



Eric Barna MD MPH
Professor of Medicine and Medical Education
Director of Education, Division of Hospital Medicine
Director of Education, Mount Sinai International
Associate Residency program Director, Mount Sinai Hospital
Acting Internship Clerkship Director, Icahn SOM
Director, Career Hospitalist Advisement Program
Director, Hospital Medicine Elective Experience
I have no financial or professional conflicts to disclose. My only investment is in the growth of our residents and the future of Internal Medicine education.



KNOW: How to structure and execute a collaborative and educationally rich teaching experience.

DO: Be deliberate in your preparation and grounded in key teaching practices
FEEL: Inspired to seize every clinical moment as a teaching opportunity—and to embrace your role as an educator with confidence

Senior residents shape more than decisions. They shape how the next generation learns to think, act, and care….
Model professionalism and psychological safety. Establish shared expectations for communication, feedback, and patient ownership.
Think aloud at key decision points. Coach through differential building and diagnostic pivots. Highlight common cognitive errors.
Deliver focused one-minute teaching moments. Turn real patients into micro-learning opportunities. Use questions to stimulate curiosity.
Demonstrate prioritization strategies. Share approaches to prerounding, handoffs, and EMR efficiency. Help anticipate bottlenecks.
Give formative feedback linked to behaviors. Celebrate growth and name strengths. Model help-seeking and self-regulation.
Invite feedback from the team. Debrief challenging encounters. Adjust teaching goals based on learner needs.


Journal of Academic Medicine: A multicenter qualitative study sampled 34 inpatient Attending Physicians from 10 U.S academic institutions. The following categories of barriers to bedside rounding/teaching were identified: Time Patient Driven Systems Issues PhysicianRelated Culture shift

Lack of bedside skill
Lack of comfort
Trainee inefficiency
Conferences
Inefficiency
Increased acuity
Patient privacy /HIPPA
Patients understanding Educational value Limited
Patient

Methods: Recruited faculty from 10 institutions including clerkship directors + prior research experience in medical education and conducted bedside rounds

Data Collection/Analysis: Digitally recorded one to one interviews identifying themes and categories generating a codebook to facilitate analysis
Results: All 10 institutions participated 34 interviews conducted focus was directed at key thematic areas





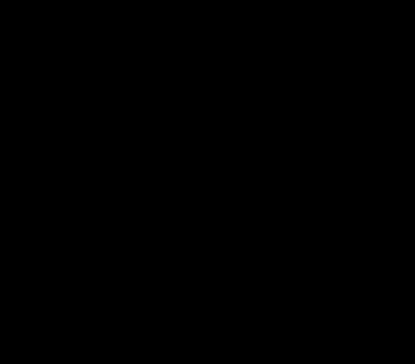
How do you position your team for bedside rounds?


ATTENDING/ RESIDENT
THE PERFECT TIME TO ASSESS MILESTONE METRICS FOR BOTH RESIDENTS AND MEDICAL STUDENTS



❑Participants: 125Faculty/Residents/Students
5IMresidencyprograms
75%wereresidentsorstudents

❑Participantsrated70attributesofSuccessfulattendingrounds



What do you do to set the stage when meeting your team on the first day of a rotation?




❑Create a safe and welcoming environment
❑ Email welcome before you come on service
❑Set clear expectations from day one
❑Identify your learners' strengths/interests
❑Use icebreakers
❑Draw a mental image your time together



❑Review the core service expectations on DAY 1 (10 minutes)
❑Set specific goals for each day on rounds (every day is different)
❑Consider a pre-round huddle with your intern/medical student to map out the morning
❑Specify bedside goals and recognize that these may change

✓ The order of presentations
✓ Presentation style (SOAP)
✓ Mini teaching topics and look ups
✓ Lightning presentations
✓ Safety Checklist

What do you do to prepare before you meet your team/trainees for clinical rounds?



❑ Chart review the evening before: Early “stealth round” on new admissions: See patients briefly before formal rounds to gather insights and set the stage for team discussion.
❑ Highlight target teaching moments: Decide which patients or cases will serve as the best anchors for teaching that day

❑ Develop a structured lesson plan: Plan how you’ll organize teaching, set timing, integrate student participation, and prepare quick references or look-ups.
❑ Plan media or visual aids: Decide if whiteboard sketches, imaging reviews, or brief slide visuals will help reinforce key teaching points.
“By failing to prepare, you are preparing to fail”
- Ben Franklin
My Personal Strategy for Preparing for Clinical Rounds
27-Minute Commute Mental preparation time before arriving at the hospital.
Focus on New Admissions Draft notes to understand the context and fiber of each case.
Identify Teaching Point
Educational Quick Card
Find key learning opportunities for the team.
Create quick reference materials with key evidence.
Think About "Look Ups" Focus on the rotating medical students .
Stealth Rounds Virtually
Check on sickest patients remotely before in-person rounds.
Round on Patients
Complete bedside visits before official clinical rounds begin.




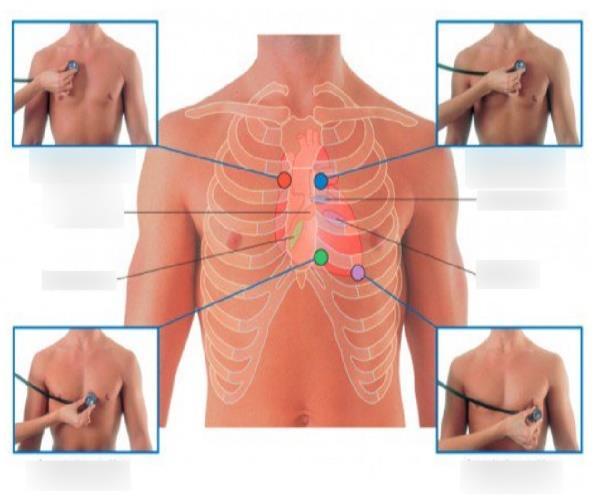
An exam skill Communication
Self Directed Learning
Saying “I don’t know”


Imitation is not just the sincerest form of flattery— it’s the first step in learning.”


❑ Models expert thinking
❑ Demystifies clinical reasoning

❑ Normalizes ambiguity
❑ Reinforces core knowledge
❑ Creates a safe learning space
❑ Promotes habit formation



Creates cognitive space
Unique lens for observation
Richer targeted feedback
Shows Trust and Respect
Think about transition points during the year.. “Resident for a Day” “Attending for a Day”

“Nothing GREAT was ever achieved without enthusiasm” -Emerson





Are any of you currently using AI in when teaching trainees?
❑ Lesson planning
❑ Media generation
❑ Differential diagnosis
❑ Pathophysiology review
❑ Coaching, remediation, feedback
❑ EBM review and dissemination
❑ “On the Go” lookups
❑ Curriculum design




f
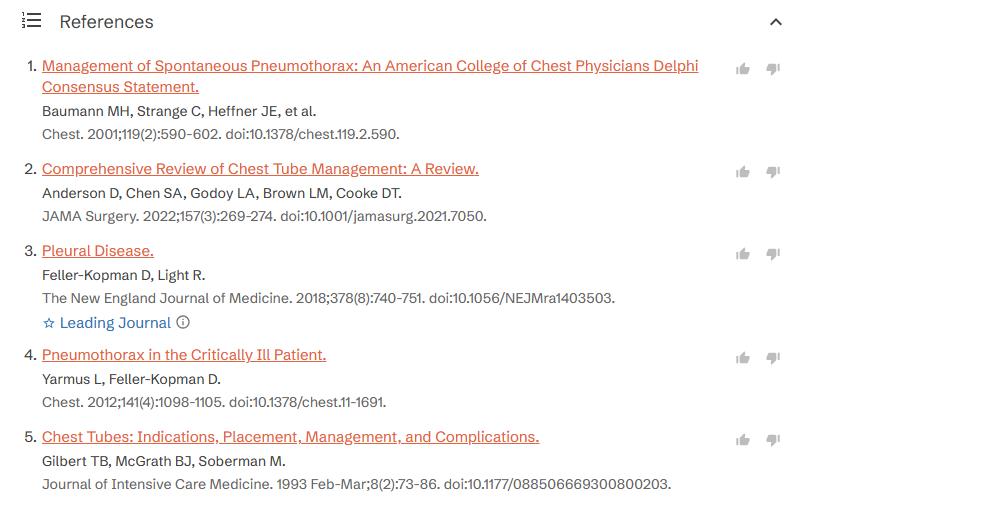
What it is:
❑ AI-driven medical search engine
❑ Synthesizes clinical evidence from top-tier journals (NEJM, JAMA, Lancet, etc.)
❑ Designed for clinicians and educators
Why it matters:
❑ Used daily by 40% of U.S. physicians
❑ Answers clinical questions with citations and reasoning
How faculty can use it:
❑ Stay current: Summarizes guidelines & recent trials
❑ Evidence on demand: Supports case prep and resident teaching
Transforms the “information firehose” into actionable, referenced knowledge in seconds

Featured Technical Tools: Chat GPT4o (now updated to 5)
Practical Uses: Create curated podcast links for targeted clinical scenarios that can easily be shared with UME/GME trainees. Consider prompt engineering if you are looking for a specific Podcast.










Build the Foundation First
1
2
Create a positive learning climate for an impactful educational alliance.
Observe Directly, Feedback Specifically
Base feedback on firsthand observationsof concrete behaviors, not assumptions.
3 Promote Self-Reflection Encourage learners to assess their own performance
4 Be Timely and Formative
Provide immediate, specific feedback throughout rotations, not just at the end.
KNOW: How to structure and execute a collaborative and educationally rich teaching experience.

DO: Be deliberate in your preparation and grounded in key teaching practices
FEEL: Inspired to seize every clinical moment as a teaching opportunity—and to embrace your role as an educator with confidence


To teach medicine is to multiply compassion— every student carries forward a part of their teacher’s care…