


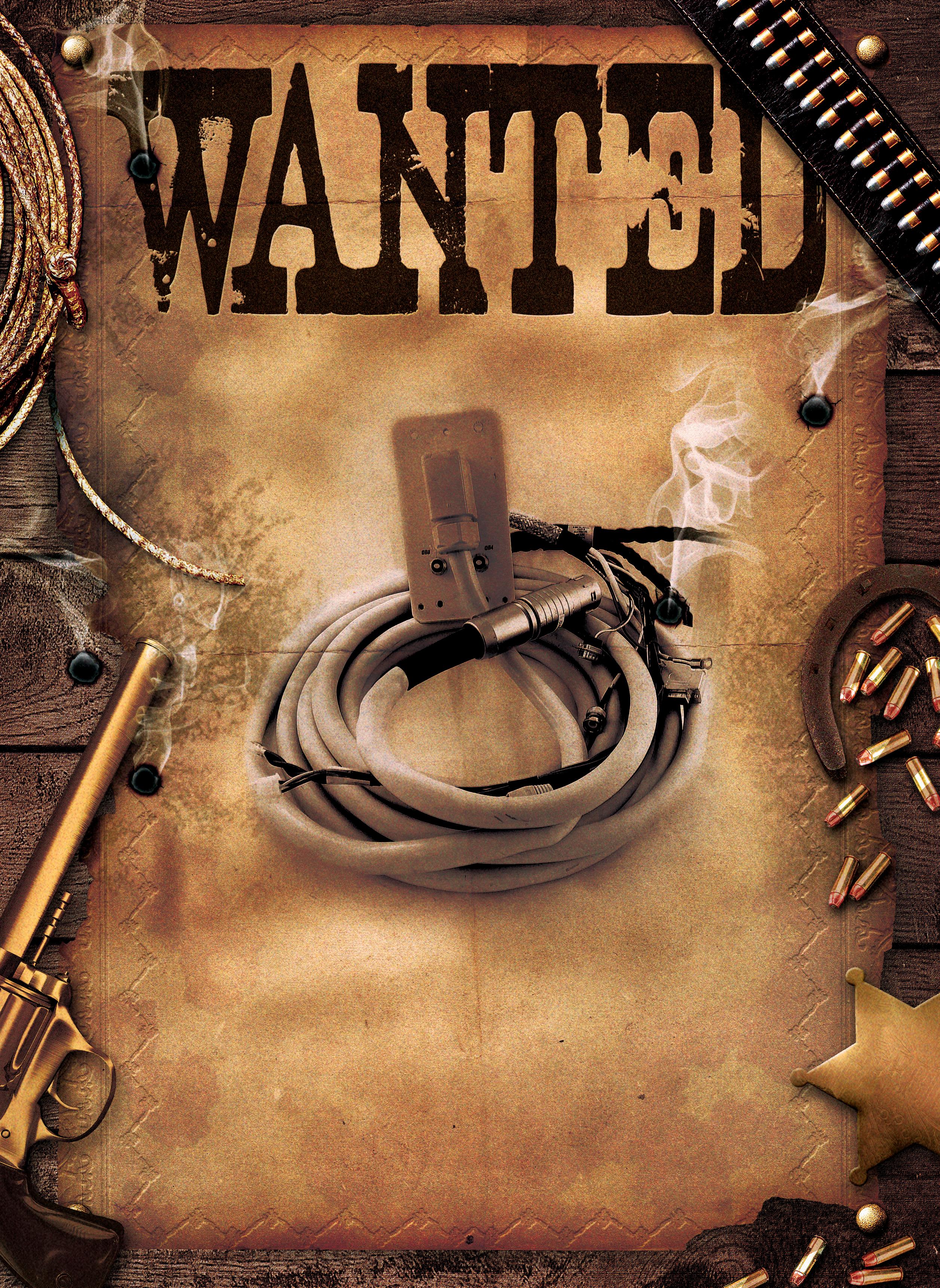













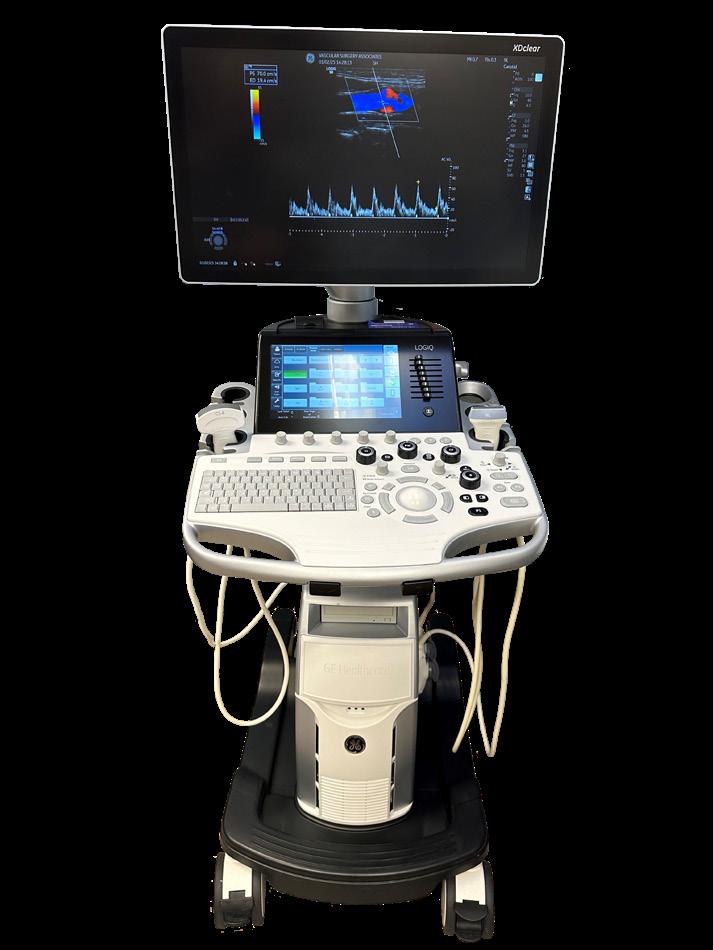
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking
XperTIS proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts ordering and order tracking.
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering. This helps maximize uptime and minimize repair costs.




Period poverty is real and something healthcare professionals should address.
Advances in women’s imaging explored amid challenges to reach every mammogram candidate.

Leah Hudkins is the clinical manager of radiology at Community Hospital of the Monterey Peninsula.


The latest news regarding new devices, studies and more.



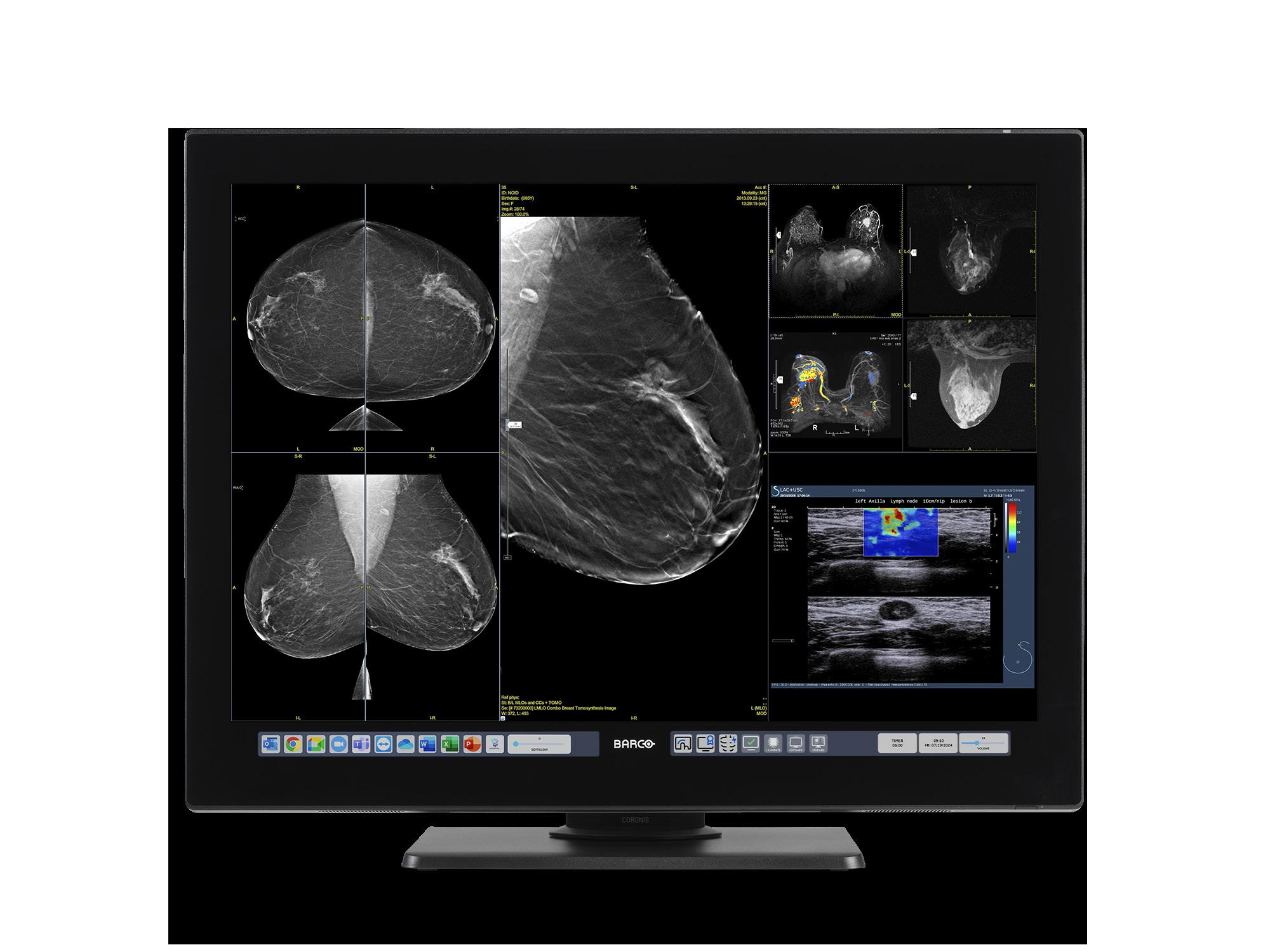
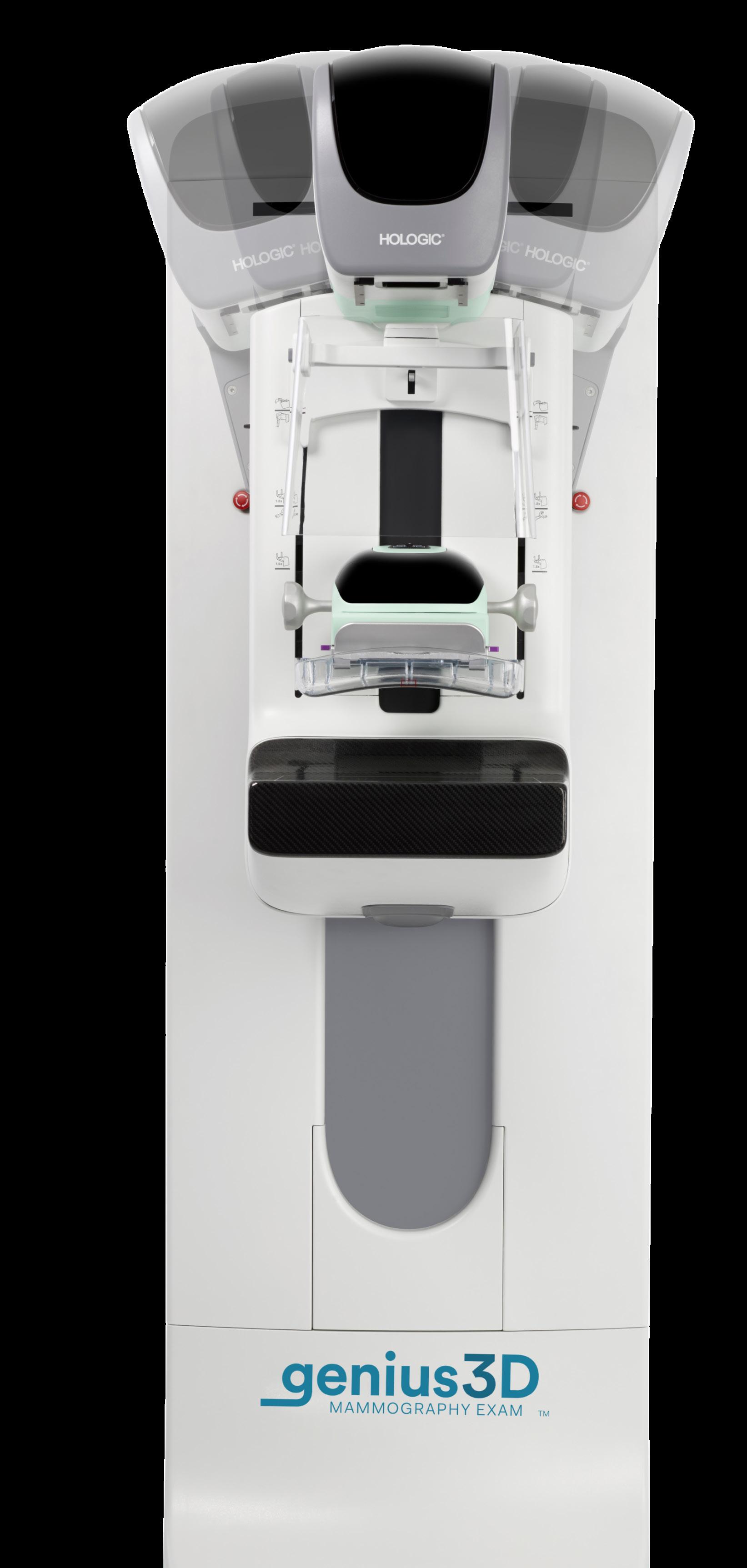
A look at women’s imaging devices.

Good leaders know they cannot force growth, but they can cultivate it.
MD
Phone:
President John M. Krieg john@mdpublishing.com
Vice
Kristin Leavoy kristin@mdpublishing.com
Vice
Jayme
jayme@mdpublishing.com
Senior
Megan
megan@mdpublishing.com
Editor
Editorial
Beth
Kimberly
Megan
Dean
Art
Karlee
Taylor
Alicia
Kristin Leavoy
Webinars
Digital
Cindy
Kennedy Krieg
Haley
Accounting
Diane





CLINICAL MANAGER OF RADIOLOGY, COMMUNITY HOSPITAL OF THE MONTEREY PENINSULA

LLeah Hudkins is an imaging professional on the rise. Her career contrinues to advance at a rapid pace.
eah Hudkins, RT(R)(MR), MRSO, continues to seek out continuing education opportunities as she reaches new heights in diagnostic imaging. Her education is impressive with an associate degree in radiography, a bachelor’s in medical imaging technology and a master’s in radiologic and imaging sciences.
Hudkins currently serves as the clinical manager of radiology at Community Hospital of the Monterey Peninsula. After a recent interview, it is obvious that she is a rising star with unmatched potential.
Q: WHERE DID YOU GROW UP?
A: I am originally from Northern Indiana, near Notre Dame. Now I call sunny Monterey, California my home!
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/ EDUCATION?
A: I graduated from Indiana University twice, once with an associate degree in radiography and then with a bachelor’s degree in MRI. I obtained my MR safety officer certification in 2020. After working in imaging for nearly a decade, I went back to school again – I can’t seem to stay away! I graduated from California State University with a master’s degree in radiology management in 2023.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: I was the first person in my family to attend college, and I
didn’t have any family working in healthcare. I knew first and foremost that I wanted to help people, and I excelled in science and physics courses. I found the imaging world to be intriguing and fast-paced –perfect for me!
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: The majority of my job satisfaction is derived from two sources. First and foremost is supporting my community, both my team and our patients. Helping people through some of life’s toughest moments is why I entered the healthcare field to begin with. Mentoring my team as they care for our patients and grow in their careers is also an incredibly rewarding experience. Secondly, my internal validation comes from challenging myself in the ever-changing landscape of imaging. It is a wonderful boon to specialize in a field where there are new technologies and skills to learn every day. I always have goals to set my sights on and push myself to achieve.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: I flourish in fast-paced, social environments. My hard-working team is a network that supports and magnifies each other’s efforts, creating far more impact in our patients’ lives than any one of us could do alone. I love that I can support these wonderful people and subsequently watch their success and growth, both in their professional and personal lives.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: What we do in imaging is critical in both diagnosis and treatment development for our patients. Our work often determines the trajectory of a patient’s care plan. The physics and skill required to obtain the best exams possible has always kept me interested. Each day brings different and exciting opportunities for us to do our best for our patients.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: As a leader in imaging, my greatest professional accomplishment is the notable increase in employee engagement along with the ability to keep up with consistent volume growth. We have low staff turnover despite multiple large-scale changes over the last two years. My unwavering commitment to clear communication and transparency, paired with adaptability, allows me to connect with my team efficiently and accurately. Our department is now set up for success at a foundational level.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: One of the first things that people learn about me is that I need to continually challenge myself, both professionally and personally. I like to look forward to my future goals, of which I have many! To start with, I plan to sit for my CRA credential, complete the final piece of my Lean Six Sigma certification, and begin my doctoral studies in healthcare strategic leadership. I will continue volunteering my time to multiple imaging membership groups, and I will also be sitting on a local leadership committee that focuses on shaping the future of Monterey County. •
FAVORITE HOBBY:
SUP (stand-up paddleboarding)
FAVORITE SHOW: “Ted Lasso”
FAVORITE FOOD: Lasagna
FAVORITE VACATION
SPOT:
Anywhere with a beach!
1 THING ON YOUR BUCKET LIST:
I would love to sail the Pacific islands.
SOMETHING YOUR COWORKERS DON’T KNOW ABOUT YOU:
I live on my boat in the nearby harbor – my backyard is full of otters and seals!

Corewell Health Director of Imaging
Services Kim Pratt gives her mom a hug. Her mom’s work as a nurse motivated Kim Pratt to pursue a career in healthcare.
Corewell Health Director of Imaging Services Kim Pratt, MHL, RT(R)(M)(CIIP), enjoys providing thoughtful and empathic healthcare to patients. It is a reason she entered the healthcare field after seeing first-hand how a caregiver can have a positive impact.
“My mother worked in the medical field before she retired. She loved her job and caring for patients, and I wanted that for myself as well,” Pratt explains.
She adds that there is another reason she decided specifically to embark on an imaging career.
“X-ray is really cool!” she exclaims.
“There are a lot of aspects that I love about my job. I love the people I work with and that I get to serve others,” Pratt adds. “I truly enjoy collaborating, supporting teams, and solving challenges together. I also like the projects we work on and tackle together.”
Pratt’s use of the word “we” is intentional. She sees herself as part of the team and that sense of “shared” responsibilities is a pillar of her approach to leadership.
“I believe leadership is dynamic, shaped by self-awareness, built on trust and driven by shared purpose. My approach is grounded in my values of collaboration, integrity, loyalty, respect and personal development which guide my decisions and shape how I show up for my team,” she says. “I lead with understanding and strive to create an environment where people feel seen, heard, and empowered to contribute their best. Leadership is not a title, but rather a responsibility to serve, support and inspire.”
Pratt attributes her growth as a leader partly to the guidance of a mentor who nudged her into learning situations.
“One example is when I expressed a desire to build confidence in my role. My mentor encouraged me to participate in a meeting that involved facilitating discussions with a diverse group of professionals. It was a challenging experience, but it pushed me out of my comfort zone and significantly boosted my confidence,” Pratt says.
“I remain eager to grow and strive to be the best version of myself. Mentors have not only shaped my perspective but also opened doors to opportunities I might not have encountered on my own,” she adds. “I’ve had the privilege of serving as a mentor in my organization’s WISH Mentorship Program, and I’ve come to appreciate that mentorship is a mutually rewarding experience. This year, I’ve also partnered with my leader to support and participate in our Imaging Mentorship Program – a group mentorship designed for leaders on our team to learn about new topics related to their development, learn from each other, and discuss relevant issues that they face as leaders in imaging.”
Pratt values mentorships and the impact they have had on her life and career.
“I have several mentors that help me grow professionally and personally. While I have participated in official mentorships, many of the mentorships I have had over the years have been unofficial and built off of relationships I have developed,” she explains. “I have worked for and with so many great people, all with various qualities I admire. I love to learn and grow and so many leaders and team members at all levels have added tremendous value to my life.”
Corewell Health Imaging Director David Buczkowski, MSA, RT (R/CT), says Pratt is a talented leader.
“Kim has been an exceptional colleague to work with. What stands out is her collaborative spirit. Corewell Health East is 2-plus hours away from Corewell Heath West and Corewell Health South, but working with Kim seems like she is right down the hall every day,” Buczkowski says. “Using MS Teams features daily for video meetings and chatting, you would never expect we are geographically separated. We strategize, collaborate, and run projects seamlessly as a fully integrated imaging service.”
He adds that her impact on women’s imaging continues to improve Corewell Health and patient care.
“Kim’s passion for women’s health has been a great example for me to witness. She collaborates at a very high level across the state of Michigan while partnering with many contributors in the woman’s health space,” he says. “Kim, as many directors do, has a balancing act of working off priorities and figuring out time management daily. Kim has done a great job owning large projects, working with informatics, and peers across Corewell Health while always putting the patient first. Kim is also a solid staff advicare and advocate for the imaging profession. Kim continues to lead by example by bringing innovative ideas to the table during any brainstorm session. She also has a very fun approach and keeps the team in good spirits.”
“I sincerely appreciate Kim as a peer and friend,” Buczkowski says.
Her leadership style works well for Corewell Health. It also works well away from work where she and her husband, Rich,
works as a team to parent “two boys that have grown into respectful and caring young men. My husband and I are very proud of the men they are.”
“I’m lucky to share my home with a wonderful family. My husband, Rich (27 years), and I are blessed to have my mom and dad living with us too – it’s a full and loving house. We have two amazing sons: Alex and Andrew. Andrew is married to Lexi, and they recently welcomed our sweet grandson, Aiden, who’s just 6 months old and already the center of attention. Alex’s girlfriend, Katlynn, is also a special part of our lives.”
The Pratt family’s future appears bright.
Pratt says she expects diagnostic imaging’s future to continue to shift and adapt to new technologies.
“Imaging, like healthcare, is ever-changing, but with the digital world expanding and improving, the digital patient experience is making healthcare more accessible. Artificial intelligence is advancing rapidly, reshaping the way we detect, diagnose and deliver care,” Pratt says.
In closing, Pratt shares the mission statement she created for herself. It is a statement that she often revisits and “to this day it still holds true.”
“Honor God in everything while growing spiritually, professionally, and personally. Impact others through service and education,” Pratt’s mission statement reads. “Honor. Grow. Impact.” •
1. What is the last book you read? “Ask for Andrea” by Noelle Ihli
2. Favorite movie? “Man on Fire” with Denzel Washington
3. What is something most of your coworkers don’t know about you? I played softball for a community college for one semester before going to X-ray school.
4. What is one thing you do every morning to start your day? Thank God for another day! And I love to have a morning cup of coffee.
5. Best advice you ever received? Let your values be your guiding compass. This holds true to personal, professional and organizational values.
6. Who has had the biggest influence on your life? My parents. They have raised me to honor God in all I do, respect others, work hard, and be on time! My dad would always say if you are on time, you are late!
7. What would your superpower be? Teleporting! I have given this a lot of thought throughout my travels. I do not love traffic, and the ability to teleport would open all new possibilities.
8. What are your hobbies? Listening to audio books, puzzles, bowling. I love movies and crime shows. Hanging out by the water while my husband fishes. I also plan to make playing with my grandson a hobby.
9. What is your perfect meal? I love a good steak! Mostly I love my husband’s cooking, so restaurants have their work cut out for them to impress me.

Wh en Omar W. Jarrah launched FDM Enterprises, he wasn’t looking to reinvent the wheel. He just wanted to make sure the wheel – whether it belonged to an MRI, CT scanner, or injector – was turning smoothly. After 25 years in the medical imaging trenches and a career that started in the U.S. Army, Omar knew there was room to improve how service and support were delivered in the imaging space.
“I’ve spent decades watching big companies forget the little things,” he says. “And in this industry, those ‘little things’ are usually what keep patients waiting, hospitals frustrated, and engineers running around in circles.”
That frustration inspired him to start FDM Enterprises – a company dedicated to offering preventive maintenance, troubleshooting, and repair support with the kind of persistence, preparation, and precision you’d expect from someone with military roots. ICE Magazine recently found out more about FDM Enterprises including what to expect in the future.
Q: CAN YOU TELL US A LITTLE ABOUT YOUR COMPANY?
Jarrah: As a veteran with 25 years’ experience, I started FDM Enterprises to support others in the industry with their MRI, CT and injector service needs. Offering PMs and service support to peers and clients with highly competitive rates. We have been expanding into titanium tools and are looking to offer other services.
Q: HOW DOES YOUR COMPANY STAND OUT IN THE IMAGING SPACE?
Jarrah: It comes down to one principle: support –
done better, faster, and without the inflated price tag. While many service providers focus on locking in giant contracts and dazzling sales metrics, FDM Enterprises puts its energy into what matters most: customer satisfaction and reduced downtime. Hospitals and imaging centers are often surprised to learn that with FDM, they can get their MRI, CT, and injectors serviced in a single service event – a rarity that minimizes disruptions to patient care. We’ve all seen the chaos when three different vendors are needed for three different systems. Why not fix it all at once and let the clinicians get back to doing what they do best?
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY?
Jarrah: In the next five to 10 years, I see FDM Enterprises not just as a service provider, but as a driver of competition and quality improvement in the imaging service industry. My long-term goal is to raise the bar by proving that proactive, customer-focused service doesn’t have to come at premium rates. And at the heart of it all is a very simple philosophy: solve problems, fix things, and make life easier for both peers in the industry and the patients relying on those machines. Honestly, the best part of this job is knowing that when I fix something, I’ve played even the smallest part in helping a patient get the care they need. That’s the kind of satisfaction you can’t put a price on.
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE ICE MAGAZINE READERS TO KNOW?
Jarrah: Please reach out and connect. Who knows how we may be able to help each other to improve patient care. •
For more information, visit fdmenterprises.com.






BY MATT SKOUFALOS
When Dr. Refky Nicola isn’t in the classroom or the imaging department, you might find him in the recording studio, preparing for a podcast.
In addition to working as an associate professor of radiology at SUNY Upstate Medical University in Syracuse, and as chief of radiology services at Community General Hospital of Greater Syracuse, Nicola has spent the past three years working as an assistant editor of the Radiology Journal and RadioGraphics podcasts.
Produced by the Radiologic Society of North America (RSNA) as a learning component of its publications of the same names, the podcasts have become another way for Nicola, who also works as a peer reviewer for both journals, to expand his learning and professional development.
“I’ve always had an interest in podcasts in general, [and] as a way to get through my commute,” he said. “Right before [the novel coronavirus] COVID-19 pandemic, the Radiology Journal was looking for podcasters.”
“The society has seen a need for podcasts, and that space continued to grow, and I think as it grew, it became an integral part of the journal,” Nicola said. “I think having the team that we have, all of us [having] very different interests and backgrounds in radiology helped it take off.”
The Radiology Journal podcast hits about 8,000
downloads per month, and the RadioGraphics podcast about 4,000, Nicola said. Their objectives vary slightly: the RadioGraphics podcast is intended for an education audience, and covers topics that are important to imaging trainees and medical students, while the Radiology Journal podcast focuses on cutting-edge research within the radiology field.
Its format begins with Nicola and his fellow podcast editors examining a published article from either of the journals in question, connecting with its authors, and working to elevate their findings into a conversation that’s digestible for the podcast audience in an interview style.
“I ask questions about the things in the article,” he said. “I hit the ground running. I like gathering information and talking to people, putting things together, [and] creating a story for people. My objective would be to try to let [the podcast audience] understand what’s in the article from the author’s perspective.”
After recording their interviews, production editors clean up the audio, master it, and release the episode. In that environment, Nicola sees his role as helping to create bridges between peer-reviewed academic material and the more casual listening environment of a podcast. In addition to reaching an audience that can benefit from understanding the journal content in that different format, he said that it also helps elevate the profile of the research itself.
“Studies have shown that articles that have associated episodes get more downloads, and have higher metric scores; it does have a ripple effect


with having an article associated with a podcast,” Nicola said.
“I think people want a dialogue regarding the article, and I think people want somebody to tell them the important parts,” he continued. “You might not read the article, but if you listen to it you might want to read it, [and] if you give people a chance, they’ll tell their side of the story in terms of the message they’re trying to convey.”
Beyond improving the connection among the audience, the researcher, and their work, Nicola said that podcasting has made him a better listener, and deepened his appreciation for the work that his colleagues in the field put into their research.
“When people write these articles, they put a tremendous amount of time and effort into their development,” he said. “It’s only fair to allow them to educate the public or the radiologists about what their message is. That’s what I try to do. I see myself as an intermediary between the article and the audience.”
As well as bringing his audience closer to the material of the RSNA publications, Nicola said that his podcasting experience has afforded him the chance to interview “reputable, respected people within the society of RSNA,” while connecting with peers with which he typically hasn’t had the opportunity to interact.
“That’s been one of the most memorable moments for me,” he said. “I got to speak to some leaders in the field, and just getting their perspective on radiology,
their career, their lives, is really fascinating. I’ve really enjoyed that.”
“I learn from these people every day,” Nicola said. “It’s nice.”
When he’s not at work, or pursuing his other interests, Nicola likes to exercise, particularly running and biking. He also enjoys traveling – he’s toured parts of Europe, including Portugal, Greece, and Sweden –and spending time with his wife and children.
“Being outdoors and traveling to a new place and a new country is something that I really look forward to all the time,” Nicola said. “If I can travel, I like to do it.”
In addition to growing the podcasts he helps to produce, Nicola said he’s interested in having more in-depth conversations with the radiology community. Whether that takes the form of multi-episode stories or other innovative formats, he’s happy to engage with his peers, his production team, and the listening audience to help make radiology topics more accessible and available.
“We still have a lot of things to do,” Nicola said. “As a team, we’re very progressive, innovative, energetic. We as a group work very hard, and we always appreciate people listening and giving their feedback. It’s nice to know that people are actually listening because we all put a lot of work into it.”
The RadioGraphics podcast can be found online at rsnaradiographics.libsyn.com/
The Radiology Journal podcast can be found at rsnaradiology.libsyn.com/ •

KyphoLift, a breakthrough in diagnostic imaging support systems, exhibited at the ISMRM & ISMRT Annual Meeting & Exhibition earlier this year. KyphoLift Founder Brandon Johnson also recently attended the AHRA Annual Meeting in Las Vegas.
ISMRT attendees received a live, hands-on demonstration of the KyphoLift and KyphoWedge, designed to revolutionize patient positioning in diagnostic imaging.
Accurate imaging starts with proper positioning – but for patients with kyphosis, obesity, or limited mobility, standard positioning practices often fail. Manual lifting, unstable pillow stacks, and frequent repositioning compromise safety and image quality. KyphoLift offers a new standard of care: empowering technologists to safely and efficiently position patients without the need for additional staff, even during low-coverage shifts.
“Imaging accuracy shouldn’t be dependent on how many hands are available,” said Johnson. “We created KyphoLift to solve the real, daily challenges radiology teams face – enhancing safety, improving comfort, and enabling more diagnostic scans with less hassle.”
KyphoLift features include:
• Enables safe, solo positioning of patients
• Reduces injury risk for technologists and patients
• Increases patient comfort and stability
• Improves image quality for better diagnostic confidence
• Boosts scan throughput and clinic efficiency With increasing patient volume and a global technologist shortage, KyphoLift is uniquely positioned to streamline radiology workflows and improve outcomes.
Calidar Inc. has announced the successful imaging of the first patient with its 4D mammography system, according to a press release.
The imaging system harnesses X-ray diffraction and AI to measure novel molecular-level signals of disease, offering the potential to significantly improve diagnostic accuracy. This procedure was the first known in-human measurement of X-ray diffraction spectra and represents a major advancement in the field of medical imaging, the release states.
Despite decades of innovation in medical imaging, breast cancer and other soft tissue diseases remain difficult to detect noninvasively with sufficient precision. In the United States alone, approximately 1.5 million breast biopsies are performed each year, with up to 80% of those (1.2 million) ultimately diagnosed as benign. These unnecessary procedures contribute to over $6 billion in annual healthcare spending, a cost borne by both patients and payers. Meanwhile, delayed diagnoses because of inconclusive imaging result in an estimated 50,000 breast cancer patients annually whose treatment is postponed, increasing treatment costs and decreasing survival rates. For clinicians, unnecessary biopsies add strain to understaffed hospitals, with radiologist workloads nearly doubling and pathologist case volumes increasing by over 40% in the past decade.
The press release states that this first-of-its-kind 4D mammography system, designed by the Calidar team of Stefan Stryker, Josh Carpenter, and Mitchell Greene, addresses these limitations by measuring how X-rays scatter at the molecular level – a process known as X-ray diffraction. This produces a unique structural signature that reflects the internal composition of breast tissue. Unlike traditional X-ray images, which rely on shape and density, X-ray diffraction imaging reveals a new dimension of diagnostic data: what the tissue is made of, not just what it looks like. In prior ex vivo studies of breast tissue, these tissue-specific fingerprints enabled classification of cancerous and benign samples with four times the precision of conventional imaging techniques.
The first-in-human study will assess how well the 4D mammography system can distinguish between healthy tissue and breast cancer in patients and compare performance to existing mammogram devices. The study is being conducted in collaboration with Baptist Health Hardin in Elizabethtown, KY, led by Principal Investigator Craig Kamen, MD.
The current study focuses on the use of the 4D mammography system in a diagnostic application, where patients already present with findings that require further evaluation. Future studies are planned to expand its use into breast cancer screening, with the goal of enabling earlier detection and improving outcomes for even more patients.
The 4D mammography system is investigational and has not been cleared or approved by the U.S. Food and Drug Administration. It is not available for commercial sale and is limited to investigational use in the United States under FDA’s abbreviated IDE requirements.
AdvaMed, the Medtech Association, is among 67 stakeholder groups, including patient advocacy groups and state medtech and life sciences associations, urging the Centers for Medicare and Medicaid Services (CMS) to create a timely, streamlined pathway for Medicare patients to access FDA-authorized breakthrough medical technology.
In a letter to CMS Administrator Dr. Mehmet Oz, the 67 organizations noted medtech enables remarkable patient outcomes, yet FDA-designated, authorized breakthrough medtech faces years of delays in Medicare coverage.
“Despite this remarkable impact and the continuous pace of innovation, Medicare patients face a significant and unacceptable barrier to accessing innovative medical technology,” the letter states. “A recent study alarmingly revealed that for technologies requiring a new reimbursement pathway, nearly six years passed between FDA market authorization and Medicare coverage. Patients should not be forced to wait the better part of a decade for access to safe and effective medical technology that holds the potential to meaningfully improve their health and life.”
A streamlined, predictable Medicare coverage pathway for medtech the FDA has deemed useful, safe, and effective would “demonstrate CMS’ commitment to patientcentered care and ensure that Medicare beneficiaries can







benefit from the rapid advancements in medtech without unnecessary delays, helping make for a stronger, healthier country,” the letter continues.
“FDA is the global gold standard with its rigorous medtech safety and efficacy standards,” said Scott Whitaker, AdvaMed president and CEO. “When FDA has identified a medtech solution as a ‘breakthrough’ and cleared it as safe and effective for patients, we believe Medicare should cover it. As this Administration and AdvaMed work toward our mutual goal of making Americans healthy again, I want to thank Dr. Oz and Commissioner Makary for their commitment to improving Medicare beneficiaries’ access to the breakthrough medtech that could improve their health and even save their lives.”
The effort to achieve breakthrough coverage is gaining momentum. In a recent interview, FDA Commissioner Marty Makary said he and CMS Administrator Dr. Oz were working on automatic coverage of FDA-authorized breakthrough medtech to avoid a “repeat, duplicative approval process.”
U.S. senators have introduced the bipartisan Ensuring Patient Access to Critical Breakthrough Products Act to accelerate Medicare coverage.










































































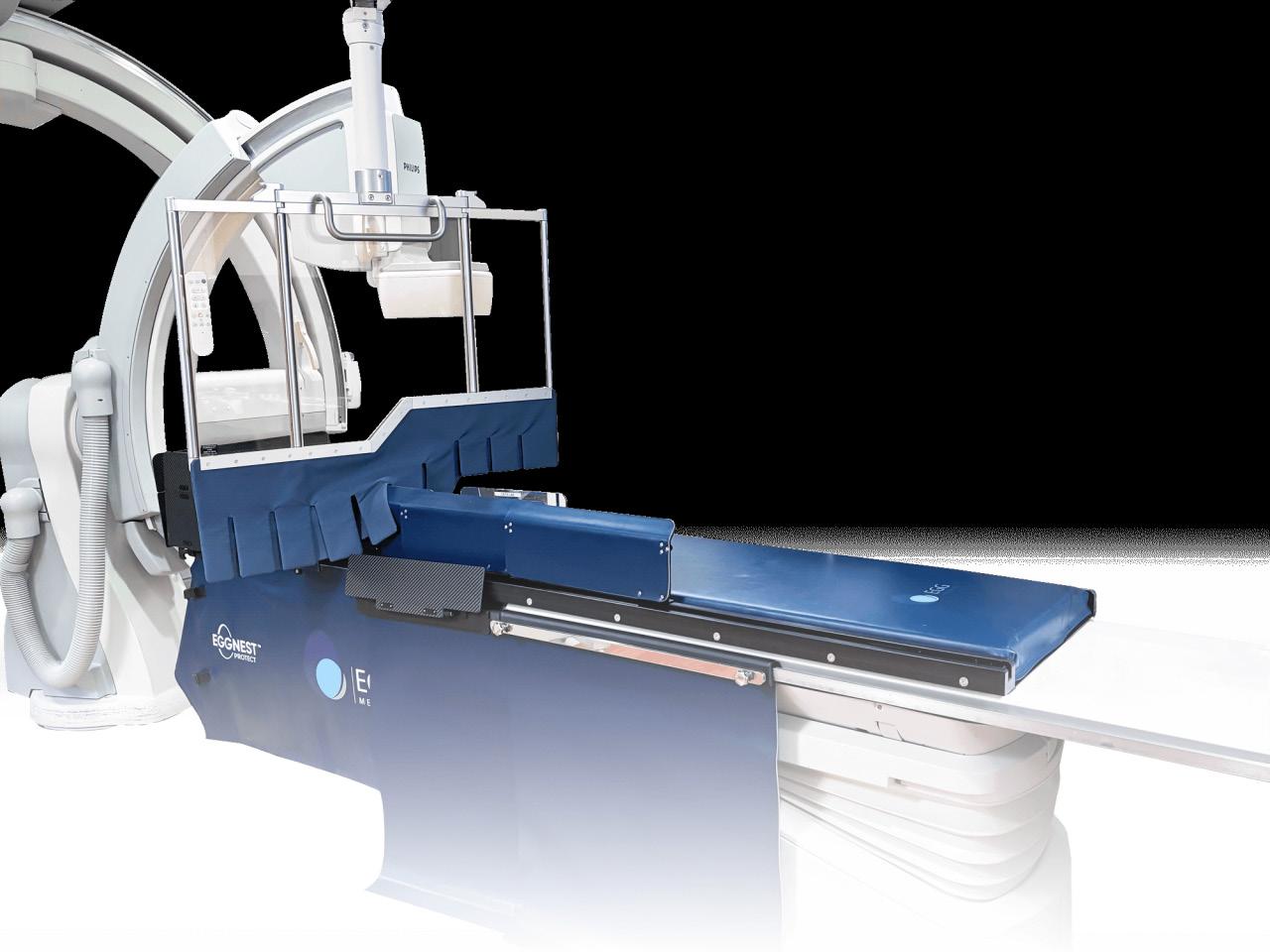
A recent study published in the Journal of the Society for Cardiovascular Angiography & Interventions (JSCAI) highlights the effectiveness of the EggNest Complete radiation shielding system, demonstrating its ability to protect all personnel in the catheterization lab from scatter radiation, according to a press release. The findings show that while other next-generation systems offer protection for the primary operator and assistant, the EggNest Complete system provides significant protection for the entire interventional team.
The study, titled “Comparative Effectiveness of 2 NextGeneration Scatter Radiation Shielding Systems,” compared the EggNest Complete system with the Rampart IC system and a no-shielding condition using an anthropomorphic phantom. The results showed that both the EggNest Complete and Rampart IC systems significantly reduced radiation exposure for the operator and assistant positions compared to no shielding. However, the EggNest Complete system provided additional significant protection for staff at the head of the bed and the nursing positions, a benefit not observed with the Rampart IC system.
“From the beginning, Egg Medical has had three guiding principles: we need to protect the entire team from scatter radiation, we can’t interfere with workflow or patient access, and the reduction in radiation exposure must be nearly complete. The study by Riley et al shows very clearly that the EggNest Complete system dramatically reduces radiation exposure for everyone in the room, and that the operator and assistant are almost completely protected. That is a marked improvement to safety for everyone who works in X-ray guided procedures,” said Dr. Robert Wilson, CEO of Egg Medical.
The study’s authors note that interventional cardiology procedures expose healthcare professionals to prolonged ionizing radiation, which poses significant health risks including heightened rates of malignancy, cataracts and orthopedic injuries. Traditional lead aprons, while offering some protection, are heavy (up to 25 pounds) and can lead to musculoskeletal injuries. A recent SCAI survey found that 66% of operators reported musculoskeletal pain attributed to their time in the cardiac catheterization laboratory.
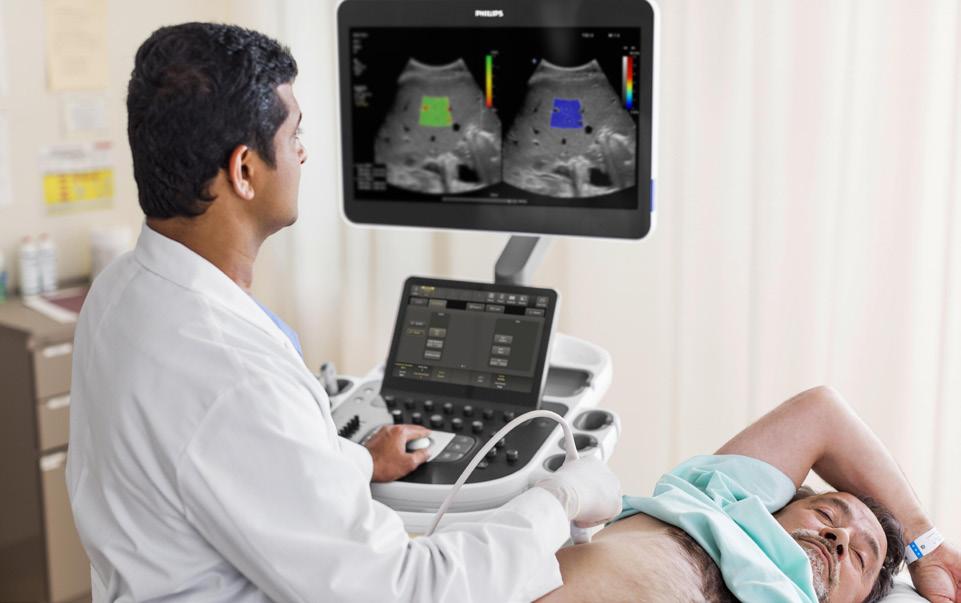
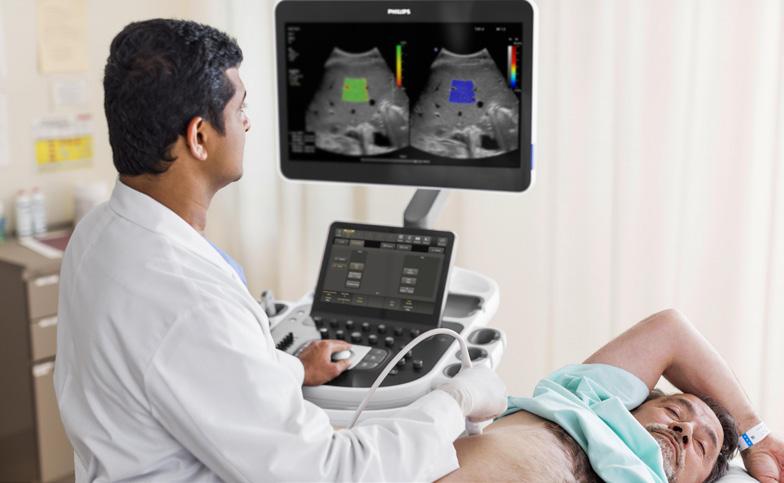
Philips, a global leader in health technology, has announced a plan for new investments of more than $150 million in U.S. manufacturing and research and development (R&D). As part of the announcement, Philips unveiled the expansion of its Reedsville, PA, manufacturing facility, which produces AIenabled ultrasound systems for hospitals across the U.S.
These investments come on top of Philips’ annual $900 million R&D investment in the U.S. as well as investments in nearly 17,000 colleagues across 40 facilities in the United States. Philips has employees in every U.S. state supporting innovations used by clinicians and patients in 90% of hospitals across the country.
The investment includes the expansion of its Reedsville, PA, site and the recently announced expansion of Philips’ Image Guided Therapy facility in Plymouth, MN. It also includes additional manufacturing and R&D projects which will come over the next several years to support the company’s growth in the U.S.
The Reedsville site, which currently manufactures transducers, will also customize the software and configurations of ultrasound systems for specific clinical procedures in cardiovascular, general and maternal care following the expansion. As an example, Philips’ CV ultrasound platform delivers advanced tools to help doctors diagnose structural heart and coronary artery disease quickly and confidently.
“The proposed planned expansion of our manufacturing
facilities is a demonstration of our deep commitment to the U.S. region,” said Jeff DiLullo, Chief Region Leader, Philips North America. “Each year, Philips spends $900 million in R&D in the U.S. to drive innovation and deliver cuttingedge technology that empowers healthcare professionals to diagnose, treat and monitor patients more effectively. Increasing our manufacturing and R&D capabilities will create jobs and accelerate our ability to deliver better care for more people with innovative AI-enabled solutions.”
The expansion of the Reedsville site is expected to add 24,000 square feet of manufacturing space in addition to 40,000 square feet of warehouse space and is expected to create 120 skilled manufacturing jobs. The recently announced expansion of Philips’ image-guided therapy facility in Plymouth, MN, which includes the construction of a new medtech training center, is expected to create over 150 new jobs.
DeepHealth Inc., a wholly owned subsidiary of RadNet Inc. and a leader in AI-powered health informatics, has received FDA 510(k) clearance for TechLive – a remote scanning solution enabling centralized operation and supervision of MR, CT, PET/CT, and ultrasound procedures. TechLive empowers technologists to scan for multiple locations, enables improved operational efficiency, extends center operating hours, and enhances access to complex procedures. More than 300 of RadNet’s MR, CT, PET/CT, and ultrasound systems are now connected with DeepHealth’s TechLive solution, resulting in increased patient throughput and improved quality through remotely matching expert staff with complex modalities in real-time.
Over the past decade, radiology workloads have steadily increased, while the number of qualified technologists has not grown proportionally. In a pilot deployment at 64 locations inside of RadNet’s New York area facilities, TechLive significantly contributed to a 42% decrease in MRI room closure hours during the second
quarter of 2025 as compared with the same period in 2024, allowing more patients to receive timely scans.
Additionally, as a result of the remote expert involvement during the same pilot deployment, TechLive contributed to an increase in complex procedures. Furthermore, in extending remote scanning capabilities to ultrasound, TechLive is enabling experienced senior sonographers and physicians to remotely guide technologists on-site through complex cases in a modality that is heavily dependent upon real-time, operator expertise.
“TechLive represents a paradigm shift in how we approach imaging operations,” said Sham Sokka, Ph.D., chief operating and technology officer at DeepHealth.
“By enabling real-time remote expertise, we are not only addressing today’s staffing challenges, we are creating a foundation for more efficient, financially sustainable, and high-quality patient care across the broadest set of imaging modalities. This FDA clearance validates DeepHealth’s vision of a connected imaging ecosystem that scales human expertise beyond physical boundaries.”
West Physics has launched its Survey Meter Calibration Service, designed to help hospitals, imaging centers, and industrial facilities ensure accurate radiation measurements, regulatory compliance, and operational readiness with minimal disruption.
Survey meters are critical tools in maintaining a safe environment for patients and staff, yet many facilities face challenges with inconsistent calibration practices, long turnaround times, and disorganized documentation, leading to compliance gaps and operational inefficiencies.
“Our clients have consistently shared concerns about unreliable calibration processes, slow turnaround times and the risks these pose to their teams and patients,” said Dr. Geoffrey West, president and chief executive officer at West Physics. “We developed this service to address these pain points directly, providing a dependable, expert-led calibration program that facilities can trust.”
Key Features of the Service:
• Fast, Predictable Turnaround: Minimizes downtime with efficient mail-in calibration service.
• Proactive Scheduling: Ensures timely calibration sequencing to help you stay on schedule and avoid any

lapses in compliance.
• Shipment Tracking: Stay informed every step of the way with our state-of-the-art proprietary tracking system.
• Free Efficiency & Conversion Chart in Every Report: Easily, quickly and accurately convert cpm to dpm.
This service is delivered by West Physics’ team of experienced medical and health physicists, ensuring that calibration is performed with a deep understanding of the regulatory requirements and operational challenges unique to healthcare and industrial environments.
“As regulatory expectations increase, facilities need a reliable partner who not only calibrates meters but also helps maintain a robust safety culture with fast and efficient turnaround times,” added West. “This launch is part of our commitment to supporting clients with comprehensive, high-quality solutions that protect patients, staff and reputations.”
The West Physics Survey Meter Calibration Service is currently available as an add-on service for all existing West Physics medical and health physics customers. Wider availability as a stand-alone service to be announced at a later date.
Image One Medical is the only Engineer-Owned medical equipment service group that is fully dedicated to Florida’s amazing base of Imaging Centers, Hospitals, and Cancer Treatment Centers. We have a mission: Self perform on every aspect of our business. Specialize on specific modalities: Pet CT, CT & MRI, and Focus in a key geographic region.
Fort Myers I Fort Lauderdale I Tampa I Orlando
FLORIDA BASED
Dealer and servicer of PET CT, CT and nuclear medicine
• Equipment service: full coverage plans
• Equipment sales: installation, relocation and project management
• Mobile coach construction, refurbishment, maintenance and management

• Self performing team of in-house engineers • High level problem solving for Siemens and GE PET CT, CT and nuclear medicine
• In-house inventory of 40+ systems and parts for repair
• 24 hour service with quick uptime guarantee


Frost & Sullivan has announced that Siemens Healthineers was awarded the 2025 North America Company of the Year Recognition in the advanced visualization applications industry for its outstanding achievements in diagnostic innovation, seamless platform integration, and customer impact.
This recognition underscores Siemens Healthineers’ market leadership in transforming medical imaging with intelligent automation, scalable technology and end-to-end workflow solutions. Frost & Sullivan evaluates companies through a rigorous benchmarking process across two core dimensions: visionary innovation and customer impact. Siemens Healthineers excelled in both, demonstrating a compelling ability to align long-term product development with the evolving demands of healthcare systems while executing consistently across complex, high-stakes clinical environments.
“By continuously translating real-world insights into high-performing solutions, Siemens Healthineers maintains its reputation as a preferred partner across global health systems,” said Anantharaman Viswanathan, research director at Frost & Sullivan.
Guided by a focused growth strategy centered on organic development, digital innovation and deep customer partnerships, Siemens Healthineers shapes the future of advanced visualization (AV) by delivering scalable, integrated platforms that enhance diagnostic confidence and operational agility. The company’s sustained investment in
intelligent imaging software and adaptive workflow integration has enabled it to lead in a sector increasingly defined by complexity, interoperability, and performance at scale.
At the core of Siemens Healthineers’ AV leadership is its syngo.via platform, which powers disease-specific, multi-modality applications for specialties such as radiology, oncology, neurology, and cardiology. Seamlessly integrated with the company’s enterprise imaging backbone, Syngo Carbon, syngo.via offers 3D and 4D visualization, AI-enabled segmentation, and robust quantitative analysis – all designed to empower clinicians to make fast and accurate decisions across the care continuum. The interoperability and modularity of this ecosystem distinguish it from fragmented solutions, allowing healthcare providers to standardize diagnostics, streamline data continuity, and reduce variability in interpretation.
Innovation extends beyond clinical tools to include Siemens Healthineers’ delivery model. Unlike competitors that rely on external acquisitions, the company offers a fully homegrown ecosystem, engineered for consistency, security, and adaptability. Shared digital workspaces enable multi-site collaboration, ensuring that radiologists, referring physicians, and entire care teams can access and interpret imaging results regardless of location. These collaborative capabilities are further supported by structured reporting tools and embedded clinical decision support, which help unify diagnostic standards and promote evidencebased practice.
FUJIFILM Healthcare Americas Corporation, a leading provider of diagnostic and enterprise imaging solutions, today announced the U.S. launch of the FDR Go iQ, an innovative portable digital radiography (DR) solution built for hospitals and ambulatory surgery centers. Equipped with intuitive touchscreen controls and a display at the tube head, as well as convenient built-in smart charging, technologists can acquire x-ray room image quality at the patient bedside.
“This new portable digital radiography system represents a major step forward in imaging mobility, performance, and user experience,” said Rob Fabrizio, director of strategic marketing, medical imaging systems, FUJIFILM Healthcare Americas Corporation.
FDR Go iQ features include:
• A built-in 3D camera with advanced positioning guidance and ability to upgrade to future AI technologies
• Intelligent smart charging automated in bin connection keeps the detector powered for extended use
• A touchscreen tube head display and controls, provide advanced positioning and tube alignment guidance, motion detection and exam parameters easily within reach
• An extra-large 19-inch display for confident image verification at the bedside
• A slim and lightweight design at just 22.5 inches wide and
970 pounds for optimized mobility in tight spaces
• Mark-free polyurethane wheels and 360-degree swivel casters for smooth travel and turning
• Dedicated storage with a detector lock
• Convenient detector holding slots at the top of the main body to hold the DR detector securely during bagging and wipe down
• Wipes and gloves storage to support fast access and infection controls
The system features innovative technologies to optimize image quality, workflow and patient safety. The FDR Go IQ coupled with FDR D-EVO III ultra-lightweight glass-free detectors feature Fujifilm’s exclusive Hydro AG antibacterial coating and patented Irradiated Side Sampling (ISS) for higher-resolution and improved dose efficiency compared to conventional circuitry designs. by acquiring its data on the patient side of the circuitry, ISS increases sharpness and Detective Quantum Efficiency (DQE) and reduces scatter and blur at ultra-low doses. Additionally, the system’s onboard technologist console features Fujifilm’s proprietary Dynamic Visualization™ II intelligent feature recognition processing which automatically adapts to anatomic characteristics and hardware to produce exceptional images with higher detail and contrast levels throughout.


GE HealthCare has announced commercial availability of an advanced floor-mounted digital X-ray system, Definium Pace Select ET, designed to deliver high-image quality and optimize efficiency in highly demanding environments while enhancing access and affordability.
X-ray exams often serve as the entry point to diagnostic imaging, accounting for 60% of all imaging studies conducted, resulting in an ever-increasing workload for radiologists and technologists. This increased demand, combined with acute staffing challenges where 80% of healthcare organizations are short-staffed and radiology technologists have the highest vacancies, high burnout levels and work-related injuries, creates critical barriers to providing timely, effective diagnostic imaging for patients in need of X-ray imaging.
GE HealthCare’s new Definium Pace Select ET solves for many of these challenges by automating manual, repetitive steps and helping to reduce physical strain. The system leverages AI to ensure accurate patient positioning and consistent image quality across various clinical conditions while streamlining the technologist workflow to maximize the patient experience and throughput.
“Burdened with the stress and pressure to keep radiology departments running smoothly and profitably, we aim to empower technologists with a system that consistently makes the first image count,” said Sharad Sharma, Global
General Manager, X-ray, at GE HealthCare. “With its advanced digital capabilities and automation, Definium Pace Select ET allows technologists of all experience levels to deliver consistent high-quality images to serve the full range of anatomies and patient populations.”
Building on the trusted Definium platform from GE HealthCare, the Definium Pace Select ET system brings advanced automation and workflow features to a flexible, floor-mounted system with elevating table, in-room exam control, and common user interface to assist technologists.
“This launch reinforces our commitment to provide accessible, efficient, and high-quality care for patients, while alleviating stress from the technologist’s workday by minimizing repetitive tasks and automating steps,” said Jyoti Gupta, Ph.D., President & CEO of Women’s Health and X-ray at GE HealthCare. “We remain dedicated to advancing our technology through transformative digital and AIenabled capabilities that will remove barriers to timely and effective diagnostic imaging for any patient in need of X-ray imaging.”
The Definium Pace Select ET system brings the same high image quality typically seen in more expensive overhead tube suspension (OTS) systems to the affordability focused floor-mounted market. Designed and developed with extensive customer feedback, the system brings:

• Advanced automation to reduce workflow steps and physically demanding movements for technologists, potentially minimizing work-related injuries.
• Image variability reduction through the AI-enabled Helix Advanced Image Processing to provide consistent highquality images.
• Prevention of errors before they occur through automated positioning, protocol selection, patient size (body habitus), and collimation via the Intelligent Workflow Suite, and a quality check prior to radiation exposure. •




Since 1985, Radiological Service Training Institute (RSTI) has built a reputation grounded in consistency, integrity, and a deep commitment to the people it serves.
Now marking its 40th year, RSTI’s story is one of people: those who built it, those who teach within its walls, and the thousands of imaging professionals who have carried that training into real-world practice across the country and the world.
Originally founded by three visionaries – Terry Speth Sr., Larry Cornell Sr., and John Perez – RSTI was created as an independent training center serving the needs of the entire industry, from OEMs to in-house hospital teams to ISOs. Their multivendor approach was groundbreaking, offering state-of-the-art equipment, expert technical instruction, and hands-on learning that builds confidence and careers – a philosophy that remains core today.
A YEAR OF GROWTH AND GRATITUDE
The milestone year of 2025 brought transition, recognition and evolution. Two long-serving team members, Vicki Smith and Donna Hastings, recently retired, concluding remarkable careers that shaped RSTI’s operations, culture and community. Their legacy reinforces a core belief: “It’s our people that make the difference.”
That belief also extends to the exceptional instructors, whose expertise and dedication continue to set RSTI apart. These professionals don’t just teach system repair, they shape engineers prepared to solve problems, think critically, and uphold the highest standards in the field. The focus isn’t on shortcuts. It’s on building careers that last.
In 2025, RSTI earned two TechNation Tech Choice Awards – Outstanding Vendor of the Year and Influencer of the Year – honors voted on by the HTM community it supports.
While rooted in its original mission, RSTI continues to adapt for today’s field service professionals. Recent developments include an updated “Servicing the Philips DXR Family” course and upgrades to the GE IGS/Innova Cath Lab and Philips Ingenuity/Brilliance CT platforms. A new “GE Signa, Optima, & Discovery MRI Family” course will launch soon, supported by the installation of a new GE MRI system on-site.
As a proud DoD SkillBridge and GI Bill approved provider, RSTI offers qualified, transitioning military members, family members and veterans hands-on training that often leads directly to careers in hospitals and healthcare organizations nationwide. With a minimum commitment of two weeks, many complete hands-on training to begin a rewarding career within hospitals and healthcare service organizations nationwide.
To our leadership, training and parts team, alumni, instructors, retired leaders, and HTM community – thank you for being a part of the RSTI legacy. Whether you’re entering the field or refining your expertise, we are honored to be part of your journey. •


1.REGISTER
Register to view the webinars each month
2.WATCH
Watch recorded webinars on-demand
3.EARN
ARRT Category A CE credits pending approval

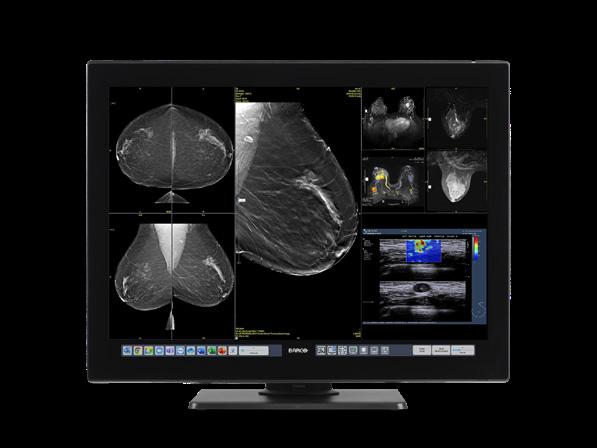
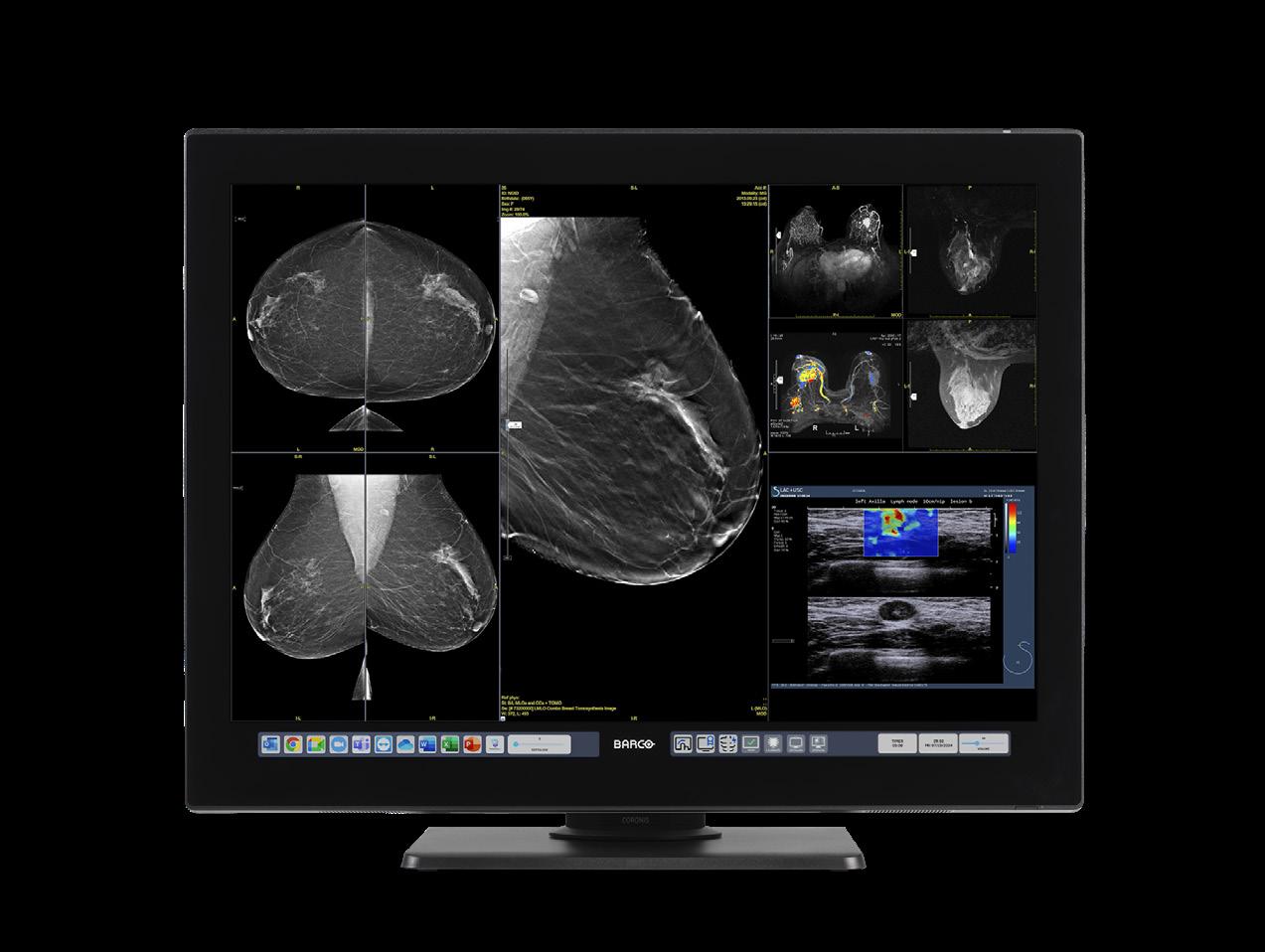
Wo men’s imaging is one of the most dynamic and evolving areas in healthcare, with advances in technology, patientcentered care, and population health initiatives shaping its future. Radiology and imaging directors are at the forefront of these changes, working to expand access, improve outcomes, and enhance the patient experience.
Imaging Community Exchange (ICE) Magazine invited leaders in the field to share their perspectives on the opportunities, challenges, and trends that are shaping women’s imaging today.
Participants in this Director’s Circle article on women’s imaging are:
• University Hospitals Breast Center Assistant Nurse Manager-Radiology Department Chelsie Bittinger, RN, BSN, CBCN;
• University Hospitals Breast Centers Mammography Supervisor-Radiology Department Jill M. Gullett, RT(R)(M); and
• Emory Healthcare Director of Patient Care Services-Radiology Tracy E. Powell MSN, ANP-BC;
• Advanced Radiology’s Richard Reaven, MD.
Bittinger and Gullett combined their answers. Their answers are labeled as B&G.
Q: WOMEN’S IMAGING CONTINUES TO EVOLVE WITH ADVANCES IN TECHNOLOGY AND SCREENING GUIDELINES. FROM YOUR PERSPECTIVE, WHAT IS THE BIGGEST OPPORTUNITY RIGHT NOW TO IMPROVE OUTCOMES FOR PATIENTS?
B&G: The biggest opportunity to improve outcomes in women’s imaging can be by expanding access to care, providing faster results and clearer communication, using advances such as abbreviated MRI, contrastenhanced mammography and applying AI tools to ensure consistent quality promotes better outcomes. By reducing anxiety through timely access, quick results, and shared decision-making, we can help patients stay on track with care and improved outcomes. With innovative approaches like abbreviated MRI, contrast-enhanced mammography, and AI tools, we can expand access to high-quality imaging and increase adherence to screening guidelines.
POWELL: The biggest opportunity for women’s imaging is increased education around the importance of early screening and detection. Daily, radiologists play a significant role in identifying abnormalities, especially with mammography. We now utilize digital breast tomosynthesis or 3D mammography which improves cancer detection. Also, interventional radiologist have various treatment options for pelvic health such as treatment for pelvic venous congestion and uterine fibroids.
REAVEN: I think the biggest opportunity to improve outcomes will be to address the current struggles getting women to come in for the annual breast imaging. Right now, only about half of the women over age 40 currently get an annual breast imaging examination. The other half are still experiencing breast cancer, we just aren’t able to find it if we can’t see it. Our job as breast imaging radiologists is to find and diagnose breast cancer at its earliest and most treatable stage. One of the ways that will be important moving forward will be compressionfree options that are just as accurate or even more
accurate than a mammogram, including dedicated low-dose breast CT device.
Q: HOW IS YOUR DEPARTMENT ADDRESSING DISPARITIES IN ACCESS TO WOMEN’S IMAGING SERVICES, PARTICULARLY FOR UNDERSERVED OR RURAL POPULATIONS?
B&G: Imaging departments can reduce disparities and improve access to women’s imaging services by combining technology, community engagement, and practical support. Strategies include scheduling teams offering incentives to rural patient populations, deploying mobile mammography units to bring care directly to underserved areas, and partnering with local organizations to provide outreach and education on breast health and screening guidelines. These efforts make imaging more convenient, raise awareness, and ensure essential services reach all populations.
POWELL: The disparities in women’s health remain a huge issue when so many women are underinsured. This particularly affects women of color and those living in rural areas. The only way to close the gap is through private and federal funding of programs focused on preventative care and early detection. We must also address the shortage of physicians in rural areas. Care can be expanded with increased utilization of advanced practice providers such as NPs and PAs.
REAVEN: Mobile imaging units can play a significant role in rural populations, and hopefully local county and state specific health outreach programs can help the underserved populations. We obviously need more of both of these in order to make a significant impact in underserved and rural women’s health.
Q: ARTIFICIAL INTELLIGENCE AND ADVANCED IMAGING TECHNOLOGIES ARE INCREASINGLY INTEGRATED INTO BREAST AND PELVIC IMAGING. HOW ARE YOU BALANCING INNOVATION WITH ACCURACY, PATIENT SAFETY, AND WORKFLOW EFFICIENCY?


B&G: To effectively leverage AI and advanced imaging technologies, departments must thoroughly validate tools for accuracy, maintain ongoing quality control, and integrate them seamlessly into existing workflows. Continuous staff training helps radiologists, technologists, and support teams understand both the capabilities and limitations of these innovations, reducing errors and enhancing proper use. Prioritizing patient safety through system safeguards and protocols, along with streamlined workflows to prevent bottlenecks, ensures reliable and efficient care. Ultimately, careful evaluation of these innovations, well trained staff, prioritizing patient safety measures, and adherence to ethical standards are essential for maximizing the benefits of these technologies.
POWELL: There must be checks and balances when using modern technology to ensure accuracy and patient safety. One way would be to use AI as a second reader tool and not a replacement for human beings. Also, regular audits would be essential to track discrepancies between AI and radiologists.
REAVEN: I think we need to carefully weigh the pros and cons of artificial intelligence before we go straight into full deployment across the board. There are a lot of questions that remain to be answered, including: Who will pay for these technologies? What are the medicolegal implications of using AI in the radiology space if there is an explicit plan to replace the human radiologist?


Q: WHAT STRATEGIES HAVE BEEN MOST EFFECTIVE IN IMPROVING PATIENT EXPERIENCE AND REDUCING ANXIETY DURING MAMMOGRAPHY, ULTRASOUND, OR MRI FOR WOMEN’S HEALTH?
B&G: Creating a positive patient experience in women’s imaging requires efficient scheduling, clear communication, supportive staff, and a focus on privacy and dignity. Reducing wait times through streamlined workflows helps minimize anxiety, while offering calming options such as music or visuals can further ease stress. Encouraging questions and involving patients in care decisions enhances their sense of control and comfort. Together, these strategies build trust, reduce anxiety, and create a more supportive environment throughout the imaging process.
POWELL: The best strategy for any examination is the human connection with empathy and communication. Using technology such as videos to view prior to testing along with instructions. For mammography especially, taking time to explain the imaging test prior and being honest that the test is not comfortable but using reassurance will help alleviate anxiety.
REAVEN: Education about what to expect is the most important strategy in reducing anxiety and discomfort. But again, using a compression-free imaging modality can be extremely helpful in reducing barriers to entry.
Q: LOOKING AHEAD, WHAT DO YOU BELIEVE WILL BE THE MOST IMPACTFUL TREND OR DEVELOPMENT IN WOMEN’S IMAGING OVER THE NEXT FIVE YEARS?
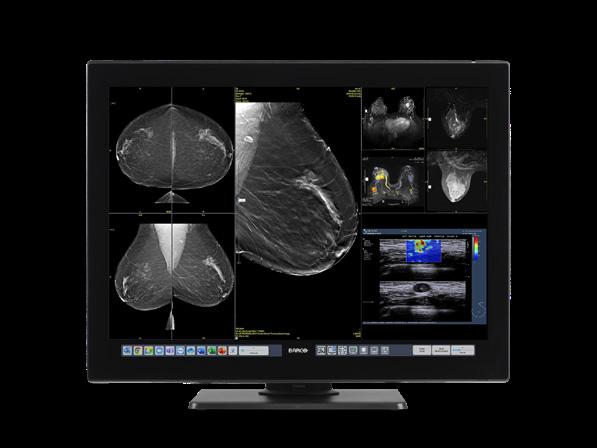
B&G: Over the next five years, women’s imaging will be reshaped by artificial intelligence (AI), machine learning, and modern technologies like contrastenhanced mammography (CEM). AI will improve early detection by spotting subtle changes on mammograms, ultrasounds, and MRIs that can lead to faster and more accurate diagnoses. Risk-based screening tools will allow more personalized schedules, while AIpowered education and communication can reduce anxiety and keep patients more engaged. Automation of routine tasks – like triage, lesion characterization, and reporting – will ease radiologists’ workload and speed up results. CEM, which uses a contrast agent to highlight abnormal areas, provides a cost-effective alternative to breast MRI –especially for women with dense breasts or higher cancer risk. Together, these advances will make women’s imaging more precise, efficient, and patientcentered.
POWELL: The advancements in using pelvic MR for quicker diagnosis of chronic pelvic pain. Also, mammography advances such as contrast enhanced mammography or whole breast ultrasound for dense tissue will be impactful. Finally, robust education on preventative healthcare and early detection. This is a moot point if healthcare is not affordable or accessible. Reducing the number of uninsured Americans is essential.
REAVEN: I think that finding the answers to the questions above will be most impactful in what transpires over the next few years. How we decide what role AI plays in the radiology workflow will be essential. Also, finding a way to bring more women into an annual breast imaging examination will be essential. •
For more information about Bleekley Medical call 1-800-233-5539, visit our website at beekley.com, or email info@beekley.com
The U.S. breast cancer death rate has dropped by about 44% since 1989, due to advances in early detection and treatment; this decline has prevented approximately 517,900 deaths over that period.
Source: American Cancer Society



IMV Medical Information Division, a part of Science and Medicine Group, released its 2025 Mammography and Breast Imaging Market Outlook Report, providing in-depth insights into the current and future state of the U.S. breast imaging market.
Based on an IMV-hosted online survey conducted from January to March 2025 with over 200 mammography professionals from U.S. hospitals and imaging centers, this in-depth report explores key trends and priorities in mammography and breast imaging, from procedure volume to equipment planning and technology adoption.
“The results of IMV’s survey indicate that 78% of respondents anticipate an increase in mammography procedures in 2025 compared to 2024,” said Davin Korstjens, Director of Market Intelligence (Diagnostic Imaging) Insights.
“This trend aligns with projections for new cases of invasive breast cancer and ductal carcinoma in situ, reinforcing the need for expanded imaging services and upgraded equipment.”
Key Insights from the 2025 Report:
• Mammography procedure volumes are expected to rise by high single-digit percentages year-over-year.
• Over 60% of procedures are diagnostic; more than one-third are for screening.
• Hologic remains the most considered OEM, followed by GE and Siemens.
• Patient satisfaction is ranked as the top departmental priority.
Two reports from Grand View Research also predict growth in the “global breast imaging market” and in the related “global women’s health diagnostics market.”
Grand View Research reports that the global breast imaging market size was estimated at $4.7 billion in 2022 and is projected to reach $9.0 billion by 2030, growing at a CAGR of 8.6% from 2023 to 2030.
“Factors such as the rising prevalence of breast cancer, technological breakthroughs in the domain of breast imaging, and investment from several organizations in breast cancer screening programs drive the market,” according to the report.
In terms of region, North America was the largest revenue generating market in 2022. Asia-Pacific is expected to
experience the fastest rate of growth in the global market over the forecast period.
The ionizing technology segment held the largest market share of around 63.2% in 2022 and is anticipated to witness the fastest growth over the forecast period, according to Grand View Research.
“The segment will expand in the upcoming years as a result of the introduction of new ionizing technologybased breast imaging technologies,” the report states.
“Additionally, advancements in currently available ionizationbased technologies are likely to receive significant funding, contributing to the market’s expansion over the forecast period. Moreover, the majority of market participants’ ongoing commitment to raising the number of technology expenditures made in order to offer superior products in the market.”
Furthermore, due to numerous efforts made for breast cancer early detection, the mammography segment of the global breast imaging market is expanding, the report adds.
“The United States Preventive Services Task Force, for instance, has created standards for mammography screening. A cross-sectional study on the most accurate techniques for breast cancer diagnosis was conducted and published in the journal Clinics in July 2020 under the title ‘Evaluation of the accuracy of mammography, ultrasound, and magnetic resonance imaging in suspect breast lesions.’ According to the study, mammography provided a more accurate assessment of worrisome breast masses. The procedure is the most preferred way to diagnose breast cancer because of its accuracy. These benefits contribute to the mammography segment of the breast imaging market growth. “
Grand View Research also reports that several significant market companies are concentrating on mammography for breast cancer diagnosis.
The use of artificial intelligence in breast cancer screening might assist to lessen the workload of healthcare personnel, the report adds. Such advancements in mammography for breast imaging are expected to contribute to the growth of the breast imaging market over the forecast period. Furthermore, various advances in the area have reduced overdiagnosis and improved sensitivity to identify tiny carcinomas. These constant improvements in this sector are anticipated to boost segment growth. •
Help your team shine during ACR accreditation with Bella Blankets Protective Coverlets. Ninety-two percent of ACR accreditation failures in mammography are due to positioning. Improving this technique can make a big difference – for accreditation, image quality and patient care. Bella Blankets provide a secure, non-slip surface that helps keep breast tissue in place, allowing your team to get closer to the chest wall, achieve better positioning, and capture clearer images. In a clinical study patient images using Bella Blankets were compared to prior-year images where no protective coverlet had been used:
• 77% of patients had increased tissue acquisition
• When measuring the PNL in both views, the average increase was 0.41 cm
• 48% of patients showed improved visualization of pectoralis muscle
• Visualization of retroglandular tissue went from 86% PY (prior year) to 96% CY (current year)
• Visualization of IMF as “open” went from 67% PY to 87% CY
1Gerald J. Randall, M.S. (DABR) (Certified Licensed Medical Physicist), “Mammo Protective Coverlets Testing”, March 3, 2017.
*Disclaimer: Products are listed in no particular order.

Discover the MyLab ultrasound series by Esaote, offering comprehensive women’s health solutions. Its advanced technologies include MicroE for breast imaging, which utilizes a multi-step algorithm to detect microcalcifications that may be missed in traditional 2D scans. The system features AIpowered eDetect for precise contouring and automatic lesion measurements, enhancing workflow and consistency. AutoOB AI quickly performs obstetric measurements in seconds, saving time. XVRA technology accurately calculates follicle volume, helping identify the best oocytes and increasing pregnancy chances.


GE HealthCare’s Pristina Via system offers a thoughtful approach to mammography, designed to enhance the screening experience for both technologists and patients. Addressing common concerns about in-room workflow and patient comfort, the system incorporates features such as zero-click acquisition, no wait time between exposures, vendor-neutral prior image comparison, and the lowest radiation dose used. These features combine to help streamline technologists’ workflow, quickly. Pristina Via aims to
optimize the imaging process by reducing repetitive steps and minimizing wait times between exposures. The system is designed to facilitate a more efficient workflow, countering the perception that mammograms are overly time-consuming. This efficiency allows for image acquisition in as little as two minutes, making the overall appointment quicker for patients. The Pristina Via represents an evolution in breast imaging technology, with a focus on making screenings more accessible and supporting the early detection of breast cancer.
The Koning Vera Breast CT (Koning Vera or Vera Scan) is a groundbreaking 3D breast imaging system designed to advance the way clinicians visualize and evaluate breast tissue. Unlike traditional mammography, Koning Vera produces true three-dimensional images with exceptional spatial resolution, offering a comprehensive view of the breast. This dedicated breast CT technology eliminates the need for compression, improving patient comfort while maintaining diagnostic clarity. Built for precision, Koning Vera enables physicians to assess lesions and tissue structures with confidence, supporting more informed clinical decisions. Its advanced imaging capabilities are designed to complement existing modalities, enhancing the diagnostic toolkit for breast health specialists. For patients, the experience is faster, more comfortable, and less intimidating – factors that may encourage more women to undergo regular imaging. For clinicians, Koning Vera represents a step forward in imaging innovation, designed with both workflow efficiency and clinical excellence in mind.


The Mammomat B.brilliant is the first completely redesigned mammography platform from Siemens Healthineers in over a decade. It includes new 3D image acquisition and image reconstruction technology as well as features for full-field digital mammography; breast biopsy; and titanium contrastenhanced mammography. Building on the 50-degree wide-angle image acquisition capabilities that are the hallmark of Siemens Healthineers and offering the widest angle available, the Mammomat B.brilliant introduces PlatinumTomo 3D technology that enables this wide-angle tomosynthesis acquisition in under five seconds.¹ The system’s fast detector and new X-ray tube use flying focal-spot technology to visualize microcalcifications more clearly. New UltraHD image reconstruction technology reduces metal artifacts, crisply visualizes calcifications, and offers customizable image settings. The system also provides a synthetic 2D image with no additional radiation exposure to the patient, reducing the need for full-field digital mammography images. Other features improve patient comfort as well as enhance user workflow and ergonomics compared to the system’s predecessor, the Mammomat Revelation.
¹ Data on file. For average breast size of 50/50 glandular/adipose tissue and 5 cm thickness.

The Genius AI Detection PRO solution is Hologic’s latest and most advanced AI solution to support breast imaging. It uses the proven combination of 2D and 3D cancer detection AI and analyzes prior exams, improving the accuracy of breast screening results.1 The all-in-one user interface features automated pre-reporting, breast density scoring, patient history and image quality checks, driving efficiency and giving radiologists confidence in their assessments.2 The Genius AI Detection PRO solution’s integrated 2D/3D deep learning algorithm improves cancer detection performance.3 With the ability to use priors in its analysis, the solution can also increase specificity and drive an additional reduction in false positive marks per case.1 The image quality review checks also support accuracy in reading, and the automated breast density assessment reduces inter-reader variability and enables more accurate breast density scoring.2 The solution is designed to support workflow efficiency for clinicians. It offers a pre-reporting feature, which integrates and helps auto-populate key fields in the
patient’s report, as well as intuitive lesion and case scoring that can help radiologists quickly assess the suspicion level of a case with a simple color-coded, 1-10 scale.
References:
1 K240301 510(k) Summary Manufactured by Therapixel. Distributed by Hologic.
2 S. Pacilè, et al. (2024). Evaluation of a multi-instant multi-modal AI system supporting interpretive and noninterpretive functions. Accepted for publication in the Journal of Breast Imaging, https://doi.org/10.1093/jbi/ wbae062.
3 S. Pacilè, et al. (2023, May). Application of artificial intelligence to mammography-tomosynthesis combined images for breast cancer screening. [conference presentation]. SBI 2023
• Register for free and apply to any of our listings
• Browse our 350+ open positions across the United States

• Get directly connected with industry hiring managers
• A talent network of 3600+ actively looking biomedical and imaging professionals
• A variety of listing and advertising options
• Social media, print, and eNews promotion
“HTMjobs.com is a remarkable website that can be used by any personnel looking for employment, internships, or just a good read from their Career Center . The site offers job postings from employers in the HTM industry, as well as resources for job seekers to help them prepare for their job search, including resume tips, interview advice, and more.”
By Matt Skoufalos
Breast cancer screening is at once one of the most significant, life-saving components of women’s healthcare, and also one of the most under-utilized, potentially difficult to access, and under-reimbursed. Finding ways to address those challenges involves advancing not only the technological solutions that underpin breast imaging modalities but the disparities in access to them.
SuccesScientific Marketing Manager for Women’s Health at Siemens Healthineers North America Karen Anderson works to connect women to the resources they need to be screened for breast cancer. Nationwide, Anderson notes that the modality she described “the number-one gold standard in mammography” – digital breast tomosynthesis (DBT), or 3D mammography – is still not universally available.
“We’re getting there, but not all facilities have that,” Anderson said. “Some of those facilities still are not caught
up, either for funding, or the ability to provide those types of tests for all people in their community.”
Another consideration that affects screening rates is geography, and – notably in 2025 – the political climate. About four to six times per year, Siemens Healthineers partners with local healthcare organizations to conduct mobile mammography outreach in communities across the country. Those initiatives can find varying degrees of success depending upon the amount of trust that residents have in the process.
This year, Siemens Healthineers made a significant push to provide mobile mammography outreach for women in w, Texas, advertising a five-day screening event on local news channels, flyers in area businesses, and through community partners. However, some people feared that it was a pretense for immigration enforcement, and called asking whether the event was legitimate.
“[We heard] ‘Is this real? Is this an ICE raid?’” Anderson said. “When you have women in these communities,



especially what’s going on today, they are concerned. I never would have thought about that in a million years.”
Ultimately, the outreach initiative brought in 100 women for screening – about half of the figure that it had intended to reach. Eighty percent of those who were screened had never had one before, Anderson said.
“I was there performing these mammograms,” she said. “It was huge to be able to provide that service for that community.”
The encounter underscored another reality of breast cancer screening – namely, that whether women are screened appropriately and consistently depends greatly upon their socioeconomic status, income level, education level, and overall degree health literacy. Perhaps unsurprisingly, lower-income patients participate in breast cancer screenings less frequently, face greater difficulties accessing such services, and don’t necessarily grasp the importance of the process to their health.
According to the National Cancer Institute Cancer Trends Progress Report, in 2023, fewer than 80 percent of American women aged 50 to 74 had received a mammogram within two years. Those numbers fell further based on income (to 71.3 percent for women at less than 200 percent of the federal poverty level) and education (to 69.9 percent for women with less than a high-school education).
If you have it in an area where there’s no transportation, they can’t get there,” Anderson said. “If they are not educated on not knowing that these events can be done, they won’t come. Then you have a lack of awareness in certain cultures and ethnic groups.
“If they are not educated about the event or not aware the event is happening, they won’t come. Finally, you have a lack of awareness in certain cultures and ethnic groups.” Then fewer individuals can be screened, therefore fewer cancers are found.
“Those things really prevent women from coming, and all we can do is continue to educate, to rally, to talk to one another to get your mom, your sister, your aunt, your friend, to get screened,” she said. “The only way we can cure cancer is to find it, and the only way you can find it is getting your mammogram.”
Working around those barriers involves developing a comprehensive knowledge of the individual, and connecting them to the entire team of medical professionals dedicated to their care.
“It takes an entire village to help women navigate this whole process,” Anderson said: “a technologist and radiologist to perform the procedure, a pathologist to diagnose the tissue sample, and a navigator or personal physician to deliver the results and the next step.”
“If you don’t have an entire team working with this, you do have so many women give up and decide I’m never going to do this again,” she said.
Dr. Rachel Preisser of the GRACE Breast Imaging and Medical Spa in Clive, Iowa, believes that the most helpful approach to understanding a patient’s cancer risk involves developing a comprehensive understanding of the myriad factors that contribute to it. As much as breast imaging technologies have continued to improve through the years – and Preisser acknowledges the emergence today of modalities that didn’t exist even 15 years ago – the physician’s understanding of patients’ breast health must become far more individuated.
“Breast imagers have always been at the forefront of technology, pushing the envelope with AI; using computeraided detection years and years ago,” Preisser said. “We’ve always been looking for ways to improve what we do.”
When it comes to clinical approaches, however, “there’s been a huge shift,” she said.
“I want to know about genetics, family history, [breast] density, and [cancer] risk because what I recommend to a patient is going to be very different based on what I get back from that patient,” Preisser said. “As we learn more about all the different contributing factors, it’s about how we deliver that care.”
Preisser’s belief that breast care should not be delivered along a one-size-fits-all model inspired the approach that she and her partner Dr. Andrea Lamphiear developed at GRACE Physicians. There, patients are guaranteed to see a fellowship-trained breast imager to discuss their personal breast cancer risk and risk modification strategies. According to the Iowa Cancer Registry, the state has the second-highest

overall cancer incidence in the country, and the fastest-rising, which underscores the importance of patient education and a personalized clinical approach to breast cancer screening.
“Programs are most effective when everyone who should be screened is being screened,” Preisser said. “In my state, it’s about 70 percent of eligible people participating. That, to me, as a breast imager, is really heartbreaking, and we have to do better.”
“We know that screening mammograms are a really effective tool,” she said. “We have reduced breast cancer death by 44 percent since 1989 because we have been getting people diagnosed earlier and getting them screened.
“It’s something that takes time,” Preisser said. “It takes interest; it takes the care providers being able to know ‘this is what I want to do.’ ”
Preisser also pointed out that systemic gender inequities in the healthcare system have also impeded women’s healthcare. The National Institutes of Health Office of Research on Women’s Health noted that, as recently as the 1970s, “few women worked in either medicine or science, and many women believed that women’s health needs were a low priority in the scientific and medical fields.” It wasn’t until 1986 that NIH policy encouraged researchers to include women in studies, and until 1993 that inclusion of women in medical research was enacted into law.
Finally, a 2021 study in Obstetrics and Gynecology, “Reimbursement for Female-Specific Compared With MaleSpecific Procedures Over Time” concluded that “there is a lower relative value of work, driven by specialty-specific compensation rates, for procedures performed for womenonly than equivalent men-only procedures.”
“When you are dealing with a system that does have a capitalistic component, providers aren’t being paid as much for the same complexity of care,” Preisser said. “It’s very common for women to be diagnosed with breast cancer; it’s been a little bit of a fight to get the data that we need to have evidence-based care.”
Another complication for women who are recommended to have annual screenings for breast cancer because of their risk factors is that they may not have the $1,000 to $3,000 to cover the costs of those procedures. That reality
“The only way we can cure cancer is to find it, and the only way you can find it is by getting your mammogram.” –Karen Anderson

seems to conflict directly with the intention of the national breast density inform law, which was meant to direct women who need secondary screenings to contrast-enhanced mammography (CEM), or breast MRI. Preisser believes that such cost pressures eventually will lead to insurance groups reducing reimbursement rates to the point of unsustainability.
“How do we make this accessible to everyone?” she said. “We have tons of different modalities and tons of great technology. A lot of it comes down to what patients can access.”
“Contrast-enhanced mammography is so much cheaper than a breast MRI,” Preisser said, “but it doesn’t make sense necessarily because you have to spend money on all of this equipment to get started on it, and there isn’t a distinct CPT code that allows us to charge for the procedure. You lose money every time you do one, and it takes a lot of time.”
Dr. Richard Reaven, a practicing radiologist with Advanced Radiology in Baltimore, Maryland, and a consultant on the advisory board for breast CT manufacturer Koning, also believes that the most significant advances in breast cancer screening are built as much upon established technologies like mammography as they are improving accessibility to them.
State and federal breast density inform laws have helped women understand the distinct cancer risks associated with the density of their breast tissue, and for the nearly 50 percent of women who have dense breasts, Reaven said they should learn when to speak with their physicians about different imaging options. Each is not without its challenges.
“Ultrasound is very operator-dependent; some technologists happen to be very good at finding cancers on ultrasound, but there’s only so many of those to go around,” Reaven said. “There’s also a high false-positive rate; a lot of abnormalities that are found that end up being benign are not going to change the clinical outcome of that patient.”
“MRI is a cross-sectional, three-dimensional modality, and that’s an advantage,” he continued. “It can be really helpful in finding three-dimensional tissue abnormalities. The disadvantage is that MRI is incredibly expensive compared to mammography, and requires massive equipment. Getting on
the schedule for a breast MRI can be problematic, and there are only so many MRIs in the country.”
“I do think that dedicated, low-dose breast CT is one of those things that can really be a helpful tool when it comes to imaging the breast,” Reaven said. “It’s a 3D modality; we can absolutely see things in three dimensions that we cannot with traditional mammography or tomosynthesis. It is not reliant on compression, making it a much more comfortable examination. As more and more women hear about this as a potential option, I think they’ll respond positively to it, because it really does offer a truly 3D examination.”
One of the key factors that drives the advancement of breast cancer screening technologies is clinical research, and the anticipated results of several, major national studies are expected in the coming years. Projects like the Tomosynthesis Mammographic Imaging Screening Trial (TMIST), the Women Informed to Screen Depending on Measures of Risk (WISDOM) study, or the 2023 study, “Estimating Breast Cancer Overdiagnosis After Screening Mammography Among Older Women in the United States” all hold weight in the evolution of evidence-based screening approaches.
Mark Horvath, president of the breast and skeletal health solutions division of Hologic Inc. of Marlborough, Massachusetts, said that studies like these contribute significantly to the development and advancement of breast cancer screening modalities.
“It’s an exciting time to see national and international studies like TMIST and the WISDOM study investigating topics that are also key focuses for Hologic – particularly, 3D mammography and individual risk factors,” Horvath said. “These studies help inform our product development and support the clinical value of our technologies.”
Other data sources play a factor, too. Breast density inform laws underscore the value of 3D mammography in helping to detect cancer in women of a variety of breast densities.
“We are proud to have been one of the pioneers of 3D mammography, and are continuing to develop and improve our technology to support patients with dense breasts and ensure they
get the best care possible,” Horvath said.
Manufacturers like Hologic further anticipate that 3D mammography, like many imaging modalities, will be further augmented with artificial intelligence (AI) driven technologies, which may help improve early breast cancer detection rates, or clarify mammogram interpretations.
“AI represents a wealth of possibilities and is one of the most significant advancements in breast imaging since digital breast tomosynthesis,” Horvath said. “AI has elevated 3D mammography by leaps and bounds, transforming what we can see and how efficiently we can see it.”
“At Hologic, we’re investing in and integrating AI capabilities that can flag suspicious areas on an image, prioritize urgent cases, and support radiologists in making more confident decisions,” he said.
Finally, some of the work that may advance the cause of breast cancer screening isn’t based in technology at all. Horvath described a public education campaign that Hologic launched during Breast Cancer Awareness Month last year aimed at clarifying misconceptions around preventive screening exams.
“Some myths from patients included thinking that eating healthy and exercising regularly eliminates breast cancer risk; that they were too young to worry about breast cancer; and that mammograms were painful and could cause dangerous radiation exposure,” Horvath said.
“Through the campaign, we shared facts and research busting those myths, shed light on breast density, and outlined what women of different age groups can expect from their annual well woman exam. We also included a mapping tool to allow patients to find where they could get a Hologic mammogram near them,” he added.
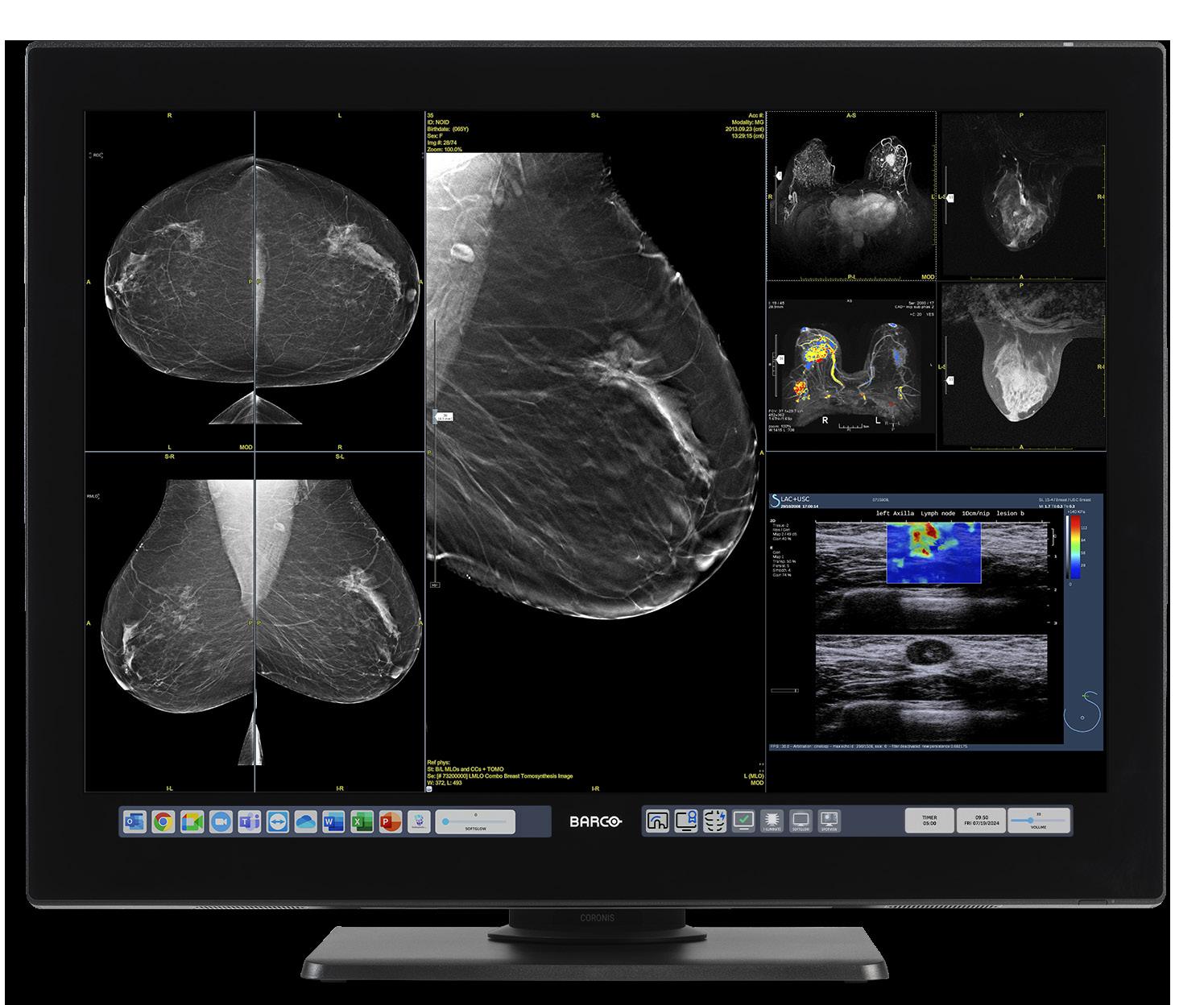
Hologic continued its “Bust the Myth” campaign with new information in October 2025.
Whether any or all of these analog and technological approaches will help to drive down breast cancer deaths will rely upon their accessibility and availability to women of all financial means, cultural backgrounds, and levels of education. The work of finding innovative solutions to achieve these ends doubtless must persist. •

BY NICOLE DHANRAJ
She skipped her MRI because she didn’t have a pad
“I didn’t want to lie on the MRI table like that. I was on my period, I didn’t have anything with me, and I was too embarrassed to say anything.”
Stories like this don’t make it into the chart. But they happen more often than we realize. Across the U.S., patients are canceling or avoiding imaging appointments – not because of cost or transportation – but because they’re menstruating and unprepared.
Period poverty, or the lack of access to menstrual hygiene products, affects nearly 17 million people in the U.S. It’s a quiet but powerful barrier to care – and one that radiology departments can no longer afford to ignore.
Radiology is often the entry point for diagnosis. If patients skip that step due to shame, lack of access, or fear of embarrassment, we’re not just losing an appointment – we’re losing trust, time, and critical opportunities to intervene early.
• 1 in 4 teens in the U.S. has missed school due to lack of access to period products (PERIOD & Thinx, 2021).
• 44% of teens say they feel stressed or embarrassed when they don’t have products; 49% say the lack of access makes them feel like institutions don’t care about them (Campoamor, 2024).
• Period poverty is also linked to higher rates of depression, especially among college students (Gupta, 2024).
Globally, 800 million people are menstruating at any moment, and 500 million lack access to adequate hygiene (UNFPA, 2023). In clinical settings, that lack of access can quietly block people from showing up for care, especially in imaging where patients are expected to change clothes and lie still – often without much privacy.
The tampon tax adds insult to injury. In 20 U.S. states, menstrual products are taxed as “luxury goods,” while essentials like condoms, some medications, and even golf memberships are tax-exempt (Alliance for Period Supplies, n.d.).
The average menstruating person spends $1,773 on menstrual products in their lifetime – and between $100 and $225 of that goes to tampon taxes, depending on where they live (UNFPA, 2023). All of this in a country where women earn 23% less than men on average, and where 12.8% of women and girls live in poverty.
Removing the tampon tax in California, for instance, was projected to reduce state revenue by $55 million annually. In New York, the number was $14 million. But for millions of patients, the value is measured not in lost tax revenue, but in restored dignity and access to care.

This is not just a public policy issue – it’s a departmental practice issue. Here’s how imaging centers and radiology leaders can help:


• Stock free menstrual products in restrooms and prep areas – especially in facilities serving public health or school-based populations.
• Train staff to offer compassionate care without stigma. Menstruation affects patients of all genders, and dignity should never be conditional.
• Partner with local nonprofits like The Pad Project, PERIOD, or Alliance for Period Supplies to provide products and distribute resources.
• Advocate internally for policy changes that recognize menstrual equity as part of your health equity initiatives.
The patient who skipped her MRI didn’t need counseling. She didn’t need a prescription. She just needed a pad.
That moment – avoidable and invisible –represents a wider pattern that radiology departments have the power to break. By recognizing menstrual equity as a clinical access issue, not a side conversation, we take one step closer to delivering the kind of inclusive, barrierfree care that all patients deserve.
Let’s make sure no one delays diagnosis because they couldn’t afford a product that should have been there waiting. •
References
Alliance for Period Supplies. (n.d.). State policy map and tampon tax overview. Retrieved from https://www.allianceforperiodsupplies.org/
Campoamor, D. (2024, August 13). The one back-to-school item teens shouldn’t have to buy. Parents. Retrieved from https://www.parents. com/how-period-poverty-affects-today-steens-8669010
Global Citizen. (n.d.). Everything you need to know about the tampon tax. Retrieved from https://www.globalcitizen.org/en/content/ tampon-tax-explained-definition-facts-statistics/










































































































































































































































































































EMOTIONAL INTELLIGENCE
BY DANIEL BOBINSKI
We need teams. A single violinist can be great, but the sound doesn’t compare to an orchestra. Similarly, a ship needs a crew or it’s not getting out of the harbor.
Workplaces need teams, too, but many teams are nowhere near as effective as they could be. The reasons are many. Some teams lack structure. Others suffer from poor communication. Still others are ineffective because of unclear roles and responsibilities. But perhaps the most significant factor that causes teams to falter is a fundamental misunderstanding of the different ways people operate.
Peak performance emerges when people understand not only their own work style, but also how to adapt to the styles of others. After all, teams are made up of individuals, and when individuals can’t connect effectively, the team suffers. As it’s often said, “a chain is only as strong as its weakest link.”
What’s important to understand is that effective collaboration cannot be forced. To achieve top levels of performance, the right conditions must be created and nurtured, much like a gardener preparing the soil. Gardeners don’t make plants grow; the genetic coding inside each plant does that. But when the right conditions are in place, growth occurs naturally.
The same holds true in professional environments. Good leaders know they cannot force growth, but they can cultivate it. Therefore, the best leaders encourage people to become students of how others naturally operate and communicate.
Dozens of different work styles have been identified over the years, but
a common thread running through all of them is how people approach interpersonal effectiveness. We can look at that on a style continuum, with what I call “Style Focused” people on one end and “Style Flexible” people on the other.
Style Focused individuals believe in the power of consistency. They’ve developed approaches that work for them, and they strive to stay true to their natural communication and work styles.
On the other hand, Style Flexible professionals read people and situations, then adjust their communication, their work style, and their approach to create better outcomes. They understand that what works with one person may not work with another, and they’re willing to adapt accordingly.
In every workplace, knowing when and how to adapt often determines professional success.
Where we think we are on the style continuum may or may not be accurate. For example, when teaching this material to a group of senior executives, most identified themselves as highly flexible. However, when I asked their direct reports, those managers described their executives as quite rigid in their communication style.
This disconnect is common. Many people see themselves as more adaptable than others perceive them to be. That’s why self-awareness is the foundation of emotional intelligence. Self-awareness helps us recognize our natural style.
Following that, social awareness enables us to read the styles of others. Good relationship management dictates that we adapt our approach to build trust. Together, these competencies of self-

awareness and relationship management transform individual effort into greater workplace effectiveness.
The following questions can help you see your tendencies.
Although they present binary choices, be honest about your instinctive responses. Your first reaction often reveals your true preference.
SELF-ASSESSMENT: STYLE FOCUSED OR STYLE FLEXIBLE?
Choose the response that most closely reflects your natural instinct in each situation:
When you encounter tension in a professional setting, you typically:
a) Adjust your approach accordingly
b) Stay true to your natural communication style
When presenting information to colleagues, you:
a) Adjust the level of detail based on their preferences
b) Present information in the way that feels most natural for you
When someone challenges your recommendations, you:
a) Ask questions to understand their concerns
b) Confidently explain your reasoning and evidence
You’re working with someone whose preferred communication method is different from yours. You:
a) Adapt to accommodate their method
b) Continue using your own
When collaborating with people whose work styles differ greatly from yours, you:
a) Adjust your approach to complement theirs
b) Focus on your strengths and natural style
In a disagreement with a client, you:
a) Seek first to understand their point of view
b) Seek first to explain your point of view
When influencing someone’s decision, you:
a) Tailor your approach to what motivates them
b) Use the influence strategies that work best for you
When your usual communication isn’t connecting, you:
a) Mirror their style
b) Stay authentic and trust connection will develop
When feedback suggests your goal needs adjustment, you:
a) Modify the goal to fit the situation
b) Stay committed to your original goal
When joining a new team, you:
a) Observe group dynamics and blend your style
b) Rely on your natural strengths that made you successful
If you chose mostly “a” responses, you lean toward being Style Flexible. You adapt your approach based on people and situations.
If you chose mostly “b” responses, you lean toward being Style Focused. You believe in leveraging your proven strengths and building relationships through consistency.
Here’s what decades of emotional intelligence research shows: people who develop style flexibility consistently achieve higher performance ratings and advance more rapidly. The ability to read situations and adapt accordingly not only improves professional outcomes but also strengthens relationships. This is true among colleagues as well as in crossdisciplinary teams.
In health care environments, this adaptability is more than a workplace advantage; it also helps patients. Physicians, nurses, and technicians who flex their style can foster smoother handoffs, reduce miscommunication, and create climates in which patients feel heard. When small errors can carry high costs, adjusting communication helps create safer, more reliable care.
The good news is that flexibility can be developed. By studying how others perceive and process information, you can make conscious choices to adjust situationally. In doing so, you create conditions in which collaboration, trust, and high levels of performance can flourish.
Bottom line, developing the ability to consciously choose your approach based on the situation is a significant part of the pathway to top performance. •
— Daniel Bobinski, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@protonmail.com or 208-649-6400.


BY BETH ALLEN DIRECTOR’S CUT
Ironically, at the start of MRI Safety Week 2025, we heard the news of a tragic MRI safety incident in New York that resulted in a death. While the details of how this occurred are still being uncovered, it shows how quickly something like this can happen. There is no benefit to judge the situation or assume this could not happen to me. It is an opportunity to be introspective and identify what we can do better.
It was almost 25 years ago when we heard about a tragedy involving a 6-yearold boy and an oxygen tank that became a missile when it was brought into the scan room, killing him. This event set the stage for more stringent MRI safety recommendations across the country. Many of our technologists have heard of this incident but may not have been even born when it took place. Those of us that were working in the field at the time remember hearing about it and were deeply affected by it. Of course, we
grieve for the boy, his parents and the loss they suffered. As technologists, we also had empathy for the staff involved and how that made a mark on them for the rest of their lives. It just takes one poor decision, made in haste, while responding to an emergency.
Events such as these are not a fluke or a freak accident. We know that if we bring metal near the MRI scanner, it will be pulled into the magnet with extreme force. Whether that is a patient gurney, a wheelchair, a floor buffer, a ladder, a gun – anything. It happens fast, before you have time to do anything about it. Unfortunately, it is easy to become comfortable or complacent when you work in this environment every day. Our workplace becomes like home. For our patients, it may be a place of high anxiety. They may not really listen to us and since we are comfortable, we may not be paying close attention either. Sounds like a recipe for disaster. Our processes, workflows, checks and balances need to take all of this
into account. We need to run a tight ship, since there really isn’t room for error. We need to work our safety checklist every single time.
For starters, zones should be set up according to ACR recommendations. This isn’t always easy if we are in a site built for MRI decades ago. So, if it is difficult to have a barrier to enter Zone III, review what is there. Is it good enough?
Everyone in the site needs to understand the zones and what each designation means. ACR and IAC require clear signage designating the zones.
Zone I is generally the lobby or reception space. This area requires no MRI safety screening.
Zone II is a transition from the general population area and the restricted area close to the MRI suite. It is the patient changing and screening zone.
Zone III is where the technologist operates the MRI scanner and just outside the MRI scan room door. Anyone in this area needs to be properly screened and accompanied by MRI personnel. Prior to entering this space, all ferromagnetic objects should be removed. This includes anyone accompanying the patient.
Zone IV is the entire room the MRI scanner is housed in. Access to this zone is strictly prohibited to those that have been screened and given final clearance by the MR personnel with level 2 training. The magnet is always on.
The door to Zone IV is just a passageway. The door should be opened only to allow passage into or out of Zone IV. The door should be closed immediately after getting from one zone to the other. Every time.
We must account for the fact that the patient may not hear us, may have cognitive decline, or be so nervous they are not processing what we are saying to them.
I heard an ad the other day for the world’s first completely invisible hearing aid. Sounds great for someone needing one. Sounds scary to our MRI team. It really comes down to the basics. Stay alert, stay alive.
The MRI scanner can do incredible things. It is a truly amazing diagnostic tool. But we have to proceed with caution. Treat Zone IV as the home of an easily angered, powerful wizard. Respect his power and he may grant you the answers to your questions. Casually enter his domain and dismiss his authority, and he will crush you. This is a wake-up call to anyone that works anywhere near an MRI scanner. This isn’t folklore. It is imperative to the safety of us all to be aware of the danger.
Don’t be the headline. Keep it safe, keep it consistent. Make sure the rules are in place and followed every time.
Thank you for all you do. •



BY MARK WATTS
In the rapidly evolving world of medical imaging, we’ve come to understand two distinct forms of AI. On one hand, there’s Generative AI – the powerful but passive assistant we’ve grown accustomed to. Great for summarizing data or drafting reports, but ultimately a tool that lacks the ability to execute complex workflows on its own. Then we have Agentic AI, which is a more autonomous system designed to plan and execute multi-step processes with minimal human input. While Retrieval Augmented Generation (RAG) has given us a glimpse of how to ground generative AI in a foundation of reliable, up-to-date information, a new architectural leap is emerging that doesn’t just improve how AI works, but fundamentally changes its role.
That leap is the rumored multi-experts feature of GPT-5. Instead of a single, monolithic AI model trying to be an expert in every field, this new architecture leverages a Mixture of Experts (MoE). This means the model is composed of a series of specialized sub-models, each a “domain expert” in a specific area of medicine. When a complex patient case is presented, a central “router” intelligently delegates different parts of the inquiry to the appropriate expert modules.
For a neuro-oncology patient, this could mean an expert on radiology interpreting the MRI, another on genomics analyzing the tumor’s mutations, and a third on oncology reviewing the latest treatment protocols. This is a profound shift. We are moving from a single tool to a digital consulting board – a virtual grand rounds where specialized AI agents collaborate seamlessly to analyze a patient’s case. Their power lies not in their individual brilliance, but in their collective ability to synthesize a vast amount of specialized knowledge.
This emerging AI architecture mirrors and supercharges a philosophy of care that has long been the gold standard at institutions like the Mayo Clinic. The famous Mayo doctrine is not about celebrating a single, brilliant physician. It’s a deliberate rejection of professional ego in favor of a singular, uncompromising commitment to excellence for the patient. The Mayo model is built on the principle that the best possible care for a single patient – the N of 1 – comes from bringing together a diverse, multidisciplinary team of experts to collaborate on their case. The multi-expert AI system is the digital embodiment of this very philosophy. The individual AI modules don’t compete; they collaborate. Their singular purpose is to serve the patient’s needs by contributing their specific expertise without the friction, scheduling conflicts, or cognitive biases that can sometimes arise in human collaboration.

HOW MULTI-EXPERT AI SUPERCHARGES THE N OF 1
Let’s imagine that same neuro-oncology patient again. With a multi-expert AI, the radiologist isn’t just getting an image flagged for a tumor; they’re getting a comprehensive, integrated report. The system’s radiology expert analyzes the scan, the genomics expert identifies a rare genetic marker, and the oncology expert crossreferences that marker with a global database of clinical trials and successful treatments. The final output isn’t just a radiology report or a pathology summary; it’s a synthesized, “N of 1” treatment plan that provides the entire care team with a complete picture.
This allows for a level of precision and personalization that is currently unachievable at scale. It ensures that every patient, no matter where they are in the world, can
benefit from the collective wisdom of an interconnected, “expert” team. This system’s power lies in its ability to synthesize information from a patient’s EHR, their imaging, and their genetic data, and then compare it to millions of other cases to find the most effective path forward. This isn’t just about making workflows more efficient; it’s about fundamentally elevating the standard of care.
This new class of AI is not simply a better tool. It is a new collaborator that mirrors our highest ideals in medicine: a relentless focus on the patient and a commitment to excellence that supersedes all else. •
— Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.


BY JAKE BUEHLER ASRT Chief Communications Officer
Th e American Society of Radiologic Technologists (ASRT) Be Seen campaign is spreading awareness about medical imaging and radiation therapy professionals. Through commercials, videos, social media posts, earned media placements, paid advertising and word-of-mouth, Be Seen is raising the visibility and respect for the profession by educating the public, other health care professionals, prospective students and elected officials about the vital role medical imaging and radiation therapists play on the health care team.
As ASRT’s mission is to advance and elevate the medical imaging and radiation therapy profession and to enhance the quality and safety of patient care, the Be Seen campaign is an effective initiative to help ASRT meets its goal.
Millions of people have viewed Be Seen content, and its viewership continues to grow every day. The campaign’s first phase generated more than 50 million total views on a variety of platforms and ASRT is confident that the campaign’s second phase, which launched in June, is going to keep the momentum moving forward.
The campaign’s second phase highlights 12 individual practice areas in the medical imaging and radiation therapy profession. ASRT is producing 30-second commercials for each practice area. ASRT’s strategy behind producing individual commercials is to make sure the nation understands that medical imaging and radiation therapy
professionals are performing the procedures and are providing patients with high-quality care every single day. Doctors and nurses aren’t performing those highly technical and advanced procedures and treatments; radiologic technologists are. It’s vital the public, other health care groups and elected officials understand that important distinction.
The commercials are supported by Be Seen digital advertisements, earned media initiatives and social media campaigns, resulting in a comprehensive communications plan that spreads the word about the medical imaging and radiation therapy profession.
The first three commercials highlight radiographers, magnetic resonance technologists and radiologist assistants. They have been streaming on connected TV throughout the summer and are spreading on social media platforms. Radiologic science professionals and others can share the commercials with their colleagues, friends and family by visiting ASRT’s YouTube channel, youtube.com/@ASRTOrg. Also, if medical imaging and radiation therapy facilities would like to air the commercials, contact pr@asrt. org.
GE HealthCare is supporting the Be Seen campaign through access to medical imaging equipment, cross-promotional opportunities and subject matter expertise. GE HealthCare’s facilities in Wisconsin served as the filming locations for the radiography, MR and RA commercials and will be used for future individual practice area commercials. Visit asrt.org/BeSeen to learn more about the campaign, access all the completed commercials and tell stories about being a medical imaging and radiation therapy professional. •







Despite a significant increase in Americans’ aerobic and strength activity, external factors like smoke-filled air and the lapse of a COVID-era food program may be making us less fit overall.
Those are the primary conclusions from the 18th annual ACSM American Fitness Index rankings published by the American College of Sports Medicine (ACSM) and the Elevance Health Foundation, the philanthropic arm of Elevance Health, which annually tracks how well the 100 largest U.S. cities support healthy, active lifestyles.
The Fitness Index results – based on 35 evidence-based indicators – showed three indicators changed in an unhealthy direction – air quality, food insecurity and reports of excellent or very good health – each getting slightly worse. Declines in air quality can be attributed to wildfires and droughts; in addition to U.S. wildfires, smoke from wildfires across several Canadian provinces traveled south and impacted millions of people in the Northeast and Great Lakes regions in 2024. Ninety-nine of 100 cities in the Fitness Index had an increase in their food insecurity percentage. Research shows this may be a result of the expiration of the expanded Child Tax Credit and the end of other COVID-era programs supporting access to food.
City and county officials can use the Fitness Index as a data-driven baseline to measure progress and make informed decisions to further improve residents’ health. Arlington, Virginia; Washington, D.C.; Seattle, Washington; San Francisco, California and Denver, Colorado are the top five cities in this
year’s rankings. Rounding out the top 10 fittest cities are Minneapolis, Minnesota; Madison, Wisconsin; Atlanta, Georgia; Sacramento, California; and San Diego, California. Full rankings and scores, a call-to-action report, a city comparison tool and other insights are accessible on the Fitness Index website: americanfitnessindex.org
“The Fitness Index has become a trusted and powerful tool to help us better understand and address the physical, behavioral and social drivers of health in communities, while providing the data and expertise that empower advocates and city officials to take action,” said Shantanu Agrawal, MD, chief health officer at Elevance Health. “Elevance Health Foundation enjoys our partnership with ACSM and the opportunity to leverage these insights and tailor our efforts to address specific community needs.”
Agrawal emphasized the partnership’s mutual vision to improve lives.
“Elevance Health Foundation is working with communities to address social drivers of health in our country, including physical activity and the critical issue of food insecurity,” he continued. “Since 2021, our foundation has awarded more than $30 million to nonprofit organizations addressing food insecurity while improving health outcomes, reaching more than 1.2 million Americans. Our efforts are well received and rewarding, and ACSM is working nationally to extend and enrich lives through the power of movement.”
While challenges still exist, the Fitness Index data show a 9% increase on average in residents meeting the aerobic activity guidelines: 59.9% in 2025 is up from 50.9% previously reported. More impressively, in 94 of the 100 largest U.S. cities and their
residents reported improved aerobic activity levels; the largest increases were reported in Plano, Texas, and Fort Wayne, Indiana. Cities also reported a significant increase in residents meeting aerobic and strength activity guidelines. Of the 100 cities assessed, 89 averaged a 7.6% increase, with the largest increase observed in Richmond, Virginia (18.8%).
This upward trend among the largest 100 cities shows a growing commitment from both cities and their residents to promote and maintain active lifestyles and improve overall health through increased aerobic and strength activities.
Other notable improvements were seen in decreased rates of smoking (73 cities had a 2.6% decrease, on average). In addition, there was an increase in funding for parks; 64 cities reported an average increase of $48 per capita. Among these cities, seven had a per capita increase of more than $100.
“We celebrate the best efforts of individuals and municipalities to improve overall health and fitness levels,” said ACSM past-president and chair of the Fitness Index Advisory Board Stella Volpe, Ph.D., FACSM, ACSM-CEP. “These efforts are always going to be affected – good or bad – by a broad variety of other factors. This year, pollution from wildfires and legislation addressing food insecurity that limited further progress. Regardless, such challenges should never deter us from supporting and expanding healthy lifestyles for all.”
Volpe said the Fitness Index offers three distinct ways community leaders and residents can make a difference:
• Fuel Your Knowledge: Armed with Fitness Index data on a composite of health behaviors, chronic diseases, and community assets based on the most recent data available, residents can advocate for local initiatives and policy changes in their own communities.
• Celebrate Success and Inspire Action: The Fitness Index celebrates strides that the ranked cities have made toward promoting a culture of health and fitness. It is a source of inspiration for city leaders and residents alike, motivating them to pursue even greater achievements.
• Join the Movement: Cities are offered essential tools and resources by the Fitness Index to help leaders and residents assess their communities’ health and fitness landscape and work together to advocate for positive changes.
“Healthy living starts where we live, learn, work and play,” she continued. “By getting involved in grassroots advocacy, you can help create a community that encourages and supports a healthy, active life.”
Volpe said there are two new indicators this year – trail miles and splashpads, and an update to measuring tennis courts to include pickleball and dual-use courts. She said the advisory board adjusts indicators annually, noting that the data provides a framework for ongoing evaluation, enabling cities to monitor their progress and celebrate their achievements in building healthier and more vibrant communities. •


“Leadership and learning are indispensable to each other.”
– John F. Kennedy


In December 2025, we will announce the eight imaging directors or managers selected by our ICE audience for their outstanding contributions.
CM




Tri-Imaging Solutions introduces a















platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools streamlines parts ordering and tracking.


Tri-Imaging Solutions introduces a cutting-edge management, engineer performance, and diagnostic tools and video tutorials, Designed for efficiency, the platform setting a new standard for reliability in medical
downtime and optimizes operations,



proactively monitors system health, supports engineers in repairs, and enhances the supply chain process by giving teams seamless access to parts
XperTIS offers step-by-step repair guidance, helping engineers troubleshoot efficiently while ensuring faster, more accurate parts ordering This helps maximize uptime and minimize repair costs.
Tri-Imaging Solutions introduces a cutting-edge platform that enhances supply chain management, engineer performance, and system monitoring. It provides engineers with diagnostic tools and video tutorials, and streamlines parts ordering and tracking. Designed for efficiency, the platform minimizes downtime and optimizes operations, setting a new standard for reliability in medical imaging.

• $300 a month
• 1/6 page ad included the marketplace
• Up to 5 categories in ICEDEX
• Your company name, website and phone included in your ICEDEX listings
• Your company name in the alphabetical business index
• Appear in the print and digital magazine