




Prepzyme® Forever Wet creates a long lasting moisture barrier. As seen here, instrument remains wet to the touch for days after application.







Prepzyme® Forever Wet creates a long lasting moisture barrier. As seen here, instrument remains wet to the touch for days after application.

The latest breakthrough in enzymatic pre-cleaning sprays, Prepzyme®
Forever Wet’s unique humectant properties form a moist coating over the instruments that lasts for days.

•The humectant formulation creates a moisture retention barrier which keeps soiled instruments and scopes moist for a prolonged period of time – unlike a GEL which HAS NO MOISTURE RETENTION properties
•Operating room safe, non-aerosol, multi-tiered enzymatic spray helps prevent bio-burden from drying on the surface of soiled instruments and scopes
•Ideal for transporting soiled instruments that may sit for an extended period of time
•Reduces tray weight during transport compared to liquid presoaks
•Soiled sharps are visible through humectant
• Decreases spills and potential cross-contamination






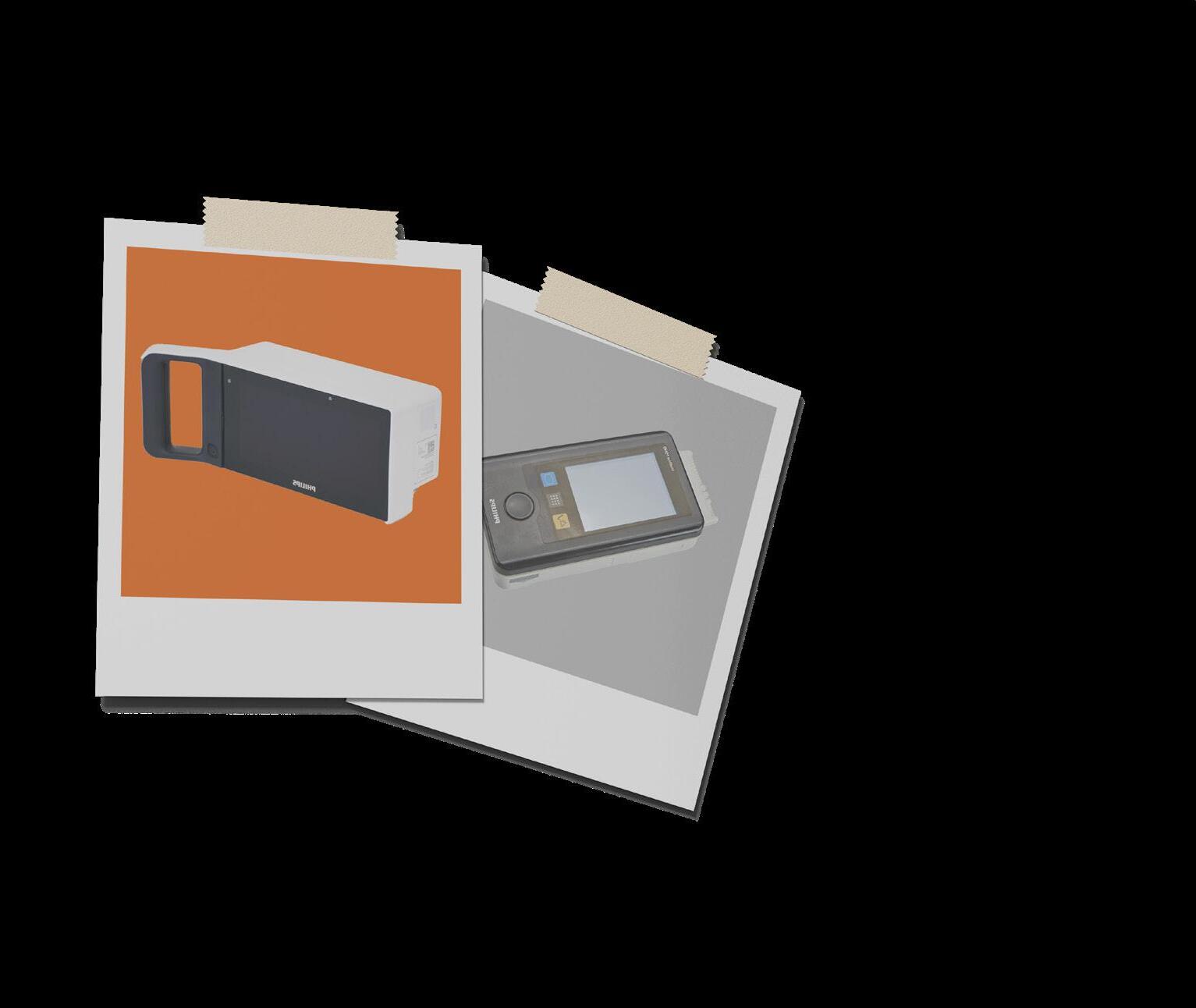

UltraSAFE addresses the common issues associated with formalin exposure to create a safer, standardized, and costeffective solution to the challenges Perioperative Nurses face daily. We all know by now that formalin is carcinogenic and bad for our health. We also know that formalin is the accepted standard and is not going anywhere, which is why it is critical that you advocate for your health to ensure you can manage specimens in the safest way possible. That means ZERO EXPOSURE and complete automation. UltraSAFE offers exactly that. Say goodbye to manual filling and costly spills and take the guesswork out of documentation. With UltraSAFE, time to fixation, weight of specimen, and formalin quantity are recorded on a printed label to ensure the integrity of each specimen. The future is safe; UltraSAFE.


• Enclosed and vented dispensing chamber for complete operator and specimen safety
• Built-in scale for automatic specimen weighing
• Programmed maximum and minimum formalin levels for correct ratio

• Printed labels with customizable fields for complete documentation
• One-way valve lids for automatic filling and formalin fume protection
• Easy to use touchscreen with on-board tutorial videos for training






It is more important now than ever to prepare the next generation of OR nurses as the surgical environment becomes more demanding and experienced nurses retire. Early exposure to the OR helps spark real interest, builds confidence and shows students what working in this specialty truly involves.




(Vol.
#3)


PUBLISHER
John M. Krieg
john@mdpublishing.com
VICE PRESIDENT
Kristin Leavoy kristin@mdpublishing.com
VICE PRESIDENT OF BUSINESS DEVELOPMENT
Jayme McKelvey jayme@mdpublishing.com
EDITOR
John Wallace editor@mdpublishing.com
ART DEPARTMENT
Karlee Gower
Taylor Hayes
Alicia Brown
ACCOUNT EXECUTIVES
Megan Cabot
Emily Hise
DIGITAL SERVICES
Cindy Galindo
Kennedy Krieg EVENTS
Kristin Leavoy
ACCOUNTING
Diane Costea
WEBINARS
Linda Hasluem
EDITORIAL BOARD
Vangie Dennis, MSN, RN, CNOR, CMLSO Assistant Vice President, Perioperative Services, AnMed
Justin Fontenot, DNP, RN, NEA-BC, FAADN Associate Professor, Tulane University School of Medicine, New Orleans, LA
Natalie Lind, Education Director for the Healthcare Sterile Processing Association, HSPA
Pat Thornton, MSM, RN, CNOR Perioperative Consultant, RNFA Dermatology Institute
Dawn Whiteside, DNP, MSN, RN, CNOR, NPD-BC, RNFA, Director of Education, CCI
Julie Williamson, BA Director of Communications, HSPA

Preoperative skin antisepsis is a critical part of reducing the bacteria on the skin that may cause infection prior to surgery.1 There are many factors to consider in the determination of which antiseptic to use for a particular patient.
ChloraPrep™ Skin Prep for:
Proven efficacy
Backed by over 60 clinical studies, ChloraPrep™ stands out with scientifically proven results.
Persistent protection
Enjoy peace of mind of persistence for at least 7-days.2,3
Orange tint
Our hi-lite orange tint helps mark the prep area and reduces the risk of clinical misdiagnosis based on skin coloring during post op care.4,5,6,7
Fully sterile
BD® sterile applicators and solutions help prevent the risk of intrinsic and extrinsic contamination.8,9

ChloraPrep™ Skin Prep demonstrates at least PERSISTENCE1,2



Follow the QR Code to discover the difference of unmatched experience on proven performance.
1. Association of preoperative Registered Nurses (AORN). Guidelines: Key Takeaways for Patient Skin Antisepsis. https://www.aorn.org/article/guidelines-key-takeaways-for-patient-skinantisepsis 2. Beausoleil C, Comstock SL, Werner D, Li L, Eby JM, Zook EC. Antimicrobial persistence of two alcoholic preoperative skin preparation solutions. J Hosp Infect. 2022 Nov;129:816. 3. Degala, et al. United States Patent 9,078,934. July 14, 2015. BD, the BD Logo and ChloraPrep are trademarks of Becton, Dickinson and Company or its affiliates. ©2025 BD. All rights reserved. BD-143543 (2/25) 4. Adeyinka A, Kondamudi NP. Cyanosis. In: StatPearls [Internet]. Treasure Island (FL):StatPearls Publishing; 2022 Jan. Available from: https://www.ncbi.nlm. nih.gov/books/NBK482247/ 5. Fletcher J. Bruise colors: Causes,timescale, and when to see a doctor. Medical News Today. 2020 Jan 4. Available from: https://www.medicalnewstoday.com/ articles/322742 6. Mount Sinai. Jaundice Information. Available from: https://www.mountsinai.org/health-library/diseases-conditions/jaundice 7. 2021 AORN Guidelines for Perioperative Practice: Patient Skin Antisepsis. 8. Food and Drug Administration. https://www.fda.gov/drugs/drugsafety/ucm374711.htm 9. Weber DJ, Rutala WA, Sickbert-Bennett EE. Outbreaks associated with contaminated antiseptics and disinfectants. Antimicrob Agents Chemother. 2007 Dec;51(12):4217-24.
BD, the BD Logo and ChloraPrep are trademarks of Becton, Dickinson and Company or its affiliates. © 2025 BD. All rights reserved. BD-143543 (3/25)
By Dawn Whiteside
Nearly a decade ago, the American Nurses Association (ANA) updated its position on workplace violence, declaring that “nurses must be afforded the same level of respect and dignity as others” (ANA, 2017). In the seven years since the ANA launched its #EndNurseAbuse pledge, the nursing profession has taken a firm stance: violence of any kind, from any source, is unacceptable.
Nurses and employers across all settings – clinical, academic, and research – must work together to foster a culture of respect, free from incivility, bullying, and violence. Yet, recent data reveals just how urgent this issue remains. According to National Nurses United (NNU), over 80% of nurses experienced at least one form of workplace violence in 2023, and more than 45% reported an increase in violence on their specific units (NNU, 2024).
Whether treating patients who have experienced trauma or recovering from it themselves, nurses need support. One such intervention is Psychological First Aid (PFA), an early psychosocial approach that helps reduce acute stress and promotes adaptive coping mechanisms
in individuals following trauma (Vernberg et al., 2008).
PFA is endorsed by the World Health Organization (WHO) and focuses on listening without forcing disclosure, identifying and addressing immediate needs, and encouraging connection to personal support systems (Figueroa et al., 2024). The Hobfoll model of PFA highlights five essential elements: safety, calm, self-efficacy, connectedness, and hope. This model utilizes techniques such as active listening, relaxation strategies, problem-solving, and fostering social connections. Remarkably, even a single session has shown reductions in anxiety, depression, and PTSD symptoms (Figueroa et al., 2024).
Still, the best way to reduce workplace violence is through prevention.
The Occupational Safety and Health Administration (OSHA) mandates that all healthcare organizations implement a workplace violence prevention plan. These plans must consider unit-specific risk factors, including patient population, staffing levels, and the surrounding environment (NNU, 2024). An effective assessment should include walkthroughs of care areas, frontline staff input, and a thorough review of prior incident reports.
Following this assessment, hospitals should adopt behavioral, administrative, and environmental strategies, such as identifying highrisk patients, installing security cameras and metal detectors, and limiting visiting hours. In one study, implementing such strategies led to a 50% decrease in violent incidents (NNU, 2024).
Despite these promising interventions, employer responses to violence remain inconsistent. According to a 2023 NNU survey:
• 42% investigated reported incidents
• 28% offered counseling
• 43% implemented training or retraining
• 21% made procedural changes
• 17% discouraged reporting
• 29% blamed the employee
• 45% ignored the report altogether (NNU, 2024)
Worse still, only 10% of respondents said their employers had implemented any preventive measures at all. Many facilities still view violence as an unfortunate but a normal part of the job.
A complicating factor is that approximately 90% of violent incidents are perpetrated by patients. When a patient’s medical condition contributes to violence, it can be difficult for law enforcement to
intervene, as establishing intent is challenging (NNU, 2024).
Despite these obstacles, it is essential that healthcare institutions not only have a workplace violence prevention plan but also ensure it is transparent, actionable, and developed with input from those on the frontlines.
PFA, though originally developed for humanitarian crises, is proving to be a critical tool in addressing the trauma of workplace violence in healthcare. As nurses continue to face this growing threat, they must be equipped not only with clinical skills but also with the psychological support systems to care for themselves and each other.

• Active Listening (10-20 minutes)

– Dawn Whiteside, DNP, MSN-Ed, RN, CNOR, NPD-BC, RNFA is the Director of Education and Professional Development of the Competency & Credentialing Institute.
Dr. Whiteside has over 35 years of experience as a perioperative nurse in many roles including circulator, scrub, first assistant, team leader, charge nurse, manager, and educator. She serves on the ABSNC Board of Directors as well as the editorial board for OR Today. As an educator, Dr. Whiteside is passionate about developing educational materials for all members of the perioperative team.
References
American Nurses Association (ANA). (2017). Take the pledge to #EndNurseAbuse. https://www.myamericannurse. com/take-pledge-end-nurse-abuse/ Figueroa, R. A., Cortés, P. F., Miller, C., Marín, H., Gillibrand, R., Hoeboer, C. M., & Olff, M. (2024). The effect of a single session of psychological first aid in the emergency department on PTSD and depressive symptoms three months post-intervention: Results of a randomised controlled trial. European Journal of Psychotraumatology, 15(1). https:// doi.org/10.1080/20008066.2024.2364443
National Nurses United (NNU). (2024). High and rising rates of workplace violence and employer failure to implement effective prevention strategies is contributing to the staffing crisis. nationalnursesunited.org/sites/default/files/ nnu/documents/0224_Workplace_Violence_Report.pdf
Vernberg, E. M., Steinberg, A. M., Jacobs, A. K., Brymer, M. J., Watson, P. J., Osofsky, J. D., Layne, C. M., Pynoos, R. S., & Ruzek, J. I. (2008). Innovations in disaster mental health: Psychological first aid. Professional Psychology: Research and Practice, 39(4), 381–388. doi:10.1037/a0012663
Goal: Provide reassurance using empathy and companionship. Trauma survivors are encouraged to talk without being interrupted. The provider uses listening, paraphrasing, and reflection.
• Breathe Retraining (5-10 minutes)
Goal: A feeling of calm as a result of extended exhalation. Breathing exercise focusing on intentional inhale and extending the exhalation.Count upon inhalation and count while exhaling.
• Categorization (5-10 minutes)
Goal: Assist the survivor to regain control of the traumatic event and increase purposeful thinking.Assist with identification and prioritization of needs and concerns.Encourage communication with significant individuals.
• Referral (5-10 minutes)
Goal: Implement regular social support and maintain close relationships with family and friends. Refer survivor to social support that is specifically linked to the person themselves and the trauma experience. Perform the actual work of finding the best social support network (making phone calls, accompany survivor to appointment).
• Psychoeducation (5-10 minutes)
Goal: Assist the survivor with understanding trauma reactions and what to expect. Provide information about common reactions to trauma. Ensure understanding of warning signs, ways of coping, access to mental healthcare and myths.
Nurses Reporting

By Tricia Dixon-Thomas, MSN, RN
Can your patients tell the difference when they interact with your direct employee versus someone from an agency? Does your staff feel a difference? Do your metrics show a variance based on who provides a service? Whether support or direct care staff, outsourced services must follow your policies and procedures and be held to the same high standards as the rest of your team.
Historically, ambulatory surgery centers have contracted with both support staff and direct care providers, whereas hospitals have relied more on contractors for nonclinical roles like IT and billing. However, staffing shortages and other organizational goals have caused a shift in hiring practices, with more hospitals leaning towards contracting with telemedicine providers, anesthesiology services and more.
Either way, subcontractors represent you, and therefore your commitment to compliance, operational efficiency, and quality care. Poor service from contractors can lead to delays, rework, or compliance issues. Mismanaged contracted services (e.g., instrument
processing, billing errors, or inadequate documentation of anesthesia services) increase legal and reputational risks. Periodically evaluating your contracted services is a risk management necessity as well as an accreditation requirement.
ACHC standards for contractors cover the same basic principles, regardless of the healthcare setting:
• The governing body must oversee services provided by a third party and ensure these services are provided safely and effectively.
• Contractor services must be included in the organization’s Quality Assurance and Performance Improvement (QAPI) Program.
• Contracts must be reviewed annually.
When evaluating a contracted service, set clear expectations. The contract should specify the services to be delivered, the methods to be used, and the expected level of quality. For direct care services, staffing agencies should provide evidence of competencies and how they were assessed. But this does not mean your hospital or ASC can omit orientation to your own policies and procedures, nor does it absolve your organization
from completing relevant due diligence – including credentialing and privileging for provider roles.
Even if the contracted service is required to provide relevant metrics, collect your own data. Check whether the services are provided within the agreed upon time frames, whether they impact patient satisfaction surveys, and if the contracted personnel adhere to your policies and procedures. Communicate corrective actions according to the contract’s provisions.
Developing quality indicators
To embed contracted services within your QAPI Program, establish specific quality indicators. Examples of commonly used metrics that can be applied to contracted services include:
Anesthesia Services
• Patient safety outcomes (e.g., adverse reactions, post-anesthesia complications)
• Timeliness of anesthesia administration and recovery
• Compliance with ASA (American Society of Anesthesiologists) guidelines
• Patient satisfaction scores related to pain management

Sterilization and Infection Control Services
• Sterility failure rates (e.g., positive biological indicator tests)
• Compliance with CDC & OSHA guidelines
• Turnaround time for sterilized instruments
• Hand hygiene compliance of contracted personnel
Medical Equipment Maintenance and Repair
• Percentage of equipment failures during procedures
• Response time for urgent repairs
• Preventive maintenance compliance rate
• Documentation of equipment testing and calibration
Medical Billing & Revenue
Cycle Management
• Claim denial rate due to billing errors
• Turnaround time for claims submission
• Accuracy of coding and compliance with CMS regulations
• Patient billing complaints and resolution times
Housekeeping & Environmental Services
• Frequency of compliance audits (e.g., surface disinfection, temperature, humidity, and air pressure logs)
• Incidence of hospital-acquired infections (HAIs)
• Completion rates of daily cleaning checklists
• Inspection results from regulatory agencies
Laboratory & Pathology Services
• Turnaround time for test results
• Accuracy of test results (error rates)
• Compliance with CLIA (Clinical Laboratory Improvement Amendments) standards
• Patient safety incidents related to lab errors
Waste Management & Biohazard Disposal
• Compliance with EPA & OSHA regulations
• Proper segregation of medical waste
• Incidents of improper disposal
• Staff training compliance on waste handling
IT & Electronic Medical Records
(EMR) Services
• System uptime percentage
• Data breach or cybersecurity incidents
• Resolution time for user-reported issues
• HIPAA compliance for data security
Security & Facility Management Services
• Incident reports related to unauthorized access
• Staff and patient satisfaction with security presence
• Response time for security concerns
• Adherence to emergency preparedness protocols
What you stand to gain
Using quality indicators to review contract services contributes to regulatory compliance, but that’s not all. Tracking quality metrics identifies trends, addresses deficiencies, and improves workflows. Setting clear, measurable benchmarks (e.g., infection rates, equipment maintenance logs, billing accuracy) holds contractors accountable for their services and performance. When you evaluate performance, your organization gets the best value for your money. Thorough and thoughtful analysis of the data produces meaningful results that only serve to make your organization better.
Read the fine print
While some contracts are considered “evergreen,” reviewing them periodically (the ACHC Standard requires annual review) is important to ensure they continue to meet the organization’s needs. If an existing contract does not meet your needs, make revisions during the next review.

– Tricia Dixon-Thomas, MSN, RN is a Clinical Review Specialist for the ASC and OBS Accreditation Programs at Accreditation Commission for Healthcare (ACHC) with more than 20 years of experience in ASCs. She is passionate about teaching and mentoring the next generation of outstanding managers and directors in the outpatient surgical environment.
By Gerry O’Dell, O’Dell and Hodge Consulting, and Deborah Havlik, DAHavlik Consulting LLC
The items that can affect the energy transfer are “wet” steam (i.e., too much condensed water in the steam usually caused by contamination in the steam) or steam that is superheated (steam that is too dry because it has been heated beyond its saturation point) creating a dry heat process. Both can result in a lack of sterilization.
Contained product sterilization is where indirect contact of the heating medium with the external surfaces of contained product is used to create moist heat internally to sterilize the product within the container. It is performed using heat transfer methods such as steam or steam-air mixtures, water sprays, or water immersion. For many practitioners, this concept is best described by the method used to sterilize growth media in the microbiology laboratory; in this case the energy transfer occurs by conduction or convection². Healthcare products that can be sterilized using contained product processes are items such as intravenous solutions and dermal fillers.
Moist heat sterilization is a faster sterilization process than dry heat sterilization and typically occurs at lower temperatures for shorter times. However, dry heat sterilization can be a cost-effective, efficient method to sterilize those items that are conducive to the process.
While most often used in the pharmaceutical industry for depyrogenation and thus sterilization of product containers, dry heat sterilization can also be an option for healthcare products that cannot withstand exposure to moisture at high temperatures. This is a simple process; the two parameters of dry heat sterilization are time and temperature. Besides the ISO 20857 standard³, PDA TR.3,4 provides guidance for dry heat processes. Examples of healthcare products sterilized by dry heat include ophthalmic products, silicone implants, wound care products, and dental instruments.
Conclusion
Heat sterilization with either moist or dry heat can be an effective method for sterilization for medical devices that
can withstand the temperatures of the process and are common methods of sterilization for other types of health care products. The requirements and guidance for these processes are defined by standards.¹,³
References
[1] ANSI/AAMI/ISO 17665:2024, Sterilization of health care products — Moist heat — Requirements for the development, validation and routine control of a sterilization process for medical devices. Association for the Advancement of Medical Instrumentation; 2024. Arlington, VA.
[2] Technical Report (TR) 1:2007, Validation of Moist Heat Sterilization Processes: Cycle Design, Development, Qualification and Ongoing Control. Parenteral Drug Association; 2007. Bethesda, MD
[3] ANSI/AAMI/ISO 20857:2010/(R)2015, Sterilization of health care products — Dry heat — Requirements for the development, validation and routine control of a sterilization process for medical devices. Association for the Advancement of Medical Instrumentation; 2010. Arlington, VA.
[4] Technical Report No. 3 (Revised 2013) Validation of Dry Heat Processes Used for Depyrogenation and Sterilization. Parenteral Drug Association; 2013. Bethesda, MD.

Reduce your insufflation costs by up to 50% with the NEBULAE® I System and NTI’s portfolio of generic insufflation/smoke evacuation tubing options.
Maintain Stable Pressure
Adjustable pressure settings to accommodate pediatric to bariatric laparoscopic and robotic procedures.
Reduce Cost
Reduce costs up to 50% by eliminating the need to purchase proprietary equipment.
Remove Smoke
Evacuate smoke and reduce CO2 gas usage.
The Association for the Advancement of Medical Instrumentation (AAMI) released a new technical information report (TIR) to guide healthcare facilities on the safe external transport of medical devices.
AAMI TIR109:2025 External transport of medical devices processed by health care facilities provides recommendations for transporting processed medical devices in a way that maintains the integrity of sterilized packages. It also provides guidance for the safe and effective transport of contaminated items.
Due to logistical and financial reasons, there has been a growing trend with healthcare facilities transporting items from one facility to another. Whether devices are transported to a facility across the street or at a greater distance, there have been numerous safety concerns related to the practice. The guidance in TIR 109 addresses some of the key challenges healthcare facilities face.
In most cases, medical devices are transported outside of the healthcare
facility over public roadways; therefore, the items transported must comply with the specific local, state or federal regulations, including the Department of Transportation’s (DOT’s) Hazardous Materials Regulation, the Occupational Safety and Health Administration’s (OSHA’s) Bloodborne Pathogens Standard (29 CFR 1910.1030), and Environmental Protection Agency (EPA) requirements. TIR109 addresses this regulatory information.
Quality systems are woven into all aspects of sterile processing, and this remains true when performing external transport. TIR109 includes a section describing quality system considerations to ensure work practices and environmental controls maintain the integrity of the product and minimize the potential for contamination of used devices. It is recommended that the healthcare facility have a policy that describes documentation and records, identification and traceability of instruments, inspection and release procedures, safety procedures, training procedures, and supplier controls and monitoring. Guidance is also provided for
the physical area for both loading and unloading to promote effective and efficient design and processes. Further, the TIR underscores the importance of using the correct transport carrier to prevent device damage and contamination to or from the external environment. Containers should remain closed during transport with a latching mechanism and tamper-evident seals. All transport carriwers should be clearly labeled with the processing status to identify whether the items are clean, sterile or contaminated. They should also clearly identify what is contained, from where the contents originated, and to where they are being transported, as well as the date and time.
Protective packaging can be used to maintain the integrity of a sterile package. TIR109 provides guidance about when and how to utilize protective packaging. Transport carts are another mode used for external transport, and each cart should have a unique identifier that allows for traceability to maintenance records. Recommendations for the types of carts are provided in TIR109. The cart should be able to move smoothly,

"From packaging to vehicle standards, every detail matters when devices travel beyond facility walls."
with little vibration and shock. Regular maintenance on the wheels should be performed to ensure they turn, function and lock properly.
Ergonomics are another important consideration. The handle height should be considered to prevent user strain, and the cart’s maximum gross load should always be followed. The TIR also provides guidance for proper cart cleaning.
Even though transport vehicles are not typically managed by the sterile processing department, TIR109 does include recommendations pertaining to the transport vehicle. The vehicles should be safe and reliable and comply with federal, state and local regulations. It is important to minimize shock and vibration that can damage devices or packaging. The area used to transport items is referred to as the cargo space; this is an enclosed area within the vehicle.
TIR109 features requirements for the cargo space that includes protecting the cargo from significant changes in temperature and humidity. The document includes environmental and cleaning considerations for the transport vehicle.
Personnel performing the transport should have training and education. The TIR provides a list of topics that should be included in the training and recommends having policies for any related special licenses and other driving requirements. If an outside transport company is used, the healthcare facility should have a process in place to regularly evaluate their compliance with regulations. Should a healthcare facility require information about monitoring the external transport condition, TIR109 features an annex with monitoring information. An annex on packaging considerations for transport carriers is also provided and describes how to protect the packaging integrity and contents from damage.
Maintaining the integrity of processed items and following safety precautions for contaminated items is a fundamental practice of sterile processing. TIR109:2025 External transport of medical devices processed by health care facilities provides valuable information to help ensure items are transported safely and in compliance with regulations. This article provides a high-level summary of the guidance in TIR109. The full document can be purchased at https://array.aami.org/ doi/10.2345/9781570209048.ch1 or by scanning the QR code.

By James X. Stobinski, Ph.D, RN, CNOR, CSSM(E), CNAMB(E)
A recent conversation with a colleague at NIFA prompted me to explore the topic of the consistency of perioperative nursing care. This nurse works as a surgical assistant and participates in a high volume of cases with a diverse selection of perioperative nurses and his opinion carries weight. This made me consider this issue from the quality improvement lens. My thoughts turned to a straightforward question –How do we assess the quality of perioperative nursing care?
One measure of the quality of care is whether all the appropriate care happened in a case. From a quality assurance perspective this is the sort of thing we measure in routine audits. Putting on my research hat, I began a quick scan of the literature and came to very recent work on the topic of missed nursing care to include perioperative nursing specific articles.
The topic of Missed Nursing Care (MNC) fits well within the framework of Avedis Donabedian’s work on healthcare quality.¹ Donabedian’s Structure-ProcessOutcomes Model has held up remarkably well over time and is useful in examining this topic. From that perspective it would be easy enough to audit the process of nursing care, document the omissions and then address those aspects. I would argue that the complex reasons nursing care is missed exceeds that simplistic view. A broader, more nuanced look is needed and that will also bring us to an examination of the structure that supports nursing care.
Missed nursing care can be viewed from a large picture nursing perspective. There is an excellent, recent systematic review and metaanalysis on this topic by Gong and colleagues.¹ These researchers tell us that MNC, “… refers to any aspect of essential patient care that is omitted or delayed” and that this “…presents substantial risks to patient safety and the quality
of care.”¹ In their review they state that, “The raw prevalence of missed care ranged from 6.8% to 98.1% …”¹ By any measure that is a significant portion of missed care which clearly could have a negative impact on patient outcomes. Among the reasons for missed care include unexpected increases in patient census, inadequate staffing and urgent patient care issues.¹
More relevant to my recent discussions is the MNC found in perioperative nursing. I am pleased to note the very recent work of the prolific Australian perioperative nurse researcher Dr. Brigid Gillespie. Gillespie, and her fellow researchers Harbeck and Chaboyer, report perioperative specific results using the MISSCARE Survey-Operating Room and correlated these results to selfreported rating of perioperative nursing competency as measured with the Perceived Perioperative Competence Scale-Short Form (PPCS-SF).³ , 4 They reported that, “participants’ age directly predicted the frequency of missed care,
nurse role satisfaction, perceived perioperative competence, and reasons for missed care.” The reasons given for missed perioperative care included, “team communications and interruptions, limited resources, and … inadequate skill mix and staffing.”³ The theoretical model outlined by these authors predicted 22.6% of the frequency of missed care.
A modern operating room is a complex, technology-intensive environment with an emphasis on efficiency. Operating margins have tightened in recent years, placing even more pressure on nursing staff. Many experienced perioperative nurses left the profession in the pandemic. That lost expertise coupled with increasing time pressures and the continual onslaught of technological innovation may contribute to missed care. This research can inform further study
on the how and why of missed perioperative nursing care. Future research may give us actionable items for perioperative leaders to close these shortfalls in care. Donabedian’s framework and the exemplary work of these Australian nurses outline a potential research trajectory.

– James X. Stobinski, Ph.D., RN, CNOR, CSSM(E), CNAMB(E), is the director of hospital and ASC relationships with National Institute of First Assisting (NIFA). He is also a member of the Central Michigan University faculty.
References
1.Donabedian, A. (1966). Evaluating the Quality of Medical Care. The Milbank



Memorial Fund Quarterly, 44(3), 166–206. https://doi. org/10.2307/3348969
2.Gong, F., Mei, Y., Wu, M., & Tang, C. (2025). Global reasons for missed nursing care: a systematic review and metaanalysis. International Nursing Review, 72(1), e13096. https:// doi.org/10.1111/inr.13096
3.Gillespie, B.M., Harbeck, E., & Chaboyer, W. (2023). The Association between Operating Room Nurses’ Characteristics, Competence, and Missed Nursing Care: A National Survey. Journal of Nursing Management.
4.Gillespie, B. M., Harbeck, E., & Chaboyer, W. (2025). The frequency and reasons for missed nursing care in Australian perioperative nurses: A national survey. Journal of Clinical Nursing, 34(3), 883–893. https:// doi.org/10.1111/jocn.17082



Join perioperative professionals throughout the Southeast for CE-accredited education, exhibits with leading vendors, and great networking events at the 2025 Southeast Councils of periOperative Nurses, powered by OR Today. Registration is now open for the November 1-2 conference in sunny St. Augustine, Florida. Visit the website at southeastperiop.com.
The event is proudly supported by North Carolina, South Carolina, Tennessee, Georgia and Florida Councils of periOperative Registered Nurses offers up to 10 CEUs.
The 2025 theme is "The Power of You: Circles of Care.” It highlights individuals who have embraced their purpose and made a meaningful impact on the world. Through powerful presentations, speakers will showcase how everyday actions, thoughts, and values contribute to sustaining a purposeful life and driving collective progress at personal, local, national, and global levels. What better way to inspire the next generation than by honoring those who lead with purpose?
Along with educational sessions, the conference offers an opening keynote, a Lunch & Learn event, an exhibit hall brunch, Daisy Foundation Awards presentation and a closing keynote. The conference also accepts poster submissions.
Brenda C. Ulmer MN, RN, CNOR, FAORN, Perioperative Nurse Educator, encourages perioperative nurses to attend.
“Based on feedback from last year, attendees can expect a well-planned conference with attention to details that enhance the attendee experience,” Ulmer said. “Coming out of the pandemic in 2021, Georgia Council realized we needed help to restart our statewide perioperative meetings. We were also in the midst of seeking surgical smoke legislation in Georgia, so a well-run and organized conference was necessary. We had worked with Kristin Leavoy and OR Today in the past, and knew she produced the quality we wanted and needed. The partnership in 2021 was very successful, maximizing the strengths of people within the partnership.”
Ulmer said is ready to network and share ideas at the conference.
“Witnessing, again, the synergy of our regional perioperative nurses and industry partners in an informative
and educational format that ultimately improves evidencebased perioperative nursing,” is what Ulmer said she is looking forward to at the conference.
“Blending together the number of national perioperative leaders we have in the southeast with a greater concentration of attendees from our region accomplishes two outcomes,” Ulmer said. “One, the conference gives the national leaders a chance to interact with local perioperative professionals. That is extremely important because the local level is where all important healthcare takes place. Two, the conference gives local and regional perioperative nurses up close and personal interaction with their colleagues who are already national leaders, creating an opportunity to make connections and communicate with people who serve as role models. This interaction creates a synergy that is beneficial for both.”
Early-bird Registration is $99 (valid until 9/1/25) and includes:
• All education and exhibit hall admission
• Continental Breakfast on Saturday, Nov. 1
• Lunch & Learn on Saturday, Nov. 1
• Exhibit Hall Reception on Saturday, Nov. 1
• Exhibit Hall Brunch on Sunday, Nov. 2
After September 1, registration is $125. It is $150 to register at the event.
Find all the details and register today at southeastperiop.com or scan the QR code below.




OR Today is proud to have AORN Connecticut Chapter 0701’s support for the 2025 Periop ConneCT conference. The event will be held October 11-12, at the Omni New Haven Hotel at Yale in New Haven, Connecticut. Join perioperative professionals throughout Connecticut and the Northeast for CE-accredited education, exhibits with leading vendors, and great networking events.
Learning Objectives for the Conference include:
• Advance Clinical Excellence and Innovation: Offer CE-accredited education sessions covering the latest advancements in perioperative care, such as implicit bias awareness, minimally invasive surgeries, and progressive pain management strategies. This ensures participants gain cutting-edge knowledge and skills to enhance patient care.
• Foster Professional Networking and Collaboration: Create a platform for perioperative professionals to network, share best practices, and collaborate with peers and leading vendors through exhibits and interactive sessions. This aims to build a strong professional community and encourage collaboration across the Northeast.
• Promote Leadership and Career Development: Provide workshops and presentations focused on leadership, advocacy, and professional growth, such as sessions on workplace violence prevention, navigating incivility, and career development strategies. This will empower attendees to take on leadership roles and drive positive change in their workplaces.
The 2024 Periop ConneCT conference was a major success and 2025 looks to build on that momentum.
“I enjoyed everything about the event,” said Elaine McDunnah, RN staff, retired Midstate Medical Center. “This was a wonderful experience and I look forward to next year.”
Surgical Services Hartford Healthcare at Charlotte Hungerford Nurse Manager Kathryn Grant found the educational sessions beneficial last year.
“I enjoyed ‘This is the way I have always done it.’ It is a chronic issue across health care I also enjoyed ‘A Strap goes a long way.’ Safety is paramount,” Grant said.
“The program had offerings that all of the specialties could benefit from,” said Jeanne Ring, MSN, RN, CNOR, professional development coordinator with Bristol Hospital “All of the programs were excellent.”
“The educational sessions were all engaging and informative and the perfect length of time,” said Yale New Haven Hospital Surgical Technology Program Coordinator Angel Pickett.
“It was really nice to network and see other healthcare professionals that I haven’t seen in some time,” Pickett added.
“Overall, the sessions were good, informative and had the audience engaged,” said St. Francis Hospital Certified Surgical Technologist Kimberly Rojas.
Yale New Haven Hospital’s Marie Tammaro, RN, described the educational session. “They were informative, and the speakers were highly educated in their content.”
“I enjoyed the conference,” she added.
Find out more and sign up for the Periop ConneCT newsletter at PeriopConneCT.com or scan the QR code.
FUJIFILM Healthcare Americas Corporation, a leading provider of endoscopic imaging and endosurgical solutions, announced that its EN-840T Double Balloon Enteroscopy (DBE) Scope, an endoscopic imaging technology that enables access to the entire small intestine for diagnosis and therapeutic intervention, has been selected as the winner of the “Best New Endoscopy Technology Solution” award in the 9th annual MedTech Breakthrough Awards program. MedTech Breakthrough is an independent market intelligence organization that recognizes the top companies, technologies and products in the global digital health and medical technology market.
The EN-840T DBE scope represents a major update to Fujifilm’s pioneering Double Balloon Enteroscopy technology. The EN-840T DBE scope features several compelling features, including its ability to allow for blood or mucus to be aspirated while a therapeutic device is inserted, enabling quicker hemostasis. The scope also provides a dedicated forward water jet channel for irrigation and enables clinicians to quickly clear debris like blood on the mucous membranes for clearer visualization of the bowel wall.

“As a company with a history of “firsts” in the endoscopy field, we’re honored to be recognized by MedTech Breakthrough for our ergonomically designed EN-840T DBE scope,” said Tai Fujita, general manager of endoscopy and vice president, FUJIFILM Healthcare Americas Corporation. “Approximately 2.39 million Americans have Inflammatory Bowel Disease (IBD), which includes Crohn’s disease and ulcerative colitis.
Left undiagnosed and untreated, these diseases can lead to serious complications. We’re proud to offer clinicians a tool that will help them access difficult to reach pathways within the digestive tract, enabling them to more effectively diagnose and treat a wide array of small intestine diseases, gastrointestinal bleeding, and removal of small bowel polyps.”
A CMOS (Complementary Metal-Oxide-
Semiconductor) image sensor in the EN-840T DBE scope ensures vivid, HD, high-quality images, providing speed and clarity for diagnosis. The scope also leverages LED multi-light technology along with Fujifilm’s Linked Color Imaging (LCI) and Blue Light Imaging (BLI) modes to provide endoscopists with enhanced visualization and enable optimal detection during small bowel procedures.
The EN-840T DBE scope also provides adaptive bending and advanced force transmission technology for improved access and scope maneuverability in challenging anatomy.
The MedTech Breakthrough Awards program celebrates excellence and innovation in the health and medical technology industry, recognizing the companies, products, and solutions driving meaningful progress and improving patient care. This year’s program attracted more than 4,500 nominations from over 18 different countries throughout the world.
Cleveland Clinic has announced a partnership with Regent Surgical to develop ambulatory surgery centers that enhance access, streamline care delivery, and provide support for physicians and care teams.
“Ambulatory surgery centers provide an important setting for health systems to expand access to surgeries, and to be more efficient in the delivery of services,” said Cleveland Clinic CEO and President Tom Mihaljevic, M.D., holder of the Morton L. Mandel CEO Chair. “Regent’s capabilities in managing and operating ambulatory surgery centers will enable us to focus on continuing to provide the highest quality care for our patients and will enhance our ability to grow and offer that care to more patients.”
Ambulatory surgery centers offer an alternative to traditional hospital-based care. Surgeries performed at ASCs require patients to only spend a short amount of time recovering at the center, after which they return home to complete their recovery. ASCs offer convenient access for patients who need surgical care.
Regent works with health systems to develop, manage and operate surgery center partnerships with a focus on increasing access to high-quality care. Cleveland Clinic and Regent
will work together to develop future ASC locations in U.S. markets. Cleveland Clinic is the majority owner of the joint venture and will have branding on all ASCs.

“We’re proud to partner with Cleveland Clinic to deliver long-term value for patients, physicians, and the communities they serve,” said Travis Messina, chief executive officer of Regent. “Together, we will create accessible, patient-centered surgical environments that emphasize both clinical excellence and compassionate care.”
Founded in 2001, Regent Surgical has established itself as a leader in outpatient care delivery. The company operates and manages ASC locations in partnership with leading health systems across 13 states, focusing on enhancing care quality, improving patient experience, and driving operational excellence.

Vicarious Surgical Inc. has signed an agreement with UMass Memorial Medical Center intended to support adoption and utilization of its robotic system through enhanced perioperative practices, surgeon education and other engagement strategies.
UMass Memorial Medical Center, the flagship academic medical center of UMass Memorial Health, is the largest notfor-profit hospital in Central Massachusetts with 826 licensed beds and the clinical partner of the University of Massachusetts Chan Medical School. UMass Memorial Health is committed to providing advanced medical care to residents across the region.
The collaboration will focus on strategic operational efforts including streamlining inventory management and sterilization protocols and the standardization of pre-procedure processes and post-procedure care. It will also include case observation for surgeons and Vicarious Surgical system testing. Additionally, the collaboration will include efforts such as sharing insights on research developments, peer-to-peer education and promoting best practices.
“We’re excited to work with UMass Memorial Medical

Center to drive excellence in the application of our robotic technology,” said Adam Sachs, CEO and co-founder of Vicarious Surgical. “This collaboration will allow us to develop and implement optimized perioperative workflows and initiatives that are critical for successful adoption and utilization of our system. UMass Memorial’s regional leadership and commitment to advancing surgical care make them an ideal partner.”
“As an organization dedicated to educating and mentoring the next generation of health care professionals, we are continually seeking ways to improve surgical outcomes and care delivery,” said Dr. John Kelly, Chief of General and Minimally Invasive Surgery at UMass Memorial Medical Center. “Our work with Vicarious Surgical will allow us to explore the potential of this technology with an ultimate goal of improving patient care.”
Vicarious Surgical will collaborate directly with the UMass Memorial Medical Center team of experienced robotic surgeons and supporting staff, leveraging their expertise to refine and validate best practices in the identified focus areas.



The Wound Care Collaborative Community (WCCC) is leading a groundbreaking initiative looking to develop a standardised preclinical testing framework for wound dressings. This collaboration involves clinicians, materials management and procurement teams, regulators, and industry experts, aiming to enhance patient care through clinically relevant and consistent evaluations.
Mölnlycke Health Care has been a steadfast supporter of the WCCC from the start, working alongside other major wound care players on the project to improve patient outcomes.
In a recent publication in the Wounds journal, the WCCC calls for a new era of wound dressing standards rooted in clinical relevance, biological validity, and consistency across product development and evaluation.
Standardized, meaningful testing is not just about better comparisons – it is about fostering innovation. A clear, testing framework that is shared by all stakeholders:
• Helps clinicians make better-informed decisions based on consistent, evidence-based product evaluations, recognised by various stakeholders
• Progresses industry design and drives refinement of products with real-world performance in mind
• Helps researchers and regulators agree on functional dressing properties that align with clinical needs and ensure that preclinical testing appropriately reflects these needs
Dr. Sarah Griffiths Langbord, chair of the WCCC Gaps Dressing Standards Work Group, explains that the initiative has developed from an imminent need for standardization. “Wound dressings are currently evaluated using various test methods, many of which are incompletely specified or insufficiently relevant to real-world wound care scenarios. This has resulted in individualised modifications by test users with no established best practices and no consistent baseline set of standardised tests for pre-clinical evaluations.”
The WCCC urges the wound care community to get involved, as they need feedback from a wide range of stakeholders including clinicians, materials management and procurement teams, regulators, and industry experts. By identifying gaps in current standards, the WCCC can drive innovation in wound dressing development, shape research priorities, and highlight external funding opportunities to support pre-clinical research.
Stakeholders can help the WCCC by taking a survey here: https://bit.ly/4cN7sIZ





soma@somatechnology.com (800) 438-7662
somatechnology.com @Somatechintl

The 2025 AORN Global Surgical Conference & Expo, held from April 5-8 in Boston, Massachusetts, brought together perioperative professionals from around the world for four days of education, innovation, and networking. Hosted by the Association of periOperative Registered Nurses (AORN), the event focused on advancing surgical care and fostering professional growth.
Conference highlights included cutting-edge clinical education sessions and a leadership summit. Attendees had access to more than 60 continuing education contact hours through sessions, posters, and hands-on activities. The conference also offered specialized tracks.
Attendees engaged in sessions covering the latest in robotic-assisted surgery, infection prevention, and minimally invasive techniques. The conference emphasized evidence-based practices and emerging technologies shaping the future of perioperative care.
The Leadership Summit featured keynote speaker Mike Lee, a renowned leadership coach, who inspired attendees to reach new heights in perioperative care. The summit provided strategies to build high-performing teams and navigate complex healthcare challenges.
The conference showcased international perspectives, with presentations representing countries such as Nigeria, Sweden, Australia, and Portugal. Notably, Johnson & Johnson hosted a Chinese nursing delegation, and nurses from Japan participated, highlighting the event's global reach.
The expo floor buzzed with activity as attendees explored the latest surgical technologies and connected with industry leaders. Interactive workshops and handson labs allowed participants to apply new techniques and tools directly relevant to their practice. Networking events included evening parties, volunteer activities, mentor programs, and speed networking sessions, fostering connections among perioperative professionals.
Attendees took to LinkedIn to share praise for the AORN Global Surgical Conference & Expo.
Cassie Scott, a perioperative charge nurse manager, expressed her enthusiasm: “This week’s AORN Global Surgical Conference and Expo in Boston was an amazing experience. This was not just attending a conference, this is being part of a community where like-minded people share the same passion and enthusiasm and strive to continuously

learn, improve practices, adopt new technologies, and enhance patient care.”
Melissa Vibberts, MPS, director of brand management at Beekley Medical, shared: “AORN is one of my favorite conferences to attend, I am so happy that our leadership team was there to experience the energy firsthand!”
Marisa Hamamoto, a keynote speaker and founder of Infinite Flow Dance, shared her experience: “What an honor to be a keynote speaker at AORN Global Surgical Conference and Expo 2025. Thank you to the 3500 nurses in the audience for sharing time and space with me.”
The AORN LinkedIn account expressed gratitude: “What an incredible success! AORN Global Surgical Conference & Expo 2025 wouldn't have been possible without the passion, energy, and dedication of our amazing perioperative nurses and the entire periop community.”
David Wyatt, Ph.D., RN, NEA-BC, CNOR, FAORN, FAAN, CEO and executive director at AORN, added: “Thank you to everyone who brought their dedication and enthusiasm for perioperative care to #AORN2025! From the packed sessions to powerful keynotes, hands-on learning to heartfelt connections, this is what Together We Rise looks like.”
Mark your calendars for the next AORN Global Surgical Conference & Expo, scheduled for April 11-14, 2026, in New Orleans, Louisiana. Building on the success of the 2025 conference, the upcoming event promises to deliver another enriching experience for perioperative professionals worldwide.
A new virtual training course designed to equip operating room personnel and healthcare professionals with critical laser safety knowledge is launching this fall. The Medical Laser Safety Officer (MLSO) Course will be held online September 27-28, 2025, and is open for registration at medicallasersafety.com.
As laser technology continues to revolutionize surgical and clinical care, the risks associated with its use demand strict safety protocols. This comprehensive two-day course is approved by the Board of Laser Safety (BLS) and fulfills the training prerequisite to sit for the Certified Medical Laser Safety Officer Exam.
Course Overview
Led by nationally recognized experts Vangie Dennis, MSN, RN, CNOR, CMLSO, FAORN, and Patti Owens, BSN, MHA, RN, CNOR, CMLSO, the MLSO course delivers in-depth instruction on laser biophysics, tissue interaction, and safety management. Attendees will explore multi-wavelength laser technologies and review standards from ANSI Z136.3-2024, the AORN Laser Safety Guidelines (2020), and CSA Z7001:24.
Participants will gain the tools to:
• Understand laser-tissue interactions and classifications
• Assess and control laser-associated hazards
• Develop and evaluate laser safety programs
• Navigate compliance with regulatory bodies including TJC, CMS, OSHA, AAAHC, and QUAD A
• Address safety in surgical, dental, dermatological, and ophthalmological settings
Who Should Attend

The course is designed for perioperative nurses, surgical technologists, radiation safety officers, biomedical engineers, dental personnel and laser safety officers (LSOs).
Course Details
• Dates: September 27-28, 2025
• Format: Live Virtual Training
• Cost: $795
• Early Bird Registration: $695.00
• Registration: www.medicallasersafety.com
Why It Matters
Having a certified Medical Laser Safety Officer is not optional –it’s essential. Without proper oversight, healthcare facilities risk regulatory violations, patient harm, and compromised staff safety. This course arms attendees with the knowledge and certification path necessary to manage these risks effectively.
For additional details about the course or to register, visit www. medicallasersafety.com.
Learn more about the Certified MLSO exam at www.lasersafety.org.
Join perioperative professionals throughout the Southeast for CE-accredited education, exhibits

Global Markets Insights reports that the patient temperature management market size was valued at $3.4 billion in 2023 and is estimated to grow at 5.6% CAGR from 2024 to 2032.
Allied Market Research published a report that states that the patient temperature management market was valued at $3.1 billion in 2023, and is estimated to reach $6.5 billion by 2035, growing at a CAGR of 6.3% from 2024 to 2035.
The growth of the patient temperature management market is driven by an increase in the number of surgical procedures, rise in government initiatives for patient temperature management, and advancements in technology. However, the high cost of patient temperature management devices is a significant restraining factor for the growth of the patient temperature management market. On the other hand, high growth potential in emerging countries provides lucrative opportunities for market growth.
By product, the system segment held the largest market share in 2023, accounting for more than four-fifths of the patient temperature management market. The same segment is expected to register the highest CAGR of 6.4% during the forecast period. This is attributed to an increase in demand for advanced temperature regulation solutions. Technological advancements
in automated systems enhance efficiency and patient safety. Rising surgical procedures and critical care needs further drive segment growth.
By application, the operations segment held the largest market share in 2023, accounting for more than two-fifths of the patient temperature management market owing to rise in the number of surgical procedures requiring precise temperature control. The increase in the adoption of advanced temperature management systems in operating rooms further supports segment growth.
However, the infants and pediatric segment is expected to witness the fastest CAGR of 6.9% from 2024 to 2035 owing to increase in neonatal and pediatric surgeries requiring precise temperature regulation. Rising awareness of temperature management in neonatal intensive care units (NICUs) further supports market expansion.
By end user, the hospitals segment held the largest market share in 2023, accounting for more than half of the patient temperature management market owing to the high volume of surgeries and critical care procedures performed in hospitals, which require advanced temperature regulation. The growing adoption of temperature management systems in hospital settings to ensure patient safety and optimal outcomes also contributes to this dominance.
However, the neonatal intensive care unit segment is expected to witness the fastest CAGR of 6.8% from 2024 to
2035 owing to increase in the number of premature births and the need for precise temperature management in neonatal care. Advancements in technology and rise in focus on improving neonatal outcomes further contribute to the demand for specialized temperature regulation in NICUs.
Region-wise, North America held the largest market share in 2023, accounting for more than two-fifths of the patient temperature management market due to the high prevalence of chronic diseases and surgeries requiring temperature management, along with the region’s advanced healthcare infrastructure. In addition, the growing adoption of technologically advanced temperature regulation systems and increasing healthcare expenditure in North America further fuel market growth. The presence of key market players and ongoing research and development also contribute to the region’s leading position.
However, Asia-Pacific is expected to witness the fastest CAGR of 7.3% from 2024 to 2035 owing to increase in demand for advanced healthcare solutions due to a rising population and improving healthcare infrastructure. In addition, growing awareness of temperature management in critical care settings and an expanding number of surgeries and neonatal care facilities in the region contribute to the market’s rapid expansion.
In today’s demanding surgical landscape, healthcare teams need every tool working in their favor. Maintaining normothermia is not only a clinical priority – it’s a critical strategy in reducing the risk of surgical site infections (SSIs). That’s where Thermoflect steps in. Thermoflect products are engineered to make patient warming simple, safe and effective. From the moment of application, they begin retaining body heat to help prevent redistribution temperature drop (RTD), a common but preventable complication during surgery. Unlike traditional warming systems, Thermoflect relies on advanced heat-reflective science, not electricity. The result? A reliable, cost-effective, and energy-efficient solution that supports both clinical outcomes and operational efficiency.


In today’s demanding surgical landscape, healthcare teams need every tool working in their favor. Maintaining normothermia is not only a clinical priority – it’s a critical strategy in reducing the risk of surgical site infections (SSIs). That’s where Thermoflect steps in. Thermoflect products are engineered to make patient warming simple, safe and effective. From the moment of application, they begin retaining body heat to help prevent redistribution temperature drop (RTD), a common but preventable complication during surgery. Unlike traditional warming systems, Thermoflect relies on advanced heatreflective science, not electricity. The result? A reliable, cost-effective, and energy-efficient solution that supports both clinical outcomes and operational efficiency.
The IQool Advanced Surface System manages and maintains patient temperature for warming or cooling applications or to maintain normothermia. Designed with intelligence to accurately and rapidly reach target temperature, the IQool System offers 3 separate zones of treatment via torso, thigh and the optional head/neck pads. Their non-adhesive, advanced pads with crush resistant delivery channels enable simple, quick skin-checks for optimal patient care. The silicone pads last the duration of care preventing replacement disposable needs and can be wiped clean when soiled. With minimal service requirements, the system utilizes a bacteriostatic coolant which inhibits bacterial growth simplifying maintenance. Institutional temperature protocols can be programmed into the console for intuitive set-up and therapy initiation. Data captured from the case can be easily downloaded for insightful reviews of system and patient performance during therapy. The IQool System provides simplified temperature control with built-in intelligence for adult patients.
The established efficiency of the HotDog Patient Warming System is now enhanced by the Warming Mattress + Return Electrode. This integrated system combines electrosurgical grounding with premier underbody warming, promoting intraoperative safety and simplicity. The system uses reusable air-free, conductive heating to ensure uniform temperature distribution, utilizing reusable warming blankets and mattresses controlled by the HotDog Multiport Temperature Management Controller for precise thermal regulation. Distinguished by its environmental and economic benefits, the HotDog Patient Warming System is clinically proven to maintain patient normothermia, setting a higher standard in perioperative care.


The top-rated StaCool Vest Core Body Cooling System keeps surgical teams cool, comfortable, and completely mobile, allowing them to focus completely on the task at hand during long procedures. Despite elevated ambient temperatures due to multiple layers of sterile medical garb, the StaCool Vest maintains a consistent, comfortable core body temperature thanks to ThermoPaks in the front and back, which provide hours of cooling relief. With no hoses or bulky coolers, this unique design is self-contained, so wearers can move about as desired. Micro-thin, highly breathable materials are easy to care for, providing wearers with unsurpassed cooling comfort without compromising mobility. A thermal barrier is built in to ensure the wearer does not get too cold. Available in unisex sizes from xx-small to xxx-large, StaCool Industrial Vests are fully adjustable to suit all body types and sizes. A spare set of ThermoPaks are included with each vest to extend cooling time and comfort. Optional monogramming is available to personalize vests.
SurgiSLUSH fully automated, set and forget freezers with sealed, portable containers keep sterile slush safely protected until dispensed for use, rather than exposed to ambient for hours. Fully automated freezers with sealed, portable containers enable multi-room, multi-case supply, which maximizes capital budget value. Great technology delivers great economics. This modern sterile slush system addresses two critical issues experienced by users of traditional open-basin slush units: extended ambient exposure before slush use and difficult-to-detect sterile barrier failures. Humans cannot see through inches of ice. “Sealed slush provides hours of protection for each patient and enables visual confirmation of sterile barrier integrity before every use,” says Patrick Kammer, C Change Surgical’s CEO. “A new time/motion study white paper measured the average time of unprotected ambient exposure with open-basin slush units in 47 cases. The authors found average ambient



exposure to be just minutes under three hours. This exposure occurs before slush is even put to use.” Efficient set and forget technology by SurgiSLUSH makes, maintains and protects expert-quality sterile slush. Users erase distracting sterile field labor during complex cases. SurgiSLUSH delivers sealed sterile protection, streamlined workflow, and portable, multi-room supply.
By Don Sadler


The nursing shortage in the U.S. has been welldocumented. The Bureau of Labor Statistics projects nearly 200,000 nurse openings annually through 2030, while one million nurses are projected to retire by this date.
Nurse staffing challenges are especially acute in operating rooms. This is because of a number of factors including the highly technical requirements of perioperative nursing and the lack of exposure to the specialty in nursing schools. All of this makes it critical for the industry to lead and inspire the next generation of perioperative nurses.
David Reinhart, DNP, MBA, RN, CNOR, FAAN, director of education, EHC, Perioperative Services Enterprise with Emory Healthcare in Atlanta, Georgia, teaches Periop 101, the Association of periOperative Registered Nurse’s (AORN) comprehensive training program for OR nurses.
“Undergraduate nursing programs continue to lack perioperative nursing curriculum,” says Reinhart. “Therefore, I believe that healthcare organizations will continue to have challenges recruiting and retaining nurses to work in perioperative services.”
“It’s more important now than ever to prepare the next generation of OR nurses as the surgical environment becomes more demanding and experienced nurses retire,” says Michael Rempel, DNP, RN, CNOR, pediatric trauma program manager in the trauma service at University Hospital in Newark, New Jersey. “Early exposure to the OR helps spark real interest, builds confidence and shows students what working in this specialty truly involves.”
Dawn Whiteside, DNP, MSN-Ed, RN, CNOR, NPD-BC, RNFA, director of education and professional development with the Competency and Credentialing Institute (CCI), agrees.
“The shortage of staff in the perioperative specialty is significant. There
is a high number of nurses in leadership roles who will be retiring very soon, leaving a large vacancy that may not be addressed through succession planning,” she says. “To fill this gap, we must collaborate with hospitals and academia to offer exposure to our specialty during pre-licensure training.”
The nurses at CCI have collaborated with Edgewood College to offer perioperative training electives for students in their fourth or fifth semesters, says Whiteside. The courses consist of fundamental and advanced pre-licensure perioperative services training.
“By the end of the second course, the students have demonstrated levels of competency for the different perioperative standards of practice,” says Whiteside. “Right now, one hundred percent of our students who decide OR is their specialty are getting hired as soon as they graduate.”
Since 2021, when the perioperative training electives were first offered, 50 nursing students have completed the foundational course and seven have completed the advanced course.
“Eighteen students chose periop as their specialty after graduation and they were all hired to the OR of their choice,” says Whiteside.
Amanda Heitman, BSN, RN, CNOR, perioperative educational consultant and owner of Periop Anew, believes that having enough preceptors and mentors is one of the biggest challenges to preparing the next generation of OR nurses.
“We are in a constant cycle of orienting,” she says. “It’s hard to share your knowledge day after day and then see those you have worked to develop leave because they didn’t know what to expect before they started, or they didn’t have the right foundation to sustain them.”
Heitman stresses that any nurse can serve as a mentor, regardless of their level of experience.
“You don’t have to be in the OR for 10 years or more to be a mentor,” she says. “You just need to be there when other nurses are struggling or want to share their
accomplishments. Mentoring doesn’t have to be difficult – just offer to have coffee with someone and talk about their day.”
Whiteside calls mentoring “a huge responsibility that is essential to supporting the next generation of OR nurses. Mentors must be supportive and have the interpersonal skills to establish long-term relationships.”
“Experienced nurses can support new nurses and students by having a positive attitude, introducing them to the team and asking questions to understand their level of competence,” says Whiteside. “My first mentor was the director of perioperative services at my first job after nursing school. We still keep in contact, and I think of her every time the topic of mentorship comes up.”
Rempel believes that mentors are essential for preparing the next generation of OR nurses by providing guidance, support and hands-on experience that can’t always be taught in the classroom.
“However, with the growing shortage of experienced nurses, it’s crucial for hospitals to identify, train and develop nurses into mentors through structured programs. Without proper training, even the most dedicated nurses may experience burnout from the added responsibility of mentoring,” says Rempel. “By prioritizing mentor development, hospitals can strengthen their workforce, improve retention and ensure that the next generation of nurses is well-prepared.”
Rempel recommends that hospitals create structured mentoring programs and combine them with nurse residency programs that pair seasoned veterans with new nurses.
“This will build their confidence, teach them critical skills and help them adapt to the fast-paced OR environment,” he says.
“Front-line nurse leaders play a key role in this process, not only guiding new nurses but also bridging the gap between nursing education and practice.”
Rempel leads the AORN perioperative academic mentoring partnership program that pairs experienced nurse mentors with new nurses to help them transition from the classroom to practical training.
“This program helps new perioperative

nurses apply theoretical concepts to realworld practice,” he says.
Early in his career, Rempel mentored a new graduate RN through the AORN mentorship program.
“The AORN program provides a great structure for mentorship by allowing me to offer consistent support and advice,” he says. “We discussed everything from clinical skills to navigating the complexities of OR culture. Being part of the AORN program was a deeply fulfilling experience and reinforced how mentorship helps both the new nurse and the mentor grow.”
To become a mentor to young OR nurses, Rempel urges experienced nurses to share personal experiences that highlight the unique aspects of perioperative nursing and show their passion by discussing what makes this specialty so rewarding.
“Recognize their accomplishments and provide ongoing encouragement and constructive feedback while also acknowledging the challenges new nurses face and reflecting on what they need to continue to build on,” he says.
At Hartford HealthCare in Hartford,
Connecticut, perioperative nursing students are placed in OR rotations, capstones and observation days.
“The OR educator plays a key role in ensuring that students are prepared for their time in the operating room and OR personnel are supportive when hosting students of differing skill levels,” says Nurse Scientist and OR Educator Jennifer Hehl, Ph.D., RN, CNOR, ONC.
Heitman agrees.
“Whether it is a self-developed course or a program like Periop 101, one key to success is having a dedicated perioperative nurse educator who can guide new OR nurses and support them in every stage of their development,” Heitman says. “To add value to these structured programs, it’s important to allow nurses to experience all the roles within the perioperative setting.”
“For example, I have found that when you allow nurses to learn the scrub role, they find that it helps them be a better circulator because they are aware of what is happening at the field,” adds Heitman.
Hehl calls the OR “the restricted zone.”
“Back in 1996, my nursing school did not support a clinician in the OR,” says Hehl. “Fast forward to my first job in the OR and I was in a foreign world with
some nice people, but many more were unfriendly. I have always wanted to make the OR more accessible to students and friendlier to new RNs.”
“Practice in the perioperative area is unique and unfamiliar for nursing students compared with floor nursing practice,” says Fusae Ogino, MSN, BS, RN, CNOR, RN III, Bone and Joint Institute, Hartford Hospital. “The OR is very limited access, which makes it a mysterious area for nursing students who wonder how nurses practice in the OR.”
As a med-surg clinical instructor, Ogino brings students into the OR for observation.
“They’re always excited to witness surgeries that they learned about in textbooks,” he says. “This is a great experience for understanding different interdisciplinary roles, collaboration, teamwork and different nursing practices from floor nursing.”
“It’s also an excellent opportunity to introduce different nursing specialties to students as career paths they can choose from,” says Ogino. “In fact, some of my students have transferred to OR nursing from med-surg floors due to the observation experience during their clinicals.”
“The OR is a restricted zone – but it shouldn’t be a mystery.”
– Fusae Ogino, MSN, BS, RN, CNOR
Hehl points to several benefits of mentoring students and permitting them in the OR.
“By mentoring students, you realize how much you’re capable of. It also improves teamwork by making precepting a team effort. And having an open, welcoming unit culture is more pleasant for all staff, which improves recruitment and retention,” Hehl says.
Implementing a program that allows students in the OR requires leaders who are willing to host observations and clinical placements.
“You also need to provide regular feedback to the team to build confidence in good outcomes,” says Hehl. “It helps to have involved nurse educators or experienced preceptors to organize and run the program. AORN Toolkits are available to help.”
Rempel believes that teaching young nurses and students how to apply what they learn in the classroom to real-world situations is essential.
“This is especially true in the OR,” he says. “While theory provides the foundation, it’s the hands-on experience that truly helps nurses understand how to put that knowledge into practice.”
To bridge the gap, hospitals and ASCs can partner with local universities to offer courses that help young nurses transition from theory to practice. “Universities provide the theoretical knowledge,

while hospitals give students hands-on experience in the OR,” says Rempel.
Rempel recommends establishing a Dedicated Education Unit (DEU) program in which students work directly with experienced OR nurses in a real clinical setting. “With a strong DEU program, nursing students can receive targeted training and support to help ensure that they are well-prepared to succeed in the OR when they graduate,” he says.
Another way to translate classroom theory to real-world practice is to allow nursing students to work in both the circulator and scrub roles.
“Understanding both roles helps nursing students see the bigger picture and become more adaptable in the OR,” says Rempel.
According to Whiteside, implementation of theory isn’t always tangible in the early stages of training.
“In the program we offer, we make sure to include case studies and build upon them each week,” she says. “Our process is to assign reading related to different theories, provide guidance on this during their clinical day and then create an assignment that will demonstrate key understanding of the theory in application.”
“New theories consistently gravitate around the nursing process and different schools of nursing teach around different theories,” says Reinhart. “Once new nurses are hired, it’s important to train them in strong work ethics that always put patients


first and emphasize being an advocate for patients.”
Whiteside believes it’s critical that current OR nurses are welcoming and encourage new nurses as they learn the perioperative specialty. “New hires can demonstrate an immense amount of excitement and energy,” she says. “But nothing will deflate those feelings like staff that lacks empathy and kindness toward them.”
“The atmosphere must be one of acceptance, education, training and learning to promote mentorship for new nurses coming into our specialty,” says Whiteside.
Heitman stresses the importance of veteran OR nurses unselfishly sharing their knowledge and experience with younger nurses.
“We need to remove the old mindset of ‘eating our young’ and keeping information to ourselves because Dr. Smith can’t do surgery without me,” she says. “The only way to do this is by fostering an atmosphere of continuous learning.”
Continued growth of perioperative nursing will require active recruiting, says Heitman. “The OR is hidden behind the scenes so we need to allow others to observe our environment and what we do – whether this is college, high school or even middle school students or nurses from other areas.”
“Allow them to see a different side of nursing and the amazing opportunities in the perioperative world,” Heitman adds.


We offer cooling vests and accessories to keep all members of the OR staff comfortably cool and focused when the operating room temperature is heated to AORN and Joint Commission recommendations! We have dedicated members of our team that are committed to helping you choose the perfect apparel for your OR room and staff.
The lightweight CoolOR® Circulating Water System keeps surgeons and staff cool and comfortable by continuously circulating cold water through tubing sewn within the vest. The surgical cooling vest system features a safe, water-tight cooling reservoir, quick-connect couplings, insulated water lines, attached wheels and a retractable handle.
Discreet pockets hold your choice of reusable cooling pack technologies. This is a cost-effective option that allows for freedom of movement while providing effective cooling.





UNLIKE OTHER PRODUCTS ON THE MARKET, CoolOR® IS FULLY STOCKED AND READY TO SHIP WITHOUT DELAY.
Are your surgeons feeling the heat in the operating room? Introducing the CoolOR® Circulating Water System, a game-changer in surgical comfort. Here’s why it’s a must-have for your team:
• CONTINUOUS COOLING
• WATER-TIGHT RESERVOIR
• QUICK-CONNECT COUPLINGS
• INSULATED WATER LINES
• PORTABILITY
CHOOSE COOLOR®: Because comfort matters, especially when lives are at stake. Contact us today to explore our high-quality water circulating systems and experience the difference firsthand!

“This role is really where my passion lies and allows me to lead in areas that I am really passionate about –perioperative nursing and services.”

By Don Sadler
If variety is the spice of life, Leigh Ann Bartlett’s nursing career is as hot as a ghost pepper. Leigh Anne’s nursing career began in 1995 on a Progressive Care Unit at the University of North Carolina (UNC) Health Wayne, formerly Wayne Memorial Hospital, in Goldsboro, N.C.
“I worked there for a couple of years on swing shifts,” she recalls, “but when I planned to get married, I realized the schedule didn’t allow for much work-life
balance. So, I applied for a staff nurse position in the operating room. The OR is one of those areas where you either love it or hate it – and I realized pretty quickly that I loved it.”
After several years in the OR, Leigh Anne expanded her scope into nurse case management and discharge planning, focusing on orthopedic and surgical population. In this role, she implemented protocols and best practices, always striving for improvement. “That’s where I began to understand the ‘big picture’ of healthcare,” she explains. “Of course,
we’re here to care for patients, but hospitals are also businesses, and we must be good stewards of our resources.”
In 2006, Leigh Anne returned to East Carolina University to pursue a master’s degree in nursing administration, which she completed in 2009. The following year, she became nurse manager of the surgical joint and replacement unit at Wilson Medical Center. After two years, she transitioned to East Carolina University (ECU) Health Duplin Hospital as director of patient care services, overseeing a wide range
of departments in a rural community hospital in eastern North Carolina. In this role, she led multidisciplinary teams across women’s care, surgical services, and central sterile processing. She also launched an outpatient oncology and infusion clinic and served as program director of the 25bed inpatient behavioral health unit. She, also, served as the chair of the perioperative leadership team for the large healthcare system while she was there. Her team at Duplin received the AORN Go Clear Award under her leadership.
Despite her broad experience, Leigh Anne’s passion has always remained in the operating room and perioperative specialty. Her commitment led her to active involvement in the Association of periOperative Registered Nurses (AORN), where she served as Chapter President of Coastal North Carolina (2015-2016), Council Treasurer (2016-2019), and Council Secretary (2019-2021) along with many other roles at the local and state level. She has also served as the chair of the AORN Leadership Specialty team, and in 2025, she was elected to the national AORN Board of Directors.
“My involvement in AORN has been instrumental in advancing my career,” she says.
Currently, Leigh Anne is the director of surgical services at the University of North Carolina (UNC) Health Johnston, two community hospitals serving Smithfield and Clayton, North Carolina. “This role is really where my passion lies and allows me to lead in areas that I am really passionate about – perioperative nursing and services,” she says.
The most rewarding part of her job is teaching and mentoring other nurses. Leigh Ann served as a system mentor for new nurse leaders at ECU health and graduated from the hospital’s Enriching Leadership Program.
“One of my biggest challenges is knowing when to let go because we’re very lean,” she says. “Work-life balance is important for everyone so as nurses we need to know when to step away so our jobs don’t completely consume us and take up too much family time.”
One of the highlights of Leigh Ann’s
career was when ECU Health Duplin Hospital received the AORN Go Clear Smoke Evacuation Award (Gold Level) in 2020. She’s currently involved with the North Carolina National Legislative Forum, helping get smoke evacuation legislation passed in the state.
“The bill unanimously passed the House and is headed to the Senate, so hopefully it will be signed into law this year,” she says.
Looking ahead, Leigh Ann is excited about the potential of artificial intelligence to help deliver better care for surgical patients.
“I’m hoping it will enable us to pull away from the computer a little more and focus more on our patients,” she says. “But we’re going to have to be very strategic about how AI is used from a legal standpoint to make sure we’re all protected and that all team members trust it. Nurses need to understand that AI isn’t there for a punitive reason – it’s there to uncover opportunities for us to grow and improve patient safety.”
Leigh Ann expects perioperative nursing to continue to evolve and change in the future, especially with advancements in robotics and minimally invasive surgery.
“How much more will we be moving to an outpatient setting and what will this look like?” she asks. “We’re going to have to remain strategic about this because the outpatient setting isn’t always optimal. There’s a time and place for both settings and hospitals can learn from outpatient facilities when it comes to providing more efficient patient care.”
Outside of her formal job duties, Leigh Anne has served in her community as a volunteer nurse for the mobile medical unit ERT team at The Bridge Church, where she and her family worship. She is also a 10year member of The Bridge Church’s American Kentucky Mission Team.
Her family loves to camp along the East Coast, sometimes bringing their two dogs: an English bulldog and a Maltipoo. And Leigh Ann’s daughter Paige is pursuing a nursing career.
“She’s very interested in perioperative and possibly pursuing a career as a nurse anesthetist, so I’m really excited about this,” says Leigh Ann.





An international team of researchers at the University of Manchester, Baylor College of Medicine and collaborating institutions has discovered a natural mechanism that protects the heart from heart failure with preserved ejection fraction (HFpEF), a serious condition in need of effective treatment.
The team reports in Circulation, a journal of the American Heart Association, that when the cardioprotective mechanism fails, it promotes the development of HFpEF. Importantly, restoring the
mechanism prevents the progression of the condition. The findings provide a promising therapeutic target to prevent and treat this life-threatening disease.
“HFpEF is a complex, multifactorial disease associated with metabolic stress. One of the factors involved is the toxic accumulation of lipids in heart cells,” said co-author Dr. Tamer Mohamed, associate professor of surgery and director of the Laboratory for Cardiac Regeneration at Baylor. “This study was the result of a productive multidisciplinary collaboration. We worked with slices of human hearts affected by HFpEF, a method developed in my lab at
Baylor, integrating the findings with the results from studies in mouse and rat models of the condition to better understand what drives this lipid overload.”
The team began by assessing gene changes in hearts from people diagnosed with metabolic stress along with various cardiovascular complications and found alterations in the expression of 488 genes.
“We found particularly relevant the simultaneous reduction of the expression of genes XBP1 and EDEM2 in human HFpEF hearts,” Mohamed said.
The link between EDEM2 and other conditions has been studied, but its
role in the heart remains unexplored.
“We discovered that the XBP1 protein regulates the Edem2 gene in animal models and that EDEM2 was downregulated in hearts from individuals with metabolic disorders and in mouse models,” Mohamed said. “Further evidence supported the involvement of EDEM2 and XBP1 in cardiovascular diseases and lipid regulation.”
To investigate whether XBP1 and EDEM2 were directly involved in lipid toxicity and HFpEF, the researchers removed the Xbp1 or the Edem2 gene in mice. Consequently, these mice became more vulnerable to metabolic stress-induced heart lipid toxicity and cardiac dysfunction.
“It was exciting to see that restoring XBP1 or EDEM2 alleviated lipid overload in the heart and reversed HFpEF,” Mohamed said.
This comprehensive study uncovered that XBP1 and EDEM2 work together to maintain a healthy lipid balance in heart cells. The findings provide molecular and functional evidence that deficiency of XBP1-EDEM2 leads to lipid toxicity in the heart, accelerating the onset and development of heart failure in metabolic disorders.
“Our findings support further study of the XBP1s and EDEM2 pathway as a promising therapeutic target for mitigating cardiac lipotoxicity and progression of HFpEF,” Mohamed said.


FOLLOWS THE PATIENT THROUGH THE ENTIRE PERIOPERATIVE JOURNEY

PRE-OP INTRA OPERATIVE POST-OP
Next-Generation Patient Warming, Encompass offers Passive and Active Warming.


Find Out More About Our Comprehensive Patient Warming Offering



By Miguel J. Ortiz
As we enter the second half of 2025, health and exercise will continue to be a topic of conversation with ourselves and others. A lot of us, depending our circumstances, might have adopted a pattern of inconsistent workouts and poor eating behaviors. The lack of movement, and too much sitting for all those Zooms calls, has led to a weaker core and poor breathing in many individuals.
What people need to understand is that proximal core strength will enhance distal joint strength. Which basically
means that a stronger core means stronger hips, shoulders and knees. So, who wouldn’t want that? The problem is that most people think they need a lot of time, but you don’t. Consistency with proper movement is the name of the game and all you need to do is practice these three movements daily. Whether you take 5 minutes or 30 minutes, these three movements – when done properly regardless of how much time you have – will have a tremendous effect on your core stability. They will have you moving much better going into the end of the year.
The first movement starts on the ground to isolate the core. If you are
not on a carpet or soft surface you will need a mat as we begin with the classic “dead bug” (tinyurl.com/ygnqgv7r). This movement may look easy, but it requires focus to do it properly. Start with knees bent at 90 degrees and arms punching toward the ceiling. You want to start by moving opposite arm and leg while maintaining your back on the floor and extend the arm and leg as far as possible. This helps strengthen your core and helps with coordination. It also opens up the hip and shoulder.
The second movement includes a kneeling position and starts to involve upper body rotation. It challenges your balance which, again, is very important
when it comes to core strength. This exercise is the “kneeling torso rotation” (tinyurl.com/yh39hw5v). Once in a comfortable kneeling position, active the back foot, seated upright with arms in an extended position. If your right foot is in front you want to lift your right arm toward the ceiling and rotate to your right as your reach behind while keeping your arms at 90 degrees. In this kneeling position, it focuses on challenging the core by stabilizing the hips but requires rotation of the upper body. The trick is to maintain stability while taking the upper body through a different range of motion.
The third movement goes in and out of a standing and seated position. You will
need a chair or bench. This exercise is the squatted torso rotation and reach (w). By doing this movement from a seated position, we are able to concentrate more on the stretch of our shoulder and back. Start by being ready to squat and once down open one shoulder away and toward the ceiling while using the opposite arm to create leverage and drive that leg wide. For example, when rotating to the right you should feel the stretch in your right shoulder, right lower back and left inner thigh.
I recommend preforming these movements daily for a total of 10 reps per movement at minimum.
- Miguel J. Ortiz is a personal trainer in Atlanta, Georgia. He is a member of the National Personal Trainer Institute and a Certified Nutritional Consultant with more than a decade of professional experience. He can be found on Instagram at @migueljortiz.



OUT OF THE OR fitness






By Grace O
A ntioxidants have multiple roles in the body and one of the most studied is the ability to reduce oxidative stress.
Antioxidants are one of our body’s best weapons when it comes to aging, because they fight aging at a cellular level and help keep cells from “rusting.”
Research has demonstrated that antioxidants can slow down aging by reducing oxidative stress, a natural byproduct of essential cellular
activities such as energy production, detoxification, digestion, respiration, cognition, and exercise. These processes generate free radicals, unstable molecules that initiate oxidation.
Free radicals play a vital role in stimulating important physiological processes, including immune system function and cellular signaling pathways. However, an excess of free radicals leads to an imbalance that triggers a chain reaction of electron theft, resulting in tissue damage.
Antioxidants help mitigate this damage by neutralizing free radicals, thereby maintaining cellular health and slowing the aging process. If the balance of oxidative stress gets too high, it can cause damage and “aging” to cells. This is where antioxidants come in; they protect your cells, preventing and repairing damage caused by oxidative stress. This balance is what keeps cells healthy and prevents damage that comes along naturally with living and aging.
Luckily for us, there are many delicious foods that are natural antioxidants that we can incorporate into our diet, which will counter the stress our cells encounter. You probably already know that deeply colored fruits and vegetables like berries and red cabbage contain generous amounts of antioxidants.
Here are some antioxidant super foods we should focus on:
• Almonds: are rich in vitamin E, an antioxidant which helps protect both brain and skin health.
• Beans: are rich in polyphenols, which are powerful antioxidants. Look for colored beans including black, pinto, and kidney, for even more antioxidant compounds. Beans are also high in fiber which can help improve digestion and support detoxification.
• Berries: blueberries, strawberries, blackberries, and raspberries are rich in flavonoids and antioxidant vitamins such as vitamin C. Many experts recommend including berries in the diet daily.
• Dark Chocolate: varieties over 70% cocoa are rich in flavonoids which are a potent antioxidant found in cocoa. That’s right: chocolate is part of a healthy diet because it’s so rich in antioxidants!
• Sweet Potatoes: these orange vegetables are rich in beta-carotene, which helps protect vision and skin from early aging and cellular damage. Orange and red foods should be a regular part of your diet because of their antioxidant compounds.
My Aztec Berry Salad recipe is a delicious way to put antioxidants on the menu, and it’s a perfect salad for summer.
– Grace O is the creator of FoodTrients, a unique program for optimizing wellness and longevity. She is the author of three award-winning cookbooks. Her latest cookbook is Anti-Aging Dishes from Around the World. You can find more age-defying recipes at Foodtrients.com/recipes. Recipes and photos reprinted with permission of FoodTrients.com and Anti-Aging Dishes from Around the World cookbook by Grace O.


The Aztecs recorded using chia seeds as far back as 1540. This colorful and refreshing salad is perfect for summer afternoons and evenings. Serve this salad as a starter, side dish, or light summer meal
Benefits: Chia seeds provide energy in the form of healthy fats (including anti-inflammatory omega-3 fatty acids) and plant-based protein. Fresh, seasonal berries provide a concentrated source of beneficial antioxidants such as vitamin C and anthocyanins, which improve capillary function in the brain, eyes, and skin.
Ingredients
For the salad:
• 2 cups (packed) roughly chopped baby spinach
• 1 cup fresh strawberries, sliced
• 1 cup fresh blueberries
• 1 cucumber, diced
• ½ cup sunflower kernels
• ¼ cup (loosely packed) chopped fresh basil leaves
For the dressing:
• 2 Tbs. extra-virgin olive oil
• Juice and zest of 1 lemon
• 1 tsp. minced garlic
• 1 Tbs. chia seeds
• 1 tsp. honey or maple syrup
• 1 Tbs. water
• Salt and freshly ground black pepper to taste
Combine salad ingredients in a large mixing bowl. In a separate bowl, whisk together the dressing ingredients. Toss the salad with the dressing immediately before serving.

By Daniel Bobinski, Th.D.
You’ve probably had those days when your inbox is flooded, your boss drops a lastminute project on you and three different colleagues need something ASAP. Said another way, chaos happens. Although we can’t control when chaos descends around us, we can control how we respond to it, and that’s where our power lies.
Let me share how something I read 40 years ago completely changed my perspective. William Glasser’s book “Control Theory” (now published as “Choice Theory”) tells us how we can positively impact our mental, emotional, and physical health when we make proactive choices.
What follows is how Glasser’s perspective matters to your daily work life.
In terms of physiology, your body mostly runs on autopilot. Your heart beats, your lungs breathe, and your digestive system processes that cup of coffee without you having to think about it. No conscious choices are required in these activities. But what many people overlook is that how our bodies function is impacted by our emotions.
Emotions are a bit more complicated. We may get frustrated when a colleague takes credit for our
work or we get anxious before a big presentation. Emotions tend to just happen. We have some control here, but not much. However, you need to know your emotions are impacted by your thoughts.
We have more control over our thoughts. When a project goes sideways, sometimes we automatically jump to worst-case scenarios. But a different choice is thinking about how to make things right. That’s because we have more control over our thoughts than our emotions.
Finally, we need to know that our thoughts are impacted by our actions, and we have total control over our actions. Outside of reflexes (like pulling your hand away from a hot coffee mug), we have complete control over what we do. We choose to speak up in meetings. We choose to help team members or stay late to finish a project.
So there’s the chain reaction. Your actions influence your thoughts, which affect your feelings, which impact your physiology. This means if you’re feeling nauseous because you’re stressed about a deadline, if you change your actions you will shift your thoughts, which will, in turn, transform your feelings which then impacts your physiology.
Let’s say you’re overwhelmed by a massive project and getting stress headaches. Rather than dwelling on how impossible the project seems (a
thought) and feeling anxious about it (emotion), you could choose to divide the project into smaller tasks and tackle just one segment (an action). This action leads to the thought, “I’m making progress,” which creates a feeling of accomplishment rather than anxiety. You may then notice your stress headache fading away.
The key is to make proactive choices instead of reactive ones. When you consciously choose healthy actions you create better thoughts, which creates better feelings, and ultimately you have better physical well-being.
Bottom line, what actions you choose in the face of chaos will impact your mental, emotional and physical health. And those choices are always up to you.
Daniel Bobinski, is the author of the best-selling book “Creating Passion-Driven Teams” and the owner of Workplace Excellence. Also a certified behavioral analyst, Daniel consults and conducts training on workplace effectiveness and leadership development. He can be reached at danielbobinski@protonmail.com or eqfactor.net.




Reduce


Check










INGREDIENTS:
• 1 cup DairyPure Milk50 Vanilla
• 3 chai tea bags, divided
• Nonstick cooking spray
• 2 cups old-fashioned oats
• 1/2 teaspoon salt
• 2teaspoons baking powder
• 2 tablespoons flaxseed
• 1 teaspoon vanilla
• 1/3 cup maple syrup
• 1/2 cup chopped pecans
In small pot, heat milk until hot but not simmering. Take off heat and place two chai tea bags in milk. Steep tea in milk until cool, about 30 minutes, then discard tea bags.
Preheat oven to 350 F. Spray mini muffin pan with nonstick cooking spray. In large bowl, stir cooled chai milk, oats, salt, baking powder, flaxseed, vanilla and maple syrup.
Open third chai tea bag and measure 2 teaspoons tea. If tea is coarse, blitz in spice grinder or use mortar and pestle to grind more finely. Stir tea into batter and let mixture sit 10 minutes so oats can soak up milk.
Give batter another stir then fill each mini muffin cavity about 3/4 with batter, about 1 tablespoon in each. Sprinkle chopped pecans on top. Bake bites 12-13 minutes, or until toothpick inserted in center of bite comes out clean. Let cool 5 minutes.

By family features

Hustling to get out the door for a busy day may tempt you to skip breakfast but taking a few extra minutes to nourish your body helps ensure you can keep up with the day’s demands.
Breakfast is your chance to jumpstart your body. Eating breakfast offers multiple benefits, including providing energy to fuel your day and increasing your ability to focus and make decisions.
A breakfast rich in protein is also important to keep you fuller longer. Eggs may be a frequent option, yet dairy foods can be a good, protein-rich alternative.
If you’re cutting calories, an option like Milk50 contains only 50 calories per serving but the same amount of protein as other dairy milks – 9 grams per serving –along with calcium and vitamin D. This first-of-its-kind product also contains 75% less sugar than skim milk, is lactose-free and doesn’t contain any artificial flavors or colors.
A return-to-dairy trend is gaining momentum, with 58% of U.S. adults welcoming dairy back to their diets after being disappointed with the price, taste and heavy processing of plant-based beverages, according to a national survey commissioned by Dairy Farmers of America. Incorporating these real dairy favorites in your morning recipes can be a cinch.
Start your morning with a nutritious and delicious shake like a Vanilla Coffee Protein Shake, which combines cold brew coffee and frozen bananas for a refreshing treat. Or, if you’re craving something a little heartier, mix up a batch of Chai Oatmeal Energy Bites over the weekend or in the evening so you can grab one or two on the go.
Find more breakfast inspiration at milk50.com.

Serves: 1
Ingredients:
5-6 ounces DairyPure Milk50 Vanilla
1/2 banana, sliced and frozen
1/4 cup, plus 2 tablespoons, cold brew concentrate
1/2 teaspoon vanilla extract
1-2 scoops protein powder of choice
2 teaspoons simple syrup (or to taste)
Make ice cubes by pouring milk into ice cube tray and freezing until solid, about 8 hours.
To make shake: In high-speed blender, blend frozen banana slices, cold brew, vanilla, protein powder, simple syrup and 5-6 milk cubes until creamy. Serve in glass.














