Teaching on Rounds: Foundations for New DHM Faculty
Eric Barna MD
Professor of Medicine and Medical Education
Director of Education, DHM
Director of Education, MSI
Associate Residency Program Director
Clerkship Director for the Acting Internship





Eric Barna MD
Professor of Medicine and Medical Education
Director of Education, DHM
Director of Education, MSI
Associate Residency Program Director
Clerkship Director for the Acting Internship




Understand the structure, expectations, and educational principles that drive effective teaching and supervision on the Mount Sinai teaching service. DO: Lead purposeful, organized, and learner-centered rounds that integrate clinical care, teaching, technology, and timely feedback.
FEEL: Confident, inspired, and connected to the shared mission of developing compassionate, curious, and capable clinicians.
Reflecting on your experience on the teaching service, what aspects did you find most challenging?


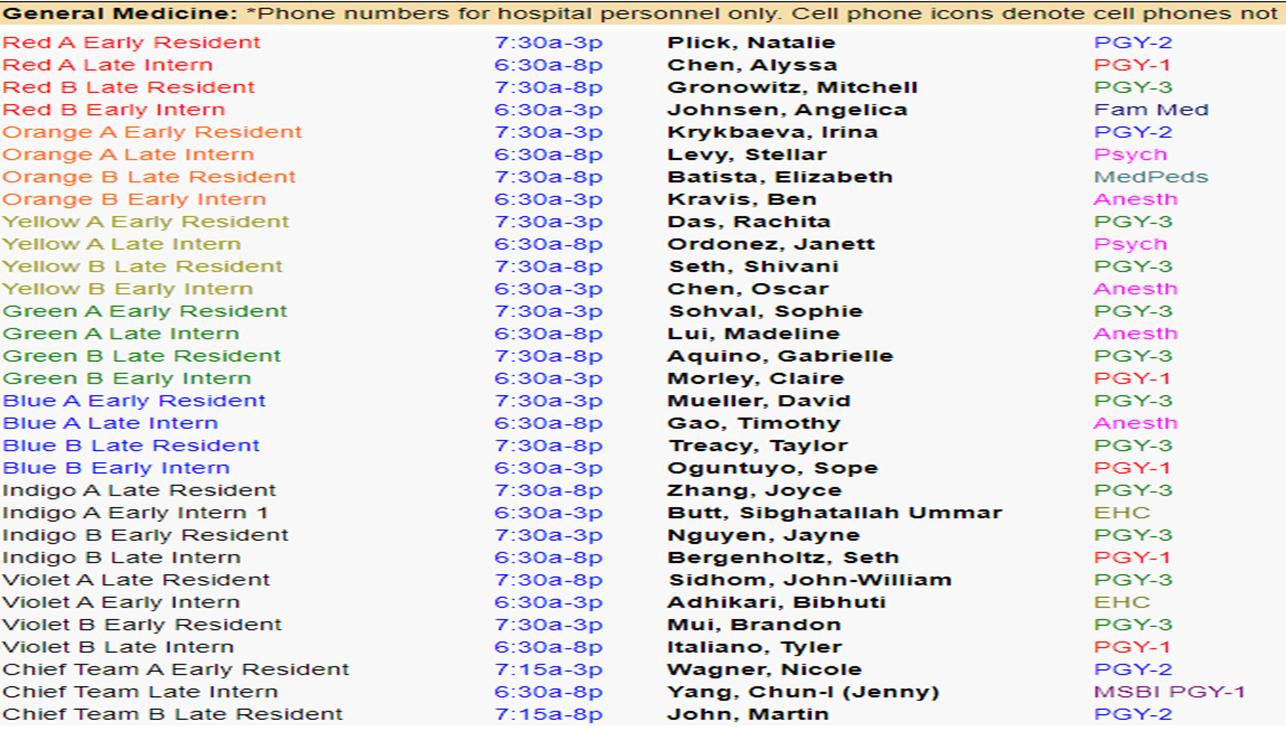
❑ 7 General Medicine Color Teaching Teams
(Red, Orange, Yellow, Green, Blue, Indigo Violet) each with a capacity of 16 patients
❑ 1 Chief Resident Team (launched AY 22/24) with a capacity increase to 16 in AY 25-26 and managed by the chief residents beginning block 7A of each year
❑ 1 High acuity ADS team (staffed by 1 hospitalist and 2 PA’s) with a capacity of 14 patients
❑ Service admission triage follows a “drip system” coordinated by the Medical Admitting Physician Assistant (MAPA)
❑ There are both third- and fourthyear medical students assigned to most teaching teams.
❑ Distribution is random and students cannot request a particular team.
❑ MS3’s: fulfilling the core IM requirement
❑ MS4’s: Functioning as Acting Interns
❑ Email from Navjeet Kaur
Short Call Until 3pm
Total Team Capacity: 16 patients
Hemi-Team Capacity: 8 patients
Long Call Until 8pm



❑ Round early and come prepared with teaching materials
❑ Check in on the pulse of the team to gauge energy and workload
❑ Use silent alarms to pace rounds and stay on time
❑ Touch base with medical students to ensure engagement and learning
❑ Run the list at 1:30 PM to review updates and plans
❑ Send a brief educational summary at the end of the day
❑ Assign “look-ups” to reinforce key learning points
Weekend
❑ Start rounds no later than 9 am
❑ Focus on clinical care alignment
❑ Provide focused and clinically relevant teaching
❑ Remain available until at least 5pm (typically into the evening)
❑ Support resident teams with new admits
Weekend Support Resources
If you need any technical support during the weekend: Contact the lead hospitalist
For any resident related matters contact: Dr. Michael Herscher or Vinh Nguyen

Clerkship Director: Eve Merrill
Associate Clerkship Director: Rex Hermansen
Carry 2-3 patients with resident supervision
Attend All Team Didactic sessions Behave Professionally
***You cannot cosign their notes for billing
5/6 Weeks (3+3)



1 Weekend
Clerkship Director: Eric Barna ***You can cosign their notes for billing





What do you do to set the stage before you meet your team on the first day of a rotation?


Create a safe and welcoming environment
Email welcome
Set Expectations on day one
Identify interests
Use icebreakers
Post round huddle to “check in”
Role
Modeling
Goals of Care
What do you do to prepare before you meet your team/trainees for clinical rounds?



❑ Chart review the evening before: Early “stealth round” on new admissions: See patients briefly before formal rounds to gather insights and set the stage for team discussion.
❑ Highlight target teaching moments: Decide which patients or cases will serve as the best anchors for teaching that day

❑ Develop a structured lesson plan: Plan how you’ll organize teaching, set timing, integrate student participation, and prepare quick references or look-ups.
❑ Plan media or visual aids: Decide if whiteboard sketches, imaging reviews, or brief slide visuals will help reinforce key teaching points.
“By failing to prepare, you are preparing to fail”
- Ben Franklin

Recall – What are the 5 criteria for TTP?
Analysis/Synthesis – What led you to that diagnosis?
Application – How will you treat this patient’s pain?

“Asking the right questions takes as much skill as giving the right answers.”
Self Assessment– What would you do differently?



❑ Models expert thinking
❑ Demystifies clinical reasoning
❑ Normalizes ambiguity
❑ Reinforces core knowledge
❑ Creates a safe learning space
❑ Promotes habit formation


“Nothing GREAT was ever achieved without enthusiasm” -Emerson

❑ Lesson planning
❑ Media generation
❑ Differential diagnosis
❑ Pathophysiology review
❑ Coaching, remediation, feedback
❑ EBM review and dissemination
❑ “On the Go” lookups
❑ Curriculum design

f
What it is:
❑ AI-driven medical search engine
❑ Synthesizes clinical evidence from top-tier journals (NEJM, JAMA, Lancet, etc.)
❑ Designed for clinicians and educators
Why it matters:
❑ Used daily by 40% of U.S. physicians
❑ Answers clinical questions with citations and reasoning
How faculty can use it:
❑ Stay current: Summarizes guidelines & recent trials
❑ Evidence on demand: Supports case prep and resident teaching
Transforms the “information firehose” into actionable, referenced knowledge in seconds


Always verify against guidelines

Citation Integrity
Confirm cited papers (misattributions)


Learners should use it as a consult note
Source Bias

May overemphasize US/Western sources
Privacy and Compliance
Use de-identified cases

Skill Dilution

Teach manual literature review





Example:
55-Year-old male with ETOH-Cirrhosis presenting with hypotension, acute blood loss anemia in the setting of an acute variceal bleed.


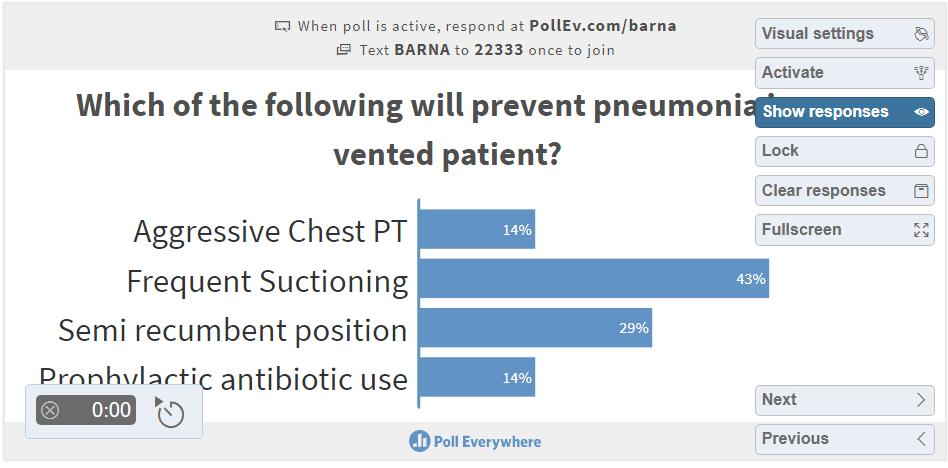
Example: Mr. Johnson is a 70 year old male with a known history of advanced COPD who presented with acute hypoxic respiratory failure was admitted to the MICU, course was complicated by an acute stroke requiring a tracheostomy and a PEG tube placement and he remains ventilator dependent. He is transferred to gen med teaching for continued care.

Beyond structure and strategy, what often leaves the biggest impression on learners is how you show up each day. These core habits help set the tone for a positive, lasting impact:
Be Approachable
Foster an environment where questions feel welcome.
For every member of the team.
Teach by Example
Especially when it comes to bedside manner.
Show Enthusiasm
Energy is contagious.
Empower Residents
With your coaching and support in the background.

Out loud so learners can see how you approach problems.
While guiding residents through reflection and refinement.

These everyday practices are what distinguish a good attending from a great one, shaping both the learning climate and the future physicians you're training.


❑ Supports clinical skill development
❑ Enhances self-reflection and professionalism
❑ Fosters a growth mindset
❑ Improves patient care
❑ Drives engagement and motivation
"If you're not getting feedback, you're not growing. And if you're not growing, you're not leading."
— Patrick Lencioni

Build the Foundation First
1
2
Create a positive learning climate for an impactful educational alliance.
Observe Directly, Feedback Specifically
Base feedback on firsthand observationsof concrete behaviors, not assumptions.
3 Promote Self-Reflection Encourage learners to assess their own performance
4 Be Timely and Formative
Provide immediate, specific feedback throughout rotations, not just at the end.
❑Timely submissions
❑New Innovations for residents and One45 for medical students
❑Honest detailed and specific comments
❑Avoid “read more”
❑Evaluations feed into broader narratives that are high stakes (CCC, MSPE)


Understand the structure, expectations, and educational principles that drive effective teaching and supervision on the Mount Sinai teaching service. DO: Lead purposeful, organized, and learner-centered rounds that integrate clinical care, teaching, technology, and timely feedback.
FEEL: Confident, inspired, and connected to the shared mission of developing compassionate, curious, and capable clinicians.

“One of the essential roles of a physician is to pass on knowledge to those who will follow.”
— William Osler