



Eric Barna MD
Professor of Medicine and Medical Education
Director of Education DHM
Director of Education Mount Sinai International
Associate Residency program Director, MSH
Acting Internship Clerkship Director ICAHN SOM


1 2 3 4 5 6
KNOW: How to structure and execute a collaborative and educationally rich teaching experience.

DO: Be deliberate in your preparation and grounded in key teaching practices
FEEL: Inspired to seize every clinical moment as a teaching opportunity—and to embrace your role as an educator with confidence

We are dedicated to delivering exceptional care, advancing medical education, and driving groundbreaking research.
8 General Medicine Teaching Services, 16 patients/team with 2 residents, 2 interns, 1 AI and 1 MS3 +/- Pharmacy students
Clinical/Work Rounds: 8am to 10 am
Mandatory Bedside Rounds
Resident Huddle @ 1:30/2pm
Patient mix: Hyperacute/Step Down


Journal of Academic Medicine: A multicenter qualitative study sampled 34 inpatient Attending Physicians from 10 U.S academic institutions. The following categories of barriers to bedside rounding/teaching were identified: Time Patient Driven Systems Issues PhysicianRelated Culture shift

Lack of bedside skill
Lack of comfort
Trainee inefficiency
EMR Shorter LOS
Increased Patient volume 2P’s:
Limited workday
Conferences
Inefficiency
Increased acuity
Patient privacy /HIPPA
Patients understanding
Educational value
Patient centered care is always patient preferred
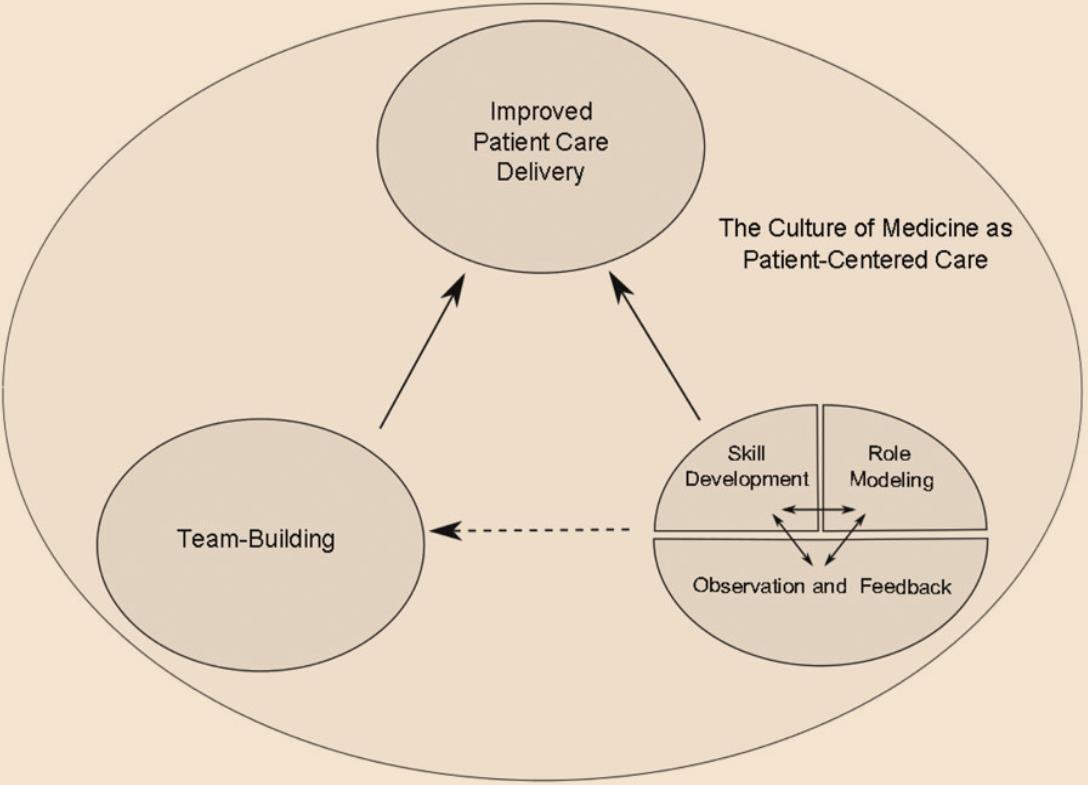
Methods: Recruited faculty from 10 institutions including clerkship directors + prior research experience in medical education and conducted bedside rounds

Data Collection/Analysis: Digitally recorded one to one interviews identifying themes and categories generating a codebook to facilitate analysis
Results: All 10 institutions participated 34 interviews conducted focus was directed at key thematic areas




How do you position your team for bedside rounds?


ATTENDING/ RESIDENT
THE PERFECT TIME TO ASSESS MILESTONE METRICS FOR BOTH RESIDENTS AND MEDICAL STUDENTS


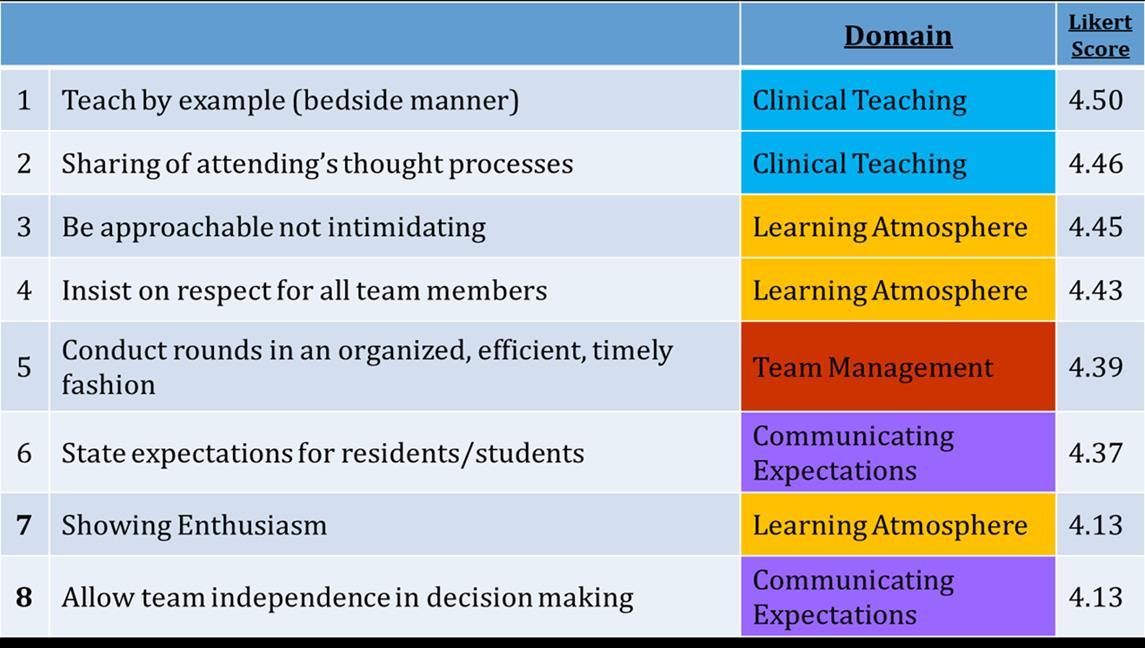
❑Participants: 125Faculty/Residents/Students
5IMresidencyprograms
75%wereresidentsorstudents

❑Participantsrated70attributesofSuccessfulattendingrounds


❑Create a safe and welcoming environment
❑ Email welcome before you come on service
❑Set clear expectations from day one
❑Identify your learners' strengths/interests
❑Use icebreakers
❑Draw a mental image your time together
❑Review the core service expectations on DAY 1 (10 minutes)
❑Set specific goals for each day on rounds (everyday is different)
❑Consider a pre-round huddle with your intern/medical student to map out the morning
❑Specify bedside goals and recognize that these may change

✓ The order of presentations
✓ Presentation style (SOAP)
✓ Mini teaching topics and look ups
✓ Lightning presentations
✓ Safety Checklist


❑ Chart check the night before
❑ “Stealth Round” on new admits
❑ Identify target teaching
❑ Create your lesson plan including- organization, timing, execution, look-ups
❑ Map out Media use
“By failing to prepare, you are preparing to fail”
- Ben Franklin

“Asking the right questions takes as much skill as giving the right answers.”
Recall – What are the 5 criteria for TTP?
Analysis/Synthesis – What led you to that diagnosis?
Application – How will you treat this patient’s pain?
Self Assessment– What would you do differently?




An exam skill Communication
Self Directed Learning
Saying “I don’t know”
Imitation is not just the sincerest form of flattery— it’s the first step in learning.”

❑ Models expert thinking
❑ Demystifies clinical reasoning
❑ Normalizes ambiguity
❑ Reinforces core knowledge
❑ Creates a safe learning space
❑ Promotes habit formation


Creates cognitive space
Unique lens for observation
Richer targeted feedback
Shows Trust and Respect

“Nothing GREAT was ever achieved without enthusiasm” -Emerson

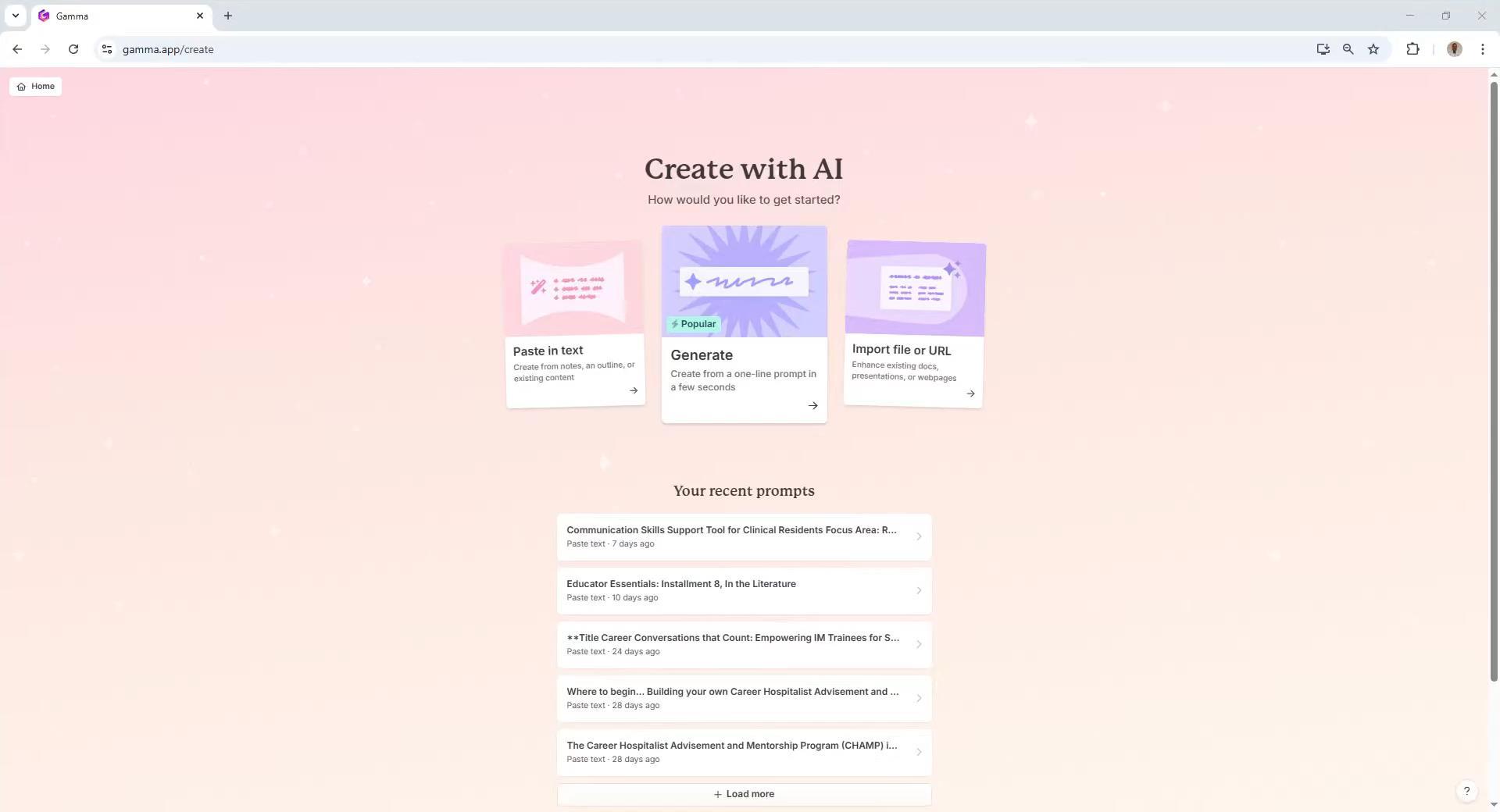
❑ Quick Lesson Plan Generation
❑ Clinical Guidelines and Evidence Summaries
❑ Quick Educational Cards for rounds
❑ Landmark Trial Summary for dissemination
❑ Clinical case simulation
❑ Interview Prep (supplement to the mock interview)



Practical Uses: Create curated podcast links for targeted clinical scenarios that can easily be shared with UME/GME trainees. Consider prompt engineering if you are looking for a specific Podcast.


Example:
55-Year-old male with ETOH-Cirrhosis presenting with hypotension, acute blood loss anemia in the setting of an acute variceal bleed.


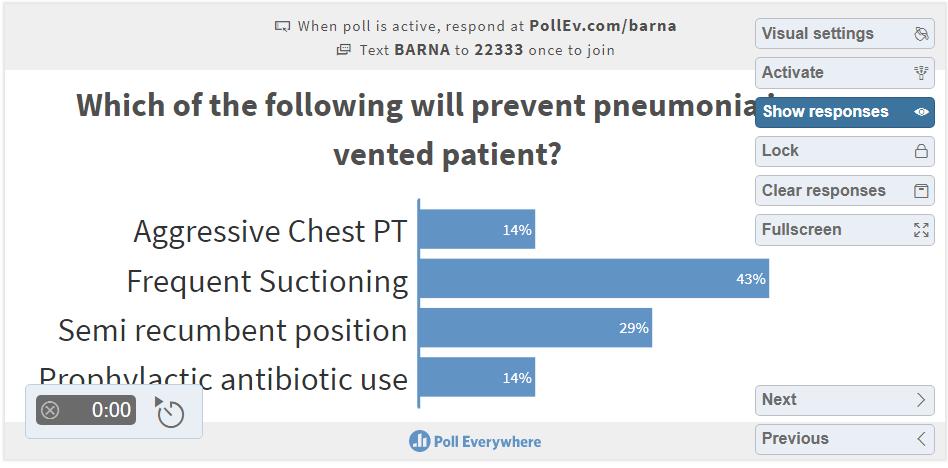
Example: Mr. Johnson is a 70 year old male with a known history of advanced COPD who presented with acute hypoxic respiratory failure was admitted to the MICU, course was complicated by an acute stroke requiring a tracheostomy and a PEG tube placement and he remains ventilator dependent. He is transferred to gen med teaching for continued care.

“Medicine is learned by the bedside and not in the classroom. Let not your conceptions of disease come from words heard in the lecture room or read from the book. See, and then reason and compare and control. But see first.”
-William Osler