IN THIS ISSUE:
Update on LightAdjustable IOLs
LALs finding their place as choice for post-refractive surgery patients.

IN THIS ISSUE:
Update on LightAdjustable IOLs
LALs finding their place as choice for post-refractive surgery patients.
Quick response and modern imaging help treat postoperative problems of corneal refractive surgery.
Faricimab a Promising Treatment for Corneal Neovascularisation English study shows clinical benefits in complex cases.
Major shift in microbiological profile of infectious keratitis post-COVID.





WITH PARTICIPATION OF THE FINNISH SOCIETY OF OPHTHALMOLOGY
The ESCRS Winter Meeting is known for offering an intimate and focused forum for discussion and learning about advancements in cataract and refractive surgery. Join your colleagues for three days of collaborative sessions and immersive learning opportunities at the Messukeskus Helsinki Exhibition and Convention Centre, 06–08 March 2026.
The 2026 Winter Meeting will combine the intellectual vigour of ESCRS, Europe’s leading organisation devoted to the study and practice of anterior segment surgery, with the sophisticated urban culture of Helsinki, a vibrant city known for its relaxed lifestyle and coastal nature.
Join fellow ophthalmologists, researchers, and industry experts at this can’t-miss event. Registration details coming soon!
Addressing Postoperative Visual Complications
Managing aberrations after laser refractive surgery requires a multi-layered approach.
Update: 3D Printing Helps Transform Ukrainian
Care Oksana Petrenko MD 07 ESCRS Update: New Members Elected to Council of Management; Support for Projects Offsets Most Congress Emissions; Winning Essay Says ‘Collective Desire’ Must Drive DEI Implementation
Improving Outcomes with Laser-Assisted Surgery
14 Understanding Long-Term Regression
Sara Sella MD
15 Fine-Tuning IOLs After Surgery
Mark A Kontos MD
16 Matching Premium IOLs to Visual Lifestyles
Andreas F Borkenstein MD
18 Need to Know: Wavefront Filtering and PPP for Aberropia
Soosan Jacob MS, FRCS, DNB
20 Emerging Microbial Trends That Could Affect Your Practices
Kyung Sun Na MD, PhD
21 Getting to the Crux of DSAEK Cuts
Thorbjörg Olafsdottir MD
22 Dedicated PCR Infection Panel to Speed Up Diagnosis
Madhavan Rajan MBBS, MS, MD, FRCSEd, FRCS(Glas), FRCOphth
23 Novel Anti-VEGF for Corneal Neovascularisation Posts Positive Results
Magdalena Niestrata PhD(Dist), MSc(Dist), MBCh(Hons), BSc(Hons), PGDip(Dist), FRCOphth, FEBO, FICO
24 Could the Corneal Transplant Pool Increase?
Gilles Thuret MD, PhD, IUF
25 Going Dutch on Acanthamoeba Keratitis
Yexin Ye MD, BSc
26 Getting to the Core of NetarsudilAssociated Honeycombing
Ursula Schlötzer-Schrehardt PhD
28 IOP Effects of Intravitreal Injections
Lilian Nguyen MD




Publisher
Filomena Ribeiro
Executive Editor
Stuart Hales
Editor-In-Chief
Sean Henahan
Senior Content Editor
Kelsey Ingram
Creative Director
Kelsy McCarthy
Graphic Designer
Jennifer Lacey
Circulation Manager
Lucy Matthews
Contributing Editors
Cheryl Guttman Krader
Howard Larkin Roibeárd O’hÉineacháin
Contributors
Laura Gaspari
Soosan Jacob
Priscilla Lynch
Timothy Norris
Andrew Sweeney
Colour and Print
CitiPost
Advertising Sales
Roo Khan
MCI UK
Tel: +44 203 530 0100 | roo.khan@wearemci.com
EuroTimes® is registered with the European Union Intellectual Property Office and the US Patent and Trademark Office.
Published by the European Society of Cataract and Refractive Surgeons, Suite 7–9 The Hop Exchange, 24 Southwark Street, London, SE1 1TY, UK. No part of this publication may be reproduced without the permission of the executive editor. Letters to the editor and other unsolicited contributions are assumed intended for this publication and are subject to editorial review and acceptance.
ESCRS EuroTimes is not responsible for statements made by any contributor. These contributions are presented for review and comment and not as a statement on the standard of care. Although all advertising material is expected to conform to ethical medical standards, acceptance does not imply endorsement by ESCRS EuroTimes. ISSN 1393-8983

Learn more about EuroTimes or connect with ESCRS at ESCRS.org
The evolution of ophthalmic surgery is a continuous process of innovation, building on previous advances, while trying to resolve any complications by refining techniques. The technological progress in this field has been a remarkable, relentless stream of new ideas tackling old problems.
This year marks the anniversary of some of the key technological turning points in ophthalmic surgery: It is the 120th anniversary of penetrating keratoplasty. In 1905, Dr Eduard Zirm performed the first full-thickness human-human corneal graft. This has since become the most widely performed and successful form of human tissue transplantation. While various lamellar techniques now offer options for select candidates, full-thickness grafts are still widely performed.
Eye surgeons who attended the 2025 ESCRS Annual Congress in Copenhagen received an update on current lamellar techniques, such as ultra- and nanothin Descemet stripping automated endothelial keratoplasty (DSAEK) and DSO/ Descemetorhexis without endothelial keratoplasty (DWEK). Attendees also received a preview of the surgical approaches in development to help overcome some of the limitations of the current ones, including techniques for corneal regeneration, such as stem cells, cultured endothelial cells, hydrogels, and 3D bioprinting.
Depending on the account, this year also represents the 75th or 76th anniversary of Sir Harold Ridley’s daring and innovative implantation of the first intraocular lens— discussed in detail in Dr Patrick Condon’s new book (Eye Healthcare, a 90-Year History of Progress), introduced in Copenhagen. The book reviews significant developments
in cataract and refractive surgery and outlines the people and decisions that led to the creation of ESCRS, JCRS, and EuroTimes. Royalties from the book will go to the Ridley Eye Foundation charity.
An interview with Dr Condon by Dr Richard Packard will appear on the ESCRS website in the heritage section, which also hosts the ESCRS interactive timeline on the history of cataract and refractive surgery. In one video on the site, Professors Thomas Neuhann and Reinhard Koch recount the evolution of IOL surgery from perilous to commonplace. The professors describe early phaco surgery uncertainties, industry struggles, and the genius of visionaries such as Drs Charles Kelman and Richard P Kratz.
The Copenhagen meeting also marked the 35th anniversary of LASIK. Another video on the web page features a discussion between LASIK pioneer Prof Ioannis Pallikaris and Prof H Burkhard Dick about his early experiences.
The Annual Congress also celebrated the 30th anniversary of the first use of femtosecond lasers in ophthalmic surgery, featuring a special timeline exhibition showcasing the history and advancements of femtosecond lasers from their inception to present-day innovations. The celebration included live video interviews with femtosecond laser pioneers Drs Ron Kurtz, Tibor Juhasz, and Burkhard Dick, which will also appear on the ESCRS website.
See you online!
Sean Henahan Editor-in-Chief
EDITORIAL BOARD

Adi Abulafia (Israel)
Bruce Allan (UK)
Noel Alpins (Australia)
Juan Alvarez de Toledo (Spain)
Gerd Auffarth (Germany)
Başak Bostanci (Turkey)
John Chang (Hong Kong SAR, China)
Béatrice Cochener-Lamard (France)
Burkhard Dick (Germany)
Mor Dickman (The Netherlands)

Joaquín Fernández (Spain)
Oliver Findl (Austria)
Nicole Fram (US)
Sri Ganesh (India)
Farhad Hafezi (Switzerland)
Nino Hirnschall (Austria)
Soosan Jacob (India)
Jack Kane (Australia)
Yao Ke (China)
Mika Kotimäki (Finland)
David Lockington (UK)
Artemis Matsou (Greece)
Cyres Mehta (India)
Jod Mehta (Singapore)
Sorcha Ní Dhubhghaill (Belgium)
Rudy Nuijts (The Netherlands)
Catarina Pedrosa (Portugal)
Konrad Pesudovs (Australia)
Nic Reus (The Netherlands)
Filomena Ribeiro (Portugal)
Andreia Rosa (Portugal)
Giacomo Savini (Italy)
Julie Schallhorn (US)
Sathish Srinivasan (UK)
Paolo Vinciguerra (Italy)
Shin Yamane (Japan)
Ron Yeoh (Singapore)
Mihail Zemba (Romania)

ESCRS’s vision is to educate and help our peers excel in our field. Together, we are driving the field of ophthalmology forward.
The country’s ophthalmologists offer valuable experience in treating ocular trauma and prosthesis design.
ANDREW SWEENEY
REPORTS
What happens to a country’s healthcare system at war? Lessons learned often lead to innovations discovered. In Ukraine, one of these pearls of wisdom is prostheses development.
The Russian invasion of Ukraine is now in its fourth year, and the war makes for grim reading. Moscow’s casualties are reported to have reached more than 1 million, while Ukrainian dead, wounded, and missing (soldiers and civilians alike) are estimated at around 400,000.
Every aspect of Ukrainian medicine has been affected, including ophthalmology. Since the moment Russian tanks moved across the border, the ESCRS has committed more than €1 million to assist Ukraine’s ophthalmologists, providing direct assistance to 26 clinics and ophthalmic departments across the country.
Yet despite the support of organisations like the ESCRS and international governments, significant challenges remain. Ophthalmologists who faced high patient volumes before the war must now contend with increasingly complex cases.


“The peculiarity of modern combat injuries to the visual organs involves multiplicity of injuries, contusion syndrome, and combined and associated injuries in 85–90% of injuries,” said Oksana Petrenko MD, one of Ukraine’s leading ophthalmic reconstructive surgeons. “These injuries are severe, and bilateral damage to the visual organs occurs in up to 60% of cases.”
Professor Petrenko’s caseload has increased exponentially since the full-scale war began. Civilians and soldiers alike have come under her care, many suffering from catastrophic ocular injuries and some who were previously denied treatment.
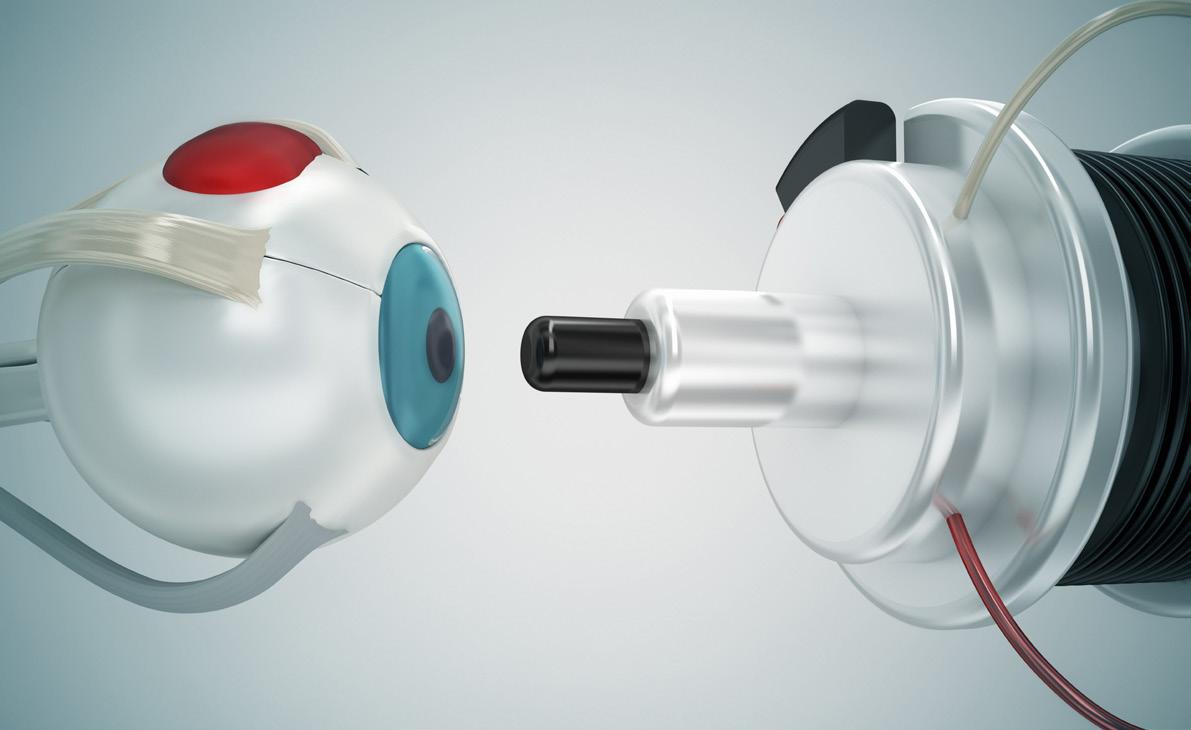
In one case, Prof Petrenko treated a male patient who had suffered the unilateral loss of his left eye (including the eyelid) in Mariupol, a city in eastern Ukraine occupied by Russia after fierce fighting in 2022. He had been shot in the left eye, with the bullet exiting above the left ear. (see image 1)
Despite being refused treatment by Russian military personnel, the patient somehow survived these injuries and managed to escape to Ukrainian-held territory after several months. The patient is now healthy, despite suffering serious infections as a result of his ordeal.
“We have seen 320 patients with catastrophic trauma like this patient since February 2022—all involving trauma and maxillofacial eye trauma,” she said. “This has turned us into a multidisciplinary team.”
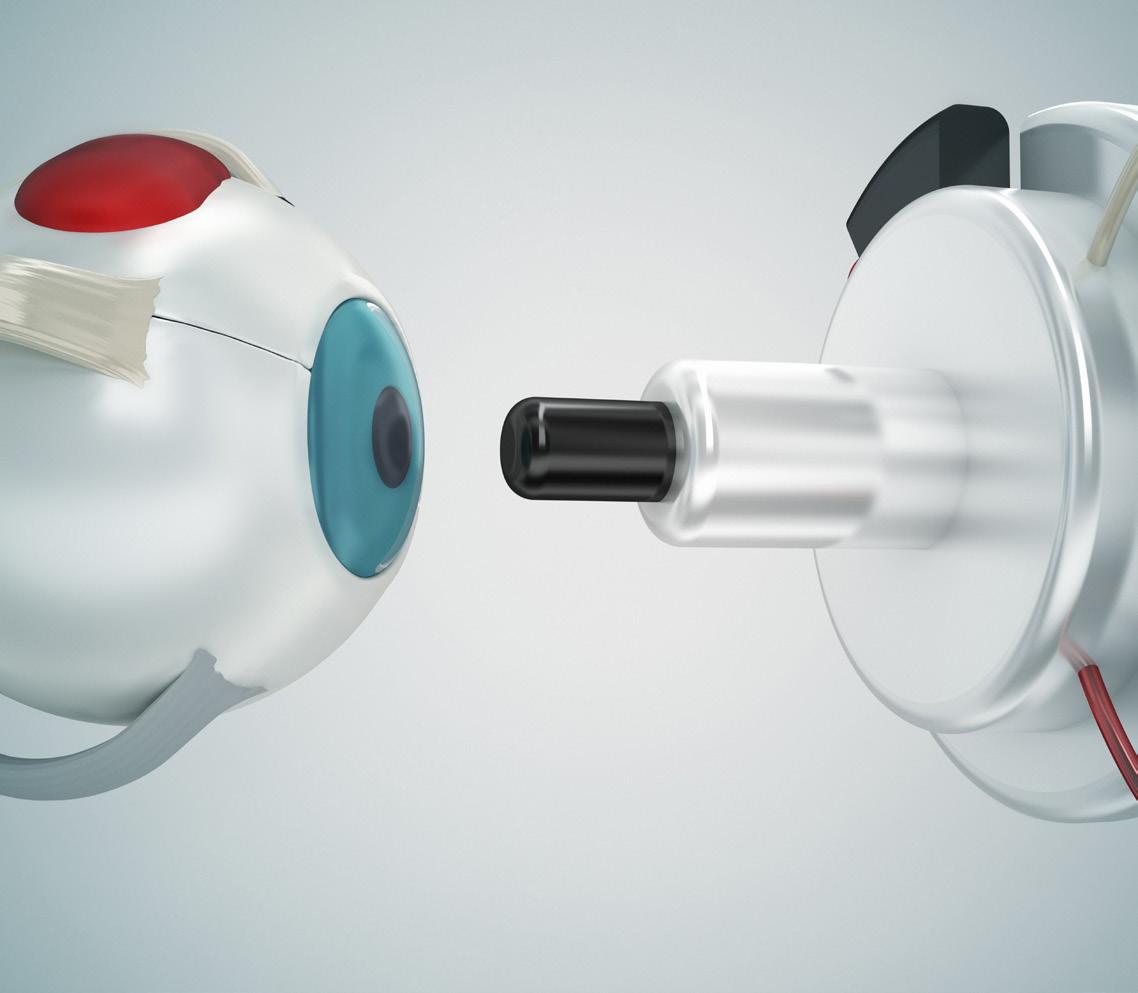
The most noteworthy aspect of this multidisciplinary approach is the work of Prof Petrenko and her colleagues in creating high-quality prostheses, primarily for those patients who have suffered mine blast injuries. The patient first undergoes a CT scan, the results of which are processed via a 3D printer to create individualised prostheses.
After enucleation or evisceration, an acrylic or silicone conformer is placed in the conjunctival fornix to maintain the conjunctival cavity. While this cannot provide sight, the procedure offers “cosmetic rehabilitation in patients afflicted with psychological problems, which disrupts their social adaptation,” according to Prof Petrenko.
“It is important to form a movable stump with sufficient volume to ensure their medical and psychological rehabilitation. The ocular prosthesis not only eliminates the cosmetic defect but also protects the cavity, maintains its shape, and ensures the correct positioning of the eyelids.”
One case Prof Petrenko was keen to highlight involved a soldier who had sustained catastrophic injuries from a mine blast and
shrapnel, resulting in the destruction of the left eye and a shattered zygomatic bone. He was fitted with a specially designed implant and prosthesis and with a supporting titanium plate on the bone— all generated from a CT scan and then 3D printed. (see image 2)
In another case, this time involving catastrophic bilateral damage, Prof Petrenko’s team performed four operations to repair conjunctival and eyelid tissue, allowing them to affix two prostheses. One of them, in the patient’s right eye, was placed directly into the orbital wall using implanted magnets.
“After we place the orbital implant, we suture everything in place, including the sclera and conjunctival membrane. In three to four weeks, if the patient hasn’t experienced any infection, swelling, etc., we can affix the prosthesis,” Prof Petrenko said.
“The results are good because the patient can socialise, and people won’t be nervous around him. It’s hard to communicate if you don’t appear to have eyes.”
The value Prof Petrenko’s work provides is clear, yet her team faces serious funding problems. They’re currently forced to pay out of pocket for essential supplies such as eyelid stitches, and they urgently need a microsurgical instrument coagulator.
Their experience with eyelid reconstruction, implantation, and prosthesis manufacturing using 3D printing should prove highly instructional to clinicians wanting to learn the latest developments in combat trauma surgery. With the war showing no sign of ending soon, unfortunately, there will be more patients who provide insight.
“A multidisciplinary approach to patients with anophthalmia provides opportunities for high-tech reconstructive surgery and achieving the maximum functional and cosmetic result. Our government does not have the opportunity to buy all the equipment we need, so support from abroad would be appreciated.”
Oksana Petrenko
MD is Professor of the Department of Ophthalmology of the Shupyk National Medical Academy of Postgraduate Education, Kyiv,
Ukraine. visionpetrenko@gmail.com
Six ESCRS members have been elected to the Society’s Council of Management and will begin serving their terms at the start of 2026.
The elected council members are as follows:
• Christina Grupcheva (Bulgaria)
• Thomas Kohnen (Germany)
• Georgios Kymionis (Greece)
• Sorcha Ní Dhubhghaill (Belgium)
• Andreia Rosa (Portugal)
• Paolo Vinciguerra (Italy)
Kymionis is new to the council, while Grupcheva previously was a co-opted member. The other four were re-elected to another term on the council.
ESCRS proactively compensated for 80% of estimated greenhouse gas emissions from its 2025 Annual Congress by supporting certified offset projects in Burkina Faso and Vietnam.
ESCRS selected the projects through its partnership with South Pole, a climate solutions organisation dedicated to delivering measurable climate change. The projects are the following:
• Providing environmentally ‘clean’ cookstoves in Burkina Faso to improve community health while reducing deforestation; and
• Developing hydropower and wind energy projects in Vietnam to displace the use of coal, create more local employment, and further Vietnam’s transition to renewable energy sources.
ESCRS is committed to calculating its overall Congress emissions and offsetting the remaining balance after the event.
‘Collective Desire’ Must Drive DEI Implementation
The winning essayist in the 2025 John Henahan Writing Prize competition
said ophthalmologists must make diversity, equity, and inclusion a priority to ensure the long-term sustainability and quality of the profession.
In his essay, “Thinking Beyond Optics: Diversity, Equity, and Inclusion (DEI) and Unconscious Bias in Ophthalmology,” Jamal Atamniy, an ophthalmologist in Vienna, Austria, stated what he considers a “fundamental truth” underlying the debate over DEI policies and initiatives: “unconscious bias and inequality continue to influence ophthalmology training, practice, and research, often to the disadvantage of clinicians and patients.”
The answer, he wrote, is to see diversity and inclusion not simply as moral imperatives but as keys to the survival of the profession and the treatment of patients.
“Biases and inequities in ophthalmology can be mitigated through DEI,” the essay concluded. “This concept should not be dismissed as merely a quota that institutions must fulfil. Its implementation should stem from our collective desire as medical professionals to provide our patients with the best care.”
The John Henahan Writing Prize competition is open annually to young ophthalmologists who submit an essay (800 words maximum) on a selected topic. The author of the winning essay receives a €500 bursary and a specially commissioned trophy. The winning essay is also published in EuroTimes
The 2025 competition asked participants to address this prompt: Diversity, equity, and inclusion (DEI) programmes, however well-intentioned, stir a variety of responses in the corporate and political worlds and in the scientific and medical spheres. What DEI and unconscious bias issues are present in the current culture of ophthalmology training, practice, and clinical research? What are the potential benefits of addressing these issues for patients and ophthalmologists? What kind of meaningful changes need to happen to move beyond ‘talking the talk’ to ‘walking the walk’?

Managing aberrations after laser refractive surgery requires a multi-layered approach.
BY ROIBEARD O’HÉINEACHÁIN
Despite progress in diagnostics and laser technology, visual aberrations may still arise after corneal laser refractive procedures. However, early diagnosis and treatment can provide excellent outcomes, and significant visual improvement is still possible with later interventions, said Vladimir Suvajac MD at an ESCRS eConnect Webinar titled “Tackling Postoperative Complications in Corneal Surgery.”
Dr Suvajac shared a few cases of postoperative visual aberrations, along with his management strategies and the treatment outcomes. The first case involved a patient who developed visual issues in their left eye two years after myopic
LASIK, showing residual or regressed myopic astigmatism and BCVA of 0.5. Corneal topography showed superior asymmetrical steepening, while aberrometry identified mainly coma, trefoil, and some spherical aberrations matching the overall ocular findings.
To address residual myopic astigmatism and higher-order aberrations, Dr Suvajac performed corneal wavefront-guided transepithelial photorefractive keratectomy (PRK) with mitomycin-C. He said he prefers surface ablation over lifting an old flap in aberrated corneas, as it enables wider treatment zones, bigger postoperative optical zones, and less epithelial

hyperplasia. Preoperative corneal epithelial mapping with OCT is crucial in these cases due to the epithelial hyperplasia or irregularities that are inherently present. Incorporating epithelial profiles in treatment planning allows for refractive outcomes that are, in most cases, comparable to the flap re-lift approach, he said.
Postoperatively, the patient’s operated eye had a decimal visual acuity of 1.0, with reduced lower- and higher-order aberrations. Coma reduced by almost 60% and spherical aberration by around 45%. Postoperative topography showed asymmetric flattening, as planned with the customized ablation.
Another case involved a 29-year-old male patient who underwent bilateral PRK in 2016. When he presented at Dr Suvajac’s clinic in 2023, he had corneal haze and mixed astigmatism (+3.0/-5.0 x 10) in his right eye with a best-corrected decimal visual acuity of 0.5. The haze induced higher-order aberrations as well as some opacity. His left eye had only mild astigmatism and a BCVA of 0.9.
Dr Suvajac treated the patient’s left eye with corneal wavefront-guided transepithelial PRK with mitomycin-C. At the two-year follow-up, the eye’s acuity was 0.9 with only 0.75 D of cylinder, and only peripheral clinically insignificant
haze. Additionally, there was a reduction in both lower- and higher-order aberrations.
“Corneal haze can often be treated effectively with PTK or corneal wavefront-guided procedures,” he said. “Since it typically affects the anterior subepithelial cornea and is not severe, treatment is usually simpler than for corneal scarring from infections or pterygium surgeries. Conservative options like topical losartan drops exist, although these are not yet commonly available in pharmacies.”
Early diagnosis and tailored treatment can restore excellent vision, even years after corneal laser surgery.
Another case involved a patient who underwent bilateral LASIK for hyperopic astigmatism in 2023. Six months postoperatively, the patient reported blurry vision in the left eye, noting they saw better when they covered that eye. The left eye had experienced a free cap during surgery. Slit lamp exam and retroillumination revealed pronounced microstriae, and OCT showed several Bowman’s membrane ruptures. Aberrometry showed micro-scattering corresponding to the observed microfolds, and contrast sensitivity was normal in the right eye but poor at high frequencies in the left eye. Bilateral contrast sensitivity was nearly as low as in the left eye alone
To achieve corneal regularization, Dr Suvajac and his team performed a phototherapeutic keratectomy (PTK) to a depth of 70 microns, followed by wet PTK smoothening, using an aberration-free, refractive-neutral ablation profile. Postoperatively, the patient had a one-line improvement in visual acuity and reported no ongoing visual symptoms with complete physiological contrast sensitivity. Both OCT and retroillumination imaging demonstrated minimal residual microfolds.
“It is not that rare to see some microfolds, and usually, they are not clinically significant. But when the patient complains, it is good to keep in mind that topography, aberrometry, or OCT images can sometimes underestimate their significance, as they are not that pronounced,” Dr Suvajac added. “And retroillumination images and contrast sensitivity testing can be helpful.”
Vladimir Suvajac MD is chief surgeon at the Eye Clinic Professional in Belgrade, Serbia. v.suvajac@bolnicaprofesional.rs
The complete seminar is available on the ESCRS website: www.escrs.org/channels/ player-videos/escrs-econnect-webinartackling-postoperative-complications-incorneal-refractive-surgery
Femtosecond laser offers a multifunctional tool for improving the safety and efficacy of cataract and refractive lens exchange procedures.
CHERYL GUTTMAN KRADER REPORTS
Use of a femtosecond laser brings many opportunities for improving outcomes of cataract and refractive lens exchange surgery, said H Burkhard Dick MD, PhD, explaining his preference for a laser-assisted approach in these procedures.
Professor Dick described several benefits of laser-assisted surgery in eyes with hyperopia or high myopia, as well as capsulotomy in both situations.
“Capsulotomy done with the laser instead of a physical instrument reduces the risk of injuring the endothelium or lens capsule when operating on hyperopic eyes that have a crowded, shallow anterior chamber,” Prof Dick explained. “In addition, the laser creates a perfectly centred and well-sized capsulotomy that will overlap the IOL optic and therefore enable accurate IOL positioning and decrease deviation from target refraction in these eyes that are particularly susceptible to refractive surprises.”
Should the case become complicated by posterior capsule rupture, the perfectly sized, positioned, and circular capsulotomy created with the laser will also enable secure placement of the optic using optic capture, he noted.
Additionally, using the laser for lens fragmentation will allow for safer and more efficient lens removal. The reduced fluid turbulence and ultrasound energy usage result in less postoperative corneal oedema, Prof Dick said.
The laser creates a perfectly centred and well-sized capsulotomy.
Regarding surgery in highly myopic eyes, Prof Dick said using the laser for capsulotomy overcomes the challenges presented by a capsular bag that tends to be large and floppy and only appears to be smaller and farther away. Furthermore, the ability to create an optimally sized capsule opening that helps maintain IOL stability by fully overlapping the optic is a particular benefit in highly myopic eyes that are at increased risk for decentration over time.
The advantages of performing laser lens fragmentation in high myopes are similar to those associated with its use in hyperopic eyes. The gentle lens removal also causes less vitreous traction, which Prof Dick said is important considering the increased risk for retinal detachment in high myopes.
He added that laser lens fragmentation has an additional advantage in cases of refractive lens exchange because it allows the manual portion of the procedure to be performed without either ophthalmic viscoelastic device (OVD) or ultrasound.
“Without the need for OVD, the procedure is shorter, and there is less iris/lens diaphragm movement,” Prof Dick explained. “With this approach, patients benefit with greater comfort, faster visual rehabilitation, and no risk for a postoperative IOP spike caused by residual OVD.”
The laser provides further opportunities for more precise astigmatic correction—whether it is to create arcuate incisions or markings on the cornea or capsule to guide toric IOL alignment, which he said also avoids parallax error and allows evaluation of postoperative IOL rotation.
Surgeons using a femtosecond laser can easily, quickly, and safely create a primary posterior capsulotomy capable of tremendously reducing the incidence of posterior capsule opacification and thus the need for Nd:YAG capsulotomy.
“Primary posterior laser capsulotomy has a particular benefit for centres that do a lot of refractive lens exchange procedures, where patients with full depth of focus simultaneous vision IOLs almost routinely return for Nd:YAG capsulotomy,” Prof Dick said.
Prof Dick spoke at the 2025 ASCRS annual meeting in Los Angeles.
H Burkhard Dick MD, PhD, FEBOS-CR is Professor and Chairman, Department of Ophthalmology, University at Bochum, Germany. burkhard.dick@kk-bochum.de
Femtosecond lasers are helping improve refractive results with fewer problems.
Complications with intracorneal ring segments (ICRS) are generally avoidable with correct keratoconus classification and proper surgical planning and technique, said Tiago Monteiro MD during an ESCRS eConnect Webinar.
Made of PMMA, ICRS are used to treat keratoconus by flattening the cornea and reducing higher-order aberrations such as coma and irregular astigmatism. Usually implanted at a stromal depth of 70–80% along the flattest topographic axis, the process now uses a femtosecond laser to create the tunnel, replacing earlier manual techniques.
Complications with ICRS can be functional or anatomical. Functional complications encompass loss of visual acuity or incorrect correction, inappropriate implant selection for the cornea type, incorrect procedure indication based on disease stage, and insufficient depth, centration, or symmetry of the intrastromal tunnel. Anatomical complications include improper implantation, extrusion, infection, inflammation, and neovascularisation.
Over the past 15 years, Professor José Alonso, Dr Monteiro, and their team have established a morphological classification system for ectasia phenotypes when identifying suitable ICRS specifications in keratoconus cases. This system uses corneal asphericity direction and assesses the relationship between topographic astigmatism and coma higher-order aberrations.1
A 2021 study found refractive failure caused nearly 60% of ICRS complications. Dr Monteiro noted that for keratoconus stage 2 or less, issues often relate to inadequate optical zones, implant arc length, or thickness. For stages 3 or 4, deep anterior lamellar keratoplasty (DALK) is generally a better option.2
A 2018 study of 26 patients with unsuccessful ICRS outcomes found that exchanging ICRS for ones adjusted in thickness or arc length led to significant improvements in corrected distance visual acuity, refractive and topographic cylinder, and coma. He noted that in cases where the original topography is available and the tunnel was created correctly, the ICRS exchange can be performed in a single procedure. However, if the topography is not available and/or the tunnel was poorly centred or at incorrect depth, the explantation and implantation should be performed six months apart.3
Dr Monteiro explained how femtosecond lasers have greatly increased the precision of intrastromal tunnel creation for ICRS implantation. In a study he conducted with colleagues comparing manual and femtosecond laser techniques, only 15.40% of eyes in the manual tunnel group achieved tunnel depths within 10 microns of the intended measurement, whereas 67.92% of eyes in the femtosecond laser group met this criterion.4
Nearly 60% of ICRS complications are caused by refractive failure.
“The implant depth is very important because if the implant is very shallow or very deep, we will have topographic overcorrection and higher postoperative astigmatism,” Dr Monteiro said. “And we are not going to achieve the refractive outcome we wanted.”
The precision of femtosecond lasers has also reduced the incidence of anatomic complications. A study comparing manual and femtosecond laser techniques found the manual approach delivered a 1.5% corneal perforation rate and a 5.7% ICRS extrusion rate, compared to the respective 0.9% and 0.0% rates with the femtosecond laser technique. The learning curve was a more important factor with manual technique as the complication rate was significantly lower during the first three years of a surgeon’s experience.5
The seminar is available at www.escrs.org/channels/player-videos/ escrs-econnect-webinar-tackling-postoperative-complications-incorneal-refractive-surgery.
For citation notes, see page 32.
Tiago Monteiro MD is based at Hospital de Braga, Braga, Portugal; Escola de Medicina Universidade do Minho, Braga, Portugal; and Hospital CUF Porto, Porto, Portugal. monteiro.tiago.pt@gmail.com


Whether standard or laser-assisted, proper technique is essential.
HOWARD LARKIN REPORTS
Due to weakened and sometimes defective posterior capsules, removing posterior polar cataracts carries the heightened risk of posterior capsule rupture (PCR). Adjustments to phacoemulsification (phaco) techniques can reduce this stress. Two experts debated the merits of using standard phaco or a femtosecond laser to pre-segment the nucleus at a recent conference.
Advantages of standard phaco
Arguing for standard phaco, Soon-Phaik Chee MD outlined techniques for preserving fragile capsules when removing posterior polar cataracts of various densities. “I truly believe standard phaco is safe and effective, and you’ll see why,” she said. Noting PCR risk with posterior polar cataracts increases when patients are younger than 40 years, have grade 4 or denser cataracts, or have a polar opacity 4.0 mm or larger, Dr Chee said anterior segment optical coherence tomography helps assess for this risk.1–3 She recommended the following strategies for avoiding PCR:
• Isolate a layer of cortex encompassing the polar opacity to be removed after nucleus phacoemulsification. Use hydrodelineation or hydrodelamination rather than hydrodissection. Viscodissection can be used to dissect the cortex and epinucleus.
• Use slow-motion phaco with reduced parameters, avoiding nucleus rotation and decentration. Successful techniques can include bimanual phaco, sideways sculpting, chop-and-tumble, manual nuclear delamination without fluid, and crossand lamellar-chopping techniques.
• Strip the cortex towards the polar opacity, lifting it last.
• Avoid polishing the posterior capsule.
• Maintain anterior chamber space and avoid overpressurising the eye.
The full procedure is like a beautiful dance, [one] facilitated by the femtosecond laser.
Furthermore, she emphasised a gentle approach as well as the importance of good technique. “If you don’t have good technique, you are going to break the capsule anyway.”
To determine whether manual or femto-assisted surgery had better outcomes, Dr Chee reviewed results from her clinic. Over five years, 187 posterior polar cataracts were removed: 136 by femto-phaco, mostly performed by Dr Chee or a fellow, and 51 manually, mostly by residents. There was a mixture of densities in both groups. Outcomes were similar among the 12 intraoperative PCRs, with 9 occurring in femto cases and 3 in manual cases—resulting in a PCR rate of 6.7% for femto, 5.9% for manual, and 6.4% overall.
“Looking at these data, my residents did quite well. Standard phaco is truly safe and effective—as long as we do the right technique,” Dr Chee concluded.
Dagny Zhu MD argued that femtosecond laser-assisted phaco is safer than standard phaco for posterior polar cataracts. Although the literature shows PCR rates have dropped from as high as 26–36% in the 1990s to around 7–8% in recent years due to improved manual techniques, she noted using femtodelineation before nuclear removal can further reduce PCR rates—one groundbreaking study by Dr Abhay Vasavada and colleagues demonstrated rates as low as 4.4%.4

Echoing Dr Chee, Dr Zhu emphasised the need to reduce stress on the capsular bag to avoid PCR. One key is avoiding sudden, rapid build-up of hydraulic pressure inside the capsular bag.
“Even if there is a tear, you still want to minimise the pressure because you don’t want to expand the tear.”
Femtodelineation helps by cutting three concentric cylinders in the nucleus, which pre-softens it to make removal more predictable and with less manipulation and creates shock-absorbing zones that cushion the posterior capsule, Dr Zhu explained. A variation on the technique adds vertical chops, further presoftening the nucleus.
Removal starts at the dense nuclear centre and moves precisely along pre-cut lines outward and downward, layer by layer, Dr Zhu said. This protects the weak posterior capsule and exposes the posterior polar component so it can be carefully removed last, starting from the epi-nucleus periphery and moving inward. The technique also leaves a perfectly centred capsulotomy in case a sulcus IOL is needed. “The full procedure is like a beautiful dance, [one] facilitated by the femtosecond laser.”
To further reduce pressure build-up in the capsule, Dr Zhu also recommended changing femto settings from standard procedures. She lowers the pulse power and increases spot separation, reducing bubbling-associated pressure rises. She also leaves a 500-micron safety zone from the posterior capsule and keeps the capsular-zonular diaphragm from bulging forward with viscoelastic.
Dr Zhu concluded that femtodelineation is safer than standard phaco for removing posterior polar cataracts. “Yes, you can get away with a manual technique, but we have data showing the PCR rate is lower with the femtodelineation.”
The debate took place during the 2025 ASCRS annual meeting in Los Angeles.
For citation notes, see page 32.
Soon-Phaik Chee MD is an ophthalmologist in private practice, visiting consultant to the Singapore National Eye Centre, and adjunct professor at Duke NUS Medical School in Singapore. chee.soon.phaik@snec.com.sg
Dagny Zhu MD is medical director and partner at NVISION Eye Centers, Rowland Heights, California, US. Dagny.Zhu@nvisioncenters.com
Patients are understandably curious to learn as much as they can about their upcoming cataract or refractive surgery. ESCRS has developed a Patient Portal on its website to help inform patients about these surgeries.
The Portal is split into two sections: Cataract and Refractive. Each section provides an easy-to-understand summary of the different types of conditions, including the benefits, risks, procedures, and aftercare of common conditions.
Each section is easily navigable, with clear diagrams and a glossary to convey all the information patients might need to help prepare for surgery or during aftercare.

Research reveals many dynamic mechanisms at play.
Long-term regression after corneal refractive surgery remains a significant challenge, with many patients experiencing a gradual return of refractive error that impacts visual durability and may require further surgery. Identifying its many causes and key risk factors is essential to improve patient selection, surgical planning, and long-term refractive stability, said Sara Sella MD.
Dr Sella noted long-term refractive regression arises from complex biological responses involving the corneal epithelium and stromal biomechanics. After myopic LASIK or SMILE, the central epithelium typically thickens to compensate for stromal tissue loss, while it thins centrally and thickens peripherally in hyperopic PRK to smooth the transition zone. Biomechanical changes occur simultaneously, as anterior stromal ablation reduces corneal rigidity, potentially causing posterior stromal steepening that alters refractive power. Cytokine signalling drives keratocyte transformation and stromal remodelling, contributing further to regression and haze formation.
In a study of 236 eyes from 119 civilian pilots in southwest China (mean preoperative SE -2.92 ± 1.11 D), myopic regression was observed in 23.6% of eyes over a 5–16-year period after corneal refractive surgery. Regression risk increased with older age at surgery (OR 1.151 per year, p = 0.022), subepithelial ablation techniques (PRK/LASEK; OR 2.769, p < 0.001), and prolonged, continuous near work (OR 0.635, p = 0.038). Cumulative flying hours and length of postoperative follow-up were not significant predictors, reinforcing the superior long-term refractive stability of intrastromal methods in occupations with high visual demands.1
A large-scale high myopia cohort (2,460 eyes) supported the pilot study. Yet, in this cohort, regression arrived swiftly and extensively, with rates up to 89% within the first year, suggesting the influence of baseline refractive error in accelerating biomechanical or healing-related shifts. A third study focused solely on modern intrastromal approaches (SMILE, FS-LASIK), painting a more reassuring five-year picture (16.1% regression) but reinforcing an environmental warning: prolonged near work can double the risk, particularly in younger patients, women, and FS-LASIK eyes. Together, these studies reveal that while surgical method and patient age consistently shape long-term stability, the context of baseline myopia, early healing response, and daily visual habits after surgery can profoundly alter the trajectory of refractive outcomes.2,3
“The take-home message is, not all procedures are equal,” Dr Sella said.
Regarding hyperopic regression, a retrospective analysis of eyes from 888 patients who underwent hyperopic LASIK at a
single centre over 14 years showed older age and earlier-generation platforms as key predictors of retreatment. However, neither corneal thickness nor preoperative refraction appeared to influence regression.4
Astigmatic regression presents its own challenges. High-cylinder cases are more prone to undercorrection or enhancement, with similar susceptibility in both LASIK and PRK. In a 20-year analysis of 785 mixed-astigmatism eyes, the overall retreatment rate was 5.2%, with most enhancements performed within 3 years. High preoperative astigmatism increased the likelihood of retreatment almost fourfold, and male gender, significant residual cylinder, and suboptimal platform choice further elevated risk. Although advances in ablation speed, cyclotorsion control, and centration have reduced residual or regressed astigmatism, they have not eliminated it.5
“When it comes to long-term regression, there is no universally superior procedure for every refractive error,” Dr Sella said. “For hyperopia, both LASIK and PRK are limited by significant regression in higher corrections, and while SMILE is promising, long-term data is lacking. For astigmatism, LASIK remains the most predictable for high cylinders, but PRK and SMILE are effective for lower corrections. For myopia, all three procedures are effective for low to moderate corrections, but high myopia remains a challenge, with similar regression rates across platforms.”
Treatment for regression should be based on the underlying cause. Diagnosis typically includes refraction, topography, epithelial mapping, and posterior elevation imaging. Myopic regression associated with posterior steepening may be managed with topography-guided PRK, hyperopic regression resulting from epithelial remodelling with PRK using mitomycin-C and an expanded optical zone, and astigmatic regression with vector-corrected wavefront- or topography-guided LASIK or PRK.
“Long-term refractive stability hinges on aligning procedure choice with patient biology, refractive target, and lifestyle factors,” she said.
Dr Sella and her colleagues developed a nomogram that aims to improve retreatment outcomes by adjusting preoperative planning to account for the epithelial contribution to regression. They hope to report their results soon. Meanwhile, a Korean team has reported promising results with machine learning models they developed to identify patients at high risk for refractive regression.6
For citation notes, see page 32.
Sara Sella MD is a cataract, refractive, and cornea surgery consultant at the Ein Tal Medical Center, Tel Aviv, Israel. eyesella66@gmail.com
Lens power adjustment technology is developing quickly.
HOWARD LARKIN REPORTS
The Light Adjustable Lens (LAL, RxSight) is the first and only intraocular lens (IOL) on the market offering post-implantation sphere and cylinder error adjustment, allowing precise refraction revisions following cataract surgery. But other IOL adjustment technologies are not far off, according to Mark A Kontos MD.
Initially developed by Nobel Prize-winning chemist Professor Robert H Grubbs PhD and Professor Dan Schwartz MD in 1997, LAL technology employs directed UV light to selectively polymerise macromers in the lens, changing lens curvature and refractive power. Once optimal power is reached after surgery, the light polymerises all remaining macromers to prevent further changes. Typically, three follow-up sessions over approximately five weeks are required to adjust and lock in treatment.
Calhoun Vision was founded in 2000 to develop the LAL, which entered FDA trials in 2007. The company and technology were re-invented and re-branded as RxSight in 2017, and the LAL gained FDA approval. As of 2024, more than 200,000 LALs had been implanted by more than 1,700 surgeons, said Dr Kontos, who is a consultant for RxSight.
The LAL is particularly useful for post-refractive surgery patients, Dr Kontos said. “There are many millions of patients who have had refractive surgery, and [they] are among the more challenging groups [for] cataract surgery.” These patients expect excellent visual outcomes, but such outcomes are more challenging due to difficulty in accurately predicting lens power.
In a recently published study, 74% of 76 post-corneal refractive surgery eyes implanted with the LAL achieved 20/20 or better uncorrected vision, with 88% corrected to 20/25 or
better and 93% correctable to 20/20 or better. Two-thirds were within 0.25 D of target, and 86% within 0.50 D.1 “For that group of patients, those are pretty amazing results,” Dr Kontos said. “I would take these results in my general cataract surgery group—let alone in those who have had refractive surgery.”
The LAL is specially designed to allow for adjustments. In the near future, femtosecond lasers may make it possible to adjust the power of many standard lenses, Dr Kontos said. The laser can be used to change the hydrophilicity of targeted areas in an IOL, altering its refractive index. This can change defocus power, toricity, and asphericity, extending depth of focus. It can even create or reverse multifocality.
Further in the future, it may be possible to adjust the effective position of lenses after surgery. Dr Kontos said a nitinol-based adjustable IOL allowing up to +1.50 D anterior change in lens position, as well as radial movement, has been tested in rabbits.2
“It will be interesting to see where all these things go. In my mind, lens adjustability is something that is here now, and it is rapidly being accepted by patients,” Dr Kontos said. “The future is bright.”
Dr Kontos spoke at the 2025 ASCRS annual meeting in Los Angeles.
For citation notes, see page 32.
Mark A Kontos MD is a former US Navy flight surgeon and an ophthalmologist currently practising at Empire Eye Physicians in Spokane Valley, Washington, and Coeur d’Alene, Idaho, US.

From monofocal to full-range solutions, each practice needs comprehensive understanding.
CHERYL GUTTMAN KRADER REPORTS
The growing arsenal of intraocular lens (IOL) options gives cataract surgeons more opportunities to meet their patients’ visual goals. However, greater choice also brings added responsibility, as surgeons must be knowledgeable about the optical principles and bench performance of several IOLs to recommend the best possible match for each patient’s visual lifestyle. Furthermore, optimizing the chance of success and patient satisfaction also requires that cataract surgeons implement what they have learned from their personal clinical experience and provide appropriate patient education to establish realistic expectations, says Andreas F Borkenstein MD.
“An IOL classification system recently proposed by the European Society of Cataract and Refractive Surgeons (ESCRS) categorizes IOLs in a clinically relevant manner by differentiating them based on functional visual outcomes defined by defocus curve metrics rather than by optical design,”1 Dr Borkenstein said. “This classification system provides a valuable framework for understanding and implementing IOL technologies. However, surgeons must also be aware [of the] differences between the various categories with respect to patient adaptation and photic phenomena that must be discussed with patients and are not covered by the functional classification.”
Expanding on these issues, he explained that enhanced monofocal and extended depth of field (EDOF) IOLs, both of which the ESCRS system classifies as partial range of depth of field IOLs (see table), typically offer a smoother adaptation period and are associated with fewer photic disturbances compared to IOLs with a full range of depth of field.
“Nonetheless, proper IOL centration and proper informed consent can mitigate patient dissatisfaction because of these issues,” Dr Borkenstein said.
Preoperative and postoperative considerations
Preoperative consultation should involve a thorough assessment of the patient’s lifestyle, visual needs, and tolerance for potential side effects. Patients who spend significant time at intermediate distances (e.g., computer work) may benefit more from enhanced or extended range of field IOLs, while those desiring maximum spectacle independence, including for reading, may be candidates for full range of field IOLs. Alternatively, surgeons can implement a ‘mix and match’ approach combining different IOL types for binocular implantation or a monovision approach targeting a different refraction in each eye.
“These techniques can enhance the overall range. It is essential, however, to have a detailed discussion with the patient beforehand, covering the advantages and limitations in daily life, to understand [their] occupational and recreational needs and jointly define a clear target refraction,” Dr Borkenstein said.
“Additionally, digital simulation tools can help patients visualize their postoperative vision, improving satisfaction and consent quality. These tools enable patients to perceive differences in contrast sensitivity, depth of focus, and potential photic phenomena with different IOLs and can support informed decision-making, especially when considering more complex lens profiles like extended or full range of focus. For visually demanding patients, this individualized approach
can also significantly improve satisfaction and reduce postoperative surprises.”
Integrating EDOF and full range of field IOLs into clinical practice also requires a structured workflow and the appropriate infrastructure. As essential diagnostic tools for surgical planning, Dr Borkenstein recommended optical coherence biometry for accurate axial length measurement, corneal topography for mapping astigmatism, and wavefront aberrometry to detect higher-order aberrations.
Postoperatively, the follow-up protocol should include early assessment of uncorrected visual acuity, lens centration, and patient-reported outcomes. Minor residual refractive errors may be addressed with glasses or laser touch-up procedures, while significant dissatisfaction should prompt re-evaluation of lens alignment or selection. However, the role of neuroadaptation should not be overlooked, Dr Borkenstein said.
“As the brain adjusts to simultaneous image processing from different focal zones, visual perception may evolve significantly over time—often within three to six months,” Dr Borkenstein said. “While many patients adapt naturally, others may benefit from targeted visual training or supportive counselling during the early postoperative phase. Addressing this process proactively can enhance outcomes and reduce the risk of dissatisfaction in the adaptation period.”
He also reminded his colleagues of the importance of comprehensive training for all medical staff interacting with
patients, ensuring the entire team is well-versed in the optical characteristics and possible side effects of the available IOLs and effective counselling strategies related to these topics. Educational materials, such as brochures, model IOLs, and simulation software, can further enhance patient understanding and decision making.
“Creating a successful premium IOL practice is not just about offering a range of products. Understanding the optical principles behind various IOL designs is essential. This underscores the importance of experimental research and optical bench testing—efforts [to which] I am personally committed. For those without direct access to such investigations, studying peer-reviewed optical performance data is vital to building a sound foundation before clinical application and, ultimately, personal experience with each lens,” Dr Borkenstein said.
“Then, appropriate diagnostics, surgical precision, and patient engagement to deliver a personalized experience can help surgeons achieve their patients’ visual goals and satisfaction.”
For citation notes, see page 32.
Andreas F Borkenstein MD is a consultant ophthalmic surgeon at the Privatklinik der Kreuzschwestern and co-owner of Borkenstein & Borkenstein Research & Laboratory Gmbh, both in Graz, Austria. crustalith@gmx.at
Trinity College, Dublin, Ireland | 07 – 09 November 2025
The ESCRS Leadership, Business, and Innovation Workshop returns on 7–9 November, bringing together forward-thinking ophthalmologists for a weekend of insight, strategy, and networking.
This workshop on all things marketing will be a dynamic, practice-driven workshop tailored for ophthalmologists and practice managers seeking to enhance their marketing capabilities in a healthcare setting.
Explore how to elevate your brand, attract the right patients, and grow your clinical impact in a competitive landscape.

Part five of this in-depth series delves further into PPP as a customisable solution for HOAs.
BY SOOSAN JACOB MS, FRCS, DNB
Pinhole optics is a fascinating field that applies a small aperture to improve image clarity and focus. It is used for treating aberrated eyes, such as those with corneal ectasia, corneal scars, or post-surgical complications. It works through the pinhole camera by cutting peripheral rays of light, thus reducing scattering of light and decreasing the circle of blur.
Pinhole optics have been used to correct higher-order aberrations by acting as a wavefront filter. It can be applied at various levels—spectacles, contact lenses, the cornea, and the IOL. Dr Agarwal (et al.) described pinhole pupilloplasty (PPP), which uses pinhole optics at the iris level. This helps further customise the effect of pinhole optics and provides some distinct advantages.
It works on a few simple, yet powerful principles.
The effect of light scattering secondary to distorted corneas is mitigated through pinhole optics. It minimises the circle of confusion on the retina and results in a sharper image, as only direct light rays reach the retina. The depth of focus also increases, thus expanding the range of vision even in pseudophakic eyes.
With pinhole pupilloplasty, the aperture size can be tailored to each patient’s degree of aberration—something no other small-aperture optic can achieve.
With PPP, the diameter of the pupil is adjustable and can be inversely related to the degree of aberrations.
PPP provides this advantage of being able to adjust the pinhole size to the number of aberrations, which is not possible with any other small-aperture optics. Thus, the degree by which the aperture is reduced does not remain uniform as in IOLs and corneal pinholes.
Stiles–Crawford
First, let’s understand the anatomy of the fovea. There are 200-fold more cones in the fovea compared to the rest of the retina. Foveal cones are tightly packed, with densities reaching 150,000–300,000 cones/mm² as opposed to peripheral cone density of approximately 5,000–10,000 cones/mm². This dense arrangement is essential for high spatial resolution and sharp central vision.
To accommodate dense packing in the foveal region, foveal cones are taller and thinner than peripheral cones, measuring 1.5–2.0 µm at the fovea versus 4.0–10.0 µm in the peripheral retina. Their shape and high refractive index relative to the surrounding intercellular medium allow them to act as optical waveguides. So, much like an optical waveguide, the waveguide-like property of cones helps them guide and preferentially transmit light entering at angles closer to their optical axis. This behaviour is a critical aspect of the Stiles–Crawford effect, where light rays entering at the centre of the pupil are perceived as brighter and more effective for vision than those entering near the periphery of the pupil, even if their physical intensities are the same.
The surgeon centres the PPP on the visual axis, unlike pinhole IOLs, where the IOL centres within the bag and not necessarily on the visual axis. Thus, the PPP can be placed accurately on the visual axis in eyes with distorted optics. Additionally, it can be placed anywhere behind the region of the cornea with good optics in highly aberrated scarred eyes, while an IOL cannot.
The surgeon can likewise adjust the PPP size intraoperatively, customising it to the patient. However, other pinhole technologies, such as IOLs and corneal small-aperture discs (e.g., Kamra inlay, CorneaGen), are made with a fixed aperture size, and the same aperture is implanted for every aberrated cornea, regardless of the number of aberrations. Yet these can only help to an extent in highly aberrated eyes.
The sizing and positioning advantages of the PPP harness the waveguide property of cones and the Stiles–Crawford effect by allowing parallel rays of light to accurately hit the optical axis of the cones, thus enhancing and optimising retinal image quality.
The IC-8 Apthera (Bausch + Lomb) needs to be available in different powers, which increases the need for a large inventory of these small-aperture monofocal IOLs. The alternative opaque optic piggyback IOL (XtraFocus IOL, Morcher) with a central clear aperture also has disadvantages, such as requiring placement in the sulcus atop another IOL. Small-aperture corneal inlays need a femtosecond pocket to be created for placement and correction of any refractive error in patients with corneal laser vision correction or cataract surgery with IOL implantation.
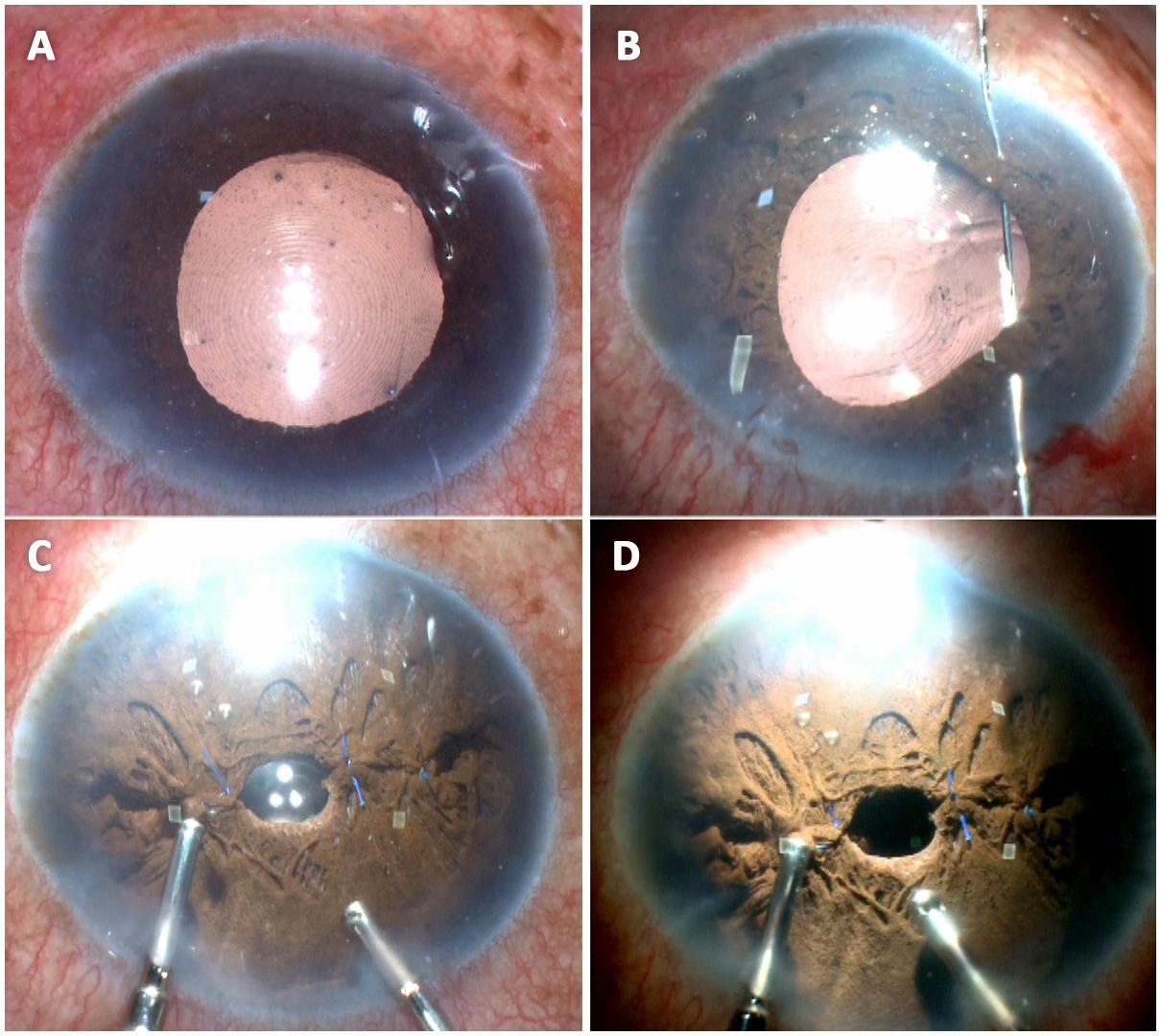
FIGURE: A) Urrets-Zavalia syndrome in a patient with multifocal IOL implanted; B) Multiple single-pass, four-throw pupilloplasty knots are tied down to make the pupil small; C) The final size and centration of the pupil is done using a vitrector probe at low cut rate (500) and about 250 mmHg vacuum. The preoperative corneal mark and the Purkinje 1 reflex are used to assess size and centration; D) A well-sized and positioned circular pupil seen using only endoilluminator light and with the microscope light switched off.
PPP, on the other hand, only requires a 10-0 prolene suture and is not dependent on expensive pinhole IOLs, small-aperture corneal inlays, or expensive laser platforms. Cataract extraction with implantation of a monofocal IOL of the surgeon’s choice is followed by PPP.
Pinhole IOLs and inlays can be used only up to 1.5 D of astigmatism. Dr Agarwal’s clinic has been able to demonstrate improvement in even high degrees of astigmatism by adjusting the size of the PPP according to the degree of astigmatism or HOA.
While pinhole IOLs are recommended in the non-dominant eye, the clinic has used the PPP in both eyes. The Kamra corneal inlay has been reported to have issues with corneal healing, fibrosis, and haze development.
In eyes with central corneal scarring close to the visual axis that is causing irregular astigmatism, even a slightly decentred PPP may surprisingly give good visual improvement without the need for high-risk corneal surgeries.
The use of the pinhole IOL is restricted in the presence of an intact posterior capsule and intact zonules. Patients can benefit from PPP irrespective of the lens or capsule status, as it can be combined with any form of secondary IOL fixation, such as glued IOL or the Yamane.
Corneal pinhole inlays are difficult to place in eyes with multiple radial keratotomy (RK) scars or in very thin corneas
in keratoconic eyes. As compared to the PPP, synthetic corneal pinhole apertures such as the Kamra inlay also have the disadvantage of interfering with corneal nutrition (predisposing to haze, scarring, or melts) and can result in irreversible damage to the cornea. A corneal transplant is also difficult in corneas with RK incisions. However, a simple cataract surgery with PPP handles these disadvantages while providing good vision.
PPP can be advantageous when combined with DMEK or PDEK, especially in complex cases such as vitrectomised eyes as it makes graft opening much easier. It also helps to maintain a better air tamponade postoperatively by preventing migration of the air bubble. Its use extends to eyes with peripheral anterior synechiae, as the tautening of the iris secondary to PPP prevents these synechiae from reforming, which helps a closed angle become an open angle.
In combination with penetrating keratoplasty
Similarly, it can be advantageous in eyes with failed penetrating keratoplasty for a planned PDEK or DMEK, as it negates higher-order aberrations associated with corneal grafts while also making PDEK/DMEK surgery much easier and faster. In these complex eyes, peripheral anterior synechiae are often seen and result in secondary glaucoma and a higher risk of graft rejection and failure.
As previously explained, PPP has multiple advantages: It opens the closed angle, helps decrease intraocular pressure, and prevents synechiae from reforming—all while providing better optics. PPP may also be performed primarily with a penetrating keratoplasty after removing the cataract and implanting an IOL.
Eyes with mydriatic pupil, e.g., secondary to Urrets-Zavalia syndrome or trauma, can benefit from PPP as well. In patients with corneal scars secondary to corneal pathology or trauma, the PPP helps improve vision without resorting to complex corneal procedures. In the presence of dense corneal neovascularisation where a corneal graft rejection is definite, a PPP can provide good quality functional vision without having to perform a high-risk corneal graft with all its attendant intra- and postoperative complications.
In the next article in this series, I will discuss the technique of evaluating the patient and performing a PPP.
This is the fifth in a multipart tutorial on higher-order aberrations. Previous articles in the series can be found at escrs.org/eurotimes.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.
A triptych of challenges paints a concerning picture for ophthalmologists across the globe.
ANDREW SWEENEY REPORTS
The end isn’t nigh, but challenges do lurk beyond the horizon. In a recent presentation, Kyung Sun Na MD, PhD outlined the three primary emerging trends in the microbial sphere that ophthalmology needs to contend with: the microbiome and its impact on human health, antimicrobial resistance, and environmental changes.
The ocular surface was once excluded from the microbiome as a ‘low biomass niche,’ Professor Na said. However, she added it is now known that commensal microbiota in the eye play an important role in immune tolerance, metabolism, and normal mucosal barrier function.
“The microbiome, tear film, and immune response work together to control ocular surface homeostasis,” she explained. “Current research indicates that the lacrimal gland should

also be included in the microbiome as it controls the ocular surface’s immune reaction and resulting inflammation.”
She further explained microbiome changes in disease show a reduction in Gram-positive organisms, a relative increase in Gram-negative organisms, and “a trend towards a decrease in alpha diversity.” The last point is particularly apparent in dry eye disease, where alpha diversity is falling; however, the presence of Corynebacterium and Staphylococcus aureus is increasing.
Regarding microbial resistance, Prof Na noted ophthalmology has yet to escape the effects of COVID-19, adding there has been a shift in the microbiological profile of bacterial keratitis, both during and after the pandemic, with a higher resistance observed in Staphylococcus epidermidis, Corynebacterium spp., and Streptococcus spp. to fluoroquinolones.
“We can see that antimicrobial resistance dropped significantly during the COVID-19 pandemic and has not returned to pre-COVID-19 levels,” Prof Na said. “This is apparent in resistance to gatifloxacin, which is commonly used in ophthalmology, and growing resistance to it [in the treatment of] Staphylococcus epidermidis, Corynebacterium spp., Streptococcus spp., and Pseudomonas.”
Turning to the third trend, Prof Na discussed how environmental factors are affecting diseases like infectious keratitis. As global temperatures continue to rise and more regions adopt a more tropical climate, the incidence and spectrum of pathogens involved in infectious keratitis intensify.
Increased travel and cultural exchanges in the wake of the pandemic are also facilitating the appearance of pathogens once considered rare as well as others new to science. Prof Na pointed to the 2024 outbreak of microsporidial keratoconjunctivitis in Japan and patients receiving corneal ulcer diagnoses as a result of monkeypox virus infections as examples.
“Air quality is also an important issue. Corneas exposed to particulate matter showed early perforation and thinning after infection with Pseudomonas aeruginosa,” Prof Na said.
“New infectious threats and antimicrobial resistance are constantly emerging. Multidisciplinary collaboration and global cooperation are essential to stay ahead.”
Prof Na presented at the 2025 EuCornea congress in Prague.
Kyung Sun Na MD, PhD is a professor at the Catholic University of Korea’s College of Medicine, Seoul. drna@catholic.ac.kr

Transportation plays a big role in when to cut lamella tissue in DSAEK surgery.
ANDREW SWEENEY REPORTS
Aclear divide currently dictates the use of Descemet stripping automated endothelial keratoplasty (DSAEK) to treat endothelial failure: either when the lamella tissue is cut in the operating theatre (surgeon cut) or when it is pre-cut at a tissue bank beforehand. According to Thorbjörg Olafsdottir MD, the use of the pre-cut technique has been increasing, as it is more efficient and eliminates the risk of graft perforation during surgical preparation. But is there a difference in detachment rates between the two techniques?
Dr Olafsdottir decided to find out by comparing the detachment rate of both the surgeon-cut and pre-cut techniques. The resulting retrospective study was conducted between 2019 and 2023 at Skåne University Hospital, Lund, Sweden.
Patients were split into three groups based on graft preparation: surgeon-cut in the operating theatre, pre-cut and transported in a dextran-containing medium, and pre-cut and transported in a dextran-free medium.
Further categorisation occurred according to risk factors for graft transplantation, of which the primary factors were a previous vitrectomy, the presence of glaucoma drainage devices, and anterior segment malformations. A single surgeon performed all surgeries in the study.
In all, 265 DSAEK surgeries were performed on 240 patients. Out of the total number of surgeries performed, 135 used the surgeon-cut technique, 82 the pre-cut technique with dextran involvement, and 48 the pre-cut technique without dextran involvement.
The mean age of the patients and donors involved in the study was comparable. However, the pre-cut, dextran-free group showed an overrepresentation of female recipients and male donors. At 1.7%, patients with risk factors were also overrepresented in this group.
A significantly higher detachment rate was found among patients receiving pre-cut grafts transported in a dextrancontaining medium (32.9%) compared to surgeon-cut grafts (14.1%) and pre-cut grafts transported in a dextran-free medium (6.3%). The findings applied to all graft recipients, including those with and without risk factors for graft detachment.
Dr Olafsdottir noted that similar results are only encountered in adolescent patients without any known risk factors, which she said makes the findings very statistically significant.
From these findings, Dr Olafsdottir suggested that using precut DSAEK tissue transported in a dextran-containing medium should be excluded from clinical consideration due to the high detachment rate. She explained that this could be due to dextran being a polysaccharide with viscous properties, which may affect tissue adhesion, although further investigation is required.
Dr Olafsdottir presented at the 2025 EuCornea congress in Prague.
Thorbjörg Olafsdottir MD is a clinical researcher at Lund University, Sweden. thorbjorg.olafsdottir@med.lu.se
New ophthalmology-specific microarray could significantly improve patient outcomes.
ANDREW SWEENEY REPORTS
Ophthalmology needs a dedicated polymerase chain reaction (PCR) panel, according to Madhavan Rajan MD.
Noting it as a vexing gap in technology for ophthalmologists, he said the materials required to create such a dedicated PCR panel are available, yet demand remains unmet.
“Presently, for the diagnosis of infections such as vision-threatening keratitis, the detection of an organism requires multiple scrapes and multiple microbial investigations. This process can take days, causing delayed diagnosis,” Professor Rajan said.
“We do not have a panel for ophthalmology. We do not have a PCR panel [capable of] detecting the most common ocular pathogens.”
Prof Rajan presented his intended solution: the iCAM test. It’s a single-sample test involving a corneal epithelial scrape with the capacity to screen for multiple ocular pathogens.
The iCAM project involves multiple experts on molecular diagnostics at the universities of Cambridge and Anglia Ruskin in England, including PCR specialists, microbiologists, and clinicians. The team developed the iCAM test using data spanning more than two decades as part of their research.
Thermo Fisher Scientific constructed the panel the team created, and it features 96 targets specific to ophthalmology, including bacteria, viruses, fungi, and Acanthamoeba. It also included positive controls, human genome regulatory single-nucleotide variant predictors, MRSA, microsporidia, and toxoplasmosis and histoplasma.
If there are co-infections, [the test] would also be able to pick up Acanthamoeba together with fungi within about 4 to 5 hours.
The iCAM was then subjected to internal quality control using external quality assessment panels and synthetic plasmid controls. Samples were processed within 4 to 5 hours “in the best situation,” and all were complete in less than 20 hours.
A subsequent clinical trial involved 34 patients with acute infective keratitis, with two samples taken from each: one for conventional microbial scraping and another for the iCAM.
Prof Rajan reported the iCAM was equally effective as conventional microbial testing, with better sensitivity for Acanthamoeba and fungal organisms. The sample reporting time was less than 24 hours for all iCAM tests—much faster than conventional testing.
The iCAM, he said, promises to fill the gap in rapid diagnostics for acute, sight-threatening keratitis, adding it will also help doctors institute the “proper antimicrobial as fast as possible” and aid in avoiding polypharmacy.
“We have heard from other speakers around the globe [how] the detection rate [of keratitis] still lingers around 50% in even the best situations. The iCAM panel could increase this rate to 80% and make it very easy to identify multiple causative organisms as in polymicrobial keratitis,” Prof Rajan said.
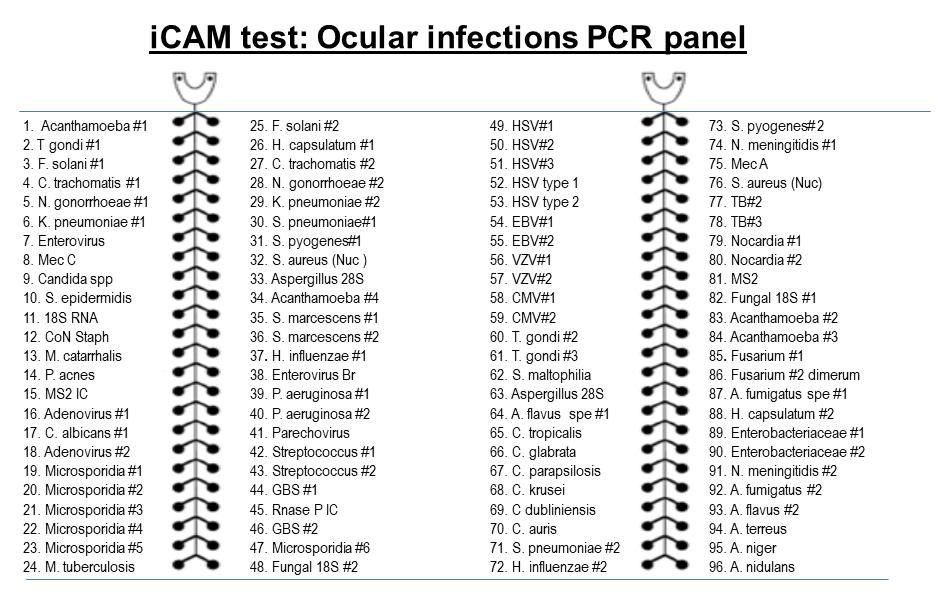
“If there are co-infections, [the test] would also be able to pick up Acanthamoeba together with fungi within about 4 to 5 hours. This compares to waiting for days before unravelling this type of mystery.”
Prof Rajan presented at the 2025 EuCornea congress in Prague.
Madhavan Rajan MBBS, MS, MD, FRCSEd, FRCS(Glas), FRCOphth is a Consultant Ophthalmologist and Clinical Lead for the Cornea and Cataract service at Cambridge University Hospitals and Clinical Academic at University of Cambridge and Anglia Ruskin University, UK. madhavan.rajan1@nhs.net
Vabysmo shows promise with a 98% reduction in corneal neovascular area.
ANDREW SWEENEY REPORTS
Anew anti-vascular endothelial growth factor (VEGF) treatment shows considerable promise in treating corneal neovascularisation, according to Magdalena Niestrata MBChB(Hons), PhD.
“New vessel growth into the avascular cornea has several aetiologies, including trauma, infection, inflammation, and chemical injury. It causes significant morbidities [such as] loss of and reduced vision, and can increase the risk of corneal graft rejection,” Dr Niestrata said.
“Conventional treatments include addressing the root cause of the neovascularisation, as well as corticosteroids, argon laser photocoagulation, and corneal transplantation. There is also, of course, anti-VEGF.”
Vabysmo (faricimab, Genentech) is an anti-VEGF treatment with a bispecific antibody that inhibits both anti-VEGF and angiopoietin-2, which reportedly decreases migration and replication of endothelial cells (allowing for the stabilisation of vascular structures), and provides improved, sustained efficacy compared to agents only targeting the VEGF pathway.
To highlight its efficacy, Dr Niestrata pointed to the results of her study at the Colchester Eye Centre (Essex, England) of 17 patients with corneal neovascularisation refractory to other treatments, which took place between 2023 and 2025. The participants suffered from numerous aetiologies, including trauma, corneal melt associated with rheumatoid arthritis, viral keratitis, and keratoconus.
98%
We achieved a near-complete resolution after treatment, with the neovascular area reduced by 98%.
Vabysmo 6 mg/0.05 mL was administered on a slit lamp and injected in divided doses intrastromally and subconjunctivally at sites nearest the new vessels, sparing the superior limbus. Pre- and postoperative anterior segment images were taken of all participants.
Describing the results of the study as a “first-in-world success,” Dr Niestrata reported that Vabysmo was “very effective as a treatment for corneal neovascularisation.” The average corneal invasion area fell by 92%, the neovascular area was reduced by 98%, and most cases exhibited near-complete vessel reduction.
“Case 1 involved significant vascularisation with keratopathy. In the post-treatment picture, it looks like the patient has a completely different eye, with fully resolved vascularisation,” Dr Niestrata said.
“In case 2, we observed quite significant vascularisation combined with lipid keratopathy. Post-treatment, the vascularisation was virtually resolved, and while some lipid keratopathy remained, the patient improved significantly.
“In cases 3 and 4, there was pretty much 360-degree vascularisation of the cornea going all the way to the centre. We achieved a near-complete resolution after treatment, with some central scarring.”
Dr Niestrata explained further studies were required to confirm its effectiveness; however, she did emphasise that her findings highlight Vabysmo’s “significant clinical benefit.” She said this could be attributed to its unusual dual action on VEGF and angiopoietin-2, which helps it to decrease migration and replication of endothelial cells.
Dr Niestrata presented at the 2025 EuCornea congress in Prague.
Magdalena Niestrata PhD(Dist), MSc(Dist), MBChB(Hons), BSc(Hons), PGDip(Dist), FRCOphth, FEBO, FICO is a Corneal Fellow at the East Suffolk and North Essex Hospital Trust, Colchester, UK. magdalena.niestrata@doctors.org.uk
Modifying or discarding major contraindications for keratoplasty could mean more patients have their sight restored.
ANDREW SWEENEY REPORTS
With any transplant procedure comes risk, but ophthalmologists may be too cautious, according to Gilles Thuret MD, PhD.
Demand for corneal transplantations is rising exponentially across the globe, yet remains largely unmet—due, in part, to the high number of medical contraindications.
The six most common of these contraindications, Dr Thuret said, are neurodegenerative disease, malignant haematological disease, melanoma, neoplastic meningitis, lymphangitic carcinomatosis, and tumours of the central nervous system.
Based on his previous research into the issue, Dr Thuret believes “many contraindications regarding corneal donation and allocation need to be reviewed and modified—or discarded altogether.” If achieved, he argues the corneal donor pool could increase by up to 70%.
To start this process, Dr Thuret polled surgeons regarding their perception of the risks associated with corneal transplantations and the ways they convey such risks to their patients. Sixty-six of the 110 surgeons who perform keratoplasty in France submitted responses.
The poll asked, “How often do you explain the risk of the transmission of general disease during transplantation to patients?” Of the respondents, 35% said they never did, while 36% only did so sometimes.
When asked why, 65% of these respondents said it was their belief “the risk [of disease transmission] was lower than that of other risks,” which Dr Thuret described as a “good approach.”
The surgeons were then asked which of the six contraindications they believed could be eliminated. The
results were as follows: neurodegenerative disease, 59%; malignant haematological disease, 45%; melanoma, 48%; neoplastic meningitis, 41%; lymphangitic carcinomatosis, 41%; and tumours of the central nervous system, 64%.
“Approximately 50% of surgeons think it’s okay for [there to be] a revision of the contraindication list, while the other 50% remain unsure,” Dr Thuret said. “There were two kinds of responses of ‘no’, the first being that the ‘risk is likely or proven’ [15% of surgeons polled], which can be addressed with educational activities.”
The second group—constituting the majority of those who responded ‘no’ (and 35% of the total number of doctors polled)—said they did so because “the precautionary principle must be applied.” Dr Thuret described this reaction as “unfortunate, as it is much less accessible to scientific reasoning.”
Dr Thuret said “taking refuge behind the precautionary principle” serves as a major brake on progress in this particular field. However, with the majority either willing to withdraw the contraindications or remaining open to change their minds based on evidence, he said he plans to launch a clinical trial to demonstrate the safety of these previously ineligible donors, who “would increase the donor pool by more than 70%.”
Dr Thuret presented at the 2025 EuCornea congress in Prague.
Gilles Thuret MD, PhD, IUF is a clinical professor at Jean Monnet University in Saint-Étienne, France. gilles.thuret@univ-st-etienne.fr


A world-first trial suggests a new medication could beat the disease.
ANDREW SWEENEY REPORTS
An effective treatment for Acanthamoeba keratitis could soon be available, a Dutch study suggests.
This topic is particularly crucial, said Yexin Ye MD, as although the organism is rare, it is vision-threatening and there is currently no international consensus on its treatment.
Dr Ye reported that, according to the Dutch Ophthalmic Society, the best course of action for Acanthamoeba keratitis is to start treatment immediately. She said the society recommends either combination therapy using biguanide and diamidine or monotherapy with biguanide alone.
However, despite prescribed aggressive treatment, patient outcomes remain poor.
“Without adequate treatment, 80.4% of patients affected by Acanthamoeba keratitis require keratoplasty or enucleation without anti-amoebic therapy,” Dr Ye said.
Enter polihexanide 0.8 mg/mL. Currently the only EMAapproved treatment for Acanthamoeba keratitis, it is a polymeric biguanide active against Acanthamoeba trophozoites and cysts.
Dr Ye said her study presents the first real-world experience of using polihexanide 0.8 mg/mL to treat Acanthamoeba keratitis in the Netherlands. Conducted as a retrospective case study involving eight patients between October 2022 and March 2025, under which the drug was administered according to compassionate use, pre-market guidelines.
All but one of the patients were contact lens wearers whose diagnoses were primarily confirmed by polymerase chain reaction/corneal culture. All had been treated with antibiotics, 62.5% with corticosteroids and 50% with antivirals. The majority, 75%, were in stage II of the disease.
Days from symptom onset ranged from 21 to 1,201. Duration of treatment ranged from 203 days to more than 100, respectively. Most patients had prolonged symptoms and experienced prior treatment.
This study presents the first real-world experience using polihexanide 0.8 mg/mL to treat Acanthamoeba keratitis in the Netherlands.
While one patient had to discontinue topical application of polihexanide 0.8 mg/mL due to a toxic response, Acanthamoeba keratitis was otherwise resolved in six out of eight patients with no signs of active infection or inflammation after epithelial closure and no required enucleations. The treatment of the remaining patients is ongoing.
Images of one of the patients’ eyes showed clear, visible improvement after treatment with polihexanide. In this case, no vision improvement surgery was necessary, though 50% of patients involved in the study did require it.
Concluding, Dr Ye said the fact no enucleations or keratoplasties were required for the patients in the study, who may otherwise have had an 80% chance of undergoing these procedures, “highlights the efficacy of polihexanide 0.8 mg/ mL.” She expressed hope for more trials into the use of this treatment, especially to help reduce potential toxic response.
Dr Ye presented at the 2025 EuCornea conference in Prague.
Yexin Ye MD, BSc is a PhD candidate in ophthalmology at the University of Maastricht, Netherlands. yexin.ye@mumc.nl
Alternative currently approved in Japan could help mitigate cases of corneal honeycombing.
ANDREW SWEENEY REPORTS
Cases of reticular corneal epithelial oedema (RCEE) are on the rise. What’s behind this increase in ‘honeycombing’?
RCEE occurring after treatment with the Rho-associated protein kinase inhibitor (ROCK) netarsudil (Rhopressa, Alcon) is a growing problem. Approved for glaucoma treatment in the US and EU, the drug’s most common side effects include conjunctival hyperaemia, haemorrhage, and cornea verticillata.
RCEE, a rarer side effect, is usually encountered in patients treated with netarsudil who also have pre-existing corneal disease, such as corneal oedema. However, cases of RCEE, characterized by its honeycomb-like pattern of superficial epithelial bullae on the cornea, are increasing, reports Ursula Schlötzer-Schrehardt PhD.
To find out more, Professor Schlötzer-Schrehardt examined a 32-year-old patient with secondary open-angle glaucoma who developed RCEE following netarsudil administration. She wanted to determine whether ripasudil (Glanatec, Kowa Pharmaceuticals), another ROCK inhibitor currently approved for use in Japan, could be an effective treatment for the patient without the risk of developing or exacerbating RCEE.
Prof Schlötzer-Schrehardt considered two hypotheses to explain bullae development associated with honeycombing. The first suggested that improved corneal endothelial pump function from a shift from stromal oedema to the corneal epithelium was the cause. The second explored whether fluid entry from the stroma into the corneal epithelium due to impaired epithelial barrier function served as the culprit.
Both hypotheses were tested in vitro using primary human corneal endothelial cells (pHCEnC) and primary human corneal epithelial cells (pHCEpC). These were incubated with netarsudil and ripasudil at subclinical concentrations which would not induce cellular toxicity.
can negatively affect cell barriers, causing epithelial bullae formation, ROCK inhibitors should stabilize proper cell function while also improving barrier function.
“Ripasudil would continuously upregulate all the molecules relevant [to the] cell matrix adhesion structure. On the other hand, netarsudil had no effect on these structural components—or even actively downregulated them,” Prof Schlötzer-Schrehardt said.
“Ripasudil appears to be superior to netarsudil in upregulating epithelial tight and adherens junctions, improving epithelial barrier function. It thereby enhances resistance to fluid entry into the epithelial layer from the stroma, preventing bullae formation.”
Ripasudil appears to be superior to netarsudil in upregulating epithelial junctions, strengthening the corneal barrier, and preventing bullae formation.
The first hypothesis resolved swiftly. Prof SchlötzerSchrehardt reported that both netarsudil and ripasudil “improved endothelial pump function but showed no relevant difference in effects and supported the use of both drugs in clinical use for corneal endothelial dysfunction and restoration.”
The second hypothesis yielded more answers. Prof Schlötzer-Schrehardt pointed out that, as Rho-kinase activities
Prof Schlötzer-Schrehardt added that while RCEE-associated honeycombing caused by netarsudil use is serious, it is also reversible, as discontinuation of the drug results in the normalization of the cells after six days. She emphasized ROCK inhibitor drugs such as netarsudil do improve corneal endothelial function, but clinicians should be aware of their potential side effects on the corneal epithelium as well.
Prof Schlötzer-Schrehardt presented at the 2025 EuCornea congress in Prague.
Ursula Schlötzer-Schrehardt PhD is a scientist at the Friedrich-Alexander University of Erlangen-Nuremberg, Germany. ursula.schloetzer-schrehardt@uk-erlangen.de

Need a quick introduction or refresher about a surgical procedure? Have a tip to share about a technique or approach you use that makes surgery easier?
The ESCRS 100 is the place to go. It’s a library of short (roughly 100 seconds), high-quality instructional videos about all fields of cataract and refractive surgery.
More than 40 videos have already been created, and additional videos are being uploaded each month.
Current videos include the following topics:
• Glass Rod technique to remove Soemmering's ring remnants
• Primary posterior capsulorhexis in the presence of a posterior capsule plaque
• Endoilluminator-assisted cataract surgery
—PUT THE ESCRS 100 VIDEO SERIES ON YOUR LIST OF MUST-WATCH EDUCATIONAL RESOURCES ! ESCRS 100
Prophylactic measures and appropriate monitoring decrease risk of significant consequences.
CHERYL GUTTMAN KRADER REPORTS
Intravitreal injections are known to cause both acute and chronic elevations in intraocular pressure (IOP). Lilian Nguyen MD discussed these risks and strategies for mitigating potential harm at a recent conference.
In most patients, any intravitreal injection will cause an immediate and very transient increase in IOP. This acute increase occurs as a volume effect and tends to be lower in those with longer eyes and those with a deeper anterior chamber. However, IOP can spike above 40 mmHg, re-equilibration may take longer in glaucomatous eyes, and the increase in IOP is sometimes sustained.
Reviewing some literature on this topic, Dr Nguyen cited a case-control study suggesting a dose-related association between chronic IOP elevation and anti-VEGF injection. In this study, eyes receiving seven injections or more per year had a higher incidence of glaucoma surgery compared to eyes receiving three injections or fewer per year.1
She also discussed a retrospective cohort study that found eyes receiving anti-VEGF injections for exudative age-related macular degeneration (AMD) were not at increased risk of developing glaucoma compared with controls that had dry AMD or no AMD.2 However, in a subgroup analysis of eyes with a pre-existing glaucoma diagnosis, eyes receiving intravitreal injections showed greater glaucoma progression and required more intensive management.
Relative to anti-VEGF agents, intravitreal corticosteroid agents are associated with a greater risk of sustained IOP elevations and glaucoma. Patients with glaucoma, a family history of glaucoma, type 1 diabetes, connective tissue disease, high myopia, and those who are older or very young (six years old or younger) are at particular risk for steroid-induced glaucoma.
“For appropriate management, it is important to know IOP elevations after intravitreal steroid injections typically occur two to four weeks after the procedure, although earlier onset can occur in pseudophakic or post-vitrectomised eyes,” Dr Nguyen said. “In addition, although IOP tends to peak at two months post-injection, chronic ocular hypertension can occur in up to one-third of eyes.”
Management strategies
Prophylactic measures for mitigating the acute IOP response to intravitreal injections include treatment with a topical IOPlowering medication before the injection or anterior chamber paracentesis in high-risk eyes. For managing sustained IOP elevations, there is evidence of efficacy using topical IOPlowering medications, selective laser trabeculoplasty, and various surgical procedures.

Vigilance for early detection of IOP elevations, however, is paramount for effective management, Dr Nguyen said.
“That means IOP should be checked immediately before and immediately after injection and then at every subsequent follow-up visit,” she explained. “In patients receiving intravitreal steroids, it is especially important to monitor IOP at around four to six weeks post-injection, as this is when subacute increases in IOP tend to occur.”
Dr Nguyen noted the need for more research on the longterm effects of repeated intravitreal injections and of the more recently available intravitreal agents. She also advocated for standardised protocols for IOP monitoring after intravitreal injections.
“Protocols are especially needed in patients with known risk factors and could include implementing IOP measurement into the routine workflow of injection clinics,” she said.
Dr Nguyen presented at the 2025 ASCRS annual meeting in Los Angeles.
For citation notes, see page 32.
Lilian Nguyen MD is Clinical Assistant Professor of Ophthalmology, The University of Texas Health Science Center at San Antonio, Texas, US. lilian.nguyen@gmail.com

Ophthalmologists and researchers (MD and/or PhD) as well as experienced ophthalmic nurses are encouraged to apply for the new ESCRS Sustainability Research (SURE) Award, which will fund projects that investigate meaningful, practical ways to promote environmental responsibility in ophthalmic care.
Two awards will be granted; each award will provide up to €10,000 per project. Applicants must be active ESCRS members at the time of application and must hold a current full- or part-time clinical or research position at a clinical or academic institution. Early-career researchers and young ophthalmologists are especially encouraged to apply.
The application period closes 01 November. Award recipients must submit an article to a peer-reviewed journal within six months after the research period concludes. The article should be made open access if accepted and submitted to the Journal of Cataract & Refractive Surgery in the first instance.
Get funding for projects to promote environmental responsibility in ophthalmic care.
Alcon will acquire Staar Surgical, maker of the Implantable Collamer Lens (ICL), under a definitive merger agreement. The deal covers the EVO ICL™ lens range for patients with moderate to high myopia, with or without astigmatism. Alcon will buy all Staar shares at $28 each in cash—a 59% premium to the 90-day VWAP and a 51% premium to the 4 August 2025 closing price—valuing the deal at roughly $1.5 billion. alcon.com
AAVantgarde Bio received FDA Fast Track designation for AAVB-039, a gene therapy in phase 1/2 trials for Stargardt disease secondary to biallelic ABCA4 mutations. The treatment aims to provide a full-length ABCA4 protein to benefit all patients with mutations of the gene. aavantgarde.com
Topcon Healthcare has invested in OKKO Health, a UK company specializing in vision testing software. OKKO Health’s smartphone app helps patients to monitor their eye health at home through a puzzle game that uses phone sensors for accurate measurements of features of vision. The partnership aims to enhance remote vision monitoring and patient engagement with eye care teams. topconhealthcare.com; okkohealth.com
Ocular Therapeutix has received an FDA Special Protocol Assessment (SPA) agreement for its Axpaxli (OTX-TKI) registrational trial in nonproliferative diabetic retinopathy (NPDR), advancing its reach beyond wet AMD. The SPA shows FDA approval of the trial’s design and goals. Axpaxli, a bioresorbable hydrogel implant delivering axitinib—a multi-target tyrosine kinase inhibitor—is being studied for several retinal conditions, including DME and NPDR. ocutx.com
Lenz Therapeutics has received FDA approval for Vizz (aceclidine ophthalmic solution, 1.44%), the once-daily, preservative-free eye drop for presbyopia. US samples will be available by October 2025, with a broader launch later. In phase 3 CLARITY trials, 71% of users improved near vision by at least three lines at 30 minutes and 3 hours without losing distance vision, and 40% maintained this improvement for 10 hours. lenz-tx.com
Boehringer Ingelheim and Re-Vana Therapeutics have announced a collaboration to develop extended-release eye disease therapies, in a deal that could be worth more than $1 billion for Re-Vana. Boehringer Ingelheim, a German pharmaceutical company, has four ophthalmic candidates in phase 2 trials and a broad human and animal health pipeline. Re-Vana, headquartered in Belfast, specializes in biodegradable ocular drug delivery systems designed to provide 6 to 12 months of sustained release and reduced injection frequency. boehringer-ingelheim.com; revanatx.com
Myra Vision received conditional FDA approval to begin a US trial of its Calibreye System for glaucoma. The ADAPT study will test the adjustable aqueous shunt in up to 70 refractory glaucoma patients over 12 months. Calibreye features four valve settings and can be adjusted postoperatively with a green laser. myravision.com

A new meta-analysis indicates oral and intravenous (IV) sedation provides comparable pain control during phacoemulsification with no increase in complications. The study’s authors reviewed 12 randomised controlled trials including 1,130 patients that compared IV with oral or no sedation and used a validated pain scale to report on pain or perioperative complications. Their analysis indicated IV sedation reduced patient-reported pain by half compared with no sedation. However, they also found no meaningful difference in pain scores between IV sedation and oral sedation with drugs such as triazolam or diazepam. In addition, there was no difference in complication rates between IV and oral sedation.
A Hanna, et al. “Intravenous vs nonintravenous sedation for cataract surgery: systematic review and meta-analysis,” 51(8): 723–730.

Remote monitoring is an effective approach for postoperative care in stable, low-risk patients following cataract surgery, according to a new retrospective review. The study’s authors analysed four randomised controlled trials and 10 observational studies on digital tools, telemedicine, or remote care in postoperative cataract management. Outcome measures included patient-reported outcomes, visual acuity, refraction, intraocular pressure, slit lamp and fundus examination, or complication prevalence. Their analysis showed nurse- or surgeon-led calls did not increase unplanned visits or complications and achieved more than 90% patient satisfaction. In addition, text message reminders increased medication adherence from 73% to 96% without altering intraocular pressure or inflammation, and an artificial intelligence call bot alerted to red-flag symptoms with 93.8% sensitivity and 86.3% specificity. Furthermore, home-based visual acuity tools measured uncorrected vision within 0.07 logMAR of standard charts and assessed refraction with a 0.32 D mean error.
JC Wanten, et al. “Efficacy of remote care in cataract surgery: systematic review,” 51(8): 731–739.
Broader adoption of immediate versus sequential bilateral surgery can reduce the environmental impact of patients’ perioperative care, according to a new cross-sectional survey. The authors surveyed 89 high-volume cataract centres across 16 European countries regarding their preoperative and postoperative visit patterns and environmental costs. In delayed sequential bilateral surgery, the average patient logged 1.3 preoperative visits per eye and 3.8 postoperative reviews, totalling 5.7 trips. Immediate sequential bilateral approaches cut that burden nearly in half—yet fewer than half of surveyed centres offer same-day bilateral surgery, and only 7% provide any virtual follow-up. The study also revealed a striking national variance in total visits per patient, ranging from 2.6 in the UK to 4.7 in Germany. While travel accounts for 10% to 31% of cataract surgery’s carbon footprint, there remains significant potential to optimise care for patient convenience and better ecological outcomes.
D Yang-Seeger, et al. “Perioperative practice patterns for cataract surgery: a cross-sectional European study,” 51(8): 647–651.
What is the one leadership skill you would like to improve? What is the one business management challenge you would like to overcome?
The ESCRS Leadership, Business, and Innovation (LBI) programme provides ophthalmologists, clinic managers, and administrators and their teams with a variety of content to enable both online and in-person learning. Podcasts, webinars, video interviews, and more are available in the LBI library to help answer questions about topics such as selling a practice, finding a good work-life balance, facilitating patient decision making, and more.
Avoiding Intracorneal Ring Segment Complications
Page 11
1. Alfonso JF, et al. Int J of Keratoconus Ectatic Corneal Dis, 2025; 11(1): 1–8. doi:https://doi.org/10.5005/jp-journals-10025-1207.
2. D’Oria F, et al. Am J Ophthalmol, 2021 Feb; 222: 351–358.
3. Monteiro T, et al. Cornea, 2018 Feb; 37(2): 182–188. doi:https://doi.org/10.1097/ICO.0000000000001449.
4. Monteiro T, et al. J Refract Surg, 2018 Mar 1; 34(3): 188–194. doi:https://doi.org/10.3928/1081597X-20180108-01.
5. Monteiro T, et al. Curr Eye Res, 2019 Dec; 44(12): 1291–1298.
Femto-Phaco for Posterior Polar Cataracts?
Page 12
1. Hayashi K, Hayashi H, Nakao F, et al. J Cataract Refract Surg, 2003 Jan; 29(1): 45–49.
2. Kymionis GD, Diakonis VF, Liakopoulos DA, et al. Clin Ophthalmol, 2014; 8: 215–217.
3. Titiyal JS, Kaur M, Shaikh F, et al. J Cataract Refract Surg, 2020 Sept; 46(9): 1266–1272.
4. Vasavada AR, Vasavada V, Vasavada S, et al. J Cataract Refract Surg, 2015 Apr; 41(4): 702–707.
Understanding Long-Term Regression
Page 14
3. Zhou J, et al. Int Ophthalmol, 2020 Jan; 40(1): 213–225.
4. Mimouni M, et al. J Refract Surg, 2018 May 1; 34(5): 316–320.
5. Sorkin N, et al. J Refract Surg, 2024 Feb; 40(2): e73–e78.
6. Kim J, et al. Graefes Arch Clin Exp Ophthalmol, 2022; 260(11): 3701–3710.
Fine-Tuning IOLs After Surgery
Page 15
1. Jones M, et al. J Cataract Refract Surg, 2024 Sep 1; 50(9): 936–941.
2. Lapid-Gortzak R, et al. J Refract Surg, 2023 Oct; 39(10): 662–667.
Matching Premium IOLs to Visual Lifestyles
Page 16
1. Ribeiro F, Dick HB, Kohnen T, et al. J Cataract Refract Surg, 2024; 50(8): 794–798.
IOP Effects of Intravitreal Injections
Page 28
1. Levin AM, et al. J Glacuoma, 2021; 30(12): 1019–1026.
2. Shah SM, et al. Am J Ophthalmol, 2022; 243: 98–108.
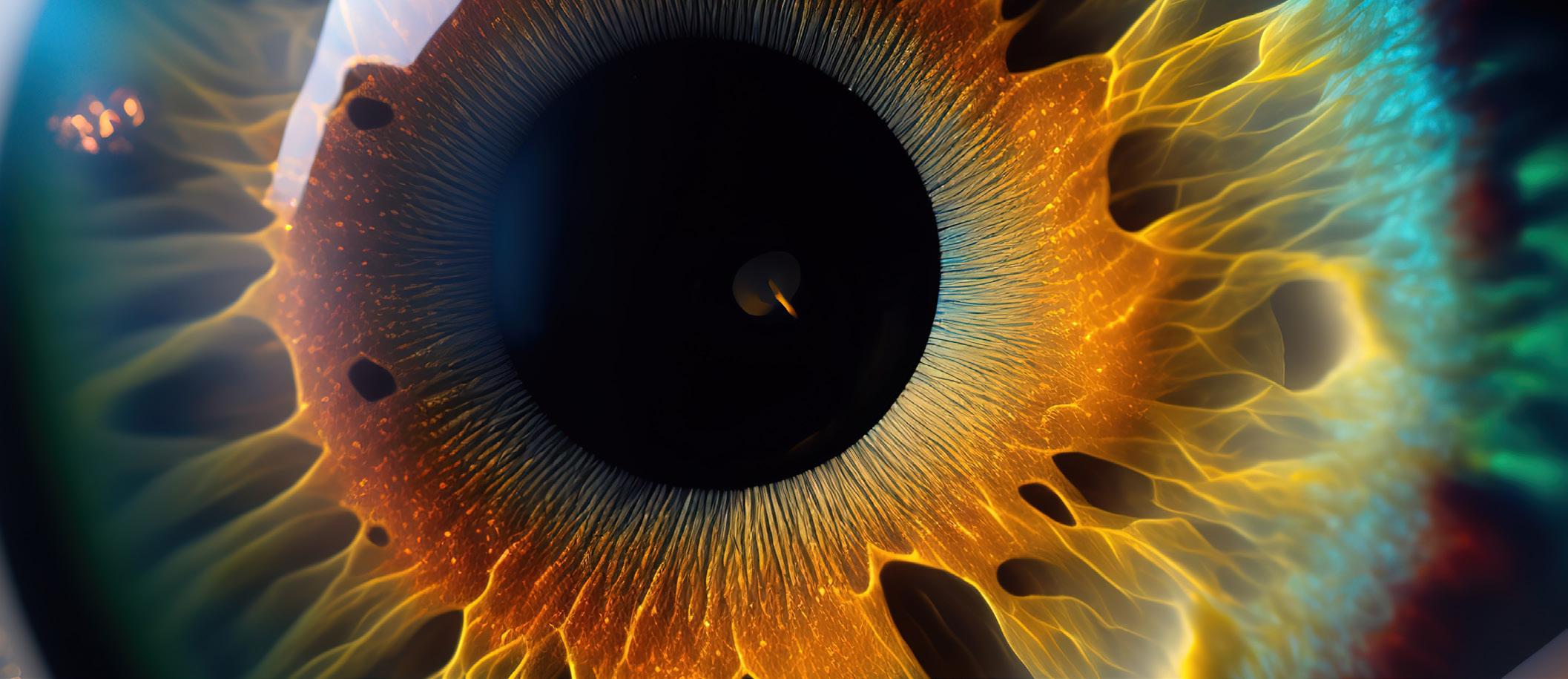
True innovation comes from good research. That’s the impetus for the ESCRS Pioneer Research Award (PRA).
The PRA aims to support and encourage independent clinical research in the field of cataract and refractive surgery. It can fund a variety of new initiatives, which may include—
• A novel research idea for the development of clinical trial studies;
• A non-interventional or observational study; or
• A natural history/epidemiological study.
An award of €25,000 is available for one grant. The competition is open to ophthalmologists up to the age of 45 (at the application deadline). Eligible participants must hold a full-time clinical or research position at a clinical or academic centre within the European region.
Applications are due by 31 October 2025.
October 18–20
American Academy of Ophthalmology Orlando, Florida, US
March 6–8
ESCRS Winter Meeting 2026 Helsinki, Finland
April 10–13
ASCRS Washington, DC, US
May 4–8
ARVO
Salt Lake City, Utah, US

March 6

October 18
April 10


May 4



1-4
• Myopic shift
• Cyclodialysis
• Hypotony
• Significant hyphema ZERO
• Stent dislocation
SAFETY1,2
OVERALL SAFETY PROFILE SIMILAR TO CATARACT SURGERY ALONE3
SIGNIFICANT IMPROVEMENTS IN VISION-RELATED QUALITY OF LIFE5
REFRACTIVELY NEUTRAL5,6,8,9 FEWER FOLLOW-UP VISITS4 DAILY ACTIVITIES7 MENTAL HEALTH7
IMPROVES OCULAR SURFACE HEALTH6,9
REDUCTION IN PATIENTS WITH SEVERE OSD SYMPTOMS5 72%
WITHIN ± 1.0D OF REFRACTIVE TARGET8 99%
1. 7-Year Efficacy and Safety of iStent inject® Trabecular Micro-Bypass in Combined and Standalone Usage. Fritz H. Hengerer . Gerd U. Auffarth . Ina Conrad-Hengerer. 2. Ten-Year Effectiveness and Safety of Trabecular Micro-Bypass Stent Implantation with Cataract Surgery in Patients with Glaucoma or Ocular Hypertension. Tobias H. Neuhann, Raphael T. Neuhann, Dana M. Hornbeak. 3. Samuelson, Thomas W., et al. “Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results.” Ophthalmology 126.6 (2019): 811-821. 4. Rodriguez-Una, Ignacio, Augusto Azuara-Blanco, and Anthony J. King. “Survey of glaucoma surgical preferences and post-operative care in the United Kingdom.” Clinical & Experimental Ophthalmology 45.3 (2017): 232-240. 5. Samuelson, Thomas W., et al. “Quality of life in primary open-angle glaucoma and cataract: an analysis of VFQ-25 and OSDI from the iStent inject® pivotal trial.” American Journal of Ophthalmology 229 (2021): 220-229. 6. Schweitzer, Justin A., et al. “Prospective interventional cohort study of ocular surface disease changes in eyes after trabecular micro-bypass stent (s) implantation (iStent or iStent inject) with phacoemulsification.” Ophthalmology and Therapy 9 (2020): 941-953. 7. Jones, Lee, et al. “Impact of minimally invasive glaucoma surgery on the ocular surface and quality of life in patients with glaucoma.” Therapeutic Advances in Ophthalmology 15 (2023): 25158414231152765. 8. Ioannidis, Alexandros S., et al. “Refractive outcomes after trabecular micro-bypass stents (iStent inject®) with cataract extraction in open-angle glaucoma.” Clinical Ophthalmology (2020): 517-524. 9- Biela, Katarzyna, et al. “Dry eye disease as a cause of refractive errors after cataract surgery–A systematic review.” Clinical Ophthalmology (2023): 1629-1638.
iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATIONS FOR USE: The iStent inject® W, is intended to reduce intraocular pressure safely and effectively in patients diagnosed with primary open-angle glaucoma, pseudo-exfoliative glaucoma or pigmentary glaucoma. The iStent inject® W, can deliver two (2) stents on a single pass, through a single incision. The implant is designed to stent open a passage through the trabecular meshwork to allow for an increase in the facility of outflow and a subsequent reduction in intraocular pressure. The device is safe and effective when implanted in combination with cataract surgery in those subjects who require intraocular pressure reduction and/or would benefit from glaucoma medication reduction. The device may also be implanted in patients who continue to have elevated intraocular pressure despite prior treatment with glaucoma medications and conventional glaucoma surgery. CONTRAINDICATIONS: The iStent inject® W System is contraindicated under the following circumstances or conditions: • In eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations. • In patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS/PRECAUTIONS: • For prescription use only. • This device has not been studied in patients with uveitic glaucoma. • Do not use the device if the Tyvek® lid has been opened or the packaging appears damaged. In such cases, the sterility of the device may be compromised. • Due to the sharpness of certain injector components (i.e. the insertion sleeve and trocar), care should be exercised to grasp the injector body.