Re-Evaluate Rinse
Time For An Evidence-Based Recommendation
Clinically-Proven Essential Oils Help Eliminate Bacteria1































Systematic reviews, meta-analyses, the European Federation of Periodontology S3 level clinical practice guidelines, and a recent consensus report from global experts, convened by Spanish Society of Periodontology and Osseointegration (SEPA)*, support the adjunctive use of antiseptic mouth rinses.1-3






























As the pressure of practice grows, your wellbeing matters too. With confidential counselling and wellbeing support available at no extra cost, Dental Protection is by your side every step of the way. It’s time to put yourself first, with the support you deserve.












GDC Scope of Practice guidance set to empower dental hygienists and
therapists
The British Society of Dental Hygiene & Therapy (BSDHT) has welcomed the General Dental Council’s (GDC) revised Scope of Practice guidance, published earlier this week. The society was actively involved throughout its development, from the initial scoping to the consultation stages.
The updated framework, which comes into effect on 1 November 2025, provides much-needed clarity across all dental professional roles and places renewed emphasis on competence, training and indemnity as the foundations of safe practice.
For dental hygienists and dental therapists, the revised guidance represents an important step forward. By moving away from fixed task lists towards competency-based role descriptions, it enables all dental professionals to work confidently and exercise professional judgement, while ensuring patients receive safe and effective care.
Key updates for dental hygienists and dental therapists include:
• Clearer role boundaries: more precise definitions reduce uncertainty and support confident clinical decision-making
• Professional judgement: recognition that dental hygienists and dental therapists can carry out a wide range of treatments, provided they are trained, competent and indemnified (or insured), even where tasks are not itemised
• Direct access reaffirmed: patients can continue to see dental hygienists and dental therapists directly within their scope of practice, helping widen access to care
• Medicines: the ability to supply and administer certain prescription-only medicines under exemptions remains supported, with suitable training
• Education and CPD: training programmes and CPD will need to reflect the clarified competencies, ensuring dental hygienists and dental therapists are fully prepared for present-day practice
• Practice implications: employers and teams should review role boundaries, delegation, supervision, indemnity and referral policies in line with the new guidance.
Rhiannon Jones, President of the BSDHT, commented: ‘The GDC’s revised Scope of Practice guidance is a significant step forward. The clarity it brings is long overdue and will help dental hygienists and dental therapists practise with confidence, ensuring they can safely use their full skill set for the benefit of patients. Just as importantly, it highlights the role of skill mix in modern dentistry, showing how the whole dental team can contribute more effectively to widening access and improving outcomes. Professional title is only the starting point: competence, proper training and suitable indemnity remain essential.’
To support members in preparing for implementation of the new Scope of Practice guidance, the GDC will host an online Q&A webinar on the 16th October 6-7:30pm. The session will explore how the changes may impact everyday practice, provide examples of best practice, and answer member questions ahead of the November start date.
Registration is open: attendees can register at: https://lnkd.in/ebMksWFF, and the new guidance can be downloaded at tinyurl.com/SofP2025. n
Over two million toothbrush packs delivered to schools in the UK government/Colgate-Palmolive partnership

More than two million toothbrushes and toothpastes have been delivered to 3-5 year olds in early years settings in the most deprived areas of England, as well as military families overseas, this September. The delivery marks the beginning of a five-year collaboration between the Government and Colgate-Palmolive to help children develop positive toothbrushing habits and set them on a path to better oral health, as part of the government’s Plan for Change.
The new scheme is expected to help up to 600,000 3-5 year olds in early years settings to develop good toothbrushing habits this school year.
Children of overseas British military families serving in bases ranging from the Netherlands, Cyprus, Germany and the Falklands who historically have been underserved will also receive toothbrushing packs as part of the government mission to address inequalities.
Health Minister Stephen Kinnock visited Tinsley Meadows Primary Academy school in Sheffield to see how the rollout was progressing in the city, where nearly 9,500 children will receive packs this year.
Removal of decayed teeth remains the most common reason for a 5-9 year old child to be admitted to hospital in England. Supervised toothbrushing is the government’s first step to improving children’s oral health as part of the commitment to raise the healthiest ever generation of children. There has also been a consultation to expand community water fluoridation to the North-East.
Health Minister Stephen Kinnock said: “We know that a third of five-year-olds in the most deprived areas have experience of tooth decay – something we know can have a lifelong impact on their health.
“This is why we are getting on with the job of delivering these toothbrush & toothpaste packs to the most deprived areas to help children have the best start in life by reinforcing good toothbrushing habits.
“We are so grateful to Colgate-Palmolive who have worked tirelessly with us to get two million packs out to more than 500,000 children for the start of this school year to deliver on our ambition.”
The two million packs have come through the innovative collaboration with Colgate-Palmolive, which has committed to donate over 23 million toothbrushes and fluoride toothpastes over the next five years to support the programme.
Across the country 3 Colgate Trucks will be delivering donated products to local authorities to support their supervised toothbrushing schemes throughout the year.
The partnership also includes oral health educational materials and products for home, so families have the support they need to make sure the good habits continue at home and over the school holidays.
Additional funding worth £11 million has been distributed to local authorities who will work to identify early years settings in target areas and encourage them to take part in daily supervised toothbrushing. n
College of General Dentistry appoints Poppy Dunton as Hygiene & Therapy Faculty Chair
The College of General Dentistry (CGDent) has appointed Poppy Dunton as Chair of the Board of its Faculty of Dental Hygiene and Dental Therapy.
A dental therapist working in general dental practice and implant clinics in Harrogate, York and Durham, Poppy is also a Tutor and Clinical Supervisor in Dental Hygiene at Teesside University, and as a dental business consultant helps ailing squat practices to improve their periodontal care. She was previously Operations Manager, CQC Manager and Lead Dental Therapist at a private dental practice group in Northampton. Having first worked in dentistry on a work placement as a 15-year-old, she has also been a receptionist, compliance and treatment coordinator and dental nurse. She joined the College as an Associate Member in 2022, enrolled on the Certified Membership Scheme, was appointed to the Board of the Faculty of Dental Hygiene and Dental Therapy and was a facilitator at the College’s NextGen Leadership Workshop in 2023. She is also a member of the British Society of Dental Hygiene and Therapy, the British Association of Dental Therapists, the

Association of Dental Implantology and the British Society of Periodontology and Implant Dentistry. The Faculty of Dental Hygiene and Dental Therapy is a constituency automatically comprising all members of the College who are dental hygienists and/or dental therapists, and the Faculty Board advances the interests of these professional groups within the College. The board also includes Sarah Murray MBE, Fiona Sandom FCGDent MBE and Jyoti Sumel. n



TJames Cooke T: 01732 371 581
E: james.cooke@purplems.com http://www.smile-ohm.co.uk/
he nights are drawing in and the shops are under invasion from elves and snowmen. Autumn is indeed upon us.
A new school year has begun but, as we all know, every day is a school day. There’s certainly a lot to learn in this issue with a whopping five hours of CPD up for grabs. As always, CPD from this magazine can be completed at cpd.the-probe.co.uk and it’s free to sign up!
SUBSCRIBE TO SMILE
Rates: UK £39.95 per year; Overseas £83 - all cheques in sterling drawn on a UK bank made payable to ‘Smile’. 8 issues including 16 hrs CPD £39.95

Published by Purple Media Solutions
The Old School House, St Stephen’s Street Tonbridge, Kent TN9 2AD Tel: 01732 371 570
Managing Editor James Cooke james.cooke @purplems.com Tel: 01732 371 581
Commercial Director Gary Henson gary.henson@purplems.com Tel: 07803 505208
Production and Designer 1 Lorna Reekie lorna reekie @purplems.com Tel: 01732 371 584
Production and Designer 2 Rob Tremain rob.tremain@purplems.com








Also in this issue, Dr Mahrukh Khwaja teaches us how to not only survive but thrive by applying the science of positive psychology on page 10. Meanwhile, on page 14, we learn about the latest consensus on dental plaque biofilm management.
Finally, with Mouth Cancer Action Month just around the corner (taking place in November), Dr Nigel Carter kicks off this edition by discussing the hidden price tag of mouth cancer on page 8.
Enjoy the magazine!
not necessarily the views of the magazine, nor of Purple Media Solutions Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee, BDS.



in association with:

Other titles
Divisional Administrator Francesca Smith francesca.smith@purplems.com Tel: 01732 371 570
Circulation Manager Andy Kirk
Managing Director Ed Hunt ed.hunt@purplems.com Tel: 01732 371 577






































Comparative efficacy of self-administered dentifrices for the management of dentine hypersensitivityA systematic review and network meta-analysis
A.J. Pollard et al. J of Dent. 130 (2023) 10443: 1-13. Independent Meta-analysis 2023 based on clinical studies of toothpaste occluding technologies only.


Aim: This systematic review used a network meta-analysis of randomized controlled trials to determine how effective self-administered toothpastes are at managing pain from dentine hypersensitivity (DH).

Study selection: Following the registration of the systematic review, the researchers conducted a search of three databases: MEDLINE, Embase, and CENTRAL. The goal was to find parallel randomized controlled trials involving adults with dentine hypersensitivity. The studies needed to use at least two recognized stimuli and evaluate the short-term effectiveness of home-use toothpaste in reducing pain. Of the 62 studies that were assessed, 32 were included in a meta-analysis, while the other 30 were described in a narrative review. To compare the relative effectiveness of different interventions, a network meta-analysis was used.

Results exclusive to occluding technologies: Among occluding technologies, PROARGIN technology showed the most included clinical studies into the Meta-Analysis. The evaluation confirmed significant short and long term improvement in dentine hypersensitivity pain relief by PRO-ARGIN technology.
Implications for practice: PRO-ARGIN technology in Colgate® SENSITIVE INSTANT
Relief toothpaste provides instant3 and long-lasting4 pain relief to patients suffering from sensitivity.
Let science find the best solution
META-ANALYSIS provides a powerful tool for synthesising data from all relevant and identifiable studies that meet pre-defined criteria. This method increases statistical power to provide precise, reliable conclusions by reviewing and consolidating results whilst managing the risk of bias.



Dentine hypersensitivity is a significant concern for you and your patients
Up to 57% of people feel the pain of sensitive teeth due to exposed dentine.1
Not all solutions are equal
Many product technologies claim to provide relief from the pain of sensitive teeth. How do you know which is the most effective when they are not all supported by the same level of scientific evidence?













An unprecedented META-ANALYSIS with 150 studies reviewed2
Independent experts came together to filter 150 studies, examine and compare findings including 62 studies to objectively assess treatments for dentine hypersensitivity. This review included available randomised controlled trials relating to the efficacy of many desensitising technologies such as PRO-ARGIN, Novamin and Stannous only.

PRO-ARGIN is the most clinically proven desensitising occluding technology2
PRO-ARGIN emerged as the most clinically proven desensitising occluding toothpaste technology for the management of dentine hypersensitivity pain.


























References: 1. Berg C, et al. J Funct Biomater. 2021;12:27. 2. Pollard et al. J of Dent. 130 (2023) 10443:1-13. Independent Meta-analysis 2023 based on clinical studies of toothpaste occluding technologies. 3. Nathoo et al. J Clin Dent. 2009;20 (Spec Iss):123–130 (For instant relief, apply directly to the sensitive tooth with finger tip and gently massage for 1 minute). 4. With continued use, Docimo et al. J Clin Dent. 2009;20 (Spec Iss):17– 22.
The hidden price tag of mouth cancer
Dr Nigel Carter, CEO of the Oral Health Foundation, explains
Few diseases carry such a heavy price as mouth cancer. In the UK, 10,825 were diagnosed in the most recent year – around 30 a day. Cases have more than doubled in a generation, yet survival rates have barely shifted. The reason is simple: too many are found too late.
The human cost is devastating. For patients, it can mean life-changing surgery, loss of speech, difficulty eating, and lasting psychological impact. For families, it is emotional strain, financial hardship, and sometimes bereavement.
The wider costs – to the health system, the economy, and society – are rarely discussed. This November, Mouth Cancer Action Month will focus on The Costs of Mouth Cancer to bring that reality into the open.
The many costs of late detection
Treating mouth cancer is not just clinically demanding – it is financially punishing. An early stage case costs around £2,600; for advanced disease, it can climb to £19,500.1
Advanced cases often require major surgery, reconstruction, radiotherapy, and prolonged rehabilitation, placing heavy demands on NHS resources. Over five years, head and neck cancers –including most mouth cancers – have cost the NHS more than £255 million, with almost £20,000 spent per patient in the first year after surgery.2
But numbers cannot capture the real cost. Late detection can mean losing the ability to speak or eat normally, living with facial disfigurement, or facing permanent changes to taste and swallowing. These are not temporary inconveniences – they alter every meal, conversation, and social interaction for life. The emotional toll is immense, often accompanied by depression, anxiety, and isolation. Families shoulder a heavy burden – becoming carers, coping with financial insecurity, and navigating a complex health system while watching someone they love endure long and painful treatment.
Around half of mouth cancer patients never return to employment after their diagnosis – a fact rarely acknowledged, yet one that underscores how farreaching the consequences can be. Employers lose skilled workers, communities lose active members, and health and social care services are left supporting needs that could have been avoided. Cancer Research UK estimates premature cancer deaths cost the UK economy £10.3 billion annually in lost productivity3 – an average of £61,000 per death – alongside up to £1.7 billion in lost paid work and £4–4.5 billion in unpaid care.4
Much of this could be prevented. Early detection saves lives, preserves quality of life and livelihoods, and spares families years of hardship. Dentistry is uniquely placed to make that difference, but relying solely on spotting lesions during routine appointments is no longer enough, particularly when many most at risk – smokers, heavy drinkers, and people in deprived areas – are the least likely to attend.
Dentistry’s reach must extend beyond the chair
No other part of the health system examines the oral cavity as often as we do, and each examination is a chance to detect potentially cancerous lesions early. Yet those who most need these checks often do not attend until the disease is advanced. This demands a more proactive approach.
Dental teams should be visible in settings beyond their surgeries – pharmacies, workplaces, care homes, and homeless shelters – to reach those who rarely access mainstream services. In practice,
why dentistry must change the way it tackles it

however, this outreach is rarely supported by NHS commissioning and is often delivered voluntarily or through short-term funding.
Partnerships with GPs, practice nurses, and cancer charities can create referral pathways for patients presenting with oral symptoms elsewhere, but without formal recognition – and payment – for this work, coverage will remain patchy.
If the government is serious about prevention, it must reinvest in community dentistry and commission these services nationally, not leave them to the goodwill of overstretched teams.
Advocacy as a professional responsibility
Dentistry has often spoken about mouth cancer within its own circles, but public engagement is still too often limited to posters in waiting rooms and leaflets for those already in the chair. Awareness must reach beyond our patient base, into spaces where at-risk groups are most likely to be found –community clubs, social housing hubs, workplaces with older employees, faith centres, and venues offering tobacco or alcohol support. Local media can help keep the conversation visible.
Commissioning groups should be encouraged –and where necessary, challenged – to include oral cancer prevention in their strategies. Nationally, the profession’s trusted voice should be used to push for policies that reduce tobacco and alcohol harm, advocate for HPV vaccination uptake, and secure funding for oral screening programmes. This is not beyond our remit – it is central to preventing disease. And it cannot be confined to November; it must be part of year-round advocacy.
Making mouth cancer everyone’s business
When detected early, survival rates can be up to nine in 10. Found late, they fall to around half.5 This contrast should make every dental professional question whether the current model – passive detection during routine appointments – is fit for purpose. Moving towards an active, searchand-engage approach will require creativity, persistence, and, in some cases, stepping outside our comfort zones.
Mouth Cancer Action Month offers a focal point for attention, but vigilance must not be seasonal. The costs of mouth cancer – in lives, livelihoods, and healthcare resources – are paid every day. We have the skills, knowledge, and public trust to lead
change. What remains is the will to redefine our role: from providers of clinical services to active agents in one of the most urgent public health battles of our time.
This November, The Costs of Mouth Cancer will be our rallying call. The challenge is to ensure that when we speak about costs, we are not talking about those counted in lives lost because the chance to act came too late.
Visit www.mouthcancer.org and support Mouth Cancer Action Month.
References
1. Ribeiro Rotta, R.F. et al. (2022) ‘The cost of oral cancer: A systematic review’, PLOS ONE, 17(5), e0266346. Available at: [PLOS ONE article] (Accessed: August 2025).
2. Kim, K. et al. (2011) ‘Long-term costs associated with healthcare use of people treated surgically for squamous cell carcinoma of the head and neck in the UK’, BMC Head & Neck Oncology, 3, 47. Available at: [BMC Head & Neck Oncology] (Accessed: August 2025).
3. Cancer Research UK. (2025) Health is wealth: tackling cancer to grow the economy. Cancer Research UK, 27 June. Available at: [CRUK report] (Accessed: August 2025).
4. Ribeiro Rotta, R.F. et al. (2022) ‘The cost of oral cancer: A systematic review’, PLOS ONE, 17(5), e0266346. Available at: [PLOS ONE article] (Accessed: August 2025).
5. Cancer Research UK. (2024) Survival for mouth and oropharyngeal cancer. Available at: Cancer Research UK (Accessed: August 2025). n
ABOUT THE AUTHOR
DR NIGEL CARTER OBE

Dr Nigel Carter OBE Chief Executive of the Oral Health Foundation.










Thriving, not just surviving
Dr Mahrukh Khwaja shares how applying the science of positive psychology can help dental professionals build resilience, boost happiness and create more positive, engaging workplaces

Dentistry can be one of the most rewarding careers, but it can also be one of the most pressured. Long days in surgery, clinical responsibilities and the demands of patient care mean that stress and burnout are common. A recent survey revealed that almost two-thirds (63%) of UK dental professionals report feeling frequently burnt out and exhausted.1
Psychologist Christina Maslach defines burnout as a syndrome with three dimensions: emotional exhaustion, cynicism or depersonalisation, and reduced personal accomplishment.2 In dentistry, this can show up as feeling drained before the day has begun, becoming detached or critical about your work, and losing the sense that you are making a difference. Early signs include low mood, pessimistic thinking, disrupted sleep, changes in appetite, or withdrawing from colleagues. Recognising these patterns early is the first step to protecting long-term wellbeing.
Changing career course
I know this from personal experience. Just a few years into practice I went through burnout and depression myself. With the help of therapy, I discovered tools such as mindfulness, selfcompassion and cognitive behavioural techniques (CBT). They helped me recover and showed me that prevention is always better than cure.
That difficult period changed the course of my career. I went on to train as a positive psychologist alongside my dental career and founded Mind Ninja (mind-ninja.co.uk), a coaching and training company that helps dental professionals protect their mental health and build resilience.
This experience also reshaped how I think about resilience. It is often misunderstood as simply being tough or “pushing through”. In reality, resilience is about navigating adversity in a way that allows us to grow stronger and flourish. It involves recognising when we are struggling, drawing on internal strengths like optimism and flexible thinking, and seeking external support from colleagues, mentors or professional organisations. True resilience is never about going it alone.
Positive psychology in practice
One way to build this kind of resilience is through positive psychology, the scientific study of wellbeing, happiness and human flourishing. One of its most
practical models is known as PERMAH, which brings together six areas of wellbeing:
1. Positive emotions – finding joy and gratitude in daily life
2. Engagement – immersing yourself in activities that create flow, whether in clinical practice or outside hobbies
3. Relationships – nurturing small moments of connection with colleagues, patients and loved ones
4. Meaning – aligning with your values so you do not lose sight of why you chose this profession
5. Accomplishment – setting achievable goals that bring a sense of fulfilment
6. Healthy habits – from good ergonomics and hydration to taking mindfulness breaks I often describe PERMAH as a wellbeing checklist. When you feel stretched or low, you can use it to identify which areas may need strengthening and take small steps to rebalance.
Habits and culture that support wellbeing
Mindfulness is one of the most accessible ways to support wellbeing. It does not require long meditation sessions; simply bringing awareness to the present moment can make a difference. A mindful breath while waiting for alginate to set or before calling in your next patient can restore calm and focus, especially if you extend the out-breath to trigger the parasympathetic nervous system. Gratitude is another simple but powerful habit. In a busy practice, it is easy to dwell on what went wrong. Taking a moment to share small wins with your team can shift perspective, lift morale and build a more positive culture over time. However, individual habits alone are not enough. Lasting wellbeing also depends on the culture of a workplace. Dental professionals can model compassion in how they interact with patients and colleagues, yet real change requires organisational commitment. Training wellbeing champions, investing in mental health first aid and challenging toxic behaviours are crucial. No amount of mindfulness can compensate for a culture that undermines values or fosters fear.
Looking ahead with hope
Despite the challenges, I feel optimistic about the future of mental health in dentistry. There is growing recognition that wellbeing is as important
Find out more
Dr Mahrukh Khwaja will be one of the first guests on BSDHT’s new podcast Dental Health Matters, launching this November. She will be discussing resilience, culture and positive psychology in-depth with BSDHT President Rhiannon Jones.
Register to hear the full episode at www.bsdht.org.uk/podcast
as clinical outcomes, and the focus is shifting from crisis management to prevention and flourishing. I hope more organisations will invest in leadership training and culture change, creating environments where every member of the dental team feels valued. By moving beyond survival mode, dentistry can create conditions where professionals truly thrive. n
References
1. Two-thirds of dental professionals “burnt out and exhausted”. Dental Protection, 2025. Available at: https://www.dentalprotection.org/uk/articles/ two-thirds-of-dental-professionals--burnt-outand-exhausted. Accessed 4 September 2025
2. Maslach M, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry 2016; 15(2): 103-111. doi: 10.1002/wps.20311
ABOUT THE AUTHOR
DR MAHRUKH KHWAJA

Dr Mahrukh Khwaja is both a practising dentist and a positive psychologist. She is the founder of Mind Ninja, a coaching and training company that delivers evidence-based wellbeing strategies for dental professionals.

32 reasons to buy the new Varios Combi Pro2


Register now


Varios Combi Pro2
Say hello to an evolution in ultrasonic and powder therapy.


Come and see the NEW Varios Combi Pro2 on stand 12-15
On stand, hands-on Workshops for dentists, hygienists and therapists Fri 28th Nov. Minimally Invasive Non-Surgical workshop - Work smarter, not harder! Dr Varkha Rattu, supported by
Sat 29th
Gentle yet powerful, reliable and exceptionally durable, Varios Combi Pro2 has a host of advanced features designed to improve efficiency, control and enhance patient comfort.
Engineered with meticulous attention to detail, Varios Combi Pro2 is an investment in clinical excellence and in the health of your patients.
NSK’s oral hygiene range is not just limited to Varios Combi Pro2. Take a look at our restorative & prophy handpieces, ultrasonic or air scalers and portable powder therapy devices.
Combi Pro2
Siobhan Kelleher, Lauren Long & Kathryn Mayo
Nov. Implant Maintenance workshop. Kathryn Mayo & Jenny Walker supported by Lauren Long,

Is your patient one of
them?
Is your patient one of them?
Colgate® PreviDent® provides the protection your patients need to help make their last cavity their last.
Colgate® PreviDent® provides the protection your patients need to help make their last cavity their last.



Anna, 61
Anna, 61
Anna, 61
Gingival recession
Gingival recession
Exposed roots

Gingival recession
Gingival recession









Calvin, 24
Calvin, 24
Mason, 6 Frequent snacking
Antidepressants
Antidepressants

Frequent snacking
Jaycee, 11
Orthodontic appliances


Frequent snacking








Carole, 28
Carole, 28
Prescription medications
Antidepressants
Assess their caries risk, and consider prescribing high fluoride to increase caries control 4

Prescription medicationsOrthodontic appliances 42% of adults1 66% of adults2 4M in the U.S.3
Prescription medicationsOrthodontic appliances 42% of adults1 66% of adults2






To help your patients prevent and reverse caries, visit colgateprofession
To help your patients prevent and reverse caries, visit colgateprofession

*"Caries risk and social determinants of health," JADA, December 2022
*"Caries risk and social determinants of health," JADA, December 2022
High Fluoride products for in-office and at-home*,†
Be confident prescribing Colgate® Duraphat®, the brand your patients know and trust^
2 Georgetown University. “Prescription Drugs” Health Policy Institute, 2019, hpi.georgetown.edu/rxdrugs/



3 “Does Dental Insurance Cover Braces?” Humana.com, www.humana.com/dental-insurance/dental-resources/dental-braces

1 “Periodontal Disease in Adults (Age 30 or Older).” National Institute of Dental and Craniofacial Research, U.S. Department of Health and Human Services, www.nidcr.nih.gov/ research/data-statistics/periodontal-disease/adults

1 “Periodontal Disease in Adults (Age 30 or Older).” National Institute of Dental and Craniofacial Research, U.S. Department of Health and Human Services, www.nidcr.nih.gov/ research/data-statistics/periodontal-disease/adults
2 Georgetown University. “Prescription Drugs” Health Policy Institute, 2019, hpi.georgetown.edu/rxdrugs/
*Colgate® Duraphat® 5000 fluoride toothpaste for patients 16 years of age and over at increased caries risk. †Colgate® Duraphat® 2800 ppm high fluoride toothpaste for patients 10 years of age and over at increased caries risk
3 “Does Dental Insurance Cover Braces?” Humana.com, www.humana.com/dental-insurance/dental-resources/dental-braces


^YouGov Omnibus for Colgate® UK, data on file June 2015. Claim applies only to the Colgate® brand. References: 1. Oral Health Survey of Adults attending dental practices, 2018. Public Health England, published 2020. 2.National
Dental Epidemiology Programme for England, Oral health survey of 3-year-old children 2020: a report on the prevalence and severity of dental decay, Public Health England. 3. National Dental Epidemiology Programme (NDEP) for England: oral health survey of 5 year old school children 2024, Office for Health Improvement and Disparities. 4. Child Dental Health Survey 2013, England, Wales and Northern Ireland National statistics, published 2015. 5. Tavss et al. Am J Dent 2003;16(6):369-374. 6. https://cariescareinternational.com/wp-content/uploads/2020/03/CCI-Practice-Guide.pdf. Last accessed July 2024.
Name of the medicinal product: Duraphat® 50mg/ml Dental Suspension. Active ingredients: 1ml of suspension contains 50mg Sodium Fluoride equivalent to 22.6mg of Fluoride (22,600 ppm F-) Indications: Prevention of caries, desensitisation of hypersensitive teeth. Dosage and administration: Recommended dosage for single application: for milk teeth: up to 0.25ml (=5.65mg Fluoride), for mixed dentition: up to 0.40ml (=9.04 Fluoride), for permanent dentition: up to 0.75ml (=16.95 Fluoride). For caries prophylaxis the application is usually repeated every 6 months but more frequent applications (every 3 months) may be made. For hypersensitivity, 2 or 3 applications should be made within a few days. Contraindications: Hypersensitivity to colophony and/or any other constituents. Ulcerative gingivitis. Stomatitis. Bronchial asthma. Special warnings and special precautions for use: If the whole dentition is being treated the application should not be carried out on an empty stomach. On the day of application other high fluoride preparations such a fluoride gel should be avoided. Fluoride supplements should be suspended for several days after applying Duraphat® Interactions with other
revision of text: July 2024.

Assessing caries risk













Name of the medicinal product: Duraphat® 2800 ppm Fluoride Toothpaste. Active ingredient: Sodium Fluoride 0.619 %w/w (2800 ppm F-). Indications: For the prevention and treatment of dental caries (coronal and root) in adults and children 10 years of age and over. Dosage and administration: Adults and children 10 years of age and over: Use daily instead of normal toothpaste. Apply a 1cm line of paste across the head of a toothbrush and brush the teeth thoroughly for one minute morning and evening. Spit out after use; for best results do not drink or rinse for 30 minutes. Contraindications: Individuals with known sensitivities should consult their dentist before using. Not to be used in children under 10 years old. Special warnings and precautions for use: Not to be swallowed. Undesirable effects: When used as recommended there are no side effects. Legal classification: POM. Marketing authorisation number: PL00049/0039. Marketing authorisation holder: Colgate-Palmolive (U.K.) Limited, Goldsworth Place, 1 Forge End, Woking, Surrey, GU21 6DB. Recommended retail price: £5.10 (75ml tube). Date of revision of text: July 2024.
Name of the medicinal product: Duraphat® 5000 ppm Fluoride Toothpaste. Active ingredient: Sodium Fluoride 1.1%w/w (5000 ppm F-). 1g of toothpaste contains 5mg fluoride (as sodium fluoride), corresponding to 5000ppm fluoride. Indications: For the prevention of dental caries in adolescents and adults 16 years of age and over, particularly amongst patients at risk from multiple caries (coronal and/or root caries). Dosage and administration: Brush carefully on a daily basis applying a 2cm ribbon onto the toothbrush for each brushing. 3 times daily, after each meal. Contraindications: This medicinal product must not be used in cases of hypersensitivity to the active substance or to any of the excipients. Special warnings and precautions for use: An increased number of potential fluoride sources may lead to fluorosis. Before using fluoride medicines such as Duraphat, an assessment of overall fluoride intake (i.e. drinking water, fluoridated salt, other fluoride medicines - tablets, drops, gum or toothpaste) should be done. Fluoride tablets, drops, chewing gum, gels or varnishes and fluoridated water or salt should be avoided during use of Duraphat Toothpaste. When carrying out overall calculations of the recommended
Leading consensus on dental plaque biofilm management
Oral diseases driven by a dysbiotic dental plaque biofilm are preventable
As dental plaque biofilm-driven oral diseases continue to place avoidable burdens on patients and healthcare systems, a collective of UK oral health leaders gathered in London on 18 July 2025 to reaffirm the evidence and align on shared prevention strategies.
Hosted by Kenvue*, the event brought together representatives from the British Society of Periodontology (BSP), the Oral Health Foundation (OHF), the British Society of Dental Hygiene and Therapy (BSDHT), and the British Association of Dental Therapists (BADT), alongside leading clinicians, academics and Key Opinion Leaders.
Opening the discussion, Professor Iain Chapple said: “We’re here today to assimilate the latest evidence from the S3-level guidelines, the Delivering Better Oral Health (DBOH) toolkit, and other sources that have changed our understanding of dental plaque biofilm-mediated diseases like periodontitis and caries. There are still many misunderstandings within the practising community, so we have brought national society leaders together to clarify the evidence and explore how we cascade this evidence consistently across the profession.”
The consensus below was developed and supported by all those in attendance and reflects Kenvue’s continued commitment to evidencebased practice and support for clinical education across the oral healthcare team.
Oral diseases driven by a dysbiotic dental plaque biofilm are preventable
‘Oral disease prevention is multi-dimensional and requires cost-effective population-level approaches, as well as personalised guidance throughout the life course,1 with specific touch points at (pre-)birth, childhood, adolescence, independent adult living and assisted living. Effective self-care plays a critical role in the prevention of dental caries and gingivitis.
Mechanical plaque removal using a fluoride toothpaste is the mainstay of dental plaque biofilm control, but a significant proportion of the population are unable to achieve levels that stabilise gingival inflammation and dental caries activity in their mouths. In such cases, additional methods of dental plaque biofilm management should be considered: these include the use of mouthrinses containing chemical agents with proven antimicrobial capability, principally chlorhexidine (CHX), essential oils (EOs) and cetylpyridinium chloride (CPC)2 and fluoride for demineralisation/ remineralisation efficacy. 3
For the use of fluoride-containing toothpaste formulations for adults, the DBOHv4 toolkit has been updated to “spit don’t rinse with water”. 3 For specific antimicrobial mouthrinses, 2 spitting and rinsing with a fluoride mouthrinse containing at least 225ppm fluoride after brushing helps build the salivary fluoride reservoir for dental caries prevention. 4 If using a mouthrinse, protocols may vary, but in periodontal care, antimicrobial fluoride-containing mouthrinse use after brushing is recommended and for caries management, fluoride mouthrinse use at a different time of day is advised.’

The following KOLs contributed to the discussion and supported the consensus, representing a cross-section of UK dental leadership from clinical practice, academia, and national associations.
• Dr Ben Atkins – Past President, Oral Health Foundation
• Professor Avi Banerjee – Professor of Cariology & Operative Dentistry, King’s College London
• Leon Bassi – Clinical Lecturer, Restorative Dentistry (Dental Therapy)
• Dr Nigel Carter – Chief Executive, Oral Health Foundation
• Professor Iain Chapple – Professor of Periodontology and Consultant in Restorative Dentistry at the University of Birmingham and the NIHR Birmingham Biomedical Research Centre
• Debbie Hemington – BADT President
• Rhiannon Jones – BSDHT President
• Simone Ruzario – BSDHT President Elect
• Dr Shazad Saleem – Joint Chair, BSP Education Advisory Committee and Faculty Member
• Dr Fiona Sandom – Lead Dental Educator for Health Education and Improvement Wales
• Professor Nicola West – BSP President, Chair and Honorary Consultant in Restorative Dentistry (Periodontology) at the University of Bristol Dental School
• Professor David Williams – Professor Emeritus of Global Oral Health, Faculty of Medicine and Dentistry, Queen Mary University of London.
“Kenvue is proud to support the advancement of oral healthcare through scientific collaboration, accessible education and clinical partnership. This latest consensus forms part of an ongoing programme to promote best practice and improve patient outcomes across the UK,” Bas Vorsteveld, Area Managing Director, Northern Europe at Kenvue.
For more information, visit https://kenvuepro.com/ en-gb/brands/listerine.
All attendees to this advisory board were paid a fair market value compensation for their time by Kenvue, which included creating and approving this consensus statement and content for release.
References
1. Global strategy on oral health. Geneva: World Health Organization 2022. Available at: https://www. who.int/publications/i/item/9789240062889. (Accessed: 31 July 2025)
2. West N et al. BSP implementation of European S3-level evidence-based treatment guidelines for stage I–III periodontitis in UK clinical practice. Journal of Dentistry 2021; 106: 103562. doi: 10.1016/j.jdent.2020.103562
3. Delivering better oral health: an evidencebased toolkit for prevention. Office for Health Improvement and Disparities, Department of Health and Social Care, NHS England and NHS Improvement. London 2021, 4th edition. Available at: https://www.gov.uk/government/publications/ delivering-better-oral-health-an-evidence-basedtoolkit-for-prevention. (Accessed: 31 July 2025)
4. Sköld UM, Birkhed D. Effect of post-brushing mouthwash solutions on salivary fluoride retention – study 1. Journal of Clinical Dentistry 2012; 23(3): 97-100. PMID: 23210421 n
About Kenvue
Kenvue globally is the world’s largest pure-play consumer health company by revenue. Built on more than a century of heritage, our iconic brands, including Aveeno®, Johnson’s®, Listerine®, Neutrogena®, and Nicorette®, are sciencebacked. At Kenvue, we realise the extraordinary power of everyday care. Our teams work every day to put that power in consumers’ hands and earn a place in their hearts and homes. Learn more at www.kenvue.com/uk




200-300% More Contact than Leading Competitors
Greater adaptation means less scaling strokes. Better for you, better for your patients.




Less Sharpening


PDT blades are thinner, sharper, and heat-treated for durability, lasting up to seven times longer.



























Ultra-lightweight Design
Solid resin handle reduces fatigue and muscle strain during prolonged use.







Superior Tactile Sensitivity
Knurled grip provides superior tactile sensitivity for precise control during procedures.


FINER • SHARPER • STRONGER
Expertly crafted to provide maximum comfort and tactile sensitivity

Alzheimer’s and dental pain management Overcoming challenges with dexterity
Oral health problems can develop for anyone, causing difficulty eating, trouble concentrating, and pain. However, for some people the experience and management of dental issues is more complex. Currently, there are an estimated 982,000 people in the UK living with dementia.i As such, it’s important to understand the various ways that patients with dementia may struggle with their oral health, how to recognise patients in pain, and how best to support individuals in treatment and pain management.


Oral health and dental pain in dementia patients
Poor oral care is observed in patients with cognitive impairment, due to decreased motor coordination and agitated behaviour making it difficult to perform oral care. Exacerbating this, patients with dementia usually attend dental appointments less often. Around 75% require assistance to perform daily activities like oral hygiene.ii
Common dental problems amongst dementia patients include caries and gingivitis which are preventable with regular brushing and a healthy diet. Tooth wear and damage, as well as dry mouth are also common, causing sensitivity, pain, and discomfort.iii Some patients with dentures may also experience pain due to sores, so it is important for ill-fitting dentures to be addressed in order to maintain quality of life.iv
Ability to communicate pain
As dementia worsens over time, the likelihood of a patient being in any type of pain increases. Daily pain is experienced by between 50% to 80% of patients with moderate to severe dementia.iv However, it can be difficult to ascertain whether patients are affected. This is because Alzheimer’s disease can cause a person to develop a masklike facial expression, minimising the facial expressions associated with pain. Some patients may also have lost the cognitive ability to communicate their pain – leaving individuals with very few options to alert their caregivers that something is wrong, with negative behaviours like screaming or aggression possible.iv
As assessment and treatment of pain in dementia patients is challenging due to the difficulty in reporting pain, undiagnosed and untreated pain is thought to affect up to a third of those in the community, and half of those in nursing homes.ii
Identifying pain and mouth care problems
For some people, dental problems can make it difficult to eat meaning that, over time, patients will eat less and potentially start to lose weight. For patients with dementia, this may be an indicator to caregivers that there is a problem in the mouth and that they may be in pain. If concerns are raised about this, it’s important for dental professionals to check the patient’s mouth for any signs of disease, infection, or irritation.iii
Aside from problems eating, there may be a number of other signs for caregivers to look out for as an indicator of dental pain. These include: frequently touching their face, facial swelling, not wearing dentures, restlessness, disturbed sleep, refusing help with dental care, or aggressive behaviour towards their carer. It is important that these symptoms are not dismissed as part of a person’s dementia, as they could be a sign that they are in pain and need help from a dentist. iii
Supporting patients and managing dental pain
In order to support patients with dementia in maintaining their oral health, there are a number of recommendations for caregivers. These includes establishing a routine to help ensure the teeth are cleaned twice per day and prevent dental problems developing. Where possible, encourage the person to clean their teeth by themselves, only stepping in if they need help. It is also useful to minimise the amount of sugar the individual consumes, again helping to prevent oral disease.v
If patients with dementia do experience oral pain, it’s important for dental professionals to recommend solutions to manage their pain at home whilst they wait for treatment. Orajel™ Dental Gelvi contains 10% benzocaine, allowing the patient or their carer to apply the local anaesthetic to the painful tooth. Dental professionals can also recommend Orajel™ Extra Strengthvii which contains 20% benzocaine, for the rapid relief of dental pain. Additionally, if patients are suffering with mouth ulcers or denture pain, Orajel™ Mouth Gelviii is the ultimate soother.
Supporting patients with advanced needs is essential as a dental professional, with conditions like dementia often having a significant impact on a patient’s ability to effectively maintain their own oral health. Dementia patients are at a higher risk of oral disease and undetected pain, so understanding how best to monitor their oral health and manage pain whist they wait for treatment is key for maintaining their quality of life.
For essential information, and to see the full range of Orajel products, please visit www.orajel.co.uk n
References available upon request
ABOUT
THE AUTHOR

For many dental professionals, tooth brushing is a simple, non-negotiable part of the everyday routine. However, effective cleaning – tooth brushing twice a day, with the removable of debris from interproximal spaces – isn’t easy for some patients.
Dexterity is something that many people may take for granted, but for those that cannot clean their dentition with ease, their clinician is a primary source of support.
Dental professionals need to be aware of prominent dexterity issues, and how they may affect a wide array of patients. They should also understand the aspects of an oral hygiene routine that can be most difficult, and identify opportunities to use alternative oral hygiene adjuncts.
Making a connection
Hand dexterity is the ability to perform small, precise hand movements with flow and accuracy. Some studies differentiate manual ability and manual dexterity, with the latter describing the proficiency of the skill to perform a manual task depending on factors such as cognition.ii
Complications may be seen throughout the entirety of an oral hygiene routine. Take the use of traditional dental floss as an example. A patient needs to take floss from a dispenser, which uses unilateral or bilateral gross motor movement of the shoulder, elbow, forearm, wrist, and fingers; then onto the action of flossing itself, they require fine motor control with manual dexterity of the arms, hands and fingers once more.iii
Studies have shown that manual dexterity is linked to the effectiveness of dental flossing,iii and some that focus on patients in residential homes have found that manual dexterity can be connected to the amount of dental plaque present.ii Where more plaque is present, patients are more likely to develop periodontal infections, which can be severely damaging in the long term.
Patients affected
Causes for limited dexterity vary, but one of the most well-known connections is age. This, alongside grip strength, is a significant predictor of hand dexterity.iv Maintaining oral health into old age is paramount, as tooth loss can be severely detrimental to general health. Edentulism, which may come from periodontal disease, impacts mastication and makes bolus formation difficult, which creates dysfunctional swallowing. This may lead to a change in diet, and an avoidance of harder foods such as meat, fruits or vegetables, which can lead to malnutrition.v The effects of malnutrition include an increase in severity of oral infections.v
Rheumatoid arthritis is another potential cause for concern. It is the most common inflammatory arthritis and affects around 1% of the UK population,vi with women under 50 around four to five times more likely to be affected by men – though this disparity diminishes with age.vii As well as changes to systemic immune function, rheumatoid arthritis can cause physical impairment, most frequently affecting the wrist, proximal interphalangeal joint (middle of each finger) and the metacarpophalangeal joints (knuckles).vii This complicates oral hygiene routines, especially those that utilise traditional dental floss. Patients with rheumatoid arthritis are found to have a greater risk of periodontal disease.vii
Other causes for limited dexterity may include cerebral palsy, muscular dystrophy, multiple sclerosis and stroke. viii These may appear in a patient’s medical history, or
Jenny is the Marketing Manager at Orajel.
JENNY SINCLAIR BROWN

the individual could volunteer the information during an appointment. Engaging in a discussion around the difficulties faced when performing an oral hygiene routine can then help clinicians recommend the right alternatives for a patient’s needs.
Recommending alternatives
Powered toothbrushes have been recommended in the literature for individuals with decreased manual dexterity, owing to an improved action and
Precise Working Dies in Just Minutes
T Flows beautifully—better than stone—to create a smoother die and to capture minute detail
T No hand-mixing—inject it directly from the automix cartridge into impression
control over tooth cleaning.ix By implementing this solution, the research even states that any individual can use good brushing technique, and experience greater plaque removal and improvement to gingival health, irrespective of manual dexterity. Water flossers have also been recommended for patients lacking manual dexterity x as an alternative to traditional flossing, and should still be used alongside tooth brushing. Patients can disrupt plaque and debris with jets of water, using the different pressure

T Exceptionally hard set—90+ Durometer
T Slightly flexible
T Set time: 2 minutes
options typically available, and they are also able to target bacteria beneath the gingival margin. Patients should be sure to choose high-quality and clinically proven adjuncts above all else. Clinicians can recommend those from Waterpik™, the only water flosser brand to be approved by the Oral Health foundation. With an easy-to-use oral hygiene solution in the Waterpik™ Cordless Advanced water flosser, patients can remove up to 99.9% of plaque from treated areas in just three seconds.xi Plus, it is clinically proven to be up to 50% more effective than traditional dental floss for improving gum help.xii Dexterity may make oral hygiene routines challenging, but not impossible. Clinicians can provide support to patients in appointments, as well as through appropriate recommendations for oral hygiene solutions. This helps more patients maintain their dentition, for more healthy, bright smiles.
For more information on WaterpikTM water flosser products visit www.waterpik.co.uk. WaterpikTM products are available from Amazon, Costco UK, Argos, Boots and Tesco online and in stores across the UK and Ireland. n
References available upon request
ABOUT THE AUTHOR
CHARLEANE MCINALLY

Charleane is a Dental Hygienist and Professional Educator for Waterpik.
A Legacy VPS Bite Registration Material
T Stays stacked on the occlusal surface during placement
T Optimal consistency allows patient to naturally close with zero resistance while capturing every detail
T Hardens to a plaster-like final set with a durometer of 90 to ensure precise articulations

T Set times: 30 Seconds | 60 Seconds | 2 Minutes
FROM IMPRESSION TO WHITENING TRAY IN MINUTES!






performance patients need. The name professionals recommend.


Not all water flossers are equal. Recommend by name.
Industry leader
Recognised as the #1 selling water flosser brand in the UK and in the world.
Recommended by experts
The most recommended water flosser brand by dental professionals and the only one approved by the Oral Health Foundation.
Backed by science
Removes up to 99.9% of plaque bacteria in treated areas* and be 2X as effective as string floss for improving gum health.
Standing the test of time
With 60 years of innovation, WaterpikTM has been committed to a professional- level clean for over half a century.
*in vitro, data on file Bring premium flossing to centre stage

Removes up to 99.9% of plaque bacteria from treated areas*




Reduces gingivitis up to 50% more than string floss†

Helps implant gum health up to 2x more than brushing and string flossing†
Cleans plaque around braces up to 5x better than brushing alone†
†Data on file. Visit waterpik.co.uk

The Female Dentist Board
Member: Linzy Baker Hepatitis and the dental professional

Dental hygienists and therapists provide an invaluable service, offering preventative care and education, treating oral diseases and delivering restorative treatments so that oral health is kept to the best possible standard.
There are challenges, however. From physical strain as a result of sitting in awkward positions for long periods of time, to navigating employment arrangements and difficult patients. Linzy Baker, a dental therapist based at the One to One Dental Clinic on Harley Street, is well-versed on the daily challenges and hopes that her role as a Board Member for The Female Dentist can alleviate the concerns that many may have with the profession.
“I joined The Female Dentist Board to represent dental hygienists and therapists as, after hearing about the vision and initiative, I knew this would be something of interest to my colleagues. I wanted to ensure our voices were heard and I believe that I can provide insights to both the board and members who may be seeking help. This could be for ideas around incorporating dental therapist workflows into their practices, how to connect more likeminded team members with employers and practices, or how best to utilise their team. These are topics I am often discussing with my dental colleagues already.
“I also want to help the next cohort of dental therapists and hygienists connect more; conversations have illuminated how many are isolated in their four walls, working without
support and struggling to stay motivated, with some even thinking of leaving the career. To give nationwide opportunities – not just to one location – for colleagues to connect and broaden their circles, finding like-minded individuals and life-long friends would be a great achievement and something I can envision The Female Dentist achieving.
“The network provides an inclusive hub for women in dentistry to speak freely, ask their questions (even the ones that we think we ’shouldn’t’ ask) and to be their best selves. It is a safe community where we aim to not only educate and inspire, but to have some fun. Too often I hear the stories of isolation within practices or as female bosses; those who are wanting to achieve more but feel unable to do so, women who were thriving in their career but since having children and being away from work aren’t sure how to spin all the plates. The board is full of struggles and success stories and I am greatly inspired by those I sit with and know that they will bring the best advice to the members.
“I am very excited to see The Female Dentist grow as a brand and a cohort expanding its reach to the whole of the UK and bring women in dentistry to the forefront of their careers, encouraging success and building resilience and knowledge for these women to thrive in all aspects of their lives.”
Join The Female Dentist today. For details on membership visitL https://thefemaledentist.co.uk/membership-benefits/ n

As dental professionals, we all face a certain number of occupational hazards. Among these is exposure to blood and other bodily fluids, which increases the risk of related infections such as hepatitis. Understanding how hepatitis viruses are transmitted, their potential impact on both patients and practitioners, and how to mitigate these risks is vital for maintaining a safe dental environment. With World Hepatitis Day promoted this month, I thought this a useful refresher to ensure we are all keeping ourselves as safe as possible.

The virus and its affects
There are several different types of hepatitis – A, B, C, D and E. They all affect the liver, although are caught via different transmission pathways. Hepatitis B (HBV) and C (HCV) are most common and can lead to chronic infection. They are both spread through contact with contaminated blood.i,ii Causing inflammation of the liver, hepatitis can cause a range of symptoms from muscle and joint pain to a fever, nausea, fatigue, loss of appetite, stomach pain, dark urine, itchy skin and jaundice. iii Possible indirect oral health consequences of a hepatitis infection include a higher risk of tooth loss, periodontitis and halitosis.iv
Estimated prevalence
It is estimated that 270,000 people in England have hepatitis B, with a higher-than-national-average percentage of the population affected in London.v Many of these people are believed to have acquired the infection overseas in endemic countries,vi with low mother-to-child transmission and high vaccination rates reported in the UK. Due to direct and indirect exposure to blood, dental professionals have been identified as at-risk of HBV and HCV infection. Historically, the risk of HBV was estimated at 3-4 times greater than the general population, but this has been reduced due to widespread vaccines and developed clinical precautions.vii
Implications for patient care
Where patients attend the practice with confirmed HBV status, their care may need to be tailored accordingly. For example, those with HBV are 38% more likely to have periodontitis compared to those without. This association means that gingival health should be closely monitored and high standards of oral hygiene maintained.viii
In addition, anyone with chronic liver disease will be immunocompromised. This puts them at a higher risk of bleeding and post-treatment infection, which must be considered throughout their dental care.ix
Knowing and reducing the risks
It has been suggested that the gingival sulcus contains the highest concentration of HBV infection intraorally,x highlighting the risk to dental professionals. There is also a potential danger of exposure to the virus via aerosol particles when treating an infected patient.xi
For any healthcare workers, percutaneous injuries are the most likely source of infection when it comes to HBV and HCV. Contact with blood splatter from infected individuals may also be cause for concern. xii
Prioritising prevention over cure, dental professionals who may have direct contact with patients’ blood are strongly recommended to be immunised against hepatitis B.xiii Antibody titres may be checked in the months following the primary vaccination course to support post-exposure prophylaxis decisions, should they be required.
Should accidental or potential exposure to bloodborne infections like HBV or HCV occur, individuals should follow the established post exposure prophylaxis protocols in the practice. These should be initiated as soon as possible after the incident and will likely include washing the wound, in the case of needlestick injury. Vaccination status should be reviewed and administered rapidly in the event of missing or unknown immunisation status. No treatment should be necessary for the appropriately vaccinated professional.xiv

Professional education and confidence
No matter how long you have worked in dentistry, what role you fulfil in the practice or how many patients you see in a day, it’s crucial that you understand the occupational risks you face and how to minimise them. Hepatitis is only one of the threats, and it can be reduced with meticulous preventive measures like vaccination and safe needlestick protocols.
To ensure you are confident in avoiding the dangers, there is a wealth of education and training on offer to the entire team. Online resources, training courses and seminars are widely available and should be utilised by all. n
References available upon request
DR MICHAEL SULTAN

EndoCare, led by Dr Michael Sultan, is one of the UK’s most trusted Specialist Endodontist practices. Through the use of the latest technologies and techniques, the highly-trained team can offer exceptional standards of care – always putting the patient first. What’s more, EndoCare is a dependable referral centre, to which dentists from across the country send their patients for the best in specialist endodontic treatment.























































A brand to trust
Curaden is committed to achieving excellence in oral hygiene and does so through its Curaprox product range and iTOP programme.
Chrystal Sharp works closely with the Curaprox brand. Having qualified in Orthodontic Therapy in 2012 and completed an Advanced Certification in Facial Aesthetics in 2024, Chrystal works as a private orthodontic therapist in London. She explains her love for her work:



“Orthodontics is a specialist area of dentistry and orthodontic therapists are a niche DCP role with only around 1,157 registered to date. Being a pivotal part of the patients orthodontic journey, we are uniquely positioned to build a strong rapport with our patients as we see them on a regular basis. This allows us to raise their confidence along with creating beautiful smiles. In many cases post-orthodontics, an interdisciplinary approach is required to achieve the smile they desire – we can help facilitate the need for implants, veneers or composite bonding.
“The main challenge with wearing a brace is keeping the teeth clean as bacteria and trapped food debris stick to the surfaces, often out of reach from the use of a traditional toothbrush alone. Ultimately, whatever orthodontic appliance a patient has, the risk of white spots left on the teeth and decalcification is high and needs to be carefully managed.”
Powerful products
Curaprox features a comprehensive range of products that can elevate oral hygiene for all. Chrystal highlights their usefulness:
“I’ve known about Curaprox for a long time; they represent a gold-standard in dental products. I have been working closely with Curaprox since 2022, helping to raise their profile directly with my orthodontic patients and a broader audience through social media. Curaprox have a superb product range especially when it comes to orthodontics. This includes the CS 5460 toothbrush which is also available with an orthodontic approved toothbrush head – I recommend this across the board for its soft, flexible bristles that will clasp around brackets on a traditional brace or attachments used with aligner treatment more effectively allowing for a more precise clean.
“For orthodontic patients, demineralisation of the enamel is a greater risk, with aligners trapping food and drink, and braces attracting bacteria around them. To negate the risk, I recommend the Curaprox Aligner Foam as an ideal solution, creating a protective film to restore and remineralise the teeth.”
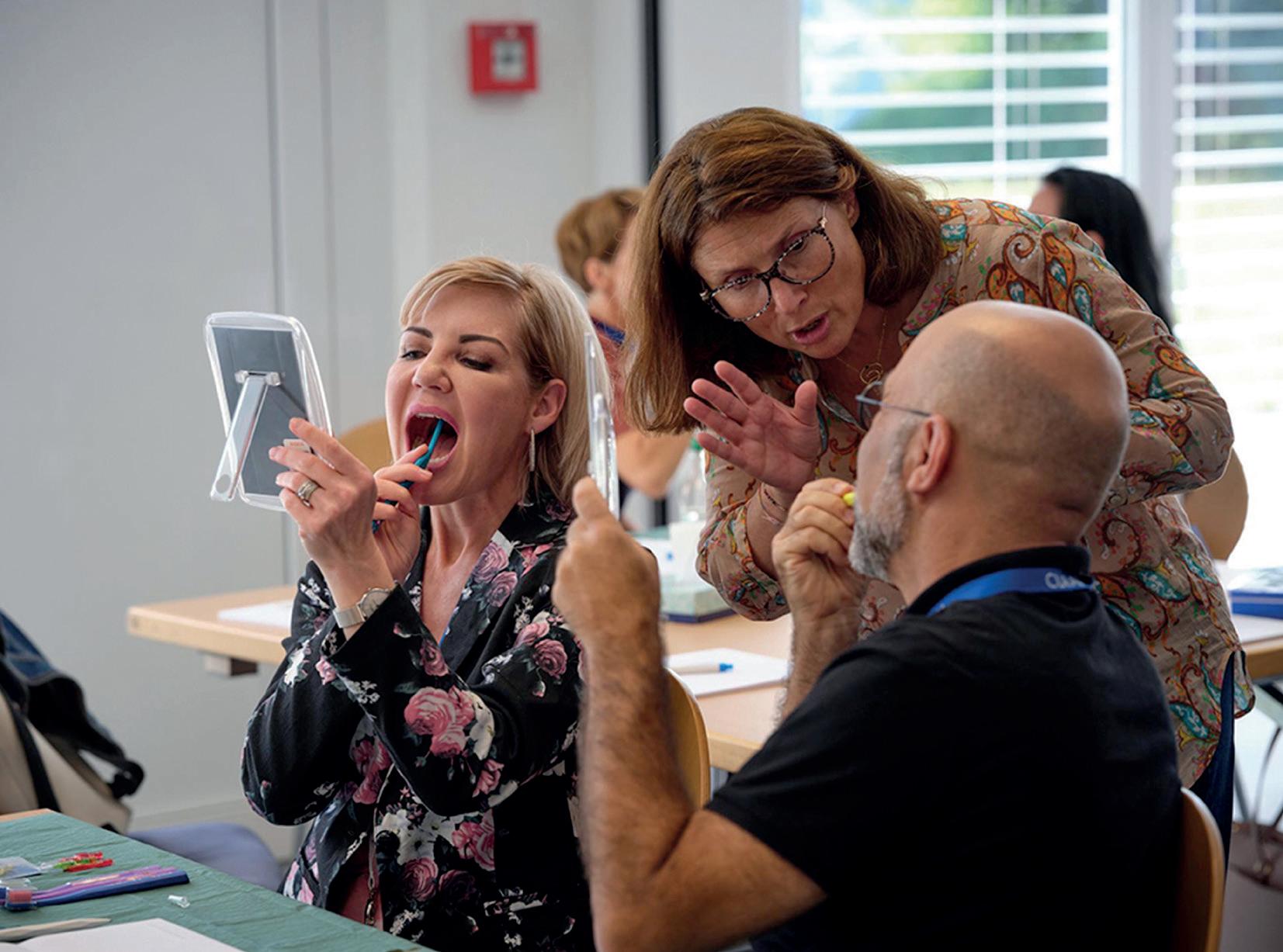
Learn, then teach
The iTOP programme is a unique opportunity for dental practitioners to enhance their understanding of oral prophylaxis, learning how best to educate their patients on correct brushing techniques.
Chrystal shares her experience:
“I completed the iTOP Introductory seminar in June 2024 and then the Advanced seminar four months later. It was an excellent experience that gave a unique insight into how to instruct, coach and guide my patients to master the skills necessary for effective biofilm management, ensuring each patient is achieving optimal oral hygiene when they are away from the clinic aiding in the creation of exceptional oral health habits and routines.
iTOP utilises a Touch2Teach element; we practise first so that we can better demonstrate correct brushing techniques to our patients. The hands-on approach puts the practitioners in the shoes of the patients. We often find that even though we are Dental Professionals we are not masters of the skill of correct toothbrushing.
“iTOP gave me a superior way of educating my patients, one that empowers them to be proactive with their oral health. Since then, I’ve seen the growth in my patients following the aftercare instructions throughout their journey creating consistent daily oral health habits they are adhering to, utilising products they genuinely love.
“What is remarkable about Curaprox’s mission is that it seeks to educate all on the value of consistent oral healthcare, not just dental professionals but the public too. From going into universities and teaching students to having ambassador events at family festivals, Curaprox considers every avenue to

teach people how best to combat oral disease for a healthier future. I look forward to continuing my partnership with Curaprox and elevating the quality of care for my patients.”
For more information about iTOP courses and to book your place on one, please visit The Curaden Academy website http://www.curadenacademy.com/
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk n

























But your recommendation can make a big difference.

Fluoride treatment will never be the same
When patients are more comfortable, they more likely to accept treatment, and dental appointments aren’t avoided.
A significant part of what makes the dental appointment appealing – or something to be anxious about – is the solutions used by the clinician. When patients are undergoing treatment that they’ve had before, such as topical fluoride application, their past encounters will no doubt change how they view their upcoming appointment.
Change the minds of those who have had bad experiences, or set the bar high for patients receiving topical fluoride treatment for the first time, when you choose the 3M™ Clinpro™ Clear Fluoride Treatment from Solventum, formerly 3M Health Care.

An exciting new formula
The feeling of a fluoride varnish on the dentition can be pleasant for some, and uncomfortable for others. The water-based, rosin-free formula of the 3M™ Clinpro™ Clear Fluoride Treatment is optimised for a simple application that glides smoothly onto the patient’s teeth. When used, 93.8% of patients judged 3M™ Clinpro™ Clear Fluoride Treatment to have a smooth mouthfeel,i which can make appointments more pleasant.
The water-based solution also aids the uptake of fluoride, helping key ingredients get to the tooth surface quicker to facilitate ionic exchange. There is no waiting for any rosins to release the fluoride ions – the minerals are right there, giving patients a shorter treatment time with a lower dosage for effective results. 3M™ Clinpro™ Clear Fluoride Treatment uses a 2.1% sodium fluoride solution, and needs a minimum contact time of just 15 minutes, encouraging your patients to say “yes”.
A taste of success
The tactile sensation of fluoride treatment isn’t the only factor affecting patient comfort – as with most solutions in dentistry, the taste needs to be enjoyable too!
The 3M™ Clinpro™ Clear Fluoride Treatment is available in three editions, including Mint, Watermelon, and Flavourless formulae. Studies have shown that children receiving topical fluoride varnishes have an increased chance of positive behaviour when they can choose the flavour of the solution.ii This sense of control can help paediatric patients have a successful time in the dental chair, with marked improvements for patients with a history of invasive dental procedures.ii
Another of the key benefits of the fast-acting water-based formula is that the taste and feeling of the 3M™ Clinpro™ Clear Fluoride Treatment barely
lasts longer than the appointment itself. Around 96% of patients couldn’t feel or taste the solution on their teeth just one hour after treatment, meaning they could go back to their day with little impact.i
Plus, other conventional fluoride varnishes may need patients to wait quite some time before eating and drinking to ensure that fluoride uptake is completely effective. This is no longer the case, as patients using this treatment can eat and drink to their heart’s delight just 15 minutes after application. In turn, fluoride treatment appointments can fit seamlessly into a day’s schedule, as patients go from dental practice to lunch without worrying about their dentition.
Simple in a clinician’s hand
As part of Solventum’s promise to support clinicians throughout all aspects of dental care, it is not enough to support optimal oral health – your workflows need to be predictable too.
The 3M™ Clinpro™ Clear Fluoride Treatment uses a unique press and go L-Pop™ single dose delivery system. It helps clinicians steadily produce the amount of solution required, before it glosses over the teeth in a fast and easy application.
Dental professionals can even dispense the formula onto a gloved hand, for application in a manner that is comfortable to them.

With an optimised delivery, and comfort for your patients, the 3M™ Clinpro™ Clear Fluoride Treatment from Solventum will change the way you support patients. Learn more by getting in touch today.
To learn more about Solventum, please visit https://www.solventum.com/en-gb/home/oral-care/ For more updates on trends, information and events follow us on Instagram at @solventumdentalUK and @solventumorthodonticsemea ©Solventum 2024. Solventum, the S logo and Clinpro are trademarks of Solventum and its affiliates. 3M is a trademark of 3M company.
References
i. 3M data on file.
ii. Karim, R., Splieth, C. H., & Schmoeckel, J. (2025). Effect of Choice of Flavor of Fluoride Varnish on Behavior in Dental Visits in Schoolchildren. Clinical and Experimental Dental Research, 11(1), e70069. n

About Solventum
Solventum, enabling better, smarter, safer healthcare to improve lives. As a new company with a long legacy of creating breakthrough solutions for our customers’ toughest challenges, we pioneer gamechanging innovations at the intersection of health, material and data science that change patients’ lives for the better while enabling healthcare professionals to perform at their best. Because people, and their wellbeing, are at the heart of every scientific advancement we pursue. We partner closely with the brightest minds in healthcare to ensure that every solution we create melds the latest technology with compassion and empathy. Because at Solventum, we never stop solving for you.
Touch a nerve
The human body is wired together with nerves, carrying electrical impulses that relay information to and from the brain. Nerves regulate our thoughts, memory, feelings and movements. However, a damaged or severed nerve can cause intense pain and discomfort, inhibiting the body’s ability to properly function.
In dentistry, implant treatments carry the risk of nerve damage, especially to the inferior alveolar nerve (IAN). A serious complication, IAN injury can cause increased sensitivity for the patient, undermining the success of the treatment and leading to further management. Dental practitioners must understand the aetiology, risk factors and management techniques of IAN injury to best lower the chances of it occurring and prevent long-term dysfunction.
Getting on somebody’s nerves
The inferior alveolar nerve is a branch of the trigeminal nerve and supplies sensory innervation to the chin, lower lip, gingivae, molars, premolars and alveolar bone – what is felt in and around the oral cavity is heavily influenced by it.i
During dental treatments, there are several causes of IAN injury. Extraction of the mandibular third molar is a notable cause, with a 0.4-13.4% incidence, i whilst the second molar region accounted for 64% of reported IAN injuries. ii
Inaccurate recognition of the IAN is reported as another frequent cause; the low bone density of the mandibular canal prevents it from appearing clearly on radiographs, leading to misjudgement on the location of the IAN and therefore a higher risk of damaging or severing it.ii
Whilst less common, local anaesthetic injections performed prior to treatment can cause direct or indirect damage to the nerve, causing compression injury. Other accidents during treatments that can damage the IAN include exposure of the inferior alveolar canal during surgery, drilling too deep, extensive use of surgical burs, and displaced tooth fragments.
Big risks and big impacts
Several risk factors are also worth highlighting. Research has found that older demographics are likelier to experience IAN injury, with an average age of 63. Secondly, women accounted for over 60% of reported cases and are therefore at a greater risk than men.ii The exact association is unclear but mandible size, changes in bone metabolism due to hormonal changes, and the development of osteoporosis (which can cause excessive resorption of the alveolar ridge following tooth extraction) can be offered as explanations.ii
In mild cases, IAN injury can be short-term and manageable. At its extreme, IAN injury has the potential for permanent disability. Its main symptoms include numbness, abnormal sensations or pain (pins and needles, tingling, burning, sharp pain), and increased sensitivity when touching the face.iii The impact of this can affect patients massively, interfering with eating and drinking, speech, kissing, applying makeup and shaving. Moreover, without the correct sensory information, patients may not feel tooth pain, leading to a higher risk of caries being undetected.
Manage and maintain
To best ensure patients have a smooth implant treatment with minimal risk to the IAN, dental practitioners should be meticulous with the diagnosis and identification of risk factors, including pre-existing disease and the close anatomic relationship between the tooth roots

and the inferior alveolar canal.iv Having CBCT scanners can achieve superior visibility levels of the mandibular canal, too.v
However, in the wake of an accident, a damaged nerve can be treated with physical therapy or by internal and external decompression, microsurgery and removal of the implant. A consistent dental care routine everyday can also help maintain the health of the IAN, ensuring that oral health is optimal with no gingivae resorption.vi
Nerves of steel
Delivering successful implant treatments is vital for patients to eat, speak and smile with confidence. To stay up to date on the latest developments, consider a membership with the Association of Dental Implantology (ADI). With over 2,000 members, the community is open to all dental professionals, from students to senior clinicians. Offering a vast range of educational resources, superb networking opportunities and discounted services, a membership with the ADI takes your implant treatments to the next level.
The inferior alveolar nerve is integral for oral health and damage to it during treatment can have a huge impact on the patient’s quality of life. However, having a heightened awareness of its risk factors and knowing the best ways to avoid surgical accidents means dental practitioners can provide long-lasting implant treatments that satisfy the patient.
For more information about the ADI, visit: www.adi.org.uk
References
i. Kwon, G. and Hohman, M.H. (2023). Inferior Alveolar Nerve and Lingual Nerve Injury. [online] PubMed. Available at: https://www.ncbi.nlm.nih. gov/books/NBK589668/.
ii. Han, J. and Han, J.J. (2024). Risk factors for inferior alveolar nerve injury associated with implant surgery: An observational study. Journal of Dental

Sciences. [online] doi:https://doi.org/10.1016/j. jds.2024.07.025.
iii. The University of Sheffield. (2020). For you the patient. [online] Available at: https:// www.sheffield.ac.uk/dentalschool/research/ integrated-bioscience/trigeminal-nerve-repair/ you-patient.
iv. Di Nardo, D. (2017). In vitro resistance to fracture of two nickel-titanium rotary instruments made with different thermal treatments. Annali di stomatologia, 8(2), p.53. doi:https://doi.org/10.11138/ ads/2017.8.2.053.
v. Karameh, R., Abu-Ta’a, M.F. and Beshtawi, K.R. (2023). Identification of the inferior alveolar canal using cone-beam computed tomography vs. panoramic radiography: a retrospective comparative study. BMC Oral Health, 23(1). doi:https://doi.org/10.1186/s12903-023-03176-8. vi. www.colgate.com. (n.d.). Inferior Alveolar Nerve (IAN): Causes & Symptoms. [online] Available at: https://www.colgate.com/en-us/oral-health/ mouth-and-teeth-anatomy/inferior-alveolarnerve-ian-causes-symptoms#. n
ABOUT THE AUTHOR
DR ZAKI KANAAN ADI PRESIDENT

Dr Zaki qualified from Guy’s Hospital, London, in 1996. His main interests lie in all aspects of Cosmetic Dentistry with a special interest in Dental Implant Treatment, where he has achieved a Master’s Degree from the GKT Dental Institute in 2001.
Moving towards a greener future with digital workflows Away with the fairies
Innovation and exceptional patient care have always been the cornerstone of successful dental practices. In a world that continues to evolve digitally in the pursuit of more convenient service, this is the perfect moment for practices to embrace more efficient workflows. While the benefits of cloud-based practice management systems are often celebrated for improving organisation, their role in advancing environmental sustainability and driving costs down are just as crucial – and frequently overlooked.


Beyond
paper reduction: A greener approach to practice management
In the UK alone, households discard enough paper each year to account for the loss of six trees.i But in dental practices, the impact of paper-based systems goes far beyond deforestation. These traditional methods contribute to higher energy consumption, the need for physical storage space and increased transport requirements – all of which contribute towards inflating the carbon footprint of a practice.
Digital practice management solutions offer an ecofriendly and cost-effective alternative. Cloud-based systems tackle these challenges head-on, delivering a host of environmental and operational benefits, including:
• Reducing energy consumption by eliminating the need for bulky, outdated servers that consume excessive power and require cooling.
• Cutting the need for printing, storing and transporting vast amounts of paperwork, which not only saves trees but also reduces waste and emissions.
• Freeing up valuable physical space in practices and admin areas.
• Minimising travel for document delivery and physical system maintenance.
A recent case studyii illustrates this transformation. Within just 12 months, a dental practice using a cloud-based solution eliminated the need to print more than 180,000 pieces of paper – saving 18.5 trees, £1,095 in paper costs and £2,822 in printing expenses. This shift from paper to digital represents more than just operational efficiency; it is a tangible step toward reducing environmental impact and lowering unnecessary costs.
Aligning with modern patient expectations
Today’s patients expect seamless digital experiences in every aspect of their lives – from banking to shopping and, of course, healthcare. They want the same digital convenience from their dental providers as they receive from their online shopping experience. By offering online appointment confirmations, electronic forms and cloud-accessible patient records, practices meet these expectations while making the patient journey smoother and more sustainable in return.
Digital workflows enable patients to complete their medical history forms from the comfort of their homes or on in-practice tablets, reducing paperwork
and time that can be better spent reviewing oral hygiene advice provided by the practice. Treatment plans and invoices can all be shared electronically, cutting waste and fostering clearer communication between patients and dental teams. It also allows forms to be easily accessed by both patient and clinician for review, without delving into paperwork stored in office spaces.
In all, this not only enhances patient satisfaction but also promotes a more sustainable and cleaner way of delivering care.
Smarter workflows and stronger teams
For dental professionals, digital solutions offer speedier access to patient information and more consistent communication within the internal team. Practices operating in the cloud face fewer disruptions from hardware failures and can implement system updates seamlessly.
The importance of speed is also seen in the marginal gains throughout the day. Quicker, simpler access to patient information and treatment plans means individuals spend less time in the dental chair, for more efficient appointments – clinicians can in turn see more people throughout the day, supporting a wider community.
Laying the groundwork for net zero
By embracing digital workflows today, dental practices are positioning themselves as leaders in sustainability for tomorrow. Cloud-based systems facilitate easier upgrades, scalability without the burden of physical infrastructure, and integration with emerging technologies that align with net-zero objectives.
Sensei Cloud: empowering smarter, more sustainable service
When it comes to ensuring reliability, security and efficiency, choosing the right technology partner is paramount. Sensei Cloud from Sensei, the practice and patient management brand of Carestream Dental, empowers dental teams to work more efficiently with a solution they can trust. With secure cloud hosting, intuitive workflows and remote accessibility, Sensei Cloud supports practices in delivering exceptional patient care while also making a positive impact on the environment.
Digital practice management solutions offer exceptional benefits to any modern dental practice. From in-house efficiency to greener outcomes, its essential that clinicians consider upgrading to a cloud-based system to make the most of each practice’s potential.
To learn more about how Sensei Cloud can help your practice thrive, visit gosensei.co.uk.
For the latest updates, follow us on Facebook and Instagram @carestreamdental.uk. n
References available upon request
ABOUT THE AUTHOR
CLAIRE MCCARTHY


Along with Santa Clause and the Easter Bunny, the Tooth Fairy is an emblem of a child’s imagination, helping to guide them through the younger years by explaining why their teeth are starting to wobble, and the reward they may receive when it falls out. This can be a coin or a figurine, a booklet or just a nice note thanking the child.
Educating children on the importance of looking after the teeth and gingivae is vital, setting them up for a proactive future where consistent daily oral hygiene lowers the risk of oral disease. Encouraging parents and guardians to maintain the Tooth Fairy tale can increase a child’s engagement with looking after their teeth.

Fantasy meets reality
To help paediatric patients better understand the long-term value of toothbrushing, Curaprox has launched the Tooth Fairy Gift Set, combining the iconic appeal of the fantasy character with first-class oral hygiene products.
Chief among these is the Curaprox Kids Toothbrush. Available in six dazzling colours – blue, pink, green, purple, red, orange – the toothbrush is visually enticing, helping to reduce any anxieties or discomfort that some paediatric patients may have. Suitable for children aged 4-12, the toothbrush contains 5,500 super-soft filaments. These are gentle on the teeth and gingivae whilst effectively removing plaque to protect the emerging secondary teeth.
The Kids Toothbrush is designed for optimal handling and efficiency. The octagonal handle comfortably sits in both smaller and larger hands, should the parent/guardian need to assist. The angled head also ensures excellent control and better access to the tooth surfaces, aiding children in honing the correct toothbrushing technique.

Claire McCarthy is Senior Director of Program & Process Excellence at Carestream Dental.
Fruity flavour
A great toothbrush needs a great toothpaste, and the Tooth Fairy Gift Set contains a Curaprox Kids Watermelon Toothpaste. It contains 1,450ppm fluoride, providing a daily defence against cavities and keeping the enamel and gingivae strong and healthy.
Whilst mint toothpastes may be too intense for children, the Kids Watermelon Toothpaste brings the cool taste of summer to every brush time. With its fruity punch, compliance will increase. Furthermore, no harmful ingredients are used to achieve the pleasant taste, with enzymes, fluoride, sorbitol and a dash of xylitol all working together to strengthen the teeth and prevent the spread of oral diseases.
Unique resources
What makes the Tooth Fairy Gift Set unique is the array of resources it provides to boost understanding and toothbrushing performance. This includes a five-step guide to cleaning teeth and a tooth loss chart to increase children’s interest in their oral health. The latter uses a simple diagram for children to work out which tooth they may have just lost, then they can mark the date. Despite its simplicity, the chart can improve children’s understanding of their own dental anatomy. Supporting this further is the series of five information videos that the child receives every 10 weeks directly from the Tooth Fairy and her helpers; professional dental hygienists. These give helpful hints and tips on how and why it is important to maintain good oral hygiene habits.
For interacting with the Tooth Fairy, the set comes with a fun hanging sign that can be placed on the bedroom door handle. A sleek tooth pouch is included for children to hold their lost tooth and tuck under the pillow.
A helping hand
To support the parents/ guardians, the Tooth Fairy Gift Set contains special envelopes, notes and tooth receipts. These add to the excitement the following morning, with children able to open the envelope and read the note from the Tooth Fairy.
As a bonus, the parents/ guardians receive a discount code for the CS 5460 Triple Pack of toothbrushes. This enables them to join their child in harnessing the excellent cleaning power of Curaprox products.
The Tooth Fairy Gift Set is lovingly designed
to appeal to children, stimulating their imagination whilst increasing their interest in looking after their oral health. Through careful education and the reliable oral hygiene products from Curaprox, the next generation can be more compliant and proactive in their self-care from a young age, setting them up for a healthier future.
To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit www.curaprox. co.uk and www.curaden.co.uk n




























Ideal for children & compromisedpatients












Prevora: advancing preventive care for high-risk patients
Dr Ben Atkins explores how Prevora modulates the biofilm, reviews the supporting evidence, and shows how tangible clinical success can re-engage high-risk patients with their oral health
The aim of this article is to give dental professionals an evidence-based understanding of oral dysbiosis and its role in caries and periodontal disease. It will also explore how Prevora can help manage dysbiosis and prevent caries in high-risk patients, while supporting sustained patient engagement in long-term oral health.
On completing this Enhanced CPD session, the reader will be able to:
• Explain the role of oral biofilm and dysbiosis in the development of caries and periodontal disease
• Describe the mechanism of action and application process of Prevora
• Summarise the evidence base supporting Prevora’s efficacy and safety in high-risk groups
• Identify which patient groups are most likely to benefit from Prevora treatment
• Discuss how preventive interventions such as Prevora can support patient motivation and engagement
Learning Outcomes: A,B,C,D
Dental caries and periodontal disease are among the most common chronic conditions worldwide. 1 Despite decades of progress in oral hygiene education and the widespread use of fluoride, many patients continue to experience preventable disease progression. For these individuals, conventional advice to brush and clean interdentally is often insufficient. 2
A key driver of this unmet need is oral dysbiosis, defined as an imbalance between pathogenic and commensal bacteria within the oral biofilm. Oral dysbiosis contributes to both caries and periodontal disease, with poor oral health increasingly recognised as a factor in wider systemic health, including diabetes, cardiovascular disease and cognitive decline.3
Prevora for high-risk patients
Prevora is a professionally applied, high-concentration (10%) chlorhexidine formulation combined with a protective sealant. Delivered in a two-stage process, it is first applied to all tooth surfaces where the chlorhexidine binds strongly to dental hard tissues, followed by a sealant layer that locks the active agent in place. Chlorhexidine reduces the harmful bacteria that cause oral dysbiosis, allowing healthy commensal bacteria to recolonise. This reduces the build-up of plaque that can lead to the development of caries and gum disease.
This simple paint-on procedure takes around 10 minutes and can be carried out by dental hygienists, dental therapists or dental nurses working under appropriate supervision. No specialist equipment is required, and the treatment can be delivered in both dental surgeries and nondental settings such as care homes.
Unlike mouth rinses or gels, which provide only short-term exposure to chlorhexidine, Prevora creates a slow-release reservoir. This ensures sustained antibacterial activity against cariogenic and periodontopathogenic bacteria, with long-

lasting substantivity. Importantly, Prevora has not been associated with the staining commonly seen with lower concentration rinses.
Evidence base and clinical experience
The effectiveness of Prevora is supported by more than 20 years of clinical research and real-world use in Canada and Europe. Two large randomised, placebo-controlled trials support Prevora’s efficacy in preventing caries in high-risk patients. In a study of 983 community-dwelling adults at risk of caries, Prevora significantly reduced the incidence of coronal caries over 13 months compared with placebo. The protective effect was greatest in high-risk individuals.4
A second trial, focusing on 236 adults with oral dryness related to polypharmacy, also reported significant reductions in new lesions.5 Smaller observational studies have investigated the role of Prevora in periodontal management. Findings include reductions in bleeding on probing, reduced gingival inflammation, and a decreased need for surgical intervention in chronic periodontitis.6 More recently, a randomised community trial demonstrated feasibility and benefits in elderly care-home residents, as well as those living independently.7
Real-world use in UK practice has also illustrated these benefits. At Trinity House Dental Care, for example, high-risk patients reported reductions in bleeding and sensitivity within weeks of treatment,
alongside less plaque accumulation. Most patients chose to continue with regular applications as part of their hygiene care, reflecting how clinical improvement and patient experience work together to reinforce the value of prevention.
Patient selection and clinical integration
Prevora is indicated in high-risk adults for the prevention of tooth decay. High-risk patients include those with:
• Diabetes or other systemic conditions with known oral health links
• A history of caries
• Oral dryness from polypharmacy, radiotherapy or menopause
• Early periodontal disease with bleeding on probing
• Peri-implant inflammation
• Frailty, care-home residence or reduced motor skills
• Low tolerance for invasive care or dental anxiety
• Planned aesthetic or restorative treatments requiring optimal oral health.
This represents a significant proportion of the UK population and highlights the scale of opportunity for preventive intervention. Recognising this potential positions Prevora as a practical option that can easily be integrated into mainstream dental care, with delivery possible as part of a routine hygiene appointment or as a standalone preventive intervention.
The Prevora application schedule is based on clinical need. Those with milder-to-moderate disease may receive two to four applications per year, while patients with more advanced disease may benefit from more frequent sessions initially, before moving to maintenance intervals.

Supporting
patient motivation
The potential for Prevora to generate behaviour change is considerable. Many high-risk patients fail to maintain consistent oral hygiene routines because of discomfort on brushing or because improvements are not immediately apparent. In contrast, Prevora often produces tangible
CPD Questions
1. How does Prevora differ from conventional chlorhexidine rinses?
A. It is a high-concentration formulation that provides a slow-release antibacterial reservoir on tooth surfaces
B. It requires patient daily use to be effective
C. It delivers only short-term antibacterial activity
D. It is applied in a single-stage process identical to a fluoride varnish
2. Which of the following patients would NOT typically be considered a candidate for Prevora?
A. A patient with oral dryness due to polypharmacy
B. A patient with early periodontal disease and bleeding on probing
C. A healthy adult with excellent oral hygiene and no history of oral disease
D. A patient with diabetes and recurrent caries
3. What evidence supports Prevora’s efficacy in reducing dental caries?
A. Case reports of two patients with improved outcomes
B. A single observational trial without controls
C. Two large randomised controlled trials showing reduced incidence of caries in high-risk adults
D. No published evidence to date
4. How can Prevora support patient motivation and engagement?
A. By providing patients with immediate cosmetic whitening
B. By producing measurable improvements such as reduced bleeding and pain
C. By eliminating the need for all oral hygiene practices
D. By guaranteeing no further disease progression
changes such as reduced bleeding, improved comfort or a cleaner sensation.
These early, meaningful changes matter because behaviour is rarely shaped by abstract risk information alone. Patients who repeatedly fail to see results from conventional advice may disengage, assuming their efforts will not pay off. By delivering measurable improvements that patients can feel, Prevora provides positive reinforcement that sustains motivation. This aligns with behavioural science, where ‘small wins’ build confidence and encourage patients to adopt healthier routines over time.
In clinical practice, this dual benefit is especially valuable for groups with entrenched disease patterns or low compliance. By helping patients feel and see improvement, Prevora supports longer-term adherence to preventive regimens.
Wider implications for practice and healthcare
The introduction of Prevora to UK dentistry has broader implications beyond individual patient care.
For practices, it represents a commercially viable preventive service that can optimise use of the whole clinical team, enhance patient loyalty, and generate responsible revenue.
For the healthcare system, interventions that reduce the burden of caries and periodontal disease in high-risk populations can contribute to easing demand on NHS dental and medical services. Preventing disease progression reduces the need for invasive procedures, emergency treatment and hospital-based care.
On a wider scale, improving oral health in vulnerable groups supports better systemic
health, aligning with national strategies to reduce health inequalities and shift the focus from treatment to prevention.
Prevention with purpose
Prevora offers dental professionals an evidence-based option for managing oral dysbiosis in high-risk patients. By combining a sustained antibacterial effect with positive reinforcement for patient behaviour, it supports both clinical outcomes and long-term engagement.
For the dental team, integrating Prevora into preventive pathways provides a practical means of reducing disease burden, improving patient experience, and contributing to wider public health goals.
Taken together, the evidence and clinical experience show that Prevora is a novel, evidencebased preventive solution that can be confidently integrated into routine care. n
References available upon request

Maintaining anterior composite restorations: a clinical perspective
Dr Teki Sowdani explains why the maintenance of anterior composite restorations is central to prevention, and how Guided Biofilm Therapy (GBT) offers a safe and effective solutio n
The aim of this article is to highlight the importance of maintaining anterior composite restorations and to outline a predictable protocol, including Guided Biofilm Therapy (GBT), that supports longterm success through preventive care.
On completing this Enhanced CPD session, the reader will:
• Recognise why maintenance is essential for the long-term success of anterior composite restorations
• Identify common challenges faced by clinicians, hygienists and therapists in maintaining composite bonding
• Understand the risks of using inappropriate powders, instruments and pastes, and how Relative Dentine Abrasivity (RDA) affects restoration safety
• Be able to apply a step-by-step maintenance protocol using Guided Biofilm Therapy (GBT) to protect composite restorations
• Appreciate how effective maintenance supports preventive care, builds patient trust and creates professional opportunities.
Learning Outcomes: A,B,C,D
It’s no secret that I love composite bonding. It has transformed both the way I smile as a patient and the way I work as a clinician. After completing more than 6,000 cases over a 10-year period, I’ve learned that successful composite bonding is not just about the treatment itself. Long-term success depends on the right after-care and maintenance. To deliver this properly, I need the full dental team on board, including hygienists and therapists.
So why has composite bonding suddenly become so popular? As dental professionals, we know it’s been around for years, yet statistics show that around a third of adults in the UK are unhappy with their smile.1 Traditionally, there were barriers to treatment that prevented many from achieving the confidence they were looking for, and composite bonding has helped break down these barriers.
Many patients are nervous about going to the dentist, so invasive procedures such as porcelain veneers, which involve tooth reduction and local anaesthetic, can be off-putting. Composite bonding is an ideal option for these patients because it doesn’t require local anaesthesia.
In the current UK climate, cost is another important factor in decision-making. Composite bonding is more affordable than many alternatives, making it a realistic entry point for patients seeking treatment.
Want or need?
In my early years, most composite bonding cases were carried out because the patient genuinely needed restorations, rather than seeking them for cosmetic reasons. Composite bonding is often associated with aesthetics, but, in day-to-day practice, it’s just as likely to be provided for patients with tooth surface loss caused by grinding or over-brushing.
Whatever the reason for treatment, maintenance is crucial. From my own experience, I know that the long-term success of composite bonding depends on how well it is maintained after placement.
What can we control?
Many of the treatments we provide now rely heavily on patient compliance. As clinicians, we do everything we can, but, ultimately, we cannot control patient behaviour. The long-term success of composite bonding, including how well it lasts and looks, will always come down to how the patient cares for it.
That does not mean we have a small role to play. Quite the opposite. It is frustrating when I hear colleagues steer patients towards alternatives such as porcelain veneers without first giving them an appropriate maintenance and care plan for their composite bonding.
We have a duty of care not only to provide the treatment to the best of our ability, but also to ensure patients have the tools and guidance to look after their restorations. Failing to do so is not just poor practice. It could even create medicolegal problems.
What’s it all about?
Composite veneer, edge bonding, composite bonding. These terms are often used with patients to describe how much composite resin is being placed and where on the tooth. When it comes to maintenance, however, it is all the same material and the same oral environment.

One of the main advantages of composite resin is its versatility. It can be placed over the entire surface of a tooth, as in a composite veneer. It can be used just on the edges of teeth, often referred to as edge bonding. It can also be placed on the buccal surface, for example in a Class V cavity.
Our responsibility as clinicians, once the restoration has been placed, is to ensure the surrounding oral tissues remain healthy and that the restoration continues to look its best, especially in the patient’s smile line.
For a deeper dive into these concepts, Dr Teki Sowdani will be presenting alongside Claire Berry at the GBT Summit London 2025. Their joint session will explore the evolving role of hygienists and therapists, with practical strategies for clinical impact and patient care.
Date and time: Friday 31 October 2025, 8:30am – 5:00pm GMT
Location: Royal College of Physicians, London
Tickets are limited so be sure to secure your place without delay at tinyurl.com/ GBTLondonSummit2025
What are the challenges?
Many of my patients who came for composite bonding already had their own dentist and hygienist. Once the bonding was complete, they would usually return to those professionals for their maintenance. Over the years, I began to notice how much the after-care varied.
It became clear to me that there was a gap in the education of some dentists, hygienists and therapists when it came to maintaining composite bonding. Whenever I saw a patient years after I had completed their bonding, they often told me their hygienist avoided cleaning around the composite for fear of damaging it. Others did attempt to clean around it, but, on closer inspection, I could see damage to the composite caused by the instruments or techniques used.
This was not necessarily their fault. They were doing their job of maintaining the patient’s overall oral health. I even noticed the same issue among hygienists within my own practice.
What not to do
These challenges often stem from uncertainty about what should and should not be done during maintenance. Composite resin can be prone to micro-scratching, which may lead to chipping and an increased risk of staining. To prevent this, clinicians should avoid using products that are abrasive to composite bonding.
Powder therapy is becoming more popular, but choosing the wrong powder can cause unintended damage to restorations. Incorrect use of hand instruments or ultrasonic scalers can also harm the surface.
Abrasive polishing pastes should not be used on composite. The abrasiveness of a paste is measured by its Relative Dentine Abrasivity (RDA). The lower the RDA, the safer it is for composite restorations.
Choosing not to clean around composites at all, due to uncertainty or lack of knowledge, is also not advisable. Patients still need effective maintenance, using the correct techniques and materials.
Finding the best solution
After seeing so much variation in how colleagues approached maintenance, I wanted to find a reliable and predictable way to protect composites without risking damage. The Guided Biofilm Therapy (GBT) protocol has proven to be the most effective solution to these challenges.
Here is my composite maintenance protocol, adapted from the EMS GBT approach:
1. Assessment – alongside a general periodontal examination, I specifically check whether any composite is causing gingival inflammation or if there are ledges that could lead to plaque retention
2. Disclose – this step is essential, as composite is usually well blended with the tooth surface and imperfections may not be easily visible without disclosure
3. Repair composite (if required) – If there is bleeding during prophylaxis, moisture control becomes difficult, so I repair any composite before moving on
4. GBT protocol using Plus powder only – I use 14 µm erythritol powder, which is safe for composite. It does not cause micro-scratching but is highly effective for removing biofilm and stain
5. Polish composite – I use polishing discs, rubber

CPD Questions
1. What factor ultimately decides how long composite bonding will last?
a) The choice of composite material
b) The patient’s behaviour and how well they care for it c) The use of local anaesthetic during treatment d) The durability of polishing discs used
2. What is one of the main advantages of composite resin?
a) It requires less training to place b) It is generally more affordable than porcelain veneers c) It can be used all over the tooth in different ways d) It does not require polishing
3. How is the abrasiveness of a polishing paste measured?
a) Relative Dentine Abrasivity (RDA)
b) Relative Enamel Abrasivity (REA)
c) Pellicle Cleaning Ratio (PCR)
d) Profilometry (PM)
4. What is the main advantage of using Guided Biofilm Therapy (GBT) for patients with composite restorations?
a) It allows the use of any powder safely
b) It provides a reliable and predictable way to protect composites without causing damage c) It eliminates the need for periodontal examinations d) It means restorations never require polishing
5. What can a strong understanding of composite maintenance offer dental professionals?
a) It sets them apart as clinicians b) It helps build patient loyalty c) It creates new professional opportunities d) All of the above
wheels and a composite polishing paste to leave a smooth, glossy surface
6. AirFoam – I avoid giving patients mouthwash with added colourings immediately after GBT. EMS AirFoam leaves a fresh taste and helps remineralise the teeth
7. Whitening gel – for patients with retainers, I recommend using whitening gel the same evening to reach interproximal areas. I advise 16% carbamide peroxide for two nights
8. Toothpaste – I recommend a toothpaste with a low RDA to reduce the risk of surface damage to composite.
I usually recommend patients attend for a combined GBT and composite maintenance appointment twice a year, unless they need more frequent visits due to periodontal issues.
What opportunities does this create?
A strong understanding of how to maintain composite restorations can really set you apart as a clinician. Patients who have invested in their smile want their composites to last as long as possible, and they will be loyal to professionals who can help them achieve that.
For dental therapists in particular, providing highquality maintenance creates new opportunities. It can spark further interest in restorative dentistry and may even inspire them to learn how to carry out anterior composite bonding themselves.
By taking maintenance seriously, we not only protect our patients’ smiles but also build trust, reputation and long-term professional satisfaction.
Reference
1. 200+ Dental Industry Statistics for 2024. FollowApp.Care 2024. Available at: https://www. followapp.care/200-dental-industry-statisticsfor-2024/. Accessed September 2025
ABOUT THE AUTHOR
DR TEKI SOWDANI

The Role of Powder Therapy and Ultrasonics in Implant Supportive Care
Jenny Walker Dip DH/DT and Kathryn Mayo DipDH, FAETC
This CPD article discusses methods for preventing and treating peri-implant diseases, as well as the role of powder therapy and ultrasonics in implant supportive care
Learning aims and objectives
• To identify the factors that lead to peri-implant disease
• To recognise the two main types of peri-implant disease
• To explain the role of powder therapy in implant maintenance.
Learning Outcomes: C
Peri-implant disease: prevalence and susceptibility
Despite the reported high success rate of dental implants, it is estimated that approximately one in five implants fail, and around 43% of patients develop peri-implant mucositis. (Berglundh et al., 2019). Effective biofilm management, both professionally and at home, is crucial for preventing peri-implant diseases. Berglundh et al. (2019) also states that the soft tissues around dental implants respond to microbial biofilm in a similar way to gingival and periodontal tissues, underlining the importance of biofilm management as the foundation of implant care.
Understanding peri-implant disease
Peri-implant disease is multifactorial, and although the soft tissue response is like that of gingival tissues, peri-implant tissues exhibit increased susceptibility to bacterial challenges due to biological, histological, and morphological differences compared to natural teeth. Moreover, Herrera et al. (2023) explained that these differences necessitate a different approach when monitoring and planning supportive care. Current guidelines indicate that the main risk factors for the development of peri-implant disease are:
• A history of periodontitis
• Poor oral hygiene
• Irregular attendance for maintenance care. Other proposed risk factors, such as tobacco use and systemic diseases, are documented but require more substantial evidence before confirming their role.
The 2017 World Workshop Classification identifies two primary peri-implant related diseases:
• Peri-implant mucositis – a reversible inflammatory condition of the peri-implant mucosa characterised by bleeding on probing and erythema without bone loss.
• Peri-implantitis – a biofilm-associated pathological condition involving inflammation of the peri-implant mucosa and progressive bone loss beyond initial remodelling.
Importantly, it is widely accepted that perimucositis is a precursor to peri-implantitis.
Early detection and intervention
With this in mind, early detection of periimplant disease is crucial, as failure to spot

NSK’s Varios Combi Pro2 is an example of a combined ultrasonic and powder therapy device for supra and sub-gingival treatment
early signs of disease may lead to irreversible bone loss. Treatment and prevention of peri-implant diseases - The EFP S3 level Clinical Practice Guideline emphasises that the detection and treatment of peri-implant mucositis are key strategies for preventing peri-implantitis. (Herrera et al., 2023)
Dental hygienists and dental therapists play a central role in monitoring implants and delivering early, personalised interventions that prevent disease onset.
Preventing peri-implant disease
The principles of prevention focus on biofilm management around implants. Effective removal of plaque biofilm is often complicated by the challenging morphology of implant restorations, especially in patients with multi-unit prostheses, where access for both patients and professionals can be difficult.
Plaque and biofilm removal
Powder therapy combines water, compressed air, and powders to deliver a minimally invasive and comfortable method for disrupting biofilm. In clinical practice, only soft, small micron-sized powders are recommended for use around implants. This approach enables efficient supraand subgingival biofilm removal, while, if used with the correct techniques, minimises trauma to the surrounding soft tissues and prevents unnecessary surface changes to the implant.
Powder therapy devices include portable units for supra- and subgingival use, which attach to the dental cart or bracket table, as well as combined ultrasonic and powder therapy

systems. These standalone combination units provide flexibility, with separate powder chambers to prevent clogging. They also allow greater control of settings, and with advances in technology, many modern units are equipped with a warm water feature that enhances delivery and further improves patient comfort. The NSK Varios Combi Pro2 system is an example of a device that supports this combined approach, exhibiting the specific characteristics mentioned.
The role of ultrasonic tips
Ultrasonic instrumentation is an option for use in implant supportive care, particularly when peri-implantitis is diagnosed and debridement of implant surfaces is required. The S3 level guidelines recommend that all patients diagnosed with peri-implantitis have one round of nonsurgical therapy. (Herrera et al., 2023)
There are a plethora of modern ultrasonic tips that can be used on implants, including thin PEEKcoated tips indicated for use in peri-mucositis cases as a single mode of instrumentation, as well as thin, delicate stainless-steel options, for peri-implantitis treatment. They are often designed with angles, rather than being straight, a long terminal shank and a short toe. These allow for gentle, controlled debridement in areas where access may be challenging, and they lend themselves well to the shape of the implant surface, ensuring effective cleaning with minimal risk of surface changes. When using ultrasonic instrumentation, it should always be applied at a low power setting to minimise invasiveness.
Supportive peri-implant care (SPIC)
For patients with dental implants, regular monitoring and supportive care delivered by a trained and competent team are essential. This ensures early detection of disease, timely intervention when disease is detected and should promote longevity. Regular reviews should highlight the role of supportive care in preventing peri-implant disease, encouraging patients to maintain high standards of home care while attending scheduled maintenance appointments. It is the responsibility of the entire dental team to promote regular attendance and deliver highquality implant-supportive care. By working collaboratively, the team ensures patient comfort, encourages compliance, and supports long-term implant success.
Conclusion
The latest advances in powder therapy and ultrasonic technology enhance biofilm management, playing a central role in a modern, preventative approach to implant maintenance. Successful implant outcomes depend on:
• Early detection of disease
• Effective biofilm management at home and professionally
• Patient comfort, which should lead to increased compliance
• Regular supportive care by a skilled dental team While retention of natural teeth, where possible, should always be a priority, dental implants offer a solution for missing teeth, which can significantly enhance a patient’s quality of life. Still, implant longevity relies on a structured program of SPIC, excellent home biofilm management, and the effective use of minimally invasive technologies, such as powder therapy, amongst other instrument options, for maintaining a healthy microbiome.
CPD Questions
1. Biofilm-induced peri-implant mucositis is a reversible condition:
a. True
b. False
2. PMPR stands for:
a. Preventive mechanical plaque removal
b. Periodontal maintenance plaque removal
c. Professional mechanical plaque removal
d. Periodontal mechanised plaque removal
3. Peri-implant mucositis and peri-implantitis are:
a. Plaque-biofilm associated conditions
b. Infectious gum diseases
c. Not caused by plaque or biofilms
d. Related to blood disorders
4. PMPR can be performed:
a. On natural teeth
b. On dental implants
c. Supra and sub-gingivally
d. All of the above
References
• Berglundh, T., Armitage, G., Araujo, M. G., Avila-Ortiz, G., Blanco, J., Camargo, P. M., ... & Zitzmann, N. (2019). Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. Journal of Clinical Periodontology, 46(Suppl 20), S286–S291. https://doi. org/10.1111/jcpe.13157
• Herrera, D., Tord Berglundh, Schwarz, F., Chapple, C., Jepsen, S., Sculean, A., Kebschull, M., Papapanou, P.N., Tonetti, M.S. and Sanz, M.
ABOUT THE AUTHORS
JENNY WALKER
DIP DH/DT AND

Jenny Walker qualified as a dental therapist from Leeds Dental Institute in 2015. Her clinical experience at a peri-implant disease referral centre in the Northwest inspired a special interest in the management of peri-implant disease and periodontitis. Jenny is a former BSP Early Career Group representative for dental therapists and hygienists (2019–2020) and has contributed to the BSP adolopment of the S3 guidelines on stages I–IV periodontitis and peri-implant disease prevention.
Kathryn Mayo graduated from the Leeds Dental Institute in 1993 and subsequently completed a teaching qualification, holding an early teaching post at the institute. Over the past 30 years, she has gained extensive experience across various dental settings and now works in private practice,
(2023). Prevention and treatment of peri-implant diseases—The EFP S3 level clinical practice guideline. Journal of Clinical Periodontology, 50(26). doi:https://doi.org/10.1111/jcpe.13823.
• Caton, J.G., Armitage, G., Berglundh, T., Chapple, I.L.C., Jepsen, S., Kornman, K.S., Mealey, B.L., Papapanou, P.N., Sanz, M. and Tonetti, M.S. (2018). A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. Journal of Clinical Periodontology, [online] 45(s20), pp.S1–S8. doi:https://doi.org/10.1111/jcpe.12935. n
KATHRYN MAYO DIPDH, FAETC

while also serving as a clinical supervisor. She runs an implant maintenance clinic for undergraduate students on the BSc programme at the University of Manchester, delivered at the ICE Postgraduate Dental Institute and Hospital. Kathryn has also played an active role in the BSP working group panels for the adolopment of the S3 guidelines on stage IV periodontitis and periimplant disease prevention. Together, Jenny and Kathryn share a strong professional interest in implant supportive care and periodontitis, and they have presented widely across the UK and Ireland on these subjects. Both Jenny and Kathryn are active members of NSK’s Ikigai Educator team.
The Dental Awards Winners’ Presentation
On Friday 27th June, the winners of the 2025 Dental Awards gathered in London to receive their trophies and celebrate their victories along with members of the judging panel and sponsors
Following the virtual presentation that streamed in May on The Probe website and Youtube channel, the winners of the 2025 Dental Awards were invited to a celebratory awards lunch to be presented with their trophies in person.
The terrace of Doggett’s Coat and Badge, overlooking Blackfriars Bridge, set the scene perfectly. The weather was kind, the sun shining

down as the best in British dentistry celebrated in style while overlooking the Thames.
After guests were greeted with a champagne reception, Dr Nigel Carter OBE, Chief Executive of the Oral Health Foundation, kicked off the proceedings with a warm welcome, and James Cooke, Editor of The Probe, presented the winners with their trophies.
As the plates were cleared and the dust settled,






THE DENTAL AWARDS

guests were treated to a performance from a renowned magician, who had been circling the room, executing close-up magic to the delight of all. His big performance for the entire room capped of the event by leaving jaws firmly on the ground.
Stay tuned in the coming weeks for details on how to enter the 2026 Dental Awards, and you too could find yourself celebrating next year!




































National Smile Month Award
NHS Ayrshire & Arran Oral Health
Improvement Team 1
Best Outreach or Charity Initiative
Edinburgh Community Food and LINKnet Mentoring 2
ODL Dental Clinic 3
Front of House
Claire Smith, Community Dental Services CIC (CDS) 4
Dental Therapist of the Year




Dental Awards 2025 Winners
Website and Digital Campaign of the Year
Emily Banks, University Dental Hospital, Cardiff 5
Dental Hygienist of the Year
Natalie Fitzpatrick, Bridge Dental Care 6
Dental Nurse of the Year
Mihaela Marian, Ten Dental + Facial 7
Practice Manager of the Year
Nicola Bushell, Community Dental Services CIC Essex 8
Young Dentist of the Year
Simran Bains, Rock Dental Practice 9
Dentist of the Year
Dr Martina Hodgson, The Dental
Architect 10
Dental Team of the Year
ODL Dental Clinic, London 3
Practice of the Year
ODL Dental Clinic, London 3

















































Taking it to heart
Learning objectives
• To understand the link between the oral cavity and infective endocarditis
• To know the risk factors of infective endocarditis
• To identify the ways in which clinicians can support at-risk patients
GDC Development Outcome: C
The UK’s population is ageing. 50 years ago, 13% of the population were 65 and over – now it is closer to 19%. Advances in technology and healthcare have improved the country’s health, with earlier diagnoses and superior treatments now accessible to a greater number of people. Whilst this is to be celebrated, the ageing population also brings many new health challenges. Despite being considered a rare disease, cases of infective endocarditis have grown due to the higher numbers of elderly Brits. ii A ten-year study iii found that, in 2009, there were 26.9 cases per million Brits. By 2019, this had nearly doubled, with 50 cases per million. A potentially fatal health complication, infective endocarditis is of particular concern to dental clinicians due to the relation it has with the oral cavity and the bacteria housed in the oral microbiome. To prevent the infection from going undetected, clinicians must be aware of the risk factors, symptoms and treatment options to best ensure that vulnerable patients have the best chance of overcoming it.
Endocarditis explained
The endocardium, the innermost layer of tissue that lines the heart’s chambers and valves, is crucial for the heart to develop and function. Infective endocarditis is the inflammation of the lining, most commonly caused by pathogens entering the blood and travelling to the heart. In 26-45% of cases, the source of these pathogens is the oral cavity. iv

Because infective endocarditis has a 50% requirement for cardiac surgery and a 30% mortality rate at one year, detecting it early is vital. iii There are many symptoms that both clinicians and patients should look out for, including: a high temperature, chills, headaches, joint and muscle pain. ii If the infection is undetected, it can lead to heart failure, in which the organ is unable to pump enough blood around the body, and/or a stroke, where blood supply to the brain is disrupted.
In the dental practice
There are several cardiac-adjacent risk factors that clinicians should also be aware of; patients presenting with these are more vulnerable to infective endocarditis. These include:
• Those with a prosthetic heart valve following replacement valve surgery
• Congenital heart disease
• Hypertrophic cardiomyopathy
• Damaged heart valves
• A history of endocarditis ii All of the above make it easier for
bacteria to bypass the immune system, with congenital or other acquired diseases causing partial loss of endothelial integrity, therefore leading to a greater risk of infection in the endocardium. v Furthermore, whilst more common in older demographics who are more likely to have had replacement valve surgery, the condition has been reported in children, especially those born with congenital heart disease. Infective endocarditis also affects twice as many men as it does women, though the reasoning for this is still unclear. ii Clinicians should consider these risk factors when identifying vulnerable patients. It is common that patients with infective endocarditis are referred to a dental practice for an assessment of their oral health. vi In this case, clinicians help patients to eliminate any infectious oral microbes that may exacerbate infective endocarditis.
Dental dangers
The prevalence of oral diseases and any secondary symptoms may lead to the spread of bacteria from the oral cavity and into the bloodstream, enabling it to infect the endocardial surfaces. As such, certain dental problems can be viewed as risk factors for bacteraemia. This encompasses traumatic injury to the mucosa or gingiva, caries, and periodontitis. Among oral diseases, carious inflammatory lesions in the oral cavity can consist of 10-20 complex bacterial flora, with many of these being Gram-negative species.v Bleeding in the oral cavity can then cause these to enter the bloodstream and move elsewhere in the body. As they are predominantly Gram-negative, they are much harder to treat.
Whilst oral surgeries can help manage infective endocarditis by removing harmful bacteria, they may also lead to bacteraemia. Such treatments include extractions, scaling, endodontic interventions and any other procedures that involve gingival manipulation or potential bleeding. vii Whilst a list of treatments can help clinicians, personal judgement is also advised as only the clinician themselves will know if a planned surgery on each individual patient will cause bacteraemia. vii
Confusion over management
Antibiotics play a crucial role in the treatment of infective endocarditis, with afflicted patients often receiving intravenous antibiotics in hospital. vi For clinicians, the use of antibiotics prior to certain dental procedures (as a way of containing harmful pathogens) has led to fierce debate; different countries have different guidelines. The UK’s National Institute for Health and Care Excellence states “antibiotic prophylaxis against IE is not routinely recommended for people undergoing dental procedures”. vii This enables a degree of autonomy on behalf of the clinician due to the “not routinely”, but there is a greater need for clarity as to when and if such a treatment is suitable.
Care and caution
Regardless of country or guidelines, one aspect of infective endocarditis management that is agreed upon is the maintenance of good oral health among at-risk patients. v The prevention of oral diseases can be achieved through diligent daily dental care and an adherence to regular dental appointments. v Periodontal evaluation, supportive periodontal care
and regular cleanings can minimise the risk of periodontal diseases.
At-risk patients should also be educated on the link between oral health and the risk of infective endocarditis. This will help them understand the lifestyle choices that can improve their oral health, such as:
• Smoking cessation
• Limiting alcohol consumption
• Improving diet / cutting down on sugar intake
• Keeping hydrated viii
Above all else, a consistent and thorough oral hygiene routine should be conducted daily. Along with traditional toothbrushing twice a day, at-risk patients should be advised to incorporate interdental cleaning into their daily dental care. Caution should be recommended too: bleeding is common when starting interdental cleaning, often as a result of plaque build-up and inflammation. Diligent cleaning will support gingival healing and prevent bleeding in the future.
For excellent results, the TANDEX FLEXI range of interdental brushes effectively reduce plaque. Spanning 11 different colour-coded sizes, patients can find the perfect options for a more comfortable experience, enhancing compliance. Greater hygiene results await when supplementing the TANDEX FLEXI brush with PREVENT Gel, from TANDEX. This adds an antibacterial property that reduces the risk of oral diseases and strengthens the enamel for a comprehensive clean.
Support now is support for the future
The ageing population of the UK will continue to present more challenges for clinicians. As infective endocarditis rates increase, being able to spot the risk


factors and support patients diagnosed with it is essential to improve survival rates and quality of life. Above all, a greater awareness of the role that the oral cavity, and the bacteria inside it, can have is required to better protect overall health. For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/
References
i. Barton, C., Sturge, G. and Harker, R. (2024). The UK’s changing population. [online] House of Commons Library. Available at: https://commonslibrary.parliament.
uk/the-uks-changing-population/.
ii. NHS (2022). OverviewEndocarditis. [online] NHS. Available at: https://www.nhs.uk/conditions/ endocarditis/.
iii. Thornhill, M.H., Dayer, M.J., Nicholl, J., Prendergast, B.D., Lockhart, P.B. and Baddour, L.M. (2020). An alarming rise in incidence of infective endocarditis in England since 2009: why? The Lancet, 395(10233), pp.1325–1327. doi:https://doi. org/10.1016/s0140-6736(20)305304.
iv. Deppe, H., Reitberger, J., Behr, A.V., Vitanova, K., Lange, R., Wantia, N., Wagenpfeil, S., Sculean, A. and Ritschl, L.M. (2022). Oral bacteria in infective endocarditis requiring surgery: a retrospective analysis of 134 patients. Clinical Oral Investigations, 26(7), pp.4977–4985. doi:https://doi.org/10.1007/s00784022-04465-2.
v. Bumm, C.V. and Folwaczny, M. (2021). Infective endocarditis and oral health—a Narrative Review. Cardiovascular Diagnosis and Therapy, [online] 11(6), pp.1403–1415. doi:https://doi.org/10.21037/ cdt-20-908.
vi. Thoresen, T., Jordal, S., Lie, S.A., Wünsche, F., Jacobsen, M.R. and Lund, B. (2022). Infective endocarditis: association between origin of causing bacteria and findings during oral infection
To answer the questions below, visit cpd.the-probe.co.uk and register/log in. Click on ‘Courses’. Search for the course with the same headline as the corresponding article.
CPD
questions – Taking it to heart
1. What is considered the biggest factor for the rise in infective endocarditis cases?
a. Unhealthy diets
b. An ageing population
c. Climate change
d. A growing population
2. How many infective endocarditis cases can be attributed to the spread of pathogens from the oral cavity?
a. 1-12%
b. 13-25%
c. 26-45%
d. 46-58%
3. Which of the following conditions are risk-factors for infective endocarditis?
a. Replacement valve surgery
b. Damaged heart valves
c. Congenital heart disease
d. All of the above

screening. BMC Oral Health, 22(1). doi:https://doi.org/10.1186/s12903022-02509-3.
vii. Thornhill, M., Prendergast, B., Dayer, M., Frisby, A., Lockhart, P. and Baddour, L.M. (2024). Prevention of infective endocarditis in at-risk patients: how should dentists proceed in 2024? British Dental Journal, [online] 236(9), pp.709–716. doi:https://doi.org/10.1038/s41415024-7355-2.
viii. Guy’s and St Thomas’ NHS Foundation Trust. (2023). Infective endocarditis - Avoiding infective endocarditis. [online] Available at: https://www.guysandstthomas.nhs. uk/health-information/infectiveendocarditis/avoiding-infectiveendocarditis. n
About the author
Jacob Watwood on behalf of Tandex.

4. Which dental condition is the least likely to lead to bacteraemia?
a. Caries
b. Trauma to the mucosa
c. Tooth staining
d. Periodontitis
5. What is the correct recommendation for using antibiotic prophylaxis to treat infective endocarditis according to the National Institute for Health and Care Excellence?
a. To be used routinely
b. To be used always
c. Not to be used routinely
d. Not to be used ever
6. How can clinicians support vulnerable patients in reducing the risk of infective endocarditis?
a. Recommend a consistent daily oral hygiene routine
b. Encourage an unhealthy diet
c. Suggest infrequent dental and doctor appointments
d. Advise regular alcohol consumption
Managing medication –the oral health challenge
Learning objectives
• To understand the link between xerostomia and oral disease
• To identify patients who may be at a higher risk of xerostomia
• •o recommend appropriate solutions that relieve the symptoms of xerostomia for afflicted patients
GDC Development Outcome: C
In April 2025, the UK government outlined actions aiming to accelerate the discovery of lifesaving drugs, helping to improve patient care and attract investment into the country’s medical research industry. There is already a growing demand among the population: in a one-year period from 2022-2023 there were 1.18 billion prescription items dispensed in England alone, a 3% increase from the year before. ii Whilst the growth in prescriptions may mean that patients are able to live with or overcome their conditions with better results, the potential side effects of a variety of medications are of major concern to dental clinicians. In particular, xerostomia most frequently develops due to regular medication use. iii For patients, this adverse side effect becomes a challenge when maintaining a healthy oral microbiome, which is why a greater understanding of the condition is important for the clinician to share with at-risk patients.
It's saliva!
Xerostomia is commonly referred to as dry mouth due to the decline in salivary levels. However, xerostomia isn’t just defined by a reduced quantity of saliva – changes in salivary composition are also part of the condition. iv An inhibited salivary flow allows microbes to better adhere in the oral cavity, clinging to the tooth surfaces and causing the biofilm to stagnate for longer. The pH of the oral cavity decreases due to xerostomia, with the saliva having a reduced buffering capability. v This creates a fertile space for oral diseases, increasing the risk of periodontitis, caries, edentulism and halitosis. iv Over 30% of adults experience xerostomia and as high as 72% of

institutionalised adults, i.e. those residing in long-term care facilities, will also report dry mouth symptoms. iv There are several risk factors for xerostomia, such as patients with Sjogren’s syndrome and cancer-related head and neck radiation, to be aware of when treating patients. But the sheer number of Brits who take medications makes xerostomia a problem that can affect millions of people, with over 400 different drugs associated with the condition. vi
An age-old, old-age problem
Medication plays a vital role in fighting disease, suppressing symptoms and improving (and often extending) quality of life. The rate of prescriptions dispensed in the UK increases every year, meeting the demands of a growing ageing population. Among the most common are medications for the cardiovascular system, the central nervous system, and the endocrine system. vii
Polypharmacy is defined as the regular use of five or more medications at the same time. This has become more common with an ageing population who rely on medications in everyday life; this group of patients is only set to expand, as a 2019 forecast stated that by 2039 the over-65 age group is expected to rise from 18.5% of the population to 23.9%.
vii Patients who fall into the polypharmacy bracket are at a higher risk of xerostomia due to the mix of medications – clinicians must be aware of the specific drugs that increase the risk of dry mouth. Antisialogogues are substances that reduce the flow of saliva. Medications that have this label include many types of:
• Anticholinergics – a class of drugs that block the action of the neurotransmitter acetylcholine
• Antidepressants / anxiolytics
• Antihistamines
• Antipsychotics
Up on CPD
• Cardiovascular agents
• Diuretics – ‘water pills’ that help the body get rid of excess fluid
• Analgesics iv
Older patients who regularly take these medications are at increased risk of xerostomia.
A generation in danger
It isn’t just older patients at risk from medication-associated xerostomia. Mental health medications are especially of concern for clinicians and the growing number of younger patients needing them may lead to higher reports of dry mouth. An estimated 1 in 6 adults have experienced moderate to severe depressive symptoms within a severalweek period, viii whilst 20% of children aged 7-16 had a probable mental health condition in 2023 – this was much higher than the 12% reported in 2017. ix
These high numbers were reflected in the rise in medications prescribed to manage mental health conditions, both for adults and children/teenagers. In 2022-2023, a staggering 89 million antidepressant drug items were prescribed. This was a 3.3% increase to the previous year, with an increase in affected patients by 2.1%. x This indicates that not only are more people being
diagnosed and in need of medication, but that some are requiring more antidepressants than they did previously –a higher frequency of medication use will intensify the risk of xerostomia. Besides antidepressant prescriptions, over 14 million antipsychotic items were approved for 860,000 identified patients, with a notable disparity in that twice as many of these patients were from more socioeconomically deprived areas versus the least deprived. x This can be an indicator for at-risk patients.
Diligent diagnosis
The diagnosis of xerostomia is often a simple procedure that measures the flow rate of saliva. Less formal indications include the adherence of lipstick to the front teeth. xi For a more precise, scientific measurement, a conventional salivary flow rate for unstimulated saliva from the gland is 0.4-1.5mL/min/gland, and for stimulated saliva the range is 1-2mL/min. Any values below 0.1mL/ min for unstimulated and under 0.7mL/ min when stimulated can be considered xerostomic. xi
Solutions at home
Diagnosis or not, patients reporting with dry mouth symptoms have several

approaches available for improving their salivary flow and protecting their oral cavity. Hydration, the elimination of common dry mouth offenders (such as tobacco and alcohol), and the discontinuation or reduction in xerogenic medications can all provide symptomatic relief of oral dryness. xii
Salivary substitutes are commercial products that lubricate the mucosa and relieve the sensation of dryness without stimulating the salivary flow. However, the use of such substitutes has challenges – a frequent intake is required for longerterm results but this can prove costly.xii
Along with a reduction in alcohol, caffeine and sugary or acidic foods, patients with xerostomia can also try using a humidifier at night and focusing on breathing through the nose rather than the mouth.
A common suggestion is the consumption of sugar-free chewing gum. As the smell, taste and mastication of food stimulates a strong flow of saliva, gum can help prevent oral dryness and is low cost, easily available and safe. However, clinicians must emphasise that sugarfree chewing gums are critical for increasing saliva production and also reducing the risk of caries. Patients with mastication difficulties, such as those with temporomandibular disorder (TMD) should avoid chewing gum so as not to aggravate the temporomandibular joint (TMJ).
Clean the gaps
For all patients suffering with xerostomia, a consistent oral hygiene routine is necessary to remove the harmful bacteria that the saliva cannot. Along with traditional toothbrushing twice a day, patients must incorporate interdental cleaning for a comprehensive clean that reaches every tooth surface.
An invaluable ally in preventing oral disease is the TANDEX FLEXI, a series of interdental brushes that covers 11 different colour-coded sizes for the best possible access to the interdental spaces. Applying each brush with PREVENT Gel, from TANDEX, adds an antibacterial boost to the cleaning. Its unique formula strengthens the enamel and reduces the risk of caries and periodontitis, supporting a healthier and happier smile.
With polypharmacy increasing among the ageing population, a rise in reported xerostomia is likely to continue. It is therefore crucial that clinicians can identify at-risk patients and offer the best solutions to manage dry mouth symptoms and prevent oral disease.

For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/ References
i. Health (2025). Prime Minister turbocharges medical research. [online] GOV.UK. Available at: https://www.gov.uk/government/ news/prime-minister-turbochargesmedical-research.
ii. NHS BSA (2023). Prescription Cost Analysis – England – 2022-23 | NHSBSA. [online] www.nhsbsa. nhs.uk. Available at: https://www. nhsbsa.nhs.uk/statistical-collections/ prescription-cost-analysis-england/ prescription-cost-analysisengland-2022-23.
iii. Talha, B. and Swarnkar, S.A. (2023). Xerostomia. [online] PubMed. Available at: https://www.ncbi.nlm. nih.gov/books/NBK545287/.
iv. Desai, J.P. and Nair, R.U. (2023). Oral Health Factors Related to Rapid Oral Health Deterioration among Older Adults: A Narrative Review. Journal of Clinical Medicine, 12(9), p.3202. doi:https://doi.org/10.3390/ jcm12093202.
v. The Oral Cancer Foundation. (2018). Xerostomia. [online] Available at: https://oralcancerfoundation.org/ complications/xerostomia/. vi. Kim, Y.-J. (2023). Xerostomia and Its Cellular Targets. International Journal of Molecular Sciences, [online] 24(6), p.5358. doi:https://doi. org/10.3390/ijms24065358. vii. Naser, A.Y., Alwafi, H., Al-Daghastani, T., Hemmo, S.I., Alrawashdeh, H.M., Jalal, Z., Paudyal, V., Alyamani, N., Almaghrabi, M. and Shamieh, A. (2022). Drugs utilization profile in England and Wales in the past 15 years: a secular trend analysis. BMC Primary Care, 23(1). doi:https://doi. org/10.1186/s12875-022-01853-1.
viii. Office for National Statistics (2022). Cost of Living and Depression in adults, Great Britain - Office for National Statistics. [online] www.ons.gov.uk. Available at: https://www.ons.gov.uk/ peoplepopulationandcommunity/ healthandsocialcare/mentalhealth/ articles/costoflivinganddepression inadultsgreatbritain/ 29septemberto23october2022.
ix. Baker, C. and Kirk-Wade, E. (2024). Mental Health Statistics for England: prevalence, Services and Funding. [online] Parliament.uk. Available at: https://researchbriefings.files.parliament. uk/documents/SN06988/SN06988.pdf.
To answer the questions below, visit cpd.the-probe.co.uk and register/log in. Click on ‘Courses’. Search for the course with the same headline as the corresponding article.
x. NHS Business Services Authority (2023). NHS releases 2023/24 mental health medicines statistics for England. [online] NHS Business Service Authority (NHSBSA). Available at: https://media.nhsbsa. nhs.uk/press-releases/5171d61695ea-4282-959b-15f8bfed6a0f/nhsreleases-2023-24-mental-healthmedicines-statistics-for-england. xi. The Oral Cancer Foundation. (2018). Xerostomia. [online] Available at: https://oralcancerfoundation.org/ complications/xerostomia/. xii. Kapourani, A., Kontogiannopoulos, K.N., Manioudaki, A.-E., Poulopoulos, A.K., Tsalikis, L., Assimopoulou, A.N. and Barmpalexis, P. (2022). A Review on Xerostomia and Its Various Management Strategies: The Role of Advanced Polymeric Materials in the Treatment Approaches. Polymers, [online] 14(5), p.850. doi:https://doi. org/10.3390/polym14050850. n
About the author Jacob Watwood on behalf of Tandex.

1. Which of the following is the growing demand for prescription medication most likely to lead to?
a. Brighter teeth
b. Xerostomia
c. More root canal treatments
d. Tooth loss
2. Which of the following statements best defines xerostomia?
a. Xerostomia stops saliva production
b. Xerostomia reduces saliva production
c. Xerostomia changes saliva composition
d. Xerostomia reduces saliva production and changes saliva composition
3. How many institutionalised adults are likely to experience dry mouth symptoms?
a. Up to 68%
b. Up to 72%
c. Up to 76%
d. Up to 80%
4. What is polypharmacy?
a. The regular intake of five or more medications
b. Multiple pharmaceutical brands
c. The regular intake of a medication
d. Multiple pharmacies in the same area
5. Which of the following medications are associated with xerostomia?
a. Antidepressants and antipsychotics
b. Anticholinergics and antihistamines
c. Cardiovascular agents and analgesics
d. All of the above
6. What can clinicians suggest to patients reporting dry mouth symptoms?
a. Regularly drink a variety of soft and alcoholic beverages
b. Chew sugar-free gum
c. Eat more snacks in the day
d. Practice mouth breathing
A team here for you
BioHorizons Camlog is committed to delivering exceptional customer service and support to complement their range of industry-leading solutions. The team has recently been expanding and Zoe Russo recently joined as Territory Manager for East London & East Anglia. With 23 years of experience in interventional cardiology – including working as an Interventional Cardiology Nurse – Zoe brings with her a plethora of experience in various healthcare-focused sales roles. As such, she understands the daily challenges of clinical practice. About why she joined the team Zoe says:
“I’ve always enjoyed interacting with customers, being on the road and meeting new people. I also wanted to utilise my knowledge and skills while learning
Safe sharps waste with Initial Medical
Safely manage your sharps with the Eco Sharps Bin from Initial Medical, and avoid injuries and infection for your team.
The Eco Sharps Bin range is made from at least 40% recycled plastic, featuring punctureresistant and seepage proof solutions. This ensures everything from needles and syringes, to scalers and burs can be disposed of without worry.
Plus, each sharps bin from Initial Medical is available in line with the colour code, ensuring you meet all relevant regulations, such Health Technical Memorandum 07-01.
Safe sharps disposal is vital in dental care, yet a 2025 survey with the British Association of Dental Nurses found that the most common point for an inoculation injury was after an
something new, which made a move into implant dentistry with BioHorizons Camlog a fantastic opportunity.
“I have loved getting stuck in and find the dental profession to be fascinating. I appreciate the importance of clinically-proven products and with BioHorizons Camlog, I know that I am delivering solutions our customers can trust.”

To find out more about the range of solutions available from BioHorizons Camlog, or to contact your local representative for support, please visit the website.
theimplanthub.com/the-team/
item was used, but before it was discarded.
Eco Sharps Bins at the point of use can support your team, and maximise their safety.

To learn more about sharps waste management, contact the Initial Medical team today.
To find out more, get in touch at 0808 304 7411 or visit the website today.
initial.co.uk/medical
Rapidly reduce dental pain with the range of solutions from Orajel
Managing patients’ dental pain remotely can be challenging, but it’s vital for helping to maintain their quality of life whilst they wait for treatment. Orajel™ offers a wide range of solutions to help your patient manage their dental pain at home. Orajel™ Dental Gel contains 10% benzocaine, allowing the patient or their carer to apply the local anaesthetic to the painful tooth. The powerful local anaesthetic temporarily blocks the pathway of pain signals along the nerves, numbing the area. For more intense dental pain, Orajel™ Extra Strength contains 20% benzocaine, for rapid relief.
Additionally, if patients are suffering with mouth ulcers or denture pain, Orajel™ Mouth Gel is the ultimate soother. It contains 10%
benzocaine and can be applied directly to the areas of the mouth that are tender or painful up to four times per day.

To find out more about the range of products from Orajel please visit the website and get in touch with the team. For essential information, and to see the full range of Orajel products, please visit the website.
Optimising value for everyday dentistry
At Dental Directory, we’re dedicated to delivering value in every aspect of our service.
Not only do we ensure competitive prices all-year round, but we also provide various promotions and bundle offers to deliver even greater cost-efficiency on products you buy every day.
But the value of our service goes far beyond price. All our solutions are supported by a team of product experts who are constantly available to provide advice and guidance to help you make the very most of the products available.
For the equipment we supply, we also have an extensive team of specifically-trained engineers across the nation. They offer advanced technical support both remotely and on-site, and they maintain a first-

time fix rate of over 90% for peace of mind that they will keep your practice running.
In addition, we offer equipment training for your team, marketing support and so much more for the practices we work with.
Discover what value means at Dental Directory today.
For more information on the products and maintenance services available from Dental Directory, please visit ddgroup.com or call 0800 585 586.
ddgroup.com
15 years of Dental Elite recruitment support
Dental Elite is celebrating 15 years of providing the dental profession with exceptional recruitment support. Having come a long way since being established from a homeoffice in 2011, the organisation now consists of a comprehensive recruitment team with specialists dedicated to each area of the market.

After almost 10 years with Dental Elite herself, Lisa McCusker, Senior Recruiter and Locum Recruitment Specialist, considers the team to be one of the company’s greatest assets, saying:
“We have an experienced team specialising in each area of dental recruitment, from locum to permanent dentists, dental team members and support staff. This allows us to focus on exactly what it is clients are looking for. We strive to go above and beyond, working tirelessly to give individuals and practices options.”
To see for yourself why Dental Elite has been so successful in delivering recruitment support to the profession for so long, contact the team today.
For more information on Dental Elite visit www.dentalelite.co.uk, email info@dentalelite.co.uk or call 01788 545 900.
An excellent recommendation to supplement oral hygiene routines
WASH&PREVENT + from TANDEX is an excellent mouthwash with 0.12% chlorhexidine and 226ppm fluoride.
WASH&PREVENT also comes in a version that contains zinc to help patients maintain extra-fresh breath. Fluoride helps to strengthen the enamel, while chlorhexidine has an antibacterial effect, helping to maintain a healthy, clean mouth, protecting patients and enhancing their daily care routines.

With the addition of zinc, patients can enjoy even greater protection! Zinc has not only been shown to fight halitosis, it is also an important mineral to support patients in fighting infections, supporting immunity and maintaining healthy soft tissue.
Recommend WASH&PREVENT and WASH&PREVENT with Zinc from TANDEX to your patients today!
For more information on Tandex’s range of products, visit https://tandex.dk/ Our products are also available from DHB Oral Healthcare https://dhb.co.uk/.
tandex.dk











































Buy 2 get 1 free (while stocks last)



Directa’s ProphyCare, is one of the most well-known brands of prophylaxis paste worldwide, offering reliable results ranging from regular cleaning of the teeth to more complicated implant maintenance procedures.ProphyCare pastes are available in different grits from coarse to extra-fine and are colour coded for easy identification. All ProphyCare pastes have a mild minty taste and do not splatter, it stays in the polishing cup during the treatment.
prophylaxis more ts have