Facial Reconstructive Surgery in humanitarian missions
Cover: Self portrait by a patient
The original text, wrote in english by the autors, wasn’t correct or review.
The author thanks Riccardo Braglia for the precious consults and comments for this book and Helsinn for the valuable sponsorship for the realization of this important scientific activity. The author also appreciate the common interest of the Foundation New Flower in Africa for supporting the population of these countries.
The author thanks Mr Gerard Depardieu for his unwavering support
Drawings by Elisabetta Rosales
Photographs by Nicolás Bruant
Graphic design and composition: Giulio Castellazzo - WellComm
Mission support: Renata Babini Cattaneo - Fondazione Uriele


In the early 1990s, my husband Alfredo Cuomo and I met the young Dr Daniel Cataldo in Paris. We were introduced by mutual friends and were impressed by his energy, enthusiasm, and rising reputation as a reconstructive surgery expert. Through Daniel, we later met renowned medical surgeon Professor Jean Marie Servant and learnt more about their combined work at the University of Paris' Saint Louis Hospital. In 1996 they had formed ‘Operation Servant’, a humanitarian mission to work with the National Niamey Hospital in Niger to perform life changing facial reconstructive surgery on infants, children and adults afflicted with Noma disease, birth defects, cancer and severe facial burns. The missions were organized by the Saint Louis Hospital and Medicin du Monde. These transformative lifechanging actions moved both my husband and myself so deeply that we decided to act as private benefactors and financed and raised additional funds to support Operation Servant in its early initial actions. We travelled to Niger over several years and witnessed first-hand the remarkable transformations made possible by the committed ‘Operation Servant’ team.
Alfredo and I founded the Cuomo Foundation in 2001, with the primary goal of assisting the underprivileged in gaining access to education and securing brighter futures.
From the early days of support for ‘Operation Servant’ our professional paths have grown in different directions yet the core objective of providing tools to create confidence, pride and a sense of belonging remain the same.
I was invited to write this additional foreword in memory of Professor Jean Marie Servant and my late husband Alfredo Cuomo. The Cuomo Foundation has agreed to fully support the printing and global distribution of this special edition to selected medical centres and professionals in honour of both of these outstanding men.
Although the Cuomo Foundation is not responsible or able to endorse the medical assertions contained in this book, we support emotionally the aims of Dr Daniel Cataldo and his desire to teach and share his formidable knowledge and experience with the next generation of specialists in this vital field of medicine.
Maria Elena Cuomo

President of Cuomo Foundation
March, 2022 - MONACO

Is essencial that a plastic surgeon has a full training in general surgery including the knowledge of the chest and vascular surgery to become a true surgeon able to cope with challenging situation and to resolve complications

To:
My mother: Maria Laura Aguero;
The memories of my father and grandfather: Carmelo Cataldo and Natale Cataldo;
The memories of Silvia Onofri and Jacqueline Dufour.
Daniel Cataldo
Surgeon College of Medecine Hopital Saint Louis Paris
Surgeon Operation Servant Paris
Surgeon General and Plastic surgery university of Buenos Aires
Daniel Marchac assistant Hôpital Enfants Malades Paris
Surgeon Maxillo-facial Hôpital Pitié Salpêtrière Paris
Surgeon Nation Heart Hospital London
Surgeon Favaloro foundation Buenos Aires
Jean Marie Servant
Surgeon of Paris Hospitals
Professor of Paris University

Head of Plastic Surgery Hospital Saint Louis University of Paris
President of the National Commision for Qualification in plasic, reconstructive and aesthetic surgery
Professor, Tokyo University
Dr Jean Philippe Binder Certificates
-French National Board of Medical Doctor -French Board of General Surgery -French Board of Plastic Surgery -Chief Resident Plastic Surgeon, departement of Plastic and Reconstructive Surgery, Prof. J. M. Servant, at the Saint Louis Hospital, Paris -Plastic reconstructive and aesthetic surgery Saint Louis Hospital, Paris - France. Professor Marc Revol
Dr Maria Goffredi
-Professor of Embryology and Histology, University of Milan -Research at the Human Morphology Sacco Hospital, Univerity of Milan -Author of Computerized morphometry in liver cirrhosis Author of Microscopic and ultrastructural morphology Author of Microscopic Histology and Anatomy -Italian Board of Anathomy an Histology -Italian College of Histology and Embriology
Dr. Mercedes Portas
-Head of Surgical Department, Burns Hospital of Buenos Aires -Head of the Radiopathology Committee -Active member of the Argentina Radiation Protection Society -Active member of the Argentine Association of Trauma -Authority in the specialty of radiation-induced burns for Latin America
Institut du Fer à Moulin Université Pierre et Marie Curie.
Ralph Diaper and Sophie Huber. Technical assistance.
Aknowledgements
• Médecins du Monde - François Fousadier: without their work in organising humanitarian missions, the operations could not be performed;
• all the anaesthetists, Gabriela Vilain, Jérôme Landru, Christian Troje, Suzanne Reysz, photograph Gérard Mateo and secretary Monique Nadal from Saint Louis Hospital Paris;
• Abdoul Toure, chief of Plastic and Reconstructive Surgery at Niamey National Hospital Niger and Issa Hamady;
• Rabi Tahirou, head nurses Zinder National Hospital Niger; Robert Roux and Dominique Comandou heads nurses Saint Louis Hospital in Paris.
• Sentinelles for their professionalism essential for the development of the mission. Manon Louanne Chatelan;
• Professeur Jean Paul Monteil, Catherine Martinaud, Sylvain Harbon, Alain Danino, from the Saint Louis hospital Paris and Satoshi Yoza from the University of Tokyo, for their collaboration;
• Loretta Forelli, President of the Industrial Association of Brescia and Red Cross for her support of the mission for many years.
Niamey National Hospital - Niger


This book is dedicated to:
Daniel Marchac: one of the foremost surgeons in France and former staff of Saint Louis Hospital, who taught me cranio-facial and aesthetic surgery as his assistant for two years at Necker Enfants Malades Hospital in Paris.
Rene Favaloro, inventor of the coronary artery by-pass, who allowed me to perform open heart surgery, crucial for my surgical progress.


Jean Yves Neveux, who taught me his skill and technique, a major influence in my development.
Elias Hurtado Hoyo, President of the Argentine Medical Association, for giving me the attitude and approach needed to resolve complications in general surgery.

Sir Magdi Yacoub, the world’s leading heart-transplant surgeon, who gave me strength, and taught me technique and surgical tactics.

Luis de la Fuente, a recognised doctor with a world-wide reputation.


My thanks to Daniel Cataldo for offering me the opportunity to write this foreword to a book which is written on the foundations of huge experience and a long career in medicine. It was an honour to accept because I was his first teacher in general and particularly thoracic surgery. I should start by saying that after striving and showing great intellectual ability, he has gained national and international recognition. He has crossed the threshold of wisdom enabling him to engrave in these pages the ideas gained as a result of the combination of knife and intellect.
After graduating as a doctor, the young Daniel chose surgery as his speciality. His career has been long and particularly rich in experience. His first post was as Registrar in General Surgery at University Hospital Carlos G Durand in Buenos Aires where I guided him to thoracic surgery together with Rene Favaloro, inventor of the coronary artery bypass. Under our support he worked in some of the most prestigious hospitals in Europe under the direction of Sir Magdy Yacoub and Jean Yves Neveux. He made a stunning impression in a very specialised speciality, not just because of his surgical skills but also because of his humanitarian frame of mind.
He developed great skill working in delicate and narrow areas in patients at very high risk. As a very young doctor interested in learning everything about surgery, he decided to switch to plastic, reconstructive and aesthetic surgery. He became the only fellow of Daniel Marchac at the prestigious hospital of Necker-Enfants Malades in Paris. Later he worked for many years at the Saint Louis Hospital at the University of Paris beside Professor Jean Marie Servant, learning about all techniques of reconstruction. The experience gained with a large number of patients with complicated problems led him to develop high ethical and moral values to operate on the poorest and weakest patients.
The title of this book, Facial Reconstruction, is the perfect definition of a concentration of ideas about this subject, providing a description of each tool available, and giving the author’s personal position after years of rigorous hard work. The ideas develop giving a clear message to the reader, professional of the speciality or not, culminating in the importance of the ability to make decisions quickly. To reach a satisfactory level of knowledge it is essential to read the chapters on specific techniques. Those described were developed for congenital diseases like hare lip as well as for the gangrene of the face known as cancrum oris, or Noma, at the Saint Louis Hospital with surgeons such as Prof Jean Marie Servant.
The specialist surgeon must be able to give clear answers to challenges presented by the individual patient at the time of consultation. The way in which the selection of patients is made at the first consultation is evidence of the ethos of the organisation, and is the result of experience and much careful thought.
Surgical interventions on the face are performed in order to improve functionality and anatomy, together with an aesthetically pleasing outcome. Achieving these outcomes requires adapting techniques and tactics to each individual patient. The procedure has enormous consequences for the patient – on personal and social levels, and for employment opportunities. The symmetry of the exterior appearance is fundamental to the judgement of health, beauty or normality in human relationships. Improvements to the appearance mean an improvement in quality of life even in countries where scars have a different value to those of occidental regions. Many of these ideas are set out in the chapter on Psychology – an unusual inclusion in a book about surgery, but one which imparts a high quality to these pages. The plastic surgeon is much more exposed than other surgical specialists to the judgement of the public. He must live with the difference between the result wanted and the result actually obtained. The book is written with the intention to be instructive, but also to be easy to read and to understand. The photographs and drawings facilitate these aims. The bibliography at the end allows amplification of the information given. All things considered, this will remain a consultative book.
Professor Dr Elias Hurtado Hoyo Consultant Professor at the University of Buenos Aires; Doctor Honoris Causa, University of Moron and foundation Barceló; Consultant Professor, Military Hospital of Buenos Aires; Member of the Argentinian Academy of Surgery; Member of the Scientific Medical Association of Córdoba; Member of the Medical Academy of Paris Member of the National Medical Association of Argentina and Paraguay on Medical Ethics; President of the Argentine Medical Association.
Noma Cancrum oris
Child (one of 11 siblings)
Noma (cancrum oris, derived from the Greek nomein, “to devour”) is an opportunistic disease associated with malnutrition, poverty and/or lack of hygiene. In most cases the causal pathogens are Fusobacterium necrophorum and Prevoltella intermedia. The disease mostly affects children under the age of six (95 - 98% of cases). Those with poor buccal hygiene and severe malnutrition, especially with protein and vitamin A deficiency, are at high risk. The different disease each have their own periodicity: most cases of Cancrum oris occur in the dry season, which results in months of famine.
Unfortunately, malnutrition is often associated with malaria, measles, chicken pox, rubella, scarlet fever, herpes, typhoid and tuberculosis further increasing the risk of Noma infection. Taking all these factors into consideration, it can be seen that Noma (especially in children) is a disease of extreme poverty.

In adults, the incidence is low (less than 5% of cases), and associated with HIV infection (see Bacteria sand virus chapter), other diseases (e.g. tuberculosis, hepatitis A, B, C and E) or cytotoxic drugs used in the management of tumours (e.g. Burkitt’s lymphoma).
Cancrum oris occur in the dry season, which results in months of famine.
Malnourished child suffering from Noma

Symptoms and progression
Death occurs when the infection reaches Point 0 (the dura mater).
Noma begins as necrotising gingivitis and rapidly spreads through the mouth disrupting anatomic barriers. It involves soft and hard tissues of the oral cavity (except the tongue), para-oral structures, and the orbit. It is a serious orofacial gangrene originating intra-orally in the gingivaloral complex before spreading extra-orally, destroying other tissues. In most cases the disease is unilateral but bilateral lesions are sometimes observed. The disease demolishes soft tissues, bone and cartilage, and if not promptly treated, leads to death within two weeks in most cases. Aspiration pneumonia, sepsis or diarrhea may worsen the clinical condition. Death occurs when the infection reaches Point 0 (the dura mater) Sequelae of Noma depend on the extent of tissue disruption and include oral incontinence, trismus, speech problems and social exclusion due to facial disfigurement.
Fever, grey gums, excessive production of saliva and lymphatic node enlargement are symptoms suggestive of a Noma infection.
Early diagnosis, before the disease becomes clinically apparent, is essential in limiting the effects of the disease: fever, grey gums, excessive production of saliva and lymphatic node enlargement are symptoms suggestive of a Noma infection.
At the start of the infection the tissues become swollen, hard and hot: the mucosa become orange and the skin loses its pigmentation. Then quite quickly, a black area appears with a boundary marking the limit of the necrotic area to be eliminated. I just a few days the scar falls off without bleeding, sometimes leaving the bone exposed. The destruction of the bone is often followed by the destruction of the dental germ.
The lesion is often larger inside than out, so the mucosal damage is more important than the cutaneous. At the time of cicatrization, the destroyed mucosa become fibrotic and prone to retraction of tissue, particularly the jaw. The gangrene often spreads to the eyelid, palate, nose, ear and mastoid region.
Classic noma lesion involving molars, canines and external incisors (three superiors and one inferior)
Differential diagnostic:
• malignant infection
• Vincent disease
• Burkitt’s lymphoma
• Leishmaniasis
Historical references
Africa is the continent where most cases of disease are reported, particularly in Niger, Nigeria, and Senegal, but people in Asia and South America are not safe from the disease.

Noma was known during the time of Hippocrates, Galen, Celsus and Aretaeus of Cappadocia. The first clear description of Noma as a clinical entity appeared in 1595 in the Handboeck der Chirurgijen by Carolus Batus. In a chapter on corrosive ulceration of the mouth in children, the author underlined the rapidly progressive nature of the disease, advising practitioners on the risks of a misdiagnosis. At the beginning of the 17th Century, Noma started to appear in the European medical literature and Arnoldus Boot mentioned it in his book Observations Medicae de Affectibus Omissis (1649). In this text the Latin words cancer oris and cancrum oris were adopted for the first time. The Dutch surgeon Cornelius van der Voorde used the word “Noma” indicating a rapidly spreading gangrene of the mouth in the humid soft tissues of children in 1680. In 1848 it was described by Tourdes as a “gangrenous infection”. The word Noma was used by Lund in 1762 to describe a gangrena of the mouth in two children.
In the 18th Century several authors in Northwest Europe observed that Noma was associated with poverty, malnutrition and measles.
Classic mid-face lesion. Infection at superior canine has spread to molars and external superior incisors
During the Second World War (19391945), Noma was seen in Europe after infectious diseases, such as chickenpox, herpes, scarlet fever, tuberculosis, gastroenteritis and bronchopneumonia.
Occurrence - Europe
Noma has been present in Europe from medieval times. In the early 1900’s it was observed in the USA in a 3-year-old child with acute myeloid leukaemia, in Germany in two adults with lymphoid leukaemia and in a child with agranulocytosis. Eckstein observed 40 cases, all in children, in Ankara, Turkey, over a period of only 3 years (1936/38). Twenty-two of these cases were observed during a malaria epidemic in 1938. During the Second World War (1939 - 1945), Noma was seen in Europe after infectious diseases, such as chickenpox, herpes, scarlet fever, tuberculosis, gastroenteritis and bronchopneumonia. At the end of the war, several cases were reported in the concentration camps of Belsen and Auschwitz.
In the decades after the war, the reduction of extreme poverty and starvation, even among the poorest sections of society, resulted in a decrease in the number of cases.
More recently Noma has been described in immunocompromised adults in more developed countries, especially in patients with blood dyscrasia. Similar features have lately been described in patients with Aids.
With improvements in hygiene and nutritional status, and the decline in outbreaks of measles and other eruptive fevers, Noma disappeared from more developed countries: in the last three decades of the 20th Century the world paid little attention to Noma.

Occurrence - worldwide
Today, the disease is almost entirely confined to developing countries, particularly in Sub-Saharan Africa, which is one of the poorest parts of the world. In this zone, known as “The World’s Noma Belt”, millions of people are affected by hunger and the infection has an incidence as high as 140,000 cases per year, with a mortality rate of 80 - 90% and 900,000 survivors suffering disfigurement. A medicinal cure usually only becomes available in a later stage, when the sequelae of Noma are already present. Unfortunately, treatment of the infection is too expensive for developing countries so the economic support of the Western world is of paramount importance. This aid is often too late and subsequent on the dissemination by the media of pictures of undernourished children. The cornerstone of the treatment of Noma is antibiotic therapy (sulphonamides and penicillin) and the surgical treatment of the sequelae. However, these treatments remain inaccessible to the majority of patients due to their extreme poverty. In Niger, with a population of almost 15 million people, the vast majority are malnourished and poor.

The disease is confined to developing countries, particularly in SubSaharan Africa, which is one of the poorest parts of the world. In this zone, known as “The World’s Noma Belt”
Cancrum oris. Three years evolution. Infection of superior molars, canine and two incisors. Evolution on his own, without medical neither surgical toilette.

Young patient suffering cancrum oris with sequestration of the superior and inferior maxillary and zigomatic bone, following the granulation tissue and wound contracture

It is rare in adults, although we have seen it in a patient with HIV undergoing treatment for immunodepression.
Moreover, the high birth rate (7 children per mother), perpetual drought, rising food prices and the lack of land suitable for farming (only 15% of the country) further worsen the people’s condition, facilitating the spread of Noma.
In fact the highest incidence of the infection is during times of famine, while the lowest incidence is after the harvest.
Most of the patients in Niger come from the desert areas, and many of these from a town called Zinder (800km east of the capital Niamey). In Nigeria, the majority are from rural areas around Sokoto.
At least 70% of cases are children of farmers. It is difficult to obtain reliable statistics but in some areas of northwest Nigeria it occurs in 6.4 of 1000 children and up to 12 per 1000 in the worst affected communities. In Niger the occurrence is between 8 and 10 per 1000.
Some research shows that the maximum incidences of the disease occurs between the ages of 2 and 5 years, when children are weaned. It is rare in adults, although we have seen it in a patient with HIV undergoing treatment for immuno-depression (see Bacteria and virus chapter).
Lack of access to hospitals remains one of the main problems: because Noma often occurs in remote and marginalized communities, death may occur before medical care can be accessed.
It is clear that the most effective approach to Noma remains prevention. Fighting extreme poverty with measures leading to economic progress would eradicate Noma completely. Failing prevention, a prompt recognition of the disease allows to treat the gangrene aggressively, avoiding disfigurement.
In conclusion, the most likely chance of survival for patients affected by Noma in Africa is support from doctors in developed Western countries. Therefore, surgical treatment in such patients is more than a mere medical approach and provides an alternative to patients lacking a future. The doctors’ efforts are completely repaid by the immense gratitude shown by the patients.
Epidemiology
Although Noma has been known for at least seven centuries, only in 1994 was it designated as a priority, we started studying it extensively in the 1980’s. The social impact of the disease is undeniable, given the high mortality rate in children and the low chance of social integration for survivors.
The countries most affected by the disease are those of the Sahel region, one of the poorest in the world - such as Niger, Nigeria, Burkina Faso and Senegal. There is a huge difference between rural and urban areas. Outside Africa, Noma is described in a few children living in Latin America, India and China.
The mortality is around 80% in 15 days, due to infectious complications like pneumonia, diarrhea and septicemia. When the scar falls, the general conditions improve.
Antibiotics therapies produce a fall in mortality in patients under treatment to about 10%. Also hyper-protein and multivitamin nutrition, local hygiene, transfusion (rare) are very importantly in order to lower mortality rate.
The mortality is around 80% in 15 days, due to infectious complications like pneumonia, diarrhea and septicemia.
Cancrum oris. 3rd week post infection.

Noma. Malnourished eight years old boy, thirty five days post infection.
In the acute phase of the disease, family and medical personnel are often unable to give a diagnosis.
Cancrum oris is easily misdiagnosed as Burkitt’s lymphoma, leishmaniasis and Vincent’s angina, among other malignant and infectious diseases. Malnourished children in poor socio-economic conditions are susceptible to a variety of pathologies and Cancrum oris often develops after herpes, malaria and chickenpox infections

In some villages the patients are hidden because the disease is considered to be “evil” or “from hell”.
The true incidence and mortality rate of Noma are unknown for the following reasons:
• Noma wasn’t registered as a disease before 1992, and no cases were officially reported by the governments of the less developed countries before 1994;
• As many cases occur in desert and remote rural areas, the mortality rate is underestimated, although it is believed to be as high as 90%;
• Most of the affected children live in small villages or in nomad families with little contact with outsiders, therefore it is hard to register the mor tality and eventual outcome;
• In African countries certain diseases like Noma are considered shameful and affected children are hidden in gloomy rooms or even with animals.
Just 10% of patients seek medical care in an early stage, even though we make as much effort as we can to facilitate communication - informing, giving telephone numbers and providing ambulances to collect patients.
Symptoms
Cancrum oris starts with an exanthematous fever or debilitating disease with the following symptoms;
• soreness of the mouth;
• tender facial swelling;
• excessive salivation;
• painful lip or cheek;
• a foul-smelling purulent secretion, a bluish-black discoloration of the skin in the affected area, and a characteristic putrid odour are usually early signs.
The mortality rate in the first years of this century was 95% for the African countries where treatment was not available. On the other hand, in countries in which penicillin, sulphonamide and ascorbic acid are routinely used (without forgetting better health conditions than in Africa) the mortality rate (%) decreases to:
• 48% in Afghanistan;
• 25% in Madagascar;
• 12% in Vietnam;
• 8% in Turkey;
• 6% in the Philippines.
Protein-energy malnutrition is related to atrophy of the lymphoid tissues in the T-dependent areas of the thymus, spleen, Waldeyer’s ring and lymph nodes. The number of all lymphocytes and of CD4 and CD5 T-cells drops, impairing the production of immunoglobulins. In fact antibody production requires the presence of antigen-presenting T-lymphocytes. This condition, especially in malnourished children, leads to a state of inflammation of gingival and periodontal tissue, increasing the susceptibility to gingivitis and Noma.
A study of 100 Nigerian children at risk of Noma found low plasma concentrations of zinc, retinol and essential amino acids, and an increased concentration of cortisol due to adrenal hyper-function. The concentration of this hormone in malnourished children is double that of those that are well-nourished.
In malnourished children, leads to a state of inflammation of gingival and periodontal tissue, increasing the susceptibility to gingivitis and Noma.
Tooth hygiene practice.
In Niger just 2% of children brush their teeth.

Cancrum oris.
Seven years old boy, infection at superior and inferior incisors and superior canine teeth.
The disease of the child whose brother will come soon.
Other characteristics of starvation are the presence of important anaerobic flora, in particular of Gram-negative rods. 88% of undernourished children had spirochaetes which were not found in well-nourished children.

African children are breastfed for a long time (1 to 2 years), then weaned abruptly, and the lack of a proper substitutive diet leads to a deficiency of vitamins, immunoglobulins, amino acids and minerals. This in turn makes them susceptible to malaria, measles, herpes, chickenpox, AIDS, hepatitis and Noma. This sudden cessation of breast feeding and subsequent weakness in Africa is called “the disease of the child whose brother will come soon.”
The reticulate endothelial system characterizing chronic malaria causes the lowering of immunity that could pave the way to Noma.
There is some discussion about whether the most important risk factor for Noma is infection rather than malnutrition: in fact, there are children in the early stages who are not malnourished. Probably malnutrition is a predisposing factor. The effects of malnutrition on the immune system are well known. For example, lack of iron is associated with anaemia, reduced neutrophils and lymphocyte activity, and decreased response to certain antigens, such as those of the herpes simplex virus. Zinc deficiency leads to atrophy of lymphoid tissues, diminution of cell-mediated immunity and phagocytosis, and tissue-repair processes.
Lack of hygiene is another important factor in the development of Noma. There are studies showing just 2% of children in Niger use a tootbrush to clean their teeth, and those are exclusively in urban centres. In the rural and desert areas, they normally use their fingers or chew sticks. None of the children operated on for Noma brushed their teeth.
Other diseases associated with Noma are malaria and measles. The reticulate endothelial system characterizing chronic malaria causes the lowering of immunity that could pave the way to Noma.
Measles was considered by some authors (e.g. Tempest) to be the most important debilitating disease preceding Noma.
In Niger just 25% of children are vaccinated. Children with measles have lower than normal energy intake and show low mobilization of hepatic vitamin A.
In poor countries this disease can rapidly turn moderate under-nutrition into a fatal condition in the majority of patients. Most of the children present ulcerative lesions of the oral mucosa which can be so impressive that they have been termed “Noma-like post-measles ulceration.”


Other infective diseases can be debilitating and can facilitate the progression of buccal lesions into Noma, such as chickenpox, diphtheria, typhus, typhoid fever, tuberculosis, AIDS, leishmaniasis, agranulocytic angina, malignant oral lesions and some manifestations of syphilis. The leishmaniases are caused by several species belonging to the genus Leishmania, a flagellate protozoan transmitted by the bite of the female phlebotomine sandfly. Extensive destruction of mucosal membranes of the nose, mouth and throat can occur in mucocutaneous leishmaniasis. The physiopathology of these necroses with their sharp boundaries are ischemic features with localized arterial thrombosis or capillary micro-thromboses which are probably secondary to infection.
First line treatments are - high protein diet, rehydration, administration of vitamins (particularly vitamin A), and antibiotic therapies with amoxicillin and metronidazole.
These are broad spectrum agents active against periodontal and oropharyngeal flora, used to limit the tissue destruction and to induce satisfactory wound healing. Surgery at this stage is contra-indicated but necrotic regions of the face should be cleaned (soft tissue and bony sequestration) and any loose teeth extracted. All areas of necrosis are completely excised using tepid water, under local anaesthesia if necessary.
Tempest found 4 cases without buccal lesions, but with lesions of the scalp (mastoid area), neck, thorax and extremities.
Noma lesion at 3 and 6 months showing healing after regular toilettes
Infective diseases can be debilitating and can facilitate the progression of buccal lesions into Noma.

Acute necrotising gingivitis
Acute necrotising gingivitis is one of the most significant manifestations and sometimes the first symptom of the disease. It could be generalized or localized. It begins with gingival oedema and sudden necrosis, with decapitation of the interdental papillae, rapidly followed by bleeding and pain. Pathognomonic signs like foetid odour, fever, greyish pseudomembranes and hypersialorroea are often present. Protein-energy malnutrition or vitamin deficiencies can lead to an increase in permanent tissue damage and the entry of oral pathogens.

Acute necrotising gingivitis. It begins with gingival oedema and sudden necrosis, with decapitation of the interdental papillae.
Pathognomonic signs like foetid odour, fever, greyish pseudomembranes and hypersialorroea are often present.
Toilette.

Hemi face necrosis evolving posteriourly.
Ear compleat necrosis. Infection start at molars (4), canines and external incisors (2).




Little is known about the prodromic phase of Noma and its duration. The absolutely first symptoms, fever and apathy, are usually misdiagnosed as malaria by the family, and medical care is extremely rare in this stage. The first signs of Noma are oedema of the cheek and gingiva. Necrotising stomatitis may be seen at the alveolar margin spreading very quickly to the cheek mucosa in just a couple of days. In the following days, discoloured, black areas appear on the external surface of the cheek. These necrotic tissues remain defined, making a clear frame of the lesion and take a typical cone shape, described by the first clinicians who observed the disease. Necrosis often causes soft tissues and bone/cartilage to rapidly slough away, destroying the mandible, maxilla and palate, exfoliation of teeth and obvious external loss of skin.
Onset of Noma infections
In 1999, Falkler described 62 children in groups: 68% of malnourish children with ANG also had herpes infection, against 10% in malnourish children without ANG. The herpes virus favours the progression of ANG in malnourished children. For other authors, like Enwonwu, some viral infections, for example herpes or cytomegalovirus, can lower the buccal mucosal defenses and facilitate the development of ANG. On the other hand, some authors think a minor lesion of the mucosa is sufficient to initiate the disease.
Malnourish can alter the viral genotype, making it much more aggressive.
The bacterial flora in malnourish children is quite different, and perhaps an infectious agent, particularly Fusobacterium necrophorum, can start the infection. Noma starts as a gum infection at one or more teeth. The severity, extent and progress of the disease are associated with which, and how many, teeth are involved. When the infection reaches the dura mater through the frontal sinus ostium the mortality rate is almost 100%.
Involvement of different types of teeth Canines
Canines are involved in 83% of cases: in 12% of cases it is the only type of tooth involved. In massive, acute manifestations of Noma, incisors and molars are usually involved as well. Because of its position, the canine has less protection from the oral mucosa, is deeper in the bone and has more gum covering than other teeth: these features facilitate the onset of the infection.
Once the infection has started, the position of the canine, close to the maxillary sinus and the lateral wall of the nose, allows the infection to involve at least the maxillary sinus mucosa and the inferior turbinate.
When the lesion is localised at a canine, it can damage just its own root or alveolar process, or spread upwards, damaging the sub-cutaneous tissue: it is extremely difficult for the infection to reach the superior turbinate or orbit floor. On the other hand, it may advance towards the skin and spread to the base of the nostril, lateral wall of the nose, inferior turbinate, inferior maxillary sinus mucosa and even spread backwards, damaging the hard palate.
The infection often spreads in combination with incisors, in which case the damage can easily reach the base of the nose and columella.
These necrotic tissues remain defined, making a clear frame of the lesion and take a typical cone shape, described by the first clinicians who observed the disease.
Once the infection has started, the position of the canine, close to the maxillary sinus and the lateral wall of the nose, allows the infection to involve at least the maxillary sinus mucosa and the inferior turbinate.
Canine ifection starting with destruction of lateral wall of the nasal pyramid and maxillary sinus.
In this patient infection spread to three incisors and molars.

This can be completely destroyed as far as the tip of the nose and the inferior inter-cartilaginous septum (see Columella chapter).
When in combination with molars, the infection can rise to the orbit floor through the posterior and superior walls of the maxillary sinus, damaging the cartilage and mucosa of the sinus, and even the temporo-mandibular articulation (extra- or intra-capsular), badly damaging it.
In patients where the infection is stronger because of the combination with incisors or molars, then Point 0 is easily reached, and the mortality is higher.
Inferior canines are less frequently involved in the disease than the superior ones, accounting for around 20% of cases, and are often associated with incisors. As the lower lip is thin, especially the cul-de-sac where the mucosa joins the chin, damage occurs right through the wall, sometimes destroying the lip completely.
Incisors.
Incisors are involved in 65% of cases, either one or two in combination with canines, less frequently with molars. Incisor only infections account for 10% of cases. The gangrene spreads upwards, damaging the base of the nose, nostril, columella (which can be completely destroyed), inferior septum, tip of the nose and often the lips. When this happens the lip is badly damaged, with important retraction of the mucosa, making reconstruction even more challenging.
Incisors: infection can damage the base of the nose, columella (can be completely destroyed) and often the lips.
When the infection starts at a canine, with the involvement of at least one or two incisors, the lower lip incurs extensive damage. Due to its thinness, infection arising from the inferior incisors can easily go all the way through it, causing severe damage to the mucosa. When a couple of incisors are involved with an inferior canine, the infection can be severe enough to lead to total destruction of the lower lip, sometimes including the chin. Reconstruction then requires the use of neck flaps and possibly free flaps: however, these are not the first choice in humanitarian missions (see Surgery of Cancrum oris chapter). In all the cases described here, the tongue is usually not affected.
Superior molar can spread to the superior wall of the maxillary sinus, the orbit, inferior eyelid and temporomandibular articulation.
Quite often, canines are also involved, in which case the infection becomes more severe. Damage is caused to the whole of the upper lip (sparing the commissure stump) and the columella, which is badly damaged as far as the tip of the nose, the inferior aspect of the maxillary sinus, often the inferior (and sometimes the medium) turbinate, and the hard palate. The infection can progress through the cheek, the internal wall of the orbit as far as the superior turbinate and the sphenoidal bone, and eventually the dura mater or Point 0. When this happens, death occurs very quickly.
Molars
Molars in isolation account for just 15% of cases. In molar-only cases, the disease can destroy the whole thickness of the cheek, sometimes without damaging the surrounding tissues, but it can reach the temporomandibular articulation (intra - or extra-capsular) harming the coronoid processes.
Molars are always involved when trismus is present. The path of the infection starting in molars, damage the posterior-superior wall of the sinus, orbit floor, 3rd turbinate, eyelid and eye causing loss of sight.
When combined with canines the incidence becomes 25%, provoking serious necrosis of the cheek. In these cases, the infection can easily reach the maxillary sinus, destroying it and destabilising the orbit floor, often leading to loss of the eye. Frequently the infection reaches the superior turbinate and Point 0.


Cancrum oris. One week post infection of inferior molars. Necrotising stomatitis started at molars.
Toilette.
Cancrum oris.
Six years old boy, infection of superior canine, two incisors and one molar. with severe damage of maxillary sinus and lateral wall of the nose. Seven weeks and two months later.



The damage caused by infection starting at different combinations of
can be summarised
Canine;
Lips
Nostril base
Lateral wall of the nose
Inferior sinus and mucosa
Anterior palate
Cheek
follows:
Noma after toilette 2 months post infection
Turbinate (inferior and medium)
Incisors;
Lip (up to 90% of its thickness)
Columella
Nostril base
Inferior septum and mucosa
Tip of the nose
Anterior palate
Lower lip: until completely destroyed
Incisors associated to a canine;
Lips leaving just a commissure stump
Destruction of the columella
Tip of the nose
Whole thickness of lateral wall of the nose
Inferior sinus almost totally
Turbinates up to the superior
Orbit, floor and lateral wall
Point 0
Molar;
• Cheek
Coronoid processes
Inferior eyelid
Maxillary sinus
Orbit floor
Turbinates
Point 0
Cancrum oris. Infection localized at first superior molar.


Molar associated to a canine;
The whole cheek
Coronoid intra-articular process
Lateral wall of the nose
Palate
Destruction of maxillary sinus
Septum
Turbinates (3)
Point 0
Observations
Even when the infection is severe enough to badly damage muscle, skin and cartilage, it does not necessarily destroy the capacity to grow a new tooth.
In some patients the lesions are purely internal – to the palate, maxilla, orbit floor, septum or sinus – with the muscle and skin remaining undamaged. In these cases the infection is rarely severe and could have started from any tooth. We divide the infection into four categories, depending on the severity:
1 localized on one or more teeth without affecting surrounding tissue; 2 limited to internal lesions of mucosa or cartilage;
3 internal and external lesions but without compromising functions (bite, containment ability of the mouth, ectropion)
4 damage to the orbit, the maxillary articulation, destruction of part of the nose or cheek, and the upper and lower lips.
The damage caused depends primarily on the extent and severity of the infection, but the direction that it takes – anterior, posterior, up or down – is also important. When the infection starts at inferior incisors or canines, it always progresses anteriorly, seriously damaging the inferior lip, which is thin, especially at the cul-de-sac where it meets the chin. It never travels posteriorly, as we never notice damage to the tongue or the floor of the mouth. When inferior molars are involved, the path could be towards the skin, resulting in a lesion which, in a few cases, perforated all the layers as a “localized hole” ; more frequently, it is associated with an upward spread towards the posterior wall of the maxillary sinus or the temporomandibular articulation.
An infection starting at superior incisors most frequently spreads to the base of the nose and columella: if a canine is involved it can easily reach the floor of the maxillary sinus and lateral wall of the nose. If the infection starts at a superior molar alone, it can spread to the superior wall of the maxillary sinus, the orbit, inferior eyelid and temporomandibular articulation. In a few cases it penetrates all the layers including the skin as a “localized hole” like inferior molar.

Picture of the skull showing the thinness of the posterior wall of the frontal sinus. Through which point 0 is easy reach.
Thanks to the Institute of Fer à Moulin - University Pierre et Marie Curie - Paris, for the research collaboration.
Noma symptoms
Simple gingivitis: symptoms
Gums liable to bleed easily
Hyper-salivation
Gum inflammation
Pain Anorexia
Necrotizing gingivitis: symptoms
Fever
Swollen face
Oedema of the face

Halitosis
Gum ulceration
Pain
Spontaneous gum bleeding
Hyper-salivation
Anorexia
Bony sequestration
Necrosis: symptoms
Fever
Halitosis
Scar boundary
Bony sequestration Jaw constriction
Foetid smell Pain Gum ulceration Anorexia
Necrosis: treatment
Amoxicillin
Metronidazole
Multi-vitamins
Painkillers
Rehydration
Management of other pathologies
Bandaging to avoid fall of the flap during transfer
Simple gingivitis: treatment
Clean the mouth with tepid salt water
Buccal hygiene
Follow the progress of the disease
Necrotizing gingivitis: treatment
Amoxicillin
Metronidazole
Multi-vitamins
Painkillers
Management of associated disease
Follow the progress of the disease
Rehydration and feeding (balanced diet) Hygiene (frequent cleaning) of the mouth and teeth
Bacteria and virus
Due to the necrosis and putrid odour of the wounds a bacteriological aetiology of Noma has long been postulated.
In the last fifteen years, several studies have allowed us to identify and characterise the bacteria present in Noma. Among the hundreds of species isolated, the most important are Fusobacterium necrophorum, Prevoltella intermedia, Prevoltella melaningogenica, Bacillus cereus, Fusobacterium nucleatum and Corynebacterium pyogenes. Bacteroides fragilis are associated with Noma in a lower percentage of cases.
The commonest bacterium is Fusobacterium necrophorum. This bacterium is present in some cases of foot rot of domestic animals, in the gut of herbivores as a commensal, in human and animal faecal remains and has occasionally it has been isolated from periodontal lesions. The infection usually arises from contamination of damaged mucous membrane or skin as it is unable to invade intact epithelium directly.
The bacteria are Fusobacterium necrophorum, Prevoltella intermedia, Prevoltella melaningogenica, Bacillus cereus, Fusobacterium nucleatum and Corynebacterium pyogenes.
Child in the 7th weeks. The infection has spread from 3 superior incisors, a canine and molars.

Fusobacterium necrophorum is an opportunistic pathogen that can invade oral tissues.
The microorganisms associated with necrobacillosis, especially Fusobacterium nucleatum, are opportunistic pathogens that can invade oral tissues when there is a local weakening of defences such as abrasions, debilitating conditions, or trauma related to, for example, the eruption of molar teeth. Necrobacillosis has many features in common with cancrum oris: in fact both are associated with painful skin ulcers, disabling conditions of the lower part of the body due to skin abrasions, with a higher incidence in malnourished children and where there is faecal contamination.
Infection with herpes virus could lower local immunity, increasing the susceptibility to bacterial flora and cytomegalovirus. Both viruses are frequently associated with periodontal diseases and release of several inflammatory cytokines. In particular interleukin 1B, a potent bone-resorptive cytokine, may play a pivotal role in periodontal diseases. On the other hand, herpetic oral lesions are involved in either damage to the mucosal barrier or reduced local immunity, leading to the proliferation of pathogenic bacteria and the development of Noma in an undernourished child.
All patients we treated contracted the disease at young age (between 2 and 7 years old), cancrum oris is not frequent in teenager and is exceptional in adulthood, but could be possible in HIV patients under immunodepression treatment (see patient below).


Noma in adult is exceptional. Patient with HIV under immunodepression treatment.
Management
The coexistence of malnutrition, small lesions of the gum due to malaria or chickenpox, along with a debilitated immune system allows Noma to invade the mouths of undernourished children leading to death in as many as 90% of patients in a few weeks. Among those who survive the gangrene, the formation of granulation tissue anticipates a period of re-epithelialisation and wound contracture.

However, symptoms like gum inflammation, fever, foetid smell, bony sequestration, gum bleeding easily provoked by touch or brushing, high volume of saliva, painful gum and anorexia usually come first. The treatment of the inflammation, in this early stage, consists in cleaning the mouth with hot salt water and general hygiene, bearing in mind that the disease spreads extremely fast. Because the infection and necrotic tissues must be eliminated before reconstruction, it is necessary to wait for re-epithelialisation. This is a slow process which can take a long time – from a minimum of 6 months to more than 1 year in patients in whom the general clinical conditions are poor. Necrotic inflammation of the gum is treated with antibiotics (amoxicillin and metronidazole), multi-vitamins and analgesics. Early reports mention the use of sulphonamides, penicillin and chloramphenicol. When the gangrenous process has involved the cheek, the antibiotics significantly decrease the risk of death but cannot reverse the damage. Related to the rapidity of the spread of the infection, the first 24-hours are crucial and the treatment includes hydration, a balanced diet and careful dental hygiene. In the next stage, swelling and severe oedema of the face are added to the fever, halitosis, gum ulceration and bleeding, bony sequestration, pain and anorexia, further complicating the clinical scenario. At this time surgery is contraindicated. When necrosis and scarring around the tissues appear, the treatment is the same as in the previous step. However the patient should be properly bandaged and taken to a hospital as soon as possible, even if is not a risk of bleeding in this step of the disease. There are still no indications to for surgery at this point and the aim of the treatment is the control of sequestration.
When the gangrenous process has involved the cheek, the antibiotics significantly decrease the risk of death but cannot reverse the damage.
Cancrum oris. Five years old boy. Lack of buccal hygiene. Molars bacterial infection. Lesion spread through all layers to the skin.

Noma. eight years old girl, two month post infection Fusobacterium necrophorum and Prevoltella intermedia.

Necrosis often causes soft tissues and bone/cartilage to rapidly slough away, destroying the mandible, maxilla and palate, exfoliation of teeth and obvious external loss of skin. Nutritional rehabilitation, oral disinfection and antibiotic treatment started in an early stage can halt the disease.

Only during granulation and re-epithelialisation there be an indication of a skin graft to accelerate healing, but very few surgeons would recommend it as a routine procedure. Noma is a life-threating disease, therefore it is crucial to keep the patient alive with antibiotic therapy and proper nutrition preparing them for reconstructive surgery. The triad of nutritional rehabilitation, oral disinfection and antibiotic treatment started in an early stage can halt the disease. Unfortunately very few patients have access to appropriate medical care in this phase, and generally it is difficult to follow them until the resolution of the clinical picture. Even if they are followed up for a long period, rehabilitation remains a major problem in countries where there are no trained doctors or infrastructure. In fact, functional problems require a long period of specialist care, especially when trismus occurs (see Trismus chapter). Other conditions like incontinentia oris may require a second operation, and there could be speech difficulties to deal with.
Attainment of the desired results takes a long time, patience and the correct programme. The social stratum from which Noma patients come contributes to making follow-up harder. In many cases, patients are unable to understand the risks and complications of surgery. The aim of surgery is always to improve functionality and aesthetically.
Surgeons must be aware that the tissue loss could be much more extensive than initially assessed because the wound has healed by contraction. In order to release contracture, correct the defect and open the mouth.
In future the goal of the surgeon must be to close the hole in the face as quickly and as simply as possible, avoiding complications and giving more attention to functional problems like trismus, rather than just the aesthetic side of the disease. However, the patients are much more interested in the aesthetic results than the functional recovery, due to the need to be accepted by a tribal society. Taking into account the previous considerations, the duty of the surgeons is to balance aesthetic results with functional improvements.
Post-operative functional rehabilitation is the cornerstone of the clinical recovery although in some cases it can be really challenging. For example, trismus has to be treated as soon as possible, otherwise the patients are not able to eat normally without a nasogastric tube. Unfortunately, if the trismus fails to improve despite the surgery, the problem can become worse, affecting the ability to swallow. Surgery immediately after the gangrene should be avoided due to the poor clinical condition. Therefore, a long programme of proper nutrition must be guaranteed in order to build up the immune defences and make the patients fit enough to endure surgery.
Cancrum oris. Four years old girl. Seven and nine weeks post infection without toilette. Proper nutrition must be guaranteed in order to build up the immune defences.


Cancrum oris.
Five years old boy. Bacteria especially fusobacterium necrophorum provoque infection of superior and inferior molars.
In nearly every case it is important not to rush the reconstructive surgery (see Surgery of cancrum oris chapter), even when it is known that it may help the patient’s growth. Patients must be well nourished, in the best possible condition and ready to cooperate before reconstruction can be attempted. For these reasons it is extremely unusual to perform surgery on children under the age of seven. Only in cases of sequestration, where release of contraction permits better conditions for healing and growth, should surgery be indicated.

Anaesthesia is one of the most important factors to consider when the decision to operate has been taken. The better the clinical conditions, the higher the chances of enduring two or more hours of anaesthesia, and of surviving the postoperative period. The anaesthetist has to consider alternative methods of intubation, especially when trismus is present. It is recommended to avoid tracheotomy, blind intubation or high pressure ventilation. The anaesthetist’s equipment and skills must be as good as possible, to allow management of the whole clinical scenario, with infrastructure which can often be inadequate (see Anesthesia chapter).
Especially in longer interventions, a lack of material must sometimes be compensated for by the anaesthetist’s knowledge and experience. As a general rule, before the surgery, it is mandatory to check the availability of the necessary technology and of an adequate blood supply. The stratification risk is crucial: in fact, although the vast majority of patients have an uneventful post-operative course, major bleeding may occur in many. In the case of a severe haemorrhage, a lack of training and experience of the medical personnel, along with the absence of immediately available intensive care, may lead to death. Nurses must be trained and instructed to follow certain patients closely, and to recognise potentially fatal complications, especially during the night shift. In conclusion, to guarantee a good outcome it is essential that expert doctors, skilled nurses and trained physiotherapists work together during the whole perioperative course, which lasts at least two months, trying to minimize the most common complications.
Embryology of the face and buccal cavity
To understand the pathological alterations to the face and buccal cavity some knowledge of the embryology around this area during development is necessary. The events in question are recognised at the 4th week after fertilisation:
• At this time the bilaminar embryonic disc is converted into a trilaminar embryonic disc: each of three germ layers (ectoderm, mesoderm and endoderm) gives rise to specific tissues and organs. The notochord separates the ectoderm from the endoderm, except in two small circular areas: these are the oropharyngeal membrane at the cephalic region and the cloacal membrane at the caudal region.
• The development of the central nervous system, which started at the 3rd week, has reached the neural tube stage. As the neural tube closes, some ectoderm cells from the edges of the neural tube are left out and develop into the neural crest. These cells migrate in the developing embryo and differentiate into many types of tissue including the mesenchyme. In the head and neck region the mesenchyme from the neural crest or ectomesenchyme will take part in the development of cartilage, bones and connective tissue in the facial and tooth regions.

• The development of the ectoderm and the formation of the neural tube cause a deformation or folding in two embryonic areas: one in the cephalic region close to the oropharynx and the other in the cloacal region. During this process the oropharyngeal membrane covers part of the ventral face of the cephalic fold. It separates the stomodeum (the primitive oral cavity) from the developing pharynx. The growth of the cephalic fold is due to the migration of neural crest cells to the anterior part of the face.
• Following the appearance of cephalic and caudal curvatures, the embryonic disk undergoes a lateral folding amending the embryo into a cylindrical entity . The roof of the yolk sac folds ventrally to form the primitive gut and the embryonic disc lifts dorsally so that the ectoderm goes to coat the outer surface of the embryo that over looks the amniotic cavity. Then the embryo, which is a flattened tridermic disk, becomes a three-dimensional structure (fig. 1).
Fig. 1
Fig. 2 Drawing of stomodeum (modified after Ten Cate)
Fig. 3 A and B the cells of the neural crest slide under the ectoderm in the facial region. C in each pharingeal arch the cells of the neural crest become the boundary of the central mesoderm region still present (modified after Ten Cate)

Face development
At the end of the 4th week the stomodeum is framed cranially by the cephalic fold and caudally by the heart prominence (fig. 2). The oropharyngeal membrane, which forms the floor of the stomodeum, begins to be absorbed, allowing communication between the stomodeum and the cranial extremity of the anterior intestine or foregut: the pharynx.

In the same period cells from the neural crest migrate (fig. 3):
• To the frontal part of the prosencephalon creating the definitive placode of the frontonasal prominence.
• To the lateral surface of the head where they invade the mesoderm, giving rise to the branchial or pharyngeal arches.
The frontonasal prominences and the pharyngeal arches will take part in the shaping of the face and the oral cavity
Pharyngeal apparatus
At the end of the 4th week of embryonic development, the branchial or pharyngeal arches appear at the level of the most cranial part of the anterior intestine or foregut. They grow in a cranio-caudal direction with lateral mesoderm enclosed between the ectoderm and endoderm: altogether there are six pairs of arches. These mesodermal arches are separated from each other by deep divisions where ectoderm and endoderm are in contact.
The external part of the division on the outer surface of the embryo (ectodermal) is called the pharyngeal groove and the internal part at the lateral wall of the pharynx (endodermal) forms the pharyngeal pouch.
Each segment consists of three components:
• Ectodermic – pharyngeal groove;
• Mesodermic – pharyngeal arch;
• Endodermic – pharyngeal pouch.
The derivatives from the pharyngeal apparatus are quite complex (fig. 4).
Each pharyngeal arch has a cartilaginous and a muscular component, a nerve and an artery. In the skeletal segments, the arch cartilage is formed from the mesenchymal cells of the neural crest, while the mesoderm of the arches produces the striated muscle.
Fig. 4
Pharingeal grooves: ectoderm and pharingeal pouches: endoderm.
Lateral views showing the development of the pharingeal apparatus.
The muscle fibres migrate in different directions and the nerve passes through to the interior of the arch of the adjacent rhombencephalon.

The motor component of the nerve spreads through the muscular tissue of the arch while the sensory branch is in the superficial epithelium coming from the arch. The arches give rise to specific nerves as follows:
• 1st arch: V pair – trigeminal nerve;
• 2nd arch: VII pair – facial nerve;
• 3rd arch: IX pair – glossopharyngeal nerve;
• 4th, 5th and 6th arches: X pair – vagus nerve.
Fig. 5
A. Lateral picture of the human hembrio of 32 days.
B. Micrography of SEM of the cranial facial region of the human hembrio of 32 days (modified after Moore).

Fig. 6
Drawing of facial prominences (modified after Duplessis) In the 5th week of development, the stomodeum is surrounded by five mesenchimal swellings called prominence.
The lower part of the face, and a large amount of the medial part, are formed from tissues from the first pharyngeal arch (also called the mandibular arch), while the other pairs of arches, together with the pharyngeal groove and the pharyngeal pouch are involved in building the neck region (fig. 5) above.

Facial prominences
In the 5th week of development, the stomodeum is surrounded by five mesenchymal swellings called prominences (fig. 6). These are:
• A frontonasal prominence: surrounds the ventrolateral part of the forebrain
• Paired maxillary prominences;
• Paired mandibular prominences.
Both maxillary and mandibular prominences derive from the first pair of pharyngeal arches.
They are initially separated by grooves which fill up progressively.
Facial growth depends on the influence of organisers from the prosencephalon and rhombencephalon. In particular the face is formed from a mesodermal mass arising between the cranial extremity of the developing brain and the heart prominence: in the centre is the depression which is the stomodeum or primitive oral cavity.

Since the 4th week the stomodeum has been closed posteriorly by the oropharyngeal membrane.
As the telencephalon develops, the frontonasal prominence becomes the roof of the stomodeum: the frontal part of this prominence forms the front while the nasal part becomes the facial border of the stomodeum and the nose (fig. 6).
Both mandibular prominences rapidly merge along the medial line to form the floor of the stomodeum. This represents the anterior extremity of the 1st pharyngeal arch (mandibular arch). Both maxillary prominences are derived from the first arch and shape the lateral walls of the stomodeum.
The maxillary and mandibular prominences result from the proliferation of the cells of the neural crest. The facial prominences are active growth areas of the underlying mesenchyme. This embryonic connective tissue is active from one process to another.
Facial development proceeds rapidly between the 4th and 8th week. The first parts to develop are the mandible and lower lip: they arise from the merging of the medial extremity of the mandibular prominence and the medial prominence.
At the end of the 4th week, bilateral oval structures appear on the surface of the frontonasal prominence. These ectodermal swellings are the nasal placodes, which will give rise to the olfactory epithelium. A horseshoe shaped part of the mesoderm rises up and transforms the nasal placodes in olfactive showers which are driven in an anterio –posterior direction on the stomodeum. The nasal placodes remain to develop the floor of the depression between these processes (fig. 6).
The proliferation of mesenchyme in the maxillary prominences causes them to expand and grow towards each other medially, pushing the nasal placodes closer together. The lateral nasal prominence fuses with the maxillary prominence forming the nasolacrimal duct between them.
Spreading in a ventral direction the maxillary prominence closes the lower edge of the nasal fossa and merges with the medial nasal prominence. The entrances to the nasal fossa become the primitive external nose. The medial nasal prominences, inside on the medial line, together with the proliferation of mesenchyme from the medial nasal prominence on the stomodeum give rise to the pre-maxillary regions of the face.
These regions give rise to the philtrum of the upper lip and to the medial part of the alveolar process which produce the incisor teeth and the primitive palate. The upper lip is built from both maxillary branches and the two medial nasal placodes.
The mandibular prominences penetrate deeply to form the lower lip and the lower part of the cheeks; the upper part of the cheeks is derived from the maxillary prominences. At this point however the lips and cheeks are not yet separated from the deeper tissues of the mandibular area.
The external nose is developing from the nasal prominences: the lateral prominences give rise to the lateral wings of the nose and the medial prominences to the medial part.
The medial nasal prominences, inside on the medial line, together with the proliferation of mesenchyme from the medial nasal prominence on the stomodeum give rise to the pre-maxillary regions of the face.
The upper lip is built from both maxillary branches and the two medial nasal placodes.
Fig. 7
Drawing of the primary palate (modified after Ten Cate)
Development of the nasal cavity and palate


The mesenchyme of the nasal prominences continues to grow and the nasal pits become deeper, shaping the primitive nasal cavity. The epithelial wall at the blind end of the primitive nasal cavity makes contact with the epithelium of the stomodeum roof making the oronasal membrane. This membrane ruptures and then the nasal cavity communicates with the stomodeum through a new channel called the primordial choana (pl. choanae).
The development of the palate occurs in different stages:
At the beginning of the 6th week the primary palate starts to form as a medial projection from the medial nasal prominence, and the nasal septum appears as a medial vertical structure originating from the frontal prominence (fig. 7).
Fig. 8
Drawing of the primary palate to secondary palate (modified after Duplessis)
Two mesenchymal projections arise from the deep superficial part of the maxillary prominence; these become the lateral palatine processes which grow each side of the tongue in a medial direction.
As they grow towards each other this causes the lowering of the tongue.
The free edges of the palatine processes fuse with each other and with the primary palate between them. This forms the secondary or definitive palate: the boundary between the secondary and primary palates on the medial line is marked by the incisive foramen (fig. 8).
The formation of the nasal septum and the secondary palate complete the division of the stomodeum into definitive nasal and oral cavities.
These processes take place between the 8th and 12th weeks of development.
Clefts of the lip and palate are common craniofacial anomalies. The defects are usually classified according to developmental criteria, with the incisive fossa as a reference point. These clefts are especially conspicuous because they result in an abnormal facial appearance and defective speech. There are two major groups of cleft lip and cleft palate. (See Tessier classification in “Cleft lip and palate” chapter).
• Anterior cleft anomalies include cleft lip, with or without cleft of the alveolar part of the maxilla. A complete anterior cleft anomaly is one in which the cleft extends through the lip and alveolar part of the maxilla to the incisive fossa, separating the anterior and posterior parts of the palate. Anterior cleft anomalies result from a deficiency of mesenchyme in the maxillary prominence(s) and the median palatine process.
• Posterior cleft anomalies include clefts of the secondary palate that extend through the soft and hard regions of the palate to the incisive fossa, separating the anterior and posterior parts of the palate. Posterior cleft anomalies result from defective development of the secondary palate and growth distortions of the lateral palatine processes, which prevent their fusion. Other factors such as the width of the stomodeum, mobility of the lateral palatine processes (palatal shelves), and altered focal degeneration sites of the palatal epithelium may also contribute to these birth defects.
A cleft lip, with or without a cleft palate, occurs approximately once in 1000 births; however, the frequency varies widely among ethnic groups; 60% to 80% of affected infants are males. The clefts vary from incomplete cleft lip to ones that extend into the nose and through the alveolar part of the maxilla. Cleft lip may be unilateral or bilateral.
A unilateral cleft lip results from failure of the maxillary prominence on the affected side to unite with the merged medial nasal prominences. This is the consequence of failure of the mesenchymal masses to merge and the mesenchyme to proliferate and smooth out the overlying epithelium. This results in a persistent labial groove. In addition, the epithelium in the labial groove becomes stretched and the tissues in the floor of the groove break down. As a result, the lip is divided into medial and lateral parts. Sometimes a bridge of tissue, called a Simonart band, joins the parts of the incomplete unilateral cleft lip.
A bilateral cleft lip results from failure of the mesenchymal masses in both maxillary prominences to meet and unite with the merged medial nasal prominences. The epithelium in both labial grooves becomes stretched and breaks down. In bilateral cases, the defects may be dissimilar, with varying degrees of defect on each side. When there is a complete bilateral cleft of the lip and alveolar part of the maxilla, the median palatal process hangs free and projects anteriorly. These defects are especially deforming because of the loss of continuity of the orbicularis oris muscle, which closes the mouth and purses the lips.
Anterior cleft anomalies result from a deficiency of mesenchyme in the maxillary prominence(s) and the median palatine process.
Posterior cleft anomalies result from defective development of the secondary palate and growth distortions of the lateral palatine processes, which prevent their fusion.
Facial bipartition type 0/14 of prof. Tessier P. classification. Operated with prof. D. Marchac. Hôpital Enfants Malades Necker.
A median cleft lip is a rare defect that results from a mesenchymal deficiency. This defect causes partial or complete failure of the medial nasal prominences to merge and form the median palatal process.
A median cleft lip is a characteristic feature of the Mohr syndrome, which is transmitted as an autosomal recessive trait.


A median cleft of the lower lip is also very rare and results from failure of the mesenchymal masses in the mandibular prominences to merge completely and smooth out the embryonic cleft between them.
A cleft palate, with or without a cleft lip, occurs approximately once in 2500 births and is more common in females than in males. The cleft may involve only the uvula; a cleft uvula has a fishtail appearance, or the cleft may extend through the soft and hard regions of the palate. In severe cases associated with a cleft lip, the cleft in the palate extends through the alveolar part of the maxilla and lips on both sides.
A complete cleft palate indicates the maximum degree of clefting of any particular type; for example, a complete cleft of the posterior palate is a defect in which the cleft extends through the soft palate and anteriorly to the incisive fossa. The landmark for distinguishing anterior from posterior cleft anomalies is the incisive fossa.
Unilateral and bilateral clefts of the palate are classified into three groups:
• Clefts of the primary or anterior palate (clefts anterior to the incisive fossa) result from failure of mesenchymal masses in the lateral palatal processes to meet and fuse with the mesenchyme in the primary palate.
• Clefts of the secondary or posterior palate (clefts posterior to the incisive fossa) result from failure of mesenchymal masses in the lateral palatine processes to meet and fuse with each other and the nasal septum.
• Clefts of the primary and secondary parts of the palate (clefts of the anterior and posterior palates) result from failure of the mesenchymal masses in the lateral palatine processes to meet and fuse with mesenchyme in the primary palate, with each other, and the nasal septum.
Most clefts of the lip and palate result from multiple factors (multifactorial inheritance), including genetic and nongenetic, each causing a minor developmental disturbance.
Several studies show that the interferon regulatory factor-6 (IRF-6) gene is involved in the formation of isolated clefts.
Some clefts of the lip and/or palate appear as part of syndromes determined by single mutant genes. Other clefts are parts of chromosomal syndromes, especially trisomy 13.
A few cases of cleft lip and/or palate appear to have been caused by teratogenic agents (anticonvulsant drugs). Studies of twins indicate that genetic factors are of more importance in a cleft lip, with or without a cleft palate, than in a cleft palate alone.
A sibling of a child with a cleft palate has an elevated risk of having a cleft palate, but no increased risk of having a cleft lip. A cleft of the lip and alveolar process of the maxilla that continues through the palate is usually transmitted through a male sex-linked gene. When neither parent is affected, the recurrence risk in subsequent siblings (brother or sister) is approximately 4%.
Other Facial defects
Congenital microstomia (small mouth) results from excessive merging of the mesenchymal masses in the maxillary and mandibular prominences of the first pharyngeal arch. In severe cases, the defect may be associated with underdevelopment (hypoplasia) of the mandible. A single nostril results when only one nasal placode forms. A bifid nose results when the medial nasal prominences do not merge completely; the nostrils are widely separated, and the nasal bridge is bifid. In mild forms of bifid nose, there is a groove in the tip of the nose.
By the beginning of the second trimester , features of the foetal face can be identified sonographically. Using this imaging technique, facial defects such as a cleft lip are readily recognizable.
Facial clefts
Various types of facial clefts occur, but all are rare. Severe clefts are usually associated with gross defects of the head.
• Oblique facial clefts are often bilateral and extend from the upper lip to the medial margin of the orbit. When this occurs, the nasolacrimal ducts are open grooves (persistent nasolacrimal grooves).
• Oblique facial clefts associated with a cleft lip result from failure of the mesenchymal masses in the maxillary prominences to merge with the lateral and medial nasal prominences.
• Lateral or transverse facial clefts run from the mouth toward the ear.
• Bilateral clefts result in a very large mouth, a condition called macrostomia. In severe cases, the clefts in the cheeks extend almost to the ears.

Cleft lip and palate
Cleft lip and palate are congenital malformations resulting from a failure of tissues to fuse, and are the commonest congenital facial deformities. The occurrence in the Western world is about 1 in 700, but higher in Central Africa at about 1 in 550. Paul Tessier listed 15 varieties of cleft (see drawing pag. 47) affecting different parts of the face such as the nose, cheeks, ears, eyes and forehead.
The cleft can be uni - or bilateral, and can vary from a small gap or incomplete cleft to a complete cleft into the nose.
Cleft palate occurs when the two parts of the hard palate fail to join completely so the roof of the mouth remains open making one cavity with the nasal cavity and could be complete (soft and hard palate) or incomplete (soft palate only).
The pathology is much more distressing for children who may develop psychosocial problems due to peer relationships, particularly for girls. At an early age the problem is not as hard as in later life.
The deformity with the resultant speech impediments, gives the perception that suffers are less attractive and intelligent. In addition the extremely poor social, cultural and economic conditions found in some parts of Africa result in a situation, rarely seen on other continents,
Young girl with unilateral cleft lip on the left side, before and after reconstruction.


Surgery: the nutritional status has to be as good as possible.
Boy with unilateral incomplete cleft lip on the left side, before and after reconstruction.


whereby human being are condemned to suffer their entire life with malformations and consequent disfigurement. So most patients, suffer from lack of confidence and become unhappy and angry. Moreover, African families are often large, so they, usually, have less parental care than their siblings further worsening their psychological development.
Surgery for the correction of these kinds of congenital malformations is complicated and to increase the chances to have an uneventful perioperative course, the nutritional status has to be as good as possible.
We often have to wait several months before we can proceed.
Self portrait by a patient.
Cleft lip Classification
• Unilateral: one nostril is involved and becomes lower;

• Bilateral: the nose becomes wider and shorter.
The cleft could be complete or incomplete, depending on whether or not it extends into the nose.
A cleft lip can affect every function of the face, disrupting growth of the maxillary and malar bones, leading to malnutrition, malocclusion, ear disease such as Eustachian tube malfunction, reduced air conduction to the middle ear, naso-respiratory obstruction and deafness.
Reconstruction is normally performed at three months, but in humanitarian missions it is preferable to wait until later, and difficult before the age of one year.
Retardation of growth is due to the pre-operative feeding difficulties added to the local social conditions.
The alar cartilage is dissected and fixed with a transfixing point and interior and exterior tulle gras dressings are applied. The alar cartilage is not malformed, just compressed.
Girl with unilateral complete cleft lip on the right side.
Before and after reconstruction.
Girl with unilateral complete cleft lip on the left side.



Before and after reconstruction.

Lady suffering unilateral complete cleft lip. Before and after surgery.

The first aim of reconstruction is to get the height and width of the lip to match the normal side.
Seven years old boy with left unilateral complete cleft lip bevore and after surgery.



The basic and most often employed technique is the Millard procedure.
The first aim of reconstruction is to get the height and width of the lip to match the normal side. A second objective is to give the lip muscular functionality by suturing the muscle fibres with those from the opposite side.
A second operation may be necessary to correct a short or insufficient red lip.
Unilateral cleft lip and palate are characterised by the large deviation of the non-cleft side of the maxilla away from the cleft.
Boy with unilateral complete cleft lip on the left side. Before and after reconstruction. Self portrait.

It can also cause speech defects and problems with the senses of smell and taste, alimentation, hearing and nasal breathing. From the aesthetic point of view it affects facial expression and appearance. The aetiology of the condition is unclear, but the most popular theory attributes it to hypoxia during pregnancy. Another possible cause could be lack of folic acid. Genetic changes (see Embriology chapter) and environmental factors, such as poor nutrition and drugs may also be involved. Certainly the rate is higher among women who smoke during pregnancy and those suffering from diabetes.
Unilateral cleft lip with nasal deformity


In these patients, it is obligatory to evaluate the lack of tissue and the distortion, in order to calculate the quantity of tissue to transfer into a normal position. One of the deficiencies of this malformation is an inherent vertical shortness on each side, involving the lip and the nose.
The non cleft side has a twisted distortion with lack of vertical length from the height of the arch of the ala to the height of the Cupid’s bow at the musculocutaneous junction. The cleft side may be the short columella and the flattened alar arch , the cartilage displaced and its flaring base attached to intact lip musculature.
The alar cartilage of the affected side is not under-developed but squish from up to down and the nose is swift to the back.
The non cleft side has a twisted distortion with lack of vertical length from the height of the arch of the ala to the height of the Cupid’s bow at the musculocutaneous junction.
Boy eight years old. Present left unilateral complete cleft lip. Before and after surgery.

Boy nine years old. Present left unilateral incomplete cleft lip. Intra-operative view, dissection of the periosteum to free both lips and the alar base.




Before and after surgery.
A unilateral cleft lip results from failure of the maxillary prominence on the affected side to unite with the merged medial nasal prominences. This is the consequence of failure of the mesenchymal masses to merge and the mesenchyme to proliferate and smooth out the overlying ephithelium. This results in a persistent labial groove. In addition, the epitelium in the labial groove becomes stretched and the tissues in the floor of the groove break down. As a result, the lip is divided into medial and lateral parts. Sometimes a bridge of tissue, called a Simonart band, joins the parts of the incomplete unilateral cleft lip.
Three patients with unilateral complete cleft lip on the left side.





Before and after surgery.

Unilateral complete left cleft lip.


Before and after surgery.
Dissection of the periosteum to free both lips and the alar base, removal of the mucosa shaping the internal flap.
Unilateral complete right cleft lip.


Before and after surgery.
Reconstruction of the nostril floor and vestibular mucosa starting from the external cleft side lifting the entire lip to the interior.
One of the most important points is to bring the muscles together and ensure that the red lip line is perfectly shaped. The muscle line is completed, followed by mucosa and skin.
Two patients with unilateral complete cleft lip on the left side.





Before and after surgery.

Lady eight years old with unilateral right cleft. Before and after surgery.

Lady nine years old with left unilateral complete cleft. Intraoperative, before and after surgery.




The alar cartilage is dissected and fixed with a transfixing point and interior and exterior tulle gras dressings are applied . The alar cartilage is not malformed, just compressed.

Bilateral cleft, absence of Cupid’s bow, present a variety degree of vertical shortness treat in embryology chapter as the frontonasal component witch is measured from a position at the nasal tip to the mid inferior of the free border of the prolabium of the upper lip . The evaluation of severe symmetrical distortion . The prolabial and columella length or a combined shortness of both .The condition is more common in Asians than Africans. When a sibling or a parent is affected, the possibility of recurrence is about 3 to 6% - if both parents are affected the risk rises to 15%.
The palate consists of the hard palate, soft palate and uvula limited anteriorly by the incisive foramen. In front of the incisive foramen are the pre-palatal structures - the alveolus, upper lip and nasal tip.
The two maxillae join each other in the midline giving a definitive shape to a normal palate. They meet anteriorly at the incisive foramen and extend posteriorly to both palatal bones.
In the upper face of the palate there is a groove shaped by the hemi-palates with the nasal cartilaginous septum at the front and vomer at the back. The pre-maxilla is anterior to and central to the incisive foramen and is completed by the four incisor teeth and nasal spine.
Posterior to the palatine process is the palatine bone with both palatine foramina which contain the main blood vessels and sensory nerves which are the most important supplying the palate.
Posteriorly there is the hamulus, on which the activity of the tensor palatine muscle depends.
The muscles are divided into those used for speech and those controlling swallowing. For speech the most important muscle is the levator palatine, together with the palatopharyngeus muscles and the superior pharyngeal constrictor.
Muscles involved in swallowing are the tensor palatini muscles and the levator palatine, the contraction of both allowing velopharyngeal closure.

Tessier Classification
Bilateral cleft lip and palate: the prolabium is thick and the philtrum is reconstructed with the prolabium skin ensuring that the width is no more than 5-6 mm. Before and after reconstruction.


Two years old boy with bilateral complete cleft lip.




Before and after surgery.
In bilateral cleft lip and palate, the protrusion of the premaxilla obliterates the columellar area, leaving the lip attached to the nasal tip. In profile, the central incisors lie anteriorly to the nasal septum.
In order to prepare children for surgery it is mandatory to provide nourishment with a flexible feeding bottle or with a customised dummy.
A palatal obturator could also be useful.
The reconstruction and the resultant scars interfere with maxillary development in children suffering cleft lip and palate. Lip and bone reconstruction, and vomer dissection, have a negative effect on facial development. In malnourished children, a cleft lip accentuates their slow development.
Two years old boy suffering bilateral complete cleft lip.
Before and after reconstruction.
Some authors prefer to perform the reconstruction in two operations. The first reconstructs the soft palate, and the second the hard palate, avoiding as far as possible dissection of the sub-periosteum of the palate and vomer. It is difficult to apply this approach in humanitarian missions.
The reconstruction and the resultant scars interfere with maxillary development in children suffering cleft lip or palate.

Lip and bone reconstruction, and vomer dissection, have a negative effect on facial development.
Eight years old girl suffering bilateral complete cleft lip.



Before and after reconstruction.
In bilateral cleft, flaps from both sides are brought together under the philtrum in order to build the muscular lip and shape the new orbicularis oris.
Appearance before and after reconstruction.
Man with bilateral complete cleft lip.




Surgical view. Lifting of the left lip flap and reconstruction of the philtrum.
The philtrum is reconstruct with sliding orbicular muscle from both lateral side under its own skin.
The prolabium does not contain any muscle which is useful for reconstruction, so the strip is reconstructed with part of the lateral lips.
The philtrum is reconstructed from the skin of the prolabium. Both laterals lip flaps are shifted under the lifted prolabium skin. The muscular strip is reconstructed under the skin of the philtrum using the orbicularis oris muscle from both lateral flaps.
A bilateral cleft lip results from failure of the mesenchymal masses in both maxillary prominences to meet and unite with the merged medial nasal prominences . The epithelium in both labial grooves becomes stretched and breaks down. In bilateral cases, the defects may be dissimilar, with varying degrees of defect on each side . When there is a complete bilateral cleft of the lip and alveolar part of the maxilla, the medial palatial process hangs free and projects anteriorly. These defects are especially deforming because of the loss of continuity of the orbicularis oris muscle, which closes the mouth and purses the lip.
Children start to say their first words at around 15 months, and cleft palate surgery is preferably performed before this, but in humanitarian missions it is difficult to perform reconstruction before the age of 2 or even 3 years.
The embryologies of cleft lip and cleft palate are completely different (see Embryology chapter). The primary palate means the lip, philtrum, alveolar bone, and hard palate forward to the incisive foramen. The secondary palate is the back of the hard palate as far as the incisive foramen and the soft palate.
Some authors do not perform soft palate reconstruction on adult patients. The degree of speech problems depends on the anatomic defects of the palate.
Bilateral cleft lip: The vermillion ridge is completely excised and the mucosa becomes important for reconstructing the central vestibule. The lateral flap should include enough tissue to be able to raise the prolabium.



Man with complete unilateral cleft lip and palate. Before and after reconstruction.

Diagram of operation technique
Procedure
Cleft lip: surgical technique
Drawings:
• higher point of normal side of philtrum / buccal commissure length,is transfer to the opposite side to create cleft side higher point of philtrum
• Higher point of normal side of philtrum / mid-point of philtrum length, is transfer to create higher point of philtrum cleft side
• point of cleft side philtrum - middle of columella (length of philtrum)
• point of cleft side philtrum - nostril (internal flap), cleft side
• philtrum point - alar base (length of the philtrum)
• around the alar base
• both sides of mucosa giving the length of the whole lip
• vestibular line 3 mm from the gum
A) Injection with physiological saline + adrenaline.
B) Dissection of the periosteum to free both lips and the alar base, removal of the mucosa shaping the internal flap.
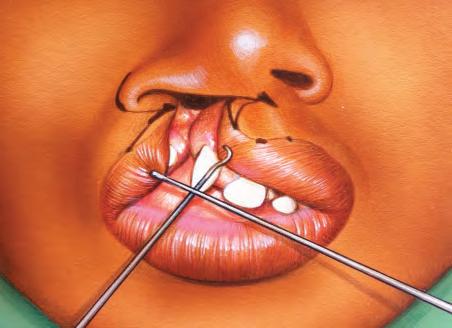
C) Dissection between orbicularis oris muscle and skin.
D) Reconstruction of the nostril floor and vestibular mucosa starting from the external cleft side lifting the entire lip to the interior, idem for the opposite side ensuring that any excess mucosa is removed so as to leave the sides ready to seal.
E) One of the most important points is to bring the muscles together and ensure that the red lip line is perfectly shaped.
F) The muscle line is completed, followed by mucosa and skin.
Old man with complete unilateral cleft lip and palate.

Before and after reconstruction.

1
Bilateral cleft: the prolabium is thick and the philtrum is reconstructed with the prolabium skin ensuring that the width is no more than 5-6 mm.


The vermillion ridge is completely excised and the mucosa becomes important for reconstructing the central vestibule. The lateral flap should include enough tissue to be able to raise the prolabium.
Flaps from both sides are brought together under the philtrum in order to build the muscular lip and shape the new orbicularis oris.
1) Appearance before reconstruction.
2-3) Dissection of the periosteum to free both lips and the alar base, removal of the mucosa shaping the internal flap.


2
4
4) Dissection between orbicularis oris muscle and skin.
3
6
5) Reconstruction of the nostril floor and vestibular mucosa and bringing the muscles together ensuring that the red lip line is perfectly shaped.

6) Final appearance.

Cleft palate
Classification
A) soft palate;
B) complete palatal cleft until the foramina of the incisors;
C) unilateral palatal and prepalatal cleft;
D) bilateral complete cleft of the palate and prepalate.


Surgical technique
Soft palate reconstruction

In the wester world the preferred age for cleft repair is around 12 - 24 months (before speech development). In the poorer regions of the world it is suggested to wait until the age of 30 months, in order to achieve a satisfactory weight and stronger immune system.
There are different approaches to this procedure. One is closure using double Z-plasties which allows elongation of the palate but may result in a fistula complication. The technique is performed with two Z-plasties of the nasal and buccal mucosa.
Another consists in the dissection of the levator palatine muscle which is slid medially and used to reconstruct the soft palate. Both mucosae (nasal and oral) are closed separately.
1-2) Cleft palate before and after reconstruction.
3-4) Cleft palate intra operative appearance.

This procedure used bilateral, bi-pedicle mucoperiosteal flap.

Old patients with cleft lip/palate are frequent in humanitarian. Phonation
reeducation is too hard to improve.
Patient with complete cleft palate, view after recontruction with Von Langerbeck’s technique. Old man with bilateral cleft lip and palate.


Before and after surgery.

The incision is performed along the lingual face of the alveolar bone and along the edge of the palatine cleft.
For reconstruction of the soft palate, the levator veli palatini muscle is dissected as far as its anatomical insertion on the posterior part of the hard palate and its position juxtaposed, becoming transversal and is stitched in the medial line to reconstruct the palatine sailing.



The oral and nasal mucosae are stitched separately.
Reconstruction of the soft palate has no effect on maxillary growth.
As it is difficult to improve vocalisation, particularly in older patients and in the absence of facilities for rehabilitation, in humanitarian missions some authors occasionally suggest just closing the hard palate.
Hard palate reconstruction: Von Langenbeck’s technique.
This procedure uses bilateral, bi-pedicle mucoperiosteal flaps.
The incision is performed along the lingual face of the alveolar bone and along the edge of the palatine cleft.
The flaps are lifted taking particular care of the pedicles.
The dissection follows the palatine and nasal mucosa which are brought medially and stitched together.
Hard palate reconstruction: Veau-Wardill-Kilner
This reconstruction utilises bilateral mucoperiosteal flaps based on the palatine artery.
Closure with V-Y with a retroposed flap creates a longer palate with retro-shifted.
Drawing of Veau-Wardill-Kilner flap palate.
The anterior-lateral area is left to heal with secondary intention. The pterygoid hamulus is fractured.
The elevator muscle is reconstructed.
Closure of the nasal and oral mucosae is performed separately.
Post-operative care
Continuous oximetry should be employed if possible and nasopharyngeal intubation could be necessary.
Post-surgical bleeding is common so at the end of the operation it is essential to ensure haemostasis. Bleeding may cause respiratory obstruction which is responsible for a mortality rate of 5 in 1000 cases. Can be treated with an infiltration of carbocaine (mepivacaine) with 1% adrenaline. Continuous bleeding can be stopped with collagen and calcium alginate. It can also be controlled with light compression of the palate.
As with most head interventions it is suggested that patients are kept in a position such that the head is higher than their feet.
With children it is important that their hands are kept away from their mouths post-surgery by employing the usual methods (e.g. bandaging the hands, use of elbow splints and fixation of the forearm).
Feeding must be done with soft food through a straw or syringe administered by trained nursing staff. Oral feeding must be avoided for at least a couple of weeks.
Antibiotics and painkillers are always administered.
Intra-operative reconstruction of the nasal aspect of the palate with bilateral vomer flap


The nasal mucosa is divided into two parts and then closed on the medial line separately from the buccal mucosa.
Position of the flaps at completion of the operation
Bleeding may cause respiratory obstruction which is responsible for a mortality rate of 5 in 1000 cases.
Bilateral cleft lip and palate with nasal deformity.


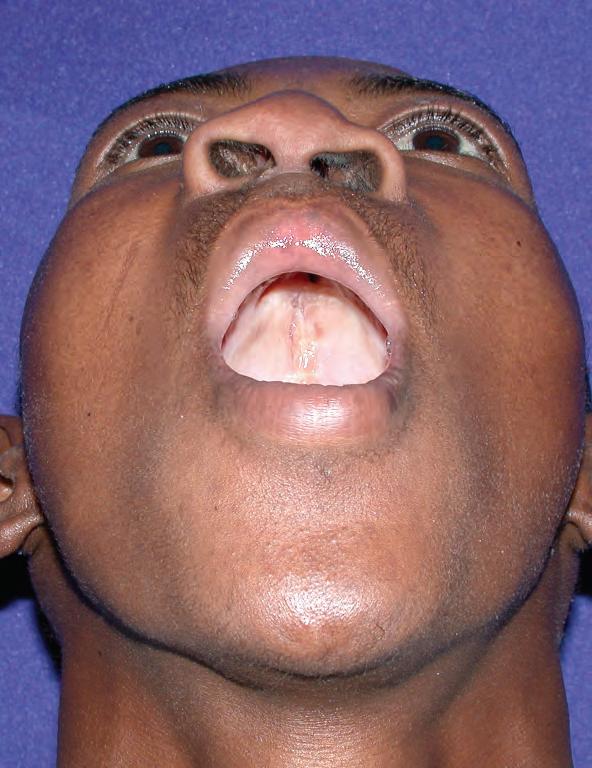


Appearance before and after reconstruction.
Self portrait by young patient
Before and after cleft lip and palate.

Palate reconstruction
Complications
The most frequent complication is fistula, which can occur in anything between 5% and 60% of cases, depending on the severity of the malformation. Fistulas are more frequent in cases of bi-lateral cleft, in the hard palate (about 37% of cases) and post-alveolar hard palate (30% of cases). Fistulas are the most troublesome complications. Surgical treatment of a fistula is the most difficult task in cleft palate; as with all kinds of fistula, it is always hard to resolve. Management of fistula is always a huge challenge to the surgeon, and it can be very difficult to achieve complete closure. Sometimes it requires more than one operation. Surgery becomes a big intervention for a small defect, in order to eliminate leakage of fluid and air into the nose, and to avoid the unhygienic lodging of food particles in crevices.
Two of the most important measures that can be taken to lower the risk of fistula are to close the oral and nasal mucosae separately, and to avoid tension in the sutures. One must also avoid a dead space between the mucoperiosteum flaps. It is recommended that the V-Y technique is not used as a first choice because it is associated with a higher risk of fistula.
When a fistula is present it can cause speech impairment and oral/nasal regurgitation. The extent of the complications that can occur depend on the size and position of the fistula.
It is not easy to cope with fibrosis and scars, specially in the hard palate where the tissues are not elastic. Mobilisation of the underlying tissues is absolutely necessary to shift them and to suture with 5/0 or 6/0 vicryl, taking care to avoid tension and paying particular attention to vascularization in tissues prone to necrosis.
The overall recurrence rate is around 13% but 90% of failed fistula repairs do result in a decrease in size.
Soft palate fistulas have the “advantage” of greater elasticity. It is suggested to close in two layers whenever possible, but sometimes this is not feasible.
There two type of fistula: the primary, which occurs after palatine cleft reconstruction, and the secondary (not in humanitarian missions) which occurs after maxillary expansion. The symptomatology depends of the size and location of the fistula.
There are two important negative effects of fistula, the most important usually being the effect on speech, although in poor social conditions, where the operative age is relatively old, this effect may not be quite so marked. The other is oro-nasal regurgitation, and keeping the fistula clean can be very challenging.
Treatment for fistula could be simply a flap shift with sutures, sometimes with a bone graft. Another possibility is a lingual or muscolomucosal flap on the facial artery (see Lip Reconstruction chapter pag 155) or even a pharingoplasty.
Incomplete closure of the soft palate results in an air-leak through the nose. This type of fistula can be repaired with superior or inferior pharyngoplasty, or by the medial transposition of the posterior pillars of the soft palate.
The overall care of patients suffering from cleft lift and palate continues for a very long time and different specialists are needed. In areas of the world lacking professionals and infrastructure, that will become the main focus of improvement for future generations.
Fistulas are more frequent in cases of bi-lateral cleft, in the hard palate (about 37% of cases) and post-alveolar hard palate (30% of cases).
The overall recurrence rate is around 13% but 90% of failed fistula repairs do result in a decrease in size.
Treatment for fistula could be simply a flap shift, with sutures, sometimes with a bone graft. Another possibility is a lingual or muscolomucosal flap on the facial artery or even a pharingoplasty.


Cancrum oris Onset and progression
The progression of cancrum oris infections has been the subject of clinical studies for the past 25 years. These have involved hundreds of patients who have survived the infection, most of whom have undergone reconstruction. The research was carried out using radiology, scanners, a reproduction of the skull of a three-year-old child and draws performed with PowerPoint. The infection starts on the mucosa, spreading into the bone and following a relatively precise path which could be in one or more of the following directions - ascendant, forwards or posteriorly. It is typically unilateral but exceptionally it can change direction and, starting from one side, can reach the opposite side, damaging it severely.
A thorough study of the topographic anatomy of the face, taking into consideration the relationship of the different features of each individual case, has provided a better understanding of the damage caused by the infection.

The research was carried out using radiology, scanners, a reproduction of the skull of a threeyear-old child and draws performed with PowerPoint.
Early stage of the drawing showing just the line of the mucosa and the xRay to better understand the evolution of the disease.


Skull of a three year old child used to study the progression of the disease.

Classification (based on origin of infection)


There are many ways to classify Noma on the basis of cutaneous defects: one of the most useful, because of its simplicity, is that of Montandon. The classification based on the origin of infection is as follows:
Type 1: the mutilation starts at 1-3 incisors, damaging the mucosa and sub-cutaneous tissue to the base of the nostril, alar ring and the whole thickness of the lip.
Type 2: the mutilation starts at 3-4 incisors and sometimes a canine, resulting in damage to the nostril, columella, inferior septum, inferior maxillary sinus, lateral wall of the nose, anterior palate and rarely point 0.
Type 3: the infection starts at 4 incisors and at least one canine and sometimes a molar, resulting in damage up to the tip of the nose. Damage could reach the 3rd turbinate as well as the internal orbit floor, and occasionally the temporo-mandibular articulation and point 0 (the dura mater). When the mandible is involved the lip could be completely destroyed.

Type 4: the infection starts at one or more molars and a canine (often 2-3 incisors), damaging the entire cheek, lip, maxilla, palate, superior turbinate, malar bone, orbit floor and temporo-mandibular articulation causing severe trismus, and reaching Point 0.
BOY, 10 YEARS OLD: 4 YEARS POST INFECTION

Infection at two superiors incisors , canine and molar resulting in lesion of the maxillary sinus, anterior palate, alar of the nose and nostril. Infection at an incisor has caused destruction of 40% of the upper lip and
a Type B columella lesion.
A first molar infection has resulted in posterior wall lesions of the maxillary sinus and cheek. This kind of infection typically reaches the medium turbinate and frequently destroys the sinus cavity, but in this case has just caused a weakening of the orbit floor.
GIRL, 8 YEARS OLD: 3 YEARS POST INFECTION
Infection at a canine resulting in a lesion at the base of the nose: as often happens in such cases, there is damage to the mucosa of the inferior wall of the maxillary sinus.
The lateral wall of the nose is slightly involved.






Infection at two incisors causing destruction of the superior lip (40%) and nostril, and a Type B columella lesion (see Columella chapter).
YOUNG MAN, 17 YEARS OLD: 11 YEARS POST INFECTION
Infection of the central incisors has spread to the lateral incisors, destroying the superior lip and causing a Type A columella lesion.
In patients where all the incisors are involved, and aggravated by the involvement of a left canine, the columella and lower septum are usually destroyed.
In this patient just a columella and nostril subcutaneous was damaged.


MAN, 33 YEARS OLD: 27 YEARS POST INFECTION
Infection at a canine, damaging the inferior part of the maxillary sinus and the base
of the alar nose, aggravated by a first molar infection, resulting in lesions of the cheek and slightly the corner of the mouth.
Involvement of incisors has destroyed 1/3 of the upper lip and caused a Type B columella lesion.

WOMAN, 25 YEARS OLD: 19 YEARS POST INFECTION

Classic canine infection, with necrosis of the base of the alar nose and cheek, as well as the superior lip and the inferior wall of the maxillary sinus.
Infection at incisors has resulted in typical destruction of the superior lip and a Type C columella lesion.
To lead to a cheek infection, it is necessary for a molar to be involved, causing damage to the posterior wall of the maxillary sinus. Exceptionally, damage to the cheek does not involve molars.






LADY 22 YEARS OLD: 17 YEARS POST INFECTION

Infection at a superior canine and two incisors, resulting in a lesion of the internal layers of the superior lip and provoking a Type A columella lesion, unusually avoiding the nose.

Typically in patients with this type of infection, where the canine is involved, there

is necrosis of the lateral wall of the nose and maxillary sinus. In this case the infection has remained low, without damaging the nose, just causing sub-cutaneous necrosis and retraction of the mucosa and a Type A columella lesion.
YOUNG MAN, 18 YEARS OLD: 12 YEARS POST INFECTION

Infection starting at a superior central incisors has spread laterally with destruction of 50% of the superior lip and a Type B columella lesion.
Involvement of a superior canine has resulted in damage to the alar base, lateral wall of the nose and the inferior part of the maxillary sinus.


Infection at a molar has caused lesions to the cheek, lip, commissure and posterior wall of the maxillary sinus.


MAN, 49 YEARS OLD: 43 YEARS POST INFECTION



Infection at a superior lateral incisors, aggravated by canine and first molar infection, has spread posteriorly, damaging the interior
layers of the superior lip and cheek. Unusually, in this case the infection has not spread upwards. Often it spreads upwards, further damaging the cheek and reaching the 3rd turbinate.

BOY, 8 YEARS OLD: 3 YEARS POST INFECTION
Infection at a inferior canine has spread posteriorly to a molar, causing a lesion of the cheek and, aggravated by infection of the lateral and central incisors, has damaged the internal layers with important retraction of the mucosa of the lip commissure. The infection starts at an inferior canine associated with a lateral incisor and, to some extent, a central incisor, it never spreads backwards, so the
floor of the mouth is unaffected. It has caused serious retraction of the mucosa, with obvious damage to the commissure. There is slight involvement of a molar, causing a cheek lesion.




YOUNG MAN, 21 YEARS OLD: 17 YEARS POST INFECTION
The infection started at a first inferior molar and canine, causing damage to the cheek, lip and commissure. It spread to the incisors resulting in necrosis of 1/3 of the inferior lip.
WOMAN, 22 YEARS OLD: 16 YEARS POST INFECTION



The infection starting at the inferior left lateral incisor and canine has spread forward to the incisors, destroying half of the inferior lip, and posteriorly to the molar, causing commissure fibrosis and lesion of the cheek.
In the case of involvement of all the inferior incisors, destruction of all the layers of the inferior lip is frequent, with necrosis as far as the chin.





GIRL, 5 YEARS OLD: 3 WEEKS POST INFECTION
Severe infection of inferior incisors and canines. The inferior lip is too weak and thin to withstand a heavy infection, particularly at the cul-de-sac where it meets the chin. This is the most challenging situation in lip reconstruction.


Infection very localised at the first inferior molar.





Infection of this kind is uncommon as it usually spreads to the neighbouring gum, which are more likely to be involved.

GIRL, 11 YEARS OLD: 6 YEARS POST INFECTION

Infection starting at a superior canine has reached the lateral wall and base of the nose and palate, damaging the lip and the maxillary sinus.


Spreading posteriorly to a molar it has resulted in lesions of the commissure and cheek.




Infection at incisors has caused destruction of 1/3 of the septum and inferior lip, and a Type B columella lesion.
WOMAN, 31 YEARS OLD: 25 YEARS POST INFECTION

Canine infection with a typical lesion of the alar base, spreading to the palate and damaging the maxillary sinus, with slight involvement of the lateral wall of the nose. The
infection has spread to a molar, resulting in necrosis of the cheek and aggravating the maxillary sinus lesion . Infection at incisors, causing necrosis of the superior lip and anterolateral palate, and a Type B columella lesion.
YOUNG WOMAN, 16 YEARS OLD: 12 YEARS POST INFECTION

Classic severe infection of first superior molar and canine, destroying the maxillary sinus (but slighyly weakened the upper part of it and the orbit) and damaging the sub-cutaneous tissue at the base of the nose.
The infection from the molar has traversed




the superior 1/3 of the sinus cavity.
The canine infection has caused a lesion of the inferior mucosa of the maxillary sinus and weakening of the sub cutaneous tissue of the lateral wall of the nose.
The lateral incisor is often involved when the canine is strongly infected.
MAN, 28 YEARS OLD: 23 YEARS POST INFECTION

Very severe infection at first superior molar, spreading forwards and upwards, completely destroying the maxillary sinus, but not reaching the eyeball. The floor of the orbit is frequently involved in these cases as the infection from molars spreads, damaging the upper wall of the cavity.
Infection at a canine has caused the destruction of the inferior-internal mucosa of the maxillary sinus: in this particular case, a lateral incisor, and to some extent a central incisor, are involved, causing sub-cutaneous damage to the nostril.


WOMAN, 22 YEARS OLD: 18 YEARS POST INFECTION
Severe infection at one superior molarspreading forwards but lower than usual, avoiding the upper part of the maxillary sinus and superior turbinate, but destroying the antero-lateral palate (aided by infection at a canine). As in most patients, when this happens, the infection fails to reach the temporo-mandibular articulation, but formation of a bony bridge results in moderate trismus.
Canine infection, which is the most frequent (83% of cases), provoking typical lesions, damaging the inferior maxillary sinus, alar ring and lateral wall of the nose. In such patients it is easier for the canine infection, aggravated
by that of neighbouring teeth, to reach Point 0 with fatal results.





Infection of the incisors, aggravated by a canine, causing a 70% loss of the superior lip (the most typical lesion caused by an incisor infection), a Type C columella lesion and damage to the septum and anterior palate.
WOMAN, 21 YEARS OLD: 17 YEARS POST INFECTION
Infection at a superior canine with classic destruction of the inferior maxillary sinus, nostril and lateral wall of the nose.
The infection has spread from molars leading to complete destruction of the sinus and reaching the superior turbinate. As usually the orbit floor is weakened by a molar infection. Point 0 is easily reached, so


the mortality is very high with this type of infection.
Infection at an incisor has resulted in damage to the septum and a Type B columella lesion.

BOY, 4 YEARS OLD: 7 WEEKS POST INFECTION


Infection starting at a superior canine with classic destruction of the alar nose, lateral wall of the nasal pyramid, inferior and medium turbinates and maxillary sinus.
Infection at superior molars spreading forward, resulting in complete destruction of the maxillary sinus, lateral palate and superior turbinate, but avoiding the orbit: this often happens when the infection is not


strong enough to reach Point 0.


Infection at incisors, aggravated by a canine infection, has resulted in complete destruction of the superior lip, damage to the septum and anterior palate, and a Type C columella lesion.
BOY, 6 YEARS OLD: 5 MONTHS POST INFECTION
Infection of two superior molars, a canine and three incisors (including slightly one ipso-lateral).
The infection at the molars has progressed forward and upward to the orbit which in most patients results in loss of the eyeball, damage to the cheek, the superior turbinate and superior 1/3 of the lateral wall of the nose. The posterior and superior walls of the maxillary sinus are also destroyed. When the molars are involved, the sinus, the orbit and the cheek are affected, and sometimes the temporo-mandibular articulation is damaged: this results in trismus.
The infero-anterior wall of the maxillary si-


nus is destroyed by the infection at the canine close to it. Lesions to the alar and lateral wall of the nose are most typical of canine infection, aggravated by infection of a lateral incisor.
Infection at a central incisor damages the inferior 1/3 of the columella, resulting in a Type B lesion.
MAN, 36 YEARS OLD: 30 YEARS POST INFECTION
Infection originating at a superior molar has spread upwards, destroying the maxillary sinus, causing loss of the eye and reaching the superior turbinate – it has just missed reaching Point 0. As often happens, the infection has spread forward rather than up, avoiding damage to the temporo-mandibular articulation.


Involvement of a canine has typically resulted in destruction of the base and lateral
wall of the nose.


The concurrent involvement of molars has resulted in complete destruction of the maxillary sinus and anterior palate. Infection at an incisor, aggravated by a canine infection, has destroyed the septum and caused a Type C columella lesion.
BOY, 4 YEARS OLD: 10 DAYS POST INFECTION

Infection at four molars on the left, with complete destruction of the cheek and maxillary sinus. The infection has ascended posteriorly, causing damage to the temporomandibular articulation, the superior turbinate, lateral wall of the nose and Point 0, with a life-threatening prognosis.

Infection at a canine has resulted in complete destruction of the lateral wall of the nose, inferior maxillary sinus and the 1st and 2nd turbinates. Infection at an inferior canine has damaged the buccal commissure
and, aggravated by infection at molars and incisors, has played an important role in the total destruction of the inferior lip.

Infection at a superior incisor results in a Type D columella lesion, while infection at an inferior incisor causes total destruction of the inferior lip

BOY, 12 YEARS OLD: 7 YEARS POST INFECTION



Infection at inferior molars, canine and lateral incisor, with destruction of the cheek and internal layer of the inferior lip.
Infection at superior molars and canine resulting in damage to the inferior and posterior walls of the maxillary sinus and destroying all layers of the cheek.


The maxillary sinus is damaged just at the inferior floor, but the superior wall and the floor of the orbit are save , the infection didn’t spread to the temporomandibular articulation.
Tongue is never involved even when the infection is important and localized.

BOY, 4,5 YEARS OLD: 15 MONTHS POST INFECTION
Infection at superiors and inferiors molars with involvement of superiors canines, one incisor and inferior canine. Destroying
all layers of the cheek, necrosis of the maxillary sinus, orbit floor, hard palate, slightly lateral wall of the nose, spread to temporomandibular articulation.

Important mucosa retraction.

LADY 22 YEARS OLD, 15 YEARS POST INFECTION
Infection at four molars and two canines with damage of the cheek, lips, maxillary sinus and temporomandibular articulation causing ankylosis.
The first operating time, is the resection of the necrotic tissue and to free tissues




especially mucosa.
The second time is a free flap of double latissimus dorsi palette to reconstruct inner and outer layers.
Condylectomy is the last resort. Trismus relief achieved 75% at 3 months and just 20% at 5 years.
BOY, 5 YEARS OLD: 2 YEARS POST INFECTION


This patient is the exception of the rule. One of the few with transversal evolution. The infection started at a superior canine and two incisors. Unusually, it has spread transversally, and after damaging the superior lip and base of the nostril, has penetrated to the lateral wall of the right maxillary sinus and the lateral wall of the nose.

Then it changed direction, spreading to the left side and damaging the septum, superior wall of the maxillary sinus and the floor of the orbit, reaching the eyeball with resultant loss of sight






Surgery of Cancrum oris
Reconstructive surgery to correct Noma disfigurement is a huge challenge for surgeons, as the deformities vary tremendously in size and shape. They can be superficial and/or deep (sinus, palate, maxilla, nasal cavity and orbit) and at the beginning of our work there was no standard surgical procedure: some patients had to be studied and treated individually before planning the procedure to be applied. Now, after years of analysis on every type of patient, the surgical procedure can be precisely determined. Moreover, a deeper understanding of the progression of the disease has made the treatment standardised.
When possible we perform a pre-surgery “toilette” in order to accelerate healing and eliminate bacteria.
The lesions vary from just mucosal/gum to huge loss of tissue, teeth, muscle, cartilage, septum, bone, palate, nose, eye and orbit floor. In half of the patients a healing tissue with great retraction is present, causing trismus.
There are some mechanisms which can be used to avoid, or at least to reduce, the risk of retraction, such as elastic or wooden instruments but they are difficult to realize in those social situation where a mother must cope with other children and lack of education. It is even difficult with adults, as they are not fully aware of the consequences of the disease.
The correction of the trismus is mandatory allowing the rehabilation and the return to a normal social life. It requires reconstruction of the mouth to avoid leakage of saliva, food and liquid, and improving the ability to open the mouth.
Reconstruction of muscle, cartilage and bone involves a wide range of surgical procedures, from little flaps to free flaps. Most of the patients require one or two operations and only few need more procedures. The operations are performed in the their home country to avoid any psychological problems that may result from expatriation/repatriation adapting the surgical approach to the resources available. It is impossible to avoid micro-surgery but we try to limit the number of cases.
The pre-operation treatment, from rehydration, hyper-caloric feeding, antibiotic therapy and wound treatment, is very important to improve the patient’s clinical conditions in the operating theatre.
Treatment of the scars should not start before 6/12 months, in order to allow complete cicatrization.
As the tissues shrink, they leave large scars which fill in during the months of cicatrization. The teeth and bones are often exposed, and bony bridge can develop at the time of fibrosis, especially in the cheek mucosa and masseter muscle, causing a retraction of the masticatory system.
Some patients had to be studied longtime before planning the procedure. After years of analysis the surgical procedure, today can be precisely determined.
Deeper understanding of the progression of the disease has made the treatment standardised.
Cancrum oris.
Boy, six years old; 5 months post infection. Infection of two superior molars, a canine and three incisors.




As the tissues shrink, they leave large scars which fill in during the months of cicatrization. The teeth and bones are often exposed, and bony bridge can develop at the time of fibrosis, especially in the cheek mucosa and masseter muscle, causing a retraction of the masticatory system.
Orbit floor and superior maxilla.
After toilette.
The damage is evaluated with regard to necrotic tissues, the development of the dentition and the growth of the skull.
The fl aps most often used are Estlander fl ap, naso-genian fl ap, frontal fl ap, latissimus dorsi fl ap, cheek rotation fl ap, cervical-facial fl ap, Webster advancement fl ap, Abbe fl ap, sub-mandibular fl ap, platysma fl ap, delto-pectoral fl ap, para-scapular fl ap and free fl aps. We don’t use hinge fl ap (Nose: surgical reconstruction) and we avoid grafting temporal fascia.
The Webster flap allows us to slide a large amount of tissue from the jowl to the centre of the face, especially to reconstruct lips, mouth commissure and columella.
The elasticity of the skin is greater in African patients than in Caucasians, which makes it possible to cover large lesions as it slides more easily.
For the reconstruction of the nose, the best results are obtained by using middle frontal flaps and sometimes converse flap with rib support if necessary.
For the reconstruction of the jowl and mouth, especially when a large amount of tissue is needed, delto-pectoral flap and platysma flap are used. Grand dorsal flap Is often used as a free flap or pedicle flap. Which one is used depends on a number of factors, including the condition of the patient and the humanitarian mission situation.
Loss of the lower lip is a huge handicap for patients, affecting the continence of the mouth and it make the surgery more challenging. Quite often the damage is deep down in the mucosa, with huge retraction of it. Occasionally advancement of the mucosa to reconstruct the red lip may be necessary after vermilionectomy. This procedure reconstructs a lower lip which easily reverses and which quite often needs moisturiser to maintain hydration.
Patients quite often have bad or weak vascularisation at the corner of the mouth and need transfixing resection flaps.
More frequently we use the technique of stair-step. In most cases we use the Estlander flap when there is a need for some tissue from one lip to repair the other. The recipient lip is prepared to host the flap which often comes with extra mucosa to cover the lack of tissue.
Sometimes a commisurotomy is necessary with orbicular muscle. The muscle is fixed laterally (both flaps) and an asymmetric z-plasty used to reconstruct the mucosa (See Lip Reconstruction chapter, page 156)
The Camille Bernard flap is another flap which can be used for total reconstruction of the lower lip. It is a sliding transfixing bilateral flap. The procedure is made easier with the excision of the bilateral triangles which are positioned at or inside the naso-genian groove (see Lip Reconstruction chapter).
The fan flap of Gilles, which is performed in patients with great skin laxity, and the McGregor flap are other varieties of fan peri-commisural approach. When using these flaps, it is necessary to leave excess mucosa to reconstruct the red lip.
Less used is the Karapandzic flap where the incision doesn’t reach the nostril but remains below it, preserving arteries, veins and nerves (see Lip Reconstruction chapter).
We don’t use hinge flap.
The elasticity of the skin is greater in African patients.
In most cases we use the Eslander flap. The recipient lip is prepared to host the flap which often comes with extra mucosa to cover the lack of tissue.
Flaps used in facial recontruction (see table on the opposite page)

Hard palate damage.




Temporoparietal flap.
Toilette.
Final appearance.
When possible we perform a pre-surgical toilette in order to accelerated healing and eliminate bacteria.
Most of the patients require one or two operations and only a few need more procedure, specially when a flap preparation is need.
Cancrum oris before toilette. Infection of four molars, canines, and three superiors incisors.




Most of patients present complex disease associated . To cope with is mandatory a mission staff with great surgical and clinical training.
Noma before surgical toilette.
Removed teeth.
After toilette.
Cancrum oris, 7 week, post infection, before and after a toilette.
Another flap frequently used is the naso-genian, which allows to reconstruct the lower lip, upper lip and columella, with the help of other flaps such as the opposite naso-genian, or sub mental or cheek and chin advancement. The naso-genian is used, especially inside the mouth, because it is devoid of facial hair. The flap could be just sub-cutaneous or built on the facial artery.
Cervical-facial advance flap and Mustarde flap are used to reconstruct the cheek, sometimes with the help of a skin graft.
Platysma flap: the platysma muscle reflects on the edge of the mandible. The main indication for this flap is to reconstruct a lack of buccal mucosa.
The dissection reaches the edge of the maxillary bone and at the end of the flap a pad of skin is harvested to become the buccal mucosa, obtaining a large arc of rotation. Care must be taken to avoid the sub-mandibular nerve which is 2 or 3cm below the edge of the mandible.
For many reasons we avoid oncologic patients, due to the lack of follow-up, medical personnel and conditions of treatment (see Tumours chapter). It is hard to imagine how big some tumours can become, making life very hard for both the patient and the family. Some can be evaluated as toilette indications.
Exclusively for men, but rarely used, is the scalp flap which must be high enough to reconstruct the lower lip.
These patients can require huge reconstructions for hygienic and functional reasons even though their life expectancy may be short.

On the other hand, neurofibromatosis of Recklinghausen has a conventional follow up (see Tumours chapter).

Nose Reconstruction
The nose is frequently damaged in Cancrum oris. In most patients, the infection spreads from the central front area of the gum. The damage is sometimes deep, involving only subcutaneous tissue, the lower part of the columella, anterior septum and the mucosa of the inferior maxillary sinus. But often the damage is more severe, causing necrosis of the nostrils, alae and lateral wall. It can even result in total necrosis of the nose, often in combination with damage to the superior lip and cheek, and may also reach point 0. A cancrum oris lesion in the central part of the face is the result of the infection started from two or more incisors and one or both canines. When the infection damages the cheek and the lateral wall of the nose a molar is probably involved as well.



Damage of the nose is the result of the infection started from two or more incisors and one or both canines.

Lesion resulting from a canine infection.
Lifting a nasogenian flap.
Final result.
Canine on its own can just provoke lesion of the lateral wall but potentialize by incisors can destroy the nasal pyramid and reach point 0
Columella lesions (se chapter) could be:
• Sub-cutaneous and periosteum under the nostrils and columella; base of columella or nostril;

• whole columella, alar of the nose/caudal septum;
• tip/lateral wall of the nose/septum.
• alar cartilage
Lesions of the nose are often associated with infection of the upper lip. The class depends on the width and severity of the lesion. When the defect is not too wide, the reconstruction can be done using local flaps. If the lesion is complex, reconstruction of the lateral wall of the nose is required, and other techniques have to be considered. The most commonly employed are frontal flap, converse flap, advancement flap, naso-genian flap and exceptionally the forearm flap, which is not the first choice in a humanitarian mission but is an excellent tissue to mould.

As the infection always spreads from the gum, the deeper layers (mucosa and muscle) are the first to be damaged. In the next stage, cartilage and bone, including the maxilla are extensively involved. Lastly, the superficial layers are involved, with partial or total destruction of the following structures: columella. alar rim, nostril, lateral wall of the nose, tip of the nose and anterior palate.
Complete destruction of the nasal pyramid.
Naso-genian flap lifting. The first step is the reconstruction of the deeper layers.
Appearance after 1st operation.

The first step is the reconstruction of the deeper layers. Tissue for the reconstruction is brought from inner and outer layers. The dome of the nose needs to be supported by bone or cartilage, whilst the lateral wall and columella only require soft tissue as they are supported by the alae and the base of the nostril. In some cases support of the tip, either on its own or in combination with the dome, is needed: rib cartilage or septum/ear cartilage are frequently employed.
Nose: surgical reconstruction
The best way to plan a nose reconstruction is to follow the principles established by Burget.
Reconstructing the nose in humanitarian missions requires respecting the needs of the patients, functionality, and resolving the problems with the minimum number of operations. The surgeon bears extra responsibility as there is little discussion with patients, and we often choose more complex procedures, aiming for the best functionality and aesthetic results. Sometimes the lesions are severe and the technique requires three operations. The follow up of these patients requires well organised missions able to take the necessary care, and able to cope with various situations (such as preparing for the next operation) and to resolve complications.
The idea is to reconstruct skin, cartilage and bone using the same types of tissue, and to evaluate the quality and quantity of tissue needed to achieve the correct proportions. Tissue from around the nose provides a better colour match than tissue from elsewhere.
Cancrum oris lesions are more variable than those we usually see as a result of other pathologies, so there is a wider range of operating techniques. The object of the reconstruction is to build a malleable but solid structure.
The ideal reconstruction often employs a complete aesthetic subunit, even if this sometimes necessitates enlarging the size of the defect: the advantage is that the scars lie in the transition zone between adjacent aesthetic subunits. Also in large transfers of tissue, scars are more acceptable than on the donor site.
All the principles that apply to the reconstruction of cancer lesions are applicable to Cancrum oris, even if the lesions are frequently different. However, other principles apply to the defects resulting from congenital deformities.
There are several different flaps that can be used for reconstructing the nose:
A) Local flap.
In humanitarian missions, local flaps, such as the rotation Rieger flap, later modified by Marchac, are seldom considered although useful when the nose is small. The local flap used to reconstruct the inner lining of the nasal vestibule is a turnover flap. Paying particular attention to the risk of poor vascularisation, the base must be thick enough to avoid suffering necrosis and retraction, which makes it difficult to reconstruct the outer lining. This turnover flap plays a key role in preparing the ground for the cover flap.
The ideal reconstruction often employs a complete aesthetic subunit, even if this sometimes necessitates enlarging the size of the defect.
The naso-genian flap frequently use to reconstruct inner layer of the nose.


B) Cheek flap.
This is very useful for repairing lateral defects of the wall of the nose. The tissue is elastic and the advancement is lateral. In certain cases, it can be divided into an inner flap to reconstruct the inner lining and an external flap to reconstruct the outer lining.
C) Naso-genian flap
This flap is the most used to reconstruct the inner layer of the nose. The former is more often employed as it has a very good arc of rotation and the scars at the donor site are less noticeable. Frequently the base of the flap is included in the reconstruction. Vascular support is provided by transverse branches from the contralateral angular artery and by a confluence of vessels from the angular and supraorbital arteries. The nasolabial is a random flap. The distal part on the cheek contains the main angular artery with a retrograde flow, while the proximal portion lies on the lateral wall of the nose. Cancrum oris patients are prone to vascularization problems, as often the vessels are compromised as a result of a canine being affected.

D) The Pers flap
This is a good choice for reconstruction of the inner lining and external wall of the alar nose. The flap is raised from the extremity to 1cm of its base. This is an example of an in and out flap, where the proximal part of the flap is used to reconstruct the internal layer (in) and the distal part become the external layer (out).
The arteries of the naso-genian region come from the outside of the alar nose: for this reason the flap must be built externally to avoid vascular damage. In a second operating time (just under local anaesthesia), the alar nose is set in the correct position and at the same time the pedicle is divided.
Pers flap drawing
Frontal flap and naso-genian flap are frequently used to reconstruct the nose.
Frontotemporal flap
One of the most popular flaps for reconstruction of the nose is a scalp flap described by Converse. This flap has many advantages in large nasal reconstructions, such as the quantity of tissue to be transferred and a good colour match. Also, for patients with a low hairline, the scalp flap technique provides more morbidity to achieve an adequate flap length. In these cases, the reconstruction can be done with an oblique Converse flap, on condition that the incision in the scalp is further back in order to maintain the vascularisation o the flap. The vascular supply is based on the superficial temporal vessels, and drainage from the flap (especially venous) from the scalping flap is superior to that of the midline forehead flap, and is more reliable, even in smokers.
On the other hand, it does produce a thick ala with a constricted airway, the scar in the donor area is not the best aesthetically, and can be disturbing even when the nose reconstruction is perfect.
The portion of skin which will serve as the nasal cover is raised superficially to the frontalis muscle, leaving only skin and a thin layer of sub-cutaneous tissue.
At the level of the hairline the plane of dissection is deepened, penetrating the galea to raise the remainder of the pedicle in the sub-galea plane.
The donor site on the scalp may be treated with split-thickening skin graft or a non-desiccating dressing. At the time of division, when the scalp portion of the pedicle is returned to its previous site, a full-thickness skin graft from the supra-clavicular region is applied. We often prefer to perform a skin graft at the time of the first operation.
This flap has the disadvantage of requiring a second procedure, which is usually performed under general anesthesia because a skin graft or other surgical improvement is necessary. However, sometimes it is possible to perform under local anesthesia.



Pre-operative appearence of lesion caused by infection at canine and incisisors 2 or 3.

Naso-genian flap to reconstruct inner layer.
Frontal flap and rib cartilage to provide skeletal support.
Final appearance.
Forehead flap
This flap can be used to replace any or all of the aesthetic subunits of the nose. It is an axial flap based on the supratrochlear and supraorbital vessels.
The medial frontal flap is a reliable flap for nose reconstruction, employed in India since the 19th Century and reintroduced in 1946 by Kazanjian. It is often the best choice for nasal skin reconstruction. In fact it is easy to work with as the vascular anatomy (supra-orbital artery and supra-trochlear artery) is regular and constant in its topography. It can be used to cover wide defects, as commonly occur in cancrum oris, or just minor ones, such as just the tip of the nose. Also it can be used to provide skin for the superficial surface or for the inner lining. In the hands of a skilled surgeon it is very reliable with a low risk of donor morbidity, as opposed to the lateral forehead flap which is associated with higher risk. Colour match and skin pliability are good: although the quality of the skin might not be the best, but it is sufficient to give a very good result.
The flap is set over the medial line with a width of around 3cm - 4cm, allowing direct closure without the help of a skin graft or another flap. The quality of the medial frontal flap scar is always aesthetically good. The flap should not be too wide, allowing an easy rotation without damaging the vascular (supratrochlear artery) support. The frontal flap has a very wide arc of rotation on the supra-trochlear artery. The vessels come from deep down and must be preserved making a careful dissection under the base of the periosteum.
If the hairline is low, it should be oblique in order to get a greater flap length able to reach the nostril base and to reconstruct the columella.
It is possible to perform this flap through the midline but the vascularisation is then poor, and the tip of the flap can suffer. In bald patients the frontal flap can be drawn very long on the axis of the supra-trochlear vessels, and can be used to reconstruct severe damage of the nose and cheek (see Cheek Reconstruction chapter).
This flap is often used to reconstruct the middle of the face, often in conjunction with a naso-genian flap to rebuild the deep layer.
Another advantage of this flap, when it is long enough, is the possibility of doubling it over at the tip to reconstruct the inner layer.
Retraction is frequent with these flaps, but they heal on their own without the need for skin grafts or other flaps.
Before starting the dissection it is recommended to measure the length of the flap, trying to minimise the risk of pedicle retraction or cephalic tension on the tip of the nose. A frontal flap can be bi - or tri-lobed. It could be para-medial, with the same pedicle on the frontal vein, which can be made visible by performing the Valsalva manoeuvre.
The dissection of the upper part of the flap should not touch the muscle and galea, which are not included in the flap, going deeper under the periosteum in the lower part and avoiding damage to the pedicle. In patients with scars between the eyebrows, Doppler sonography is recommended, to check the location and viability of the vessels, knowing that the supratrochlear artery is 2cm laterally from the midline. The blood vessels lie deep between the corrugator and frontalis muscles, becoming superficial in the distal part of the flap. The anatomy of the flap facilitates debulking, and the shape is optimal.
When the frontal hairline cannot be avoided, it is essential to carefully remove hair follicles, especially in the more distal millimetres of the flap in order to reduce the risk of necrosis in this vital part. This is made possible as the flap has a good blood supply.
The flap is rotated through 1800 and the donor site closed with excellent results. Secondary healing of the gap remaining under the hairline gives a better aesthetic result than a skin graft.
The pedicle is divided after three weeks and any excess tissue removed.
As noted above, when the hairline is low, or the nose defect is low, an oblique forehead flap is indicated. Just this portion of the flap is random and has a higher risk of necrosis. The direction is toward the opposite hemi-frontal (in a few cases it could be to the same side) in order to close the base of the nose and improve the healing of the upper donor side. If more tissue is required, then exceptionally a supplementary flap or skin graft will be necessary. The big advantage of this flap is that it heals on its own leaving a very good quality of scar.
Technique
• A Doppler ultrasonic scanner is used to identify the axial pedicle; this point lies between the mid-line and the supraorbital notch
• An exact foil template of the nasal requirement is made.
• The distance from the base of the pedicle to the most distal point of the defect is measured, and then this measurement is transferred to the central axis.
• The template is rotated through180o and set over the distal portion of the axis of the flap, which is then outlined with a surgical marker.
• The infiltration is made without adrenaline.
• The incision of the distal part of the flap is between the subcutaneous and the frontalis muscles.
• The dissection becomes deeper passing behind the muscle at the mid-portion of the forehead.
• The dissection continues towards the brow and the glabella.
• When the dissection reaches the brow, the borders are incised and the flap is carefully released.
• The flap is dissected so as to obtain a tension-free transposition.
• The distal portion of the flap is thinned to the subdermal plexus. Particular care must be taken with patients who smoke or are diabetic.
• The flap is fixed in two layers, paying attention to vascularization.
• The proximal wound could often be closed, but the distal wound, which is wider than 25mm, is left to heal by secondary healing.
• The flap is bandaged and the wounds dressed with Vaseline gauze.
• The pedicle is divided 3 - 4 weeks later when the flap is completely healed.
• The nose side of the flap is raised with 2mm of sub-cutaneous fat.
• The revision operation is performed at least six, and preferably twelve months later.
• Debulking of the flap is performed from the cephalic side when the tip of the nose is reconstructed: this approach allows it to easily reach the tip, the columella and the alar side.
Debulking of the flap is performed from the cephalic side: this approach allows to easily reach the tip, the columella and the alar side.
Cheek advancement and rotation flap to lower nostril


Noma infection started at two incisors and canine.
Appearance after first operation, alar fly and cheek advancement flap.
Appearance after second operation.


Cheek flap rotation to lower the alar ring/nostril.
Final result.
One of the most challenging problems in surgery of the nose is to lower the nostril(s). One possibility is to perform a alar nose fly and to bring tissue to increase the lenght of the lateral nasal wall.
Width reconstruction of the nose
When the infection starts at the incisors involving one or both canines and damaging the lip, patients with cancrum oris lose a large part of the nose. In fact, the lateral wall (often on one side), columella, septal cartilage, vomeronasal cartilage, lateral-anterior palate and the inferior end of the nasal bone are largely destroyed. This damage is associated with partial or complete destruction of the upper lip, adjacent area of the cheek, lower eyelid and orbit, with consequent loss of sight.
In these patients it is important to reconstruct the nose to maintain or improve their breathing. It is necessary to reconstruct the inner lining first, then the nasal floor and mucosa, the upper lip, with excess tissue at the side wall. This is important, as a completely closed inner lining which avoids retraction or stenosis could make breathing difficult. The next step is the skeleton and the outer lining. Obtaining sufficient tissue for this step, and for the whole procedure, is not always easy, especially when a previous attempt has failed. Another solution is to employ a couple of forehead flaps, in two operating times to avoid the need for skin grafts. This procedure is possible but rarely needed. Another issue with the medial forehead flap is the tunneling to the nasal part which carries a risk of fistula. A careful de-epithelialisation, avoiding pressure on the pedicle, decreases the risk of fistula. However, in most cases we prefer to avoid any risk of pressure on the pedicle by performing a short and simple operation to divide the pedicle and to spread the remaining tissue at the base of the nose in a second operating time – the scar disappears easily.
Usually, the preferred choice is a free flap, which is not the best choice in a humanitarian mission. The forearm flap has the advantage of the elasticity of the tissue making it easy to shape the new nose. It is essential to have a lot of experience with this flap at low ejection. It has a long pedicle but it is always hard to cope with problems of venous return.
If there are no contraindications, the pedicle is divided after four weeks.
The first step of the reconstruction aims to remodel the upper lip and, where possible, to reconstruct the floor of the inner lining. The second stage requires a very accurate technique to complete the inner lining, to make the support for the rib and to complete the outer skin cover. We usually suggest performing this step after a period not inferior at one month.
To keep suffering to a minimum, the inner lining is rebuilt using surrounding tissues or skin roll-out roll-in. Before setting the rib it is essential to check that the inner lining is completely closed to avoid secondary healing and possible retraction which would impair the respiratory function. When surrounding tissue is employed, the flap is called a “local turnover flap”. In this case, two or more flaps may be required, especially when a previous attempt at reconstruction has failed, resulting in insufficient tissue for the inner lining. For example, the photograph show a patient on whom a rollin was performed to obtain the tissue to cover the lesion. A forehead flap is excellent for outside reconstructing skin, and can also be very important for reconstruction of the inner lining. Other flaps, such as the temporoparietal fascia flap and free flaps, are rarely used, in humanitarian missions.
The rib bone is shaped at the tip and laterally, and is fixed to the base of the nose through the nasal bones using metal stitches.
It is necessary to reconstruct the inner lining first, then the nasal floor and the mucosa with the excess tissue at the side of the wall.
Frontal flap: we prefer to avoid any risk of pressure on the pedicle by performing a short and simple operation to divide the pedicle and to spread the remaining tissue at the base of the nose in a second operating time. Tunneling the flap carries a risk of fistula.
Noma reconstruction with radial forearm flap before modelling of superior lip and nose.


The rebuilt nose will be supported by the maxillary bone, the nasal floor and the superior lip. Care must be taken to avoid excess tissue around the lateral wall. It is essential to make a surgical plan to spread the lateral tissue, to rebuild the mucosa and to support the skeletal structure, whilst preserving the vascularisation. Cartilage is seldom used to provide skeletal support, as it often requires a sturdier base to support the frontal tissue. We prefer a rib, shaped and covered with vascularised soft tissue. The skeletal support and skin covering are performed at the same time.
When reconstruction of a premaxilla defect is needed for patients being operated on in their home country, it is suggested that a vascularised bone graft should be avoided and preference given instead to a calvarian, hip bone or cartilage graft.
Appearance post reconstruction of nasal mucosa, nose and superior lip.


The pictures show a patient in whom a very complex nose reconstruction has been performed, with a reshaping of the upper lip. In these cases two operations are necessary, and sometimes later retouching will be needed to obtain an aesthetically satisfactory result.
When performing a frontal flap there are two different approaches to managing the division of the pedicle and the debulking. This step is important for the final refinement of the flap. Usually we choose to do division and debulking a month after the operation. Some authors prefer to perform the debulking when the pedicle is still untouched rather than during a second surgery. In fact, debulking performed at a second surgery may be associated with a higher risk of suffering and it may require several small retouches.

Debulking performed at a second surgery may be associated with a higher risk of suffering

Modelling of superior lip and preparation of the nose mucosa flap.


Frontal flap and setting of the rib support.
Frontal flap sliding.
When a frontal flap plays an important role in the inner lining of the nostril a nasal obstruction may occur. In these cases, the debulking should be done by alar rim incision a month after the surgery, after the regeneration of vessels of the grafted area. The pedicle is divided 3 – 4 weeks after the operation, unrolling the base and moulding it inside the inverted “V” at eyebrow level, ensuring symmetry. Moreover, to achieve an invisible result it is important to avoid lateral tension and to eliminate all excess tissue. All scars can be reviewed later if necessary. The frontal flap is normally safe but complications could arise unless great care is taken with its width, length and tension. In particular, the inner lining must be built with care as it can suffer if there is lack of contact suturing, or incorrect pressure of the transfixing sutures or nasal packing.
The columella is an area which is often damaged, either partially or totally (see Columella Reconstruction chapter, classification). There are many ways to reconstruct it with local flaps from the base of the alar rim, naso-genian flap, nostril base flap, philtrum, internal dome mucosa and forehead flap, converse flap, Washio flap or free auricular flap among others.
In some patients a double forehead flap has been used: it is possible to use a second forehead flap, based on a supratrochlear artery, after skin reconstruction. In patients with a double forehead flap it is not necessary (and may be impossible) to close the donor sites completely and this can be achieved later. We always plan any procedure in order to avoid a skin graft.
The forehead flap is useful, and often employed for, reconstruction of the nostril, alar rim and columella. It can ensure a good contact with the mucosa, which is necessary for the vascular survival of the whole flap. Quite frequently, debulking of the alar rim is necessary and this is performed through the dome of the nose. This approach allows us to reach both the tip and the alar rim. The debulking can be done some weeks later, after revascularization of the completed flap has been established.
Rib cartilage
Reconstruction of the nasal osseocartilaginous framework is frequently needed in facial reconstruction in Cancrum oris patients. Septal cartilage alone is not sufficient for reconstruction of the large lesions caused by Noma; often a large amount of solid grafting material is needed.
The main point in favour of a rib cartilage graft is the consistent long term results with low resorption rate. It is a reliable material which rarely needs structural support. We choose the cartilaginous segment of a rib that provides a straight segment and it is possible to harvest all the required grafts from a single rib. The choice is between the cartilage from the 5th to the 7th rib. Exceptionally there is a need for an additional graft and in these cases an adjacent rib is harvested.
The incision is made over the chosen rib to facilitate the dissection. In females patients it is performed 3 - 5mm above the inframammary fold, care being taken to avoid going beyond the medial extent of the inframammary fold. Once the muscle fascia has been reached, the muscle is divided directly over the chosen rib. The most lateral extent of the dissection is demarcated by the costochondral junction.
Perpendicular cuts are made at the most medial and lateral aspects of the cartilaginous rib to allow the dissection of the perichondrium. The sub-perichondrium dissection is made circumferentially until the posterior aspect of the rib is exposed. The vessels lie on the inferior edge of the rib, and it is essential to remain in the sub-perichondrium space ensuring that the perichondrium is not violated and a bloodless dissection is performed.
In most cases the rib is attached to the base of the nose (nasal bone) with metal stitches which ensure enough stability without the need for any other rigid support between the rib and the nasal spine. It is very important to avoid any kind of traumatic edge against the skin, particularly at the tip.
Sometimes the cartilage becomes tight: in these cases it is necessary to make cuts on the anterior surface of the perichondrial flap to release tension. A curved rib stripper is slid back and forth along the rib with gentle upward force, being careful to avoid fracture of the rib. Perichondrial tears should be avoided and tight post-operative closure must be ensured, in order to avoid post-operative pain. The wound must be closed carefully in layers.


A bent rib is an option when the shorter part gives support to the columella. It can be fixed to the nasal spine if present, or to the maxillary bone. Exceptionally, to increase stability the cartilage can be fixed with strong stitches and setting with the help of remaining mucosa around and particularly on, the nasal spine. The material should be covered by mucosa from the septum, palate or maxilla, taking great care to attach it solidly and stably.
In our experience, midterm results are good with a central support. A frontal flap is strong enough to provide lateral support for the new nose.
The main aim is to reconstruct a stable nose. Correct stitching and above all, utilisation of surrounding tissue especially mucosa, to fix cartilage, help to achieve stability.
In the vast majority of patients, it is not necessary to add any cartilage for the alar rim in order to maintain the physiological function of the nostril.
As treated in other chapters, the frontal flap is the best choice to cover the nose partially or totally. It can be long enough to reach the floor of the nose, allowing total reconstruction without any tension, at the same time giving the opportunity to reconstruct the columella and inner lining. It is very important to ensure optimal vascularization and flap viability, preventing stenosis and allowing a sufficient passage of air.
It is necessary to carve the end of the flap as thin as possible to make the alar rim, and to fold more than a centimetre to make the inner lining. It is also important to remove all the hair follicles, without affecting the viability of the flap.
The most common complication is a lesion of the parietal pleura resulting in a pneumothorax. This kind of complication exceptionally requires a chest tube: a red rubber catheter under positive pressure is sufficient.
When the lesion is suspected to be wider and the decision is taken to put in drainage, the chest tube must be introduced between the 2nd and 3rd costal spaces at the level of the mid-axillary line. A 0.7cm incision is made, after which the introduction of the drain follows the superior edge of the rib as far as the pleural cavity. The tube must be strongly affixed to the skin and left in place for 24 hours. If possible, an X-ray should be taken prior to removal.
It is not the first choice in a humanitarian mission but can be very useful when the flaps we usually employ are not available.
Radial forearm flap
The radial forearm flap (see also Microsurgey chapter) is an important flap in the evolution of modern plastic and reconstructive surgery. It is also called the Chinese flap as it was first described by Song and Yang Guafon in 1978. It has become particularly important in microsurgery especially when a long pedicle is required. It is not the first choice in a humanitarian mission but can be very useful when the flaps we usually employ are not available.
The advantages of the radial forearm flap are:
• the use of thin skin which is easy to shape;
• versatility, which makes it suitable in combination with different kinds of flap;

• the simplicity of the dissection;
• the vascularization of the flap and the calibre of the vessels which allow anastomoses (various methods) without a microscope.
Disadvantage are the unaesthetic scar at donor site (particularly for women) and the sacrifice of the radial artery. It is recommended to avoid performing a bypass to the artery.

Anastomosis of superficial temporal artery and vein.



Termino-terminal with 8/0 separate stitches.
Radial forearm flap used in reconstruction of the nose.
The Washio flap is a retroauricular-temporal flap, vascularised by the retroauricular and superficial temporal nets. It is possible to include ear cartilage in this flap. It is seldom used in humanitarian missions, where the quantity of tissue is often important, but it could be considered for reconstruction of the alae, tip of the nose and columella. Disadvantages are the colour match and particularly the vascular risk.
Columella reconstruction
The columella is the strip of skin separating the nostrils, between the tip of the nose and the upper lip.


An infection starting at a superior incisor can easily spread upwards, damaging the superior lip and the columella. The degree of damage caused by an incisor infection depend on its intensity.
We present a case treated using bilateral cheek advancement flaps, together with upper medial and peri-alar skin flaps, to reconstruct the upper lip, columella and nasal base. This technique allows us to obtain sufficient tissue to reconstruct such a large defect with minimal cosmetic disfigurement.
Classification of columellar lesions
A) sub-dermal;
B) inferior or lateral partial necrosis;
C) total necrosis;
D) total necrosis including the tip of the nose;
E) total necrosis including the alar cartilage.
Columella lesion type E with alar cartilage envolvement.
A full thickness alar flap is raised after freeing it along the alarfacial groove.
Reconstruction of the columella
There are many methods of columellar reconstruction applicable and widely used in humanitarian missions. These include philtrum flap, mucosa flap from the nose (inter-alar cartilaginous) and frontal flap. Type A and B lesions can be treated with local flaps (e.g. naso-genian flap). For type C lesions there are several solutions: the alar edge of the nose, philtrum and internal nose mucosa, naso-facial flaps (inferior or superior), and free ear (helix) cartilage can be used. In class D and E it is necessary to use a forehead flap, converse flap or Washio flap (exceptionally), with or without cartilage support.




Nostril alar rim threshold flap
Of the many techniques available for reconstruction of the columella, one of the simplest is this one, which can be perform under local anaesthesia. A full thickness alar flap is raised after freeing it along the alar-facial groove. It is then rotated in order to reach the nasal tip where it is inserted. After 3 weeks we divide the flap, giving it the necessary length to reconstruct the columella and re-establish the ala. We have performed 11 such operations, sometimes under local anaesthesia with good results in every case.
Pre operative appearance. Type C columella lesion.
Appearance after first operation with alar nostril.
Appearance after second operation.
Final result.
Destruction of the columella happens quite frequently in cancrum oris. Infection of two incisors is sufficient to cause it: if the infection is light only the sub-dermal base of the columella and nostril base are affected. However, often four incisors infected, and frequently also a canine, this can lead to total necrosis of the columella and damage to the tip of the nose.

Four incisors infected, and frequently also a canine, this can lead to total necrosis of the columella.

Pre-reconstruction: lesion type C.
Alar nostril bar flap.
Final result.

The operating approach to reconstruct important columella infection, particularly lesion type C, D and E with lack of superior lip tissue is to reconstruct in two operating times.
The first one is to perform a naso-genian flap and alar fly.

Naso-genian, alar fly flaps and advancement flap
At one time the Tagliacozzi or free forearm flap was used but these procedure, and the Washio flap, are difficult to perform in humanitarian missions - however they could be usefully employed where other possibilities are unavailable.

Patient suffering infection of canine and 3 incisors


Draw of the bilateral nasogenian flap
Rise of the advancement and nasogenian flaps
Columella reconstruction with advancement/double flap and fly flap.
The columella can be reconstructed using: alar nostril base; alar edge; helix cartilage; converse flap; naso-genian flap; frontal flap; Washio, Tagliacozzi, forearm flaps, mucosa lip flap, philtrum flap, inter-alars mucosa flap (see also Nose Reconstruction, Lip Reconstruction and Cheek Reconstruction).


Pre reconstruction Appearance. Lesion type C with right lateral component.
Drawing of bi-lateral naso-genian flap.
Intra-operative appearance.

Final result.

Cancrum oris.
Infection at three incisors and left canine.
Pre recontruction appearance
Lesion type C.
Pre-operative picture showing lack of superior lip tissue.





Naso-genian and fly alar flaps.
Appearance after first operation.
Final result.
Double naso-genian flap
Pre-recontruction Columella lesion type C.
Pre operative appearance. Drawing a double nasogenian flap to reconstruct the floor of the nose.
Setting of the inner flap.
Setting of the outer flap.
Second operating time, double naso-genian flap to reconstruct the columella.
Final result.
Nasogenian flap on the facial artery is very useful in humanitarian surgery to reconstruct upper lip and support lateral columella reconstruction.





Pre reconstruction appearance.
Pre-operative view, lack of superior lip tissue. Lesion type D with classical medium partition.




Naso-genian flap, alar flap and advancement upper lip flap.



Alar ring flap.
Final appearance after recontruction.
Type D columella lesion. Cancrum oris. Infection of four incisors and right canine. Prereconstruction appearance. Appearance after first operation. reconstruction with nasogenian flap and fly alar flap.



Final result.

Alar edge rim flap
Pre-operative appearance. Cancrum oris infection of four incisors.






Appearance after first operating time. Bilateral naso-genian flap and fly flap.
Pre recontruction. Type C lesion.
Drawing of alar edge flap.
Alar edge flap bind.
Final appearance.
Free helix flap
Pre-operative appearance. Cncrum oris. patient with infection at four incisors. Columella lesion type C.





Lifting the helix flap.
Setting the free helix flap.
Final result.

Cheek Reconstruction
Most Noma patients suffer damage to the cheek, which can be partially or totally destroyed, as far as the border with the lips, nose, orbit and jaw. In these patients the infection started at a canine frequently, but the infection can also start at a molar, often associated with a canine and, exceptionally, at an external incisor (which is often associated with a canine). Sometimes the infection stays deep, damaging just the base of the nostril and weakening the anterior wall of the sinus. The gangrene could spread through the maxillary sinus (because of contiguity), and then easily damages, in sequence; mucosa, bone, muscles, sub-cutaneous tissue and skin.

When the infection starts at a canine then the lateral wall of the nose suffers lesions, as well as the inferior and medium turbinates. It is rare for the superior turbinate to be affected following infection from just a canine: this requires the involvement of at least one molar. Quite often the cheek and lateral wall of the nose are both damaged. The involvement of the cheek suggests that the infection began at a molar; however the involvement of the upper lip indicates that an incisor is also infected. When the gangrene spreads to the ascending branch of the mandible, it can reach the coronoid process, causing trismus: in these patients, molars are always involved.
Cancrum oris. Molar are heavily involved and canine and external Incisors are badly damaged.
When the infection starts at a canine then the lateral wall of the nose suffers lesions, as well as the inferior and medium turbinates and associated with molar, can damage seriously the cheek.
The body flaps most often employed are the latissimusdorsi and the deltopectoral.
It can be difficult to evaluate the size of the lesion before the release of the tissues. In fact flaps which at first seem big enough for reconstruction are sometimes insufficient to completely cover the lesion. One has also to consider that the need is usually greater inside than out. As the gangrene starts in the gum, spreading first through the mucosa before reaching the skin, often the amount of tissue destroyed is more important interiorly. However in few cases, Noma damages the muscles and skin more than the mucosa, therefore the resection of the secondary tissue may be greater, spreading through the soft tissue, the inferior edge of the maxilla, the orbit and the temporal region.
Surgical approach
There are many ways and flaps availables to reconstruct the cheek an other parts of the face. In Humanitarian usually employed cheek rotation flaps, forehead flaps, latissimus dorsi flaps, submandibular flaps and others developed in nose, lips and columella chapters. The submental flap was not employed in the past but has become very useful due to its flexibility and adaptability to reconstruct the lower part of the face, and there are always more indications for this flap. The body flaps most often employed are the latissimus-dorsi and the deltopectoral.
Using a latissimusdorsi flap we can obtain as much tissue as necessary to cover the lesion inside and out, support the orbit and close the palate, in one or at the most two interventions without bony graft support.
Free flaps are the last choice in humanitarian missions, but the indications for them can be expected to rise as more trained personnel become available to cope with them. The forearm flap is quite simple to dissect and provides thin skin with a large choice for drawing and shaping. It brings enough tissue to reconstruct the inside and outside, support the orbit and close the palate and lateral wall of the nose in just one intervention. (Division is performed 4 weeks later). The calibre of the vessels is good enough for it to be reliable and allow a wide choice of vascular anastomoses (see Nose Reconstruction and Microsurgery chapter). Free flaps are the last choice in humanitarian missions, but the indications for them can be expected to rise as more trained personal become available to cope with them.
Scar contraction and trismus are severe, therefore only after the release of the trismus and the debridement of the tissue can the surgeon accurately assess the true size of the defect and the amount of tissue required for reconstruction. Using a latissimus-dorsi flap we can obtain as much tissue as necessary to cover the lesion inside and out, support the orbit and close the palate, in one or at the most two, interventions. Other flaps such as frontal flaps, temporal fascia flaps and submental flaps can also be alternative choices, but sometimes do not provide enough tissue to completely cover the lesion so associated flaps may be necessary.
Another option is a prefabricated superficial temporal fascia flap to reach the corner of the mouth. It is quite thin and elastic, but carries a risk of severe retraction at the end of the healing process. We recommend shaping the skin pad for the reconstruction of the oral mucosa wide, even posteriorly, as after the release of the scar and resection of the necrotic tissue, the size of the defect is larger than expected and the tissue need is much greater than initially thought. If there is insufficient tissue, then mucosal shrinkage becomes an important concern. Post-operative contraction may occur especially when trismus coexists.
The deltopectoral flap
In humanitarian missions, the deltopectoral flap is very useful for reconstructing the inferior part of the face. We avoid free flaps as far as possible and a latissimus dorsi flap could be too heavy.

• is a useful surgical technique with several advantages: • it is reliable, bringing enough tissue to cover the defect;
• it is easy to raise; • it is associated with few complications; and • it gives an acceptable colour match.
However, it requires a skin graft to cover the donor area and at least two operations. The drawing of the flap is rectangular: the superior edge is parallel to the clavicle and the inferior edge 5cm lower, above the nipple over the pectoral muscle as far as the deltoid, then it follows a path to the delto-pectoral sulcus. The flap is between two points of low venous pressure, the neck and axillary region. The length of the flap is equal to the superior edge, and particularly in Africans the elasticity allows us to reach the cheek under the zygomatic area.
Cancrum oris. Molars are heavily involved and canine and external Incisors are badly damaged.




Pre operative appearance.
Lifting of deltopectoral and platysma flaps.
Reconstruction of inner lining using a platysma flap with skin palette.
Final appearance.
Platysma muscles

It often needs retouching to improve the shape but in combination with an inner flap could be an excellent choice.
The deltopectoral flap is an axial flap. Blood supply comes from the parasternal perforator vessels which have a suitable calibre. They arise from the internal mammary vessels at the1st, 2nd and 3rd intercostal spaces, and exit close to the external edge of the sternum, thus the length of the flap should not be more than 1.5cm further away. When the flap is raised, to prevent damage to the vascular pedicle, it is useful to place the fingers against the edge of the sternum. The fascia must be taken with the flap as the vessels are superficial to the fascia. The acromiothoracic artery must be ligated and care must be taken to avoid damaging it.
The deltopectoral flap can reach the cheek under the zygomatic bone, also the mastoid region, the ear, parotid area, chin and buccal commissure. However, it require a skin graft to cover the donor area, it so needs two operations

The donor area can be grafted simultaneously and the flap is divided after a minimum of 4 weeks. If the patient is malnourished, it could be one or two weeks more. For noma reconstructive surgery the deltopectoral flap could be better than a free flap or a latissimus-dorsi flap, which is sometimes too thick. The surgery is quick and easy to perform, the quantity and quality of tissue are sufficient and there is no muscle. But the disadvantage of the deltopectoral flap is that it requires a second operation.
For the corner of the mouth and surrounding cheek, another possibility is a sub-mandibular flap (see pag. 130).
For noma reconstructive surgery the deltopectoral flap could be better than a free flap or a latissimus-dorsi flap, which is sometimes too thick.
Intra-operative view of inner lining reconstruction with platysma skin/palate flap.
Inner lining reconstruction
Platysma flap and temporoparietal fascia flap are a alternative choice for reconstructing the buccal lining:
Platysma flap
One of the most useful flaps in humanitarian missions is the platysma flap, particularly for reconstruction of the buccal mucosa.

In the cheek lesion started at molars, the lesion of the buccal mucosa is often very wide. This flap, in combination with a delto pectoral flap to reconstruct the outer lining, could be the best choice.
Often in cancrum oris, the width of the skin palette required is more than originally thought, and it is necessary to draw the palette after freeing retracted tissues.
In infections arising from molars, the damage can extend above the zygomatic arch and destroy the inferior eyelid. The platysma flap has a large arc of rotation and can reach the superior part of the face. However, we normally employ this flap below the zygomatic arch.
The platysma flap has a large arc of rotation and can reach the superior part of the face. However, we normally employ this flap below the zygomatic arch.
Intra-operative view of the skin/ palate platysma flap setting.
The area of the skin included can reach dimensions of 6 -10 cm.
Platysma muscle - anatomy
The platysma is a superficial muscle directly connected to the skin (unlike most others muscles). It runs obliquely upward and medially, along the side of the neck. It starts at the level of the pectoral and deltoid muscles, at about the level of the second rib. It is attached to the inferior border of the mandible and the skin over the lower part of the face. The platysma muscle is innervated by the cervical branch of the facial nerve, or the cervical and mandibular branches of the facial nerve. Vascularization is from branches of the submental and suprascapular arteries.
Harvesting the platysma flap
After freeing tissue and measuring the size of the intraoral defect, the drawing of the flap is initially an ellipse, with the inferior margin above the clavicle. The area of skin included can reach dimensions of 6 - 10cm. The inferior incision is performed through the muscle and the superior incision just through the skin. The skin only is raised superiorly or laterally (Z) leaving the muscle with the skin island down. The flap is raised including the sternocleidomastoid fascia. The platysma musculocutaneous flap is rotated superiorly by 180° and fixed into the oral cavity. Special care must be taken to avoid twisting or stretching of the flap.
A tunnel must be built under the mandible skin and sub-cutaneous fat before the platysma flap is rotated.
Temporo-parietal fascia flap
Temporoparietal flap is a good choice to reconstruct a buccal lining defect.
This flap is performed in a two-step procedure. The first step consists in building it with a split-skin graft to the exposed fascia, and the second, five days later, in transferring the flap to the face and mouth, where the capacity for retraction is considerable. This flap should be moved under the zygomatic arch to reconstruct the buccal lining, and above it for reconstruction of central defects, such as the lining of the nose, the upper lip and pre-maxilla. The temporal fascia is just below the skin and subcutaneous fat, about 2mm – 3mm thick. Below it we find loose areolar tissue which covers the deep temporalis muscle, the temporalis muscle and the peri-cranium.
Advantages
• it is thin and supple;
• it produces the required shape;
• it has a good vascular supply and;
• can reach the buccal cavity easily.
Drawing of the deeper side lifting of temporomandibular flap.
A disadvantage is that it requires two operations: the prefabricated flap with split-skin graft applied to the temporoparietal fascia is transferred to the face after a period of 5 – 7 days. It is important to take into account significant contraction of the flap, and for this reason it is not our first choice.
This flap can be used to reconstruct a buccal lining defect after release of total or partial trismus and can also be used to correct defects of the maxillary sinus, nose, upper lip and premaxilla.

Surgical technique
The temporoparietal fascia lies under the skin and sub-cutaneous fat. It is quite thick (3mm) and is vascularised by the superficial temporal vessels which cross the zygomatic arch and can be easily palpated. The superior temporal vessels are divided into parietal and frontal branches crossing the superior limit of the helix. The temporoparietal fascia flap is vascularized from the parietal artery wich is draw using palpation and Doppler sonography.
The vein runs alongside the artery and superficially but at the upper pole of the ear it may take a different course and lie up to 3cm posterior to the artery.
It is also necessary to draw the path of the frontal branch of the facial nerve. It runs obliquely under the temporoparietal fascia, following a line from the lower point of the ear and the superior edge of the orbit, becoming superficial at the level of the zygomatic arch.
As usual any badly sited teeth are extracted, the mouth inspected and the degree of trismus is evaluated.
With the scalp shaved, we draw the superficial temporal artery, aided by Doppler ultrasonography. The incision is performed following the artery from the superior border of the helix up to the midline. The dissection to expose the temporoparietal fascia is performed by shaping a 10cm triangle whose side is the temporal region and whose centre is at the upper midline of the skull, starting from the top, avoiding hair follicles and taking care to preserve the small veins of the fat layer overlying the fascia.
Accurate haemostasis is essential. The middle temporal artery and vein lie superficially at the lower part of the triangle.
The split-skin graft with the same shape as the triangle is applied. A drain is set before closure of the flap, followed by bandaging with the correct pressure. After one week, which is necessary for the graft to take, we expose the graft surface which would be irregular in most cases. Sometimes a seroma develops.
Taking all necessary precautions to prevent damage to the vessels, the incision is extended downwards in the preauricular crease as far as the zygomatic arch. The dissection of the temporoparietal flap starts from the upper point of the skull and goes down to the zygomatic arch. The underlying pericranium and fascia temporalis allow a non-vascular dissection. The frontal vessels must be ligated at the anterior aspect of the flap. During dissection attention must be paid to the middle temporal artery which is on the superior edge of the zygomatic arch. Care must be taken to avoid the frontal nerve.
For the flap to reach the buccal cavity it is necessary to create a tunnel which can be done by making an excision of the deep temporal fascia below the zygomatic arch, or by removing the zygomatic arch by osteotomy (temporo muscle flap). Taking care that the pedicle is not stretched or twisted, with the help of a small tube we can reach the buccal cavity. The flap is unfolded and matched to the defect in the inner lining starting at the deepest point. The anterior part of the flap is sutured to the flap used to reconstruct the outer lining.
The incision is performed following the artery from the superior border of the helix up to the middle line.
For the flap to reach the buccal cavity it is necessary to create a tunnel which can be done by making an excision of the deep temporal fascia below the zygomatic arch.
Lesion resulting from infection at superior first molar and a canine.
Reconstruction of inner lining and outer layer using a double cheek flap.
Final result.
The upper edge must reach the supra-zygomatic area in order to prevent ectropion of the lower eyelid.
Cheek rotation flap
This flap is used for closure of small defects in the infra-orbital and nasolabial regions. It has a very good blood supply and gives excellent colour and texture matches. It could be extended behind the earlobe and to the neck (cervical flap), making sure the flap is large enough to reach the desired area, and rotation of the flap must provide enough tissue to close the defect. The reliability is quite high but the donor area might require a skin graft.
Surgical technique
Draw the triangular outline of the defect to be excised. The anterior edge of the cheek flap should be slightly bigger than the defect. The upper edge must reach the supra-zygomatic area in order to prevent ectropion of the lower eyelid. The dissection continues around and behind the earlobe and down into the neck. After ensuring that the flap is large enough to cover the defect, care must be taken during dissection to avoid the frontal nerve and a branch of the facial nerve. In most patients, mobilisation is required and the whole cheek should be mobilised. With the help of hooks, we check that the tissue is sufficient to close the defect without tension, particularly under the orbit, again to prevent ectropion. However, tension must be applied cranio-laterally of the orbit. In most patients, reconstruction of the lower eyelid with cartilage is also necessary.
This flap suffers from a high incidence of haematoma thus accurate haemostasis is mandatory. Post-operative haematoma causes necrosis of the flap.





Closure starts at the temporal region, from posterior towards the nose, trying to earn tissue in each stitch to facilitate the rotation. Finally, the pre-auricular scar is closed from top to bottom.
Before finishing, the tension and viability of the flap must be assessed and consideration given to the need for a skin graft to the pre-auricular area. As always for facial interventions, a Redon must be set.


This flap suffer from a high incidence of haematoma thus accurate haemostasis is mandatory.
Cheek lesion caused by infection originating at superior molars. Damaging seriously the maxillary sinus and the orbit floor.



Intra-operative view. Lifting of the flap
Positioning of skin flap.
Final appearance.
Latissimus dorsi flap
For Cancrum oris reconstruction, the availability of a good quality of soft tissue is preferable to performing bone reconstruction.
This is one of the most useful flaps in humanitarian missions. It is reliable because of the constant position of the pedicle and the diameters of the vessels and most importantly, it can be performed in one operation. It provides a large quantity of tissue and the skin adapts to reconstruct the mucosa. The availability of a good quality of soft tissue is preferable to performing bone reconstruction.
Reconstruction of the palette can be performed with the same palette used to reconstruct the cheek.
In African patients, using a pedicled latissimus dorsi flap, we think it is possible to get enough tissue to reconstruct until 2/3 of the face.

With the central point just under the armpit where the subscapular vessels arise, after cutting the tendon, the arc of rotation is sufficient to allow it to easily reach the face just under the orbit as well as the opposite side of the face.
This is a myocutaneous flap which can be performed either with a pedicle or as a free flap. It is recommended not to get closer than 5cm to the iliac crest. The blood supply network allows some skin to be brought forward to the anterior border of the muscle making it possible to get dimensions of 35cm x 25cm. Going too far back towards the vertebrae should be avoided because it carries a high risk of necrosis.
The vascularization arises from a dominant pedicle and another accessory segmentare. The dominant pedicle is the dorsal thoracic artery coming from the inferior scapular artery born from the axillary artery.
Cancrum oris patient, 46 years old. Infection of molars, canine and three incisors.


Drawing on the skin of three skin palettes.
Lifting the flap.
Intra-operative stage inner reconstruction after microsurgical anastomosis.


Immediate post-operative appearance.


Final appearance.

Lesion caused by infection of superior and inferior molars, inferior canine and inferior lateral incisor.


Reconstruction of the inner lining with pectoral skin flap palate. Skin graft.



Final appearance.

A few centimeters from its origin, the subscapular artery is divided in circumflex scapular artery (which supplies the subscapular muscle, the skin of the scapular and the parascapular flap) and the thoracodorsal artery (which get inside the latissimus dorsi muscle 6 cm-15 cm from its origin at the subscapular artery behind the anterior edge of the muscle. In most cases, the neuro-vascular pedicle is divided between an external pedicle following the anterior edge of the muscle for 1 cm – 4 cm posteriorly, and a internal pedicle which follows the superior edge of the muscle. Sometimes the pedicle is divided into 3 or 4 branches. In 9 cases out of 10, the subscapular artery and vein born at the same level of the axillary artery. Exceptionally, the artery arise more proximally and joins the vein at the level of the circumflex scapular vesseils, or even lower.
Rotation arch: the point of rotation is in the upper part of the axillary at the level of the sub-scapular vessels, in the region of the humeral tendon of the muscle. The rotation allows the flap to reach the inferior part off the face. In patients with short neck and long chest, the superior edge of the muscle can reach the temporal region. It is possible to make palettes up to 35 cm by 25 cm, but it is suggested not to closer 5cm from the iliac crest.
In patients with short neck and long chest, the superior edge of the muscle can reach the temporal region. It is possible to make palettes up to 35 cm by 25 cm.
Lesion caused by infection at all right site molars, canines and two incisors.



Positioning of the latissimus dorsi flap.
Final result.
Latissimus dorsi muscle
Latissimus dorsi flap: advanges:
• reliability; the pedicle contains of nerves and vessels which are consistently long and of large diameter;
• technical simplicity; it can be used with a pedicle or as a free flap;
• it requires only one operation and one operating position;
• it provides a large volume and quality of tissue, preferable to performing bone reconstruction;
• it has a very large arc of rotation;
• the skin is hairless;
• when the muscle is twisted it is possible to make a skin graft;
• reconstruction of the palette can be performed with the same palette used to reconstruct the cheek;
• a pedicle flap, is possible to get enough tissue to reconstruct more than a third of the inferior face.
Surgical Technique
The drawing must be done with the patient standing with hand on hip. This position makes it easier to feel the anterior edge of the muscle which is 3cm – 4cm forward in relation to where we feel. The origin of the subscapular pedicle at the bottom of the armpit must also be drawn. The shape of the flap must follow certain guidelines. If it is small, it must reach no further than 30cm from the armpit and be harvested at the same level of the muscle: if large it can be 40cm from the armpit and forward in relation to the muscle.
For the procedure the patient is laid with a support under the back to raise the side of the operation, with the arm in abduction to expose the axillary pit. The drawing is done on the skin pad following the anterior edge of the muscle.
The intervention starts with an incision from the bottom of the arm pit to the skin pad following the drawing of the anterior edge of the muscle.
The anterior border of the muscle is localised in the middle of the vertical line.
The muscle is dissected out, raising it and being careful with the pedicle which is about 2cm - 3cm from the edge.
A pedicled flap for reconstruction of the lower region of the face, the flap is tunneled under the pectoralis major.
The superior edge of the latissimus dorsi is identified at the inferior angle of the scapula and the serratus muscle is easily identified with this approach.
The latissimus dorsi is separated from the serratus. When lifting the flap from inferior to superior it is important not to dissect underneath the serratus muscle.
The muscle is detached from the last four ribs, going up following the pedicle as far as the axillary region and axillary vessels, paying attention to coagulation as this area can bleed profusely. Haemostasis is important, and all branches coming from the thoracic and scapular vessels are tied to give strength to the flap and enlarge the vessels. This is followed by dissection of the pad, bringing the pedicle with it, until reaching the tendon which is sectioned to leave the flap just under the vascular pedicle to give more mobility and increase the arc of rotation of the flap as it is often employed in humanitarian missions rather than free. If it is a pedicled flap for reconstruction of the lower region of the face, as is often necessary in humanitarian missions, the flap is tunneled under the pectoralis major, which must be freed widely to avoid any compression of the pedicle, particularly against the clavicle.

Infection of superior canine, three incisors and first molar.

After positioning of latissimus dorsi flap.
Finally, the nerve is cut, which allows more length and reduces the size of the flap, which is helpful in the final shaping of the face.
The donor region is bandaged with vaseline gauze, being grafted in a second operation. This flap provides sufficient tissue for reconstruction of the mucosa layer but it may be necessary to make a skin flap as well.


The flap is widely used in pedicle form due to its positive characteristics: reliability, quantity of tissue, quality of skin and length. In humanitarian missions it is employed in 90% of patients to reconstruct neck, chest, limbs and cheek. In some patients it is necessary to use the free flap version, which is easy due to the length of its pedicle (9cm - 12cm) and the large calibre of its blood vessels (2.5mm - 3.5mm on average) because in the conditions pertaining in hospitals in poorly developed countries, it is not easy to perform microsurgery.

There are no contra-indications for this flap, as these patients have never had radiotherapy which would damage the axillary vessels. The only disadvantage could be the heaviness of the flap, and the un-aesthetic scar in the donor region.
Moulding the latissimus dorsi flap to reconstruct the palette and cheek. A frontal flap is used to complete reconstruction of the lateral wall of the nose.
Final result.
The frontal flap is a reliable flap with good color match.
Classic Noma lesion resulting from infection originating at two incisors, a canine and a molar.
Use of frontal flap for reconstruction of inner lining and outer layer.
Frontal flap
Historically, the frontal flap Is the most useful flap employed for reconstruction of the nose (see Nose Reconstruction chapter), and occasionally the cheek. However, in the treatment of cancrum oris, it is often used to repair damage to the cheek, in most cases in combination with reconstruction of the lateral wall of the nose. Lesions starting from a canine result in damage to the lateral wall of the nose and maxillary sinus, and easily spread to the cheek: the damage to the cheek can be severe, especially when a molar is involved.




The frontal flap is a reliable flap with good colour match and its flexibility makes it easy to shape. It has the advantage that it heals by itself with a good quality of scar and without the need for a skin graft. It is suggested that the division be performed 3 weeks later, often with local anesthesia.
Positioning of the frontal flap.
Final result.
Lesion resulting from infection originating from at least one incisor, a canine and two molars.

The vascular anatomy is regular and constant in its topography and is based on the supraorbital and supra-trochlear arteries coming from deep down. These must be preserved by making a careful dissection under the base of the periosteum.


The flap is set over the medial line with a width of around 3cm – 4cm, allowing direct closure without the help of a skin graft or another flap. The quality of the medial frontal flap scar is always aesthetically good. It should not be too wide, allowing an easy rotation without damaging the vascular (supra-trochlear artery) support. The frontal flap has a very wide arc of rotation on the supra-trochlear artery. The vessels come from deep down and must be preserved making a careful dissection under the base of the periosteum.




The internal part of the inferior eyelid is reconstructed with the thicker part of the frontal flap which it is not possible to debulk. Sometimes this flap can be retracted.
Final appearance.
High lesion reaching 3rd turbinate.
Drawing of frontal flap.
Cheek flap, intraoperative use of cheek advancement flap.





Use of nasogenian flap for reconstruction of the inner lining.
Final result.
When the hairline is low an oblique forehead flap is indicated. The direction is toward the opposite hemifront (exceptionally to the same side). The great advantage of this flap is that it heal on its own leaving a very good quality of scar.
If the hairline is low, it should be oblique in order to get a greater fl ap length able to reach the nostril base and to reconstruct the columella.
It is possible to perform this fl ap through the midline but the vascularisation is then poor, and the tip of the fl ap can suffer. In bald patients the frontal fl ap can be drawn very large on the axis of the suprathroclear vessels, and can be used to reconstruct severe damage of the nose and cheek.
This fl ap is often used to reconstruct the middle of the face, often in conjunction with a naso-genian fl ap to rebuild the deep layer.
The indications for the frontal fl ap are numerous with different shapes (even if the risk of suffering is raise), especially in deeper necrosis which necessitates reconstruction of the inner lining. Patients with second molar involvement often present damage to the inferior eyelid, and the frontal fl ap could still have some surgical applications.
Another advantage of this fl ap, when it is long enough, is the possibility of doubling it over at the tip to reconstruct the inner layer. In some patients, the front of the fl ap is not high enough: then it is useful to make a skin graft on the deep side of the fl ap to reconstruct the internal part of the alar ring. Retraction is frequent with these fl aps, but they heal on their own without the need for skin grafts or other fl aps.
Before starting the dissection it is recommended to measure the length of the fl ap, trying to minimise the risk of pedicle retraction or cephalic tension on the tip of the nose (see Nose Reconstruction chapter).
The dissection of the upper part of the fl ap should not touch the muscle and galea, which are not included in the fl ap, going deeper under the periosteum in the lower part and avoiding damage to the pedicle. In patients with scars between the eyebrows, Doppler sonography is recommended, to check the location and viability of the vessels, knowing that the supra-trochlear artery is 2cm laterally from the midline. The blood vessels lie deep between the corrugator and frontalis muscles, becoming superfi cial in the distal part of the fl ap. The anatomy of the fl ap facilitates debulking, and the shape is optimal. Debulking may be performed a month later. When the frontal hairline is low the drawing of the fl ap should be oblique. Sometimes hairline cannot be avoided, it is essential to carefully remove hair follicles, especially in the more distal millimetres of the fl ap in order to reduce the risk of necrosis in this vital part. This is made possible because the fl ap has a good blood supply.
The fl ap is rotated through 180 0 and the donor site closed with excellent results. Secondary healing of the gap remaining under the hairline gives a better aesthetic result than a skin graft.
The pedicle is divided after three weeks and any excess tissue removed.
As noted above, when the hairline is low, or the nose defect is low, an oblique forehead fl ap is indicated. The direction is toward the opposite hemi-frontal (in a few cases it could be to the same side) in order to close the base of the nose and improve the healing of the upper donor side. If more tissue is required, then exceptionally a supplementary fl ap or skin graft will be necessary. The big advantage of this fl ap is that it heals on its own leaving a very good quality of scar.
The frontal fl ap is often used to reconstruct the middle of the face, often in conjunction with a nasogenian fl ap to rebuild the deep layer.
Patients with second molar involvement often present damage of the cheek and the inferior eyelid. Frontal flap could still have some surgical applications.
Sub mandibular and temporoparietal flap.
Submandibular flap.
Thanks to the Institute of Fer à Moulin - University Pierre et Marie Curie - Paris, for the research collaboration.
Submandibular flap

The submandibular flap has very good indications to reconstruct a defect under the zygomatic arch as it has a long arc of rotation and is easy to shape. We have not used it, but it will be more useful for future generations. It has the disadvantage of not being the easiest flap to carve. Special attention to the vascularisation is needed, haemostasis is important too, and another problem could be the scar under the edge of the mandible which can remain in tension, particularly in Africans who are prone to develop keloids.
This is a reliable flap based on the submental artery arising from the facial artery which meanders until it reaches the digastric muscle. It gives a good colour match and the scar is hidden under the border of the mandible. The flap is drawn just under the edge of the mandible from angle to angle. With the patient in a supine position, and using an index finger/thumb pinch test, the anterior limit of the flap is drawn to give a primary closure of about 4cm (5cm - 6cm in older patients).

The flap can be raised from the lower margin after an anatomical dissection of the sub-mental subcutaneous and muscular tissues and pedicle on the sub-mental or the facial pedicle. Alternatively, it can be started from the superior margin up to the platysma muscle. In order to protect the submandibular nerve, the digastric muscle is sectioned. The mandibular gland is identified and the dissection performed close to it. The artery and vein usually lie superiorly inside the gland fascia, which is dissected away from the gland. The artery is divided into branches. The vein is dissected from proximal to distal, together with the artery which runs interiorly to it.
The edge of the mandible is exposed, taking care with the submandibular nerve, which is often close to the facial artery. For nerve detection it is sensible to use a nerve stimulator.
The digastric muscle lies in the midline and the anterior belly is divided. Behind it the mylohyoid muscle can be seen and it is also divided in the midline. The mandible is palpated at the superior and deep aspect of the flap. The dissection continues with the division of the flap away from the mandible, the platysma, digastric and mylohyoid muscles. At this point the flap is free, with a huge arc of rotation which can reach the middle of the face as far as the zygomatic arch and pre-auricular region. The donor site is closed in layers by advancement of skin from the inferior neck. Then the flap is transposed through an incision or a subcutaneous tunnel avoiding any tension. The flap reconstructs the outer lining of the cheek. When a temporal fascia flap is also used, the sub-mandibular flap lies on top of it, leaving drainage between both sides. This flap has increasing surgical indications but particular attention must be paid to possible retraction of the inner lining. A considerable skin graft is required after reconstruction and special care is required after reduction of trismus.
Some of the most useful flaps, the submental flap, may need to be performed in conjunction with a prefabricated superficial temporoparietal fascia flap for reconstruction of the buccal lining. This is very easy to perform as it is thin and supple and can reach the middle of the face. It is necessary to build the flap as large as possible, knowing that there will be retraction.
Lip Reconstruction
Introduction
There are two main points to consider in lip reconstruction in African patients: on one hand, the extend of the necrosis and on the other, the large mucocutaneous area in these subjects. in cancrum oris lesions of both lips, together with damage at the corners of the mouth, are quite frequent. In these cases, the infection originated on at least one or two incisors and a canine and - rarely - the first molar. In some patients only one lip is damaged together with the commissure. In these patients the lesions started at incisors, often in combination with a canine, but only on one side, either superior or inferior.


When the cheek as well as the upper lip is involved, the corner of the mouth, and sometimes the lower lip, are also damaged. We observe that in these cases, the infection originated in at least the last incisor and a canine and often a molar. In those cases where the lips and adjacent cheek are involved it is extremely rare to see the development of severe trismus, but trismus of Class I or Class II (rarely) is a possibility. As one of the most frequent consequences of the disease is salivary incontinence due to damage to the lip, particularly the inferior one, the goal of the reconstruction is obviously to improve retention, particularly of liquids, and aesthetic appearance. This becomes harder when an improvement to the mouth opening is also required.
In nearly all these patients we use flaps from around the mouth, the opposite lip, cheek and/or chin. It is necessary to leave cicatricial skin around the buccal area in order to reduce the size of the flap. We also leave cicatricial tissue in the mouth, in order to fix the mucosa. Skin shrinking against the mucosa could be helpful to reconstruct deeper layers. The principles applying to lip reconstruction in Cancrum oris are modified relatively to those in caucasian trauma or tumours. This makes reconstruction easier, with a lower risk of suffering and necrosis, giving a better match of skin colour and does not compromise other regions of the body. The flaps most often used to reconstruct lips are the Estlander flap, naso-genian flap (double or on a facial artery pedicle), Abbe flap, Western flap, fan flaps (Gilles flap, McGregor flap, Karapandzic flap), commissuroplasty flap, step-stair flap and scalp flap.
If the defect is large and requires a lot of tissue, then platysma flap, delto pectoral flap and neck flap are employed. In humanitarian missions it is recommended to avoid free flaps unless there is no other option.
In these patients the lesions started at incisors, often in combination with a canine.
Drawing of the naso-genian Flap. This flap can be up to 10 cm long and 3 cm wide, and provide tissue which is easy to shape. With a low risk of failure due to its good vascular supply and performing branches.
Infection at four superior incisors. Drawing of nasogenian flaps on the facial artery to reconstruct the superior lip.


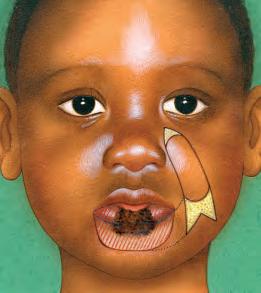
Intra operative carving of both flaps.
Positioning one of the flaps to reconstruct the inner lining.
Result after positioning of both flaps and alar fly.
Naso-genian flap
This flap first employed by surgeons in the 19th Century regained popularity in the 1960s. Tissue fom the paranasal area are transferred to reconstruct the lateral wall, septum, whole dorsum and inner layer of the nose often in combination with other flaps (see Nose Reconstruction chapter). we often employed naso-genian flap to reconstruct lips. in the absence of hair can also be used to reconstruct the inner layers of the lips. This flap can be up to 10 cm long and 3 cm wide, and provide tissue wich is easy to shape. With a low risk of failure due to its good vascular supply and perforaiting branches, it is particularly useful in humanitarian missions. When the mucosa is destroyed, this flap, with an inferior pedicle, can be very useful.

The width should be equal to the hight of the superior white lip to be reconstruct. It must be carved inside the naso-genian fold for the cutaneous pad, so in male patients care must be taken to avoid area with hair.
One of the advantage of this flap is that when there is a need for limited quality of skin and subcutaneous tissue for reconstruction of the lip and nose, it can be on subcutaneous or arterial pedicle. Subcutaneous flaps are particularly useful for reconstructing the lateral nasal wall or alar ring and are ideal for reconstruct the inner lining of the nose, but their use for lip reconstruction is very limited. On the other hand, when the flap is based on the arterial pedicle, become one of the most frequently employed flaps in lip reconstruction. We often included the facial artery in the pedicle to reconstruct the inner and outer lining of the lip (picture under) or just the inner lining (patient next page). The length of the pedicle should be more than the distance from its base to the recipient area, and in order to reach this attention must be paid to the point of rotation.

To reconstruct white lip with conservation of the red lip, the width should be equal to the height of the superior white lip to be reconstruct. It must be carved inside the naso-genian fold for the cutaneous pad. In male patients, care must be taken to avoid areas with hair. The flap must be drawn over the naso-genian fold and medially. Ginestet described a naso-genian flap for the reconstruction of the whole thickness of the superior lip. It is carved from both sides of the naso-genian fold and has an inferior pedicle taken the whole thickness. A double cutaneous naso-genian flap with an inferior pedicle can be used to reconstruct the inner and outer layers.
Cancrum oris: appearance four weeks after an infection at four inferior incisors and both canines.



Toilette.
A pedicle naso-genian flap is very useful for the reconstruction of the inferior lip, particularly the mucosa of the inner lining, wich is easily damage: a severe infection could damage all the layers.
The length of the pedicle should be more than the distance from its base to the recipient area, and in order to reach this attention must be paid to the point of rotation .
Drawing of nasogenian flap to reconstruct the inferior lip.
Naso-genian flap on the facial artery used to reconstruct inner lining.



Use the Neck flap to reconstruct the inner lining.
Appearance before commissuroplasty.

Reconstruction of total destruction of the inferior lip.




Neck rotation flap.
Pedicle Latissimus dorsi flap.
Reconstruction of inferior lip after severe infection, resulting of important damage of it, is the most challenging situation in plastic surgery. The goal of the reconstruction is to improve retention, particularly of liquids.
Estlander flap
The Estlander flap was first described in 1872. Estlander said the flap does not have a base tied to the lip, just enough for its vascularization.
Is the most commonly employed flap in Noma patients, the Estlander flap is quite similar to the Abbe flap. It is used for reconstruction of the commissure, so the pedicle becomes the new corner of the mouth. It has a great advantage over the Abbe flap because it is completed in just one operation. In many cases it is performed in conjunction with other advancement flaps.
It is absolutely reliable, gives a very good colour match and the skin is pliable. On the other hand, donor morbidity is sometimes important, requiring a second operating time in a few cases.
When there is a lesion affecting one lip, the other one could be slightly fibrotic and the commissure involved becoming Eslander indication. In this kind of lesion canines are always involved.

The incision is facilitated by finger compression and started from the non-pedicle side. It is strongly suggested to go from anterior through all layers until reaching the artery, avoiding dissection around the artery.
The first step is to release fibrotic tissue around the mouth, and from the upper and lower lips, cheek and chin.

The flap is drawn in the shape of a “V” or “W” on the lower lip) and should be wide enough to compensate for the defect between the upper and lower lips. We have a tendency to make this flap bigger than necessary. It is suggested to make smaller flap than the remaining lip. The sutures of the donor side pull the commissure down, especially if it is a wide flap. However, care must be taken to reduce the risk of microstomia by not making it too wide, even if it is necessary to reconstruct the whole area.

Drawing of the Estlander Flap.
The pedicle become the new corner of the mouth .
Cancrum oris: infection of an inferior molar, a canine and two incisors.
Reconstruction with Estlander flap.
Noma. Infection of 2 superior incisors, a canine and first molar.
Estlander W flap used to reconstruct the inner and outer layers.
Cancrum oris: Infection of molars, with mild infection of a canine and and external incisor.



Appearance after reconstruction with Estlander flap.
Care must also be taken because the coronary artery is close to the labial mucosa.

We have a tendency to make this flap bigger than necessary. It is suggested to make a smaller flap than the remaining lip.

The sutures of the donor side pull the commissure down, especially if it is a wide flap.

Self portrait by a patient before and after surgery.

Result.
Cancrum oris infection at an inferior canine and two incisors.





Drawing of the flap and freely of the inferior lip.
Reconstruction with Estlander flap.
Intra operative lifting of Estlander flap. Setting of the flap.
The tendency is to make this flap bigger than necessary. It is suggested to make a smaller flap than the remaining lip.
The Estlander flap becomes the most desirable approach for reconstructing the superficial and inner layers coming from the opposite side lip, V or W (inferior) shaped flap.
Cancrum oris. Infection of superior molar a canine and two incisors. Intra-operative appearance of the Estlander flap with additional tissue mandatory to reconstruct all layers. Result.
Estlander flap is sometimes performed with others flaps able to provide more tissue for reconstruction, particularly of the corner of the mouth and cheek. It is used to bring tissue to cover damage to the opposite lip in cases where the commissure is preserved. In these patients the lesion started in 90% at canine, which is the commonest origin of Noma infections. When the damage to the lip is severe, the involvement of 2 or 3 incisors is indicated.



These infections can easily spread deep inside to the floor of the maxillary sinus, and follow a path as far as the 3th turbinate, and even reach point 0.
If the lesion becomes superficial, the lateral wall of the nose is damaged.
When the canine infection remains low, it can spread posteriorly to the anterior palette, or anteriorly and superficially, resulting in necrosis of all the layers of the lip: if the commissure is undamaged, then the Estlander flap could be the best choice for reconstruction.
The Estlander flap becomes the most desirable approach for reconstructing the superficial and inner layers coming from the opposite side lip, V or W (inferior) shaped flap.
When the lesion affects more than 60 % of the lip, the Estlander flap can sometimes be used in combination with other flaps: an advancement flap from the contralateral side is very useful.
Contraction of the lip occurs after 6 months, and it is suggested that a commissuroplasty be performed a minimum of one year post procedure.
Surgical technique
Evaluate the need to extract any badly positioned teeth which are no longer useful as it is difficult to correct their direction and they may damage the flap. When there is a necrosis of less than half of the inferior lip, without conservation of the commissure (fibrotic) it is necessary to make an Eslander flap higher than we anticipated.
We first consider the less damaged lip, which will be the donor side.
Take the lip firmly between the fingers before injecting saline solution with adrenalin, taking particular care to avoid the pedicle. Then wait a few minutes to achieve maximum vasoconstriction and reduce bleeding.
During the coagulation time, particular care must be taken of the coronary artery, which is between the muscle and the mucosa.
The release of fibrotic tissue around the mouth and from the upper and lower lips, cheek and chin facilitates the reconstruction, giving the maximum elasticity, which reduces the size of the defect considerably, and allows us to evaluate the need for other advancement flaps.
The rotation of the flap allows evaluation of the exact amount of tissue recovered, which will inform the need to perform an additional flap.
Closure starts from inside in three layers, taking care with the sutures of the mucosa which can cause problems of retraction.
The Estlander flap can produce a rounded angle at the corner of the mouth and also microstomia, so patients quite often need commissuroplasty to correct both these defects.

Cancrum oris.
Infection of the first superior molar, a canine and three incisors.
Post operative appearance.

Advancement
flap to complete reconstruction of the lip and alar ring.

Reconstruction of the corner of the mouth.

The rotation of the flap allows evaluation of the exact amount of tissue recovered, which will inform the need to perform an additional flap.





In the superior lip, the coronary artery passes trough the muscle and runs between the deep muscular layer and the muscle until the middle, and is set around 10mm from the free edge of the superior lip at a level between the humid red lip and the the dry lip. In the inferior lip, it runs 5mm - 15mm from the edge of the flap, in 44% of patients there is a T- junction coming from the facial artery which is the submental artery.
Cancrum oris. Infection of two superior incisors, and canine.


Result. Cancrum oris. Infection of three superior incisors and a canine.
Post operative appearance after W Estlander flap reconstruction of inner and outer layers.


Infection of superior canine and two incisors.

Drawing of a W inferior Estlander flap. Intra-operative appearance. W inferior Estlander flap to reconstruct inner and outer layers. Result.
Cancrum oris. Strong infection of canine and two incisors, provoking important damage of the maxillary sinus, inferior turbinate and lateral wall of the nose.




Reconstruction of inner and outer layers with Estlander flap. Final appearance.

The lips of African people are more voluminous than other races: the white lip is larger and the red lip is fleshier and has additional tissues reserves, providing a large reservoir of cutaneous mucosa that can be used for reconstruction. The elasticity of their skin allows to obtain a large advancement flap with just a cutaneous resection.



Cancrum oris: infection of an inferior canine and three incisors.
Reconstruction with the Estlander flap and advancement flap of the superior lip. Final appearance.
When there is a necrosis of less than half of the inferior lip, without conservation of the commissure (fibrotic) it is necessary or make an Eslander flap higher than we anticipated.











Abbe flap
This is one of the most useful flaps in lip reconstruction, as there are a lot of lesions that damage just one lip without damaging the corner of the mouth. It is an all layers flap.
When the lesion of the lip is large (more than 40% of the lip) it is not enough to release tissues around the nose, lip and cheek, but it becomes necessary to bring a mass of tissue from the other lip –the release of the adjacent muscles, skin and mucosa is also helpful. The Abbe flap is extremely reliable, with a good colour match. It gives a good quality for shaping and results in less donor morbidity than any other flap.
The surgical indication for the Abbe flap is when the defect of the lip is large enough to be difficult to manage with the remaining lip tissues, even when releasing each side and advancing them towards the midline.


In the Abbe flap, nutrition is provided through a feeding tube. This aspect makes it difficult to perform this flap in very young patients.
Abbe-Burgett flap
For an aesthetic reconstruction of the lateral part of the superior lip, Burgett proposed a flap, which is an Abbé flap with the exact dimensions of the damage area. In the Abbe-Burgett flap, the scar in the donor area can be hidden in the crease of the chin, this can not be achieved when the flap is longer.
The Abbe - Burgett flap has a very few indications in Cancrum Oris patients due to the risk of bad scars on the donor side. Could just be make on the lateral lesion of the superior lip.As it is the only indication for lateral lesion of the superior lip could be employed in humanitarian missions. Such localised damage is unusual in cancrum oris: more often the lesion is widespread, reaching the maxillary sinus and lateral wall of the nose, requiring more tissue to cover it.
But it could be used for severe but limited lesions resulting from infection at a canine and an external incisor.
Surgical Technique
The first step is to draw the flap, ensuring that the width is about 60% of the defect to be covered. A knowledge of the elasticity of African skin is helpful in mobilising and getting the centre of the lesion on the donor side. The defect will be smaller after the release of the lateral part of the lip and cheek: for this reason the first step is to dissect all the tissues retracted. When the donor side is the upper lip, the shape of the flap is a “V”: if the inferior lip, it could be either a “V” or a “W”. The length of the flap must be the same as the length of the lesion, taking care to respect, if possible, the mental groove which is often in the path of the scar. Avoiding the nasolabial line in the upper lip is easier to manage.
The width of the flap should be at least 50% of the width of the defect, but not more than 35% of the width of the lip on the donor side.
Drawing of the Abbe Flap.
Drawing of the Abbe-Burgett Flap.
The Abbe flap is extremely reliable, with a good colour match.
Can be use for severe but limited lesions resulting from infection at a canine and external incisor.
When the lesion of the lip is more than 40%, it is not enough to release tissues, but become necessary to bring a mass of tissue from the opposite lip.





Infection of the superior canine and two incisors.
Carving a Abbe flap.
Reconstruction of the inferior lip in three layers.
Reconstruction of the superior lip paying particular attention to the mucosa boundary.
Post operative appearance.
The height of the flap should be the same as the height of the defect and if necessary its length can be increased on the lower lip by lengthening the lateral extension to the chin.
Vascularisation of the lip is via the coronary artery which is just posterior, closer to the labial mucosa. The anatomical position of the artery allows us to control and work with it, with little risk of damaging it.
The patient should be positioned with the neck in hyper-extension, compressing the lip with the fingers to accentuate the area. An injection of saline containing adrenalin is given (avoiding the pedicle), then we wait a few minutes to achieve the maximum vasoconstriction and reduce bleeding. The incision, which is facilitated by finger compression, is started on the non-pedicle side, paying attention to the coagulation of the coronary artery between the muscle and mucosa. For this reason it is better to go from the anterior through all the layers until reaching the artery rather than finding it with protective tissue all around, and remembering to make a small incision at the vermilion-skin line.
On the pedicle side of the flap the incision is made about 3mm - 4mm inside the vermilion. Immediately, the skin-vermilion junction is marked to place it accurately at the recipient site, as the vermilion-skin line between the donor and recipient sites must be perfect.
It is strongly suggested that no dissection is done close to the pedicle.
When the flap is ready, checking that there is no bleeding, it is rotated to the other lip to cover the defect, taking care to avoid a possible compression or twist of the pedicle. Fixation starts by suturing the donor side in three layers, taking care not to damage the artery and making sure the skinvermilion line is perfect. Before closure on the recipient side it is sometimes necessary to make accurate measurements to ensure tissue advancement, incising the mucosa along the buccal sulcus.
Care must be taken to obtain the correct quantity of tissue, paying attention to the pedicle and monitoring the colour of the flap. Stitching is done in three layers, starting from the deepest point, from the inside to the skin.
In order to free and slide more tissue it could be helpful to make a small incision around a nostril, excising the necessary tissue to slide and making closure easier. With the same frame of mind, and with the aim of taking more mucosa from the maxilla, performing an incision on the upper buccal sulcus is the best way to reduce tension and increase the likelihood of good healing.
Concentration at the end of the procedure and during the first postoperative hours is critical for the fate of the pedicle, which can become cyanotic, making it necessary to review the compression of the pedicle and the necessity of releasing some stitches.
Patients sometimes have difficulties with breathing and it is very important to check the permeability of the superior respiratory airway from nose to bronchi regularly to keep it free. Regular cleaning by the nurses is very important.
Feeding must be strictly liquid via a straw, avoiding any solid food. Division of the pedicle is usually performed after two or three weeks, but earlier in some patients, depending on the condition of the flap and the post-operative management, as some patients suffer greatly and are unable to cope with the closed mouth necessary to maintain the flap in good condition.
The length of the flap must be the same as the length of the lesion.
On the pedicle side of the flap the incision is made about 3mm - 4mm inside the vermilion.
Fixation starts by suturing the donor side in three layers, taking care not to damage the artery and making sure the skinvermilion line is perfect.
Patients sometimes have difficulties with breathing; respiratory airways must keep free.
Drawing of a Webster Flap. Great advantage of this flap is that it avoids making the lip higher than desirable.
Cancrum oris: infection of four superior incisors. Reconstruction with a Webster flap. Next operating time, to set (lower) the alar and shape the nostril.
Webster flap
This flap is simple to realise and is one of the most useful to reconstruct loss of tissue from the upper lip. Has the advantage to be quick to perform and does not leave an additional scar. Disadvantage are that the philtrum disappears, and superior lip is flat in appearance.
Indication: for a smaller lesions less than 1/3 of the superior lip laterally Another possibility is to combine two Webster flaps and one medial Abbe flap, could be performed when the lesion is medial and more than 2/3 of the superior lip, avoiding an upward positioning of the lip. It is strongly suggested in the large loss of tissue a large resection peri-alar and sub-alar to lower the hight of the lip.
The Abbe flap from the lower lip is shaped so as to make the scars the external edge of the philtrum .
A cutaneous incision is performed peri-alar with a mucosal lining of 3mm at the back of the gum-labial sulcus.



To avoid an upward positioning of the lip by performing a triangular resection it is suggested to build a rectangular resection, which could be superficial or transfixiant. To allow the flap to move medially a resection is made around the nostrils. The philtrum is often twisted, but the great advantage of this flap is that it avoids making the lip higher than desirable.
When there is a large loss of tissue it is suggested to perform a double Webster flap, with two flaps and resections around the nostril (see drawing). In this case the upper lip becomes shortened and the philtrum disappears.
The advantage of the Webster flap are that is simple and quick to perform, and does not leave an additional scar. Disadvantage are that the philtrum and the superior lip is flat in appearance
Fan flaps
The fan flaps are Gilles, Karapandzic and McGregor, which have been developed to reconstruct the lower lip. To treat a huge loss of tissue from the lower lip, big resections are performed and these flaps are widely used. The flaps employed for reconstruction in oncology and burn cases can become useful in Cancrum oris Reconstruction.
If the lesion is very large the choice could be bilateral flaps. In most of these reconstructions microstomia could be severe and detrimental to the result. In most patients with a lower lip infection, necrosis damages all the layers: vermilion, mucosa, muscle and skin. In these cases, the infection started in the gum at two or three incisors, quite often also one of the canines, and sometimes both.
As the gangrene of the lower lip can easily destroy the entire length of it, often causing necrosis or at the least, important retraction, there is nothing more challenging for a surgeon than the problem of rebuilding it, where there is never enough tissue to avoid leakage. If the commissure is conserved, then in cases where half the lip is affected we can use a Gilles or Karapandzic flap: if three quarters of the lip is damaged a Camille Bernard flap is indicated.
Indication for fan flaps:
Inferior lip: • lateral lesion between 1/2 and 3/4 of the lip, Gillies and Karapandzic flaps
• medial lesion more than 3/4 of the lip; two Karapandzic flaps
Superior lip: • lateral lesion between 1/3 and 2/3 of the lip; a unilateral fan flap

• medial lesion more 2/3 of the lip ; two Gillies flaps
• para-medial or lateral lesions more than 2/3 of the lip; a unilateral fan flap
Gillies flap
This flap is indicated for patients with great laxity of the skin, such as Africans, and is useful for reconstruction of the lower lip when the lesion is around 40% - 50%. If bigger than this (up to 70%) a bilateral flap could be a good solution. This flap can be used in Noma patients where the commissure and the superior coronary artery are not involved in the lesion. In these cases, there is almost invariably a cuff of vermilion on both sides allowing a better reconstruction of the lower lip. The flap follows a rotation bringing tissue towards the centre of the lower lip, at the same time the commissure moves too, with the risk of microstomia. Another disadvantage of this flap is the lack of innervation.
Vascularization of this flap is from both coronary artery, the width of the flap taken from the opposite lip must be equal to half of the lesion. The Z pasty allows for easy sliding and flap rotation. The Gillies flap can be performed without damage to the neurovascular pedicle
In most patients with lower lip infection, necrosis damages all the layers.
In cases where half of the lip is affected
we can use Gilles or Karapandzic flap; if three quarters of the lip is damage a Camille Bernard flap is indicated.
Drawing of a Gilles Flap.
The centre of the flap, which when rotated forms the corner of the mouth, goes up to the nasolabial fold and is rotated following the fibres of the orbicularis oris muscle.
It is important to bring enough tissue to avoid leakage of saliva.
Surgical technique
The flap must be drawn (see figure) noting that the width should be greater than the height of the defect. We always recommend extraction of any teeth liable to damage the overlying flap. The centre of the flap, which when rotated forms the corner of the mouth, goes up to the naso-labial fold and is rotated following the fibres of the orbicularis oris muscle. Then turn down towards the upper lip and 3mm – 4mm into the vermilion. Saline solution plus adrenalin is injected, taking care to avoid the pedicle, and compression applied for a few minutes to allow the injection to take effect. Start resection of the lesion, taking all the layers, going up to the naso-labial fold and back to the vermilion, raising the entire flap. Release all the tissues in retraction especially the mucosa and take the flap to the centre of the lesion, after taking measurements especially in relation to the opposite lip stump. Closure is from top to bottom and deep to superficial in three layers. The vessels are not exposed. It is important to bring enough tissue to avoid leakage of saliva due to drooping of the lower lip. An important disadvantage of this flap is denervation leading to loss of muscle function and consequent lack of lip retention with speech problems and salivary incontinence. As noted previously, microstomia can also be a complication, especially when the defect is larger than 60% of the lip. The defect created at the donor site is reconstructed by sliding tissue from the cheek.
Karapandzic flap
Drawing of a Karapandzic Flap.
This flap is indicated for reconstruction of a large (70%) central lip defect when enough vermilion remains to make advancement of the tissue possible. The main difference between this flap and others is that no back-cut is made. The incision is to the skin only, following the nasolabial fold, with some muscle fibres being moved without cutting them. This approach allows preservation of nerves and blood vessels, so mouth function is undamaged. Muscle contraction is normal with a very low risk of incontinence, which is a more frequent complication with other flaps. Like other flaps it gives a good colour match and the skin quality is such that it is easy to mould. It is a reliable flap with low risk of necrosis due to its good blood supply, but there may be a high level of donor morbidity. For a lower lip reconstruction, we can perform two flaps around the buccal commissure. When the flap is dissected we must ensure the preservation of the nerves and vessels of the lateral part and the buccal commissure.

Surgical technique
It is necessary to extract any badly positioned teeth which could damage the flap. Drawing starts by evaluating the length of the defect and determining the amount of tissue required. The incision of the upper lip should not reach the wing or ala of the nose but stop below it. Then from the cheek on each side, using the buccal commissure as a reference point, if possible draw a circular line inside the nasolabial fold and following the direction of the fibres of the orbicularis oris muscle, stopping about 1cm before the alar commissure.
The first step, after injecting adrenalin solution and waiting a few minutes, is to release all tissue – mucosa contracture, scar, skin retraction – to free the tissues and allow them to slide. As noted before, during lifting of the flap care must be taken not to damage the muscle and vessels, and particularly nerves. Just the mucosa could be detached in the lower part of the defect when necessary to lift the flap medially.
As usual the flap is closed in three layers from inside to outside. If the lesion is large, the experience of the surgeon is required to reduce the degree of inevitable microstomia. As no back-cut is made, the tissue does not slide very easily, so sometimes not enough of it is available – this problem is often solved with a bilateral flap. As the innervation of the orbicular oris muscle is preserved, the capacity for contraction is retained. This property is essential for reconstructing a competent lower lip.
McGregor fan flap
The main advantage of this flap is that it rotates around the corner of the mouth as a pivot point. So the corner of the mouth remains in its original position avoiding microstomia as much as possible. The pedicle is the same as for the Gilles flap so it is based on the vessels of the upper lip and is quite narrow. The main disadvantage is the lack of vermilion but hopefully the remaining tissue can be used to reconstruct this.
As with other fan flaps it is used for large defects (more than 60%) and could be bilateral if necessary. It is reliable with a good colour match but can suffer from a high degree of donor morbidity.
This flap is indicated for older African patients as they have more elasticity of the skin.
Surgical technique
The first step is to measure the extent of the defect to be repaired. The width of the defect gives the length of the flap from the corner of the mouth (picture). The flap is drawn with the base a little more than the height of the defect. The length should be the length of the defect plus the distance of the defect from the corner of the mouth.

Injection of saline plus adrenalin is followed by compression for a few minutes to allow the injection to take effect. Proceed to free the lips from any retraction until maximum mobility is achieved, eliminating all scars from skin and mucosa. The mucosa section must be slid to the skin section in order to allow the mucosa to reach a level sufficient for reconstruction of the red lip.
Raise the flap following the lines, cutting the tissue from the skin to the mucosa. Pay careful attention to the pedicle area to avoid damaging the vessels within 3mm of the vermilion. Fixation starts with reconstruction of the vermilion to ensure correct positioning of the other parts of the flap. Closure is from inside to outside layers and from top to bottom of the cheek.
When the maxilla is lost, speech defects and nasal regurgitation may result.
As no backcut is made, the tissue does not slide very easily. so sometimes not enough of it is available - this problem is often solved with a bilateral flap.
Drawing of a McGregor Flap.
The length should be the length of the defect plus the distance of the defect from the corner of the mouth.
Cancrum oris.
Infection of three inferiors incisors.

Result after reconstruction with Z flaps in three layers.
Drawing of a Camille Bernard Flap.
Camille Bernard flap
The Camille Bernard flap can be a good choice in humanitarian missions for reconstruction of the inferior lip.


The whole inferior lip can be reconstructed with a bilateral transfixing advancement flap of the jaws. The advancement is made by the excision or two triangles which can be positioned in the naso-genian groove or even more internally. The mucosa must be sectioned over the cutaneous section.
Excess mucosa is hemmed over the two advancement fl aps. Whenever possible, it is suggested to make the incision in the crease of the chin, as this gives a better aesthetic result. Modifi cation made by Webster, which is strongly recommend .

Infection of four inferior incisors, damaging all the layers.



Reconstruction with double cheek advancement flap. The incision in the crease of the chin in order to give a better aesthetic result.
Post-operative appearance.
Cancrum oris. Infection of three inferiors incisors. Important lesion of all layers.


Result after reconstruction with Z flaps.
If the infection is localised at one or two incisors, damage to the inferior lip may be limited to shrinkage of the mucosa. The cul-de-sac where the inferior lip joins the chin is thin so the infection can cause local damage to all the layers: in these patients, an advancement flap used without changing the direction of the muscle fibres could be sufficient to produce a continent lip. However, when exacerbated by infection at a canine, it can result in complete necrosis of the entire lip.


Cancrum oris. Infection at superior canine and two incisors.
Reconstruction with superior lip advancement flap.
Cancrum oris. Infection of first superior molar, canine and three incisors.
Result after reconstruction with superior lip advancement flap.



Cancrum oris. Infection of a canine and two incisors.

Reconstruction with advancement flap and fly alar ring.
FAMM (Facial Artery Muscolomucosal Flap)
This is useful fl ap in humanitarian missions. It is based on the facial artery which lie in the deep aspect of the Platysma and above the buccinator muscle. It can be draw with a superior or inferior base and can be up to 8 cm in length and 0.5 cm thick. The facial artery remains in the deeper aspect of the flap after sliding the mucosa and part of the buccinator muscle. This flap is useful in reconstruction of oro-nasal, palatine, alveolar, septal and lip defects.

Commissuroplasty
One of the commonest complications in lip reconstruction, particularly with the use of fan flaps is microstomia and loss of shape of the commissure. When this happens, commissurotomy is necessary.
The rounded corner of the mouth presents a great challenge to surgeons attempting to resolve problems whilst preserving its function and aesthetic properties.
It is suggested to wait six months after lip reconstruction before performing commissuroplasty.



The orbicularis oris muscle is divided and slid down the frontal plane and both flaps are fixed in the external position.
Surgical technique
The drawing is a triangle based on the corner of the mouth, paying attention to the length and shape of the opposite side before intubation. We make an external cutaneous incision. The orbicularis oris muscle is divided and slid down the frontal plane and both flaps are fixed in the external position. One asymmetric Z-plasty is used to reconstruct the buccal commissure. The first step is to excise skin and underlying tissue to deep inside the oral mucosa. This is followed by an incision of the vermilion and mucosa. Both lip flaps are then slid to the corner of the mouth if possible: if they fail to reach it the vermilion is reconstructed using advancement of the mucosa. We use a triangular flap for the corner of the mouth and lifting the mucosa for upper and lower lip.



Trismus
One of the commonest handicaps suffered by Noma patients (in around 50% of cases) is Trismus, or inability to open the mouth. Trismus can occur with or without tissue necrosis. The risk of ankylosis in the temporomandibular articulation is much higher when the lesion is further back. Lesions resulting from molar infections are liable to damage the articulation. Trismus sets in rapidly, just a few days after the start of cicatrisation. Trismus develops due to muscular scar retraction after destruction of the cheek mucosa or/and by secondary ossification. It is a pathogenesis which is quite difficult to manage.
It can be classified as follows:
1 Almost normal aperture of the mouth; slight fibrosis;
2 Difficulty opening the mouth (>50% aperture); medium fibrosis;
3 Great difficulty opening the mouth (< 50% aperture); severe fibrosis; 4 Ankylosis.

Cancrum oris. Ankylosis Infection of four molars and two canines.
Wound contraction and bony fusion between the superior maxilla and the mandible can lead to mouth aperture stricture, in some cases resulting in complete closure of the lips. The scar tissue restricts jaw movement, becoming a great challenge for surgeons. If the contraction is controlled, reconstruction should be easier.

The healing of Noma lesions is characterised by fibrous scars that outwardly reduce the cutaneous defect may lead to definitive stricture of the mouth.
Classification of Trismus in relationship to capacity of buccal aperture and fibrosis
T1 > 40 mmslight fibrosis
T2 20 mm up to 40 mmmoderate fibrosis
T3 5 mm until 20 mmsevere fibrosis
T4 until 5 mmankylosis
Trismus pathogenesis
Cancrum oris causes gangrene and pain. In most cases necrosis leads to varying degrees of fibrosis. Taken together these factors impair the muscular function due to ipsilateral or bilateral myostatic contracture leading to partial trismus, and sometimes to the hypertrophy of the coronoid process. Fibrosis and wound contraction are associated with destruction of the temporomandibular joint, bony bridge formation and extra-articular bony ankylosis. Trismus itself can lead to extra-articular fibrotic ankylosis with bony bridge formation. Even the temporomandibular joint destruction (which is not frequent) can easily lead to ankylosis.
The healing of Noma lesions is characterised by fibrous scars that outwardly reduce the cutaneous defect may lead to definitive stricture of the mouth.
Infection at molars is always present in patients suffering trismus.
Infection at molars is always seen in trismus, as it can easily spread to the temporomandibular articulation, damaging it and causing severe shrinkage of the mucosa. In some cases, a molar infection can progress through all the layers, reaching the skin without affecting the articulation, but damaging the masticatory muscles. When severe trismus or ankylosis are present, often four molars are involved, resulting internally in damage to the postero-lateral and superior walls of the maxillary sinus, the 3rd turbinate, lateroposterior palate and floor of the orbit and external damage to the inferior eyelid it can cause loss of sight. During the healing process, severe fibrosis and muscle retraction develop, even on the opposite side, with consequent aggravation of the trismus. When associated with a canine, the infection can severely damage the lateral wall of the nose and the inferointernal wall of the maxillary sinus.
As general rule the surgery should never be performed within 6 months from the onset of the infection. In Noma patients, it may be necessary to wait a full year, as malnourished patients can require several months’ preparation. In fact any minor surgery,,should be avoided before the major procedure is undertaken because it might hesitate in fibrosis and tissue damage. The only exception is when sequelae prevent adequate nutrition.
It is essential that an expert surgical team does an extensive evaluation,
which include photographs, and a report indicating the procedures and techniques to be employed.
The evaluation should include clinical conditions such as weight and comorbidities, and when possible, X-ray and magnetic resonance scanning to better assess the amounts of bone and soft tissue involved, the condition of the teeth and the capacity of the mouth to open.
Surgery is normally performed under general anaesthesia, rarely using local anaesthesia. When intubation becomes difficult we prefer nasal fibrotic use rather than tracheotomy (see Anaesthesia chapter).
In some patients the first step is to excise the hypertrophic coronoid process of the mandible together with the damaged part of horizontal bone in order to release the constriction.
Trismus severely affects the life of the patient and represents a big challenge for surgeons. Quite often the temporomandibular articulation is damaged, making anatomical reconstruction complicated and very difficult to achieve. We try to obtain as much freedom of the joint as possible, creating conditions able to avoid the recurrence of lack of mobility in future (40% at one year, 20% at 5 years).
The muscles involved in the opening of the mouth are lateral pterygoid, digastric and mylohyoid muscles, whilst those involved in the closing of the mouth are masseter, medial and temporal pterygoid. In Noma, fibrosis of the temporomandibular joint and stretching of soft tissues of the face such as skin, facial muscles and mucosa play an important role in determining the degree of trismus.
The degree of trismus also depends on severity of the initial infection, coexistence of gangrene, and wound healing process Cancrum oris damages the normal opening of the mouth in the months or years between the onset of the disease and the time of surgery. If gangrene has caused a large retraction of the soft tissues, then healing will result in contracture and fibrosis, with associated damage to the temporomandibular joint. This prevents tissues from stretching to allow the opening of the mouth. When the gangrene spreads laterally across the face other complications occur. The mouth muscles commonly become fibrotic preventing the opening of the mouth. Even the healthy muscles site on the opposite side of the infection, develop a permanent contracture due to the lack of stretching (myostatic contracture).
We observe that the temporal muscle is sensitive to inflammation becoming fibrotic in the lower part (the upper part is rarely involved), sometimes with a myostatic contracture on the contra-lateral side, where the infection is not present. This is painful, especially in the first weeks, and some authors remove the contralateral mandibular coronoid process in order to release the temporal muscle.
In some cases, the infection ends in the articulation itself, and this results in complete trismus. The syndrome is termed fibrotic extra-articular ankylosis and is a consequence of fibrosis, wound contraction and myostatic contracture. When the infection damages the facial bones they can easily develop a condition known as bony bridge. These bridges can come from the coronoid process down to the mandible, to the zygomatic arch, the maxilla and the base of the skull. This is called bony extra-articular ankylosis and is frequent in Noma patients with complete trismus.
Even the healthy muscles site on the opposite side of the infection, develop a permanent contracture due to the lack of stretching (myostatic contracture).
If gangrene has caused a large retraction of the soft tissues, then healing will result in contracture and fibrosis, with associated damage to the temporomandibular joint.
Sometimes ankylosis damage the temporomandibular joint itself, which is called intra-articular ankylosis. In these patients the approach would be extra-articular with a long follow-up time in order to achieve a better result. This procedure can not be performed routinely in humanitarian as even a month spent in the clinic after the operation is not enough to improve the pathology. Therefore the children who suffer severe trismus for a long time may achieve a good level of mouth opening.

In the future the functional recovery of the temporomandibular joint will be frequent in most patients the articulation remains in good condition regardless of the destruction due to the infection and gangrene. Even when patients suffer severe gangrene and develop a bony bridge it does not interfere with the normal function.
















In cases where the temporomandibular joint is not involved we can correct trismus. However, mandibular mobility may be compromise by another bony deformity called hypertrophy of the coronoid process.
The partial trismus and fibrotic ankylosis stage is characterised by scar development, wound contracture and fibrosis of all facial tissue – mucosa, muscles and skin – and sometimes by myostatic contracture of the masticatory muscles, skin and mucosa. In the next stage, when ankylosis sets, there is hypertrophy of the coronoid process, which damages the zygoma and causes malfunction of the maxillary articulation.
As we said, the presence of bony bridges between the mandible and facial skeleton is quite common in extra-articular ankylosis. In the very last stage, destruction of the temporomandibular joint severely damages the articulation until ankylosis sets in. We have to bear in mind the living conditions of people in areas where Noma is prevalent - lack of water and electricity, scarcity of food, extreme heat, poor roads, very few phones or other means of communication the lack of infrastructure and medical facilities such as kinesiology and radiology - all of which make reconstruction more difficult. Moreover very often a single mother raising 5 to 10 children, is unable to cope effectively to a child with a chronic disease. Taken together these conditions are not conducive to treatment, especially post-operative.
Mouth Aperture Measurement
This is typically taken between the upper and lower incisors, but in Noma patients the distortion of the anatomy, and of the teeth, especially of the canines and incisors, may make the measurement difficult. Therefore is a good rule to remove the teeth in the operating theatre prior to reconstruction, then taking two points on the maxilla and mandible to measure the aperture with the mouth open as far as possible.
Inability to open the mouth is not just a surgical matter but causes problems for anaesthesia too because laryngoscopy and endotracheal intubation are difficult if the aperture is less than 20mm (see anesthesia chapter). On the other hand, gangrene may create a huge space in the cheek which can sometimes be used to avoid a tracheotomy. These issues are dealt with in more detail in the chapter of anaesthesia.
Many circumstances must be taken into account before operating for mouth opening, particularly with very young patients. who may baulk at the prospect of a lengthy and painful physiotherapy. For these reasons sometimes it is suggested to postpone the surgery until they are older.
As previously mentioned we prefer to operate in their own countries. We are usually able to cope quite well with problems of infrastructure, hospitals, theatres and therapy, although on rare occasions (perhaps one in 1000) it is necessary to take the patient abroad. The advantages of operating locally (see Psychology chapter) include:
Avoiding the stress of expatriation and repatriation.
It’s much cheaper.
The family are present and can support the hospital staff, especially the nurses.
Mandibular mobility may be compromise by another bony deformity called hypertrophy of the coronoid process. The presence of bony bridges between the mandible and facial skeleton is quite common in extra-articular ankylosis.
Is a good rule to remove the teeth in the operating theatre prior to reconstruction, then taking two points on the maxilla and mandible to measure the aperture with the mouth open as far as possible.
Patients suffering severe trismus and ankylosis often have micrognathia, and are prone to intra-oral pathologies.


Cancrum oris. Lesion from infection orginating at four molars and two canines results in ankylosis.

Pre-operative appearance.
Ankylosis. after resection of necrotic tissue.
Trismus: surgical indications
Although extensive surgical procedures for the treatment of the sequelae of Noma, especially trismus, were described in the first half of the 20th century it is only in the last 20 years the surgery has improved patients suffering severe trismus and ankylosis often have micrognathia, and are prone to intra-oral pathologies like caries (necessitating extraction prior to surgery), periodontal disease and abscesses which have to be treated before surgery
Good hygienic conditions of the entire buccal cavity are essential for good post-operative prognosis and results.
Latissimus dorsi flap: drawing of two palettes for reconstruction inner and outer latissimus dorsi defect.
Trismus: surgical approach and technique
In our experience some of the patients operated on suffered from severe ankylosis. The mouth aperture was about 2mm – 3mm, and there were significant bony bridges between mandible, maxilla, base of the skull and zygoma. Intra-articular deformity of the temporomandibular joint was observed, with at least 35% - 40% of the bones destroyed on the affected side of the face. Nasal intubation was preferred.
In patients with trismus the first step is the asportation of scars,necrotic tissue and bony bridge. The second step is the removal of a large amount of hard tissue and dentition.
Osteotomy of the maxilla is performed including the sinus and lateral wall of the nose. In some cases, the malar bone is also removed. The ipsilateral coronoid process and the contralateral coronoid process are released when possible. Extra-articular ankylosis and intra-articular deformity of the temporomandibular joint are both common.
As the masseter muscle plays an important role in constriction, any remaining fibres have to be freed to allow complete release of the mandible.
Condylectomy is a last resort because the intra-articular intervention may cause fibrosis and lack of mobility in future. The vascularisation in the areas being operated on, is a diffuse net with no large vessels, therefore the bleeding is fairly easy to control with compression or with the normal technique of haemostasis for bone with “rubber.” It is common to see bleeding from hidden areas which again can be stopped with compression.
In patients with trismus the first step is the asportation of scars,necrotic tissue and bony bridge.
Condylectomy is a last resort because the intra-articular intervention may cause fibrosis and lack of mobility

Lifting of latissimus dorsi flap.






Constant good vessels caliber size in latissimus dorsi flap.
Pre and post surgery appearance.



In countries where blood is often contaminated with malaria, HIV and hepatitis, we try to avoid transfusions when possible. When it is necessary, as it may be in big reconstructions, we try to inform patients of the risks, and take as much care as we can to avoid them.
Results and complications of surgery
Trismus relief achieved after surgery can be 75% of patients at 3 months, at 40% at 1 year and at 20% of cases at 5 years.
To understand the reasons why the improvement is less than expected we have to try to address the following questions:
Was the reconstruction of mucosa completed?
Was a retraction of soft tissues present?
Has bone resection been used?
Were there bony bridges or damage to the coronoid process?
Was a vascularised flap, sufficiently to reduce or prevent infection and avoid scar formation?
Was secondary retraction related to lack of physiotherapy and/or lack of movement of the mandible?
When the ipsilateral flaps are used in patients with high risk of trismus should we give more importance to the conditions of the contra-lateral coronoid process?
Is the risk of retraction with skin graft flaps,possible only when trismus is present?
In the context of conditions in humanitarian, what is the best approach to keep the mouth open for the first week post-operation? Wooden spatulas?
Should the mandible be exercised several times daily for at least two months? Or is external fixation of the contralateral side necessary?
Painkillers are administered continuously for several weeks; is oral administration sufficient? Is there a risk of dependence?
Would it be possible and ethical to put patients, especially children, under deep sedation for some weeks in order to maintain an open mouth?
Post-operative management is hard even in western countries in which the rehabilitation centres have the most sophisticated and modern technologies.
In a country lacking infrastructure, and with patients coming from desert areas, rehabilitation remains a huge problem which need to be addressed. In fact good rehabilitation may lead to a better outcome.
Trismus relief achieved after surgery can be 75% of patients at 3 months, at 40% at 1 year and at 20% of cases at 5 years.
In a country lacking infrastructure, rehabilitation remain a huge problem. Improving it may lade to a better outcome.

Microsurgery
The field of microsurgery has been responsible for the most important advances reconstructive surgery has seen in the last 30 years, applying to an increasing percentage of patients. It is now an indispensable part of the whole specialty of reconstruction. It can be very useful in the humanitarian field and when the indications are absolutely positive it can be performed. The main reason for not doing it is not lack of infrastructure (which can be a problem), but the difficulties entailed in the follow-up.
On the other hand, transferring patients abroad, is not always practical or desirable due to the cost and psychological effects (see chapter “Psychology”, effects related to treatment abroad). Sometimes microsurgery is the only way to solve technical problems during humanitarian missions although its application in this context remains challenging. The learning process in microsurgery requires time and the surgeon’s skills play a pivotal role in getting optimal results. In addition to general medical problems, he/ she may have to manage unexpected surgical complications involving the chest or abdomen.
Therefore the attending surgeon needs considerable knowledge of general medicine, haemodynamics, cardiology and local endemic diseases, particularly infectious ones.
A good surgeon is one able to solve medical and surgical complications over and above the basic procedure - this quality is mandatory.
Termino-terminal anastomosis. Needles 8/0.

Termino-lateral anastomosis. Monofilament 8/0.
It is exactly fifty years since Rene Favaloro performed the first coronary artery bypass operation. This opened a new and very important chapter in the history of medicine and microsurgery.
When the face is reconstructed in children, every single factor must be considered in obsessive detail. However, improving hospital hygiene, room conditions and intensive care facilities remain the first step.
It is exactly fifty years since Rene Favaloro performed the first coronary artery bypass operation. This opened a new and very important chapter in the history of medicine and microsurgery, saving millions of lives. Today, the procedure accounts for 30% of all cardiac surgery. Originally using a great saphenous vein, and later an internal mammary artery, attention must be paid to haemodynamic rules, tension, ejection fraction, and high and low debit areas.
For microsurgery rules, bypasses are not always the best solutions, but do offer alternatives for solving problems of vascular flow.

Strategies
Sometimes repairing the defect requires more than one surgical procedure. An option is to perform two flaps in one operation. Often there are different strategies to treat the same defect and an accurate evaluation of the patient must be done prior to surgery. For example, the nose would be reconstructed after the upper lip or pre-maxilla as it is necessary to prepare the mucosa beforehand. In recent years, huge advances have been made in the field of microsurgery, resulting in better outcomes. In summary, the aim of the surgery is to perform as few operations as possible, reducing risks, (especially of necrosis), and giving priority to functional problems. However, the surgery should also try to achieve good colour match and a satisfactory aesthetic result.
The nose can suffer inner lining lesions due to infections spreading from the incisors or canines, or both. The lesions can be localised or widespread,
involving underlying structures and tissues such as the underneath of the nostril, alar rim, columella, sinus and lip. When the defect is under the skin at the base of the nose, filling the damage with a nasogenian flap or other local flap could be sufficient. But in patients where the damage to the nose spreads to the outer wall, it is necessary to rebuild the inner lining prior to reconstructing the superficial layers. The surgical approach requires local flaps around the nose called turnover flaps. The flaps must be wide enough and short with an opposite flap to help the closure.
A single short flap, often used with an opposite flap or other local flap, is usually enough to reconstruct the inner lining. As the underlying tissues of the scar are well vascularised, the flaps must be thick to supply both skin and mucosa.
Another way to reconstruct the inner lining is with a superficial flap end which could be doubled over or twisted. Yet another method is to reconstruct the lower part of the inner lining with a nasogenian flap and a septal mucosa dissection in the upper part.

It is recommended to wait until the tissues of the inner lining are consolidated before beginning the superficial reconstruction. Vascularisation must be checked carefully until the end of the procedure in order to avoid necrosis or infection which may reduce the capacity of the airway.
Termino-lateral anastomosis. Needles 8/0.
Termino-terminal
anastomosis with 9/0 needles.

Intervention
If possible the surgery is performed using two teams. The first team performs the dissection to isolate the recipient vessels, and the second team is responsible for the removal of the flap. If only one team is available, the first stage is to verify the condition of the recipient vessels and determine accurately the points where anastomoses will be made.
Once the flap is removed, it is immersed in a heparinized saline solution (1 litre of physiological serum for four 25000 IU heparin vials - 5ml) and the vessels are irrigated with this solution by cannula. The flap is secured by two stitches to prevent excessive tension on the pedicle and prevent its accidental removal.
It is essential to be comfortable and well-prepared before starting to perform microsurgical sutures as the entire procedure lasts many hours.
When using the microscope, its setting must be perfectly adjusted before starting the intervention especially if you have not previously used the equipment. The eyepieces must be aligned and focused precisely to achieve perfect, sharp vision. Even a small error of focus is enough to trigger headaches, compromise the 3D vision and cause fatigue.
Microsurgical sutures may be end-to-end or side-to-end, carried by sutures and/or overcasting (for veins). The anastomoses could be termino-lateral or termino-terminal performed with separate sutures or surjet sutures (veins).
After the flap is re-vascularized, it is necessary to keep it warm by covering the area with a dressing impregnated with tepid physiological serum (saline solution).
Skin closure must take place without undue tension, with a non-aspirative drain. Drains or drainage tubes are placed under the flap at a distance from the anastomoses. If a drain is aspirative, it must be fixed at a distance from the pedicle in order to avoid the aspiration of vessels. The dressing should be non-compressive including a window for clinical monitoring.

Medical treatment includes effective analgesia, normal blood pressure, normovolemic haemodilution with a haematocrit target of 30%, and prevention of hypothermia.
The majority of patients undergoing free flap surgery require anticoagulation treatment with low molecular weight heparin (LMWH) post-operatively to prevent thrombosis in the lower limbs.
Latissimus dorsi flap: advantages are the length of the pedicle (9 to 12 cm) and the large calibre of its blood vessels (2.5 to 3.5) average.
Radial forearm flap: the axis is drawn on the radial artery linking the middle of the elbow to the groove of the pulse.

Radial forearm flap
This is an important flap in the evolution of modern plastic and reconstructive surgery. It is also called the Chinese flap as it was first described by Song and Yang Guafon in 1978.
The flap has become particularly important in hand surgery and microsurgery especially when a long pedicle is required. It is not the first choice in a humanitarian mission but can be very useful when the flaps we usually employ are not available. The radial artery is an external branch of the humeral artery, running from the middle of the elbow/forearm sulcus and following a line to the wrist channel. Before proceeding it is necessary to verify the vascularisation of the hand using the Allen Test. The flap is drawn over the radial artery and we can take the whole forearm flap skin with it, just leaving a stub on the cubital side. The advantages of this flap are: the skin is thin and easy to shape, it is possible to use it to make different kinds of flap, the dissection is straightforward, it is well vascularised and the vessels are quite big for performing anastomoses (various methods) without a microscope. The disadvantages are that the donor site is not aesthetically very pleasing (particularly important for women) and the sacrifi ce of the radial artery - it is recommended to avoid performing a bypass to the artery.
The dissection start at the proximal side to isolate the communicant vein between the superficial and deep venous systems in order to see the origin of the radial artery.

There are many ways to harvest the flap. The method usually suggested is to start the dissection at the proximal side to isolate the communicant vein between the superficial and deep venous systems in order to see the origin of the radial artery. This is followed by:
• Dissection of the radial pedicle on the distal side of the drawing through a longitudinal incision.
• Incision of the edge of the cutaneous pad as far as the brachial aponeurosis, being careful of the peritendon in view of the skin graft.
• Dissection from the ulnar edge to the radial artery taking skin and aponeurosis, paying attention to the medial nerve and finishing radially over the flexor carpi.


• Dissection of the radial side as far as the artery and the tendon of the RB.
• Dissection of the complete system – skin, artery and septal/cutaneous tissue – together, from proximal to distal. The dissection is started between the tendons (FCR and BR) which are separated to allow dissection of each side of the inter-tendinous septum. Haemostasis must be performed at each branch of a vessel and particularly in the proximal part which is more highly vascularised. The proximal dissection is performed as far as the origin of the radial artery.
Twisting of the radial forearm flap.
Radial forearm flap. Two of the most important advantages are long pedicle and facility for shaping. Particularly for nose recostruction.
Anastomosis of superficial temporal artery and vein.

Before cutting the artery it is necessary to verify the viability of the flap and the hand. Some colleagues perform a bypass to re-establish continuity of the radial artery.
Finally the donor site is covered with a skin graft (total or thin) and immobilised for a couple of weeks, including the wrist.
Alternatives to microsurgery
Our current aim is to perform microsurgery in the African hospitals leaving the follow up to a well-trained staff. New techniques sometimes allow us to reconstruct without microsurgery whilst achieving similar results.
The approach to facial reconstruction in Noma patients has to meet the following criteria:
• It should require preferably one, maximum two, operations;
• The procedure(s) should be easy to perform;
• There should be a low risk of bleeding;
the flap used should:
• be reliable;
• carry a low risk of morbidity;
• be flexible enough to mould; and
• give a good colour match.
For a skilled, experienced surgeon, flaps around the mouth should be straightforward – Abbe, Estlander, Karapandzic and cheek rotation flaps. The forehead flap is not difficult but requires more attention as it is often employed in combination with other flaps.
The sub-mental flap is also useful to reconstruct as far as the temporal region but too often it requires the support of other flaps, increasing the risk.
The temporoparietal fascia flap requires a skin flap, making it a more challenging procedure.
Body flaps, such as the delto-pectoral flap, are easy procedures. On the contrary, more experience is essential to perform the pedicle latissimus dorsi flap, especially when it is large.
All the flaps around the mouth (Abbe, Estlander, fan flaps) have the following advantages:
• High reliability
• Excellent colour match
• Great elasticity of thin skin
• Low morbidity
Estlander, fan and cheek rotation flaps can be performed in just one operation while the Abbe flap requires at least two procedures. All these flaps carry a risk of blood loss. The forehead flap has similar advantages in terms of reliability and good colour match, but the skin is not as pliable. Also, when it is lateral there is a slightly higher risk of donor morbidity. The sub-mental flap is a good choice for cheek reconstruction, although sometimes the colour match is not perfect, and donor morbidity can lead to development of a bad scar, even if it is situated under the mandibular border. The superficial temporal fascia flap is another option with the disadvantage of two operations.
The deltopectoral flap is easy to perform but the disadvantages are that it requires two operations, the skin is not highly pliable and, as with most body flaps, the colour may be darker than desired. The dorsal flap is challenging from the surgical point of view, demanding considerable skill on the part of the surgeon, but with this caveat it is reliable. The disadvantages are low skin pliability for the face, the colour match and the need for two operations.
Post-operative care
The responsibility of the surgeon continues after surgery and up to discharge from hospital. Even when the colleagues and nurses that the patient is handed over to are well-trained, the period of post-operative care can present problems, particularly in Africa, and it is important to ensure that all necessary equipment is available in case it is required.
In the ward, the surgeon must pay attention to the bandaging in order to maintain the correct pressure on the pedicle and skin, checking for any change of position, and keep an eye on drainage and wound healing. As we have performed paediatric procedures requiring very organised postoperative care, in an intensive care unit with specially trained nurses, for many years now, we are in a good position to give instructions on these procedures, and on the importance for healing of the correct body temperature.
We now have a well-organized team in which everyone is able to administer the prescribed therapies.
An intensive care unit (ICU) is essential for the post-operative treatment of patients undergoing reconstructive surgery, as serious lifethreatening complications may occur at any time during the hospital stay.
Among other complications, major bleeding, emergency tracheotomy if intubation cannot be performed and respiratory failure with hypoxia, are all reasons for recovery in an ICU. Moreover, in an ICU, surgeons, anaesthesiologists and nurses can be trained to manage the more common complications. General wards also need a well trained staff. Nurses closely monitoring the patients are able to promptly recognise the onset of complications requiring an emergency procedure in the operating theatre. Africa is becoming more and more developed - trained staff and organised wards, operating theatres and intensive care units are now more readily available.
Flap monitoring
An operating theatre with a specialist surgical and paramedical team should be available 24 hours a day as a quick revision may be needed in case of doubts on the viability of the flap. Flaps must be closely monitored for the first 72 hours, then the risk of vascular thrombosis decreases significantly. During the first post-operative hours, the viability of the flap is monitored every one or two hours, using standardized post-operative protocols and specially trained nursing staff (including night shifts). After ten days the risk of failure is negligible therefore the patients usually leave the hospital after 3-10 days.
Clinical monitoring involves checking the colour and temperature of skin or muscle, capillary filling time and analysis of the flow and colour of a directed bleeding. Occlusion of the artery of the flap is associated with skin pallour, lower temperature and longer capillary refill/recolouration time –more than 2 seconds. Occlusion of the vein induces a bluish skin colour with decreased capillary refill time, and dark blue bleeding from the flap edges. Continuous bleeding of the flap is an excellent indication of venous thrombosis. When the skin is deeply pigmented, the capillary refill is not evaluable unless the epidermis from a small area of skin (2-3 mm2) is removed. Regularly scrubbing with gauzes soaked with saline has to be used to remove clots and to check bleeding and the colour of the dermis. In case of doubt, a prick test with a 20 - 25 gauge needle can differentiate a viable flap (in which bleeding is bright red) from a flap with venous congestion (in which bleeding is dark and prolonged).
Muscular flaps must be percussed in search of a stretch reflex indicating tissue vitality.
Unfortunately, the clinical parameters described above are subjective, poorly reproducible (due to lighting conditions or room temperature) and not detectable in the case of a buried flap. In this situation, the removal of a palette of skin located directly above the muscle, or a palette vascularized by a collateral artery of the main pedicle of the flap - which is then called chimeric or composite - allows indirect monitoring of its vitality.
The best alternative is the use by the surgeon of a portable Doppler machine at the patient’s bedside, but this technique requires specialised training, and an optimal alignment of the probe with the flow of the artery supplying the flap. Also analysis of the signal from the vascularisation site is difficult (Disa 1999).
Marking the site of the vessels with a felt-tip pen helps the nursing team to closely monitor the Doppler, especially during the night shift.
The role of the anaesthetist is extremely important, and especially in cases of trismus, intubation can be challenging. Direct laryngoscopy is not always practical and fibre-optic intubation or blind intubation are the only ways to gain access to the airway. Therefore, a well-trained anaesthetist is an important member of the surgical team.
High pressure ventilation is not widely used during facial reconstruction, and tracheotomy is a last resort due to the high rate of post-operative complications. Another concern is surgical bleeding occurring during dissection of the neck vessels. Blood supply can be an issue due to a shortage of safe and compatible red blood cell packs, although it is not like cardiac surgery where blood may be essential at any moment. Finding blood which is of the correct group and safe is not always possible, but fortunately transfusions are rarely needed. However good progress is being made in getting the necessary transfusion quickly and safely.
Microsurgery Instruments
In microsurgery, an operating microscope is essential, but for many procedures, binocular glasses are a small, cheap and easy to store alternative. With a magnification of 2.5, they allow the preparation of recipient arteries and veins, and at 4.5 magnification provide sufficient enlargement to perform anastomoses on small vessels. Moreover, with binocular glasses a surgeon can perform anastomoses with sutures of 8/0 (latissimus dorsi flap, radial forearm or Chinese flap).
However, in the case of anastomoses on perforated vessels or collateral digital arteries, the microscope is mandatory.
Microsurgical instruments are few and can be stored in a small box. They include:
• scissors;
• forceps;
• needle holders;
• metal or plastic disposable clamps.
These instruments are fragile and expensive and require special care when cleaning and packing.
The materials for anastomoses consist of very fine needles (8/0 to 12/0) and monofilament. One must have the basic instrumentation for vascular surgery – Satinsky vascular clamps, bulldog clamps and vascular lakes.
Microclips allow fine vessels to be clamped quickly. As an alternative or in awkward conditions, fine monofilament sutures (5/0, 6/0) can be used.
Portable ecodoppler, one of the most useful instruments in microsurgery.

In difficult conditions the minimum equipment consists of:
• binocular glasses with 4.5 magnification;
• two boxes of microsurgical instruments (a second set of instruments must be sterilized and ready in case it is necessary to re-perform an anastomosis);

• two vascular boxes of microsurgical suture.
Microsurgical interventions are complex operations requiring careful selection of patients, rigorous pre-operative planning and a complete preoperative assessment. Patients should be in good condition with no additional diseases. If the patient smokes, he/she must quit at least 8 weeks prior to, and for 6 weeks after surgery. If the patient is elderly or has cardiovascular risk factors, it is necessary to do a full cardiological evaluation. Elderly patients and/or those with cardiovascular risk factors must undergo a full cardiovascular assessment – angiography, an ultrasound examination of the recipient vessels, and a complete blood report including haemostasis and blood group.
The role of the anaesthetist is essential and requires good cooperation with the surgeon. It is necessary to achieve strict control of haemodynamics during the intervention to ensure an optimal flow at the tissue transplant.
Facial burns

Facial burns present serious problems. As well as being aesthetically important, our faces contain special areas essential for vision, eating and breathing. In poor regions, even if patients survive without treatment, retraction may cause severe facial disfigurement.


Malnourish patients aggravated by undernutrition provoked by hyper metabolism are prom to develop infection.

Final appearance.

Severe lesion of inferior eyelid.





Dissection of deeper layers.
Alar nose cartilage. Cartilage setting.
In poor life conditions eyelid reconstruction sometimes need times to treat, with severe after-effect risk.

Superior eyelid flap.
Final result.
Important factors here are overcrowding, hazardous methods of cooking and heating and general lack of regard for precautions when using fuels. When facial burns are accompanied by injury to the airway, morbidity and mortality are higher even with treatment - damage to the airway should be treated as a priority. Away from civilization and without treatment, most victims die, although a few do survive.
Because of their appearance, burn victims with severe sequelae are treated as lepers and rejected by society.
Some frequent causes of burns are:
• Fire/flame – industrial or domestic fires;
• Scalding due to steam or hot liquids;
• Contact with hot objects e.g. heaters or hot kitchen plates, stoves etc;
• Electrical burns
One of the major causes of domestic accidents is cooking. This is often done on the floor or ground, making it easy for children to become burnt or scalded. A lack of mains electricity means that candles and kerosene must be used for lighting, increasing the risk of injury. However, education about the risks is improving.
A woman suffering from an acid attack


Opening the eyelids
Left: Reconstruction with orbicular oris muscle and skin graft

One of the major causes of domestic accidents is cooking, often done on the floor.
Burn of the alar ring.
Ear cartilage. Root of the helix.

Final result.
Another cause of burns which is becoming increasingly common is road accidents. Over the past 20 years, traffic has increased exponentially: together with reckless driving, this has resulted in frequent and major accidents, often causing severe burns.
Facial burns are often associated with burns to other parts of the body, particularly the hands, since the first reaction is to use them to cover one’s face – unless the victim is unconscious.

Severe burns require immediate medical attention. Burns on the face, hands and genitals can be particularly severe, but immediate treatment can help to prevent scarring, disability and disfigurement. On the positive side, Accident & Emergency services are available today: not so long ago they didn’t exist.

Also local colleagues and nurses are becoming better educated and more experienced in the management of patients. On the other hand, a shortage of ambulances is a factor which makes it difficult to cope with emergencies.
Restoration of a human face following a burn is a complex problem. Minimizing scarring and structural deformities of the burned face begins when the patient is first admitted and careful appropriate management during the acute phase can reduce the need for secondary reconstructive procedures. Current research examines new ways of stimulating cell viability to promote spontaneous healing without resort to surgery.
The contracture associated with deep burns of the face can cause local tissue distortion or, in the case of extensive injury, give rise to a complete mask-like appearance Skin grafts and local flaps offer some remedy, however the net result is often someone who has difficulty re-integrating into society.
Patient with chin/ sternal fusion which is a frequent after-effect in poor social conditions.



The latissimus dorsi muscle flap carve on the edge of the anterior border, in order to shape as need, is a good indication in humanitarian.
Final appearance after Reconstruction with pedicle latissimus dorsi flap.
Poorest society will have in a near future benefit from current research examines new ways of stimulating cell viability to promote spontaneous healing.
Burn to jaw, neck and arm.
Result after reconstruction with delto-pectoral flap and latissimus dorsi flap.
Neck contracture have a significant impact on mouth function and airway access.
Facial skin varies greatly in thickness and density of appendages, depending on the age and gender of the patient and the location of the burn.
It is difficult to over-emphasise the importance of facial appearance and function for the quality of life of a survivor. Proper, acute care of the burned head and neck is a key component not only of immediate management but for the long term outcome. The face has essential functional roles that must be maintained: these include coverage of the eyes, mouth closure, airway access and neck mobility. If the teeth are exposed due to ectropion of the lip, or airway access is compromised by microstomia, acute reconstruction should be performed. Neck contracture have a significant impact on mouth function and airway access. If these functions are threatened, early neck release should be performed.




Trauma
There are many kinds of trauma in the western world which require specialist treatment, but those seen in developing countries may be different due to differing social conditions, culture and physical response to trauma.

In Africa, road accidents are particularly serious, due to a number of factors- lack of respect for the rules, the poor conditions of cars and roads and a lack of road signs. Victims may need orthopaedic treatment and the indications for surgery or medical treatment are quite different from those in developed countries: the risk of infection, the infrastructure and physical condition may all affect the outcome.
Road accidents are particularly serious, due to a number of factors- lack of respect for the rules, the poor conditions of cars and roads and a lack of road signs.
Mandibular trauma after surgery before reconstruction.




Result. Latissimus dorsi flap lift with skin palette.
Deltopectoral flap lift.
Intra-operative final view.
Social condition facilitate injuries usually lethal from bullets, irons, wood or others.
Patient with an arrow in his head.


X-Ray.
Arrow after extraction.

In rural areas, it is common to see dry, abandoned wells: falling into one can result in serious injury or even prove fatal. In a country where life expectancy is less than 50 years, the majority of victims are children or young adults.
We treated one patient with a gunshot wound to the head. The bullet entered in the occipital region and, after passing through the brain, exited through the orbit, seriously damaging the superior eyelid: this was reconstructed, avoiding subsequent loss of the sight.
Another frequent type of trauma is shown in women who are victims of an acid attack (see Burns chapter). The resultant burns are most often to the face, and patients may require reconstruction of the nose, cheek, mouth and eyelids.

Trauma provoked by camel bite. Tried to reconstruct by local doctor.
The patient with an arrow in his head, and who survives its extraction, presents a trauma quite similar to what, in the west, we are more likely to see as a result of injuries caused by metal objects, in most cases to the head, but also to the chest and heart.
One patient involved in a car accident was impaled in the chest by a piece of bamboo, causing injuries to the pulmonary artery, left auricle and right lung, which were more typical of those caused by a metal rod. He survived the surgical intervention but unfortunately not the resultant septicemia.
Operating theatres are often not equipped to perform extra-corporeal circulation or advanced neurosurgery: nevertheless, a skilled and experienced surgeon is able to cope with critical trauma in the absence of these facilities.
Tumours
There are a high deal of tumours demand for treatment in humanitarian. Today is just possible to take care of benign ones, not still the others with mandatory necessity of multi-disciplinary speciality and infrastructure.
Keloid arround the ears, inferior part of the face, neck and sternal region.




Intra-scar resection.
Final appearance
Keloids
Hypertrophic scars and keloids are unique to humans: attempts to provoke them in animals have always proved unsuccessful. Despite a great number of studies, the aetiology of this excessive conjunctive proliferation remains unknown. The increased incidence of keloids and hypertrophic scars in people of African descent has been documented in several studies.
There is no obvious histological difference between hypertrophic scars and keloids. Clinically, the difference is that hypertrophic scars have parallel edges while keloids have irregular edges.
Many causes have been proposed, such as reaction to foreign bodies or bacterial infection. The role of the immune system in abnormal scar formation is also unclear.
Dark skin is much more prone to development of these conditions than other skin, and the young are more at risk than older people. The parts of the body most affected by keloids are around the ears, the inferior part of the face and the sternal region.
A surgical approach that applied to keloids is intra scar resection.
A useful treatment in humanitarian missions is intra-scar injection of a cortico-steroid - Kenacort 40mg/ml is normally used. This therapy can be performed 4 - 5 weeks after surgery.
Neurofibromatosis Von Recklinhausen’s disease
Neurofibromatosis Type I is a disease caused by the mutation of a gene on chromosome 17. There is no sexual or racial link. The neurological system is affected, with nerve tumours on or just under the skin and can spread to the whole body.
Neurofibromas can cause cutaneous disfigurement which can be present in infancy. There are three main types: Cutaneous neurofibromas are soft fleshy tumours arising from the peripheral nerve sheath; Subcutaneous neurofibromas are firm; Plexiform neurofibromas can involve long portions of nerves or bundles of nerves.
The disease may occur in the retina, which can lead to blindness. Particularly in teenagers it can cause learning difficulties. Neurofibromas may often evolve into cancer which can be fatal.
Many patients present with musculoskeletal abnormalities affecting the skull and facial bones, particularly the maxilla.
Surgical intervention is reserved for patients with significant discomfort or with cosmetically significant lesions.
Patient suffering from neurofibromatosis.



Result after resection of tumour.
Intra-operative view.
Espinocellular tumour.

Intra-operative view of asportation and reconstruction. Final result.
The treatment of tumours in humanitarian missions is not possible at present. It will become a reality in the near future, but will require oncologists to be permanently available, together with intensive care units, and facilities for oncology, radiology, haematology, cardiology, and intensive care unit, to guarantee patient follow up.
In a few individual cases, we have taken the decision to perform an intervention in order to relieve the chronic suffering of the patient, and to reduce the burden on family and friends. In most of these cases, hygiene and ease of movement were important considerations.
Mid-face and dorsal espinocellular tumour.




The treatment of tumours is not possible yet. Hygiene and ease of movement were important consideration in few indications.



Post 6 months
Neurosarcoma from mental nerve at mandibular canal.

Reconstruction with latissimus dorsi and deltopectoral flaps.

The risk factors are, children between the ages of 4-7, from subSaharian regions (The World’s Burkitt belt) with weak immune systems.
Young patien 14 years old suffering from Burkitt lymphoma.
Burkitt lymphoma
Burkitt’s lymphoma is a type of non-Hodgkin lymphoma in which cancer starts in cells of the immune system called B lymphocytes. These are the fastest growing human tumours. There are three types of tumour:
Endemic. This is present in equatorial Africa, or sub-Saharian or “The World’s Burkitt belt” (similar to Noma belt). It commonly affects children between the ages of 4 - 7 and is twice as common in boys as in girls. Epstein- Barr virus (EBV) is found in almost all patients (98%). There is research showing that malaria reduces resistance to EBV.The disease involves the jaw and other facial bones and also the caecum, ileum, kidneys, ovaries and breast.

Sporadic. This type is non-African and is not associated with EBV. The ileocaecal region is frequently involved.

Main complication in Burkitt treatment is kidney failure and the need for dialysis.
Immunodeficiency. This type is usually associated with HIV infection. Treatment in Africa is possible where there is a permanent presence of trained medical staff to follow the therapy and treat complications, as adequate hydration is essential, the kidneys are frequently affected and their malfunction is the main complication of treatment.
Chemotherapy is performed with cyclophosphamide, methotrexate, doxorubicin and vincristine. This can be difficult to achieve, as different rules may make it difficult to obtain the drugs, especially vincristine and they expire rapidly unless kept cool. These tumours respond to treatment faster than slower growing cancers, which can result in a hazardous condition called “tumour lysis syndrome” in most patients.
The prognosis is good with high survival rates (90% at 10 years) for low risk tumours, but for those patients with high risk tumours the mortality is around 75%.
Anaesthesia
Anaesthesia for Noma patients, particularly those suffering from trismus (at least 30% of the children, teenagers and sometimes adults), is the most difficult part of our work in Africa, because of the problems with intubation presented by patients who have difficulty opening their mouths. There are different ways to analyse and overcome the problems: currently our first choice is fibre-optic nasal intubation, which is safe and comfortable for the patients and is routine for the anaesthetist.

Anesthesia is one of the most difficult part of our work in Africa, because of the problems with intubation presented by patients who have difficulty opening their mouths and treat associated pathologies.
Dr. Gabriela Vilain, anaesthetist from Saint Louis Hospital, Paris.
Dealing with severe trismus is always very difficult and it is essential that the surgeon and anaesthetist together consider all possibilities and agree on the procedure to be followed.
When we started work in Africa we considered the traditional methods and anaesthetics for patients with difficulty in opening the mouth:
• The guided tracheal intubation;
• Nasal intubation;
• High pressure ventilation; and Non invasive ventilation (NIV)
• Tracheotomy
Intubation is usually performed under sedation which makes the procedure easier and allows us to overcome cultural and language barriers. Problems in children can be harder to solve even if they are more cooperative than their occidental peers and sometimes in general anaesthesia it is necessary to intubate with inhalation anaesthetics or even administer the anaesthetic during normal breathing. Dealing with severe trismus is always very difficult and it is essential that the surgeon and anaesthetist together consider all possibilities and agree on the procedure to be followed. This includes the possibility of performing a tracheotomy: however, this would only be considered as a last resort.
Fibre Optic is necessary in theatre room and become mandatory in severe trismus intubation.

Patient follow-up is not easy in humanitarian missions and under these conditions it is best to keep things as simple as possible. Nurses play a vital role in keeping the airway clean and free and there is always the infrastructure, or lack of it, to deal with.
We must consider that in most of the patients, oral cleaning was done months earlier, which does not give enough confidence to perform anaesthesia. In these cases, it is necessary to complete the cleaning of the mouth and remove any badly positioned teeth, often immediately after intubation and sometimes before fitting the tracheal tube. This has to be done because if left such teeth may cause decubitus, lesions of any areas they are in contact with and airway obstruction in case of accidental avulsion.
Once the airway is solidly established, all patients are packaged without exception. Particular attention must be paid to the security of the tube, which must be firmly fixed as it is vital to avoid any movement or sliding which can be a serious problem in these patients.
It is essential to clean the entire airway soon after surgery to guarantee free and safe ventilation. In this respect we try never to leave patients intubated overnight in humanitarian missions as prolonged ventilation is associated with pneumonia: therefore we extubate the patients at the end of the surgery in the operating theatre. However, the nurses must be attentive especially during the night shift because in humanitarian missions, they are the only staff following the patients.
Because we have to cope with infrastructure and instruments in very basic hospitals the procedures and methods to be employed must be kept as simple as possible. This extends to the different ways local colleagues may evaluate the needs of patients and the entire practice of medicine. Young anaesthetists working at these missions need to be focused and take great care to do their best, and, to minimise risks, if possible they should be supported by experienced anaesthetists.
At one time, operating theatre hygiene was a big issue to consider before any procedure. Today, most hospitals, even in the poorest countries, have improved their sanitation markedly. However the electricity supply is not always guaranteed and it is possible to have a power failure. Therefore even in the best hospital conditions nothing should be left to trust. It is essential that the surgeon ensures that all the necessary equipment is tested at home and again in the theatre before starting an operation. If this is not done there could be nasty surprises in store due to the often poor infrastructure, very different from our working conditions at home.
Patients must be considered in their overall clinical situation as they might be suffering from diseases such as malaria (often) or tuberculosis, whith lungs damages: blood diseases such as thalassemia and haemoglobin S (sickle-cell anaemia). As well as treating any diseases present, general conditions such as malnutrition and reduced immune response must be improved and evaluated before attempting any intervention.
In the countries where we operate, finding a specialised echocardiogram could be problematic, and the anaesthetist must be ready to diagnose any type of cardiac problem which might be dangerous for the patient. This includes CIA, CIV and aortic coarctation which can be present without any pathological or clinical manifestation. Even Fallot tetralogy, associated with cleft lip and palate malformation, can go undiagnosed. None of these pathologies are an absolute contra-indication for anaesthesia as long as they are recognised and allowed for. But the same cardiac conditions can lead to pulmonary hypertension and in these cases the indications for surgery must be reconsidered, with the prospect of transferring the patient to a specialist centre. The commonest cardiac condition affects the valves, particularly the mitral and aortic due to the high prevalence of poliomyelitis infection and rheumatic fever. In these cases, it is necessary to evaluate the degree of haemodynamic damage and the impact on the general health of the patient before deciding to perform any reconstructive surgery, which then becomes a secondary consideration.
Another important point for surgeons to consider, after evaluating the duration of the operation and the possible blood loss, is whether and how much blood might be required. In the prevailing conditions it is not always easy to obtain the quantity (and particularly the quality) of blood we need, so it is very important to be sure about the stocks available.
We try never to leave patients intubated overnight, as prolonged ventilation is associated with pneumonia.
Patients must be considered in their overall clinical situation as they might be suffering from diseases such as malaria (often) or tuberculosis, whith lungs damages.
Anaesthetist must be ready to diagnose any type of cardiac problem which might be dangerous for the patient. This include CIA, CIV, aortic coarctation or others which can be present without any pathological or clinical manifestation.
Is mandatory to have batteries to cope with power failures and any equipment needed to avoid hypothermia.
It is easier today to test patients pre-operatively and determine if they are HIV-positive, when it becomes very important for the whole staff to take the appropriate preventive measures. These days the humanitarian missions are in much better condition, and all kinds of materials are now available – not just the basics we manage with every day, but also, for example, batteries to cope with power failures and any equipment needed to avoid hypothermia.
The good anaesthetist must always remember to perform techniques that can be supported in a simple environment. In this setting it is mandatory to use drugs with the shortest half-life if available. We are usually working in hospitals where unit care for post-operative patients consists of just a bed and no other equipment. Therefore, the anaesthetist must be sure that each patient is awake and in good condition before starting on the next one. Trained nurses who know the relevant details and to whom the correct post-operative instructions are given are the best support.

Thank to review the original text to Dr. Fabrizio Monaco, Head of cardiac surgery anesthesia, Prof O. Alfieri, San Raffaele Hospital, Milan

Psychology
The psychological effects of treatment abroad must not be underestimated, and management of them is a very important aspect of our ethos. They can range from euphoria to depression and anxiety, and patients may go from one extreme to the other during the peri-operative period. The psychological problems caused by the thought of surgery are hard to cope with, both for the patients and for the hospital staff, and are worse if supplementary interventions and a long period of reeducation are required.
Having talked to psychologists from different universities, we are of the opinion that they are very familiar with psychological trauma following physical injury, but far less familiar with that caused by surgery and transfer from the home environment.
In surgery, it must always be a priority that the treatment considers the effects on body and mind together, regardless of whether it is a simple procedure in a very comfortable hospital or very complex interventions with long term pharmacological support, and in the rare occasions where immobilisation is required. Although we try as far as possible to operate in the patient’s home country, exceptionally it is necessary to transfer more complicated cases to a hospital abroad.
Young patient coming to a consulting room.

Is suggested to operate in the patient’s home country. Exceptionally it is necessary to transfer more complicated cases, abroad.
A patient together with his father. Often mothers are busy at home taking care of many siblings.
 Ph. Nicolas Bruant
Ph. Nicolas Bruant
If the patient sees the surgery as a risk, or if there are complications, separation increases the likelihood of post-traumatic sequelae.
However, as noted elsewhere, it is becoming increasingly possible to manage these cases in a local hospital, and in future perhaps the only patients to be transferred will be those requiring open heart or neurosurgery.
When contemplating surgery abroad, it is essential to consider the benefit/risk ratio and the feasibility of it being performed locally. Consent should be obtained after a full discussion, with the patient and family, of the different alternatives and likely outcomes. In the case of very young children, a sudden and/or prolonged separation from parents and siblings is an emotional experience which may be responsible for subsequent “attachment disorder” behavioural problems, anxiety and depression.
It is clear that separation from family and environment (cultural and linguistic) represents an additional stress over and above that of the surgery itself. It is especially difficult for a young child who has never before been separated from family, and more so if the separation is protracted. If the patient sees the surgery as a risk, or if there are complications, separation increases the likelihood of post-traumatic sequelae.
A sudden separation from the mother tongue is very hard on a child, and can be traumatic if he is alone (without a family member or sibling) during the transfer abroad for an operation.
Young patient with his mother. The presence of a family member can help to avoid attachment disorder, behavioral problems, anxiety and depression, and also reduce the recovery time.

Having an interpreter would help enormously, but for many reasons it is not always possible to provide one, especially at crucial times, such as in the operating theatre. With no one to explain the operation, the resultant alterations to the patient’s body and appearance can easily induce severe, acute depression. Most of the patients are young, as the disease and subsequent malformations started at a very early age, or even at birth. These young patients are accompanied by nurses during the flight but in future there is a need for these nurses to be better trained in the management of psychological problems. Sometimes a sibling accompanies the patient but often this would make it difficult for the mother to cope with a number of other children at home to manage.

Even though there is now more comfortable accommodation available for patients and for volunteers to help care for them, this is not enough to alleviate the psychological trauma they can suffer.
When a patient is told that they are to be taken abroad for treatment, their first reactions are usually excitement and anticipation preparing for the journey. In fact, regardless of the expectation of functional and aesthetic improvement, it is likely to be the only opportunity they will ever have to fly abroad, so they look forward to what seems at first to be a wonderful opportunity.
More comfortable accommodation, sometimes is not enough to alleviate the psychological trauma.
A familiar cultural and linguistic environment helps to overcome the stress of surgery.
The presence of a family member could reduce the recovery time but abroad become expensive for the organisation.
This euphoria lasts through the month between the decision and the flight, and for the week between arrival and the operation. The first postoperative days are psychologically very close to what they would be in the patient’s home country, with the advantages of better infrastructure and a more comfortable environment.
The overall length of stay depends on how many operations are to be performed. If only one procedure is necessary the post-operative course lasts about a month, but when two interventions are required it can be several months before the patient can be returned home.
The presence of a family member could reduce the recovery time but it is expensive for the organisation. The psychological problems start to show when patients begin to feel lonely and isolated due to language difficulties and lack of empathy.
This is a reality not just for the patient but for any accompanying sibling. In addition to the burden of management and economy, they often feel a desire to be back home.
Lack of company (at home there are always many people around) can make this especially painful, to the point where they may forget about the
This patient is waiting for a sibling in a ward. People in a desert area can only speak the local dialet.

Ph. Nicolas Bruant
negative aspects of home, and become depressed even in a more comfortable environment.
When patients have to be kept for several months, their psychological suffering can be quite varied. In fact, the vast majority suffer enormously: a few might be luckier, and find friends and enjoy themselves.
However, they all miss their own life and home and so it is not easy for the organisation to manage the psychological effects related to treatment abroad. Adaptation is especially hard for patients used to living in rural and desert areas, even when the conditions are better than they are accustomed to.

Real, and big problems start when it is time to go back home. The joy of seeing the family again is juxtaposed with gloom at leaving their new environment. And the pleasure of reunion with family and friends fades rapidly because re-adaptation is very hard, even when it is made gradual by keeping patients in an organisation centre before they return to their families.
It can take a long and painful time to overcome the difficulties of readaptation: the psychological scars may require support which is difficult to provide. On future missions there is a definite need to pay more attention to the psychological follow-up of patients and a deeper analysis of the problems resulting from the surgery and transfer.
It is mandatory to put into practice treatment considering the effects on body and mind together.
Big problems start when it is time to go back home. It can take a long and painful time to overcome the difficulties of re-adaptation.
Patients enjoing together to learn reading, writing and drawing.
It must always be a priority that the treatment considers the effects on body and mind together.

Bibliography
BANZET P, GHEITA A: la reconstruction de la paupière supérieure. Le lambeau de paupière inférieure. Ann Chir Plast Esthet, 1984, 29, 109-112.
BINDER JP., REVOL M., SERVANT JM. Dermohypodermites bactérienne nécrosantes et fascites nécrosantes. EMC (Elsevier Masson SAS, Paris), Techniques chirurgicales- chirurgie plastique reconstructrice et esthétiques, 45-150-A,2007( 11 pages ).
BELLAVOIR A. Anatomie des lèvres. Configuration extérieur et dispositif musculaire. In “chirurgie des lèvres”(J. Levignac). Masson. Paris, 1990. p. 3-11
BURGET G. C., MENICK F.J. Nasal support and lining: the marriage of beauty and blood supply. Plastic Reconstruct Surg, 1989, 84, 2, 189-202.
BURGET G.C., MENICK F.J. Nasal reconstruction: seeking a fourth dimension. Plast Reconstruct Surgery, 1986, 78, 2, 145-157.
BURGET G.C., MENICK F.J. The subunit principle in nasal reconstruction. Plast Reconstruct Surgery, 1985, 76, 2, 239-247.
BURGET G.C., MENICK FJ. Aesthetic reconstruction of the nose. Mosby. St. Louis, 1994 (615) pag.
CHANCHOLLE A. Les fentes labio-palatines In: Chirurgie plastique de l’enfant. Pathologie congénitale. Rapport du XXXVII ème congrès de la SFCPRE. Maloine. Paris, 1987, p, 31-132.
CHASSAURD H. Chirurgie des lèvres dans les sequelles de noma. These pour le doctorat en medicine. Universitè paris VII. Paris, 2002.
CHEKAROUA K, FOYATIER JL. Traitement des séquelles’ de brûlures: généralités. EMC
CHICHERY A, VOULLIOME D, ASSIOBO N, RECCHIUTTO J, FOYATIER JL. Réparation de séquelles de brûlure du cou. EMC (Elsevier Masson SAS Paris). Technique chirurgicales. Chirurgie plastique reconstructrice et esthétique, 45-160. 2005. 15 pages.
CONVERSE J. M. Reconstruction of the nose by scalping flap technique. Surg Clin North Am, 1959, 39, 259-335.
CONVERSE J. M., WOOD-SMITH D. Techniques for the repair of defects of the lip and cheeks. In Reconstructive plastic surgery (JM Converse). Saunders. Philadelphia, 1977. p. 1594.1544-
CONVERSE JM., WOOD-SMITH D. Techniques for the repair of defects of the lips and cheeks. In Reconstructive Plastic Surgery (JM Converse). Saunders. Philadelphia, 1977.p.1594. 1544-
DUPUIS A., SOUQUET J. R. Pertes des substance de la lèvre inférieure. In Chirurgie des lèvres (J. Levignac). Masson. Paris, 1990. p.155-174
El Khatib K, Danino A, Malka G. The frontal sinus: a culprit or a victim? A review of 40 cases. J. Craniomaxillofac Surg. 2004 Oct;32(5): 314-7. Elsevier Masson SAS, Paris. Techniques chirurgicales. Chirurgie plastique reconstructrice et esthétique, 45-160A,2005. 6 pages
EMMETT A.J.J. The closure of the defects by using adjacent triangular flap with subcutaneous pedicels. Plast Reconstruct Surg, 1997, 59, 1, 45-52.
FOYATIER JL, VOULLIAUME D, MOJALLAL A, CHEKAROUA K, COMPARIN JP. Traitement des séquelles de brûlures: brûlures de la face. EMC (Elsevier Masson SAS, Paris). Techniques chirurgicales, Chirurgie plastique reconstructrice et esthétique, 45-160B, 2005. 9 pages.
FREIDEL C., DARGENT M., BERGOING C. La reconstruction de l’aile du nez. Techniques: quelques cas. Ann Chir Plast, 1964, 9, 2 101-105. Gray’s anatomy. Elsevier, Churchill Livingtone, 2005 (39th edition). P. 567-579.
JACKSON IT. Classification and treatment of orbitozygomatic and orbitoethmoid fractures. The place of bone grafting and plate fixation. Clin Plast Surg. 1989 Jan; 16(1): 77-91.
JOHANSON B., ASPELUD E., BREINE U., HOLMSTROM H. Surgical treatment of non traumatic lower lip lesions with special reference to the step technique. Scand J Plastic reconstruct Surgery, 1974, 8, 323.
KARAPANDZIC M. Reconstruction of lip defects by local arterial flaps. Br J Plast Surg, 1974, 27, 93-97.
KAZANJIAN V.H. The repair of nasal defects with the medial forehead wound. Surg Gynecol Obstet, 1946, 33, 79-83.
LABBOZ P., LEBEAU J., RAPHAËL B., SÉGUIN P., BARTHOU B. A propos dès reconstructions nasales et latero-nasales. Étude de 68 cas. Ann Chir Plast, 1981, 26, 3, 271-275.
Lakhel-Lecoadou A, Delaporte T, Bichet JC, Lambert F, Cantaloube D. Chirurgie des brûlures graves au stade aigu. EMC (Elsevier Masson SAS, Paris). Techniques chirurgicales. Chirurgie plastique reconstructrice et esthétique, 45-157, 2000. 18 pages
LEZY JP., PRINC G. Stomatologie et pathologie maxillo-faciale. Masson. Paris, 1987. P. 15-22.
MARCHAC D. Lambeau de rotation fronto-nasal. Ann Chir Plast 1970, 15, 1, 44-49.
MARCHAC D., ARNAUD E. La distraction du maxillaire supérieur. Ann Chir Plast Esthet 42(5) :557-563, 1997
MARCHAC D., ARNAUD E. Mid-face surgery from Tessier to distraction. Child’s Nerv Syst 15 :681-694,199.
MC CARTHY Plastic Surgery. Vol 3
MCRAE M, FRODEL J. Midface fractures. Facial Plastic Surgery 2000;16(2): 107-13.
MERVILLE L.C., BUI P. Mutilation de la lèvre supérieure. In chirurgie des lèvres (J Levignac). Masson. Paris, 1990, p. 125-154.
MERVILLE L.C., RÉAL J.P. Chirurgie réparatrice des lèvres. Encycl Méd Chir, Paris, techniques chirurgicales, chirurgie réparatrice, 45400, 45402,et 45404.
MEYER R. Aesthetic aspect in reconstructive surgery of the nose. Aesthetic Plastic Surgery, 1988, 12, 4, 195-201.
MILLARD D.R. Jr. Cleft craft. The evolution of its surgery. Little, Brown, and Co. Boston, 1976. Vol I: The unilateral deformity. p. 449-485.
MONTEIL J.P. Physiologie nasale. Ann Chir Plast Esthétique, 1985,30,2,181-184.
MORAX S. Surveillance de l’appareil visuel au cours de la chirurgie plastique orbito-palpébral. Ann Chir Plast Esthet, 1984, 29,4, 311-317.
MULLIKEN JB, MARTINEZ-PEREZ D. The principle of rotation advancement for repair of unilateral complete cleft lip and nasal deformity: technical variations and analysis of results. Plast Reconstruct Surg. 1999 October; 104(5): 1247-60
MULLIKEN JB, WU JK, PADWA BL. Repair of bilateral cleft lip: review, revisions, and reflections. J Craniofac Surg. 2003 Sep; 14(5): 609-20.
MUSTARDE J.C. Repair and reconstruction in the orbital région. A practical guide. Livingstone. Edinburgh, 1969. 382 pages.
NEW G B. Sickle flap for nasal reconstruction. Surg Gynecol Obstet, 1945, 80, 497.
ONIZUKA T. Operative plastic and aesthetic surgery (en japonais). Tokyo, 1982,p.528-549.
PAVY B. Fentes labial et palatines. In: Pellerin D. Techniques de chirurgie pédiatrique. Masson. Paris, 1978. P.32-71.
PERNKOPF E. Human Anatomy Atlas.
PERS M. Cheek flap in partial rhinoplasty. A new variation the “in and out” flap. Scand J Plast Reconstruct Surgery, 1967, 1, 1, 37-44.
PONS J. A propos de temps musculaire dans les commissuro-plasties bucco-labiales. Ann Chir Plast, 1968, 13-14, 305-306.
PONS J. Brûlures des lèvres. In chirurgie des lèvres (J Levignac). Masson. Paris, 1990. p. 175-184.
PREAUX J., TEXIER M, REAL J.P. Commissuroplastie labiale d’agrandissement. Ann Chir Plast Esthet, 1987, 32, 1, 14-20.
REVOL M., GUINARD D., BARDOT J., TEXIER M., ET COLL. Réparation des pertes de substance du nez (brûlure exclues). Rapport du XXXVIII ème congrès de la Société Française de chirurgie plastique reconstructrice et esthétique. Masson. Paris, 1993.
REVOL M., VERGOTE T., SERVANT JM., BANZET P. Transfert tissulaires libres en chirurgie plastique (urgences exclus). Expérience de 10 ans. Ann Chir Plast Esthét, 1992, 37, 3
REYNAUD JP, BARDOT J, FOGLI A, MALET T, SABOYE J., ET COLL Chirurgie esthétique des paupières. Rapport du 53ème congrès de la Société Française de Chirurgie Plastique Reconstructrice et Esthétique. Elsevier Masson SAS. Issy les Moulineaux, 2008 (153 pages).
RICBOURG B. Vascularisation des lèvres. In Chirurgie des lèvres (J. Levignac). Masson. Paris, 1990., 19-26
RIEGER R.A. A local flap for repair of nasal tip. Plastic Reconstruct Surgery, 1967, 40, 2, 147-149.
RINTALA A.E., SELJAARAS A. Reconstruction of midline skin defects of the nose. Scand J Plast Reconstruct Surg, 1969, 3, 105-108.
ROUGIER J, TESSIER P, HERVOUET F, WOILLEZ M, LEKEFFRE M, DEROME P. Chirurgie plastique orbite-palpébral. Rapport de la Société Française d’Ophtalmologie. Masson. Paris, 1977. P. 85-173.
ROUGIER J., TESSIER P., ET AL Chirurgie Plastique orbito-palpébral. Masson. Paris, 1997.
ROUGIER J., TESSIER P., HERVOUT F., WOILLEZ M., LEKIEFFRE F., DEROME P. Chirurgie plastique orbito-palpébrale. Rapport de la Société Française d’Ophtalmologie. Masson. Paris, 1977. p. 423-452.
ROUTIÈRE H. Anatomie humaine descriptive et topographique. Masson. Paris, 1967 (10 ème édition), tome 1, pages 155-166, et 519-521.
RYBKA FJ. Reconstruction of the nasal tip using nasalis myocutaneous sliding flaps. Plast. Reconstruct Surg, 1983, 71, 1, 40-44.
SÉNÉCHAL G, SÉNÉCHAL B. Diplégie faciale. Intervention palliative de nécessité. Ann Chir Plast, 1982, 27, 4, 394-395.
SERVANT JM. Abu Dahbi September 2006
SERVANT JM. Chirurgie des grandes pertes de substance. Rabat mars 2004
SERVANT JM. Facial Reconstruction. Barcelona May 2011
SERVANT JM. Vastes pertes de substance des lèvres. In Chirurgie des lèvres (J Levignac). Masson. Paris, 1990. p. 193-199.
SERVANT JM., BANZET P. Le lambeau myo-cutané de grand dorsal. Son utilisation en chirurgie réparatrice. Chirurgie, 1983, 109, 233-244
SERVANT JM., BINDER J.P., REVOL M., MAY P., DANINO A. Manuel de chirurgie plastique, reconstructrice et esthétique
SERVANT JM., DIVARIS M. Réparation des pertes de substances du nez. In: Rhinoplastie esthétique fonctionnelle et reconstructrice (G. Sénéchal, A. Pech, M. Wayoff, et coll). Arnette. Paris., 1989, p. 363-394.
SERVANT JM., REVOL M. Les lambeaux fascio-cutanés, EMC (Paris). Techniques chirurgicales, chirurgie plastique, 45090, 6- 1990
SERVANT JM., REVOL M. Les lambeaux à Mésopotamie vasculaire. EMC (Paris). Techniques chirurgicales, chirurgie plastique, 45095, 6-1990
SERVANT JM., REVOL M. Les lambeaux musculo-cutanés. EMC. Techniques chirurgicales. Chirurgie plastique. 45085, 6-1990
SERVANT JM., SATOH K., LE DANVIC M., GROSLIERE D., PETOIN D.S., Mécanisme de retour veineux du lambeaux antibrachial en îlot à pédicule distal. AnnChir Plast Esthet,1988,33,3,215-222.
SOUSSALINE M. Une reconstruction labiale “pharaonique”. Ann Chir Plast Esthet, 1983, 28, 4, 397-398. e. 2ème édition, révisée et augmentée.
STRICKER M, FLOT F, CHASSAGNE JF, MELEY M, MOUGENOT A. Panorama des lésions du squelette facial. Ann Chir, 1983, 37: 49-64
STRICKER M, GOLA R. Chirurgie plastique et réparatrice des paupières et des annexes. Masson, Paris, 1990. p 1-53.
STRICKER M., GOLA R. Chirurgie plastique et réparatrice des paupières et de leur annexes. Masson. Paris, 1990. p. 215-237.
STRICKER M., GOLA R. Chirurgie Plastique et réparatrice des paupières et de leur annexes. Masson. Paris, 1990. P81-92, et 167-176.
STUZIN J.M., WAGSTROM L., KAWAMOTO H.K., WOLFE S.A. Anatomy of the frontal branch of the facial nerve: the significance of the temporal fat pad. Plast Reconst Surgery, 1989, 83,2, 265-271.
TCHAKERIAN A., RAULO Y., BARUCH J. Traumatisme chirurgicale du rameau temporo-frontal du nerf facial. Étude anatomique et conséquences cliniques. Ann Chir Plast Esthet, 1992, 37, 1, 18-26.
TEXIER M., PREAUX J., NOURYDUPERRAT G. Recontruction de la paupière inférieure par greffe chondro-muqueuse alaire et lambeau cutanéo-musculaire palpébral supérieur. Ann Chir Plast, 1981, 26, 5-9
TOUCHMANN-DUPLESSIS H., HAEGEL P. Embryologie (fascicule 2: organogenèse). Masson. Paris, 1970; p.12-21.
TREPSAT É. Le blepharochalasis. Ann Chir Plast Esthétique, 1988, 33,1, 29-31.
TROST O. Atlas didactique de traumatologie faciale. Thèse de doctorat en médecine. Faculté de Médecine de Dijon, octobre 2005.
WASHIO H. Retroauricular temporal flap. Plastic Reconstruct Surg, 1969, 43, 2, 162-166
WONG FK, HAGG U. An update on the anthologie of orofacial clefts. Hong Kong J. 2004 oct; 10(5): 331-6.
ZITELLI, J. A. The bilobed flap for nasal reconstruction. Archives of Dermatology, 1989, 125 (7), pp. 957-959.
Index
Noma Cancrum oris pag. 1
Symptoms and progression pag. 2
Hystorical references pag. 3 Occurrence - Europe pag. 4 Occurrence - worldwide pag. 5
Epidemiology pag. 7 Symptoms pag. 9
Acute necrotising gengivitis pag. 13
Onset of Noma infections pag. 15
Involvement of different types of teeth pag. 15 Canines pag. 15 Incisors pag. 16 Molars pag. 16 Observations pag. 19 Noma symptoms pag. 20
Bacteria and virus pag. 21
Embryology of the face and buccal cavity pag. 27 Face development pag. 28 Pharingeal apparatus pag. 28 Facial prominences pag. 30 Development of the nasal cavity and palate pag. 32 Clefts of the lip and palate pag. 33 Other facial defects pag. 35 Facial clefts pag. 35
Cleft lip and palate pag. 37 Cleft lip pag. 38
Unilateral cleft lip with nasal deformity pag. 41
Bilateral cleft pag. 47
The palate pag. 47 Cleft lip: surgical technique pag. 52 Cleft palate: classification pag. 54
Surgical technique pag. 54
Soft palate reconstruction pag. 54
Hard palate reconstruction: Von Lagenbeck technique pag. 56
Hard palate reconstruction: Veau-Wardill-Kilner pag. 56
Post operative care pag. 57 Complications pag. 59
Cancrum oris Onset and progression pag. 61
Classification (based on origin of infection) pag. 62
Surgery of Cancrum oris pag. 77
Flaps used in facial reconstruction pag. 80
Classification pag. 81
Nose Reconstruction pag. 85
Nose: surgical reconstruction pag. 87
Frontotemporal flap pag. 88
Forehead flap pag. 90
Technique pag. 91
Cheek advancement and rotation flap pag. 92
Width reconstruction od the nose pag. 93
Rib cartilage pag. 96
Radial forearm flap pag. 98
Columella pag. 99
Classification of columellar lesions pag. 99
Reconstruction of the columella pag. 100 Nostril alar rim thresold flap pag. 100/101
Naso-genian, alar fly flaps and advancement flap pag. 102/104 Alar edge rim flap pag. 105 Double naso-genian flap pag. 106 Free helix flap pag. 109
Cheek Reconstruction pag. 111
Surgical approach pag. 112
The deltopectoral flap pag. 113
Inner lining recontruction pag. 115
Platysma flap pag. 115
Platysma muscle anatomy pag. 116
Harvesting the platysma flap pag. 116
Temporo-parietal flap pag. 116
Advantages pag. 116
Surgical technique pag. 117
Cheek rotation flap pag. 118
Surgical technique pag. 118
Latissimus dorsi flap pag. 120
Advantages pag. 124 Surgical technique pag. 124
Frontal flap pag. 126
Submandibular flap pag. 130
Lip Reconstruction pag. 131
Introduction pag. 131
Naso-genian flap pag. 132
Estlander flap
pag. 135
Surgical technique pag. 139
Abbe flap pag. 145
Abbe-Burgett flap pag. 145
Surgical technique pag. 145
Webster flap pag. 148
Indication and technique pag. 148 Fan flaps pag. 149
Indication for fan flaps pag. 149
Gillies flap pag. 149
Surgical technique pag. 150
Karapandzic flap pag. 150
Surgical technique pag. 150
McGregor fan flap pag. 151
Surgical technique pag. 151
Camille Bernard flap pag. 152
FAMM (Facial Artery Muscolomucosal Flap) pag. 155
Commissuroplasty pag. 156
Trismus pag. 157
Classification of trismus pag. 158
Trismus pathogenesis pag. 158
Mouth aperture pag. 161
Trismus: surgical indications pag. 162
Trismus: surgical approach and technique pag. 163 Results and complications of surgery pag. 165
Microsurgery pag. 167 Strategies pag. 168 Intervention pag. 170
Radial forearm flap pag. 172
Alternatives to microsurgery pag. 174
Post-operative care pag. 175 Flap monitoring pag. 176 Microsurgery instruments pag. 177
Facial burns pag. 179
Some frequent causes of burns pag. 181
Trauma pag. 185
Tumours pag. 187
Keloids pag. 188
Neurofibromatosis Von Recklinhausen’s disease pag. 188 Burkitt lymphoma pag. 192
Anaesthesia pag. 193
Psycology pag. 197
Bibliography pag. 203

