

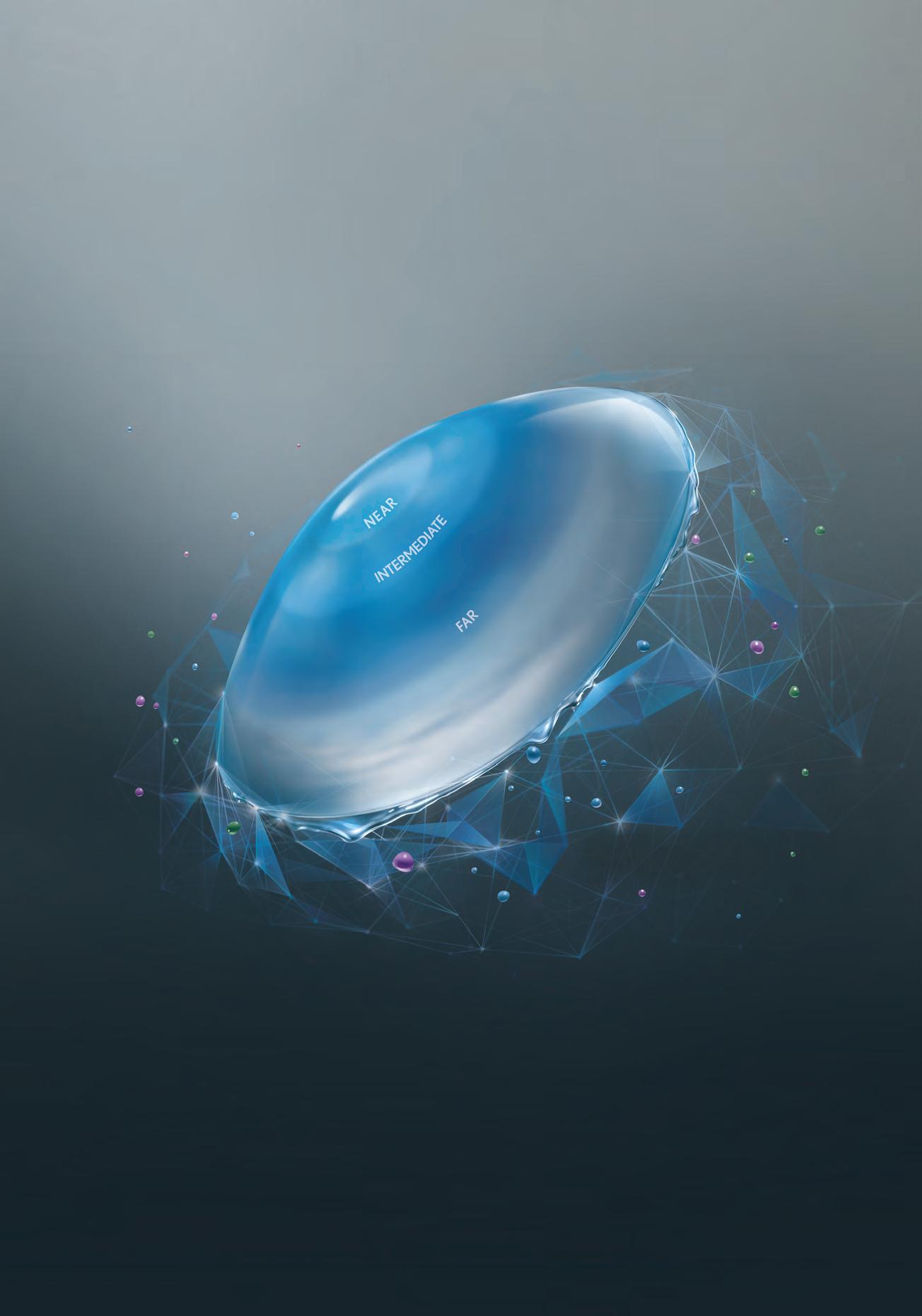
DISCOVER MORE LIGHT UTILISATION WITH LESS SCATTER†1,2
Everything you love about PanOptix®, now with half the scatter‡2,3 thanks to an unprecedented 94% light utilisation.§1-3 The lowest light scatter of any trifocal IOL.†§1-8
Clareon® PanOptix® Pro. Vision to the Power of Pro.
†Compared to Clareon® PanOptix®. Based on bench and vision simulator studies. ‡Compared to Clareon® PanOptix®. PanOptix has 88% light utilisation (12% scatter light)/PanOptix Pro 94% light utilisation (6% scatter light). §Based on manufacturer reported values and respective methodology for trifocals Clareon® PanOptix®, Envista Envy*, Gemetric, Rayner* Trifocal and AT Elana*. *Trademarks are the property of their respective owners. References: 1. Alcon data on file, 2024; [REF-25221]. 2. Alcon data on file, 2025; [REF-25218]. 3. Alcon data on file, 2025; [REF-08546]. 4. Muzychuk, A. Defocus Curve Performance of a Novel Hydrophobic Acrylic Trifocal Intraocular Lens: A prospective, Multicenter Canadian Study. ASCRS Annual Meeting, April 5-8, Boston; [REF-25948]. 5. Rayner Professional Website. https://rayner.com/en/iol/trifocal/rayone-trifocal/. Accessed December 2024. 6. Carones F. New Concept of Light Distribution for Bilateral Trifocal IOL Implantation. AAO. 2022;2022:53; [REF-23587]. 7. ZEISS AT LISA tri family. Supplement in Cataract and Refractive Surgery Today (Europe), September 2014. 8. Zeiss Cataract Insights: Laying the Myth or Reality; Digitalization enhances cataract surgery? Supplement in Ophthalmology Times, Europe; May 22, 2024; https://europe. ophthalmologytimes.com/zeiss-cataract-insight-series?page=1 Accessed December 2024.
Please refer to relevant products instructions for use for complete list of indications, contraindications and warnings. ©2025 Alcon Laboratories Pty Ltd. AUS: 1800 224 153; Auckland NZ: 0800 101 106. ALC2561 12/25 ANZ-CPR-2500018

GROWING PAINS
Australia's cohort of optometrists has increased – just not where they are needed, say leaders
GENERATION GAP
Opportunities abound for those practices who know how to mind that gap and promote contact lenses
INJECTING DEBATE
An eye health sector leader urges the Govt to press pause on changes to intravitreal injection policy
AUSTRALIA’S LEADING OPHTHALMIC








REPORT: OPTOMETRY SPREAD CONCERNS REMAIN
Ahpra’s latest annual report shows the number of optometrists continues to grow in Australia but challenges remain in getting those practitioners to where they are most needed.
That was one key takeaway from the 2024/25 report of the Australian Health Practitioner Regulation Agency (Ahpra) and National Boards.
The report revealed the number of registered optometrists rose by 4.1% to 7,340 people in the year to June 2025.
That closely resembled the 4.3% rise in all registered health practitioners in Australia, to 959,858, with a record 870,000 practitioners renewing their registration in 2024/25.
That meant there were now 3.5 practitioners for every 100 Australians, Ahpra said.
“This continues our work to ensure all Australians have access to a safe, high-quality health workforce,” it said.
Optometry Australia (OA) welcomed the report and noted the “steady growth” of optometrists.
“But numbers alone don’t tell the full story,” said OA CEO Ms Skye Cappuccio, who was to step down from the role in December 2025. “Distribution still does not align with community need.

“Although practitioner numbers have grown, this growth is largely concentrated in metropolitan areas. As a result, access to eyecare outside major cities is uneven – some regional and rural communities are serviced by resident optometrists who are working in practices, others rely on intermittent support through the Visiting Optometrists Scheme (VOS), and some pockets of rural Australia continue to face persistent undersupply and limited access to care.”
Cappuccio said adding more
optometrists “would not create a prosperous profession or improve care for the public”.
She said OA would continue to promote its Workforce Strategy, which resisted “inappropriate supply expansion”, looked to strengthen workplace conditions, maximised workforce utilisation, raised public awareness of optometry, and aimed to ensure capacity was connected to areas of greatest need.
Cappuccio was impressed by the low number of notifications –
SURVEY PROMOTES VALUE IN FACE OF OPHTHALMOLOGY FEE ‘ATTACKS’
Australian ophthalmology performs “exceptionally well by international standards”, despite the “gross failures of the public hospital system”, according to the Australian Society of Ophthalmologists (ASO).
It was responding to the latest data from the Australian Bureau of Statistics (ABS), which showed that fewer Australians were delaying or not using selected health services when needed compared with two years ago.
The data, from the ABS Patient Experiences survey, provides a snapshot of access, barriers and people’s experiences with various healthcare services.
Mr James Eynstone-Hinkins, ABS head of health statistics, said: “In 2024-25, 27% of people
delayed or did not see a GP when needed. In 2022-23 this figure was higher, at 30%.”
The survey also revealed an increase in the number of people visiting a medical specialist, including ophthalmologists.
It showed a rise to 40.4% in 2024-25, up from 39.2% in 2023-24, with those delaying seeing a specialist dropping to 18.3% compared with 20.5%.
Those visiting their specialist recorded high ratings on core measures of respectful, attentive care: 78.5% of people reported that specialists always listened to patients carefully (ranked #2), and 83.4% reported specialists always showed respect (ranked #2).
Close to one in 10 people, or 8%, cited cost as a reason for
delaying or not seeing a GP when needed, while just 8.6% said that stopped them from visiting their medical specialist, compared with 9.8% two years previously.
Dr Peter Sumich, ASO president, said that showed medical specialists, including ophthalmologists, remained a “value proposition very popular with patients who value time efficiency, a specialist rather than a training registrar, and a location convenient for them”.
or complaints – for optometrists in this year’s annual report, even with the growth in the number of practitioners.
Ahpra said it had received 13,327 notifications about the entire health and medical workforce in the year to June 2025, 19% more than the previous year.
That meant notifications had risen by 34% in the past two years, from 9,706 in 2023/24.
“We closed 12,086 notifications,” Ahpra said in the 2024/25 report. “This was 8.3% more than last year and more than any previous year. At 30 June, there were 5,627 open notifications, 26.7% (1,186) more than last year.”
It said about 50% of the notifications received were categorised as lower risk and managed by an early determination process – an
continued page 8

Keep eyes, ears open
Private ophthalmology fees have been criticised this year, with the Grattan Institute calling them high and extreme.
Alternatively, there is a lengthy wait for tertiary eyecare in the
continued page 8
Practising optometrists are well aware of diabetes’ effects on the eye, but its impact on hearing often goes unnoticed. In this month’s CPD article, Dr Mehwish Nisar highlights the link between diabetes and hearing loss, providing practical guidance on screening and referral. As Dr Nisar points out, by incorporating these strategies, optometrists can play a vital role in holistic care and improve outcomes for patients with diabetes.
page 48
AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975
Australia grew by 4.1% in 2025. Image: InsightCreativeHouse/stock. adobe.com.
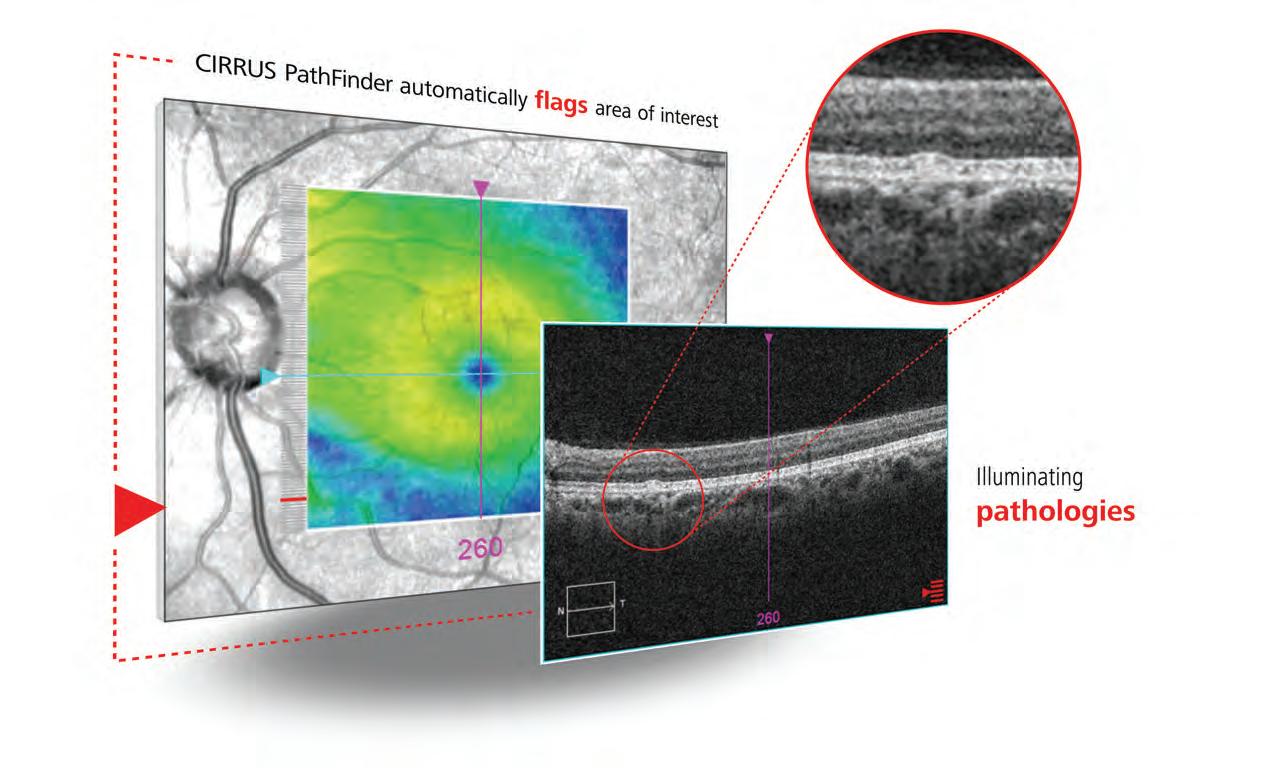
Intelligently Illuminating.
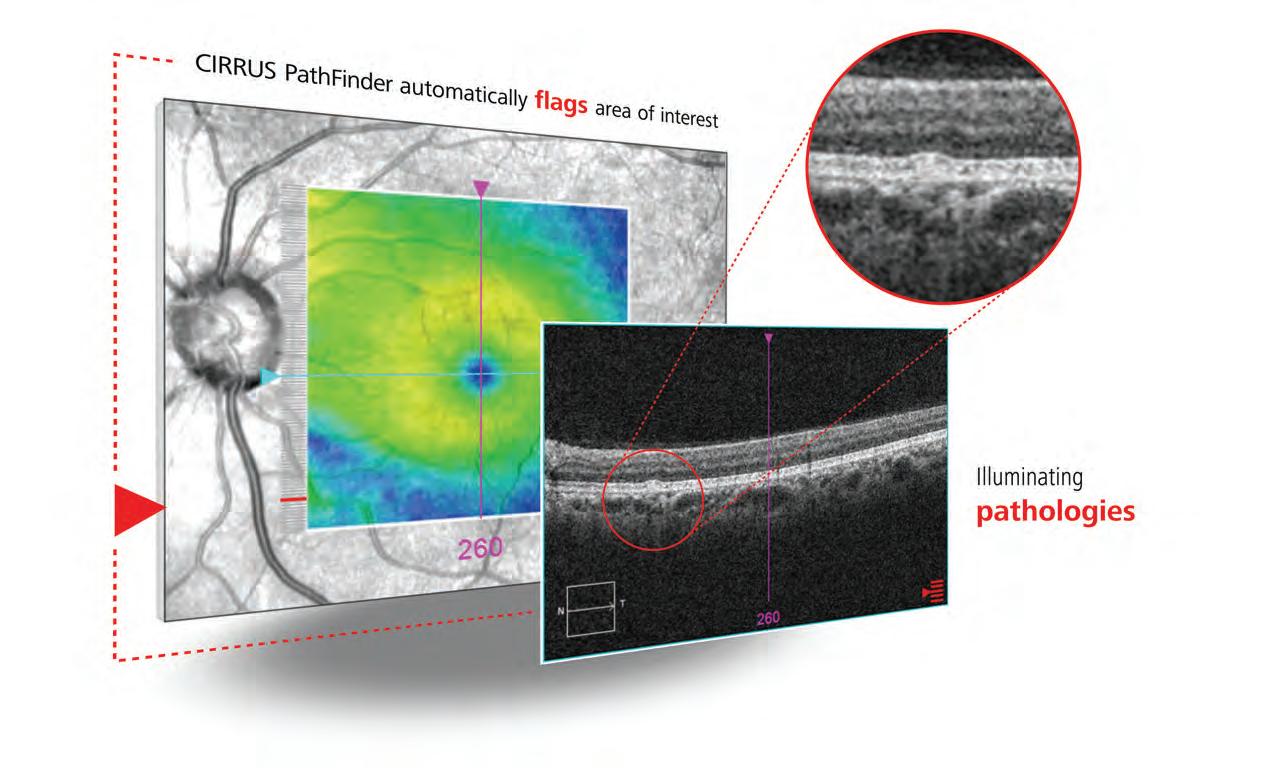
Know when to take a closer look
CIRRUS ® PathFinder™ from ZEISS is an innovative clinical support tool that enables more confident decision-making and accelerates your workflow with OCT interpretation assistance. ZEISS CIRRUS PathFinder* uses proprietary deep learning algorithms to automatically identify abnormal macular OCT B-scans that can aid in early disease detection and encourage further evaluation.
*PathFinder is available on ZEISS CIRRUS 500/5000/6000 devices

For information about ZEISS CIRRUS 6000, visit www.zeiss.com/cirrus6000
ZEISS
AU: 1300 365 470 med.au@zeiss.com
Carl Zeiss
AUSTRALIA.
IN THIS ISSUE
FEATURES

Blazing a trail

Two young optometrists are redefining early-career independence in their Perth practice.

CHALLENGES AND OPPORTUNITIES
This issue of
But first, an introduction.

This is my first edition as editor, after former head Myles Hume moved upwards and onwards to a wider group editor role here at Prime Creative Media.
My background is largely within what people would call the mainstream media, including senior editorial roles in New Zealand, and a brief stint as a reporter at the Blacktown City Star in Sydney’s hard-scrabble west.
In those roles I wrote editorials at a national level and, as a senior and features writer, covered practically every subject, from local and national politics to health, housing and social issues.
But until I joined Insight about 18 months ago, I can’t recall writing a great deal on eye health.

Scrubbing up The power of AI and use of language were among top subjects discussed at the 2025 RANZCO Congress.
Future-proofing
Two workshops at O-SHOW 2026 are set to reframe the future of eyecare in Australia.
So that’s my challenge: to continue to learn about this complex and vital sector – and all that underpins it – while helping the industry realise the opportunity it has to improve the lives of so many people in this country.
Writing of important work, we’ve taken the opportunity in our news feature to focus on optical dispensing and a growing industry challenge: retaining qualified, experienced people.
Good dispensers are those people who can build trust quickly at the pointy end of the patient’s interaction with a practice, provide tailored solutions based on lifestyle (therefore maximising sales) while reinforcing the guidance of the optometrist. It requires not only clear, practical skills but also adaptability and softer skills around communication and emotional intelligence that not all are blessed with but carry great value.
People like Mr James Gibbins and Ms April Petrusma are working to meet the challenge of increasing the number of qualified dispensers in the industry, but it appears not all are seeing the opportunity of what those people can bring to their practice.
Clearly, however, there can be great reward for those who do see that, and work to make it a reality.
At Insight, we look forward to helping support them in that great endeavour.
ROB MITCHELL Editor
UPFRONT

Just as Insight went to print, ACOD, the Australasian College of Optical Dispensing, was informed by the Victorian Government that its Skills First contract in the state would be scrapped. It is one of 58 Registered Training Organisations to be told that their contracts have been ended and they cannot offer supported places to students in 2026. The Independent Tertiary Education Council Australia said the move, announced nine days before Christmas, would likely lead to the closure of many courses and businesses, and affect the education of hundreds of tertiary students and the jobs of many teachers and trainers. IN OTHER NEWS, Optometry Australia (OA) says momentum is building for the introduction of universal pre-school vision screening in South Australia after ABC News highlighted a South Australian family whose child’s undiagnosed vision condition negatively impacted their child’s learning
WEIRD
Scientists at the University of Vienna have found that adult bristleworm eyes grow continuously thanks to a rim of neural stem cells similar to those in vertebrate eyes. The researchers say this growth is surprisingly regulated by environmental light via a vertebrate-like c-opsin. The discovery reveals deep evolutionary parallels between distant species and raises questions about how light shapes nervous systems beyond vision. It hints at hidden complexity in creatures long assumed to be simple.
WONDERFUL
An eight-year-old girl in the United States has been diagnosed with a brain tumour after an eye exam and the optometrist followed up to urge the family to get help for their daughter. Mr Jeffrey Cohen, an optometrist in New York, examined Annabeth Baah after a doctor noticed her eye was weak. Cohen found a swollen optic nerve and then followed up when the family was sent home from an emergency centre. Doctors eventually diagnosed a benign but growing tumour, which was removed before it could destroy her vision.
and confidence, renewing public attention on the need for state-wide early eye health checks. OA, the Royal Australian and New Zealand College of Ophthalmologists (RANZCO), and Orthoptics Australia and state eye health leaders have presented a joint proposal for universal four-year-old vision screening to the SA Health and Wellbeing Minister Mr Chris Picton. FINALLY, the Medical Board of Australia is to work with the medical profession on strategies to support late career doctors, including ophthalmologists, to keep practising safely as they age, opting against mandatory health checks for doctors aged over 70. The board said that new analysis of complaints outcomes showed that regulatory action involving doctors aged over 70 more commonly related to concerns beyond health, including communication, clinical care, and pharmacy or medication issues. It said these findings highlighted that health checks alone would not address the full range of risks identified.
insightnews.com.au
Published by: 379 Docklands Drive, Docklands VIC 3008 T: 03 9690 8766 www.primecreative.com.au
Chief Executive Officer
Christine Clancy christine.clancy@primecreative.com.au
Publisher Sarah Baker sarah.baker@primecreative.com.au

States more united on contacts
About 45 million Americans wear contact lenses, which is roughly 20% of the population. In Australia that percentage is about 8%. Page 19.
WACKY
Researchers in the UK have established that the strength of an individual’s handgrip is associated with age-related macular degeneration (AMD), with incidence of AMD increasing in those with worse strength. The study used the UK Biobank cohort of more than 380,000 people to identify the association and followed them over more than 12 years. They concluded that the result, which was largely the same across different sexes, highlighted the need for muscle strength interventions to be considered when looking to maintain visual health.
WHAT'S ON
THIS MONTH
34TH ANZ GLAUCOMA SOCIETY CONGRESS
15 – 16 February
The 2026 event in Sydney will emphasise high-quality clinical case studies and include a broader range of glaucoma science through keynote presentations and submitted papers. anzgsconference.com
Complete calendar page 56
NEXT MONTH
OWA WAVE 2026
CONFERENCE
21 – 22 March
The event returns with its successful hybrid conference format, including numerous speakers, CPD sessions, and two workshops in collaboration with Optical Dispensers Australia. evexus.net/au
Group Managing Editor Myles Hume myles.hume@primecreative.com.au
Editor Rob Mitchell rob.mitchell@primecreative.com.au
Senior Journalist Rhiannon Bowman rhiannon.bowman@primecreative.com.au
Commissioning Editor, Healthcare Education Jeff Megahan
Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Karyssa Arendt karyssa.arendt@primecreative.com.au
Head of Design Blake Storey
Art Director Bea Barthelson
Subscriptions T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright –No part of this publication can be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.
WORK STILL NEEDED ON NOTIFICATION PROCESS
continued from page 3
increase from 34.5% the previous year.
While the nature of concerns raised in 2025 was largely similar to the previous year, the number of notifications where the primary concern related to a practitioner’s behaviour increased to 6.9% in 2024/25, from 4.8% the previous year.
Notifications increased across all professions except midwifery and Aboriginal and Torres Strait Islander Health Practice.
Optometry represented just a fraction of those notifications, with 41 recorded by Ahpra and a total of 81 nationwide. Just one of the 554 Ahpra cases involving “immediate action” involved an optometrist.
The 81 notifications was a rise of six on the previous year and involved 71 practitioners, less than 1% of the registered optometry workforce.
OA said the low rate of notifications was a strong indicator of the profession’s “maturity, ethical culture and high clinical standards”.
“Optometrists practise in a highly regulated, evidence-based environment, and the profession has a strong culture of appropriate referrals, collaborative care and continuing professional development,” said Cappuccio.
“OA supported that through education, CPD, clinical guidelines, ethics resources, quality improvement tools and strong advocacy for safe and contemporary practice.”
She said members had noted improvements in the notification process, including better communication and transparency.
However, OA would continue to advocate for clearer, more timely updates; better recognition of low-risk cases; improved psychological support for practitioners undergoing a notification; and reduction of unnecessary delays and the potential impacts on wellbeing.
Ahpra acknowledged that the experience of going through a regulatory process could be stressful.
That was highlighted in the independent review from Ms Sue Dawson – the former NSW Health Care Complaints Commissioner.
“In line with this review, we are already working on reforming our notifications processes to support better timelines, transparency and procedural fairness,” Ahpra said.
“Public safety remains our number one priority and minimising practitioner distress is not at odds with this goal – it strengthens it. When practitioners feel supported and respected, they are more likely to

OA CEO Skye Cappuccio is pleased with the low rate of notifications for optometrists.
Image: Optometry Australia.
engage constructively with regulation, maintain their wellbeing and continue to provide safe care.”
On the increase in medical practitioners in Australia, Ahpra CEO Mr Justin Untersteiner said: “Nearly one million practitioners is a significant milestone, but we know growth isn’t just about numbers. We’re working hard to make registration easier while keeping safety front and centre.”
Ahpra said it remained on track to implement the recommendations of the independent Kruk review to bring more health specialists into Australia.
Ophthalmology is expected to be involved in those changes in the near future.
“We simplified English language requirements while maintaining public safety, expanding the list of recognised English-speaking countries from seven to 30 nations and territories,” it said in the report.
It said it also registered more than 1,000 Aboriginal and Torres Strait Islander health practitioners for the first time. Of the health practitioner workforce, 1.3% are Aboriginal and/or Torres Strait Islander.
“While this is an increase from last year, it is still well short of where we want to be, and there is much work to do to meet our goal of eliminating racism from the healthcare system.”
POLL SHOWS DECLINE IN TELEHEALTH SERVICE USE
continued from page 3
public system, placing them in “a painful dilemma”.
Dr Sumich said the ABS survey supported the idea that “ophthalmology consultations provide great value for patients who can access expert specialist opinion in their local suburb with little waiting time”.
He said the “attacks” on specialist fees were a “smokescreen to camouflage public health failure” in ophthalmology.
“Unfortunately, the disastrous state of public hospital outpatient clinics, long surgery wait times and time-inefficient services has meant more people have been forced into the private system where they are placed in financial stress.”
The survey also showed a decline in the use of telehealth services, with 22% using that option in 2024-25, compared with a peak of 31% in 2021-22.
“While telehealth maintains a stable
presence for patients facing distance barriers, in-person consultations remain the gold standard for ophthalmic care,” said Dr Sumich.
The ABS highlighted access to dental services to demonstrate challenges across Australia and in different socio-economic groups.
“The survey found that 65% of Australians living in areas of least socio-economic disadvantage saw a dental professional in 2024-25,” said Eynstone-Hinkins. “This compared with only 42 per cent of people living in most disadvantaged areas.”
And experiences of health services also differed by remoteness.
Nearly one in two people (46%) living in major cities were seen by a GP for urgent medical care within four hours, compared with 30% of those living in outer regional or remote areas.
Dr Sumich said: “It is invariably the most disadvantaged who miss out on medical care.
“The gross failures of the public hospital system in delivering

ophthalmology services leave patients with few options. We have witnessed department closures at St Vincent's Hospital and the shuttering of St George Hospital's cataract service.
“Hospitals routinely target ophthalmology budgets because it is a high-overhead specialty to provide,” he said.
“Without adequate representation on medical staff councils, ophthalmologists are rarely at the table when critical decisions are made, which means public ophthalmic care falls under the auditor's axe.”
Providing adequate services to remote regions of Australia remained an ongoing challenge, he said.
The use of telehealth services has dropped 9% since 2021-22. Image: Rostislav Sedlacek/stock. adobe.com.
DRUG PRESCRIBING PLAN SPARKS STRONG DEBATE
Optometry Australia (OA) says optometrists are “not seeking to become doctors” through proposed changes to rules governing the medicines they can prescribe for patients.
But the Australian Society of Ophthalmologists (ASO) believes the “controversial plan” introduces risks that would be higher than any benefits should the proposal go through.
It launched a campaign of opposition in the lead-up to the December 24, 2025, closure of public submissions on the proposal by the Optometry Board of Australia (OBA), which seeks to expand optometrists’ prescribing rights to include oral and topical medicines.
In response to ASO’s concerns, OA president Mr Theo Charalambous said people were “waiting too long, travelling too far and paying too much for time-sensitive treatment”.
“Enabling oral prescribing for therapeutically endorsed optometrists means more patients can begin appropriate treatment in a single consultation, rather than being sent elsewhere purely because of an

administrative restriction on topical routes,” he said.
“This reduces preventable delays, avoids unnecessary out-of-pocket costs and supports continuity of care.
“It also helps the broader system. When optometrists can manage straightforward ocular presentations end-to-end, GPs and ophthalmologists are freed to focus on more complex and surgical care –where community need is greatest.”
But the ASO disagrees.
In a statement urging opposition to the plan, it said that, unlike eye drops, systemic drugs acted throughout the body and could trigger serious adverse events, including renal failure,
The proposed changes would allow optometrists to offer a wider range of medicines to their patients.
Image: Eric Hood/ stock.adobe.com.
liver injury, cardiac complications and life-threatening allergic reactions.
The ASO said its members had witnessed this first-hand.
Its vice chair Mr Kerry Gallagher said a four-year undergraduate program in optometry, even with therapeutic content, could not provide sufficient training needed to “recognise red flags, understand systemic risks and manage complications”.
“The ability to manage these situations is not gained from theoretical teaching alone. It develops through years of medical education, work in emergency departments, eye clinics, inpatient services and ICUs, and through close collaboration with physicians, surgeons and GPs.”
ASO CEO Ms Katrina Ronne said the stakes could not be higher and the OBA proposal and reaction to it was “a defining moment for patient safety in Australia. Once these changes are locked in, they cannot easily be undone. We are calling on every Australian who values safe, high-quality healthcare to make their voice heard before it’s too late.”


IN BRIEF
EDOF CONTACTS CLEARED
The US Food and Drug Administration (FDA) has cleared the first daily disposable soft contact lens for presbyopia that uses extended depth of focus (EDOF) optical design technology, enabling commercial distribution in the United States According to a Business Wire announcement, the Deseyne (vifilcon C) daily disposable soft (hydrophilic) contact lens for presbyopia has been developed by the Cataltheia Group and its US subsidiary, Bruno Vision Care LLC. It said the lens was the first and only daily disposable contact lens for presbyopia to use patented EDOF technology. Cataltheia Group co-founder and CEO Eddie Catalfamo said the FDA clearance represented a significant step forward in non-surgical presbyopia correction..
TRAINING RATES HIGHLY
Medical trainees have rated the quality of their medical training highly in the latest Medical Training Survey, but the rate of bullying, discrimination, harassment and racism has remained unchanged. The annual Medical Board of Australia (MBA) survey reveals the insights of more than 18,000 trainees, including those studying to be ophthalmologists. It said 89% of trainees rated the quality of their clinical supervision very highly, and 86% rated the quality of their teaching and education sessions as good/excellent. But it said the rate of bullying, discrimination, harassment (including sexual harassment) and racism was unchanged from the previous survey at an average of 30%.
EXCELLENCE HONOURED
Nominations are open for the 2026 Endeavour Awards, Australia’s premier celebration of excellence and innovation in manufacturing and, for the first time, the healthcare sector is included. Innovators in Australia’s healthcare and eyecare sectors are invited to nominate for the new Innovation in Health Technology Award, which recognises technologies that improve healthcare and medical manufacturing. This category is for companies developing innovative health solutions, including medical devices, digital health platforms, biotechnologies, and pharmaceuticals. Eligible technologies must have undergone advancements within two years before nominations close on 13 February 2026, and products and technologies must be manufactured and/or commercially available in Australia. Those keen to know more can visit endeavourawards. com.au.
TREASURERS BACK SCOPE OF PRACTICE CHANGES
Optometry Australia (OA) has welcomed the announcement that Australia’s state and federal treasurers support reforms that enable health practitioners to work to their full scope of practice, as included in the updated National Competition Policy Federation Funding Agreement Schedule.
Federal Treasurer Jim Chalmers and his state and territory counterparts agreed in December to support the reforms in order to improve productivity and reduce costs in the health sector.
OA said the inclusion of full scope of practice reforms reflected growing national recognition that enabling the health workforce to use its full training was essential to strengthening access and reducing system pressures.
As outlined in the schedule, this includes streamlining regulatory processes and appropriately recognising the skills, experience and qualifications of workers, and ensuring Australians can access high quality and sustainable health and care services by removing unnecessary barriers to mobility and

Australia’s
supporting consumers to choose the most suitable provider.
Ms Skye Cappuccio, who stepped down as OA CEO at the end of 2025, said: “This is an important acknowledgement that full scope of practice is not just beneficial for patient care – it’s fundamental to a modern, efficient health system.”
OA said it looked forward to working with commonwealth, state and territory treasurers, health ministers, regulators and sector partners to ensure these productivity-boosting reforms translated into practical, on-the-ground improvements in access to essential eye care for all Australians.
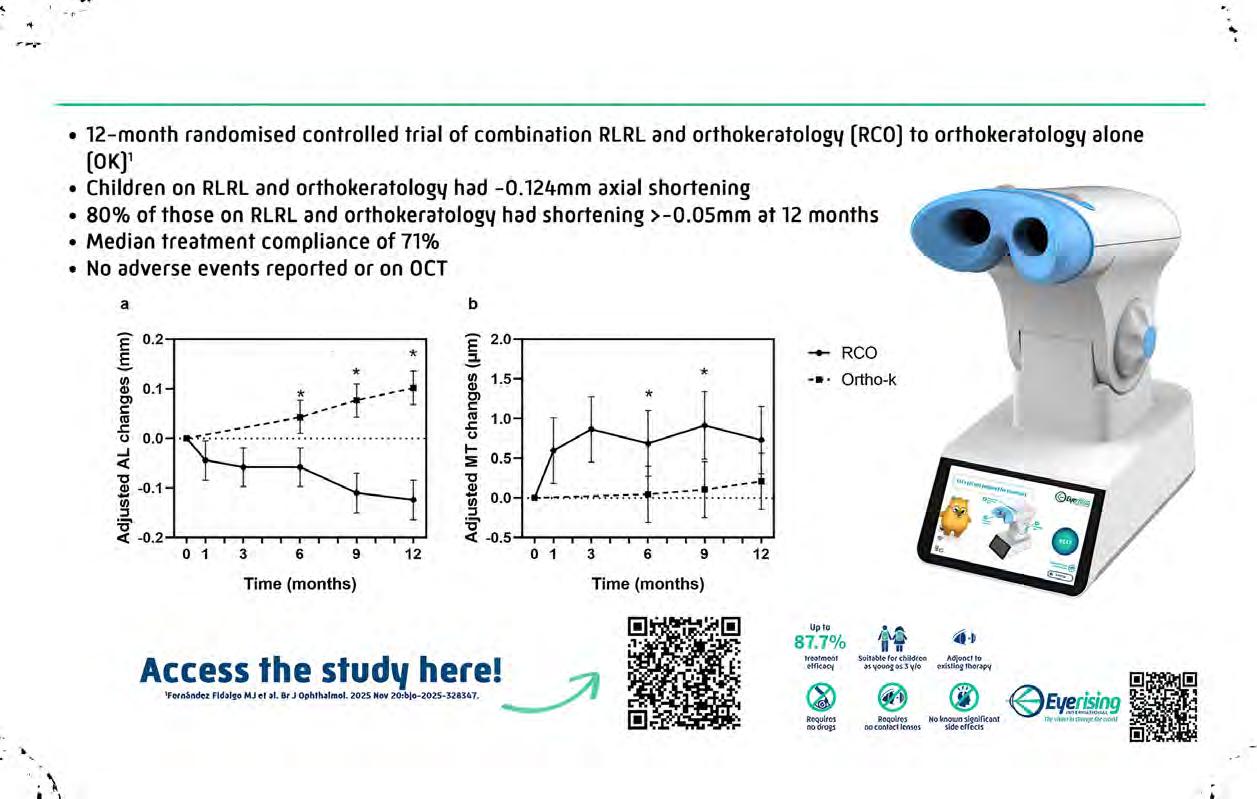
STUDY HAS ‘SIGNIFICANT IMPLICATIONS’ FOR MYOPIA

Researchers have found that increased time outdoors provides limited protection for premyopic children.
The goals of the investigators in Shanghai, China, were to provide evidence-based recommendations for myopia prevention, as well as reduce the prevalence of potentially pathological high myopia in the longer term.
LIGHTFIELD STUDIOS/stock. adobe.com.
To do that they observed 3194 children in Shanghai between the age of six and nine, who all wore wristwatches to monitor time outdoors from 2017 to 2018.
The children were either premyopes or hyperopes. Participants were all examined for cycloplegic refraction and myopic shift was studied from baseline to a one-year follow-up.
Hyperopes showed reduced myopic shift with increasing outdoor time (plateau at about 120 minutes per day).
But premyopes exhibited a J-shaped relationship between time outdoors and myopic shift, the study said.
In comparison to the subgroup with daily time outdoors of less
than 60 minutes, the difference in spherical equivalent change in the other subgroups was not statistically significant. The reduced myopic shift was only observed with time outdoors greater than 120 minutes per day, although it was still not statistically significant, said the researchers.
“We found that time spent outdoors had a limited protective effect on myopic shift among premyopic children,” said the researchers in the Shanghai Time Outside to Reduce Myopia (STORM) study, which has been published in the British Journal of Ophthalmology
“This finding reveals the unique dynamics of myopic shift within the premyopic population, highlighting the need for more intensive interventions.”
They concluded that the findings held “significant implications for future myopia prevention efforts”.
“While the protective effects of time outdoors are clear for children with hyperopia, the protective effect of time outdoors on myopic shift among children with premyopia is more limited and was only seen with longer durations of time outdoors.”
Researchers monitored more than 3000 children. Image:
state and federal treasurers have given their support to expanding scope of practice for health professionals. Image: IMAGE/stock.adobe.com.
optomap®
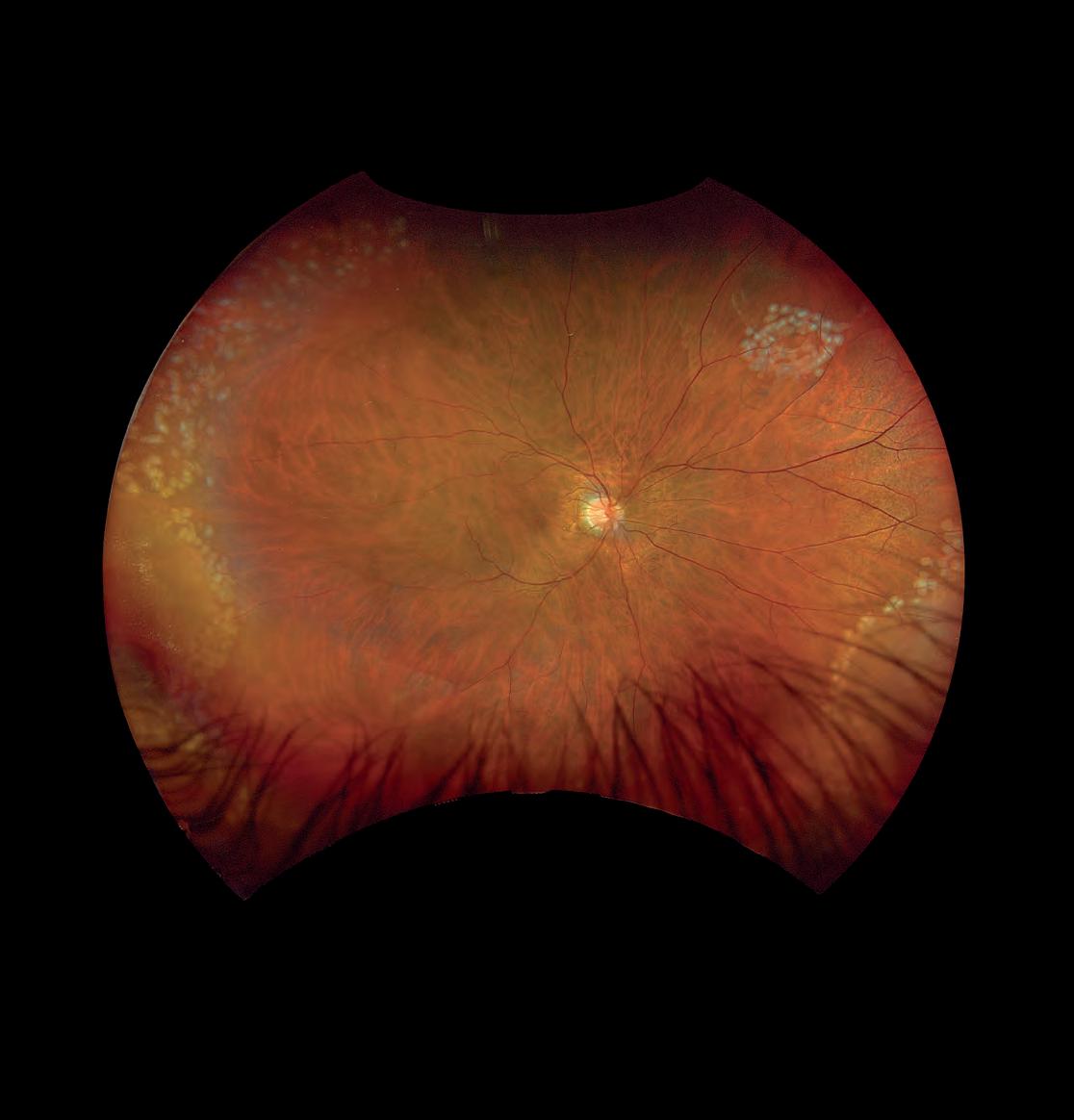
optomap®, the ONLY single-capture, 200° ultra-widefield retinal image





Finding indispensable dispensers
Surveys suggest many optical dispensers are seeking better conditions, pay and recognition. Now parts of the industry are starting to report that experienced staff are difficult to find. Insight takes a look at the issue.
Mr James Gibbins admits his home office is a bit of a mess.
The accumulated detritus is, in part, the result of his passion for the optical industry and possibly a bit of inattention after many days away from home.
The career optical dispenser and co-founder of the Australasian College of Optical Dispensing (ACOD) is surrounded by containers stacked full of frames and other optical odds and ends.
“The house is full of optical,” he says. “The garage is full of tubs and tubs of frames, and under the house there's more tubs.”
Along with Mr Chedy Kalach, the other founder of ACOD, few others have done more to advance the cause, promotion and training of optical dispensing in Australia than Gibbins.
But despite that pair’s hard work in Australia and New Zealand, and Gibbins’ well-known and infectious enthusiasm for dispensing and the optical sector in general, challenges remain.
ACOD trains hundreds of dispensers each year, putting many through its now well-established Certificate IV in Optical Dispensing; Optical Dispensers Australia (ODA) works just as hard to introduce even more to the industry through its own Introduction to Optics training, various promotions, and advocacy since forming four years ago.
But both organisations are echoing concerns from some parts of the industry: there may be a tick over 7000 optical dispensers in Australia – according to Australian Taxation Office (ATO) data – but
some employers are finding it increasingly difficult to secure and retain highly trained, experienced professionals.
And both believe that could be problematic. While there are many small and large employers who support their staff through a Cert IV, some continue to underestimate the value of an experienced or trained dispenser and also the loss of opportunity to their businesses.
The reasons, say Gibbins and ODA CEO Ms April Petrusma, are many: the lack of a clear training and career pathway; low, “unfair” pay that doesn’t reflect the complexity of the role; workplace culture in some practices that can cause burnout; and ongoing structural issues that haven’t kept up with the progression of the job title.
But Petrusma and Gibbins believe it probably boils down to one primary issue: the lack of value and understanding associated with dispensing and dispensers.
“A good, experienced dispenser brings far more to a practice than many people realise,” says Petrusma.
“Their expertise directly influences patient retention, revenue generation,
and enhances the overall reputation and credibility of the practice.”
Often they are the first and last point of contact for patients – “their communication, problem-solving and dispensing knowledge sets the tone for the entire patient journey”.
Ignoring that can come at a cost to a practice, says Gibbins.
“A great dispenser will drive up sales, sell premium lenses, minimise mistakes and remakes, and help put the reputation of the practice through the roof.”
Since establishing ACOD in 2017, Gibbins and Kalach have both worked hard to raise the training and reputations of their students, and hopefully their prospects in the industry.
After taking a bit of time to build up their own profiles, not even COVID-19 could dent their momentum, particularly in Australia, as governments encouraged people and businesses into training with subsidies and support.
Last year, the course produced 278 graduates, a mix of young and old, dispensing newbies and veterans.
Despite those record numbers, Gibbins
“A good, experienced dispenser brings far more to a practice than many people realise. Their expertise directly influences patient retention, revenue generation, and enhances the overall reputation and credibility of the practice.”
April Petrusma Optical Dispensers Australia

James Gibbins instructs his students during one of the Australasian College of Optical Dispensing workshops.
Image: Prime Creative Media.
Images: April Petrusma.

Some experienced optical dispensers go on to practice management and ownership, but others leave for different industries for better pay and conditions.
believes he and Kalach are barely scratching the surface of those who could, and possibly should, take up the training.
That education would allow what Gibbins estimates to be about 10,000 optical assistants in Australia to become dispensers, with a formal qualification and a great deal of technical knowledge to support their practices.
“We have thousands of optical assistants who've been employed for six months, 12 months or 10 years out there doing dispensing, unsupervised,” he says.
“You can train someone up to do simple readers or whatever fairly quickly, but when prescriptions become more complex, stronger, heavier, more prism elements and so on, they're lost, and they will accidentally make mistakes because they're untrained.”
That could mean spectacles that customers can’t wear, more lab work and costs, and reputational damage for the optometrist.
Despite that risk, Petrusma says many employers are still reluctant to support their staff through formal training, leaving employees to take control of their own development, which has long term detrimental effects.
“Training is inconsistent, with many dispensers expected to upskill in their own time without recognition,” she says..
“Many dispensers complete their Certificate IV or engage in CPD learning only to find that employers do not offer any financial recognition or
pathway progression in return.”
That lack of “financial recognition” is reflected in both ODA’s own surveys and the most recent income figures from the ATO.
ATO’s stats for 2022-23 showed that while ophthalmologists were again the highest paid medical professionals in the country, optical dispensers were some way further back in the ophthalmic sector, with an average income of $45,490.
Despite a rise of close to 7% on the previous year, Petrusma says the average dispenser’s wage sits only marginally above the national minimum wage.
That had contributed to the loss of many experienced dispensers, with some moving on to practice management and ownership but many simply leaving for other industries with more pay and greater career progression.
Many came into dispensing from other retail businesses, bringing great people skills and attention to detail, and Gibbins believes many have headed back there for better prospects.
So what needs to be done to raise the value of dispensing and with it the incomes and career pathways to keep talented people in the industry?
ODA believes one core issue is that the profession is misclassified as a retail rather than health role.
“Pay often does not match the skill and responsibilities of the role, especially in practices where dispensers are paid under
“Optometrists’ lifestyles are built on the dispensing sales, not their consultations.”
James Gibbins ACOD
the General Retail Award rather than an appropriate health-related classification,” says Petrusma.
“All of this is compounded by award ambiguity – ODA’s own investigations with the Fair Work Ombudsman found that classification should depend on duties, yet the official guidance remains unclear.”
Gibbins agrees.
Many of his students already have some retail experience but need greater optical and technical knowledge not always available in “on-the-job training” in busy practices.
“We need every new employee to be told you're on a pathway under supervision, you're going to do the Certificate IV in three or four months,” he says.
“Every other industry with traineeships, you go into your formal training within months. In optical, some employees like to wait two, three, four years.”
Both believe that training should also be rewarded.
That would help bring more people into the role, and keep them there longer.
“Optometry has a clear, well-established educational pathway, while dispensing remains far less visible as a professional career option,” says Petrusma. “Many potential candidates simply don’t know that dispensing exists.”
She believes meaningful improvement begins with recognising the true value of the role.
“Employers must provide competitive, transparent pay; invest in formal training; and create visible, structured career pathways,” she says.
“Workplace culture also needs attention – staff stay where they feel respected, supported and trusted.”
Gibbins says parts of the optical sector have been resistant to change, but he believes younger staff, managers and owners may have an influence on that.
For those who do, there are plenty of rewards and opportunities.
“Practice owners who actively track metrics like AOV (average order value), remake rates and patient return rates usually recognise how profoundly a skilled dispenser contributes to both patient outcomes and business success,” says Petrusma.
“But the buck doesn’t stop with a sales report – activities such as rapport building, troubleshooting, or even ensuring a problem-free handover rarely show up on a spreadsheet, yet they have enormous downstream impact.”

Gibbins says the optometrist and their clinical work is key to the business, “but the business gets generated by the spend”.
“Optometrists’ lifestyles are built on the dispensing sales, not their consultations.”
And if they are trained, treated well and stay in the sector, many of those great dispensers can become excellent practice managers, partners and owners.

Image: Fxquadro/stock.adobe.com.
Images: James Gibbins.



Scan QR code for references
* Trademarks are the property of their respective owners.
† Based on in vitro studies where TOTAL1™ was compared with PRECISION1™, Infuse*, ACUVUE OASYS MAX 1-Day*, ACUVUE OASYS 1-Day*, BioTrue ONE Day*, 1-Day ACUVUE MOIST*, clariti 1-Day*, MyDay* (39, 30, 18, 16, 16, 12, 7, 6, 5 seconds respectively) and TOTAL30™ was compared to AIR OPTIX™ Plus HydraGlyde™, Bausch+Lomb Ultra*, ACUVUE Vita , ACUVUE OASYS , Biofinity (27, 19, 15, 14, 9, 6 seconds respectively) wherein wettability was measured in seconds using the iDDrop System.
‡ Daily disposable lens data based on in vitro studies wherein wettability was measured using the iDDrop system (p<0.05).
All lenses were tested in an identical manner, soaked in a phosphate-buffered saline (PBS) solution for 16 hours +/- 2 hours (p<0.05).
§ Reusable lens data based on an in vitro study wherein wettability was measured using the iDDrop system (p<0.001).
All lenses were tested in an identical manner, soaked in a phosphate-buffered saline (PBS) solution for 16 hours +/- 2 hours (p<0.001).
Two brothers, one vision
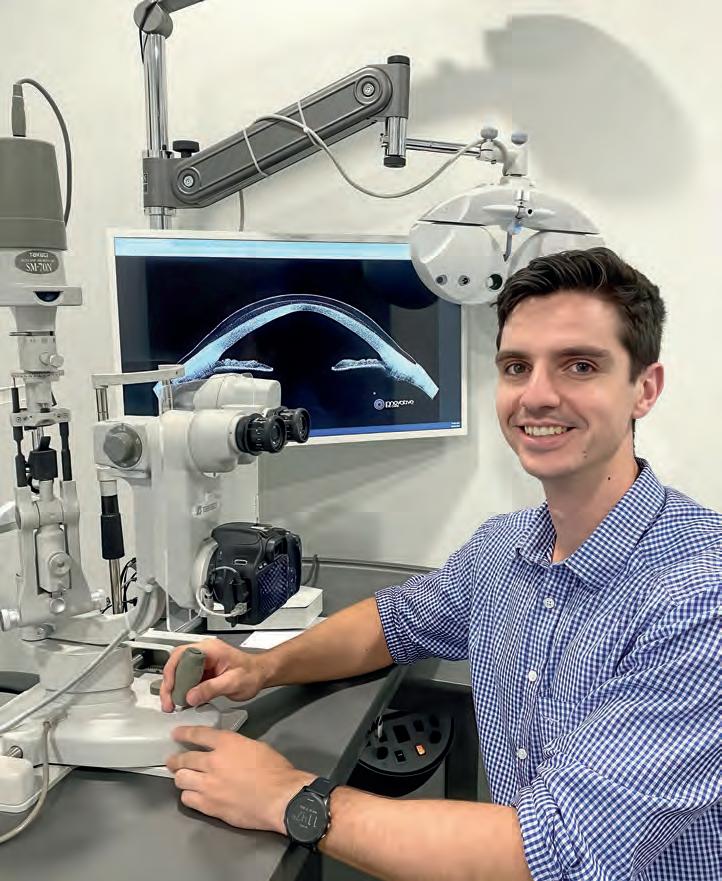
Two young optometrists are redefining early-career independence, launching a revitalised community practice in Perth and proving that ambition, teamwork and determination can propel new graduates into successful ownership.
When brothers Mr Steven and Leo Ho opened the doors to their new Perth practice in early November 2025, they were doing far more than launching a business.
They were fulfilling a shared ambition since their optometry student days, taking an unusually early step into independent practice, and – without intending to –becoming the ‘poster pair’ of what’s possible for young practitioners willing to take the leap.
Their practice, Noranda Optometrist, is a reinvention of a longstanding community clinic previously known as Noranda Eyecare. While the Ho brothers are only a few years out of university, their first month of operation proved that the community was ready for the next chapter: patient books filled almost immediately, former patients returned in strong numbers, and online chatter amplified their arrival.
For Leo, who has been working rurally in Emerald and Roma in Queensland while helping run the practice remotely, the decision to pursue ownership so early was driven by both timing and determination. For Steven, already working in Western Australia, it was the natural progression of a plan the brothers had shared for years.
“It was always a dream for both of us. We studied optometry because we wanted to open a family practice and hopefully inspire younger people to chase their goals,” Leo says.
REBUILDING A PRACTICE FROM THE INSIDE OUT
Both brothers completed their optometry degrees at Queensland University of Technology (QUT), where each served as president of the student society – roles that gave them strong networks among young optometrists nationwide.
Steven graduated in 2022 and moved to WA for work; Leo graduated in 2024 and took a rural clinical route, serving as the sole optometrist in remote Queensland towns.
As soon as Leo graduated, the brothers began scouting opportunities. Steven’s locum work in Perth meant he had a good sense of which practices might be changing hands. Their breakthrough came when they discovered the owner of Noranda Eyecare, a respected independent in Noranda Shopping Village, was preparing to retire after 28 years. The opportunity was clear, with strong goodwill, a large established patient base, and deep community loyalty. At the same time, the previous clinic

had limitations – no website, an ageing shopfront and a space in need of a major update. When the shopping centre offered the Ho brothers a larger, vacant tenancy just a few doors down, they took a bigger leap than first expected: instead of refurbishing, they would build a brand-new practice.
The process became an intensive education in planning, design and budgeting.
“We really had no idea where to start,” Leo admits, “but we knew we had to find a designer, communicate with the shopping centre, organise drawings and quotes, and just keep moving forward. There’s a lot to consider, but once it gets going, it’s going.”
Their first step was finding a designer; from there came weeks of drawings, approvals and builder quotes. Planning display areas, reception, diagnostic equipment layout and clinical rooms required countless decisions and constant coordination with centre management.
Working within the financial constraints of new graduates, the brothers hunted widely for second-hand diagnostic equipment. They purchased a slit lamp and chair from a WA practitioner closing his clinic, secured a CenterVue DRS fundus scanner, sourced an autorefractor, and bought a frequency doubling technology (FDT) visual fields machine. They are now on track to acquire their Revo FC, an advanced system that combines OCT, fundus photography, axial length measurement, and more into a single automated machine. This is a major step forward they’re incredibly excited for.
“We knew we were on a budget, so we searched everywhere – Facebook, online ophthalmology forums, retiring practitioners – just to piece together the equipment we
needed to get off the ground,” Leo says. “Once we generate a good revenue stream, we’ll definitely upgrade our equipment.”
They planned two consulting rooms but are operating with one while the practice is establishing itself. A key strategic decision was maintaining continuity by hiring the long-serving dispenser from the previous practice. They also arranged for the retiring optometrist to continue consulting one or two days a week. This gave the community confidence and helped transfer goodwill directly into the new business.
“We were very fortunate to have the previous owner’s patients follow us straight away. Our book was full in the first month,” Leo says.
Creating a retail space that looked premium but remained accessible was another deliberate design choice. Frames start at $180 – an intentional balance to surprise patients who might assume a higher price point based on aesthetics alone.
Behind the scenes, Leo and Steven have divided responsibilities around their geographic realities. Steven has handled all on-site management and fit-out tasks. Leo, based in Queensland until January, has managed administration, stock, bookkeeping and all remote tasks.
“Anything that needed to be done in person, that was Steven,” Leo says. “Anything that could be done online or through phone calls, that was me.”
A NEW GENERATION OF INDEPENDENTS
The Ho brothers’ story has attracted attention from younger optometrists because it challenges the idea that
Brothers Leo (left) and Steven Ho opened their practice in 2025.
Images: Photo by Monday Media Joondalup

practice ownership must be a late-career milestone. Their visibility isn’t accidental: both built strong peer networks through student leadership, and Leo maintains an active presence on social media, sharing humanitarian optometry and insights from eye disease cases he has managed as a new graduate, which is followed by optometry students and new graduates across Australia.
“Younger people are already feeling burnt out before they even graduate,” Leo says. “We wanted to inspire them – to show it’s possible to open your own practice and be independent.”
One message he emphasises is the importance of partnership. “Doing this alone is very difficult,” he says. “Sharing the workload makes it manageable.”
Co-directorship has shaped every aspect of their workflow, allowing them to balance the intensity of establishing a new business.
Marketing for the practice is a blend of strategic and organic. They worked with a digital agency known within WA’s independent optometry community to build their website and run initial paid advertising campaigns. Simultaneously, their social media networks generated natural interest among peers and patients.
Clinically, both brothers bring strong skills acquired from their mixed experience, with plans to expand into more specialised areas. Myopia management is a major focus for their second year in business, with the goal of purchasing a corneal topographer and building a dedicated program. Establishing relationships with local ophthalmologists and GPs is already underway.
Looking ahead, their first-year priorities include upgrading equipment, consolidating their patient base, and refining their operations now that both brothers are based in Perth, following Leo’s relocation in January 2026. They also hope to speak at universities and conferences, sharing the practical realities of early-career ownership with students and graduates.
“It’s ambitious,” Leo acknowledges, but the brothers see value in showing a realistic pathway for young optometrists wanting autonomy. Their journey is grounded in a simple idea: start small, work hard, and build momentum step-by-step.
Reflecting on their experience – from fit-outs and contracts to interstate logistics and second-hand equipment searches – Leo says the biggest hurdle was simply beginning.
“Once we got started, there was no going back.”
Co-founder Steven Ho moved to WA after graduating from QUT in 2022.



Mind the (generation) gap
New research suggests there are many challenges when encouraging different age groups into contact lenses. But for those practices willing to tailor their messaging, there are also good opportunities for practice and patient.

If men are from Mars and women are from Venus, where on earth are young people from?
It’s a question that has troubled society for hundreds of years, with each generation seemingly befuddled by the practices and rituals of the others around them.
However, new research from the US-based Contact Lens Institute (CLI) suggests that as strange and foreign as those age-groups might be, there is good reason for optical practices to do what they can to bridge that generation gap.
Before we dive in, let’s establish a few numbers that will be key to understanding this article.
Gen Z, or Generation Z, refers to a cohort of people born between 1997 and 2012, meaning they will be the ones entering your practice aged between 13 and 28 years old.
They are the successors to Millennials, also known as Gen Y, who were born between 1981 and 1996, making them aged between 29 and 44.
Last, but certainly not least to many optical businesses because of their ongoing age-related vision issues, is Generation X.
Born between 1965 and 1980, they are the 45 to 60-year-olds moving a little less quickly through your practice doors.
The CLI survey and the report that has followed it – Shifting focus: Generational perspectives of contact lenses and eye care – found some similarities in the buying practices and attitudes among those three distinct age brackets.
But it also found plenty of differences among the 1308 people polled, and some significant opportunities for practices promoting contact lenses, including the often tricky subject of dual use – patients alternating between spectacles and contact lenses.
The trick appears to be about modifying
the language and the narrative for different generations.
The data indicates that contact lens use is greater for Millennials, with 43% of that age bracket surveyed wearing them.
The youngest grou is just behind them on 35%, with the older cohort quite a way back on 22%.
The CLI says the Millennials’ figure “paints a picture of what may be possible with Gen Z”.
That gap, and the opportunity it represented, was similar when respondents were asked about dual use of spectacles and contact lenses, with 52% of contact lens-wearing Millennials favouring them over glasses, compared with 45% of Gen Z.
In a section of the report titled Gen Z Upside, the CLI said the eight-point gap (43% v 35%) represented “considerable unmet upside in patient volumes, practice revenue, and wearer lifestyle benefits”.
To offer some context, population data shows there are about 2.5 million people in Australia aged between 13 and 28; 8% of that would be about 200,000 potential patients.
The CLI report said three values ranked highest across all ages: affordability (85-89%), convenience of purchase (69-73%), and speed to obtain the product (66-71%).
Practices were encouraged to keep a tight focus on delivering in those key areas.
But the report goes a little further
to demonstrate where those generations differ in their attitude and shopping priorities.
Gen Z and Millennials are influenced more than their older Gen X peers in four areas: brand authenticity (Z: 63%, M: 63%, X: 54%), individual expression and personalisation opportunities (Z: 58%, M: 55%, X: 45%), brand social responsibility (Z: 51%, M: 47%, X: 33%), and living for today (Z: 48%, M: 48%, X: 39%).
The report says practices that tailored their communications and marketing activities along and around those ‘values’ can better engage with younger patients.
One of the biggest drivers for younger clients is social responsibility, which was a strong influence for about half of the younger generations but only a third of the older population.
According to the research, a large number of Gen Z respondents were motivated by a brand’s inclusive culture (52%), its environmental responsibility (49%), and diversity (47%), with staff diversity, philanthropic initiatives, and community involvement ranking slightly lower (43%, 42%, and 42%, respectively).
Results were similar for Millennials, but not so much for Gen X, for whom responses hovered between the mid-20% and low 30% range.
When examining the reasons for contact lens wear, of the 443 contacts users in the survey, Gen Z respondents said personal
“The younger guys, they're playing hockey, they're playing soccer, they're doing night games under lights – some of the sports won't allow glasses on the field and contact lenses are ideal.” Martin Robinson Martin’s Eyecare

Images: Martin Robinson.
Daniel Moriarty believes in patience and ‘planting the seed’.
appearance (52%), freedom from glasses (47%), and a lack of visual obstruction (40%) were their top three factors.
Millennials voted for personal appearance (50%), freedom from glasses (48%), and better comfort and ease of use (both 48%).
Gen X weighed in with freedom from glasses (54%), a lack of visual obstruction (53%), and better comfort (41%).
Of interest, optimal vision was ranked around the middle of the 12 “reasons to wear” (Z: 34%, M: 30%, X: 29%).
The CLI says this suggests that “highlighting contact lens lifestyle benefits while also reinforcing their optical advantages may promote uptake and retention”.
The two younger generations showed interest in other categories, including contact lens advancements, whereas the response of Gen X was more “muted”, with percentages lower by double digits.
Much of this comes as no surprise to three optometrists whose practices have a strong focus on contact lenses.
That expertise is what brings a lot of motivated patients into their businesses.
Mr Martin Robinson in Tasmania, Mr Daniel Moriarty in South Australia, and Mr Adam Barron in Queensland work in practices well known for fitting specialty lenses.
They see plenty of irregular corneas, keratoconus, myopia and dry eye, and patients referred to them for
orthokeratology, scleral and rigid contact lenses.
But they also deal with plenty of patients for whom contact lenses are as confusing and scary as those different generations around them.
MOTOROLA MEETS IPHONE 14
Robinson is nodding sagely as we discuss the CLI research and the implications for his and other practices.
The president of the Cornea and Contact Lens Society of Australia and man behind Martin’s Eyecare in Hobart sees plenty of X, Y and Z at his independent practice.
And he understands the need to modify his language, depending on which letter is sitting in front of him.
He knows he’s more likely to get a “hard no” from Gen Xers on contact lenses, which confirms their lowly status in the CLI research.
But he also believes an opportunity remains with that group.
“Gen X, that’s my generation,” says the 50-year-old.
“Many wore contact lenses when they were younger but stopped wearing them 20-30 years ago because they hurt their eyes or their eyes were dry or had irritation.”
To counter that, Robinson explains the technological advances in that time, and that there are now new contact lenses that will suit them and solve their problems.
“The comparison is like the difference between a Motorola handheld phone and an iPhone 14 – there's a hell of a lot of technology between those two phones.”
He agrees that the motivations of younger generations are very different and need to be understood and addressed.
“I've got kids that are fearless, they’re happy as Larry and there's no dramas with contact lenses.
“I've got other kids that are in their teenage years, that are so frightened of contact lenses they induce a vasovagal reflex (a sudden drop in heart rate and blood pressure) and they pass out in the fitting process.”
Often that’s a result of “nonsense, fake stories floating around” on the internet and in their social channels.
But there’s some real frights too.
“Did you see that story about that woman who had 24 contact lenses stuck up under a lid?” he says. “There’s almost a generation of people that have watched that, and they are really scared and don't try contacts.”
So he addresses their “hidden fears”, and “if you can solve that and answer that problem, they will jump in and try the lenses”.
It’s also about addressing lifestyle and the active sports of the younger generations, rather than the often more slow-paced pastimes of their older counterparts.
“Older people, we’re more likely to play a round of golf,” says Robinson.
“The younger guys, they're playing hockey, they're playing soccer, they're doing night games under lights – some of the sports won't allow glasses on the field and contact lenses are ideal for those guys.”
Environment and social concerns are other influences where the attitudes of younger and older generations diverge, as highlighted in the CLI survey.
“The Gen-Xers may not be particularly
Adam Barron says younger patients are keener to give contact lenses a try.

Image: Heron Eye Care.
Image: Daniel Moriarty.
motivated about environmental concerns,” Robinson says. “The young ones are absolutely aware of it.
“They are going to be more aligned with a lens that's healthy for the environment, that's going to have less environmental impact, and they are interested in the ethical, moral aspects of certain contact lens companies – their zero-waste approach.”
PATIENCE WITH YOUR PATIENTS
Mr Daniel Moriarty is a young man blessed with the patience of those many years older.
Like Robinson, the 27-year-old optometrist at South Australia’s Innovative Eye Care sees plenty of keratoconus, myopia and dry eye.
Many of his patients are referred to the practice by ophthalmologists, GPs and other optometrists less familiar with contact lenses.
Those ones tend to be “pretty motivated”, he says.
But he also deals with plenty of patients reluctant to try on contact lenses, a problem for many practices around the country.
And sometimes he has to be a little more patient.
When one of those clients complained of short-sightedness but balked at wearing contact lenses, Moriarty decided to play the long game.

“I just sort of planted the seed,” he says. “We put lubricating drops in her eyes, just to get something in her eyes. And then, the next year rolled around and she was ready to go, ready to give contact lenses a try.”
A little more patience is needed when dealing with the older generation as well.
“I think if you try to fit someone that's probably a little bit older, they might be more resistant, because it's going to potentially be challenging to handle lenses,” he says.
“If you're patient with them, there's not really too much of an issue . . . if they're not keen, as long as you plant that seed, I think you'll find that they’ll be keen next time you see them.”
His younger patients, on the other hand, are much more likely to give it “a crack”.
Many have already tried contact lenses as part of their ortho-k treatment, which helps soften their attitude when they move beyond the rigid version.
“You get a lot of the younger patients whose attitude is just to give it a try.”
He says they are also more likely to be keen on mixing and matching their spectacles and contact lenses.
Older patients, possibly recalling the stigma of wearing glasses when younger, are more likely to favour contact lenses.
But frames are now much more stylish, modelled by plenty of popular influencers and now socially acceptable.
“They are just more fashionable and the
younger patients probably don't have that trauma.”
B UILDING TRUST – QUICKLY
Barron has also noticed differences between the generations in attitudes towards contact lenses.
The senior optometrist at Heron Eye Care in Toowoomba, Queensland, says he treats a “conservative demographic”, with a fair percentage of his patients over 50.
“And that can be pretty heavy going in the contact lens space,” he says.
“You've got to have a pretty damn good multifocal on board – the older generation appreciate that because they get better acuity and less eye strain with computer use.”
Gen-Xers are keener on price and convenience and prefer to do their shopping, including optometry services, closer to where they live.
“And as soon as you go older than that, that's when comfort becomes really, really critical.”
Price is less of an issue with Millennials, he says.
“They're normally pretty busy people, and they want things to work, so you’ve got to tick those boxes – they want good stuff.”
He finds the youngest cohort are more likely to mix and match their shopping with online purchases.
But as the others have pointed out, they are also more likely to give contact lenses a go, which can make then ideal to work with.
Older people are more reluctant to try contact lenses but opportunities remain.
“It’s usually single-focus lenses, which are dead easy,” says Barron. “Also nice, super easy corneas; their tear pillows are more likely to be better, it's probably going to be easier to fit.
“From an ocular surface point of view, from a refractive complexity point of view and vision comfort, they're more likely to be more dexterous.”
He too hears plenty of nonsense from all generations about “big, scary and uncomfortable” contact lenses.
“We try to control that within our consult rooms.”
He finds that once patients are in the clinic’s “inner sanctum”, optometrists are able to “delete all the rubbish that's associated with any kind of pressures and just be blunt with people”.
That is about building a level of trust that transcends the generation gap.
“No person on the planet comes in with a placard saying, ‘I want contact lenses’,” he says.
“Our most valuable commodity as clinicians is trust.
“If you're going to put a 14-millimetre slice of plastic in someone's eye, they have to trust you, and you have to build that trust as fast as you possibly can with every single patient, whatever their age.
“The pillars of successful contact lens sales are good vision, good comfort and good handling – if you can nail those three things every single time, you will have a very successful contact lens practice.”
Image: Syda Productions/stock.adobe.com.

Laying down the Ultra challenge
Bausch + Lomb believes it has the product to improve the vision and lifestyles of many presbyopes. Now it is calling on optometrists to take another closer look at contact lenses, in the interests of their patients and practices.
Depending on what angle you are looking from, encouraging Australian practices and patients to use contact lenses is either a massive challenge or a grand opportunity.
Mr Simon Hanna, Bausch + Lomb’s (B+L) national professional services manager in Australia, likes to think of it as the latter.
But he knows he has his work cut out.
In other parts of B+L’s global marketplace, contact lenses have greater penetration –for instance, adoption rates in the US are approximately 17%.
In Australia, it’s more like 5-13%, and there is plenty of historical hesitancy towards contact lenses in patients and even practices.
But Hanna has good reason to be optimistic and favour opportunity over obstacles.
He not only has a proven product featuring advanced technology, he also has the clinical and observational data to back the company’s claims that the contact lenses will help patients see and feel better.
B+L launched its Ultra One Day Multifocal contact lenses in May 2024. That followed the arrival of its spherical version a few years earlier.
The latest lens design ticked all the boxes – it is entered in the Australian Register of Therapeutic Goods (ARTG 341559 ) and featured plenty of innovative technology to tempt both practice and patient.
That innovation includes a next-generation material called kalifilcon A, with Advanced MoistureSeal technology to deliver “a highly wettable surface and excellent breathability for healthy lens wear”.
The Advanced MoistureSeal technology works with a breakthrough ComfortFeel innovation the company says infuses the lens with eye health ingredients such as
moisturisers/conditioners, osmoprotectants and electrolytes.
It says this helps to deliver comfort for a full 16 hours of lens wear and support a stable and healthy ocular environment.
But Australia remains a tough market for contact lenses, so Hanna and the company knew they would need extra evidence to convince practitioners.
That came in the form of a field observation study undertaken in the US before the official launch of the Ultra One Day Multifocal lens –known as Infuse Multifocal.
The study sought the feedback of almost 300 early adopters and the practices supporting them.
Of those 290 contact lens wearers, 91% said the B+L product felt “incredibly soft, smooth and weightless”, with 90% agreeing that it allowed them to move “effortlessly” between various tasks throughout the day.
That supported other trials from the company demonstrating ease of fitting and comfort for both the daily and monthly lenses.

The clinical study showed 87% of patients could be successfully fitted in one visit and 99% in two visits, if the practitioner followed the fitting guidelines.
The research showed the Ultra One Day Multifocal contact lens provided clear vision at near and far distances in 80% of patients, as well as clear vision when driving at night for 75% of respondents.
“That gave us the confidence to go to market, knowing that the optometrists who are prescribing this are going to have quite a high success rate,” says Hanna.
He believes optometrists should also have plenty of confidence, knowing they’re prescribing a multifocal lens that’s able to improve the vision issues of many patients. The fact presbyopia is a growing category is a bonus.
“Our recommendation is that optometrists prescribe a lens, rather than let the patient decide or trial multiple ones and see what fits feels better,” he says.
“The optometrists really have that obligation to make sure they are prescribing what's best for their patients, and this is a premium, prescribed lens.”
To help practitioners build their confidence, not only in the B+L products but also contact lenses in general, Hanna has been conducting a number of education sessions and attending events around Australia.
Part of that is to help the sector understand the innovative technology in the B+L lens, but it’s also a chance to “bust a few myths” about contact lenses.
“This year we are talking to optometrists about this idea that patients with dry eye

Above: Bausch + Lomb’s Ultra One Day Multifocal contact lenses include a next-generation material called kalifilcon A, with Advanced MoistureSeal technology.
Images: Bausch + Lomb.
Simon Hanna has been demonstrating the value of contact lenses around the country.
have, historically, not been able to wear contact lenses,” he says.
“Because of the innovative technology of the materials and the ComfortFeel technology of the Ultra One Day lenses in particular, what we have found is that more and more people can wear contact lenses and not have that discomfort.”
“The ComfortFeel technology involves a unique combination of eye health ingredients which support the ocular surface and supports patients who are likely to have evaporative dry eye disease or have discomfort or dryness.
“This is also where the advanced MoistureSeal technology comes in,” says Hanna. “The hydrophilic wetting agents actually boost the water content of the lens to 55% and it optimises the wettability of the surface of the lens.
“And the lens material is a silicone hydrogel, which provides greater oxygen permeability.”
Comfort or the lack of it, is the number one reason people stop wearing contact lenses, he says.
“Patients generally don't drop out of contact lenses because of price, handling or convenience.
“They're happy to sacrifice some of their vision, but they're not happy to sacrifice comfort. ”
But patients don’t have to sacrifice any
vision with the Ultra One Day Multifocal lenses, says Hanna.
They can actually improve it.
The product is targeted at the growing cohort of presbyopic patients over the age of 40.
“Those people tend to have very different and demanding visual needs, depending on their lifestyle or their vocation.
“Their expectations are high – they go to the gym after work, they're going out, they spend a lot of time online and on their devices.”
To enable that and support vision across many different tasks, the Ultra One Day Multifocal lens features a 3-Zone Progressive Design , ensuring consistent focus at all distances with smooth transitions between zones.
In clinical testing, 90% of wearers agreed the lens allowed them to move effortlessly from various tasks throughout the day.
Hanna says they should perform well, and perhaps better than spectacles.
“The pair of glasses that sit on the outside of your face are static lenses.”
“The contact lens sitting on the cornea of the eye itself means that when the patient needs to look at something up close, their eye naturally goes to that centre zone,” he says.
“When they are looking in the distance their eye knows to pick up the outer circle of
the three-zone lens, so you're not having to find the sweet spot.
“So if you can get a lens that performs really well, like the Ultra One Day Multifocal does, in terms of its three-zones design, and it's comfortable because of the other proven technologies – the Advanced MoistureSeal and ComfortFeel Technologies – that's also really convenient in terms of a multifocal option.”
An option that makes sense for those looking to build their practice and business.
“The opportunity, it seems, is not just for B+L – patients and practices can benefit as well,” says Hanna.
“Contact lens patients generally will be patients that are more loyal to the business, people that will come back more frequently, and so you're more likely to see them and their family for regular eye conditions and routine eye checks,” he says.
“They tend to see their optometrists more frequently than the sort of once every two or three years for a normal eye test.”
“B+L has the product,” says Hanna. Will the industry take up the challenge and seize the opportunity?
• ALWAYS READ THE LABEL AND FOLLOW THE DIRECTIONS FOR USE.
NOTE: References are available upon request or in the online version of this article.

“Make this year all about your team, the real heroes of your business” “Want
Bausch + Lomb ULTRA® ONE DAY Multifocal
proven 3-Zone Progressive™ Design with a complete
contact lenses
and
technologies to
and
MoistureSeal® and ComfortFeel Technologies








FORECASTING THE FORCES DEFINING 2026
With therapeutic breakthroughs reshaping clinical expectations, deepening debate around workforce pressures, and sensory health becoming increasingly integrated, the events of 2025 have set the pace for an even more consequential year ahead. As Australia’s eyecare sector absorbs historic advances in geographic atrophy treatment, ongoing scrutiny of workplace conditions, and the rapid convergence of vision and hearing services, industry leaders are now turning their attention to 2026 – identifying the developments likely to redefine patient care, service delivery, and the profession itself.
THEO CHARALAMBOUS
Organisation: Optometry Australia, president
Area of interest: Optometry advocacy
Optometry in Australia is at an important crossroads. Encouragingly, our full scope of optometric practice, and the contribution our profession can and does make to community health, is gaining stronger recognition. At the same time, the sector faces significant challenges, particularly the need to address workforce oversupply and to ensure that workplaces enable optometrists to practise with clinical autonomy and genuine professional satisfaction.
Optometry Australia remains committed to leaning into both the opportunities and the pressures before us, while ensuring we are well placed to support the profession through any challenges that lie ahead. We will continue to advocate for fair and sustainable working conditions, a halt to further increases in optometry student numbers, and broad recognition of the full clinical scope of our highly trained and highly skilled profession.
APRIL PETRUSMA
Organisation: Optical Dispensers Australia, CEO
Area of interest: Optical dispensing
The 2026 rollout of the newly updated Certificate IV in Optical Dispensing course will play a major role in shaping optical dispensing education. After more than a decade without an update, the refreshed qualification better reflects current technology, patient expectations, and modern dispensing practices. With industry input collected throughout 2025, the new course will equip upcoming dispensers with stronger foundations and a highly relevant skill set – making it a significant milestone for both learners and employers.
Retention of experienced staff will remain a key challenge in 2026. Although wages improved over the past two years, continued progress is essential to keep the profession competitive. Encouragingly, interest in dispensing careers continues to grow through ODA’s pre- and post-employment initiatives, with the ‘ODA Introduction to Optics’ training program gaining significant traction from both within and outside of the industry.

Looking ahead, one of the major highlights for 2026 is the ODA Fiji Conference in July, uniting eyecare professionals for a weekend of learning, networking and cultural experiences. For the first time, delegates will enjoy engaging lectures and hands-on workshops all balanced with ample opportunities to relax, connect, and experience the spirit of Fiji.
PAUL BOTT
Organisation: Specsavers ANZ, managing director
Area of interest: Corporate optometry

In 2026, we will continue changing lives through better sight and hearing. Our ambitions include expanding advanced dry eye treatment, accelerating myopia management, embracing new technologies and continually upskilling our people to make great care even more accessible.
Over the past five years, we’ve completed 22.5 million eye tests, four million hearing screens and treated 65,000 patients’ eye conditions – impact that inspires our next chapter. This year, we’ll unveil a bold five-year strategy focused on prevention, accessibility, and innovation, overcoming challenges like workforce distribution and rising service demand.
References: 1. Results from a 20-site, 3-week study of Bausch + Lomb (kalfilcon A) Daily Disposable Multifocal contact lenses on 294 habitual multifocal soft contact lens wearers – B&L Data on file (2023). Study 916: A Study to Evaluate the Product Performance of a New Silicone Hydrogel Multifocal Contact Lens – Topline Results. 03 Mar 2023. Sponsored by Bausch & Lomb. 2. B&L Data on file (2021). Study 893: Product Performance Evaluation of a Novel Silicone Hydrogel Contact Lens: Kalfilcon A Patient Comfort and Vision Outcomes for subset of patients who reported wearing their lenses for 16 or more hours per day. 19 Feb. 2021. Sponsored by Bausch & Lomb. 3. Data on File. Sponsored by Bausch & Lomb. Rah, M. Ocular Surface Homeostasis & Contact Lens Design. (2021). 4. B&L Data on file (2019). Kadence International. April 2019. Results of a consumer symptoms survey of 318 silicone hydrogel daily disposable contact lens wearers. Sponsored by Bausch & Lomb. © 2025 Bausch & Lomb Incorporated. Bausch + Lomb ULTRA® ONE DAY Multifocal is a trademark of Bausch & Lomb Incorporated or its a liates. Bausch & Lomb (Lomb (New Zealand)
We’ll also continue to focus on our people and customers – we’re one of the best places to work in our nation and in 2025 were ranked the number one brand for customer experience by KPMG in Australia – and we want to continue this work. With 457 practices full of passionate team members, Specsavers will set new standards in clinical excellence and customer service, ensuring more Australians and New Zealanders experience life-changing care.

Image:
Theo
Charalambous.
Image: April Petrusma.
Image: Paul Bott.
ELIZABETH KODARI
Organisation: EssilorLuxottica, vice president, store operations, ANZ
Area of interest: Corporate optometry
I envision eyecare and eyewear continuing shifting toward a closer partnership between clinical services, technology and personalised customer experience. As AI enabled tools, medtech and advanced diagnostics become more common, optometry practices will evolve beyond traditional retail models and adopt new ways of delivering healthcare and answer customers’ needs. The industry will lean more heavily into practice and service differentiation, using innovation, and personalised care to build loyalty and elevate patient experience.
At EssilorLuxottica, wearable technology will remain a key pillar, as audiology and broader hearing care will keep expanding within optical settings, supported by brands like Nuance Audio Glasses and growing demand for more complete health solutions. Real challenge will be delivering consistency and capability at scale. 2026 will be a year of strong opportunity, especially for organisations that, like us, invest in their people, strengthen the link between clinical and retail teams and create simple, seamless end-to-end experiences.
TONY JONES
Organisation: ProVision, CEO
Area of interest: Independent optometry
As we move into 2026, ProVision is committed to taking a leading position and helping independent optometrists navigate an increasingly complex landscape through education, innovation, and tailored support. The strategic use of technology and AI can be transformative for the patient experience, patient outcomes, practice efficiencies, and business intelligence insights. Technology is only valuable when successfully adopted, however. Change management will be critical, and our sold-out PRISM26 conference in July 2026 addresses this directly, with sessions on AI-powered practices, prismatic leadership, future-thinking strategies, and rethinking patient connection in a data-driven world.

We'll continue to strengthen our recruitment and HR services, and wellbeing resources for members to help practices create fulfilling environments that attract and retain talent in a rapidly evolving workspace. Privacy and cybersecurity remain non-negotiable as digital integration deepens, and ProVision has invested in new tools for 2026 to help practices navigate these responsibilities. We've also refined our value proposition to deliver stage-specific support for independent optometrist owners throughout their practice journey, with exciting announcements coming soon.
PHILIP ROSE
Organisation: Eyecare Plus, general manager
Area of interest: Independent optometry
The need to use a variety of online platforms to reach patients with eye health and eye wear messages will be paramount in 2026. Myopia and dry eye management is going to be more mainstream and becomes a powerful differentiator and a strong revenue driver for the independent practices. Practices without specialty services will fall behind.
Retail focussed optical chains are increasingly telling the public that a trip to the optometrist is a shopping experience rather than healthcare. To meet this, independent practices need to learn to use the power of brands while maintaining their own high level of clinical patient care. Independent practices will increasingly be looking for how they can achieve this outcome.
As more early career optometrists and dispensers are considering practice ownership, we are increasing our resources to assist with the purchase of existing and the establishment of brand-new practices. Our membership levels, from unbranded to fully branded, provide the flexibility necessary to find the perfect fit for each practice. Independent optometry is stronger together.
AMANDA TROTMAN
Organisation: Optical Distributors and Manufacturers Association, CEO
Area of interest: Trade suppliers and manufacturers
Some suppliers are impacted through a reduced potential client base when independent practices sell to chains. I’m also seeing a few brave entrepreneurial optometrists take on the challenge of buying into or opening sites and I’m hoping this will increase. Suppliers are looking for efficiencies so there’ll no doubt be more collaborations, mergers, automation and systems integration.
I’m focused on how I can gain more insights from our data and research to help suppliers service practices and practices service consumers. Associations such as ODMA, trade rather than health focused and not recipients of government funding, rely on revenue generated through their own promotional offerings and given how competitive it is to secure advertising and live event spend, need to keep focused on providing professional events, education, digital channels and print publications that reach suppliers customers and prospects, providing suppliers strong ROI.
My challenge is that suppliers have such high cost of business pressures in this economic environment. There is an opportunity for us to leverage ODMA Eyetalk ’s trusted brand and provide new ways for suppliers to reach and engage with our strong independent practice audience that are ODMA’s live event attendees and Eyetalk
DR PETER SUMICH
Organisation: Australian Society of Ophthalmologists, president
Area of interest: Ophthalmology



The issue likely stealing headlines in 2026 relates to specialist fees. The Albanese government, and Health Minister Mark Butler in particular, have threatened to use new legislation to limit access to Medicare rebates if specialists charge more than three times the schedule fee.
Of course, the great problem is that the Medicare rebate is uncalibrated to the cost of a medical service and serves no metric purpose at all.
Whilst there may be some Schadenfreude from other professional groups, the precedent of government control over professional fees is the thin end of the wedge.
In all likelihood, many specialists would opt to ignore Medicare altogether, and charge like dentists with patients receiving no rebate. The government doesn't seem to realise that the rebate is the patient's money, not the doctors. There will be many unhappy patients if they don't get a rebate, small as it is.


Image:
Dr Peter Sumich.
Image: Amanda
Trotman.
Image: Philip Rose.
Image: Tony Jones.
Image: Elizabeth Kodari.
PROFESSOR PETER MCCLUSKEY
Organisation: Royal Australian and New Zealand College of Ophthalmologists, president Area of interest: Ophthalmology
In 2026, ophthalmology will be shaped by continued workforce pressures and rising demand from ageing populations. Colleges, like government, face pressure to meet these demands. This puts RANZCO under increasing scrutiny from governments and regulators.
A central challenge will be ensuring that government reforms, including those arising from the Kruk Report, do not jeopardise patient safety or dilute training quality. The college does not control funding pipelines that create additional training places yet is often expected to absorb the consequences of policy decisions. There is also a risk that workforce maldistribution is overlooked in favour of simply increasing overall numbers. Ensuring government recognises this nuance, and that solutions address where specialists are needed, not just how many, will require sustained advocacy.
For the college, 2026 offers an opportunity to consolidate ahead of full AMC accreditation in 2027. This includes embedding the curriculum, strengthening education and training outcomes, and using data-driven decision-making to improve quality, equity, and long-term sustainability.


Organisation: Orthoptics Australia, president Area of interest: Orthoptics

ASSOCIATE PROFESSOR AMANDA FRENCH

In late 2025, major reforms to the National Disability and Insurance Scheme (NDIS) and the Aged Care Rules were announced, with impacts for allied health providers and community access to care expected to flow through in 2026. The Thriving Kids initiative, designed to support children with autism and/or developmental delay outside the NDIS, is under development, and orthoptists are well placed to provide vision screening and therapy under the scheme. The National Allied Health Digital Uplift Plan to enable allied health professionals to access and share health information within My Health Record was published in 2025. This access to the digital ecosystem will allow for greater involvement in collaborative care and more timely, person-centred care provision. This is an important step towards a connected digital health system for the future.
Lastly, the final report of the Dawson review of the National Regulation and Accreditation Scheme recommends strengthening and expanding regulation through integrated risk-based models, potentially extending to currently self-regulated professions like orthoptics. This presents an opportunity to strengthen professional standards, enhance public safety and support more accurate workforce planning.
PROFESSOR LAUREN AYTON
Organisation: Centre for Eye Research Australia and The University of Melbourne Area of interest: Clinical research
We are on the precipice of personalised medicine for eyecare, and 2026 will continue to show growth in this area. Several fascinating clinical trials are underway, including gene therapy and molecular photoswitch drugs to restore vision to people who are blind. It’s exciting to offer these opportunities to patients who previously had no therapeutic options.
One big challenge is developing clinical trial outcome measures that are sensitive, specific, and meet regulatory requirements. Promising drugs sometimes fail trials because endpoints don’t work, not the drugs themselves, so work will continue on new options like the in vivo adaptive optics imaging at The University of Melbourne’s Department of Optometry.
CERA will welcome two international leaders in 2026 – Professor Pete Williams (Karolinska Institute, Sweden) and Dr Sloan Wang (UMass Chan Medical School, USA) – to boost expertise in regenerative medicine, glaucoma, and retinal diseases. We look forward to expanding international networks to accelerate new treatments and scientific discoveries.
PROFESSOR KEITH MARTIN
Organisation: Centre for Eye Research Australia managing director Area of interest: Clinical research


In 2026, the most important shift will be our movement from slowing decline to genuinely restoring vision in conditions like glaucoma. With advances in gene therapy, cell therapy and neuroprotective strategies, we are beginning to see the possibility of repairing or replacing damaged retinal ganglion cells and optic nerve pathways. This represents a profound change in how we think about treatment, from managing loss to actively recovering function. What keeps me awake at night is the widening funding gap needed to support the full economic cost of medical research in Australia. As the science becomes more complex and globally competitive, the mismatch between real research costs and available funding threatens our ability to deliver world-leading discovery, retain talent, and translate breakthroughs into clinical impact. Addressing this gap is critical if Australia is to remain at the forefront of ophthalmic innovation.
Looking ahead, CERA has invested in new facilities for both discovery and clinical research, and new researchers to expand our strengths in glaucoma, regenerative medicine and retinal disease. This gives us a real opportunity to progress more treatments from the laboratory into clinical trials, and ultimately to reduce vision loss and blindness.

Image:
Professor Keith Martin.
Image:
Professor
Peter McCluskey.
Image: A/Prof Amanda French.
Image:
Professor Lauren Ayton.
Image: Jason Holland.

RANZCO Congress the biggest yet


The power of AI and language were among top subjects discussed at the 2025 RANZCO Congress as leading ophthalmic figures from around Australia and the world gathered for the annual deep dive into industry innovations, issues and opportunities.
Organisers say RANZCO 2025 was the largest congress yet, a highly successful event with an “electric” atmosphere.
Much of that was generated by the more than 2800 attendees who made it to the Melbourne Convention and Exhibition Centre for the event between 14-17 November, most of whom attended in person, with close to 200 following the conference online.
Those in Melbourne for the four days experienced insightful sessions covering sector innovation and issues, plus a comprehensive look at new technology, products and techniques.
More than 90 exhibitors in the trade hall kept them across new products and technology.
The program at the Royal Australia and New Zealand College of Ophthalmologists event kicked off with the Global Eye Health Workshop and various CPD and RANZCO committee forums.
The official event started on Saturday with an emotional and insightful look into the power of language.
When award-winning speaker, author and artist Ms Rachel Callander steps on stage to address health professionals, her message is simple but profound: the language clinicians choose can either build a bridge with patients – or create an unnecessary chasm.
It’s a belief shaped by the short life of her daughter, Evie, and by countless encounters with medical professionals who, often unintentionally, conveyed fear instead of clarity.
Callander was a young wedding photographer living in New Zealand when she discovered she was pregnant.
It was news she admits “felt like an impending doom” for a young, wannabe artist not expecting or seeking out a life of structure and familial routine.
But when Evie was born, “all my fears melted away”.
However, those first moments of joy were soon replaced by medical crisis, confusion and, critically, damaging language. Doctors delivered a diagnosis of chromosomal abnormalities using terms such as “incompatible with life”, “defective”, and even “retardation”.
Callander recalls feeling as if her beloved daughter had been reduced to “a collection of faulty body parts and big scary words”.
Evie’s early years were medically complex, and her life precarious, but she grew into a child of joy and “superpowers” as Callander affectionately reframed what others saw as faults or negatives.
"The reframe, says Callander, was necessary for her survival."
Strangers often asked, “What’s wrong with your child?” and she realised that the narrative she chose could change the way others saw her daughter. Rather than focus on what others might perceive as disabilities, Callender recast them as in a more personal and positive light.
“In that moment,” she says, “they saw a human being, not a diagnosis.”
What she learned from healthcare interactions was equally defining.
Confusing jargon left her feeling isolated, inadequate and terrified to ask questions.
A specialist once offered an avalanche of technical explanations; the only words she grasped were “short arms”, which made no sense in relation to her daughter until a later clinician gently asked, “What do you know about chromosomes?” and drew a simple picture of a chromosome and its ‘arms’.
“In 10 seconds,” she says, “I learned more than in the previous hour.”
For Callendar, that moment became a benchmark for what good communication feels like: clear, calm, curious, and human. And a catalyst to push for change. Her experience has significant
implications for medical specialists, including ophthalmologists and other eyecare professionals, who often deliver life-altering news.
“With eyes, you’re working with a whole person,” she says. Vision changes reshape daily life, identity and independence. Clinicians who ask grounding questions, including What’s your understanding of what’s happening? What matters most to you? Is there anything I’ve said that you’ll go home and Google?, help patients navigate fear and protect dignity.
Evie lived just two and a half years, but she inspired what Callander now describes as her life’s work: reframing medical language.
She has created photographic art books celebrating children with chromosomal and genetic conditions, capturing their “superpowers” rather than their labels.
Families repeatedly tell her how deeply diagnostic language has wounded them – words like “dysmorphic” or “abnormal” becoming damning identities rather than descriptions.
Today, Callander teaches a variety of communication strategies designed to reduce confusion and build trust.
Her message to clinicians is practical.
"I know you don't go to work to intentionally cause harm," she said.
"Communication is hard, and you cannot make decisions when you’re confused. But with clear, compassionate language, everything changes.
“With a few practical, human-centred tools and strategies, you as a clinician can share the knowledge you have, listen to the lived experience and expertise of the patient, and deliver the best care possible."
WORKFORCE PRESSURES DOMINATE
Following Callander, Dr Kristin Bell used her RANZCO Plenary address to lay out the forces reshaping the ophthalmology workforce – and the steps RANZCO is
One of the many presentations that drew big audiences at RANZCO Congress 2025 in Melbourne. Images: RANZCO.

Hospital, and RANZCO’s regional education chair and lead of its regionally enhanced training network, said the eye health system was entering “a period of profound change”.
Demographic, economic and technological pressures continued to push demand for ophthalmology services higher, she said.
And rising obesity, chronic disease and an ageing population were also driving up costs, with healthcare spending “steadily rising as a portion of GDP”.
Yet despite three decades of national reports, she said there had been “very little change in the distribution of medical practitioners per 100,000 people” between 2013 and 2022.
Much of Dr Bell’s focus was on distribution – or the lack of it.
Around 29% of Australians live regionally, yet only 16% of the ophthalmology workforce is based outside major cities.
The imbalance is even starker for First Nations communities: while 59% of Aboriginal and Torres Strait Islander people live regionally, just 0.1% of ophthalmologists identify as indigenous.
“Regional background is the strongest predictor of future regional practice,” she noted, citing evidence across medical specialties.
Rural clinical school attendance also increases the likelihood of regional work, but students “lose interest in rural training as they move to the cities”, and one-year terms are too short to foster connection to place.
Longer placements, Dr Bell told the audience, “really do increase the likelihood of future regional practice”.
She also highlighted a trend towards narrowing scope post-training.
While more than 80% of trainees believe they finish with the required skills for comprehensive practice, fewer than 20% feel prepared to work broadly, and more than 90% intend to subspecialise.
of difference”.
The structural challenge, Dr Bell argued, is that 87% of ophthalmology service delivery now occurs in the private sector, while specialist training is anchored in public hospitals.
Limited public capacity, combined with uneven distribution of public services, is “the single biggest barrier” to training enough ophthalmologists for the whole population.
Dr Bell outlined RANZCO’s recent actions under Vision 2030, of which she is the clinical lead, including revised curricula to ensure graduates are comprehensive generalists, parity in selection points for rural and First Nations applicants, and expansion of the Regional Enhanced Training Network.
research unit at Bristol Eye Hospital, UK, gave an address about how medical retina services across the UK have been reshaped over the last few years to help deal with capacity pressures.
In her Retina Update Lecture, Dr Bailey outlined how the use of networked electronic patient records, enhanced roles within the multidisciplinary team, mobile treatment units, diagnostic hubs and closer links with community optometry were easing capacity pressures on the National Health Service (NHS).
She began by emphasising the scale of the challenge.
“The vast majority of patients with medical retina disorders are having their care under the National Health Service,” she said, noting that chronic conditions such as diabetic retinopathy and treatments for wet age-related macular degeneration (AMD) were not routinely covered by private insurers.
Combined with the UK’s relatively low ophthalmologist-to-population ratio compared w ith some other countries, the result has been long-standing capacity challenges. The Covid pandemic also resulted in additional challenges as routine work was postponed during the lockdowns.
To help to manage this demand, she described how Bristol Eye Hospital had developed a hub-and-spoke model of care built on a fully paperless electronic medical record system.
Among the most striking innovations is a mobile macular unit, located in a supermarket car park and fitted out with an OCT room, injection room and clinical spaces.
“AS MORE PEOPLE CLUSTER IN MAJOR CITIES, COMPETITION INCREASES, AND SUB-SPECIALISATION BECOMES A POINT OF DIFFERENCE”.
The college was also “building strong relationships with government, other specialist colleges and health authorities”.
Looking ahead, RANZCO is calling for national governance measures, including jurisdictional KPIs for training distribution, better visibility of outpatient activity, and agreed access standards for public eyecare.
Workforce data will be critical: “It’s crucial we have the data we need when we go to government,” Dr Bell said, urging members to complete the perpetual workforce survey.
“Reform is not a choice – it is inevitable,” she concluded. “We are in a period where decades are happening in weeks, and we must take a united voice to government to ensure equitable eyecare for our patients.”
RESHAPING CARE DELIVERY
Dr Clare Bailey, consultant ophthalmologist and clinical lead of the retinal treatment and
“It’s extremely popular with patients, who find it very convenient, and of course has very good parking!,” she said.
The unit, along with outreach injection clinics, means patients can access treatment closer to home.
That access was supported by an electronic patient records system that could be accessed by all appropriate medical professionals.
“It doesn’t specifically matter at which location the patient is seen, because we have one electronic patient record.”
Other units have developed similar systems for outreach treatment clinics.
Workforce innovation has also been important.
Nurses now deliver the vast majority of intravitreal injections nationwide, while shared-care optometrists undertake extended roles, including triage, grading and virtual clinic assessments.
Dr Bailey described them as “an absolutely integral and outstanding part of our team''.
The opening presentation by Rachel Callander was a highlight of the event.

During COVID-19, Moorfields Eye Hospital and Bristol Eye Hospital established large diagnostic imaging hubs that have since become permanent and now handle the majority of medical retina follow-ups.
Technicians at each hub take images with OCT, widefield colour and autofluorescence imaging.
The imaging appointment takes about 15-20 minutes, with subsequent grading of the images by the clinical team.
Patients would receive tele-consultations with consultants based on clinical need after the initial grading.
Dr Bailey said their service audit had shown that over 99% of images were of sufficient quality for grading.
A major recent advance in Bristol has been a new electronic referral pathway directly to the hospital from community optometrists, enabling them to send full-resolution DICOM OCT scans and colour images directly into the hospital system.
She said this had saved a hospital appointment in 73.4% of cases, significantly reducing travel burden for patients while boosting treatment timeliness.
She described a scheme from Gloucestershire whereby the hospital ophthalmic scans, visual fields and GP letters could be reviewed by community optometrists, which had led to a significant reduction in unnecessary referrals and avoided duplication.
Dr Bailey said these changes in the supported research participation and real-world data collection. The UK experience had shown that digitally enabled triage, multidisciplinary working, diagnostic hubs and community-aligned care could deliver faster, more efficient outcomes for patients and the health system.
MYTH, MAGIC OR MONSTER?
In his Glaucoma Update Lecture, Professor Gus Gazzard confronted the promise and the
pitfalls behind “interventional glaucoma”, a term that has gained traction since around 2010 and generally refers to earlier, non-pharmacological interventions aimed at lowering intraocular pressure (IOP).
This mainly includes procedures like selective laser trabeculoplasty (SLT), minimally invasive glaucoma surgeries (MIGS), but in some cases early trabeculectomy or lens extraction.
The idea is to reduce or eliminate dependence on long-term eye drops, offering a more proactive, procedure-focused pathway for managing glaucoma.
Prof Gazzard, director of the glaucoma service at Moorfields Eye Hospital in the UK and one of the world’s most cited glaucoma researchers, acknowledged the hype surrounding the term.
“I think there’s an awful lot of jargon that some individuals are hiding behind,” he said.
His aim was to separate hype from hope, and to propose “non-incisional glaucoma care” as the logical entry point into any interventional pathway.
He contrasted the historical “drops, drops and more drops – then trab” sequence with today’s reality. “Seventy-five per cent of glaucoma specialists in the US now use SLT as primary treatment,” he noted, with medications and surgery used only as required.
This shift was supported by several landmark trials: the EAGLE (Effectiveness in Angle-closure Glaucoma of Lens Extraction) trial confirming clear lens extraction in primary angle closure disease; the TAGS (Treatment of Advanced Glaucoma Study) research revisiting primary trabeculectomy for advanced glaucoma; and the LiGHT (Laser in Glaucoma and Ocular Hypertension) trial, which has become the cornerstone of the SLT-first approach. Among newly diagnosed mild-to-
moderate patients, SLT delivered 70% drop-free control at six years, alongside a 30% slower rate of visual field deterioration compared with medication.
“The medication group did worse, even though they were treated to the same target pressure,” he said.
Emerging horizon data suggested similar effects with phaco-MIGS combinations, with five-year results showing a three-fold reduction in the need for future incisional surgery compared with cataract surgery alone.
These visual-field differences, though numerically small, matter, Prof Gazzard argued, citing work linking even modest mean deviation losses to impaired driving, reading speed, falls and reduced physical activity.
But he also issued strong cautions. Not all MIGS are equal – or even truly “minimal”.
Some devices and procedures carry under-reported risks, he said, from 90% hyphaema rates in certain trials to hypotony risk with supraciliary approaches.
“We have to be clear-eyed about the balance of safety and risk,” he said.
Medications are not benign either: non-adherence, BAK (benzalkonium chloride) toxicity, goblet cell loss and long-term conjunctival changes carry their own harms.
His conclusion: interventional glaucoma is not a myth – the evidence for non-pharmacological care is now substantial; it is not magic – advanced disease still demands “proper surgery for proper pressures”; and there is “some monster in the detail”, particularly around unacknowledged complications, confirmation bias, and the cost implications of a “MIGS-for-most” approach.
“Getting people away from medications is a good thing, but we must be very careful that enthusiasm doesn’t outstrip evidence.”
There was plenty of innovation and new technology to see and use on the trade floor.










Forward thinking
Early-career optometrist THOMAS FORD has carved a path from rural practice to partnership with George & Matilda Eyecare, blending clinical excellence, community innovation and leadership, while fast becoming a key thought leader within the industry.
When Thomas Ford officially stepped into partnership at George & Matilda Eyecare’s practice in Griffith, a regional city in the northern Riverina region of western New South Wales, in July 2025, the move from clinician to business partner was an undisputed career milestone. But above all, it was a vote of confidence in his performance and leadership potential.
Ford had been at the practice for just 18 months when he was approached to consider elevating into a partnership position. Only four years post-graduation, the opportunity was as unexpected as it was welcome. His early career had already spanned private ophthalmology, work with Myopia Profile alongside Dr Kate Gifford, locum roles across rural and metro settings, and involvement with Optometry Australia – experiences that gave him a diverse and agile view of clinical care.
Today, he practices alongside a four-person team: including a practice manager, dispenser and graduate optometrist, offering full-scope optometry to the Griffith community, which is home to around 35,000 people.
Leaning into his passion for ocular pathology and therapeutics, Ford is relishing the complexity of clinical decision-making in a town without full-time ophthalmology services.
“We have a visiting ophthalmologist attend once per month, with a public waitlist of over 24 months to gain an initial appointment,” he explains. “Otherwise, patients have to travel to Wagga, two hours away, Albury three hours, or Sydney six.”
This geographical reality fuels his commitment to practising at the fullest extent of current optometric scope – and advocating for what an optometrists’ scope should become. It’s a theme that threads throughout his work, particularly in paediatric vision, therapeutics and advanced clinical care.
CHAMPIONING CHILDREN’S VISION
One of Ford’s biggest contributions in 2025 emerged from a concern echoed across the profession: the number of school-aged children with undiagnosed vision problems.
He was inspired by Optometry Australia research which found that almost half of Australian children had not received an eye test by age 9.
“We know that 1 in 5 Australian children have an undetected vision problem, that vision is responsible for 80% of a child’s learning, and that by the year 2050 half of all children will be myopic. This prompted us to act” he said.
In New South Wales, the StEPS (Statewide Eyesight Preschooler Screening) program screens children in kindergarten or preschool, but no statewide follow-up exists for older cohorts.
Sensing a gap with real consequences for learning outcomes, Ford and his team initiated a free, voluntary vision screening project at a local public primary school. Conducted over two days in August 2025, the program assessed 90 children whose families had provided consent. The results were stark: two-thirds of participating students had an undetected vision issue requiring follow-up care.
Families received summaries of results and recommendations to visit their preferred local optometrist if problems were detected – “we encouraged the agency of parents and their children, allowing genuine choice in selecting a preferred eyecare provider”, he notes, reflecting the program’s community-first ethos.
The effort quickly translated into increased visits from concerned parents and children, with Ford describing paediatric eye care as the future of both the practice and of the industry more broadly. “Our practice is fast gaining a reputation for excellence in paediatric vision and eye health” he says. “We’re working hard to safeguard the vision of future generations, one child at a time.”
The initiative drew attention beyond the school gates. In October 2025, the school principal nominated the team for the
Murrumbidgee Primary Healthcare Awards, where they were crowned winners in the Innovation category. It’s recognition Ford describes as humbling and gratifying, but secondary to the project’s impact.
“It’s so rewarding to be regarded as a trusted advisor to children and their parents,” he says, “we’re fortunate to be able to play our part in ensuring good eye care for life while setting children up for success.”
The G&M Griffith practice now plans to continue vision screenings annually, finishing coverage of the original school’s student body before expanding to a new local primary school each year. Ford expects similar findings elsewhere and sees the initiative as a crucial step towards long-term community eye health.
“Breaking down barriers, doing things differently, and having a hyper-local approach to community eyecare is at the heart of what we do.”
FELLOWSHIP, MENTORSHIP AND ADVOCACY
Even as his community work gained recognition, Ford simultaneously achieved one of optometry’s highest international professional honours: Fellowship of the American Academy of Optometry (FAAO).

To qualify, he spent 18-24 months preparing extensive case reports, often complex cases seen in rural practice detailing presentation, pathophysiology, clinical reasoning and treatment. He then travelled to Boston in
“IT’S ALL ABOUT MINDSET; THE DESIRE, THE DRIVE TO DO THINGS DIFFERENTLY, WHILE HELPING THOSE IN OUR LOCAL COMMUNITY.”
October 2025 to sit an oral examination before being awarded fellowship at the academy’s conference, attended by around 8,000 optometrists from across the world.
For Ford, the fellowship reflects a commitment to excellence and innovation in eyecare. It also fuels his passion for mentoring early-career optometrists. Over the past year, he has supervised placement students from Deakin University and Flinders University, valuing the reciprocal learning and the fresh perspectives students bring to complex clinical scenarios.
Mentorship, he notes, is often missing in the profession, which is why he values the guidance he now receives from his G&M Professional Services Manager, a relationship he describes as his first true mentorship experience.
“I’m privileged to have such amazing support provided by trusted mentors who

Images: Thomas Ford
Thomas Ford combines clinical excellence, community innovation and leadership, while fast becoming a key thought leader within the industry.

help me to continue growing.”
In November 2025, Ford expanded his leadership further, accepting an appointment to the board of Optometry NSW/ACT. With a strong commitment to ensure a modern, agile and member-focussed organisation, he intends to better engage early career optometrists to secure the organisations future as a vital professional body.
Looking ahead, he is committed to advocating for oral therapeutics to be added to the Australian optometry scope of practice. In regions like Griffith, where public ophthalmology waits can stretch to two years and GP appointments can take weeks, the ability for optometrists to prescribe
oral medications would significantly reduce treatment delays. He hopes to see progress toward implementation by late 2027.
“It will make a huge difference to our patient’s visual prognosis and quality of life,” he says, “while reducing service duplication and ensuring greater efficiency of our overburdened healthcare system.”
TECHNOLOGY, TEAM GROWTH AND A CLEAR VISION
With momentum building across clinical practice, community health, advocacy and education, Ford is already planning for 2026 and beyond. The Griffith practice welcomed a graduate optometrist, Isabel Salvestro,
in August, and he is enthusiastic about supporting her continued development in line with the practice’s values.
This year will also bring new clinical capabilities, with the delivery of an Optos ultra-widefield device: the first in Griffith. It’s expected to enhance retinal care across the region, enabling earlier detection, more accurate triage and more effective co-management with other providers. Not all patients with retinal concerns will need to make lengthy trips to ophthalmology services; others may be referred sooner and more appropriately.
“We’ll have the opportunity to better support other practices, ophthalmologists, GPs and patients with retinal concerns,” he notes. “It’ll be great for the practice and for the community alike.”
With plans for expanded paediatric vision programs and an ongoing appetite for innovation, Ford is optimistic about the coming year both professionally and clinically.
“It’s all about mindset; the desire, the drive to do things differently, while helping those in our local community.”
“One of the things I value most is how supportive George & Matilda Eyecare have been. Their backing gives me the freedom to drive these initiatives beyond day-to-day consulting and to continue elevating the standard of eyecare.”

The George and Matilda Eyecare Griffith team were recognised for their innovative children’s vision screening program, following nomination by the school principal.


An expanding ecosystem
ZEISS Medical Technology outlines how its integrated imaging and workflow tools work together to enhance clinical efficiency, improve decision-making and support future-focused practice growth.
When ZEISS announced its acquisition of the Dutch Ophthalmic Research Center (DORC) in late 2024, it marked a new phase in vitreoretinal and cataract surgery.
At RANZCO 2025, Australian surgeons were given their first detailed look at the expanded product family now available under the ZEISS banner, including the EVA NEXUS surgical platform and the latest-generation TDC (two-dimensional cutter) VELOCE cutter.
According to ZEISS Medical Technology, the transition of DORC products into its broader portfolio will give ophthalmologists access to a unified, next-generation ecosystem for anterior and posterior segment surgery.
For Australian vitreoretinal specialists, the integration brings together DORC’s innovations in fluidics and cutter design with
ZEISS’s established strengths in imaging, digital workflow and surgical visualisation.
Among those with extensive hands-on experience is Professor Hideyasu Oh, clinical professor at Kyoto University and head of ophthalmology at Hyogo Prefectural Amagasaki General Medical Center in Japan. A leading figure in vitreoretinal surgery, Prof Oh has long been a dedicated user of the DORC EVA NEXUS system and has played a key role in validating its latest innovation – the VELOCE cutter.
"The most important features of EVA NEXUS for me are the excellent control of intraocular pressure and outstanding efficiency of cutting," he said.
STABILITY AND PRECISION AT THE RETINA
According to ZEISS Medical Technology, the EVA NEXUS uses a VTi pump system
Above: The platform is designed to consolidate vitreoretinal and cataract functions through a single programmable footswitch.
designed to provide controlled flow and aspiration, supporting a stable intraoperative environment even during close work at the retinal surface.
In combination with this, the company’s VELOCE cutter has been engineered with a reduced distance between the cutter port and the tip to support precision in high-risk zones.
Prof Oh said the system gives him confidence when operating near delicate tissue.
“I really feel I can work at a very near distance from the retina. This is mainly due to proximity of the cutter opening to the tip of the new VELOCE cutter. Thanks to
VTi pump technology the flow mode also contributes to this because it will avoid inadvertent cut and thus we can safely approach to the vicinity of the retina,” he says.
ZEISS notes that the VTi pump architecture combines flow and vacuum control to maintain consistent intraocular pressure (IOP) throughout surgery. This is a key element of the EVA NEXUS platform and is intended to minimise fluctuations that can influence surgical risk.
The emphasis on predictable behaviour at the tissue interface positions the platform for both routine and challenging vitreoretinal procedures.
The engineering focus on port-to-tip proximity and controlled flow is particularly relevant for peripheral vitreous shaving, a step that often determines surgical outcome in detachment and proliferative vitreoretinopathy cases. The system’s stability profile is consistent with ZEISS Medical Technology’s stated aim of giving surgeons more control in procedures where retinal mobility or thinning elevates the risk profile.
EFFICIENCY GAINS IN VITREOUS REMOVAL
Efficiency has been a major area of analysis for surgeons evaluating the EVA NEXUS.
According to ZEISS, the VELOCE cutter uses an enhanced dual-mode fluidics approach intended to improve removal rates while maintaining consistent cutting performance across core and peripheral vitrectomy.
Prof Oh said his clinical findings, supported by experimental data, indicate a significant increase in vitreous removal efficiency.
“Efficiency is the most outstanding feature of the VELOCE cutter when compared to its prior version,” he says.
“According to our data from both animal experiments and clinical cases (in collaboration with Professor Fanis Pavlidis), we found the efficiency of removing vitreous is increased by more than 40%, a dramatic improvement which all users will certainly notice.”
He added that the cutter is not only efficient during the core vitrectomy stage of the procedure but also behaves consistently during more delicate phases.
“The new cutter can not only remove the vitreous with superb efficiency during core vitrectomy but also exhibits very secure and steady cutting during shaving the peripheral
The VELOCE cutter has been engineered with a reduced distance between the cutter port and the tip to support precision in high-risk zones.

vitreous in non-complex retinal detachment cases and also in cases with necrotising retina, a situation that we surgeons need to pay highest attention to.”
The continuous duty cycle design of the cutter is intended to maintain traction-minimising behaviour. According to ZEISS, this is aligned with surgeon expectations in cases involving necrotising retina or elevated anatomical sensitivity. The focus has been on supporting stable aspiration, reduced turbulence and predictable cutting action at both high and low flow settings.
The company notes that improved efficiency contributes to shorter and more controlled theatre time – an important operational consideration for high-volume surgical lists. With the integration of DORC technologies into the ZEISS portfolio, the VELOCE cutter sits within a workflow that is designed to maximise consistency across different procedural steps.
INTEGRATED WORKFLOW AND MULTIFUNCTIONAL CONTROL
At RANZCO 2025, one of the most discussed features of the EVA NEXUS was its integrated operating environment, a hallmark of ZEISS technology.
The company says the platform can consolidate vitreoretinal and cataract functions through a single programmable footswitch that controls cutter modes, phaco mode, laser activation, vacuum settings, flow adjustments and IOP regulation.
Prof Oh emphasises that VELOCE cutter performance and stable IOP are two of the most important variables when comparing platforms.
"Without constant and precise control, we cannot maximise the cutter performance and the maintenance of the intraocular pressure, which are important for efficiency and safety, respectively."
Professor Hideyasu Oh Kyoto University

“First, performance of the cutter including both vacuum mode and flow mode. Fluidics control is also a key player. Without constant and precise control, we cannot maximise the cutter performance and the maintenance of the intraocular pressure, which are important for efficiency and safety, respectively.”
He highlights the role of the footswitch as key to the platform’s usability.
“Regarding the footswitch performance, the multi-functionality of the EVA NEXUS is outstanding. It works for not only switching the phaco or vitrectomy modes as we normally expect, but also emission of laser photocoagulation (without exchanging the footswitch) and even a fine control of intraocular pressure.”
ZEISS reports that this integration is intended to streamline surgical workflow and reduce the need for external peripherals or additional switching during procedures.
By placing laser, vitrectomy, phaco and IOP functions under unified control, surgeons can operate with fewer interruptions and maintain consistent hand positioning.
With the full DORC portfolio transitioning over to ZEISS ANZ, the company has looked to offer a harmonised system in which cutters, consumables, fluidics modules and illumination tools are designed to operate within one environment. This supports clinics that conduct both anterior and posterior segment procedures and require flexibility in operating theatre configuration.
THE PIPELINE
With ZEISS already established in microscopy and digital visualisation, the addition of the DORC portfolio fluidics and cutter technologies is intended to create a comprehensive ecosystem that optimises retinal disease detection, management and treatment that includes intraoperative imaging, tissue manipulation and data-supported decision tools.
ZEISS has indicated that the combined ZEISS/DORC portfolio will continue to evolve to support this type of integrated guidance.
Images: Zeiss.
Fundus imaging system with TrueColor confocal technology.

The world’s 1st slit lamp mounted rebound tonometer, makes measuring intraocular pressure (IOP) easy, quick and accurate.
The 1st TrueColor confocal imaging device for ultra-high resolution widefield imaging.


TrueColor high-resolution confocal fundus retinal imaging system with blue autofluorescence (FAF).

With 200 degrees of positional freedom, measure intraocular pressure (IOP) of patients in a sitting, standing, elevated or supine position.

With Fluorescein Angiography capability for ultra-high resolution and widefield images and videos.

Tonometer for all eye care professionals to measure the intraocular pressure (IOP) of patients in a sitting or standing position.





Raising the roof
Two workshops at O-SHOW 2026 are reframing the future of Australian eyecare – one spotlighting women driving change, the other equipping clinicians to master non-clinical aspects of the myopia epidemic.
For decades, optometry conferences have been a stage for optics, innovation and the occasional free microfibre lens cloth. But at O-SHOW 2026, something subtler yet seismic is shifting.
Two workshops hosted by show organisers the Optical Distributors & Manufacturers Association of Australia (ODMA) are putting business strategy, mentorship and real-world practice wisdom at centre stage.
Taking place on 16 August 2026 at O-SHOW in Melbourne, the two sessions –Myopia Mastery and Women in Optics – are aimed at practice owners, managers and practice staff.
MYOPIA MASTERY
With myopia rates rising and more corporate networks rapidly entering the space, ODMA’s Myopia Mastery workshop is designed with practicality in mind. It is intended to equip independent practice owners and managers with insights and practical business tips and to assist with promoting
“We’re not competing with
clinical
delivery. We’re delivering business solutions. Evidence backed but commercially actionable.”
Amanda Trotman ODMA CEO
evidence-based solutions and strong, family-centred communication.
Sponsored by HOYA, the half-day workshop from 9.30am to 12.30pm won’t be clinical in its delivery, says ODMA CEO Ms Amanda Trotman.
“Having your practice set up to deliver myopia services is essential” she says.

The workshop will give practice owners real tips for delivering myopia services across all the disciplines, including marketing pointers and assistance with patient-facing language.
The workshop will arc away from the clinical and toward commercial uptake across product domains: spectacle lenses, orthokeratology (orthok) lenses, atropine eye drops, paediatric frame merchandising, in-practice displays, equipment and technology, and marketing documentation.
Presentations will also cover consumer behaviour insights, tips for marketing to families, social media campaign tips and communication.


Every supplier who is presenting in the workshop – lens providers, frame suppliers,

Belinda Musitano.
Images: ODMA
Suppliers presenting in ODMA’s Myopia Mastery workshop are also exhibiting in the O-SHOW trade fair.
Celia Bloxom.
Heidi Hunter.



atropine partners – are also exhibiting in the O-SHOW trade fair.
“So if people are interested,” Trotman says, “they only need to walk 20 metres and they have the rest of that day and the next day to follow up with those suppliers in detail.”
Workshop speakers, including Ms Allison Abdullah from Lens Avenue and Dr Emma Gillies from Purple Key Consulting, will deliver segments on marketing and patient-family dialogue – the commercial communication skills where independent practices need fluency.
WOMEN IN OPTICS
The Women in Optics leadership event, taking place from 1.30pm to 5.00pm, marks the first event where women in leadership have had substantial input into the events topics.

an emerging voice gaining recognition for her candid, business-first worldview.
“Roni brings a fresh voice to the professional speaking space,” she says.
Founder of The Wellbeing Edge, a motivational speaker, and wellness advocate, Millard’s keynote will set the theme around resilience, time management, and achieving and maintaining life balance.


“Women tend to want to talk about the real stuff. They don’t want to be spoken at the whole time,” Trotman says, which leads to the workshop’s core: round-table conversations across six pre-selected topics.
It will ride the momentum of the inaugural event that took place in mid-2025 at ODMAFair in Sydney.
The 2025 event was facilitated by keynonte speaker Carli Phillips with an emphasis on wellbeing. This time, ODMA is implementing a collective advisory format to bring out lived experiences of female optical professionals while offering practical tips in various key business areas.
With the venue capped at 80 delegates, the workshop’s format is orchestrated to generate discussion and connection.
“We want to keep it intimate. That connection between people is the whole point,” Trotman says.
Trotman will open the workshop by introducing keynote speaker Ms Roni Millard,
She’ll be joined by independent practice owner Ms Belinda Musitano from Eyes@ Optometry in Western Australia who “will weigh in on some real-life perspectives” toward the end of Millard’s address, Trotman explains.
The workshop’s next session focuses on legal and financial matters – arguably the least glamorous but most structurally important topic for female practice leaders’ security and independence, Trotman says.
ODMA has approached a Melbourne-based law firm whose client base is largely medical professionals to lead the session.
“We want practice owners to have everything set up right for their future business protection, including insurance, structures, assets, financial agreements, and strategic planning,” Trotman says.
The session is positioned to prevent avoidable legal or financial woes. To complement the law firm’s advice, Trotman has formed a supporting panel of independent female practice leaders who will relay “things that have happened to them that caused financial issues – what to avoid, what to fix earlier, what they would do differently”.
Registration forms will list all six topics with space for participants to nominate three preferences. “We’ll assign people to tables beforehand,” Trotman says. “That way, when they take their seat at the table, they’re ready to begin; they’re meant to be there.”
Each table has a facilitator, better known as an ‘ambassador’ – a layer of ongoing professional support Trotman wants to continue after the event.
“We really want our ambassadors to become the people emerging women leaders can lean on,” she says. The ambassador cohort includes respected independent owners such as Ms Helen Summers from the Northern Territory, Ms Heidi Hunter from the Newcastle region, and Dr SooJin Nam from Sydney.
Ambassadors at each table will take notes, synthesise key takeaways, and then deliver summaries to the entire cohort.
“This way, every table still gets the key takeaways on every topic,” Trotman says.
The program closes with principal optometrist of Eyeconic Optometry
Southport Ms Celia Bloxom, both ambassador and voice of inspiration.
Emma Gillies.
Shaina Zheng. Roni Millard.
Laura Moore.
Helen Summers.
Dr SooJin Nam.
IMPROVES SIGNS AND SYMPTOMS
IN AS LITTLE AS 2 WEEKS 1
The results are clear. NovaTears® demonstrates statistically significant and clinically meaningful improvements in the signs and symptoms of Dry Eye Disease associated with Meibomian Gland Dysfunction.
weeks 2
RELIEVES
NovaTears® is a unique preservative-free non-emulsion eye lubricant utilising patented EyeSol® Technology:
Lubricates the surface of the eye, spreading quickly without blurring vision
Preservative, phosphate, water and surfactant free.
PROTECTS
NovaTears® acts as a lipid layer stabiliser & evaporative barrier for improved tear film stability & quality:
Stabilises & thickens outer tear film
Allows replenishment of underlying water layer with natural tears.
shelf life after opening


STREAMLINED AUTHORITY CODE 6172
PBS Information: Authority Required (STREAMLINED): Severe dry eye syndrome in patients who are sensitive to preservatives in multi-dose eye drops.
Reference 1. Tauber J, Berdy GJ, Wirta DL, Krösser S, Vittitow JL, on behalf of the GOBI Study Group, NOVO3 for Dry Eye Disease Associated with Meibomian Gland Dysfunction: Results of the Randomized Phase 3 GOBI Study, Ophthalmology (2023), dol: https://doi.org/10.1016/j.ophtha.2022.12.021. NovaTears ® Eye Drops (Perfluorohexyloctane 100% v/v, 3mL) are for the lubrication and relief of dry and irritated eyes. Do not use NovaTears ® with contact lenses. If using any other eye medication, allow at least 15 minutes between using the other product and applying NovaTears ®. NovaTears ® should not be used in children under 18 years. NovaTears ® should not be used while pregnant or breastfeeding.

Love at first sight
Two eyecare professionals have seen the design and development of Tokai Optical’s lenses first-hand, including its latest HR and HR-W single-vision range. They tell Insight why they are happy to promote them for patients, and even friends and family.
Ms Simone Liewes can’t talk right now. She’s unwell, confined to her home and unable to speak, so no chance of an interview with Insight about Japanese optical company Tokai Optical’s latest range of lenses.
A voice she may not have at the moment, but there is passion aplenty in the answers she supplies to written questions.
Passion for her industry, passion for her role as a “dispenser and fitter” at Victoria practice Eyes on Dromana, passion for patients.
And a healthy respect for the passion of those behind Tokai’s engineering and products, including its latest range – the HR (High Resolution) and HR-W single-vision lenses.
As Liewes practically screams in her replies to our questions – I LOVE GLASSES.
She has since childhood, proudly wearing them at school when others would shrink from the slings and arrows of childish taunts.
“I have been collecting glasses since before I started working in optics and rotate through my collection almost daily,” she says.
That love was reciprocated when she happened upon a role in optics.
“My ex-husband worked with a guy who's dad was best mates with the optical mechanic at a small independent practice,” says Liewes.
“They had heard on the grapevine that they were looking for an apprentice, ideally a mature one.
“My boys were both in school and I was looking to get back into the workforce, so one day I popped in, just to introduce myself – the owner took one look at me and said 'I love your glasses, you've got the job'.”
If the rest is history, Liewes discovered that a big part of her future would revolve around Tokai – its lenses and optical coatings.
Like her, Tokai was then relatively new to
the Australian market. But when she tried her first Tokai lenses, it was, well, literally love at first sight.
“Being someone who was new to optics at the time and as someone who only wears single-vision lenses I was very much in the mindset of 'oh it's a single-vision lens, how much difference could there be?'.
“I could not believe the difference in clarity.”
Now it is Tokai and Tokai only that she wears.
“Since wearing the Lutina lens combined with a mix of their amazing tints, I will not wear anything else,” she says.
“My current favourite is a tie between my Lutina with Double Rose tint and Lutina with Pink Fine Colour.”
That goes for her family and friends as well.
Liewes is still getting up to speed with the HR and HR-W lenses, because they are relatively new to Australian practices.
But she remembers well one particular patient she fitted with the lenses – “the only patient that has ever made me tear up”.
“She had advanced Parkinson's and two stimulating implants in her head. Unfortunately, one of these was placed a little too close to her optic nerve resulting in significant prismatic vision.
“She had a pair of glasses that were simply unwearable due to her mobility and posture – they were far too heavy and would slide straight off her face.
“She wanted a fun, lightweight, funky frame that would hide her significant prescription, but putting in the perfect lens was the important bit.
“I went with Tokai,” says Liewes.
“Her speech wasn't the best due to her condition, but I will never forget her reaction – I put the glasses on her face, she broke out in a huge smile, then, without saying a word she just walked out our front door to go

and look at the horizon. “Both myself and her husband could not stop smiling.
“If that isn't testament to the power of a well-made lens then I don't know what is.”
It helps that Liewes has also witnessed for herself, how well made those lenses are.
She says a recent trip to Tokai’s Japan factory was “eye-opening and heartwarming – to see and hear firsthand the passion and commitment of the engineers involved in product development”.
“They pride themselves on their uniqueness in the market, so much so that their company motto around promoting customer first and originality is displayed in every single room throughout the facility.”
Liewes says that makes her “proud to be able to promote and offer their products”.
She admits she doesn’t always understand the complexity of the technology behind the company’s lenses and coatings, but she believes and loves the results she sees for herself – for her friends, family and her patients.
A FOCUS ON THE FOVEA

Tokai says that technology means that the HR and HR-W lenses are not just a premium single-vision lens but a different category of single-vision altogether.
Mr Justin Chiang is the company’s Australia general manager.
He says that rather than treating vision as a static, centred task, the HR concept began with a deeper question: how does the eye actually behave when we look around, move, and track the world.
Development focused on the fovea centralis, the tiny, highly specialised region of the macula responsible for the sharpest vision.
“While small in size, its significance is enormous,” says Chiang.
“It is where we perceive the greatest detail, the highest contrast, and the clearest motion.
“But the fovea is not positioned on the visual axis. It sits slightly off to the temporal side.
“This means that when the eye rotates, the direction in which light must travel to reach
Simone Liewes has loved glasses since she was a child.
Image: Simone Liewes.
Image:
Kevin Li.
Kevin Li (left), with University of Canberra dispenser Chantelle Morgan-Bruce and student Brian Truong.
this point is not perfectly aligned with the optical centre of a typical lens.”
He says traditionally single-vision lenses assume the optical centre of the lens and the eye’s rotation centre line up.
“That assumption works only when the wearer looks straight ahead. Once they look sideways – examining a mirror, checking a blind spot, following a child running across a playground, or scanning multiple screens – the eyes naturally rotate, and clarity breaks down.”
Chiang says the Tokai design addresses this mismatch by redirecting transmitted light so that it reaches the foveal region more effectively.
The HR lens “expanded the area of crisp peripheral clarity and supported the eye’s natural preference for smooth pursuit –tracking objects with the eyes instead of relying on head movement”.
He says the company has improved on this with the HR-W lens.
“HR-W applies aspheric optimisation to both
“One version maximises clarity and visual stability across the widest field, preferred by active users and drivers.
“Another design supports enhanced comfort at near vision, taking into account the larger rotational movements the eye performs during close work and digital engagement.
“A third design also yields a slimmer profile, offering a cosmetic advantage particularly noticeable in higher prescriptions – something that many dispensing opticians immediately appreciate when fitting fashion-forward or rimless frames.”
GREATER CLARITY AT THE EDGES
Among those appreciative practitioners is Mr Kevin Li, an optical dispenser/supervisor at the University of Canberra’s student-led optometry clinic.
He can attest to how the HR and HR-W lenses deliver greater clarity in peripheral vision and with fewer aberrations, especially in patients with higher prescriptions.
Like Liewes, he took a bit of a roundabout route to the optics industry, starting his working life fixing TVs, videos, microwaves
dispensing and optometry.
As part of that he supervises students working with patients at the university’s optometry clinic, and does plenty of dispensing himself.
And when many of his high-script patients complain of issues with peripheral vision and a lack of clarity, often it’s the Tokai HR or HR-W lens that he will reach for.
“As you go up in your prescription, visually, most people will find they have a lot of aberrations towards the side of the lenses,” he says.
“All of my patients that have had HR lenses have said they've physically gone, they can see a lot and it doesn't matter which part of the lens they look through, it is crystal clear.”
Because the clinic is run by the university, Li’s judgements are driven primarily by patient-outcomes rather than any need to make a profit.
That means he is always focused on what is the best lens for the patient.
He believes Tokai shares that thinking.
“The work ethic and the philosophy about the lens itself is very much about let's give patients the best lenses we can humanly, possibly make, without the price tag that goes with it.”
Li says that allows him to offer premium, high-end “Mercedes Benz-like” lenses at the cost of a much cheaper model.

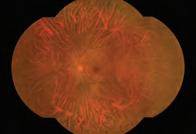
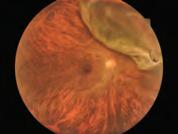
Proveo 8x 3D
Digital Ophthalmic Microscope

Experience 3D 4K visualisation, featuring real-time data integration from phacoemulsification to Optical Coherence Tomography in a single cockpit-view. Enhanced visual information, guiding surgical decisions and multiple viewing possibilities, ensuring a comfortable ophthalmic surgery experience.

Let’s Talk
1800 225 307
vision@paragoncare.com.au
vision.paragoncare.com.au

Request a quote now


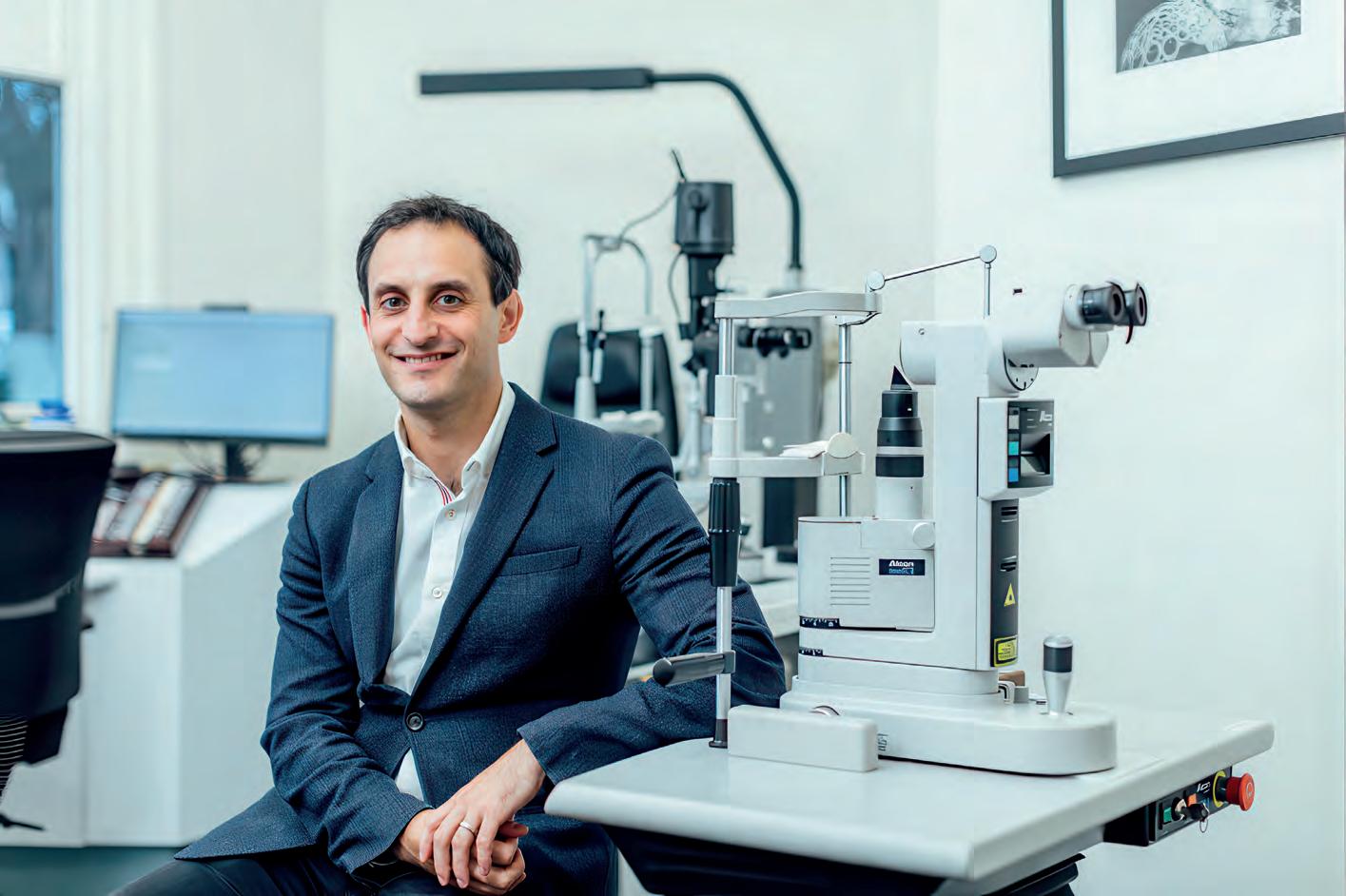
Rayner’s tailored IOL solutions
An Australian ophthalmologist has found that for most of what he sees in his clinic and surgery, the British intraocular lens manufacturer has designed a solution that improves his patients’ vision and well-being.
There’s a modern expression that suggests whatever you might want or need, there’s probably an app for that.
Eye surgeon Dr Justin Sherwin believes there is an intraocular lens (IOL) equivalent. He notes that IOL selection remains individualised, and he routinely uses a range of IOL platforms depending on patient anatomy, visual goals, and ocular comorbidities.
And now he has the data to back up that confidence.
Dr Sherwin has a special interest in cataract, refractive and glaucoma surgery. He is director of Peninsula Eye Centre and practices at Bayside Eye Specialists, Vista Eyes Laser Clinic, and the Royal Victorian Eye and Ear Hospital, with an honorary appointment at Vision Australia.
He also serves as vice president of the Australian Society of Ophthalmologists, lectures nationally and internationally, and sits on multiple industry advisory boards.
He also has a keen interest in learning about new technology and ophthalmic advances.
As an early adopter who works across multiple IOL platforms, he has followed the development of several advanced lens technologies closely, including those designed by British IOL manufacturer Rayner.
In particular, he has closely followed the development of the RayOne EMV and Galaxy IOLs.
He regularly engages with peers in Australia and internationally through clinical collaboration, research activity, education, and ongoing dialogue with key opinion leaders.
“I looked more closely at the emerging evidence of the Galaxy IOL, particularly the pivotal multicentre trial published in the Journal of Refractive Surgery,” he says.
Encouraged by what he saw in both the published data and early clinical experience, he has implanted more than 100 Galaxy lenses since the IOL became available in Australia last year.
That’s helped him build a greater understanding about which patients are better suited to either the EMV or the Galaxy, or perhaps one of Rayner’s other IOLs, including its standard monofocal,
toric and Sulcoflex pseudophakic supplementary IOL products.
“Rayner has a wide range of products that can address a broad range of refractive needs, during cataract and lens-based refractive surgery,” he says.
That includes the EMV IOL, developed in partnership with Australian ophthalmologist Professor Graham Barrett.
EMV works by increasing positive spherical aberration to gently stretch the patient’s range of vision.
The dominant eye is generally set for plano, with the non-dominant eye given a modest, myopic target (micro-monovision).
“In appropriately selected patients, this strategy works extremely well, particularly for those who place a high value on intermediate vision and functional near vision,” says Dr Sherwin.
These patients are not as focused as others on complete spectacle independence and may be comfortable with reading glasses for near work but seek better intermediate vision to help with using their phones, computers and other devices.
“One of the key strengths of the EMV
Image: Justin Sherwin.
Dr Justin Sherwin is an early adopter of eyecare technology.

“One of the key strengths of the EMV lens is its very monofocal-like side-effect profile, particularly with respect to glare and halos.”
Dr Justin Sherwin Peninsula Eye Centre
lens is its very monofocal-like side-effect profile, particularly with respect to glare and halos,” he says.
“Presbyopia-correcting IOLs perform best in patients with otherwise healthy eyes, including an excellent tear film, regular astigmatism, low levels of higher-order aberrations, and healthy corneas, optic discs and maculae.”
He also favors the EMV in myopic patients and in those who are physiologically suited to, or have previously tolerated, monovision through contact lens wear.
“Contact lens trials can also help to determine who would be suitable for this mono-vision approach.”
He prefers the Galaxy IOL for those patients seeking complete spectacle independence.
The product, designed using a proprietary AI engine trained on patient outcomes and the expertise of Brazilian ophthalmologist Dr João Lyra, employs spiral optics technology that distributes light evenly across the retina.
“It is particularly well suited to patients seeking a full functional range of vision with a high likelihood of spectacle independence, while still prioritising visual quality.”
Many such patients are also conscious of the glare and halos associated with some earlier diffractive multifocal IOL designs.
“Early clinical trial data suggest that the incidence of symptomatic, visually disturbing dysphotopia is reduced compared with earlier diffractive multifocal designs, which increases
surgeon confidence in delivering consistent outcomes across the visual range.”

Dr Sherwin says while there is a Rayner IOL for practically every patient, there are some for whom even the power of an EMV or Galaxy may not be optimal.
“The potential for independence at intermediate and near distances is closely linked to the degree of visual limitation imposed by underlying pathology,” he says.
“In patients with significant ocular comorbidities, such as moderate to severe glaucoma or age-related macular degeneration, alternative IOL strategies may be more appropriate.”
However, for patients without significant vision-limiting comorbidities, he is confident that Rayner offers suitable IOL options to improve visual outcomes.
He emphasises that these views reflect his own early real-world experience and are consistent with results reported in the published Galaxy clinical trial.
Dr Sherwin has just completed an early real-world audit of his first 80 Galaxy patients. While the dataset is relatively small and observational in nature, it provides useful early insight into outcomes in routine clinical practice. The numbers involve patients who either had cataract surgery or refractive lens exchange.
More than 80% of those patients had 6/6 or better intermediate-distance vision – “very good vision for seeing computer or phone screens and car dashboards and the likes”.
At near-vision – 40cm – the mean was
N5, with 84% N5 or better, and 93% of the patients surveyed were within 0.50 D of their refractive target.
“There was a high likelihood of functional spectacle independence, acknowledging that individual visual demands and expectations vary.”
He says those results are “promising and very reassuring”.
Just as important was the figure zero –the number of explants he had done.
Dr Sherwin notes he did not formally assess dysphotopia in the survey, but neither had any of his patients complained about those, despite some of his clients often requiring plenty of night-time driving over considerable distances.
And he has also had success using the Galaxy on patients who have had laser refractive surgery.
“The Galaxy IOL has proven relatively forgiving from that point of view, but careful patient selection is key.”
He has also become more comfortable with the Galaxy IOL’s hydrophilic material, an area that has traditionally raised caution among some surgeons.
“Concerns around hydrophilic lenses largely relate to historical reports of secondary calcification, but it’s important to understand the context in which those events occur,” he says.
Secondary opacification following exposure to intraocular gas or air — most commonly after retinal or corneal surgeries — is a recognised but very uncommon phenomenon. Importantly, primary in-the-bag hydrophilic IOL opacification after routine cataract surgery is exceedingly rare.
“With modern IOL designs and appropriate patient selection, this has not been a clinically meaningful issue in my experience,” Dr Sherwin says.
He adds that recent data presented by researchers from St Thomas’ Hospital, London, at the 2025 ESCRS Congress show modern hydrophilic and hydrophobic IOL materials to be clinically and statistically equivalent in rates of posterior capsular opacification.
That, along with his research and his own patients’ feedback, has Dr Sherwin picking a surge in the Galaxy’s use once the product is included in Australia’s Prostheses List (PL), which he believes could come early in the new year.
“My cohort has been limited to people without private health insurance, so only uninsured cataract surgery patients and refractive lens exchange patients,” he says.
He notes that appropriate patient selection, counselling, and expectation management remain central, regardless of IOL platform.
“Once Galaxy is listed on the PL in Australia, I expect we’ll see a significant increase in uptake, particularly among surgeons looking for a full range of vision options with excellent visual quality.”

Dr Justin Sherwin predicts a significant uptake of the Galaxy IOL once it is listed on Australia’s Prostheses List.
Image: Rayner.
Image: Justin Sherwin.







Diabetes and hearing loss: Referral guidance for optometrists
Practising optometrists are well aware of diabetes’ effects on the eye, but its impact on hearing often goes unnoticed. Dr MEHWISH NISAH highlights the link between diabetes and hearing loss, providing practical guidance on screening and referral. By incorporating these strategies, optometrists can play a vital role in holistic care and improve outcomes for patients with diabetes.

The systemic and ocular changes that occur during the progression of diabetes mellitus are well-known to optometrists. However, the impact of diabetes on the auditory system is a less recognised but equally important consideration.
Compelling evidence indicates that individuals with diabetes are twice as likely to experience hearing loss compared with those without the condition, with the risk increasing further with age and the duration of diabetes.1
This significantly impairs the quality of life and diabetes self-management.
The routine interactions between optometrists and their diabetic patients can offer opportunities to detect early auditory dysfunction, facilitate timely referrals, and advance holistic care. 2
Such proactive screening expands the optometrist's role from eyecare specialist to broader advocate for the patient’s sensory wellbeing, and fosters a more integrated approach to chronic disease management.
THE OVERLOOKED LINK: DIABETES AND SENSORINEURAL HEARING LOSS
The evidence base connecting diabetes and sensorineural hearing loss is robust and growing. Multiple epidemiological

studies and meta-analyses demonstrate a higher prevalence and accelerated progression of sensorineural hearing loss in individuals with diabetes.1,3
A recent analysis found significantly higher hearing loss rates in Type 2 diabetes patients versus controls (53% vs 25.2%, p < .0001), with 15% unilateral and 29.6% bilateral loss in the diabetic group (both p < .01). 3
Sensorineural hearing loss, the most common diabetes-associated hearing loss, involves inner ear or auditory nerve damage with insidious progression.4
The underlying pathophysiological mechanisms mirror those of diabetic retinopathy: microangiopathy impairs cochlear blood supply, neuropathy disrupts auditory nerve transmission, metabolic disturbances harm hair cells, and basement membrane thickening impedes exchange processes, all cumulatively affecting high-frequency hearing and speech comprehension.5,6
WHY HEARING LOSS MATTERS IN COMPREHENSIVE DIABETES CARE
Untreated hearing loss profoundly impacts quality of life, causing social isolation, depression, and cognitive decline.7
Within diabetes management, hearing impairment disrupts essential patient-provider communication, compromising diabetes education, self-management, and treatment adherence, and ultimately worsening health outcomes. Additionally, hearing loss independently increases fall risk, compounding existing diabetes-related concerns from peripheral neuropathy. Early identification and intervention enable healthcare providers to mitigate these risks, enhancing overall patient wellbeing and optimising comprehensive diabetes care outcomes.8
SHARED PATHOPHYSIOLOGY: THE EYE AND THE EAR
Both the retina and cochlea are highly specialised, metabolically active structures dependent on intricate microvascular networks, rendering them exceptionally vulnerable to diabetic injury.5
Emerging evidence strengthens this connection: studies demonstrate that individuals with proliferative diabetic retinopathy face significantly elevated
ABOUT THE AUTHOR:
Centre for Hearing Research (CHEAR) School of Health and Rehabilitation Sciences The University of Queensland
Optometrists need to be mindful of hearing loss as well as visual issues when working with patients.
Image: New Africastock.adobe.com.
Image: Mehwish Nisar.
hearing loss risk compared with those with non-proliferative or absent retinopathy.5,9
This correlation positions advanced retinal disease as a systemic warning signal extending to auditory compromise.4
Table 1 compares the shared pathophysiology and differences between diabetic retinopathy and sensorineural hearing loss.
GUIDANCE FOR OPTOMETRISTS:
INTEGRATING HEARING AWARENESS
Optometrists are ideally placed to identify at-risk patients for diabetes-related hearing loss. By incorporating simple screening strategies into routine clinical practice, they can facilitate timely referrals.10,11
IN-PRACTICE SCREENING
The first step in identifying a potential hearing problem is to ask. A few targeted screening questions can be highly effective in flagging patients who may require further investigation (Table 2). These questions should be asked of all patients with diabetes, regardless of age or retinopathy status. A positive response should prompt a recommendation for a formal hearing assessment. In addition to direct questioning, validated screening questionnaires can be a quick and effective way to identify patients who may have a hearing problem.
REFERRAL TRIGGERS AND PATHWAYS
The decision to refer a patient for a hearing assessment should be based on a combination of the patient’s history, clinical findings and risk factors (Table 3). The presence of diabetic retinopathy, particularly PDR, should be considered a major red flag for other microvascular complications and should prompt a strong recommendation for a comprehensive hearing assessment.12
If a patient expresses any concerns about their hearing, it is essential to document these in the patient’s record and to make a formal referral.
The referral can be made to the patient’s general practitioner (GP), who can then coordinate a referral to an audiologist, or directly to an audiology clinic if local pathways permit.
The referral letter should clearly state the patient’s diabetes status, any relevant ocular findings, and the specific auditory concerns raised by the patient.15
Integrating hearing awareness into diabetes-related eyecare does not require optometrists to be audiologists. Instead, it involves adopting a proactive, observational approach to identify potential auditory concerns and facilitate timely referrals to appropriate specialists.
STRENGTHENING INTERPROFESSIONAL REFERRALS AND COLLABORATIVE CARE
Effective diabetes complication management demands collaborative,
Tissue Characteristics
Microangiopathy
Mitochondrial Dysfunction
Neural Degeneration
Oxidative Stress & Inflammation
Clinical Detection
Progression Pattern
Risk Correlation
Clinical Implication
Highly specialised, metabolically active tissues with intricate microvascular networks vulnerable to diabetic pathology
Endothelial dysfunction, basement membrane thickening, pericyte loss, capillary non-perfusion
High metabolic demand increases vulnerability to hyperglycaemia-induced mitochondrial dysfunction and ATP depletion
Neural degeneration secondary to microvascular damage affects both organs
Hyperglycaemia-induced oxidative stress and inflammation cause apoptosis and cellular dysfunction
Insidious, progressive deterioration linked to glycaemic control
Both increase with diabetes duration, poor glycaemic control (elevated HbA1c), hypertension, and hyperlipidaemia
Presence of retinopathy (especially PDR) strongly suggests systemic microvascular compromise
Retinal layers with ganglion cells and photoreceptors
Microaneurysms, haemorrhages, cotton wool spots, neovascularisation
Retinal ganglion cells require high ATP production
Ganglion cell and nerve fibre layer damage, causing visual field defects
Ganglion cell apoptosis, photoreceptor dysfunction, blood-retinal barrier breakdown
Fundoscopy, fundus photography, OCT imaging
Variable (mild NPDR moderate/severe NPDR PDR); may include macular oedema
PDR indicates advanced microvascular disease
Visible marker of systemic microvascular damage
Stria vascularis and sensory hair cells
D isrupted stria vascularis blood supply; outer hair cell loss (basal turns)
Stria vascularis marginal cells have high mitochondrial density; vulnerable to ATP depletion
Auditory nerve damage and hair cell loss impairing sound transmission
Hair cell apoptosis, stria vascularis dysfunction, loss of endocochlear potential
Pure-tone audiometry and specialised hearing tests
High-frequency SNHL (4-8 kHz) progressing to lower frequencies; bilateral and symmetrical
PDR associated with 7.74× higher risk of hearing loss
Often underdiagnosed; impacts communication, quality of life, diabetes self-management
SNHL = Sensorineural Hearing Loss; ATP = Adenosine Triphosphate; OCT = Optical Coherence Tomography; NPDR = Non-Proliferative Diabetic Retinopathy; PDR = Proliferative Diabetic Retinopathy; HbA1c = Glycated Haemoglobin (glycosylated haemoglobin)
Category
interprofessional approaches, with optometrists best positioned to initiate crucial hearing care referral pathways. 2
Optimal care utilises integrated electronic health records enabling seamless, secure information sharing among optometrists, GPs, endocrinologists, and audiologists, ensuring comprehensive patient profiles across providers.
Optometry practices should develop clear, formal referral protocols with local audiology clinics and GPs through pre-printed referral pads, digital templates, or secure messaging channels that streamline processes.
Multidisciplinary team meetings and informal case discussions significantly enhance coordination for complex diabetic patients. 2,4
Practical communication improvements
Question
noticed any changes in your hearing recently?"
you find it difficult to follow conversations in noisy environments, such as restaurants?"
you frequently need to ask people to repeat themselves?"
include clear, concise referral letters that explicitly state the patient's diabetic status, the referral rationale, and relevant ocular findings.
Optometrists should explicitly request feedback from audiologists or GPs on assessment findings, thereby closing the communication loop and enriching their understanding of patients' systemic health status, and ultimately fostering more comprehensive, coordinated diabetes care across specialties.11,15
DETECTION AND PREVENTIVE OPPORTUNITIES
Early hearing loss detection in diabetic populations enables timely intervention, potentially slowing progression, improving communication, and enhancing quality of life.
TABLE 1. Shared Pathophysiology Between Diabetic Retinopathy and Sensorineural Hearing Loss 3,11
TABLE 2. Example of screening questions for patients with diabetes
TABLE 3. Diabetes and hearing loss – optometric referral guidance5,13,15
Patient
Diabetes + No DR + No hearing concerns
Diabetes + No DR + Hearing concerns
Diabetes + NPDR + No hearing concerns
Educate on the diabetes-hearing link. Recommend hearing check if >2 years since last assessment. Document. Routine
D ocument concerns. Refer to the GP/audiologist for a comprehensive assessment. Standard
Educate on systemic diabetes effects and the retinopathy-hearing link. Strongly recommend a hearing check. Document. Standard
Diabetes + NPDR + Hearing concerns D ocument concerns. Emphasise heightened risk. Refer to GP/audiologist. Request feedback. Standard-Urgent
Diabetes + PDR (any hearing status)
Urgent ophthalmology referral for PDR. Simultaneously refer to the GP/audiologist for hearing assessment. Communicate findings to GP/endocrinologist.
While standardised screening guidelines remain undeveloped, pragmatic approaches include baseline hearing assessment following diabetes diagnosis, periodic screenings every one to three years, particularly for patients with diabetic retinopathy, poor glycaemic control, or microvascular complications, and prompt assessment when hearing difficulties emerge.
Optometrists can employ opportunistic screening through simple questions to identify patients requiring formal audiological evaluation, a practical approach for busy practices.
Formal audiological assessment by qualified audiologists using pure-tone and speech audiometry remains the diagnostic gold standard. 3
Additionally, validated smartphone applications and online hearing screeners provide initial indicative assessments; while non-diagnostic, these tools can motivate professional evaluation, and optometrists can recommend them to concerned patients as preliminary screening steps before formal audiological referral.
POPULATION CONSIDERATIONS:
FOCUS ON AT-RISK GROUPS
Specific population risks and cultural factors critically inform diabetes and hearing loss management.
In Australia, Aboriginal and Torres Strait
References:
1. Nisar M, Dawes P. Diabetes and hearing loss: A call to action for early detection and prevention. Australian Journal of General Practice 2025;54:747-9.
2. C olagiuri R. The optometrist's role in the multidisciplinary diabetes team: towards a more holistic approach. Clinical and Experimental Optometry 1999;82(2-3):55-8.
3. Kim CHs, Lauritsen KL, Nguyen SA, Meyer TA, Cumpston EC, Pelic J, et al. Characteristics of Hearing Loss in Type 2 Diabetes Mellitus: A Systematic Review and Meta–Analysis. Otolaryngology–Head and Neck Surgery 2025.
4. K han MA, Qureshi A, Faisal Z, Fatima K, Farooq M, Ahmed W. Assessing the Correlation between Hearing Loss and Diabetic Retinopathy Severity in Patients at A Tertiary Care Hospital in Pakistan: Correlation Between Hearing Loss and Diabetic Retinopathy Severity in Patients. Pakistan Journal of Health Sciences 2025:176-80.
5. Alizadeh Y, Jalali MM, Sehati A. Association of different severity of diabetic retinopathy and hearing loss in type 2 diabetes mellitus. American Journal of Otolaryngology 2022;43(2):103383.
6. Kurt E, Öztürk F, Günen A, Sadikoglu Y, Sari RA, Yoldas TK, et al. Relationship of retinopathy and hearing loss in type 2 diabetes mellitus. Annals of ophthalmology 2002;34(3):216-22.
Urgent
Islander peoples experience significantly elevated Type 2 diabetes rates with earlier onset and severe complications, alongside alarmingly high chronic otitis media rates and childhood-onset hearing loss, exacerbating diabetes-related hearing loss and creating profound auditory challenges.1
Culturally and linguistically diverse immigrant communities also demonstrate higher diabetes prevalence and less
Protocols should incorporate routine holistic sensory screening using validated point-of-care tools, identifying both retinopathy and hearing loss in optometry and general practice settings.
Enhanced interdisciplinary training would strengthen understanding and improve referral processes and collaborative management.
Technological innovations –tele-audiology and AI-powered remote screening – promise expanded accessibility in underserved populations, mirroring successful tele-ophthalmology models.
Additionally, patient empowerment through comprehensive complication education will enhance self-management engagement and screening adherence, optimising long-term visual and auditory health outcomes.
CONCLUSION
Hearing loss is a significant and often-overlooked complication of diabetes with a substantial impact on an individual's quality of life.
Optometrists, as primary eyecare providers, are in a unique position to
“THE PRESENCE OF DIABETIC RETINOPATHY, PARTICULARLY PDR, SHOULD BE CONSIDERED A MAJOR RED FLAG FOR OTHER MICROVASCULAR COMPLICATIONS AND SHOULD PROMPT A STRONG RECOMMENDATION FOR A COMPREHENSIVE HEARING ASSESSMENT.”
utilisation of hearing care services.7,14
Addressing these disparities requires accessible screening programs, culturally relevant educational materials, and robust partnerships with indigenous health services and multicultural community organisations for equitable, effective care delivery.
LOOKING AHEAD: INTEGRATION IN DIABETES PROTOCOLS
Future diabetes management requires integrated, patient-centred approaches transcending “siloed specialist care”.
7. Strutt PA, Barnier AJ, Savage G, Picard G, Kochan NA, Sachdev P, et al. Hearing loss, cognition, and risk of neurocognitive disorder: evidence from a longitudinal cohort study of older adult Australians. Aging, Neuropsychology, and Cognition 2022;29(1):121-38.
8. V ignesh S, Jaya V, Moses A, Muraleedharan A. Identifying early onset of hearing loss in young adults with diabetes mellitus type 2 using high frequency audiometry. Indian Journal of Otolaryngology and Head & Neck Surgery 2015;67(3):234-7.
9. Shin YU, Park SH, Chung JH, Lee SH, Cho H. Diabetic retinopathy and hearing loss: results from the Fifth Korean National Health and Nutrition Survey. Journal of Clinical Medicine 2021;10(11):2398.
10. G ündoğan M, Gündoğan F, Bayram N, Demircan S, Mutlu C. Evaluation of hearing function in patients with type 2 diabetes mellitus and investigation of its relationship with stages of diabetic retinopathy. Journal of Diabetes & Metabolic Disorders 2025;24(1):143.
11. Al-Abed SA, Hakooz MM, Teimat MH, Aldurgham GA, Alhusban WK, Hjazeen AA, et al. A correlational study of hearing loss and severity of diabetic retinopathy among Jordanian patients. Cureus 2023;15(8).
12. A rmstrong D, Stratton RD, Afzal A. Oxidative stress and antioxidant protection : the science of free radical biology and disease. 1st ed. ed. Hoboken, New Jersey: Wiley Blackwell; 2016.
identify patients at risk and facilitate early referral for auditory assessment. By recognising the shared pathophysiology of the eye and the ear in diabetes, and by integrating simple screening questions and referral practices into their routine care, optometrists can play a vital role in improving the overall health and wellbeing of their patients with diabetes.
The time has come to break the silence on diabetic hearing loss and embrace a more integrated approach to sensory care in diabetes management.
13. O oley C, Jun W, Le K, Kim A, Rock N, Cardenal M, et al. Correlational study of diabetic retinopathy and hearing loss. Optometry and Vision Science 2017;94(3):339-44.
14. Nickbakht M, Furze C, Nisar M, Waite M, Scarinci N, Newall J, et al. Factors influencing the use of hearing services by diverse ethnic communities in Australia. Ear and hearing 2025:10.1097.
15. D iSogra RM, Beck DL. How chronic illnesses impact hearing, balance, and cognition: a guide for hearing care professionals. Hearing Review [Internet]. 2025 Mar 12 [cited 2025 Nov 8]; Available from: https://hearingreview. com/hearing-loss/health-wellness/how-chronic-illnesses-impact-hearing-balance-and-cognition-a-guide-forhearing-care-professionals

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.


DR = Diabetic Retinopathy, NPDR = Non-Proliferative Diabetic Retinopathy, PDR = Proliferative Diabetic Retinopathy,
GP = General Practitioner
KEEP KIDS UNSTOPPABLE
With ACUVUE® Abiliti® 1-Day Soft Therapeutic Lenses for Myopia Management




A UNIQUE ROLE IN THE VISION LOSS JOURNEY
Clinical and research orthoptist JACINTA WALZ explores how orthoptists are uniquely placed to support patients experiencing vision loss, through initial presentation and diagnosis to therapy, management and rehabilitation.

"THE ORTHOPTIST IS UNIQUELY PLACED TO BE A HUMAN FACE AND STABLE RELATIONSHIP FOR PATIENTS IN AN OTHERWISE DESTABILISING AND OFTEN DISTRESSING PROCESS OF VISION LOSS."
For patients, the early part of the vision loss journey can be emotionally distressing, and the battery of testing and multiple doctors’ appointments can be tiresome and confusing. Here, the orthoptist is well-equipped to support patients with crucial education alongside empathetic and balanced patient education.
All experiences of vision loss have significant emotional, psychological, and functional implications for patients. In the case of unexplained vision loss these consequences can be exacerbated by multiple doctor visits, complex testing, and lengthy wait-times which extend periods of uncertainty and confusion.
Among this suite, visual electrophysiology plays a crucial role in assessing baseline function of the visual system to localise and diagnose disease. Testing itself, is a lengthy and highly specialised process and patients spend up to several hours with a clinician. During this time, questions regarding potential diagnoses, as well as the reasoning for and process for testing often arise. There is a general lack of understanding regarding the need for and process of testing in the general community, and often within the ophthalmic community as well. As a result, patients often present without a background understanding of why they need testing, or what it will look like.

and disconcerting for patients when the process is not clearly described or explained. Precise application of electrodes, particularly corneal electrodes, requires detailed knowledge of the eye and visual system to ensure accurate results and protect patient safety. Excellent communication and empathy are also required to support patient cooperation and attention throughout assessment. A need that is only heightened when working with children, and patients with additional needs and disabilities.
multiple external services or making recommendations within their own clinical framework to provide low vision support. Orthoptic expertise in explaining the implications of a diagnosis on functional vision and daily living can help support the patient beyond the testing environment, investing in their material functional needs especially in cases where treatment and recovery of vision is not currently possible.
During the appointment, therefore, technicians without ophthalmic expertise are faced with having to provide nuanced counsel or refer patient questions to their specialist at another time. Here, orthoptists are especially skilled to fill this gap, bringing a detailed ophthalmic understanding alongside empathetic patient counsel.
As specialised eyecare professionals, orthoptists are accustomed to providing disease-specific patient education in the clinical space to utilise a deep understanding of ocular anatomy and physiology and clinical experience. This expertise lends itself naturally to providing counsel and education for patients experiencing complex vision loss.
Guiding patients through complicated vision testing is part and parcel of the orthoptist’s role. Testing can be confronting, tiring,
In the suite of electrophysiology tests, each one targets a different structure or function of the visual system. While the various electroretinograms (ERGs) can look similar, each is designed to measure different retinal functions, from localised macular function in the pattern and multifocal ERGs, to global rod and cone function in the full-field ERG. To patients, these tests can seem repetitive and tiresome. Without clear discussion of the function of each test, attention can wane, affecting the reliability and accuracy of results, and introducing artefacts that can impact diagnostic interpretation. The technician’s understanding of ocular anatomy and physiology, and their ability to convey this clearly to patients is critical for supporting patients during testing to obtain accurate and meaningful results. Beyond testing, once a diagnosis is made, orthoptists are well-equipped to journey with patients through accessing rehabilitative and therapeutic support, acting as either the connecting point between
Journeying alongside patients through their vision loss creates opportunities for orthoptists to work to their full scope of practice. From investigation, diagnosis and counsel, to accessing low vision support, the orthoptist is uniquely placed to be a human face and stable relationship for patients in an otherwise destabilising and often distressing process of vision loss. Creating spaces for these skillsets to be explored and developed to meet an ever-growing need in our healthcare system also supports the growth and development of the orthoptic workforce to provide higher quality, individualised healthcare that supports the patient’s direct needs and goals throughout their eyecare journey.
Image: Sai Thaw Kyar/Shutterstock.com
Orthoptists are accustomed to utilising their understanding of ocular anatomy and physiology to provide disease-specific patient education.
ABOUT THE AUTHOR: Jacinta Walz is a PhD candidate at University of Technology Sydney, and a clinical and research orthoptist and electrophysiology technician at the Save Sight Institute at University of Sydney.
Image: Jacinta Walz
ORTHOPTICS AUSTRALIA is the national peak body representing orthoptists in Australia. OA’s Vision is to support orthoptists to provide excellence and equity in eye health care. Visit: orthoptics.org.au
A FRONT-ROW SEAT TO A CHANGING INDUSTRY
With 55 years’ experience in the optical industry, LYN SIMEON shares her personal journey through the evolving world of contact lenses.

“EDUCATION AND REGULAR CHECK-UPS REMAIN ESSENTIAL, NO MATTER HOW MODERN THE LENSES BECOME.”
After more than five decades in the optical industry, I still smile when I think about how much has changed, and how much I’ve loved being part of it. I began my optical career in 1970, not knowing that it would lead me through OPSM, private practice, casual work with Specsavers, and eventually to my current role as a manager with Teachers Health Fund. Each step has shaped me, challenged me and broadened my understanding of eyecare in ways I never expected – especially these last 14 years, where my role as manager of eyecare, dental and membership services has expanded my knowledge far beyond optics alone.
But if there’s one thread running through my career, it’s contact lenses. Their evolution has mirrored the evolution of our industry, and I’ve been fortunate to witness it all from the front row.

When I entered optics, most people wore hard contact lenses. Soft lenses existed, but the early versions were still finding their place. It’s amusing now to think back to Leonardo da Vinci imagining, in 1508, that vision could be corrected by placing water over the eye. Then in 1887, F.A. Müller created the first real contact lens – out of glass, heavy and uncomfortable. Thankfully, by the 1930s we had hard plastic lenses, and by the 1960s soft lenses were introduced. By the time I started working in the 1970s, soft lenses were being mass-produced and rapidly becoming popular.
With them came a cleaning and care regime that would make today’s contact lens wearers’ eyes widen. Cleaning and storing lenses was an involved, sometimes stressful process. Patients had to wash lenses by hand using detailed, multi-step instructions. I remember selling sterilising machines early in my career – bulky, humming boxes that promised to make the job easier. Then there were the solutions: cleaners, conditioners, soaking liquids, enzyme tablets. If a patient skipped a step or misunderstood a label, you could almost guarantee discomfort later.
Comparing that era to now is like comparing a typewriter to a smartphone.
Disposable lenses have changed everything. Their design has not only improved convenience but also reduced the risk of infection and irritation. Patients who were once anxious about cleaning routines suddenly had a lens option that fit seamlessly into their lives.
And the choice available today is remarkable. Daily disposables, extended wear lenses, toric lenses for astigmatism, and lenses designed for keratoconus have opened the door for more people to wear contacts comfortably. Multifocals have improved the quality of life for patients requiring both distance and near correction, while coloured lenses have given people a fun, cosmetic option to express themselves.
Then there’s the future, summed up in two words: smart lenses. The idea that lenses may one day monitor health indicators like blood sugar or deliver medication directly to the eye would have sounded like science fiction when I started working in eyecare. Now, it’s within reach.
I’ve always enjoyed watching how contact lenses shape people’s confidence and daily life. For athletes, they offer freedom – no glasses slipping down the nose or fogging up mid-game. For others, contact lenses allow a natural look where their face is free of frames.
I’ve seen patients walk out taller, happier, relieved to find vision that feels easy and natural.
But progress brings new challenges, too. Coloured lenses sold online are cause for concern. Without proper fitting or professional guidance, people risk infections or complications that could have been avoided. A practitioner doesn’t just fit the lens; they teach, support and monitor eye health. Education and regular check-ups remain essential, no matter how modern the lenses become.
Looking back, I feel proud of the part I’ve played. From counselling nervous first-time wearers to staying across the latest technologies, the work has always felt meaningful. Contact lenses are more than just medical devices. They offer freedom, practicality and confidence, and they continue to evolve with every generation.
Looking ahead, I believe younger people will see contact lenses not only as vision aids but as smart tools that blend health, lifestyle and technology. And if the past 55 years have taught me anything, it’s that this journey is far from over.
ABOUT THE AUTHOR: Lyn Simeon worked with OPSM for 35 years, becoming a manager and lens specialist for the west region. She then managed a private practice for seven years while also undertaking casual work with Specsavers, before moving to Teachers Health Fund, where she has spent the past 14 years as manager of eyecare, dental and membership services.
Image: sergey Kolesnikov/Shutterstock.com
LYN SIMEON
Soft contact lenses were rapidly becoming popular when Lyn Simeon started working in eyecare in the 1970s.
Image: Lyn Simeon.
PROTECT YOUR PRACTICE AGAINST MEDICARE FRAUD
Practice owners and managers need to understand that risk is not just about what goes on in their clinic rooms; there is also plenty of risk and responsibility around what happens with Medicare claims and billing.

Your practice manager is away for four weeks of long overdue leave, so you bring in an experienced temporary administrator to help manage billing and reception. A few days into the role, she quietly asks if you have changed your bulk billing policy.

“YOU NEED APPROPRIATE OVERSIGHT OF ADMINISTRATIVE PROCESSES, CLEAR EXPECTATIONS, AND SYSTEMS THAT ARE FOLLOWED CONSISTENTLY.”
According to your software, several pensioners and health care card holders have recently been recorded as owing small cash gaps. Yet the processed Medicare claims show bulk billed services with no patient contribution.
She also notices that item numbers for some tests appear in the system without corresponding clinical entries. When she raises her concerns, you realise these entries occurred before she arrived and were processed under your regular manager’s login.
At first, you assume it is a staff training issue or a documentation error. But as you compare records more closely, more inconsistencies emerge. You start to worry not only about the financial implications, but also about the risk to your professional reputation if Medicare considers these anomalies fraudulent. Situations like this are deeply uncomfortable for practitioners. Most optometrists and ophthalmologists trust their staff and work in close teams. However, Medicare misuse and internal fraud can stay hidden for long periods, often only surfacing when someone new looks at the data with fresh eyes. Even honest practices can unintentionally create opportunities for misuse if their internal systems are not strong enough.
Understanding your legal obligations and improving oversight can significantly reduce your risk.
Delegating Medicare billing responsibilities does not remove a practice’s accountability.
MEDICARE FRAUD IN EYECARE PRACTICES
Fraud in health settings often begins with small administrative shortcuts

rather than deliberate wrongdoing. Common patterns include:
SKIMMING GAP PAYMENTS
A staff member bulk bills a patient but collects a separate cash or EFTPOS gap that is not recorded in the system.
Altering item numbers
This includes modifying billed items without the practitioner’s knowledge. For example, upgrading a consultation item or adding a diagnostic test such as optical coherence tomography or visual fields that was never performed.
FALSE CANCELLATIONS AND REVERSALS
This occurs when a staff member reverses or reprocesses claims to manipulate payments or hide discrepancies.
These acts exploit administrative vulnerabilities rather than clinical decision making. However, responsibility for what is billed under your provider number rests with you, even when you delegate tasks to staff.
YOUR OBLIGATIONS
As a practitioner, you must take reasonable steps to ensure all claims made under your provider number are accurate and supported by clinical records. Delegating billing responsibilities does not remove your accountability.
That means taking an active interest in how billing is handled in your practice. You do not need to micromanage staff, but you do need appropriate oversight of administrative processes, clear expectations, and systems that are followed consistently.
If Medicare identifies irregularities, you may be required to repay benefits or undergo a Professional Services Review. In more serious cases, fraudulent activity can lead to criminal investigation.
This is why oversight must be deliberate and consistent. The aim is not to introduce suspicion into your team, but to ensure your systems are strong enough to protect both your staff and your practice.
PRACTICAL STEPS TO PROTECT YOUR PRACTICE
1. Strengthen recruitment and screening
Ensure that all staff who handle billing or payments undergo appropriate integrity checks, including reference
checks and a probationary period. Temporary staff can also help reveal blind spots, as in the vignette.
2. Limit access within your systems
Configure your practice management software so staff can only perform functions relevant to their roles and so changes are automatically recorded. Your systems should clearly show who made an entry or amendment, and when they made it, making it easier to identify and resolve issues if questions are later raised. Limit who can alter item numbers, reverse transactions, create new patient records or modify bank details and ensure staff do not access systems using shared log-ins.
3. Review Medicare billings regularly
Practitioners should receive and review daily or session-based summaries of the items billed under their provider number. These reviews help detect errors and irregularities early.
4. Reconcile accounts frequently
Weekly and monthly reconciliation of Medicare payments, EFTPOS reports, diagnostic testing volumes and practice software records is essential. Any inconsistencies should be followed up quickly.
5. Require shared approval for high-risk tasks
Where possible ensure two authorised staff members approve refunds, reversals and adjustments. Staff who reconcile accounts should ideally have read-only access.
6. Maintain STRONG FINANCIAL CONTROLS
Clear processes for cash handling, overtime approval, banking and payroll reduce opportunities for misuse. Cash should be banked daily.
7. Consider independent book-keeping or external review
Engaging an external provider to handle bookkeeping or payroll introduces separation of duties that protects the practice. Confirm they comply with privacy obligations, store data within Australia and follow strong cyber security standards.
ABOUT THE AUTHORS: Sonya Black is legal team manager – Workplace Law, Avant. Gail Wang is risk advisor, Member Advisory Services, Avant.
Below:
Image: Sonya Black.
Images: Gail Wang.
PATIENTS CAN’T LIVE WITH AN UNFAIR SYSTEM

BY DR KATHY CHAPMAN
Eye health professionals know better than anyone that sight-saving treatment for macular disease is not optional – it’s essential. Yet, more than 12,200 Australians face the prospect of losing access to intravitreal (eye) injection treatment due to the Federal Government’s proposed changes to the Medicare Benefits Schedule (MBS) items for eye injections.
In early 2025, the Government deferred its decision to reclassify these injections from Type B to Type C for private health insurance purposes by a year, with further consultation held in November.
If the change goes ahead on 1 July 2026, most patients who have been using their private health insurance to cover the cost of eye injections in private hospitals and day surgeries will no longer be able to do so. Instead, they’ll face significant out-of-pocket costs in private clinics.
When news of this reclassification broke, our Helpline received over 100 phone calls from community members concerned about affording treatment if this planned change proceeds. Their concern is valid: cost is a leading reason people stop treatment.
The outcome of this proposed reclassification is not just an isolated change, but another sign of a system which fails to recognise that many Australians are already struggling with the affordability of sight-saving treatment for their macular disease.
The Government has an opportunity to continue to pause the reclassification and address the broader affordability problem before it worsens. That is why Macular Disease Foundation Australia (MDFA) is urging the government to further delay this change until
reforms are introduced ensuring adequate access to affordable eye injection treatment across Australia.
As we know, eye injection treatment for macular disease is lifelong and frequent. There are an estimated 1.9 million people in Australia living with a macular disease. In 2023, around 109,000 people with a treatable macular disease, including neovascular age-related macular degeneration (AMD), diabetic macular oedema, and retinal vein occlusion, received eye injection treatments in the private system.
Treatment persistence is a significant problem in Australia, with approximately 50% of people discontinuing treatment within five years of starting eye injections.
A key reason for this is cost burden. In 2023, only 28% of patients nationally had eye injections that were bulk-billed, meaning that more than 72,000 people had no choice but to pay out-of-pocket costs to keep their sight, with more than 12,200 people using their private health insurance to cover costs.
In Australia, public hospital eye injection outpatient services are either unavailable or overstretched across the nation, so for most people treatment in the private system with significant ongoing out-of-pocket costs is the only option.
Add to that the other costs of living with a macular disease, like eye specialist appointments and low vision aids, and it is little wonder that financial burden becomes overwhelming, particularly for people on an age pension.
We recently released research revealing that the median total annual cost for people living with macular disease who receive sight-saving eye injections is 12% ($3,621) of the annual government pension payment. Our research also found that for almost 1 in 10 Australians who receive eye injections, the cost of living with their condition is more than $6,000 every year.
The financially vulnerable are the last people who should have to pay through the nose to keep their vision.
MDFA has made key recommendations to the government. We propose:
• Reforming the Extended Medicare Safety Net so it does not reset at

the start of the calendar year for pension card holders receiving ongoing eye injection treatment for neovascular AMD, from the second calendar year after starting treatment.
• Establishing a Neovascular AMD Treatment Incentive Program to encourage ophthalmologists to bulk-bill pension card holders having eye injections for neovascular AMD, supporting the most financially vulnerable patients who are most at risk of stopping treatment due to burden of cost.
• Integrating the Pharmaceutical Reform Agreements into the National Health Reform Agreement to ensure that PBS-listed eye injection treatments are available and adequately funded in public hospital eye injection outpatient clinics in every state and territory. We are running an advocacy campaign, asking people to share how treatment costs have impacted them. These stories will be sent to Federal Health Minister Mr Mark Butler.
We would appreciate your support by encouraging patients to contact MDFA to share their concerns. A downloadable letter template is available at www.mdfoundation.com.au/eyeinjection-typec-change/. Sight-saving treatment is essential – not just for those who can afford it. The Government must act now to ensure that access challenges to affordable treatment don’t stand in the way of preserving vision. Your support can help make that happen.
ABOUT THE AUTHOR
Name: Dr Kathy Chapman
Qualifications: BSc, M Nutr & Diet, PhD
Affiliations: CEO of Macular Disease
Foundation Australia
Location: Sydney, Australia
Years in industry: 4 (+30 years in public health)
ABOVE: MDFA says more than 12,200 Australians risk losing access to intravitreal injections if the Federal Government's proposed changes are adopted.
"The Government has an opportunity to continue to pause the reclassification and address the broader affordability problem before it worsens."
Image: MDFA.
Image: Iuriistock.adobe.com.
EVENTS CALENDAR
To list an event in our calendar email: rob.mitchell@primecreative.com.au

FEBRUARY
34TH ANZ GLAUCOMA SOCIETY CONGRESS
Sydney, NSW 15 – 16 February anzgsconference.com
100% OPTICAL London, UK 28 February – 2 March 100percentoptical.com
MARCH
RANZCO GLOBAL EYE HEALTH & INTERNATIONAL AGENCY FOR PREVENTION OF BLINDNESS CONFERENCE Hobart, Australia 6 – 8 March conferences.com.au/2026ranzco
OWA WAVE 2026 CONFERENCE Fremantle, Australia 21 – 22 March optometry.org.au
4TH INTERNATIONAL OPHTHALMOLOGY CONFERENCE (IOC2026) Singapore 23 – 26 March ophthalmology.magnusconferences.com
MAY
OPTOMETRY NSW/ACT SUPER SUNDAY Sydney 24 May optometry.org.au

AUGUST
O-SHOW 2026
Melbourne 16 – 17 August o-show.com.au
19TH APAC VITREORETINAL SOCIETY (APVRS) CONGRESS
Brisbane 28 – 30 August apvrs.org/congresses
SEPTEMBER
SPECSAVERS CLINICAL CONFERENCE 2026
Gold Coast 12 – 13 September specsaversclinicalconference.com.au

Brisbane is to play host to the 19th APAC Vitreoretinal Society Congress in August.
The 2026 Specsavers Clinical Conference will be heading back to the Gold Coast.
The catwalk, featuring new frames and designs, will be a feature of the 100% Optical event in London in February.
Image: 100% Optical.
Image: Specsavers.
Image: Matt Murray/stock.adobe.com.
SPECSAVERS’ DAME MARY PERKINS AWARD FOR OUTSTANDING PATIENT CARE HONOURS
OPTOMETRISTS WHO HAVE MADE AN EXTRAORDINARY IMPACT ON THE VISION AND LIVES OF THEIR PATIENTS. INSIGHT TALKS TO SOME OF THE FINALISTS ABOUT THAT

Specsavers Stories –AMY
GOLLSCHEWSKY
Why did you pursue an optometry career?
I chose optometry because I wanted a career in healthcare where I could make a meaningful difference in people’s lives. I value the balance of clinical skills and patient care and the ability to educate people about their vision and eye health.
How did you come to work at Specsavers?
I was working for another corporate when an opportunity arose in my suburb. I was impressed by Specsavers’ focus on affordable, accessible eyecare and the collaborative clinical environment. I have felt supported professionally and academically, with opportunities for growth and leadership. I’ve also formed strong relationships with local ophthalmologists and healthcare professionals while having the freedom to practice within my chosen scope.
Why were you nominated for the Dame Mary Perkins Award?
I was nominated for the management of a patient that not only saved his vision, but also saved his life.
What did you do in handling this case?
The 38-year-old patient came in for a routine exam, which revealed significant inflammation and unexplained retinopathy. I referred him urgently to his GP and followed up when he did not respond, leading to diagnoses of uncontrolled hypertension and diabetes. Further exams confirmed primary open angle glaucoma.
What was the outcome?

Through coordinated care with optometry, ophthalmology, and his GP, his health and wellbeing improved. His glaucoma was managed early, preventing significant vision loss – a major risk at his age. He became happier, healthier, and more motivated, changing the course of his life.
How did Specsavers’ training and support help you with this patient?
Specsavers invests in professional development through annual clinical conferences, webinars, and workshops that keep us current with clinical standards and technology. This training builds confidence to manage patients empathetically, and Oculo streamlines referrals and clinician communication. We also benefit from strong relationships with local ophthalmologists who provide advice and support.
What did you learn from helping and supporting the patient?
This case showed that multiple comorbidities can coexist and not to settle on a single diagnosis.
When the patient returned with acute visual field loss after a migraine, I initially suspected a vascular incident. However, further examination, family history, and consultation led to diagnosing primary open angle glaucoma.
Why are you proud to be a Specsavers optometrist?
Every day I make a real difference by providing quality eyecare and eyewear to people from all backgrounds. I love being part of a team that values community connections and offers reassurance when patients leave feeling supported.
SPECSAVERS STATS: Name: Amy Gollschewsky | Current position : Senior optometrist | Location: Specsavers Midland Crescent | Years within the business: 13 years (including 10 years at Specsavers Ellenbrook)
Specsavers
SO LET’S TALK!
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Optometrist employment enquiries: Specsavers Recruitment Services –anz.srsdepartment@specsavers.com
Locum employment enquiries: ANZ.locumteam@specsavers.com
Graduate employment enquiries: apac.graduateteam@specsavers.com
ALL SPECSAVERS STORES NOW WITH OCT
Optometrist Joint Venture Partnership Opportunity –New Store in Cobram, VIC!
Be part of something new! Specsavers is seeking an Optometrist to join us as a Joint Venture Partner at our Cobram store. Nestled on the banks of the Murray River, Cobram is a charming town celebrated for its sandy river beaches, scenic landscapes, and vibrant local community. As a Joint Venture Partner, you’ll enjoy a guaranteed salary, a share in dividends, and the chance to build and lead your own team. The store will feature a modern fit-out with OCT, digital displays, and the latest equipment. With accessible financial support through Specsavers’ loan program, and full back-office support including payroll, accounts, and BAS, you’ll be set up for success from day one.
Optometrist Opportunity Kadina – Relocation Bonus
Ready for a change? Our Kadina store is looking for a Full-Time Optometrist to join the team from April/May. Earn up to $120K + super plus a $5K relocation bonus. You’ll work in a modern 5-room clinic with advanced tech including HFA III and IPL, alongside two supportive Optometrists. The team is fun, social and big on flexibility, making it easy to enjoy nearby beaches, cafés, markets and wineries. With a largely older patient base, you’ll take on meaningful clinical work daily, from glaucoma co-management to diabetic eye care, cataracts, red-eye treatment and foreign body removal.
Optometrist Opportunity – Specsavers Shirley, NZ
Join Specsavers Shirley in Christchurch as a full-time Optometrist and kickstart 2026 with an exciting new role. Enjoy a supportive team, modern equipment, and a varied patient base. With excellent development opportunities and a strong clinical focus, this is the perfect place to grow your skills and make a real community impact.
Graduate Opportunities
The Specsavers ‘Early Bird Package’ is now live! For select opportunities across Australia and New Zealand, final year optometry students will be eligible for either a $30,000 or $20,000 sign on bonus when they sign an employment contract before June 30 2026. With continued growth in providing eyecare to patients across ANZ, now is an exciting time to join a company that is leading and defining the future of the optical profession. If you’re a final year student or recently graduated, please contact anz.graduateoptometry@specsavers.com for more information.
Images: Specsavers.
People on the move

OPTOMETRY AUSTRALIA APPOINTS NEW CEO
Optometry Australia (OA) has appointed Mark Nevin as CEO, following the departure of Skye Cappuccio. Nevin has held executive leadership positions across multiple peak bodies, including CEO of the Royal Australian and New Zealand College of Radiologists, the Australasian Institute of Digital Health, Cancer Council Australia and, most recently, Lifestart Disability Services. His career has spanned governance, system redesign, regulatory affairs and the adoption of new clinical and digital technologies. Nevin began his professional life as an optometrist in Ireland and the UK. He later oversaw policy and strategy for three UK optometry bodies and served on the executive committee of the European Council of Optometry and Optics.

NEW CHAIR AT MACULAR DISEASE FOUNDATION AUSTRALIA
Macular Disease Foundation Australia (MDFA) has announced Professor Sanchia Aranda AM as its new chair, following Graeme Head AO stepping down after four years in the role. Prof Aranda, who joined the MDFA board in 2025, brings extensive expertise across health, education, research, disability and the for-purpose sector. She has led organisational transformation, strengthened governance, championed consumer involvement in cancer research, and is highly experienced in leading public education campaigns. Currently chair of Scope Australia and the Victorian Comprehensive Cancer Centre Alliance, Prof Aranda began her career in nursing and was the first nurse to lead Cancer Council Australia as CEO.

ESSILORLUXOTTICA PROMOTES KODARI TO LEADERSHIP ROLE
Elizabeth Kodari has recently been appointed vice president, store operations, EssilorLuxottica ANZ. Kodari joined the group as an OPSM optometrist in 2015, and has significantly contributed to the business in different capacities over the years, most recently leading the NSW, VIC, ACT and TAS optical teams. Carl James, senior vice president, operations ANZ at EssilorLuxottica said he has had the privilege of working with Elizabeth over the years, and has no doubt her leadership and technical competencies will lead her and the team to many successes.

MARKETING DIRECTOR ADVANCES CAREER AT ALCON
Alcon has announced Ronak Patel has been appointed as country franchise head – Vision Care Australia and New Zealand. In her new role, Patel will apply her wealth of commercial and business development experience to deliver value to eyecare professionals and support sustainable growth across the optometry industry. Most recently, Patel held the role of area marketing director for APAC, where she led Alcon’s international marketing strategy and go-to-market plans across six highly diverse markets in APAC. Patel holds an MBA from Manchester Business School and a BSc in medicinal chemistry from the University of Manchester. She joined Ciba Vision/Alcon in 2008.

VITREORETINAL SURGEON JOINS MORETON EYE GROUP
Dr Aaron Chidgey has joined Moreton Eye Group as a vitreoretinal surgeon, bringing more than 20 years’ experience across optometry and ophthalmology. He trained in optometry at Queensland University of Technology and completed his medical degree at the University of Queensland, before undertaking ophthalmology training at Sydney Eye Hospital. Dr Chidgey completed subspecialty vitreoretinal training at Princess Alexandra Hospital in Brisbane and Moorfields Eye Hospital in London. Now based in Brisbane, he works across private practice and public hospitals, with clinical interests including medical retinal disease and complex vitreoretinal surgery.

OPTICARE APPOINTS EXPERIENCED PROFESSIONAL SERVICES MANAGER
Opticare has welcomed Jessica Kingsley as its new professional services manager. Kingsley is an accomplished optometrist with a Master’s degree specialising in sports vision, and brings extensive experience in clinical practice, business development, key account management, and product education. Previously employed at Zeiss, her career provides her with a well-rounded understanding of the optical industry, combining both clinical and commercial expertise.
Meet Dr. Marshall Mrocki
OD BSc (Hons)

From an early age, Marshall Mrocki was captivated by how things worked, whether it was the human body or the mechanics of a device, he would pull apart just to rebuild. That curiosity led him from early aspirations in medicine, through to studies at both Melbourne University and Monash University, and ultimately into optometry: a profession where science, human connection, and hands-on problem-solving collide.
“Helping people see clearly felt like helping them see their future,” Marshall says. “The eye is complex, fascinating—and it shapes how we experience the world.”
Marshall’s career has taken him from retail roles to busy metropolitan practices, and a life-changing move to the Central Coast during the pandemic. But it was by chance, a single message on LinkedIn, that introduced him to George & Matilda Eyecare. What began as a conversation quickly evolved into something far bigger: a long-term pathway to partnership.
“I always wanted to make an impact,” Marshall explains. “Partnership gives me the ability to steer the ship without being overwhelmed by everything happening behind the scenes.”
What Marshall found with G&M was a model tailored for optometrists who want independence while having the support in running a business. This model protects time with patients while easing the administrative burden that can compromise quality care.
Today, as Partner of George & Matilda Eyecare for Optique, Double Bay, and Optometrist of the year in 2025, Marshall is building not only a thriving practice but also deeper community impact—leading dry eye initiatives, introducing IPL therapy, and planning school and aged-care outreach programs.
“It’s the only corporate-style model I know that doesn’t compromise patient-first care,” he says.
“If you want to grow, lead, and truly serve your community, G&M gives you the platform to do it.”

Chris Beer, CEO, Dr Marshall Mrocki, Emma McKeon

