



































































The European Commission’s proposal for the phase-out of the use of dental amalgam across the EU from 1st January 2025 has completed its First Reading in the EU Parliament. MEPs voted in favour of the phase-out.
On 14th July 2023, the European Commission adopted a proposal to revise the Mercury Regulation, to introduce a total phase-out of the use of dental amalgam and prohibit the manufacture and export of dental amalgam from the EU from 1 January 2025 – five years earlier than expected. Ahead of the vote, the Committee on the Environment, Public Health and Food Safety (ENVI) had tabled a total of 18 amendments to the Commission’s original proposal. The amendments specifically relating to dental amalgam included:
• Some additions to the background/ context for the phase out, with additional references to mercuryfree alternatives
• A reference to emissions from crematoria (though no proposed measures to deal with these emissions)
• The exception to the ban on use of amalgam for dental practitioners meeting “the specific medical needs of the patient” has been amended to refer to the “duly justified specific medical needs of the patient”
• A proposal for a further Commission report (to be delivered by June 2026) on the feasibility of withdrawing exemptions for the use of amalgam by 2030
Only two amendments were rejected: one that intended to introduce a derogation for the use of dental amalgam in treatment until 31st December 2026 “where dental amalgam is a relevant

material for dental care and is one of the relevant publicly reimbursed methods of dental fillings” and another that intended to insert a derogation such that “the manufacture and export of dental amalgam shall be permitted for the specific medical needs of the patient … until 31 December 2026”.
The amended legislative proposal has now been referred back to the ENVI committee for interinstitutional negotiation.
Although the UK is no longer part of the EU, there would still be ramifications.
The British Dental Association (BDA) has warned that the European Parliament’s vote will send shockwaves across the UK’s already struggling dental services.
Silver amalgam is the most common material for NHS permanent fillings across the UK. Fillings represent around a quarter of all courses of NHS treatment delivered in England, with amalgam used in around in around a third of procedures. The BDA estimates treatment times and costs of alternative
materials are over 50% higher than those of amalgam.
The EU vote will hit all four UK nations but will have a disproportionate impact on services in Northern Ireland, which has the highest proportion of filled teeth of any UK nation. Under postBrexit arrangements, Northern Ireland will be expected to phase out dental amalgam on the same basis as EU member states. Divergence means the rest of the UK faces disruption and higher costs given the impact on supply chains, despite no formal ban.
In an open letter to all four UK Chief Dental Officers, the BDA stresses there are currently no alternative restorative materials that compete with amalgam on speed of placement or longevity, meaning the ban will eat into clinical time and resource that are in short supply, likely creating further access barriers. There are no indications where the millions in additional funding required will come from nor the workforce to carry out the tens of thousands of extra clinical hours.
MEPs also backed amendments stating that Member States need to “ensure appropriate reimbursement is made available for mercuryfree alternatives” to limit the socioeconomic impact. The BDA says the same approach is need from all UK Governments.
While the BDA has long supported a phase-down in dental amalgam, it believes this rapid phase-out is neither feasible nor justifiable. Dental amalgam has been in use and extensively studied for 150 years as a restorative material. Its safety and durability are well established, and it remains the most appropriate material for a range of clinical situations. ■
The number of dentists on the UK Register, following the recent annual renewal period, has increased when compared to recent years.
On the morning after removals, there were 44,209 dentists on the Register. This is a 2.5% increase compared to last year with 1,079 more dentists on the register.
These figures provide a useful benchmark for the total number of dentists registered in the UK.
While the GDC (General Dental Council) recognises there are important issues of concern, including access to NHS dental services and significant ongoing recruitment challenges in some
areas, it is important to note that this data does not provide insight into the number of professionals working in different patterns (e.g. full time vs part time), how many dentists are working in NHS services compared to private practice, local workforce conditions, or the numbers of professionals working in different roles (e.g. academic).
However, for the first time, as part of the dentists’ renewal process in 2023, the GDC has gathered data about the work dentists do, including the number of hours they are working, whether they are working in the NHS or privately, and in clinical or non-clinical roles. These figures will reportedly be published once the analysis is complete. ■


















What a whirlwind month January was! To anyone out there who claims that nothing much happens during the first month of the year, I present to you: dentistry.
It’s always a struggle to pick out what could be deemed the most important news to feature within these pages, but this month proved the most challenging yet. We went back and forth several times on which story should run on the front page, ultimately deciding upon the EU’s potential ban on dental amalgam, which will have a direct impact on dentistry in Northern Ireland, and a knock-on effect across the rest of the UK. Alun Rees also discusses the situation on page 40. The other top-story contender was the news of The Mirror’s Dentists For All campaign, which further ingrains the dental access crisis in the public consciousness. The tabloid shone the spotlight on yet more alarming statistics, including the fact that 40% of children do not receive regular NHS check-ups, while 104,133 children attended hospital with rotten teeth over the past five years. Read all about it on page 6.
A lot more happened before 2024 reached 31 days old, including the announcement of the Labour Party’s Child Health Action Plan. Bas Vorsteveld discusses that on page 14.
Before I leave you to explore the issue, a quick reminder to get your Dental Awards submissions in by the 23rd February deadline. Page 50 provides further details. Best of luck!









The Probe is published by Purple Media Solutions.
Registered in England. Registered number 5949065
Managing Editor: James Cooke
Commercial Director: Gary Henson
Divisional Administrator: Francesca Smith
Production Designer 1 : Lorna Reekie




Production Designer 2: Rob Tremain
Digital Content Manager: Stephen Wadey
Circulation Manager: Andy Kirk
Director: Ed Hunt
Managing Director: Steve Hardiman
Regular Contributors: Lisa Bainham, Nigel Carter, Barry Cockcroft, Ollie Jupes and Pam Swain
E-mail news, stories or opinion to james.cooke@purplems.com
Circulation/Subscriptions: The Probe Subscriptions, Perception SaS, PO Box 304, Uckfield, East Sussex, TN22 9EZ, Tel: 01825 701520, https://purplems.my-subs.co.uk ©Purple
Media Solutions Ltd, 2014. All rights reserved. ISSN 0032-9185. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies, and information retrieval systems. While every effort has been made to ensure that the information in this publication is correct and accurate, the publisher cannot accept



liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine.
The views expressed in The Probe are not necessarily the views of the magazine, nor of Purple Media Solutions
Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth



















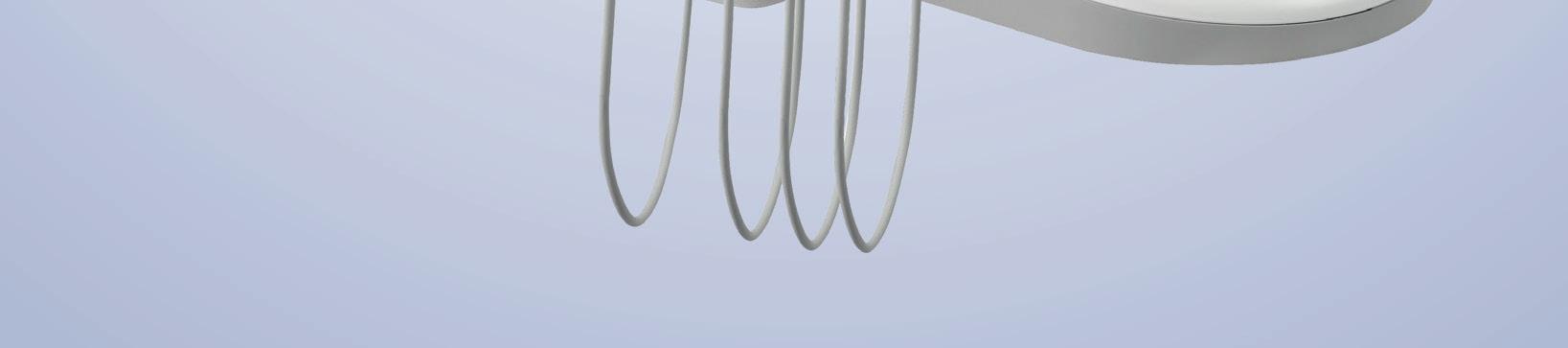
A-dec 300•CORE









A competitive solution that doesn’t betray A-dec quality. A-dec is thrilled to announce its latest promotion for the UK & Ireland - the A-dec 300 CORE package! This configuration is set to provide dentists with the ultimate combination of functionality and flexibility at a great price point.
• Fully Ambidextrous A-dec Chair
• Traditional Delivery System including; 3/1 Syringe, 2 x Midwest Outlets, Acteon Scaler
• 3-Position Assistant’s Arm including; 3/1 Syringe, HVE and SE, Standard Touchpad
• Tray Holder
• LED Light Scan the QR code or contact us for a full specification.





The Daily Mirror made headlines of its own across the dental community in January with the launch of ‘Dentists For All’. The national campaign arrived accompanied by an article penned by Martin Bagot: ‘Britain’s dental health crisis exposed as hundreds of children in hospital with bad teeth*’. The piece highlighted the latest data to the general public, showing that 40% of children do not receive regular NHS check-ups and that 104,133 children went to hospital with rotten teeth over the past five years. In 2022 alone, there were reportedly 116 extractions every day.
The BDA welcomed the national campaign to save NHS dentistry. With patients in Bridlington now facing nin- year waits for NHS care, ‘Dentists for All’ sees the paper throw its weight behind the calls for wholesale reform of the discredited NHS contract fuelling the current access crisis.
The Mirror is making 3 demands:
1. everyone should have access to an nHs dentist: More than 12 million people were unable to access NHS dental care last year – more than 1 in 4 adults in England. At the same time 90% of dental practices are no longer accepting new NHS adult patients. Data from the House of Commons Library showed 40% of children didn’t have their recommended annual check-up last year.
2. Restore funding for dental services and recruit more nHs dentists: The UK spends the smallest proportion of
its heath budget on dental care of any European nation. Government spending on dental services in England was cut by a quarter in real terms between 2010 and 2020. The number of NHS dentists is down by more than 500 to 24,151 since the pandemic.
3. Change the contracts: A Parliamentary report by the Health Select Committee has branded the current NHS dentists’ contracts as “not fit for purpose” and described the state of the service as “unacceptable in the 21st century”. Dentists also get paid the same for delivering three or 20 fillings, often leaving them out of pocket. The system should be changed so it enables dentists to treat on the basis of patient need.
While the UK Government has repeatedly stated its goal is to ensure everyone who needs NHS dentistry can access it, there is no evidence of action to deliver on that ambition.
Ministers have rejected calls from the Health Select Committee for a decisive break from Units of Dental Activity and have dragged their heels over publication of a recovery plan first pledged last Spring.
“A wealthy 21st century nation has seen its citizens pulling out their own teeth with pliers, while others queue from the crack of dawn to access care,” says British Dental Association Chair Eddie Crouch. “Underfunding and failed contracts, the crisis millions face is the result of political choices. The Mirror is
showing leadership we desperately need to see from Westminster.”
The Mirror’s campaign prompted the Association of Dental Groups (ADG) to restate its own campaign to boost Britain’s dental workforce. As Britain’s dental crisis deteriorates, ADG is urging the General Dental Council (GDC) to speed up the approval of qualified dentists through the overseas registration exam (ORE). At present, there is a bottleneck of 2,000 overseas dentists waiting to take the ORE, which is characterised by lengthy delays.
As Neil Carmichael, Chair of the ADG, explains: ‘That’s 2,000 dentists that could be practising, at a time when the UK dentistry is crying out for greater resource.’
Martin Bagot published another piece in The Mirror just three days later, spotlighting the rise in mouth infections leading to sepsis**.
The Mirror reports a dentist working in secondary care in the north of England, speaking anonymously, who observed: “We’re now seeing patients dying from toothache. We’ve never witnessed this before, and there have been multiple cases. One patient came into A&E, was intubated immediately, but died of dental infection without ever regaining consciousness.” n
*https://www.mirror.co.uk/news/ uk-news/britains-dental-health-crisisexposed-31916816
**https://www.mirror.co.uk/news/health/ oral-cancer-surging-uk-amid-31924464
Christie & Co, has launched its Business Outlook 2024 report, which reflects on the themes, activity and challenges of 2023 and forecasts what 2024 might bring across the industries in which Christie & Co operates in, including in the dental sector. The report makes the following predictions:.
• The transactional volume within the market to rebound. However, it’s anticipated that these levels will still fall short of the peak witnessed in 2022. This forecast suggests
a gradual recovery and stabilisation of market activity, moving towards a more sustainable pace in comparison to the previously heights reached.
• M&A activity from corporate operators will reflect a strategic recalibration, with these entities showing restraint in their investment choices and a heightened focus on longterm value over immediate expansion.
• During a period where corporate entities are exercising enhanced selectivity in their acquisitions, experienced multi-site
independent operators and first-time buyers are poised to capitalise on this opportunity. This scenario presents a prime opportunity for these operators and newcomers to expand their foothold in the market and establish a stronger presence.
• Some group operators will continue with strategic plans to review and divest underperforming or non-core sites, reflecting a focused effort to streamline their operations and enhance overall efficiency. n
Registration for the 2024 British Dental Conference & Dentistry Show (BDCDS), co-located with Dental Technology Showcase (DTS), is officially open. The events are set to take place on the 17th and 18th of May at the NEC in Birmingham.
Alex Harden, Portfolio Director at organiser CloserStill Media, commented: “We are excited to bring together the dental community for two days of learning, innovation, and collaboration. This year, we’re pushing boundaries – not only
will attendees get to witness the evolution of dental practice, but they’ll also be part of a movement setting new standards in patient care. So, this event will be a cornerstone for dental professionals seeking to advance their knowledge and practice.’”
The extensive conference programme will be taking place across 14 theatres with over 150 hours of CPD to choose from.
Confirmed speakers so far include Paul Tipton, Simon Chard, Finlay Sutton, Lisa Bainham, and Maria Lessani.
The British Society of Dental Hygiene and Therapy (BSDHT) has reported that the 2023 poster competition, sponsored by Colgate, was an unequivocal success. BSDHT members were invited to submit an abstract in advance of the OHC. The Society was thrilled to receive a total of 12 entries, 10 of which were forwarded to the final judging stage, the quality of which surpassed expectations by showcasing remarkable creativity, skill and passion for their subject matter. All posters were prominently displayed in the hall of the Oral Health Conference Bournemouth for public
viewing and attracted a steady stream of conference delegates interested in the high-quality content.
The winners were as follows:
1st: Vaida Kaunaite - Beyond bouncing back: Exploring undergraduate dental profession students’ perceptions of resilience.
2nd: Laura McClune - A mixed method study to establish the current level, nature and attitude to the provision of treatment under direct access for dental hygienists and dental therapists who are members of the British Society of Dental Hygiene and Therapy.
3rd: Clare Haylett - What intervention delivery methods are the most advantageous
new service launched in nottingham
Nottingham City Council is working with Community Dental Services CIC (CDS) to launch a new oral health improvement service. The Nottingham City Oral Health Improvement Team will focus on improving oral health and reducing health inequalities across the city. Maintaining good oral health has a significant impact on overall health and quality of life, while poor oral health means people often cannot participate fully in society due to pain, poor nutrition and loss of confidence. In England, tooth decay is still the most common reason for hospital admission in children aged between six and ten years. However, it can impact on individuals of all ages. The team will deliver the oral health programmes, based on local need, working with partners to target where they can have the greatest impact. n
Holding all GDC hearings remotely would disadvantage certain dental professionals undergoing a fitness to practise investigation, the Dental Defence Union (DDU) has said. The DDU made the comments in its response to GDC proposals that all practice committee and registration appeal committee hearings will be held remotely by default. Under the proposals, dental professionals would have to make a specific request for a hearing to be held in person. The consultation is open until 12 February and dental professionals can review the proposals and respond with their views n
The Enhanced CPD Theatre is back by popular demand for 2024 and will cover all the relevant updates in dentistry standards alongside essential topics such as consent and dentolegal issues, medical emergencies, and dental radiography.
Registration is free for dental and lab professionals, and can be completed online through the official websites. For more information and to register, please visit birmingham.dentistryshow.co.uk for BDCDS or the-dts.co.uk for DTS. n
at improving the oral health of prisoners and the efficacy of prison dental services? n

Cavity Training, a leading provider of dental nurse training, has started automatically enrolling all of its student dental nurses as Student Members of the British Association of Dental Nurses (BADN).
“BADN membership embeds the concepts of professionalism, ethics and life-long learning into dental nurse training, and involves student dental nurses in the dental nursing community,” said BADN Honorary President Joan Hatchard. “We are delighted to welcome Cavity student dental nurses into the BADN family.” n
The new year has brought some changes in leadership at Frank Taylor & Associates (FTA), with Oliver Acton taking over as Managing Director. Oliver has been Creative Director of FTA Media since January 2018, a role he will continue to perform alongside his new responsibilities.
Lis Hughes will remain in the business to ensure a smooth handover and continue to drive the next-generation strategy. “Oliver is a logical successor and a natural leader,” commented Lis. “He will help strengthen our position as the leading expert in the selling and buying of dental practices in the UK.” n




Ionce worked in an open-plan practice. This was in the 90s. And it was glorious.
The octagonal ground floor was where the two private practice owners worked. The area had about six units, separated by low screens, where the dentists and two hygienists operated. It was similar upstairs, where us NHS folk dwelt. The beauty of open plan, for me, was that I could hear everything my colleagues were saying and it was reassuring to hear that they were having as hard a time of it as I was and, for the first time in my practising career, I didn’t feel isolated. It was nice to know I wasn’t the only one.
I doubt that sort of surgery arrangement would be allowed nowadays - what with the CQC and confidentiality and all that - but I found the arrangement incredibly cosy, especially when a colleague would often poke his head over the screen out of my patient’s line of sight to give me a wink, a thumbs-up, or an incredibly rude gesture if he didn’t agree with what I was saying to my patient.
The two principal dentists were inspirational. In fact, one of them had been my dentist from the mid-70s and, as a direct result of my treatment with him, I decided to go to dental school. Both the dentists always appeared super-cool and relaxed, and were always happy to give advice if sought. One day, at the end of a session, I went down to the ground floor and heard laboured grunting noises coming from Dan’s unit. I stealthily looked over the partition to find him making the unearthly noises as he bashed sevensorts out of a rubber stress ball, which was modelled in the shape of a dental lecturer I once knew in the Prosthetics department.
“Saves me hitting my head against a brick wall,” he said, embarrassed, when he spotted me. He then said two words which told me everything: “Perio patient.” He needed to explain no further. I was sceptical about the efficacy of the stress ball, but since he led me into dentistry in the first place, I was prepared to accept Dan’s assessment as scientifically proven - though I never indulged in pummelling a rubber man’s face to relieve my stress myself. Having witnessed a normally sane man carrying out the procedure close up, I decided to preserve my dignity and self-respect.
I have always felt that dentistry is an incredibly stressful way to make a living but, last night, I caught up with the first three episodes of ITV’s Mr Bates vs The Post Office and came to the realisation that I really don’t know what REAL stress is. The TV drama hit home with me since, around 2005, one of my patients was one of the victims of the Horizon scandal. My patient had been postmaster at a local village store and had been accused of misappropriating £16,000 from the post office in which he had worked for about 20 years. That suspended postmaster had been told by Post Office investigators that he was the ONLY person who had claimed to have experienced problems with the Horizon system, despite the fact that shortly after he had been accused of fraud, he met dozens of postmasters through a newly formed action group, who had been similarly accused of embezzlement. They were all relieved to find others in similar

circumstances. They had all felt isolated. I don’t know what happened to my patient. I was told that he had moved away from the village after he lost his livelihood. Now, I wouldn’t for a millisecond suggest that the horrific nightmare the postmasters have had to endure has any parallels in dentistry, but the way ordinary, honest people working for the post office had their protests of innocence ignored, despite the growing evidence that the Post Office was shielding a faulty computer system, does have some resonance with dentistry. A few minutes ago, as I type, on Radio 4’s The Great Post Office Trial , one contributor referred to the Horizon system as “Not fit for purpose.” Now, where have we heard that before?
I’ll tell you exactly where you have heard it before. It was when a Health Select Committee in Parliament agreed that the NHS dental contract was “not fit for purpose” in 2022. And yet, still it exists in its current form. Heaven only knows how big the stress balls that people like BDA Chair Dr Eddie Crouch and GDPC Chair Dr Shawn Charlwood have to utilise when dealing with such an obdurate Health Department, led by a gaslighting Tory Government.
I use the term ‘gaslighting’ advisedly. How else would you describe a Prime Minister’s assertion in January 2023 that, “As a result of the newly reformed NHS dentistry contract, there are now more NHS dentists across the UK with more funding, making sure people get the treatment they need”?
‘Newly reformed NHS dentistry contract.’ Dwell on that for a minute…
WHAT??
The minimal tweaks introduced by the Government in 2022, that the BDA referred to as “modest and marginal fixes
to the widely discredited NHS dental contract”, could hardly be described as ‘newly reformed’. Yet, that was what the Government labelled them. Just like the postmasters, who are we to argue?
Well-reasoned arguments against the introduction of the UDA-based dental contract were trampled over in 2005 when Labour ploughed through all the warnings that it would be a disaster and soldiered on, to ultimately create a disaster that subsequent Tory and coalition Governments seemed quite happy to let fester.
But Government gaslighting seems to have taken an almost sinister turn when it was recently found that prominent Members of the Government have been sending out letters to BDA members – actual dentists - which contain a blatant falsehood.
One letter sent by Dominic Raab said: “The government has recently announced an average pay uplift for dentists of 8.8 per cent, with the aim of retaining more dentists and improving service provision.”
In September 2023, Dr Charlwood confirmed that only a 5.13% uplift would be imposed for GDPs in England. He wrote on the BDA website, “Despite the extremely high levels of dental inflation, this allows for an uplift in respect of practice operating costs of just 3.23%. This is insulting and outrageous. It bears no relation to the actual increases in the costs for delivering NHS dentistry.”
Of the letters sent out, Dr Crouch said, “I hope this is a simple error, but identical messages have been received from several MPs, including members of the cabinet. When recovery plans are being pulled together, mistakes or misrepresentations like this can have real consequences.”
But it’s not only the Government that indulges in gaslighting and obfuscation. I wrote in December that the General
Dental Council’s media office said it would not “proactively provide additional commentary and spokespeople from the GDC, including on matters related to fitness to practise,” when reporters from the news outlet GDPUK asked questions about Fitness to Practise investigations and the potential suicide of registrants. The GDC has effectively shut up shop on answering questions about the longawaited results of its ‘research project’ into the deaths of 16 registrants between 2019 and 2021. It has been 13 months since the investigation was commenced, yet the GDC has delayed the release of its ‘findings’ because it requires “expert advice on interpreting and presenting the data”. I wonder how much longer that is going to take, bearing in mind the interest expressed by registrants? Hopefully the GDC isn’t using the Post Office as a role model, or it would take nothing less than an ITV blockbuster to shift them into gear.
Meanwhile, Dame Andrea Leadsom, the Government minister responsible for dentistry, is working “flat out” on the Dental Recovery Plan and says that it will be announced “very shortly”. Do we believe that? Not that it will be delivered very shortly - but that it will recover NHS dentistry.
If you DO believe that, I have an amazing 100% cure for stress I can sell you, for only 250 quid. Although, to be honest, like Dame Andrea’s promise, it just looks like a load of balls. n
About the author ollie Jupes is the pseudonym of a former nHs dentist. He monitors dentistry on twitter X as @DentistGoneBadd


Manufacturer’s Lifetime Warranty


12-Month Interest Free Payment Plan

“ The customer service has been exceptional. From visiting the practice within a few days of contacting Swallow Dental, all the way through to a tailored product description, measurements and delivery of the loupes…”
















“ The loupe is positioned so low that I can see directly out of my glasses without having to tilt or adjust my head to see over my loupes, it’s amazing to see how much I was tilting my head with my previous loupes…”




We recently published the results of a survey, which revealed that over one third of the dental professionals surveyed (35%) said they were unable to take breaks during the working day and did not eat or drink. The lack of intake of fluids or nutrition has been shown to impair performance.
More than half the respondents (52%) said they felt emotionally exhausted to the extent that it was affecting their mental wellbeing. The pressure to deliver high-quality dental care only exacerbated their symptoms. Alongside this, 36% also said the fear of dentolegal issues arising from staff shortages is having a negative impact on their mental health.
Healthcare practitioners have a responsibility to put the interests of their patients first. It is not surprising, therefore, that clinicians will occasionally make personal sacrifices – so-called discretionary effort – to ensure that patients are treated and receive any necessary care. The pressures to meet performance targets only add to the burden and encourage clinicians to consistently forego breaks, skip meals, and go without nourishment for lengthy periods.
Studies into performance and human factors support that hunger and thirst are significant factors in patient safety incidents. Even moderate dehydration levels have been identified to adversely affect cognitive function and performance 1 . It has been quoted that a deficit in body water of as little as 2% body weight can impair physical performance. The fact that over half of
the members surveyed told us they are worrying about how exhaustion and burnout are impacting the safe delivery of patient care demonstrates how significant this is for the profession.
Working under such conditions, and not being able to deliver optimal care, inevitably risks burnout, causing staff to be absent from work or choosing to leave the profession altogether.
At a time when practices are already reporting difficulty in recruitment, this further adds to the practice pressures, and has a knock-on effect on the health of remaining staff.
Clearly, feeling exhausted at work is dangerous; it is considered that cumulative tiredness and fatigue can have a similar effect to being under the influence of alcohol. Whilst other high-risk roles have put in place restrictions to prevent people working without a break, this isn’t something that has been fully adopted into a healthcare environment. One study on human factors highlights that tiredness and fatigue affect situational awareness, and warns that healthcare professionals should not think themselves immune while they work many hours without taking a break 2
With the challenges facing the dental industry now, it is all too easy to overlook aspects of wellbeing when faced with staff shortages and patient demands and needs. There isn’t an immediate solution to resolve the dental crisis.
The pressures and stresses caused by recruitment challenges will continue for some time to come, and it is incumbent on all members of the dental team to recognise the signs of fatigue and take action to ensure team members are

taking regular breaks, eating balanced and nutritious meals, staying hydrated, and getting enough sleep each night. These small steps can make a difference in improving wellbeing and ensure that operators continue to practice safely and to a high standard. We would also advise practices to promote a culture that encourages team members to speak up and call out if they are struggling personally or are worried a colleague may be at risk of exhaustion and burnout.

It is positive to see that the NHS recognises the significance of these issues. Recently published information by NHS employers not only highlights the risks arising from fatigue but also provides guidance for employers and employees on steps to avoid this arising 3 Dental Protection has long-been aware of the high pressures and stresses that dental teams work under, and I would encourage any member experiencing work-related stress to make use of our 24/7 counselling service and other wellbeing support, which is a benefit of membership. The counselling service is provided through a third-party partner and is completely confidential. n
1. Parry D, Oeppen RS, Gass H, Brennan PA. Impact of hydration and nutrition on personal performance in the clinical workplace. Br J Oral Maxillofac Surg. 2017;55:995–8
2. Brennan & Oeppen, 2021. Human Factors Recognition to Enhance Team Working and Safer Patient Care. https://link.springer.com/ chapter/10.1007/978-981-15-1346-6_42
3. Sleep, fatigue and the workplace | NHS Employers https://www.nhsemployers. org/articles/sleep-fatigue-andworkplace • https://link.springer.com/ chapter/10.1007/978-981-15-1346-6_42 • https://link.springer.com/ chapter/10.1007/978-981-15-1346-64_42
About the author Yvonne shaw, Deputy Dental Director at Dental protection

Some decent, different and informed commissioning would help again
In 2002, when I was approached about joining the Department of Health with a view to helping address the major difficulties people were then facing in accessing NHS dental care, I would have been surprised to learn that, having made real progress up to 2015, it has been allowed to deteriorate again so seriously. My background in piloting capitation as a way to remunerate dental service providers gave me an insight into how difficult moving to capitation would be but I was certainly not expecting the move to local commissioning would happen so swiftly. I was told, 20 minutes after starting as Deputy Chief Dental Officer in the November, that the introduction of local commissioning was already in the legislative process. The principle was not surprising given that access had been declining since 1992, and the NHS was powerless to improve the situation.
Up to this point, my career had been pretty typical for a dentist involved in dental politics; LDC member, LDC chair, GDSC member and, finally, GDSC vice chairman. At my interview, which was surprisingly challenging, given that I had been pressed to apply, I was asked to give a presentation about how I would tackle the current access problems, assuming the legislation around local commissioning would pass through Parliament. I still have a copy of that presentation! In it, I pointed out that dental services had never been commissioned before and that they would need to establish a team of people who understood what commissioning meant, develop commissioning leads in PCTs and SHAs, and work closely with them from the centre. I also said that there needed to be more investment. Everything in that presentation happened; we set up a dedicated access team run by Primary Care Commissioning, identified commissioning leads in PCTs and SHAs, and agreed that we should all meet face to face every month. We also established a new contract steering group with a focused membership that I pressed should include the BDA. My feeling was that the BDA were nervous about being involved and only agreed when we accepted that they would never agree anything on behalf of their members.
I recently attended the LDC officials’ day on behalf of the British Fluoridation Society and was able to chat with many people who had been involved in those discussions, national and local, many years ago. I got the feeling that there was a real desire among many people who are still committed to the NHS and mixed practice to feel that they were being listened to and to be made to feel that they had a contribution to make. From what I heard, I came to the conclusion that people did not
feel they were being listened to by those at the centre and, even worse, where people in the ICBs (basically SHAs reborn) tried to be flexible and helpful, within the legislation, they were being deterred from the centre.
This clearly has to change. ‘Place boards’ have replaced PCTs and SHAs are now ICBs, but the political pressure is growing just the same as it was 20 years ago. Access improved between 2006 and 2015, and access difficulties were not widespread.
Funding has since flatlined despite patient charges rising far more rapidly than contract values. Progress on developing a more diverse and appropriate workforce is painfully slow and true flexible commissioning is hard to find in spite of the benefits it would bring to patients, providers and the NHS.
Perhaps those at the top of dentistry in the NHS should look again at setting up a dental access programme. PCC are still around, working with ICBs in many areas and, I am sure, could help. The dental schools will no doubt increase their intake but that will take five years to have any impact. Work is in progress to improve the efficiency and capacity of the ORE exam but, without a more sympathetic PLVE system, the growth will be mainly in the private sector. The real risk to NHS dentistry will come if, after the election, either of the two main parties decides to do something radical. The current incumbents seem content to just stand back and let NHS dentistry wither on the vine and, if returned to power (looking unlikely at the moment!), I suspect they would carry on in just that way.
If there is a change at the election, then the BDA must decide whether it will work constructively with a new administration, recognising that Labour were in power in 2006, when the current system was introduced.
At the moment, NHS GDS contracts are open ended, not time limited, and have an agreed contract value which cannot be unilaterally reduced unless there have been a number of years of under delivery. Any change to this nature of contracting would be very risky for those committed, by conviction or necessity, to the NHS, and may not be what was anticipated. We are now in the run up to the next general election, so political leaders will say anything to get elected later this year. It will be after the election that the real work will begin. n
The term, safeguarding, refers to protecting others from abuse, often with professionals, people and organisations coming together to achieve this.
Safeguarding is the responsibility of everyone at your place of work. Usually, a focus is placed on safeguarding children, but adults can be just as vulnerable. You should be aware that you are looking for more signs of abuse and neglect than you would with a child.
According to the Social Care Institute for Excellence (2013), there are seven areas of abuse for adults. That is physical; emotional, sexual, neglect and acts of omission, financial, discriminatory, and institutional.
abuse
Abuse may not be readily apparent. Sandra White, Clinical Director of the Association of Dental Groups and former National Lead for Dental Public Health, explained it: “Sometimes a ‘feeling’ or noticing something that ‘just doesn’t seem right’ can play a vital part in the jigsaw that can make the difference to someone in a vulnerable position.”
You may notice signs such as unusual bruising or being accompanied by another person who prevents them from communicating effectively.
Pay attention to physical and behavioural signs that may indicate abuse, such as unexplained injuries, changes in behaviour, or signs of fear.
Be aware of the patient’s overall demeanour, communication style, and any reluctance to speak openly.
Language barriers can occur as the UK is a diverse and rich cultural community. Patients who do not speak English fluently may want family members or carers who are bilingual there.
However, not everyone will be able to –or might not want to – explain all dental implications. This is why it is important, if possible, to have a translator who can effectively explain what is happening during an appointment.
taking action
You should avoid confronting anyone directly if you suspect there is abuse happening, as you may put both you and the patient in harm’s way. You must give any essential emergency dental treatment needed by the patient.
You can create a private and confidential environment for discussions with patients, especially when addressing sensitive topics related to abuse or safeguarding concerns.
You should not send them to A&E without contacting the medical staff directly in case they do not attend. Maintain thorough and accurate patient records, including detailed notes on observations, conversations, and any concerns related to potential abuse. Document any injuries with photographs, if appropriate and with the patient’s consent. These should be kept confidential and accessed only be relevant personnel.
training in the workplace
In safeguarding you are not alone as a dental practice, and it is important to know where to direct patients in your area if you suspect that they need help.
Keep information ready and available for all staff to contact the relevant parties when they suspect a safeguarding issue. These can all be found online in your local area.
Listed below are the telephone numbers of agencies that may be able to help if you believe a patient is in danger:
• National 24h Domestic Violence helpline for Women: 0808 2000 247
• National Domestic Violence Helpline for Men: 0808 8010 327
• Honour Helpline for advice on forced marriage and honour-based violence: 0800 5999 247
• ChildLine (for children and young people) Telephone: 0800 1111 (free).
• Broken Rainbow for advice and support for LGBT victims of domestic abuse: 0845 2604 460
Work collaboratively with other healthcare providers, social services, and law enforcement as needed. Share information appropriately and responsibly to ensure the safety of the patient. Training should be given to every member of staff and at regular intervals. Everyone should be made aware of their roles and responsibilities within your practice. You could find some case studies to show your staff, so they can see the positive difference they can make to someone’s life.
An example of this can be Mrs R, an elderly woman who was being abused after her son was overwhelmed with caring for her. Social workers stepped in and helped both parties to stop the abuse. When contacting support for anyone who you suspect is suffering from abuse, you will have to pass on the following details:
• What your concerns are
• Name of the person at risk
• Age of the person at risk
• Address of the person at risk
If there is no immediate danger, you can speak to your local council’s adult safeguarding team or co-ordinator. You can also speak to the police about the situation. Some forms of abuse are crimes, so the police will be interested.
If you are looking for more resources to help with safeguarding in your dental practice, Public Health England published a toolkit (3 April 2019) - Safeguarding in General Dental Practice: A Toolkit for Dental Teams. This is available online at www.gov.uk.
Oral health is vitally important to general health and wellbeing; being safe and free from abuse is just as important.
About the author
Dr Barry Cockcroft
CBe is the former Chief Dental officer for england and current chair of the British Fluoridation society.

All staff members should also be made aware of the NHS Safeguarding app. This can be accessed via Apple iOS or Google Play. It can also be downloaded by visiting your device’s appropriate app store and searching for ‘NHS Safeguarding’. It provides 24-hour help and has a directory of safeguarding contacts for every local authority in England.
A visit to www.bda.org/safeguarding is also recommended for more information and guidance on how to implement good safeguarding in your practice. n
About the author
Karen Coates, oral Health Content specialist at the oral Health Foundation, and RDn

Despite the pressures currently facing dentistry, patients continue to show their appreciation for individual dental professionals. A DDU survey 1 of over 460 dental professionals found that 90% had received a gift or thank you message from patients over the past year.
The most common gifts were chocolates, which 70% of respondents had received, followed by flowers, which a third had been gifted (33%) and alcohol which a quarter received (28%). The more unusual presents included a home-grown cabbage, a back scratcher, dog toys, and a sheep (which was declined).
Nearly half of dental professionals (49%) said they were as likely to receive a gift now as before the pandemic, whereas a third (38%) said gifts were less likely now.
It’s heartening to know that patients are choosing to show appreciation for the care they’ve received from dental professionals. Of course, none of us expect to receive gifts, especially given the rising costs of living. Many colleagues explained they get as much satisfaction from doing a good job.
This can be problematic because of the perceived risk to dental professionals’ objectivity.
If you are unsure about whether it is appropriate to accept a gift or hospitality, it’s a good idea to seek an objective opinion from a colleague and get advice about the ethical implications from your dental References:


Nevertheless, it can be a morale booster to know patients have gone out of their way to show their appreciation.
However, gift giving can raise ethical dilemmas. Guidance from the GDC on receiving gifts 2 advises dental professionals to refuse any gifts if they could affect or be seen to affect your professional judgement.
Most of those responding to our survey (89%) had no concerns about motives for gift giving. But a small number were concerned a gift may breach professional boundaries (6%) or that patients may be trying to influence a decision (3%).
We recommend you don’t accept expensive gifts. But bear in mind that even small gifts could ring alarm bells in the context of other behaviour. For example, a gift from a patient you suspect has romantic feelings for you. In such situations, it might be better to politely refuse the present, however small.
The DDU believes it is worth recording gifts in a register, even those of low value, in case concerns are raised in future. Only a quarter of respondents to our survey (24%) said their workplace had such a register, while 19% weren’t sure, and more than half (56%) didn’t keep a record. So, this may be an area you want to consider as a practice.
Along with gifts from patients, professional contacts, such as equipment and product suppliers may also offer to treat dental professionals to hospitality or gifts.
1. https://www.theddu.com/presscentre/press-releases/patientsshow-appreciation-with-chocolatesflowers-and-home-grown-veg-ddusurvey-reveals
2. https://standards.gdc-uk.org/pages/ principle1/principle1.aspx
































































Last month, the Labour Party announced their Child Health Action plan. While the Action Plan covers children’s health broadly, one of its seven points contains proposals to address the current crisis in children’s oral health care. It aims to deliver 700,000 extra urgent dental appointments per year, recruit dentists to areas that need them with a targeted enhanced recruitment scheme, and introduce a targeted national supervised toothbrushing programme for 3–5-year-olds in government-funded breakfast clubs. Sir Keir Starmer said on the issue that tooth decay should be “consigned to the history books”. It’s clear to us at Haleon that access to dental care is becoming out of reach, and education around oral health is not sufficient. The rising inaccessibility of dental care and inadequate oral health education has led to one million children never visiting the dentist 1 Meanwhile, oral health professionals are facing extreme pressure, with many looking to leave the NHS, exacerbating the already widely reported ‘dental deserts’ spreading across the UK. Our Dental Health Barometer survey found that over a third of NHS oral health professionals cited time constraints as the top reason for not being able to offer preventative care advice to patients. We want to address this, as
well as to find ways to support oral health professionals by providing this advice outside of the dentist surgery.
As a company with a large portfolio of oral health products and extensive experience working with consumers, patients and oral health professionals, we feel responsible and determined to empower people to practice better everyday self-care, which in turn will help oral health professionals. We have significant experience in this, and through our Shine Bright campaign, we aim to help support schools in providing advice to children on dental care, helping inspire them to keep their teeth bright and healthy. We recognise the pressures that teachers already face and so we’re providing free resources for teachers and parents, to offer an engaging way to teach pupils about oral hygiene at home and at school. Boosting supervised toothbrushing and offering to work in partnership with industry, this proposal could play a part alongside other initiatives, to significantly improve the profile of preventative oral care.
Supervised toothbrushing plays just one key part of our broader initiatives to educate the nation on preventative advice that we’d like to see rolled out further. Research from our Dental Health Barometer found that preventative oral health advice is only being consistently offered to
patients by one third (34%) of oral health professionals. Preventative advice can be defined as proactive dental care and advice that helps a patient to take action to maintain a healthy life. An example of this is lifestyle recommendations, such as reduction of sugar intake. We agree with the Child Health Action Plan and believe that supervised toothbrushing can play its part in tackling the current crisis in children’s dental health. At Haleon, we want to continue to empower children, parents, teachers, and the wider population to educate themselves on habits that can improve their dental hygiene and for them to take oral health care into their own hands. In turn, this will allow patients to avoid more serious dental issues in the long term and alleviate demands on time-constrained oral health professionals.
This education on oral health is as important for the parents as it is for the children to fill the current knowledge gap. Along with teachers, we recognise that we must also help parents to understand the benefit for their children through making informed choices with the right products and solutions, and that they feel supported in doing so. With scientific evidence linking oral health and system health, poor oral health is a key risk factor that must be prioritised for parents.
To summarise, it is critical that children’s dental health is a universally prioritised objective. Collaboration between government, the dental health industry and consumer healthcare is crucial in enabling this. While supervised toothbrushing forms just one point of Labour’s Child Health Action Plan, reinforcing the importance of preventative care is the first step towards finding a solution for the wider current dental issues facing the UK. We eagerly await the government’s Recovery Plan for Dentistry, and we will continue to focus on preventative oral health care as a solution, empowering individuals and professionals, whilst looking at ways to develop new initiatives to support dental professionals in line with the announcement, so that we can improve better everyday health for all. n
Reference
1. British Dental Association, 2nd May 2023, https://bda.org/news-centre/ press-releases/Pages/DentistsGovernment-sitting-on-side-lines-aschild-oral-health-gap-widens.aspx
About the author Bas vorsteveld, Haleon vice president and General Manager Great Britain and ireland.


Use it with reciprocating or rotary movement, with or without the integrated apex locator - you choose.
-Easy to use
-Integrated apex locator
-360º rotatable contra-angle allowing easier access -Cordless


What makes your practice stand out from the rest? Is it your team of specialists?
Your unique décor?
The flexibility you offer patients? In an increasingly competitive environment, it has never been more difficult to distinguish yourself from the crowd. That’s why it’s so important to continually reinvest in the business. From the team you create to your marketing activities and building maintenance, actively working on the business is essential for success in both the short- and long-term.
A major area that dental practices invest in today, is their equipment and technology. In what is becoming an increasingly digital profession, access to some of the latest equipment is vital for dental teams striving to deliver high-quality, efficient and longlasting patient care. There are several ways in which the right equipment can impact the business.
Modern solutions have been designed to improve the quality of care that can be delivered across all healthcare sectors. For instance, health information technology has been identified for its potential to reduce human error, improve clinical outcomes, improve care coordination and increase efficiencies. Specifically within dentistry, intraoral scanners have been shown to be significantly faster and more efficient than conventional impression methods in some cases, with no compromise in accuracy. Improved clinical care and enhanced outcomes are just one way in which clinicians can encourage patient
satisfaction, and therefore their loyalty to the practice. Good patient relationships can also positively influence professional job satisfaction, and a happy team that provides excellent dentistry is the only kind of team that will make your practice truly stand out!
Whether attempting to tackle the backlog of NHS patients seeking care, or trying to grow and sustain your private dental business, productivity is crucial within everyday activities. In the same way that the right equipment and technology streamlines the patient experience, they can also facilitate more efficient workflows for the professional team. You need equipment that functions in the way you need it to, that will adapt to your work rather than the other way around.
The benefits are multiple – smoother daily routines for the team and faster surgery turnaround times mean more patients can be seen with no compromise in quality of care delivered. Not only does this support patient access to care, but it also optimises profitability for the business.
Just as you need equipment to promote efficiency in the practice, you also need it to be reliable. An all-singing-all-dancing imaging machine is a fantastic investment for practices that provide a lot of implant treatment – but it is a worthless addition if it is constantly breaking down.
That’s why practices must invest in technologies that can be trusted to work consistently and correctly. Equipment must

be of a high enough quality to withstand the rigours of daily life in the practice, to be durable and robust. It can help to choose a supplier with a reputation for reliable equipment, and one that offers rapid technical support in the event of a malfunction. It’s important that you are confident you can get your practice back up and running with minimal down time, should an issue occur. You need your business to stand out, but for all right reasons.
Regardless of whether you are investing in new imaging equipment, decontamination solutions or dental units, you want to buy right first time. Most practices will follow a thorough decision-making process in order to adequately research the options on the market and determine which are most suitable for the business. Both the technology itself and the support services available alongside should be measured against the aforementioned areas, in addition to any specific criteria required for your team or patients.
For industry-leading solutions that come with exceptional customer support, consider working with RPA Dental for your dental chair, imaging equipment and decontamination
Facebook stands out as a powerful platform, offering dental businesses an opportunity to connect with their existing and potential patients. However, navigating the complexities of Facebook advertising requires a strategic approach that goes beyond a one-size-fits-all mentality.

targeting: the art of specificity without overkill Facebook’s targeting capabilities are undeniably robust, but there’s an art to leveraging them effectively. Trusting Facebook’s algorithms is paramount, as the platform aims to deliver results that benefit you while showing ads to the right patients. Striking a balance between specificity and broadness is crucial. While it might be tempting to micromanage your target audience, overly detailed targeting can bypass the organic capabilities of Facebook’s AI.
In dentistry, relying on Facebook’s ability to identify trends and engage users can often be more effective than manual targeting. Instead of delving too deep into what you think individual interests and activities are, it’s advisable to adopt a specific, yet broad, approach by only using age and location options.
ad placement: where your ads make an impact
Understanding where your practice’s Facebook ads appear is vital for optimising their impact. Ads can be displayed in users’ News Feeds on both Facebook and Instagram, as well as Facebook and Instagram Stories, the right column of the desktop site, and even extend to third-party apps and websites through the Audience Network. If you’re using Facebook Business Manager, your ads will be seamlessly seen across multiple platforms without the need to run separate Instagram ads.
pixel and retargeting: harnessing the power of data
The Facebook Pixel serves as “big brother” on your dental practice’s website, tracking user interactions and providing valuable insights into ad performance. It eliminates the need for manual retargeting, as Facebook dynamically selects different ads within your ad sets to show to users who have previously visited your website.

This level of automation streamlines the retargeting process, allowing you to focus on creating ad content and your other business needs.
Before you start to look at Facebook advertising, it’s crucial to establish clear goals for your dental practice. Whether it’s building your brand awareness, increasing post engagement, driving website traffic, or generating leads/new patients, your goals shape the direction of your ad campaigns. Here at Connect, we recommend combining brand awareness ads with lead generation ads to ensure an all-bases approach to social media growth. It’s about quality over quantity – focusing on meaningful leads rather than sheer website hits.
needs. A range of technologies are available, including brands like Stern Weber, Castellini, MyRay, KaVo and Mocom. The team are also committed to going above and beyond the call of duty to ensure that you have all the information, inspiration and support you need to bring your vision to life. Dr Mehdi Yazdi has been a customer for some time and comments: “It has been a real pleasure working with RPA Dental over the last five years. They give me on-going support and guidance, to ensure our practice can continue to flourish and grow.”
There are many things you can do to make your practice stand out. Many of these are optimised by utilising the right technology and equipment, so investing wisely in this area is essential. For more detail about the solutions available through RPA Dental, please visit www.dental-equipment.co.uk, call 08000 933 975 or email info@rpadental.net n
about the author adam shaw, sales Director at rpa Dental Ltd.

it’s not a quick fix: have patience in the learning process
Facebook Ads are not a quick fix for your growth. They undergo a learning process to understand your target audience and optimise ads for effectiveness. In the field of dentistry, where the target audience is geographically limited, attention to ad creation and budget allocation becomes crucial. Testing multiple ads is essential to refine the approach and achieve optimal results.
Facebook ads should complement other marketing efforts
Facebook Ads should be like adding a powerful boost to your overall marketing efforts. It’s like having an extra gear in your dental marketing engine. When your Facebook Ads work hand-in-hand with the other ways you promote your practice, such as through offline marketing, emails, or traditional ads, all your marketing is on the same team. This teamwork doesn’t just make your practice more visible – it makes it memorable. n
about the author Jay Dickens, social Media Manager at connect My Marketing - Meta and Google certified. connectmymarketing.com


From LED lighting and the advent of the paperless dental practice to being an amalgam-free zone, dentists up and down the country are seeking new and better ways to improve their sustainability credentials. It’s not just a case of swapping your plastic water cups for paper ones these days, although this remains a good place to start.
Many others have installed a reverse osmosis machine to reduce their energy needs, in respect of generating suitable contaminant-free water for autoclaves and dental unit water lines (DUWLs).
Becoming a sustainable practice can be a daunting prospect. After all, it touches every aspect of the set-up – from the car you drive to the surgery, to the energy provider you choose and the materials you use. For example, take composite resins, these can have environmental impacts during production and disposal. Using sustainable and biodegradable materials whenever possible can help minimise these impacts. Dental professionals can also try to avoid single-use devices where appropriate –by using stainless steel impression trays, prophy cups and suction tips. You can get eco-friendly prophylaxis instruments that are combined with exchangeable tips. This reduces waste, lowers costs and conserves resources because only dull working ends are discarded instead of the entire instrument.
What a waste
Waste generation is a key sustainability issue. Dental practices produce huge amounts of waste including single-use items such as disposable syringes, masks and gloves, as well as disposable materials from dental procedures. Appropriate waste management and recycling programmes can help mitigate the issue.
Indeed, in March 2023 the NHS clinical waste strategy set out NHS England’s ambition to transform the management of clinical waste by eliminating unnecessary waste, finding innovative ways to reuse, and ensure waste is processed in the most cost-effective, efficient, and sustainable way. One of its key aims is to improve waste segregation and compliance by aiming for a 20-20-60 waste split – 20% incineration waste, 20% infectious and 60% offensive waste.
When it comes to instruments, reusable hand instruments have always been essential within the dental practice. They are cost-effective and excellent for infection prevention when cleaned, disinfected and sterilised to the rigorous guidance of HTM01-05/ SDCEP. Disposable products may seem inexpensive upfront but the repeated cost of purchasing the product, the volatility of the price when demand is high, and the inevitable environmental impact of extra waste can make disposables more expensive in the long run.
Steam sterilisation
The best way to sterilise dental instruments is through steam sterilisation. It is highly effective in killing bacteria, viruses and other microorganisms, ensuring instruments are safe for reuse. It is also a method widely accepted and recommended by regulatory bodies worldwide including the World Health Organization. So, peace of mind for both dental professionals and patients!

If you’re worried about the amount of water it uses, don’t be. Steam sterilisation uses minimal water compared to cleaning methods like chemical disinfection. Another sustainable benefit is that it eliminates the need for harsh chemicals, reducing the risk of harmful residues or toxins.
Investing in the right instrument decontamination equipment can help improve your processes and reduce your
carbon footprint. Eschmann offers a range of highly reliable and long-lasting solutions to choose from. The Little Sister SES 3000B autoclave offers both ‘B’ and ‘N’ type cycles, as well as rapid drying to minimise cycle times. With its 17-litre capacity, it can hold five full-size instrument trays so more items can be processed at a time, helping to cut down the amount of water and electricity used. It is also available with the comprehensive Care & Cover servicing and maintenance package, which keeps equipment running efficiently for longer. This means your autoclave can last for many years, helping to send less waste to landfill. Sustainable dentistry is all about delivering high-quality care without damaging the environment. It’s not an easy ask but small steps can often lead to big changes. The Centre for Sustainable Healthcare has developed a practical resource for dental teams wishing to take action to make their practice more sustainable. You can access it at sustainablehealthcare.org.uk/dental-guide. For more information on the highly effective and affordable range of infection control products from Eschmann, please visit www. eschmann.co.uk or call 01903 875787 n
about the author Nicky Varney, Senior Marketing Manager at eschmann.

Whilst we are not in peak allergy season, every dental professional will know that threats can be encountered daily in the dental practice. Some solutions used in the practice can be troublesome for susceptible patients or clinicians, but thankfully unfortunate outcomes can be avoided with an appropriate armamentarium. Allergies can impact oral health over time – potentially resulting in dry mouth or malocclusion from mouth breathing because of irritated airways – but the greatest risks to a person’s health may be posed by the products used in everyday treatments.
powerful reactions
When an at-risk patient interacts with an allergen, they can experience a variety of different effects. At their mildest, an individual may have a running nose or extensive sneezing, maybe even itchy skin or a raised rash. In the most unfortunate situations, patients in the dental practice could experience anaphylaxis. This is an extreme allergic reaction that may transpire as swelling of the tongue and throat, and difficulty breathing or swallowing, amongst other symptoms, and it is life-threatening.
Harmful allergic responses in the dental practice are uncommon, but not implausible. Just this past summer, tabloid news outlets reported on allergic reactions to veneers that left a patient with ‘elephant skin’. Historically, multiple cases have seen young people with dairy and milk product allergies develop anaphylaxis after using toothpaste and mousses containing Recaldent.
These are outliers from standard daily proceedings, but it’s important to know that such cases do exist. Clinicians should put in place provisions for those with known allergies, and be able to proceed appropriately if a patient suffers a reaction whilst under the dental team’s care.
Allergic reactions may take both patient and clinician by surprise. Neither party may be able to predict the effect that a singular ingredient will have, and if a patient has not displayed such symptoms before, a severe reaction could be a shock.
In mild cases, an antihistamine may be enough to treat a patient and alleviate any symptoms. When a reaction is more severe and poses an extreme threat to the patient’s health, then an alternative response could be needed.
The GDC states that dental professionals must follow the guidance on medical emergencies and training updates issued by the Resuscitation Council UK. In their standards for primary dental care, they specify that dental professionals must be educated in cardiopulmonary resuscitation (CPR) and provide other advanced life support skills if trained to do so. This may include specific reactions to anaphylaxis. An ambulance must be called immediately, and the patient placed in a comfortable position to aid in the restoration of blood pressure or the relief of breathing problems. The administration of adrenaline is the firstline treatment in such cases and is allowed to be provided unprescribed by an “appropriate
practitioner” (including dentists) when used from an emergency drug supply. Adrenaline is part of the equipment that practices must ensure they have in case of emergency.
Reactionary measures of this ilk can save lives, and by quickly identifying major problems, patients can receive the highest standard of care needed in any given situation. However, as always, prevention is better than cure.
avoiding a turn for the worse
Within the dental practice, accurate record keeping will help to ensure that people at risk of certain medical emergencies are identified in advance of any proposed treatment.
Consulting patients and their records can help dentists to select the appropriate treatment solutions and minimise the risk of a severe reaction occurring.
There are several potential dental-centric stimuli to trigger an allergic reaction. Antibiotics are the main cause of perioperative anaphylaxis in the UK with an incidence of 4.0 per 100,000 administrations, and amoxicillin, in particular, is most likely to be associated with such a response.
However, perhaps the most prominent allergen risk in the dental practice is, of course, latex. The natural rubber proteins found within latex have the potential to cause asthma, urticaria, and, although rare, anaphylaxis. Allergies to this specific substance are more common among health professionals than the general population, potentially around 9.7% and 4.3% respectively, which increases the need for appropriate measures to be in place for latex-free workflows.
This means providing suitable alternatives throughout the practice, to ensure completely latex-free workflows can be achieved. Practices must be able to demonstrate that they have carried out an assessment to judge which types of gloves they should provide. They should also have an effective glove use policy that takes into account individuals – including both clinicians and the general public – who may have a latex allergy. In any case, the practice should always be prepared for allergen needs. With Initial Medical, dental practices can stock up on a wide range of medical supplies including latex-free gloves. Our glove range is available in sizes extra-small to extra-large and can be bulk bought as 10 boxes of 100 for ultimate convenience, delivered to your door. Although allergen risks are always likely to be present in the dental practice, with adequate training and preparation, potentially harmful stimuli can be negated from treatments. To find out more, get in touch at 0808 304 7411 or visit www.initialmedical.co.uk. n
about the author rebecca Waters, category Manager at initial Medical, has worked in the healthcare sector for the past 17 years and was a research chemist with Bayer cropscience prior to joining rentokil initial in 2003

GRAND ESTHETICS
Delivers Immediate natural-looking esthetics


GRAND RELIABILITY
Stable and strong foundation designed for long term success



GRAND SIMPLICITY
Ease of use at its best One prosthetic platform.

Scan the QR Code and check all the Grand Morse benefits!


GRAND STABILITY
Designed for predictable immediate treatments in bones I, II, III and IV





















































CQUA HYDROPHILIC SURFACE











































e ydrophilic surface presents a smalle ntact angle when in contact with liquids This provides greater accessibility of organic fluids to Acqua implant surface 1)








The use of intraoral scanning (IOS) has increased exponentially over recent years. It has gained a lot of traction in orthodontics and studies have proven both time-efficiency and comfort benefits. Most of these studies are conducted in adult patients and yet a large percentage of the volume of orthodontic patients are children and/ or adolescents.
Indeed, according to the British Orthodontic Society, orthodontics in children is in high demand. In excess of 200,000 children and teenagers in England and Wales have treatment every year, with growing numbers of young people seeking treatment on a private basis.
The paediatric patient presents different challenges compared to adult patients which means a dental professional needs to adapt their way of working with them. So, what advantages can IOS bring for younger patients?
comfort blanket
One of the most significant advantages of IOS in children’s orthodontics is the increased comfort it provides. Children have smaller oral cavities, which makes it more difficult to take impressions whatever method you use. And this may cause more discomfort as a result. However, traditional methods of taking dental impressions often involve the use of messy and unpleasant materials, such as alginate. Children, especially those who are apprehensive about dental visits, commonly find this process uncomfortable and distressing.
The prevalence of dental anxiety in children ranges from 6% to 20% and a 2013 national survey in the UK found very high levels of dental anxiety in 14% of young people aged 12, and in 10% of 15-year-olds. Most children prefer intraoral scanning – one study found that 89.3% of children felt stressed with the conventional methods, compared to 3.6% with the digital method.

Another benefit of intraoral scanning in children’s orthodontics is the improved accuracy and precision of treatment planning. As you know, the digital impressions captured by the intraoral scanner provide high-resolution images of the teeth and gingiva, allowing orthodontists to obtain more detailed information about the patient’s oral structures. This information can then be used to create a precise treatment plan, ensuring that the orthodontic treatment is tailored to the child’s specific needs.
Additionally, intraoral scanning allows for better communication between the orthodontist, the child, and their parents. The digital images can be displayed on a computer screen, making it easier for the orthodontist to explain the treatment process and show the child


and their parents the current condition of their teeth and gums. And what child do you know who isn’t happy looking at a screen? According to Specsavers, children in the UK aged between 5-16 years spend a total of 6.3 hours on screens a day! And furthermore, a study by the National Institute for Health and Care Research, shows that audiovisual distraction slightly reduced the heart/pulse rate in children and improved children’s cooperation during treatment.
Intraoral scanning also offers time-saving benefits for both the child and the dental professional. With intraoral scanning, the digital impressions can be obtained in a single appointment, reducing the overall treatment time. This is especially beneficial for children, as it minimises their time spent in the dental chair. The average attention span of an 8-year-old is 16-24 minutes, rising to 24-36 minutes for a 12-year-old.
perception is all
And while the two methods in children have been found to have a similar time frame, regarding the perception of time, 64.3% of children thought that the conventional method was longer. Similarly, while the gag reflex and breathlessness were found to be similar between digital scanning and conventional impressions, children were significantly more nauseated and less comfortable with alginate impressions than with digital impressions in the maxilla.
Suitable for patients both young and old, the award winning Virtuo VivoTM Intraoral Scanner from Straumann® is a light and small solution (only 130g), ergonomically designed to provide a pen-like grip and exceptional patient comfort. Hard and soft tissue can be scanned from multiple orientations, capturing difficult-to-see areas with minimal effort. Resulting scans are in colour and high resolution. The scanner boasts a removable, autoclavable sleeve in coated metal to ensure proper hygiene for the patient and practice.
Intraoral scanning offers numerous benefits in children’s orthodontics. From increased comfort to enhanced treatment planning, these advantages are transforming the orthodontic experience for children. With its improved accuracy, better communication, and time-saving capabilities, intraoral scanning is revolutionising the way orthodontic treatment is delivered to children. By embracing this technology, dental professionals can provide more efficient, effective, and enjoyable experiences for their young patients. For more details, please visit https://www.straumann.com/digital/us/en/ home/equipment/io-scanners.html n
When US president Abraham Lincoln was shot dead in 1865, the perpetrator, John Wilkes Booth, escaped to Virginia. Discovered hiding in a barn, he was shot dead on the spot. But for many years afterwards, rumours circulated that Booth had escaped and was still alive. So strong was the national unease, Booth’s body was disinterred and examined again in 1893. The family dentist identified the body by the odd formation of his jaw that had been noted in his dental records during a visit for the restoration of a filling.
Similarly at the end of World War 2, rumours were rife that Adolf Hitler had escaped and were only quashed when remnants of a bridge were identified in the pieces of his jaw that matched his dental records, and was confirmed by his dentist Hugo Blaschke.
While extreme examples, they do illustrate just how important accurate dental records can be. They are a valuable tool for identifying individuals, especially in situations where traditional methods may not be possible, such as in cases of accidents, natural disasters, or criminal investigations.
Each person’s dental structure is unique, and dental records can help in establishing a person’s identity. By comparing dental records, such as dental x-rays, bite marks, and other dental evidence, forensic experts can also identify suspects, victims, or missing persons in criminal investigations or mass disaster incidents.
Of course, good record keeping is a regulatory requisite of competent professional dental practice. It is essential to the provision of safe and effective care. In general, the function of good record keeping is to support:
• Patient care and self-empowerment
• Interdisciplinary and patient/clinician communication
• Effective clinical judgements and evidence the decision-making process
• Continuity of care
• Clinical and medico-legal risk analyses and complications mitigation
• Clinical audit, research, allocation of resources and performance planning.
Dental records provide important information about an individual’s oral health history, including previous dental treatments, allergies, medications, and any existing conditions. This information is vital for dental professionals to provide appropriate and personalised care, monitor progress, and make informed treatment decisions.
They are also essential for legal purposes. They can be used as evidence in legal cases, insurance claims, personal injury cases, and compensation claims. Detailed documentation of oral health, treatments, and conditions can support claims or refute false allegations.
Digital technology has revolutionised the record keeping process, of course, allowing the dental team to work faster, smarter and more efficiently than ever before. There was a time, not so long ago, when a patient record would have consisted of paper forms held in a paper folder with written notes and some radiographic films.
The advent of electronic records including digital images and scans provide safer, quicker and more detailed information than traditional technologies. When data is digital, the dentist and patient can benefit from high quality clinical information, enhanced diagnostic capabilities and more efficient implementation of major treatment plans. Patients always have the right to access their notes and may request a copy of their records. Electronic records are easily shared and allow patients to review and fully consider their options when deciding and consenting to a course of treatment, for example. This transparency can foster a sense of trust between dental professionals and patients, and encourages collaboration in treatment decision-making which is always a positive.

To help busy dental professionals, Kiroku, the AI digital note taking platform, has introduced Kiroku Docs that converts clinical notes – including those from patient records – into documents at the click of a button. Kiroku Docs can generate many different types of documents, including consent forms, treatment planning letters and referral letters, from the notes taken. Each fully customisable document template pulls the relevant information from the notes guaranteeing no duplication of effort. Given that clinicians need to communicate with a wide range of people (from patients and specialists through to insurance companies), Kiroku Docs can also adapt the language it uses. For example, it can translate complex clinical terminology into layman’s terms. With dental professionals being required to record ‘complete, accurate and contemporaneous’ notes and the GDC specifying that you must record ‘as much detail as possible’, the advent of the digital age makes a patient’s dental records more robust than ever. They help ensure accurate and personalised dental care while serving as a valuable resource in various legal and forensic contexts. They give patients a greater involvement and understanding of their care too which serves to improve the entire dental experience. Now that’s really something to take note of.
To find out more about Kiroku, or to start your free trial, please visit trykiroku.com n
about the author Hannah Burrow, ceO of Kiroku.










Effectively engaging with dental patients affords an array of advantages for both the patient and the practice. Individuals will be better educated, more informed and more confident in the services they receive from your practice. The business also benefits from happier and more devoted patients who return to the practice for many years to come. There are several ways to build the patient-practitioner relationship, and modern technologies should be considered in order to assist the process.
Building rapport
As is the focus in every aspect of dentistry, establishing and developing rapport with patients is important for delivering highquality care. When patients feel they can be honest with their dental team, a more comprehensive picture can be pieced together, enabling the dentist to more accurately tailor treatment according to their needs. By better understanding a patient’s motivations, fears and constraints, a dentist can also make specific at-home oral hygiene recommendations for more effective results.
Building a positive rapport with patients affords a myriad of benefits for the dental team and practice as well. A US survey found that improved patient relationships led to a significant uptick in income for dental practices. In addition, a strong patient-dentist relationship is associated with increased patient satisfaction and loyalty to the practice, meaning happier patients that keep coming back.
A major barrier to good dentist-patient relationships is trust, though this is difficult to measure. A Norwegian study showed that levels of trust and confidence in dental practitioners among older patients were directly related to their oral health-related quality of life. It is widely acknowledged that effective communication is a cornerstone of earning this trust from patients.
patient engagement
Research has shown that good patient communication also leads to more patientcentred care, enhanced compliance with treatment plans and better health outcomes. Additionally, it has been proven that good quality communication encourages greater patient involvement in their oral health decision-making.
Many of the main barriers to patient engagement can be overcome by building rapport and ensuring effective communication, but other aspects require a different approach. For instance, time constraints in the busy dental practice can make it difficult to explain oral health status or treatment procedures in adequate detail to facilitate patient understanding. Therefore, finding ways of streamlining the professional workflow to create more time with the patient will also be hugely beneficial.
effective communication
For all these reasons and more, it is essential to develop a strong patientdentist relationship through effective communication. Many patients will require an amalgamation of communication techniques to really benefit, including both verbal and non-verbal tools.
Regarding the former, it’s vital that clinicians use easy-to-understand language when describing a patient’s existing oral health condition. This can be greatly improved with the use of visual aids like images, diagrams and videos. Such resources can also be useful when explaining treatment procedures, which can help to manage patient expectations and support informed consent.
Beyond this, consideration must also be given to how patients are communicated with outside the practice. Maintaining their engagement with oral health between appointments is crucial, and can be achieved by finding effective and convenient ways to interact with them throughout the year. Using appropriate and easily accessible technologies can not only make this part of the patient relationship more effective, but also more efficient for the dental team, saving precious time and other resources across the business.
For example, industry-leading practice management software available in the market today offers a solution for digitalised and automated document management, in addition to improved patient accessibility to their treatment information. AeronaDental software offers an innovative Design & Sign feature, which digitises practices’ documentation processes. Dentists can create templates for frequently used files, saving time and ensuring consistency in formatting. Patients can also access and sign these documents with ease, from the comfort of their own home, with complete peace of mind that the integrity and confidentiality of data is protected.
the foundations of better health
The relationship between patients and the dental team must be carefully curated for high-quality care and patient engagement. Making sufficient time and using suitable tools to do it right will have a substantial impact on both patients visiting the practice and the business itself over time. Patients are empowered to take more responsibility for their wellbeing and comply with professional recommendations for improved oral health. The resulting boost in patient satisfaction is also nothing but good news for the practice, which benefits from a stable clientele, as well as word-of-mouth recommendations.
For more information, please visit aerona.com n

about the author
Mark Garner, General Manager, areona Dental.

Within a profession which is constantly developing thanks to the continuous integration of new technology, making wise investments is an excellent way to stay ahead of the competition. However, sometimes, this can be easier said than done. With so many options available on the market, it may be difficult to assess which options are most appropriate for your unique dental practice. The right investment may be the key to boosting diagnostics and treatment success, and helping more patients say ‘yes’ to treatment.
While cone-beam computed-tomography (CBCT) scanners are not an essential piece of equipment for all dental practices, for many they are ideal for improving diagnostic capabilities and treatment planning, and for carrying out regular treatment reviews. CBCT scanners produce highly accurate images which enable clinicians to clearly visualise the clinical situation, and make accurate assessments – proving very useful across a range of clinical scenarios including dental implants, orthodontics, and endodontics. It is important to take into account the risks of radiation in every case, and CBCT should only be used if the benefits outweigh any potential risks. The recommendation in any case is to use the smallest possible field of view, and the lowest radiation exposure to reduce any risks to your patients. Cases should also always be selected carefully, to ensure that imaging is justified and benefits the patient.
In practices which regularly provide dental implant treatment, it can be very helpful to have a CBCT scanner, as imaging is usually required throughout the treatment process. CBCT may be used to evaluate the linear measurements of the ridge height, width, and bone quality, assess the surface topography of the alveolar ridge, as well as illustrate the relevant vital anatomical structures, and recognise any incidental pathology (such as airway asymmetry, endodontic lesions, and temporomandibular joint disorder).
Its accuracy and image clarity can be ideal for diagnosis, allowing clinicians to firmly conclude whether dental implant treatment is appropriate. It can also improve treatment planning, when used alongside relevant software, high-quality imaging ensures accuracy. This can also improve treatment acceptance as patients are able to clearly understand their treatment plan, allowing the clinician to deliver a clear explanation.
CBCT imaging is particularly useful in the diagnostic stages of endodontic treatment. Scans are able to improve diagnostic accuracy, and increase confidence in diagnosis, decision making, and treatment planning. CBCT Imaging may be used to asses for dental trauma, root resorption, vertical root fractures, and root canal anatomy. This allows clinicians to provide a more accurate diagnosis, and develop the most appropriate treatment plan for each individual case.
CBCT imaging can make orthodontic treatment more predictable, allowing you to treatment plan with accuracy, and enabling patients to have a clear idea of their clinical situation, and of how their treatment will likely progress. This, in turn, helps to manage patient expectations, increase acceptance, and boost patient satisfaction. This type of imaging, when used in orthodontics, is commonly indicated to assess anomalies of dental positions, like impacted or ectopic teeth for example, as it allows the visualisation of impacted teeth in detail, offering a threedimensional view of the situation.
Having a CBCT scanner in the practice will reduce the number of referrals needed, and therefore the number of appointments patients are required to attend, and accessing imaging quickly will mean that treatment planning can proceed as soon as possible. When you choose the Axeos 2D/3D specialist system, available through Clark Dental, you can experience the best of 2D and 3D imaging, all in one device. The Axeos offers 4 volume sizes, from 5cm x 5.5cm to 17cm x 13cm, giving you more flexibility for a range of applications. Investing in the most appropriate equipment for your unique dental practice will inevitably improve treatment workflows and outcomes, and lead to the increased satisfaction of your patients. While it is important to consider the effects that radiation may have on patients, weighing up the benefits and risks, in cases where it is appropriate, CBCT imaging serves as a useful diagnostic tool across a range of clinical scenarios.
For more information call Clark Dental on 01268 733 146, email info@clarkdental. co.uk or visit www.clarkdental.co.uk n
about the author Stuart clark, Managing Director, clark Dental.


BioMin® F is the only toothpaste that delivers low level Fluoride with Calcium and Phosphate ions continuously for 12 hours after brushing. These combine to form Fluorapatite on the tooth surface ensuring the teeth are 10 times better protected to survive acid attack and therefore less prone to decay.
Soluble Fluoride, used in all other toothpastes, is rapidly washed away by saliva and has little clinical benefit just over an hour after brushing.
BioMin® F solves the problem of traditional soluble Fluoride toothpastes.
BioMin® F bioglass is the result of 15 years research and development at Queen Mary’s University, London. Uniquely, this slowly dissolving bioactive glass adheres to tooth structure releasing optimal proportions of
Calcium, Phosphate and Fluoride ions over a 12 hour period after brushing. In contrast traditional Fluoride toothpastes contain soluble Fluorides which are rapidly washed away by saliva and ingested.
Developed over 20 years ago, NovaMin® represents the first generation bioglass used in toothpastes though it was not originally developed for this purpose. It had initially been formulated for bone grafting. Only later was it used in toothpastes because of its adherent and slow dissolving capabilities to release Calcium and Phosphate. It does not contain Fluoride nor optimum proportions of Calcium and Phosphate minerals.
First generation NovaMin®, the active ingredient in Sensodyne Repair and Protect, is a bioglass without Fluoride. Repair and Protect incorporates additional soluble Fluoride which rapidly washes away like all

other saliva soluble Fluoride toothpastes. In contrast, BioMin® F represents a more advanced second generation bioglass, which has been specifically developed for dental applications and is uniquely formulated to slowly release Fluoride, Calcium and Phosphate ions over a 12 hour period after brushing. It facilitates rapid and continual production of stable, acid-resistant Fluorapatite within dentinal tubules and on tooth surfaces.
BioMin® F with controlled release Fluoride facilitates constant Fluorapatite development on the tooth surface, which increases the acid-resistance of natural tooth enamel by 1,000%. All other toothpastes contain soluble Fluoride salts that are rapidly washed away providing far less protection.
the Fluoride 1350, 1450 and 1500 misconception
Some wrongly believe that the optimal toothpaste should contain 1,500ppm of Fluoride. This figure is not based upon optimal clinical benefit, but is simply the legal maximum a toothpaste can contain without having to comply with more onerous product registration requirements. No manufacturer can add more Fluoride to a toothpaste without a Pharmaceutical Product Licence. Manufacturers add as much soluble Fluoride as they are legally allowed to in order to maximise preventive properties before the Fluoride is washed away. BioMin® F does not have this problem because of its controlled continuous release of Fluoride with Calcium and Phosphate. Brush twice a day with BioMin® F and Fluoride is ever present doing a fine job!
BioMin® F – Safer than high Fluoride toothpastes
The higher the Fluoride content the greater the risk of Fluorosis by accidental imbibition, especially amongst children and people more prone to swallowing their toothpaste.
With its dramatically lower 530ppm Fluoride content this risk is minimised, whilst still delivering 12-hour Fluoride protection!
Brush twice daily for 24-hour Fluoride protection and reduced sensitivity
BioMin® F has been formulated to contain Fluoride, Calcium and Phosphate ions in the optimum proportion for rapid remineralisation. What’s more, as the oral pH decreases after consumption of sugary and acidic food and drink, the bioactive glass dissolves quicker, resulting in even faster release of these minerals, which in turn neutralises acid helping to stabilise the pH further and helping to protect the teeth from decay.
BioMin ® F bioglass particles are engineered to be 60% smaller than those found in NovaMin® products, resulting in less abrasivity and deeper penetration of the dentinal tubules with acid resistant Fluorapatite. So, the formation of Fluorapatite is not just on the surface of the teeth, but also deep within the dentinal tubules. The tubular occlusion achieved with BioMin® F is much more resistant to dissolution, providing more effective and longer-lasting relief from dentine hypersensitivity. No other toothpaste can deliver such effective remineralisation of teeth and long-term protection against dentine hypersensitivity, no matter how much they spend on expensive machinery and advertising!
Published research shows that BioMin® F outperforms other sensitivity toothpastes in its ability to block dentinal tubules, resulting in superior and longlasting sensitivity relief (Studies available upon request).
For further information visit the Trycare website, www.trycare.co.uk/biomin, contact your local Trycare representative or call 01274 885544. n
We’re lucky to live at a time where we have a broader range of patients entering the dental chair every day. More people are openly expressing themselves as members of the LGBTQ+ community, which can help clinicians identify potentially unique treatment needs.
With greater awareness of the risks presented to these patients, dentists can devise more effective treatment plans for each individual.
Blanket assumptions cannot be made for every LGBTQ+ patient, and they will have completely different oral health statuses dependent on their daily lives.
Being LGBTQ+ does not predispose you to oral health issues, but coping with stresses in daily life – such as homophobia, transphobia, social stigmas, or social isolation and rejection – may contribute to stress and oral healthrelated concerns. For example, lesbian, gay and bisexual adults smoke tobacco and drink alcohol at higher rates than their heterosexual peers, have a higher risk of poor mental health, and have an increased risk of oral disease due to harmful eating behaviours. Each of these have been established as factors for oral health issues.
Another significant threat displayed in a variety of reports in recent years is that LGBTQ+ people are consistently more likely to use drugs than their heterosexual counterparts. The Crime Survey for England and Wales from 2022 observed around 31% of bisexual people and 30% of gay and lesbian individuals had taken an illicit drug in the previous year. This drops to 8% of heterosexual people, which is nearly four times lower.
Cannabis was highlighted as being used
by around 23% and 28% of gay/lesbian and bisexual individuals respectively. With frequent use, patients can expect to experience dry mouth (xerostomia) and periodontal disease. In fact, studies have shown an increased prevalence of gingival disease when a patient smokes cannabis, regardless of tobacco use. In turn, patients need to maintain an effective oral hygiene routine that can minimise its effects or repair the damage caused.
Talking with a patient about their substance use is often difficult; approaching the topic tactfully is essential and must not be interpreted as accusatory or judgemental. It may only be viable to ask relevant questions after trust has been established between clinician and patient, but the answers could support a better suited solution for each patient.
Also within the LGBTQ+ community, transgender patients may present some unique oral health needs as a result of ongoing transitional treatments.
Transgender patients may undergo hormone replacement therapy (HRT) to feel better aligned with their preferred gender identity. Waiting times for referral and treatment are currently very long, but it is key that dental professionals provide exceptional oral healthcare whilst it is being undertaken. Hormones change immunological responses which can potentially put patients at an increased risk of infection. A female-to-male transgender patient may be taking on HRT that increases the production of testosterone, whilst inhibiting oestrogen. An increased immune function has been linked with oestrogen deficiency, meaning patients undergoing this therapy may experience more intense gingival inflammation during periodontitis flare ups.
On the other hand, male-to-female transgender patients may be having HRT that increases oestrogen, and subdues testosterone production. An excess of oestrogen could also result in inflammation, making the development of periodontitis more likely. Not all transgender patients will be undergoing HRT, and they may not feel entirely comfortable disclosing whether they are or not. However, awareness around the topic is helpful when approaching treatment plans, as well as providing excellent care in regular check-ups.
an effective relationship
If these factors are just the tip of the iceberg, what can clinicians do to help? The most important step may be in communication. Engaging with each patient through an individual approach, expressing a nonjudgemental manner and placing pro-LGBTQ+ leaflets or signs around a practice could help patients feel more comfortable and motivate regular dental visits. An effective patient-dentist relationship may also encourage LGBTQ+ patients to open up about personal details such as substance use or HRT experiences. In each appointment, it is essential to reiterate the need for excellent oral hygiene routines, as improved plaque control can reduce gingival inflammation. As such, patients should brush consistently twice a day with a soft bristled brush and fluoridated toothpaste. Interproximal cleaning is also key, as regular toothbrushing is generally unable to clean these sites effectively. A brilliant oral hygiene routine relies upon consistency and the tools used every day. Clinicians could recommend their patients use the Waterpik Cordless Advanced Water Flosser. A compact solution that eliminates plaque in interdental spaces, the Waterpik Cordless Advanced is up to 50% more effective than

traditional floss for improving gingival health. By massaging and stimulating the gums, they are kept strong and healthy with improved circulation.

Diving into the unique challenges that face LGBTQ+ patients is essential for every clinician. By understanding the adaptions needed to everyday care, and creating a welcoming and encouraging environment, dental professionals can ensure this community is optimally treated for the coming years. For more information on Waterpik Water Flosser products visit www.waterpik.co.uk. Join the 3,000+ dental teams who have already benefitted from a professional Waterpik Lunch & Learn. Book your free session for 1 hour of verifiable CPD and a free Waterpik Water Flosser – available either face to face or as a webinar – at waterpik.co.uk/professional/lunch-learn/. n
about the author Susan joined Waterpik as a professional educator over 4 years ago, delivering Lunch & Learn educational sessions to dental professionals.

The link between general and oral health has been widely explored in the literature, and as clinicians we see the impact in front of us every day. We know and understand the importance of holistic approaches to dentistry, but there is a wide-spread change to health that still isn’t spoken about enough within the profession, especially regarding how it can affect implant surgery and restoration.
I’m talking about the menopause, a natural part of aging that traditionally affects women between the ages of 45 and 55, though it can occur earlier. The impact on an individual’s life is significant. Clinicians must consider how it changes a dental treatment plan by looking at some of the larger systemic issues.
a variety of challenges
The menopause can put a patient’s dentition at severe risk of infection and decay. Several hormonal changes occur which can make the gingiva more susceptible to plaque, with an increased risk for gingivitis and periodontitis. The weakened response from the body may be consistent with the increased presence of xerostomia in many patients, with studies observing reduced salivary flow in menopausal women. Losing the antibacterial properties of the saliva may accelerate the development of cavities, tooth decay and oral disease. Saliva also facilitates chewing, swallowing food and speech – a reduction because of hormonal changes can evidently begin to affect everyday life.
However, I want to primarily focus on the significant impact of osteoporosis, in particular, on dental implant success. The Royal Osteoporosis Society says that around 3.5 million people in the UK live with the condition, and half of women over 50 will suffer from it. The menopause creates a deficiency of oestrogen, which is key to the regulation of bone remodelling by controlling the production of cytokines and growth factors from the bone marrow and cells. This leads to the upregulation of immune cells and osteoclasts, and further increases production of boneresorbing cytokines. In turn, patients develop significantly weaker bones during and following this time period.
In the oral cavity, the osteoporotic alveolar bone has diminished tooth support. The literature has made links between osteoporosis and the progression of tooth loss, which may create a greater need for dental implant restorations – but also a change of approach.
The success rate of dental implant surgery is affected by bone quality and quantity at the dental implant site.
The consensus across the literature suggests that osteoporosis has no detrimental effect on implant failure and the percentage of osseointegration. Despite this, the presence of the condition does interfere with the mechanical stability of an implant. Each patient and implant site must be treated for its unique qualities, and closely monitored in the years following
placement to identify potential signs of failure. Clinicians must also consider any other medical treatments their patients are receiving. As a result of the menopause, some individuals could choose to undergo hormonal replacement therapy (HRT). This increases oestrogen in a bid to prevent osteoporosis, and is particularly important in the event of early menopause.
However, despite its promise, HRT has a mixed range of effects on implant success.
Some studies find that HRT can seriously derail implant osseointegration, with lower implant success rates and increased bone loss around implants in HRT-treated individuals – modifications to the regenerative abilities of bone tissues is a commonly cited reason. Other reports find no significant influence on implant success at all. It is not a contraindication for treatment, but patients taking HRT must be informed about their potentially greater risk of osseointegration failure and choose whether to continue from there.
There is still the opportunity to provide excellent results in the face of these challenges. A bone graph may be required in some cases. It could be carried out prior to or simultaneously with implant placement, and has become a reliable technique for restoring bone loss. The material used may differ between patients; both autogenous bone or bone-like substitutes are suitable options.
This should only be used in the appropriate cases – some post-menopausal patients may
still retain sufficient bone density in their jaw for a successfully placed implant. However, when judged to be ideal, placement can provide an excellent foundation for an implant treatment.
Clinicians must be well-trained and confident in placing both the implant and the bone graft, not only to follow GDC guidelines, but to deliver the best possible result for the patient.
Developing your skillset and providing care to patients like those going through the menopause is possible with One To One Implant Education. The Postgraduate Diploma in Implant Dentistry helps clinicians tackle the core elements through an excellent peer mentoring system, whilst the Postgraduate Diploma in Advanced Techniques in Implant Dentistry focuses on hard and soft tissue augmentation for a comprehensive understanding of some of the most complex procedures in the field.
Menopause can be a difficult time of change for many women. The development of osteoporosis is one of a variety of challenges that dental professionals must be aware of, but, with tailored care from knowledgeable clinicians, brilliant solutions can and will be provided.
To reserve your place or to find out more, please visit 121implanteducation.co.uk or call 020 7486 0000. n
about the author Dr Fazeela KhanOsborne, principal implant and restorative Surgeon.
















The Digital Ultra™ is the right choice for clinicians who prefer to work in a digital environment but want critical parameters displayed both numerically and as electronic flow tubes. The ease of color-coded, fingertip controls is an additional feature of the flowmeter. Its sealed flush surface makes it easy to disinfect or barrier-protect. The unit’s design complements aseptic, contemporary operatory environments.



























The Porter SILHOUETTE nasal mask is a revolutionary new dental nitrous oxide mask and tubing designed by a dentist for dentists. comfortable nasal mask that creates an excellent seal around the nose reducing leakage and allowing for a predictable nitrous experience.











Incidence of dental caries may be declining in the UK, but there is still work to do. It is estimated that almost one in three UK adults have tooth decay, with an average of 2.1 decayed teeth per person. Nearly 11% of threeyear-olds surveyed in 2018 had already experienced dental decay in an average of three teeth, while 23% of five-yearolds had received the diagnosis too. Extractions due to tooth decay remain a leading cause of hospital admissions for 0 to 19-year-olds in the UK, with nearly 27,000 episodes recorded in 2021/22.

Though the overall figures don’t paint a fantastic picture, there is more information to be learned by digging deeper.
For example, it’s important for dental professionals to be aware of the inequalities that exist in this field. Statistics from 2018 suggested that 32% of the adult population in the South West of England had caries, compared to 21% in the South East. Similar differences were found between the regions among children, with 34% of five-year-olds in the North West and 16% in the South East experiencing some form of decay. Data has also shown a significant difference in the level of decay between regions, averaging 0.5 d3mft (the number of decayed teeth and those lost or filled
due to decay) in the South East and 1.3 in the North West.
Though the impact of regional inequalities appears to be reducing with time, the gap remains unacceptably high.
Various approaches are being considered and implemented across the UK in an attempt to further reduce the regional inequalities with regards to dental decay.
Water fluoridation is one option.
An area of interest since the 1930s, studies have clearly demonstrated the oral health benefits of fluoridated water, showing a notable reduction in dental caries in locations of higher fluoride concentrations. It has even been estimated that the number of hospital admissions for tooth extractions among children could be reduced by 17% with fluoridated water!
Despite the many positives, there is still some resistance among the general public to fluoridation of the main water supply. Studies are available that suggest adverse developmental effects in children due to maternal fluoride exposure, as well as other negative effects like hypothyroidism, skeletal fluorosis, and enzyme and electrolyte derangement. However, much of this research has been criticised by experts, authorities and professional bodies, suggesting that water fluoridation should still be a priority – especially in more socioeconomically deprived areas of the nation. Some areas that have recently been advocating for or looking into water fluoridation for these reasons include Nottinghamshire and Isle of Man.
Regardless of the wider discussion around water fluoridation, there are various other – smaller scale – strategies that dental professionals can support patients with in the fight against dental caries. An effective oral hygiene routine and chewing sugar-free gum between meals both go a long way to reducing the risk of decay. Preventive treatments like pit and fissure sealants, alternative remineralising agents to fluoride and potentially even chlorhexidine varnish may also be beneficial.
Perhaps the most important aspect, however, is ensuring that patients are aware of the risks dental caries presents and how to protect their oral health, as well as that of their children.
Part of the problem contributing to oral health inequalities in the UK may be the health literacy of the nation. It has been estimated that 41% of working-age adults in the England don’t fully understand or make use of everyday health information. This number increases to 61% when the recommendations or advice also involve numeracy skills. Given that health literacy is directly linked to health outcomes and service use, it is crucial that public education be enhanced.
For dental professionals, this once again highlights the need to engage with patients and ensure that they really understand the importance of oral hygiene. It is necessary to communicate with patients in a way that allows them to effectively digest the information offered and apply it to their
own lives. This is true when describing their current oral health status, including their risk of caries, as well as explaining potential treatments and therapies that could improve their situation.
Chairsyde is a state-of-the-art consultation platform that is designed for just this reason. It offers a library of animations that clearly and easily communicate a broad range of dental conditions and diseases, as well as the treatments associated with them. The videos cover the risks of disease progression, in addition to the benefits, limitations and potential risks of all recommended therapies, encouraging patient understanding for longterm health benefits and improving the quality of their consent.
reducing the caries burden
Dental caries can have a significant impact on patients’ lives and the wider healthcare system. Continuing to reduce the prevalence of dental decay in the UK is essential for better health in the future. Though general trends are looking positive, it’s time to tackle the inequalities to ensure that all areas of the nation are benefiting from improved oral health. For more information, or to book a demo, please visit www.chairsyde.com or call 020 3951 8360 n
about the author loven Ganeswaran, Ceo and founder, Chairsyde.

During each check-up there are many assessments which must be undertaken to establish a patient’s oral health status. This should always involve examining patients’ dental and periodontal health, looking for signs of caries and gingivitis, and recommending preventative advice or treatments. However, for a thorough oral health check, clinicians should always look out for signs of oral cancer, and take action if they find anything suspicious.
thorough examination
To check for the early signs of oral cancer, it’s important to know what to look for. When oral cancer is identified in its early stages, treatment outcomes are far more successful, and less invasive when compared to later stages. Clinicians should check for mouth ulcers which have lasted longer than 3 weeks, red or white patches inside the mouth, and lumps in the mouth, lips, and throat. Clinicians should also ask patients if they have experienced any oral pain, or had difficulty swallowing or speaking. Visual oral examinations are essential for picking up on and monitoring changes in the mouth. However, if clinicians do not easily recognise the early-stage symptoms of mouth cancer – because they do not come across them regularly, or are unfamiliar with them – it can mean that signs go unnoticed, with both dentists and patients unaware of the problem until it becomes more severe.
tests to aid in early-stage cancer assessments
In order to help pick up on the early signs of oral cancer, there are a number of adjunctive tests which can help clinicians to determine whether a lesion could be cancerous. Visual oral examinations are the gold standard, however, additional tests can be helpful when clinicians are unsure. Adjunctive tests include toluidine blue staining, autofluorescence, chemiluminescence, cytology, and narrow band imaging.
Toluidine blue stain is used to differentiate lesions which may be at a high-risk of progressing, helping to identify mouth cancer earlier, with a study showing its reliability. Autofluorescence is a rapid test used to identify a change in concentration of fluorophores, to aid in the recognition of malignant tissues. Chemiluminescence testing is used to distinguish between pre-cancerous and malignant lesions, as abnormal cells reflect the wavelength used – although research shows this is less effective than toluidine blue staining. Cytology can be efficient at identifying early cancer, and is non-invasive. Cancerous cells can be more easily brushed away when compared to normal cells, which can then be analysed under a microscope. Narrow band imaging has been shown to be a promising adjunctive test, highlighting the surficial blood vessels as blue or brown in order to more easily identify abnormalities. Research suggests that, compared to the other adjuncts mentioned above, narrow band imaging is the most useful aid.

By identifying abnormalities early, and beginning treatment before the cancer reaches its later stages, clinicians avoid a ‘watch and wait’ approach, which can allow cancer to progress untreated until it is advanced enough for a biopsy. By adopting measures to aid initial assessments, when clinicians spot an abnormality, they may be able to pick up on mouth cancer more quickly. However, the previously mentioned adjunctive tools can be invasive and time consuming, potentially discouraging patients from accepting tests, and allowing more time for the cancer to progress. As such, it may be beneficial for clinicians to use a noninvasive and rapid test to quickly highlight areas of concern during check-ups. A point of care system would allow clinicians to quickly establish a patient’s risk level, to therefore inform further tests or referrals.
The BeVigilant™ OraFusion™ system from Vigilant Biosciences® is able to accurately determine the risk of oral cancer based on biomarkers found in saliva combined with lifestyle factors. Producing a result in just 15 minutes, the innovative system is ideal
for detecting mouth cancer early, enabling clinicians to conduct a simple test each time they notice an unusual lesion. A German study reveals that clinicians use the system to test patients who they deem to be at a heightened risk of mouth cancer due to use of alcohol and tobacco as a tool to encourage behaviour changes. The test also provides a baseline test result for patients.
In order to identify the signs of oral cancer in its early stages, clinicians must be familiar with its symptoms, and should have the adjunctive tools necessary to assist them in identifying unusual lesions. While there are a number of tests that clinicians may use when assessing a lesion, these are often invasive, and can take time to produce results. As such, utilising innovative new tools to assist in the early detection of mouth cancer can help to improve outcomes, and reduce the impact of the required treatment for patients.
For more information, please visit www.vigilantbiosciences.com or email info@vigilantbiosciences.com n
about the author after a long career in medical devices, Phil Silver created total tMJ, which distributes innovative technologies from leading healthcare manufacturers to dentists and clinicians around the UK.




Kevin O, Dentist



Love the Oralieve range… I literally had a patient this morning and Oralieve has changed her life… the samples have been an absolute blessing


hygiene for sensitive and dry mouths • A unique combination of bioactive ingredients and enzymes
• Supplements patients’ natural saliva



• Helps protect tissue and promote a healthy mouth


• Ultra mild mint flavours • SLS free • Fluoride protection • Offers comfort and protection for oral tissues Effective relief of dry mouth symptoms – day and night

When it comes to preventive healthcare measures, Britain has a rich history. Edward Jenner developed the first smallpox vaccine in 1796. British scientists helped build the evidence base to establish the link between smoking and cancer during the 1950s. And in 2007, in England, it became illegal to smoke in enclosed public places.
A more recent example, and more pertinent to dentistry, has been the sugar tax (aka the UK soft drinks levy introduced in 2018). It was designed to reduce the sugar intake of children (thereby addressing the nation’s obesity and tooth decay problems) and it may just be yielding results.
According to a study published recently in BMJ Nutrition, Prevention & Health, researchers at the Medical Research Council Epidemiology Unit at Cambridge found that the levy may have reduced the number of under-18s having a tooth removed due to tooth decay by 12% (saving more than 5,500 hospital admissions for tooth extractions).
As you know, preventive dentistry focuses on reducing the risk of decay (together with the prospect of gum disease and tooth loss) through preventative measures, or spotting it early so advice can be offered on how to treat it.
Air abrasion is a modern technique that is gaining in popularity. It involves the use of a fine stream of particles, such as aluminium oxide or silica, that are propelled
by compressed air onto the tooth surface to remove decay, remove temporary cements, repair composite restorations, or remove stains. Unlike traditional drilling, air abrasion is minimally invasive and offers several benefits.
One of the key benefits of air abrasion is its ability to preserve healthy tooth structure. Traditional drilling requires the removal of healthy tooth structure along with the affected area. This can weaken the tooth and may require more extensive restorative procedures, such as dental fillings or crowns. In contrast, air abrasion selectively removes only the decayed or discoloured portions of the teeth, leaving the healthy tooth structure intact. This not only helps to preserve the strength of the tooth but also minimises the need for additional restorative work, resulting in a less invasive and more conservative treatment approach.
Air abrasion also eliminates the need for local anaesthesia in many cases. Traditional drilling often requires the use of local anaesthesia to numb the tooth and surrounding tissues, as it can cause discomfort and sensitivity. In contrast, air abrasion is relatively painless and does not generate the heat or vibration associated with drilling, making it possible to perform many preventive dental procedures without the need for anaesthesia. This is particularly advantageous for patients who have a fear of needles or dislike the feeling of numbness associated with local anaesthesia.
Dental X-rays have become fundamental to modern dentistry. The insight they offer is unmatched and, in turn, they inform treatment plans in endodontics, implantology, orthodontics and cosmetic dentistry.
Modern dental imaging adaptions have made 2D and 3D outcomes useful in their own right, but a final diagnosis will always rely on a dental professional’s interpretation. Should an inaccurate or missed reading occur, patients can suffer greatly with their health and the loss of time and money that has to be committed to appointments and treatments. It’s important to understand what can go wrong with imaging, and how these hurdles can be mitigated. The rise of improved technology may be considered the greatest step to date.
Diagnostic errors made by clinicians at any stage of the treatment process can put patients at risk. There are a multitude of factors that could impact radiological error, from the capabilities of present technology, to staff workloads or ineffective reporting environments.
Clinical fatigue is a common concern. Visual and mental tiredness may come with the repetition of similar tasks, a potential result of staffing shortages or inefficient workload distributions. Inaccuracies may also increase as professionals are put under pressure. One study found that under strict time constraints, dentists missed 67% of bone loss and 40% of tooth decay on
The process is generally less traumatic and more comfortable for patients too. Traditional drilling generates heat and friction, which can lead to discomfort and pain. Additionally, the noise and vibrations produced by the drill can cause anxiety and unease in some patients. Air abrasion, on the other hand, is a silent and vibration-free procedure, making it a more comfortable and relaxing experience. This can be especially beneficial for children and individuals with dental phobia, as it can help to reduce their anxiety and improve their overall dental experience.
On top of these advantages, air abrasion also offers shorter treatment times. Traditional drilling can be time-consuming, as it requires multiple steps, such as anaesthesia administration, drilling, and filling. Air abrasion, on the other hand, is a relatively quick procedure, as it combines the removal of decay or stains with the application of preventive materials, such as dental sealants or fluoride varnishes, in a single step. This not only saves time for both the dental professional and the patient but also reduces the overall chair time and improves efficiency in the practice.
To help patients perform more effective at-home preventative oral care, consider recommending the FLEXI range of interdental brushes from TANDEX to help keep plaque at bay. Available in 11 different sizes, there is a correct solution for each patient, ensuring a comfortable and effective clean. Each product’s handle is flexible, and the brush

can be bent into the perfect shape to clean in between the posterior teeth. Additionally, FLEXIMax features an ergonomic handle for an even easier clean. Plus, FLEXI brushes can be used to easily apply PREVENT GEL, which contains 0.12% chlorhexidine and 900ppm fluoride for antibacterial and enamel strengthening properties.
Air abrasion is a valuable tool in preventive dentistry due to its ability to preserve healthy tooth structure, provide precise treatment, eliminate the need for anaesthesia, offer a more comfortable experience for patients and reduce treatment times.
For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from CTS Dental Supplies www.cts-dental.com/ n
sample X-rays. When participants were not kept to the stopwatch, they correctly identified all relevant pathologies.
Many associate dentists feel that they work under tremendous pressure, under the burden of high-volume targets and the need to see so many patients in the limited hours of the day. Combating this to preserve diagnostic confidence is difficult. It may mean practices put further supports in place for mental health and stress management, or, though it is far easier said than done, hire more staff to relieve the pressures felt by overworking.
Changes like this may not always be possible. In turn, it’s important to provide clinicians with the greatest opportunity to successfully draw diagnostic outcomes. If time constraints and stress cannot be sufficiently alleviated, the equipment they use could make the most difference.
To ensure an accurate diagnosis can be made, clinicians must be informed by clear radiographic images. Obstructions can misrepresent or hide oral health issues, resulting in repeated appointments and scans, and potentially delays to treatments – leaving patients to suffer unnecessary pain. Systems that utilise cone-beam computed tomography (CBCT) may be impacted by metal artifacts. This is especially relevant in dentistry due to the common use of metallic restorative materials, posts, cores, and dental implants. Clarity issues come into play as the density of the metal surpasses the range that a computer will measure, and attenuates X-ray beams – including those targeting
adjacent structures. The result may be an extremely dark or light band that disfigures the image, reducing its quality and effective use in diagnostics. Patients will have to undergo further scans as a result, meaning an increased exposure to radiation, simply because a clinician cannot identify an obscured element as a result of a nearby artifact. There is also the challenge of extensive image noise. This is the grainy texture with harsh discrepancies between light and dark pixels, potentially making accurate diagnoses difficult to achieve. The distribution of lighter and darker pixels is entirely random, but investing in modern systems and software that reduces noise could bring increased clarity to diagnostic workflows.
a matter of perspective
Dental professionals can only make confident observations based on the images in front of them. It makes sense that with a greater breadth of information, more comprehensive insights can be created. Herein lies the advantage of 3D imaging, commonly seen in dentistry today with CBCT workflows. 2D imaging is not able to present as much information as 3D CBCT scans. The latter can record and display more dynamic viewpoints, rather than the singular perspective of a straighton X-ray. There are incredible applications in treatment planning. For example in endodontic workflows, clinicians can actively segment canals and better determine their curvature, and the benefits are similarly fruitful for diagnosis. CBCT scans improve the detection rate of root canals and periapical spaces, offering clinicians greater diagnostic accuracy.

about the author Kimberley Lloydrees, on behalf of tandex, graduated from the University of Sheffield in 2010, where she now works as a clinical tutor in Dental Hygiene and therapy as well as working in practice. She has spent her career working across a variety of specialist private and mixed dental practices, for the mOD and volunteering her time to a dental charity in nepal.
There may not be a need to use CBCT scans in every case, and its application instead of 2D radiography should be assessed case-by-case. Employing a versatile system that covers all manner of diagnostic workflows could be ideal. Dental professionals should consider the CS 8100 3D Evo Edition from Carestream Dental, the 4-in-1 system that delivers high-quality 3D and 2D panoramic results. Incredible detail can be seen at 75 microns, with the ANR algorithm reducing image noise whilst preserving clinical detail. Plus, implants and fillings are not a detriment with CS MAR (Metal Artifact Reduction), which drastically diminishes metal artifacts to improve image quality and reduce misinterpretation.
A confident diagnosis is the basis for effective treatment. By supporting clinicians in practices and making incredible equipment accessible, dental professionals have the greatest opportunity to accurately identify oral health problems and provide patients with the highest level of clinical care.
For more information on Carestream Dental visit www.carestreamdental.co.uk
For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
about the author nimisha nariapara is the trade marketing manager at Carestream Dental covering the UK, middle east, nordics, South africa, russia and CIS regions.

Aligners offer a comfortable and aesthetically pleasing solution for straightening teeth, especially in adult patients. Many choose the technique due to its invisibility and the majority expect an improvement in selfconfidence following treatment. However, it is essential for dental professionals to effectively manage patient expectations when discussing aligner treatment to ensure a successful and satisfying outcome.
To begin with, it is important to educate patients about the realistic expectations they should have regarding dental aligners. While aligners can effectively correct a wide range of orthodontic issues, there are limitations to what they can achieve. Patients need to understand that aligners are most suitable for mild to moderate cases of malocclusion and tooth misalignment. Severe cases may require other treatment options such as braces or even surgery. By setting realistic expectations from the start, patients are less likely to be disappointed in the outcome.
All in good time
Another aspect of managing patient expectations is explaining the treatment timeline. Unlike traditional braces, aligner treatment is typically shorter. However, it is important for patients to understand that the duration of treatment varies depending on the specific case. Some patients may require aligners for a few months, while
others may need them for over a year. Revisions are sometimes required when teeth don’t move as planned, so patients need to be informed that they might require additional sets of aligners to target specific areas. By providing a general estimate of the treatment duration, patients can plan accordingly and understand that patience is crucial throughout the process. It is also vital to discuss the commitment and responsibility required for successful aligner treatment. Because aligners are removable, it means that patients must be diligent in wearing the aligners as prescribed by their dentist. Aligners should be worn for at least 22 hours a day to ensure optimal results. Patients should understand that failure to comply with the recommended wearing time may prolong the treatment or even result in unsatisfactory outcomes. In addition to wearing aligners consistently, patients must also comply with the maintenance and cleaning instructions provided by their dental professional. Aligners should be removed before eating or drinking anything other than water, as certain substances can stain or damage them.
No pain, no gain
Alongside explaining the commitment required, it is crucial for dental professionals to address any potential discomfort that patients may experience during aligner treatment. While aligners are generally more comfortable



than traditional metal braces, patients may still encounter some initial discomfort during the adjustment period. It is important to inform patients that this discomfort is temporary and often subsides within a few days as they become accustomed to wearing the aligners. By preparing patients for potential discomfort, they can better manage their expectations during the early stages of treatment.
Dental professionals should openly communicate the potential risks and limitations associated with aligner treatment too. For instance, patients may experience slight changes in speech or a feeling of pressure on the teeth during the initial stages of treatment. It is essential to address these concerns and provide reassurance that these effects are temporary. Additionally, patients should be made aware that aligners may not be suitable for everyone and that alternative treatment options may be necessary in some cases.
ClearCorrect® aligners from the Straumann Group are made from a proprietary ClearQuartz tri-layer material that provides greater orthodontic control by combining two layers of resilient polymers with an elastomeric








inner layer, producing a gentle but consistent application of force. The material has also been found to be more stain-resistant than other leading brands when tested with cola, red wine, coffee and mustard. ClearCorrect aligners also feature a flat trimline above the gingival margin resulting in comfortable and retentive oral device.
Managing patient expectations plays a pivotal role in ensuring a successful and satisfying outcome with dental aligners. By setting realistic expectations, educating patients about the treatment timeline and commitment required, discussing potential discomfort, and addressing any limitations or risks, dental professionals can enhance patient satisfaction and promote a positive experience throughout the aligner treatment journey. Effective communication and transparency are key to managing patient expectations and achieving your and their desired results. For more details, please visit straumann.com/clearcorrect/gb/en/ landing/clearcorrect-aligners.html







Dental implants are rapidly becoming the gold standard for replacing missing teeth due to their durability, functionality and natural aesthetic appearance. One crucial factor that ensures the long-term success of dental implants is stability. As you know, the stability of an implant determines its ability to bear occlusal loads and maintain integration with the surrounding bone.
There are several factors affecting stability. It begins with implant site preparation. This is a critical step that directly influences implant stability and several techniques can be employed to prepare the implant site properly:
• Bone Augmentation: In cases where the available bone volume is insufficient, bone augmentation techniques like bone grafting, sinus lifting, and ridge expansion can be employed. These procedures promote bone formation, providing a solid foundation for implant placement.
• Drilling Protocols: The use of specific drilling protocols helps in preparing the implant site accurately. Sequential drilling, which involves progressively increasing the drill diameter, ensures that the bone is adequately prepared to receive the implant and promotes primary stability.
• Piezoelectric Implant Site Preparation (PISP): PISP has been demonstrated to improve secondary stability compared with conventional drilling techniques. The design of dental implants contributes significantly to their stability. Two important design aspects to consider include their microgeometry and surface modification. The macrogeometry of dental implants, such as tapered or cylindrical shapes, influences their stability. Tapered implants offer enhanced primary stability due to their ability to engage the surrounding bone more effectively. Meanwhile, surface modification
techniques, such as sandblasting and acid etching, are employed to increase the surface area and enhance osseointegration. These modifications promote better implant stability by allowing for greater contact between the implant and the surrounding bone.
Guided surgery involves the use of computer-aided design (CAD) software and surgical guides to ensure accurate implant placement. This technique improves implant stability by reducing the chance of error during surgery. Guided techniques provide a precise, predictable and minimally invasive approach to implant placement, resulting in enhanced primary stability.
Resonance Frequency Analysis (RFA) is a non-invasive diagnostic tool used to assess implant stability. RFA measures the stability of dental implants by analysing their vibrational frequency. A specialised device, known as an implant stability analyser, is used to determine the implant’s stability through resonance values. RFA offers quantitative data to objectively assess implant stability, facilitating informed decision-making during the healing process.
Immediate loading, also known as ‘Teeth in a Day’, allows for the placement of a prosthesis on the implant immediately after surgery. This technique, when performed under specific conditions, can promote early function and stabilisation of the implant. Immediate loading protocols require careful patient selection, adequate implant primary stability, and appropriate occlusal load management to achieve long-term success.
Various bone management techniques can be employed to improve long-term dental implant stability too. The use of bioactive materials, such as growth factors or bone graft substitutes, enhances bone formation and integration around the implant. These materials stimulate osseointegration, leading
to improved stability. Barrier membranes are also used in guided tissue regeneration procedures to prevent soft tissue ingrowth and promote bone regeneration. By isolating the implant site from surrounding soft tissues, barrier membranes encourage new bone formation, contributing to successful implant stability.
Using the right equipment can help towards implant stability as well. With Implantmed, the high-quality, high-performance surgical motor from W&H, the placement of implants is assured and efficient. With an intuitive user interface, colour touch screen and glass surface, Implantmed offers the highest levels of design and comfort. It also offers maximum flexibility thanks to its wireless foot control and its higher torque compact motor. Boasting an automatic thread cutter function integrated into Implantmed, the tightening torque control provides support when placing implants and prevents excessive compression of the bone when inserting the implant. This reduces the risk of bone loss, enhancing stability and facilitating stress-free healing of the implant.
To carry out RFA, it is important to use the appropriate equipment to evaluate with accuracy. The Osstell Beacon, from W&H, produces results within a matter of seconds, showing clinicians when an implant is successfully osseointegrated, and can therefore be loaded. Additionally, because the Osstell Beacon operates wirelessly, it offers excellent freedom of movement. Data captured using the Osstell Beacon can be stored safely and compared on the Osstell Connect platform. By using high-quality equipment, clinicians receive accurate results about implant stability, allowing them to progress treatment with confidence and certainty.
The Osstell Beacon helps the clinician to objectively determine implant stability and to assess the progress of osseointegration, without jeopardising the healing process. It allows the avoidance of long treatment
As dentists, we want to provide the best possible experience for all of our patients. Whether they are coming to us for routine care, or they require endodontic, orthodontic or periodontal therapy, our goal is to improve their health while achieving aesthetic and functional outcomes that will last. Among the list of elements we have to consider is how to optimise the recovery and healing process for patients, reducing the pain and discomfort that they experience. For my fellow endodontists or colleagues with an interest in endodontics, this can be a particularly difficult aspect to manage.
It has been reported that patients experience pain following a root canal procedure in around 43% of cases. Though the intensity of discomfort lowers with time, it can last for anything from a few hours to a several days. A combination of mechanical, chemical and microbial factors is thought to
play a role in peri-radicular inflammation. It has also been suggested that the severity of preoperative pain experienced can influence postoperative pain.
I was interested to come across a recent study that considered the impact of anaemia on post-endodontic pain. The research found that 82% of anaemic patients reported pain, compared to only 61% among the non-anaemic control (for clarity, ‘pain’ was registered in this study where even the most minor discomfort was felt). It has been postulated that an iron deficiency inhibits the haemoglobin’s ability to transport oxygen to the peripheral tissues, which reduces neuronal function. Anaemia is estimated to affect approximately 30% of the global population, with iron deficiency being the most common cause. As such, it is likely to affect several of our patients at any given time, making it a necessary consideration for the dental team.
Other factors that may lead to increased postoperative endodontic pain include

times, improving healing and ensuring the achievement of predictable results. When it comes to high-risk patients, it is important to do everything possible to maximise the success of dental implant treatment. This means ensuring patients understand how best to maintain their oral health, and that the implants selected are appropriate for the individual case. By doing this, good primary stability is encouraged, as well as successful osseointegration and functional dental implants. Ensuring accuracy is crucial when measuring this, as implant stability will determine how and when clinicians choose to progress with treatment and loading. It is important that implants are stable prior to this.
Achieving optimal dental implant stability is vital for long-term implant success. Implant site preparation techniques, implant design considerations, guided surgery, RFA, immediate loading techniques, and bone management methods all play integral roles in enhancing the stability of dental implants. By incorporating these techniques and tools into dental implant procedures, clinicians can ensure predictable outcomes and improve patient satisfaction in terms of functionality and aesthetics.
To find out more visit www.wh.com, call 01727 874990 or email office.uk@wh.com n
about the author Kate Scheer, marketing executive, W&H (UK) Ltd

the tooth being treated – treatment of maxillary molars has been associated with less pain than that of mandibular molars. The presence of acute pulpitis has also been linked with higher post-treatment discomfort for the patient.
Prevention and management
As is true in any area of dentistry, avoiding complications and preventing sources of postoperative pain where possible are essential. When approaching an endodontic case, this might involve ensuring aseptic conditions throughout, careful instrument selection, biochemical debridement of the root canal space, and using antiinflammatories or antimicrobial solutions, among other considerations.
A variety of medications can also be administrated following root canal therapy in order to manage pain and reduce symptoms. It can help to communicate clearly with patients and ensure that they understand the origins of any possible discomfort so that
they are prepared to manage their pain at home. Not only can this improve their overall experience of treatment, but it is also likely to have a positive impact on their recovery.
applicable in all areas
Of course, no matter what area of dentistry you focus on, or what type of treatment your patient seeks, minimising postoperative discomfort is a must. A thorough medical history will highlight any systemic conditions that might impact their dental treatment journey. By combining this with clear communication and wellplanned management strategies, you can ensure your patient has the best possible dental experience. n
about the author endoCare, led by Dr michael Sultan, is one of the UK’s most trusted Specialist endodontist practices.


When creating a product, especially in the healthcare industry, brands can find themselves limited in trying to cater to every type of patient. When medical equipment limits who can comfortably and safely use it, this can alienate entire demographics of end users and exacerbate existing challenges they may already face. This is certainly true of bariatric dental patients. Research into this topic has found equipment safety and suitability of dental chairs as a main concern when providing dental care for treating bariatric patients (GeddisRegan et al., 2019). When querying several dental chair manufacturers, Reilly (et al) found that the maximum lifting weight for modern chairs is approximately 140 kg (23Ib) – a maximum lifting weight that isn’t compatible with bariatric patients who weigh over 159kg.
Further research highlights how patient anxiety varies amongst patients who are obese and those who are a “normal” weight, with obese women experiencing a higher rate of dental-related fear (Marshall et al, 2016). Whilst dental anxiety isn’t exclusive to obese patients, this fear can lead to a harmful cycle of seeking symptom-driven dental care rather than attending regular checkups. This oversight regarding obese patients and equipment design has
led to dental professionals restricted in their provision of care, with many suggesting alternative care options like dental hospital referrals or refusing treatment altogether due to safety weight limitations.
Beyond safety, the Equality Act details the need to ensure every individual receives equal access to services regardless of physical disability (Equality act, 2010). With Public Health England estimating obesity to affect 60% of adult men and 50% of adult women by 2050 (England, P.H., 2017), healthcare providers must act to ensure their surgeries can accommodate this fast-growing demographic of future patients.
The A-dec 500 dental unit was manufactured for everyone’s comfort and safety. With a maximum lifting weight of 227 kg (35 Ib), dental professionals can rest assured knowing they won’t be restricted in who they can treat safely. Venkata Kalisetty of Willow Street Dental shares his experience buying an A-dec 500 for his bariatric patients.
“Having a powerful chair that could handle 35 Ib was non-negotiable as we needed to fulfil an NHS contract which required the install of at least one dental unit that caters to bariatric patients.
“We went to various brands and multiple showroom appointments, but found it incredibly difficult to find a dental chair that would be equally safe and comfortable for our bariatric patients.
“We were so pleased to see the variety of features that accommodate the comfort and safety of our bariatric patients. From the backrest with wide wings that help cradle the patient’s shoulders to the wide chair base that provides amazing stability when lifting.”
- Venkata Kalisetty, Willow Street Dental
At A-dec, we take pride in ensuring our range of reliable and versatile equipment exceeds the expectations of our customers, but also believe that this should always extend to their patients. We understand that for some people visiting the dentist may come with its own set of challenges and apply that to our design process ensuring that every patient experience is a positive one.
To find out more the about our thoughtfully designed equipment, visit https://unitedkingdom.a-dec.com/ dental-chairs/a-dec-500 n
References
1. Geddis-Regan, A. et al. (2019) ‘Care pathways and provision in Bariatric Dental Care: An exploration of patients’ and dentists’ experiences

in the North East of England’, British Dental Journal, 227(1), pp. 38–42. doi:10.1038/s41415-0190459-4.
2. Reilly D, Boyle C, Craig D (2009) Obesity and dentistry: a growing problem. Br Dent J 207: 171-175
3. Marshall A, Loescher A, Marshman Z (2016) A scoping review of the implications of adult obesity in the delivery and acceptance of dental care. Br Dent J 221(5): 251-255
4. England, P.H. (2017) Health matters: Obesity and the Food Environment, GOV.UK. Available at: https://www. gov.uk/government/publications/ health-matters-obesity-and-thefood-environment (Accessed: 19 January 2024).
5. Equality act 2010, Legislation. gov.uk. Available at: https://www. legislation.gov.uk/ukpga/2010/15/ contents (Accessed: 22 January 2024).
Around the world, prevalence of oral disease is a major concern, with rates of caries, periodontitis, and tooth loss continuing to increase. Regardless of the cause, be it insufficient exposure to fluoride, a diet high in sugars, or inadequate access to oral health care, populations around the world continue to have trouble managing their oral health, resulting in high levels of disease. As such, it is important for general dentists and dental specialists alike to come together to support patients and offer them care which supports their long-term health.

Reports from the World Health Organization suggest that 3.5 billion people worldwide are affected by oral diseases, with 2 billion suffering with caries in their permanent dentition. If left untreated, caries can advance and become a severe problem. Disease can progress through the dentine, causing pulpitis and eventually leading to pulp infection and necrosis. Regular dental appointments are essential for monitoring lesions, and taking a preventative approach. This is because, when managed conservatively, the pulp can be encouraged to recover, even in cases with deep carious lesions.
A traditional caries treatment might include removing all carious dentine, however modern techniques opt for a minimally invasive approach, hoping to preserve as much natural tissue as possible, for as long as possible. This means selectively removing caries to reduce the risk of pulp exposure. Similarly, in previous years the complete removal of caries exposed pulp was the preferred treatment approach, with some clinicians’ opinions now shifting in favour of vital pulp treatments to encourage the repair of natural structures where appropriate.
Patient needs continue to become more complex, with high expectations for treatment results perpetuated by social media. While this presents opportunities for growth and innovation, it can also be challenging for dental professionals to meet these needs. Around the world, patients will face different challenges based on their background and environment. Because of this, it’s important to cater to the individual needs of every patient, to offer the type of treatment which will best benefit them. Assessing each unique case using the most effective diagnostic techniques and consulting the latest research to provide the most appropriate approach is essential to provide patients with the highest standards of care. By carefully managing damaged pulp through vital pulp treatment, for example, you may find favourable success rates in comparison to a pulpectomy. Education is key here, as the field of endodontics continues to grow
For any new and novice dentist, the challenges facing the industry also represent opportunities. Now is the time to get ready for what is coming, in order to help more people and, in doing so, boost your service offering and earning potential.
We are already seeing trends for more complex treatments, and an increased demand for solutions to difficult dental dilemmas across the population. The patient demographic is changing too, with higher numbers in the 65 and over age bracket. The future burden of oral disease among the ageing population is a complex matter, though, as you will know patients in their 60s, 70s and beyond who remain motivated to practise dental hygiene that is exemplary, by anyone’s standards. They are committed to regular, routine visits and are fully engaged with any advice the dental team gives them.
But, despite their excellent habits and behaviours, they need to understand that, occasionally, an intervention will be required. Over time, changes to their teeth, periodontium, oral mucosa, salivary glands, also to oral motor and sensory function, naturally occur. Elderly adults are also going to present with age-related wear and tear, as well as dentition that has previously been restored. Modern methods of teeth restoration are far more conservative and concerned with preserving healthy tissue
and change, with technology playing a much bigger part in many clinicians’ daily workflows.
When clinicians from different backgrounds come together, the international dental community is able to discuss the ways in which dental protocols can be improved for the good of patients’ wellbeing. Global networking proves to be an important way of advancing dental education and services around the world, with clinicians encouraged to share their knowledge and expertise with the dental community and receive feedback from their peers.
As dental tourism continues to pose challenges for some patients and clinicians, the importance of global collaboration is further highlighted. Clinicians, from all areas, must be committed to producing the best possible outcomes for their patients. This is essential to ensure that those patients who are most in need, receive appropriate care, which supports oral health in the longterm. In doing this, clinicians should identify barriers to oral health, and innovate to help make improvements.
Events such as the World Endodontic Congress (WEC) of the International Federation of Endodontic Associations (IFEA) encourage endodontic clinicians from around the world to meet and discuss progress in the field. Organised by the British Endodontic Society (BES) in 2024, the event provides insights into the endodontic health of the global population, the unique challenges faced in different areas, and presents an opportunity for endodontists to collaborate to find solutions and inspire

development. With expert speakers from around the world, including Daniel Černy, Elisabetta Cotti, Adham Abdel Azim, Phil Tomson, and Paul Lambrechts, coming together for the event in Glasgow, from the 11th – 14th September 2024, to present sessions on cutting-edge endodontic techniques, delegates can expect an enriching programme.
Meeting with endodontic clinicians from around the world is beneficial for promoting progress in the field. In order to understand the various challenges faced by clinicians and patients from different backgrounds, professionals must discuss their experiences, and the modern innovations available to them to improve the situation for themselves and their patients. As rates of oral diseases including caries and periodontitis are projected to continue to rise, the dental community must collaborate on a global scale to minimise the impact, educate patients, and provide treatments which aim to promote the long-term health of the dentition.
Register today for IFEA WEC 2024 at ifea2024glasgow.com/registration
For more information about the BES, or to join, please visit britishendodonticsociety.org.uk or call 01494 581542 n
than past modalities, which may have compromised the long-term stability of the teeth and gingiva.
Elderly people are also more prone to caries, including root caries which are often painless. Other, normal and agerelated changes to expect include a thicker pre-dentine layer, the pulp space having reduced dimensions and dentine that is “more likely to have cracks within its structure”. As with all patients, pulpitis can remain undetected until an infection has set in.
Older patients want to enjoy all the benefits of a functional and beautiful smile. If there is a viable alternative to a removable prosthesis to replace a damaged tooth, for example, or to an extraction, they will be interested and want to learn more.
Endodontic therapy is a positive choice for patients of all ages; a minimally-invasive and highly ethical way to save a tooth. It can be delivered efficiently and cost-effectively, allowing people to get on with their lives, knowing that function and aesthetics have been restored. Endodontics can be transformative, not just to health but to wellbeing. It’s a treatment that will get people out of any pain, and avoid the emotional trauma that can come with having a tooth surgically removed. If infection has been diagnosed for a diligent elderly patient, tell them that this does not mean they have failed to look
after their teeth. Instead, they should consider this to be interceptive treatment to put them back on track. Rather than think their routine is no longer working, they just need a little more help. This is modern dentistry - preventive care in action that will offer robust protection against future problems. Successful endodontics will not just eliminate infection, but it will prevent reinfection, too. This is why it is absolutely worth investing in, especially at a practice committed to using cutting-edge techniques and materials, to make the process simple, quick and pain-free. When recommending a tooth be endodontically treated, give your patients the full picture. The words ‘root canal’ can be loaded, especially for older adults who may have had bad experiences. Explain how comfortable you will make them. Bring the dental nurse, dental therapist and/or dental hygienist in to your planning sessions, so there can be a discussion about recovery and the maintenance schedule. Although a highly-successful option, endodontic patients do need to know if and when to worry post-treatment, and when to get in touch with the practice. Talk about the equipment and materials you will use, and how you only select the very best. COLTENE’s endodontic range has been designed to support stable outcomes, also ease of use and flexibility. Its HyFlex EDM file-shaping sequence means clinicians
often only need one or two files during the whole process, supporting great value, too. If you are delivering a non-surgical retreatment, the COLTENE REMOVER file is ideal. Also known for offering exceptional customer service, dentists and practice can join its Rewards programme to get even more out of the products they choose. Getting older does impact on oral health, but it would be a mistake to assume that all elderly patients are uninterested in conservative therapies. An extraction is not the only choice for many people post 65, and endodontic therapy can offer a way to keep a tooth in function and prevent future problems. Many older adults want to keep taking care of their teeth so, if they’re suitable, offer them the choice of conservative endodontics that they deserve. When delivered using premium tools and materials, they can stay in good oral health and smiling beautifully for years to come.
For more on COLTENE, visit coltene.com, email info.uk@coltene.com or call 0800 254 5115. n
about the author mark allen, General manager at COLtene

Uncomplicated healing after an oral surgical procedure is a key stage for both patient and clinician. When it comes to dental implants, the time needed for healing can vary. While the restoration can sometimes be fitted at the time of implant placement, in staged graft cases, implant placement is delayed between six weeks to six months to allow the bone to regenerate. This prolongs the overall duration of implant treatment and inconveniences the patient who has to wear a temporary restoration much longer.
Platelet rich plasma (PRP) and platelet rich fibrin (PRF) are two types of autologous blood-derived products that have gained popularity in the field of dentistry for their bioactive role in enhancing healing of various hard and soft tissue defects. While both PRP and PRF contain a high concentration of platelets, they differ in their method of preparation and composition, leading to different properties and outcomes in dental healing.
Platelet concentrates are produced by obtaining a small amount of the patient’s own blood and processing it to separate the platelet-rich portion from other components. This is typically done through centrifugation, a process that separates blood components based on their density. PRF is rich in growth factors and bioactive molecules, such as platelet-derived growth factor, transforming growth factor-beta, vascular endothelial growth factor, and insulin-like growth factor, amongst others. These growth factors play a vital role
during all four stages of wound healing by stimulating cell proliferation, angiogenesis, and the synthesis of extracellular matrix components.
Second generation PRF platelet concentrates are produced without the addition of anticoagulants or bovine thrombin. They are obtained by collecting blood in specially designed tubes that facilitate the formation of a fibrin clot. The blood sample is then centrifuged at a slower speed compared to PRP, resulting in the formation of a fibrin matrix containing highly concentrated matrix of leukocytes and platelet produces. The fibrin network in PRF acts as a scaffold that traps the platelets and allows for the slow release of growth factors over an extended period.
The main difference between PRP and PRF lies in their method of preparation, composition and fibrin architecture. PRF offers a more sustained release of bio-active products such as cytokines and growth factors due to the fibrin matrix. Additionally, PRF retains leukocytes, which have osteoimmune modulating properties that have been shown to significantly enhance hard and soft tissue healing and regeneration. In dentistry, PRF has been used to enhance healing after various treatments, such as tooth extractions, implant placement, periodontal surgeries, and bone grafting.
The application of PRF in dental procedures involves either the direct application of the platelet concentrate at
the surgical site or the incorporation of these biomaterials into grafting materials to form “sticky bone”. PRF promotes angiogenesis, enhance soft tissue healing, and accelerate wound closure. In addition, these biomaterials have been shown to improve bone regeneration and enhance the integration of dental implants.
Clinician’s choice
Autologous platelet concentrates have been employed in dentistry as well as medicine and surgery for several years to promote both hard- and soft-tissue healing.
The advantages of incorporating autogenous platelet concentrates (PRF) during oral surgical procedures such as bone grafting encompass reduced healing time, improved angiogenesis and enhanced bone regeneration, socket sealing through the fibrin matrix, antibacterial properties, and decreased post-extraction pain and infection risk.
A new paper authored by the eminent Professor Cemal Ucer and Dr Rabia Khan exploring alveolar ridge preservation (ARP) and applications of PRF could change future approaches for many clinicians. Their paper, ‘Alveolar Ridge Preservation with Autologous Platelet-Rich Fibrin (PRF): Case Reports and the Rationale’, demonstrates how implants could be placed just 8 weeks following ARP when augmented with PRF, creating the potential for reduced treatment durations and enhanced implant success. Such promising results are exemplary of the work associated with the Centre
Reconstructive Surgery, the renowned ZAGA Centre in Manchester offering patients clinically backed treatment approaches for predictable zygomatic treatments. PRF has emerged as a valuable adjunct in oral surgery and implantology for its ability to enhance healing and promote tissue regeneration. PRF can be produced in solid or liquid format. Depending on the specific needs of the patient and the procedure, dental clinicians can choose between these autologous platelet concentrate preparations to optimise the healing process and improve patient outcomes.
Professor Ucer will be leading an advanced course with live surgery on the management of tooth loss with immediate implant placement or alveolar ridge preservation with PRF which will be launched in February 2024.
To request a copy of Professor Ucer’s newly published paper on socket grafting and PRF or to enquire about the new course please contact Professor Ucer at ucer@icedental.institute or Mel Hay at mel@mdic.co
01612 371842
www.ucer-clinic.dental n
about the author Prof. Cemal Ucer, BDS, mSc, PhD, FDtFed., ItI Fellow, Specialist Oral Surgeon

You don’t get a second chance to make a brilliant first impression. Whilst the sentiment is usually applied to those moving jobs or meeting new people, it still rings true for dentistry. Impressions are essential throughout restorative care, providing the base for an accurate diagnosis and treatment planning with meticulous detail. The final result of a restoration or prosthesis will rely heavily on the accuracy of the initial impression, for a closeto-perfect fit. With a fantastic impression, patient outcomes can be optimised.
As such, it’s important to understand how clinicians can make the most of every impression, for excellent results and a satisfied patient.
a matter of material
Impression taking dates back to the 18th century, and has since become a pivotal fixture in modern dentistry. The choice of material will be unique for each professional and treatment planning process. Understanding the advantages provided and the accommodations needed for the many options is key.
For example, polyether is a hydrophilic material that is suitable for humid surroundings, and provides excellent detail as its wettability allows dental gypsum to flow easily in the impression. It has very good elastic properties; modern iterations have avoided the difficulties of removal from a patient’s mouth when fully set and rigid, and without by-products from a setting
reaction, it maintains good dimensional stability. However, clinicians must be aware that, due to its hydrophilic properties, it requires specific storage in environments of less than 50% humidity.
On the other end of the spectrum, a hydrophobic material like condensation silicone is also widely used. It undergoes a polycondensation process that releases alcohol, contributing to the contraction of an impression. It can create accurate impressions when poured quickly after use, and has good elastic restoration after removal from the mouth, but its contraction means the impression may be less precise with the passing of time.
The potential solutions are not limited to these examples and there may not be a single best impression material for all treatment planning processes. When a clinician tailors their choice to their advantage, brilliant results can be created.
Today, physical impressions are not used in every aspect of modern dentistry, with advances to technological solutions supporting new workflows. Of these revolutionised options, intraoral scanners have emerged as an option.
Notably, their use has been reported to provide significantly more efficient and faster results than conventional methods – in some cases – whilst maintaining comparable accuracy in results. They may be especially useful in short-span scans, but some studies are sceptical about their use
with completely edentulous patients and over longer distance spans. Despite this, they may still be optimal for a number of applications, such as attaining impressions for the development of crowns and bridges.
Further on from the allure of an intraoral scanner’s convenience, there are concerns surrounding their accuracy when developing prostheses that come into contact with local soft tissue. A variety of studies agree that digital measurements at a subgingival marginal level are sometimes not clinically acceptable, making them inappropriate in these cases, especially where a crown’s margins are positioned deep (1.5-2mm) into the sulcus.
When preparing for the impression itself, soft tissue management could be the difference between restoration failure and success. If a prosthesis closely interacts with the gingiva, it is essential that the initial impression takes account of this – if not, the restoration may face a high chance of failure.
To effectively prepare the site for the impression, clinicians must appropriately displace local soft tissue, fluids and debris through gingival retraction. Traditional methods utilise a retraction cord to displace the soft tissue, however this could damage the gingiva, and when placed in an already inflamed or damaged sulcus, pre-existing problems may be exacerbated.
This has prompted some clinicians to seek out effective alternatives. Pastes, foams and gels are popular, being atraumatic to
the gingival tissue, without residue, and a simple, time-saving application. Cordless techniques put less pressure on the gingival tissue, meaning a fantastic impression can be created without compromising the patient’s wellbeing.
The ideal solution could be the 3M Astringent Retraction Paste, from 3M Oral Care, a preferred product for dental professionals*. The formula offers fast and precise gingival retraction, targeted through an extra-fine tip that fits right into the sulcus. Its long-lasting haemostatic effect makes it ideal on already damaged or lacerated soft tissue, for a comfortable and safe alternative to retraction cords.
Adapting the preparation process to each case’s needs is essential to creating an excellent impression that determines an even greater restoration. Today’s dental workflows offer the largest number of treatment solutions available to each clinician, but choosing the best tools throughout the process can help patients receive the greatest care possible.
For more information, call 08705 360 036 or visit www.go.3M.com/ocsdpr 3M is a trademark of the 3M Company.
*Dental Advisor 2023: https://www. dentaladvisor.com/awards/2023-toppreferred-product-awards/#preferredproducts


































































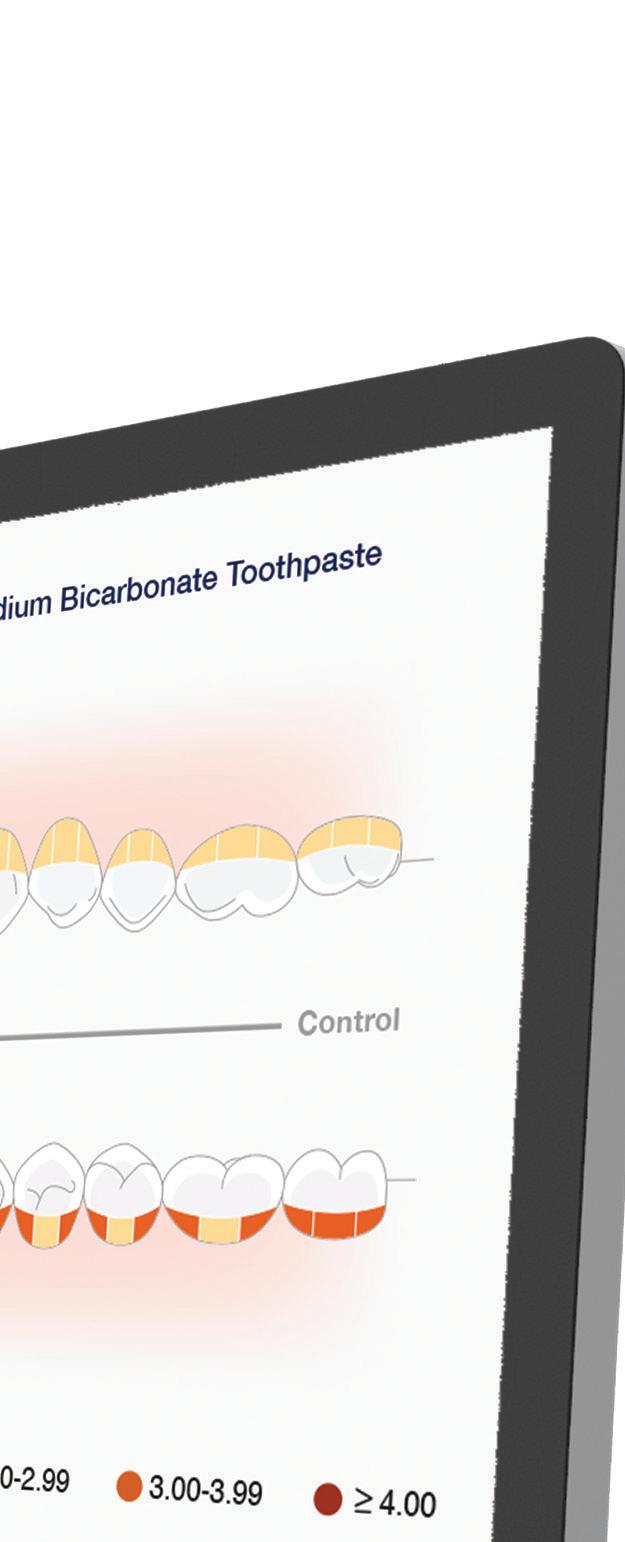




Corsodyl Toothpaste is the #1 Dentist recommended toothpaste brand for gum problems



Dr sherif Kandil explains the NASA technology driving the latest innovation in clear aligners, enabling professionals to provide the first shape-shifting clear aligner
In the 21st century, the interplay between NASA’s achievements and oral healthcare has profoundly impacted the oral health of dental patients, especially in the field of orthodontics.
Advancements in technology have revolutionised orthodontics, making them more efficient, less invasive, and more comfortable for patients.
a new milestone
In the rapidly evolving world of orthodontic care, the introduction of this revolutionary technology marks a significant milestone, not only offering superior precision and efficiency but also championing an eco-conscious approach to dental care.
Indeed, ClearX emerges as a groundbreaking offering that stands apart in its approach, efficacy, and commitment to sustainability. Developed from advanced space-age technology, these aligners are not just another product in the market but a beacon of innovation, precision, and environmental responsibility.
At the core of this remarkable design is its groundbreaking shape-shifting technology. These aligners, equipped with heat boosters, adapt their shape to ensure faster and more precise treatment outcomes. The patented technology has achieved a refinement rate of just below 15%, allowing dental professionals to deliver high-precision care with fewer adjustments, enhancing the overall patient experience.
Where it all began
The inception of this technology is a tale of extraordinary innovation, inspired by materials developed in NASA’s labs. We know that NASA’s utilisation of shape memory alloy, nickel-titanium (NiTI), in the 1970s, revolutionised orthodontics by applying the use of straight wires using NiTi too, marking a pivotal milestone in the 1980s.
Now, we see the same pattern emerge again; this time using smartshape memory plastics. Using high-temperature shape-memory polymers, this has followed the same path of technology advancement in orthodontics, as it did back in the 1980s with NiTi shape-memory alloys.
This pioneering approach was honed through years of research by K Line Europe GmbH, the parent company of ClearX, resulting in a product that significantly reduces the need for multiple aligners. This legacy enables dental professionals and patients alike to be confident in what might seem like a new kid on the block but is, in fact, steeped in a rich history that focuses on combining hightech manufacturing with outstanding service to provide patients with the perfect smile.
In fact, as Europe’s leading Original Equipment Manufacturer (OEM) for orthodontic clear aligners, the company has redefined the landscape through intelligent use of cutting-edge technology, opening the access for clear aligner providers to innovative solutions.
optimised efficiency and efficacy
What’s more, this technology is a testament to optimised efficiency in orthodontic treatment. It does this by reducing the number of aligners needed and shortening overall treatment times while achieving the same desired outcome.
Each clear aligner is designed and manufactured in a way to preprogramme the shape to 2 or more different shapes. When the patient wears the aligner, it has, for example, shape 1. After one week wearing it, the patient boosts the aligner through a specific device called the Booster. After the patient gets out the aligner from the booster, it has already adopted a new preprogrammed shape, i.e. shape 2. The


patient wears it for another week to allow the teeth to move to shape 2. Then the patient could wear the next aligner in the sequence and does the same again with the Booster.
This efficiency benefits patients through faster smile makeovers and enables dental professionals to cater to a larger patient base without sacrificing quality. The time and resource savings translate into superior service and heightened patient satisfaction.
eco-conscious design
In a world producing over 1.2 million aligners daily, which are not recyclable, the environmental impact is undeniable.
However, things are about to change! Alongside evidence-based efficacy and patient comfort, as touched upon briefly earlier, a pivotal aspect of the technology is its ecofriendly design. These aligners are crafted to minimise environmental impact without compromising on clinical efficacy.
By cutting down the number of aligners used (by up to 50% thanks to the 4D technology), there is a significant reduction in plastic waste, offering a sustainable alternative in orthodontic treatments. This allows patients to align their dental care with their environmental values, making the ClearX design a responsible choice in the market.
In the world of clear aligners, the emphasis remains on delivering individualised, bespoke care for each patient. Every aligner is tailored to the distinct needs and characteristics of the person it is designed for, emphasising the importance of personalised care.
This concept of individual care goes beyond the aligners themselves, permeating every aspect of the patient experience. The journey to master and integrate this degree of customisation in both clinical procedures and patient interactions highlights the delicate equilibrium between providing tailormade patient care and ensuring efficient operational practices, areas in which this new technology triumphs. the difference is clear These new aligners are not merely an orthodontic product; they represent a significant leap in the integration of advanced technology, precision, and eco-consciousness in dental care. By harnessing the power of space-age materials, this technology has helped to create a process that embodies innovation and sustainability. As the clear aligner industry continues to expand, ClearX has been able to position itself at the forefront, redefining the ecological footprint of orthodontic care and leading the charge towards a more sustainable future in dental health.
Embracing this protocol in your practice is not just about adopting a new product, but about being part of a movement that values precision, efficiency, and environmental stewardship. This incredible technology offers an opportunity to elevate the standard of care in your practice while aligning with the growing global emphasis on sustainability.
For further information, please visit www.clearxaligners.com. n
about the author Dr sherif Kandil is the inventor of Clearx technology and shape-shifting clear aligners.

On average, practices sold to Group Buyers completed for the highest price in Central England at 8.68x EBITDA
- from the Dental Elite Interim Goodwill Report 2023
Scan the QR Code to download the 2023 Interim Goodwill Report or call us for a FREE valuation


In order to produce the best results for patients, prosthetically guided implant planning is essential. In order to produce an outcome which is aesthetic, functional, and easy for patients to maintain, clinicians must consider the final prosthesis, and the way in which this will inform dental implant placement.
Guided dental implant surgery provides clinicians with the tools they need for accurate surgeries and highly predictable results. While both freehand and guided methods can result in success, guided placement can help to lower the risk of complications, and ensure that the implant is placed in an ideal location. As such, it’s important that clinicians who wish to offer this method have access to the facilities they need to produce surgical guides, in order to provide predictable treatment to each and every patient.
the facilities needed for guided placement
In dental implantology, there is no ‘one size fits all’ approach. Different patients have different requirements, with some needing a single implant, others multi-unit solutions, and some full-arch treatments. Practices which do not have the resources in-house to accommodate each of these scenarios may find that they must refer patients elsewhere. However, when you provide guided implant treatment with Smile in a Box™, you gain access to all of the facilities you need to offer a wide range of implant treatment options. Smile in a Box™ allows clinicians and their patients to benefit from the Straumann® digital workflow – without the need for practices to invest in additional hardware or software.
Guided implant surgery workflows are made simple with Smile in a Box™. It’s easy to submit your case, so the team can plan the implant treatment ready for you to review and approve during a live online session. You’ll also have the option to plan the treatment yourself, if you prefer. Smile in a Box™ can then get started creating surgical guides and/or temporary restorations for you to approve, as well as offer high-quality,
or all patients, an effective and consistent oral hygiene routine is key for maintaining excellent oral health. No matter their oral health status, or whether they have undergone dental treatment, removing plaque and bacteria is key for preventing disease and minimising the risk of infection post dental treatment. Curaprox offers a line of Perio plus mouth rinses which caters to every patient. The range includes Perio plus Balance, Perio plus Regenerate, and Perio plus Forte all of which contain chlorhexidine, sodium fluoride, CITROX®, and PVP-VA. Each active ingredient is included to improve and protect patients’ oral health.
Perio plus Balance is designed for longterm use. Containing 0.05% chlorhexidine, Perio plus Balance reduces the risk of tooth decay, and is ideal for patients who have impaired motor skills as it can improve the results of cleaning.
centralised
CAD/CAM production. Once everything is ready, Smile in a Box™ delivers all of the components you’ll need to your practice in time for treatment –conveniently packaged in a box.
access the straumann® digital ecosystem
When practices outsource to Smile in a Box™ for their guided dental implant planning and guide manufacture, they gain access to the benefits of Straumann® digital solutions. The process is seamless, making each treatment a breeze, perfect for busy practices who would like to provide high-quality guided dental implant treatment to their patients. Smile in a Box™ allows clinicians to cater to everything from single tooth to edentulous cases. This makes it simple to meet the needs of patients, without investing in additional software or equipment.
Plus, clinicians gain easy access to the Straumann Group implant portfolio, including Straumann®, Neodent®, and Anthogyr® systems – simply select the best option for each patient.
Predictable care in every case
In order to provide predictable care in your practice, guided workflows offer security for you and your patients. With high-accuracy, taking into account the resulting prosthesis to achieve ideal placement, clinicians can ensure the best options for every patient. Plus, the flexibility afforded to clinicians who utilise Smile in a Box™ allows practices to meet the needs of a broader range of patients. This is the perfect option for those who are looking to provide an increased volume of dental implants, and for growing practices with limited resources and high demand. With access to innovative Straumann® technology, what better way to give your treatments the best chance of success?
To find out more about guided dental implant treatment planning with Smile in a Box™, please visit the website and get in touch with the team.
For more information on the Straumann Smile in a Box™, visit straumann.com/ digital/en/discover/smile-in-a-box.html n
Intended for occasional use, the revitalising Perio plus Regenerate mouth rinse promotes the healing of the gingiva. With a chlorhexidine concentration of 0.09%, and containing hyaluronic acid, it supports the regeneration of soft tissues following oral surgery, and is useful for treating dry mouth.

Perio plus Forte is your partner in intense healing
Perio plus Forte is the most intense mouth rinse of the range, intended for short-term use, and to promote intensive healing. The mouth rinse contains the highest level of chlorhexidine – 0.2%. This offers protection against harmful bacteria, by preventing the formation and accumulation of plaque. Perio plus Forte is best used before and after invasive dental procedures and to aid the healing of very irritated gums.
All Perio plus products contain CITROX®. The ingredient is naturally-derived from bitter oranges, and combined with polylysine amino acids to enhance its efficacy and prolong its working time.
Working particularly effectively when combined with chlorhexidine, it provides protection against bacteria, quickly eradicates biofilm and slows down its regrowth, and provides a pleasant taste to encourage compliance.
With Perio plus mouth rinse solutions suitable for the needs of every patient, oral health maintenance is made simple. The range is alcohol-free to prevent irritation, and contains PVP-VA. This forms a protective film over the teeth, gingiva, and

mucous membranes, and is combined with xylitol to prolong the results up to 12 hours. This is ideal for providing a strong defence against dental caries.
In addition to the Perio plus range of mouth rinses, Curaprox helps you to cater to the specific needs of every patient with the Perio plus Support toothpaste and Perio plus Focus Gel. The Perio plus Support toothpaste is ideal for use alongside any mouth rinse. Formulated with 0.09% chlorhexidine and CITROX®, the toothpaste helps to eliminate bacteria and offer long-term protection against infection. Plus, xylitol and sodium fluoride help to protect the teeth against decay and caries, with hyaluronic acid and PVP-VA working to regenerate and protect the gingiva.
Recommend Perio plus Focus to patients who are in need of intense, targeted care. The gel is ideal for patients who have undergone oral surgery, as it can be applied easily to prevent the build-up of plaque and minimise the risk of infection. It is formulated using hyaluronic acid, which soothes the gingiva and aids soft tissue regeneration.
By recommending the Perio plus range of solutions to your patients, you offer them a high standard of oral hygiene care, which is designed to support them in healing and preventing infection and disease. You know your patients’ needs best. This is why Perio plus mouth rinses, toothpaste, and gel are designed to meet the specific requirements of your patients – whether they need a daily oral hygiene boost to reduce plaque, or are recovering from oral surgery or dental treatment, there’s a solution for them. Please get in touch with the helpful team at Curaprox to find out more about the Perio plus range, and start recommending it to your patients.
For more information about Curaprox products, please visit curaden.co.uk n





































































































As dentists, we can often feel like we are standing at the foot of a huge mountain of immediate and pressing things to be completed. We might be facing challenging situations, complex patient treatments, detailed presentations to prep, time-intensive

continuing personal development, key lectures to deliver, events to attend, and any number of everpresent time constraints. My biggest motivator is the quick win.
I look at my outstanding things to do list and always start by getting through a few of the smaller tasks. This is my preferred way to do most things – and it also serves to (eventually) get the bigger projects done.
In my book, a quick win can be anything that takes less than half an hour and, ideally, less than 15 minutes. It might be replying to a few emails, making on-the-spot decisions, reviewing a patient case file, delegating, planning, or making some phone calls. But, what’s really useful to me, is doing the quick wins that prepare the groundwork for me to tackle the more demanding projects. Sometimes, simply getting off a blank page is all you need to kickstart your more time-intensive work.
There are a few well-known animal kingdom analogies here, including eating bite-size pieces of frog or elephant – you’ll know the ones. The idea is that you pick your most difficult or undesirable project first to get it out of the way. “Eat the frog” and then you can go on with your day knowing the worst is behind you. I’m not sure I agree with the entire sentiment of this. Difficult things are always made up of a series of smaller, sequential actions. In essence, the quick wins are effective precursors to completing the more complex issues. Sometimes you can’t get it all done at once –especially if you work in a team or have an ongoing treatment plan you are working through with a patient.
Rooting everything in Kaizen theory (as is my life’s philosophy), achievements can and should be made through incremental progress. Kaizen means ‘good change’ and reflects the results of slowly and continuously improving.
“Kaizen allows for continuous change in a way that doesn’t ask too much of people’s time and energy. It is peoplefriendly and easy.”
– Captain J Travis Doyle, Dover Air Force Base
When it comes to any learning experience, the quick wins are joyful and quite tangible. Each one bolsters confidence and lays the steps for the next layer of understanding. A succession of instant achievements becomes something much bigger and, together, has a greater impact. When I am teaching, I like to adopt this approach, as it provides a stepby-step route for students to a feeling of positivity and accomplishment. Also, without the small steps, you are not likely to make much real progress towards your final goals: quickly get to grips with A and then we can move onto A+B, and so on.
A quick win is especially satisfying as you can chart your progress, tick things off, and see how you are moving forward. So why not apply
Sometimes I feel very out of touch. The European Parliament has banned the use of Dental Amalgam from 1st January 2025. According to the BDA, the news will send “shockwaves across the UK’s already struggling dental services”. All well and good – the BDA has its finger on the pulse and knows many things that I do not.
But, but, but… my surprise is that anyone is still using Dental Amalgam. I completed the sale of my practice in May 2005 – that’s nearly 19 years ago – and my last Denplan “inspection/assessment” was probably a couple of years before that. As the practice had no mercury spillage kit, we were

deducted points, which was a little annoying, as the reason that we didn’t have the kit was that we had no mercury. No alloy either. No capsules. Not even an old amalgamator.
In short, the only mercury in the practice was safely incorporated in ancient amalgam restorations in extracted teeth or in the suction traps following removal prior to their replacement with tooth-coloured restorations, or even my personal favourite: gold.
As an aside, when I used to suggest the use of gold restorations to patients, their initial reluctance was usually overcome when I pointed out that you see most gold deployed in the mouths of dentists, their spouses, or their staff.
Back to amalgam: Surely the “phasing out” has been going on for some considerable time? Didn’t the Minimata Convention set a deadline for the discontinuation of its use? Or is my memory playing tricks with me?
Or could this be something to do with Europe bullying the poor Brits again by forcing them

the principle of the quick win with a little bit of Kaizen magic to the larger challenges, seeing them as a series of smaller tasks that make up the whole? Quick wins are just all the steps we need to take towards completing the more complicated or timeconsuming things we face but in manageable chunks of time and effort. So, instead of looking up at the mountain, start small and keep going. In no time, you’ll reach the summit without realising it. n
to stop using a discredited and polluting material? Could amalgam be saved by Brexit?
Dental Amalgam did do wonderful work for several generations. I still have half a dozen “alloys”, as they say in the US, which makes them close to 50 years old.
One question I would ask, if you are still an amalgam user, is this: Would you restore the teeth of your daughter or son, wife or husband with dental amalgam? Thought not. Why would you use it for anyone else then?
Of course, the first answer is because to use any alternative for patients you treat under NHS regulations would have to attract a realistic fee for the time and materials involved to place the material correctly – and that’s unlikely to happen.
Once again, we hit the buffers of the paradox between care and cost, which dental businesses have struck repeatedly, and increasingly, since the turn of the century. Accept the King’s shilling in the form of NHS rules and regulations, and you must spend from your own pocket for
About the author Dr Dhiraj Arora has two dental practices in Twickenham and Gerards Cross. He is also a Dental foundation Training educational supervisor for Health education england, Honorary Lecturer in endodontics at QMUL Masters programme, and runs his own courses via evo endo in Central London for general dentists. His background spans nHs and private settings, from Harley street to community HealthCare.


the privilege. Have an honest, up front, relationship with your patient about what, why, how and how much, and you can shoulder responsibility for doing what you were trained to do and not have to fudge the issue or, worse, upsell trinkets to make ends meet.
I don’t know how many times I have read the prophets of doom write on social forums that this is the end, only for the same people to bleat once again six months later at yet another cut. If you choose to compromise once again, then carry on, but if you dread having to square the NHS circle do something before it’s too late – for your sanity, for your quality of life and for your professional future. n












The mental health of practitioners is always an important topic of discussion within dentistry, addressing a great issue that has plagued so many individuals in the field: burnout.
The World Health Organization has previously described burnout as an “occupational phenomenon” rather than a medical condition, seen as a result of unsuccessfully managed chronic workplace stress.
Over the past few years, clinicians may well have succumbed to such exhaustion, leaving them drained, feeling negatively towards their role and less efficient in it, too. Finding ways to manage the pressures of dentistry and the emotional fatigue it may bring, and in turn fall back in love with the profession, is essential when the dental world begins to feel overwhelming.

Burnout can round the corner at any time, and it has become a growing issue within dentistry. This was true even before the Coronavirus pandemic, which may have only stoked the flames.
A 2019 study found that nearly 44% of its respondents felt that their level of stress was more than they could cope with, with the greatest reasons concerning regulation in dentistry, litigation and dissatisfied patients. Evidently, many dental professionals aren’t alone with this feeling. The odds are someone else in your practice may be experiencing these excessive pressures too. Burnout is troubling for a number of reasons. Firstly, the health of dental professionals could be compromised as a result of their occupation. Burnout has been seen to consistently link with cardiovascular diseases, musculoskeletal pain and depressive symptoms. The aforementioned study found nearly one in five dental professionals had seriously considered committing suicide at some point in their life, which calls for greater support for clinicians in a high-pressure profession.
Patients may suffer too. A high amount of stress and musculoskeletal disorders among dental professionals are linked with work ability and productivity loss, which could mean fewer individuals are treated over time, with potential errors to be made.
Finding ways to alleviate burnout is often easier said than done. Clinicians may find it difficult to pull themselves out of a rut, or even feel that as a consequence of improving their own health, they have to let the growth of their practice stagnate. After all, doesn’t taking a step back – which
could bring relaxation and rejuvenation – require less time with patients, who receive less care? In addition, simply pulling away doesn’t necessarily impact the daily challenges that cause burnout.
The first step to beating burnout is looking around at the situation and assessing what can be done. Talking to trusted professionals, friends and family can be essential for feeling support, as well as potentially brainstorming some possible solutions.
It’s then important to look at your day-today life and implement effective changes. Reclaiming time for yourself may be key to finding that ever-mystical work-life balance. Whilst it may feel like a thin line to tread, it could bring clinicians out of stressful environments and help to regain control over their everyday lives, as well as enhancing overall practice performance. This could mean strict boundaries are set on when work emails are addressed, or how much of weekends and evenings are spent reorganising notes.
Creating time in your week to do the things you love – be it spending time with friends and family, playing sports, or enjoying a hobby – may mean reducing your workload. To do so, the team that surrounds you could make the greatest difference.
surround yourself with talent
Delegating tasks is essential to freeing up time for personal and professional growth. To do so, clinicians must surround themselves with a team that they trust, who also buy into their ethics and share similar professional goals. Assigning extra roles to others is not the same as evading responsibilities; instead, it creates a culture of collaboration, where the team pulls in one direction and becomes more efficient.
Honing this culture is key to building a happy team and a productive practice, with the opportunity to take on new ventures and grow a patient base as a result. It could also increase an individual’s capacity for brilliant work every day by alleviating burnout.
Understanding how to build a team that buys into your vision and allows you to better structure a work-life balance is possible with the Business and Mindset Mastery course from the IAS Academy. Led by marketing scientist and entrepreneur Dr Prav Solanki, the day’s training helps clinicians devise an actionable plan for practice and personal growth, including ways to create and achieve goals in all aspects of life. Dr Solanki also provides insight on business processes and how to engage patients, to better improve their care journey.
Healthcare professionals seem to experience higher rates of burnout than other members of the working public, and it is a serious issue in modern day dentistry. Reaching out to those around you and amongst your team for comfort, advice and help could not only see your everyday life improve, but your practice grow, too.
For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470
(Press 1) n
About the author
Dr Tif Qureshi, founder and a Clinical Director of iAs Academy.
Correct use of tooth shades is essential when providing cosmetic dentistry, and creating fantastic smiles that patients love for years to come. To achieve exceptional results, professionals must first understand the colour matching process, and its significance in modern treatments.
Colour me intrigued
Oral health and appearance have a wellknown impact on an individual’s psychological well-being. Adolescents and young adults, in particular, place great significance on their facial characteristics, and when expectations aren’t met, they could experience a detrimental impact on their self-perception, self-image and overall quality of life.
Tooth colour will inevitably play a part in this subconscious judgement. Studies have shown that irrespective of age and gender, whiter teeth are seen to optimise appearance. It should come as no surprise that teeth whitening is one of the most heavily demanded aesthetic procedures today, with many individuals motivated by social media. However, tooth colour is obviously relevant in many other aspects of dentistry. In particular, when providing a restoration, it is vital to make it look as natural as possible. Colour matching here can be difficult, but when done well, the difference in outcome could transform from tolerable to exceptional.
Clinical vision
Colour theory and dentistry combine when judging the value (or lightness), chroma (saturation) and hue (dominant colour) of a tooth visually. This conventional technique is based on the Munsell colour system, which challenges the colour wheel by expanding it into three dimensions.iv
Applying a solely visual approach is not completely reliable, though.
Firstly, the clinician could make a mistake. This can be attributed to something as simple as colour blindness (which affects up to 4.5% of the UK population) or nerve fatigue, which may require short glances at a tooth for a more accurate decision. The lighting conditions may also affect colour matching, as could brightly coloured clothing and lipstick since colour perception is affected by an object’s surroundings. We must also consider that a tooth isn’t just one block colour; there is nuance that must be accommodated for. The primary colour of the teeth will be strongly determined by the dentine, and the more translucent enamel would play a small role with its ability to scatter wavelengths in the blue range. Hydroxyapatite crystals in the enamel contribute enormously to light scattering, as do the tubules within the dentine. Once again, under different lighting conditions, these may each react differently, resulting in contrasting decisions on the tooth shade depending on the practitioner or time of day.
At the cutting edge

reflections on the teeth, which goes a long way to help correct the overestimation of white opacities that can occur when using flash photography. The technique can also avoid issues with colour difference discrepancies when using shade guides. Research has shown that digital images taken with a polarising filter are superior to those without, especially in conditions of excess light, proving this to be a useful solution for enhanced shade matching.
Another technique clinicians are using is the eLAB system, designed by Dr Sascha Hein. This involves using a polar-eye filter alongside AI and advanced image processing algorithms to auto-calibrate RAW photographs and then automatically shade map teeth for exceptionally well colour matched restorations.
When used in addition to a purely visual technique, these techniques can help clinicians make valuable decisions that change the course of cosmetic dental treatment dramatically. They also enhance communication between the dentist and dental technician, by transferring a more accurate representation of the shade required for restorations. Of course, it’s important to be fully trained with the equipment available, ensuring a complete understanding of the processes and technologies involved.
expand your horizons
To build this knowledge and experience, clinicians could throw themselves into high quality training courses, or attend seminars on the topic by respected names in dentistry. By seeking insight from leading professionals, you can ensure you are at the edge of innovative treatment plans and equipment offerings. This way, you can continue to provide beautiful yet natural-looking outcomes that your patients will adore.
Expanding your experience and skillset in the cosmetic dental field is simple as a member of the British Academy of Cosmetic Dentistry (BACD), a world leading authority composed of professionals passionate about developing the future of aesthetic and restorative dentistry. BACD membership provides access to world-class speakers and exceptional CPD content, with educational events regularly covering subjects such as colour matching, whitening and restorative dentistry. It also connects you directly to the BACD community, which consists of many individuals who can provide help and advice on a variety of aspects of cosmetic dentistry. Cosmetic dentistry is built on providing patients brilliant aesthetic results. Tooth colour is an enormous component of this, but with the right knowledge and experience, and tools at the cutting edge of the field, clinicians can make seamless restorations easier and more accurate than ever before. For further enquiries about the British Academy of Cosmetic Dentistry visit www.bacd.com n
In order to obtain a superb, objective judgment, many clinicians use modern and increasingly effective tools.
For example, cross-polarised photography reduces or completely eliminates specular
About the author Luke Hutchings, president of the British Academy of Cosmetic Dentistry.

Annabel Thomas is Chief Operations Officer of the British Endodontic Society (BES). She discusses her experience of working within the society
Ihad actually never heard of the term ‘endodontology’ before starting with the society but, having worked with metallurgists, auctioneers, psychotherapists and psychiatrists before, I thought, why not dentists? After all, each of these professional groups use conferences as one way of learning and networking; manage their organisation by committee; and have the development of their profession as their object. I’m still waiting for my degree in Geography to come in useful – and no, it doesn’t help me find places to hold conferences!

In a way, the society found me. A colleague at the Royal College of Psychiatrists knew Dr Carl Nehammer (BES Past President) and they told me about an opportunity to work with the BES.
As Chief Operations Officer for the BES, my role has changed over the years. It has always involved attending Council Meetings, arranging conferences, budgeting, and managing membership subscriptions but, with the increasing

use of technology, I’ve added web technology, social media, and public relations to the role! Additionally, Charity Commission and Company House administration, exhibition planning, and large Congresses have also become part of the responsibilities! Suzanne McLean
now supports me part-time with managing memberships and awards. What I enjoy most about the BES are the members. They are all prepared to give their time to developing the profession, and are supportive and enthusiastic – and they all know how to enjoy themselves!
Outside of work, I play tennis and some golf. I also volunteer in our local library for a few hours a fortnight. Plus, of course, I enjoy socialising!
For more information about the BES, or to join, please visit britishendodonticsociety.org.uk


Human Bone



OsteoBiol® xenografts cleverly retain most of natural bone Collagen/ Mineral matrix. They reflect the massive progress in biomaterials technology. Collagen has been shown to stimulate bone regeneration processes(5). Two experimental studies showed about 50% newly formed bone after one and two months in rabbit femurs(5) and maxillary sinuses(6), respectively. Generally, gradual graft resorption and adequate new bone formation(1,4) can be expected. Scientific literature and clinicians report adequate bone regeneration and high implant success rates(1-4)



Truly, OsteoBiol® represents the next generation of bone regenerative materials.



All GDC registrants must complete CPD and log it on the GDC’s e-CPD system. DCPs (dental nurses, hygienists, therapists, technicians) need to declare their CPD each year by 31 July – dental nurses have to complete 50 hours of verifiable CPD in each five-year cycle. So far, so good… But here’s where it gets tricky: Within those five years, each year by 31 July a dental nurse* has to have logged at least 10 hours over two subsequent years. In other words, if they log six hours in Year 1, they must log at least 4 hours in Year 2, and then at least six hours in Year 3, and so on.
On the one hand, the GDC says it is trying to be “less prescriptive” – plans are underway to do away with the scope of practice and rulesbased guidance to registrants, and introduce “guidance”, which puts the onus on the registrant’s own experience and knowledge, thus leaving dental nurses vulnerable to exploitation – but on the other, they are requiring registrants to declare a minimum amount of CPD each year, in an unnecessarily complicated system! In the midst of the worst recruitment and retention crisis dentistry has ever known, with general dental practices struggling to get and keep dental nurses (although, as Rebecca

Why? I have no idea! Surely a much simpler plan would be to require dental nurse registrants to complete and log 10 hours each year? Or allow them – as adult registered healthcare professionals – to decide for themselves when they are going to complete CPD within their fiveyear cycle?
Silver recently pointed out – there is not a lack of dental nurses, there is a lack of dental employers prepared to pay acceptable salaries and treat dental nurses as fellow registered professionals! There are plenty of dental nurses – they are just choosing to work in other fields, where they can earn a reasonable
salary and be treated like colleagues, not skivvies!), the GDC is erasing dental nurses from the Register for minor CPD infractions. Being erased from the Register means you can’t work in dentistry. If you failed to log the required number of hours by the deadline –perhaps because you have had a baby, or lost a parent or a spouse, or been in hospital, or have been in an accident (all pretty traumatic things to happen) what does the GDC do? It strikes you off the Register, so you can’t work and, therefore, can’t earn!
Let’s be clear: I’m not talking about people who have got to the end of their five-year cycle and failed to complete their required hours. I’m talking about people who are an hour or two short of the “10/2” requirement in the middle of their cycle. People who could easily make up the missing CPD in the following months. Instead of being sympathetic to their personal difficulties, the GDC says, “Sorry, the legislation doesn’t give us leeway to make allowances, no matter how awful your situation – we are just going to exacerbate your problems by taking away your right to work and earn money to pay your bills.”
BADN is meeting with the GDC on this very subject – and I can say that some GDC staff do realise the ludicrousness of striking off registrants for missing an hour of CPD, particularly in the current crisis, and are trying to change the system. But, like the mills of God, the GDC grinds extremely slowly –and in the meantime, hundreds of dental professionals are unable to work because of a minor infraction. Indeed, many of them are so
Over the last few months, I have seen increasing numbers of practices either wanting to introduce a dental plan or increase the number of patients joining an existing plan.
For me, it’s something that will be a practice-builder, especially as we are seeing many practices withdraw from NHS dentistry or reduce their contracts.
In some areas, practices are being asked to provide access to higher needs/urgent dental care as a priority over those whose dental health is good and stable. Some practices are having difficult conversations with patients who have been attending every six months for many years, who are now deemed to be not in the highneed group.
So, how do we communicate this with our patients? It’s likely
that your Front of House teams will be at the forefront of these conversations.
I believe there needs to be a clear and honest approach as well as alternative options provided to this group of patients. Offering NHS patients the choice to join a member plan is a great way for them to be able to continue the care and frequency of visits they have been accustomed to, but it is vital that these changes are implemented and offered very carefully.
Can you offer a range of plans appropriate for different age groups?
• 0-6 years
• 7-18 years
• Young Adult Plan – 18-25 years
• Adult Simple
• Adult Comprehensive
As with any plan, you can customise what is included (or not). Using a plan provider still allows you to do this.

disgusted with the way they have been treated, they do not intend to return to dentistry.
Which is why we are supporting the Saving Grace campaign and petition – see the BADN website or look it up on Google – now is the time for common sense to prevail! n
* I am using “dental nurse” as an example here – but the same could apply to any GDC registrants, only the numbers of hours required and the date are different.
About the author pam swain is Chief executive of BADn

Here are some other considerations to plan for:
• Check your financials – What are your hourly costs, and what do you need to generate per hour to make the profit you require?
• Zoning – Calculate how many patients you will need to provide exams for over the year, allocating and zoning accordingly. For example: 600 plan patients, each with 2 x 15-minute exam visits per year means will require approximately 6.5 hours per week. This can then be applied for hygiene visits, etc.
Decide how you are going to notify patients, plan your marketing, and remember to be confident and positive about your service.
Ensure that patients feel and experience added value. I have witnessed so many conversations whereby a patient’s practice has withdrawn NHS care and offered

private options. The patient has commented that if they are going to have to pay, they will find a “proper” private practice, not an NHS practice that has just decided to become private with no added value for those converting. Train your team not to fall into these conversations and show those patients that you are a “proper” practice that will deliver an amazing service. n
About the author Lisa Bainham is president at ADAM and practice management coach at practice Management Matters.

When a patient presents seeking dental implant treatment, it’s important to conduct thorough assessments. Open conversations with patient about what they should expect from treatment is equally important, as well as discussing any potential risks, and providing them with the space to ask any questions they may have. Additionally, clinicians must make accurate clinical records of each consultation, to protect themselves in the event that a patient complains about their treatment.
During each implant consultation, there are a number of key factors which must be discussed and assessed to ensure that each patient is a good candidate for dental implants. For example, if the patient is a smoker, clinicians should explain that smoking can increase the risk of implant failure and provide cessation advice. Or, if clinical assessment reveals that the patient has active periodontitis, clinicians should recommend that this is treated and stabilised prior to considering dental implants to ensure the best chances of success.
Additionally, there are a number of factors which must be assessed at each follow up appointment, to ensure there is an accurate record of the implant’s situation. Monitoring the patient’s satisfaction with their prosthesis at each appointment, regarding aesthetics, functionality, and cleanability can help to determine if changes are
needed. Clinicians should also record any inflammation in the soft tissues surrounding the implant, the patient’s oral hygiene, bleeding on probing scores, the depth of any pockets, occlusion, mobility, contact points and emergence profile, and take radiographs annually for the first three years of function. Each of these allow clinicians to understand any potential issues, and advise the patient about future treatments or management techniques that may be required to maintain their oral health.
The value of nuanced discussions with patients
Dental implant treatment is unique in that, when compared to many other restorative options, it is expensive and elective. As such, dental implant patients are likely to have very high expectations. While this is to be anticipated, it’s important that this is managed, to ensure that the patient understands the limitations of the treatment, and to help avoid disappointment if their ‘perfect’ smile cannot be achieved in the way that they had hoped. Conversations surrounding what to expect should be completely personal to each patient, depending on their initial situation, and what they perceive to be a good outcome. In order for the patient to provide consent, they must be fully informed about the treatment, and what they can realistically expect to happen, in addition to any risks and complications. This also enables them to ask any questions they may have as a result of these conversations, and it’s important to allow patients the time to do this. It can
also be helpful to send patients a summary of their appointment and information about treatment options afterwards – keeping lines of communication open, should they have any additional queries, or if they would like more time to reflect on the information and consider their options.
All records of consultations must be contemporaneous, accurate, and complete in order to be acceptable to the GDC. Traditionally, this has required either a dentist on their own, or with the assistance of their dental nurse, to write notes during the appointment. However, this process could leave room for information to be missed, which may become tricky should a patient make a complaint. Additionally, physically taking notes during each appointment may mean that clinicians are distracted, and unable to fully engage with their patients. Audio recording may be a helpful adjunct for many clinicians. This allows them to engage in nuanced conversations with their patients without the need to constantly take thorough notes at the same time. Some modern recording systems are even able to transcribe the audio, making it simple to see what was discussed. Additionally, this provides the opportunity for clinicians to listen back to previous appointments prior to seeing patients, to refresh their memory, and learn from their experiences. Most valuably, of course, is the benefit of a completely accurate and contemporaneous record of each appointment, exactly as it
happened. This offers additional context too, enabling clinicians to hold a record of the tone of all conversations had, and get a sense of the patients’ feelings towards treatment options and plans.
Members of the Association of Dental Implantology (ADI) benefit from a 20% discount on a Dental Audio Notes subscription. The software package for audio recordings is designed to support consultations by providing a comprehensive record of the appointment. Dental Audio Notes also manages storage, security, and privacy of data, for total peace of mind. As such, clinicians only need to press ‘record’ and begin their appointment, and Dental Audio Notes will take care of the rest in a secure and compliant manner.
Keeping accurate records of all appointments, including dental implant consultations, is essential for providing patients with high standards of care. In order to be sufficient, records must be accurate and contemporaneous, making audio recordings a fantastic adjunct to written notes, supporting the clinician in the event that they need to refer back to a previous appointment.
For more information, please visit www.adi.org.uk
About the author
Dr Zaki Kanaan, ADI President.











Dr Aled Clement’s success story
In the dynamic world of dentistry, Tipton Training continues to shine as a beacon of advanced post-graduate dental education, providing dentists the opportunity to learn new skills and gain more experience in different fields of the profession.
With an increasing demand for dental implants, driven by patient preference and technological advancements, Tipton Training’s Level 7 Certificate in Dental Implantology offers a comprehensive pathway for dentists to advance their skills and expand their treatment options in practice.
One dentist that has up-skilled and fulfilled their ambitions with the help of Tipton Training is Dr Aled Clement, who has notably achieved a remarkable milestone by successfully completing all four of Tipton Training’s core Level 7 Certificate courses, with his latest accomplishment being the Level 7 Certificate in Dental Implantology.
In an exclusive interview, Dr Clement generously shares insights into his inspiring journey, highlighting the profound impact that Tipton Training and its courses have had on his skills, confidence, and patient care.
Having qualified from Cardiff University in 2009 and spending eight years working as an associate, Dr Clement made a pivotal decision to acquire his own practice. With the practice being predominantly private, Dr Clement recognised the need to up-skill to meet the demands of providing private dental treatments to his patients. Reflecting on his journey, Dr Clement states: “Having worked through the Restorative, Operative and Aesthetic courses with Tipton Training, Implants were the missing component of the practice. Why refer these patients out of the practice when we could provide them in-house, with the right training?
“Having met Dr Maria Hardman during the restorative course (one of the lead mentors on the Implant course), I started a collaboration with Maria to introduce dental implants into my practice.
“The next obvious step was to gain the qualification necessary for myself to begin providing implants to my patients. I was
also keen to continue my training with Tipton Training, as their qualifications are formal Level 7 courses, quality assured by EduQual and approved by the Royal College of Surgeons of England.”
Therefore, in early 2023, Dr Clement embarked on his Implant training with Tipton Training, marking the commencement of a transformative learning journey.
Completing the Level 7 Certificate in Dental Implantology was nothing short of a gamechanger for Dr Clement. “It has given me the confidence and skills to select suitable patients for implant placement, as well as being able to effectively treatment plan and place implants surgically.”
While he was already engaged in restoring implants through his collaboration with Dr Maria Hardman, the formal teaching received during the Implant course was invaluable in refining his skills in restoring and placing implants.
Dr Clement commends the approachability of the dental tutors on the Implant course, emphasising that, “They are always more than happy to go over anything that the delegates may not understand or to help with treatment planning. The course is designed in a holistic manner in that treatment planning is restoratively driven and delegates are taught to look at the whole clinical picture, not just at the edentulous area.
“The live surgery days are always staffed with the full teams including supervising dentists, experienced dental nurses, dental technicians, and representatives from the implant suppliers, giving superb support at every stage throughout the implant journey.”
The course has empowered Dr Clement to deliver optimal dental care whilst expanding his treatment options. He notes: “My patients now have more treatment options


and no longer have to be referred out to other dentists to complete their treatment. I can work confidently in the knowledge that I am providing the best possible dental care to my patients and that I have a strong network of like-minded colleagues that I can call on for help and assistance if necessary.”
Support and guidance
Applauding the unparalleled support and guidance provided by the mentors, Dr Clement attests: “The support and guidance are second to none. They go above and beyond to ensure you are getting the most out of your educational journey with Tipton Training.
“The learning experience is a perfect blend of academia and hands-on training with instructors that actively work in practice and are therefore able to share their wealth of knowledge and experience from the real world of implant dentistry.”
advice for dentists considering similar training
Drawing on his extensive experience, Dr Clement undeniably recommends the Tipton Training Level 7 Certificate in Dental Implantology to fellow dentists considering learning a new skill and venturing into the realm of implants. His message is clear: “It will give you the confidence you need to identify and treat your patients with implants. My dentistry has changed for the better since undertaking the courses with Tipton Training. I am a happier and more confident dentist for having completed their courses.”
To those contemplating enrollment, Dr Clement offers reassurance. “There is nowhere better to begin your post-

graduate education than Tipton Training!” His endorsement is rooted in Tipton Training’s rich history of successfully training thousands of dentists for more than 30 years.
Dr Clement concludes by adding: “My patients benefit every day from what I have learnt during Tipton Training’s courses, and I am so much happier and confident in my career since my training.”
Dr Clement’s journey serves as a testament to Tipton Training’s unwavering commitment to nurturing dental professionals and propelling them towards excellence in their careers, affirming Tipton Training to be the premier destination for post-graduate education. Encouraging fellow dentists to embark on a similar path, Dr Clement declares, “I can honestly say it has changed my career for the better.”
If you are ready to begin your own Implant journey with Tipton Training and achieve similar success, visit www.tiptontraining. co.uk or call +44 (0)161 348 7849. n





















Guests join us from all areas of the industry to provide their own unique perspectives on a wide range of topics, from manufacturers and figureheads of various dental organisations, to those in the trenches working in practice, and more.





For











Nothing is o limits in The Probe Dental Podcast, so be sure to tune in wherever you get your podcasts!






































































Ski trips are exciting. Nothing compares to the exhilaration of descending a snow-filled mountain on a sunny day, marvelling at the amazing surrounding scenery. But the extreme weather conditions that make the trip so good, such as icy temperatures and intense sun, can wreak havoc on the lips. Indeed, somewhat ironically despite the cold, lips are more likely to get burnt on the slopes than at the beach because at high altitude the sun is more harmful than at sea level.
In addition, the gleaming white snow acts like a mirror, reflecting up to 80% of the sun’s ultraviolet (UV) light, which means double trouble for the lips as they are hit from both above and below. Added to that, although the mountain air is cleaner, it is a poor filter as there is less in the way for the scorching UV rays to pass through. Indeed, the World Health Organisation (WHO) reports that UV rays strengthen by up to 12% with every 3,000ft increase in altitude.
However, many still argue that it seems odd to apply SPF when surrounded by a carpet of snow and, even if they apply sunscreen to their faces whilst on the slopes, they often leave their lips unprotected, which can result in them becoming burnt and scaly.
But the good news is that most lip problems are preventable, so here is a proactive guide to keeping our patients’ lips healthy and protected whilst on a snowy holiday.
uV rays
Unfortunately, there is still much confusion about the sun’s ultraviolet A, B and C waves, and what they do.
UV irradiation in the form of UVA is long wave, capable of passing through clouds. It is associated with ageing as it infiltrates the skin, affects the elastin, and leads to wrinkles, sun-induced skin damage and cancer. UVB is shortwave and the form of UV irradiation most associated with sunburn and malignant melanoma and basal cell carcinoma. So, both UVA and UVB are harmful when they enter the atmosphere, remember.
• UVAgeing
• UVBurning
UVC has the shortest wavelength and is of less concern as it is usually absorbed by the ozone layer (so long as it is not depleted).
Sun protection factor
SPF stands for ‘sun protection factor,’ although it really means ‘sunburn protection factor.’ SPFs are rated on a scale of 6 to 50+ based on the level of protection they offer, with grades between 6 to 14 offering less protection and ratings of 50+ proffering the most effective UV protection. It actually means that, with an SPF of 30, it would take 30 minutes to get burnt, while SPF 15 means 15 minutes of exposure can cause sunburn.
Why wear SPf lip balm?
As mentioned above, lips are often overlooked when it comes to sun protection, but they contain no protective melanin, and the skin is thinner and less robust than the rest of the face, making them vulnerable to UV rays and susceptible to abnormalities including carcinoma. The lower lip is particularly at risk because it usually protrudes more resulting in increased exposure to the sun.
Therefore, SPF is essential with a minimum of factor 30 lip balm recommended for high altitudes – although children and those with very fair skins will need an SPF as high as 50. It needs to be reapplied regularly, especially after eating and drinking, and to make the protection even more effective, it helps to apply a generous layer of moisture first. Ideally, it needs to be a broad-spectrum balm to help block both UVA and B rays, and prevent the burning and damage that can cause lip abnormalities. It also helps if it’s water-resistant in case of face-planting into the snow! Luckily, ski jackets are designed with plenty of pockets to stash SPF lip balm in.
• It is important to remember that some balms containing an SPF may not have any UVA protection, meaning that despite best efforts to hydrate and protect the lips, they still get damaged. Therefore, always read the label and use a recommended product.
• It cannot be stressed enough that SPF lip balm needs to be reapplied every two hours, or immediately after eating, drinking, face planting, and excessive sweating.
• Wherever possible, sit in the shade whilst enjoying refreshments, especially in the middle of the day when the sun is at its most powerful.
• Keep hydrated as this prevents the lips from drying out. However, that means drinking lots of water – not Aperol Spritz!
• Since wearing a wide-brimmed hat while skiing is not practical, it makes sense to wear a face mask. As dental professionals,
we are accustomed to wearing a mask and they became a way of life during the recent pandemic. But they are even more familiar to experienced skiers. Not only will a good face mask protect the lips from UV rays but also keep air pollutants and flying debris at bay.
from slopes to slumber… Après-ski is French for ‘after ski’ and refers to all the fun activities to participate in after a ski run. But it is important to remember the skin barrier on the lips will have been blasted not only by the icy temperatures and a day spent on the slopes, but also the subsequent central heating and dry sauna air. So, before exploring what the ski resort has to offer, it makes sense to apply a moisture rich balm to comfort lips, followed by a dedicated lip mask before bed. And finally, as F.M. Alexander said, ‘People do not decide their futures, they decide their habits and their habits decide their futures.’ This is so true of getting into the habit of wearing SPF lip balm, as failure to do so can result in very sore lips.
References available on request. n
about the author ali Lowe is an awardwinning dental hygienist based in Cardiff. She is the founder of fit Lip uK – a campaign aimed at encouraging people to wear SPf lip balm in order to protect their lips, prevent lip cancer and keep their mouth healthy.

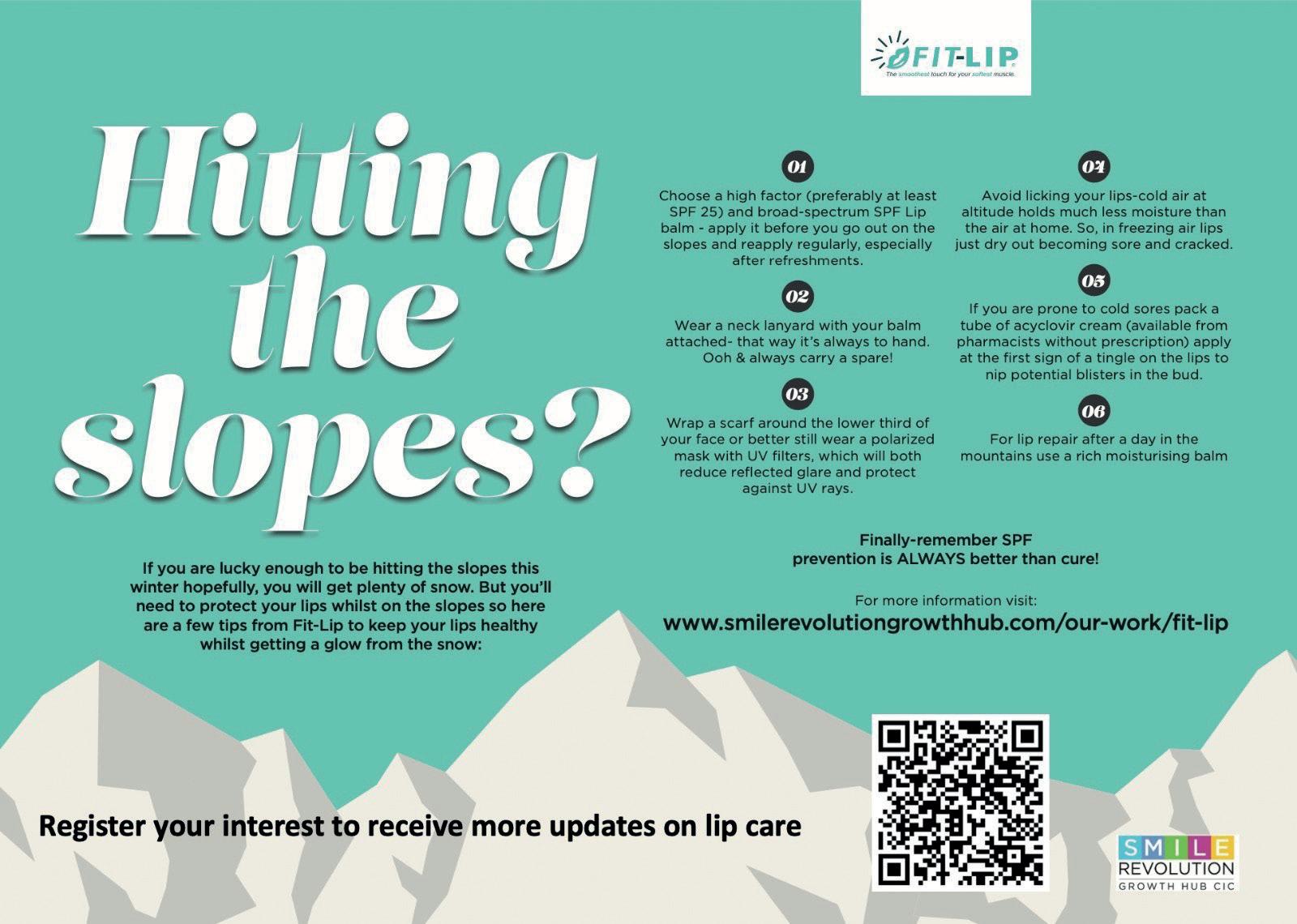






























Entries are open for The 2024 Dental Awards, closing on 23rd February. This year, the process of entering yourself or nominating a colleague or practice for The Dental Awards is easier than ever. Simply visit The Probe website at the-probe.co.uk/awards and complete the online form, uploading supporting materials where required. You can save your application progress at any time to return to later should you need to gather further evidence.
The most highly esteemed dental awards ceremony out there, each of the categories are judged by a panel of well-known industry experts with superior knowledge of their respective fields. The event provides an annual showcase for practices looking to shine a spotlight on the vast skill and talent that exist within their teams. The 12 categories are:
• National Smile Month Award
• Dentist of the Year
• Young Dentist of the Year
• Dental Therapist of the Year
• Dental Hygienist of the Year
• Practice Manager of the Year
• Dental Nurse of the Year
• Front of House/Receptionist Award
• Practice of the Year
• Team of the Year
• Best Outreach or Charity Initiative
• Best Website or Digital Campaign
The high volume of entries in 2023, from dentists, dental therapists, dental hygienists, dental nurses, front of house and practice managers, as well as dental teams and practices as a whole, truly reinforced the immense ability, technique and flair present within the profession, as well as the high esteem in which the Dental Awards is held.
2024 marks the 26 th edition of this prestigious event that, for more than a quarter of a century, has sought to recognise the outstanding individuals and teams whose dedication and drive continues to raise standards throughout the UK dentistry profession.
Winning or becoming a finalist in the Dental Awards is a tremendous accolade that provides a significant boost to the profile of a practice. Not only is the event an opportunity to share in the happiness and success of those who win an award, but it offers the chance to see what fellow dental professionals are doing across the United Kingdom.
All entries must be received by 23 rd February 2024.
Visit the-probe.co.uk/awards/ to find out more about entering this year’s awards.
Good luck! n



















in particular, offering insights into managing this often-overlooked
When it comes to tooth wear, as a practising dentist, there are two primary aetiologies that I encounter most frequently.
The first, erosion, is often linked to dietary habits. An excessive intake of acidic beverages, including fizzy drinks and alcohol, particularly those with added citrus like lemon, contributes significantly to dental erosion. Additionally, the prevalence of modern diets high in acidic fruits further exacerbates this condition.
Medical issues such as bulimia and gastroesophageal reflux disease (GERD) also play a role, as they introduce gastric acids to the oral environment.
The second major aetiology is attrition, largely due to bruxism – the grinding and clenching of teeth. This physical wear is often a response to psychological stress, which has become increasingly common in our fast-paced society.
the prevalence and consequences of bruxism
Various reports suggest that anywhere from between 20 to 30% of the population grinds their teeth to some degree, and virtually everyone will clench and brux at some point. It is, in fact, a more significant issue than decay and periodontal disease in terms of prevalence.
Tooth wear caused by bruxism is called occlusal disease in dental circles. Occlusal disease encompasses problems arising from the way teeth meet and function together. This includes joint and muscle problems, breakdown of dental restorations, and broader implications on overall health and well-being.
The condition often affects one or possibly two components of the masticatory system, typically not all at once. If the temporomandibular joints are affected, it can lead to joint pain, difficulties in chewing, or noises like clicking and grating. Muscle involvement often results in headaches, facial aches, and pains behind the eyes. Teeth can wear down, fillings and restorations can break, and the periodontal ligaments can become stressed, leading to tooth mobility.
It may have further repercussions, depending on the way sufferers respond to these symptoms. For instance, this condition often leads to heightened tooth sensitivity, prompting a shift towards softer food choices. Consequently, individuals tend to consume foods rich in carbohydrates while avoiding tougher textures, like meats, which are more challenging to chew.
This dietary adjustment can result in a notable reduction in protein and fibre intake, thereby potentially impacting overall body health. Such changes in
eating patterns not only affect oral health but can also have far-reaching implications on the individual’s general well-being, both physical and psychological.
Managing bruxism and occlusal disease requires a multifaceted strategy, with the primary aim of alleviating stress.
In treatment terms, the first line of defence in managing bruxism is the use of occlusal splints. These devices, when correctly designed and used, can prevent further damage to the teeth and jaw. However, their effectiveness depends on factors like design, cost, and patient compliance. Understanding the theory behind splints is crucial, as some types can worsen the condition. For example, soft splints, which are generally the only option available on the NHS, can be helpful for some but detrimental for others, while hard acrylic, fully adjusted splints offer more predictable results. When teeth are already damaged, restorative treatment becomes necessary. This can range from using composite materials for minor repairs to full reconstructions using ceramics or gold, the latter of which is particularly well-accepted by older patients. The choice of material and technique must be tailored to each patient’s specific needs and circumstances.
Restorative treatments also need to take into consideration the correct occlusal principles to ensure longevity of the restorations and health of the masticatory system.
General dentists can manage a significant proportion of cases involving bruxism and occlusal disease. Continuous education and practical training are crucial for dentists to diagnose, treat, and manage these conditions effectively.
About 80 to 90% of treatments fall within the scope of general dental practice, with the remaining cases requiring specialist referral.
It is not at all as daunting as you might think, when you consider that to get started dentists need to understand just five principles:
1. Establishing jaw joint position: our initial approach focuses on aligning the jaw joint into its proper position, referred to as either ‘centric relation’ or ‘retruded axis position’. Despite the different terminologies used in occlusion, both terms signify the same position, aiming to align the condyle (jaw joint) correctly.
2. Ensuring tooth contact: once the jaw joint is accurately positioned, it is crucial to verify that all teeth make simultaneous contact. This uniform contact across all teeth is essential for a comfortable occlusion.
3. Anterior guidance during

movement: in movements such as forward and backward or sideto-side motions, it is important that the front teeth facilitate the sliding motion while the back teeth disengage. This concept, known as ‘anterior guidance’, is key to proper dental function.
4. Avoiding back teeth interference: during various movements, including bruxism, it is important to ensure that the back teeth do not interfere with one other. This means avoiding balancing side or nonworking side interferences which create class 2 leverage to maintain oral health.
5. Posterior stability: the focus here is on ensuring that the forces exerted on the back teeth are directed down the long axis of each tooth. This approach seeks to ensure that every posterior tooth has three points of contact to prevent tilting and maintain stability.
So, the key to managing these conditions lies in education.
Understanding the principles of occlusion, the mechanics of splint therapy, and the nuances of restorative treatments is essential.
Dentists must be proactive in identifying signs of bruxism and occlusal disease and should not hesitate to implement appropriate interventions, such as splints, to prevent further damage.
embracing a holistic approach
As dental professionals, we must integrate these insights into our practice, ensuring comprehensive care for our patients. This approach not only addresses immediate dental
concerns but also considers the broader implications on the patient’s overall health and quality of life. n

If you would like to know more about this important postgraduate topic, Prof. tipton will be delivering a presentation entitled ‘treatment Options for the Bruxist and Wear Patient’ at the British Dental Conference & Dentistry show, to be held in Birmingham on 17 and 18 May. For further details, to register for your tickets and to see the full line up of expert speakers, simply visit birmingham.dentistryshow.co.uk.
About the author Prof. Paul tipton is an internationally acclaimed specialist in Prosthodontics who has worked in private practice for over 30 years. He is now Professor of Restorative and Cosmetic Dentistry at the City of London Dental school. In addition, Prof. tipton is the founder of tipton training Ltd, one of the UK’s leading private dental training academies (tiptontraining.co.uk).

The World Endodontic Congress (WEC) is delivered by the International Federation of Endodontic Associations (IFEA), and will be hosted by the British Endodontic Society (BES) in September 2024. Entitled “Phases & Interfaces” the event will be held at the Scottish Event Campus (SEC), Glasgow, where delegates can expect an enriching educational and social programme against the stunning Scottish backdrop. The international event brings together world-leading speakers presenting sessions on a wide range of topics – ideal for endodontists and those with an interest in the field to expand their knowledge.
An enriching educational and social programme
Delegates can expect an exciting educational programme, presented by a range of international and UK based speakers, these will include Daniel Černy, Elisabetta Cotti, Adham Abdel Azim, Phil Tomson, and Paul Lambrechts. Session themes include trauma, regeneration, imaging, vital pulp therapy, surgical endodontics, restorative dentistry, and systemic health, with speakers introducing clinical techniques, and discussing new technological developments.
The social programme offers delegates the ability to come together with colleagues for the perfect balance between learning and socialising. Upon their arrival on the 11th September, delegates can attend the Glasgow Science Centre for a Welcome Reception. Here, the IFEA WEC 2024 will officially open, and attendees will have the opportunity to network with endodontists, general dentists, and other dental specialists from around the world.
For those looking for a real taste of the culture, join colleagues for a Scottish ceilidh. Held at the Merchant Square, attendees will have the opportunity to take part in traditional Scottish dancing
in Glasgow’s culture, fashion, and food quarter. Additionally, the Congress Dinner offers delegates the chance to socialise at the iconic Kelvingrove Art Gallery and Museum. This evening of live music, networking, and dancing, with a full Scottish menu and a Scottish Piper will not be one to miss, bringing the field together in a truly unique environment.
World-class networking
Networking is a key aspect of the WEC, allowing delegates and speakers from around the world to meet and discuss recent developments in endodontics, cutting-edge techniques, and the newest technology. With plenty of opportunities to socialise and learn with colleagues from across the world and various dental disciplines, the WEC offers attendees the ability to expand their knowledge of the profession in a supportive and innovative environment.
This is particularly useful for our members who are new to endodontology, and those who are looking to enter the field. It will be ideal for professionals who would like to better identify and treat issues for their patients and network with experienced endodontists who accept referrals. Delegates who are looking to improve their endodontic abilities should also consider getting involved with the BES Early Career Group.
Scotland within reach
IFEA has partnered with Glasgow Convention Bureau to source discounted accommodation nearby the venue. For the best discounted delegate rates, attendees should book early to avoid disappointment. Taking place at the SEC, situated on the north bank of the river Clyde, the WEC is well positioned for delegates to make the most of their time in Glasgow.
The city is well connected, and the WEC is the perfect excuse to discover what it has to offer. With Glasgow Science


Centre, The Clydeside Distillery, Pollok Country Park and Burrell Collection, and so much more all within reach, what better way to get to know a new city? Plus, for keen golfers looking to extend their stay in Scotland, the WEC has arranged a number of premier golf experiences in association with SGH Sporting Events to enable delegates to play on some of Scotland’s most renowned golf courses.
BES membership and registration for WEC
Registration for this highly anticipated event is open and, thanks to the support of




our sponsors and exhibitors, promises to deliver an excellent social and educational programme for the benefit of delegates. All of this is alongside a fantastic trade exhibition, allowing delegates to discover all of the latest tools and technology to enable them to improve the care they provide. Be sure to register in plenty of time to secure your place at the best rates.
Register today for IFEA WEC 2024 at ifea2024glasgow.com/registration
For more information about the BES, or to join, please visit www.britishendodonticsociety.org.uk or call 01494 581542





























Josette Camilleri is a Clinical Professor of Endodontics and Applied Materials and Honorary Specialty Dentist at the School of Dentistry, Institute of Clinical Sciences, College of Medical and Dental Sciences, University of Birmingham. After qualifying as a dentist from the University of Malta, she completed her doctoral degree supervised by Professor Tom Pitt Ford at Guy’s Hospital, King’s College London and then returned to the University of Malta to fulfil roles undertaking research and teaching in Civil and Structural Engineering and Restorative Dentistry Departments. Having published more than 160 papers in peer-reviewed international journals, Josette focuses her research in the field of endodontic materials. About the topic, she says:
“I have researched extensively hydraulic cements collectively known as bioceramics, which are not new in dentistry. They first entered the dental market back in 1993, but for many years there were few materials on the market that were used mostly as reparative materials. Currently, many companies have produced their own bioceramics, increasing their

availability to dental professionals.
“Although they are all put into the same category of ‘bioceramics’, it is essential that clinicians realise how different the materials can be. This means that they all interact with their environments differently and therefore produce varying results. Every patient’s treatment is unique – details like the amount of blood present or

the irrigation method implemented will affect how the material reacts. Given the growing trend for bioceramics in practice over the past decade, I have been lecturing more and more on the topic due to the increased interest in these materials and the clinical challenges being faced.”
Considering why these challenges occur, Josette continues:
“We can’t apply the same clinical techniques to different materials and expect the same results. Biomaterials are water-based while the rest of the endodontic materials have different chemistries.
“Other factors like the irrigation solution used, the flow properties of the bioceramics being placed and how it interacts with the dentine all need to be considered to avoid challenges.”
So, how can these issues be avoided in order to achieve the best endodontic outcomes? Josette suggests that clinicians need to better understand the materials they are using. The protocols for using bioceramics and the way the materials are developed in the lab also need to change.
“Clinicians need improved access to education about the materials on the market,” she says. “It is crucial to really understand bioceramics and how they work. This training and sharing of information must come from independent sources – individuals, training providers or academics who are not affiliated with a particular company. This is why it’s so important to hear from people in the field at conferences.
“Further still, unless the standards and protocols are rewritten, we will continue to have issues in practice when bioceramics are applied. Current techniques are not suitable for the chemistry of the materials.
“There is also still plenty of development needed with bioceramics. We have spent too long testing the materials in the wrong way, treating them as if they are
the same as each other. Clinical techniques can’t be enhanced until the testing methodologies in the lab are updated – they need to be clinically translatable from lab to practice for the best results. Material science in endodontics is not very advanced and we have been doing the same thing for the last 50 years. This needs to change. There needs to be more collaboration between industry and profession to ensure the right materials are created.”
Josette will be among the highlyesteemed speakers to present at BDIA Dental Showcase this year, where she will be sharing some of her extensive expertise to help dental professionals improve their understanding of the endodontic materials they use in practice every day. About her session and the event in general, Josette adds:
“I’ll be reviewing bioceramics from a clinical perspective, exploring the challenges and providing some guidance for clinicians to avoid common complications. We will cover material selection, as well as discussing their properties in detail, how to use them effectively and where to find out more. Products will be good for one patient but not another, so familiarity with the materials is key.
“I attended BDIA Showcase last year as a speaker. It was very well set out and extremely well organised with everything running smoothly. A lot of people attended and there was a very good company turn out to ensure a vibrant event.”
If you only attend one dental event this year, make it BDIA Dental Showcase. It is the longest running dental exhibition for a reason! Keep up-to-date with the monthly newsletter and register for your free pass today at dentalshowcase.com/.
BDIA Dental showcase 2024 22nd-23rd March
exCeL London dentalshowcase.com n
More than 80% of the population suffer from back pain occasionally, more than a third chronically. With its back-friendly properties, the Bambach® Saddle Seat has been inspiring users in doctors’ and dentists’ surgeries for more than 25 years.
A “normal” chair forces the spine into an unhealthy posture, which increases the pressure on the intervertebral discs enormously. This causes health issues and pain usually in back, neck, arm, hand or shoulder. The Bambach® Saddle Seat supports the pelvis, allowing the spine to assume its natural and healthy “S”-posture. As a result, the Bambach® Saddle Seat actively prevents an unhealthy (incorrect) sitting posture. Improved posture not only has a positive effect on
Unlike most wipes which are made from polypropylene, Bossklein V-WIPE ZERO Eco-XL wipes are constructed from 100% natural, biodegradable fibres. Wipes are made from renewable, plant-based viscose and sustainably sourced.
The fast-acting Bossklein V-WIPE ZERO formulation contains no alcohol and takes advantage of safer and greener chemical components to create a simpler and more effective product. Ideal to use on the majority of wipeable surfaces, including dental chairs. Wipes have a pleasant apple aroma.
Each flowpack with stay fresh lid removes the need for a dispenser tub further reducing the amount of plastic consumed. Packs contain 100 large wipes
With over 28,000 individual products in stock, Trycare not only supply all their Surgical and General Practice specialist products from Adin, Centrix, EVE, Tecnoss OsteoBiol, Tokuyama and many more market leading manufacturers, but everything else you need too! This includes everything available from Acteon to Zhermack, including glass ionomers like GC’s Fuji II. You can get it all from Trycare!

health, but has also been proven to increase productivity and the quality of work. It significantly reduces the pressure on the intervertebral discs and spine. The new BamBasic® has the original Bambach® seat surface but comes at a more affordable price. Please do not hesitate to contact us for more information.
Tel: 020 8532 5100 ask@fortunabambach.com n
measuring 240x200mm each. V-WIPE ZERO Eco-XL wipes are available now.
For more information call 0800 132 373 or visit www.bossklein.com n


For further information contact your local Trycare representative, call 01274 885544 or visit www.trycare.co.ukn
The Association of Dental Implantology (ADI) is the UK’s go-to organisation for anything and everything related to dental implants.
It has long extended a warm welcome to all members of the team, not just dentists, offering bespoke educational programmes for nurses, practice managers, hygienists and therapist alongside clinicians, at its Annual Congress.
This is because the ADI acknowledges a whole team approach is key to the patient’s experience and long-term success. A coordinated team means anyone considering implant therapy will be fully informed on every step of their
With over 28,000 individual products in stock, Trycare not only supply all their Surgical and General Practice specialist products from Adin, Centrix, EVE, Tecnoss OsteoBiol, Tokuyama and many more market leading manufacturers, but everything else you need too! This includes everything available from Acteon to Zhermack, including alginate impression materials like Kulzer’s Alginoplast. You can get it all from Trycare!
For further information contact your local Trycare representative, call 01274 885544 or visit www.trycare.co.ukn

CloserStill Media is delighted to announce that registration for the British Dental Conference & Dentistry Show (BDCDS) co-located with Dental Technology Showcase (DTS) is officially open.
These premier events are set to take place on the 17th/18th May at the NEC in Birmingham. Poised to be an extraordinary gathering for dental professionals, showcasing the latest innovations, research, and developments in dentistry, BDCDS and DTS promise to offer an unparalleled platform for learning, networking, and professional growth.
The extensive conference programme will be taking place across 14 theatres with over 150 hours of CPD to choose from. Speakers so far include Paul Tipton, Simon Chard, Finlay Sutton, Lisa Bainham,
and Maria Lessani.

The Enhanced CPD Theatre is back by popular demand and will cover all the relevant updates in dentistry standards alongside essential topics such as consent and dentolegal issues, medical emergencies, and dental radiography. Registration is free for dental and lab professionals and can be completed through the official websites. For more information and to register, please visit the website for BDCDS or the-dts.co.uk for DTS and save the dates in your diary!n
Dr Eoin O’Sullivan is a Specialist in Prosthodontics and a well-known teacher, lecturer and mentor in the UK and abroad. He will discuss digital tools available to enhance communication between dentist and dental technician from the Clinical Theatre on behalf of Align Technology at 14:00 on Friday 22nd March at BDIA Dental Showcase 2024. He says:
“We are in an era of exciting digital technology across dentistry, with new things constantly coming along. However, this can be overwhelming, which can be a barrier to adaptation. So too can the initial financial outlay for the relevant equipment.

“I will share what I use, what works for me and how it could impact other practices. Adopting technology can improve predictability, convenience and efficiency of the clinical workflow, significantly improving communication as well. The return on investment can also outweigh the initial cost much quicker than some believe. But you don’t have to radically change everything about your practice to start benefitting. I will ensure that my session is very relevant to the general dental practitioner who wants to get started in digital.” Register for BDIA Showcase 2024 today at https://dental-showcase-2024.reg. buzz/register-free-pr! n
journey, and understand the rationale for each stage of their treatment plan.

As part of its offering, the ADI has comprehensive patient leaflets, to deepen their understanding about dental implants, and what to expect. ADI members get a number of these free, with a discounted rate thereafter.
Just one of the many benefits of joining the ADI! n
With over 28,000 individual products in stock, Trycare not only supply all their Surgical and General Practice specialist products from Adin, Centrix, EVE, Tecnoss OsteoBiol, Tokuyama and many more market leading manufacturers, but everything else you need too! This includes everything available from Acteon to Zhermack, including local anaesthetic like Dentsply’s Xylocaine. You can get it all from Trycare!
For further information contact your local Trycare representative, call 01274 885544 or visit www.trycare.co.uk n

Effective dentistry doesn’t have to be complicated. The team at Carestream Dental understands that brilliant care often lies in its simplicity, which led to the development of the ground-breaking CS 7200 Neo Edition, addressing everyday needs with ease.
The flexible and cable-free imaging plates are simple to position and can be used for periapical, bitewing and paediatric exams. Plus, by including a USB and Ethernet connection, the CS 7200 Neo Edition is a versatile chairside or practicewide solution.
Make the CS 7200 Neo Edition a system that lasts in your practice, with the new extended warranty guarantee from Carestream Dental. Lean on our 125 years
of experience, and access spare parts when you need them, to keep your care reliable in the long-term.
To learn more about the simple solution to intraoral plating systems, consider the CS 7200 Neo Edition, and contact the Carestream Dental team today. n

Choosing high-quality dental tools for your practice can help you treat patients faster and more effectively.
The DIATECH Z-Rex range of dental burs from COLTENE is designed to make working with today’s highly popular, high-performance ceramics easier. The burs make adjusting, trepanning, or removing restorations such as zirconia straightforward.
The range features a unique synthetic diamond mixture which delivers durability and efficiency. Its hardness is 70% higher when compared to conventional bondings.
The instruments are available in two grits: medium to reduce the likelihood of microfractures, and coarse for increased crown cutting-efficiency. They are conveniently
Perio plus+ mouthwashes are so effective, they are only recommended for shortterm, guided use.
With Perio plus+ mouthwashes, chlorhexidine (CHX), well-known for reducing bacterial plaque, combines with CITROX® a mix of organic plant compounds, derived from bitter oranges. Choose which mouthwash to use with your patients, according to their oral health situations: Regenerate (for intensive care post-surgery); Balance (for people at increased risk of dental disease) and Forte (following invasive dental procedures). Perio plus+ products can also be recommended before the delivery of certain treatments, for an extra line of defence against infection.
To ensure exceptional clinical care for every single patient, specialist endodontics may be required. If this isn’t something you can offer in-house, consider referring to EndoCare.
We work with you to confirm the diagnosis and create a treatment plan. You will also be kept up to date at every stage of treatment.
The alcoholfree solutions also contain PVP-VA, which forms a protective film over the teeth, gums and mucous membranes. For powerful, optimised protection, recommend Perio plus+.

For more information, please call 01480 862084, email info@curaprox.co.uk or visit www.perioplus.com/uk n
Once the referred treatment is complete, your patient will return to your routine care, out of pain. We can provide any postoperative support or guidance you may need to facilitate optimal recovery and maintenance in the long-term. We offer a range of solutions, including post removal, endodontic microsurgery and retreatment in complex cases. Our team consists of experts and specialists in the field, who will do everything in their power to save a tooth wherever possible. Contact us today to find out more. For further information please call EndoCare on 020 7224 0999 Or visit www.endocare.co.uk n
A late-night Instagram scroll led Savannah, GA dentist Steven Berwitz to discover the advantages of Kiroku, the AI digital note taking platform. He’d been using a voice dictation service for his notes and was frustrated that it did not have a dental vocabulary.
“The pre-made templates were a big help in the initial stages of using the software. Being able to click through my notes is such a time saver and that is a big deal,” he says. “The AI picking up changes that I have made and suggestions helps too. Overall, anything that can keep my notes detailed and quickly entered is a plus.”
“If you are looking to have your notes concise, orderly and detailed and save
If you’re looking to grow your practice but not sure about making an acquisition, did you know a merger could prove a better option?
Mergers can be a less expensive way of expanding because the EBITDA (earnings before interest, tax, depreciation and amortisation) can be bought at a much lower price than if you were to buy a practice outright.
Leveraging the synergistic relationship between two practices can improve performance and help boost innovation, reduce costs and outperform competitors. Combining two practices under the same roof means they are easier to manage as a single business too.
individually packaged in blisters which facilitates ease of tracking too.

To find out how the DIATECH Z-Rex range can take your treatments to the next level, visit the website today!
For more on COLTENE, visit www. coltene.com, email info.uk@coltene.com or call 0800 254 5115. n

Dental Elite has more than a decade of experience in the buying and selling of dental practices and has created a range of free guides to help dental professionals through the process. A full step-by-step guide, Considering a Merger, is available via its website. To find out how Dental Elite can assist with your business decisions, contact the team today.
For more information contact the Dental Elite team on 01788 545900 https://dentalelite.co.uk/n
time in the process, then this is for you!”
Steven has already recommended Kiroku to a number of dentists. “When I have shown them what it does, they are really impressed. I fully believe in this platform and believe it can assist other providers as well.”

For more information about how Kiroku can help you in your practice, get in touch with the team today.
To find out more about Kiroku, or to start your free trial, please visit trykiroku.comn
Eschmann offers an array of industryleading solutions that are designed for unparalleled reliability, longevity and workflow efficiency.
Eschmann will deliver and install your new equipment seamlessly, and even provide an option for later taking away the old model so you don’t need to worry about disposing of it correctly!
Equipment options available to dental practices from Eschmann include the Little Sister range of autoclaves. The latest range features ‘B’ type vacuum and ‘N’ type non-vacuum models in a variety of capacities to suit your needs. The Enbio handpiece steriliser is also the fastest ‘B’ type autoclave on the market, offering
cycles from as little as 15 minutes.

Plus, all Eschmann autoclaves can be supported by the Care & Cover servicing package, which includes Annual Validation and Pressure Vessel Certification, annual service and software upgrades, unlimited breakdown cover, unlimited Eschmann parts and labour, Enhanced CPD user training and on-site support from 50+ Eschmann engineers nationwide.
For a new autoclave and the removal of your old unit contact Eschmann today. n
Immediate implants have never looked so good
Meet and exceed patient expectations by delivering swift and aesthetic implant treatments, with solutions from Neodent®, a Straumann Group Brand.
Difficult cases in the posterior region can be treated with confidence with the Neodent® Grand Morse® Helix® range; a specially crafted wide design with an optimised emergence profile can fulfil immediate implant needs and facilitate a natural looking result.
Alongside the implant, wide healing abutments are especially effective at maintaining the molar emergence profile, minimising infection and helping patients feel confident in their smile.
Neodent® offers several other exceptional options to create impressive
implant results: the NeoArch® implant systems provide immediate restoration for edentulous patients; the Neodent® Helix GM Narrow facilitates results in the smallest of interdental spaces; and the Neodent® Ceramic Implant System, Zi, creates a metal-free implant solution that is impressively effective and aesthetic. Join the clinicians providing their patients with high-quality and visually excellent implants. Contact the Neodent® team today to learn more.n

For a CBCT scanner that is as versatile as it is precise, consider implementing the CS 8100 3D Evo Edition, from Carestream Dental, in your practice.
2D panoramic capabilities and CBCT imaging with 3D model scanning combine to create a well-rounded solution for any clinical need. With applications in endodontics, orthodontics and implantology, treatment plans can be informed by ultra-high-resolution images. The brilliant ANR algorithm reduces image noise, and our Tomosharp algorithm makes panoramic images ultra-sharp.
Carestream Dental is proud to make the CS 8100 3D a mainstay in your workflows for many years ahead, with an outstanding extended warranty. Covering spare parts
Without the appropriate measures in place, gypsum waste from your practice can be seriously dangerous to the world around you. Trust Initial Medical and choose the Eco Gypsum Waste Containers, for effective waste management.
The containers provide for the careful storage of gypsum waste in your practice, allowing for safe disposal in accordance with Environmental Permitting Regulations 2016. Plus, the containers are manufactured from 100% recycled polymers, to further reduce your impact on the environment.
This green solution doesn’t end here. Initial Medical will help you to meet legal regulations by handling the segregation
ClearCorrect®, a brand from the Straumann Group, represents the finessing of decades of material science, research and innovation.
The result is a superior aligner, with proven results. Made with ClearQuartz™ tri-layer material, ClearCorrect® clear aligners are comfortable, engineered for precision, comfort and aesthetics. Thanks to the unique properties of ClearQuartz™, this solution is able to retain ten times more of its initial force, compared to competitors. The high and flat trimline facilitates optimal force transmission, for more accurate tooth movement and enhanced root control. ClearCorrect® aligners are also more stain
How much is your practice worth? Valuing your business is something you’ll want to do before selling it, merging with another or even for raising finance to make an acquisition of your own. Doing it accurately is a difficult and complex task.
In the Business Theatre at the BDIA Dental Showcase in March, Julie Randle, senior practice consultant at Dental Elite, will be exploring the ins and outs of dental practice valuations and sales. She will highlight key areas which principals need to address to ensure a correct valuation.
“Health checks are important because we are looking at key indicators within a valuation,” she says. “We can then give pointers on how to increase turnover or how to have guaranteed income streams but also
throughout the entire system, our expertise can be relied upon to truly maximise your investment.

To learn more about the CBCT system that makes patient assessments simple, contact the Carestream Dental team. For more information on Carestream Dental and our new extended warranties visit the website. For the latest news and updates, follow us on Facebook and Instagram @carestreamdental.uk n
of your waste, before it is disposed of at a specialist landfill site.

We pride ourselves on exceptional service whenever you need it. A personal Initial Medical consultant will be on-hand to manage your service agreement and answer any queries your practice has around waste disposal.
To learn more about implementing safe waste measures like the Eco Gypsum Waste Containers in your practice, contact the team today.
To find out more, get in touch at 0808 304 7411 or visit the website today n
Ensuring patients receive the best care for their condition is the highest priority for every dental professional. When an individual presents the need for specialist oral surgery, consider referring them to the Centre for Oral-Maxillofacial and Dental Implant Reconstruction.
Based in Manchester, the acclaimed International ZAGA Centre practices with a team of experienced professionals who will see a patient within two weeks of receiving a referral.
The practice is led by Specialist Oral Surgeon, Professor Cemal Ucer, whose extensive experience in dental implantology that dates back over two and a half decades has made him a celebrated figure in the field.
Clear aligner design is key for improving patient compliance. This is why ClearCorrect® aligners are designed to apply consistent force, and optimise patient comfort.
The tri-layer design of ClearQuartz™ material ensures that patients have a more comfortable experience as the flexible inner layer applies a third less initial force on the teeth. This provides greater orthodontic control as it combines two layers of resilient polymer and an elastomeric inner layer. Additionally, digital manufacturing software from ClearCorrect® enhances the trimline design of each aligner to help ensure a

When the need for complex treatment requires specialist attention, dental professionals can rely on the team that provides patients with effective, affordable care and only restores dentitions with tried and trusted techniques and materials.
To learn more about the referral service that could transform your patients’ lives, contact the team today.
Please contact Professor Ucer at ucer@ icedental.institute or Mel Hay at: mel@mdic.co - 01612 371842 n

more custom, comfortable fit. This trimline design makes ClearCorrect® aligners 2.5 times more retentive than scalloped aligners, reducing the need for engagers.
For more information, please visit the ClearCorrect® website.
For more information on ClearCorrect®, visit: www.clearcorrect-uk.comn
resistant than the leading aligner brand.i

With ClearCorrect®, you can achieve more predictable outcomes and enhance comfort for patients – to find out more, visit the website today.
For more information, visit www.clearcorrect-uk.com n
look at their core costs and how that spend is reflected in their accounts.
“A lot of accountants are not dental specialists –they don’t always know what can be added back into a valuation, such as depreciation, staff welfare and training costs.”

Sessions will be invaluable to dental practice owners attending BDIA Dental Showcase, regardless of whether a sale is imminent or still years away. The advice you take away could shape the future of your business. discover the full conference programme on the website. register for for free today at https://dentalshowcase-2024.reg.buzz/register-free-pr!
Interdental tools are able to effectively reduce plaque between the teeth, making them a great choice for patients’ daily oral hygiene routines.
The FLEXI range of interdental brushes from TANDEX is ideal for your patients. Available in 11 different sizes, you can help patients find the perfect interdental brushes for them. FLEXI brushes are ideal for reducing plaque between the teeth, and should be used daily for the best results. Each size is easily identifiable by the ISO and PHD (passage hole diameter) numbers on their box, as well as their unique colours.
For patients who need an extra boost, recommend PREVENT GEL from TANDEX. It contains 0.12% chlorhexidine and 900
ppm fluoride to strengthen the enamel and provide an antibacterial effect.
For more information about oral hygiene solutions from TANDEX, please get in touch with the team.
For more information on Tandex’s range of products, visit www.tandex.dk/ or visit Facebook:www.facebook.com/TandexUK
Our products are also available from CTS Dental Supplies: www.cts-dental.com/ and DHB Oral Healthcare https://dhb.co.uk/n

The Virtual Vivo™ intraoral scanner –available from the Straumann Group –offers an entry-level solution for clinicians who are looking to get started on their digital dental journey.
It is simple to use with guided workflows at each step allowing those new to the field to benefit from integrated connectivity.
The high-resolution colour scanning improves patient communication, while precise real-time data can be validated immediately to ensure that an accurate 3D model is created.
The scanner is also fast, offering the power of two miniaturised 3D scanners in one small hand-held device for greater practitioner and patient comfort.

To open up a new universe of possibilities in your practice, introduce the Virtual Vivo™ intraoral scanner from the Straumann Group today.
For more details, please visit the website.n
Planmeca Viso G3 brings industry-leading usability and visibility for various clinical needs, including endodontic treatments and implant planning. With a field of view (FOV) ranging from 3 x 3 to 20 x 10 cm, the unit not only offers high-quality 3D images of the entire dentition, but is able to capture detailed panoramic as well as extraoral bitewing images for interproximal diagnostics. The unit can also be equipped with the Planmeca ProCeph one-shot cephalostat and, when the time is right, upgraded to Planmeca Viso G5 for a larger maximum 3D volume.
You can expect a cutting-edge CBCT
imaging experience with the Planmeca Viso G3. And what’s more, you can see it for yourself on the Planmeca stand at Dental Showcase in March.

Available to order now, contact Planmeca for more information. n
New year’s resolution to enhance your implantology skills to take them to the next level? Or fed up of having to refer more complex cases to other centres?
An Advanced Certificate in Full Mouth Oral Implant Rehabilitation offered by ICE Postgraduate Dental Institute and Hospital/ University of Salford is designed for the experienced implant dentist who wishes to expand the scope of their practice to include the reconstruction of fully edentulous single or dual arches using both the analogue and fully digital workflows including stackable fully guided systems from Megagen and Southern Implant systems
University of Salford’s implant training hub, the ICE Postgraduate Dental Institute
When cleaning interdentally, brushes are often easier to master than string floss and more effective at optimising plaque removal, too.
The right-size brush is crucial to success which is why the CPS Prime interdental brushes, by leading Swiss oral hygiene brand Curaprox, are available in a range of sizes, colour-coded for your and your patient’s convenience.
That is not the only reason to use and recommend the CPS Prime. The bristles are long and super-fine, opening like an umbrella to remove debris and bacteria in one efficient in-and-out movement. They’re durable too, so good value. When it’s time to replace the brush head, you only need to remove this part of
Dr Len D‘Cruz is the Head of BDA Indemnity, as well as an experienced clinician who runs a 7-surgery practice in London. He will be among the speakers in the Business Theatre, sharing his expertise regarding principals’ legal responsibilities to their patients. Len shares what delegates can expect:
“Holding an NHS contract creates a vicarious liability for practice owners regarding the actions of self-employed dentists. All practices and/or limited companies that run practices have a duty of care to their patients, regardless of whether or not the principal has treated them. A recent GDC case about topping up fees has made the mixing of NHS and private treatment in England and Wales different, and dentists need to know how
According to mental health charity Mind, 60% of employees say they’d feel more motivated and more likely to recommend their organisation as a good place to work if their employer took action to support mental wellbeing. And in a challenging time for recruitment in the dental sector, ‘word of mouth’ referrals are a helpful adjunct to the hiring process. Ways to promote wellbeing in the workplace include encouraging the practice team to take full lunch breaks and take their full annual leave entitlement. Flexible working can help too. For example, a later start time twice a week to enable a team member to accommodate exercise.i

and Hospital in Salford Quays, Manchester, boasts state-of-the-art teaching and clinical facilities. The course is led by the celebrated dental clinician and Specialist oral Surgeon Professor Cemal Ucer and Professor Simon Wright MBE.
Visit the website today to discover what new skills you could master in restorative dentistry!
Please contact Professor Ucer at: ucer@icedental.institute or Mel Hay at mel@mdic.co 01612 371842 n

the tool, clicking the new one into place on the reusable handle. Less waste, less cost – just a brilliant everyday clean. Motivate your patients to clean between, with CPS Prime range. For more information, please visit: www.curaprox.co.uk n
Dr Kaye McCaig has recently completed the IAS & ClearCorrect Level 1 Online course from the IAS Academy. She describes her experience:
“I chose to sign up to the course as the practice I work in already provides ClearCorrect aligners, so I wanted to begin training to be able to provide these for my patients. I liked the fact that there was an online element, which can be referred back to again in the future, and gave me the ability to take part in the practical exercises without needing to travel to attend an in-person course.
“All of the information was relevant and well presented. I found it easy to understand. I would definitely recommend
to others who are interested in starting their clear aligner training, and would choose the IAS Academy for future courses.”
Please contact the IAS Academy team for more information about the course. For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1) n
this relates to the way treatment options are communicated to patients.

“There are many changes impacting the profession right now and BDIA Dental Showcase is the best place to find out about these from a range of people who are experts in their fields. I hope delegates will gain further insight into the challenges practice owners face when running their practices and what they can do to mitigate the risks. They’ll also better understand the impact legal cases have had on the landscape of dentistry.”
BDIA Dental Showcase, 22/23rd March, ExCeL Londonn

Dental Elite is a well-established dental recruitment agency specialising in sourcing and hiring for jobs in the dental sector. To find out how Dental Elite can assist with your recruitment needs – or if you’re looking for a new professional challenge – contact them today. For more information contact the Dental Elite team on 01788 545900 n
Looking for software that combines powerful imaging, practice management, clinical workflows and intuitive design in one platform? Built on feedback from real practices, Sensei Cloud is an innovative, cloud-based dental software solution from Sensei, the practice and patient management solution brand from Carestream Dental.
The platform acts as a digital mentor with a focus on analytics so dental professionals can make smarter decisions regarding patient care and practice management. In addition to clinical data, business performance metrics and analytics are a prime feature, too. Realtime dashboards provide live financial data, enabling practice owners to track
“It’s a game changer!” says Zohaib Hassan of his experience with Kiroku, the AI digital note taking platform.
Based in Brigstock Dental Practice in Thornton Heath, Surrey, general dental practitioner Zohaib has been using Kiroku for over five months now and has become a huge fan. “I like the fact there is a template for absolutely everything, alongside the ability to adjust templates to your own style and personalise them,” he enthuses.
“Having that constant worry of ‘do my notes cover me?’ is horrible,” Zohaib admits. “But Kiroku helps reduce this stress.
“With Kiroku you are able to use the information in the template or remove it if

and act on key insights. Sensei Cloud aims to simplify the entire workflow and is suitable for all practices, no matter the specialty. Practices offering dental, periodontal and orthodontic treatments can seamlessly integrate the software across departments.
To learn more about Sensei Cloud visit the website today!
For more information on Sensei Cloud visit gosensei.co.uk
For the latest news and updates, follow us on Facebook n

it is not appropriate. And because you’re filling out a template you are less likely to miss out vital bits of information. The other key benefit is that the software prompts the user to ask patients for details we may forget during examinations.”
For more information about how Kiroku can help you in your practice, get in touch with the team today.
To find out more about Kiroku, or to start your free trial, please visit trykiroku.comn
Buying a dental practice is a big decision. It’s not without its risks and therefore requires careful consideration and planning.
There are some key stages a would-be buyer needs to move through in order to make a legal acquisition. For example, the timing and execution of the Care Quality Commission (CQC) application is crucial to ensure that the practice is able to begin operation after ownership is transferred.
Dental Elite has more than a decade of experience in the buying and selling of dental practices and has created a range of free guides to help dental professionals through the process. A full step-by-step guide, The Selling Process, is available via its website.
Dental professionals in the UK and Ireland who choose COLTENE brands can now benefit from a new loyalty programme, COLTENE Rewards.
To begin with, for each pound/euro spent on COLTENE products, customers earn one COLTENE coin which can be redeemed against a fantastic range of goods (including Fitbit watches and Apple iPads) as well as COLTENE products. By joining the programme, customers automatically receive a bonus bundle of coins but the more dental customers spend, the greater the rewards. Coin bundles increase in size each time a customer reaches a new tier of spending. Customers can also earn
To find out how Dental Elite can assist with your business decisions, contact the team today.
For more information contact the Dental Elite team on 01788 545900n


coins by sharing information about their practice. This enables COLTENE to personalise offers and tailor its communications. To find out more about the programme, visit the website today!
For more information, info.uk@coltene.com and 0800 254 5115
COLTENE loyalty scheme https:// rewards.coltene.com n
To help patients maintain good oral hygiene practises between routine appointments, consider recommending easy-to-use tools, like a Waterpik® Water Flosser.
This innovative solution is clinicallyproven to be twice as effective as string floss for reducing gingival bleeding. It is also an effective alternative to subgingival antibiotics for periodontal maintenance. It need only be used for one minute each day in order to deliver benefits to your patients, making it simple to integrate with an existing oral hygiene routine.
To find out more, why not book a Lunch & Learn session at your practice with one of our passionate Professional Educators? For more information on Waterpik®
Water Flosser products visit: www.waterpik.co.uk.
Waterpik® products are available from Amazon, Costco UK, Argos, Boots, Superdrug and Tesco online and in stores across the UK and Ireland. Join the 3,000+ dental teams who have already benefitted from a professional Waterpik® Lunch & Learn. Book your free session for 1 hour of verifiable CPD and a free Waterpik® Water Flosser – available either face to face or as a webinar – at www.waterpik.co.uk/professional/ lunch-learn/ n
As the face of dentistry continues to change, digital workflows are proving more and more effective. This is why Clark Dental is proud to offer dental practices the ideal option for a complete digital workflow.
The Cerec Primescan intraoral scanner offers clinicians easy handling, as well as an intuitive touchscreen for ease of use. The highly accurate scanner is able to process over one million 3D points per second, meaning that your dental images will always be reliable. Data can be shared to the Primeprint 3D printer, which is ideal for producing surgical guides, full-scale models, nightguards and more – in your own practice.
The Axiom X3® implant system from Anthogyr, a Straumann Group brand, is designed to save you and your patients time in the dental chair.
It is suitable for minimally invasive treatment types, and allows for short treatment times thanks to its optimal primary stability. The Axiom X3® will allow you to meet the needs of every patient, allowing you to offer excellent treatment options, regardless of their clinical situation or bone type.
Consider using the Axiom X3® implant system – the versatile treatment solution, suitable in even challenging situations.
For more information about the AxiomX3

It has been estimated that 41% of working-age adults in the England don’t fully understand or make use of everyday health information. Health literacy is directly linked to health outcomes and service use, so it’s crucial that public education be enhanced.
Chairsyde is a state-of-the-art consultation platform that is designed to help dentists do just this among their patients.
It offers a library of animations that clearly and easily communicate a broad range of dental conditions and diseases – including dental caries – as well as the treatments associated with them. The videos cover the risks of disease progression, in addition to the benefits,
In order to create an accurate impression, a clear working view of the tooth is crucial.
Astringent Retraction Paste from 3M Oral Care is a fast, convenient and effective solution for gingival retraction, offering an advantage over gingival retraction cords that can be difficult and time-consuming to place.
Boasting an extra-fine tip, the Astringent Retraction Paste from 3M Oral Care delivers a 15% aluminium chloride astringent paste right into the sulcus, gently pushing the gingival tissue away from the tooth so dental professionals can efficiently capture a detailed impression of the preparation margin. It can be used for taking material-based or digital impressions for Class II and V fillings.

Additionally, the Primemill milling machine is capable of producing stunning restorations, with a wide range of options available. This even includes a Super Fast mode, which delivers high-quality zirconia crowns in as little as 5 minutes.
For more information, please contact the team at Clark Dental.
For more information call Clark Dental on 01268 733 146, email info@clarkdental. co.uk or visit www.clarkdental.co.uk n
Have you considered the potential rewards of investing in shares, but are unsure where to start? In a free consultation with money4dentists, you can discuss the options available to you, with advice from experienced specialist independent financial advisers.
Whether dealing with a stockbroker, an online trading service or the stock broking department of your bank, each method slightly unique – which can be extremely confusing.
By working with independent financial advisers, you can better understand the possibilities that await you in the stock market, as well as deciding upon the amount you are willing to invest, and at what level of risk.
limitations and potential risks of all recommended therapies, encouraging patient understanding for long-term health benefits and improving the quality of their consent.
To find out more, contact the team at Chairsyde today!
For more information, or to book a demo, please visit www.chairsyde.com or call 020 3951 8360 n


One cord can be replaced by Astringent Retraction Paste from 3M Oral Care, enabling temporary retraction of the marginal gingiva and providing a dry sulcus on a healthy periodontium. It also offers long-lasting haemostasis.
To find out more about this awardwinning* retraction paste, please contact the team at 3M Oral Care.
For more information, call 08705 360 036 or visit www.go.3M.com/ocsdpr n

money4dentists have worked exclusively with dental professionals for over 16 years, with unmatched insight and understanding of the unique financial landscapes that surround those in the profession. This way, investors can find the best advice for their individual situation. For more information, please call 0845 345 5060 or 0754DENTIST. Email info@money4dentists.com or visit www.money4dentists.com n
For those looking to sell a share of their dental practice, bringing in a business partner, or where a group of people are purchasing a whole practice, consideration should be given to the partnership routes carefully. What is often overlooked is that each partnership type will impact on the partners income and, because of this, the valuation of the practice. In addition, whilst the partnership type can be suitable at the time of formation, there needs to be the ability to adapt for the duration.
So, what are the typical partnerships?
As the name suggests, each of the expense-sharing co-principals take on the responsibility of the overheads (typically 50:50), regardless of the gross fees generated. This could mean one principal generates £400,000 of income with another generating £250,000 of income. If the total expenses of the practice were £300,000 this would leave one principal with £250,000 profit (£400k - £300k/2) and the other with £100,000 profit (£250k - £300k/2).
Whilst this can seem a fair calculation, as it takes into account that each principal has the same facilities, it often does not give much flexibility for changes. It

should also be noted that, during the term of the partnership, should any income/patient base be transferred to someone else, then a valuation and payment to the partner should be made to keep the balance of what is owned, as it were purchased, or gross fees split in this way from the start.
This type of partnership is very rare due its nature, other than for married couples. Each principal will potentially generate different fees and work different days, but the profit is shared equally between the number of partners. Whilst a group of friends may purchase a whole practice together, potentially buying equal shares, this is often a recipe for disaster, as someone may wish to
reduce their working commitment in the future, which would directly impact the other partners, who could feel an unfair balance of work to profit.
‘associate-led model’
This is certainly becoming a more popular model, in which the partner receives an associate payment for the gross fees that they generate, followed by a split of the remainder of profit (or loss) in accordance with their ownership. This is often considered a partnership with more flexibility, as if a principal wishes to reduce from five days to three, then their ‘associate’ income will drop. However, if an associate takes up the other days/income, then this would not impact the other partners. The (surplus) profit should also remain the same.
For many people, retirement is an exciting prospect which brings greater freedoms in later life. Whilst stepping away from the dental practice can be both formidable and thrilling, there are multiple ways to prepare for such an enormous change.
The biggest concern will likely surround your income. Pensions can often be confusing: one metaphorical ‘pot’ where your lifetime contributions sit in the ether, promising to sustain you in the years to come. This can be daunting. How will it stretch? What is the best way to budget it? What will my day-to-day spending look like decades down the line?
A solution to alleviate worries and provide an element of certainty could be a pension annuity, sometimes called an income for life.
simplicity in stability It’s important to understand what an annuity is, and the difference it can make to your retirement income. The money that has been stored away in your pension pot over your career, earned through dentistry or otherwise, can be accumulated, and a portion may be designated to purchasing an annuity.
This will provide you with a stable annual income for life, with a myriad of stipulations dependent on the type of deal you acquire, and from whom you purchase it. In its most basic form, you would receive a steady income stream following retirement. The rate may take into consideration your age, your health, and budget to spend on the annuity.
The younger you are, the lower your income rate from the annuity will likely be. This is because the value will account for your life expectancy, and its difference to the purchasing age. For example, a 60-year-old would have a markedly lower annual rate than a 75-year-old with a similarly clean history of health issues. The younger individual has a longer period wherein they are expected to use the income, and so the annuity value will be stretched thinner over the ensuing years.
Finding the right annuity for you will offer a number of benefits. It’s worth considering that this may not be the same as a colleague’s, and choosing between agreements should not be done on a whim.
The most basic option is perhaps a level annuity. As the name suggests, payments remain stable over time. A dental professional would be able to retire, exchanging their pension pot for an income that is simple to plan for month to month. These may pay greater instalments at first compared to some variable deals – an appealing short-term benefit – but beware of the threat of inflation. In the years to come, it may leave you with less spending power, and the smallest rise in the inflation rate could prove troublesome. Conversely, an escalating annuity could be designed to raise at a fixed rate or in line with the Retail Prices Index (RPI) in an attempt to keep your income relatively stable over time. This will, of course, aid in part against any
impact of inflation, but will likely mean that initial payments are lower, since the funds will have to stretch into the future.
It’s worth talking through your medical history with a potential annuity provider to see how an offer may change. An impaired or enhanced annuity could increase the value of the payments you receive if a short life expectancy is presumed. Dental professionals may be eligible if they live with a medical condition such as diabetes, heart disease or high blood pressure, or if they are obese or a regular smoker. Providing accurate information could not only aid your application in its value, but will ensure your provider cannot withdraw it at a later date.
Don’t make the decision alone
Choosing the right annuity agreement for your lifestyle and spending demands is essential. You may want to assess your options to see how they work alongside your NHS pension, if you haven’t solely committed to private care. It may also be worth finding an annuity that continues paying your pension to a spouse after you pass – called a joint life annuity – for further stability.
It looks to be prime time to purchase an annuity too, with rates soaring by around 54% in just the last two years. Seeking advice from the experts at money4dentists could help you find the best possible plan, and make the most of your investment. The team at money4dentists are committed to helping dental professionals find the solutions that suit them best, and will traverse
As the profit split would be different for each of the partnership models, the valuation of each would be different. As such, when selling or buying into a partnership, it is important to get expert advice to not only assess the profit models but value of the practice under the partnership type that you are entering into. Sometimes, where there is an existing partnership with one person retiring with, say, an associate buying in, if the associate is buying a different level of gross fees to what the retiring principal is selling then this affects the remaining partner’s share and may mean a payment to them is also required. Where there is a collective of people all purchasing a (whole) practice, they again would need to consider the type of partnership that they are wanting to enter into. This would impact the amount that each pay (which can be different), as well as borrowing and future income. PFM Dental has been helping partnership buy-ins and sales for over 30 years, as part of its valuations and sales service. n
about the author
Martyn bradshaw is a Director of PfM Dental and heads up the dental practice sales agency.


the complex terrain of today’s pension annuity offers for your ideal agreement. With decades of exclusive advice for those in dentistry, money4dentists understands the unique intricacies of the profession, and how it affects your pension choices.
Annuities are back in vogue, and it’s never been more important to purchase the right option when retirement looms closer. Consulting sound financial advice and understanding what you may want from your post-retirement income is the recipe for success and stability, long into your twilight years.
For more information, please call 0845 345 5060 or 0754DENTIST, email info@money4dentists.com or visit www.money4dentists.com n
about the author Richard
T Lishman, Managing Director of
the 4dentists Group of companies.

Very few businesses are immune to the effects of a competitors in their marketplace. Although the real entrepreneurs are the ones always seeking to invent something unique that will change our lives
– Walt Disney, Bill Gates and Sir James Dyson spring to mind – for the rest of us, competition and their activities are something we must all stay aware of.

Therefore, we should not dismiss any potential competitive advantage as insignificant. I read a post last week that asserted “being likeable doesn’t close deals.” Which is sort of true.
In an absolute sense, likeability, by itself, won’t win new clients or patients for you. I mean, it’s possible that it could, but it’s not very probable.
On the other hand, it is also quite wrong to say that ‘likeability’ won’t win you new clients. Because, when everything else is equal in the mind of the prospective client/patient, being likeable might just be the difference between winning and losing.
So, how often is everything else equal? A lot. All the time.
Consider these stats for Warwickshire from the ‘Office for National Statistics’. It shows the number of companies in each of these categories:
• Motor Trades: 860 companies
• Accommodation & Food Services: 1,350 companies
• Property: 965 companies
• Healthcare: 865 companies
• Finance and Insurance: 425 companies If there are more than 100 companies offering virtually the same product and services with similar capabilities at roughly the same price, there is little chance that prospective customers will be able to differentiate between them.
The point is that, in highly competitive situations, you can’t
dismiss any potential advantage as being insignificant or unimportant. Like being likeable.
At the end of the day, being likeable might give you the fraction of a percentage boost that wins that client for you.
Sir Dave Brailsford, of the INEOS professional cycling team in the Tour de France, is famous for his gospel of “marginal gains”.
He examines every possible aspect of his riders’ equipment and performance, no matter how small and seemingly insignificant. If it can be improved to help his team’s performance, and its probability of winning a race by even a fraction of a percentage point, then he works to make it better.
In winning patients, these “marginal gains” that spell the difference between winning and losing are almost all about you. It’s when who you are is more important than what you know.
Consider this: Cian McLoughlin and his team at Trinity Perspectives in Australia have conducted thousands of interviews with people. He summarised their findings from these interviews into the ‘9 Reasons You Win Clients and the 9 Reasons You Don’t Win Clients’.
Only one of the 18 combined reasons had to do with price, and that was
where the price was too cheap and was therefore seen as a risk.
The primary reasons cited by people for why they were attracted (or not) to a business was because of human issues.
And what was one of the nine most frequently cited reasons people gave for not engaging with a business? They did not ‘feel an emotional connection’ with the people they were dealing with. You know? Like being likeable.
To win clients you still have to offer a competitive product at a competitive price but, when all else is equal, the slim margin of victory (or defeat) will often come from those things that too many ‘experts’ dismiss as insignificant. Like being likeable. So, be prepared to watch, listen, and talk in that order.
Your ability to win clients is a direct reflection of your prospect’s opinion of the value of their experience with you. n
about the author chris Mayor, commercial Director, Lily Head Dental Practice sales

















Marketing is a long-term process that can really help to grow your practice and boost its value
In the run up to selling your dental practice, getting your business plan in order is crucial. Having clear, concrete goals will help potential buyers understand what you’re trying to achieve and that you’re serious about selling the business. How you market your practice and how well you do it is a key component.
Marketing can help increase the value of a practice too. It can create practice recognition and increase patient awareness about the services it offers. By effectively communicating the value and benefits of their practice, principals can differentiate themselves and attract more patients, ultimately increasing the value of the business. And a larger patient base often translates into increased revenue and improved business value.
be strategic
With limited resources, dental practices need to be strategic in their advertising and promotional efforts to maximise their return on investment (ROI). When investing in marketing activities, it is essential to know which initiatives are generating the most revenue and which are not yielding the desired results. By setting specific goals and targets, principals can allocate their budget in a way that prioritises those initiatives that deliver the highest returns. This data-driven approach can help you make informed decisions, allowing you to optimise your marketing efforts and maximise your ROI.
Your budget needs to show what your marketing goals are (e.g. increase your number of patients, increase number of whitening treatments) and how much you
intend to spend to achieve them. Then break it down into the different activities such as paid advertising, social media advertising, websites, email marketing, leaflets and flyers.
So, how much should your budget be? It depends on the size and goals of your practice, how established it is and how much money you have available to support your efforts. According to research by Alba SEO Services, 38% of small businesses asked spent less than £1k on marketing each year. As a general rule, new businesses allocated between 12-20% of their gross revenue on marketing, while established ones spend between 6-12%. be informed
Once you’ve allocated a spend, it’s important to track it. There are various tracking metrics but one that is pertinent to a dental practice budget is Cost per Lead (CPL). CPL calculates how much you have spent on generating leads for every patient/ treatment request that you acquire. This can help you understand how much you are spending in order to attract that one new patient/treatment request. The more information you gather, the better decisions you can make about repeating or amending your activity. For example, if you spent £350 on a Facebook Ad campaign that generated only a handful of enquiries but you know that regular emails result in a 200% ROI, it’s much easier to see where you should focus your future marketing efforts.
But how do you calculate the ROI of a marketing campaign? Simply put, you take the sales growth of the practice, subtract the marketing costs and then divide by
the marketing cost. So, if revenues grew by £1k and the campaign cost £100 then the ROI is 900%. Of course, this type of calculation does assume that the total month over month sales growth is down to the marketing campaign which might not be accurate. For a better, more meaningful ROI, comparisons are needed, so revenues in the months prior to the campaign, for example, would help show the impact more clearly.
Managing a marketing budget promotes efficiency and effectiveness. With limited resources, dental practices cannot afford to waste their marketing spend on ineffective strategies. By setting a budget, principals can prioritise the most effective marketing channels and tactics, ensuring that they are reaching their target audience and driving results. It also fosters accountability and responsibility. By assigning specific funds to different marketing activities, practices can hold themselves accountable for the results. This encourages a more disciplined and structured approach to marketing, ensuring that every pound is spent wisely and with a clear purpose. It also helps in evaluating the success or failure of various marketing initiatives, allowing dentists to learn from their mistakes and make improvements moving forward. Additionally, managing a marketing budget promotes long-term growth and sustainability. By carefully planning and controlling marketing expenses, dental practices can ensure that they have a consistent and sustainable marketing presence. This helps in building practice awareness, attracting new patients, and
How often do patients leave your surgery enthusiastic about improving their oral hygiene, only to return a few months later having made little positive progress? It is an unfortunate yet common occurrence, but this doesn’t have to be the case.
in one ear, out the other?
There are several reasons why a patient may not remain motivated once they leave the dental practice. The first is that they didn’t understand what was being asked of them. This highlights the importance of effective communication with patients, ensuring that they fully comprehend their situation and any recommendations being made for them.
Another issue might be that they don’t have the time, resources or finances to implement the plan that was discussed. This is why lifestyle factors should be considered when reviewing at-home oral hygiene routines, enabling dental professionals to tailor advice according to individual needs and demands.
The other barriers can be a little more difficult to manage, because patients
might not feel comfortable sharing their financial circumstances. They may be embarrassed to admit they don’t have interdental brushes or the means to buy a new mouthwash or any other oral health adjunct that has been advised. It’s essential to approach the topic sensitively, or perhaps provide a few options with different price points so patients can select the most viable solution for them.
It is also important to be aware that patients may simply forget details given to them during a dental appointment. In fact, whether a patient understands the information they receive in the dental practice or not, they are unlikely to remember everything discussed after the occasion.
Research has suggested that patients recall only half the amount of dental health advice delivered by professionals during an appointment. As this could affect their motivation in the long-term, it is important to remind patients of discussions and recommendations after their visit.
Providing written information that patients can read at home may be
fostering patient loyalty. It also allows them to build a solid foundation for future growth and expansion.
Managing a marketing budget is of utmost importance for dental practices. It allows them to control their costs, track their ROI, promote efficiency, foster accountability, adapt to changing market conditions, and promote long-term growth and sustainability. By allocating their resources wisely and prioritising their marketing initiatives, dental practices can maximise their marketing efforts, achieve their desired business outcomes and bolster their intrinsic value.
To find out how Dental Elite can assist you in managing budgets to optimise your success in a future sale, contact the team today on 01788 545900 or visit https://dentalelite.co.uk/ n


about the author Luke Moore is one of the founders and Directors of Dental elite and has overseen well in excess of 750 practice sales and valuations. With over 19 years working in the dental industry, Luke has extensive knowledge in both dental practice transfers and recruitment and understands the complexities of nHs and Private practices.
business bites addressing everything business
useful, though there is a risk that leaflets get left in the car or accidently thrown away once they get home. Chairsyde offers an alternative solution. The state-of-the-art patient consultation platform provides an array of animations to use in the practice that explain oral health conditions as well as related treatments, including associated benefits, limitations and risks. These animations are automatically saved to patient notes and can then be emailed directly to patients for them to review at their leisure. Not only is this a fantastic recap of appointment discussions, but it also supports patients in improving oral hygiene techniques at home.
a collaborative effort
Enhancing patients’ oral health requires a collaborative effort between professionals and the patient themselves. Good communication is essential, but finding ways to motivate patients once they leave the practice and between appointments is important too. With the right tools, this is made possible. n

Loven Ganeswaran, ceO and founder
Helping dentists around the world empower their patients to make better decisions about their health.

We’re a specialist dental practice sales agency, so whether you are looking to sell your dental practice on the open market, selling to your associate or intrigued with Corporate interest, we’ve helped thousands of dentists like you.
You cannot be in better hands with our expert valuers, a single point of contact throughout the sale and in-house legal team, allowing us to
advise you from start to finish.

We work with dentists all over the UK
Our scale and reach means we’re here to help wherever you’re based
Practice sales over the past 12 months 50+
Current dental accountancy clients 1200+
Practice finance raised in the last year £15m+




Accurate valuations for associate & principal led models with advice on enhancing the practice value.

We liaise with solicitors, buyers, and CQC to ensure everything is in place to minimise stress and give a smooth sale.

Get access to 1000s of pre vetted purchasers, being individuals, small groups and all of the major corporates.

We have specialist dental solicitors with expertise in commercial law, property law, and CQC processes.

We will ensure your practice attracts the best possible price by negotiating the sale on your behalf.





