ENDOCRINOLOGY FOCUS
42
TYPE 2 DIABETES
Type 2 Diabetes: A Cluster of Diseases Personalised medicine in diabetes will improve care with reduced resources if we become better at diagnosing the various forms of type 2 diabetes Written by Professor Carel Le Roux, MBChB, FRCP, FRCPath, PhD, Diabetes Complications Research Centre, UCD and Dr Sarah Cooney, MBChB, Academic Intern, Beaumont Hospital
Professor Carel Le Roux
Dr Sarah Cooney
Type 2 diabetes is a heterogeneous syndrome caused by abnormalities in carbohydrate and fat metabolism. The causes of type 2 diabetes are multifactorial and include both genetic and environmental elements that affect beta cell function and tissue sensitivity.1 However, despite this
expansive description, in clinical practice currently type 2 diabetes tends to be oversimplified with a one size fits all approach. Recent developments have changed our understanding of the diversity within type 2 diabetes, which may hold the key to better treatment.
796
As it stands currently, the all-purpose approach can be seen in every aspect of type 2 diabetes. There are no hallmark clinical features, and both clinical presentation and complications vary widely between patients.2 The diagnosis is one of exclusion, based on hyperglycaemia once type 1 diabetes, monogenic or secondary causes have been ruled out as the source. The lack of a uniting diagnostic step is one of many indicators that there are likely multiple processes ongoing, that cannot all be detected through a single means.3 This may be where personalised medicine can make a difference. New technologies and analytic methods allow us to discover more refined disease subtypes that help to optimise disease management to match individual pathology. Personalised medicine had its beginnings, and shows most benefit when it comes to monogenic, and typically rare
diseases. In type 2 diabetes this breakthrough first came in the discovery of mature onset diabetes of the young or MODY. This paved the way for the role of genetics in type 2 diabetes and theories began to emerge of type 2 diabetes as an end result of multiple pathologies- in a similar way to anaemia having a wide range of distinct causes and pathophysiological pathways. However, as research progressed, rather than the discovery of further monogenic or high impact genes to be targeted in treatment, genome wide association studies (GWAS) identified that the majority of genetic variance is caused by a large number (>400) of common variants. Type 2 Diabetes is instead a polygenic disease with limited contribution from low frequency variants. Put into practice this means that for the majority of people it is not a single genetic variant that will be the cause for development of type 2 diabetes
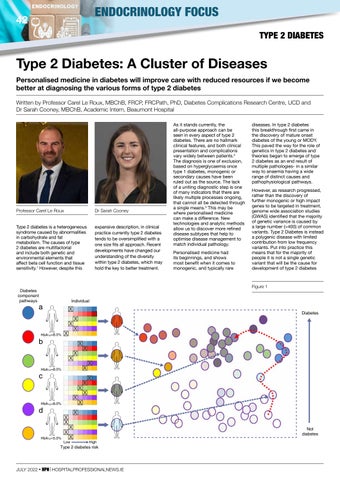
Diabetologia (2017) 60:793–799 Figure 1
Diabetes component pathways
Individual
a
Diabetes
HbA1c =8.0%
b
HbA1c =8.0%
c
HbA1c =8.0%
d
HbA1c =5.0%
Not diabetes Low
High
Type 2 diabetes risk
Fig. 1 The ‘palette’ model of type 2 diabetes. The concepts are illustrated using a model of six diabetes component pathways (‘base colours’) and four individuals, of whom have diabetes. The grids display the range JULY 2022 • HPN | three HOSPITALPROFESSIONALNEWS.IE of trait variation for each of these component pathways and the position of
two dimensions here for illustrative purposes) with respect to the status of each of the component pathways (with hue denoting the mixture of type 2 diabetes-associated contributions and saturation broadly reflecting diabetic status). Some individuals, such as individual ‘a’, lie at the extremes and