel is a Biomedical Technician I with Mountainside & Pascack Valley Hospital-New Jersey.


Danielle McGeary, CHTM, PMP, Vice President, HTM AUG 20 at 2PM ET
Registration on WebinarWednesday.live.
Eligible for 1 CE credit from the ACI.

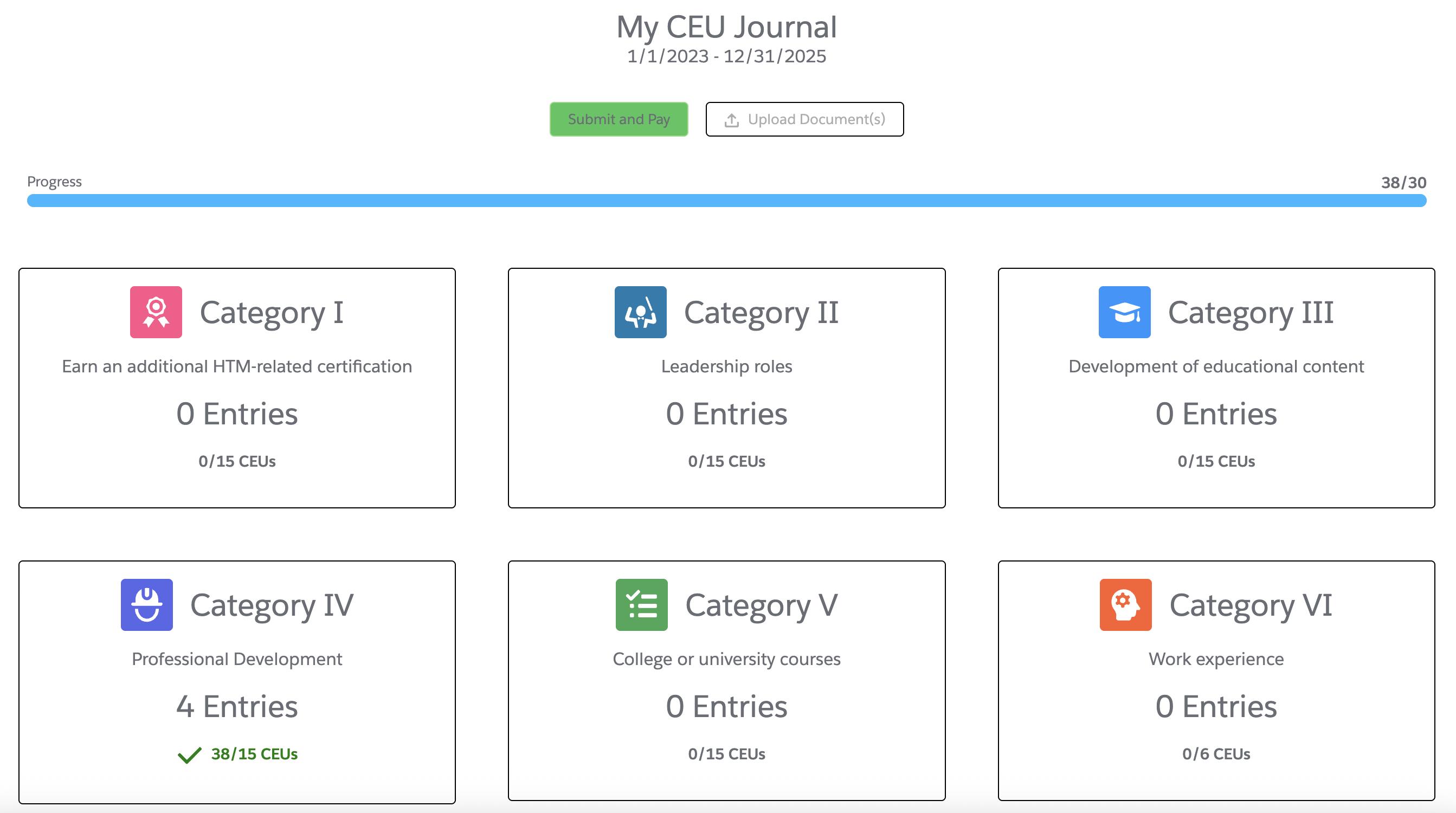
There is tremendous value and impact that comes with earning ACI certifications, including the qualifications, expectations, and long-term benefits of maintaining them. ACI certification recognizes healthcare technology management professionals who demonstrate advanced knowledge of medical devices and clinical practices, along with strong technical and problem-solving skills critical to the maintenance and
repair of healthcare technology. AAMI has a new CEU journal and tracking process, which now allows certified individuals to update and manage their CEUs in real time. This improvement is designed to streamline recertification and make it easier than ever to stay on top of your professional development.
For more information, visit aami.org.



All webinars, podcast, and product demos are eligible for 1 CE credit from the ACI.
The Webinar Wednesday session “AEDs Under the Microscope: Why Testing is Non-Negotiable” delivered critical insights into these lifesaving devices. It was sponsored by Rigel Medical and eligible for 1 CEU from the ACI.
Automated External Defibrillators (AEDs) save lives – but only if they work when it counts. Rigel Medical North America
Product Manager Lewis Lennard dove into the science of cardiac arrest and the vital role of defibrillation and CPR in emergency survival. He examined why regular AED maintenance and functional testing are essential, not optional. Biomeds were able to learn the legal mandates around AED deployment, how to ensure the devices are ready for action, and the consequences of missed testing.
In summary, the webinar helped HTM professionals understand the life-saving importance of regular AED maintenance and testing during cardiac emergencies. It explored the science behind cardiac arrest and the role of CPR and defibrillation in improving survival outcomes. Attendees also discovered more about legal requirements for AED availability and why accurate detection of shockable rhythms through routine testing is critical.
The webinar also included a live Q&A session where Lennard fielded queries from attendees and provided insightful answers that delivered additional insights.
Almost 200 individuals registered for the webinar with 98 logging in for the live presentation. A recording of the webinar is available for on-demand viewing and 1 CEU from the ACI at WebinarWednesday.live.
Alan Nicewarner, CBET, BSW Health in Texas won a Swiss Force Meister Multi-Tool during the webinar.
Attendees provided feedback via a survey that included the question, “Excluding CE credits, why do you attend Webinar Wednesday?”
“I enjoy hearing different perspectives and advice from experienced technicians,” said Joshua Abner, BMET III, Cape Fear Valley.
“Keeps biomeds such as myself informed of upcoming and/or existing policies, software, and devices relevant to the biomedical career field. Helps keep my medical device knowledge a little sharper,” Nicewarner said.
“I value continuing my education in this industry which is constantly evolving,” Biomedical Equipment Technician 1 Cody Gutierrez said.
Watch these webinars on-demand at webinarwednesday.live
The Webinar Wednesday Tools of the Trade Live Demo “Strategic Data Analysis and Planning for HTM Departments” featured FSI’s Capital Planning and Analytics tools. It was sponsored by FSI and eligible for 1 CEU from the ACI.
Presenters Joe Stockman, director of product experience at FSI, and Justin Ryan, a product owner with CMS Analytics at Enstoa Strategic, provided analysis of historical data and how it is essential for effective future planning in HTM departments. They showed how it enables teams to optimize day-to-day operations while aligning with long-term departmental goals.
The webinar explored how to use tools within FSI’s CMMS to evaluate department performance metrics, develop and communicate future plans, and monitor progress over time.
Attendees were able to view a live demo of FSI’s Capital Planning and Analytics tools and learn how to leverage them together for maximum impact. Capital Planning centralizes departmental budget data, making it easier than ever to track spending and create budget plans – directly from the dashboard and without messy spreadsheets. Analytics, developed in partnership with Enstoa, helps teams optimize resource allocation through data-driven insights and clear, actionable views of key metrics for ongoing tracking and reporting.
An informative question-and-answer session delivered additional insights to attendees.
The webinar was popular among HTM professionals with almost 100 HTM professionals registered for the webinar. Those who missed the live presentation can watch an on-demand recording of the webinar and earn 1 CEU from the ACI at WebinarWednesday.live.
Columbus Regional Health Imaging Biomedical Technician Michael Lucas won a Swiss Force Meister Multi-Tool during the webinar.
Attendees provided feedback via a survey that included the question, “What was your single biggest takeaway from today’s product demo?”
“Data analysis is important,” said Marco Guerra, a biomedical equipment analyst with UC San Diego Health.
“I enjoyed a glimpse into a mature data analytics platform. We’re currently building out similar dashboards with data from our CMMS,” shared Ernest Oates, a director of HTM and QA with Renovo Solutions.
“The importance of the implementation of the modernized and updated CMMS,” said Zach Wilbur, BMET 2, UMH-Sparrow.
“I like that everything is in a single package and can be quickly accessed,” shared Brett Hayes, CBET, Ochsner LaFayette, General Orthopaedic Hospital.



Onsite
On-demand BMET/HTM Technician(s) & Manufacture Remediation/Recall Support
Repair estimate within 48 hours, quick turnaround time & extensive list of loaners available at no charge
MMS will deploy a team of technicians to your facility to complete Annual Periodic Maintenance on your Infusion Pumps All types of medical equipment - new or refurbished

MedWrench is an online resource for medical equipment professionals (biomeds, HTMs, imaging professionals, etc) to engage with their peers about medical equipment repairs, source parts and locate a service company. The following are examples of how the MedWrench community members help each other in the website’s forums.
Q: I have a AMSCO Eagle 10 autoclave which the 5V power supply went bad and replaced for another 5V 3A power supply. The problem now is that the temp reading is unstable and the digits are blinking on the display. The temp reading doesn’t goes over 102 C and is giving error code E98. I removed the thermistor connection and when checking the temp reading on menu F1, still unstable and blinking.
A: E98 is “Abnormal rapid rise in temperature (greater than 10F in seconds)”. Double check water is making it into the reservoir? The Air Vent or fill solenoids could be leaking letting all the stream out which would stop it from getting much above 100C.
Q: During self test at about 84%, the “self test failure” message is show on display. Reading infocounter, the last error, one month old is HC204002, but nothing about actual state. Monitoring serial output, the last message is “JVM Zip Error: C :\jars\dicomToRI.jar.: Fatal error wihile inflating....” Any advice will be appreciated.
A: Hey, that “JVM Zip Error” with dicomToRI.jar is a pretty clear sign your Java environment or one of the app files is corrupted. The self-test failing at 84% ties into that because the software can’t properly load a critical component. Here’s what I’d suggest:
• Try reinstalling or repairing the Java Runtime Environment on the DryStar — sometimes it gets corrupted.
• If you have access, replace or reflash the dicomToRI.jar file (or the whole software package if possible).
• Check your system disk or storage for any errors that might cause file corruption.
• If this machine uses a recovery or service disk, consider running a full software reinstall.
This isn’t a hardware failure per se, more of a software/data problem causing the system to fail its self-test. Hopefully that points you in the right direction!
For more FREE forum information, visit medwrench.com/forums.









Two qualities matter when choosing a clinical engineering partner: skill and responsiveness. Highly trained Agiliti biomed techs and imaging engineers respond quickly when you need help repairing and maintaining medical equipment — so it’s always patient ready when your clinicians need it.

• Beds and Stretchers
• Infusion Pumps
• Ventilators
• Monitors
• Anesthesia
• Ultrasound
• Imaging Equipment
• And more

e chNation invited HTM professionals to share tips, advice and insights regarding the maintenance and repair of beds and stretchers for this installment of the popular Roundtable feature article.
Participants in this month’s Roundtable article are:
• Chris Braaten, Regional Director of Operations, Gulf Coast Region, Intelas;
• Chad Dyches, Resident Regional Manager, Intelas;
• Israel Garcia, Senior Director of Field Operations, MultiMedical Systems; and
• Brian Herty, Senior Director of Solution Management, Clinical Engineering, Agiliti
Q: WHAT ARE THE MOST COMMON ISSUES YOU ENCOUNTER WITH HOSPITAL BEDS AND STRETCHERS?
BRAATEN: One of the most common challenges that operations teams face around the management of
beds and stretchers is the lack of designated storage space. When storage space is limited, beds and stretchers may be left in hallways or tucked into corners, which not only creates clutter and potential safety hazards but also makes it difficult to track their status. The need for consistent processes and implementing a standardized workflow for equipment triage will flag problems and notify the appropriate teams, like clinical engineering, with support in escalating repairs when needed, and making more beds available quicker.
DYCHES: Biomedical equipment technicians (BMETs) frequently encounter recurring issues with hospital beds and stretchers, both of which endure constant use in clinical environments. Common problems with hospital beds include electrical failures such as broken controls, faulty motors, and damaged wiring, as well as actuator wear, brake system malfunctions, mechanical damage to components like side rails, battery issues, and faulty sensors or limit switches. Infection control is also a concern when surfaces are cracked or damaged. Stretchers often present
hydraulic system leaks, brake and steering issues, structural damage from impacts, worn mechanical linkages, degraded mattresses, and malfunctioning control handles. Across both device types, BMETs contend with broader challenges, including a lack of manufacturer support for older models, difficulties in sourcing parts, incomplete or outdated documentation, and frequent damage because of staff misuse or rough handling.
GARCIA: Bed adjustment failures (head, foot, height): Often due to motor failure or broken actuators. Stretcher height mechanism failure: Manual or hydraulic lifts can become stuck or inoperable. Brake failures: Worn-out or misaligned brake components are a safety hazard. Wheel/caster damage: Makes beds and stretchers hard to maneuver, especially over uneven surfaces. Side rail damage: Bent or broken rails may not lock properly, creating fall risks.
HERTY: Bed maintenance is one of the most underappreciated responsibilities of a clinical engineering team. Hospitals own a lot of beds, and they are high-use devices that are constantly moved and exposed to fluids and cleaners. Without proper upkeep, failure is inevitable. The most common issues we see are side rails that won’t lock or release, broken brakes or casters, failed controls and mattress/surface damage. These types of repairs directly impact safety, staff efficiency and patient flow. Staying ahead of these issues is a great way for CE to build credibility with nursing and operations.
Q: WHAT ARE THE BIGGEST SAFETY CONCERNS DURING REPAIR OR MALFUNCTION OF BEDS/ STRETCHERS?
BRAATEN: The most significant safety concerns a team can encounter is related to infection control. Teams need clearly defined and consistently followed processes, to ensure patient safety. Closely following that is the concern around patient falls, such as instances with faulty pillow speakers or bed alarms. Addressing these concerns requires a dual focus: reinforcing infection control protocols with clear workflows and ensuring that all communication tools and safety mechanisms are regularly tested and promptly repaired.
DYCHES: During the repair or malfunction of hospital beds and stretchers, significant safety concerns arise because if the complex electromechanical systems involved, posing risks to both technicians and patients. Key hazards include uncontrolled movement, which can cause crush injuries, electrical shocks from exposed
wiring, and high-pressure fluid releases resulting from hydraulic or pneumatic failures. There’s also a danger of equipment tip-over, battery-related fires, or chemical hazards, as well as patient harm from malfunction during use, such as falls or pressure injuries. Additionally, infection control becomes a concern if damaged surfaces harbor pathogens, and unsafe work practices or lack of personal protective equipment (PPE) can lead to physical injuries or contamination. Preventive measures include using lockout/tagout procedures, ensuring stability, wearing appropriate PPE, tagging out malfunctioning equipment, and adhering strictly to hospital safety and disinfection protocols.
GARCIA: Failure of side rails: Malfunctioning or improperly secured side rails can lead to patient falls. Bed height or tilt issues: Inability to properly adjust the bed may increase fall risk or impair patient care (e.g., during CPR or transfers). Inadequate braking: If bed brakes fail or are not engaged, the bed may roll unexpectedly. Heavy components: Removing or replacing motors or bed frames can lead to musculoskeletal injuries without proper equipment. Improper positioning: Attempting to repair without stabilizing the bed/stretcher can lead to it tipping or shifting.
HERTY: For our technicians, the biggest safety risk during repairs are crush injuries, electrical shock and strain from awkward lifting. Beds can drop unexpectedly if actuators fail or aren’t properly supported during repair. Electrical components also pose a hazard if power isn’t fully disconnected or if wires are exposed. And, because beds are heavy and bulky, there is a risk of strain when repositioning or removing large parts without a lift or additional help.
BRAATEN: Our preventative maintenance schedule is annually for those that we cover.
DYCHES: Under CMS and Joint Commission guidelines, healthcare facilities using an alternate equipment maintenance (AEM) program can tailor preventive maintenance (PM) schedules for hospital beds and stretchers based on risk assessments and manufacturer guidance, provided they ensure safety, reliability, and compliance. Typically, hospital beds undergo annual PM, semi-annual for high-use or ICU units, focusing on visual inspections, functional tests, electrical safety, mechanical systems, and labeling. Stretchers are similarly inspected annually, with checks on structural


integrity, built-in weighing scales, mobility systems, infection control, and safety labeling. To remain compliant, facilities must document their rationale for schedule adjustments, track failure trends, maintain safety testing, and update procedures in response to manufacturer alerts or safety notices.
GARCIA: Standard preventive maintenance (PM) schedule for hospital beds and stretchers is typically designed to ensure safety, functionality, and compliance with healthcare regulations. Specific schedules can vary depending on manufacturer recommendations, hospital policies, and bed/stretcher types (manual, electric, bariatric, ICU, etc.).
HERTY: At Agiliti, we adhere to PM intervals based on the guidelines provided by the OEM. This approach ensures both regulatory compliance and patient safety. The most common PM interval is annual, with some increased PM intervals for high-use areas where equipment is more prone to wear and failure.
BRAATEN: The introduction of new technology can certainly increase the maintenance workload, however, the benefits to patients far outweigh any added tasks or complexity. Enhanced technology often brings increased comfort, improved communication with clinical care teams, and more personalized safety features. These advancements directly contribute to better patient outcomes and satisfaction. Additionally, success of any new technology hinges on its usability. It’s important to have systems that are designed with an


intuitive, user-friendly interface, to support the clinical caregiver’s use and experience.
DYCHES: The integration of advanced technology features into hospital beds, such as bed-exit alarms, nurse call system interfaces, built-in weighing scales, and network connectivity, has significantly increased the maintenance demands on BMETs. These features introduce greater system complexity, requiring more in-depth troubleshooting for issues like false alarms, sensor faults, or communication failures. Preventive maintenance (PM) routines are now longer and more detailed, often involving software checks, calibration, and battery testing. Additionally, BMETs need specialized tools and ongoing training to handle manufacturer-specific technologies and diagnostic procedures. The rise in user-reported issues, often because of misconfiguration rather than true malfunctions, adds to the service burden. Moreover, interdependence with IT systems and network infrastructure means BMETs must frequently collaborate across departments, further stretching their time and resources. Overall, these enhancements, although beneficial to patient care, result in a significantly heavier and more complex maintenance workload.
GARCIA: More equipment equals more assets to maintain. Each bed-exit sensor, call button, integration module, etc., needs regular checks, calibration, and sometimes software updates. Devices with moving parts or sensors (e.g., pressure sensors in bed-exit alarms) require more frequent inspection or recalibration. Batteries or wireless components may need routine replacements or charging. Systems like bed-exit alarms often connect to centralized nurse call platforms or EMRs.
When something fails, maintenance teams must: Determine if the fault is in the sensor, network, server, or integration software; and collaborate with IT, clinical engineering, or third-party vendors.
HERTY: Added technology has increased the maintenance workload, mainly through more points of failure. This leads to a higher volume of service calls and longer troubleshooting times. It’s no longer just about fixing what’s broken – technicians now need to understand how the bed interacts with these integrated systems. This, in turn, also shifts the required skill set, making more advanced training necessary to keep pace with bed innovation.
BRAATEN: When evaluating new beds or stretchers, it’s important to focus on several key requirements: First are the clinical requirements: The equipment must support safe patient handling, be compatible with existing workflows, and offer features that enhance patient care and comfort. Next, we consider the facility requirements. This includes dimensions for proper fit within rooms and storage areas, durability for high-use environments, and compatibility with current infrastructure, such as doorways, elevators, and storage solutions. An increasingly important factor is how intuitive the user interface is: Beds and stretchers should be easy for both clinical and support staff to operate. Lastly, keep in mind how many physical connections to the wall there are – reducing potential tripping hazards and maintenance issues.
DYCHES: When evaluating new hospital beds or stretchers, it is essential to consider a comprehensive mix of clinical, technical, and financial factors to ensure long-term value and patient safety. Biomedical teams should focus on serviceability, including ease of maintenance, availability of parts, training, and the complexity of integrated technologies. Clinical staff require ergonomic, easy-to-clean equipment that prioritizes patient safety through features such as bed-exit alarms and adequate size and weight capacity. Administrators should assess the total cost of ownership, warranty terms, standardization opportunities, and vendor reputation. Additionally, all stakeholders must consider logistical compatibility with existing systems, ease of transport, and reliable power backup. A structured evaluation framework ensures that the beds or stretchers chosen are safe, maintainable, cost-effective, and suitable for clinical needs.
GARCIA: Build quality: Resistance to wear and tear in high-traffic environments. Serviceability: Easy access to
components for repairs. Parts availability: Long-term access to replacements. Vendor support: Local service, training, and warranty coverage.
HERTY: When evaluating new beds or stretchers, it’s important to balance clinical needs with operational efficiency. Clinical teams are very focused on patient safety, comfort and ease of use, as these factors directly impact their patients, their daily work and their safety. For clinical engineering, the focus shifts to durability, serviceability and life cycle cost. When making this decision, be sure to engage the full stakeholder team to align your organization around frontline care and longterm sustainability. And, I would be remiss if I didn’t mention that purchasing a new bed or stretcher should factor in the type of support surfaces that will be used on the frame. Compatibility is important. Finding a bed that can accommodate a broad range of support surfaces –from standard foam to air – will offer greater flexibility and standardization, while better supporting clinicians in treating all patient types.
DYCHES: Standardizing preventive maintenance (PM), especially for tech-heavy beds, and developing custom AEM protocols can reduce workload while maintaining safety. Cross-team communication, particularly with nursing and facilities, is crucial, as many bed issues stem from use and handling rather than mechanical failure. With beds increasingly networked, integration challenges with nurse call systems and EMRs require postinstallation verification. Tracking data, such as failure rates and life cycle costs, can drive smarter PM planning and justify replacements. Lastly, HTM professionals should advocate for early involvement in purchasing decisions to ensure technical needs are considered. Tools like PM templates and evaluation matrices can further support the community. Ultimately, bettermanaged beds enhance patient care and reflect positively on the HTM department’s impact.
GARCIA: As healthcare technology professionals, we’re not just maintaining equipment, we’re maintaining care continuity, patient safety, and staff efficiency.
HERTY: Hospital beds and stretchers continue to be more technology driven. With increased functionality, connectivity and smart features, they are no longer simple pieces of equipment. Make sure your teams are ready for advanced technology – invest in training or find a partner that specializes in this space. These devices play a critical role in patient care and staff safety. They may not always get attention, but they’re a foundational component of safe and efficient care.


• The fastest growing HTM talent network in the country.
• 300+ open opportunities throughout the United States.
» A variety of posting options ranging from single-job postings to 12-month unlimited memberships.
“My HR department advertised on various government sites and our web site but we did not get a single applicant in over 120 days. Fairbanks Alaska is hard to recruit for but I took out an ad on HTM Jobs and got two good applicants in less than 30 days. I am hiring them both. Thanks HTM Jobs.”
- D. Anderson, Tanana Chiefs Conference
Featured Employers: Agiliti, InterMed, TRIMEDX, Kaiser Permanente, Renovo Solutions, SPBS, Inc., Universal Medical Resources, Inc. and more!
BY K. RICHARD DOUGLAS
Those who train military fighter pilots often say that if the fighter is shot down, the value of the pilot far exceeds the jet. They mean that beyond the obvious value of a human life, but also because of the amount of investment the military makes in a fighter pilot.
The training that produces an elite aviator is extensive and significant.
This kind of career development produces some of the best pilots in the world and has been the subject of movies and books. The top gun training program for Navy pilots is widely known. This type of investment in advancing the skills produces an invaluable product.
Ongoing training and education are components of career advancement within the HTM profession as well. Training allows a biomed to increase their value to the department and allows the department to keep more service in-house. More specialized training can put a biomed on a career path into leadership.
With the exodus of older biomeds as many retire, there remains the challenge of continuity of staffing levels, maintaining crucial knowledge and developing replacements for departing leadership.
All of these challenges fall within the realm of succession planning. While often challenges for department managers and
directors, the evolving nature of retirements and new staff and management openings provide opportunities to HTM professionals for career advancement and goals.
The career ladder for a biomed is motivating because it can take a determined individual from a BMET 1 to a vice president. Training and experience coupled with career goals could take a BMET 1 to a vice president, but for those who want to continue to work with their hands, there are career paths that lead to specialized roles or cybersecurity positions.
HTM professionals who are interested in adding education opportunities, degrees, certifications or specialty endorsements may be able to find funding for that education internally.
In their presentation at the May 2025 HTM Mixer Denver; “From Job to Career: Building Your Future in HTM,” David Scott, CBET, and Brad Kaiser, CBET, asked attendees if their employer offered tuition reimbursement.
The presenters said that biomeds may be able to get education reimbursement through their employers to advance their careers.
“I always recommend young techs to use tuition reimbursement. If you have it where you work and are not using it then you are missing out a money that could be given to you. There are now online degrees you can get from the convenience of your home. Another way is advanced planning. By working with a supervisor/manager to identify areas of opportunity and plan ahead to get training for that opportunity. If you plan ahead enough it can usually be worked into the budget for the next year,” Scott says.
Kaiser also says that a good starting point is to work with a supervisor or director.
“During one-on-one sessions and annual reviews, it would be wise for a tech to discuss the benefits of the training, potential money it could save the dept, how it will increase uptime and other ancillary benefits,” he suggests.
The presenters say that another way for a biomed to advance their career is through certification. Scott offered some special insights in this area.
“Of course, I’m going to say the AAMI CBET instructor-led review that I do. This review is a new take on the old CABMET CBET Review I did for years. It was purchased by AAMI in 2019. I went along with the purchase. I instruct this review along with Don Armstrong. I always tell people to look at the outline that’s in the handbook. It’s never too early to start studying. It’s not an easy test and many people fail it,” Scott says.
He says that AAMI has other resources like the “CBET Smart Practice.” This is a bank of over 900 practice questions.
“These resources from AAMI all cost on top of the cost for the test. ($425) CABMET has a free CBET Study Check/CBET Study Flashcards – CABMET (https://cabmet.org/cbet-studycheck). It has crossword puzzles and flashcards, depending on what you like best. It can be done on your phone so you can study a little whenever you have some downtime on the go. It is not all inclusive and is under development and will improve in the future. I feel like the review that Don and I do gets people headed in the right direction, but people still need to put in the work,” Scott says.
He says that the review helps people identify weak areas
that require additional study.
“Most people usually have one area they know more about than other areas. For me, it was anatomy and physiology. Others, it might be electronics or IT. It’s important to know the make-up of the test and the percentages that are asked in category of the test. Fifty percent of the test is medical devices as related to patient care and reasoning and problem solving. The CBET test is broad based and covers all aspects of BMETs’ work and knowledge to do the job. It’s very easy working in HTM to get in a silo and only know the areas you work in. That’s why it’s important to look at the outline and understand what will be covered on the test,” Scott adds.
How can people be more comfortable about stepping outside their comfort zones and embrace new skills to enhance their careers?
“The only way to progress in this field is to challenge yourself. Start small and then expand. Shadowing a senior technician is a gateway to knowledge and experience working on more difficult modalities. Also, express this desire to grow to your leadership team and work with your leaders to develop an action plan. Keeping a record of your growth can empower you to realize how far you’ve come,” Kaiser says.
In a presentation from the 2025 Southern California MD Expo, Scott teamed up with Naka Piohia, network team leader, biomedical engineering, for the presentation “Effective Leaders Develop Their People.” In that presentation, Piohia and Scott laid out the importance of succession planning into
some of its key elements. A few bullet points are:
• Organizational stability: succession planning is essential for maintaining stability within an organization during transitions in leadership.
• Risk mitigation: effective succession planning helps mitigate risks associated with losing key leaders, ensuring a smooth transition.
• Knowledge transfer: it ensures the transfer of critical knowledge and skills from outgoing leaders to future successors.
• Employee engagement: succession planning supports employee engagement by providing career development opportunities and career paths.
The presenters said that leadership should be aware of which internal employees may be candidates for manager roles. As part of an annual appraisal review, leadership should be asking staff if promotion into manager roles is the career path that they are pursuing.
Also, some members of staff may not be interested in leadership roles currently because of extenuating circumstances but may be open to opportunities in the future.
Piohia says that leadership should not overlook the tech 1 and tech 2 members of the team who might have management experience from prior jobs that might prove valuable.
The presenters pointed out that there are many important skills that biomeds can learn by being a part of a biomed association or becoming a part of the leadership of one of those organizations. They also pointed out that there should be areas where biomed staff can learn specialized skills as part of succession planning.
Some of the categories that those skills fit into include communication skills, product management, customer relations, project management, budgeting and forecasting and performance improvement.
Piohia says that executive professional development can include OEM factory training, tech-to-tech cross training, job rotation and mentorship and job shadowing.
Scott and Piohia say that assigning some of the duties of those taking PTO to another member of staff can test that person and highlight their ability to take on additional responsibilities.
Presenting at the 2025 MD Expo in Southern California, Douglas Redwine, regional director of biomedical engineering at Piedmont Healthcare and founder of R.E.D STEM & ARTS spoke about the need to foster cross-generational knowledge
as experienced biomeds retire.
Redwine presented: “Passing the Baton: Strategies for Cross Generational Knowledge Transfer in HTM.”
He likened the handoff of the baton in a relay race to the handoff of knowledge from retiring biomeds to newer biomeds.
One method of achieving this goal is to create a mentor/ trainee program. Redwine says that senior techs should understand their evolving roles as mentors.
“Designing an effective mentor/trainee program requires intentional planning, ongoing support, and a clear alignment with organizational goals. The first step is to provide mentors with well-defined expectations regarding their responsibilities and the desired outcomes of the program. It’s important that both mentors and trainees understand the overarching mission and how their relationship contributes to that vision,” Redwine says.
He says that equipping mentors with the correct resources is also critical.
“It includes access to training materials if applicable, dedicated time carved out of their schedules for mentorship activities such as rounding to visit customers and shadowing on troubleshooting projects, and ongoing support from leadership. Without proper tools and protected time, even the most passionate mentors can struggle to be effective,” Redwine says.
He says that structured follow-up is essential.
“Hosting periodic check-ins or feedback sessions with both mentors and trainees creates an opportunity to evaluate progress, identify challenges, and share successes. These conversations not only foster accountability but also help refine the program over time. A strong mentor/trainee program doesn’t just transfer knowledge, it builds confidence, leadership skills, and helps cultivate a culture of continuous growth within the HTM department,” Redwine adds.
He adds that every voice should be heard.
“Ensuring all staff members, including new hires, can contribute meaningfully to decisions and strategic planning begins with cultivating a culture of openness and inclusion. Leadership must be intentional about creating spaces where sharing ideas is not only welcomed but expected. This means going beyond traditional hierarchies and establishing platforms where every voice has the opportunity to be heard, regardless of tenure,” Redwine says.
He suggests that one practical approach is to ensure that information and updates are transparent and easily accessible.
“Internal newsletters, digital dashboards, team huddles and
Ensuring all staff members, including new hires, can contribute meaningfully to decisions and strategic planning begins with cultivating a culture of openness and inclusion.
Leadership
must be intentional about creating spaces where sharing ideas is not only welcomed but expected. This means going beyond traditional hierarchies and establishing platforms where every voice has the
opportunity to be heard, regardless of tenure.
- Douglas Redwine
informal meeting luncheons can serve as valuable tools for keeping everyone informed and engaged. These forums also create opportunities for team members to ask questions, share insights, and feel part of the bigger picture,” Redwine says.
He says that within his own experience, he has found that technology can help bridge gaps and encourage participation.
“I’ve used tools like Mailchimp to send out virtual surveys, allowing team members to share feedback anonymously and candidly. By following up and sharing the results with the team, I not only highlight that their voices matter, but also foster an environment where feedback directly influences decisions. This kind of inclusive approach strengthens team cohesion, drives innovation, and helps ensure that strategic goals reflect the insights and experiences of the entire team, not just a select few,” Redwine says.
How can the older, experienced techs be motivated to engage in mentoring?
“Motivating seasoned technicians to take on mentorship roles isn’t always an easy task, but I tackle it by beginning with authentic, personal engagement. As a leader, I make it a priority to have one-on-one conversations with experienced staff where I share a clear vision for the need of mentorship and why their involvement is essential,” Redwine says.
He says he is certain to express to the senior techs how much he values their expertise.
“These conversations are about more than just assigning a task, but more so about inspiring purpose. I remind them of what it felt like to be new in the field – uncertain, hungry to learn, and looking for guidance. I often ask them to reflect on what they needed most at the start of their careers and then help them see how they can now be that anchor for someone else,” Redwine adds.
As biomed departments work to develop internal resources, there is a vast pool of potential new recruits that come out of diverse backgrounds according to Brian Bell, Ph.D., lead faculty for biomedical engineering technology at St. Petersburg College and founder of HTM Workshop.
He says that there are likely recruits across career fields.
“Army vets; not just BMETs, but also airplane mechanics, people who did electrical work, mechanical work, etcetera,” Bell says.
He says that other candidates can include career changers such as hospital nurse techs who want to work with equipment, cellphone repairers, etcetera.
And then, new to college students just starting out.
“My experience is one and two make up the majority of new BMETs but there are the occasional first time out of college students,” Bell says.
He says there is a need to partner together to replace retiring biomeds by recognizing that it is a team effort.
“Getting the word out, showcasing what a BMET does, telling friends and family. I would say most of my recruits are word of mouth,” Bell says.
With more and more baby-boom generation HTM professionals retiring every day, the needs to recruit and develop staff will both sustain the biomed profession and individual departments into the future. Utilizing in-house knowledge and talent, and fostering the next generation of leaders, are activities that must become a part of every biomed shop’s culture.
Presentations mentioned in this article may be viewed on the MD Expo playlist on www.TechNation.TV
TechNation magazine is excited to announce its 2025 class of 40 under 40, powered by Young Professionals at MD Expo (YP at MD). The 40 professionals in this feature were nominated based on their professional achievements, earned merits and the positive influence they bring to the HTM industry.
YP at MD influenced the idea of starting the TechNation 40 under 40. Established in 2019, the purpose of the YP at MD networking group is to provide a space where younger professionals can network with their peers to share ideas, build relationships, and feel empowered to grow in their professional roles.
“Our first 40 under 40 class was announced in 2022 and was a huge success. TechNation is excited to keep our 40 under 40 an annual spotlight feature in the August issue. The 2025 40 under 40 class is made up of hardworking and dedicated HTM professionals who have done amazing work in our industry. We look forward to celebrating their achievements!”
YP at MD Leader Megan Cabot said.
For more information on YP at MD,






Thank you to TechNation’s 40 Under 40 sponsors for recognizing the up-and-coming talent in the HTM industry. Your support of our young professionals will ensure the future of HTM is bright!








YOUNG PROFESSIONALS AT MD EXPO!




Joanna Manjarrez
TechNation is proud to power the Young Professionals at MD Expo (YPs at MD), a networking group designed to foster a sense of community among young professionals in the Biomedical/HTM industry.
Lead YP at MD
“
Having a support system—someone who understands the ups and downs of your professional journey can make all the difference. During difficult times, knowing you’re not alone brings confidence. And when people feel supported, they’re more likely to stay and grow in their careers. That’s exactly what the HTM industry needs: young professionals who are inspired to stay, evolve, and eventually lead. YP at MD plays a vital role in that journey. It’s more than just a group, it’s a stepping stone, and I’m incredibly proud of what we’ve built together.

Sydney Krieg
“...So many professional relationships are born from YP at MD which is why it is such a valuable asset to the industry.”

“YP at MD is a great way for Younger HTM Professionals to network while also building lifelong relationships with one another by sharing ideas, experiences, and much more.”
Scan Here
to learn more about YP at MD!









Emily
Hise





“YP at MD is an incredible resource to anyone up and coming in the industry. It makes room for younger professionals to network while also celebrating their wins without immediately comparing themselves to someone with decades more experience than them.”





Service Strategy Analyst with TRIMEDX
If HTM had a superhero, what would their superpower be?
Their superpower would be “Technoportation”—the ability to instantly appear wherever a device is failing, armed with the exact tool or part needed. They’d keep hospitals running smoothly, saving the day without anyone even knowing there was a crisis.

Site Manager with TRIMEDX at SSM DePaul in St. Louis
What’s one moment in your career that made you think,
“Yes, this is why I do what I do?”
Both of my children (2 boys) were born in the hospital I worked at and my wife had high risk pregnancies for both. At every appointment, during delivery, surgery, and recovery I would catch myself looking at the equipment like any biomed does in a room, and would just feel relief and peace of mind. Every device had a colleague or friend’s or even my own initials and instead of feeling anxious or worried, I was at peace.

BMET I at Sodexo
What’s a “boring” part of your job that you secretly love?
A “boring” part of my job that I secretly love is being in central sterile. Even though I may not be able to fix the sterilizers, I like to understand how the device is working and provide as much information to the vendor that I can. Being able to calibrate washers is something little that I could learn to do to help the facility.

Biomed Specialist with Kettering Health Soin Medical Center
What skill do you think future HTM leaders must develop now to stay ahead?
Communication will always be important.

What’s one moment in your career that made you think, “Yes, this is why I do what I do?”
As I was working on a lengthy flow cytometry repair early in my career, I noticed a technician was hovering quite a bit behind me. Eventually the technician let me know that if I did not get it fixed within the next few hours, someone might not get a kidney. After completing the repair and as I worked, I felt pride in knowing that I was contributing to someone else’s chance at a healthier life.

Field Service Manager at ReNew Biomedical Services
What’s a “boring” part of your job that you secretly love?
I travel full-time for work, so I spend a lot of time on the road, something many might consider the “boring” part of the job. For me, it’s actually something I enjoy; it gives me time to reflect, prepare for the day, and appreciate the different places our work takes us.
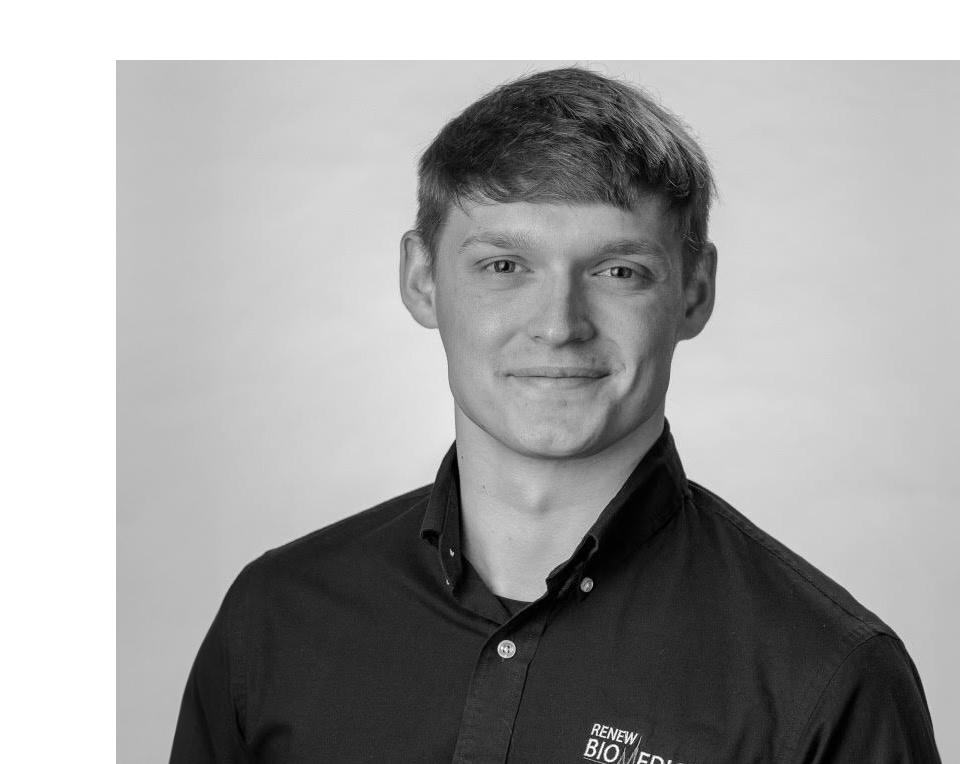

Biomed Supervisor at Kettering Health
What’s a “boring” part of your job that you secretly love?
Most people might find documentation boring, but to me, the sense of order and clarity makes it rewarding. There’s something oddly satisfying about creating order out of chaos. Having everything meticulously documented and organized feels like you’re setting the stage for everything to run smoothly and
Clinical Engineer at Hoag Memorial Hospital
What’s a “boring” part of your job that you secretly love?
I secretly enjoy digging into device logs and documentation. It may seem tedious, but uncovering hidden patterns or issues before they escalate feels like solving a rewarding puzzle.

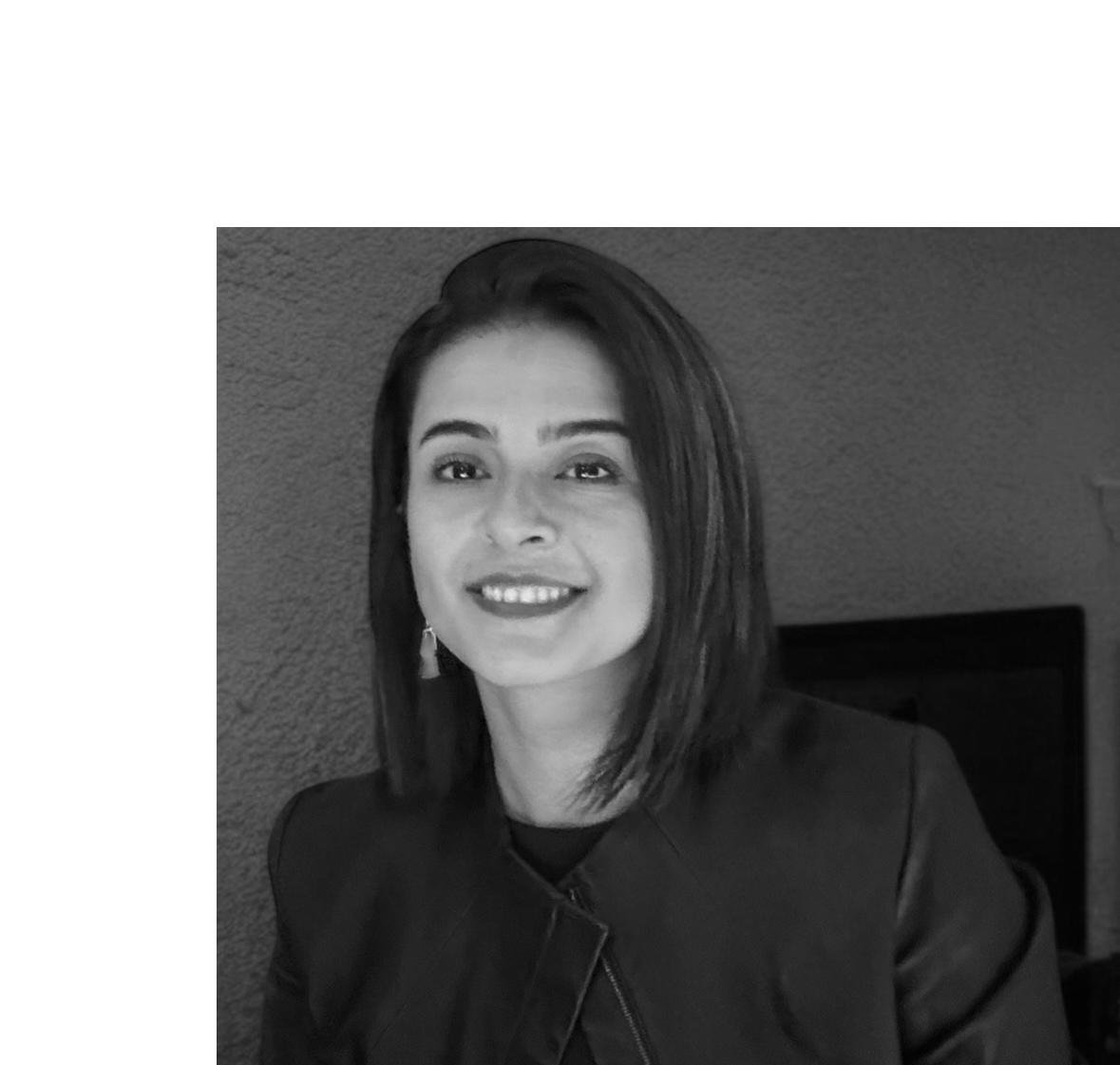
Integration Management Office Project Director at TRIMEDX
What skill do you think future HTM leaders must develop now to stay ahead?
HTM leaders need to fully lean into relationship building and development. There’s a known and obvious focus on understanding data analysis and embracing AI and machine learning; with this increased focus, the skillset that will set HTM leaders apart is their ability to connect with and create trust among people.

Enterprise Business Development Executive at PartsSource
What’s one moment in your career that made you think,
“Yes, this is why I do what I do?”
I can’t pinpoint just one moment, but honestly, every time I talk with HTM professionals, I’m reminded why I love what I do. The focus is always on supporting the clinical staff and going above and beyond to ensure quality patient care, and as my customers, the passion that drives them is the same passion that drives me. I want to support them the way they support their customers because as someone who’s had a child in and out of hospitals, I know how much that matters.

Biomedical Equipment
Technician at GE Healthcare
Inclusion Strategy and HR
Communications Senior
Manager with TRIMEDX
What’s one moment in your career that made you think, “Yes, this is why I do what I do?”
I do not have one exact moment that made me feel this feeling, but I do always feel this feeling whenever I see a patient using a piece of equipment that I have repaired as I know that the equipment is working at 100% and is providing the necessary support for them to get better.

What skill do you think future HTM leaders must develop now to stay ahead?
I think any current or future leader needs to prioritize inclusive leadership practices and improve their emotional intelligence. We won’t be able to develop our incoming, untapped talent if we do not create an environment where they can be their authentic selves.

What’s a bold prediction you have for the future of HTM?
As time passes, I believe HTM will evolve from being a support function into a strategic leadership role within healthcare systems. Biomedical equipment technicians and clinical engineers won’t just maintain technology; they’ll lead hospital-wide initiatives in data analytics, cybersecurity, and AIdriven predictive maintenance.
Vice President, Organizational Learning and Workforce Strategy with TRIMEDX
What’s a “boring” part of your job that you secretly love?
I often compare it to creating a “crystal ball” by analyzing and exploring data to understand industry trends and future forecasts. I secretly love uncovering opportunities to innovate or improve.


Biomedical Equipment
Technician with Henry Ford Health/TRIMEDX
What skill do you think future HTM leaders must develop now to stay ahead?
“Definitely adaptability, technology is always changing and I think current and future HTM leaders need to be able to continue to learn, adapt, and grow constantly to stay ahead.”
Manager/ HTM Networking & Cybersecurity Lead at Sigma Health Consulting, LLC
What’s a “boring” part of your job that you secretly love?
I enjoy writing formulas and bits of code, whether it’s in Excel, Power Apps, PowerShell, etc., to help automate or streamline tasks and workflows. While it can seem tedious, I find it very satisfying to create solutions that make tasks easier and more efficient for others.



Senior Site Manager at LCMC West Jefferson Medical Center-TRIMEDX
What’s a bold prediction you have for the future of HTM?
I believe that nearly all equipment in the future will be connected to a network and have built-in artificial intelligence, including all the HTM CMMS software out there. It’s clear to see that the future of technology, in general, is shifting towards the implementation of AI. Eventually, we’ll be able to ask our CMMS AI how to troubleshoot a specific problem and it will walk us through the entire troubleshooting process.
Clinical Engineering, Periop Team Lead at Duke University Hospital
What skill do you think future HTM leaders must develop now to stay ahead?
Future HTM leaders must prioritize “AI Orchestration & Ethical Governance” to stay ahead. This involves strategically designing and managing complex AI systems that automate core HTM functions like maintenance and cybersecurity. Simultaneously, they must navigate the ethical implications of AI, ensuring data privacy, algorithmic fairness, and human accountability in a rapidly evolving technological landscape.


Senior Imaging Engineering Specialist with Ohio Health
Engineer at Sysmex
What’s a “boring” part of your job that you secretly love?
I secretly love the process of adding new equipment into our database. There’s something oddly satisfying about it, assigning a fresh tag number, entering all the new details, attaching the installation documents. And of course, the best part: placing those crisp, brand-new stickers. It’s a small ritual, but it feels like the official start of something important.
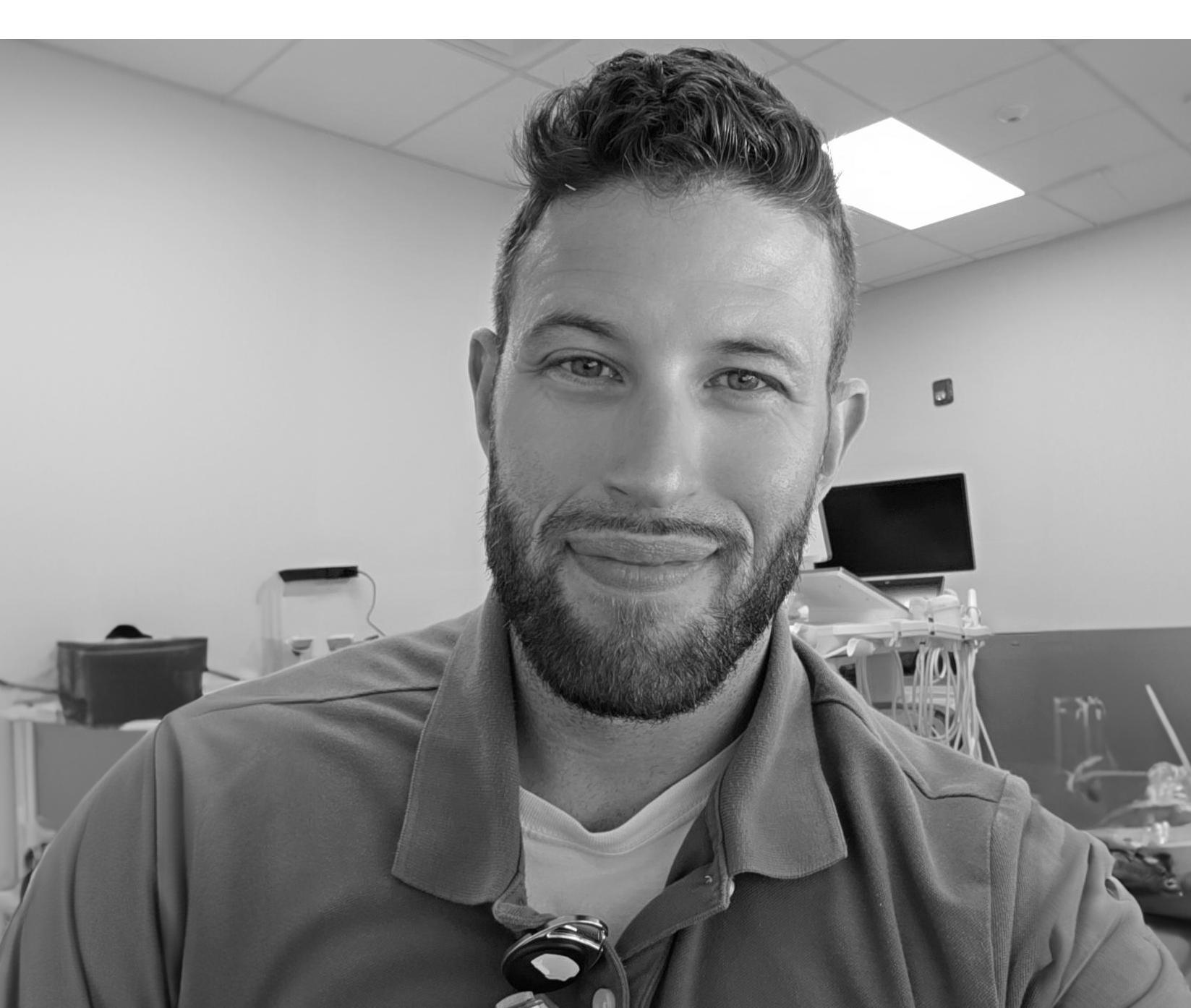
How has Ricardo contributed to the HTM industry?
Ricardo has impacted the HTM industry through his passion to learn and teach. He keeps a positive attitude, while thriving to stay knowledgeable in the field.

Lead Biomedical Equipment
Technician with Buffalo General
Hospital (Kaleida Health)
If HTM had a superhero, what would their superpower be?
An HTM superhero would be able to rapidly identify any equipment fault simply by touching it, similar to a “technopath” with built-in diagnostic vision. No missed alarms, no mysterious errors, just immediate action to keep patients safe and clinicians supported.
Biomedical Engineer at Western North Carolina VA Healthcare System
What’s a “boring” part of your job that you secretly love?
I secretly enjoy organizing chaotic inventories, as the process of uncovering device details and transforming unreliable data into trustworthy insights is very rewarding. Even though it takes a lot of time and effort to keep the inventory updated, I’m always excited to tackle the challenge!


What’s one moment in your career that made you think, “Yesthis is why I do what I do?”
At my first duty station as a military BMET, I was tasked on a quarterly mission to support a small, remote group of islands in Micronesia. In addition to servicing a variety of equipment in their medical, veterinary, and dental clinics, I serviced some AEDs on the ambulances and fire trucks. Early in the week I found one of the AED’s batteries were fully depleted and replaced them with a set I brought with me. A few days later, that AED was used to revive a patient on their way to the hospital. It was the first time I
What is something people may not know about Deborah?
Deborah is serving with her twin sister on board. Her sister serves in the HR department, so the scrubs or the fancy clothes are always an easy way to distinguish the two, until you meet them during the weekend.
Deborah is teaching her sister, Dorcas, some biomed language, so both can pretend to be the biomedical part of the twin.


Healthcare Cybersecurity Analyst at Nave Security
What’s a boring part of your job that you secretly love?
Listening. Whether in cybersecurity or clinical engineering leadership, actively listening to people’s problems can feel mundane, but it’s incredibly powerful. It’s where advocacy begins and where real solutions and trust are built.
Strategic Account Executive at CapExpert
What’s one moment in your career that made you think, “Yes, this is why I do what I do?”
The day I was able to help a health system avoid buying a whole bunch of “brand new” equipment by simply rediscovering what they already owned. It felt like finding buried treasure. Saving them hundreds of thousands of dollars and reducing waste! That’s a winwin that reminds me why this work actually matters.


What’s one moment in your career that made you think, “Yes, this is why I do what I do?”
There are quite a few moments that made me feel “yes, this is why I do what I do.” But, one of the most profound one’s is a simple one. There is a pathologist that has a microscope that makes me take 4 hours for a 30-minute cleaning. When I look at it from the beginning to the end, seeing the transformation makes me feel so pleased with myself. He does the most cases out of all the pathologists in the state’s hospital system. I always feel bad for taking so long but I do what I do because of the patient. The pathologist needs to see clear slides and to be able to comfortably go between

Service Engineer
MW
What’s a bold prediction you have for the future of HTM?
I predict that HTM will become more integrated with AI and remote diagnostics, allowing for less downtime of medical systems. This would allow for engineers to focus more on higher impact, more strategic work. Instead of spending time on troubleshooting and preventable failures, their attention could be shifted to more complex repairs.

Regional Account
Manager – Central U.S. with Tri-Imaging Solutions
What’s a bold prediction you have for the future of HTM?
I believe that the newer generations, and specifically my generation, will bring back the formality and the importance of relationships and communications. AI and technology have taken over the way we live our lives so much so that we have lost the touch of personal relations and communication. I predict the future will be digital – but our leaders will revert to the value of real relationships, trust, and strong partnerships.

Biomedical Equipment Technician II at Intelas
What skill do you think future HTM leaders must develop now to stay ahead?
While it’s essential for biomedical technicians to stay informed about new devices and best practices in preventive maintenance, I believe it’s equally important for leadership to proactively explore and implement artificial intelligence (AI) in our field. As AI becomes more integrated into healthcare technology, staying ahead of its applications will be critical for continued growth and relevance in the profession.

Biomedical Technician II with KaleidaHealth
What skill do you think future HTM leaders must develop now to stay ahead?
HTM leaders should say informed on new and developing technologies, and come up with strategies to use them in the future.

Biomedical Engineer/ Senior Consultant at Sigma Health Consulting
If HTM had a superhero, what would their superpower be?
Foresight. While some may not want to know the future, I believe it would be incredibly helpful to have prior knowledge of events such as a medical device failure or patient safety incident to prevent it from ever occurring. If you could prevent a potentially harmful situation from happening, why wouldn’t you? And, just imagine a world with no more corrective work orders, right?

If HTM had a superhero, what would their superpower be?
The ability to instantly diagnose and fix any medical device issue. Imagine an HTM hero with “Techno-Touch” powers, where just a single tap on equipment restores functionality flawlessly!
Biomedical Engineering Technician II at Tufts Medical Center-TRIMEDX
What’s one moment in your career that made you think, “Yes, this is why I do what I do?”
For me, it was when I got a piece of medical equipment back up and running during an emergency, and seeing it directly contribute to a patient’s recovery made me think, “This is why I do what I do.


Field Service Engineer with Sebia USA
What’s a “boring” part of your job that you secretly love?
A “boring” part of my job that I secretly love is running quality control after repairs and maintenance. While some may find it tedious to watch machines run patient samples and controls, I find it fascinating. Seeing the equipment in action and appreciating all the intricate mechanisms working together gives me a real sense of satisfaction and respect for the technology.

KELLY THAKKAR
Director of Sales at J2S Medical
What’s a bold prediction you have for the future of HTM?
My bold prediction is that future medical equipment will be smart enough to warn us before something goes wrong. HTM teams won’t just fix things, they will stop problems before they start. The focus will be on preventing downtime.

VISN 2 Healthcare Technology Manager at New York/ New Jersey VA Health Care Network
What’s a bold prediction you have for the future of HTM?
Every piece of medical equipment will have a digital twin that simulates performance, risks, and repair scenarios, letting HTM test solutions virtually before touching anything. This would help forecast when components will degrade, how changes will affect performance and the impact of potential repairs.

Level II Biomedical Engineer at VMS Ventura Medtech Solutions
How did Jose first get interested in HTM?
Jose’s interest in the HTM industry began in high school when he was fortunate enough to secure an internship in biomedical engineering. This experience sparked his passion for fixing machines and devices.


What’s one moment in your career that made you think, “Yes- this is why I do what I do?”
I was asked to retrieve the rescue data from an AED owned by our local fire department. This wasn’t my first time performing this job task. However, it was the first time that the device had my PM inspection sticker on the device. The device was used to save the life of a teenage boy who went into sudden cardiac arrest. It was both humbling and extremely motivational to see that my work had gone on to ensure the emergency staff had a quality, functional tool to save a life.

What’s one moment in your career that made you think, “Yes- this is why I do what I do?”
One of my jobs had me working with assisted-living centers and I was able to help a patient sleep more comfortably by fixing their bed and they were so grateful and it made me happy that someone’s family member was being treated with respect.

Experience high precision combined with intuitive usability for testing Mechanical Ventilators, Anesthesia Devices and more.






BY VICKI SALEMI
n the age of social media when our attention spans have shrunk and we continue scrolling in a matter of seconds, how can you speak effectively at work to command attention in a meeting?
If you’re wondering if our attention spans have shortened, you’re not alone. According to a podcast on the American Psychological Association, the average attention span in 2012 was 75 seconds. As for now? It’s closer to the mid-40s. Coupled with scrolling on social media, streaming TV shows and movies online and how we consume media and content, it’s more important than ever to be effective in communicating at work to capture everyone’s attention without noise. This is especially significant if you’re creating online content about your work to keep this top of mind.
According to Bill McGowan, and CEO of Clarity Media Group, two-time Emmy Award-winning journalist and author of the new book, “SPEAK, MEMORABLY: The Art of Captivating an Audience,” 45 seconds is an ideal length of time to create a tease or promotional video. “A perfect example of this is the course I host on LinkedIn Learning called, ‘The Media-Savvy Executive.’ The video intro that teases the course is just over 45 seconds, but each video lesson is three minutes or less,” said McGowan. If you’re delivering content, such as a speech, in person,
preparation is key. McGowan said, “After your content is all set, and there’s not major editing left to be done, you should adopt an 8-to-1 ratio of rehearsal time to total running time. That means if you have a 15-minute speech to give, you should be practicing out loud for two hours. So, if your presentation is on a Thursday afternoon, run through it three times on Monday, twice on Tuesday, twice on Wednesday and once on Thursday morning.”
By then you should be well-versed in the material, so if there’s a technology malfunction or you’re without your slides, you’ll be able to power through the presentation. Rehearsing aloud is key. “None of us ever makes a mistake running through our speech or presentation silently in our own heads,” said McGowan. “Only when you hear it, can you make the necessary adjustments in pace, pitch and projection. The goal is to never shortchange the prep time, no matter how good you get. Remember, it’s the diligent commitment to practice that made you better.”

Vicki Salemi is a career expert for Monster, an author, a speaker and consultant, TV commentator and former corporate recruiter. Send your questions to hello@vickisalemi.com.

BY ERIC MASSEY
remember the first time I was asked to step into a leadership role. I wasn’t given a training manual, a mentor, or even a clear explanation – just a new title and a new set of expectations. I had mastered PM completion, KPI goals, and EOC reporting, but no one had ever taught me how to lead a team.
Like many in the HTM industry, I was promoted because I was a high-performing technician – not because I was prepared for leadership. This is the silent struggle in our field. Leadership is often treated as an afterthought, something expected to develop organically once the title changes. But leadership isn’t a title. It’s a mindset. And the transition from technician to leader requires more than operational expertise – it demands personal growth, emotional discipline, and an entirely new way of thinking.
HTM professionals are some of the most technically brilliant individuals in healthcare, but as teams grow and responsibilities expand, many technicians are often thrust into leadership roles without a clear roadmap. The result? Burnout, reactive communication, and a growing disconnect between frontline execution and strategic direction. Many new leaders struggle because they haven’t received adequate training in managing people, prioritizing time, or delegating effectively. Using basic tools, such as Excel for financial tracking and PowerPoint for quarterly business reviews, or even adopting a structured approach to team development, was not on their training lists. The greatest challenge I see in the field – and the one I have experienced – is time management. Most first-time leaders try to do everything themselves. They don’t yet realize that effective leadership comes from building others up – not carrying the whole load alone. I know this because I lived it. For years, I thought being a great leader meant solving
every problem myself. It took both professional and personal pressures to realize that leadership is about empowering your team, not micromanaging them. I had to develop the people around me so they could thrive – and, in turn, lighten the burden I carried.
A turning point in my journey occurred when I began working with my close friend and life coach, Ali Rae, from Peak Mentality. Through her guidance, I learned how to manage my time more effectively, establish a consistent morning routine, and maintain a daily journal. Most importantly, I learned to prioritize my health. At my lowest, I weighed 265 pounds and experienced panic attacks from the stress. Once I decided to invest in my personal development, everything began to shift. I lost 75 pounds, found balance, and became a more present and effective leader.
I applied everything I learned to my teams, helping them gain clarity, communicate more effectively, and manage their energy and growth. The result? Happier teams, stronger performance, and a better quality of life for everyone involved.
Closing the leadership gap in HTM starts with one core shift: developing the mindset of a leader before the position requires it.
In HTM, we track CMMS data, maintain compliance, and pursue technical certifications. We all must remember that leadership is a skill, too, and it deserves the same level of intention and commitment. Whether you’re a new supervisor or a future director, treat leadership development like your next CEU.
1. Responsibility Over Blame Leaders don’t get to point fingers. They take ownership. Instead of saying, “This wasn’t my fault,” great leaders ask, “What could I have done differently?” Ownership builds trust – and trust, in turn, builds teams.
2. Respond, Don’t React
HTM leaders face high-pressure situations daily. The ability to pause, breathe, and respond with clarity instead of reacting emotionally is what sets great leaders apart.
3. See Beyond the Task
Technicians are trained to solve problems. Leaders are trained to develop people. Your job is no longer to fix equipment – it’s to build and mentor the team that fixes the equipment. That shift requires vision, patience, and communication.
Our Foundations program is just one way Compass One Healthcare is shaping the future of HTM leadership – and I’m proud to see our latest class step into that future, ready to lead. The next generation of HTM leaders won’t rise by accident. They’ll rise by design – starting with the mindset to lead well before the title arrives.

Eric Massey is the regional director of operations with Intelas.
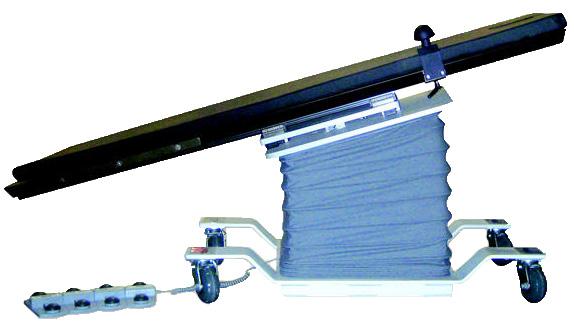

AUGUST 13
SPONSORED BY
WEBINAR WEDNESDAY
Joe Stockman and Justin Ryan lead Smart Tools for Smart Operations: AI and Technology in HTM/HFM
AUGUST 20
SPONSORED BY
TOOLS OF THE TRADE
AAMI’s New CEU Journal and The Importance of ACI Certification with Danielle McGeary, VP of HTM for AAMI.
SPONSORED BY

TOOLS OF THE TRADE Maximizing Technician Efficiency Through Integrated Testing
SPONSORED BY

AEDs Under the Microscope: Why Testing is Non-Negotiable
SPONSORED BY
TOOLS OF THE TRADE Strategic Data Analysis and Planning for HTM Departments

SPONSORED BY
Why Training is Key to a Strong Workforce with Donald Armstrong
SPONSORED BY

Mastering Precision Gas Flow Measurement and Ventilation Testing
All webinars, podcast, and product demos are eligible for 1 CE credit from the ACI.










BY PHIL ENGLERT
Medical device owners are increasingly frustrated by the limited information medical device manufacturers share about known but undisclosed vulnerabilities in medical technologies and the speed at which they patch known vulnerabilities. Leveraging the Food and Drug Administration’s MAUDE may be a way to drive expediency.
The FDA’s MAUDE database – short for Manufacturer and User Facility Device Experience – is a public repository of adverse event reports involving medical devices and is part of the FDA’s postmarket surveillance strategy. Its primary purpose is to help the FDA monitor device performance, detect potential safety issues, and support benefit-risk assessments after devices are on the market. Mandatory reporters (like manufacturers, importers, and
healthcare facilities) must submit reports when a device may have caused or contributed to a death, serious injury, or malfunction. Voluntary reporters (such as healthcare professionals, patients, or caregivers) can also submit reports if they observe or experience a device-related issue.
MAUDE is a passive surveillance system that collects adverse event reports involving medical devices, such as malfunctions, serious injuries, or deaths, from manufacturers, importers, user facilities, and even voluntary reporters like healthcare professionals and patients. The MAUDE database helps regulators and the public identify patterns, like recurring malfunctions or emerging risks, that might not have been evident during premarket testing. It’s a passive surveillance system with limitations: reports may be incomplete or unverified, and it doesn’t provide incidence rates or confirm causality. Still, it’s a powerful tool for spotting red flags and prompting further investigation.
The FDA’s MAUDE database can include cybersecurity-related reports, but it’s not explicitly
categorized that way. If a cybersecurity issue, like a ransomware attack that disables a device or a vulnerability that leads to unauthorized access, results in a malfunction or safety concern, it can be reported through MAUDE. However, the database does not have a dedicated “cybersecurity” tag or filter. Reports involving cyber incidents are typically described in the narrative fields, which means identifying them requires keyword searches or manual review.
The FDA has been increasingly focused on cybersecurity in recent years. Since 2023, it has had explicit authority to request detailed cybersecurity documentation during device submissions, and it encourages manufacturers to report vulnerabilities and incidents that could impact patient safety, even if no harm has occurred.
Here’s how to use the FDA’s MAUDE reporting system to document cybersecurity-related concerns with medical devices in your hospital or healthcare facility. While MAUDE isn’t cyber-specific, it accepts any adverse event or device malfunction that could impact patient safety, including cyber issues. Here’s an example of how a MAUDE report scenario might look when documenting a known vulnerability in a medical device, even if no patient harm has occurred yet. This is formatted as a narrative entry you’d typically find in the database.
Device Name: Infusion Pump
Manufacturer: Acme MedTech
Model Number: IPX-3000
Event Date: 2025-05-14
Report Date: 2025-05-17
Event Type: Malfunction
Reporter: User Facility (Hospital Biomedical Engineering Department)
Narrative:
During a routine vulnerability assessment conducted by hospital IT and Biomedical Engineering, we identified that the Acme IPX-3000 infusion pump model utilizes an outdated communication protocol (Telnet) for remote access by vendor service technicians. This protocol lacks encryption and authentication controls.
The vulnerability is well-documented in manufacturer security bulletins and independent cybersecurity audits. An exploit could allow unauthorized actors on the hospital network to intercept or alter pump programming commands.
Although no adverse patient events have occurred, the lack of vendor-provided firmware updates or configuration options to disable insecure protocols represents a persistent security risk. We have taken

interim steps to isolate affected devices on a VLAN and restrict access until a patch or mitigation guidance is released.
This report is submitted to raise awareness of systemic cybersecurity design issues and potential future patient safety implications. The manufacturer has been notified.
Other vulnerability issues that can also be submitted through MAUDE include: a cyber vulnerability that leads to a device malfunction or unavailability (e.g. ransomware disables a ventilator); unauthorized access is gained to a network-connected medical device (e.g. successful remote tampering of infusion pump settings); an attempted breach exposes patient data or risks device configuration; patch failures or delayed firmware updates result in system instability or raise concerns about device safety, device availability, or data privacy; or a device exhibits unusual behavior suspected to be malware-related.
To submit a report, go to FDA’s MedWatch voluntary reporting page (http://tinyurl.com/47yv22f8) or submit manually using the Mandatory MedWatch Form 3500A. Include thorough narrative descriptions, even if “cybersecurity” isn’t a checklist item, and consider appending logs or communication summaries as attachments to support your narrative. Be sure to include descriptor words like “cybersecurity,” “vulnerability,” “software weakness,” or “security misconfigurations” in the narrative as appropriate.
To protect patients’ safety and help drive meaningful changes, medical device owners must move beyond frustration and toward action. By proactively reporting cybersecurity-related vulnerabilities, whether or not harm has occurred, through the FDA’s MAUDE database, hospitals and biomedical teams can spotlight systemic design flaws, pressure manufacturers to expedite patches, and contribute to a growing body of evidence that shapes smarter regulation.
In an era where connected care is critical and cyber threats are rising, leveraging MAUDE is not just compliance – it’s advocacy. Every report is a signal that cybersecurity is patient safety, and silence is no longer an option. Start by documenting vulnerabilities, collaborating with IT, and making your voice heard – because the pulse of future-ready healthcare depends on it.

Phil Englert is vice president medical device security with HealthISAC Inc.
BY GARRETT SEELEY
recently encountered a problem caused by an in-room module startup being outrun by an updated control computer. This caused the startup process to need modification to boot smoothly. The experience made me wonder; why did this happen? After all, as troubleshooters we are naturally curious.
Upon exploring this case, the work order logs showed that this startup issue did not occur before a recent upgrade. Therefore, the upgrade itself was likely the cause. All diagnostics passed, and the unit was operational per the OEM. After observing the problem and comparing it with a non-upgraded system, it became evident that the new control was booting up much faster than before. It would boot up and time out communications before the exam room equipment could finish booting. This is most likely due to the hard drive. Let me explain.
There have been some tremendous advances in hard drive and storage technology leading to exciting results. Boot times and access speeds have improved dramatically because of the M.2 Solid State Drive (M.2 SSD). If you are not familiar with this drive, it differs significantly from the traditional platter-style drive. Let’s start with how a drive works. A traditional Hard Disk Drive (HDD) is almost like a record; it is a magnetic disk spinning under a read/write head that picks up or places individual magnetic 1s and 0s. The data is stored in a circular track, and the individual sections of the track that
hold the bytes are called sectors. Advancements in hard drive technology mean that these drives are still the most affordable for large volumes of space, often several terabytes (a trillion bytes is one TB) in size. The faster the disk spins, the faster the drive can pull data. The SATA data interface is the most common modern interface for these hard drives. It is adequate for an HDD because the spinning of the drive platter is the speed limiter. SATA has access speeds of up to 600 MB (million bytes) per second, with practical speeds closer to 500 MB/s. Despite this limit, a traditional hard drive was still faster than standard USB version 2.0 drives, CF (Compact Flash) cards, or other typically removable digital media. For reference, these use a USB 2.0 interface of around 50 MB/s or a USB 3.0 at 640MB/s. These drives are essentially a persistent style of memory used for storage. Memory itself is not storage, it is very fast but is a temporary area for the processor. I like to say that it is a workspace, not a storage space, as storage retains information while powered off. Flash drives and removable cards offer persistent storage but are slower due to their interface. Therefore, at the time of USB 2.0, HDDs were the fastest way to store and retrieve data. This only held true while flash circuits remained slow. As their speed increased and overall size shrank, it became possible to use flash format in a new type of drive, a Solid-State Drive (SSD). SSDs used the same interface as HDDs. The SSD is fully digital without spinning parts. With SSD, the SATA interface became the speed limiter. SSDs used the SATA interface to its fullest
capacity and had a distinct speed advantage over HDDs. Over time, their size increased enough to be usable as primary storage for computers. For a brief period, SSDs were used as the main hard drives for computers. Due to improvements in HDD design, HDDs retained their place as non-operating system storage drives. This is due to their larger size and lower cost. Most systems used SSDs for the operating system and critical programs, while HDDs were used for large data storage that did not require rapid access.
The evolution of computer speed continued. To further increase SSD speed, developers adopted a different interface, the PCIe card bus – the slot used for upgrading computer functions, primarily with highspeed video cards. This redesign resulted in the M.2 interface, where the SSD is placed directly on the high-speed bus. It initially increased speed fivefold compared to standard HDDs, and as SSD technology developed, these speeds increased. Currently, M.2 drives can be up to 25 times faster than standard SSDs, resulting in much faster boot times and overall system performance. A M.2 SSD can transfer up to 3 GB/s (3000MB/s) or even more. Now, hard drives are storing and retrieving information at about 1/10th of the speed of the main system memory. The M.2 SSD is getting faster with each update.
The control was booting too quickly, finishing its boot sequence, requesting communication, and timing out before the exam room side could finish booting. This was the problem. The in-room system used an embedded Windows system on removable media, specifically a CF card, which was not upgraded along with the control using a new M.2 drive. The CF system was on a USB 2.0 style interface. It can function as a main storage drive, but it is extremely slow in comparison to other drives. The only solution was either preventing power loss or starting the room modules a minute before rebooting the control, which we implemented. My concern is not just for rare conditions like restarting after a power loss, but to be aware of how design changes can cause operational challenges in the field. This is a prime example of why HTM professionals need to understand IT components to improve their troubleshooting skills. It’s impossible to know when this information will be useful. In this case, it was foundational knowledge that explained the overall problem of the system and provided for solutions. When it comes to IT components, there is already a learning curve on this material, and it will only become more obvious in time. Study up!

Garrett Seeley is a Biomedical Equipment Support SpecialistImaging with VISN 17: VA North Texas Health Care System.
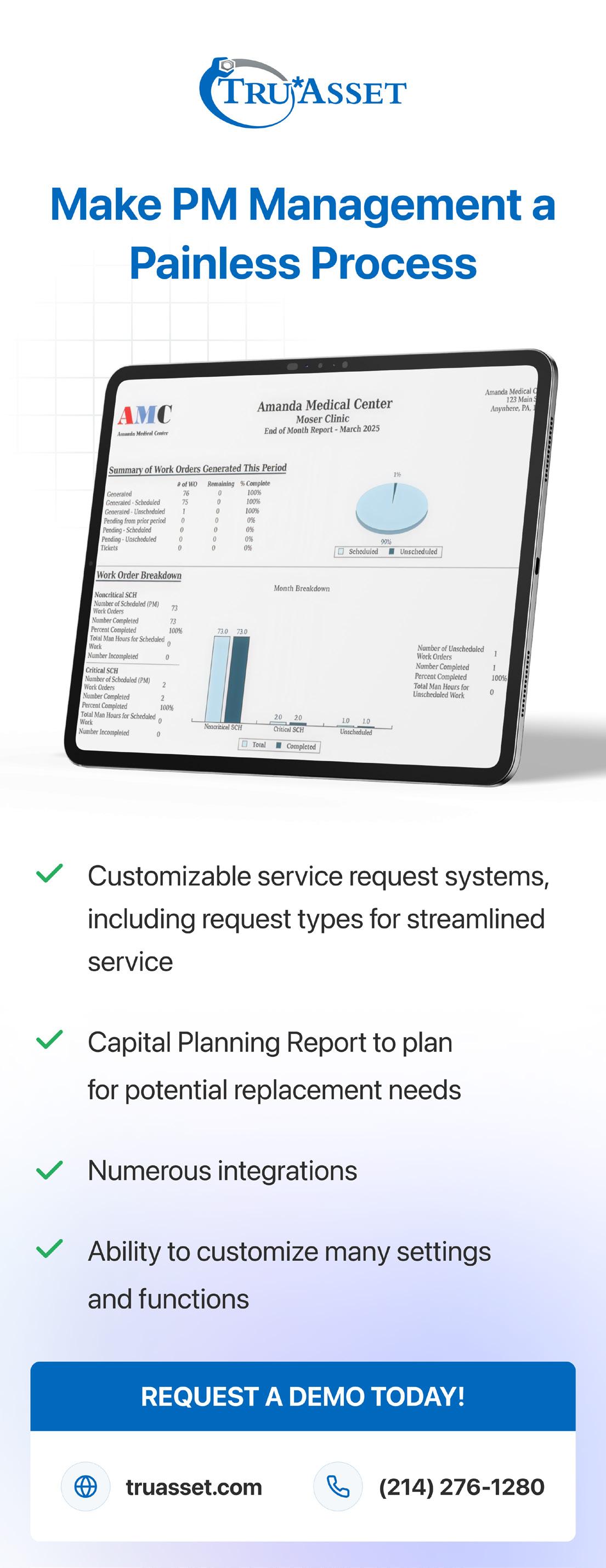

BY NATHAN PROCTOR
More and more lawmakers are coming around to Right to Repair advocates’ simple premise: People should be allowed to fix their stuff.
The campaign for the Right to Repair has been steadily building support – and this year, we’ve accelerated that pace even further. Here are some of the big recent highlights.
On May 19, Washington Gov. Bob Ferguson signed two Right to Repair bills, one covering most consumer electronics and appliances, and another covering powered wheelchairs.
Then, over a one week span at the end of May into early June, the Oregon and Nevada state legislatures passed their own wheelchair Right to Repair bills, while Texas and Connecticut lawmakers passed measures about fixing personal electronics. Other than wheelchairs, medical equipment continues to be a challenge to include in legislation.
This surge of progress makes 2025 the most productive one ever for our work on Right to Repair –and the year is not even halfway over.
MILITARY RIGHT TO REPAIR GAINS BIPARTISAN SUPPORT
In an op-ed on Fox News Digital published on May 29, Senators Sheehy (R-Mont.) and Warren (D.-Mass) announced their plan to push a new military Right to Repair bill to reform the military’s outdated procurement process. As the Senators note, the current process forces the military to rely on contractors to repair weapons systems and equipment and leads “to three critical problems: readiness, cost and lack of competition.”
Not surprisingly, a recent bipartisan and nationally representative poll of likely 2026 general election voters PIRG commissioned from Lake Research Partners and The Tarrance Group showed that voters overwhelmingly support Congress passing a law ensuring the U.S. military can repair its own equipment. The support was strongly bipartisan, with 78% of Republicans and 73% of Democrats supporting Congressional action.
Medical device repair has been one of the topics around Right to Repair for the military. Several service veterans shared stories from their time fixing medical equipment, even in war zones, while facing significant obstructions from manufacturers.

Nathan Proctor is senior director of the U.S. PIRG Campaign for the Right to Repair.
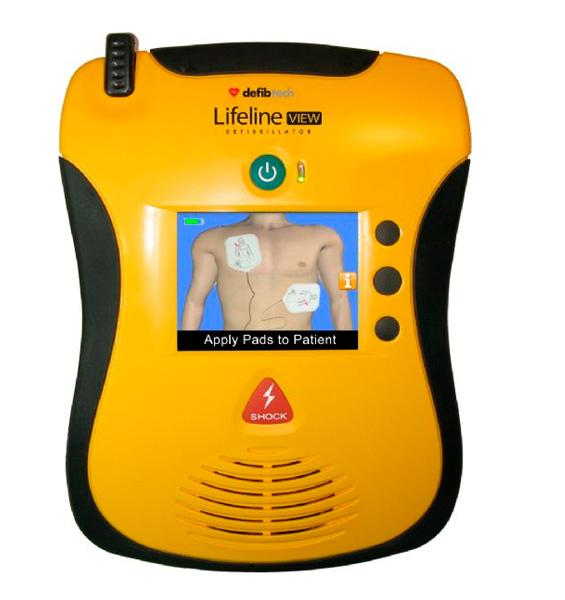
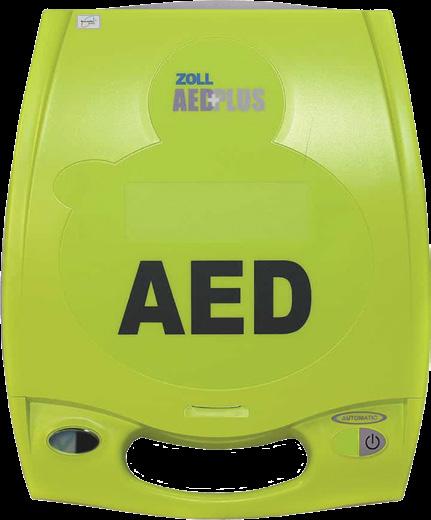







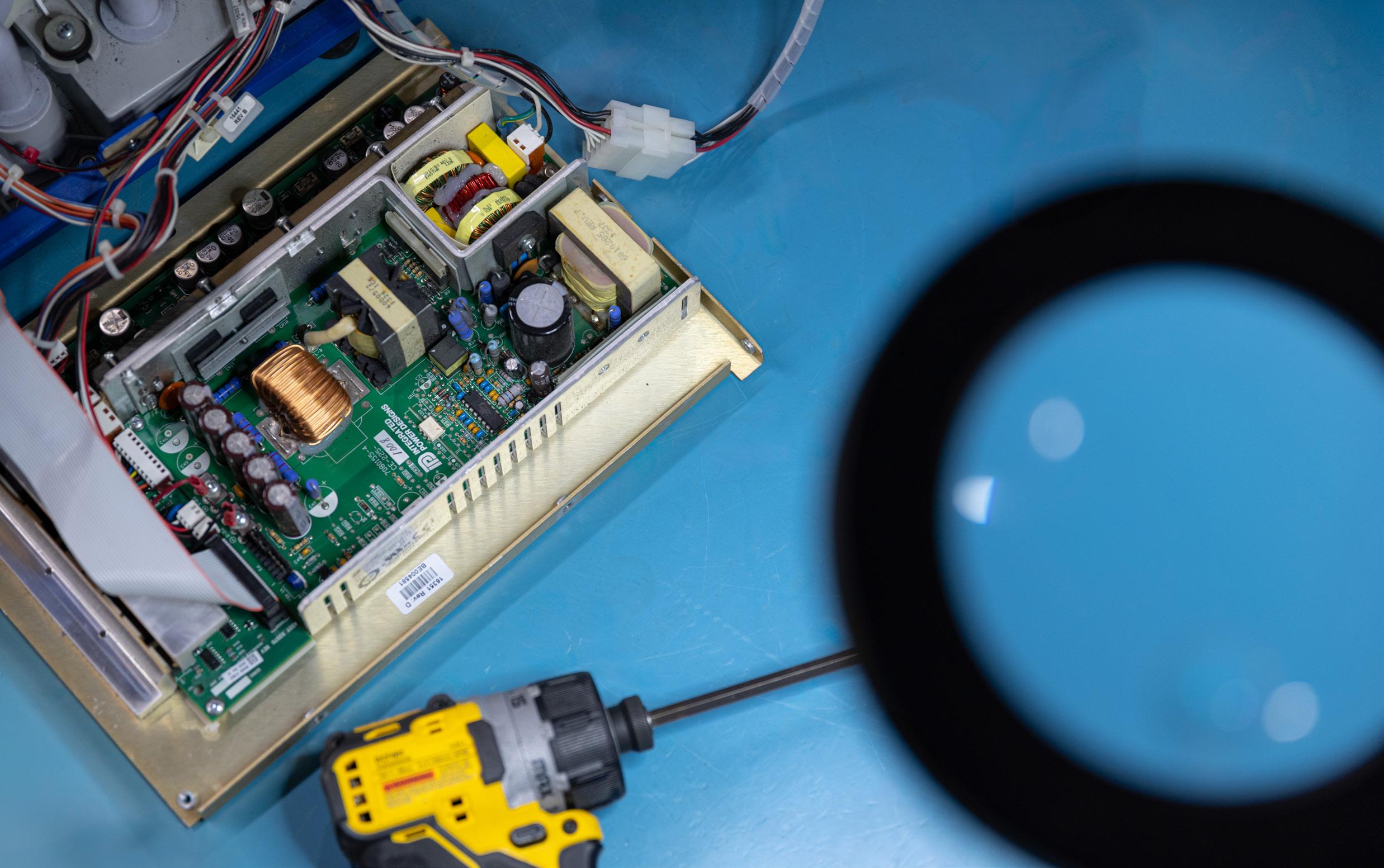
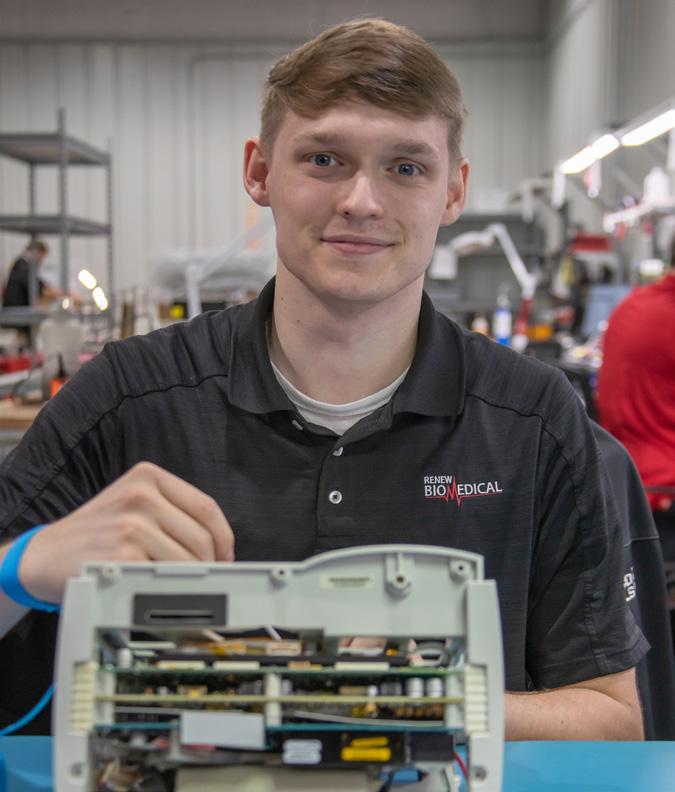

BY STEVEN J. YELTON, P.E., AAMIF
I’m proud to have been asked to participate in the 100th anniversary of the Japanese Society of Medical Instrumentation (JSMI) at its 100th annual Congress in Yokohama, Japan. In preparation for the congress, I was able to investigate the relationship between AAMI and JSMI. I found out that it has been a long and rewarding relationship. The following includes some excerpts from my JSMI presentation abstract.
I thought it would be interesting to devote this column to sharing some background and overview of the relationship between these two organizations. Many of us have participated in events with JSMI when many of their members attend the AAMI Exchange, but likely didn’t know the background.
AAMI was started in 1965 when it’s articles of incorporation were filed. This fact caused me to be fascinated that JSMI was celebrating 100 years in existence this year. AAMI, shortly after its incorporation, decided to have an active role in certification and international medical device standards. AAMI launched the BMET certification program in 1971 and then the clinical engineering certification program in 1973. The radiation equipment specialist certification was added in 1979, and laboratory
specialists in 1981.
For AAMI, standards development got a huge boost in the 1980s when the European Community declared its reliance on standards as a form of regulation in its organizing documents. “Suddenly, it was to industry’s advantage to participate in these efforts and harmonize standards across different markets,” says Mike Miller, former CEO of AAMI.
According to its website, the Japan Society of Medical Devices, a general incorporated association, was established on March 16, 1923, with the objectives of contributing to the advancement of medicine and the development of the medical device industry, while contributing to the spread of science and technology related to medical devices. At the 7th General Meeting of the Japan Medical Association in 1926, it was recognized as the 34th subcommittee of the Japan Medical Association, and on April 1, 2011, it obtained legal status as a general incorporated association and continues to exist to this day.
The membership of the JSMI is made up of medical professionals such as doctors, medical and medical researchers, nurses, clinical engineers, sterilization technicians, and material department staff, as well as science and engineering researchers involved in the research and development of medical devices, and medical
device-related companies responsible for product development, manufacturing, and distribution, and is an academic organization that advocates contributing to the advancement and development of medicine and medical devices.
Over the years, both organizations have worked closely to enrich the global healthcare technology community. JSMI has been a vital contributor to AAMI’s annual conferences, providing sponsorships for educational programs and cohosting scientific sessions. In return, AAMI has sent its members to Japan, offering expertise and insight into various facets of medical technology. These exchanges have proven valuable, fostering mutual respect, understanding, and a deep sense of international solidarity in healthcare innovation.
The origins of this enduring relationship date back to the leadership of Dr. Masakazu, the then-chairman of JSMI’s International Liaison Committee, and Dr. Harold Laufman, AAMI’s president at the time. Their visionary collaboration, initially marked by the exchange of ideas and the introduction of AAMI’s quality systems course to Japan, laid the foundation for a bond that would grow and thrive.
As AAMI continues its collaboration with JSMI, we look forward to a future of shared innovation, learning, and growth. The partnership between AAMI and JSMI exemplifies how cooperation across borders can drive progress in healthcare, benefiting patients and healthcare systems worldwide.
AAMI’s work is guided by its core mission to promote the safe and effective use of health technology. Central to this mission is the Develop-Adopt-Apply model, which ensures that AAMI’s standards and guidance documents are relevant and impactful:
1. Develop: Identifying and creating the right standards at the right time to address emerging challenges and technologies.
2. Adopt: Actively promoting the adoption of these standards by medical device manufacturers, regulators, and healthcare organizations worldwide.
3. Apply: Ensuring that standards are effectively implemented in real-world settings to drive tangible improvements in safety and efficacy.
This model drives AAMI’s core work, which includes standards development, training and certification programs, and events designed to engage the global community and advance healthcare technology.
In honor of JSMI’s 100th annual Congress, AAMI reaffirms its commitment to fostering safe, effective healthcare technology through global partnerships and cooperation. Together, we can continue to shape the future of healthcare and improve patient safety for generations to come..

Steven J. Yelton, P.E., AAMIF; is a senior HTM consultant for a large health network in Cincinnati, Ohio and is a professor emeritus at Cincinnati State Technical and Community College where he teaches biomedical instrumentation (HTM) courses. He is a member of the AAMI Foundation board of directors.
is a customer service based parts provider that specializes in all imaging modalities and manufacturers. Created to offer hospitals and ISO’s a cost effective and time saving solution for ordering imaging replacement parts, equipment moves, ultrasound probe repair and on-site service. Contact us today, we are confident you will see us as THE Parts Solution!
1 They connect ECG electrodes to a patient monitoring device, 2 words
6 Device that attaches peripheral devices to a computer
8 Small flexible tube inserted into a body cavity for draining off fluid or introducing medication 10 ____ output monitor: device used to assess kidney function and fluid balance
11 Factor that influences the longevity of medical equipment
12 Military leave, for short
_____ screen, interface for viewing patient vitals and data
18 Quiet!
19 It measures various forms of hemoglobin and oxygen content in blood
Vital gas for the operation of MRI machines, symbol
Device used to measure thicknesses
Lined up, 3 words
A tympanic thermometer measures body temperature from this organ
Approximate arrival time, abbr.
Tie the knot
Set of two
____ Cap: headgear embedded with electrodes to record brain activity
Drivers licenses, for example
Temperature control, for short










The words can appear horizontally, vertically, diagonally, and may be spelled forwards or backwards.
1. Forty under forty
2. Emerging Leaders
3. HTM Trailblazers
4. Future of Biomed
5. Innovation
6. Rising Stars
Samantha Gallegos
Clinical Engineer Tech II
Intermountain Health, Peaks Region
Five things I have at my desk are...
• Fluke ProSim 4 vital signs simulator
• Hemostats
• Powered Screwdriver
• Tape Measure
• Stitch figurines that I love.
Submit your bench to be featured in TechNation at 1technation.com/my-bench/. You could win a $25 Amazon gift card via the “What’s On Your Bench” Contest!
7. Next Gen
8. YP at MD
9. Young Professionals
10. Ambitious
11. Motivated
12. Outstanding
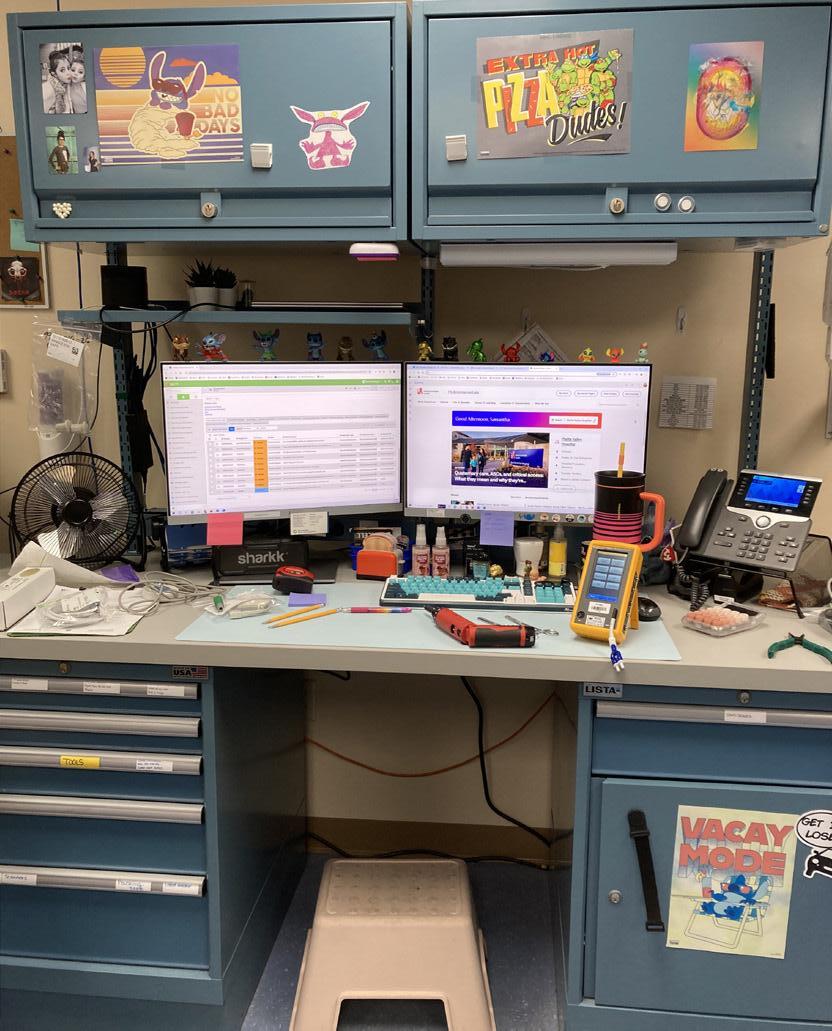
MedWrench has you covered with thousands of manuals, user guides, and expert insights right at your fingertips.



No account?

When time is critical and patient care depends on reliable equipment, there’s no room for digging through drawers or chasing down missing manuals. MedWrench is your one-stop destination for medical equipment resources - INSTANTLY SEARCHABLE, ALWAYS AVAILABLE.
Need a manual? Browse thousands of equipment pages on
No problem. Sign up in seconds and start exploring.
The 2025 AAMI eXchange brought together the HTM community, as well as some sterile processing professionals, for an unforgettable weekend filled with education sessions, HTM leadership training, a career fair, a charity golf tournament, and much more!
1. The Girls on Fire went live from the TechNation booth with AAMI’s roaming reporter the Bearded Biomed Chace Torres.
2. G. Wayne Moore and Dr. Binseng Wang pose with moderator Larry Hertzler after their debate on medical device remanufacturing.
3. AAMI BMET Apprenticeship graduates receive recognition on the main stage.
4. MD Publishing Founding President John Krieg popped into the AAMI broadcast booth to celebrate TechNation’s 15th anniversary.

5. The annual golf tournament provided fun and networking.
6. Jayme McKelvey welcomes over 150 attendees that gathered for the prize drawings after participating in the annual MedWrench Ben C. Scavenger Hunt at the AAMI eXchange.
7. The AAMI eXchange exhibit hall included industry-leading companies.
8. AAMI Foundation scholarship honorees enjoy a moment in the spotlight.




1 3 6 4 2 7 5 8



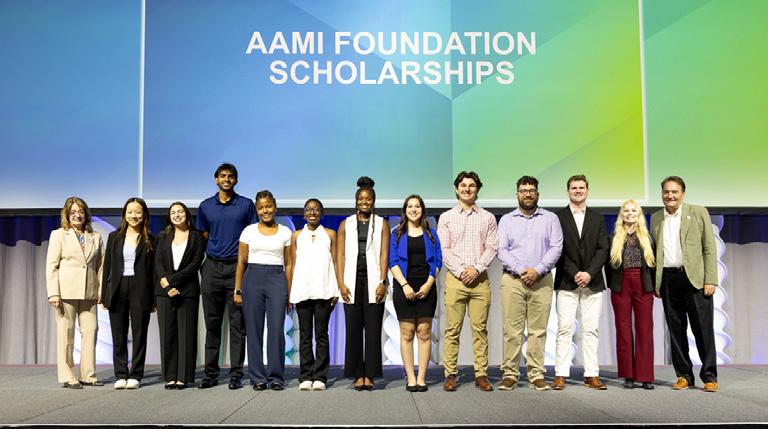




Admar Neuro admarneuro.com • 728-900-3969
AM Bickford ambickford.com • 800-795-3062
BC Group bcgroupstore.com.com • 314-638-3800
Interlight interlightus.com • 800-743-0005
Jet Medical jetmedical.com • 714-937-0809
Metropolis International metropolismedical.com • 718-371-6026
PM Biomedical pmbiomedical.com • 800-777-6474
Pronk Technologies, Inc. pronktech.com • 800-609-9802
Renovo Solutions renovo1.com
Secure Mount securemount.com • 517-784-9613
Tri-Imaging Solutions triimaging.com • 855-401-4888
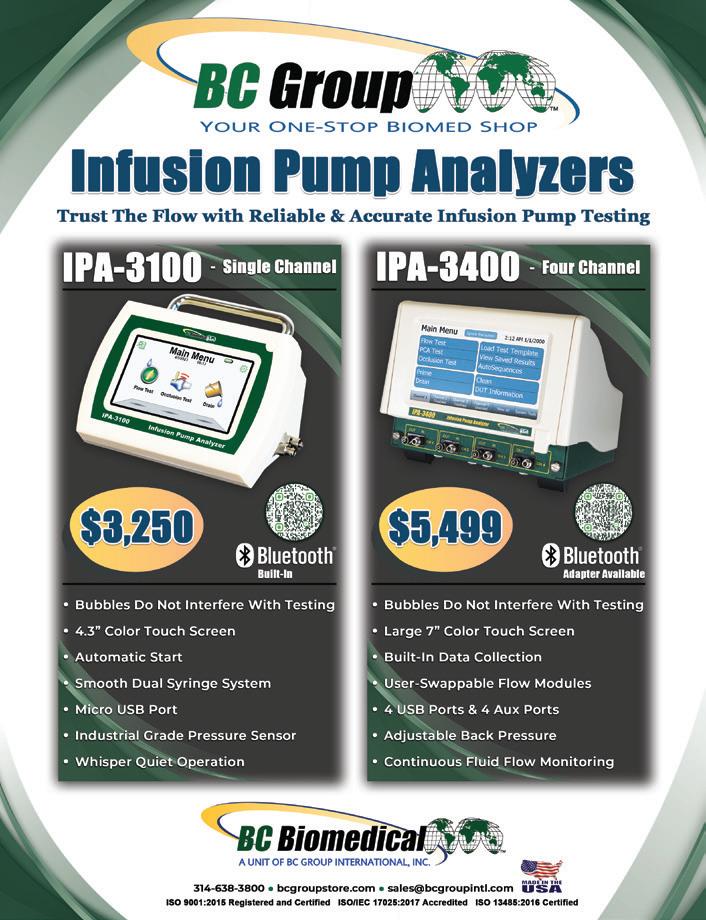
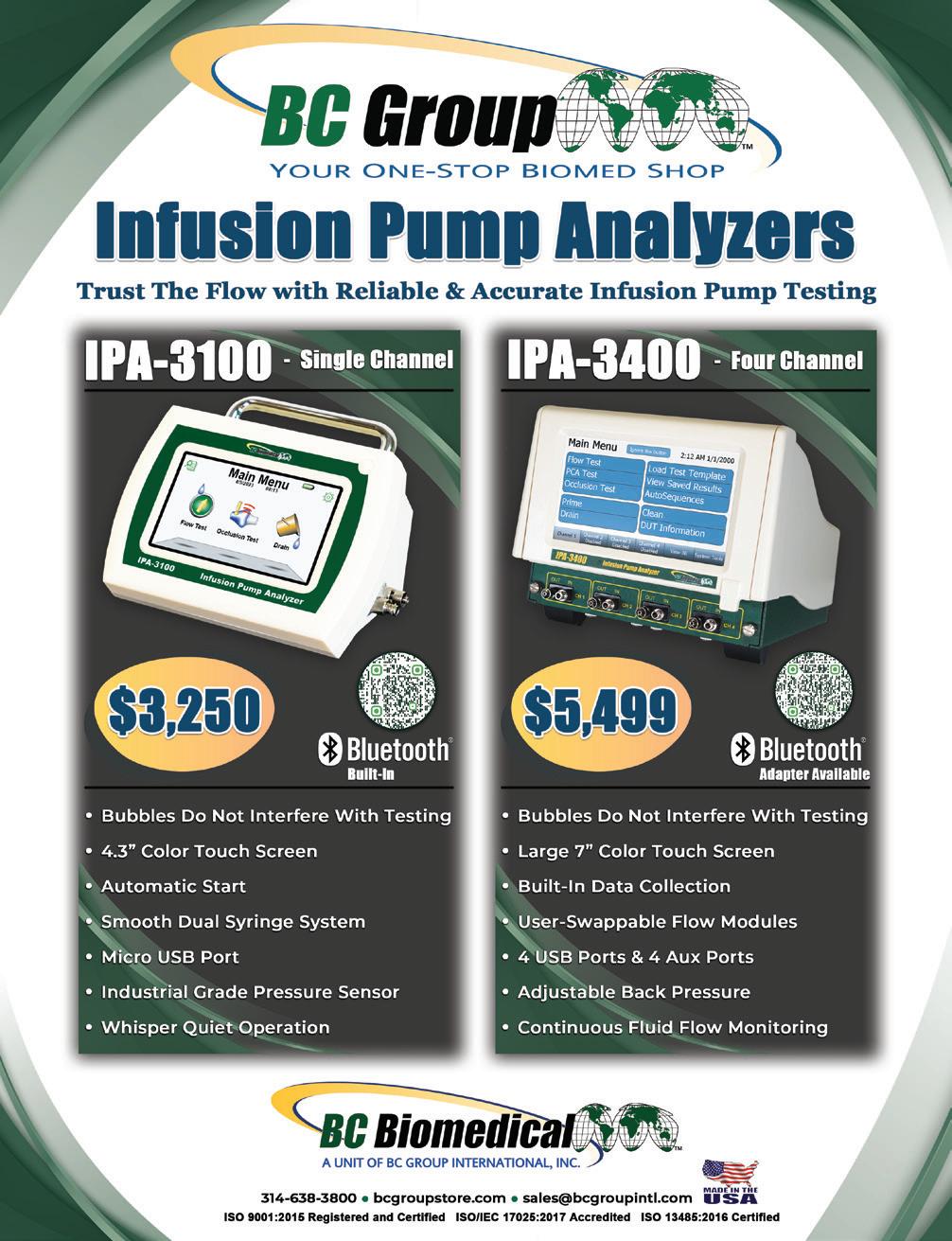

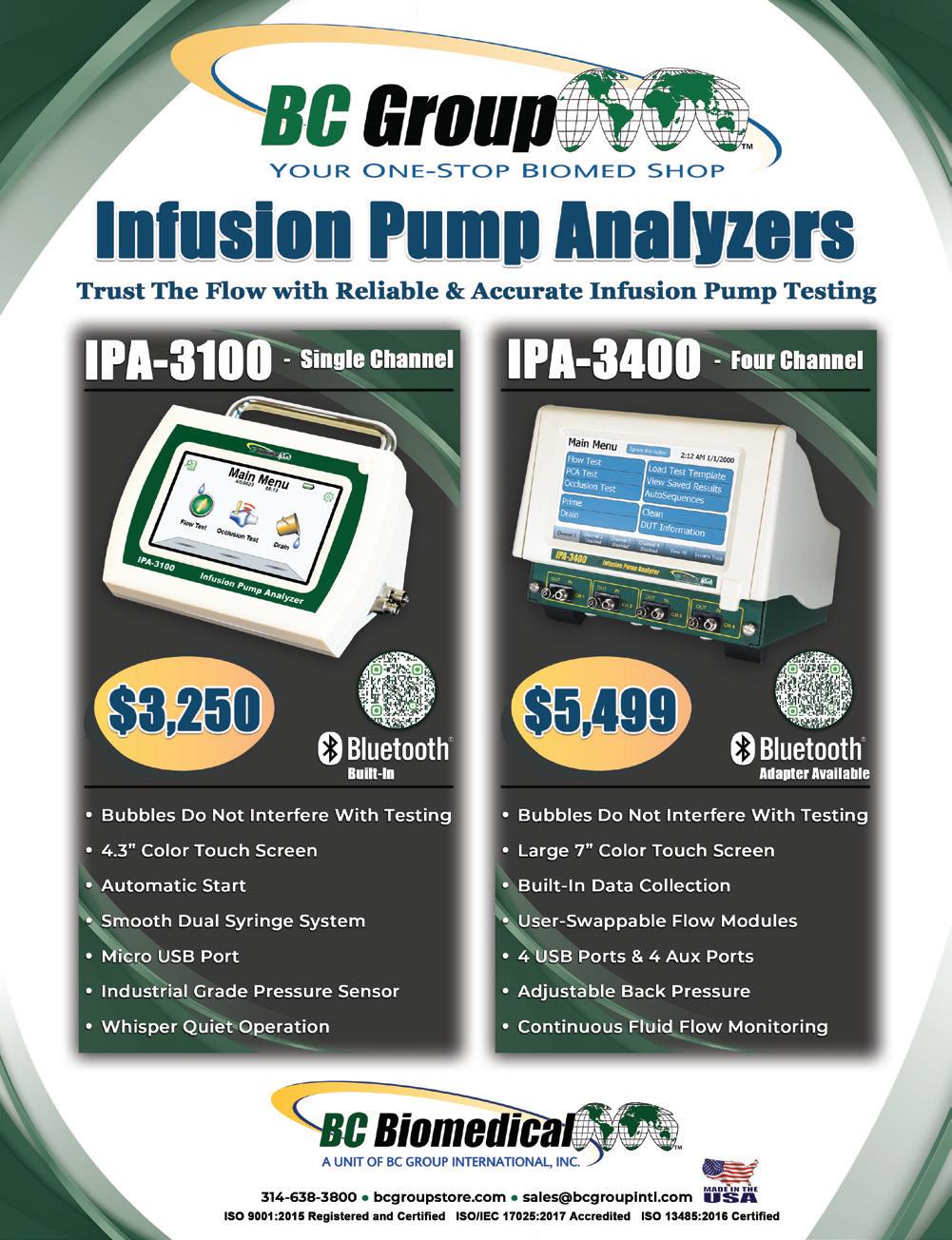

...Since you are still flipping through this magazine, it simply means you still have not found an honest, reliable, pre-owned imaging company that sells working systems.
Well, Look No Further!


























Tcutting-edge platform system monitoring. streamlines parts ordering and tracking. minimizes downtime and optimizes operations, medical imaging.
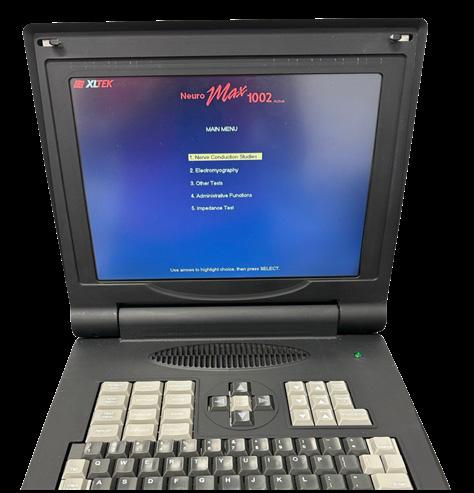








cutting-edge platform that enhances supply chain and system monitoring. It provides engineers with tutorials, and streamlines parts ordering and tracking. tform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.


Tri-Imaging
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs
cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.







XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs
Check out our Youtube channel for more information and exclusive content!

Regular






Even the most rigorous reprocessing protocols can miss hidden debris or damage. Our advanced borescope goes where the eye can’t — deep into narrow lumens — using AI to ag anomalies in real time. Because when it comes to patient safety, nothing should go unnoticed.

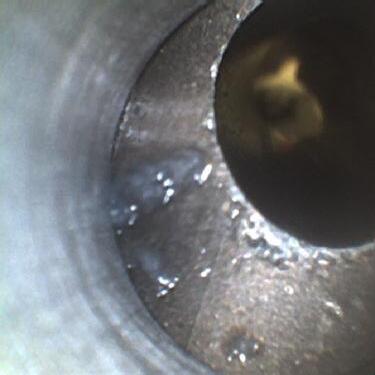

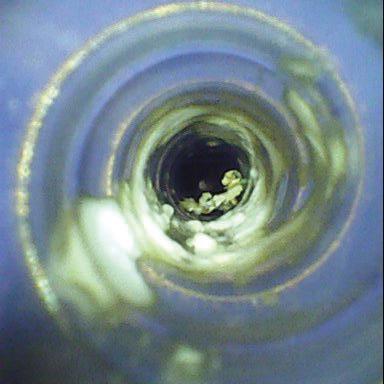

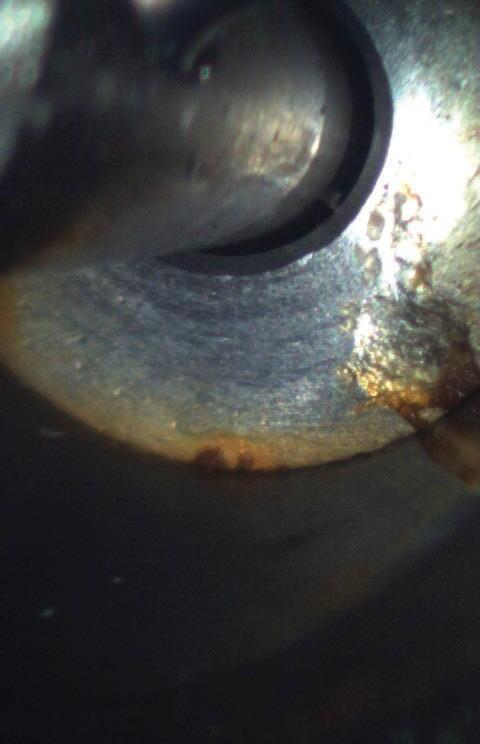


WatchDog AI will notify sta when an instrument has a condition hazardous to patient safety, thereby reducing instrument-associated infections.
WatchDog AI detects mechanical damage at an early stage which enables instruments to be removed from service while repair costs are relatively low. The Flexible Inspection Scope o ers enhanced vision and magni cation and is designed to inspect internal channels of potentially soiled or damaged items. Use of the Flexible Inspection Scope helps to meet AAMI guidelines for borescope use and inspection of instruments with internal channels.







Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.



Tri-Imaging Solutions introduces a cutting-edge platform that management, engineer performance, and system monitoring. diagnostic tools and video tutorials, and streamlines parts Designed for efficiency, the platform minimizes downtime setting a new standard for reliability in medical imaging.
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering. This helps maximize uptime and minimize repair costs
Tri-Imaging
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering. This helps maximize uptime and minimize repair costs. Solutions
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs

XperTIS o helping while ens ordering minimize
Cardiac Monitoring Jet
International X-Ray Brokers internationalxraybrokers.com • 508-559-9441
Metropolis International, LLC Metropolismedical.com • 718-371-6026
Tri-Imaging Solutions triimaging.com • 855-401-4891
Neurodiagnostics
Admar Neuro admarneuro.com
Diagnostic Solutions diagnostic-solutions.com
International X-Ray Brokers internationalxraybrokers.com • 508-559-9441
International X-Ray Brokers internationalxraybrokers.com • 508-559-9441
Biomedical pmbiomedical.com • 800-777-6474
Soma Tech Intl somatechnology.com





































MD Expo Dallas featured a powerful keynote address by Michael Hoffman and Andrew Szabo on Positively Outrageous Service (POS) principles.





A new expert article on cybersecurity and the Shifting Gears feature were added in 2021 to deliver informative and fun stories.

Everyone was a winner at MD Expo Las Vegas with educational sessions, networking events, a packed exhibit hall, glamorous showgirls and the king of rock ‘n’ roll himself!










Choose the right capital equipment, supplies, and health IT for your facility with guidance from ECRI Instituteʼs team of biomedical and cybersecurity engineers, clinicians, and human factors experts.



ECRI is a trusted authority on healthcare technologies that improve the quality and cost-effectiveness of patient care.
Get test results and ratings, free of vendor bias


Stay on top of risks with hazard and recall notifications
Compare technology with overviews and specifications
Learn more at www.ecri.org/solutions/device-evaluations or contact us today at 610-825-6000, x5891.