ALSO IN THIS ISSUE
ESCRS Digital Data Project
Ophthalmologists, data scientists, and industry seek to quantify anterior segment benchmarks.

ALSO IN THIS ISSUE
ESCRS Digital Data Project
Ophthalmologists, data scientists, and industry seek to quantify anterior segment benchmarks.
Multiple benefits include better training and surgical outcomes.
When to Remove a Phakic IOL?
To avoid complications, watch endothelial cell counts—but don’t wait too long.
What’s the Difference?
Gender variability in biometric parameters can affect surgical outcomes.




Pelin
16 The Holy Grail of ICL Sizing Erik L Mertens MD, FEBO, FWCRS, PCEO
17 Mastering IOL Exchange
Mirko Jankov MD, PhD
18 When Is It Time to Remove a Phakic IOL?
Rudy MMA Nuijts MD, PhD
19 No Surgical Surprises
Oliver Findl MD, MBA, FEBO
20 Are There Differences Between Male and Female Eyes?
Marie-José Tassignon MD, PhD, FEBO; Víctor Lázaro-Rodríguez MD, FEBO, FICO; Nic Reus MD, PhD; Sotiria Palioura MD, MSc, PhD; and Anders Behndig MD, PhD
21 Mapping to Guide Post-LASIK Enhancement
David Huang MD, PhD
22 Delivering Uncompromising Cataract Care
Massimo Busin MD; Iva Dekaris MD, PhD; Elisabeth Patsoura MD, MRCOphth; Joaquín Fernández MD, PhD; Björn Bachmann MD, FEBO; and Alfonso Vasquez-Perez MD, FRCOphth, CertLRS, FEBOS-CR
24 Need to Know: Aberrations, Aberrometry, and Aberropia
Soosan Jacob MS, FRCS, DNB
28 Increasing Uptake of First-Line SLT
Christine Funke MD
29 New Options for Glaucoma Patient Management
Sarah H Van Tassel MD

Publisher Filomena Ribeiro
Executive Editor
Stuart Hales
Editor-In-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Creative Director
Kelsy McCarthy
Graphic Designer
Jennifer Lacey


Circulation Manager
Lucy Matthews

Contributing Editors
Cheryl Guttman Krader
Howard Larkin
Roibeárd O’hÉineacháin
Contributors
Laura Gaspari
Soosan Jacob
Timothy Norris
Andrew Sweeney
Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 | roo.khan@wearemci.com
EuroTimes® is registered with the European Union Intellectual Property Office and the US Patent and Trademark Office.
Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983
Correction: An earlier version of “Are Postoperative Topical Antibiotic Drops Still Needed?” (EuroTimes Online, Q2 2025) included a publication error suggesting cefuroxime is active against Enterococci, among other bacteria. The article has since been corrected to clarify cefuroxime is not active in such cases, and updated versions are available on the ESCRS website.

Learn more about EuroTimes or connect with ESCRS at ESCRS.org
We’re very sad to report the passing of our friend and colleague Simonetta Morselli.
Simonetta Morselli was someone special—and she had charisma! From a young age, she realised she had to work hard to achieve the goals she set for herself: from her degree in medicine until mastering ocular surgery. Simonetta was a born surgeon, intuitive in adapting the procedures learned and ready to learn new ones with a critical spirit. Her professional place was important and recognised both in Italy and Europe, especially in her dedication to young people and the teaching of ocular surgery.
Her scientific activity, which began at university and continued well into her service as Chief of Ophthalmology, S Bassiano Hospital, Bassano del Grappa, testifies to her continuous interest in our profession and its developments. She organised the first Italian Association for Cataract and Refractive Surgery (AICCER) congress in Verona in 2006. Her first lecture at an ESCRS meeting took place in Innsbruck while she was still in residency, and she continued lecturing at our meetings for the rest of her professional career. Since then, she has led the Young Ophthalmologist Programme at ESCRS meetings. She has always devoted herself to our Society with sincere dedication. Her involvement was outstanding and completely devoid of any personal interest.
Simonetta’s strong personality, combined with her natural tendency for service, was something that fascinated all of us. You could always count on her for advice, help, or some much-needed comfort. She also loved cooking, where she exercised her imagination and proved to be a very good chef! She used to say she experienced the same enthusiasm cooking as performing surgery. Many may remember her on stage in Rimini a few years ago, together with a famous Italian chef.
EDITORIAL BOARD

Adi Abulafia (Israel)
Bruce Allan (UK)
Noel Alpins (Australia)
Juan Alvarez de Toledo (Spain)
Gerd Auffarth (Germany)
Başak Bostanci (Turkey)
John Chang (Hong Kong SAR, China)
Béatrice Cochener-Lamard (France)
Burkhard Dick (Germany)
Mor Dickman (The Netherlands)

Joaquín Fernández (Spain)
Oliver Findl (Austria)
Nicole Fram (US)
Sri Ganesh (India)
Farhad Hafezi (Switzerland)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Jack Kane (Australia)
Yao Ke (China)
Mika Kotimäki (Finland)

Simonetta was also an exceptional skier, so much so that she became a certified ski instructor to pass along her passion and enthusiasm for the sport.
Even during her long illness, Simonetta taught us a lot: as a fighter, she faced the first stages two years ago; she got back on her feet again and continued her normal activities until a few weeks ago, when her condition worsened and stopped her from doing something that she loved for the first time in her life…her work!
Lovingly assisted by her husband Vincenzo, she passed away in silence, almost as if not to disturb all of those whom she loved so much.
We are left with a void, but know deep down we share the belief that she helped make all of those who knew her better people. Our love and affection for her will never end.
Until we meet again, farewell Simonetta!
Roberto Bellucci MD

David Lockington (UK)
Artemis Matsou (Greece)
Cyrus Mehta (India)
Jod Mehta (Singapore)
Sorcha Ní Dhubhghaill (Belgium)
Rudy Nuijts (The Netherlands)
Catarina Pedrosa (Portugal)
Konrad Pesudovs (Australia)
Nic Reus (The Netherlands)
Filomena Ribeiro (Portugal)
Andreia Rosa (Portugal)
Giacomo Savini (Italy)
Julie Schallhorn (US)
Sathish Srinivasan (UK)
Paola Vinciguerra (Italy)
Shin Yamane (Japan)
Ron Yeoh (Singapore)
Mihail Zemba (Romania)

ESCRS has assembled a team of ophthalmologists, data scientists, private equity investors, and clinical researchers to lead an effort to create high-quality, open-access data sets that can spark groundbreaking research in cataract, refractive, and corneal surgery.
The ESCRS Digital Health Special Interest Group plans to leverage the Society’s Digital Research Awards programme and host digital health symposia at the ESCRS Annual Congress to help further this effort. To jump-start this initiative, the group has assembled a project team to build a library of links to existing open-access image data sets relevant to cataract, cornea, and refractive surgery.
“We all know that in clinical medicine, if we want to analyse any intervention or new treatment, we need a lot of data,” says Magdalena Niestrata PhD, FRCOphth, FEBO, FICO, a Corneal Fellow at the East Sussex and North Essex Foundation Trust, who is leading the project group. “The more data we have, the more accurate the results. And what we’ve seen in ophthalmology is that, compared to the posterior segment, the anterior segment has relatively little data available.”
To establish a benchmark, Niestrata and some colleagues conducted PubMed and Google searches to identify publicly available anterior segment image data sets. Of the 26 data sets they found, most were small and incompletely described, and half of the images were from normal eyes. The results of their research were published in a November 2024 article in the Journal of Cataract & Refractive Surgery.
The JCRS article prompted ESCRS to create the project group and establish a central, publicly accessible database for anterior segment data and images. The group hopes to entice researchers to upload their results and contribute to the collective data pool, thereby enhancing the overall quality and quantity of available data.
To encourage ophthalmologists to use the data set library, the group has created an AI-powered bot that works in multiple languages and searches for data sets in response to spoken commands. “I continually text it, and it sends us alerts when it thinks there is a new article,” Niestrata says. “It doesn’t eliminate the need for us, of course, but there is a lot we can use it to help with.”
Next steps for the project group include enhancing the bot to be more interactive and user-friendly and making the data sets more accessible to a global audience. The team also aims to include more diverse data sets, such as multimodal imaging, topography, biometry, and anterior segment OCT data, to provide a broader range of data for research and analysis.
The ESCRS Eye Journal Club has posted the latest episode of its popular series of interviews with leading ophthalmic experts.
The 40-minute episode, hosted by Artemis Matsou, Alfredo Borgia, and Victoria Till, features Professors Rudy Nuijts and Andreia Rosa discussing patient dissatisfaction after extended depth of focus intraocular lens implantation. The discussion is based on a paper of the same name published in the May 2025 issue of the Journal of Cataract & Refractive Surgery.
The Eye Journal Club produces ‘non-live’ webinars in which two expert panellists discuss a topical paper with two or three young ophthalmologist moderators from the ESCRS. Eye Journal Club webinars are published on the ESCRS website as a video or podcast available to download.

ESCRS Eye JC Ep. 37: Dissatisfaction after implantation of extended depth-of-focus intraocular lenses

Need a quick introduction or refresher about a surgical procedure? Have a tip to share about a technique or approach you use that makes surgery easier?
The ESCRS 100 is the place to go. It’s a library of short (roughly 100 seconds), high-quality instructional videos about all fields of cataract and refractive surgery.
More than 40 videos have already been created, and additional videos are being uploaded each month.
Current videos include the following topics:
• 4-flanged fixation of an artificial iris and closed-loop IOL
• Inserting the DMEK graft
• Descemet membrane stripping
• Hydrodissection
—PUT THE ESCRS 100 VIDEO SERIES ON YOUR LIST OF MUST-WATCH EDUCATIONAL RESOURCES ! ESCRS 100

The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
BY LAURA GASPARI
Aglobal consensus on simultaneous vision intraocular lenses (SVL) classification is an ambitious goal, and collaboration among everybody involved is pivotal. Experts gathered at the 2025 ESCRS Winter Meeting in Athens to discuss this topic during a TOGA Session, which placed panellists from all parties in a circle, as equals, in a modern version of the Greek agora.
Last year, the ESCRS Functional Vision Working Group, led by President Filomena Ribeiro MD, PhD, published an editorial in the Journal of Cataract & Refractive Surgery where they proposed an evidence-based new functional classification dividing lenses into two categories: partial range of field (ROF) and full ROF.1,2 In turn, partial ROF IOLs can be divided into narrow (monofocal IOLs), enhanced (monofocal-plus IOLs) and extended (EDOF) range. Full ROF IOLs divide into continuous, smooth, and steep.
As Joaquín Fernández MD, PhD explained in the introduction to the TOGA Session, this proposed classification system is the result of a thorough analysis of 10 years of literature using statistical methods like cluster analysis and was not based on the working group’s opinion as experts.
“The key to global consensus is criteria, and this is a starting point. What could be the best way to reach consensus?” he asked the participants.
Francesco Carones MD, as President-elect of the American European Congress of Ophthalmic Surgery (AECOS) European Executive Committee, pointed out that collaboration between scientific societies is crucial, as a consensus on such classification can make interaction with companies and, above all, patients, easier.
“The classification must be scientific, driven by data, and easy [for patients] to understand, because if you get into too many details, they may be quite confused,” he said, adding it could also help overcome the language barriers in current IOL classifications.
However, classification is a step beyond mere nomenclature, as Professor Ribeiro underlined, emphasising that the result for patients is also important and the basis for continuing functional classification.
“We should couple this classification with patients’ reports about dysphotopsia, independence of glasses, and quality of vision. But the problem is the way we are reporting these
outcomes now, because they are not yet standardised. And we need to do it,” she remarked. Prof Ribeiro noted the road ahead is still very long, and surgeons’ recommendations on what an IOL provides should focus on the patients rather than an optical bench or design.
The key to global consensus is criteria, and this is a starting point.
Prof Fernández remarked that before producing a new functional classification, the ESCRS group published a standardised model explaining how to acquire and report data to create a strong systematic review and to craft something as a community. Now, there is a need for validated and standardised questionnaires to acquire other information for a subclassification beyond the depth of field.
This debate garnered plenty of participation from representatives of the industry. Speakers recognised industry collaboration and support as crucial in all this work. However, as Burkhard Dick MD, PhD commented, “Every IOL needs control trials, otherwise we cannot say that it is evidence-based.” In recent years, he added, some lenses came out without multicentre trials validating the results, something that needs to be changed.
Dr Carones raised another important issue about clinical studies: trials need to be conducted in hospital and university settings more often, where patients do not have expectations based on cost.
“I am urging this organisation to consider doing both arms of studies, in public hospitals and private practices, because, in the latter, you have the real-world experience of patients,” he said.
All the attending industry representatives pointed out that manufacturers are obliged to supply some evidence of their products before releasing them on the market. However, they recognised the importance of having this classification as a common language and as a benefit to everybody, from
surgeons to patients all over the world. They praised the ESCRS for the effort, making themselves fully available for future collaborations.
An interesting perspective came from Sorcha Ní Dhubhghaill MBBCh, PhD, who spoke as a surgeon in university hospital settings. “Typically, we are not the best clients for these lenses, but since I have started to implement this simplified classification, I have noticed two things: first, patients started to understand the benefits of lenses other than standard monofocal; second, residents, who have everything to learn and no time, find this approach good to understand what these lenses can do,” she said.
Finally, Prof Fernández pointed out that the working group does not want this classification to complicate things, especially for industry. “The idea is to give the best information to our patients, and to give you an easier and fairer way to compare and transmit evidence and escape the market-oriented fight we are seeing right now,” he concluded.
For citation notes, see page 32.
Filomena Ribeiro MD, PhD, FEBO is the head of the Department of Ophthalmology, Hospital da Luz, Lisbon, and President of the ESCRS. filomenajribeiro@gmail.com
Joaquín Fernández Pérez MD, PhD is based at Qvision, Department of Ophthalmology of Vithas Almería Hospital, Spain. joaquinfernandezoft@qvision.es
Francesco Carones MD is medical director and physician CEO of Advalia-Carones Vision in Milan, Italy. fcarones@carones.com
H Burkhard Dick MD, PhD, FEBOS-CR is professor and chairman of the Ruhr University Eye Hospital in Bochum, Germany, and ESCRS president elect. dickburkhard@aol.com
Sorcha Ní Dhubhghaill MBBCh, BaO, PhD, Dip(stats), FEBO, FEBOS-CR, MRCSI(ophth) is Head of Department, Ophthalmology, at the Brussels University Hospital (UZ Brussel), Belgium. sorcha.ni.dhubhghaill@uzbrussel.be
The ESCRS and ASCRS have agreed to work together on the evidence-based functional classification of simultaneous vision intraocular lenses. The collaboration was finalised at an early morning meeting held during the annual ASCRS conference in Los Angeles. The joint ESCRS/ASCRS project is led by Douglas Koch, past president of the ASCRS, and ESCRS President Filomena Ribeiro. The ESCRS group includes Burkhard Dick, Thomas Kohnen, Oliver Findl, Rudy Nuijts, Béatrice Cochener-Lamard, and Joaquín Fernández. The details will be available at the ESCRS Congress in Copenhagen later this year.
Individualised planning models could reduce ectasia risk and improve outcomes.
HOWARD LARKIN REPORTS
Today’s refractive diagnostic and treatment devices are capable of submicron precision. Yet they’re typically guided by generalised surgical planning algorithms that assume population-level responses to biometric measures, with adjustment for just one or two individual variables—primarily drawing from the surgeon’s previous results for the same procedure.
In addition to limiting the precision of refractive outcomes, current surgical planning approaches give minimal guidance on individual risk for ectasia, said William J Dupps Jr MD, PhD. Simplified nomograms for guiding procedures such as intracorneal rings and astigmatic keratotomy are even less reliable, and emerging treatments lack nomograms altogether.
“Every one of these corneal procedures is going to invoke biomechanical responses,” Professor Dupps said. “Some rely on those responses to get the treatment effect. And yet we don’t really have a biomechanical approach to understanding where that patient is likely to end up, and how we could optimise treatment. If we could find a unifying clinical decision tool that considers [individual biomechanics], that would be fantastic.”
The current approach is retrospective, Prof Dupps pointed out. “We look at what has happened in the past and try to predict what will happen in the future.” It is probabilistic and population-based, with little attention to the biomechanical realities of the patient to be treated. He proposes the new approach should be more prospective, deterministic, and individualised.
Every one of these corneal procedures is going to invoke biomechanical responses.
A computational modelling approach using moreindividualised patient biomechanical data analysed through a finite element method (FEM) could fit the bill, Prof Dupps said. FEM is a structural engineering method to create a digital twin for interrogating shape and mechanical behaviour under stress. The structure is divided into smaller elements, and the relationships between these elements are mathematically represented, allowing assessment of the global system.
Granular data for constructing such models of individual eyes comes from tomography to define eye surfaces. Demographic data and intraocular pressure are other elements introduced. Variables from emerging biomechanical measurements may also be included. Combining these data creates a 3-D eye model to verify against the existing eye.
This digital twin is then subjected to various procedure simulations, with all responses recorded. Factors such as treatment zone, flap placement, and refractive correction are considered. Outcomes assessed include refraction, astigmatism, and some measures of biomechanical stress and strain.
Models exist for LASIK, PRK, and lenticule extraction— with some more mature than others, Prof Dupps said. Validation studies of some early models showed a strong correlation with refractive outcomes but were limited due to the assumption all eyes have similar biomechanical responses.
Adding corneal hysteresis as a global biomechanical factor improved model performance, Prof Dupps said. “We improve outcomes when we incorporate that simple marker.”
Eventually, more precise biomechanical data might come from dynamic OCT and Brillouin microscopy, which can measure focal corneal stiffness at thousands of points, he added. This could make the analysis even more precise and predictive of individual treatment responses.
Prof Dupps spoke at Refractive Day of the 2025 ASCRS annual meeting in Los Angeles.
William J Dupps Jr MD, PhD, MS, FARVO is professor of ophthalmology and biomedical engineering at the Cole Eye Institute and Cleveland Clinic Lerner College of Medicine of Case Western Reserve University in Cleveland, Ohio, US. duppsw@ccf.org

Fine-tuning refractive outcomes to meet patient expectations.
TIMOTHY NORRIS REPORTS
To achieve optimal results with post-presbyopic IOL enhancement, it is important to understand the ‘five Ws’ of enhancement: who should perform it, why it should be done, what amount of correction should be entered and when, and where or how it should be performed, Francesco Carones MD advised.
Dr Carones underlined the role of the refractive or vision-corrector surgeon, explaining it would be better if the one performing the procedure implemented the original treatment. He believes the surgeon should understand the problem, quantify the magnitude of correction, choose the most appropriate procedure, and decide the timing for the enhancement.
The amount of correction, timing, and the appropriate procedure are all critical to achieve this best result.

Achieving a mandatory perfect refractive result is important for Dr Carones mainly because patients are becoming increasingly demanding—although he noted most of them did pay a ‘premium fee,’ thus expecting the best possible outcome. Presbyopia-correcting IOLs, however, come with many issues. Diffractive optics, for example, are not forgiving at all. Refractive optics tend to be more forgiving but provide less range of focus, which may not be wide enough. Moreover, night dysphotopsia amplifies when the light does not focus on the macula.
What to correct—or how much to correct—may be critical, so Dr Carones stressed always focusing on the purpose behind enhancing. He advised surgeons to ensure the patient really understands the advantages and disadvantages of getting close to the target via an intervention. Astigmatism over -0.75 D sphere should be considered for correction as a critical amount, especially when implanting diffractive optics, so it is advisable to speak with the patient about the advantage of correcting residual refractive error, he said.
When dealing with enhancement, the two variables to consider are the amount of astigmatism and the visual axis. If the sphere equivalent is plano but the axis is wrong, an enhancement should be considered as soon as possible, Dr Carones explained. When the amount is wrong both with and without
a wrong axis, it might be necessary to wait for refractive stability. When there are three variables, like amount, axis, and sphere, it is always recommended to wait for refractive stability, he added.
But for how long? The majority of the many variables to consider relate to the healing process. Dr Carones observed it might be advisable to wait a month for the refractive stabilisation before opting for an enhancement. Figuring out how to proceed is the final decision, which he described using his personal decision tree: (1) start with the IOL rotation; if this is not a good option, then use (2) LASIK; if even this is not a good option, try (3) PRK, followed by (4) supplemental IOL and (only if any of the above are indicated) IOL exchange.
“Dealing with presbyopia-correcting IOLs frequently deserves a fine tuning. The amount of correction, timing, and the appropriate procedure are all critical to achieve this best result,” he concluded.
Dr Carones spoke at the 2025 ESCRS Winter Meeting in Athens.
Francesco Carones MD is Medical Director and Physician CEO at the Advalia Clinic of Milan,
Italy.

New IOL appears to increase rates of spectacle independence.
ROIBEARD O’HEINEACHAIN REPORTS
Anew meta-analysis and systematic review appears to confirm the Tecnis Eyhance™ (Johnson & Johnson) intraocular lens offers equivalent distance visual acuity and significantly better intermediate and near visual acuity with greater spectacle independence compared to standard monofocal IOLs. However, further studies are needed to confirm outcomes in contrast sensitivity and patient-reported experiences across various enhanced monofocal IOLs, the study’s authors note.1
“Physicians should inform patients that the Eyhance IOL provides improved intermediate and near vision compared to conventional monofocal IOLs in around one line of visual acuity,” Joaquín Fernández MD, PhD, lead author of the study, told EuroTimes. “This increases around 20% the probability of achieving spectacle independence at intermediate and near [distance] for partial range of field (ROF) enhanced IOLs in comparison to partial ROF narrowed IOLs.”
The meta-analysis reviewed studies from Medline (PubMed), Embase (Ovid), and trial registries comparing the Eyhance IOL with other monofocal IOLs in patients who underwent bilateral cataract surgeries from 2019 to 2024. The primary outcomes analysed were monocular distance-corrected visual acuities, defocus curves, and contrast sensitivity; secondary measures included binocular visual acuities and patient-reported outcomes like spectacle independence and photic phenomena.
Investigators retrieved 148 records from systematic searches and clinical trial databases, with 31 meeting eligibility criteria. These included 8 randomised clinical trials and 23 case series, all having a follow-up period of approximately one month. The defocus range analysed was 0.0 D to -2.0 D. Comparator IOLs were the Tecnis ZCB00, the Tecnis AAB00, Clareon CNA0T0 (Alcon), the Vivinex iSert and Vivinex
Impress (Hoya), the RayOne Monofocal (Rayner), the IsoPure (BVI Medical), the zoe Primus-HD (Ophthalmo), and the AcrySof SN60WF (Alcon).
The meta-analysis found no significant differences in corrected distance visual acuity (CDVA) between the Eyhance and monofocal IOLs. However, Eyhance showed better performance with considerable differences in mean distance-corrected intermediate visual acuities (DCIVA; -0.09 logMAR) and mean distance-corrected near visual acuity (DCNVA; -0.08 logMAR; p < 0.0001). A subgroup analysis revealed no significant difference in DCIVA and DCNVA between the Eyhance and other enhanced IOLs, such as the zoe Primus-HD, Vivinex Impress, and IsoPure. Comparing the Eyhance with remaining conventional monofocal IOLs, the mean differences increased to -0.11 logMAR and -0.12 logMAR for DCIVA and DCNVA, respectively (p < 0.0001).
For binocular uncorrected visual acuities, the study similarly found no significant differences in uncorrected distance visual acuity (UDVA) between the Eyhance and monofocal lenses, but significant differences in favour of the Eyhance for binocular uncorrected intermediate visual acuity (UIVA; logMAR -0.14) and uncorrected near visual acuity (UNVA; logMAR -0.15).
Monocular distance-corrected defocus curves demonstrated statistically significant differences in visual acuity between the Eyhance and monofocal IOLs at defocus levels ranging from -0.5 D to -2.0 D, with a gradual increase in effect as defocus increased. Clinically relevant differences between the Eyhance and the monofocals were observed for defocus levels beyond -1.0 D, including when compared to the IsoPure.
Binocular distance-corrected defocus curves demonstrated similar results, with statistically significant differences between Eyhance and monofocal IOLs at defocus levels ranging
from -0.5 D to -2.0 D. Clinically relevant differences appeared at defocus levels beyond -1.0 D. Four studies comparing Eyhance with other enhanced monofocal IOLs reported no statistically significant differences in defocus curves. Additionally, there was no notable dif ference between Eyhance and Tecnis ZCB00 or Clareon CCA0T0/CNA0T0 in only two studies qualified with a critical risk of bias. However, in these particular studies, notable differences were observed favouring Eyhance in binocular DCIVA (-0.05 logMAR, p < 0.001 vs Clareon CCA0T0/CNA0T0) and binocular UIVA (-0.39 logMAR, p < 0.001 vs Tecnis ZCB00).
of achieving spectacle independence at intermediate distances, with an odds ratio of 7.85. A study comparing Eyhance to zoe Primus-HD showed similar spectacle independence rates, and when this study was exclud ed, the odds ratio increased to 11.5. For near distance spectacle independence, Eyhance also performed better than the other lenses, with an odds ratio of 2.16, though the effect size was smaller.

The five studies that reported photopic monocular distance contrast sensitivity function without glare found no significant differences between Eyhance and monofocal IOLs, especially for low and middle spatial frequencies. Binocular contrast sensitivity differences between Eyhance and other IOLs were under 0.1 logCS across all spatial frequencies, indicating no clinical relevance. Additionally, Eyhance did not increase the occurrence of frequent or very frequent photic phenomena such as halos, glare, or starbursts.
Professor Fernández noted the variations seen in the increased range of field afforded by the Eyhance compared to the standard monofocals could be mainly due to differences in testing methods and conditions, patient factors such as age and ocular comorbidities, and variations in surgical technique such as micromonovision targeting.
“Future studies should follow the standards of JCRS for measuring and reporting IOL outcomes and the recommendations for writing manuscripts. They include the use of standardised testing protocols, such as ETDRS charts at 85 cd/m², reporting on environmental light conditions and pupil diameter, and postoperative variables that can influence performance,” Prof Fernández said. “In addition, reporting should focus on monocular distance-corrected outcomes for assessing IOL performance and binocular uncorrected for procedure performance. Studies should also evaluate how variations in the procedure such as micromonovision, etc., can affect the performance.”2,3
For citation notes, see page 32.
Joaquín
Fernández Pérez MD, PhD is based at Qvision, Department of Ophthalmology of Vithas Almería Hospital, Spain.
joaquinfernandezoft@qvision.es
What is the one leadership skill you would like to improve? What is the one business management challenge you would like to overcome?
The ESCRS Leadership, Business, and Innovation (LBI) programme provides ophthalmologists, clinic managers, and administrators and their teams with a variety of content to enable both online and in-person learning. Podcasts, webinars, video interviews, and more are available in the LBI library to help answer questions about topics such as selling a practice, finding a good work-life balance, facilitating patient decision making, and more.
Finding the best choice among different PIOLs with several considerations.
TIMOTHY NORRIS REPORTS
Phakic IOLs offer several different options for refractive correction of patients in the range of 40 to 50 years old, especially for myopic patients who may be more at risk of retinal detachment.
“Not only [do] these lenses reduce the risk of retinal detachment and endophthalmitis with respect to lens exchange, but being able to preserve the natural lens, it is also possible to preserve some of the natural accommodation of the eye,” said Erik L Mertens MD.
The first lens to evaluate, he added, is the IPCL V2.0 (Care Group), an implantable phakic contact lens with a refractive-diffractive optic profile made with a reinforced hybrid acrylic material. This lens comes in a wide variety of sizes, between +15 D and -30 D of sphere, and a cylinder up to +10 D.1
There is, however, a downside: The surgeon needs to be careful when implanting the toric version, he cautioned. A study published in the Journal of Cataract & Refractive Surgery noted this lens scored a rate of rotation four and a half times higher than the toric ICL (Visian).2,3 Even with a larger diameter, the IPCL did not induce a lesser amount of rotation. For this reason, Dr Mertens warned, the surgeon must be aware of and prepared for the risk.
Another viable phakic lens is the Viva ICL (STAAR), an IROF lens that provides continuous vision, working with spherical aberration.4 The problem with this lens is the difficulty centring the posterior phakic IOL on the visual axis. Inducing high-order aberration in this type of lens without centration can induce coma.
Ophtec’s Artiplus is one of the newest lenses on the market. It requires a larger incision than those for implanting ICLs and IPCLs; however, no sutures are necessary. The lens comes with -15 D to +2.5 D increments with an add power of 2.5 D. Fortunately, the vision correction is in the centre, with
the near correction next to it, providing far and near correction even in smaller pupils. Even in cases of decentration, Dr Mertens said this lens provides acceptable results.
The results appeared in an open-label, prospective non-controlled clinical trial conducted in nine participating centres with a 3-year follow-up. Reviewing the data, Dr Mertens highlighted the very good results for intermediate and near visual acuity. In the defocus curve, 51% of eyes achieved 20/16 for far vision, with an average of 20/25 reading capability at 33 centimetres. For 25 centimetres, patients scored 20/40 vision on average.
Regarding safety, downsides, and materials, Dr Mertens compared the three lenses, with ICL being highly biocompatible due to the collamer material. Additionally, it has a long-term safety profile and proven stability, but it can induce coma when the centration is not on the visual axis. The IPCL, on the other hand, is stiffer, he said. There is a toric version, but the rotation issues must be taken into consideration. Lastly, the Artiplus, made of polysiloxane, does not currently come with a toric version.
“This lens is already available in Europe, with more studies on the way to prove its feasibility,” Dr Mertens concluded.
Dr Mertens spoke at the 2025 ESCRS Winter Meeting in Athens.
For citation notes, see page 32.
Erik L Mertens MD, FEBO, FWCRS, PCEO is Director, Founder, and Ophthalmic Surgeon of Medipolis, Antwerp, Belgium, and Chief Medical Editor of Cataract & Refractive Surgery Today ( CRSToday ). e.mertens@medipolis.be


Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Amultimodal large language model (LLM) showed promising results in analysing and interpreting meibography images and detecting morphological abnormalities and subtle changes; further studies are expected to prove it as an asset for the diagnosis process, according to Pelin Kiyat MD.
“The medical community has witnessed a significant progression of the artificial intelligence role in the field,” she said. “Large language models have the potential to gain importance due to their capability to process and interpret both visual and textured medical data.”
To demonstrate, Dr Kiyat presented on a study involving a new LLM called Claude Sonnet 3.5 (Anthropic), which contains newly designed features for analysing multimodal data. The purpose of the study was to evaluate the performance of Claude Sonnet 3.5 in interpreting quantitative and qualitative alterations in meibomian glands through meibography images, of which the study included 228. An experienced ophthalmologist evaluated and graded the morphological changes and the drop-out ratio of meibomian glands using upper and lower eyelid meibography captured with an infrared microscope. The images were graded from zero to three according to a previously defined system. A subset of 160 images was selected to ensure 40 images each of the four grades.1 The study asked Claude Sonnet 3.5 to analyse the meibography images, provide the graded gland drop-out, and describe the morphological abnormalities.
Standard sentence prompts were used to obtain consistent LLM responses, then compared to the ophthalmologist’s manual evaluations and classified as correct or incorrect. Researchers assessed performance by calculating the percentage of correct answers and the LLM’s ability to identify morphological changes. For quality assurance, a new account was created for the study, the conversation history was cleared between
the images, and the same ophthalmologist performed all image inputs.
The study results showed human evaluation identified morphological abnormalities in 48 images (30%), with heterogeneous lumen diameters (33 eyes) the most prevalent—including both dilated and narrowed lumens, glandular tortuosity (17 eyes), lumen length shortening (16 eyes), and hyperreflective gland residues (11 eyes). Claude Sonnet 3.5 showed high accuracy in grading meibomian gland drop-out, with only 12 images incorrectly analysed. It achieved 100% sensitivity in detecting morphological abnormalities by correctly identifying all 48 images. In addition, Claude Sonnet 3.5 found that 12 images initially defined as normal in the manual evaluation had subtle morphological changes, such as mild tortuosity, inconsistent spacing, and minor gland fusion.
Furthermore, these results demonstrate Claude Sonnet 3.5 as an effective tool to support early diagnosis, presenting an opportunity to speed up patients’ flow through the clinic system. However, further studies are required to address the incorrect grading or the tendency to underestimate severe cases.
“This technology could particularly benefit high-volume ophthalmology clinics by potentially reducing diagnostic time while maintaining accuracy,” Dr Kiyat concluded.
Dr Kiyat spoke at the 2025 ESCRS Winter Meeting in Athens.
For citation notes, see page 32.
Pelin Kiyat MD is an ophthalmologist at the Department of Ophthalmology, Izmir Democracy University, Buca Seyfi Demirsoy Training and Research Hospital, Izmir, Turkey. pelinkiyat@hotmail.com

Obtaining the perfect vaulting to maximise performance and lower the risk of complications.
TIMOTHY NORRIS REPORTS
In phakic IOL surgery, particularly ICL implantation, sizing remains a serious matter of concern, a ‘holy grail’ that needs to be obtained as well as deeply understood. As Erik L Mertens MD explained, “a low vault is not a problem anymore with the central hole, but a large vault can create dysphotopsia and in some cases lead to serious and blinding complications, such as closed-angle glaucoma.”
To correctly measure the dimension of the eye and the anterior chamber, Dr Mertens recommended a CSO (costruzione strumenti oftalmici) MS39 spectral domain OCT and either an Artemis or the Escalon UBM (Sonomed). Despite needing a trained operator to obtain a good measurement, the Escalon UBM is equipped with very advanced software that accurately identifies the anterior and posterior part of the cornea, the anterior and posterior capsule, and both the angle and sulcus measurements, he said. Furthermore, the software analyses the alignment and highlights good measurements for the surgeon, providing all the data needed for calculating the exact size of the ICL.
As for the MS39, Dr Mertens suggests a combination of two formulas, both available on the device as a software add-on: one developed by Andrea Russo, the other (the LASSO formula) stemming from Dr Mertens’ cases with the collaboration of Professors Karel van Keer and Thomas Kohnen, who worked on the mathematics and the statistics alongside his team. According to Dr Mertens, the combination of the LASSO formula with the IOLMaster measurements provides data with both an absolute error and a standard deviation that are lower than many other formulas, including the Nakamura formulas and the STAAR OCOS nomogram.
Cumulative predictive accuracy of the LASSO formula scores 68% within 100 micrometres, 92% within 200, and 100% within 300 compared to 62% and 57% at 100, 73% at 200, and
Sizing remains a serious matter of concern, a ‘holy grail’ that needs to be obtained as well as deeply understood.
81% and 78% at 300 micrometres of the Nakamura NK2 and OCOS formulas, respectively, he said. Combining the ICLS GURU with Andrea Russo’s formula and the LASSO formula, it is possible to achieve an ideal vault—targeted between 250 and 750 micrometres—87% of the time. On the other hand, 13% of patients did achieve a safe vault, 10.5% with a low vault (lower than 250 but higher than 150 microns) and 2.5% with a high vault (between 750 and 1,000 microns), Dr Mertens said, observing that in 100% of treated patients, a safe vault was the minimum achievable outcome.
When sizing is considered, he noted the anterior OCT is much more practical than the UBM for ICL calculation.
“Being a noninvasive procedure, this kind of measurement is much more comfortable for the patients, providing a very predictable postoperative vault prediction within a 0.2-millimetre range in 92% of cases and a 0.3-millimetre range in 100% of cases,” Dr Mertens concluded.
Dr Mertens spoke at the 2025 ESCRS Winter Meeting in Athens.
Erik L Mertens MD, FEBO, FWCRS, PCEO is Director, Founder, and Ophthalmic Surgeon of Medipolis, Antwerp, Belgium, and Chief Medical Editor of Cataract & Refractive Surgery Today ( CRSToday ). e.mertens@medipolis.be
Tips and tricks for an uncomplicated replacement procedure.
TIMOTHY NORRIS REPORTS
As cataract surgery becomes more and more a branch of refractive surgery, pseudophakic patients are increasingly asking for their intraocular lens to be replaced due to higher expectations and a lack of satisfaction. IOL exchange, however, is usually performed only for specific reasons. According to Mirko Jankov MD, PhD, it is mainly dissatisfaction with the refractive outcomes that pushes patients to drive a hard bargain.
“Of my last 15 cases of IOL exchange, I had to exchange the lenses not because of misplacement, dislocation, inflammation, or opacification of the IOL or the posterior capsule, but because the patient was highly dissatisfied,” he said. “This was especially common in patients with multifocal IOLs.”
Professor Jankov explained how lens exchange can be challenging even in the simplest cases, where the posterior capsule, the whole anatomy of the bag, and the zonules are intact. However, even in this easy scenario, the lack of proper instrumentation can make everything difficult, so ensuring the correct hooks, the microforceps, and strong enough scissors are available is still extremely important. He further emphasised the endothelium needs protection from being touched during the procedure by any means necessary.
Regarding the incision site, Prof Jankov suggested making the process easier by going for an incision that is too small: a 2.5–3.0 mm incision is better to avoid both complications without incurring a longer recovery time. When dealing with rigid IOLs, however, a larger incision may still be required.

If it is not possible to dissect the original incision, targeting the temporal approach is suggested to reduce the risk of induced astigmatism. Any of the available techniques for IOL exchange start with a good viscodissection, he observed. It is very important to start the viscodissection from the posterior part—failing to do this first will make it difficult to move the lens soon after, he added.
Master the technique and have the right instruments. And always be aware that damaging the endothelium, the capsule, or the zonules can lead to undesired complications.
Moreover, during the cutting phase, some parts of the IOL can become a potential danger not only for the endothelium but the integrity of the capsular bag, emphasising the need for caution.
Amongst the different IOL extraction techniques, such as the classic cut, the Pacman, the FLAIR, and the cartridge pullthrough, Prof Jankov chose the ‘twist and out’ as his preferred approach. This technique allows twisting the lens and folding it inside the anterior chamber while a spatula protects the endothelium. Describing it as a very elegant technique, he said another version uses a cannula shaft to give the surgeon complete use of both hands.
The technique choice, however, is not only driven by the surgeon’s preference, Prof Jankov observed, but the IOL material, its location, the presence of fibrosis, and other anatomical variables that make some techniques more suitable than others. Especially important is the presence of a capsular bag already treated with YAG capsulotomy, which can make things much more difficult.
“Master the technique and have the right instruments,” he said. “And always be aware that damaging the endothelium, the capsule, or the zonules can lead to undesired complications.”
Prof Jankov spoke during the 2025 ESCRS Winter Meeting in Athens.
Mirko Jankov MD, PhD is clinical director at the LaserFocus Clinic of Belgrade, Serbia; Sarajevo, Bosnia and Herzegovina; and Budva, Montenegro. mirko. jankov@laserfocus.eu
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
TIMOTHY NORRIS REPORTS
Corneal decompensation caused by phakic IOLs may severely jeopardize surgical outcomes, especially DMEK, suggesting a timely explantation as the best solution. According to Rudy Nuijts MD, PhD, the phenomena of corneal endothelial cell loss years after phakic IOL implantation is well known. Citing a previous study, Professor Nuijts observed how the most prominent outcome was the nine-year average between lens implantation and detection of significant cell loss.1
“In the beginning, everything is fine, and you really have to wait for a long time before seeing significant negative effects,” he said.
The decision to suspend the I-CARE phakic IOL from the market in March 2007 prompted the French government to issue a rule dictating that every phakic IOL that causes a loss of endothelial cells higher than 25% or a density under 1,500 cells per square millimetre should be explanted as soon as possible. This position was later adopted by the FDA in the United States, making it a globally accepted guideline.
So, what about endothelial cell loss in rigid iris fixation IOLs, such as the Artisan? In an effort to answer this question, Prof Nuijts performed an 18-year study, from January 1998 to June 2016, on 507 eyes from 289 patients who received a myopic or toric iris-fixated PIOL implant at the University Eye Clinic Maastricht in the Netherlands. Reviewing the 6-month to 10-year postoperative data, the proportional cell loss of the Artisan myopia and toric lenses was 16.6% and 21.5% (respectively) and 10.9% and 15.8% (respectively) when corrected with the physiological 0.6% yearly loss. Such rates were two to three times higher than would be seen physiologically, he observed.2
However, only 1% of patients had the lens explanted before the 10-year threshold, rapidly increasing to 6% in the study over the complete follow-up, with a mean time of explantation set at 12 years. The indications were cataract surgery with pooled endothelial-related causes accounting for 6% of cases. The authors observed a similar drop in the survival curve after 10 years in a complementary 8-year prospective clinical cohort study on foldable iris-fixated PIOLs, with the Artisan hyperopia group being the most susceptible to explantation due to endothelial cell loss.3
As for the ICL, a 2019 study showed a cell loss rate of 5.3% at 10 years, lower than the iris-fixated PIOL, but still high compared to the physiological rate, Prof Nuijts observed.4
A bilensectomy, namely lens removal combined with phacoemulsification, should be the first option if the cell count is higher than 1,500 per square millimetre, he suggested.
Despite some short-term benefits, patients in the literature with an ongoing corneal decompensation who were treated with DMEK scored an endothelial cell loss of 39.9% at 12 months postoperatively and up to 55.6% at year 2 and 62% at 4 years. The endothelial cell loss after a cumbersome surgery as DMEK is quite extensive, he observed.
However, time is of the essence to avoid irreversible damage. “If you have to perform a DMEK in this scenario, you will lose almost half of the cells in one year with related issues, such as IOL calculation errors, swollen cornea, and limited corneal visualisation,” Prof Nuijts explained.
“Check the endothelial cell status every year postoperatively and before you [perform] surgery on these patients and explant the lens using the parameters of 25% loss or 1,500 cells per square millimetre [as a] threshold.”
Dr Nuijts spoke at the 2025 ESCRS Winter Meeting in Athens.
For citation notes, see page 32.
Rudy MMA Nuijts MD, PhD is Professor of Ophthalmology and Director of the Cornea Clinic Center for Refractive Surgery at the University Eye Clinic Maastricht, Maastricht University Medical Center (MUMC), Netherlands. rudy.nuijts@mumc.nl

Tips and tricks to avoid going off target during a cataract and refractive surgery.
TIMOTHY NORRIS REPORTS
Refractive surprise is not just about a negative surgical outcome. It causes anisometropia, a switching of the dominant eye, and remarkably high patient dissatisfaction. Oliver Findl MD discussed methods to avoid such a dire scenario, ensuring a positive surgical outcome and a happy patient.
“The chances of having a 20/20 result really decrease as soon as you have some kind of residual ametropia,” he said, citing a study by Dr Steve Schallhorn on 40,000 eyes.1 “As you can expect, patients’ satisfaction also drops significantly the more you are off target.”
Professor Findl said the key to ensuring a good and predictable refractive outcome is prevention through three main strategies: a precise preoperative measurement, securing a healthy ocular surface, and using an accurate and modern IOL calculation.
While measuring axial length is now very precise, Prof Findl observed that corneal measurements are still tricky, especially when toric lenses and astigmatism are involved. Therefore, his first suggestion is to rule out irregular astigmatism by performing a keratometry or an anterior segment OCT. The imaging and pachymetry values, topography, and tomography of the classic Placido, as well as corneal thickness, are all useful.
The ocular surface is also worth considering. As shown in a study by Dr William B Trattler, 60% of routine cataract patients are actually asymptomatic dry eye patients who do not regularly use eye drops and show no apparent issues, but have an unstable tear film observable using a keratometry or a topography.2 If unchecked, this is something that can cause an error in the preoperative measurements. Postponing surgery until the dry eye is managed is a good option that two out of three ophthalmologists already take into consideration, Prof Findl said.
Corneal irregularities also need consideration, especially if the patient underwent previous corneal refractive surgery, he explained. It is also essential to rule out the presence of keratoconus. Ultrasound may also be helpful when biometry measurements can be unpredictable due to a rocky cataract, he added.
Carefully observing biometry results when searching for red flags is also important to avoid refractive surprises. According to Prof Findl, red flags include a difference of 1.0 D between eyes in the average keratometry score (Avg K), an Avg K higher than 47 or lower than 41.0 D, high astigmatism with a cylinder higher than 2.5 D, anterior chamber depth less than 2.0 mm and more than 4.2 mm, and axial length longer than 30.0 mm and especially shorter than 22.0 mm.
“Optimise your biometry technique, validate your equipment, and make sure all IOL calculations are double or triple checked,” he advised. He also recommended keeping IOL constants optimised.
60%
60% of routine cataract patients are actually asymptomatic dry eye patients who do not regularly use eye drops and show no apparent issues.
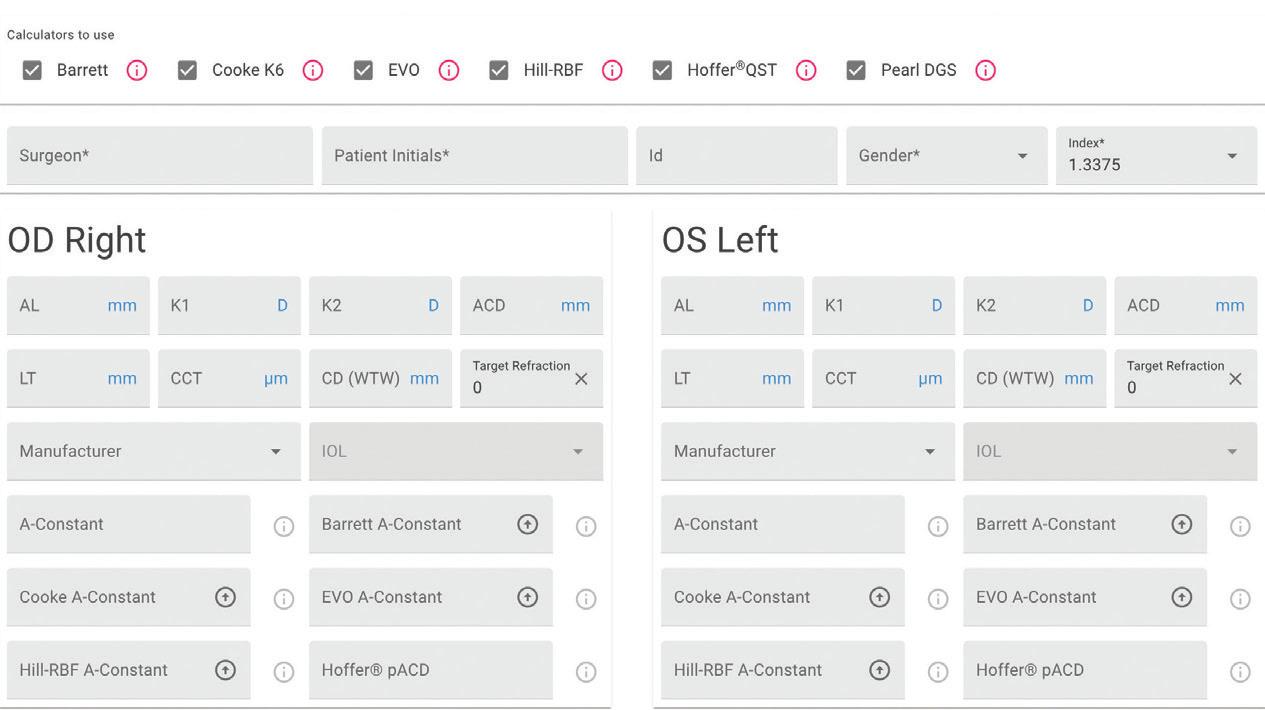
While there are many choices for finding the correct formula, Prof Findl observed “most of them are now aggregated into the free online ESCRS IOL Calculator.”
Prof Findl spoke at the 2025 ESCRS Winter Meeting in Athens.
For citation notes, see page 32.


TOGA Session panel underlined the need for more studies on gender differences.
LAURA GASPARI REPORTS
Male and female eyes have important differences in biometrical parameters that need further study to better understand the surgery and treatment outcomes. An expert panel debated this topic during a TOGA Session held during the 2025 ESCRS Winter Meeting in Athens chaired by Marie-José Tassignon MD, PhD.
“There are already differences between male and female eyes in babies, and they continue in adults. Now, whether that is important, I do not know because nobody ever studied it,” she commented.
While there is data about gender differences in the lenses and axial length of baby eyes, she said what is missing is an extensive study on adult eyes.
Professor Tassignon reported that the Project Gullstrand Study Group, named for Nobel Prize winner Allvar Gullstrand, measured the eyes of a large sample of all ages and found some differences between female and male eyes in refractive errors, with different parameters such as axial length, lens thickness and shape, and anterior chamber volume.
In recent years, various fields of medicine have focused more on gender differences to better address patients’ needs. But this has not always been the case.
“Most do not know that until 1993, most women were not allowed to participate in clinical trials,” said Sotiria Palioura MD, PhD. “And that means a lot of the data we have now in medicine is based on only half the population.”
An example of these significant differences lies in cardiac marker troponin levels, as the actual cut-off is much lower in women than men. The discrepancy led to many missed heart attacks, and research has only expanded in the last three or four years. Moreover, gender differences also appear in drug dosages that are sometimes calculated for adult males, resulting in women complaining more often about side effects.
In a surgical specialisation such as ophthalmology, differences in biometrical parameters of the eye are particularly impactful, as Víctor Lázaro-Rodríguez MD suggested. “Women have steeper corneas, shallower anterior chambers, shorter axial length, and greater diameter, and these differences have been significant in surgical outcomes,” he said.
Some IOL calculation formulas consider gender, such as the Kane formula, Nic Reus MD, PhD pointed out, which has proven to improve surgical outcomes. “In ophthalmology, especially in cataract surgery, most operated patients are women because they live longer and have higher chances of getting cataract than men. So, is there a bias towards women having better outcomes than men in ophthalmology?” he asked.

From the audience, Anders Behndig MD, PhD commented that the Swedish Cataract Register showed the biometry prediction error in women was higher than in men. “It was annoying and shocking, and it turned out the SRK/T formula we used did not really account for the steeper corneas or shorter eyes of women,” he recalled. “When we switched to more modern formulas, like the Haigis formula, this difference disappeared.”
Differences between female and male eyes do not just stop at biometric parameters or anatomical issues, but continue with systemic factors. Few studies have been done on gender differences in arterial hypertension risks, cholesterol, or systemic medical treatments, Prof Tassignon emphasised.
Age could make a significant difference between female eyes as well. Menopause is crucial, Dr Palioura observed, as other fields of medicine have found it creates huge changes in women’s bodies, where the oestrogen drops to one-third of its original level. Therefore, young women’s eyes probably behave differently from those of women in menopause.
This, Prof Tassignon concluded, really demonstrates how more studies are needed on the issue. “There are quite a lot of variables and there is already a good attempt to get good and solid results, but we are not completely there.”
Marie-José Tassignon MD, PhD, FEBO is emeritus professor and head of the department of ophthalmology, University Hospital, Antwerp, Belgium. marie-jose.tassignon@uza.be
Víctor Lázaro-Rodríguez MD, FEBO, FICO is ophthalmologist at the Hospital de la Santa Creu i Sant Pau and the Institut Català de Retina, both in Barcelona, Spain.
Nic Reus MD, PhD is an ophthalmologist at Amphia Hospital, Breda, Netherlands. nreus@amphia.nl
Sotiria Palioura MD, MSc, PhD is US-trained eye surgeon working in Athens, Greece. info@sotiriapalioura.gr
Anders Behndig MD, PhD is the co-chair at EUREQUO, former president of the Swedish National Cataract Register and Swedish Ophthalmological Society, and professor at Umeå University Hospital, Sweden. anders.behndig@umu.se

OCT can help differentiate between ectasia, steep island, and epithelial deformation.
HOWARD LARKIN REPORTS
Normal corneas have a relatively uniform epithelial thickness, typically ranging from 50 to 59 microns with a standard deviation of less than 3.6. But post-LASIK corneas can show focal steepening, often coinciding with distinct patterns of epithelial thinning or thickening.
OCT imaging with topography analysis can help differentiate focal steepening caused by ectasia, steep central islands, and epithelial deformation. This is crucial for guiding enhancement treatments, which must be tailored to each specific cause, according to David Huang MD, PhD.
Primary versus secondary epithelial effects
In ectasia, weak spots in the cornea bulge forward and increase the local curvature. The epithelium responds to the curvature change by focal thinning in a process called secondary epithelial modulation, Professor Huang explained. Ectatic conditions include keratoconus, post-LASIK ectasia, or pellucid marginal degeneration.
By comparison, conditions such as dry eye, contact lens wear, and exaggerated lid-wiper effect can cause primary epithelial deformation. In these cases, focal epithelium thickening is often associated with topographic steepening.
“These are opposite patterns,” Prof Huang said. “These epithelial thickness variations generally coincide with characteristic corneal steepness and total cornea thickness variations.”
Post-LASIK treatment
Prof Huang noted maps of inferior steepening, posterior cornea elevation, and epithelial thinning coincide in postLASIK ectasia. Treatment options include corneal crosslinking, possibly followed by phototherapeutic keratectomy (PTK). Scleral lenses are another option.
Corneal steepening is also seen with epithelial thinning to compensate in cases of steep central islands, but posterior elevation is normal. Treatment options include topography-guided ablation, transepithelial PTK, and scleral lenses, Prof Huang noted.
However, sometimes due to an exacerbated lid-wiper effect after hyperopic LASIK, corneal steepening is seen in cases of epithelial deformation, but posterior elevation is normal and inferior epithelial thickening is seen, which causes the deformation. “This can be treated with [topography-guided] ablation, but you would want to treat any dry eye first,” Prof Huang said.
Summing up, Prof Huang laid out diagnostic indicators based on OCT mapping for the three conditions:
• Ectasia: anterior topography steepening, posterior topography steepening, epithelial thinning
• Steep central island: anterior topography steepening, posterior topography normal, epithelial thinning
• Epithelial deformation: anterior topography steepening, posterior topography normal, epithelial thickening
Prof Huang made his comments at Refractive Day of the 2025 ASCRS annual meeting in Los Angeles.
David Huang MD, PhD is co-inventor of OCT, holds The Wold Family Endowed Chair in Ophthalmic Imaging, and is professor of ophthalmology and biomedical engineering at Casey Eye Institute, Oregon Health and Science University, Portland, Oregon, US. huangd@ohsu.edu

Expert panel considers tips and tricks for cataracts and compromised corneas.
ROIBEARD O’HEINEACHAIN REPORTS
Cataract surgery in patients with compromised corneas presents many complexities. A recent ESCRS eConnect webinar hosted by Iva Dekaris MD, PhD and Massimo Busin MD gathered a panel of experts to discuss the challenges and innovative solutions available.
Elisabeth Patsoura MD began the discussion by noting cataract surgery always carries some risk to the cornea, especially in eyes with corneal disease. However, a careful, standardised approach can minimise these risks.
She pointed out a significant percentage of cataract patients also have dry eye disease, which can be aggravated by cataract surgery. Factors include preoperative and postoperative medications, the surgical microscope’s phototoxic effects, the corneal incision, and the speculum or docking station.
Fortunately, ophthalmologists can adopt several measures to mitigate the impact of cataract surgery on the ocular surface. These include the use of intracameral mydriatics, the topical application of dispersive ophthalmic viscosurgical devices (OVDs), and reducing the intensity of the microscope
illumination during stages where such bright light is unnecessary. They should also consider postoperative administration of preservative-free topical antibiotics, steroids, and dry eye medications, Dr Patsoura said.
Eyes susceptible to endothelial loss from cataract surgery include those with concurrent corneal pathologies such as Fuchs’ endothelial dystrophy syndrome or even keratoconus. Additionally, eyes with inflammatory ocular diseases, previous angle-closure glaucoma, pseudoexfoliation, shallow anterior chambers, hard nuclei, or systemic conditions such as diabetes are also at risk.
Dr Patsoura observed research has shown a soft-shell OVD technique reduces endothelial cell loss. She added nuclear fragmentation with phaco-chop is better than stop-and-chop and divide-and-conquer techniques because it requires less phaco time and energy. Using torsional phaco is safer than longitudinal phaco for the same reason, and burst mode is also safer than continuous linear mode, especially for corneas with a low endothelial cell count.
Recent IOL power calculation formulas tailored for keratoconus-affected eyes demonstrate reduced prediction errors compared to traditional formulas. The ESCRS IOL power calculator has supported surgeons in performing calculations using these advanced formulas, said Joaquín Fernández MD, PhD.
He noted conventional formulas often lead to a hyperopic shift in keratoconus that increases with each disease stage. The older formulas assume a normal anterior-posterior corneal ratio, which is disrupted in keratoconic eyes. The irregularity of the cornea in such eyes can lead to unreliable keratometry readings. Furthermore, irregular corneas affect vision quality, making refraction measures unreliable and repeatability poor.
Studies comparing the accuracy of older IOL calculation formulas in eyes with keratoconus have consistently shown the SRK/T formula has the lowest prediction errors. However, a recent meta-analysis shows the newer formulas optimised for keratoconus provide results comparable to those achieved in normal eyes. The best performance was reported by the Barrett True-K formula using a measured posterior (BTK-MPC), followed by the Barrett True-K using predicted posterior cornea (BTK-PPC) and the Kane formula.1
Surgeons can access the new formulas with measured posterior cornea through the online ESCRS IOL power calculator. In the case of the BTK formula, surgeons specify the history of keratoconus, whether the posterior cornea is measured or predicted, the biometer used, and whether they will be implanting a toric IOL. In the case of the Kane formula, surgeons simply specify the eye has keratoconus, Professor Fernández said.
Moving the conversation to the surgical stage, Björn Bachmann MD said there are several strategies to enhance visualisation during cataract surgery in patients with opacified corneas.
The primary incision should be opposite the clearest part of the cornea. To achieve a good red reflex, the pupil should be maximally dilated using either pharmaceutical or mechanical methods. Coaxial lighting is preferable over full-field illumination to minimise glare.
When the cataract procedure is combined with vitrectomy, an intravitreal endolight or chandelier is another option. It has the advantage of reduced stray light with little reflection and high contrast. However, it is important to keep the light at a safe distance from the posterior capsule to prevent capsular tears. An anterior light source at a lower intensity will enhance the three-dimensional perception of the intraocular structures.
In triple Descemet membrane endothelial keratoplasty (DMEK) procedures, removing the oedematous corneal epithelium enhances visualisation during cataract surgery. Alternatively, or additionally, glycerine eye drops can be applied. Techniques to avoid staining diseased endothelium with trypan blue include filling the anterior chamber with air before injecting the dye or using OVD and manipulating the cannula near the anterior lens capsule.
In recent years, surgeons have transitioned predominantly to lamellar keratoplasty. At Moorfields Eye Hospital, DMEK accounts for half of the keratoplasty procedures, with one-third involving combined surgery with phacoemulsification, said Alfonso Vasquez-Perez MD.
Combined cataract and DMEK procedures are recommended for Fuchs’ dystrophy patients aged 55 or older with adequate cornea visualisation for safe phacoemulsification, a corneal thickness greater than 640 microns, and diurnal vision fluctuations. It is important to use hydrophobic acrylic IOLs because air tamponade can cause opacifications in hydrophilic lenses. The difference in biometric readings, specifically keratometry, before and after DMEK is minimal.
For cataract patients needing deep anterior lamellar keratoplasty (DALK), sequential surgeries generally provide optimal refractive outcomes. However, for patients without useful vision in the other eye, a combined procedure might be more suitable. In such cases, the combined procedures typically begin with a partial keratectomy to enhance visualisation during the cataract surgery. Manual dissection of the stroma during the DALK procedure may be preferred over the big-bubble technique to avoid the need for conversion to penetrating keratoplasty.
In rare cases, such as a corneal perforation, an open-sky triple procedure may be necessary. General anaesthesia is recommended. After trephination, performing the capsulorhexis in dry conditions with vision blue improves visualisation. Following cataract extraction, it is best to insert the IOL vertically into the bag and finish by suturing the graft.
The webinar can be seen in its entirety on the ESCRS website
For citation notes, see page 32.
Massimo Busin MD is based at University of Ferrara, Ferrara, Italy. mbusin@yahoo.com
Iva Dekaris MD, PhD is based at Eye Hospital Svjetlost, University of Rijeka, Zagreb, Croatia. Iiva.dekaris@gmail.com
Elisabeth Patsoura MD, MRCOphth is based at Ophthalmos Research & Therapeutic Institute, Athens, Greece. ophthalmos@ophthalmos.gr
Joaquín Fernández Pérez MD, PhD is based at Qvision, Department of Ophthalmology of Vithas Almería Hospital, Almería, Spain. joaquinfernandezoft@qvision.es
Björn Bachmann MD, FEBO is based at University Eye Clinic, Cologne, Germany. bjoern.bachmann@uk-koeln.de
Alfonso Vasquez-Perez MD, FRCOphth, CertLRS, FEBOS-CR is based at Moorfields Eye Hospital, London, UK. alfonsoperez.1@nhs.net
Understanding the nomenclature and techniques.
BY SOOSAN JACOB MS, FRCS, DNB
Optical quality of the eye is affected not just by higher-order aberrations (HOAs) but also by diffraction and scatter. Thus, even the perfect lens has a limit to its resolution.
Fraunhofer diffraction occurs when light passes through a circular aperture, known as an Airy disc. The Airy disc or pattern refers to the best possible focused spot of light created by the diffraction pattern formed when light passes through a perfect lens with a circular aperture. A uniformly illuminated circular aperture creates a bright central spot, followed by a series of concentric rings. An optical system where the resolution is not limited by any HOAs but only by diffraction is called a diffraction-limited optical system. Except with a very small pupil, even the best eyes have optical quality below the diffraction limit.
Ocular scatter can degrade the visual image just as HOAs and diffraction can. This occurs due to light passing through media with optical inhomogeneity—i.e., spatial variations in the refractive index. Scatter is due to a combination of refraction, reflection, and diffraction. For example, scatter can occur secondary to a synthetic intracorneal ring segment within the cornea of a different refractive index. Incident light would get partly reflected, partly refracted, and partly undergo internal reflections before getting refracted/reflected again. Light falling at the edge would also undergo diffraction. These phenomena cause retinal image degradation, resulting in glare and hazy vision. Scatter causes local disturbances to the wavefront but are not responsible for shape errors.
Discussed in part one of this series (May/June 2025 issue), HOAs are basically responsible for an irregular wavefront as opposed to a plane (parallel rays) or spherical (converging or diverging rays that come to a point focus) wavefront. HOAs are primarily due to corneal pathology, although other conditions such as crystalline lens or the IOL may also be responsible. Total ocular aberrations are composed of corneal aberrations and internal aberrations.
This quantifies the overall magnitude of wavefront deviations from an ideal wavefront. It is plotted in microns on the exit pupil and dependent on pupil size. Aberrometry refers to measurement of the HOAs. Aberrometers are used to mea-
sure the ocular monochromatic HOAs. The result is shown as an aberration map describing the variation in the optical path distance from the source to the retinal image through each point of the pupil. It is important to look at not only the magnitude of each mode but also the possible combinations, as certain combinations can change overall retinal image quality and, therefore, visual acuity. Many devices can measure ocular aberrations:
Hartmann-Shack aberrometer A narrow laser beam is focused on the retina to generate a point source. The outcoming light rays experiencing all the ocular aberrations are split into multiple focal spots by a lenslet array on a CCD camera, with their displacement from the ideal used to reconstruct the wavefront. This is less effective for highly irregular corneas such as keratoconus and post-surgical corneas. Examples include the Zywave aberrometer (Bausch + Lomb) and VISX WaveScan (AMO).
Tscherning aberrometer A grid of laser spots is projected onto the retina, and a camera captures the distorted pattern to determine wavefront errors. This can work better in cases with highly irregular corneas but is less commonly used. The WaveLight Allegro Analyzer (Allegro) is one example.
Raytracing aberrometer A thin laser beam is directed into the eye parallel to the visual axis. Each entrance point provides a projection on the retina, which is measured. A set of entrance points forms a set of projections, and a refraction map is reconstructed from these data. It works well in highly aberrated eyes. The iTrace (Tracey Technologies) is an example.
Dynamic skiascopy Dynamic skiascopy is based on principles of time-based clinical retinoscopy. A projecting apparatus shines a scanning slit of light through a projecting lens and a set of mirrors. This light reflected off the retina passes through another lens (a receiving lens) and an aperture, ending on a set of photodetectors. Both the projecting and receiving systems rotate synchronously, allowing a comparison between the perceived light and the initially projected slit-shaped beams of light. The OPDScan aberrometer (Nidek) is an example.
Anterior and posterior corneal surface mapping The anterior and posterior corneal surfaces can be mapped

by different machines, and Zernike polynomials can be calculated from this data. Examples include the Placido disc for anterior corneal surface, OCT for posterior corneal surface in the MS-39 (CSO), and Scheimpflug imaging for both corneal surfaces in the Pentacam (Oculus).
Zernike modes
The wavefront error (WE) can be decomposed as a sum of weighted Zernike modes. The root mean square (RMS) allows quantification. Once measured, a series of polynomials is used to describe the wavefront. Each polynomial describes a mathematical wavefront shape, and the coefficient of each polynomial gives the weight of that aberration in the total wavefront map. The RMS of a perfect optical system is 0.00 microns. Mean RMS is 0.10 microns at 30 years and 0.25 microns at 60 years. The Zernike pyramid has many modes. Let us consider some of these:
Piston (Z00 ) Not a true optical aberration, as it does not model curvature in the wavefront and does not affect image quality. It causes a full shift of the image.
Tip/tilt Also not a true optical aberration, as it neither models curvature in the wavefront nor affects image quality. Horizontal tilt (Z1 -1) shifts the image vertically while vertical tilt (Z11) shifts the image horizontally. Tilting the wavefront in one or two principal meridia causes a slant in the image.
Defocus, astigmatism These are the second-order aberrations that constitute the lower-order aberrations (LOAs), corrected with spherocylindrical glasses.
Coma Coma is a third-order aberration and causes a comet-shaped pattern, i.e., a point of light with a ‘tail’ (see figure). It has an area of myopia adjacent to an area of hyperopia in the same meridian. Vertical (Z3 -1) and horizontal (Z31) coma are denoted in the Zernike pyramid. The optical asymmetry causes some rays to focus incorrectly, creating coma. When peripheral rays focus earlier than paraxial rays, a smaller image (lower magnification) is produced, referred to as negative coma. If peripheral rays are focused
further than paraxial rays along the optical axis, they produce a larger image (greater magnification), and the aberration is termed positive coma.
Images of points far away from the optical axis are not sharp but comet-shaped since the images created are of increasing ring size. Each ring is the image generated from a specific area of the cornea, thus forming a comet shape. The ‘comet’ may have its ‘tail’ pointing away from or towards the optical axis, depending on whether the coma aberration is positive or negative, respectively, assuming there is no defocus in the system. Coma interacts with the presence of other LOA and HOA, meaning its effects become more complex and may not exactly follow the positive/negative classification.
In keratoconus, light from the retina exits the eye faster from the superior cornea and is delayed leaving the inferior cornea. This gap is magnified further because light exiting superior cornea starts travelling even faster as air has lower refractive index, which creates vertical coma aberration.
Trefoil Trefoil is another third-order aberration. It is a triangular astigmatism with three axes. Orientation varies between 30 and 150 degrees, and the values are repeated twice more every 120 degrees. Vertical trefoil (Z3 -3 , 90-210330 degrees) is more frequent than horizontal (Z3 3, 30-150270 degrees). Normal value ranges between 0.00 and 0.50 microns at a mean pupil diameter of 6.5 mm (< 0.25 is associated with better vision).
Trefoil has a lesser effect on image quality compared to an equal amount of coma. In most people, vertical trefoil is coupled with vertical coma, resulting in a better image quality than the trefoil or coma independently. People with large amounts of aberrations (RMS > 0.4) sometimes have coma-trefoil vertical coupling, which helps keep their acuity at good levels. In aberrated eyes, the interaction depends on the phase of the HOA, and improvement/ degradation can occur. Trefoil can cause glare and halos.
Spherical aberration (Z40) Positive and negative spherical aberration—it can cause a decrease in contrast
sensitivity and halos around light. Negative spherical aberration has been used to increase depth of focus. Spherical aberration will be discussed in detail in the next part of this series.
Secondary astigmatism It can have an oblique (Z4 -2 , 45 degrees/135 degrees) or horizontal/vertical (Z42, 0 degrees/90 degrees, WTR/ATR) orientation, is a complex, non-symmetrical wavefront distortion, and has a four-lobed pattern that cannot be fully corrected with regular cylinder.
Quadrafoil and horizontal/vertical (Z
Secondary coma [Vertical (Z (Z foil (Z fifth-order aberrations.
Aberropia
Just as myopia, hyperopia, and astigmatism refer to certain types of refractive errors, a decrease in the visual quality or
quantity secondary to higher-order aberrations also needs to have a well-defined nomenclature. The often-used blanket term, irregular astigmatism, is a misnomer—for example, when considering the central column of the Zernike pyramid with rotationally symmetrical modes. We therefore coined the term aberropia in 2002 to denote refractive errors secondary to HOA. Aberropia results in a large circle of blur, increased point spread function, and decreased quality of vision. It can be congenital or acquired and can arise from the tear film (uneven tear film), cornea (keratoconus, post-LASIK ectasia, post-keratoplasty, corneal scars), lens (incipient cataract, subluxation, lenticonus, capsular striae), IOL (subluxated or decentred IOL, multifocal/extended depth of focus IOLs, other newer aberration-based IOLs), vitreous (vitreous floaters, opacities), or even retina (thickened hyaloid, fine epiretinal membrane).
This is the second in a multipart tutorial on higher-order aberrations.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.

Committee representatives of ESCRS organise and present sessions at meetings organised by our national and sister societies. These sessions are typically delivered by a group of speakers on a current topic selected by ESCRS in person or virtually.
These sessions provide useful education as well as collaboration between societies promoting and sharing benefits across both memberships.
escrs.org/education/academies/

ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.
Automated gonio lens-free procedure increases efficiency without sacrificing outcomes.
CHERYL GUTTMAN KRADER REPORTS
Adopting direct selective laser trabeculoplasty (DSLT) offers a solution for helping glaucoma specialists and general ophthalmologists meet the increasing demand for services from the expected growing population of patients with glaucoma, according to Christine Funke MD.
“I am using DSLT frequently in my clinic, and I think and hope this machine will help push the envelope so SLT is used more as first-line therapy for IOP lowering,” Dr Funke said. “DSLT is a simple and user-friendly procedure. By eliminating the need for a gonio lens, it also means there should be no more excuses for not doing SLT.”
DSLT provides a fully automated and precise laser treatment to the trabecular meshwork, and the procedure is both user- and patient friendly. It is performed in most cases with patients standing in front of the machine. After placing a lid speculum and completing the alignment, the treatment itself takes just 2.5 seconds per eye.
Most patients are more comfortable having the procedure done while they are standing, and the experience for them is almost like having a photo taken.

Disposable lid speculums are provided by the manufacturer. To enable a 360-degree view of the sclera, Dr Funke recommended manually prying the speculum open.
During the entire procedure, she uses ‘verbal anaesthesia,’ walking the patients through each step.
If both eyes need treatment, Dr Funke prefers to perform simultaneous bilateral DSLT.
“I know I get less reimbursement for the same-day approach, but I like to make the procedure as efficient as possible,” she said. “The patients are very happy to get both treatments done in one visit.”
“Most patients are more comfortable having the procedure done while they are standing, and the experience for them is almost like having a photo taken,” Dr Funke explained. “Patients simply have to keep the eye open and stare at the fixation light, but I do have a staff person assist with stabilisation by placing a hand on the back of the patient’s head.”
Offering more pearls for success with DSLT, Dr Funke noted patients feel the treatment more than they do during traditional SLT, so she recommended bolstering the pretreatment topical anaesthesia regimen. Dr Funke’s protocol includes two rounds of proparacaine drops followed by tetracaine. She also prescribes topical prednisolone three times a day for 3 days postoperatively because the eye may be more sensitive after DSLT than SLT.
Dr Funke observed that it can take a little longer to achieve correct eye alignment with DSLT, especially for new users. Therefore, she advised placing the lid speculum after completing alignment to avoid excessive ocular surface drying.
Dr Funke said that her clinical experience with DSLT is consistent with the results of the 12-month controlled GLAUrious trial showing that the benefits of DSLT for lowering IOP and medication use are similar to SLT.
“DSLT is an absolute game changer if you want to be more efficient with laser trabeculoplasty,” Dr Funke said. “Because it allows us to increase our treatment volume and availability, I would still be happy to use it instead of SLT, even if its efficacy was slightly less.”
Dr Funke spoke at the 2025 ASCRS Glaucoma Specialty Day in Los Angeles.
Christine Funke MD is a fellowship-trained glaucoma specialist in private practice at Barnet Dulaney Perkins Eye Center, Phoenix, Arizona, US. christine.funke@bdpec.com
Bausch + Lomb has received CE Mark approval for its LuxLife full range of vision intraocular lens (IOL). The preloaded, non-diffractive IOL with Pure Refractive Optics (PRO) technology provides continuous vision from distance to near. The lens comes in cylinders from +0.75 D to +6.00 D and features a dual injector system for various injection techniques during implantation. bausch.com
Rayner has announced its receipt of the King’s Award for Enterprise 2025. The award honours RayOne EMV, an innovative IOL developed with Professor Graham Barrett and launched in 2020. This lens extends a patient’s range of vision by up to 1.50 D using a patented non-diffractive optic profile with controlled positive spherical aberration, offering monofocal levels of contrast sensitivity, low dysphotopsia, and high patient satisfaction. rayner.com
Amgen announced that teprotumumab (Tepezza, Amgen) has received marketing authorisation from the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) as the first therapy specifically licensed for treating adult patients with moderate-to-severe thyroid eye disease (TED). amgen.com
Viridian Therapeutics announced it received a breakthrough therapy designation from the US FDA for veligrotug, a drug candidate for thyroid eye disease (TED). The designation was based on the drug’s significant improvement and resolution of diplopia in chronic TED, and its rapid proptosis response. Viridian completed two phase 3 trials, which showed veligrotug met primary and secondary endpoints and was well tolerated. The company plans to submit a Biologics License Application to the FDA later this year, with a US launch expected in 2026 if approved. viridiantherapeutics.com
Topcon has announced new initiatives to expand its role in digital medicine, including the launch of the Institute of Digital Health (IDHea), an ocular data-as-a-service platform designed to offer AI-powered analytics and connectivity for medical research. Additionally, Topcon has collaborated with Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology to create Cascader Limited, which aims to use AI to detect and manage eye diseases and other systemic conditions. Topcon has also acquired RetInSight, a company producing AI algorithms to analyse optical coherence tomography (OCT) images to detect and monitor major retinal diseases. Furthermore, Danish MedTech company EYE-GO announced that Topcon Healthcare will become a strategic investor, supporting the development of MistGo® Digital, a new microdosing drug delivery system with a digital adherence monitoring platform. topconhealthcare.com

A recent report recommends the establishment of a new task force, akin to the Ophthalmic Instrument Cleaning and Sterilization Task Force, to address high-level disinfection (HLD) requirements imposed by regulatory bodies and hospital infection control groups for ophthalmic outpatient clinics. The report proposes these agencies employ an outdated classification system to criticize ophthalmologists for not adhering to HLD as specified in newer manufacturer instructions for use. This classification categorizes devices—such as ultrasound probes, fundus and laser contact lenses, and gonioscopy lenses—alongside other medical instruments like gastrointestinal endoscopes, laryngoscope blades, and anorectal manometers, thereby mandating HLD. However, there have been no instances where the ophthalmic devices in question have been linked to the spread of infection. Given the significant OR turnover time required for HLD, clinics are compelled to purchase additional devices to maintain patient volume. Consequently, the report says manufacturers lack the motivation to develop sustainable or reusable devices. IC Kuo. “Disinfection of outpatient ophthalmic devices: a critique of ‘semicritical‘ designation,” 51(5): 355–358.
Preoperative lens tilt varies widely among patients, with some cases exceeding a threshold that could affect postoperative refractive outcomes, according to a retrospective study. The study evaluated preoperative biometry data and anterior segment OCT images from 4,689 eyes of 2,489 cataract patients through optical biometry (IOLMaster 700, Zeiss) and AS-OCT. Using logistic regression and machine learning, correlations were found between lens tilt and biometry parameters such as anterior chamber depth, axial length, equator thickness, and lens decentration. The mean lens tilt was 4.9 degrees, with 6.7% of eyes having a tilt greater than 7.0 degrees. A predictive model for assessing tilt risk showed an accuracy with an area under the curve of 0.862. Given correlations between preoperative lens tilt and postoperative IOL tilt, this model could improve future IOL power calculations and visual outcomes in cataract patients.
H Khalil, et al. “MD Quantification of physiological tilt of the phakic eye using biometry parameters and AS-OCT,” 51(5): 366–370.
DEMODEX EXACERBATES MEIBOMIAN GLAND DYSFUNCTION
Demodex blepharitis (DB) can significantly exacerbate meibomian gland dysfunction (MGD), according to the results of a retrospective study. The study’s authors reviewed the case records of 438 patients with data available for collarettes and MGD signs (telangiectasia, meibum expressibility, meibum quality, and meibography). Among all patients with MGD, 45% were found to have DB. Conversely, among patients with moderate-to-severe DB (collarettes grades 2 to 4), 96% to 99% were found to have MGD grade 2 to 4 meibum quality or grade 1 to 4 MG atrophy. Structural and functional measures of MGD were significantly worse in eyes with collarette grades 2 to 4 than in those with collarette grade 0.
E Yeu, et al. “Meibomian gland structure and function in patients with Demodex blepharitis,” 51(5): 359–365.

Patients are understandably curious to learn as much as they can about their upcoming cataract or refractive surgery. ESCRS has developed a Patient Portal on its website to help inform patients about these surgeries.
The Portal is split into two sections: Cataract and Refractive. Each section provides an easy-to-understand summary of the different types of conditions, including the benefits, risks, procedures, and aftercare of common conditions. Each section is easily navigable, with clear diagrams and a glossary to convey all the information patients might need to help prepare for surgery or during aftercare.
Towards a Unified IOL Classification
Page 8
1. Ribeiro F, et al. “Evidence-based functional classification of simultaneous vision intraocular lenses: seeking a global consensus by the ESCRS Functional Vision Working Group,” J Cataract Refract Surg, 2024 Aug; 50(8): 794–798.
2. Ribeiro F, et al. “Should enhanced monofocal intraocular lenses be the standard of care? An evidence-based appraisal by the ESCRS Functional Vision Working Group,” J Cataract Refract Surg, 2024 Aug; 50(8): 789–793.
A Game-Changer in Spectacle Independence?
Page 12
1. Fernández J, et al. “Visual and patient-reported outcomes of an enhanced versus monofocal intraocular lenses in cataract surgery: a systematic review and meta-analysis,” Eye, 2025; 39: 883–898.
2. Fernández J, et al. “Standard for collecting and reporting outcomes of IOL-based refractive surgery: update for enhanced monofocal, EDOF, and multifocal IOLs,” J Cataract Refract Surg, 2022; 48: 1235–1241.
3. Fernández J, Rocha-De-Lossada C, Rodríguez-Vallejo M. “Recommendations for Writing Clinical Research Manuscripts: From Monofocal to Multifocal Intraocular Lenses,” Int J Environ Res Public Heal, 2022; 19: 17036.
Pros and Cons of Phakic IOLs
Page 14
1. Stodůlka P, Slovak M, Sramka M, Polisensky J, Liska K. “Posterior chamber phakic intraocular lens for the correction of presbyopia in highly myopic patients,” J Cataract Refract Surg, 2020 Jan; 46(1): 40–44. doi:https://doi. org/10.1097/j.jcrs. 0000000000000033
2. Taneri S, Dick HB. “Initial clinical outcomes of two different phakic posterior chamber IOLs for the correction of myopia and myopic astigmatism,” Graefes Arch Clin Exp Ophthalmol, 2022 May; 260(5): 1763–1772. doi:https://doi.org/10.1007/ s00417-021-05465-w
3. Kilic D, Förster A, Mertens E, Dick HB. “Rotational Stability After Implantation of Two Different Phakic Toric Intraocular Lenses,” J Refract Surg, 2023 Jul; 39(7): 463–472. doi:https:// doi.org/10.3928/1081597X-20230512-03
4. Packer M, Alfonso J, Aramberri J, Elies D, Fernández J, Mertens E. “Performance and Safety of the Extended Depth of Focus Implantable Collamer Lens (EDOF ICL) in Phakic Subjects with Presbyopia,” Clin Ophthalmol, 2020 Sept 18; 14: 2717–2730. doi:https://doi.org/10.2147/opth.s271858
AI Shows Promise for Meibography Grading
Page 15
1. Arita R, Suehiro J, Haraguchi T, Shirakawa R, Tokoro H, Amano S. “Objective image analysis of the meibomian gland area,” Br J Ophthalmol, 2014; 98(6): 746–755. doi:https://doi.org/10.1136/bjophthalmol-2012-303014
When Is It Time to Remove a Phakic IOL?
Page 18
1. Alió JL, et al. Ophthalmology, 2006 Dec; 113(12): 2213–2220.
2. Jonker SMR, et al. Ophthalmology, 2018 Apr; 125(4): 486–494.
3. Jonker SMR, et al. Am J Ophthalmology, 2018 Oct; 194: 110–119.
4. Nakamura T, et al. Am J Ophthalmology, 2019 Oct; 206: 1–10
No Surgical Surprises
Page 19
1. Schallhorn SC, et al. “Effect of residual sphere on uncorrected visual acuity and satisfaction in patients with monofocal and multifocal intraocular lenses,” J Cataract Refract Surg, 2024 Jun 1; 50(6): 591–598.
2. Trattler WB, et al. “The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye,” Clin Ophthalmol, 2017 Aug 7; 11: 1423–1430.
Delivering Uncompromising Cataract Care
Page 22
1. O Reitblat, et al. “Intraocular lens power calculation accuracy in patients with keratoconus: Network meta-analysis and systematic review,” Clinical & Experimental Ophthalmology, 2024 Dec 3. doi:https://doi.org/10.1111/ceo.14470
September 4–7 EURETINA
Paris, France
September 12–16
2025 ESCRS Congress Copenhagen, Denmark
September 12
ESCRS iNovation Day Copenhagen, Denmark
September 25–28
German Ophthalmology Society Berlin, Germany
October 18–20
American Academy of Ophthalmology Orlando, Florida, US

25 Sept


18 Oct



1-4
• Myopic shift
• Cyclodialysis
• Hypotony
• Significant hyphema ZERO
• Stent dislocation
SAFETY1,2
OVERALL SAFETY PROFILE SIMILAR TO CATARACT SURGERY ALONE3
SIGNIFICANT IMPROVEMENTS IN VISION-RELATED QUALITY OF LIFE5
REFRACTIVELY NEUTRAL5,6,8,9 FEWER FOLLOW-UP VISITS4 DAILY ACTIVITIES7 MENTAL HEALTH7
IMPROVES OCULAR SURFACE HEALTH6,9
REDUCTION IN PATIENTS WITH SEVERE OSD SYMPTOMS5 72%
WITHIN ± 1.0D OF REFRACTIVE TARGET8 99%
1. 7-Year Efficacy and Safety of iStent inject® Trabecular Micro-Bypass in Combined and Standalone Usage. Fritz H. Hengerer . Gerd U. Auffarth . Ina Conrad-Hengerer. 2. Ten-Year Effectiveness and Safety of Trabecular Micro-Bypass Stent Implantation with Cataract Surgery in Patients with Glaucoma or Ocular Hypertension. Tobias H. Neuhann, Raphael T. Neuhann, Dana M. Hornbeak. 3. Samuelson, Thomas W., et al. “Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results.” Ophthalmology 126.6 (2019): 811-821. 4. Rodriguez-Una, Ignacio, Augusto Azuara-Blanco, and Anthony J. King. “Survey of glaucoma surgical preferences and post-operative care in the United Kingdom.” Clinical & Experimental Ophthalmology 45.3 (2017): 232-240. 5. Samuelson, Thomas W., et al. “Quality of life in primary open-angle glaucoma and cataract: an analysis of VFQ-25 and OSDI from the iStent inject® pivotal trial.” American Journal of Ophthalmology 229 (2021): 220-229. 6. Schweitzer, Justin A., et al. “Prospective interventional cohort study of ocular surface disease changes in eyes after trabecular micro-bypass stent (s) implantation (iStent or iStent inject) with phacoemulsification.” Ophthalmology and Therapy 9 (2020): 941-953. 7. Jones, Lee, et al. “Impact of minimally invasive glaucoma surgery on the ocular surface and quality of life in patients with glaucoma.” Therapeutic Advances in Ophthalmology 15 (2023): 25158414231152765. 8. Ioannidis, Alexandros S., et al. “Refractive outcomes after trabecular micro-bypass stents (iStent inject®) with cataract extraction in open-angle glaucoma.” Clinical Ophthalmology (2020): 517-524. 9- Biela, Katarzyna, et al. “Dry eye disease as a cause of refractive errors after cataract surgery–A systematic review.” Clinical Ophthalmology (2023): 1629-1638.
iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATIONS FOR USE: The iStent inject® W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject® W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject® W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS: • For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body.